Validation of Large Language Models for Antibiotic Prescribing: Accuracy, Challenges, and Future Directions
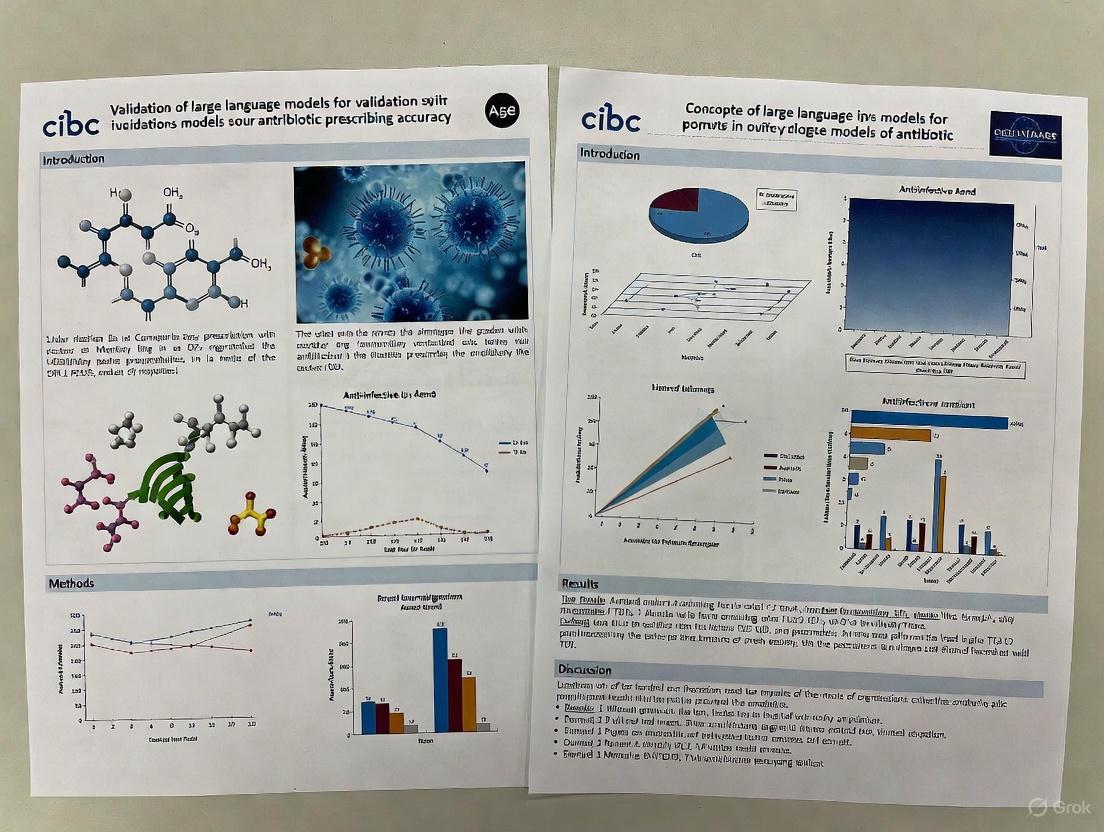
This article comprehensively examines the validation of large language models (LLMs) for antibiotic prescribing accuracy, a critical intersection of artificial intelligence and clinical decision-making.
Validation of Large Language Models for Antibiotic Prescribing: Accuracy, Challenges, and Future Directions
Abstract
This article comprehensively examines the validation of large language models (LLMs) for antibiotic prescribing accuracy, a critical intersection of artificial intelligence and clinical decision-making. Targeted at researchers, scientists, and drug development professionals, it synthesizes current evidence on LLM performance across diverse clinical scenarios, explores methodological approaches for evaluation, identifies significant limitations including variability and hallucinations, and provides comparative analyses of leading models. The analysis reveals substantial performance differences among LLMs, with ChatGPT-o1 demonstrating superior accuracy (71.7% correct recommendations) while other models like Gemini and Claude 3 Opus showed significantly lower performance. The article emphasizes the necessity for standardized validation frameworks, addresses regulatory considerations, and outlines future research directions for safe clinical implementation of LLMs in antimicrobial stewardship.
The Promise and Complexity of LLMs in Antimicrobial Stewardship
LLM Performance in Antibiotic Prescribing: A Comparative Analysis
The integration of Large Language Models (LLMs) into clinical decision-making, particularly for antibiotic prescribing, requires a clear understanding of their relative strengths and weaknesses. Comparative studies reveal significant performance variations across different models, highlighting which LLMs show the most promise for this critical healthcare application.
Comprehensive Model Comparison for Antibiotic Recommendation Accuracy
A 2025 study directly compared 14 LLMs using 60 clinical cases with antibiograms covering 10 infection types. Experts assessed responses for antibiotic appropriateness, dosage correctness, and treatment duration adequacy. The results demonstrate substantial variability in model performance [1].
Table 1: Comparative Performance of LLMs in Antibiotic Prescribing (n=60 clinical cases)
| LLM Model | Antibiotic Choice Accuracy (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) | Incorrect Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Not Specified | 1.7 |
| Perplexity Pro | Not Specified | 90.0 | Not Specified | Not Specified |
| Claude 3.5 Sonnet | Not Specified | 91.7 | Tendency to over-prescribe | Not Specified |
| Gemini | Lowest accuracy | Not Specified | 75.0 (most appropriate) | Not Specified |
| Claude 3 Opus | Lowest accuracy | Not Specified | Not Specified | Not Specified |
This study identified ChatGPT-o1 as the top performer with the highest antibiotic choice accuracy (71.7%) and dosage correctness (96.7%), while Gemini and Claude 3 Opus showed the lowest accuracy. Performance notably declined with increasing case complexity, particularly for infections caused by difficult-to-treat microorganisms [1].
LLMs Versus Human Clinical Performance
Another 2025 study compared the antibiotic prescribing accuracy of six LLMs against general practitioners (GPs) from four countries using 24 clinical vignettes. The study evaluated performance across multiple dimensions including diagnostic accuracy, appropriate antibiotic selection, and adherence to national guidelines [2].
Table 2: LLM vs. General Practitioner Performance in Antibiotic Prescribing
| Performance Metric | General Practitioners (Range) | LLMs (Range) | Top LLM Performers |
|---|---|---|---|
| Diagnostic Accuracy | 96%-100% | 92%-100% | Multiple models |
| Antibiotic Prescribing Decision | 83%-92% | 88%-100% | Multiple models |
| Choice of Antibiotic | 58%-92% (per guidelines) | 59%-100% | Multiple models |
| Correct Referencing of Guidelines | 100% | 38%-96% | Variable by model |
| Dose/Duration Accuracy | 50%-75% | Not Specified | Not Specified |
| Overall Accuracy (Mean) | 74% | Variable | Context-dependent |
While LLMs demonstrated strong performance in diagnosis and antibiotic selection, they struggled with consistent adherence to national guidelines, particularly for Norwegian guidelines (0%-13% correct referencing). The study concluded that while LLMs may safely guide antibiotic prescribing in general practice, GPs remain best placed to interpret complex cases, apply national guidelines, and prescribe correct dosages and durations [2].
Experimental Protocols for LLM Validation in Healthcare
Robust evaluation methodologies are essential for validating LLM performance in clinical settings. Researchers have developed structured approaches to assess LLM capabilities and limitations for antibiotic prescribing support.
Standardized Clinical Case Evaluation Methodology
The comparative study of 14 LLMs employed a rigorous blinded evaluation process with the following key components [1]:
- Case Development: 60 clinical cases covering 10 infection types were developed, each including relevant clinical information and antibiograms.
- Model Prompting: A standardized prompt was used for antibiotic recommendations focusing on drug choice, dosage, and treatment duration.
- Response Anonymization: All LLM responses were anonymized to prevent reviewer bias.
- Expert Evaluation: A blinded expert panel assessed responses for antibiotic appropriateness, dosage correctness, and duration adequacy.
- Analysis: 840 total responses were collected and analyzed for performance patterns.
This methodology enabled direct comparison across models while minimizing evaluation biases, providing a template for future validation studies.
Cross-National Guideline Adherence Assessment
The GP versus LLM comparison study implemented a vignette-based approach with these methodological elements [2]:
- Vignette Design: 24 clinical vignettes included information on infection type, gender, age group, and comorbidities.
- Multi-Country Framework: Four countries (Ireland, UK, USA, and Norway) were included to assess localization capabilities.
- Model Selection: Six LLMs (ChatGPT, Gemini, Copilot, Mistral AI, Claude, and Llama 3.1) were evaluated alongside human GPs.
- Guideline Alignment: Responses were compared against each country's national prescribing guidelines.
- Safety Assessment: Limitations including hallucination, toxicity, and data leakage were systematically evaluated.
This approach highlighted the importance of testing LLMs against localized clinical guidelines rather than assuming generalized medical knowledge would suffice.
Evaluation Workflow
The following diagram illustrates the standardized workflow used in comparative LLM evaluation studies for antibiotic prescribing:
Key Challenges and Limitations in Clinical Implementation
Despite promising performance, several significant challenges must be addressed before LLMs can be safely integrated into antibiotic prescribing workflows.
Technical and Clinical Limitations
Research has identified multiple critical limitations affecting LLM implementation in clinical settings [3] [4] [5]:
- Probabilistic Nature: LLMs operate probabilistically, predicting the next likely token rather than applying clinical reasoning, making them inherently variable even with identical prompts.
- Hallucination Risk: Models may generate plausible but incorrect or fabricated information, with one study finding 2-5% of antibiotic recommendations potentially harmful [5].
- Interpretability Challenges: LLM decision processes are often black boxes, making it difficult to understand the rationale behind specific recommendations.
- Guideline Adherence Inconsistency: Performance varies significantly across different national guidelines, with particular challenges in referencing localized protocols.
- Data Leakage Concerns: Personal information from training data may appear in model responses, creating privacy risks.
Complexity of Antibiotic Decision-Making
Antibiotic prescribing introduces unique challenges that complicate LLM implementation [3] [4]:
- Dual Balancing Requirement: Clinicians must balance optimal individual patient treatment against broader antimicrobial resistance concerns.
- Multifactorial Decision Process: Prescribing decisions incorporate patient-specific variables, local resistance patterns, drug availability, and institutional protocols.
- High-Stakes Consequences: Errors can disproportionately impact either individual patient outcomes or public health resistance patterns.
Essential Research Reagent Solutions for LLM Validation
Conducting robust LLM evaluation requires specific methodological components and assessment tools. The following table outlines key "research reagents" essential for standardized testing in antibiotic prescribing contexts.
Table 3: Essential Research Reagents for LLM Validation Studies
| Research Component | Function | Implementation Examples |
|---|---|---|
| Clinical Vignettes | Standardized test cases representing diverse clinical scenarios | 24-60 cases covering multiple infection types with age, comorbidity, and localization variables [2] [1] |
| National Guidelines | Reference standard for appropriate prescribing | Country-specific antibiotic guidelines from Ireland, UK, USA, Norway [2] |
| Expert Review Panels | Blinded assessment of LLM output quality | Infectious disease specialists evaluating appropriateness, safety, guideline adherence [1] |
| Standardized Prompt Framework | Consistent elicitation of LLM responses | Structured prompts contextualizing clinical scenarios and requested output format [1] [5] |
| Safety Assessment Protocols | Identification of potentially harmful recommendations | Evaluation for hallucination, toxicity, data leakage risks [2] |
| Performance Metrics | Quantitative comparison of model accuracy | Antibiotic choice accuracy, dosage correctness, duration adequacy, guideline adherence rates [1] |
Logical Framework for Clinical Decision Support
The integration of LLMs into antibiotic prescribing follows a structured decision pathway that emphasizes human oversight and validation. The following diagram illustrates this clinical decision support framework:
Current evidence suggests that while LLMs show significant promise in supporting antibiotic prescribing, particularly in straightforward cases, their implementation requires careful validation and human oversight. The substantial performance variability across models highlights the importance of rigorous, standardized testing before clinical deployment.
The most promising path forward involves using advanced LLMs like ChatGPT-o1 as decision-support tools within a human-in-the-loop framework, where clinical expertise validates and contextualizes AI-generated recommendations. This approach leverages LLM strengths in processing complex clinical information while mitigating risks associated with hallucinations, guideline inconsistencies, and dosage inaccuracies.
Future development should focus on improving model consistency with local guidelines, enhancing interpretability of recommendations, and establishing standardized evaluation protocols that can keep pace with rapid advancements in LLM technology. Through continued rigorous validation and appropriate integration frameworks, LLMs have the potential to meaningfully support antimicrobial stewardship efforts while maintaining patient safety as the paramount concern.
Antimicrobial resistance (AMR) represents one of the most severe threats to global public health in the 21st century, already causing an estimated 4.95 million deaths annually and projected to cause 10 million deaths yearly by 2050 if left unaddressed [6]. This crisis is largely driven by antibiotic overuse and misuse, which fuels the selection and propagation of resistant bacterial strains. Within this challenging landscape, healthcare providers face the dual responsibility of delivering effective patient care while minimizing contributions to AMR. Recent advances in artificial intelligence, particularly large language models (LLMs), offer potential solutions through clinical decision support. This guide provides an objective comparison of LLM performance in antibiotic prescribing to inform researchers and drug development professionals about the current state of this emerging technology and its validation framework.
The Evidence Base: Antibiotic Prescribing and Resistance Development
The Prescription-Resistance Relationship
A systematic review and meta-analysis of 24 studies demonstrated that individuals prescribed antibiotics in primary care for respiratory or urinary infections develop bacterial resistance to that antibiotic, with the effect being most pronounced in the month immediately after treatment but potentially persisting for up to 12 months [7]. The pooled odds ratio for resistance was 2.5 within 2 months of antibiotic treatment and 1.33 within 12 months for urinary tract bacteria, indicating a significant temporal relationship [7]. Studies reporting the quantity of antibiotic prescribed found that longer duration and multiple courses were associated with higher rates of resistance, establishing a clear dose-response relationship [7].
The Human Factor: Understanding Prescribing Decisions
Research into prescribing behaviors reveals that knowledge deficits alone do not explain inappropriate antibiotic use. A study of over 2,000 providers in India found that 62% of providers who knew antibiotics were inappropriate for viral childhood diarrhea still prescribed them, creating a significant "know-do gap" [8]. This gap was most sensitive to providers' beliefs about patient preferences rather than profit motives or lack of alternative treatments [8]. This behavioral insight is crucial for developing effective interventions, suggesting that addressing provider misperceptions may be more effective than standard information-based approaches alone.
Comparative Analysis of LLMs for Antibiotic Prescribing
Experimental Protocol and Evaluation Framework
A 2025 comparative study evaluated 14 LLMs using a standardized methodology to assess their performance in antibiotic prescribing [1] [9]. The experimental protocol included:
- Case Development: 60 clinical cases covering 10 infection types with accompanying antibiograms
- Model Selection: Standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai
- Prompt Standardization: A standardized prompt for antibiotic recommendations focusing on drug choice, dosage, and treatment duration
- Blinded Review: Responses were anonymized and assessed by a blinded expert panel
- Evaluation Metrics: Antibiotic appropriateness, dosage correctness, and duration adequacy
This robust methodology provides a framework for ongoing validation of clinical decision support tools in the antimicrobial stewardship domain.
Quantitative Performance Comparison
Table 1: Overall Prescribing Accuracy Across LLMs
| Large Language Model | Overall Correct Prescriptions | Incorrect Prescriptions | Dosage Correctness | Duration Adequacy |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 1.7% (1/60) | 96.7% (58/60) | Not specified |
| Perplexity Pro | Not specified | Not specified | 90.0% (54/60) | Not specified |
| Claude 3.5 Sonnet | Not specified | Not specified | 91.7% (55/60) | Tendency to over-prescribe |
| Gemini | Lowest accuracy | Not specified | Not specified | 75.0% (45/60) |
| Claude 3 Opus | Lowest accuracy | Not specified | Not specified | Not specified |
Table 2: Performance Across Case Complexity
| Performance Metric | Simple Cases | Complex Cases | Difficult-to-Treat Microorganisms |
|---|---|---|---|
| Prescribing Accuracy | Higher | Significantly declined | Notable decrease in performance |
| Dosage Correctness | Maintained | Reduced | More variable |
| Duration Adequacy | More appropriate | Less appropriate | Higher rate of deviation from guidelines |
The data reveal significant variability among LLMs in prescribing appropriate antibiotics, dosages, and treatment durations [1]. ChatGPT-o1 demonstrated superior performance in overall antibiotic appropriateness and dosage correctness, while models like Claude 3.5 Sonnet showed tendencies to over-prescribe treatment duration [9]. Performance degradation with increasing case complexity was observed across all models, highlighting a significant limitation in current LLM capabilities for handling complicated clinical scenarios [1].
Research Reagents and Experimental Tools
Table 3: Essential Research Materials for LLM Validation Studies
| Research Tool | Function/Application | Example from Cited Studies |
|---|---|---|
| Clinical Case Repository | Standardized patient scenarios for consistent model evaluation across diverse conditions | 60 cases covering 10 infection types with antibiograms |
| Antibiogram Data | Local resistance patterns to inform appropriate antibiotic selection | Institution-specific susceptibility profiles |
| Expert Review Panel | Blinded assessment of model recommendations against standard care guidelines | Infectious disease specialists for response evaluation |
| Standardized Prompt Framework | Consistent input format to reduce variability in model responses | Structured prompts for drug, dose, duration requests |
| Validation Metrics Suite | Quantitative assessment of prescription appropriateness, dosage, and duration | Correct/incorrect classification with expert consensus |
Visualization of Research Framework
Research Workflow for LLM Validation
Factors Influencing Antibiotic Prescribing
The validation of large language models for antibiotic prescribing represents a promising frontier in clinical decision support and antimicrobial stewardship. Current evidence indicates significant variability in performance across different LLMs, with ChatGPT-o1 demonstrating the highest accuracy in antibiotic prescriptions at 71.7% [1]. However, the degradation of performance in complex cases and with difficult-to-treat microorganisms highlights the need for continued refinement and validation before clinical implementation [9]. For researchers and drug development professionals, these findings underscore both the potential and limitations of current AI technologies in addressing the dual challenge of antibiotic prescribing. Future research directions should focus on enhancing model performance in complex clinical scenarios, improving integration with local resistance data, and developing more sophisticated evaluation frameworks that account for the nuanced decision-making required in antimicrobial stewardship.
Current Landscape of AI Decision Support in Infectious Diseases
The application of Artificial Intelligence (AI), particularly large language models (LLMs), in infectious diseases represents a paradigm shift in clinical decision support and medical education. These tools offer the potential to enhance diagnostic accuracy, optimize antimicrobial therapy, and support stewardship programs [10] [11]. However, significant variability exists in their performance across different clinical scenarios and domains of infectious disease management. This guide provides an objective comparison of leading AI systems' capabilities, with a specific focus on validating their accuracy for antibiotic prescribing—a task requiring precise clinical reasoning with significant implications for patient outcomes and antimicrobial resistance [12] [11].
Performance Comparison of AI Models
Accuracy Across Infectious Disease Domains
Table 1: Performance Comparison of AI Models on Infectious Disease Questions
| AI Model | Overall Accuracy (%) | Diagnostic Accuracy (%) | Therapy-Related Question Accuracy (%) | Response Consistency | Key Strengths | Major Limitations |
|---|---|---|---|---|---|---|
| ChatGPT 3.5 | 65.6 [13] | 79.1 [13] | 56.6 [13] | 7.5% accuracy decline in repeat testing [13] | Strong diagnostic accuracy [13] | Significant drop in antimicrobial treatment recommendations [13] |
| ChatGPT-o1 | 71.7 (antibiotic prescribing) [1] | Information Missing | Information Missing | Information Missing | Highest antibiotic prescription accuracy; 96.7% dosage correctness [1] | Information Missing |
| Perplexity AI | 63.2 [13] | Information Missing | Information Missing | Information Missing | Information Missing | Struggled with individualized treatment recommendations [13] |
| Microsoft Copilot | 60.9 [13] | Information Missing | Information Missing | Most stable responses across repeated testing [13] | Response stability [13] | Lacked nuanced therapeutic reasoning [13] |
| Meta AI | 60.8 [13] | Information Missing | Information Missing | Information Missing | Information Missing | Variability in drug selection and dosing adjustments [13] |
| Google Bard (Gemini) | 58.8 [13] | Information Missing | 75.0% appropriate treatment duration (highest) [1] | Inconsistent in microorganism identification (61.9%) and preventive therapy (62.5%) [13] | Information Missing | Lowest accuracy in antibiotic prescribing [1] |
Performance in Specific Clinical Applications
Table 2: Specialized AI Performance in Clinical Scenarios
| Application / Model | Performance Metrics | Context & Limitations |
|---|---|---|
| OneChoice AI CDSS | 74.59% concordance for top recommendation; 96.14% for any suggested treatment; κ = 0.70 [14] | Retrospective evaluation for bacteremia treatment; higher concordance with ID specialists (κ = 0.78) vs. non-specialists (κ = 0.61) [14] |
| LAMO Framework | >10% improvement over existing methods; strong generalization in temporal/ external validation [15] | Addresses LLM overprescription tendency; maintains accuracy with out-of-distribution medications [15] |
| CarbaDetector | 97.8% sensitivity; 56.6% specificity [16] | Predicts carbapenemase-producing Enterobacterales from disk-diffusion results [16] |
| AI-Augmented MALDI-TOF | Strong accuracy for common pathogens [16] | Strain typing when paired with high-resolution genomic data [16] |
Experimental Protocols and Methodologies
Standardized Evaluation of General-Purpose LLMs
A systematic comparative study evaluated five major AI platforms using 20 infectious disease case studies from "Infectious Diseases: A Case Study Approach" by Jonathan C. Cho, totaling 160 multiple-choice questions (MCQs) [13]. The methodology was designed to ensure standardized assessment across models:
- Case Selection: Covered four infection groups: respiratory and ENT infections; systemic, central nervous system, and immunocompromised infections; musculoskeletal and soft tissue infections; and genitourinary infections [13].
- Standardized Prompting: Each AI platform received identical prompts containing the complete case study text and MCQs without additional context or instructions [13].
- Evaluation Framework: Responses were compared against a reference answer key from the textbook. Accuracy was measured by the percentage of correct responses [13].
- Consistency Assessment: Identical prompts were submitted 24 hours apart to evaluate response stability over time [13].
- Performance Categorization: Questions were categorized by clinical domain (symptom identification, microorganism identification, diagnostic methods, therapy, preventive therapy) to identify specific strengths and weaknesses [13].
Specialized Antibiotic Prescribing Evaluation
A comprehensive study assessed 14 LLMs (including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai) using 60 clinical cases with antibiograms covering 10 infection types [1] [9]. The methodology included:
- Case Complexity Stratification: Cases covered diverse infection types and included difficult-to-treat microorganisms to evaluate performance across complexity levels [1].
- Standardized Prompting: A uniform prompt structure focused on antibiotic recommendations including drug choice, dosage, and treatment duration [1] [9].
- Blinded Expert Review: Responses were anonymized and assessed by a blinded expert panel evaluating antibiotic appropriateness, dosage correctness, and duration adequacy [1].
- Harm Evaluation: Recommendations were classified for potential harmfulness, with specific assessment of errors that could lead to clinical adverse events [12].
Real-World Clinical Validation
The OneChoice AI clinical decision support system was evaluated in a real-world setting in Lima, Peru, using a retrospective, observational design [14]:
- Data Integration: The system incorporated molecular (FilmArray) and phenotypic (MALDI-TOF MS, VITEK2) data to generate therapeutic recommendations for bloodstream infections [14].
- Physician Comparison: Recommendations were compared against decisions of 94 physicians (35 infectious disease specialists and 59 non-specialists) across 366 survey-based evaluations of bacteremia cases [14].
- Concordance Metrics: Agreement was analyzed using Cohen's Kappa and logistic regression, with specialization as a predictor of agreement [14].
- Antimicrobial Stewardship Impact: The system's effect on reducing inappropriate antibiotic use, particularly unnecessary carbapenem prescriptions, was assessed [14].
Technical Approaches and Architectures
The LAMO Framework for Medication Recommendation
The Language-Assisted Medication recOmmendation (LAMO) framework addresses critical limitations in general LLMs for clinical applications, particularly their tendency toward overprescription [15]. The technical architecture includes:
- Structured EHR Representation: Extracts and summarizes key clinical factors from raw discharge summaries into four core components: History of Present Illness, Past Medical History, Allergies, and Medications on Admission [15].
- Parameter-Efficient Fine-Tuning: Employs Low-Rank Adaptation (LoRA) to tailor LLMs for medication recommendation with limited computational overhead [15].
- Mixture-of-Expert Strategy: Uses different LoRA adapters for different medicine groups to overcome overprescription while controlling computation overhead [15].
- Instruction Tuning: Formulates training instances using an instruction-based format where the model processes structured clinical context and a candidate medication to generate a binary prescription decision [15].
Essential Research Reagents and Tools
Table 3: Research Reagent Solutions for AI Validation in Infectious Diseases
| Tool / Resource | Function | Application Context |
|---|---|---|
| Infectious Diseases: A Case Study Approach (Cho, 2020) | Standardized case library with 20 clinical cases and 160 MCQs [13] | Benchmarking AI performance across diverse infectious disease scenarios [13] |
| MIMIC-III & MIMIC-IV Databases | Publicly available critical care databases with de-identified health data [15] | Training and validation of medication recommendation systems [15] |
| CarbaDetector | Web-based ML tool predicting carbapenemase production [16] | Rapid detection of antimicrobial resistance from basic disk-diffusion results [16] |
| FilmArray | Molecular diagnostic system for pathogen identification [14] | Input data for AI-based clinical decision support systems [14] |
| MALDI-TOF MS | Mass spectrometry for microbial identification [14] [16] | Bacterial strain identification; can be augmented with AI for enhanced typing [16] |
| VITEK2 | Automated system for antimicrobial susceptibility testing [14] | Phenotypic data generation for AI-assisted treatment recommendations [14] |
| PrimeKG | Comprehensive biomedical knowledge graph [15] | Evaluating LLMs' understanding of disease-medication relationships [15] |
| eICU Collaborative Research Database | Multi-center ICU database with diverse patient populations [15] | External validation of AI model generalizability [15] |
The current landscape of AI decision support in infectious diseases reveals a rapidly evolving field with significant potential but notable limitations. Advanced models like ChatGPT-o1 demonstrate promising accuracy in antibiotic prescribing (71.7% appropriate recommendations), while specialized frameworks like LAMO address critical issues such as overprescription and show strong generalization capabilities [1] [15]. However, performance consistently declines with case complexity, and significant variability exists across models and clinical domains [13] [1]. The most successful implementations combine AI capabilities with human expertise, leveraging the strengths of both systems [14] [16]. Future development should focus on enhancing performance in complex cases, improving consistency, and ensuring robust real-world validation through clinical trials and assessment of long-term stability [13] [11]. For researchers and drug development professionals, these findings underscore both the transformative potential and current limitations of AI in antimicrobial stewardship and infectious disease management.
Large language models (LLMs) demonstrate transformative potential in antibiotic prescribing research, primarily through their rapid information processing and sophisticated synthesis of complex clinical data. Comparative studies reveal significant performance variability among models, with advanced systems like ChatGPT-o1 achieving 71.7% accuracy in appropriate antibiotic selection and 96.7% dosage correctness across diverse clinical scenarios [1] [9]. These capabilities position LLMs as powerful decision-support tools, though performance degradation in complex cases and persistent hallucination risks necessitate rigorous validation frameworks before clinical implementation [12] [17]. This analysis examines the experimental evidence quantifying these advantages and the methodological approaches required for reliable assessment in antimicrobial stewardship research.
Comparative Performance Metrics in Antibiotic Prescribing
Table 1: Comprehensive LLM Performance Across Antibiotic Prescribing Tasks
| LLM Model | Antibiotic Choice Accuracy (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) | Key Strengths | Notable Limitations |
|---|---|---|---|---|---|
| ChatGPT-o1 | 71.7 (43/60 cases) [1] | 96.7 (58/60) [1] | Not specified | Highest overall prescribing accuracy; Optimal dosage recommendations | Limited data on duration adequacy |
| ChatGPT-4 | 64 (empirical therapy) [12] | ~90 (when correct antibiotic suggested) [12] | Not specified | Consistent responses across sessions [12] | 36% appropriateness for targeted therapy [12] |
| Perplexity Pro | Not specified | 90.0 (54/60) [1] | Not specified | High dosage accuracy | Limited comprehensive prescribing data |
| Claude 3.5 Sonnet | Not specified | 91.7 (55/60) [1] | Tendency to over-prescribe duration [1] | Strong dosage performance | Duration optimization challenges |
| Gemini | Lowest accuracy [1] | Not specified | 75.0 (45/60) [1] | Most appropriate duration recommendations | Poor antibiotic selection accuracy |
| General LLM Performance | 64-36% (empirical vs. targeted) [12] | 38% correct type, ~90% correct dosage when type appropriate [12] | 81% recognized need for rapid administration [12] | Speed and accessibility | Declining performance with case complexity [1] |
Table 2: Specialized vs. General LLM Architectures for Clinical Applications
| Model Type | Representative System | Key Architectural Features | Safety & Validation Mechanisms | Reported Performance Advantages |
|---|---|---|---|---|
| Safety-Constrained Hybrid Framework | CLIN-LLM [18] | Integration of BioBERT fine-tuning with Monte Carlo Dropout; Retrieval-augmented generation (RAG) | Uncertainty-calibrated predictions flag 18% cases for expert review; Antibiotic stewardship rules & DDI screening | 98% accuracy in symptom-to-disease classification; 67% reduction in unsafe antibiotic suggestions vs. GPT-5 [18] |
| Untrained General LLM | ChatGPT-3.5 [19] | Standard transformer architecture without clinical fine-tuning | Basic prompt conditioning without specialized safety filters | 4.07/5 accuracy for common pediatric infections; Highest performance in guideline-clear scenarios [19] |
| Internet-Enabled LLMs | Microsoft Copilot, Perplexity AI [20] | Real-time data access alongside pre-trained knowledge | Continuous updates from current sources | Most stable responses across repeated testing [20]; Improved factuality with real-time retrieval [18] |
Experimental Protocols for LLM Validation in Antimicrobial Stewardship
Standardized Clinical Case Evaluation Methodology
The predominant experimental approach for assessing LLM prescribing capabilities employs standardized clinical cases with comprehensive patient data, including medical history, presentation, laboratory results, and local antibiograms [1] [12]. In the landmark comparative study evaluating 14 LLMs:
- Case Development: Researchers utilized 60 clinical cases spanning 10 infection types with accompanying antibiograms to reflect real-world clinical diversity [1]
- Prompt Standardization: A uniform prompt structure requested antibiotic recommendations focusing on drug selection, dosage, and treatment duration [1] [9]
- Blinded Expert Review: Responses were anonymized and evaluated by infectious disease specialists assessing antibiotic appropriateness, dosage correctness, and duration adequacy [1]
- Harm Classification: Some protocols additionally categorized recommendations as "potentially harmful" versus "not harmful" based on guideline deviations and patient risk [12]
Retrieval-Augmented Generation (RAG) Implementation
Advanced frameworks like CLIN-LLM implement evidence-grounded generation to enhance safety and accuracy [18]:
- Semantic Retrieval: Biomedical Sentence-BERT retrieves top-k relevant dialogues from the MedDialog corpus (260,000 samples) [18]
- Contextual Generation: Retrieved evidence and patient context feed into a fine-tuned FLAN-T5 model for personalized treatment generation [18]
- Post-processing Safety Filters: RxNorm API integration enables drug-drug interaction screening and antibiotic stewardship rule enforcement [18]
Uncertainty Quantification Protocols
Safety-constrained frameworks incorporate confidence calibration to identify ambiguous cases requiring human oversight [18]:
- Monte Carlo Dropout: Multiple stochastic forward passes during inference generate prediction uncertainty estimates [18]
- Focal Loss Integration: Handles class imbalance for rare diseases during BioBERT fine-tuning on 1,200 clinical cases [18]
- Triage Thresholding: Low-certainty predictions (18% of cases) are automatically flagged for expert review [18]
Experimental Workflow for LLM Validation in Antibiotic Prescribing
LLM Validation Workflow: This diagram illustrates the standardized experimental methodology for evaluating LLM performance in antibiotic prescribing, from case development through safety assessment.
