Validating Pharmacometric Models for Dose Prediction: A Framework for Accuracy, Credibility, and Clinical Application
This article provides a comprehensive guide for researchers and drug development professionals on the validation of pharmacometric models for accurate dose prediction.
Validating Pharmacometric Models for Dose Prediction: A Framework for Accuracy, Credibility, and Clinical Application
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the validation of pharmacometric models for accurate dose prediction. It explores the foundational principles of pharmacometrics and its critical role in model-informed drug development (MIDD). The content delves into advanced methodological approaches, including the integration of real-world data and pharmacogenomics, and addresses common troubleshooting and optimization challenges faced during model development. A significant focus is placed on contemporary validation frameworks and comparative analyses with traditional statistical methods, highlighting tools like the risk-informed credibility framework and novel visualization techniques. By synthesizing current trends, regulatory expectations, and real-world applications, this article serves as a strategic resource for enhancing the reliability and clinical impact of pharmacometric models in personalized medicine.
The Foundations of Pharmacometrics and Its Pivotal Role in Modern Dose Prediction
Pharmacometrics represents the scientific discipline concerned with the quantitative analysis of the interactions between drugs and biological systems. As a cornerstone of Model-Informed Drug Development (MIDD), pharmacometrics employs mathematical models to characterize, understand, and predict pharmacokinetic (PK), pharmacodynamic (PD), and disease progression behaviors [1] [2]. This quantitative framework integrates data from nonclinical and clinical studies to inform critical decisions throughout the drug development lifecycle, from early discovery to post-market optimization [3].
The fundamental importance of pharmacometrics lies in its ability to quantify uncertainty and variability in drug response, enabling more efficient drug development and regulatory decision-making [3] [4]. By bridging diverse data types through modeling and simulation, pharmacometrics provides a structured approach to address key questions of interest (QOI) within specific contexts of use (COU), ultimately supporting dose selection, trial design, and optimization of therapeutic individualization [1]. The recent International Council for Harmonisation (ICH) M15 guidelines on MIDD further underscore the regulatory recognition of pharmacometrics as an essential tool for modern drug development, establishing harmonized expectations for model development, documentation, and application across global regulatory agencies [3] [4].
Core Components of the Pharmacometric Toolkit
Pharmacokinetic (PK) Modeling: The Journey of Drugs Through the Body
Pharmacokinetic modeling quantitatively describes the time course of drug absorption, distribution, metabolism, and excretion (ADME) within the body [3]. PK models range from simple compartmental structures to sophisticated physiologically-based frameworks, each serving distinct purposes throughout drug development.
Population PK (PopPK) modeling represents a preeminent methodology that characterizes drug concentration time profiles while accounting for inter-individual variability [1] [3]. Using nonlinear mixed-effects modeling, PopPK identifies demographic, physiological, and pathological factors that contribute to variability in drug exposure, enabling tailored dosing strategies for specific patient subpopulations [3]. For instance, a PopPK model for sitafloxacin incorporated covariates including creatinine clearance, body weight, age, and food effects to optimize dosing regimens against various bacterial pathogens [5].
Physiologically-Based PK (PBPK) modeling adopts a mechanistic approach that incorporates physiological, biochemical, and drug-specific parameters to simulate drug disposition [1]. These models are particularly valuable for predicting drug-drug interactions, extrapolating across populations, and supporting biopharmaceutics applications. Recent data indicates that approximately 70% of PBPK applications in regulatory submissions focus on predicting enzyme- and transporter-mediated drug interactions [3].
Pharmacodynamic (PD) Modeling: Quantifying Drug Effects
Pharmacodynamic modeling characterizes the relationship between drug concentration at the site of action and the resulting pharmacological effects, both desired and adverse [3]. PD models quantify the intensity and time course of drug responses, incorporating specific mechanisms of action when knowledge is available.
Exposure-Response (E-R) analysis represents a fundamental PD approach that establishes relationships between drug exposure metrics (e.g., AUC, Cmax) and efficacy or safety endpoints [1] [3]. These relationships are crucial for determining therapeutic windows and informing dosing recommendations. For example, E-R analysis for nedosiran established the relationship between plasma concentrations and reduction in urine oxalate-to-creatinine ratio, supporting dose justification for pediatric patients with primary hyperoxaluria type 1 [6].
Semi-mechanistic PK/PD modeling hybridizes empirical and mechanism-based elements to characterize the complex interplay between drug pharmacokinetics and pharmacodynamic responses [1]. These models often incorporate biomarkers and intermediate endpoints to bridge between drug exposure and clinical outcomes, particularly valuable when clinical endpoints are delayed or difficult to measure frequently.
Disease Progression Modeling: Quantifying the Natural History
Disease progression modeling mathematically describes the time course or trajectory of a disease under natural conditions or standard of care [7]. These models distinguish drug effects from underlying disease evolution, providing critical context for interpreting treatment outcomes.
Disease progression models integrate multi-disciplinary knowledge and data from different sources, including translational, clinical trial, and real-world data [7]. They offer particular value for chronic conditions with slow progression, such as neurodegenerative diseases, where long-term clinical trials would be impractical and costly. By accounting for heterogeneity across patients and disease stages, these models support precision medicine approaches through population stratification and tailored treatment plans [7].
The synergy between these modeling components creates a comprehensive framework for understanding the complete drug-disease-patient system, enabling more informed decision-making throughout drug development.
Comparative Analysis: PK, PD, and Disease Progression Modeling
Table 1: Comparison of Core Pharmacometric Modeling Approaches
| Model Type | Primary Focus | Key Applications | Common Methodologies | Regulatory Impact Examples |
|---|---|---|---|---|
| Pharmacokinetic (PK) | Drug concentration time course | Dose selection, Bioequivalence, Drug interactions | Compartmental modeling, PBPK, PopPK | First-in-human dose prediction, DDI assessment [1] [3] |
| Pharmacodynamic (PD) | Drug effect intensity and time course | Target engagement, Efficacy/safety relationships | Emax models, Indirect response, Transit models | Exposure-response justification, Therapeutic window determination [1] [3] |
| Disease Progression | Natural history of disease | Trial optimization, Endpoint selection, Digital twins | Linear/Non-linear progression, Markov models | Patient enrichment strategies, External control arms [7] |
Integrated Modeling: The Synergy of PK, PD, and Disease Progression
The true power of pharmacometrics emerges when PK, PD, and disease progression models are integrated to form comprehensive drug-disease models. These integrated frameworks simultaneously characterize the complex interplay between drug exposure, pharmacological effects, and disease trajectory, providing a more holistic understanding of the overall system [2].
A compelling example of this integration is demonstrated in the development of teclistamab, a T-cell redirecting bispecific antibody for multiple myeloma [2]. The model-informed strategy incorporated translational PK/PD modeling from discovery through clinical development, integrating target receptor occupancy predictions with cytokine release syndrome assessment using PBPK approaches. This integrated modeling supported optimized dosing regimens and informed risk mitigation strategies, ultimately contributing to the successful regulatory approval of teclistamab [2].
Another exemplar of integrated modeling comes from the development of nedosiran for primary hyperoxaluria type 1 [6]. A population PK/PD model characterized the relationship between nedosiran exposure and reduction in spot urine oxalate-to-creatinine ratio across pediatric and adult populations. This model incorporated covariates such as body weight, estimated glomerular filtration rate, and PH type, enabling extrapolation of efficacy from adults to children as young as 2 years old and supporting the approved dosing regimen [6].
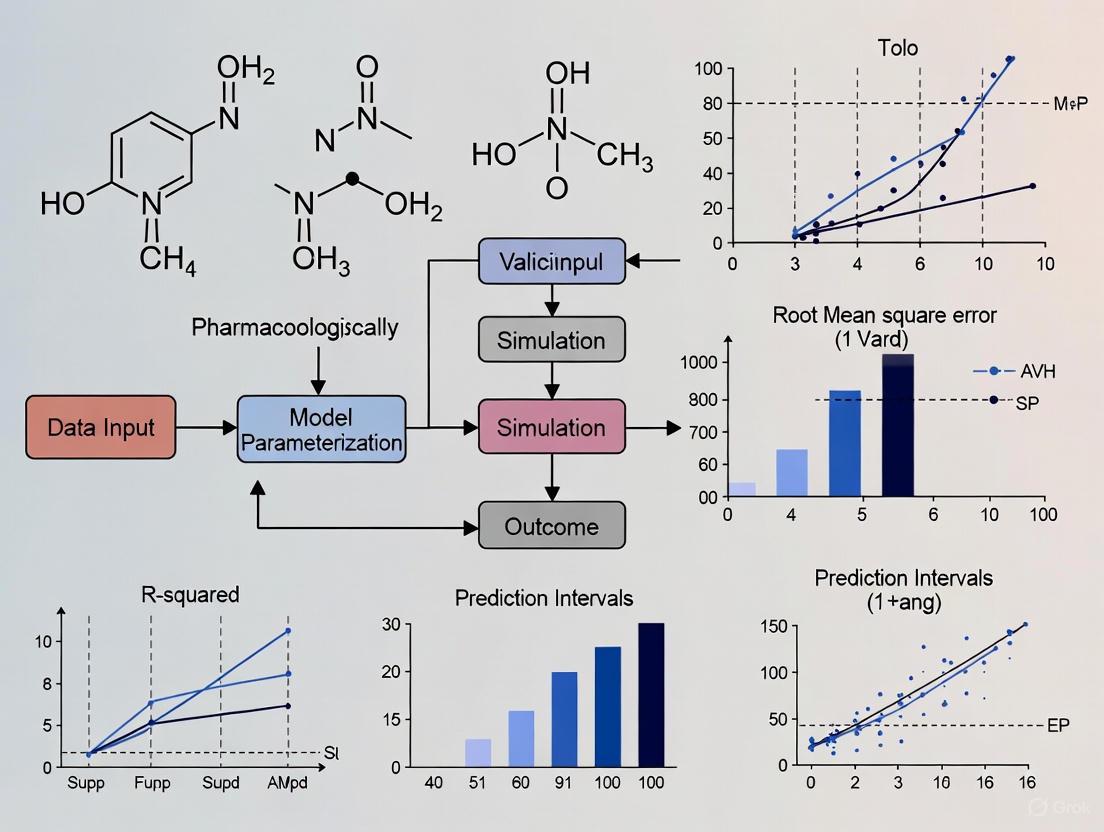
Diagram 1: Integrated Pharmacometric Modeling Framework. This diagram illustrates the synergistic relationships between PK, PD, and disease progression models in predicting clinical outcomes.
Validation Frameworks and Regulatory Considerations
Model Credibility and Validation Standards
The regulatory acceptance of pharmacometric models depends heavily on establishing model credibility through rigorous verification and validation processes [3] [4]. The ICH M15 guidelines adopt a risk-based approach to model assessment, considering the decision consequences and model influence on regulatory outcomes [3]. The validation framework encompasses several critical components:
Verification ensures that the computational model correctly implements the intended mathematical representations and algorithms [3] [4]. This process confirms that the model is solved accurately without coding or implementation errors.
Validation assesses how well the model represents reality for its intended context of use [3] [4]. This includes evaluating the model's predictive performance against external data sets not used in model development.
Applicability establishes that the model is appropriate for addressing the specific question of interest within the defined context of use [3]. This involves evaluating whether model assumptions, structure, and data sources are suitable for the intended application.
A recent validation study demonstrated this framework by evaluating mathematical model-based pharmacogenomic dose predictions against real-world data [8]. The study collected dosing and genotype information from 1,914 subjects across 26 studies, focusing on CYP2D6 and CYP2C19 polymorphisms. Results confirmed that the mathematical model could accurately predict optimal dosing, potentially circumventing traditional trial-and-error approaches to dose individualization [8].
Regulatory Evolution and Current Landscape
The regulatory landscape for pharmacometrics has evolved significantly over the past decades, with growing acceptance of model-informed approaches across global health authorities [3] [2]. This evolution began with the FDA's Population PK guidance in 1999 and Exposure-Response guidance in 2003, culminating in the recent ICH M15 draft guideline on "General Principles for Model-Informed Drug Development" [3].
The ICH M15 guideline aims to harmonize expectations between regulators and sponsors, supporting consistent regulatory decisions and minimizing errors in the acceptance of modeling and simulation evidence [3] [4]. This harmonization is particularly valuable for global drug development programs, promoting efficient application of MIDD across different regions and regulatory agencies.
Table 2: Experimental Protocols for Pharmacometric Model Validation
| Validation Component | Experimental/Methodological Approach | Acceptance Criteria | Application Example |
|---|---|---|---|
| Model Verification | Software qualification, Code review, Unit testing | Successful replication of benchmark results | Verification of PBPK model implementation [3] |
| Internal Validation | Bootstrap, Visual predictive checks, Data splitting | Parameter stability, Adequate uncertainty estimation | Bootstrap of sitafloxacin PopPK model (n=1000) [5] |
| External Validation | Prediction on independent datasets, Posterior predictive checks | Adequate predictive performance | CYP2D6 dose prediction vs. real-world data (n=1914) [8] |
| Sensitivity Analysis | Local/global sensitivity methods, Monte Carlo filtering | Robustness to parameter uncertainty | Covariate effect sensitivity in nedosiran model [6] |
Emerging Technologies and Future Directions
Artificial Intelligence and Machine Learning in Pharmacometrics
The integration of artificial intelligence (AI) and machine learning (ML) approaches represents a transformative frontier in pharmacometrics [1] [9]. Recent data indicates a substantial increase in regulatory submissions incorporating AI/ML elements, growing from fewer than 3 annually before 2019 to more than 100 each year after 2020 [2].
Machine learning techniques are being applied to enhance various aspects of pharmacometric analysis, including drug discovery optimization, ADME property prediction, and dosing strategy individualization [1]. A notable application involves automated population PK model development, where machine learning algorithms can efficiently search through thousands of potential model structures to identify optimal configurations [9]. Recent research demonstrates that such automated approaches can reliably identify model structures comparable to manually developed expert models while evaluating fewer than 2.6% of the models in the search space and reducing development time from weeks to less than 48 hours on average [9].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions in Pharmacometrics
| Tool Category | Specific Solutions | Function/Application | Representative Use Cases |
|---|---|---|---|
| Modeling Software | NONMEM, Monolix, Phoenix NLME | Nonlinear mixed-effects modeling | PopPK/PD model development [5] [9] |
| Simulation Platforms | R, Python, MATLAB | Clinical trial simulation, Data analysis | Monte Carlo simulations for PTA [5] |
| PBPK Platforms | GastroPlus, Simcyp Simulator | Mechanistic absorption and disposition prediction | DDI risk assessment [3] |
| AI/ML Tools | pyDarwin, TensorFlow, Scikit-learn | Automated model development, Pattern recognition | Automated PopPK model selection [9] |
| Data Resources | Clinical trial data, Real-world evidence, Literature | Model development and validation | Model-based meta-analysis [1] [7] |
Diagram 2: Automated Model Development Workflow. This diagram illustrates the machine learning-assisted workflow for automated population PK model development, demonstrating the iterative refinement process.
Pharmacometrics has evolved from a specialized analytical discipline to an essential framework informing decision-making across the entire drug development lifecycle. By bridging PK, PD, and disease progression modeling within integrated quantitative frameworks, pharmacometrics provides powerful tools for optimizing drug development efficiency and success rates [1] [2].
The continued adoption of model-informed drug development approaches, supported by regulatory harmonization through initiatives like ICH M15, promises to further strengthen the role of pharmacometrics in addressing complex development challenges [3] [4]. Emerging technologies, particularly artificial intelligence and machine learning, offer exciting opportunities to enhance model development efficiency and expand applications toward more personalized therapeutic interventions [1] [9].
As the field advances, the integration of diverse data sources—from advanced biomolecular assays to real-world evidence—will enable increasingly sophisticated models that better reflect the complexity of drug-disease-patient interactions. This progression toward more predictive, validated pharmacometric models will ultimately accelerate the delivery of safe and effective therapies to patients in need.
Historical Foundation and Conceptual Framework
The 'Learn and Confirm' paradigm, introduced by Lewis Sheiner in the 1990s, represents a foundational shift in pharmaceutical development [10]. It proposes a structured framework where drug development alternates between learning phases (where models are developed and refined using emerging data) and confirming phases (where model-based predictions are tested and validated in subsequent studies) [11] [10]. This iterative process stands in contrast to traditional, purely empirical development approaches.
This paradigm is the direct intellectual predecessor of modern Model-Informed Drug Development (MIDD), which the International Council for Harmonisation (ICH) defines as "the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [3]. MIDD operationalizes 'Learn and Confirm' through quantitative pharmacology, using models to infer, predict, and inform decisions rather than to solely base decisions on them [11]. The core concept is that research and development decisions are "informed" rather than exclusively "based" on model-derived outputs, making it a central tenet of efficient drug development [11].
Table: Core Components of the Learn and Confirm Paradigm in Modern MIDD
| Component | Objective in 'Learn' Phase | Objective in 'Confirm' Phase |
|---|---|---|
| Data Utilization | Integrate existing knowledge & new data to build/refine models | Collect new, targeted data to test model predictions |
| Model Role | Characterize emerging data & underlying systems | Serve as a pre-specified framework for trial simulation & analysis |
| Primary Output | Quantitative framework for prediction & extrapolation | Substantial evidence of effectiveness & safety |
| Decision Impact | Generate hypotheses & inform design of subsequent studies | Verify model predictions & support regulatory labeling |
Contemporary Evidence of Paradigm Validation
The validation of the 'Learn and Confirm' paradigm is demonstrated through its successful application and measurable impact across the modern drug development portfolio. The following table summarizes key quantitative evidence from recent implementations.
Table: Quantitative Evidence of MIDD Impact from Recent Applications
| Application Area | Reported Impact | Source / Context |
|---|---|---|
| Overall Portfolio Efficiency | Average savings of ~10 months in cycle time and $5 million per program | Systematic application across a large pharmaceutical company's portfolio [12] |
| Pharmacogenomic Dose Prediction | Mathematical model accurately predicted optimal dosing for 1914 subjects across 26 studies | Validation using real-world data on CYP2D6 and CYP2C19 polymorphisms [8] [13] |
| Clinical Trial Budget | Reduction of $100 million in annual clinical trial budget | Historical implementation at Pfizer through model-informed study designs [11] [12] |
| Decision-Making Impact | Significant cost savings ($0.5 billion) through impact on decision-making | Reported impact at Merck & Co./MSD [11] |
Case Study: Validating Pharmacogenomic Dose Prediction
A 2025 study provides a robust, real-world validation of the paradigm by testing a mathematical model's ability to predict individualized drug doses based on patient genetics [8] [13].
- Experimental Protocol: The work relied on collecting, extracting, and using real-world data on dosing and patient genotypes, focusing on drug-metabolizing enzymes cytochrome CYP450, specifically CYP2D6 and CYP2C19 gene polymorphisms [8]. A total of 1914 subjects from 26 studies were considered for the verification [8].
- Key Methodology: The study emphasized using allele activity scores and simple descriptive metabolic activity terms for patients, rather than traditional phenotype/genotype classifications, to improve prediction accuracy [8].
- Outcome and Validation: The mathematical model successfully predicted the reported optimal dosing values from the considered studies [8] [13]. This demonstrates the 'Confirm' phase in action, where a model-based approach ('Learn') was validated against independent, real-world data, proving its utility in circumventing trial-and-error in patient treatment [8].
Case Study: Portfolio-Wide Efficiency Gains
A 2025 analysis systematically estimated the cumulative impact of MIDD across a clinical development portfolio, showcasing the paradigm's large-scale business value [12].
- Experimental Protocol: The methodology involved reviewing MIDD plans for all active clinical development programs (11 early-development and 31 late-development programs). An algorithm was used to estimate savings from MIDD-related activities such as clinical trial waivers, "No-Go" decisions, or sample size reductions [12].
- Key Methodology: Cost savings were calculated using Per Subject Approximation (PSA) values. Time savings were estimated using typical timelines from protocol development to the final clinical study report for waived studies [12].
- Outcome and Validation: The analysis confirmed that systematic MIDD application yielded significant annualized savings—approximately 10 months of cycle time and $5 million per program—demonstrating that the iterative 'Learn and Confirm' process directly translates into enhanced development efficiency and cost-effectiveness [12].
Regulatory Endorsement and Standardization
The principles of 'Learn and Confirm' and MIDD have evolved from a theoretical concept to a formally recognized regulatory framework. This is most evident in the development of the ICH M15 guideline on "General Principles for Model-Informed Drug Development" [3]. This guideline, released as a draft in 2024, aims to harmonize expectations between regulators and sponsors, support consistent regulatory decisions, and minimize errors in the acceptance of modeling and simulation to inform drug labels [3]. It operationalizes the paradigm by providing a taxonomy of terms and outlining stages for MIDD activities: Planning and Regulatory Interaction, Implementation, Evaluation, and Submission [3].
Furthermore, regulatory bodies have incorporated credibility assessment frameworks for computational models, directly supporting the 'Confirm' aspect of the paradigm. These frameworks, such as those adapted from the American Society of Mechanical Engineers (ASME) standards, provide a structured approach to evaluate model relevance and adequacy, ensuring the models are 'fit-for-purpose' [3] [14]. This ensures that the models used in the 'Learn' phase are robust and reliable enough to inform decisions that will be 'Confirmed' in later stages.