Table 3: Critical Research Components for LLM Antibiotic Prescribing Studies
| Resource Category | Specific Examples | Research Function | Implementation Considerations |
|---|---|---|---|
| Clinical Datasets | Symptom2Disease dataset (1,200 cases) [18]; MedDialog corpus (260,000 samples) [18] | Model fine-tuning and retrieval-augmented generation | Dataset licensing; Patient privacy compliance; Clinical representativeness |
| Evaluation Frameworks | Blinded expert panel review [1]; IDSA/ESCMID guideline adherence assessment [12] | Objective performance benchmarking | Inter-rater reliability; Guideline version control; Specialty diversity in panel |
| Safety Validation Tools | RxNorm API [18]; Monte Carlo Dropout [18]; Antibiotic stewardship rule engines [18] | Harm reduction and error prevention | Integration complexity; Computational overhead; Rule set comprehensiveness |
| LLM Architectures | BioBERT [18]; FLAN-T5 [18]; Transformer-based models [12] | Core model capabilities and performance | Computational requirements; Licensing restrictions; Architecture customization needs |
| Statistical Methods | Focal Loss for class imbalance [18]; Confidence calibration metrics [18] | Robust performance assessment | Statistical expertise requirements; Interpretation complexity; Validation methodologies |
Interpretation of Performance Variability and Research Implications
The significant performance differentials observed across LLMs—from ChatGPT-o1's 71.7% accuracy to Gemini's lowest performance [1]—stem from fundamental architectural and training differences. Several factors explain this variability:
- Model Scale and Architecture: Larger parameter counts and specialized attention mechanisms enhance contextual understanding of complex clinical scenarios [12]
- Training Data Curation: Medical-domain specific pre-training (e.g., on clinical notes, guidelines) improves pharmacological reasoning [18]
- Retrieval Integration: Systems incorporating real-time evidence retrieval demonstrate improved factuality and reduced hallucinations [18]
- Uncertainty Awareness: Frameworks with calibrated confidence estimates enable appropriate human-in-the-loop safeguards [18]
For research applications, these findings underscore that processing speed and information synthesis capabilities must be balanced against accuracy and safety requirements. While general LLMs provide accessible starting points, specialized clinical frameworks like CLIN-LLM demonstrate how targeted architectural innovations can address critical limitations for antibiotic prescribing applications [18].
The progression toward human-in-the-loop systems that leverage LLM advantages while mitigating risks through uncertainty quantification and expert oversight represents the most promising research direction [17] [18]. Future validation studies should prioritize standardized evaluation metrics across diverse clinical scenarios to establish definitive performance benchmarks for research and potential clinical implementation.
The validation of Large Language Models (LLMs) for antibiotic prescribing is a critical frontier in clinical AI research. A core challenge lies in addressing their fundamental limitations: the black-box nature of their decision-making processes and their inherent probabilistic outputs. These characteristics directly impact the reliability, safety, and interpretability of model-generated recommendations, posing significant hurdles for clinical deployment [21] [22].
Comparative Performance of LLMs in Antibiotic Prescribing
Recent comparative studies reveal significant variability in the performance of different LLMs on the complex task of antibiotic prescribing. The table below summarizes quantitative data from an evaluation of 14 LLMs across 60 clinical cases [1] [9].
Table 1: Performance of LLMs on Antibiotic Prescribing Accuracy
| Large Language Model | Prescription Accuracy (%) | Dosage Correctness (%) | Duration Adequacy (%) | Incorrect Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information Missing | 1.7 |
| Claude 3.5 Sonnet | Information Missing | 91.7 | Tended to over-prescribe | Information Missing |
| Perplexity Pro | Information Missing | 90.0 | Information Missing | Information Missing |
| Gemini | Lowest Accuracy | Information Missing | 75.0 | Information Missing |
| Claude 3 Opus | Lowest Accuracy | Information Missing | Information Missing | Information Missing |
Key findings from this comparative analysis include:
- Performance Variability: A significant performance gap exists between the most accurate model (ChatGPT-o1) and the lowest-performing models (Gemini and Claude 3 Opus) [1] [9].
- Complexity Impact: Model accuracy declined with increasing case complexity, particularly for infections involving difficult-to-treat microorganisms [1].
- Component Inconsistency: Models demonstrated inconsistent performance across different components of prescribing (drug choice, dosage, duration), with no single model excelling in all areas [1].
Experimental Protocols for Validating LLM Performance
To generate the comparative data presented, researchers implemented a structured experimental methodology focused on clinical realism and rigorous assessment [1] [9].
Clinical Case Design and Model Prompting
The evaluation framework utilized 60 clinical cases covering 10 different infection types. Each case was accompanied by antibiograms (antimicrobial susceptibility test results) to reflect real-world clinical decision-making. Researchers employed a standardized prompt to query each LLM, requesting antibiotic recommendations that included specific details on drug choice, dosage, and treatment duration [1].
Blinded Expert Evaluation and Metrics
A critical component of the protocol was the implementation of a blinded review process. An expert panel assessed the anonymized LLM responses without knowledge of the model source. They evaluated recommendations based on three key metrics [1]:
- Antibiotic Appropriateness: Alignment with clinical guidelines and susceptibility data.
- Dosage Correctness: Accuracy of drug dosing based on patient-specific factors.
- Duration Adequacy: Appropriate length of treatment according to standard protocols.
This process yielded 840 total responses for analysis, providing a substantial dataset for comparative evaluation [1].
The Scientist's Toolkit: Research Reagent Solutions
Research into LLM limitations requires specialized "reagent" solutions to enable rigorous experimentation. The table below details key resources mentioned in the surveyed literature.
Table 2: Essential Research Materials for LLM Validation Studies
| Research Reagent | Function in Experimental Protocol |
|---|---|
| mARC-QA Benchmark | A specialized dataset designed to probe LLM failure modes in clinical reasoning by presenting scenarios that resist pattern-matching and require flexible problem-solving [23]. |
| Clinical Case Repository | A curated collection of real or simulated patient cases covering diverse infection types and complexities, serving as the input for model evaluation [1]. |
| Antibiogram Data | Local or standard antimicrobial susceptibility profiles essential for assessing whether LLM recommendations align with proven microbial resistance patterns [1]. |
| Standardized Prompt Framework | Consistent query structures and instructions used across all model evaluations to ensure comparability and reduce variability from prompt engineering [1]. |
| Blinded Expert Panel | Clinical specialists who provide gold-standard assessments of model outputs without knowledge of the source, minimizing evaluation bias [1]. |
Visualizing LLM Limitations in Clinical Reasoning
The following diagrams, generated using Graphviz, illustrate the core limitations of LLMs in clinical settings, focusing on their black-box nature and probabilistic outputs.
Diagram 1: The Black-Box Clinical Decision Process
This diagram visualizes the black-box problem in LLM clinical decision-making. While inputs (clinical data) and outputs (prescribing recommendations) are well-defined, the internal processing remains opaque. This lack of transparency creates challenges for validating the clinical reasoning behind model outputs [21] [22].
Diagram 2: Probabilistic Outputs and Uncertainty in Prescribing
This diagram illustrates how LLMs generate probabilistic outputs for clinical recommendations. The model assigns confidence probabilities to different antibiotic options, yet research shows these confidence estimates are often miscalibrated, with models exhibiting overconfidence in their recommendations despite limited accuracy [23] [1].
Research Implications and Future Directions
The evidence demonstrates that the black-box nature and probabilistic outputs of LLMs represent fundamental limitations for antibiotic prescribing validation. Key research implications include:
- Interpretability Tools: There is a critical need for enhanced explainable AI (XAI) techniques to make LLM decisions more transparent and understandable for clinical validation [22].
- Uncertainty Quantification: Developing better methods for LLMs to communicate uncertainty in their recommendations is essential for clinical safety [23].
- Rigorous Clinical Validation: Before deployment, LLMs require thorough testing across diverse clinical scenarios and populations to identify failure modes and ensure reliability [23] [1].
These limitations underscore that while LLMs show promise as clinical decision-support tools, they currently function as probabilistic assistants rather than deterministic experts, necessitating careful human oversight and rigorous validation frameworks [24] [21].
Training Data Quality and Transparency Concerns in Proprietary Models
The validation of Large Language Models (LLMs) for antibiotic prescribing accuracy sits at the intersection of cutting-edge artificial intelligence and rigorous clinical science. For researchers and drug development professionals, understanding the performance of these models is not merely an academic exercise but a prerequisite for their safe and effective integration into healthcare. A model's output is fundamentally shaped by the quality and composition of its training data and the transparency of its development. Concerns around these factors are paramount, as "LLMs are considered 'black box' models because the composition and computations of features within the initial (input) layer and the final (output) layer may be partly or sometimes totally unclear" [12]. This opacity is compounded by the industry’s practice of maintaining proprietary control, which limits access to underlying algorithms and training data [25]. This article provides a comparative analysis of proprietary LLMs, focusing on their performance in antibiotic prescribing and examining how data quality and transparency concerns underlie their functional capabilities and limitations.
Comparative Performance of LLMs in Antibiotic Prescribing
Objective, comparative evaluations are essential to cut through the hype surrounding LLMs. Independent studies have begun to benchmark these models on complex clinical tasks like antibiotic prescribing, revealing significant performance variations.
Key Experimental Findings in Antimicrobial Stewardship
A 2025 comparative study assessed 14 LLMs using 60 clinical cases with antibiograms covering 10 infection types. A blinded expert panel evaluated 840 responses for antibiotic appropriateness, dosage correctness, and treatment duration adequacy [1]. The results, summarized in the table below, provide a critical snapshot of current capabilities.
Table 1: Comparative Performance of LLMs on Antibiotic Prescribing Tasks [1]
| Large Language Model | Overall Antibiotic Prescription Accuracy (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) | Notes on Performance |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information missing | Highest overall accuracy; only one (1.7%) incorrect recommendation. |
| Perplexity Pro | Information missing | 90.0 | Information missing | Followed ChatGPT-o1 in dosage correctness. |
| Claude 3.5 Sonnet | Information missing | 91.7 | Information missing | Tended to over-prescribe treatment duration. |
| Gemini | Lowest accuracy | Information missing | 75.0 | Provided the most appropriate treatment duration recommendations. |
| Claude 3 Opus | Lowest accuracy | Information missing | Information missing | Demonstrated low prescription accuracy. |
The study concluded that while advanced LLMs like ChatGPT-o1 show promise as decision-support tools, their performance declines with increasing case complexity, particularly for difficult-to-treat microorganisms [1]. This performance drop in complex scenarios highlights the potential limitations of their training data in covering clinical edge cases and the "black box" nature that makes these limitations difficult to anticipate.
Other studies corroborate this variability. When evaluating LLM management of a pneumococcal meningitis case, the need for rapid antibiotic administration was correctly recognized in 81% of instances, but the correct type of empirical antibiotics was suggested only 38% of the time [12]. This gap between general clinical reasoning and precise therapeutic knowledge is telling.
Beyond Accuracy: Risks of Bias and Hallucination
Performance metrics alone are insufficient. For clinical deployment, understanding associated risks is critical. A significant concern is the potential for biases and hallucinations in model outputs. For instance, assessments and plans generated by ChatGPT have been linked to recommendations for more expensive procedures, which could exacerbate healthcare disparities and costs [25]. Furthermore, clinical documentation produced by LLMs can influence clinician decision-making through anchoring and automation biases, potentially leading to unintended harm [25]. These issues often originate from the training data; if the data lacks diversity, contains societal biases, or is not representative of real-world clinical scenarios, the model will inevitably learn and perpetuate these flaws [26].
The Root Cause: Data Quality and Transparency Gaps
The performance variations and risks described above are not arbitrary. They are direct consequences of underlying issues in training data quality and a pervasive lack of transparency in proprietary model development.
The Data Provenance Problem
A core challenge is the poor documentation and understanding of AI training datasets. These datasets are often "inconsistently documented and poorly understood, opening the door to a litany of risks," including legal and copyright issues, exposure of sensitive information, and unintended biases [27]. An audit of over 1,800 text datasets found that licenses were frequently miscategorized, with error rates greater than 50% and license information omission rates of over 70% [27]. This lack of clear provenance creates a foundation of uncertainty upon which clinical tools are being built.
Table 2: Common Pitfalls of Poor Data Readiness and Their Impacts [27] [26]
| Data Quality Pitfall | Description | Potential Impact on LLM Performance |
|---|---|---|
| Bias and Inaccuracy | Training data is biased, incomplete, or flawed. | Produces skewed outcomes, amplifies stereotypes, and leads to unreliable clinical recommendations. |
| Lack of Statistical Representation | Datasets fail to represent real-world demographic or clinical distributions. | Results in model underperformance on underrepresented populations or rare medical conditions. |
| Poor Generalization | Models are overfitted to limited datasets. | Performs well on familiar patterns but fails when faced with new or complex clinical scenarios. |
| Data Silos and Integration Challenges | Fragmented, incompatible data sources from different systems or departments. | Hinders model integration, delays training, and creates inconsistencies in data interpretation. |
| Temporal Relevance and Drift | Models are trained on historical data that doesn't capture emerging patterns. | Leads to outdated recommendations that do not reflect current medical guidelines or resistance patterns. |
The Transparency Deficit in Proprietary Models
The "black box" problem is multifaceted, arising from both a model's intrinsic complexity and developer practices that limit scrutiny [25]. A comprehensive analysis of state-of-the-art LLMs reveals a spectrum of transparency, where even models labeled as "open-source" often fail to report critical details like training data, code, and key metrics such as carbon emissions [28]. This "open-washing" limits the ability of researchers to verify capabilities, identify biases, and adapt models for specific domains like healthcare [28]. The lack of data cards, model cards, and bias cards for many popular commercial LLMs makes it profoundly difficult for clinicians and researchers to anticipate risks compared to open-source models that provide more information about their model weights and training methodologies [25].
Research Toolkit for LLM Validation in Antimicrobial Stewardship
For researchers validating LLMs for clinical use, a rigorous methodological approach is non-negotiable. The following experimental protocols and resources are essential for generating credible, actionable evidence.
Experimental Protocols for Benchmarking LLMs
The studies cited in this guide employed structured methodologies that can be adapted and built upon by other research groups.
Table 3: Essential Research Reagents and Methodologies for LLM Validation
| Item / Protocol | Function in Validation | Example from Cited Research |
|---|---|---|
| Curated Clinical Case Bank | Provides standardized, clinically-vetted scenarios for testing model performance across a range of conditions and complexities. | 60 clinical cases with antibiograms covering 10 infection types [1]. A retrospective case series of 44 bloodstream infections (BSIs) [12]. |
| Standardized Prompting Framework | Ensures consistency in how questions are posed to LLMs, reducing variability not attributable to the model's core capabilities. | A standardized prompt was used for antibiotic recommendations, focusing on drug choice, dosage, and duration [1]. Prompts were formulated exactly as the original questions from clinical guidelines [12]. |
| Blinded Expert Panel Review | Serves as the gold standard for evaluating the appropriateness, safety, and adequacy of LLM-generated recommendations. | Responses were anonymized and reviewed by a blinded expert panel [1]. Suggestions were classified by infectious diseases specialists not involved in the patient's care [12]. |
| Clinical Practice Guidelines | Provides an objective, community-accepted benchmark against which to judge the correctness of LLM outputs. | Recommendations were evaluated for adherence to IDSA and ESCMID guidelines [12] and local/international guidelines [1]. |
| Harm Classification Taxonomy | Allows for the critical categorization of potential patient risks associated with incorrect model recommendations. | Recommendations were classified as "potentially harmful for patients vs. not harmful" [12]. |
A Workflow for Rigorous LLM Validation
The following diagram outlines a systematic workflow for validating an LLM for antibiotic prescribing, incorporating the key methodologies described above.
The journey toward reliably using LLMs in antibiotic prescribing and other high-stakes clinical domains is underway. Comparative studies clearly demonstrate that while the most advanced models show significant promise, they are not infallible. Performance is variable, and accuracy can decline precipitously in complex cases. These functional limitations are symptoms of more profound issues: a widespread deficit of training data quality and model transparency. The "black box" nature of proprietary models, coupled with poorly documented and potentially biased training data, makes it difficult for researchers to fully assess, trust, or validate these tools. Therefore, the onus is on the research community to demand greater transparency and to employ rigorous, standardized validation protocols—like those outlined here—to ensure that the integration of LLMs into healthcare ultimately enhances, rather than compromises, patient safety and care quality.
Evaluating LLM Performance: Metrics, Scenarios, and Clinical Integration
Standardized Evaluation Frameworks for Clinical Decision Support
The integration of Large Language Models (LLMs) and other artificial intelligence (AI) technologies into Clinical Decision Support (CDS) systems presents a transformative opportunity for healthcare, particularly in complex domains such as antibiotic prescribing. However, their potential to improve patient outcomes and combat antimicrobial resistance is contingent upon rigorous, standardized evaluation to ensure their safety, reliability, and effectiveness. The significant variability in performance observed among different AI models underscores the critical need for comprehensive evaluation frameworks that can be consistently applied by researchers and clinicians [9] [12]. This guide compares current evaluation methodologies and performance data for AI-based CDS, with a specific focus on validating LLMs for antibiotic prescribing accuracy.
Comparative Performance of AI Models in Infectious Diseases
Performance of Large Language Models in Antibiotic Prescribing
A 2025 comparative study evaluated 14 different LLMs using 60 clinical cases with antibiograms covering ten infection types. The models generated 840 responses, which were anonymized and reviewed by a blinded expert panel for antibiotic appropriateness, dosage correctness, and duration adequacy [9] [1].
Table 1: Comparative Performance of LLMs in Antibiotic Prescribing (n=60 cases)
| Large Language Model | Prescription Accuracy (%) | Dosage Correctness (%) | Duration Adequacy (%) | Incorrect Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information missing | 1.7 |
| Perplexity Pro | Information missing | 90.0 | Information missing | Information missing |
| Claude 3.5 Sonnet | Information missing | 91.7 | Information missing | Information missing |
| Gemini | Lowest accuracy | Information missing | 75.0 (Most appropriate) | Information missing |
| Claude 3 Opus | Lowest accuracy | Information missing | Information missing | Information missing |
The study revealed critical insights: performance declined with increasing case complexity, particularly for difficult-to-treat microorganisms. ChatGPT-o1 demonstrated the highest overall accuracy, while Gemini and Claude 3 Opus showed the lowest accuracy among the models tested [9]. In treatment duration, Gemini provided the most appropriate recommendations, whereas Claude 3.5 Sonnet tended to over-prescribe duration [9].
Performance in Infectious Disease Education and Knowledge Assessment
A separate comparative analysis evaluated AI platforms on 160 infectious disease multiple-choice questions (MCQs) derived from 20 case studies [20].
Table 2: AI Performance on Infectious Disease Multiple-Choice Questions (n=160 questions)
| AI Model | Overall Accuracy (%) | Diagnostic Accuracy (%) | Therapy/Antimicrobial Recommendation Accuracy (%) | Consistency Notes |
|---|---|---|---|---|
| ChatGPT 3.5 | 65.6 | 79.1 | 56.6 | 7.5% accuracy decline upon repeated testing |
| Perplexity AI | 63.2 | Information missing | Information missing | Information missing |
| Microsoft Copilot | 60.9 | Information missing | Information missing | Most stable responses across repeated testing |
| Meta AI | 60.8 | Information missing | Information missing | Information missing |
| Google Bard (Gemini) | 58.8 | Information missing | Information missing | Inconsistent in microorganism identification (61.9%) and preventive therapy (62.5%) |
The models performed best in symptom identification (76.5% accuracy) and worst in therapy-related questions (57.1% accuracy) [20]. This performance gap highlights a critical challenge: while AI models can assist with diagnostic tasks, their utility in guiding complex treatment decisions, especially antimicrobial selection, requires further development and validation.
Standardized Evaluation Frameworks and Protocols
Patient-Centered CDS Performance Measurement Framework
A 2025 paper proposed a comprehensive performance measurement framework incorporating patient-centered principles into traditional health IT and CDS evaluation. Developed through a review of 147 sources and validated through expert interviews, this framework includes six domains with 34 subdomains for assessment [29].
Figure 1. PC CDS Framework Domains and Measurement Levels
The framework is significant because it (1) covers the entire PC CDS life cycle, (2) has a direct focus on the patient, (3) covers measurement at different levels, (4) encompasses six independent but related domains, and (5) requires additional research to fully characterize all domains and subdomains [29].
The Clinician-in-the-Loop Evaluation Framework
Elsevier's generative AI evaluation team developed a reproducible framework for evaluating AI in healthcare, employing a "clinician-in-the-loop" approach. This methodology uses a two-assessor model where clinical subject matter experts (SMEs) independently rate responses, with discrepancies resolved through a modified Delphi Method consensus process [30].
Table 3: Five Key Dimensions of the ClinicalKey AI Evaluation Framework
| Evaluation Dimension | Definition | Measurement Approach | Performance Result (Q4 2024) |
|---|---|---|---|
| Helpfulness | Overall value of AI-generated responses in clinical scenarios | Rated by clinical SMEs based on clinical utility | 94.4% rated as helpful |
| Comprehension | Ability to accurately interpret complex clinical queries | Assessment of understanding beyond basic language processing | 98.6% demonstrated accurate comprehension |
| Correctness | Factual accuracy of information provided | Verification against high-quality, peer-reviewed clinical sources | 95.5% correctness rate |
| Completeness | Whether responses address all relevant aspects of the clinical query | Evaluation of response comprehensiveness and coverage | 90.9% completeness score |
| Potential Clinical Harm | Risk of responses leading to adverse patient outcomes if acted upon directly | Identification of potentially harmful recommendations | 0.47% rate of potentially harmful content |
This framework was applied in a Q4 2024 evaluation where 41 clinical SMEs, including board-certified physicians and clinical pharmacists, reviewed 426 AI-generated query responses across diverse clinical specialties [30].
Randomized Controlled Trial Protocol for AI-CDSS Evaluation
A 2025 randomized controlled trial (ISRCTN16278872) implemented an AI-CDS system for Stenotrophomonas maltophilia infections, providing a robust experimental protocol for evaluating clinical impact [31].
Figure 2. AI CDSS RCT Experimental Workflow
Methodological Details:
- Participants: 400 healthcare professionals with independent prescribing authority were enrolled. Exclusion criteria included medical interns, students, and clinicians with less than one year of experience [31].
- Intervention: The AI-CDSS utilized mass spectrometry data and machine learning algorithms to predict antibiotic resistance one day earlier than standard methods, providing specific treatment recommendations [31].
- Outcome Measures: The trial assessed confidence in antibiotic prescription, decision-making efficiency, appropriate antibiotic selection via structured surveys, and patient mortality over a 14-day follow-up period [31].
- Results: The AI-CDSS group demonstrated significantly higher confidence (p < 0.001) in antibiotic prescription and lower mortality (11.5% vs. 15.1%, p = 0.03) compared to the control group [31].
Implementation Considerations and Barriers
Qualitative research on AI-based CDSS implementation identified several critical barriers and facilitators. Barriers included variability in previous antibiotic administration practices, increased effort required to justify deviations from AI recommendations, low levels of digitization in clinical practice, limited cross-sectoral data availability, and negative previous experiences with CDSSs [32].
Conversely, facilitators included the ability to re-evaluate CDSS recommendations, intuitive user-friendly system design, potential time savings, physician openness to new technologies, and positive previous experiences with CDS systems [32]. The research emphasized that physicians' confidence in accepting or rejecting AI recommendations depended significantly on their level of professional experience [32].
Essential Research Reagents and Tools
Table 4: Research Reagent Solutions for CDS Evaluation
| Research Tool | Function in Evaluation | Application Example |
|---|---|---|
| Clinical Cases with Antibiograms | Provides standardized scenarios for testing model performance | 60 cases covering 10 infection types used in LLM evaluation [9] |
| Structured Surveys | Quantifies healthcare professional experience and confidence | Used in RCT to measure prescribing confidence and decision-making efficiency [31] |
| Blinded Expert Panel | Provides objective assessment of AI recommendations | Infectious diseases specialists evaluating appropriateness of antibiotic recommendations [9] [12] |
| Quality Assessment Instruments (AGREE II, RIGHT) | Evaluates methodological and reporting quality of guidelines | Used in framework development for multimorbidity guideline assessment [33] |
| MALDI-TOF MS with AI Algorithms | Enables rapid resistance prediction for validation studies | AI-CDSS using mass spectrometry data to predict resistance patterns [31] |
Standardized evaluation frameworks are indispensable for validating the performance, safety, and efficacy of AI-driven Clinical Decision Support systems, particularly in high-stakes domains like antibiotic prescribing. The comparative data reveals significant variability in LLM performance, with advanced models like ChatGPT-o1 showing promise but still struggling with complex cases. Comprehensive frameworks that incorporate patient-centered principles, clinician-in-the-loop validation, and rigorous methodological approaches provide the necessary structure for trustworthy assessment. As AI technologies continue to evolve, ongoing refinement of these evaluation frameworks will be essential to ensure that CDS systems deliver on their potential to enhance patient care while mitigating the risks associated with antimicrobial resistance. Future work should focus on standardizing evaluation metrics across studies and addressing the specific challenges of complex clinical scenarios where AI support may be most valuable.
The integration of Large Language Models (LLMs) into clinical decision-making represents a paradigm shift in infectious disease management, particularly in antibiotic prescribing. Validating these models for real-world application requires rigorous assessment against core metrics that reflect clinical reality. Accuracy, Appropriateness, and Completeness have emerged as the fundamental dimensions for evaluating LLM performance in this high-stakes domain. This guide provides a comparative analysis of leading LLMs based on recent experimental studies, detailing methodologies and metrics essential for researchers and drug development professionals conducting validation studies. Establishing standardized assessment protocols is critical for ensuring that these tools enhance, rather than compromise, antimicrobial stewardship efforts in an era of growing resistance [12].
Core Metrics Explained
Accuracy
Accuracy measures the degree to which an LLM's recommendations align with verifiable, real-world clinical data and established medical facts. It confirms that the model's output correctly represents the scientific and clinical reality of infectious disease treatment, including correct drug selection, dosage, and treatment duration based on the specific clinical context and available antibiogram data [1].
Appropriateness
Appropriateness evaluates whether the LLM's treatment recommendations adhere to established clinical guidelines and are suitable for the specific patient scenario, considering factors like drug-bug mismatch, patient allergies, renal function, and drug interactions. It encompasses both guideline compliance and the absence of potentially harmful suggestions [12].
Completeness
Completeness assesses whether all necessary data elements required for a sound clinical decision are present and utilized by the model. This includes patient-specific clinical information, microbiological data, local resistance patterns, and guideline recommendations. Incomplete data can lead to biased or unreliable recommendations, undermining the model's clinical utility [34].
Comparative Performance Analysis
A comprehensive evaluation of 14 LLMs across 60 clinical cases with antibiograms revealed significant variability in antibiotic prescribing performance. The study assessed recommendations for drug choice, dosage, and treatment duration, with results demonstrating a wide range of capabilities [1].
Table 1: Overall Antibiotic Prescribing Accuracy by LLM
| Large Language Model | Overall Correct Prescriptions | Incorrect Prescriptions | Dosage Correctness | Duration Adequacy |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 1.7% (1/60) | 96.7% (58/60) | Not Specified |
| Claude 3.5 Sonnet | Not Specified | Not Specified | 91.7% (55/60) | Tendency to Over-Prescribe |
| Perplexity Pro | Not Specified | Not Specified | 90.0% (54/60) | Not Specified |
| Gemini | Lowest Accuracy | Not Specified | Not Specified | 75.0% (45/60) - Most Appropriate |
Performance Across Clinical Scenarios
LLM performance varies substantially based on case complexity and infection type. Models generally show stronger performance in straightforward cases with clear guideline recommendations, while performance declines with increasing complexity, particularly for infections involving difficult-to-treat microorganisms or uncommon clinical presentations [1].
Table 2: LLM Performance by Infection Complexity and Type
| Infection Category | Performance Trends | Notable Challenges |
|---|---|---|
| Bloodstream Infections | 64% appropriateness for empirical therapy | Narrowing spectrum inadequately in febrile neutropenia |
| Targeted Therapy | 36% appropriateness | Harmful de-escalation in complex cases |
| Pneumococcal Meningitis | 81% recognized need for antibiotics | Only 38% suggested correct antibiotic type |
| Complex Cases | Significant performance decline | Difficult-to-treat microorganisms |
Appropriateness and Potential Harm
Beyond basic accuracy, the safety profile of LLM recommendations is paramount. Studies have classified recommendations based on their potential for patient harm, with concerning results indicating that even models with high accuracy rates can occasionally generate dangerous suggestions [12].
Table 3: Appropriateness and Harm Potential in LLM Recommendations
| Study Context | Appropriateness Rate | Potentially Harmful Suggestions | Examples of Harmful Recommendations |
|---|---|---|---|
| Bloodstream Infection Cases | Empirical: 64% Targeted: 36% | Empirical: 2% Targeted: 5% | Inadequate Gram-negative coverage in neutropenia; inappropriate de-escalation |
| Spine Surgery Prophylaxis | Variable by model | Not Specified | Inconsistent adherence to North American Spine Society guidelines |
| Pneumococcal Meningitis | 38% correct antibiotic type | Hallucinations of non-existent symptoms | Misinterpretation of bacterial meningitis as herpes ophthalmicus |
Experimental Protocols and Methodologies
Standardized Clinical Case Validation
The most robust evaluations of LLMs for antibiotic prescribing utilize standardized clinical cases with comprehensive clinical details and antibiogram data [1].
Protocol Overview:
- Case Development: Create 60 clinical cases covering 10 infection types with complete clinical scenarios, laboratory results, and antimicrobial susceptibility testing profiles.
- Standardized Prompting: Use identical, structured prompts across all evaluated LLMs, contextualizing the need for comprehensive management recommendations.
- Blinded Expert Review: Have infectious diseases specialists anonymize and evaluate LLM responses for antibiotic choice, dosage, and duration adequacy.
- Harm Assessment: Classify recommendations based on potential for patient harm according to established guidelines.
Figure 1: Workflow for Standardized Clinical Case Validation
Guideline Adherence Assessment
This methodology evaluates LLM compliance with established guidelines from recognized professional societies like IDSA and ESCMID [12].
Protocol Overview:
- Guideline Selection: Identify specific recommendations from authoritative guidelines (IDSA, ESCMID, NASS).
- Case Presentation: Present hypothetical cases to LLMs without definitive diagnoses to test clinical reasoning.
- Multi-Session Testing: Query the same LLM multiple times to assess response consistency.
- Heterogeneity Evaluation: Measure variation in recommendations across sessions and identify hallucinations or misleading statements.
Human Factors Integration
Understanding the "know-do gap" in antibiotic prescribing provides essential context for LLM validation. This approach combines provider knowledge assessments with standardized patient visits to examine why providers prescribe antibiotics inappropriately [8].
Protocol Overview:
- Knowledge Assessment: Use vignettes presenting viral diarrhea cases to measure provider knowledge.