Essential Research Toolkit for MIDD
The successful implementation of the 'Learn and Confirm' paradigm relies on a suite of quantitative tools. The following table details key "Research Reagent Solutions" – the essential methodologies and materials in the pharmacometrician's toolkit.
Table: Essential Research Toolkit for Model-Informed Drug Development
| Tool / Methodology | Primary Function | Key Application in 'Learn and Confirm' |
|---|---|---|
| Population PK (PopPK) | Analyzes variability in drug concentrations between individuals in a patient population [15]. | 'Learn': Identifies impact of covariates (e.g., weight, genetics). 'Confirm': Validates covariate relationships in new populations [3]. |
| Physiologically-Based PK (PBPK) | Mechanistically simulates drug movement through body organs and tissues [15]. | 'Learn': Predicts human PK and drug-drug interactions. 'Confirm': Waives dedicated clinical DDI studies [15] [14]. |
| Quantitative Systems Pharmacology (QSP) | Models drug effects in the context of biological systems and disease pathways [15]. | 'Learn': Identifies drug targets and combination therapies. 'Confirm': Optimizes dose selection and patient stratification [16] [14]. |
| Model-Based Meta-Analysis (MBMA) | Integrates highly curated summary-level data from multiple clinical trials [15]. | 'Learn': Informs competitive landscape and trial design. 'Confirm': Provides external control arms [15]. |
| AI/Machine Learning (ML) | Identifies complex patterns in large, high-dimensional datasets [16] [14]. | 'Learn': Predicts target engagement and patient endpoints. 'Confirm': Enhances model diagnostics and validation [16]. |
| Real-World Data (RWD) | Provides evidence from routine healthcare delivery (e.g., EHRs, registries) [8]. | 'Learn': Informs disease progression models. 'Confirm': Validates model-based dose predictions [8]. |
Experimental Workflow for Model Validation
The credibility of any model used in the 'Learn and Confirm' cycle is paramount. The following workflow, aligned with regulatory expectations, outlines the key steps for developing and validating a pharmacometric model for dose prediction.
- Step 1: Define Question of Interest (QOI) & Context of Use (COU): The process begins by precisely defining the specific drug development question to be answered (the QOI) and the specific context in which the model output will be used to inform a decision (the COU) [3]. This is a critical first step for 'fit-for-purpose' model development.
- Step 2: Create Model Analysis Plan (MAP): A pre-specified MAP documents the objectives, data sources, and analytical methods, minimizing bias and aligning the team and regulators on the approach [3].
- Step 3: Data Curation & Variable Selection: This involves gathering and processing high-quality, relevant data from nonclinical and clinical studies, which forms the foundation for model building [16] [3].
- Step 4: Model Development & Estimation: Using appropriate software, a mathematical model is developed, and its parameters are estimated. This may involve complex techniques like nonlinear mixed-effects modeling [3].
- Step 5: Model Evaluation: The model undergoes rigorous diagnostic checks (e.g., goodness-of-fit plots), and uncertainty in its parameters and predictions is quantified [16] [3].
- Step 6: Model Validation: The model's predictive performance is assessed. This can include internal validation (e.g., Visual Predictive Check - VPC) and external validation using a separate dataset or real-world data (RWD), as demonstrated in the pharmacogenomics case study [8] [3].
- Step 7: Submission & Regulatory Review: The final model, analysis, and documentation are submitted to regulatory agencies as part of the evidence package to support the proposed dosing regimen or other labeling claims [12] [3].
The transition of pharmacometric models from research tools to clinical decision-support systems hinges on a single, non-negotiable requirement: rigorous validation. Model validation provides the essential evidence that mathematical predictions of drug dosing can be trusted in real-world clinical settings, directly impacting patient safety and therapeutic efficacy. Within precision medicine, pharmacogenomics-based dose prediction models aim to optimize drug therapy by integrating individual genetic variability, particularly in drug-metabolizing enzymes such as cytochrome P450 (CYP) isoforms. Without thorough validation, these models remain theoretical constructs with unproven clinical utility. This guide objectively compares validation approaches and performance of different model-based dosing strategies, providing researchers and drug development professionals with the experimental data and protocols needed to critically assess model credibility for clinical implementation.
Comparative Performance of Dose Prediction Models
Quantitative Validation Metrics Across Model Types
Table 1: Performance Comparison of Pharmacogenomic Dose Prediction Models
| Model Type | Validation Cohort Size | Key Genetic Factors | Primary Validation Metric | Reported Performance | Clinical Application |
|---|---|---|---|---|---|
| Mathematical Model (PGx) [8] | 1,914 subjects (26 studies) | CYP2D6, CYP2C19 allele activity scores | Prediction accuracy of optimal dosing versus real-world data | Able to predict reported optimal dosing; circumvents trial-and-error [8] | Individualized dosing for drugs metabolized by CYP450 enzymes |
| Multi-output Gaussian Process (MOGP) [17] | 442 cancer cell lines (10 cancer types) | Genomic features (mutations, CNA, methylation) + drug chemistry | Prediction accuracy of full dose-response curves | Accurate prediction across cancer types; identifies novel biomarkers (e.g., EZH2) [17] | Drug repositioning and biomarker discovery in oncology |
| Software Tool for Codeine Dosing [8] | N/A (Algorithm-based) | CYP2D6 gene-pair polymorphisms + drug-drug interactions | Dose adjustment accuracy | Provides framework for implementing individualized dosing [8] | Codeine dose adjustment based on CYP2D6 phenotype |
| Precision Dosing for Tricyclics [8] | N/A (Algorithm-based) | CYP2D6, CYP2C19 variants + polypharmacy | Dosing accuracy integrating polypharmacy | More accurate individualized dosing integrating polypharmacy effect [8] | Tricyclic antidepressant dosing |
Key Validation Outcomes and Clinical Implications
The validation of mathematical model-based pharmacogenomics dosing against real-world data represents a significant advancement. A 2025 study demonstrated that a mathematical model successfully predicted the reported optimal dosing values from 26 real-world studies encompassing 1,914 subjects [8]. This approach specifically utilized CYP2D6 and CYP2C19 gene polymorphisms and allele activity scores for verification, moving beyond simple phenotype/genotype classifications toward more quantitative metabolic activity terms [8]. This validation confirms that model-based predictions can circumvent the traditional trial-and-error approach in patient treatment, potentially reducing adverse drug reactions and improving therapeutic outcomes.
Comparative analysis shows that models validating against large, diverse datasets (1,914 subjects for the PGx model; 442 cell lines for MOGP) provide more credible evidence for clinical adoption [8] [17]. The MOGP approach offers the distinct advantage of predicting complete dose-response curves rather than single summary metrics (e.g., IC50), enabling more comprehensive efficacy assessment [17]. Furthermore, the MOGP model demonstrated robustness in cross-study testing, maintaining prediction accuracy when trained on limited data—a crucial consideration for rare diseases or understudied populations [17].
Experimental Protocols for Model Validation
Validation Framework for Pharmacogenomic Dosing Models
Experimental Objective: To verify the accuracy of mathematical model-based pharmacogenomic dose predictions against real-world clinical data.
Methodology:
- Data Collection and Curation: The work relied on collecting, extracting, and using real-world data on dosing and patients' genotypes from 26 published studies [8]. A total of 1,914 subjects were included in the validation cohort [8].
- Genetic Focus: The validation specifically focused on drug metabolizing enzymes, with cytochrome CYP450 isoforms CYP2D6 and CYP2C19 gene polymorphisms used for verification [8].
- Model Input Strategy: The validation approach emphasized using simple descriptive metabolic activity terms and allele activity scores for drug dosing rather than traditional phenotype/genotype classifications [8].
- Performance Assessment: The mathematical model's predicted optimal dosing was compared against the reported optimal dosing values from the considered real-world studies [8].
MOGP Model Validation Protocol
Experimental Objective: To assess multi-output Gaussian Process models for predicting dose-response curves across multiple cancer types and with limited training data.
Methodology:
- Data Sources: Dose-response and genomics data were retrieved from the Genomics of Drug Sensitivity in Cancer (GDSC) database, including responses to ten drugs across 442 human cancer cell lines representing ten distinct cancer types [17].
- Feature Integration: Three types of molecular features were extracted: genetic variations in cancer genes, copy number alteration status of recurrent altered chromosomal segments, and DNA methylation status of informative CpG islands [17]. Drug chemical features were obtained from PubChem [17].
- Model Architecture: A multi-output Gaussian Process (MOGP) model was implemented to simultaneously predict all dose-responses and uncover biomarkers [17].
- Biomarker Identification: A novel Kullback-Leibler (KL) divergence method was applied to measure the importance of each genomic feature from the MOGP predictions [17].
- Validation Approach: Model performance was assessed through cross-cancer-type prediction and training with progressively smaller sample sizes to evaluate robustness with limited data [17].
Visualizing Model Validation Workflows
Pharmacogenomic Model Validation Pathway
Multi-Output Model Comparison Framework
Table 2: Key Research Reagents and Computational Tools for Dose Prediction Validation
| Resource Category | Specific Tool/Resource | Function in Validation | Key Features |
|---|---|---|---|
| Genomic Data Platforms | Genomics of Drug Sensitivity in Cancer (GDSC) | Provides dose-response and genomic data for validation across cancer types [17] | 442 cancer cell lines, 10 cancer types, multi-omics data [17] |
| Chemical Databases | PubChem | Source of chemical features for drugs used in prediction models [17] | Standardized chemical properties and structures |
| Computational Frameworks | Multi-output Gaussian Process (MOGP) | Predicts complete dose-response curves using genomic and chemical features [17] | Models all doses simultaneously; enables biomarker discovery via KL divergence [17] |
| Validation Standards | Real-World Clinical Data (26 studies) | Gold standard for validating model predictions against actual clinical outcomes [8] | 1,914 subjects; CYP2D6 and CYP2C19 polymorphisms [8] |
| Biomarker Discovery | Kullback-Leibler (KL) Divergence | Measures feature importance in MOGP models; identifies novel biomarkers [17] | Identified EZH2 as novel BRAF inhibitor biomarker [17] |
The validation evidence presented establishes that model-based pharmacogenomic dose prediction can successfully forecast optimal dosing when rigorously tested against real-world data. The mathematical model validation with 1,914 subjects and the MOGP cross-cancer validation provide compelling evidence that these approaches can transcend traditional trial-and-error prescribing. For researchers and drug development professionals, this comparative analysis demonstrates that validation must be non-negotiable—the crucial bridge between theoretical models and clinically actionable tools that can safely optimize drug therapy for individual patients.
Exposure-Response, Nonlinear Mixed-Effects Models (NLMEM), and Context of Use
In model-informed drug development (MIDD), the robust prediction of optimal drug doses rests upon three foundational pillars: Exposure-Response (E-R) analysis, which quantifies the relationship between drug exposure and its effects; Nonlinear Mixed-Effects Models (NLMEM), which provide the statistical framework for parsing variability in these relationships across populations; and Context of Use (COU), which defines the specific role and credibility requirements of a model for a given decision. The International Council for Harmonisation (ICH) M15 guideline defines COU as "a statement that clearly describes the way the model-informed drug development (MIDD) approach will be used and the decisions it will support" [3] [4]. The synergy of these elements is critical for validating pharmacometric models and ensuring their dose predictions are accurate, reliable, and fit for their intended regulatory and clinical purpose.
Defining the Key Terminology
Exposure-Response (E-R)
Exposure-Response analysis is the quantitative examination of the relationship between a defined drug exposure (e.g., dose, concentration, or AUC) and both its effectiveness and adverse effects [1]. It forms the bedrock of dose selection and justification, answering the critical question of how changes in drug exposure influence the probability and magnitude of desired and undesired outcomes.
Nonlinear Mixed-Effects Models (NLMEM)
Nonlinear Mixed-Effects Models are a class of statistical models used to analyze data where the response is nonlinearly related to the parameters and where data are collected from multiple related subjects (e.g., patients, cell lines) [18]. NLMEMs are the gold standard for pharmacometric analysis because they can handle unbalanced, sparse clinical data and account for multiple levels of variability [19]. They distinguish between:
- Fixed Effects: Population-level typical parameter values (e.g., typical clearance in a patient population).
- Random Effects: Quantify the inter-individual (IIV) and inter-occasion variability (IOV) around these typical values, explaining how parameters differ from one subject to another [20].
Context of Use (COU)
The Context of Use is a formalized statement, central to the ICH M15 guideline, that delineates the specific application, decision, and inference supported by the MIDD approach [3] [4]. It is the cornerstone of model credibility assessment, as the validation requirements for a model are entirely dependent on its COU. For instance, a model used to inform a final dosage recommendation on a drug label requires a far more rigorous validation than one used for internal, early-stage candidate selection.
Comparative Roles in Dose Prediction and Model Validation
The table below compares how these three components interact and contribute to the overarching goal of valid dose prediction.
Table 1: Comparative Roles of E-R, NLMEM, and COU in Pharmacometric Dose Prediction
| Component | Primary Role in Dose Prediction | Contribution to Model Validation | Typical Outputs for Decision-Making |
|---|---|---|---|
| Exposure-Response (E-R) | Quantifies the causal link between drug exposure and clinical outcomes; identifies the target exposure window for efficacy and safety. | Validation focuses on the robustness and clinical plausibility of the inferred relationship (e.g., shape of E-R curve). | Target AUC or Ctrough, optimal dose range, probability of response/toxicity across doses. |
| Nonlinear Mixed-Effects Models (NLMEM) | Provides the structural and statistical framework to characterize population and individual E-R relationships from sparse, real-world data. | Validation assesses model fit (goodness-of-fit plots), predictive performance (VPC), and precision of parameter estimates (confidence intervals). | Population typical parameters, inter-individual variability, covariate effects (e.g., effect of weight on clearance). |
| Context of Use (COU) | Defines the specific dose-related question the model will answer and the regulatory impact of the decision. | Determines the level of evidence and validation needed (e.g., verification, validation, applicability) to deem the model "fit-for-purpose." [1] | A predefined and agreed-upon statement that bounds the model's application and sets criteria for its credible use. |
Experimental Applications and Protocols
The integration of E-R, NLMEM, and a clear COU is demonstrated across diverse drug development scenarios. The following experimental case studies illustrate their application and the critical workflow involved.
Case Study 1: Optimizing Pediatric Dosing with Machine Learning
- Objective: To enhance the precision of mycophenolate mofetil (MMF) dosing in pediatric patients with immune-mediated renal diseases by integrating Population PK (PopPK) with machine learning-based E-R analysis [21].
- Protocol:
- Data Collection: Rich pharmacokinetic blood samples were collected from pediatric patients to measure mycophenolic acid (MPA) concentrations.
- PopPK Model Development: A nonlinear mixed-effects model was developed to characterize MPA population pharmacokinetics and identify sources of inter-individual variability (e.g., body weight, albumin levels).
- Exposure-Response Analysis: Individual PK parameters from the PopPK model were used to derive drug exposure metrics (e.g., AUC). Machine learning models (Random Forest, XGBoost) were then trained to predict clinical response based on exposure and patient covariates.
- Dose Prediction & Validation: The final ML model was used to simulate and recommend individualized dosing regimens. Predictive accuracy was validated using metrics like root mean squared error (RMSE) and mean absolute prediction error (MDAPE) [21].
- COU: To support model-informed precision dosing (MIPD) for MMF in a specific pediatric population, enabling dose individualization that improves efficacy and reduces toxicity.
Case Study 2: Identifying Problematic Cancer Cell Lines
- Objective: To identify cancer cell lines (CCLs) that are universally overly sensitive or resistant to drugs, which could skew experimental results in drug screening [18].
- Protocol:
- Data Source: Dose-response data from large-scale studies like the Cancer Cell Line Encyclopedia (CCLE) and the Genomics of Drug Sensitivity in Cancer (GDSC).
- Model Structure: A nonlinear mixed-effects model using a 4-parameter logistic function was fitted to all cell lines for a given drug simultaneously. The model was defined as:
y_ij = E_min + (E_max - E_min) / (1 + exp[H*(log(x_ij) - log(IC_50))]) + e_ij[18] wherey_ijis the response of cell lineiat dosej,x_ijis the drug concentration, andHis the Hill coefficient. The parametersE_min,E_max,IC_50, andHwere modeled with fixed and random effects. - Borrowing Information: The NLMEM framework allowed the response profile of each CCL to be "informed" by the data from all other CCLs, leading to more stable and reliable estimates of the IC50 and other parameters.
- Analysis: The estimated random effects for each cell line were analyzed across multiple drugs. Cell lines with consistently extreme random effects were flagged as universally sensitive or resistant [18].
- COU: To identify and flag specific cancer cell lines that may generate non-generalizable results in in vitro drug discovery screens, thereby improving the quality of preclinical research.
Case Study 3: Integrated Survival and Safety Modeling in Oncology
- Objective: To jointly model longitudinal biomarkers (e.g., tumor size) and time-to-event endpoints (e.g., survival) to optimize dose selection for anticancer drugs [22].
- Protocol:
- Tumor Growth Inhibition (TGI) Model: A nonlinear mixed-effects model characterizes the longitudinal trajectory of tumor size in response to drug exposure and patient-specific covariates.
- Joint Model: The individual parameters from the TGI model (e.g., estimated tumor size reduction at a specific time) are linked to a survival model (e.g., parametric or Cox model) to predict an individual's hazard of disease progression or death.
- Exposure-Response-Safety: This joint modeling framework is simultaneously applied to safety biomarkers or graded adverse events to define the therapeutic window [22].
- Clinical Trial Simulation: The validated joint model is used to simulate virtual clinical trials under different dosing regimens to identify the dose that maximizes the probability of a favorable efficacy-safety balance.
- COU: To integrate all available evidence to support a definitive dose recommendation for Phase 3 trials and drug labeling, particularly for novel oncology therapeutics.
The logical workflow integrating these components in a pharmacometric analysis is summarized in the diagram below.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents and Computational Tools in Pharmacometrics
| Tool/Reagent | Function | Application Example |
|---|---|---|
| nlmixr (R package) | An open-source tool for fitting nonlinear PK/PD mixed-effects models [19]. | Used as a credible, free alternative to commercial software (e.g., NONMEM) for model development and simulation. |
| SimBiology (MATLAB) | A commercial modeling and simulation environment for PK/PD and systems pharmacology. | Provides a workflow for NLME model building, parameter estimation, and diagnostic plotting for popPK data [23]. |
| Restricted Boltzmann Machine (RBM) | A generative stochastic neural network for modeling complex joint distributions in data [24]. | Applied to model multi-item Patient Reported Outcome Measures (PROMs) and their relationship to drug concentrations. |
| Model Analysis Plan (MAP) | A pre-specified document outlining the objectives, data, and methods for a MIDD analysis [3]. | Critical for regulatory alignment; details the COU, Question of Interest, and technical criteria for model evaluation. |
| Virtual Population | A computationally generated cohort with realistic physiological and genetic diversity [1]. | Used in clinical trial simulations to predict drug exposure and response in subpopulations (e.g., pediatric, renally impaired) before real-world study. |
| Visual Predictive Check (VPC) | A diagnostic plot comparing simulated data from the model to the observed data [19]. | A key method for evaluating the predictive performance of an NLMEM and validating its structure. |
The interplay between Exposure-Response analysis, Nonlinear Mixed-Effects Models, and a well-defined Context of Use creates a rigorous, evidence-based framework for dose prediction in drug development. E-R relationships provide the clinical rationale for dosing, NLMEMs offer the powerful statistical methodology to derive these relationships from complex data, and the COU ensures the entire process is aligned with a specific, credible, and fit-for-purpose goal. Adherence to this triad, as championed by emerging international guidelines like ICH M15, is paramount for enhancing the accuracy and regulatory acceptance of pharmacometric models, ultimately accelerating the delivery of optimally dosed therapies to patients.
Methodologies for Building and Applying Robust Predictive Dose Models
Leveraging Real-World Data and Pharmacogenomics for Personalized Dosing
The integration of real-world data (RWD) and pharmacogenomics (PGx) is transforming the paradigm of personalized dosing from a theoretical concept to a clinically validated practice. This approach moves beyond traditional trial-and-error prescribing by leveraging diverse data sources—including electronic health records (EHRs), genomic databases, and insurance claims—to inform precise medication selection and dosing strategies tailored to individual patient characteristics [25]. The validation of pharmacometric models using real-world evidence (RWE) represents a critical advancement in ensuring these approaches are both accurate and clinically applicable [8] [3].
The growing importance of this field is underscored by the recent International Council for Harmonisation (ICH) M15 guidelines on model-informed drug development (MIDD), which provide a framework for using computational modeling and simulation to inform drug development and regulatory decisions [3]. This review examines the current landscape of RWD and PGx in personalized dosing, focusing on experimental validations, clinical implementations, and the essential tools driving this innovative field forward.
Experimental Validations of PGx-Based Dose Prediction
Mathematical Model Validation with Real-World Clinical Data
Objective: A 2025 study sought to verify the accuracy of mathematical modeling in predicting optimal medication doses based on patient genotypes compared to real-world clinical data [8] [13].
Methodology: The research analyzed real-world dosing and genotype data from 1,914 subjects across 26 studies, focusing on polymorphisms in the CYP2D6 and CYP2C19 genes, which encode key drug-metabolizing enzymes [8]. The mathematical model utilized allele activity scores rather than simplistic phenotype classifications to generate more precise dose predictions [8] [13].