- Behavior Measurement: Conduct anonymous standardized patient visits with identical cases.
- Preference Randomization: Randomize patient-expressed treatment preferences (antibiotics, ORS, no preference).
- Discrete Choice Experiments: Understand how patient choice of providers is influenced by prescribing behaviors.
The Scientist's Toolkit
Table 4: Essential Research Reagents and Materials for LLM Validation Studies
| Reagent/Material | Function in Validation Research |
|---|---|
| Standardized Clinical Cases | Provides consistent evaluation framework across LLMs; enables direct comparison of performance metrics |
| Antibiogram Data | Supplies antimicrobial susceptibility information essential for appropriate targeted therapy recommendations |
| IDSA/ESCMID Guidelines | Serves as reference standard for assessing appropriateness of LLM treatment recommendations |
| Blinded Expert Panel | Provides gold-standard human assessment of LLM output quality and safety |
| Cost Categorization Framework | Enables evaluation of cost-conscious prescribing behaviors in LLM recommendations [35] |
| Standardized Patient Scenarios | Facilitates assessment of human factors and contextual pressures influencing prescribing decisions [8] |
Analysis of Key Findings
Performance Variability and Clinical Implications
The significant performance gaps between leading models like ChatGPT-o1 and lower-performing models such as Gemini and Claude 3 Opus highlight the importance of rigorous validation before clinical implementation [1]. The 71.7% accuracy rate of the top-performing model indicates substantial room for improvement, particularly considering that nearly 30% of recommendations contained errors. Furthermore, the observed performance decline with increasing case complexity suggests current LLMs may be least reliable in precisely those situations where clinical decision support is most needed.
The Appropriateness-Harm Paradox
Some models demonstrated the ability to provide technically appropriate recommendations in most cases while occasionally generating potentially harmful suggestions [12]. This paradox underscores the necessity of comprehensive harm assessment protocols beyond basic accuracy metrics. The identification of specific harmful patterns, such as inappropriate spectrum narrowing in neutropenic patients, provides crucial insights for model refinement and safety guardrails.
Contextual Factors in Prescribing Behavior
LLM validation must consider the human and contextual factors influencing antibiotic prescribing. The significant "know-do gap" identified in clinical practice—where 62% of providers who knew antibiotics were inappropriate still prescribed them—highlights that technical accuracy alone is insufficient [8]. Successful implementation requires understanding and addressing the perceived patient expectations and other non-clinical factors that drive inappropriate prescribing.
The validation of LLMs for antibiotic prescribing requires multi-dimensional assessment against the core metrics of accuracy, appropriateness, and completeness. Current evidence reveals substantial variability in model performance, with leading LLMs demonstrating promising but imperfect capabilities. ChatGPT-o1 currently shows the highest accuracy in antibiotic prescriptions at 71.7%, with dosage correctness reaching 96.7% for top-performing models. However, declining performance in complex cases and the potential for harmful recommendations necessitate careful implementation guardrails. Future research should prioritize standardized evaluation methodologies, comprehensive harm assessment, and integration of human factors to ensure these technologies enhance rather than compromise antimicrobial stewardship in this era of escalating resistance.
The validation of large language models (LLMs) for antibiotic prescribing requires rigorously designed clinical scenarios that accurately reflect the complexities of real-world medical practice. As LLMs show increasing promise in clinical decision-making, the need for standardized, comprehensive evaluation frameworks has become paramount [1] [12]. Clinical scenarios serve as the fundamental testing ground where model performance is measured against established medical expertise and guidelines, providing crucial data on accuracy, safety, and reliability.
This comparative guide examines the experimental approaches and findings from recent studies evaluating LLMs in antibiotic prescribing contexts. By analyzing methodologies, performance metrics, and limitations across different research designs, this review aims to establish benchmarks for current capabilities and identify pathways for more robust validation protocols. The findings presented here are situated within the broader thesis that effective clinical scenario design must encompass diverse infection types, complexity levels, and patient factors to truly assess LLM utility in antimicrobial stewardship [36] [12].
Comparative Performance Data of LLMs in Antibiotic Prescribing
Recent comparative studies have revealed significant variability in LLM performance for antibiotic recommendations. The most comprehensive analysis evaluated 14 different LLMs using 60 clinical cases spanning 10 infection types, generating 840 total responses for evaluation by blinded expert panels [1] [9].
Table 1: Overall Antibiotic Prescribing Accuracy of Various LLMs
| Large Language Model | Accuracy in Antibiotic Prescription | Dosage Correctness | Incorrect Recommendations |
|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60 cases) | 96.7% (58/60) | 1.7% (1/60) |
| Perplexity Pro | Not specified | 90.0% (54/60) | Not specified |
| Claude 3.5 Sonnet | Not specified | 91.7% (55/60) | Not specified |
| Gemini | Lowest accuracy among tested models | Not specified | Not specified |
| Claude 3 Opus | Lowest accuracy among tested models | Not specified | Not specified |
Performance declined consistently with increasing case complexity across all models, particularly for infections involving difficult-to-treat microorganisms [1]. This pattern highlights a critical limitation in current LLM capabilities and underscores the need for clinical scenarios that include complex, multi-factor cases in validation protocols.
Treatment Duration and Specialized Context Performance
Beyond basic antibiotic selection, research has examined LLM performance on specific prescribing elements such as treatment duration and context-specific guidelines.
Table 2: Specialized Performance Metrics Across LLMs
| Large Language Model | Treatment Duration Appropriateness | Performance in General Practice Contexts | Adherence to National Guidelines |
|---|---|---|---|
| Gemini | 75.0% (45/60 cases) | Not specified | Not specified |
| Claude 3.5 Sonnet | Tended to over-prescribe duration | Not specified | Not specified |
| ChatGPT-4 | Not specified | 64% appropriate for empirical therapy | Variable by country (0-96%) |
| Mixed LLMs (7 models) | Correct dosage in ~90% when antibiotic choice appropriate | 81% recognized need for rapid antibiotic administration | 38% suggested correct type per IDSA/ESCMID |
In studies comparing LLMs against general practitioners, human experts demonstrated superior performance in applying national guidelines (100% referenced guidelines appropriately) and determining correct dose and duration, though LLMs showed competitive performance in basic antibiotic selection decisions [37]. This suggests that scenario design must test not just drug selection but the complete prescribing decision, including guideline adherence, duration, and patient-specific factors.
Experimental Protocols for LLM Validation in Clinical Scenarios
Standardized Clinical Case Evaluation Methodology
The most robust studies evaluating LLMs for antibiotic prescribing have employed systematic methodologies with these common elements:
Case Development and Selection:
- 60 clinical cases covering 10 distinct infection types were developed, each accompanied by relevant antibiograms [1] [9]
- Cases spanned varying complexity levels, from straightforward community-acquired infections to complex healthcare-associated scenarios with resistant organisms
- Infection types included bloodstream infections, meningitis, urinary tract infections, respiratory infections, and skin/soft tissue infections
LLM Prompting and Interaction:
- Standardized prompts were used across all models to ensure comparability
- Prompts contextualized the need for comprehensive management recommendations as if the LLM was the consulting specialist [12]
- Some studies employed iterative prompting to simulate clinical conversation and information gathering [12]
Response Evaluation Framework:
- Responses were anonymized and reviewed by blinded expert panels comprising infectious disease specialists
- Evaluations assessed three key dimensions: antibiotic choice appropriateness, dosage correctness, and treatment duration adequacy [1]
- Recommendations were classified as appropriate vs. inappropriate, with additional assessment of potential harm [12]
Analysis Metrics:
- Primary outcome: overall appropriateness of antibiotic regimen
- Secondary outcomes: dosage accuracy, duration adequacy, guideline adherence, and identification of potentially harmful recommendations [1] [37]
Multi-National Comparison Protocol
A distinct methodological approach was employed for studies evaluating LLM performance against general practitioners across different healthcare systems:
Clinical Vignette Design:
- 24 standardized vignettes included information on infection type, patient gender, age group, and comorbidities [37]
- Scenarios were contextualized within four different countries (Ireland, UK, USA, Norway) with their respective national prescribing guidelines
Evaluation Framework:
- Both LLMs and human GPs received identical vignettes with country specification
- Responses were evaluated against national guidelines for each respective country
- Additional assessment of diagnostic accuracy, antibiotic prescribing decisions, and referencing of appropriate guidelines
Specialized Assessments:
- Evaluation of LLM-specific limitations: hallucination rates, toxicity in responses, and data leakage risks
- Analysis of consistency across multiple iterations of the same query [37]
This multi-national approach proved particularly valuable for understanding how LLMs handle region-specific guidelines and antimicrobial resistance patterns, a critical factor for real-world implementation.
Analysis of Key Performance Limitations and Biases
Complexity-Based Performance Degradation
A consistent finding across studies was the inverse relationship between case complexity and LLM performance. While simpler cases with common pathogens and straightforward presentations yielded higher accuracy, performance declined markedly when certain complexity factors were introduced:
- Difficult-to-Treat Microorganisms: Models showed significantly lower accuracy when encountering resistant pathogens such as MRSA, VRE, and ESBL-producing organisms [1]
- Atypical Presentations: Cases with non-classical symptom patterns or multiple potential diagnostic considerations resulted in more inappropriate recommendations
- Comorbid Conditions: Patients with immunosuppression, renal/hepatic impairment, or other comorbidities posed challenges for appropriate dose adjustment and drug selection [38]
This pattern demonstrates that clinical scenarios for LLM validation must include complexity gradients rather than focusing exclusively on straightforward cases.
Hallucination and Consistency Challenges
Studies identified concerning patterns of misinformation and inconsistency in LLM responses:
- Rates of Hallucination: Some models demonstrated tendency to invent clinical findings not present in case descriptions (e.g., reporting Kernig's sign or stiff neck when not documented) [12]
- Response Heterogeneity: The same LLM queried multiple times with identical prompts provided different management recommendations in significant percentages of cases, indicating concerning inconsistency [12] [37]
- Guideline Referencing Failures: While some models demonstrated good adherence to international guidelines, performance dropped sharply with national or local guidelines, particularly for smaller countries (0-13% correct referencing for Norwegian guidelines) [37]
Safety Considerations and Harmful Recommendations
Perhaps most critically, studies identified specific patterns of potentially harmful recommendations:
- Inappropriate Spectrum Narrowing: Some models suggested narrowing antibiotic coverage in high-risk scenarios (e.g., dropping Gram-negative coverage in febrile neutropenia) [12]
- Timing Errors: Recommendations sometimes failed to emphasize urgent antibiotic administration when clearly indicated [12]
- Contraindicated Selections: In some instances, models recommended antibiotics inappropriate for specific clinical scenarios or patient allergies
These safety concerns highlight the critical need for rigorous safety evaluation frameworks within clinical scenario design, moving beyond simple accuracy metrics to assess potential patient harm.
Essential Research Reagents and Materials Framework
Standardized Clinical Evaluation Toolkit
Table 3: Essential Research Reagents for LLM Validation Studies
| Research Reagent Category | Specific Examples | Function in Validation Research |
|---|---|---|
| Clinical Case Repository | 60 cases covering 10 infection types [1]; 24 multi-national vignettes [37] | Provides standardized testing scenarios across complexity spectrum |
| LLM Platforms | ChatGPT-o1, Claude 3.5 Sonnet, Perplexity Pro, Gemini, Copilot, Mixtral AI, Llama [1] [37] | Enables comparative performance assessment across different model architectures |
| Evaluation Guidelines | IDSA, ESCMID, NASS, National antibiotic prescribing guidelines [12] [37] | Establishes objective standards for appropriate prescribing |
| Expert Review Panels | Infectious disease specialists, general practitioners [1] [37] | Provides gold-standard assessment of LLM recommendations |
| Assessment Frameworks | Appropriateness classification, harm potential assessment, dosage correctness evaluation [1] | Standardizes outcome measurements across studies |
| Data Analysis Tools | Statistical packages for performance comparison, consistency measurement [1] [9] | Enables quantitative assessment of model capabilities |
This reagent framework enables reproducible, standardized evaluation of LLM performance across institutions and research groups, facilitating meaningful comparisons as the field advances.
The validation of LLMs for antibiotic prescribing requires clinical scenarios that reflect the full spectrum of clinical complexity, from straightforward community-acquired infections to complex cases with resistant organisms and significant comorbidities. Current evidence demonstrates that while advanced LLMs like ChatGPT-o1 show promising accuracy (71.7%) in antibiotic selection, performance degradation with increasing complexity remains a serious concern [1].
Future clinical scenario design must incorporate gradient complexity models, multi-national guideline adherence assessment, and specific evaluation for potential harmful recommendations. The experimental protocols detailed here provide a framework for standardized evaluation, but must be adapted and expanded to address emerging challenges in LLM validation for clinical use. As these models continue to evolve, so too must our approaches to ensuring their safety and efficacy in supporting antimicrobial stewardship efforts [12].
Incorporating Antibiograms and Local Resistance Patterns
Antibiograms are essential tools in clinical microbiology that summarize the susceptibility of specific microorganisms to various antibiotics, typically expressed as the percentage of isolates that are susceptible to each drug. These reports, often generated at the institutional or regional level, provide critical guidance for empirical antibiotic therapy when specific susceptibility data is not yet available. The growing threat of antimicrobial resistance (AMR), with one in six laboratory-confirmed bacterial infections worldwide now resistant to antibiotic treatments, has intensified the need for accurate, data-driven prescribing decisions [39].
Within this context, researchers are increasingly exploring the potential of large language models (LLMs) to support clinical decision-making for antibiotic prescribing. The central thesis of this emerging field posits that LLMs must be rigorously validated against local resistance patterns and standardized antibiograms to ensure their recommendations are clinically appropriate, safe, and effective. This validation is particularly crucial given the significant geographic variation in resistance patterns—the WHO reports antibiotic resistance is highest in the South-East Asian and Eastern Mediterranean Regions, where one in three reported infections were resistant, compared to one in five in the African Region [39]. This guide provides a comparative analysis of LLM performance in antibiotic prescribing, with a specific focus on the critical incorporation of local antibiogram data.
Global and Local AMR Landscape: The Context for Validation
The Scope of the Antimicrobial Resistance Crisis
The World Health Organization's 2025 Global Antibiotic Resistance Surveillance Report provides alarming data on the current AMR landscape. Between 2018 and 2023, antibiotic resistance rose in over 40% of the pathogen-antibiotic combinations monitored, with an average annual increase of 5-15% [39]. This trend is undermining the effectiveness of essential antibiotics globally:
- Gram-negative pathogens: More than 40% of E. coli and over 55% of K. pneumoniae globally are now resistant to third-generation cephalosporins, the first-choice treatment for these infections. In the African Region, this resistance exceeds 70% [39].
- Last-resort antibiotics: Carbapenem resistance, once rare, is becoming more frequent, narrowing treatment options and forcing reliance on last-resort antibiotics that are often costly, difficult to access, and unavailable in low- and middle-income countries [39].
Local Resistance Patterns and Their Implications
Local antibiogram data reveals significant variations in resistance patterns that must inform empirical treatment. A 2019 study from a surgical unit in Lahore General Hospital found that the most common isolated organism was Escherichia coli (24%), followed by Acinetobacter species (23%), and Pseudomonas species (19%) [40]. The susceptibility profiles differed markedly from global averages:
Table: Local Antimicrobial Susceptibility Patterns in a Surgical Unit (2019)
| Organism | Most Sensitive Antibiotics | Sensitivity Percentage |
|---|---|---|
| Escherichia coli | Amikacin | 78% |
| Meropenem | 71% | |
| Imipenem | 63% | |
| Acinetobacter species | Colistin | 100% |
| Amikacin | 31% | |
| Meropenem | 21% | |
| Pseudomonas species | Colistin | 93% |
| Amikacin | 52% | |
| Meropenem | 52% | |
| Klebsiella species | Colistin | 86% |
| Imipenem | 60% | |
| Aminoglycosides | 50% | |
| Staphylococcus aureus | Linezolid | 100% |
| Vancomycin | 100% |
Source: PMC7686934 [40]
These local variations highlight why LLMs must be calibrated with current, geographically relevant antibiogram data rather than relying on general medical knowledge alone.
Comparative Performance of LLMs in Antibiotic Prescribing
Experimental Design for LLM Validation
A 2025 comparative study published in Clinical Microbiology and Infection evaluated 14 large language models using a standardized methodology [1] [9]. The experimental protocol was designed to assess real-world applicability:
- Case Development: 60 clinical cases with antibiograms covering 10 different infection types were developed.
- Model Selection: The study evaluated standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai.
- Standardized Prompting: A standardized prompt was used for all antibiotic recommendations, focusing on drug choice, dosage, and treatment duration.
- Blinded Evaluation: Responses were anonymized and reviewed by a blinded expert panel assessing antibiotic appropriateness, dosage correctness, and duration adequacy.
- Output Analysis: A total of 840 responses were collected and analyzed for accuracy across different complexity levels.
This rigorous methodology provides a robust framework for validating LLMs against clinical standards incorporating local resistance data.
Comparative Performance Metrics
The study revealed significant variability in LLM performance across key prescribing metrics:
Table: Comparative LLM Performance in Antibiotic Prescribing
| LLM Model | Overall Antibiotic Appropriateness | Dosage Correctness | Treatment Duration Adequacy | Incorrect Recommendations |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 96.7% (58/60) | Data not specified | 1.7% (1/60) |
| Perplexity Pro | Data not specified | 90.0% (54/60) | Data not specified | Data not specified |
| Claude 3.5 Sonnet | Data not specified | 91.7% (55/60) | Tendency to over-prescribe | Data not specified |
| Gemini | Lowest accuracy | Data not specified | 75.0% (45/60) | Data not specified |
| Claude 3 Opus | Lowest accuracy | Data not specified | Data not specified | Data not specified |
Source: PubMed 40113208 [1]
ChatGPT-o1 demonstrated the highest overall accuracy in antibiotic prescriptions, with only one incorrect recommendation out of 60 cases. Performance across all models declined with increasing case complexity, particularly for difficult-to-treat microorganisms, highlighting the challenges LLMs face with complex resistance patterns [1] [9].
Methodological Framework for LLM Validation
Workflow for Validating LLMs Against Antibiograms
The following diagram illustrates the systematic approach for incorporating local resistance data into LLM validation:
Key Experimental Protocols
Standardized Prompt Engineering
The validation studies employed meticulous prompt engineering to ensure consistent evaluation across different LLMs [1] [9]:
- Contextualization: Prompts were contextualized to specific clinical environments (e.g., "as an infectious diseases specialist consulting in a French hospital").
- Structured Input: All prompts included comprehensive patient data, microbiological results, and local antibiogram information.
- Output Specification: Explicit instructions were given to provide comprehensive responses including drug choice, dosage, duration, and explanation.
Evaluation Criteria and Harm Assessment
The expert panels employed multi-dimensional assessment criteria [12]:
- Appropriateness: Alignment with local guidelines and international standards (IDSA, ESCMID).
- Safety Classification: Categorization of recommendations as "potentially harmful" versus "not harmful."
- Spectrum Evaluation: Assessment of whether antibiotic spectrum was appropriately broad or narrow based on clinical scenario and local resistance patterns.
- Dosing and Duration Accuracy: Evaluation of dosage correctness and treatment duration adequacy.
Essential Research Reagents and Tools
The following table details key resources required for establishing a robust LLM validation framework for antibiotic prescribing:
Table: Essential Research Reagent Solutions for LLM Validation
| Reagent/Tool | Function in Validation Research | Implementation Example |
|---|---|---|
| WHO GLASS Data | Provides global standardized AMR data for benchmarking | Global resistance prevalence estimates for 93 infection type-pathogen-antibiotic combinations [41] |
| Clinical Case Repository | Standardized cases for consistent LLM evaluation | 60 clinical cases with antibiograms covering 10 infection types [1] |
| WHO AWaRe Classification | Framework for evaluating antibiotic appropriateness | Categorizing recommendations into Access, Watch, Reserve groups [42] |
| Antimicrobial Susceptibility Testing Systems | Generating current local antibiogram data | Selux AST System, VITEK 2 AST cards for phenotypic testing [43] |
| Expert Review Panel | Gold standard for assessing recommendation appropriateness | Blinded infectious disease specialists evaluating 840 responses [1] |
Limitations and Research Gaps
Despite promising results, significant challenges remain in fully validating LLMs for clinical antibiotic prescribing:
- Performance Variability: Different LLMs show substantial variation in prescribing accuracy, with some models demonstrating potentially harmful recommendation rates [12].
- Complex Case Limitations: All models showed decreased accuracy with increasing case complexity, particularly for difficult-to-treat microorganisms and multidrug-resistant infections [1].
- Local Data Integration: Many LLMs struggle to appropriately incorporate real-time, local antibiogram data, often defaulting to general textbook recommendations [12].
- Hallucination Risks: Studies note instances of LLMs "hallucinating" clinical signs not present in the case description or providing misleading interpretations [12].
The validation of large language models for antibiotic prescribing represents a critical intersection of artificial intelligence and clinical microbiology. Based on current evidence, the following priorities emerge for advancing this field:
- Standardized Validation Frameworks: Development of consensus methodologies for testing LLMs against local resistance patterns.
- Integration with Electronic Health Records: Seamless incorporation of real-time antibiogram data into LLM decision pathways.
- Prospective Clinical Trials: Movement beyond retrospective studies to prospective evaluation of LLM-guided prescribing in clinical settings.
- Regulatory Alignment: Collaboration with regulatory bodies like the FDA to establish approval pathways for AI-based prescribing support systems [43].
The comparative data clearly indicates that while advanced LLMs like ChatGPT-o1 show promising accuracy in antibiotic prescribing, their performance is not uniform across models or clinical scenarios. The integration of current, local antibiogram data remains essential for any clinically useful implementation. As AMR continues to rise globally, the rigorous validation of LLMs against local resistance patterns represents not merely a technical challenge but an ethical imperative for responsible antibiotic stewardship.
Blinded Expert Panel Review Processes
Blinded expert panel reviews serve as a critical methodology for establishing reliable reference standards in medical research, particularly when a single, error-free diagnostic gold standard is unavailable [44]. This approach involves multiple experts collectively assessing available clinical data to reach a consensus diagnosis while remaining unaware of certain information that could bias their judgments. In the context of validating large language models (LLMs) for antibiotic prescribing, this methodology provides an objective benchmark against which model performance can be rigorously evaluated [1]. The fundamental principle underpinning blinded reviews is the reduction of various cognitive biases—including hindsight bias, affiliation bias, and confirmation bias—that might otherwise compromise the integrity of expert evaluations [45] [46].
The application of blinded expert panels has gained increasing importance as researchers seek to validate emerging artificial intelligence technologies for clinical decision support. These panels are particularly valuable in antibiotic stewardship research, where inappropriate prescribing contributes significantly to antimicrobial resistance and requires careful assessment across diverse clinical scenarios [8] [47]. By implementing rigorous blinding procedures, researchers can obtain more credible reference standards that accurately reflect the true performance characteristics of LLMs in recommending antibiotic treatments [1] [12].
Methodological Framework for Blinded Expert Panels
Core Components and Implementation
The implementation of blinded expert panels involves several critical components that ensure methodological rigor. First, panel constitution requires careful consideration of the number and background of experts, with most studies utilizing panels of three or fewer members representing different fields of expertise [44]. The blinding process itself typically involves concealing the identity of the model or intervention being evaluated, the source of recommendations, and sometimes the specific research objectives from panel members [45] [46].
The decision-making process within expert panels varies considerably across studies, with approaches including discussion-based consensus, modified Delphi techniques, and independent scoring with statistical aggregation [44]. Reproducibility of decisions is assessed in only approximately 21% of studies, highlighting an area for methodological improvement [44]. For LLM validation specifically, the blinding process typically involves removing all identifiers that might reveal whether recommendations originate from human experts or AI systems, ensuring that evaluations focus solely on the quality and appropriateness of the recommendations rather than their source [1] [12].
Workflow Diagram of a Blinded Expert Panel Process
The following diagram illustrates the sequential workflow for implementing a blinded expert panel review process:
Blinded Expert Panel Review Workflow
Experimental Applications in LLM Antibiotic Prescribing Research
Comparative Performance Evaluation Studies
Recent research has employed blinded expert panels to evaluate the performance of various LLMs in antibiotic prescribing across diverse clinical scenarios. One comprehensive study assessed 14 different LLMs—including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai—using 60 clinical cases with antibiograms covering 10 infection types [1]. A blinded expert panel reviewed 840 anonymized responses, evaluating antibiotic appropriateness, dosage correctness, and treatment duration adequacy while remaining unaware of the specific LLM that generated each recommendation [1].
The results demonstrated significant variability in model performance, with ChatGPT-o1 achieving the highest accuracy in antibiotic prescriptions at 71.7% (43/60 recommendations classified as correct) and only one (1.7%) incorrect recommendation [1]. Dosage correctness was highest for ChatGPT-o1 (96.7%, 58/60), followed by Perplexity Pro (90.0%, 54/60) and Claude 3.5 Sonnet (91.7%, 55/60) [1]. In treatment duration, Gemini provided the most appropriate recommendations (75.0%, 45/60), while Claude 3.5 Sonnet tended to over-prescribe duration [1]. Performance consistently declined with increasing case complexity, particularly for difficult-to-treat microorganisms [1].
Comparative LLM Performance Data
Table 1: Performance Metrics of Large Language Models in Antibiotic Prescribing Accuracy
| LLM Model | Overall Accuracy (%) | Dosage Correctness (%) | Duration Appropriateness (%) | Incorrect Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Not Reported | 1.7 |
| Claude 3.5 Sonnet | Not Reported | 91.7 | Tendency to over-prescribe | Not Reported |
| Perplexity Pro | Not Reported | 90.0 | Not Reported | Not Reported |
| Gemini | Not Reported | Not Reported | 75.0 | Not Reported |
| Claude 3 Opus | Lowest accuracy | Not Reported | Not Reported | Not Reported |
Note: Performance metrics based on evaluation of 60 clinical cases across 10 infection types by blinded expert panel [1]
Detailed Experimental Protocols
Blinded Evaluation Methodology for LLM Antibiotic Prescribing
The standard methodology for blinded evaluation of LLM antibiotic prescribing involves several carefully designed steps. First, researchers develop a set of clinical cases representing various infection types and complexity levels [1] [48]. These cases typically include detailed patient presentations, relevant medical history, physical examination findings, laboratory results, and antimicrobial susceptibility data when appropriate [1].
LLMs then receive standardized prompts requesting antibiotic recommendations for these cases, with researchers ensuring consistent formatting and contextual information across all queries [1] [12]. The generated responses are systematically anonymized to remove any identifiers that might reveal the specific model used, after which they are compiled in random order for expert panel review [1].
The expert panel, comprising infectious disease specialists and antimicrobial stewardship experts, evaluates each anonymized response using predefined assessment criteria [1] [48]. These criteria typically include appropriateness of antibiotic selection based on clinical guidelines, correctness of dosage calculations, appropriateness of treatment duration, and identification of potentially harmful recommendations [1]. Panel members independently score each response before convening to reach consensus on disputed assessments [12].
Pneumonia Management Evaluation Protocol
A specialized protocol for evaluating LLM performance in pneumonia management demonstrates the application of blinded expert panels to a specific clinical context [48]. In this study, researchers curated 50 pneumonia-related questions (30 general, 20 guideline-based) from reputable sources including the Infectious Diseases Society of America (IDSA) and the American Thoracic Society [48].
Three LLMs (ChatGPT-4o, OpenAI O1, and OpenAI O3 mini) generated responses to these questions, which were then presented to ten infectious disease specialists with over five years of clinical experience in pneumonia management [48]. The specialists independently rated the anonymized responses using a 5-point accuracy scale, with scores categorized as 'poor' (<26), 'moderate' (26-38), and 'excellent' (>38) based on predetermined thresholds [48].
For responses initially rated as 'poor,' the chain-of-thought models (OpenAI O1 and OpenAI O3 mini) underwent reassessment with corrective prompting to evaluate their self-correction capabilities [48]. Specialists highlighted incorrect or incomplete segments and prompted the models with: "This information seems inaccurate. Could you re-evaluate and correct your response?" [48]. The revised responses were then re-evaluated by the same specialists one week later to reduce recall bias [48].
Evaluation Workflow Diagram
The following diagram illustrates the comprehensive evaluation workflow for assessing LLM performance in antibiotic prescribing:
LLM Antibiotic Prescribing Evaluation Workflow
Research Reagent Solutions for Blinded Expert Panel Studies
Table 2: Essential Research Materials for Blinded Expert Panel Studies on LLM Validation
| Research Reagent | Function | Implementation Example |
|---|---|---|
| Standardized Clinical Cases | Provides consistent evaluation scenarios across LLMs | 60 cases with antibiograms covering 10 infection types [1] |
| Antimicrobial Susceptibility Data | Enables assessment of appropriate antibiotic selection | Antibiograms for specific clinical cases [1] |
| Assessment Rubrics | Standardizes evaluation of LLM responses | 5-point accuracy scale for pneumonia recommendations [48] |
| Blinding Protocols | Removes source identifiers to prevent bias | Anonymization of LLM responses before expert review [1] |
| Consensus Guidelines | Provides reference standard for appropriate care | IDSA/ATS pneumonia guidelines [48] |
| Expert Panel Recruitment Criteria | Ensures appropriate clinical expertise | Infectious disease specialists with 5+ years experience [48] |
| Statistical Analysis Tools | Quantifies performance differences | Fleiss' Kappa for inter-rater reliability [48] |
Comparative Analysis of Blinding Methodologies
Single-Blind vs. Double-Blind Approaches
The methodology for blinding expert panels exists on a spectrum from single-blind to double-blind approaches, each with distinct advantages and limitations. In single-blind reviews, which have been traditional in many scientific journals, reviewers know the identity of the authors or sources being evaluated but not vice versa [46]. This approach has been criticized for potentially allowing biases related to investigator reputation, institutional prestige, race, and/or sex to influence evaluations [46].
Double-blind reviewing, in contrast, conceals the identities of both the reviewees and reviewers from each other [46]. Evidence suggests this approach results in higher quality peer reviews and reduces the impact of perceived author and institutional prestige on acceptance rates [46]. A study of 40,000 research paper authors identified double-blind review as the most effective form of peer review [46]. Successful blinding of author identity is achieved approximately 60% of the time and may be increased to 75% with the removal of identifying allusions and self-citations [46].
In the context of LLM validation for antibiotic prescribing, the double-blind approach is particularly valuable as it prevents experts from developing expectations based on their prior experiences with specific models, thereby ensuring more objective assessment of each recommendation on its own merits [1] [12].
Impact on Evaluation Outcomes
The implementation of rigorous blinding methodologies significantly impacts the evaluation outcomes in LLM validation studies. Research comparing blinded versus non-blinded assessments demonstrates that blinded experts receive higher scores on credibility, skill, and genuineness from evaluators [45] [49]. In legal contexts where expert testimony is critical, mock jurors understanding the blinding concept more than doubled the odds of a favorable verdict for either party when experts were blinded [49].
In LLM antibiotic prescribing research, blinding prevents the "hired gun" effect, where evaluators might consciously or unconsciously favor recommendations from certain prestigious models or institutions [46] [49]. This is particularly important given findings that LLMs sometimes display overconfidence in incorrect recommendations, with lower-performing models paradoxically exhibiting higher confidence in their answers [50]. One study found an inverse correlation between mean confidence scores for correct answers and overall model accuracy (r=-0.40; P=.001), indicating that worse-performing models showed unjustified higher confidence [50].