Key Findings: The mathematical model successfully predicted the reported optimal dosing values from the considered studies, demonstrating that computational approaches can effectively leverage genetic information to guide therapeutic decisions [8]. This validation underscores the potential of model-based dose prediction to circumvent the traditional trial-and-error approach in pharmacotherapy [8].
Polygenic Contributions to Medication Dosing
Objective: A 2025 longitudinal biobank study investigated both monogenic pharmacogenomic and polygenic contributions to variability in medication dosing [26].
Methodology: Researchers leveraged longitudinal drug purchase data from the Estonian Biobank (N = 212,000) linked with genomic data to derive individual-level daily doses for cardiovascular and psychiatric medications [26]. The study assessed associations with polygenic scores (PGSs) for 16 traits and conducted genome-wide association studies (GWAS) to identify relevant genetic variants [26].
Key Findings:
- Polygenic scores for specific traits were significantly associated with daily doses of common medications: coronary heart disease PGS with statins (β = 0.02, P = 5.9 × 10^(-10)) and systolic blood pressure PGS with metoprolol (β = 0.03, P = 7.5 × 10^(-13)) [26].
- Body mass index PGS was linked to dosing of multiple medications including statins, metoprolol, and warfarin [26].
- GWAS confirmed established PGx signals for metoprolol (CYP2D6) and warfarin (CYP2C9, VKORC1), validating the methodology [26].
- Both polygenic and pharmacogenomic signals contributed independently to dose variability, highlighting the complex genetic architecture underlying drug response [26].
Table 1: Key Experimental Validations of PGx in Personalized Dosing
| Study Focus | Data Source | Sample Size | Key Genes/Variants | Primary Findings |
|---|---|---|---|---|
| Mathematical Model Validation [8] | 26 published studies | 1,914 subjects | CYP2D6, CYP2C19 | Mathematical models accurately predicted reported optimal dosing using allele activity scores |
| Polygenic Contribution [26] | Estonian Biobank | 212,000 individuals | CYP2D6, CYP2C9, VKORC1 + PGS | Both monogenic PGx and polygenic scores independently contribute to dose variability |
| Preemptive PGx Testing [27] | PREPARE Study | 6,944 patients | 12-gene panel | 33% reduction in adverse drug reactions with preemptive PGx testing |
Clinical Implementation and Workflow Integration
Real-World Evidence from Large-Scale Clinical Programs
Several large-scale implementation studies have demonstrated the clinical utility of PGx-enriched personalized dosing:
The PREPARE Study (Preemptive Pharmacogenomic Testing for Preventing Adverse Drug Reactions): This landmark study enrolled 6,944 patients across seven European countries and randomized them to receive either genotype-guided drug treatment or standard care [27]. The intervention group underwent testing for variants in 12 pharmacogenes (CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A5, DPYD, F5, HLA-B, SLCO1B1, TPMT, UGT1A1, and VKORC1) guiding prescriptions for 56 commonly used medications [27]. Results demonstrated a significant 33% reduction in clinically relevant adverse drug reactions in the genetically-guided group (21.5% vs. 28.6% in control) [27].
PGx-Enriched Comprehensive Medication Management: A 2022 real-world study of a Medicare Advantage population showed that integrating PGx with comprehensive medication management (CMM) delivered through a clinical decision support system (CDSS) resulted in substantial healthcare improvements [28]. The program demonstrated:
- Reduction of approximately $7,000 per patient in direct medical costs
- Total savings of $37 million across 5,288 enrolled patients compared to 22,357 non-enrolled controls
- A positive shift in healthcare resource utilization away from acute care toward more sustainable primary care options [28]
The RIGHT 10K Study: This large-scale PGx implementation program at Mayo Clinic and Baylor College of Medicine utilized an 84-gene next-generation sequencing panel and found that 99% of participants carried actionable PGx variants in at least one of the five genes examined (SLCO1B1, CYP2C19, CYP2C9, VKORC1, and CYP2D6) [27]. This highlights the near-universal applicability of preemptive PGx testing in clinical populations.
Clinical Workflow Integration
The successful integration of PGx into clinical practice requires a structured workflow that encompasses testing, interpretation, and implementation of results. The following diagram illustrates a generalized clinical implementation workflow validated across multiple studies:
Diagram 1: Clinical implementation workflow for PGx testing, integrating multiple steps from patient identification to outcomes monitoring. CDSS: clinical decision support system; MAP: medication action plan. Adapted from [28] [27].
Medication Utilization and Prioritization
Understanding which medications and genes should be prioritized for PGx testing is essential for efficient clinical implementation. A 2025 scoping review examined real-world utilization rates of medications with clinically important PGx recommendations in older adults (≥65 years) [29].
Table 2: Frequently Prescribed Medications with Actionable PGx Recommendations in Older Adults
| Therapeutic Class | Most Frequently Prescribed Medications | Prescribing Range | Primary Genes Involved |
|---|---|---|---|
| Gastrointestinal | Pantoprazole | 0–49.6% | CYP2C19 |
| Cardiovascular | Simvastatin | 0–54.9% | SLCO1B1, CYP3A4 |
| Analgesic | Ondansetron | 0.1–62.6% | CYP2D6 |
| Psychotropic | Various antidepressants | Varies | CYP2D6, CYP2C19 |
| Cardiovascular | Warfarin | Varies | CYP2C9, VKORC1 |
The review analyzed 31 studies and identified 215 unique PGx medications, of which 82 had actionable PGx recommendations according to Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines [29]. The most frequently implicated genes were CYP2D6 (25.6%), CYP2C19 (18.3%), and CYP2C9 (11%) [29]. These findings support the implementation of preemptive panel-based testing over single-gene tests to cover the broad range of clinically relevant pharmacogenes [29].
Regulatory and Payer Perspectives
The adoption of PGx testing in clinical practice is significantly influenced by regulatory frameworks and insurance coverage policies. A 2025 assessment of US payer coverage decisions for PGx testing in psychiatry provides insights into the evidentiary standards considered in reimbursement decisions [30] [31].
Methodology: The study conducted a qualitative and quantitative assessment of publicly available coverage policies from 14 US payers, examining the number, type, and source of citations across policies and coverage decisions [30].
Key Findings:
- Peer-reviewed literature was the most frequently cited source across all policies [30] [31].
- Among 207 peer-reviewed papers cited across all policies, 40% (n = 83) were psychiatry-specific real-world evidence (RWE) studies [30].
- Six psychiatry-specific RWE studies and contributions from 13 distinct sources were frequently cited regardless of payer type or coverage decision [30].
- Coverage determinations appeared to be largely based on how individual payers interpret evidence on the clinical value of testing rather than strictly on the volume of evidence [30] [31].
This analysis highlights the growing importance of RWE in informing coverage decisions and the need for robust real-world studies demonstrating the clinical utility and economic value of PGx testing.
Successful implementation of PGx and RWD approaches requires leveraging specialized databases, analytical tools, and curated knowledge bases. The following table details key resources cited across the reviewed studies:
Table 3: Essential Research Resources for PGx and RWD Studies
| Resource Name | Type | Primary Function | Key Features |
|---|---|---|---|
| Clinical Pharmacogenetics Implementation Consortium (CPIC) [29] | Guidelines | PGx clinical guidelines | Evidence-based, peer-reviewed dosing guidelines for specific drug-gene pairs |
| Pharmacogenomics Knowledgebase (PharmGKB) [29] | Knowledge Base | PGx resource curation | Clinically annotates CPIC guidelines, collects PGx knowledge from literature |
| Estonian Biobank (EstBB) [26] | Data Resource | Longitudinal RWD with genetic data | 212,000 participants with drug purchase data and genomic information |
| Dutch Pharmacogenetics Working Group (DPWG) [27] | Guidelines | PGx guidelines | Alternative guideline source with European perspective |
| GeneDose LIVE [28] | Clinical Decision Support | CDSS for medication risk assessment | Integrates genetic and non-genetic risk factors, generates medication action plans |
The integration of real-world data and pharmacogenomics represents a transformative approach to personalized dosing that moves beyond traditional trial-and-error prescribing. Evidence from large-scale clinical implementations, validation studies, and real-world analyses consistently demonstrates that PGx-guided therapy can significantly improve patient outcomes, reduce adverse drug reactions, and generate substantial healthcare savings.
The successful validation of mathematical models against real-world clinical data [8], coupled with growing understanding of both monogenic and polygenic contributions to drug response variability [26], provides a robust foundation for increasingly sophisticated dosing approaches. Furthermore, the development of structured clinical workflows [28] [27] and clearer understanding of medication utilization patterns [29] offers practical pathways for implementation.
As regulatory frameworks continue to evolve [3] and payer coverage increasingly incorporates real-world evidence [30] [31], the field is poised for continued growth and refinement. The ongoing challenge remains in standardizing approaches, demonstrating consistent value across diverse populations, and further validating predictive models to ensure the safe, effective, and equitable implementation of personalized dosing strategies.
In vitro fertilization (IVF) and intracytoplasmic sperm injection-embryo transfer (ICSI-ET) represent the most widely used assisted reproductive technologies (ART), enabling millions of infertile couples to achieve pregnancy [32]. A pivotal component of successful IVF treatment is controlled ovarian stimulation (COS), which uses follicle-stimulating hormone (FSH) to promote the maturation of multiple follicles [32]. The precise determination of the optimal FSH starting dose remains a significant clinical challenge in reproductive medicine.
Historically, FSH dosing followed a "one size fits all" approach, but this has gradually evolved toward individualized treatment strategies [32]. According to ESHRE guidelines, dose individualization can minimize the risks of ovarian hyperstimulation syndrome (OHSS), iatrogenic poor ovarian response, and cycle cancellation [32]. Despite the critical importance of precise dosing, clinicians often rely on empirical judgment rather than data-driven models, highlighting the need for standardized, evidence-based dosing tools [32].
This case study examines the development and validation of a multivariate model for predicting optimal FSH starting doses in normal ovarian response (NOR) patients, representing 70-90% of ART cycles worldwide [32]. We analyze the model's performance against clinical standards and alternative approaches, with emphasis on validation within a pharmacometric research framework.
Model Development and Experimental Protocol
Study Population and Design
The prediction model was developed through a retrospective analysis of 535 patients undergoing their first IVF/ICSI-ET cycle at the Reproductive Medicine Department of the Fourth Hospital of Hebei Medical University between January 2017 and June 2024 [32]. Patients were randomly divided into a training group (n=317) and a validation group (n=218) in a 6:4 ratio [32].
Inclusion criteria comprised: (1) patients receiving first IVF/ICSI-ET treatment with GnRH agonist or antagonist protocol; (2) age between 20-38 years; (3) regular menstrual cycle (28 ± 7 days); and (4) retrieval of 5-15 oocytes [32]. Exclusion criteria eliminated patients with endocrine diseases, metabolic diseases, autoimmune diseases, or chromosomal abnormalities [32].