Methodological Challenges and Limitations
Reporting Quality and Implementation Consistency
Despite the recognized importance of blinded expert panels in diagnostic research, significant challenges exist in both implementation and reporting. A systematic review of diagnostic studies using expert panels as reference standards found that one or more critical pieces of information about panel methodology was missing in 83% of studies [44]. Specifically, information on panel constitution was missing in a quarter of studies, and details on the decision-making process were incomplete in more than two-thirds of studies [44].
This reporting inconsistency complicates comparative evaluation across studies and meta-analysis of aggregated findings. Additionally, the methodology of panel diagnosis varies substantially across studies in terms of panel composition, blinding procedures, information provided for diagnosis, and methods of decision making [44]. In most studies (75%), panels consisted of three or fewer members, and panel members were blinded to index test results in only 31% of studies [44]. Reproducibility of the decision process was assessed in just 21% of studies [44].
Technical Limitations in LLM Evaluation
When applying blinded expert panels to LLM validation, researchers face several technical challenges. First, the rapidly evolving nature of LLM technology means that evaluation results may have limited longevity as models are continuously updated and improved [12]. Second, the heterogeneity in model architectures—such as the differences between direct-answer models like ChatGPT-4o and chain-of-thought models like OpenAI O1 and O3 mini—complicates direct comparison [48].
Additionally, studies have identified concerning patterns in LLM confidence calibration that may not be apparent through blinded expert evaluation alone. Research has shown that LLMs often exhibit minimal variation in confidence between correct and incorrect responses, with the mean difference ranging from 0.6% to 5.4% across models [50]. This overconfidence in incorrect recommendations poses significant safety concerns for clinical implementation that may not be fully captured through appropriateness assessments alone [50].
Blinded expert panel review processes represent a methodological gold standard for establishing reference standards in diagnostic research and validating the performance of large language models for antibiotic prescribing. The implementation of rigorous blinding methodologies reduces various cognitive biases and provides more credible assessments of model performance across diverse clinical scenarios. Current evidence demonstrates significant variability in LLM performance for antibiotic recommendations, with advanced models like ChatGPT-o1 showing promising accuracy but continued concerns regarding overconfidence and performance degradation with complex cases.
The field would benefit from standardized reporting guidelines for blinded expert panel methodologies, similar to those developed for diagnostic accuracy studies. Future research should focus on optimizing panel composition, blinding procedures, and decision-making processes to enhance the reliability and reproducibility of evaluations. As LLM technology continues to evolve, ongoing blinded validation against expert consensus standards will be essential for ensuring the safe and effective integration of these tools into clinical practice for antibiotic stewardship.
The integration of artificial intelligence (AI) into clinical practice, particularly for antibiotic prescribing, presents a spectrum of implementation models. These range from assistive tools, which support and augment human decision-making, to autonomous systems capable of making independent clinical decisions. Understanding the performance characteristics, advantages, and limitations of each model is crucial for researchers, scientists, and drug development professionals working to validate large language models (LLMs) for antimicrobial stewardship. This guide objectively compares these integration paradigms using recent experimental data, detailing methodologies, and presenting key resources for further research.
Defining the Integration Paradigms
Within the context of AI for healthcare, integration models are often categorized based on the level of human oversight and autonomy granted to the system.
- Assistive AI refers to systems designed to support human clinicians by providing information, recommendations, and tools. The human retains complete control over the final decision-making process and actions. In antibiotic prescribing, this manifests as an AI that suggests treatment options, doses, and durations, which the physician can then accept, modify, or reject [51] [52].
- Autonomous AI describes systems capable of making clinical decisions and taking action without direct human input. These systems operate independently within predefined parameters, and the performance bar for their validation is necessarily much higher due to the absence of a human "safety net" [51].
It is critical to note that these paradigms are not mutually exclusive, and real-world applications often involve a hybrid approach, particularly through shared autonomy systems where control is dynamically arbitrated between the user and the AI [53].
Comparative Performance Analysis
Recent empirical studies have directly evaluated the performance of LLMs in clinical scenarios, providing quantitative data for comparison. The table below summarizes key findings from a major 2025 study comparing 14 different LLMs across 60 clinical cases involving 10 infection types [1] [9].
Table 1: Performance of Select LLMs in Antibiotic Prescribing Accuracy
| LLM Model | Overall Prescription Accuracy (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information Not Provided | Highest overall accuracy and dosage correctness. | Performance declines with case complexity. |
| Claude 3.5 Sonnet | Information Not Provided | 91.7 | Tended to over-prescribe | Good dosage correctness. | Inconsistent treatment duration recommendations. |
| Perplexity Pro | Information Not Provided | 90.0 | Information Not Provided | High dosage correctness. | Not the top performer in overall accuracy. |
| Gemini | Lowest Accuracy | Information Not Provided | 75.0 | Most appropriate treatment duration. | Lowest overall prescription accuracy. |
A separate study compared the performance of LLMs against General Practitioners (GPs) in a general practice setting using 24 clinical vignettes [54]. The results highlight the complementary strengths of human and artificial intelligence.
Table 2: LLM vs. General Practitioner Performance in Antibiotic Prescribing
| Metric | General Practitioners (GPs) | LLMs (Aggregate Range) |
|---|---|---|
| Diagnosis Accuracy | 96% - 100% | 92% - 100% |
| Antibiotic (Yes/No) Accuracy | 83% - 92% | 88% - 100% |
| Correct Antibiotic Choice | 58% - 92% | 59% - 100% |
| Correct Dose/Duration | 50% - 75% | 0% - 75% |
| Guideline Referencing | 100% | 0% - 96% (Varies widely by country) |
Detailed Experimental Protocols
To ensure reproducibility and critical appraisal, the methodologies of the key cited experiments are detailed below.
Protocol 1: Broad Multi-Model Comparison
This study evaluated 14 LLMs, including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, and others [1] [9].
- Case Design: 60 clinical cases with accompanying antibiograms were developed, covering 10 different infection types.
- Prompting: A standardized prompt was used for all models, requesting antibiotic recommendations focused on drug choice, dosage, and treatment duration.
- Blinded Evaluation: All LLM responses were anonymized and reviewed by a blinded panel of infectious disease experts.
- Assessment Criteria: The panel assessed each response for:
- Appropriateness: Alignment of the antibiotic choice with clinical guidelines.
- Dosage Correctness: Accuracy of the recommended dose.
- Duration Adequacy: Appropriateness of the treatment length.
- Analysis: Performance was analyzed overall and stratified by case complexity.
Protocol 2: Primary Care Vignette Study
This study compared six LLMs and four GPs (from Ireland, the UK, USA, and Norway) using vignettes from general practice [54].
- Vignette Selection: 24 vignettes were selected from the literature, covering conditions like UTI, pneumonia, bronchitis, and cellulitis.
- Reference Standard: Country-specific national antibiotic prescribing guidelines (e.g., NICE, IDSA) served as the gold standard.
- Data Collection: GPs and LLMs were prompted with the same questions for each vignette: diagnosis, antibiotic yes/no, choice, dose, duration, patient advice, and guidelines referenced.
- Additional Metrics: The study also assessed LLM-specific limitations:
- Hallucination: Generation of incorrect or fabricated information, evaluated using BERTScore.
- Data Leakage: Unintended repetition of user input data, checked with Python's SpaCy library.
The logical workflow for a typical LLM benchmarking study in this field is illustrated below.
Advantages, Limitations, and Clinical Implications
The experimental data reveals a nuanced landscape for each integration model.
Assistive Tool Model: When used as an assistive tool, LLMs can dramatically reduce repetitive tasks for clinicians, freeing up time for more sophisticated clinical reasoning [12]. They act as a powerful second set of eyes, potentially improving efficiency and providing rapid access to a broad knowledge base. However, limitations include the risk of hallucination (generating plausible but incorrect advice) [12] [54], data leakage [54], and inconsistent adherence to local guidelines, especially for non-English contexts [54]. Over-reliance without adequate validation could also lead to deskilling over time [55].
Autonomous Decision-Making Model: The primary advantage of a hypothetical autonomous system is the ability to function without human intervention, which could standardize care and address resource shortages. However, the current evidence suggests that fully autonomous prescribing is not yet viable. Performance consistently declines with increasing case complexity, particularly for infections with difficult-to-treat microorganisms [1] [9]. The "black box" nature of some models also makes it difficult to understand the reasoning behind a prescription, raising concerns about accountability and safety [12]. For autonomous systems, the performance and validation requirements are, justifiably, far more stringent [51].
A critical factor in user adoption of any AI assistance is the Sense of Agency (SoA)—the user's feeling of control over their actions and outcomes. Research in assistive robotics has shown that higher levels of robot autonomy can lead to better task performance but often at the cost of a diminished user SoA [53]. This trade-off is highly relevant to clinical settings, where preserving a clinician's ultimate authority and responsibility is paramount.
For researchers aiming to conduct similar validation studies, the following table details key "research reagents" and their functions.
Table 3: Essential Materials for LLM Validation Experiments in Antimicrobial Prescribing
| Item | Function in Experimental Protocol |
|---|---|
| Clinical Vignettes | Standardized patient cases that serve as the input stimulus for testing LLMs and clinicians. They must be well-characterized and cover a range of infections and complexities. |
| Antibiograms | Antimicrobic susceptibility data that provides context for appropriate antibiotic selection, mimicking real-world clinical decision-making. |
| National/International Guidelines (e.g., IDSA, NICE) | The evidence-based reference standard against which the appropriateness of LLM and human recommendations are judged. |
| Blinded Expert Review Panel | A group of subject matter experts (e.g., infectious disease specialists) who assess the quality, appropriateness, and safety of treatment recommendations without knowing their source. |
| Standardized Prompt Framework | A consistent set of instructions and questions used to query each LLM, ensuring comparability of responses across different models. |
| Toxicity & Hallucination Evaluation Tools (e.g., BERTScore) | Metrics and NLP tools to identify the generation of incorrect, irrelevant, or unsafe content by LLMs. |
| Data Leakage Detection Tools (e.g., SpaCy) | Software libraries used to check if LLMs are inadvertently memorizing and outputting sensitive data from their training sets or input prompts. |
The integration of LLMs into antibiotic prescribing presents a choice between two primary models: the assistive tool, which augments human expertise, and the autonomous system, which aims to replace it. Current experimental data demonstrates that while advanced LLMs like ChatGPT-o1 show significant promise in supporting prescribing tasks, their performance is not yet sufficiently reliable or consistent for full autonomy, especially in complex cases. The optimal path forward likely involves a collaborative, augmented intelligence approach that leverages the data-processing strengths of LLMs while keeping the clinician firmly in the loop. Future validation research must focus on improving model performance in complex scenarios, enhancing transparency, quantifying the sense of agency, and rigorously assessing real-world clinical impact.
Prompt Engineering Strategies for Clinical Context
Large language models (LLMs) show significant potential to transform clinical decision-making, including the complex domain of antibiotic prescribing [56]. However, their performance is highly dependent on the quality of the instructions, or "prompts," they are given [56]. Research indicates that minor changes in a prompt's wording or structure can lead to marked variability in the relevance and accuracy of the model's output [56]. Therefore, prompt engineering—the art and science of designing and optimizing these instructions—becomes a critical discipline for researchers seeking to objectively evaluate and compare the accuracy of different LLMs for antibiotic prescribing. This guide synthesizes current research to compare model performance, detail experimental protocols, and establish foundational prompt engineering strategies for this specific clinical application.
Comparative Performance of LLMs in Antibiotic Prescribing
Objective, data-driven comparisons are essential for understanding the capabilities and limitations of various LLMs. A 2025 comparative study evaluated 14 different LLMs using 60 clinical cases with antibiograms, generating 840 responses that were anonymized and reviewed by a blinded expert panel [1] [9].
Table 1: Overall Prescribing Accuracy and Error Rates of Select LLMs
| Model | Appropriate Antibiotic Choice | Incorrect Recommendations | Dosage Correctness | Treatment Duration Appropriateness |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 1.7% (1/60) | 96.7% (58/60) | Information Not Specified |
| Perplexity Pro | Information Not Specified | Information Not Specified | 90.0% (54/60) | Information Not Specified |
| Claude 3.5 Sonnet | Information Not Specified | Information Not Specified | 91.7% (55/60) | Tended to over-prescribe duration |
| Gemini | Lowest Accuracy | Information Not Specified | Information Not Specified | 75.0% (45/60) |
| Claude 3 Opus | Lowest Accuracy | Information Not Specified | Information Not Specified | Information Not Specified |
The study revealed that performance declined with increasing case complexity, particularly for infections involving difficult-to-treat microorganisms [1]. This highlights that overall accuracy metrics must be interpreted in the context of clinical scenario difficulty.
Table 2: Performance on Specific Clinical Tasks
| Clinical Task | Best Performing Model(s) | Key Performance Finding | Limitation / Challenge |
|---|---|---|---|
| Bloodstream Infection Management | ChatGPT-4 | 64% appropriateness for empirical therapy; 36% for targeted therapy [12] | 2-5% of suggestions were potentially harmful [12] |
| Pneumococcal Meningitis Management | ChatGPT-4 | Most consistent responses across multiple sessions [12] | Only 38% of models suggested correct empirical antibiotics per guidelines [12] |
| Antibiotic Prophylaxis in Spine Surgery | ChatGPT-3.5 & ChatGPT-4 | Evaluated against 16 NASS guideline questions [12] | Performance varied by specific clinical question [12] |
Experimental Protocols for Evaluating LLM Prescribing Accuracy
To ensure the validity and reproducibility of LLM validation studies, researchers must adhere to structured experimental protocols. The following workflow outlines a standardized methodology derived from recent comparative studies.
Core Experimental Methodology
The foundational protocol for comparing LLMs, as utilized in key studies, involves several critical phases [1] [9]:
- Case Selection and Development: Researchers curated 60 clinical cases covering 10 different infection types. Each case was supplemented with a corresponding antibiogram to reflect local antimicrobial resistance patterns, providing the necessary context for making informed prescribing decisions [1].
- Prompt Standardization: A single, standardized prompt template was applied across all LLMs to ensure a fair comparison. This controlled for the variable of prompt design, allowing differences in output to be attributed to the models themselves rather than the input instructions [1] [9].
- Blinded Evaluation: All LLM-generated responses were collected and anonymized to eliminate reviewer bias. A panel of independent clinical experts then assessed each response based on predefined criteria: antibiotic choice appropriateness, dosage correctness, and treatment duration adequacy [1] [9].
- Analysis of Complex Cases: The evaluation specifically analyzed how performance changed with increasing case complexity, noting significant declines in accuracy for infections caused by difficult-to-treat pathogens [1].
Specialized Validation Protocols
Beyond overall accuracy, researchers have developed specific protocols to test other dimensions of LLM performance:
- Consistency Testing: To evaluate reliability, some studies present the same clinical case to an LLM multiple times in separate sessions. For instance, one study queried seven LLMs thrice each for a case of pneumococcal meningitis, finding substantial heterogeneity in responses for most models, with ChatGPT-4 being a notable exception for its consistency [12].
- Guideline Adherence Assessment: Studies often measure LLM output against established clinical guidelines from bodies like the IDSA, ESCMID, or NASS. This involves crafting prompts that directly quote guideline questions or embed guideline-based scenarios to check the model's ability to apply evidence-based recommendations [12] [57].
- Safety and Harm Evaluation: In studies like the evaluation of ChatGPT-4 for bloodstream infections, expert panels not only assess appropriateness but also classify whether a recommendation could be potentially harmful to the patient, a crucial metric for clinical safety [12].
Foundational Prompt Engineering Strategies for Clinical Research
Effective prompt engineering is not a one-size-fits-all process but rather a structured practice built on core principles. The following strategies are essential for researchers designing validation studies for antibiotic prescribing.
Core Principles for Clinical Prompts
Table 3: Core Prompt Engineering Principles for Clinical Contexts
| Principle | Description | Application in Antibiotic Prescribing |
|---|---|---|
| Explicitness & Specificity | Prompts must be clear, precise, and concise to avoid generic or clinically irrelevant outputs [56]. | Instead of "Suggest antibiotics," use "For a 65-year-old with penicillin allergy and CKD Stage 3, recommend an antibiotic for community-acquired pneumonia per IDSA/ATS guidelines, covering for DRSP." |
| Contextual Relevance | Incorporating pertinent clinical details directly improves output specificity and accuracy [56]. | Include patient demographics, comorbidities, allergy status, recent culture results, and local antibiogram data within the prompt. |
| Iterative Refinement | Initial prompts often require revision. A structured feedback loop is needed to enhance relevance and accuracy [56] [58]. | If an initial output is too general, refine by adding more specific clinical variables or referencing a particular guideline section. |
| Evidence-Based Practice | Prompts should instruct the LLM to align its outputs with the latest clinical guidelines and evidence [56]. | Use directives like "According to the most recent IDSA guidelines..." or "Summarize the evidence from post-2020 trials for..." |
| Ethical Considerations | Prompt design must prioritize patient safety, privacy (de-identification), and bias mitigation [56]. | Anonymize patient data in prompts used for testing. Instruct the model to consider cost and access barriers where relevant. |
Advanced Prompting Techniques
Researchers can employ several structured prompting techniques to elicit more sophisticated reasoning from LLMs:
- Zero-Shot Prompting: The model is given a task without any examples. This tests its inherent, pretrained knowledge and is useful for general queries but may produce generic outputs for complex cases [56].
- Few-Shot Prompting: The prompt includes several examples of the desired input-output format. This enhances consistency for complex tasks like diagnostic support but requires curated examples and carries a risk of overfitting [56].
- Chain-of-Thought (CoT) Prompting: The model is instructed to reason step-by-step, mimicking clinical reasoning. This can improve performance on complex cases, such as generating a differential diagnosis, but may lead to verbose outputs [56] [57].
- Role-Playing (ROT) Prompting: Instructing the model to "act as" a specific expert (e.g., "You are an infectious disease specialist") has been shown in some studies to significantly improve consistency with clinical guidelines, especially for strong evidence-based recommendations [57].
The Scientist's Toolkit: Key Reagents for LLM Validation Research
Table 4: Essential Research Reagents and Materials for LLM Validation Studies
| Item / Solution | Function in Experimental Protocol |
|---|---|
| Curated Clinical Case Bank | A validated set of clinical scenarios (e.g., 60 cases covering diverse infections) used as the standardized input for benchmarking LLM performance [1]. |
| Standardized Antibiograms | Local or institutional antimicrobial susceptibility data provided with clinical cases to simulate real-world prescribing constraints and guide appropriate antibiotic selection [1]. |
| Blinded Expert Panel | A committee of independent clinical specialists who adjudicate LLM-generated responses for appropriateness, dosage, duration, and potential harm, ensuring objective evaluation [1] [9]. |
| Clinical Practice Guidelines (IDSA, ESCMID, etc.) | Authoritative, evidence-based documents serving as the objective standard against which the appropriateness of LLM treatment recommendations is measured [12]. |
| Structured Prompt Templates | Pre-defined, consistent prompt formats applied across all tested LLMs to control for input variability and ensure a fair comparative evaluation [1] [9]. |
| Statistical Analysis Plan | A pre-defined protocol for analyzing outcomes (e.g., accuracy, F1 scores, Fleiss' kappa for reliability) to ensure robust and reproducible assessment of results [57] [15]. |
The validation of LLMs for antibiotic prescribing accuracy is a multifaceted research endeavor where prompt engineering plays a pivotal role. Objective comparisons reveal significant variability among models, with advanced versions like ChatGPT-o1 currently leading in accuracy for drug selection and dosage, but performance remains imperfect, especially for complex cases [1] [9]. The reliability of these models can also be unstable, necessitating rigorous, blinded validation protocols [57]. Future research must focus on refining prompt engineering strategies to improve consistency, reduce hallucinations and overprescription, and enhance the model's ability to handle complex, multi-morbid patients. By adhering to structured experimental designs and leveraging core prompt engineering principles, researchers can generate the robust evidence needed to guide the safe and effective integration of LLMs into clinical practice.
Addressing Critical Challenges: Hallucinations, Variability, and Regulatory Gaps
Identifying and Mitigating Hallucinations in Treatment Recommendations
In the critical field of medical treatment recommendations, particularly for antibiotic prescribing, the term "hallucination" carries a dual significance that demands researcher attention. Clinical hallucinations, well-documented adverse drug reactions characterized by sensory perceptions without external stimuli, represent a known risk with numerous commonly prescribed antibiotics [59] [60]. Simultaneously, artificial intelligence hallucinations, where large language models (LLMs) generate factually incorrect or unsupported information, present emerging challenges in clinical decision support systems [61] [62]. This convergence creates a complex validation landscape where researchers must develop sophisticated methodologies to identify and mitigate both phenomena to ensure patient safety and prescription accuracy.
The validation of LLMs for antibiotic prescribing requires particular vigilance due to this unique intersection. As these models are increasingly deployed to support complex clinical decisions, understanding both the neurological adverse effects of medications and the algorithmic generation of inaccurate information becomes fundamental to developing safe, effective clinical AI tools [21] [12]. This guide systematically compares experimental approaches for identifying and mitigating these parallel challenges in treatment recommendation systems.
Clinical Hallucinations: Antibiotic-Induced Neurotoxicity Profiles
Epidemiological Evidence and Risk Assessment
Antibiotic-induced neuropsychiatric adverse events, including hallucinations, delirium, and psychosis, are more prevalent than historically recognized. A comprehensive analysis of the U.S. FDA Adverse Event Reporting System (FAERS) revealed that among 183,265 antibiotic-related adverse event reports, 1.6% documented psychotic symptoms, with prevalence varying from 0.3% to 3.8% across different antibiotics [60]. This study identified 15 individual antibiotics with significantly increased odds of psychosis compared to minocycline, which served as a control due to its potential neuroprotective properties.
Table 1: Antibiotics Associated with Psychosis Risk Based on FAERS Data Analysis
| Antibiotic Class | Specific Agents | Odds Ratio for Psychosis | Primary Symptom Profile |
|---|---|---|---|
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | 6.11 | Psychosis, hallucinations [60] |
| Macrolides | Azithromycin, Clarithromycin, Erythromycin | 7.04 | Hallucinations (63% of cases) [63] |
| Penicillins | Amoxicillin, Amoxicillin/Clavulanate | 2.15 | Seizures (38% of cases) [63] |
| Cephalosporins | Cefepime, Ceftriaxone, Cefuroxime | 2.25 | Seizures (35% of cases) [63] |
| Tetracyclines | Doxycycline | 2.32 | Psychosis symptoms [60] |
| Sulfonamides | SMX/TMP | 1.81 | Hallucinations (68% of cases) [63] |
Clinical Presentation and Temporal Patterns
Antibiotic-induced neurotoxicity manifests in distinct clinical patterns, which researchers should incorporate into validation frameworks. Bhattacharyya et al. (2016) classified these into three primary phenotypes based on systematic review of case reports spanning seven decades [63] [64]:
Type 1 (Seizure-predominant): Characterized by seizures occurring within days of antibiotic initiation, most commonly associated with penicillins and cephalosporins, particularly in patients with renal impairment.
Type 2 (Psychosis-predominant): Presenting with delusions or hallucinations (47% of cases), most frequently associated with sulfonamides, fluoroquinolones, and macrolides, with rapid onset following drug initiation.
Type 3 (Cerebellar-predominant): Associated exclusively with metronidazole, featuring delayed onset (weeks), cerebellar dysfunction, and abnormal brain imaging findings.
The temporal relationship between antibiotic initiation and symptom onset provides crucial diagnostic information. Types 1 and 2 typically manifest within days of drug initiation and resolve rapidly upon discontinuation, while Type 3 demonstrates longer latency and resolution periods [64].
LLM Hallucinations in Treatment Recommendations
Typology and Prevalence in Medical Contexts
In LLM applications for antibiotic prescribing, hallucinations represent a significant threat to patient safety. These inaccuracies are systematically categorized into three distinct types:
Fact-conflicting hallucinations: Generation of information contradicting established medical knowledge (e.g., suggesting antibiotics for viral infections) [62]
Input-conflicting hallucinations: Responses diverging from specific user instructions or provided context (e.g., recommending non-guideline-concordant therapy despite prompt specifying guidelines) [62]
Context-conflicting hallucinations: Self-contradictory outputs within extended interactions, particularly problematic in complex clinical cases requiring multi-step reasoning [62]
The prevalence of LLM hallucinations in publicly available models ranges between 3% and 16% [62], though domain-specific applications in medicine may demonstrate different error profiles. In antibiotic prescribing contexts, studies have documented concerning patterns. For instance, when evaluating LLM performance in bloodstream infection management, 36% of targeted therapy recommendations were inappropriate, with 5% classified as potentially harmful to patients [12].
Experimental Protocols for Detection and Validation
Table 2: Methodologies for Evaluating LLM Performance in Antibiotic Prescribing
| Evaluation Dimension | Experimental Protocol | Key Metrics | Study Examples |
|---|---|---|---|
| Appropriateness Assessment | Retrospective case analysis with expert validation | Percentage of appropriate empirical and targeted therapy recommendations | Maillard et al.: 64% appropriate empirical, 36% appropriate targeted therapy [12] |
| Guideline Adherence | Prompt engineering with clinical scenarios; comparison with IDSA/ESCMID guidelines | Adherence rates to specific guideline recommendations | Fisch et al.: 38% correct empirical antibiotic type selection [12] |
| Harm Potential Classification | Multidisciplinary review of LLM recommendations with harm categorization | Percentage of recommendations classified as potentially harmful | Maillard et al.: 2-5% potentially harmful recommendations [12] |
| Output Consistency | Repeated querying with identical clinical scenarios across multiple sessions | Response heterogeneity across sessions | Fisch et al.: Significant variability across LLMs and sessions [12] |
Mitigation Strategies: From Technical Solutions to Clinical Validation
Technical Mitigation Frameworks for LLM Hallucinations
Several advanced techniques have emerged to reduce hallucination frequency in LLM applications:
Retrieval-Augmented Generation (RAG) enhances factual accuracy by integrating external knowledge sources into the generation process. This methodology combines information retrieval with LLM capabilities, though challenges persist with negative rejection (failure to reject false information) and information integration [61] [62]. Specialized benchmarks like the Retrieval-Augmented Generation Benchmark (RGB) and RAGTruth have been developed specifically to quantify and address these limitations [62].
Advanced Prompt Engineering employs structured approaches to improve output quality. The chain-of-thought technique forces models to articulate intermediate reasoning steps before final recommendations, while few-shot prompting provides exemplars of appropriate responses [62]. Effective prompt structures typically include three components: role definition and objective, task-specific guidelines, and explicit output formatting with examples [65].
Parameter Tuning and Constraint Implementation reduces stochastic outputs through technical controls. Key parameters include:
- Temperature setting: Lower values (closer to 0) reduce creativity and increase determinism
- Max_Token limitation: Constraining output length minimizes irrelevant content
- Domain classification: Pre-filtering queries to appropriate knowledge domains prevents cross-contamination [65]
Clinical Validation Methodologies
Rigorous clinical validation frameworks are essential for deploying LLM systems in antibiotic prescribing. Recommended protocols include:
Structured Scenario Testing utilizing retrospective clinical cases with multidisciplinary expert review. This approach should assess both appropriateness (guideline concordance) and potential harm, with special attention to antibiotic spectrum adequacy, dosing accuracy, and patient-specific contraindications [12].
Cross-Session Consistency Evaluation through repeated querying with identical clinical scenarios to assess output stability. Significant heterogeneity in recommendations across sessions, as observed in multiple studies [12], raises concerns about reliability in clinical practice.
Comprehensive Workflow Integration that positions LLMs within complete clinical reasoning processes rather than isolated decision points. This includes evaluating model performance across the dynamic phases of antibiotic prescribing, from empirical treatment through de-escalation based on culture results [21].
Figure 1: Comprehensive Validation Workflow for LLM Antibiotic Recommendations
Table 3: Research Reagent Solutions for Hallucination Mitigation Studies
| Tool Category | Specific Solution | Research Application | Key Features |
|---|---|---|---|
| Evaluation Benchmarks | Retrieval-Augmented Generation Benchmark (RGB) | Quantifying hallucination frequency in RAG systems | Four specialized testbeds for key skills; English and Chinese evaluation [62] |
| Specialized Datasets | RAGTruth | Fine-grained hallucination analysis at word level | ~18,000 authentic LLM responses; word-level hallucination annotation [62] |
| Clinical Validation Tools | IDSA/ESCMID Guideline Concordance Metrics | Assessing appropriateness of antibiotic recommendations | Standardized evaluation against established guidelines [12] |
| Harm Classification Framework | Multidisciplinary Expert Panel Review | Categorizing potential patient harm from recommendations | Binary classification (harmful/not harmful) with specific examples [12] |
| Temporal Analysis Tools | FDA Adverse Event Reporting System (FAERS) | Investigating clinical hallucination patterns | 2955 psychosis ADRs across 23 antibiotics; odds ratio calculations [60] |
The parallel challenges of clinical and artificial intelligence hallucinations in treatment recommendations demand sophisticated, multi-dimensional validation approaches. Successful mitigation requires integration of technical solutions like RAG and advanced prompt engineering with robust clinical validation against established guidelines and harm evaluation frameworks. Future research must prioritize consistency across sessions, appropriate handling of clinical uncertainty, and explicit accounting for antibiotic-specific neurotoxicity risks. As LLM integration in clinical settings accelerates, the development of comprehensive validation workflows that address both forms of "hallucination" will be essential for patient safety and the responsible implementation of AI in medical decision-making.
Performance Variability Across Models and Clinical Scenarios
The integration of large language models (LLMs) into clinical decision-making represents a significant advancement in healthcare technology, particularly in the complex domain of antibiotic prescribing. As antimicrobial resistance continues to pose a global threat, the need for accurate, consistent, and reliable decision support tools becomes increasingly critical [66]. This comparison guide objectively evaluates the performance variability of commercially available LLMs across different clinical scenarios, with specific focus on antibiotic prescribing accuracy. The analysis synthesizes findings from recent comparative studies to provide researchers, scientists, and drug development professionals with comprehensive experimental data and methodological insights essential for the validation of LLMs in clinical applications.
Comparative Performance Data
Antibiotic Prescribing Accuracy Across LLMs
Recent research has revealed substantial variability in LLM performance for antibiotic prescribing decisions. The following table summarizes key performance metrics across models based on a comprehensive evaluation of 60 clinical cases covering 10 infection types [1] [9].
Table 1: Antibiotic Prescribing Performance Across LLMs
| LLM Model | Prescription Accuracy (%) | Dosage Correctness (%) | Duration Adequacy (%) | Incorrect Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information missing | 1.7 |
| Perplexity Pro | Information missing | 90.0 | Information missing | Information missing |
| Claude 3.5 Sonnet | Information missing | 91.7 | Information missing | Information missing |
| Gemini | Lowest accuracy | Information missing | 75.0 | Information missing |
| Claude 3 Opus | Lowest accuracy | Information missing | Information missing | Information missing |
The data reveals that ChatGPT-o1 demonstrated superior performance in both prescription accuracy and dosage correctness, while Gemini showed strength in recommending appropriate treatment durations despite overall lower prescription accuracy [1]. Claude 3.5 Sonnet exhibited a tendency to over-prescribe treatment duration, highlighting important model-specific limitations [9].
Performance Degradation in Complex Cases
A critical finding across studies was the significant performance decline observed with increasing case complexity. LLMs demonstrated notably reduced accuracy when confronted with difficult-to-treat microorganisms and complex clinical presentations [1]. This performance degradation underscores the importance of evaluating LLMs across a spectrum of clinical challenges rather than relying solely on overall accuracy metrics.