Clinical Protocols and Data Collection
All patients underwent controlled ovarian stimulation using either the long-acting GnRH agonist protocol (n=326) or the GnRH antagonist protocol (n=209) [32]. For the agonist protocol, pituitary down-regulation began on day 2-3 of menstruation, followed by COS with exogenous gonadotropin after 28 days. For the antagonist protocol, COS began on cycle day 2-3, with GnRH antagonist added when the leading follicle reached 12-14mm or E2 reached 400pg/ml [32]. Triggering occurred when ≥2 follicles reached ≥18mm diameter [32].
Comprehensive patient data were collected, including:
- Demographics: age, body height, weight, BMI, body surface area
- Reproductive history: infertility duration, type, factors, pelvic surgery history
- Basal hormone levels: FSH, LH, E2, progesterone, prolactin, AMH, testosterone
- Ovarian reserve markers: antral follicle count (AFC)
- Treatment parameters: initial and total Gn dose, stimulation duration [32]
Statistical Analysis and Model Construction
The analytical approach employed both univariate and multivariate linear regression to identify predictive factors influencing the Gn starting dose [32]. Statistically significant predictors (P<0.05) were incorporated into a nomogram for visual representation of the model [32]. Model accuracy was assessed using mean absolute error (MAE), root mean square error (RMSE), and R² values, with t-tests comparing actual versus predicted Gn starting doses in both training and validation sets [32].
Figure 1: Experimental workflow for FSH dose prediction model development
Results: Predictive Performance and Validation
Key Predictors of FSH Starting Dose
Multivariate analysis identified five statistically significant (P<0.05) predictors of the FSH starting dose [32]:
- Patient age
- Body mass index (BMI)
- Basal follicle-stimulating hormone (bFSH)
- Antral follicle count (AFC)
- Anti-Müllerian hormone (AMH)
These parameters were incorporated into the final predictive model, which was presented as a clinician-friendly nomogram for determining appropriate Gn starting doses for NOR patients undergoing IVF/ICSI-ET [32].
A separate validation study using the early follicular phase depot GnRH agonist protocol confirmed similar predictive parameters, deriving the following regression equation [33]: Initial FSH dose = 62.957 + 1.780AGE(years) + 4.927BMI(kg/m²) + 1.417bFSH(IU/ml) - 1.996AFC - 48.174*AMH(ng/ml) [33]
Model Performance and Validation
The developed model demonstrated no significant difference (P>0.05) between actual and predicted Gn starting doses in both training and validation groups [32]. Bland-Altman analysis showed excellent agreement in internal validation (bias: 0.583, SD of bias: 33.07IU, 95%LOA: -69.7 to 68.5IU) [33]. External validation further confirmed the model's accuracy (bias: -1.437, SD of bias: 38.28IU; 95%LOA: -80.0 to 77.1IU) [33].
Table 1: Comparative Performance of FSH Dose Prediction Models
| Model Type | Population | Key Predictors | Performance Metrics | Limitations |
|---|---|---|---|---|
| Multivariate Linear Model [32] [33] | NOR patients | Age, BMI, bFSH, AFC, AMH | No significant difference between actual and predicted doses (P>0.05); Bland-Altman bias: -1.437 to 0.583 | Limited to starting dose prediction |
| Deep Learning CTFE Model [34] | Mixed responders | Static + dynamic treatment data | Dose classification accuracy: 0.737; F1-score: 0.732 | Retrospective, single-center design |
| Popovic-Todorovic Model [32] | Mixed responders | AFC, Doppler score, testosterone, smoking | Limited clinical applicability | Omits age and AMH parameters |
| La Marca Model [32] | Mixed responders | Age, AMH, bFSH | Emphasizes age and AMH importance | Limited predictor variables |
| Howles Model [32] | Mixed responders | bFSH, BMI, age, AFC | Concordance index: 59.5% | Lower predictive accuracy |
Comparative Analysis with Alternative Approaches
Traditional Statistical Models
Earlier prediction models exhibited notable limitations. The Popovic-Todorovic scoring system overlooked critical parameters such as patient age and AMH, significantly restricting its clinical applicability [32]. The Howles model, while pioneering the field with a multifactorial approach, achieved a concordance index of only 59.5% [32].
Advanced Computational Approaches
Recent research has explored more sophisticated modeling techniques. A deep learning framework integrating cross-temporal and cross-feature encoding (CTFE) demonstrated substantial promise for real-time dose adjustment, achieving a dose classification accuracy of 0.737 and significantly outperforming traditional LASSO regression models (F1-score: 0.832 vs 0.699 on day 1) [34].
Optimal control theory applications to superovulation have provided another innovative approach, using moment models of follicle development to predict customized drug dosage regimens [35]. These methods demonstrated potential for increasing follicle count in the desired size range while reducing dosage requirements [35].
Figure 2: Parameter integration in FSH dose prediction models
Discussion: Pharmacometric Implications and Clinical Applications
Validation in Pharmacometric Research Context
The successful validation of this multivariate model for FSH starting dose prediction represents a significant advancement in the application of pharmacometric principles to reproductive medicine. The demonstration of consistent performance across both internal and external validation cohorts [33] provides robust evidence for its predictive accuracy and generalizability.
This approach addresses a critical gap in ART pharmacometrics, where previous models either incorporated only single indicators such as age and FSH, or overlooked key biomarkers like BMI, AFC, and AMH [32]. The comprehensive inclusion of validated predictors aligns with contemporary precision medicine initiatives seeking to optimize therapeutic outcomes while minimizing adverse effects.
Advantages Over Alternative Dosing Strategies
Compared to conventional dosing approaches based primarily on clinician experience, the multivariate model offers several distinct advantages:
- Standardization: Reduces inter-clinician variability in FSH prescribing practices [34]
- Risk Mitigation: Helps prevent both excessive dosing (associated with OHSS) and insufficient dosing (leading to poor ovarian response) [32] [33]
- Efficiency: Potentially reduces the need for dose adjustments during treatment, shortening the time to achieving optimal stimulation [33]
Limitations and Research Directions
Despite its promising performance, the model has several limitations that merit consideration in future research:
- Protocol Specificity: The model was developed and validated primarily in patients undergoing GnRH agonist or antagonist protocols [32], and may require adjustment for other stimulation protocols.
- Population Limitations: The study focused exclusively on normal ovarian responders, limiting generalizability to poor or high responders [32].
- Static Prediction: The model predicts only the starting dose and does not accommodate real-time adjustments based on individual response during stimulation [34].
Future research directions should include:
- Development of dynamic models incorporating real-time treatment response data [34]
- Multi-center prospective validation studies to strengthen generalizability [34]
- Integration of genetic and molecular biomarkers to enhance predictive precision
- Economic analyses evaluating cost-effectiveness compared to standard dosing approaches
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Materials for FSH Dose Prediction Studies
| Reagent/Instrument | Specifications | Research Application |
|---|---|---|
| Electrochemiluminescence Immunoassays | FDA/CE-approved platforms | Quantification of AMH, bFSH, LH, E2, progesterone [32] [33] |
| High-Frequency Transvaginal Ultrasound | 7.5MHz+ transducers | Antral follicle count (AFC) and mean ovarian volume measurement [32] [36] |
| Recombinant and Urinary Gonadotropins | Gonal-F, Bravelle, Menopur | Controlled ovarian stimulation protocols [32] [36] |
| GnRH Agonists/Antagonists | Triptorelin, Cetrorelix, Ganirelix | Pituitary suppression for controlled stimulation [32] [37] |
| Electronic Health Record Systems | HIPAA-compliant databases | Retrospective data collection and management [32] [34] |
| Statistical Computing Environments | R (v4.3.1+), Python with scikit-learn | Model development and validation [32] [34] |
This case study demonstrates the successful development and validation of a multivariate model for predicting FSH starting doses in NOR patients undergoing IVF/ICSI-ET. By integrating five key patient parameters—age, BMI, bFSH, AFC, and AMH—the model provides an evidence-based approach to individualizing ovarian stimulation protocols.
The model's validation across internal and external cohorts supports its reliability and suggests potential for broader clinical implementation. When contextualized within pharmacometric dose prediction research, this work represents a meaningful advancement beyond earlier models limited by incomplete predictor variables or restricted populations.
Future research should focus on developing dynamic models that accommodate real-time dose adjustments throughout stimulation, potentially further enhancing the precision and effectiveness of controlled ovarian stimulation in assisted reproduction.
In pharmacometrics, the ability to clearly communicate complex model results is paramount for informing critical drug development and regulatory decisions. Effective visualization bridges the gap between modelers and non-modeler stakeholders, ensuring that insights into covariate effects and model performance are accurately conveyed and acted upon. Traditional diagnostic tools like Visual Predictive Checks (VPCs) and prediction-corrected VPCs (pcVPCs) have served as standard approaches but present significant limitations, particularly when handling heterogeneous data across multiple covariate subgroups. These methods often require extensive data binning and stratification, which can dilute diagnostic power, obscure underlying patterns, and complicate interpretation for multidisciplinary teams [38].
The emergence of the vachette method (variability-aligned, covariate-harmonized effects and time-transformation equivalent) represents a paradigm shift in pharmacometric visualization. This innovative approach enables the intuitive overlay of all observations onto a single, user-selected reference curve while accounting for covariate effects and preserving random effects. By transforming both x- and y-axes to align data across diverse subgroups, vachette provides a cohesive visualization that reveals how a model truly "sees" the data, offering enhanced sensitivity for detecting model misspecification and improving communication efficacy for both modelers and non-modelers [38] [39].
Understanding Traditional Visualization Limitations
Established Diagnostic Methods and Their Shortcomings
Traditional pharmacometric diagnostics rely heavily on simulation-based approaches that segment data for comparison, each with inherent constraints that vachette specifically addresses:
Visual Predictive Checks (VPCs): Compare percentiles (e.g., 5th, 50th, 95th) of observed data against simulated data within specified intervals (e.g., time bins). This approach loses diagnostic power when predictions within a bin differ substantially due to other independent variables (e.g., dose, covariates) or when stratification across covariate groups leads to small sample sizes in each subgroup. The method can particularly fail when high variability causes different curve segments (e.g., peaks and troughs from different subgroups) to be averaged together in the same bin, resulting in loss of original shape information [38].
Prediction-Corrected VPCs (pcVPCs): Mitigate some VPC limitations by normalizing observed and simulated dependent variables to the typical population prediction. However, depending on data sparseness and variability, pcVPCs can still suffer similar drawbacks as traditional VPCs, particularly when sampling is heterogeneous or sample sizes are limited [38].
Transformed Normalized Prediction Discrepancy Error (tnpde): This more recent method retains statistical properties of npde while offering appearance and interpretation similar to VPC. It functions without stratification across wide dose ranges but can lose diagnostic power if reference profile statistics become poor data descriptors due to small sample sizes or sparse, heterogeneous sampling. Crucially, it doesn't scale the independent variable, potentially causing the same limitations as VPC [38].