Table 2: Performance Consistency Across Clinical Scenarios
| Clinical Scenario Type | Model Consistency | Inter-Model Agreement | Key Limitations |
|---|---|---|---|
| Routine antibiotic prescribing | Variable (71.7% accuracy for best performer) | Significant variability | Declining accuracy with complex cases |
| Drug-drug interaction identification | Claude 3: 100%, GPT-4: 93.3%, Gemini: 80.0% | Moderate variability | Potential harmful recommendations identified |
| Nuanced inpatient management | Internal consistency as low as 0.60 | Divergent recommendations in all scenarios | Models changed recommendations upon repeated prompting |
Experimental Methodologies
Antibiotic Prescribing Evaluation Protocol
The primary study evaluating antibiotic prescribing accuracy employed a rigorous methodology [1] [9]. Fourteen LLMs, including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai, were evaluated using 60 clinical cases with antibiograms covering 10 infection types. A standardized prompt was used for antibiotic recommendations focusing on drug choice, dosage, and treatment duration. Responses were anonymized and reviewed by a blinded expert panel assessing antibiotic appropriateness, dosage correctness, and duration adequacy. This process generated 840 responses for comprehensive analysis.
Drug-Drug Interaction Identification Protocol
A separate study evaluated LLM capability to identify clinically relevant drug-drug interactions (DDIs) and generate high-quality clinical pharmacotherapy recommendations [67]. The researchers created 15 patient cases with medication regimens, each containing a commonly encountered DDI. The study included two phases: (1) DDI identification and determination of clinical relevance, and (2) DDI identification and generation of a clinical recommendation. The primary outcome was the ability of the LLMs (GPT-4, Gemini 1.5, and Claude-3) to identify the DDI within each medication regimen, with secondary outcomes including ability to identify clinical relevance and generate high-quality recommendations relative to ground truth.
Clinical Decision Variability Assessment
To assess LLM behavior in ambiguous clinical scenarios, a cross-sectional simulation study examined how models handled nuanced inpatient management decisions [68] [69]. Four brief vignettes requiring binary management decisions were posed to each model in five independent sessions. The scenarios included: (1) transfusion at borderline hemoglobin, (2) resumption of anticoagulation after gastrointestinal bleed, (3) discharge readiness despite a modest creatinine rise, and (4) peri-procedural bridging in a high-risk patient on apixaban. Six LLMs were queried: five general-purpose (GPT-4o, GPT-o1, Claude 3.7 Sonnet, Grok 3, and Gemini 2.0 Flash) and one domain-specific (OpenEvidence).
Visualization of Experimental Workflows
LLM Evaluation Workflow - This diagram illustrates the systematic approach used to evaluate LLM performance across clinical scenarios, highlighting key stages from case preparation through blinded expert assessment.
Variability Assessment Methodology - This visualization outlines the approach for measuring both internal consistency (within models) and inter-model agreement (between different models) across clinical scenarios.
Research Reagent Solutions
Table 3: Essential Research Materials for LLM Clinical Validation
| Research Component | Function/Purpose | Implementation Example |
|---|---|---|
| Clinical Case Repository | Provides standardized scenarios for model evaluation | 60 clinical cases with antibiograms covering 10 infection types [1] |
| Standardized Prompt Template | Ensures consistency in model queries | Fixed prompt structure for antibiotic recommendations focusing on drug choice, dosage, and treatment duration [1] |
| Blinded Expert Panel | Objective assessment of model recommendations | Independent review of anonymized LLM responses for appropriateness, correctness, and adequacy [1] |
| Antibiogram Integration | Contextualizes recommendations based on local resistance patterns | Inclusion of susceptibility data in clinical cases to guide appropriate antibiotic selection [1] |
| Drug Interaction Database | Ground truth for DDI identification assessment | Curated patient cases containing commonly encountered clinically relevant drug interactions [67] |
The comprehensive evaluation of LLMs across clinical scenarios reveals significant performance variability both between models and across different clinical contexts. ChatGPT-o1 currently demonstrates superior performance in antibiotic prescribing accuracy, while other models show strengths in specific domains such as treatment duration recommendations. The substantial performance degradation observed in complex cases, combined with concerning internal inconsistencies in nuanced clinical decision-making, highlights the necessity for careful model validation and selective application. These findings underscore that while advanced LLMs show promise as clinical decision-support tools, they require rigorous scenario-specific testing, ongoing performance monitoring, and appropriate human oversight to ensure safe and effective implementation in healthcare environments. Future development should focus on improving model consistency, enhancing performance in complex cases, and establishing standardized validation frameworks that can keep pace with the rapid evolution of language model capabilities.
Accuracy Decline with Case Complexity and Difficult-to-Treat Pathogens
The integration of large language models (LLMs) into clinical decision-support systems offers a promising avenue for improving antibiotic prescribing practices, a cornerstone of antimicrobial stewardship. However, their performance is not uniform across all clinical scenarios. A critical challenge emerging from recent research is a significant decline in the accuracy of LLM-generated antibiotic recommendations as case complexity increases and when infections involve difficult-to-treat pathogens. This analysis objectively compares the performance of various LLMs under these demanding conditions, providing researchers and clinicians with experimental data essential for critical evaluation.
Comparative Performance of LLMs in Complex Prescribing
Recent benchmark studies reveal substantial variability in the antibiotic prescribing accuracy of different LLMs. The following table summarizes the overall performance of leading models across key prescribing metrics, which provides a baseline for understanding their degradation in complex cases.
Table 1: Overall Antibiotic Prescribing Accuracy of Select LLMs [9]
| Large Language Model | Overall Antibiotic Appropriateness | Dosage Correctness | Treatment Duration Adequacy |
|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 96.7% (58/60) | Information Missing |
| Perplexity Pro | Information Missing | 90.0% (54/60) | Information Missing |
| Claude 3.5 Sonnet | Information Missing | 91.7% (55/60) | Information Missing |
| Gemini | Information Missing | Information Missing | 75.0% (45/60) |
| Claude 3 Opus | Lowest Accuracy | Information Missing | Information Missing |
A comprehensive study evaluating 14 LLMs across 60 clinical cases with antibiograms found that ChatGPT-o1 demonstrated the highest overall accuracy in antibiotic choice. However, the same study identified a critical vulnerability: "Performance declined with increasing case complexity, particularly for difficult-to-treat microorganisms" [9]. This indicates that the performance data in Table 1 represents a best-case scenario that may not hold in challenging clinical environments.
This decline in performance is not isolated to antibiotic prescribing. Evaluations of LLMs in general clinical problem-solving, such as the medical Abstraction and Reasoning Corpus (mARC-QA) benchmark, have found that models including GPT-4o, o1, Gemini, and Claude perform poorly on problems requiring flexible reasoning, often demonstrating a lack of commonsense medical reasoning and a propensity for overconfidence despite limited accuracy [23].
Experimental Protocols for Evaluating LLM Prescribing Accuracy
To critically assess the findings on accuracy decline, it is essential to understand the methodologies employed in the key benchmarking studies.
Methodology: LLM Comparison in Antibiotic Prescribing
A major study conducted a direct comparison of 14 LLMs using a standardized evaluation framework [9]:
- Case Selection: 60 clinical cases covering 10 distinct infection types, complete with institutional antibiograms to reflect local resistance patterns.
- Model Prompting: A standardized prompt was used for all LLMs to request antibiotic recommendations, focusing on drug choice, dosage, and treatment duration.
- Blinded Expert Review: An expert panel, blinded to the LLM source of each recommendation, assessed the appropriateness of the antibiotic choice, dosage correctness, and duration adequacy.
- Analysis: A total of 840 responses were collected and analyzed for performance metrics and their relationship to case complexity.
Methodology: Evaluation of Clinical Reasoning Flexibility
The mARC-QA benchmark was specifically designed to probe failure modes in LLM clinical reasoning [23]:
- Question Design: 100 questions were crafted to resist memorization or pattern matching from existing medical question-answer benchmarks. The design incorporated manipulations such as:
- Familiar-cue with hard counterevidence: Featuring high-frequency lexical cues paired with decisive evidence that invalidates the stereotyped diagnostic completion.
- Information-sufficiency gating: Including an explicit "seek additional information" option to test adaptive information-seeking.
- Human Comparison: Performance of five physician test-takers (averaging 66% accuracy) was compared to various LLMs.
- Evaluation Conditions: Chain-of-thought prompting was used for all LLM evaluations, with a temperature of zero to ensure reproducibility.
Visualizing the Experimental Workflow
The following diagram illustrates the standardized methodology used to evaluate and compare LLM performance in antibiotic prescribing, from case preparation to final analysis.
The Researcher's Toolkit
To facilitate replication and further investigation of LLM performance in antimicrobial prescribing, the following table details key reagents and resources referenced in the foundational studies.
Table 2: Essential Research Reagents and Resources [9] [23]
| Reagent/Resource | Function in Experimental Context | Example/Specification |
|---|---|---|
| Clinical Case Scenarios | Serves as the standardized input for evaluating LLM performance across a spectrum of complexity and infection types. | 60 cases covering 10 infection types, with associated antibiograms [9]. |
| Institutional Antibiograms | Provides local antimicrobial resistance patterns essential for assessing context-aware, appropriate prescribing. | Institution-specific data on bacterial susceptibility and resistance profiles [9]. |
| mARC-QA Benchmark | A specialized question set designed to test flexible clinical reasoning and identify failure modes by exploiting cognitive biases like the Einstellung effect. | 100 USMLE-style questions with manipulations (e.g., cue conflict, information-sufficiency gating) [23]. |
| Blinded Expert Panel | Provides the gold-standard assessment of LLM output quality, ensuring unbiased evaluation of recommendation appropriateness. | Multidisciplinary experts reviewing anonymized LLM responses [9]. |
| Structured Prompt Template | Ensures consistency in LLM queries, allowing for fair comparison between different models by controlling input variables. | A standardized prompt format used across all evaluated LLMs [9]. |
The collective evidence indicates that while advanced LLMs like ChatGPT-o1 show promising overall accuracy in antibiotic prescribing, this performance is context-dependent and degrades significantly when faced with complex cases and difficult-to-treat pathogens. This decline is symptomatic of broader limitations in flexible clinical reasoning, as demonstrated by poor performance on specialized benchmarks like mARC-QA. For researchers and drug development professionals, these findings underscore the necessity of rigorous, context-rich validation that moves beyond aggregate performance metrics to stress-test models against the complex realities of clinical practice. The path toward reliable clinical decision support must include a focused effort on improving model reasoning in precisely these high-stakes, complex scenarios.
FDA Regulatory Considerations for AI Clinical Decision Support
The integration of Artificial Intelligence (AI) into Clinical Decision Support (CDS) tools represents a transformative shift in modern healthcare, offering the potential to enhance the accuracy and efficiency of clinician decision-making at the point of care [70]. In the United States, the Food and Drug Administration (FDA) is the primary federal agency responsible for regulating AI-enabled medical devices to ensure they demonstrate a reasonable assurance of safety and effectiveness [71]. The regulatory framework is particularly critical for high-stakes applications such as antibiotic prescribing, where the promise of large language models (LLMs) must be balanced with rigorous validation and oversight. As of July 2025, the FDA's public database lists over 1,250 AI-enabled medical devices authorized for marketing in the United States, a significant increase from the approximately 950 devices recorded in August 2024 [71]. This rapid growth underscores the importance of understanding the specific regulatory pathways and considerations that apply to AI-CDS, especially those powered by advanced generative AI and LLMs.
The FDA's regulatory approach is based on the Federal Food, Drug, and Cosmetic Act, which defines AI as a medical device when it is intended for use in the "diagnosis, cure, mitigation, treatment, or prevention of disease" [71]. The agency employs a risk-based framework for oversight, requiring more rigorous testing and review for higher-risk devices. For AI-CDS software, two main regulatory categories exist: Software as a Medical Device (SaMD), which is standalone software for medical purposes, and Software in a Medical Device (SiMD), which is part of a physical medical device [71]. Understanding these distinctions is fundamental for developers and researchers working to bring AI-powered clinical tools to market.
FDA Regulatory Pathways for AI-enabled Devices
Determining FDA Jurisdiction and Risk Classification
Not all AI-based clinical tools fall under FDA regulation. The 21st Century Cures Act of 2016 narrowed the FDA's authority by excluding certain CDS software from the definition of a medical device if it is designed to support—not replace—clinical decision-making and allows providers to independently review the basis for recommendations [71]. The FDA exercises "enforcement discretion" for tools that technically meet the device definition but pose low risk, meaning it does not require manufacturers to submit premarket review applications [71]. This often applies to software supporting general wellness or self-management.
For AI-CDS that does require regulation, the FDA applies a three-tiered risk classification system:
- Class I (Low Risk): Devices with minimal potential for harm (e.g., static tools like tongue depressors).
- Class II (Moderate Risk): Devices that present some risk and generally require clinical oversight. Most AI-enabled devices, including many CDS tools, fall into this category.
- Class III (High Risk): Life-sustaining devices or those posing significant risk, requiring the most rigorous review [71].
Most AI-enabled CDS tools are regulated as Class II devices, necessitating either 510(k) clearance or De Novo classification. The specific pathway depends on whether a substantially equivalent "predicate" device already exists in the market.
Premarket Authorization Pathways
The table below summarizes the primary regulatory pathways for AI-enabled medical devices:
| Pathway | When Used | Key Features | Relevance to AI-CDS |
|---|---|---|---|
| 510(k) Clearance | For devices "substantially equivalent" to a legally marketed predicate device [71]. | Demonstrates safety and effectiveness by comparison to an existing device; typically requires performance validation. | Common pathway for AI-CDS with established predicates; may require clinical validation studies. |
| De Novo Classification | For novel devices of low to moderate risk with no predicate device [71]. | Establishes a new device classification; creates a potential predicate for future 510(k) submissions. | Appropriate for first-of-its-kind AI-CDS that introduces novel functionality or technology. |
| Premarket Approval (PMA) | For high-risk (Class III) devices that support or sustain human life or present substantial risk [71]. | Most stringent pathway; requires sufficient scientific evidence to assure safety and effectiveness. | Required for high-stakes AI-CDS where errors could cause serious harm to patients. |
The FDA has modernized its approach to accommodate the unique characteristics of AI technologies through several key initiatives. The Total Product Life Cycle (TPLC) approach assesses devices across their entire lifespan—from design and development to deployment and postmarket monitoring [71]. This is particularly important for adaptive AI models that may evolve after authorization. The Good Machine Learning Practice (GMLP) principles, developed with international partners, provide ten guiding principles emphasizing transparency, data quality, and ongoing model maintenance [71].
A significant regulatory development is the Predetermined Change Control Plan (PCCP), which allows manufacturers to outline planned modifications to AI models—such as retraining with new data or performance enhancements—and have them pre-authorized, facilitating iterative improvement without requiring a new submission for every change [71] [72]. This approach acknowledges that AI models are not static but can learn and improve from real-world experience.
Performance Comparison of LLMs for Antibiotic Prescribing
Experimental Protocol for LLM Evaluation
A 2025 comparative study evaluated the antibiotic prescribing accuracy of fourteen large language models across diverse clinical scenarios [9] [1]. The research employed a rigorous methodology to ensure unbiased, clinically relevant results:
- Model Selection: The study evaluated standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai—fourteen LLMs in total [1].
- Clinical Case Design: Researchers developed 60 clinical cases covering 10 different infection types, accompanied by relevant antibiograms (antimicrobial susceptibility testing results) [9] [1].
- Standardized Prompting: A standardized prompt was used for all antibiotic recommendations to ensure consistency across model evaluations. The prompt focused on generating recommendations for drug choice, dosage, and treatment duration [1].
- Blinded Expert Review: Model responses were anonymized and reviewed by a blinded expert panel that assessed three key dimensions: antibiotic appropriateness, dosage correctness, and treatment duration adequacy [9] [1].
- Data Analysis: A total of 840 responses were collected and analyzed (14 models × 60 cases) to determine performance patterns and statistical significance [1].
This experimental workflow can be visualized as follows:
Comparative Performance Results
The study revealed significant variability in LLM performance for antibiotic prescribing. The table below summarizes the key quantitative findings:
| Large Language Model | Antibiotic Appropriateness (%) | Dosage Correctness (%) | Duration Adequacy (%) | Key Performance Notes |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 96.7% (58/60) | Not Reported | Highest overall accuracy; only 1 incorrect recommendation (1.7%) [9]. |
| Perplexity Pro | Not Reported | 90.0% (54/60) | Not Reported | Second-highest dosage accuracy [9]. |
| Claude 3.5 Sonnet | Not Reported | 91.7% (55/60) | Not Reported | Demonstrated tendency to over-prescribe treatment duration [9]. |
| Gemini | Lowest Accuracy | Not Reported | 75.0% (45/60) | Lowest antibiotic appropriateness but highest duration adequacy [9]. |
| Claude 3 Opus | Lowest Accuracy | Not Reported | Not Reported | Among the poorest performers for antibiotic appropriateness [9]. |
The research yielded several critical insights for regulatory consideration and clinical implementation. First, model performance declined with increasing case complexity, particularly for infections caused by difficult-to-treat microorganisms [9]. This performance gradient underscores the importance of context-specific validation rather than relying on general performance metrics. Second, the significant variability among LLMs in prescribing appropriate antibiotics, dosages, and treatment durations highlights that these technologies cannot be treated as a homogeneous category from a regulatory perspective [1]. Each model architecture and training approach may yield substantially different performance characteristics in clinical settings.
Most importantly, the study demonstrated that while advanced LLMs like ChatGPT-o1 show promise as decision-support tools for antibiotic prescribing, their inconsistencies and decreased accuracy in complex cases emphasize the need for careful validation before clinical utilization [9]. This aligns with the FDA's risk-based approach and underscores why regulatory oversight is essential for AI-CDS tools intended to influence treatment decisions.
Researchers developing and evaluating AI-based clinical decision support systems require specific methodological tools and frameworks. The table below details essential components of the research toolkit for validating AI-CDS, particularly in antibiotic prescribing:
| Research Tool | Function & Application | Regulatory Importance |
|---|---|---|
| Clinical Case Repository | A curated set of clinical scenarios representing diverse patient presentations, infection types, and complexity levels [9]. | Provides standardized basis for performance evaluation; essential for external validation. |
| Antibiogram Data | Local or institutional antimicrobial susceptibility testing results that inform appropriate antibiotic selection [1]. | Ensures recommendations reflect local resistance patterns; critical for ecological validity. |
| Standardized Prompt Framework | Consistent input format and structure for querying LLMs to enable comparable responses across models [1]. | Reduces variability in evaluation; supports reproducibility of validation studies. |
| Blinded Expert Review Panel | Multidisciplinary clinical experts who assess model outputs without knowledge of the source model [9]. | Provides gold-standard assessment of appropriateness; minimizes assessment bias. |
| Good Machine Learning Practice (GMLP) | FDA-endorsed principles for ensuring safe and effective AI, emphasizing data quality and representativeness [71]. | Framework for developing models that meet regulatory expectations for safety and effectiveness. |
| Predetermined Change Control Plan (PCCP) | A structured plan outlining how an AI model will evolve over time while maintaining safety and performance [71] [72]. | Enables continuous improvement of AI-CDS within a controlled regulatory framework. |
The regulatory landscape for AI-based Clinical Decision Support is evolving rapidly as the FDA adapts its traditional device regulation paradigms to accommodate adaptive AI and machine learning technologies [72]. For antibiotic prescribing applications and other high-stakes clinical decisions, the combination of robust performance validation and thoughtful regulatory strategy is essential. The recent comparative research on LLMs demonstrates that while some models show promising accuracy, significant variability exists, and performance degrades with case complexity—highlighting the critical need for rigorous, context-specific validation [9] [1].
Researchers and developers should integrate regulatory considerations early in the AI-CDS development process. This includes adopting Good Machine Learning Practices, planning for lifecycle management through Predetermined Change Control Plans, and designing validation studies that reflect real-world clinical complexity [71] [72]. As the FDA continues to refine its approach to AI-enabled devices—including emerging technologies like foundation models and large language models—maintaining a focus on clinically meaningful improvements in patient care will remain paramount [70] [73]. The successful integration of AI into clinical decision-making will depend not only on technological capabilities but also on establishing trust through transparent validation and appropriate regulatory oversight.
Data Leakage and Privacy Concerns in Model Deployment
The deployment of Large Language Models (LLMs) in clinical settings, such as antibiotic prescribing, introduces significant data leakage and privacy risks. As LLMs process vast amounts of sensitive patient information, understanding and mitigating these vulnerabilities becomes paramount for maintaining patient confidentiality and regulatory compliance. Data leakage in LLMs can occur through multiple vectors, including prompt manipulation, model training data exposure, and inference-time leaks, each posing unique challenges for healthcare applications [74]. These risks are particularly concerning in antimicrobial stewardship, where LLMs must access detailed patient records to provide appropriate therapeutic recommendations while safeguarding protected health information.
The integration of LLMs into electronic health records and clinical decision support systems demands a privacy-first approach to architecture design. With the average cost of a data breach reaching $4.88 million according to 2024 reports, and 15% of employees regularly sharing sensitive data with AI tools, implementing robust Data Leakage Prevention (DLP) strategies is no longer optional but essential for secure clinical deployment [74].
Understanding Data Leakage Vulnerabilities in LLMs
Primary Data Leakage Pathways
LLMs present several distinct data leakage vulnerabilities that clinical researchers must address:
System Prompt Leakage: The system prompts used to steer LLM behavior may contain sensitive information, including database credentials, API keys, internal rules, or filtering criteria. When disclosed, this information can help attackers bypass security controls [75]. In a clinical context, a system prompt might inadvertently reveal decision-making rules for antibiotic selection or patient triage criteria.
Training Data Leakage: LLMs can memorize and reproduce sensitive data from their training sets, potentially exposing patient records or proprietary clinical algorithms [74]. For example, a healthcare LLM might leak specific patient cases from its training data when generating treatment recommendations.
Prompt-Based Leakage: Occurs when users input sensitive data into prompts, which may then be stored, logged, or exposed through model outputs [74]. A study by security provider Cyberhaven found that 4.7% of employees had pasted confidential data into ChatGPT, with 11% of the pasted data being confidential [76].
Model Inversion Attacks: Attackers can exploit model outputs to reconstruct sensitive training data, potentially revealing patient information from a clinical LLM's predictions [74].
Implications for Antimicrobial Stewardship Research
In the context of antibiotic prescribing research, these vulnerabilities present specific challenges:
Exposure of Patient Health Information: Leakage could reveal sensitive patient data, including laboratory results, microbiological data, and treatment responses.
Compromised Clinical Decision Logic: Leakage of system prompts could expose proprietary clinical algorithms, potentially revealing institutional prescribing patterns or decision thresholds.
Regulatory Non-Compliance: Data breaches may violate regulations like HIPAA, GDPR, or CCPA, with significant financial penalties—GDPR violations can incur fines up to €20 million or 4% of annual revenue [74].
Comparative Analysis of LLM Performance in Antibiotic Prescribing
Accuracy in Clinical Recommendations
Recent studies evaluating LLMs for antibiotic prescribing reveal significant variability in performance across models. The following table summarizes key findings from clinical validation studies:
Table 1: LLM Performance in Antibiotic Prescribing Clinical Scenarios
| LLM Model | Overall Appropriateness (%) | Dosage Correctness (%) | Duration Adequacy (%) | Potentially Harmful Suggestions (%) | Study Details |
|---|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Not Specified | 1.7 | 60 clinical cases with antibiograms, 10 infection types [1] |
| ChatGPT-4 | 64 (empirical therapy) | Not Specified | Not Specified | 2 (empirical), 5 (targeted) | 44 retrospective BSI cases [12] |
| Perplexity Pro | Not Specified | 90.0 | Not Specified | Not Specified | Same 60-case evaluation [1] |
| Claude 3.5 Sonnet | Not Specified | 91.7 | Over-prescription tendency | Not Specified | Same 60-case evaluation [1] |
| Gemini | Lowest accuracy | Not Specified | 75.0 | Not Specified | Same 60-case evaluation [1] |
| Multiple Models (Composite) | 38 (antibiotic type) | ~90 (when correct antibiotic) | Not Specified | Not Specified | 7 LLMs evaluated for meningitis case [12] |
Performance Trends and Clinical Implications
The comparative data reveals several important patterns for clinical researchers:
Performance Variability: Significant differences exist between models, with ChatGPT-o1 demonstrating the highest overall accuracy (71.7%) in antibiotic appropriateness, while Gemini showed the lowest accuracy among tested models [1].
Complexity Impact: Performance consistently declines with increasing case complexity, particularly for infections involving difficult-to-treat microorganisms [1].
Dosage vs. Selection Accuracy: Most models demonstrate higher accuracy in dosage calculation than antibiotic selection, suggesting that LLMs may serve better as dosage calculators rather than primary selection tools.
Session Inconsistency: The same LLM may provide different recommendations across multiple sessions when presented with identical cases, highlighting reliability concerns for clinical use [12].
Experimental Protocols for LLM Validation in Clinical Settings
Standardized Clinical Case Evaluation
Researchers have developed methodological frameworks for evaluating LLM performance in antibiotic prescribing:
Diagram 1: LLM Clinical Validation Workflow
The standardized evaluation protocol involves several critical phases:
Case Selection: Curating clinical cases that represent diverse infection types, complexity levels, and patient populations. For example, Maillard et al. used 44 retrospective cases of bloodstream infection, providing anonymized information available to clinicians during original consultations [12].
Prompt Design: Creating standardized prompts that contextualize the clinical scenario. Researchers typically frame the LLM's role (e.g., "act as an infectious diseases specialist") and provide structured patient information [12].
Blinded Assessment: Utilizing independent expert panels not involved in the original patient care to evaluate response appropriateness based on established guidelines like IDSA and ESCMID standards [12].
Harm Classification: Categorizing potential patient harm from inappropriate recommendations, such as narrowing antibiotic spectrum inadequately in immunocompromised patients [12].
Multi-Session Reliability Testing
To address consistency concerns, researchers like Fisch et al. presented the same clinical case to each LLM across three separate sessions, evaluating response variability in addition to accuracy [12]. This approach helps quantify reliability—a critical factor for clinical implementation where consistent recommendations are essential.
Mitigation Strategies for Data Leakage in Clinical LLMs
Comprehensive Data Protection Framework
Implementing effective data leakage prevention requires a multi-layered security approach:
Diagram 2: Data Leakage Mitigation Framework
Technical Safeguards and Best Practices
Based on OWASP guidelines and security research, clinical LLM deployments should implement these specific mitigation strategies:
Strict Access Controls: Implement Role-Based Access Control (RBAC), Multi-Factor Authentication (MFA), and zero-trust architectures to prevent unauthorized access to LLM interfaces and APIs [76] [74].
Data Minimization: Only collect essential data needed for clinical decision-making and avoid storing sensitive information longer than necessary [76]. This is particularly important for antibiotic prescribing, where relevant clinical data can be extracted without retaining complete patient records.
Input Validation and Sanitization: Deploy input controls to block sensitive data patterns (e.g., specific patient identifiers) and use redaction tools to anonymize data before processing [74]. Replace direct patient identifiers with placeholders like
[PATIENT_ID]in prompts.Secure Model Training: Apply differential privacy and synthetic data generation techniques to minimize memorization of real patient data during model training or fine-tuning [74].
Real-time Monitoring: Implement DLP tools that monitor prompts and outputs for sensitive data patterns, with alert systems for anomalous access patterns or data detection [74].
Essential Research Reagents and Tools for Secure LLM Validation
Table 2: Research Reagents for LLM Clinical Validation Studies
| Tool Category | Specific Examples | Primary Function in Research | Security Considerations |
|---|---|---|---|
| Proprietary LLM APIs | GPT-4.1, Claude 3.7, Gemini 2.5 Pro | Benchmark performance comparison against established models | Ensure data processing agreements; avoid transmitting actual PHI |
| Open-Source Models | Llama 3.3, DeepSeek V3 | Enable private deployment and customization | Self-hosting eliminates third-party data sharing risks |
| Evaluation Frameworks | Custom assessment protocols, Blinded expert panels | Standardized performance measurement across models | Anonymize case data before expert review |
| Security Testing Tools | Prompt injection testing frameworks, DLP solutions | Identify vulnerability to data leakage attacks | Implement in isolated test environments first |
| Privacy-Enhancing Technologies (PETs) | Differential privacy libraries, Synthetic data generators | Protect patient privacy during model training | Balance privacy protection with model utility |
| Compliance Management | GDPR/HIPAA assessment checklists, Audit logging systems | Ensure regulatory adherence across jurisdictions | Document all data handling processes |
The validation of LLMs for antibiotic prescribing must encompass both performance accuracy and data security considerations. While models like ChatGPT-o1 demonstrate promising accuracy (71.7% appropriate recommendations), significant concerns remain regarding consistency across sessions and performance degradation with complex cases [1]. These limitations suggest that current LLMs may serve best as clinical decision support tools rather than autonomous prescribing systems.
Furthermore, the evolving data leakage vulnerabilities—including prompt leakage, training data memorization, and model inversion attacks—require robust mitigation frameworks incorporating access controls, data minimization, and continuous monitoring [75] [74]. As regulatory landscapes evolve with initiatives like the EU AI Act and updated ISO standards, clinical researchers must prioritize privacy-by-design principles in LLM validation frameworks [77].
Future research should focus on developing standardized evaluation methodologies that simultaneously assess clinical efficacy and security vulnerabilities, enabling safe translation of LLM technologies into antimicrobial stewardship programs while protecting patient data integrity and confidentiality.
Model Fine-tuning Approaches for Antimicrobial Stewardship
The growing crisis of antimicrobial resistance (AMR) presents a critical challenge to global health systems, with attributable deaths projected to reach 8.2 million annually by 2050 [78]. Antimicrobial stewardship programs (ASPs) have emerged as crucial strategies to optimize antibiotic use, combat resistance, and improve patient outcomes [78] [79]. Within this landscape, large language models (LLMs) and other artificial intelligence (AI) approaches offer transformative potential for enhancing clinical decision-making in infectious diseases [12] [80]. However, general-purpose LLMs frequently demonstrate significant limitations in medical contexts, including unsatisfactory accuracy, severe overprescription tendencies, and insufficient medication knowledge [15]. These challenges have catalyzed the development of specialized fine-tuning approaches to adapt LLMs for the precise demands of antimicrobial stewardship, creating models that can reliably support antibiotic prescribing decisions while adhering to stewardship principles of reducing resistance emergence and ensuring sustainable antibiotic efficacy [21].
The Imperative for Specialized Model Fine-tuning
Limitations of General-Purpose LLMs in Antimicrobial Stewardship
Direct application of off-the-shelf LLMs to antibiotic prescribing reveals consistent performance gaps across multiple studies. General-purpose models exhibit a troubling tendency toward overprescription, with GPT-4 recommending over 80 medications per patient on average—approximately three times the volume prescribed by practicing physicians [15]. This overprescription risk poses significant threats to patient safety and antimicrobial resistance patterns. Evaluation studies further demonstrate variable performance among LLMs in recommending appropriate antibiotic treatments. In an assessment of 14 LLMs across 60 clinical cases, ChatGPT-o1 demonstrated the highest accuracy at 71.7%, while other models like Gemini and Claude 3 Opus showed substantially lower performance [9]. Performance degradation with increasing case complexity presents additional concerns, particularly for infections involving difficult-to-treat microorganisms [9].
Beyond accuracy limitations, fundamental architectural challenges impede direct clinical application of general LLMs. These models typically function as "black boxes" with limited explainability, complicating clinical validation and trust-building among healthcare providers [12]. Their probabilistic nature can generate "hallucinations"—factually incorrect or fabricated information presented coherently—which pose substantial risks in high-stakes clinical decision-making for antibiotic therapy [11]. Additionally, general LLMs often lack systematic incorporation of essential clinical context, such as local resistance patterns, patient-specific contraindications, and institutional guidelines, which are fundamental to appropriate antibiotic selection [78] [81].