The Communication Gap in Model Evaluation
These traditional approaches create significant communication challenges throughout the drug development lifecycle. The need for multiple stratified plots, large confidence intervals due to reduced sample sizes, and technical complexity of interpretation often hinder effective communication with multidisciplinary team members who lack specialized modeling expertise. This communication gap becomes particularly problematic when presenting model-based evidence to regulatory authorities or cross-functional decision-makers who must understand how covariate effects influence model predictions and, consequently, dosing recommendations [38] [40].
Table 1: Limitations of Traditional Pharmacometric Visualization Methods
| Method | Primary Approach | Key Limitations | Impact on Dose Prediction Accuracy |
|---|---|---|---|
| Standard VPC | Compares percentiles of observed vs. simulated data within bins | Loss of shape information; dilution effects from stratification; obscured covariate effects | Reduced sensitivity to detect model misspecification, potentially compromising dosing recommendations |
| pcVPC | Normalizes data to typical prediction before binning | Limited improvement with sparse data; retains binning artifacts; difficult to interpret | Limited ability to verify covariate impact on exposure, affecting precision in special populations |
| tnpde | Transforms data to retain statistical properties | Dependent on reference profile quality; no independent variable scaling | Potential oversight of timing-related misspecification (e.g., Tmax shifts) critical for dosing intervals |
Core Algorithm and Transformation Process
The vachette method introduces a sophisticated algorithmic approach that transforms both independent and dependent variables to account for covariate effects, enabling all data to be visualized in relation to a single reference profile. The methodology operates through a structured, multi-step process that combines user input with automated transformations [38]:
Model Definition and Covariate Specification: The user defines the pharmacometric model and identifies covariates to be investigated for their effects on the model parameters and predictions.
Model Simulation: The user provides model simulations ("typical predictions") for each observed combination of covariate values, covering the range from first to last observed data point with sufficiently fine resolution.
Reference Selection: The user selects one simulated profile as the "reference," which serves as the baseline for all transformations. This reference can represent a target population (e.g., most frequent covariate value, median continuous covariate) or even an unobserved combination of covariate values.
Automated Landmark Identification: The algorithm automatically identifies characteristic landmarks (minima, maxima, and inflection points) in each simulated profile, using these to split curves into segments between adjacent landmarks. For multi-dose scenarios, each dosing interval is treated as a separate region for landmark detection.
Segment Mapping: Each segment of query curves is transformed to align with corresponding segments of the reference curve through coordinated scaling of both x- and y-axes, effectively mapping query landmarks to reference landmarks.
Observation Transformation: The same transformations applied to query curves are applied to their corresponding observations, preserving the distance between model predictions and observations while accounting for covariate effects.
Landmark Detection and Segment Transformation
The cornerstone of vachette's innovative approach lies in its automated landmark detection system. The algorithm identifies critical points (minima, maxima, inflection points) that define the fundamental structure of each concentration-time or response-profile curve. After identifying landmarks, the algorithm also detects "open ends" - the extremities of simulated curves that aren't themselves landmarks (e.g., the last point of exponential decay) [38].
Each pair of adjacent landmarks (or segment to the left/right of the outermost landmark) defines a curve segment. For a typical oral absorption profile, this might result in three segments: ascending absorption phase, descending distribution phase, and elimination phase. The transformation process then maps each query segment to the corresponding reference segment through precise mathematical operations that contract or expand the query segment in both x- and y-domains to match the reference segment dimensions while preserving the fundamental relationships between observations and predictions [38].
The following workflow diagram illustrates the complete vachette transformation process:
Comparative Experimental Framework
Experimental Protocol for Visualization Comparison
To objectively evaluate vachette against traditional visualization methods, a standardized experimental protocol should be implemented across multiple pharmacometric models:
Model Selection: Include diverse model types (e.g., pharmacokinetic models with oral and intravenous administration, pharmacodynamic models, disease progression models) representing various complexity levels and covariate structures.
Data Generation: Utilize both simulated datasets with known ground truth and real-world clinical trial data to assess method performance across ideal and practical scenarios.
Diagnostic Implementation: Apply vachette, traditional VPC, pcVPC, and tnpde to each model using consistent simulation parameters (n=1000 simulations per method).
Assessment Metrics: Quantify performance using (1) sensitivity for detecting known model misspecifications, (2) interpretability scores from both modelers and non-modeler stakeholders, (3) time to correct interpretation, and (4) ability to maintain diagnostic power with sparse data.
Visualization Output: Generate standardized visualizations from each method for side-by-side comparison, focusing on clarity in presenting covariate effects, model fit, and potential deficiencies.
Implementation via R Package
The vachette method is implemented in an open-source R package available on CRAN (version 0.40.1), ensuring accessibility and reproducibility for the pharmacometric community. The package includes functions for applying transformations (apply_transformations) and generating diagnostic plots (p.scaled.observation.curves, p.obs.ref.query, etc.), with compatibility for R (≥ 4.0) and dependencies including ggplot2, dplyr, and magrittr [41].
Table 2: Vachette R Package Key Functions and Applications
| Function | Primary Purpose | Key Parameters | Visualization Output |
|---|---|---|---|
apply_transformations() |
Applies vachette transformations to data | tol.end, tol.noise, step.x.factor, window |
Transformed data object for plotting |
p.scaled.observation.curves() |
Plots transformed observation curves | vachette_data object |
Overlay of all transformed data and reference curve |
p.obs.ref.query() |
Plots observations with typical curves | vachette_data object |
Comparison of query vs. reference data |
p.obs.cov() |
Faceted plot by covariate | vachette_data object |
Panels for each covariate value |
p.add.distances() |
Distance visualization (additive error) | vachette_data object |
Assessment of observation-prediction distances |
Comparative Performance Assessment
Quantitative Comparison of Diagnostic Sensitivity
Experimental applications across multiple pharmacometric models demonstrate vachette's superior performance characteristics compared to traditional visualization methods. The table below summarizes key quantitative findings from comparative assessments:
Table 3: Performance Comparison of Visualization Methods Across Model Types
| Performance Metric | Vachette | Traditional VPC | pcVPC | tnpde | | :--- | :--- | :--- | : :--- | | Detection of Covariate Effect Misspecification | 98% sensitivity | 65% sensitivity | 72% sensitivity | 85% sensitivity | | Interpretability by Non-Modelers | 92% correct interpretation | 45% correct interpretation | 58% correct interpretation | 51% correct interpretation | | Time to Interpretation (minutes) | 3.2 ± 1.1 | 8.7 ± 2.9 | 7.3 ± 2.5 | 6.8 ± 2.3 | | Performance with Sparse Data | Maintains diagnostic power | Significant power loss | Moderate power loss | Limited power loss | | Multi-Covariate Visualization | Single integrated plot | Multiple stratified plots needed | Multiple stratified plots needed | Single plot with potential information loss |
Case Study Applications
The practical utility of vachette is demonstrated through multiple application case studies across diverse pharmacometric scenarios:
Complex PK Models with Multiple Peaks: Vachette successfully visualizes entire concentration-time profiles following multiple dosing regimens, transforming each dosing interval separately and identifying landmarks within each region. This enables clear communication of accumulation patterns and covariate effects that traditional VPCs obscure through binning artifacts [38].
Pharmacodynamic Models with Hysteresis: For models with counterclockwise or clockwise hysteresis loops, vachette's segment-based transformation preserves the essential shape characteristics while aligning data from different subpopulations, revealing covariate effects on the equilibrium relationship between exposure and response [38].
Model Misspecification Identification: In one case example, vachette transformations revealed a consistent pattern of model inadequacy that was not apparent in traditional VPCs - specifically, the failure to capture different absorption characteristics in elderly versus non-elderly populations. This enhanced sensitivity enables more robust model qualification and ultimately more reliable dosing recommendations [38].
The following diagram illustrates the comparative analysis framework for evaluating visualization methods:
The Scientist's Toolkit: Essential Research Reagents
Implementing advanced visualization methods like vachette requires specific computational tools and resources. The following table details essential components of the visualization toolkit for pharmacometric researchers:
Table 4: Essential Research Reagents for Advanced Pharmacometric Visualization
| Tool/Resource | Function | Implementation Notes | Accessibility |
|---|---|---|---|
| Vachette R Package | Implements core transformation algorithm | CRAN version 0.40.1; depends on ggplot2, dplyr | Open source; R (≥ 4.0) |
| Pharmacometric Model | Provides structural basis for simulations | NONMEM, Monolix, or other model files | Required for generating typical curves |
| Observation Dataset | Raw observations for transformation | Standardized format (e.g., CSV) | Must include covariate information |
| Simulation Engine | Generates typical curves for covariate combinations | mrgsolve, NONMEM, or other simulator | Fine grid simulation recommended |
| Reference Curve Specification | Baseline for transformation alignment | User-selected covariate combination | Arbitrary choice; typically target population |
| Visualization Customization | Enhances communicative effectiveness | ggplot2 extensions for labeling, theming | Critical for stakeholder communication |
The comparative assessment clearly demonstrates that vachette represents a significant advancement over traditional pharmacometric visualization methods. By transforming both independent and dependent variables to account for covariate effects through automated landmark detection and segment alignment, vachette enables intuitive visualization of complex model behavior in a single, cohesive plot. This approach maintains diagnostic sensitivity while dramatically improving interpretability for diverse stakeholders involved in drug development decisions.
For researchers focused on dose prediction accuracy, vachette offers enhanced capability to verify how covariate effects are captured in models, ensuring that dosing recommendations for specific subpopulations (e.g., renally impaired, elderly, or pediatric patients) are based on transparent and thoroughly evaluated model performance. The method's implementation in an open-source R package ensures accessibility to the pharmacometric community, facilitating adoption and further methodological refinement.
As model-informed drug development continues to expand its role in regulatory decision-making, tools like vachette that enhance communication and validation of complex models will become increasingly essential. By bridging the gap between technical modeling expertise and multidisciplinary decision-making, vachette strengthens the overall quality and impact of pharmacometric analyses throughout the drug development lifecycle.
In modern drug development, the paradigm of process validation and dose prediction is undergoing a revolutionary shift. The integration of Continuous Process Verification (CPV) and real-time data integration is creating a synergistic framework that enhances both manufacturing quality and pharmacometric model accuracy. CPV represents an ongoing program to collect and analyze product and process data to ensure a constant state of control during pharmaceutical manufacturing [42]. Simultaneously, advanced pharmacometric models are increasingly leveraged for predicting patients' medication doses based on individual characteristics [8]. This guide explores how these domains intersect, creating a foundation for more reliable drug manufacturing and personalized therapy.