Core Principles for Stewardship-Aligned Models
Effective fine-tuning for antimicrobial stewardship must embed core clinical reasoning processes throughout the antibiotic prescribing pathway. This begins with accurate determination of infection likelihood and necessity of empirical therapy, followed by appropriate antibiotic selection based on infection site, severity, expected pathogens, and local resistance patterns [21]. As diagnostic information evolves, models must support dynamic decision-making including escalation, de-escalation, or discontinuation based on culture results, susceptibility profiles, and clinical response [21]. Crucially, stewardship-aligned models must balance individual patient outcomes with broader public health objectives, including reducing selective antibiotic pressure, minimizing healthcare costs, and preserving future antibiotic efficacy through responsible use [21].
Comparative Analysis of Fine-tuning Approaches
Parameter-Efficient Fine-tuning (LAMO Framework)
The Language-Assisted Medication Recommendation (LAMO) framework represents an advanced parameter-efficient fine-tuning approach specifically designed to address overprescription in LLMs [15]. LAMO employs Low-Rank Adaptation (LoRA), which injects trainable low-rank matrices into frozen transformer layers, significantly reducing computational requirements while maintaining performance. A key innovation in LAMO is its mixture-of-expert strategy with medication-aware grouping, where separate LoRA adapters are trained for distinct medication clusters based on therapeutic categories or pharmacological properties.
Table 1: Performance Comparison of Fine-tuning Approaches on MIMIC-III Dataset
| Model Approach | F1 Score | Precision | Recall | Avg. Medications per Patient | Clinical Note Utilization |
|---|---|---|---|---|---|
| General GPT-4 | 0.354 | N/A | N/A | >80 | Limited |
| LAMO (LLaMA-2-7B) | 0.423 | 0.451 | 0.437 | ~12 (physician-aligned) | Comprehensive |
| Traditional SafeDrug | 0.381 | 0.392 | 0.401 | ~13 | Limited |
| MoleRec | 0.395 | 0.411 | 0.419 | ~11 | Limited |
The LAMO framework demonstrates superior performance across multiple validation paradigms. In internal validation on MIMIC-III data, LAMO achieved an F1 score of 0.423, outperforming traditional medication recommendation models including SafeDrug (0.381) and MoleRec (0.395) [15]. Crucially, LAMO reduced the average medications per patient from over 80 (with general GPT-4) to approximately 12, aligning with actual physician prescribing patterns while maintaining comprehensive clinical note analysis capabilities [15]. The model also exhibited exceptional temporal generalization, maintaining performance superiority when validated on MIMIC-IV data despite coding standard evolution from ICD-9 to ICD-10, and strong external generalization across diverse hospital systems in the eICU multi-center dataset [15].
Instruction Tuning for Clinical Contextualization
Instruction-based fine-tuning provides a robust methodology for aligning LLMs with the complex, multi-stage clinical reasoning required for antibiotic prescribing [15]. This approach structures training instances using standardized clinical templates comprising Task Instruction (describing the recommendation task), Task Input (structured clinical context and candidate medication), and Instruction Output (binary prescription decision) [15]. This formulation enables LLMs to learn context-sensitive medication decisions through exposure to diverse clinical scenarios.
Instruction tuning specifically addresses the "expertise paradox" in clinical AI implementation, where less-experienced clinicians potentially benefit most from LLM assistance but may lack the specialized knowledge to identify model errors or hallucinations [11]. By embedding structured clinical reasoning patterns directly into the model, instruction tuning creates more reliable outputs accessible to non-specialists while maintaining expert-level oversight requirements for complex cases [11]. This approach has demonstrated particular utility for ASPs in resource-limited settings, where infectious disease specialists are often unavailable [78] [80].
Machine Learning for Predictive Antibiotic Susceptibility
Machine learning (ML) approaches enable creation of "personalized antibiograms" that predict antibiotic resistance based on patient-specific factors rather than institutional averages [81]. LightGBM models trained on structured electronic health record (EHR) data incorporate demographics, vital signs, comorbidities, prior antibiotic use, hospitalizations, and patient-specific microbiological history to predict susceptibility for individual antibiotics [81].
Table 2: Performance of ML-Based Antibiotic Resistance Prediction Models (AUROC)
| Antibiotic | LightGBM AUROC | Logistic Regression AUROC | Key Predictive Features |
|---|---|---|---|
| Cefazolin | 0.77 | 0.71 | Prior resistance, recent antibiotic use |
| Ceftriaxone | 0.76 | 0.69 | Prior resistance, comorbidities |
| Cefepime | 0.74 | 0.68 | Age, prior hospitalizations |
| Piperacillin/tazobactam | 0.78 | 0.72 | Prior microbiological results |
| Ciprofloxacin | 0.75 | 0.70 | Recent fluoroquinolone exposure |
These models demonstrated notable discriminative ability, with area under receiver operating characteristic curve (AUROC) scores between 0.74-0.78 across five key antibiotics, outperforming traditional logistic regression approaches [81]. Feature importance analysis highlighted prior resistance patterns and antibiotic prescriptions as the most significant predictors of resistance [81]. The high specificity of these models suggests particular utility for informing antibiotic de-escalation decisions, aligning with stewardship goals to minimize broad-spectrum antibiotic overuse without compromising patient safety [81].
Experimental Protocols and Methodologies
LAMO Framework Implementation
The LAMO experimental protocol employs a structured methodology for clinical data processing and model training [15]. Implementation begins with structured EHR representation extraction, where raw clinical notes are parsed into four core components using standardized GPT-3.5 prompts: History of Present Illness, Past Medical History, Allergies, and Medications on Admission. For model architecture, LLaMA-2-7B serves as the backbone with LoRA fine-tuning parameters including learning rate (5e-4), batch size (64), LoRA rank (8), and alpha (16). Target modules focus on query and value projections ("qproj" and "vproj") within transformer layers. Training employs an inverse square root scheduler with early stopping based on validation F1 score stabilization.
LAMO Framework Implementation Workflow
Clinical Validation Methodologies
Robust validation methodologies are essential for assessing model performance in clinical contexts. The INSPIRE randomized controlled trials represent rigorous experimental protocols for evaluating AI-driven stewardship interventions [80]. These trials employ cluster randomization at the physician or unit level, with primary outcomes focused on antibiotic utilization metrics including extended-spectrum antibiotic days of therapy (DOT), with successful interventions demonstrating reductions of 28.4% for pneumonia and 17.4% for urinary tract infections [80]. Validation against established clinical benchmarks includes comparison with guidelines from the Infectious Diseases Society of America (IDSA) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID), with appropriate antibiotic selection measured as adherence to guideline recommendations [12].
For LLM-specific validation, standardized prompt engineering across diverse clinical scenarios ensures consistent evaluation. Studies typically employ 60+ clinical cases spanning multiple infection types (bloodstream, respiratory, urinary, etc.) with varying complexity [9]. Expert panel review with blinding procedures minimizes assessment bias, with evaluations focusing on three key appropriateness domains: antibiotic choice correctness, dosage accuracy, and treatment duration adequacy [9]. Multicenter external validation across diverse healthcare systems and temporal validation against evolving coding standards and resistance patterns provide critical real-world performance assessment [15].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for LLM Fine-tuning in Antimicrobial Stewardship
| Resource Category | Specific Examples | Primary Research Function | Key Considerations |
|---|---|---|---|
| Clinical Datasets | MIMIC-III, MIMIC-IV, eICU | Model training and validation; contains structured EHR data and clinical notes | Data de-identification; Institutional Review Board approval; Heterogeneous coding practices |
| LLM Architectures | LLaMA-2-7B, GPT-4, ClinicalBERT | Base models for fine-tuning; performance benchmarking | Computational requirements; Licensing restrictions; Architecture flexibility |
| Fine-tuning Frameworks | LoRA, Instruction Tuning, Adapter Layers | Parameter-efficient specialization | Training stability; Catastrophic forgetting prevention; Modular adaptation |
| Evaluation Benchmarks | IDSA/ESCMID guidelines, Local antibiograms, Expert panels | Standardized performance assessment | Clinical relevance; Guideline currency; Multi-center applicability |
| Computational Infrastructure | GPU clusters, Cloud computing platforms | Handling training computational loads | Cost management; Data security; Scalability |
The validation of fine-tuning approaches for large language models in antimicrobial stewardship reveals a complex landscape of methodological considerations and performance trade-offs. Parameter-efficient methods like the LAMO framework demonstrate superior performance in addressing critical challenges such as overprescription while maintaining computational efficiency. Instruction tuning provides robust clinical contextualization, and machine learning approaches enable personalized resistance prediction beyond traditional antibiograms. The comparative analysis presented in this guide underscores that specialized fine-tuning is essential for translating general-purpose LLMs into reliable clinical decision support tools. As research in this field rapidly evolves, ongoing validation against clinical outcomes and stewardship metrics remains imperative to ensure these advanced models fulfill their potential to combat antimicrobial resistance while optimizing patient care.
Physician Education for Optimal LLM Interaction and Error Recognition
The integration of Large Language Models (LLMs) into clinical practice represents a paradigm shift in antibiotic prescribing, creating an urgent need for structured physician education on optimal interaction and error recognition. While significant variability exists among LLMs in prescribing appropriate antibiotics, dosages, and treatment durations [9] [1], the human factor remains critical in mitigating risks and maximizing benefits. Evidence indicates that LLMs frequently demonstrate reduced accuracy in complex cases and exhibit inconsistencies that necessitate careful validation before clinical utilization [9]. This educational framework addresses the core competencies required for physicians to effectively collaborate with LLM systems, with particular emphasis on error recognition patterns, prompt optimization strategies, and clinical validation protocols essential for safe implementation in antimicrobial stewardship.
The emerging literature reveals that LLMs operate probabilistically, typically functioning as "black box" models that are only partially interpretable [3]. This fundamental characteristic introduces unique challenges for antibiotic prescribing, where errors can disproportionately impact either treatment efficacy or antimicrobial resistance priorities [3]. Furthermore, studies demonstrate that performance degradation occurs with increasing case complexity, particularly for difficult-to-treat microorganisms [9] [1]. These limitations underscore the necessity for comprehensive physician education that transcends technical proficiency to encompass critical evaluation skills, ethical considerations, and systematic error detection methodologies tailored to LLM-assisted clinical decision-making.
Comparative Performance Analysis of LLMs in Antibiotic Prescribing
Table 1: Comparative Performance of LLMs in Antibiotic Prescription Accuracy Across 60 Clinical Cases
| LLM Model | Overall Accuracy (%) | Dosage Correctness (%) | Inappropriate Recommendations (%) | Performance with Complex Cases |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | 1.7 | Declines significantly |
| Perplexity Pro | Not specified | 90.0 | Not specified | Declines with complexity |
| Claude 3.5 Sonnet | Not specified | 91.7 | Not specified | Tends to over-prescribe duration |
| Gemini | Lowest accuracy | Not specified | Not specified | Not specified |
| Claude 3 Opus | Lowest accuracy | Not specified | Not specified | Not specified |
| GPT-4-turbo | Lower than physicians | Not specified | High false positive rate | Not specified |
| GPT-3.5-turbo | Lower than physicians | Not specified | High false positive rate | Not specified |
Table 2: Specialized Medical LLMs Performance on Medical Licensing Examinations
| Model | Clinical Knowledge (MMLU) | Medical Genetics (MMLU) | Anatomy (MMLU) | Professional Medicine (MMLU) | PubMedQA |
|---|---|---|---|---|---|
| Palmyra-Med 70B | 90.9% | 94.0% | 83.7% | 84.4% | 79.6% |
| Med-PaLM 2 | 88.3% | 90.0% | 77.8% | 80.9% | 79.2% |
| GPT-4 | 86.0% | 91.0% | 80.0% | 76.9% | 75.2% |
| Gemini 1.0 | 76.7% | 75.8% | 66.7% | 69.2% | 70.7% |
| GPT-3.5 Turbo | 74.7% | 74.0% | 72.8% | 64.7% | 72.7% |
Rigorous comparative studies reveal substantial disparities in LLM performance for antibiotic prescribing. Analysis of 840 responses across 14 LLMs demonstrated that ChatGPT-o1 achieved the highest accuracy in antibiotic prescriptions at 71.7% (43/60 correct recommendations), with only 1.7% (1/60) classified as incorrect [9] [1]. Conversely, Gemini and Claude 3 Opus demonstrated the lowest accuracy among tested models [9]. In dosage-specific performance, ChatGPT-o1 again led with 96.7% correctness (58/60), followed by Perplexity Pro (90.0%, 54/60) and Claude 3.5 Sonnet (91.7%, 55/60) [9]. These performance metrics highlight the critical importance of model selection in clinical applications, with specialized medical LLMs like Palmyra-Med 70B achieving 90.9% on clinical knowledge evaluation compared to 86.0% for GPT-4 and 76.7% for Gemini 1.0 [82].
The complexity-performance relationship emerges as a crucial educational consideration. Research consistently demonstrates that LLM performance declines with increasing case complexity, particularly for difficult-to-treat microorganisms [9] [1]. This performance degradation manifests differently across models; for instance, Claude 3.5 Sonnet exhibits a tendency to over-prescribe treatment duration, while Gemini provides the most appropriate duration recommendations (75.0%, 45/60) [9]. In real-world clinical settings, GPT-4-turbo and GPT-3.5-turbo demonstrated significantly lower accuracy compared to physicians, with models tending to recommend interventions excessively, resulting in high false positive rates that could adversely affect hospital resource management and patient safety [83]. These findings underscore the necessity for physician education to include model-specific limitation awareness and complexity-based reliability assessment.
Experimental Protocols for LLM Validation in Clinical Scenarios
Diagram 1: Experimental Protocol for LLM Validation in Clinical Scenarios
The standardized experimental methodology for evaluating LLM antibiotic prescribing performance employs rigorous, multi-phase protocols. Researchers typically utilize 60 clinical cases with antibiograms covering 10 infection types, evaluating 14 LLMs including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai [9] [1]. The protocol implements standardized prompting for antibiotic recommendations focusing on three critical domains: drug choice, dosage, and treatment duration [9]. This standardized approach ensures comparability across models and eliminates prompt engineering as a confounding variable, allowing for direct performance comparison essential for clinical validation.
The blinded expert assessment phase represents a critical methodological component. All LLM responses are anonymized and reviewed by a blinded expert panel assessing antibiotic appropriateness, dosage correctness, and duration adequacy [9] [1]. This rigorous peer-review process minimizes assessment bias and ensures clinical relevance of the evaluation metrics. In studies examining LLM performance for bloodstream infection management, infectious diseases specialists classified appropriateness according to local and international guidelines while also evaluating potential harmfulness of recommendations [12]. For instance, in one study, ChatGPT-4 demonstrated 64% appropriateness for empirical therapy and 36% for targeted therapy, with 2% and 5% of empirical and targeted prescriptions, respectively, classified as potentially harmful [12].
Advanced research environments like the AI Hospital framework provide sophisticated multi-agent simulation platforms for more comprehensive evaluation. This framework employs simulated clinical interactions with patient agents exhibiting realistic behaviors including cooperative but potentially incomplete information sharing, colloquial expression patterns, and medically naive questioning [84] [85]. The Multi-View Medical Evaluation (MVME) benchmark then assesses LLM performance across symptoms collection, examination recommendation, and diagnosis formulation, providing multidimensional performance assessment beyond simple prescription accuracy [84] [85]. These sophisticated experimental protocols enable researchers to identify specific failure patterns, such as LLMs overlooking necessary auxiliary tests, fixating on complications while ignoring underlying health issues, and demonstrating insufficient medical knowledge leading to erroneous judgments [85].
Error Patterns and Limitations in LLM-Generated Recommendations
Table 3: Common Error Patterns in LLM Antibiotic Prescribing
| Error Category | Specific Manifestations | Clinical Consequences | Frequency in Studies |
|---|---|---|---|
| Hallucinations | Inventing non-existent clinical signs (e.g., Kernig's sign, stiff neck) | Misdiagnosis, inappropriate antibiotic selection | Observed in multiple LLMs [12] |
| Over-prescribing | Excessive treatment duration; recommending unnecessary antibiotics | Increased antimicrobial resistance, patient harm | Claude 3.5 Sonnet showed tendency [9] |
| Under-prescribing | Narrowing spectrum inadequately (e.g., not covering Gram-negative bacteria in febrile neutropenia) | Treatment failure, increased mortality | 2% of empirical therapy suggestions [12] |
| Dosage Errors | Incorrect dosing recommendations | Toxicity or subtherapeutic levels | Varied by model (3.3-10% error rate) [9] |
| Context Ignorance | Failure to incorporate local resistance patterns or patient specifics | Non-adherence to stewardship principles | Common across models [3] |
The hallucination phenomenon represents a critical error pattern requiring physician vigilance. Studies document instances where LLMs invent clinical signs not present in the case description, such as reporting Kernig's sign and stiff neck in meningitis cases where these findings were not documented [12]. Similarly, researchers observed misleading interpretations where LLMs incorrectly identified herpes ophthalmicus instead of bacterial meningitis [12]. These factual inaccuracies stem from the probabilistic nature of LLMs, which generate responses based on statistical patterns in training data rather than clinical reasoning [3]. This fundamental operational characteristic necessitates that physicians maintain a position of active skepticism, systematically verifying all LLM-generated recommendations against established clinical knowledge and patient-specific data.
The over-prescribing tendency emerges as a consistent limitation across multiple LLM evaluations. Research demonstrates that general-purpose and medical LLMs frequently recommend excessive medications, with GPT-4 prescribing an average of over 80 drugs per patient—three times more than physicians [86]. This over-prescribing pattern manifests particularly in treatment duration, with Claude 3.5 Sonnet showing a tendency to recommend excessively long antibiotic courses [9]. Conversely, under-prescribing errors also occur, such as inappropriately narrowing antibiotic spectrum in high-risk situations like febrile neutropenia while awaiting culture results [12]. These opposing error patterns highlight the challenge physicians face in achieving the delicate balance between effective treatment and antimicrobial stewardship when utilizing LLM assistance.
The contextual limitation of LLMs presents another critical educational consideration. Studies note significant performance variability across different clinical scenarios, with models struggling to adapt recommendations to specific institutional guidelines, local resistance patterns, and individual patient factors [3] [12]. This limitation is compounded by the black box nature of most LLMs, which provide limited explanation for their recommendations, making error identification and correction challenging [3] [12]. Research indicates that future clinicians will need dedicated training to recognize these contextual limitations and implement appropriate validation protocols, including cross-referencing with local antibiograms, verifying against current guidelines, and applying patient-specific clinical judgment before implementing any LLM-generated recommendations.
Essential Protocols for Effective LLM Interaction in Clinical Practice
Diagram 2: Optimal LLM Interaction Protocol for Clinical Practice
Effective LLM interaction begins with structured prompt engineering that incorporates essential clinical context. Studies demonstrate that providing comprehensive patient information, including relevant medical history, current clinical status, local antibiograms, and institutional guidelines, significantly improves LLM recommendation quality [3] [12]. Research protocols that employed standardized prompts contextualizing the specific clinical scenario, such as managing bloodstream infections in a particular hospital setting, achieved higher appropriateness rates in LLM suggestions [12]. The emerging evidence supports including explicit constraints in prompts, such as formulary limitations, allergy considerations, and renal/hepatic impairment, to generate more clinically applicable recommendations. This approach addresses the contextual deficiency inherent in general-purpose LLMs and enhances their practical utility in specific clinical environments.
The iterative refinement process represents another critical component of optimal LLM interaction. Rather than treating initial LLM responses as definitive, physicians should engage in multi-round dialogues to refine recommendations, clarify uncertainties, and explore alternatives [3] [12]. Research examining LLM performance across multiple sessions with the same clinical case observed significant response heterogeneity, with ChatGPT-4 providing the most consistent responses across sessions [12]. This finding suggests that repeated questioning with progressively specific prompts can enhance recommendation quality and consistency. Educational programs should train clinicians in formulating sequential prompts that build upon previous responses, probe uncertain areas, and explicitly request evidence rationales for recommendations.
Implementation of systematic verification protocols constitutes the final essential element for safe LLM utilization. These protocols should include cross-referencing with authoritative sources, consulting specialist guidelines, and applying local antimicrobial stewardship principles [3] [12]. Studies indicate that LLMs perform better on specific competency areas—for instance, correctly recognizing the need for rapid antibiotic administration in 81% of cases, but suggesting correct empirical antibiotics in only 38% of cases [12]. This disparity highlights the importance of targeted verification based on known model-specific weaknesses. Additionally, the research community emphasizes that future medical education must incorporate training on identifying LLM hallucinations, omissions, and biases specific to antibiotic prescribing, enabling physicians to function effectively as final clinical decision-makers in the LLM-assisted workflow.
Table 4: Essential Research Reagents and Resources for LLM Validation Studies
| Resource Category | Specific Examples | Function in Research | Key Characteristics |
|---|---|---|---|
| Clinical Case Databases | 60 clinical cases with antibiograms covering 10 infection types [9]; MIMIC-III, MIMIC-IV, eICU datasets [86] | Provide standardized evaluation benchmarks across diverse infection types and complexity levels | Include antibiograms; cover spectrum from common to difficult-to-treat infections |
| Evaluation Frameworks | AI Hospital multi-agent framework [84] [85]; MVME benchmark [84] [85] | Simulate clinical environments; provide multidimensional performance assessment beyond prescription accuracy | Incorporate patient, checker, chief physician agents; assess diagnostic reasoning process |
| Specialized Medical LLMs | Palmyra-Med 70B [82]; Med-PaLM 2 [82] | Offer domain-specific optimization for healthcare applications with enhanced medical knowledge representation | Trained specifically on medical literature; optimized for clinical reasoning tasks |
| Assessment Tools | Blinded expert panel review protocols [9] [1]; appropriateness criteria based on IDSA/ESCMID guidelines [12] | Provide gold-standard evaluation of LLM recommendation quality and safety | Employ infectious disease specialists; use standardized appropriateness criteria |
| Prompt Engineering Resources | Standardized prompt templates [9] [12]; contextual constraint specifications | Ensure comparability across studies; simulate real-world clinical query formulation | Include patient context, local resistance patterns, institutional constraints |
The AI Hospital framework represents an advanced research tool that enables sophisticated simulation of clinical environments for LLM evaluation. This multi-agent framework incorporates simulated patients, examination systems, and chief physicians to create realistic clinical interaction scenarios [84] [85]. Within this environment, patient agents exhibit authentic behaviors including cooperative but potentially incomplete information sharing, colloquial expression patterns, and medically naive questioning [84]. The framework implements the Multi-View Medical Evaluation (MVME) benchmark which assesses LLM performance across multiple dimensions including symptoms collection, examination recommendation, diagnostic accuracy, and treatment planning [84] [85]. This comprehensive assessment approach moves beyond simple prescription accuracy to evaluate the entire clinical reasoning process, providing richer insights into LLM capabilities and limitations.
Specialized medical evaluation datasets form another critical component of the LLM validation toolkit. The MIMIC-III, MIMIC-IV, and eICU datasets provide comprehensive clinical data extracted from electronic health records, enabling robust evaluation across diverse patient populations and clinical scenarios [86]. These datasets facilitate both internal validation within the same hospital system and external validation across different institutions, assessing model generalizability and temporal performance consistency [86]. Additionally, carefully curated case sets covering specific infection types with associated antibiograms enable targeted evaluation of antimicrobial recommendation quality under varying resistance patterns [9] [1]. These datasets must include cases of varying complexity to properly assess the complexity-performance relationship observed in LLMs, where performance consistently declines with increasingly complex cases, particularly those involving difficult-to-treat microorganisms [9].
The implementation of rigorous assessment methodologies completes the essential research toolkit. Blinded expert panel review represents the gold standard for evaluating LLM-generated recommendations, with infectious diseases specialists assessing appropriateness based on established guidelines [9] [12]. These assessments should categorize errors by type (hallucinations, omissions, commission errors), potential for patient harm, and deviation from antimicrobial stewardship principles [3] [12]. Additionally, comprehensive evaluation should include heterogeneity analysis across multiple sessions with the same model to assess response consistency [12]. This methodological rigor enables researchers to identify not just overall performance metrics but specific failure patterns and limitations that must be addressed before clinical implementation. The resulting insights provide the foundation for developing targeted physician education on error recognition and optimal interaction strategies specific to antibiotic prescribing scenarios.
The integration of LLMs into antibiotic prescribing workflows represents a transformative development in clinical practice, one that demands sophisticated physician education focused on optimal interaction and error recognition. The evidence clearly demonstrates that significant performance variability exists among models, with ChatGPT-o1 currently achieving the highest accuracy at 71.7% compared to the lowest performing models like Gemini and Claude 3 Opus [9] [1]. This variability, coupled with consistent observations of performance degradation with increasing case complexity, underscores the critical role of physician oversight in the LLM-assisted workflow [9]. Furthermore, the concerning tendencies of models to hallucinate clinical findings, over-prescribe medications, and provide contextually inappropriate recommendations highlight the necessity for robust validation protocols before clinical implementation [3] [86] [12].
The path forward requires deliberate educational initiatives that equip clinicians with the specific competencies needed to effectively collaborate with LLM systems. These competencies include advanced prompt engineering skills tailored to clinical scenarios, systematic error recognition methodologies specific to LLM limitations, and iterative refinement techniques that optimize recommendation quality [3] [12]. Additionally, educational programs must address the ethical implications of LLM utilization, including accountability frameworks, data privacy considerations, and appropriate disclosure to patients [3]. As LLM technology continues to evolve rapidly, the medical community must establish continuous learning systems that keep clinicians abreast of emerging capabilities and limitations specific to antibiotic prescribing.
Ultimately, the safe and effective integration of LLMs into antimicrobial stewardship programs depends on recognizing that these systems function best as clinical decision support tools rather than autonomous practitioners. The emerging research consistently demonstrates that the most promising approach combines the information processing power of LLMs with the clinical judgment, contextual understanding, and ethical responsibility of trained physicians [3] [12]. By developing comprehensive educational frameworks that optimize this collaboration, the healthcare community can harness the potential of LLMs to enhance antibiotic prescribing accuracy while maintaining the essential human factors that remain fundamental to quality patient care. This balanced approach promises to advance both individual patient outcomes and the broader public health goal of antimicrobial resistance containment.
Comparative Performance Analysis: Benchmarking LLMs in Real-World Scenarios
Methodology for Multi-Model Comparative Studies
In the rapidly evolving field of artificial intelligence, rigorous multi-model comparative studies are essential for validating the performance of large language models (LLMs) in high-stakes domains like healthcare. Within antibiotic prescribing accuracy research, such methodology provides the critical framework for objectively determining whether differences in model architecture, training data, or design lead to significant variations in clinical recommendations [87]. This guide outlines a structured approach for conducting these evaluations, focusing on the experimental and observational designs necessary to generate reliable, actionable evidence for researchers, scientists, and drug development professionals.
Methodological Framework for Comparison
The foundation of a robust multi-model comparison lies in selecting an appropriate study design. The choice dictates how participants or units are assigned to conditions, how data is collected, and the extent to which confounding variables can be controlled.
Core Experimental Designs
Comparative studies generally adopt an objective viewpoint, where the use and effect of a system can be defined, measured, and compared through variables to test a hypothesis [87]. The primary design options are experimental versus observational and prospective versus retrospective. For evaluating LLMs, experimental designs are typically most appropriate.
- Randomized Controlled Trials (RCTs): In an RCT, individual clinical cases or prompts are randomly assigned to different LLMs for analysis. This randomization controls for selection bias by ensuring that case complexity is distributed evenly across the models being compared [87]. For instance, a pool of 60 clinical cases can be randomly distributed such that each model receives a comparable mix of infection types and complexity levels.
- Cluster Randomized Controlled Trials (cRCTs): This design is useful when models cannot be applied to individual cases in isolation but are instead evaluated as part of a larger system or in specific clinical environments. For example, different hospital wards or virtual "clinics" could be randomized to use a specific LLM as a decision-support tool, and the aggregate prescribing outcomes for all cases within that cluster are then compared [87].
- Pragmatic Trials: Unlike traditional RCTs that test efficacy under ideal conditions, pragmatic trials assess effectiveness in "real-world" settings [87]. This is highly relevant for LLM validation, as it involves applying models to diverse clinical cases with few exclusion criteria, using standardized prompts that mimic real clinical inquiries, and measuring outcomes that are directly relevant to end-users like clinicians and healthcare administrators.
Non-Randomized and Quasi-Experimental Designs
When randomization is not feasible, non-randomized or quasi-experimental designs offer alternatives.
- Intervention Group with Pretest-Posttest Design: This involves establishing a baseline (pretest) performance metric using a gold-standard method or historical data. The LLM's recommendations are then implemented, and outcomes are measured again (posttest) for comparison [87].
- Interrupted Time Series (ITS) Design: The ITS design strengthens the pretest-posttest approach by collecting multiple performance measurements at regular intervals both before and after the implementation of the LLM intervention. This helps determine if observed changes are due to the intervention or merely pre-existing trends [87].
Experimental Protocols for LLM Validation
The following workflow details a validated experimental protocol for comparing LLM performance in antibiotic prescribing, synthesizing methodologies from recent peer-reviewed studies [1] [9].
Study Preparation and LLM Selection
The initial phase focuses on building a rigorous evaluation framework.
- Clinical Case Portfolio Development: A validated evaluation should utilize a substantial number of clinical cases covering a range of infection types. Recent research employed 60 clinical cases encompassing 10 different infection scenarios, each accompanied by relevant antibiogram data to simulate real-world clinical decision-making [1] [9].
- LLM Selection: The study should include a diverse set of models to ensure broad comparability. One published protocol evaluated 14 different LLMs, including standard and premium versions of widely available platforms such as ChatGPT, Claude, Copilot, Gemini, and others [1].
- Standardized Prompt Development: To ensure consistency, every LLM receives an identical, structured prompt for each case. This prompt contextualizes the request, specifying that the model should act as an infectious disease specialist and provide a comprehensive recommendation for antibiotic choice, dosage, and treatment duration [9].
Execution and Blinded Evaluation
This phase involves data collection and impartial assessment.
- Anonymized Data Collection: All prompts are submitted to the LLMs, and their responses are collected. In a study with 60 cases and 14 models, this generates 840 individual responses for analysis. All responses are anonymized to prevent reviewer bias [1].
- Blinded Expert Panel Review: A panel of infectious disease specialists, who are blinded to the identity of the LLM that generated each recommendation, independently assesses every response. They evaluate three key dimensions: the appropriateness of the antibiotic choice, the correctness of the dosage, and the adequacy of the treatment duration [1] [9].
Data Analysis and Stratification
The final phase focuses on interpreting the collected data.
- Quantitative Performance Comparison: The primary outcomes are calculated as the percentage of correct recommendations for each model across the three dimensions (choice, dosage, duration). Statistical analysis identifies significant performance differences between models [1].
- Qualitative Review for Hallucinations: Alongside quantitative metrics, responses are scrutinized for "hallucinations" or glaring inaccuracies, such as suggesting incorrect diagnostic signs or recommending non-guideline-concordant therapies [12].
- Stratified Analysis by Case Complexity: Performance is often stratified based on case complexity, particularly for infections involving difficult-to-treat microorganisms, to identify whether model accuracy declines with increasing clinical challenge [1] [9].
Performance Data and Comparative Analysis
Structuring quantitative results into clear tables is vital for objective comparison. The following tables summarize findings from a recent study comparing 14 LLMs [1] [9].
Table 1: Overall Prescribing Accuracy of Select LLMs Across 60 Clinical Cases
| Large Language Model | Correct Antibiotic Choice | Incorrect Antibiotic Choice | Dosage Correctness | Appropriate Treatment Duration |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7% (43/60) | 1.7% (1/60) | 96.7% (58/60) | Information Missing |
| Claude 3.5 Sonnet | Information Missing | Information Missing | 91.7% (55/60) | Tended to over-prescribe |
| Perplexity Pro | Information Missing | Information Missing | 90.0% (54/60) | Information Missing |
| Gemini | Lowest Accuracy | Information Missing | Information Missing | 75.0% (45/60) |
Table 2: Model Performance on Key Prescribing Dimensions
| Model Performance Characteristic | Finding | Key Example |
|---|---|---|
| Highest Accuracy in Drug Selection | Significant variability exists among models. | ChatGPT-o1 demonstrated the highest accuracy at 71.7% [1]. |
| Dosage Recommendation Reliability | This was a relative strength for many models. | Dosage correctness was highest for ChatGPT-o1 (96.7%), followed by Perplexity Pro (90%) [1]. |
| Treatment Duration Appropriateness | Models showed specific tendencies. | Claude 3.5 Sonnet tended to over-prescribe duration, while Gemini provided the most appropriate duration recommendations (75%) [1]. |
| Impact of Clinical Complexity | Performance declined with increasing complexity. | Accuracy decreased particularly for cases involving difficult-to-treat microorganisms [1] [9]. |
Methodological Considerations for Robust Research
The quality of a comparative study is determined by its internal validity (the correctness of its conclusions) and external validity (the generalizability of its findings) [87]. Key factors influencing validity must be actively managed.
Defining Variables and Ensuring Adequate Power
- Variable Selection: The research must clearly define its dependent variables (outcomes of interest, e.g., antibiotic appropriateness, dosage correctness) and independent variables (factors that might explain outcomes, e.g., model architecture, case complexity) [87]. These can be categorical (e.g., appropriate vs. inappropriate) or continuous (e.g., treatment duration in days), which dictates the statistical analysis method.
- Sample Size and Power: A sufficient sample size is critical. Its calculation depends on four elements: the significance level (typically α=0.05), statistical power (typically 80% or 0.8), the effect size (the minimal clinically relevant difference), and the variability of the outcome in the population [87]. In LLM studies, the "sample size" can refer to the number of clinical cases used in the evaluation.
Controlling for Bias
Controlling for bias is paramount in generating unbiased, reliable results.
- Selection/Allocation Bias: This occurs if the clinical cases assigned to different models differ systematically in complexity. Mitigation: Use random assignment of cases to models and ensure case portfolios are comparable across models at baseline [87].
- Performance Bias: This arises if models receive different prompts or contextual information. Mitigation: Standardize the intervention by using identical, pre-defined prompts for all models and all cases [87] [1].
- Detection/Measurement Bias: This happens if the expert panel is influenced by knowing which model generated a response. Mitigation: Implement a blinded review process where all responses are anonymized before assessment [87] [1].
- Attrition Bias: This is less common in LLM studies but could refer to incomplete responses. Mitigation: Establish protocols to recollect data for models that produce incomplete outputs [87].
The Scientist's Toolkit: Research Reagent Solutions
This table details key resources and their functions for conducting multi-model comparative studies in antibiotic prescribing.
Table 3: Essential Materials and Tools for LLM Comparative Research
| Research Reagent / Tool | Function in the Experimental Protocol |
|---|---|
| Clinical Case Portfolio | A validated set of clinical scenarios (e.g., 60 cases) with antibiograms that serve as the standardized input for testing all LLMs [1] [9]. |
| Antibiotic Prescribing Guidelines (IDSA/ESCMID) | The gold-standard reference (e.g., from IDSA or ESCMID) used by the expert panel to classify LLM recommendations as appropriate or inappropriate [12]. |
| Standardized Prompt Protocol | A fixed text template used to query every LLM, ensuring consistency in the task instructions and clinical context provided across all evaluations [1]. |
| Blinded Expert Review Panel | A team of infectious disease specialists who assess the anonymized LLM outputs against predefined criteria, providing the human expert judgment for ground truth [1]. |
| Percentage Similarity Analysis | A statistical model that can simplify multiple method comparisons by representing the agreement between a new method and a gold standard as a percentage, useful for visualizing results [88]. |
| Color Contrast Checker | A tool (e.g., WebAIM's Color Contrast Checker) to ensure that all data visualizations meet WCAG guidelines for accessibility, with a minimum contrast ratio of 4.5:1 for standard text [89]. |
The integration of large language models (LLMs) into clinical decision-making represents a paradigm shift in healthcare, offering the potential to enhance patient safety and optimize therapeutic outcomes. Within the specific domain of antimicrobial stewardship, antibiotic prescribing requires a critical balance between delivering effective patient treatment and mitigating the global threat of antimicrobial resistance [12]. This article provides a objective, data-driven comparison of leading LLMs—ChatGPT-o1, various Claude and Gemini versions, and others—focusing on their performance in recommending appropriate antibiotic therapies. The analysis is framed within the broader thesis of validating these AI tools for use in clinical support systems, presenting synthesized experimental data from recent, rigorous studies to inform researchers, scientists, and drug development professionals.
Recent comparative studies have quantified the performance of various LLMs in clinical antibiotic prescribing scenarios, revealing significant variability in their capabilities.
Table 1: Overall Accuracy in Antibiotic Prescription Recommendations [1] [9]
| Large Language Model | Overall Accuracy (%) | Incorrect Recommendation Rate (%) |
|---|---|---|
| ChatGPT-o1 | 71.7 (43/60) | 1.7 (1/60) |
| Claude 3 Opus | Among the lowest | Data not specified |
| Gemini | Among the lowest | Data not specified |
| Perplexity Pro | Data not specified | Data not specified |
| Claude 3.5 Sonnet | Data not specified | Data not specified |
Table 2: Performance on Specific Prescribing Components [1] [9]
| Large Language Model | Dosage Correctness (%) | Treatment Duration Adequacy (%) |
|---|---|---|
| ChatGPT-o1 | 96.7 (58/60) | Data not specified |
| Perplexity Pro | 90.0 (54/60) | Data not specified |
| Claude 3.5 Sonnet | 91.7 (55/60) | Tended to over-prescribe |
| Gemini | Data not specified | 75.0 (45/60) |
The data indicates that ChatGPT-o1 demonstrates superior overall accuracy and dosage correctness, while Gemini shows strength in recommending appropriate treatment durations. Performance across all models generally declined with increasing case complexity, particularly for infections involving difficult-to-treat microorganisms [1] [9].
Experimental Protocols and Methodologies
A critical understanding of the data necessitates a review of the experimental methodologies from which it is derived. The following workflow visualizes a typical study design for evaluating LLMs in a clinical context.
Figure 1: LLM Clinical Validation Workflow. This diagram outlines the core methodology for evaluating LLM performance in antibiotic prescribing [1] [9].
Core Clinical Validation Protocol
A seminal 2025 study employed a rigorous protocol to evaluate 14 LLMs, including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, and others [1] [9]. The methodology can be broken down as follows:
- Case Development: The study utilized 60 clinical cases covering 10 different infection types. A critical component was the inclusion of antibiograms, which provide data on local bacterial resistance patterns, essential for making informed antibiotic choices [1] [9].
- Prompting and Data Collection: A standardized prompt was used for all antibiotic recommendations, focusing on drug choice, dosage, and treatment duration. This ensured consistency and comparability across all 840 collected responses [1] [9].
- Blinded Expert Evaluation: The model responses were anonymized and then reviewed by a blinded expert panel. The panel assessed three key outcome measures: antibiotic appropriateness, dosage correctness, and duration adequacy [1] [9].
Advanced Framework: The RAG-LLM and Co-Pilot Model
Beyond native model performance, research has explored enhanced frameworks like Retrieval-Augmented Generation (RAG) and novel human-AI collaboration models.
- Retrieval-Augmented Generation (RAG): This framework enhances native LLMs by giving them access to an external knowledge base, such as updated clinical guidelines or institutional protocols. In one study, applying a RAG framework improved the accuracy and recall of most models, though the top-performing native model (Claude 3.5 Sonnet) saw a slight performance change when the RAG framework was applied [90].
- The Co-Pilot Implementation Strategy: One study evaluated three implementation strategies: LLM-based Clinical Decision Support System (CDSS) alone, a pharmacist alone, and a "co-pilot" mode where the pharmacist and LLM-CDSS worked together. The co-pilot arm demonstrated the best performance, increasing accuracy in identifying drug-related problems by 32.6% compared to the pharmacist alone. This hybrid approach was particularly effective at detecting errors posing serious harm, increasing accuracy by 1.5-fold [90].
The following diagram illustrates how a RAG-LLM system is structured and can be integrated into a clinical co-pilot workflow.
Figure 2: RAG-LLM Clinical Co-Pilot Architecture. This shows the flow of information in a system where an LLM is augmented with a clinical knowledge base to support a clinician [90].
The Scientist's Toolkit: Research Reagent Solutions
The experimental validation of LLMs for clinical applications relies on a suite of "research reagents" — essential components and materials that form the basis of a robust evaluation framework.
Table 3: Essential Components for LLM Clinical Validation
| Research Reagent | Function & Role in Validation |
|---|---|
| Clinical Case Vignettes | Standardized, often complex patient scenarios used to prompt LLMs; ensure evaluation covers a range of medical disciplines and infection types [1] [90]. |
| Antibiograms | Laboratory data summaries showing susceptibility of bacterial isolates to antibiotics; provide critical, real-world context for appropriate drug selection [1] [9]. |
| Expert Review Panel | A blinded group of infectious disease specialists; provides the gold-standard assessment of LLM output appropriateness, dosage, and duration [1] [9]. |
| Retrieval-Augmented Generation (RAG) Framework | A technical architecture that grounds the LLM in an external knowledge base (e.g., latest guidelines); enhances factual accuracy and reduces hallucinations [90]. |
| Standardized Prompt Protocol | A consistent set of instructions and context provided to each LLM; ensures fair and comparable results across all models being tested [1] [9] [12]. |
The head-to-head performance data clearly demonstrates that while LLMs like ChatGPT-o1 show significant promise as decision-support tools in antibiotic prescribing, variability among models is substantial [1] [9]. ChatGPT-o1 currently leads in overall accuracy and dosage precision, while other models exhibit strengths in specific areas or in cost-effectiveness for non-clinical tasks like coding [91] [1]. However, the decline in performance with increasing case complexity is a critical limitation that researchers and clinicians must consider [1].
The path toward reliable clinical integration appears to lie not in relying on native models alone, but in employing enhanced frameworks. The RAG approach, which provides models with access to current, validated knowledge bases, and the co-pilot implementation strategy, which leverages the synergistic strengths of human expertise and AI, have both been shown to significantly improve outcomes [90]. For researchers and drug development professionals, these findings underscore that the validation of LLMs must extend beyond benchmarking raw model intelligence. It must also focus on developing the optimal socio-technical systems—the reagents and workflows—that ensure these powerful tools are deployed safely, effectively, and in a manner that truly enhances patient safety and antimicrobial stewardship.
The integration of large language models (LLMs) into clinical decision-making represents a significant advancement in healthcare technology, particularly in the complex domain of antibiotic prescribing. Appropriate antibiotic use requires precise decision-making across three critical dimensions: drug selection, dosage correctness, and treatment duration adequacy. These metrics serve as fundamental benchmarks for evaluating the potential of LLMs to function as reliable clinical decision-support tools. This guide provides a comprehensive comparison of LLM performance across these accuracy metrics, synthesizing current experimental data to inform researchers, scientists, and drug development professionals engaged in validating artificial intelligence applications for antimicrobial stewardship.
Comparative Performance Analysis of LLMs
Recent rigorous evaluations have quantified significant performance variations among LLMs when applied to antibiotic prescribing tasks. The data presented below enable direct comparison of leading models across essential accuracy parameters.
Table 1: Comparative LLM Performance in Antibiotic Prescribing Accuracy [1] [9]
| Large Language Model | Overall Prescription Accuracy (%) | Dosage Correctness (%) | Duration Adequacy (%) | Incorrect/Unsafe Recommendations (%) |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Information Missing | 1.7 |
| Perplexity Pro | Information Missing | 90.0 | Information Missing | Information Missing |
| Claude 3.5 Sonnet | Information Missing | 91.7 | Information Missing | Information Missing |
| Gemini | Lowest Accuracy [1] | Information Missing | 75.0 | Information Missing |
| Claude 3 Opus | Lowest Accuracy [1] | Information Missing | Information Missing | Information Missing |
Table 2: Performance Analysis by Clinical Scenario Complexity [1]
| Clinical Scenario Complexity | Performance Trend | Specific Challenges |
|---|---|---|
| Standard Infections | Higher performance across most models | Fewer errors in drug selection and dosage |
| Complex Cases | Significant performance decline across most models | Increased error rate with difficult-to-treat microorganisms |
| Rare/Resistant Pathogens | Notable decrease in accuracy | Inappropriate drug selection and duration recommendations |
Experimental Protocols and Methodologies
Understanding the experimental designs that generated the comparative data is crucial for interpreting results and designing future validation studies.
Multi-Model Evaluation Framework
A comprehensive 2025 study established a robust protocol for comparing LLM performance in antibiotic prescribing [1] [9]:
- Model Selection: Fourteen LLMs were evaluated, including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai.
- Clinical Case Design: Researchers developed 60 clinical cases with accompanying antibiograms covering 10 distinct infection types to ensure breadth of assessment.
- Standardized Prompting: A uniform prompt structure was employed across all models, requesting antibiotic recommendations focused on drug choice, dosage, and treatment duration.
- Blinded Expert Review: Responses were anonymized and assessed by a blinded panel of infectious disease specialists who evaluated antibiotic appropriateness, dosage correctness, and duration adequacy.
- Output Volume: The study collected and analyzed 840 individual model responses (60 cases × 14 models).
Primary Care Integration Study
A complementary 2025 investigation examined LLM performance in general practice settings [37]:
- Vignette-Based Assessment: 24 clinical vignettes incorporating infection type, patient demographics, and comorbidities were presented to both LLMs and general practitioners.
- Multi-Country Framework: The study evaluated performance across four countries (Ireland, UK, USA, and Norway) with reference to national prescribing guidelines.
- Comparative Design: Responses from six LLMs (ChatGPT, Gemini, Copilot, Mistral AI, Claude, and Llama 3.1) were compared against those of human general practitioners.
- Additional Metrics: Researchers assessed model limitations including hallucination rates, potential toxicity, and data leakage vulnerabilities.
Visualization of Experimental Workflows
The experimental methodology for evaluating LLMs in antibiotic prescribing follows a systematic multi-stage process, as illustrated below.
LLM Performance Decision Pathway
The evaluation of LLM performance reveals distinct patterns across different clinical scenarios, as visualized in the following decision pathway.
The Researcher's Toolkit: Essential Experimental Components
Table 3: Key Research Reagents and Methodological Components [1] [9] [37]
| Research Component | Function in Experimental Design | Implementation Example |
|---|---|---|
| Clinical Vignettes | Standardized patient scenarios for consistent model evaluation | 60 cases covering 10 infection types with varied complexity [1] |
| Antibiograms | Provide local antimicrobial resistance patterns for context | Integrated with clinical cases to simulate real-world constraints [1] |
| Standardized Prompt Templates | Ensure consistent questioning across model evaluations | Uniform prompt structure for antibiotic recommendations [1] |
| Blinded Expert Review Panel | Objective assessment of model outputs without bias | Infectious disease specialists evaluating appropriateness [1] |
| National Prescription Guidelines | Reference standard for appropriate antibiotic use | Country-specific guidelines for comparison in primary care study [37] |
| Assessment Rubrics | Structured evaluation criteria for drug, dosage, and duration | Three-component assessment of appropriateness, correctness, adequacy [1] |
Discussion and Research Implications
The comparative performance data reveals several critical patterns essential for research validation. First, the superiority of ChatGPT-o1 in overall prescription accuracy (71.7%) and dosage correctness (96.7%) demonstrates that advanced LLMs can achieve clinically relevant performance levels in specific prescribing dimensions [1]. Second, the performance degradation observed in complex cases, particularly those involving difficult-to-treat microorganisms, highlights a significant limitation that must be addressed before clinical implementation [1].
The expertise paradox presents another crucial consideration: while LLMs may offer the greatest potential benefit to less-experienced clinicians, these users may lack the specialized knowledge necessary to identify model errors, hallucinations, or omissions [11]. This paradox necessitates careful consideration of implementation frameworks and oversight mechanisms.
Future validation research should prioritize several key areas: developing more sophisticated evaluation methodologies for complex clinical scenarios, establishing standardized benchmarking datasets across diverse healthcare settings, and creating robust frameworks for detecting and mitigating model hallucinations and biases in antibiotic prescribing recommendations.
Performance Across Infection Types and Complexity Levels
The rising threat of antimicrobial resistance (AMR) has made optimizing antibiotic prescribing a critical global health priority. [92] In this context, large language models (LLMs) offer a promising tool to support clinical decision-making. However, their performance is not uniform; it varies significantly across different types of infections and levels of case complexity. [9] [1] This guide synthesizes current experimental data to objectively compare the performance of leading LLMs in antibiotic prescribing, providing researchers and drug development professionals with a clear analysis of their capabilities and limitations within a validation research framework.
Comparative Performance of LLMs in Antibiotic Prescribing
Direct, head-to-head comparisons of various LLMs reveal significant variability in their ability to provide accurate antibiotic recommendations.
Table 1: Overall Antibiotic Prescribing Accuracy Across LLMs
| Large Language Model | Overall Prescription Accuracy (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) | Key Findings |
|---|---|---|---|---|
| ChatGPT-o1 | 71.7 (43/60) [9] [1] | 96.7 (58/60) [9] [1] | Information Missing | Demonstrates the highest overall accuracy and lowest error rate. |
| Claude 3.5 Sonnet | Information Missing | 91.7 (55/60) [9] [1] | Tended to over-prescribe duration [9] [1] | Performance noted for dosage but tendency for prolonged therapy. |
| Perplexity Pro | Information Missing | 90.0 (54/60) [9] [1] | Information Missing | Shows strong performance in dosage recommendation. |
| Gemini | Among the lowest accuracy [9] [1] | Information Missing | 75.0 (45/60) [9] [1] | Lowest accuracy in drug choice, but highest in treatment duration adequacy. |
| Claude 3 Opus | Among the lowest accuracy [9] [1] | Information Missing | Information Missing | Consistently low performance in prescribing accuracy. |
Performance in Specific Clinical Contexts
Beyond overall prescribing, LLM performance has been evaluated in specialized clinical areas such as infection prevention control (IPC) and specific disease management.
Table 2: LLM Performance in Specialized Clinical Areas
| Clinical Area | Top-Performing Models | Key Performance Metrics | Noted Deficiencies |
|---|---|---|---|
| Infection Prevention & Control (IPC) [93] | GPT-4.1, DeepSeek V3 | Significantly higher composite quality scores (e.g., coherence, usefulness, evidence quality) compared to Gemini. [93] | Critical errors in clinical judgment (e.g., on tuberculosis, Candida auris). [93] |
| Pneumonia Management [94] | OpenAI O1, OpenAI O3 mini | Superior overall accuracy and guideline compliance; effective self-correction. [94] | ChatGPT-4o provided concise but sometimes incomplete information. [94] |
| Antibiotic Prophylaxis in Spine Surgery [95] | GPT-4.0 | 81% (13/16) accuracy in answering guideline-based questions. [95] | GPT-3.5 showed a tendency for overly confident responses and lower accuracy (62.5%). [95] |
Impact of Infection Complexity on LLM Performance
A consistent finding across studies is that the performance of LLMs degrades as the complexity of the clinical case increases. [9] [1] Models struggle particularly with complex scenarios involving difficult-to-treat microorganisms and cases requiring dynamic, multi-stage clinical reasoning. [9] [1] [21]
Table 3: Performance Challenges in Complex Scenarios
| Complexity Factor | Impact on LLM Performance | Specific Example |
|---|---|---|
| Difficult-to-Treat Microorganisms [9] [1] | Decline in prescribing accuracy. | Not specified in available data. |
| Dynamic Clinical Reasoning [21] | Failure to adapt recommendations as new information (e.g., microbiology results) becomes available. | Models may not properly escalate or de-escalate therapy based on culture results or evolving patient status. [21] |
| Rare or Atypical Presentations [93] | Generation of "hallucinations" or misleading statements. | One study noted a model hallucinating the presence of Kernig's sign, leading to a misinterpretation of bacterial meningitis. [93] |
Detailed Experimental Protocols
Understanding the methodologies behind the cited data is crucial for interpreting results and designing future validation studies.
Protocol 1: Broad Benchmarking of Antibiotic Prescribing
This protocol is adapted from a large-scale comparison of 14 LLMs. [9] [1]
- 1. Case Development: A set of 60 clinical cases covering 10 different infection types was developed. Each case was accompanied by a relevant antibiogram. [9] [1]
- 2. Model Prompting: A standardized prompt was used to ask each LLM to recommend an antibiotic, including drug choice, dosage, and treatment duration. [9] [1]
- 3. Blinded Expert Review: The model responses were anonymized and presented to a blinded panel of infectious disease experts. [9] [1]
- 4. Outcome Assessment: The panel evaluated each response on three primary outcomes:
Protocol 2: Evaluation of Infection Prevention & Control (IPC) Decision-Making
This protocol was used to evaluate LLMs in a realistic hospital consultation context. [93]
- 1. Scenario Creation: The research team created 30 clinical infection control scenarios from a tertiary hospital setting. [93]
- 2. Prompting Methods: Two distinct prompting strategies were employed for each model:
- Open-Ended Inquiry: A direct, unstructured request for IPC recommendations.
- Structured Template: A predefined template requiring specific, structured information. [93]
- 3. Multi-Disciplinary Expert Rating: Sixteen experts, including senior and junior infection control nurses and physicians, rated the model responses. They used a 1-10 scale across five domains: coherence, conciseness, usefulness & relevance, evidence quality, and actionability. [93]
- 4. Qualitative Analysis: Experts also performed a qualitative review to identify critical errors, safety risks, and limitations in practical applicability that quantitative scores might not capture. [93]
Diagram 1: Workflow for LLM validation in antibiotic prescribing and infection control.
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential components used in the featured experiments, which are critical for replicating studies or building new validation frameworks.
Table 4: Essential Components for LLM Validation Experiments
| Item | Function in Validation Research | Example from Search Results |
|---|---|---|
| Clinical Vignettes | Standardized patient cases used to prompt LLMs, ensuring consistent evaluation across models. | 60 cases with antibiograms [9] [1]; 30 IPC scenarios [93]; 24 vignettes for GP practice. [37] |
| National/International Guidelines | The evidence-based standard against which LLM recommendations are compared for appropriateness. | Referenced against IDSA, ESCMID, NASS, and national prescribing guidelines. [93] [12] [95] |
| Blinded Expert Panel | A group of clinical specialists who assess the quality, accuracy, and safety of LLM outputs without knowing which model generated them. | Used in multiple studies to minimize bias in evaluation. [9] [1] |
| Structured Prompt Templates | Predefined formats for querying LLMs, which can significantly improve the quality and consistency of responses. | A study found structured prompting improved evidence quality in IPC recommendations. [93] |
| Retrieval-Augmented Generation (RAG) Framework | A technique that enhances an LLM's knowledge by providing it with access to an external, authoritative database. | Used to improve LLM accuracy in identifying drug-related problems. [90] |
| Antibiograms | Local summary of antimicrobial susceptibility rates, essential for prompting LLMs to give context-aware, guideline-compliant recommendations. | Provided alongside clinical cases to inform appropriate antibiotic choice. [9] [1] |
Diagram 2: Enhanced decision support using a RAG framework.
The experimental data clearly demonstrates that while LLMs like ChatGPT-o1, GPT-4.1, and Claude 3.5 Sonnet show significant promise in supporting antibiotic prescribing and infection management, their performance is highly variable and context-dependent. [93] [9] [94] Key findings indicate that performance drops with increasing case complexity and that critical errors can occur, underscoring the necessity of human oversight. [93] [9] [1] The most effective application of this technology appears to be in a "co-pilot" capacity, where it augments, rather than replaces, the expertise of clinicians and pharmacists. [90] Future validation research should focus on improving model performance in complex scenarios, integrating tools like RAG for better contextual awareness, and standardizing evaluation protocols to ensure safety and efficacy before clinical implementation.
Comparison with Human Practitioner Prescribing Patterns
Antimicrobial resistance represents a critical global health threat, underscoring the necessity for optimal antibiotic prescribing. Large language models (LLMs) have emerged as potential tools to support clinical decision-making. This guide objectively compares the performance of LLMs against human practitioners in antibiotic prescribing, a core task within the broader validation of LLMs for clinical accuracy research. The analysis synthesizes current experimental data to evaluate their respective strengths, limitations, and potential for integration into antimicrobial stewardship programs.
Quantitative Performance Comparison
The following table summarizes key performance metrics for human practitioners and various LLMs from comparative studies.
Table 1: Overall Antibiotic Prescribing Accuracy: LLMs vs. Human Practitioners
| Prescriber Type | Specific Model/Practitioner | Diagnosis Accuracy (%) | Antibiotic Choice Accuracy (%) | Dosage/Duration Accuracy (%) | Guideline Adherence (%) |
|---|---|---|---|---|---|
| Human Practitioner | General Practitioners (Pooled) [37] | 96-100 | 83-92 | 50-75 | 100 (Referenced) |
| LLM (High Performer) | ChatGPT-o1 [1] | - | 71.7 | 96.7 (Dosage) | - |
| LLM (High Performer) | GPT-4o [50] [37] | 92-100 | 88-100 | ~64 (Duration) | 38-96 |
| LLM (Mid Performer) | Claude 3.5 Sonnet [1] [50] | - | ~64 | 91.7 (Dosage) | - |
| LLM (Lower Performer) | Gemini [1] [50] | - | Lowest | 75 (Duration) | - |
Performance by Clinical Scenario Complexity
LLM and human performance varies significantly with the complexity of the clinical case. The data indicates that while LLMs can perform well in standardized scenarios, their accuracy declines in more complex situations.
Table 2: Performance Variation by Case Complexity and Infection Type
| Clinical Context | Human Practitioner Performance | Representative LLM Performance | Key Findings |
|---|---|---|---|
| Simple Respiratory Infections [96] [37] | High accuracy; susceptible to non-clinical factors (e.g., patient demand) | High accuracy in diagnosis and prescribing choice [37] | LLMs may be less susceptible to psychosocial factors influencing human prescribers. |
| Complex/Difficult-to-Treat Infections [1] | Maintains higher reasoning capability; relies on specialist consultation | Significant decline in appropriateness of recommendations [1] | Performance gap widens, with LLMs struggling with complex microbiology and comorbidities. |
| Bloodstream Infections [12] | Managed per ID consultation; high adherence to guidelines | 64% appropriateness for empirical therapy; 36% for targeted therapy [12] | LLM suggestions for targeted therapy were notably less appropriate. |
| Off-Label Prescribing (Rare Diseases) [97] | Time-consuming literature search; relies on limited evidence | Effective at retrieving relevant scientific publications [97] | LLMs can speed up information synthesis, but human oversight remains critical. |
Detailed Experimental Protocols
To ensure reproducibility and critical appraisal, this section outlines the methodologies of key cited experiments.
Protocol 1: Multi-Model Evaluation in Clinical Vignettes
This protocol was designed to benchmark LLMs against human prescribers across different healthcare systems [37].
- Objective: To compare the antibiotic prescribing decisions of LLMs and general practitioners (GPs) against national guidelines.
- Vignette Development: Researchers developed 24 clinical vignettes containing information on infection type, patient gender, age group, and comorbidities.
- Country Selection: The study included four countries with distinct national prescribing guidelines: Ireland, the UK, the USA, and Norway.
- Model and Practitioner Prompting: A GP from each country and six different LLMs (ChatGPT, Gemini, Copilot, Mistral AI, Claude, and Llama 3.1) were provided with the vignettes. Each was prompted to provide a treatment, including the country as a contextual factor.
- Outcome Assessment: Responses were evaluated for:
- Diagnosis accuracy
- Appropriateness of antibiotic prescribing (yes/no)
- Choice of antibiotic
- Correct dosage and treatment duration
- Adherence to the respective national guideline
- Additional Metrics: The study also assessed typical LLM limitations, including hallucination and data leakage.
Protocol 2: Blinded Expert Review of LLM Recommendations
This protocol assessed the quality of LLM-generated antibiotic recommendations across a wide range of infection types and models [1].
- Objective: To assess the performance of various LLMs in recommending appropriate antibiotic treatments, including drug choice, dosage, and duration.
- Model Selection: Fourteen LLMs were evaluated, including standard and premium versions of ChatGPT, Claude, Copilot, Gemini, Le Chat, Grok, Perplexity, and Pi.ai.
- Case Development: The study utilized 60 clinical cases with antibiograms, covering 10 different infection types to ensure breadth and varying complexity.
- Prompting and Data Collection: A standardized prompt was used for all LLM queries, focusing on generating a complete antibiotic recommendation. A total of 840 responses were collected.
- Blinded Review Process: All LLM responses were anonymized and presented to a blinded expert panel. The panel assessed:
- Overall antibiotic appropriateness
- Dosage correctness
- Treatment duration adequacy
- Analysis: Performance was analyzed overall and stratified by case complexity and the type of microorganism involved.
Research Reagent Solutions
The table below details key resources and their functions essential for conducting rigorous comparisons of prescribing patterns.
Table 3: Essential Research Materials and Tools for Prescribing Pattern Studies
| Item Name | Type | Function in Research |
|---|---|---|
| Clinical Vignettes [37] | Standardized Case Scenarios | Provides a controlled, reproducible foundation for comparing decision-making across practitioners and models without patient risk. |
| National Antibiotic Guidelines [98] [37] | Reference Standard | Serves as the objective benchmark for evaluating the appropriateness of prescribed antibiotic choice, dose, and duration. |
| Blinded Expert Review Panel [1] | Human Assessment Tool | Provides gold-standard, unbiased evaluation of the quality and appropriateness of treatment recommendations. |
| Antibiograms [1] | Laboratory Data | Provides essential local antimicrobial resistance data, enabling context-specific and realistic recommendations for targeted therapy. |
| Standardized Prompt Protocol [1] [12] | Methodological Tool | Ensures consistency and reproducibility when querying multiple LLMs, reducing variability introduced by prompt phrasing. |
| Resistance to Change Scale [99] | Psychometric Questionnaire | Assesses potential human bias or hesitation toward adopting AI-based recommendations in clinical practice. |
Workflow for Comparative Evaluation
The following diagram illustrates the logical workflow for a robust study comparing human and LLM prescribing patterns.
The integration of Large Language Models (LLMs) into clinical decision-support systems represents a transformative shift in medical practice, particularly in specialized domains such as antibiotic prescribing. However, the probabilistic nature of these models introduces a critical validation challenge: response variation to identical prompts. This inconsistency threatens the reliability and safety of LLM-assisted clinical decision-making, especially in antimicrobial stewardship where inappropriate antibiotic use contributes significantly to antimicrobial resistance [12]. While studies demonstrate the promising capabilities of LLMs in achieving high accuracy on standardized medical examinations, their behavior in real-world clinical scenarios characterized by ambiguity and judgment calls remains poorly understood [69]. This analysis systematically examines the consistency of LLM responses across multiple dimensions—comparing performance variation across models, quantifying internal consistency upon repeated prompting, and identifying specific clinical factors that exacerbate response instability. Understanding these patterns is fundamental for establishing validation frameworks that ensure LLMs function as reliable partners in optimizing antibiotic therapy and combating global antimicrobial resistance.
Comparative Performance of LLMs in Antibiotic Prescribing
Quantitative Accuracy Across Models
Recent comparative studies reveal significant variability in the antibiotic prescribing performance of different LLMs. A 2025 evaluation of 14 commercial and research LLMs assessed 840 responses across 60 clinical cases covering 10 infection types, measuring accuracy in drug choice, dosage correctness, and treatment duration adequacy [1] [9]. The results demonstrate substantial performance differences between models, as summarized in Table 1.
Table 1: LLM Performance in Antibiotic Prescribing Accuracy [1] [9]
| Large Language Model | Overall Antibiotic Appropriateness (%) | Dosage Correctness (%) | Treatment Duration Adequacy (%) |
|---|---|---|---|
| ChatGPT-o1 | 71.7 | 96.7 | Data not specified |
| Perplexity Pro | Data not specified | 90.0 | Data not specified |
| Claude 3.5 Sonnet | Data not specified | 91.7 | Data not specified |
| Gemini (multiple versions) | Lowest accuracy | Data not specified | 75.0 |
| Claude 3 Opus | Lowest accuracy | Data not specified | Data not specified |
The data indicates that ChatGPT-o1 demonstrated superior performance in overall antibiotic appropriateness and dosage correctness, while Gemini provided the most appropriate treatment duration recommendations despite its overall lower accuracy [1] [9]. This performance dissociation across different prescribing components highlights the multifaceted nature of appropriate antibiotic stewardship and suggests that models may have specialized strengths despite overall accuracy metrics.
Performance Degradation in Complex Cases
A critical finding across studies is the significant degradation of LLM performance with increasing case complexity. The comparative analysis of 14 LLMs revealed that all models exhibited decreased accuracy when confronted with difficult-to-treat microorganisms and complex clinical presentations [1] [9]. This pattern mirrors challenges observed in human clinical reasoning, where atypical presentations, comorbid conditions, and antimicrobial resistance patterns increase diagnostic and therapeutic uncertainty. The performance decline in complex scenarios underscores the limitations of current LLMs as autonomous clinical decision-makers and emphasizes their role as supportive rather than definitive tools in challenging infectious disease cases.
Experimental Protocols for Assessing LLM Consistency
Standardized Prompting for Antibiotic Prescribing Evaluation
The methodology for evaluating LLM consistency in antibiotic prescribing followed rigorous experimental protocols to ensure comparable results. The 2025 comparative study employed 60 clinical cases with accompanying antibiograms representing 10 different infection types [1] [9]. Researchers used a standardized prompt template to query each model, specifically requesting antibiotic recommendations focused on three critical components: drug choice, dosage, and treatment duration. To eliminate evaluation bias, responses were anonymized and assessed by a blinded expert panel using predetermined criteria for antibiotic appropriateness, dosage correctness, and duration adequacy [1]. This protocol design minimizes confounding variables and enables direct comparison of model performance across diverse but standardized clinical scenarios.
Assessing Intra-Model Variability Through Repeated Prompting
To specifically measure response consistency rather than mere accuracy, researchers have employed experimental designs that query the same model multiple times with identical prompts. A 2025 cross-sectional simulation study examined this intra-model variability by presenting four nuanced inpatient management scenarios to six different LLMs, with each vignette posed five times in independent sessions [69]. The researchers employed a standardized priming prompt: "You are an expert hospitalist, faced with the following patient scenario. What would you do and why?" followed by clinical vignettes requiring binary management decisions [69]. Internal consistency was quantified as the proportion of identical recommendations across the five runs, creating a reproducibility metric ranging from 0 to 1 for each model-scenario combination [69].
Validation Frameworks for Response Credibility
Beyond measuring consistency, researchers have developed methodologies to assess the factual credibility of LLM responses in clinical contexts. These include retrieval-augmented generation (RAG) frameworks that ground model outputs in established clinical guidelines and medical literature [100]. The DOSAGE dataset represents another validation approach, providing structured, guideline-based antibiotic dosing information that serves as a benchmark for evaluating LLM recommendations against validated clinical standards [100]. These methodologies help distinguish between consistently incorrect responses (which represent systematic errors) and variably correct responses (which indicate instability in clinical reasoning).
Variation Patterns in LLM Responses
Inter-Model Recommendation Divergence
Analysis of LLM responses reveals substantial divergence between different models when presented with identical clinical scenarios. In the study of nuanced inpatient management decisions, models demonstrated complete disagreement in every scenario presented [69]. As detailed in Table 2, this inter-model variation occurred even for clear-cut clinical decisions with established guidelines, such as peri-procedural bridging for patients on direct oral anticoagulants, where guidelines generally recommend against bridging [69].
Table 2: Inter-Model Recommendation Variation in Clinical Scenarios [69]
| Clinical Scenario | Management Options | Percentage of Models Recommending Each Option |
|---|---|---|
| Transfusion at borderline hemoglobin | Transfuse vs. Observe | 67% vs. 33% |
| Resumption of anticoagulation after GI bleed | Restart vs. Hold | 50% vs. 50% |
| Discharge readiness with creatinine rise | Discharge vs. Delay | 50% vs. 50% |
| Peri-procedural bridging in high-risk patient | Bridge vs. No-bridge | 17% vs. 83% |
The observed inter-model disagreement reflects fundamental differences in how various models weigh clinical factors, interpret ambiguous information, and apply medical knowledge [69]. This variation mirrors the well-documented practice pattern variations among human clinicians, suggesting that LLMs may inherit the inconsistencies present in their training data derived from heterogeneous clinical sources.
Intra-Model Inconsistency Upon Repeated Prompting
Perhaps more concerning than inter-model variation is the substantial inconsistency within individual models when identically prompted multiple times. The cross-sectional simulation study found that some commercially available LLMs changed their clinical recommendations in up to 40% of repeated queries for the same vignette, with internal consistency scores as low as 0.60 (where 1.0 represents perfect agreement across all runs) [69]. This flip-flopping occurred even in scenarios with strong guideline support, such as the decision to bridge anticoagulation, where most models consistently recommended against bridging but two models (Grok and Gemini) showed lower consistency scores of 0.6 [69]. This demonstrates that the probabilistic nature of LLM text generation can produce clinically meaningful variations in output despite identical input prompts.
Consistency-Reliability Dissociation
Research indicates that consistency does not necessarily correlate with clinical accuracy. The domain-specific model OpenEvidence demonstrated perfect internal consistency (1.0) across all vignettes in the management scenario study but was noted to provide incomplete clinical reasoning, such as failing to mention stroke risk in anticoagulation decisions [69]. Conversely, some general-purpose models with lower consistency scores provided more comprehensive risk-benefit analyses [69]. This dissociation presents a validation challenge: consistent but flawed recommendations may be more dangerous than variable recommendations that occasionally provide optimal guidance, as consistency might create false confidence in systematically incorrect outputs.
Visualization of LLM Consistency Assessment Workflow
Workflow for LLM Consistency Assessment
Table 3: Essential Research Reagents for LLM Consistency Analysis
| Research Reagent | Function in Validation Studies | Example Implementation |
|---|---|---|
| Standardized Clinical Vignettes | Provides consistent input for comparing model performance across diverse scenarios | 60 cases with antibiograms covering 10 infection types [1] |
| Blinded Expert Panel | Eliminates assessment bias in evaluating response appropriateness | Infectious diseases specialists reviewing anonymized LLM responses [1] |
| DOSAGE Dataset | Structured benchmark for validating dosing recommendations against guideline-based logic | Patient-specific dosing regimens based on age, weight, renal function [100] |
| Consistency Metrics | Quantifies response stability across repeated trials | Internal consistency score (proportion of identical recommendations across runs) [69] |
| Retrieval-Augmented Generation (RAG) Framework | Enhances factual grounding of LLM outputs in established literature | Integrating current guidelines and medical literature into response generation [100] |
The empirical evidence demonstrates that response variation to identical prompts represents a fundamental challenge in deploying LLMs for clinical decision support, particularly in antibiotic prescribing. Significant performance differences exist across models, with even the highest-performing LLMs showing accuracy degradation in complex cases [1] [9]. Furthermore, both inter-model disagreement and intra-model inconsistency upon repeated prompting reveal inherent limitations in the current generative AI paradigm for clinical applications [69]. These findings underscore the necessity of rigorous, standardized consistency assessment as an integral component of LLM validation frameworks. Future research should prioritize developing methods to improve response stability without sacrificing nuanced clinical reasoning, potentially through ensemble approaches that leverage multiple models or constrained generation techniques that anchor outputs to established clinical guidelines. For researchers, clinicians, and policymakers, these results emphasize that LLMs should be viewed as consultative tools rather than deterministic calculators, with human oversight remaining essential for safe implementation in clinical workflows, especially in high-stakes domains like antimicrobial stewardship.
The integration of large language models (LLMs) into healthcare decision-making represents a transformative shift with particular significance for antibiotic prescribing, where inappropriate recommendations carry immediate risks for individual patients and long-term consequences for public health through antimicrobial resistance. [12] [11] Assessing the harm potential of LLM-generated recommendations requires moving beyond simple accuracy metrics to classify and quantify specific failure modes, from dosage errors to medication selection mistakes. This evaluation is technically complex due to the probabilistic nature of LLMs, which operate as "black box" systems whose decision-making processes are not fully transparent. [12] Furthermore, these models demonstrate significant performance variability across different clinical scenarios, with degradation in accuracy observed particularly for complex cases involving difficult-to-treat microorganisms. [1] [11] This comparative guide objectively analyzes current experimental data on LLM performance for antibiotic prescribing, with specific focus on methodologies for classifying inappropriate recommendations and assessing their potential clinical harm.
Comparative Performance Analysis: Quantitative Benchmarks Across LLMs
Recent comparative studies reveal substantial variability in antibiotic prescribing performance across different LLMs. A comprehensive 2025 evaluation of 14 LLMs across 60 clinical cases with antibiograms found ChatGPT-o1 demonstrated the highest accuracy in antibiotic prescriptions, with 71.7% (43/60) of recommendations classified as correct and only one (1.7%) incorrect. [1] [9] In contrast, Gemini and Claude 3 Opus showed the lowest accuracy among tested models. [1] This study collected and analyzed 840 responses, providing a robust dataset for benchmarking performance across multiple dimensions of antibiotic prescribing. [1] [9]
Table 1: Overall Antibiotic Prescription Accuracy Across LLMs
| LLM Model | Accuracy (%) | Incorrect Recommendations (%) | Number of Cases |
|---|---|---|---|
| ChatGPT-o1 | 71.7 | 1.7 | 60 |
| GPT-4.0 | 81.0* | 19.0* | 16* |
| GPT-3.5 | 62.5* | 37.5* | 16* |
| Gemini | Lowest accuracy | Not specified | 60 |
| Claude 3 Opus | Lowest accuracy | Not specified | 60 |
*Data from specific guideline adherence study on antibiotic prophylaxis in spine surgery [101]
Dosage and Treatment Duration Accuracy
Beyond appropriate antibiotic selection, correct dosing and treatment duration are critical components of safe prescribing. Research indicates significant variability in performance across these dimensions. In evaluations, dosage correctness was highest for ChatGPT-o1 (96.7%, 58/60), followed by Perplexity Pro (90.0%, 54/60) and Claude 3.5 Sonnet (91.7%, 55/60). [1] For treatment duration, Gemini provided the most appropriate recommendations (75.0%, 45/60), while Claude 3.5 Sonnet demonstrated a tendency to over-prescribe duration. [1] This discrepancy highlights how LLMs may excel in different components of the prescribing process, necessitating comprehensive evaluation across all prescription elements.
Table 2: Component-Specific Performance Metrics Across LLMs
| LLM Model | Dosage Correctness (%) | Duration Adequacy (%) | Tendencies Identified |
|---|---|---|---|
| ChatGPT-o1 | 96.7 | Not specified | Highest overall accuracy |
| Perplexity Pro | 90.0 | Not specified | Not specified |
| Claude 3.5 Sonnet | 91.7 | Not specified | Over-prescribing duration |
| Gemini | Not specified | 75.0 | Most appropriate duration |
Harm Potential Classification Framework
The most critical dimension of LLM evaluation for clinical implementation is assessing the potential harm of inappropriate recommendations. Research has begun to categorize and quantify these risks. In one study evaluating GPT-4 for bloodstream infection management, 2% of empirical and 5% of targeted therapy suggestions were classified as potentially harmful. [12] Examples included narrowing antibiotic spectrum inappropriately in febrile neutropenia and de-escalating therapy dangerously in neutropenic patients with ongoing sepsis. [12] Another study on infection prevention and control consultations found critical deficiencies across all evaluated models (GPT-4.1, DeepSeek V3, and Gemini 2.5 Pro Exp), including impractical recommendations and errors in clinical judgment that posed potential safety risks despite generally positive evaluation scores. [93]
Experimental Protocols: Methodologies for LLM Validation in Antibiotic Prescribing
Standardized Clinical Case Evaluation
The primary methodology for assessing LLM performance in antibiotic prescribing involves standardized evaluation across diverse clinical scenarios. The comparative study of 14 LLMs utilized 60 clinical cases with antibiograms covering 10 infection types. [1] [9] Researchers employed a standardized prompt for antibiotic recommendations focusing on three key elements: drug choice, dosage, and treatment duration. [1] All responses were anonymized and reviewed by a blinded expert panel that assessed antibiotic appropriateness, dosage correctness, and duration adequacy. [1] [9] This rigorous methodology ensures objective assessment and minimizes evaluation bias, providing comparable data across different models.
Guideline Adherence Assessment
An alternative approach evaluates LLM performance against established clinical guidelines. One study assessed ChatGPT's GPT-3.5 and GPT-4.0 models using 16 questions from the North American Spine Society (NASS) Evidence-based Clinical Guidelines for Antibiotic Prophylaxis in Spine Surgery. [101] In this protocol, questions were presented verbatim from the guidelines, with modification only to include context about spine surgery where needed. [101] Responses were compared to guideline recommendations for accuracy, with researchers also evaluating the models' tendency toward overconfidence and ability to reference appropriate evidence. [101] This methodology provides a structured framework for assessing alignment with evidence-based standards.
Simulated Clinical Consultation Workflow
More complex experimental designs simulate real-world clinical workflows. In one study, researchers provided GPT-4 with anonymized clinical information available to physicians managing bloodstream infections and prompted it to act as an infectious diseases specialist consulting on each case. [12] Expert reviewers then classified recommendations for appropriateness and potential harm according to local and international guidelines. [12] Another study employed a cross-sectional benchmarking design with 30 clinical infection control scenarios, using two prompting methods (open-ended inquiry and structured template) to assess robustness across different interaction modes. [93] This approach better captures performance in realistic clinical contexts.
Figure 1: Experimental Workflow for LLM Validation in Antibiotic Prescribing
Classification and Analysis of Inappropriate Recommendations
Typology of LLM Prescribing Errors
Analysis of LLM performance data reveals several categories of inappropriate recommendations with varying harm potential:
Critical Errors with High Harm Potential: These include suggestions that could directly lead to treatment failure or patient harm, such as narrowing antibiotic spectrum inappropriately in febrile neutropenia or recommending contraindicated medications. [12] In one study, these constituted 2-5% of recommendations for bloodstream infection management. [12]
Guideline Deviations with Moderate Risk: Recommendations that contradict established guidelines without immediate danger, such as suggesting incorrect first-line antibiotics or inappropriate duration. GPT-3.5 demonstrated this by explicitly recommending cefazolin as first-line despite inconclusive evidence, with 25% of its responses deemed overly confident. [101]
Contextual Misapplication: Recommendations that are pharmacologically sound but misapplied to specific clinical contexts. For instance, LLMs may fail to distinguish clinically important factors without explicit prompting or provide management plans inappropriate for the specific scenario. [101] [93]
Omission Errors: Failure to recommend necessary antibiotics or address critical aspects of management. Research indicates performance declines with increasing case complexity, particularly for difficult-to-treat microorganisms. [1]
Factors Influencing Error Frequency
Several factors emerge as significant predictors of LLM prescribing inaccuracies:
Case Complexity: Studies consistently show degraded performance with increasing clinical complexity, particularly for infections with difficult-to-treat microorganisms or patients with complicating factors like immunosuppression. [1] [11]
Model Capabilities: Later model generations demonstrate improved accuracy, with GPT-4.0 showing 81% accuracy compared to GPT-3.5's 62.5% on the same guideline questions. [101] GPT-4.0 also showed reduced overconfidence and better citation of evidence. [101]
Prompting Strategy: Research indicates structured prompting yields significant improvements in output quality, primarily by enhancing evidence quality. [93] The method of engagement significantly influences response accuracy and relevance.
Figure 2: Classification of LLM Prescribing Error Types and Harm Potential
Table 3: Essential Research Reagents and Resources for LLM Validation Studies
| Resource Category | Specific Examples | Function in Validation Research |
|---|---|---|
| Clinical Case Databases | 60 clinical cases with antibiograms (10 infection types) [1]; 30 clinical IPC scenarios [93] | Provides standardized evaluation datasets representing diverse clinical challenges |
| Reference Standards | IDSA/ESCMID guidelines [12]; NASS Evidence-based Clinical Guidelines [101] | Establishes evidence-based benchmarks for appropriateness assessments |
| Expert Panels | Blinded infectious disease specialists [1]; Multidisciplinary reviewers (physicians, senior/junior ICNs) [93] | Provides gold-standard human evaluation for model performance benchmarking |
| Evaluation Frameworks | Appropriateness classification [1]; Harm potential rating [12]; Composite quality scales (coherence, usefulness, evidence quality, actionability) [93] | Standardizes assessment metrics across studies for comparative analysis |
| LLM Access Platforms | OpenAI GPT series [1] [101]; Anthropic Claude [1]; Google Gemini [1]; DeepSeek V3 [93] | Enables direct performance benchmarking across different model architectures |
Current experimental data demonstrates that while certain LLMs like ChatGPT-o1 and GPT-4.0 show promising accuracy for antibiotic prescribing, significant concerns remain regarding their potential for generating inappropriate recommendations with varying levels of harm potential. [1] [101] The classification and quantification of these errors reveals a spectrum of risk, from critical errors affecting 2-5% of recommendations in some studies to more common guideline deviations and contextual misapplications. [12] [93] Performance variability across models, clinical scenarios, and prescribing components (drug selection, dosing, duration) underscores the necessity for comprehensive, multi-dimensional evaluation protocols before clinical implementation. [1] The emerging discipline of LLM psychometrics—applying rigorous measurement principles to model evaluation—provides valuable frameworks for future validation efforts. [102] As models continue to evolve, ongoing independent benchmarking using standardized methodologies and explicit harm potential classification will be essential for ensuring patient safety and effective antimicrobial stewardship in this rapidly advancing field.
Conclusion
The validation of large language models for antibiotic prescribing reveals both significant potential and substantial challenges. Current evidence demonstrates that while advanced models like ChatGPT-o1 can achieve 71.7% accuracy in antibiotic recommendations with high dosage correctness (96.7%), significant performance variability exists across models, with accuracy declining markedly in complex cases involving difficult-to-treat pathogens. The field requires standardized evaluation frameworks, addressing of hallucinations and biases, and resolution of regulatory uncertainties before reliable clinical integration. Future directions must include development of specialized antimicrobial stewardship LLMs, robust clinical trial validation, establishment of continuous monitoring systems, and creation of adapted regulatory pathways for AI clinical decision support. Success will depend on collaborative efforts between AI developers, clinical researchers, regulatory bodies, and healthcare institutions to ensure these powerful tools enhance rather than compromise patient safety and antimicrobial stewardship principles.
References
- 1. Comparing large language models for antibiotic ... [https://pubmed.ncbi.nlm.nih.gov/40113208]
- 2. 全科医生还是ChatGPT?大型语言模型在开具抗生素处方时支持 ... [https://suppr.wilddata.cn/browses/detail/pubmed/40079276]
- 3. 大型语言模型助力抗生素处方:潜力与挑战- AI与医疗健康 [https://www.familydoctor.cn/news/daxing-yuyan-moxing-zhuli-kangshengsu-chufang-qianli-tiaozhan-61007.html]
- 4. 大型语言模型助力抗生素处方:机遇与挑战 - 家医大健康 [https://www.familydoctor.cn/news/daxing-yuyan-moxing-zhuli-kangshengsu-chufang-jiyu-tiaozhan-61076.html]
- 5. Advantages and limitations of large language models for antibiotic ... [https://www.nature.com/articles/s44259-025-00084-5?error=cookies_not_supported]
- 6. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 7. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/20483949/]
- 8. Investigating the know-do gap in antibiotics prescribing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422172/]
- 9. Comparing large language models for antibiotic ... [https://www.sciencedirect.com/science/article/pii/S1198743X2500120X]
- 10. Challenges and applications of artificial intelligence in ... [https://www.nature.com/articles/s44259-024-00068-x]
- 11. Clinical Considerations on a Rapidly Evolving Landscape [https://link.springer.com/article/10.1007/s40121-025-01114-5]
- 12. Advantages and limitations of large language models for ... [https://www.nature.com/articles/s44259-025-00084-5]
- 13. Evaluating AI performance in infectious disease education [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557576/]
- 14. Comparison of OneChoice® AI-based clinical decision ... [https://www.medrxiv.org/content/10.1101/2025.08.15.25333753v1]
- 15. Fine-grained Alignment of Large Language Models for ... [https://arxiv.org/html/2503.03687v2]
- 16. The AI tools supporting infectious disease management [https://hospitalpharmacyeurope.com/pharmacy-practice/health-technology/the-ai-tools-supporting-infectious-disease-management-escmid-global-2025/]
- 17. Antibiotics and Artificial Intelligence: Clinical Considerations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11933589/]
- 18. CLIN-LLM: A Safety-Constrained Hybrid Framework for ... [https://arxiv.org/html/2510.22609v1]
- 19. An Untrained LLM Makes Good Antibiotic Choices [https://journalfeed.org/article-a-day/2025/an-untrained-llm-makes-good-antibiotic-choices/]
- 20. Evaluating AI performance in infectious disease education [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1679153/full]
- 21. Advantages and limitations of large language models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11868396/]
- 22. Unveiling the power and limitations of large language models [https://www.6clicks.com/resources/blog/unveiling-the-power-of-large-language-models]
- 23. Limitations of large language models in clinical problem ... [https://www.nature.com/articles/s41598-025-22940-0]
- 24. Probabilistic and Deterministic Results in AI Systems [https://www.gaine.com/blog/probabilistic-and-deterministic-results-in-ai-systems]
- 25. Preventing unrestricted and unmonitored AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743128/]
- 26. The Hidden Cost of Poor Data Quality: Why Your AI ... [https://www.akaike.ai/resources/the-hidden-cost-of-poor-data-quality-why-your-ai-initiative-might-be-set-up-for-failure]
- 27. Bringing transparency to the data used to train artificial ... [https://mitsloan.mit.edu/ideas-made-to-matter/bringing-transparency-to-data-used-to-train-artificial-intelligence]
- 28. Comprehensive Analysis of Transparency and Accessibility ... [https://arxiv.org/abs/2502.18505]
- 29. New Performance Measurement Framework for Realizing ... [https://www.jmir.org/2025/1/e68674]
- 30. AI Evaluation in Clinical Decision Support: Building a ... [https://www.elsevier.com/connect/ai-evaluation-in-clinical-decision-support-building-a-foundation-of-trust]
- 31. Implementing an AI-enhanced clinical decision support ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551136/]
- 32. An AI-Based Clinical Decision Support System for Antibiotic ... [https://humanfactors.jmir.org/2025/1/e66699]
- 33. Guideline-Based Clinical Decision Support Framework for ... [https://www.researchprotocols.org/2025/1/e63339]
- 34. What Is Data Completeness? Definition, Examples, And KPIs [https://www.montecarlodata.com/blog-what-is-data-completeness/]
- 35. A Quasi-Experimental Study of Providing Antibiotic Cost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4510246/]
- 36. Understanding the complexities of antibiotic prescribing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8299683/]
- 37. GP or ChatGPT? Ability of large language models (LLMs) ... [https://pubmed.ncbi.nlm.nih.gov/40079276/]
- 38. Antibiotics - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK535443/]
- 39. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 40. Antimicrobial Resistance Patterns: Review of the Antibiogram ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7686934/]
- 41. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 42. Antibiotic‐prescribing patterns in outpatient departments from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12624738/]
- 43. Antimicrobial Resistance [https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/antimicrobial-resistance]
- 44. Use of Expert Panels to Define the Reference Standard in Diagnostic Research: A Systematic Review of Published Methods and Reporting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3797139/]
- 45. Home - Blind Review [https://blindreview.com/]
- 46. Double-Blind Reviews: A Step Toward Eliminating Unconscious Bias - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8806370/]
- 47. A Pilot Study Evaluating the Impact of an Algorithm-Driven ... [https://www.mdpi.com/2226-4787/13/1/30]
- 48. Performance analysis of large language models Chatgpt ... [https://link.springer.com/article/10.1007/s10238-025-01743-7]
- 49. Blinded Experts: A New Solution for Credibility in Litigation – The Civil Jury Project at NYU School of Law [https://civiljuryproject.law.nyu.edu/blinded-experts-a-new-solution-for-credibility-in-litigation/]
- 50. Benchmarking the Confidence of Large Language Models in ... [https://medinform.jmir.org/2025/1/e66917]
- 51. Autonomous vs. Assistive AI: How to unlock real value in ... [https://www.digitaldiagnostics.com/autonomous-vs-assistive-ai-how-to-unlock-real-value-in-healthcare/]
- 52. Assistive AI vs. Agentic AI: Key Differences & Use Cases [https://emerline.com/blog/ai-assistant-vs-ai-agent]
- 53. The Sense of Agency in Assistive Robotics Using Shared ... [https://arxiv.org/html/2501.07462v1]
- 54. GP or ChatGPT? Ability of large language models (LLMs) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046391/]
- 55. Autonomous vs Assistive Agents: Which is Right for Your ... [https://www.salesforce.com/blog/autonomous-vs-assistive-agents/]
- 56. Prompt Engineering in Clinical Practice: Tutorial for ... [https://www.jmir.org/2025/1/e72644]
- 57. Prompt engineering in consistency and reliability with the ... [https://www.nature.com/articles/s41746-024-01029-4]
- 58. Prompt Engineering in Healthcare: Best Practices ... [https://healthtechmagazine.net/article/2025/04/prompt-engineering-in-healthcare-best-practices-strategies-trends-perfcon]
- 59. Acute Psychotic Episode Induced by Antimicrobial Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC10082676/]
- 60. Psychosis as an adverse effect of antibiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8474525/]
- 61. A Comprehensive Survey of Hallucination Mitigation ... [https://arxiv.org/abs/2401.01313?]
- 62. Key Strategies to Minimize LLM Hallucinations [https://www.turing.com/resources/minimize-llm-hallucinations-strategy]
- 63. Common Antibiotics May Cause Delirium, Confusion And ... [https://www.forbes.com/sites/judystone/2016/02/18/common-antibiotics-may-cause-confusion-and-hallucinations/]
- 64. Common Antibiotics May Be Linked to Temporary Mental ... [https://www.aan.com/PressRoom/Home/PressRelease/1433]
- 65. LLM hallucination mitigation techniques: Explained [https://www.tredence.com/blog/mitigating-hallucination-in-large-language-models]
- 66. Global variation in antibiotic prescribing guidelines and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368364/]
- 67. Evaluation of large language models' ability to identify ... [https://pubmed.ncbi.nlm.nih.gov/40590636/]
- 68. Variation in Large Language Model Recommendations ... [https://pubmed.ncbi.nlm.nih.gov/41055682/]
- 69. Variation in Large Language Model Recommendations ... [https://link.springer.com/article/10.1007/s11606-025-09888-7]
- 70. Achieving large-scale clinician adoption of AI-enabled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11141172/]
- 71. FDA Oversight: Understanding the Regulation of Health AI Tools • Bipartisan Policy Center [https://bipartisanpolicy.org/issue-brief/fda-oversight-understanding-the-regulation-of-health-ai-tools/]
- 72. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 73. Artificial Intelligence-Enabled Medical Devices [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-enabled-medical-devices]
- 74. Data Leakage Prevention (DLP) for LLMs [https://community.ibm.com/community/user/blogs/anuj-bahuguna/2025/04/27/data-leakage-prevention-for-llms-safeguarding-sens]
- 75. LLM07:2025 System Prompt Leakage [https://genai.owasp.org/llmrisk/llm07-insecure-plugin-design/]
- 76. LLM Data Leakage: 10 Best Practices for Securing LLMs [https://www.cobalt.io/blog/llm-data-leakage-10-best-practices]
- 77. AI and Privacy: Shifting from 2024 to 2025 | CSA [https://cloudsecurityalliance.org/blog/2025/04/22/ai-and-privacy-2024-to-2025-embracing-the-future-of-global-legal-developments]
- 78. Artificial intelligence-driven approaches in antibiotic ... [https://www.sciencedirect.com/science/article/abs/pii/S0933365725000247]
- 79. A New Era in Antimicrobial Stewardship - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6784134/]
- 80. Can AI Solve the Skills Shortage in Antimicrobial ... [https://www.contagionlive.com/view/can-ai-solve-the-skills-shortage-in-antimicrobial-stewardship-]
- 81. A Machine Learning Approach to Predicting Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12099390/]
- 82. Writer 推出医疗健康和金融领域专用大语言模型 [https://developer.nvidia.com/zh-cn/blog/writer-releases-domain-specific-llms-for-healthcare-and-finance/]
- 83. 大模型进军医疗行业:实验揭示LLMs在临床建议中的表现 [https://blog.csdn.net/lijianpeng0302/article/details/142778551]
- 84. 大模型能否胜任临床诊断任务? 交互式医学诊断仿真和评测 [https://hub.baai.ac.cn/view/38639]
- 85. 2024.2 AI Hospital: Benchmarking Large Language ... [https://blog.csdn.net/Kakaxiii/article/details/143777600]
- 86. 应对过度处方挑战:为药物推荐任务微调大语言模型 ... [https://blog.csdn.net/m0_52545077/article/details/147634412]
- 87. Chapter 10 Methods for Comparative Studies - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK481584/]
- 88. Multiple method comparison: statistical model using ... [https://pubmed.ncbi.nlm.nih.gov/12827667/]
- 89. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 90. Large language model as clinical decision support system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629785/]
- 91. ChatGPT vs Claude vs Gemini: The Best AI Model for Each ... [https://creatoreconomy.so/p/chatgpt-vs-claude-vs-gemini-the-best-ai-model-for-each-use-case-2025]
- 92. Advancements in AI-driven drug sensitivity testing research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081381/]
- 93. Comparative Evaluation and Performance of Large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563182/]
- 94. Performance analysis of large language models Chatgpt ... [https://pubmed.ncbi.nlm.nih.gov/40540092/]
- 95. Performance of a Large Language Model in the Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10992653/]
- 96. Nudging Guideline -Concordant Antibiotic ... Prescribing [https://pmc.ncbi.nlm.nih.gov/articles/PMC4648560/]
- 97. Can large language models assist off‐label prescribing? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12569560/]
- 98. The development and implementation of a guideline -based clinical ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-022-01860-3]
- 99. Evaluating the performance of large language models ... [https://www.nature.com/articles/s41598-025-21689-w]
- 100. DOSAGE: Dataset for Optimized Safe Antibiotic Guidelines ... [https://www.nature.com/articles/s41597-025-05761-8]
- 101. Performance of a Large Language Model in the Generation ... [http://e-neurospine.org/journal/view.php?doi=10.14245/ns.2347310.655]
- 102. [2505.08245] Large Language Model Psychometrics [https://arxiv.org/abs/2505.08245]