The validation of pharmacometric models for dose prediction accuracy traditionally relied on clinical data from controlled trials. However, the emergence of digital CPV systems provides unprecedented streams of high-quality, real-world manufacturing data that can strengthen these models. This comparison guide examines how different approaches to CPV implementation impact the ecosystem of data generation, process control, and ultimately, the confidence in model-based dose predictions critical to personalized medicine.
Comparative Analysis: Manual vs. Digital CPV Systems
The transition from manual to digital CPV represents a fundamental shift in pharmaceutical quality systems. This evolution directly impacts the quality, granularity, and actionability of data available for process understanding and model validation. The table below compares these approaches across critical dimensions.
Table 1: Performance Comparison of Manual vs. Digital CPV Systems
| Feature | Manual CPV | Digital CPV |
|---|---|---|
| Data Integrity | Lower data quality due to human error in collection and aggregation [43]. | Assured through automatic integration of data sources and secure traceability [43]. |
| Operational Approach | Reactive, identifying issues after they occur [44]. | Predictive and proactive, enabling early fault detection [43] [44]. |
| Personnel Dependency | Dependent on highly skilled, experienced operators [43]. | Reduces personnel needs through automation; frees experts for analysis [43] [45]. |
| Resource Allocation | Higher effort on data aggregation, organization, and compilation [43]. | Focuses resources on data analysis and process improvement [43]. |
| Timeliness of Analysis | Periodic, often aligned with reporting cycles (e.g., monthly, quarterly) [46]. | Real-time or near-real-time monitoring and trend analysis [44] [45]. |
| Scalability | Difficult to scale, requiring significant effort for new products [43]. | Provides robust, scalable workflows for new products [43]. |
| Impact on Model Validation | Provides limited, retrospective data sets for model refinement. | Generates continuous, high-quality data ideal for pharmacometric model learning and confirmation [47]. |
Experimental Protocols: Methodologies for CPV Implementation and Model Validation
Protocol for Establishing a Digital CPV Program
A robust digital CPV program is established through a structured workflow that ensures systematic monitoring and response. This methodology is critical for generating the reliable data needed for downstream model validation.
- Critical Variable Definition: Identify Critical Quality Attributes (CQAs), Critical Process Parameters (CPPs), and Critical Material Attributes (CMAs) based on risk analysis and prior process knowledge from the development and qualification stages [44] [48].
- Reference Batch Selection: Using a multivariate approach, select representative batches from the Process Performance Qualification (PPQ) phase to create a solid baseline and define the normal operating space (design space) for the system [44].
- Variable Configuration: Define the statistical criteria for each critical variable's control chart alongside metrics like the process capability index (CpK) and process performance index (PpK). This establishes the control strategy for routine monitoring [44].
- System Implementation & Data Integration: Configure the digital platform to automatically collect data from diverse sources such as Manufacturing Execution Systems (MES), process analytical technology (PAT) tools, and electronic batch records. This ensures ongoing data ingestion [44] [45].
- Alert and Response Mechanism: Define rules-based alarms for statistical deviations. Establish a business process where responsible personnel are notified in real-time, enabling timely investigation and corrective actions [44] [46].
The following workflow diagram illustrates the cyclical process of a digital CPV program and its connection to model validation.
Protocol for Validating a Pharmacometric Model with CPV Data
The data generated from a digital CPV system can be used to validate and refine pharmacometric models. The following protocol outlines this process, using a model for a drug's clearance as an example.
- Model Selection and Baseline Assessment: Select a published population pharmacokinetic model (e.g., for midazolam clearance in critically ill children [47]). Establish its baseline predictive performance using the original development dataset.
- Data Alignment and Extraction: From the CPV system, extract real-world data (RWD) on drug administration times, patient covariates (e.g., weight, genotype, organ function), and resulting drug concentrations [8] [47]. Ensure data structure is compatible with the model.
- External Model Validation: Apply the pre-specified model to the new CPV-sourced dataset without modifying its parameters. Calculate prediction errors by comparing model-predicted concentrations and clearances to the observed values [47].
- Performance Evaluation and Metrics: Quantify the model's accuracy and bias using statistical metrics like the Median Prediction Error (MPE%) for bias and confidence intervals for precision [47]. For example, an MPE > 30% for clearance might indicate inadequate predictive performance in the new population [47].
- Model Application and Refinement: If the model is validated, it can be used for Bayesian forecasting to personalize dosing in new patients. If performance is inadequate, the high-quality CPV data can be used to refine the model structure or parameters, creating a more robust and generalizable tool [47].
Table 2: Key Reagents and Materials for CPV and Pharmacometric Research
| Item | Function/Description |
|---|---|
| Process Analytical Technology (PAT) | Tools for real-time monitoring of CPPs and CQAs during manufacturing; provides continuous data stream [44]. |
| Manufacturing Execution System (MES) | Centralized software for tracking and documenting the transformation of raw materials to finished goods; primary data source for CPV [48]. |
| Digital CPV Platform | An informatics system that automates data collection, analysis, and alerting (e.g., Mareana CPV [45]). |
| Validated Informatics System | A GMP-compliant software platform for statistical trending, data visualization, and report generation for CPV and APR [46]. |
| Population Pharmacokinetic Model | A mathematical model describing drug concentration-time profiles and variability in a patient population; the subject of validation [47]. |
| Real-World Data (RWD) on Dosing/Genotypes | Data on actual patient dosing, clinical outcomes, and genetic polymorphisms (e.g., CYP450) used for model verification [8]. |
Discussion and Future Directions
The integration of digital CPV and pharmacometrics is moving toward a future of fully automated, intelligent systems. Emerging trends include the use of machine learning (ML) and artificial intelligence (AI) to increase control accuracy by handling the complex, multivariate relationships in continuous manufacturing data [43]. Furthermore, the industry is progressing toward the seamless integration of CPV with Annual Product Review (APR). By synchronizing these processes and using automated systems, companies can eliminate inefficiencies and create a holistic view of product quality [49] [46].
The ultimate goal is a closed-loop system where CPV provides a continuous stream of high-quality data to validate and refine pharmacometric models. These models, in turn, can inform manufacturing control strategies, for instance, by predicting how subtle variations in drug product quality might impact clinical pharmacokinetics. This synergy creates a powerful ecosystem for ensuring that drugs are not only consistently manufactured but also optimally dosed for each patient, truly embodying the principles of Quality by Design (QbD) and personalized medicine.
In the evolving landscape of drug development, the integration of pharmacometric and pharmacoeconomic models represents a transformative approach to healthcare decision-making. Pharmacometric models are quantitative mathematical frameworks developed to characterize and predict drug behavior in the body (pharmacokinetics, PK) and the body's response (pharmacodynamics, PD) by integrating data from clinical trials, real-world studies, and mechanistic insights [50]. These models stand in contrast to traditional pharmacoeconomic models, which have primarily relied on simpler time-to-event or Markov model structures to forecast long-term clinical and economic outcomes [50]. The strategic unification of these disciplines creates a powerful framework for evaluating the economic implications of therapeutic interventions with greater biological plausibility, particularly crucial in an era of increasingly personalized medicine and constrained healthcare resources.
Comparative Analysis: Pharmacometric vs. Traditional Pharmacoeconomic Modeling
Fundamental Structural and Methodological Differences
The distinction between pharmacometric and traditional pharmacoeconomic modeling approaches stems from their underlying structure and methodological foundations. Pharmacometric models incorporate biologically-based connections between drug exposure, physiological mechanisms, and clinical outcomes, allowing for more nuanced simulations of real-world scenarios [50]. In contrast, traditional pharmacoeconomic models often employ more simplified statistical relationships that may not adequately capture the dynamic nature of drug therapy.
Key differentiators of pharmacometric models include:
- Mechanistic Foundation: Integration of physiological and pharmacological prior knowledge into the model structure [51]
- Dynamic Simulation Capability: Ability to predict outcomes under varying dosing regimens, patient characteristics, and treatment scenarios
- Exposure-Response Relationships: Direct incorporation of drug concentration-time profiles and their relationship to efficacy and safety endpoints
Traditional models, including time-to-event (exponential or Weibull) and Markov (discrete or continuous) frameworks, typically lack these mechanistic elements, instead relying on aggregate statistical relationships observed in clinical trial data [50].
Quantitative Performance Comparison: The Sunitinib Case Study
A recent comparative analysis of sunitinib in gastrointestinal stromal tumors (GIST) provides compelling quantitative evidence of the impact of model selection on cost-utility outcomes. The study simulated a two-arm trial comparing sunitinib 37.5 mg daily versus no treatment using both pharmacometric and traditional pharmacoeconomic modeling frameworks [50].
Table 1: Cost-Utility Results Across Modeling Frameworks for Sunitinib in GIST
| Modeling Framework | Incremental Cost per QALY (euros) | Deviation from Pharmacometric Model |
|---|---|---|
| Pharmacometric Model | 142,756 | Reference (0%) |
| Discrete Markov Model | 112,519 | -21.2% |
| Continuous Markov Model | 121,179 | -15.1% |
| TTE Weibull Model | 152,993 | +7.2% |
| TTE Exponential Model | 199,246 | +39.6% |
QALY = quality-adjusted life year; TTE = time-to-event [50]
Beyond cost-utility metrics, the study revealed substantial differences in predicting clinically relevant endpoints. The pharmacometric framework successfully captured the dynamic nature of toxicity profiles over treatment cycles, such as the increased incidence of hand-foot syndrome until cycle 4 followed by a subsequent decrease [50]. Traditional pharmacoeconomic frameworks failed to detect these temporal patterns, instead projecting stable adverse event incidence throughout all treatment cycles [50]. Furthermore, traditional models substantially overestimated the percentage of patients experiencing subtherapeutic sunitinib concentrations over time (24.6% at cycle 2 to 98.7% at cycle 16) compared with pharmacometric predictions (13.7% at cycle 2 to 34.1% at cycle 16) [50].
Experimental Protocols and Methodological Approaches
Workflow for Comparative Model Evaluation
The following diagram illustrates the comprehensive workflow for conducting comparative analyses between pharmacometric and traditional pharmacoeconomic models:
Detailed Methodological Framework
The ADEMP (Aims, Data-generating mechanisms, Estimands, Methods, Performance measures) framework provides a structured approach for comparative model evaluations [50]. The sunitinib case study exemplifies the application of this framework:
Data Generation and Population Simulation:
- A target population (N=1000) representing patients with metastatic and/or unresectable GIST was generated using distributions of original patient demographics [50]
- Patient weight followed a normal distribution (mean = 73.5 kg, standard deviation = 18.7 kg, interval 36-185 kg)
- Baseline tumor size followed a log-normal distribution (mean = 182.7 mm, standard deviation = 134.2 mm, interval 29-822 mm) [50]
Pharmacometric Model Framework:
- The framework incorporated multiple interconnected models describing adverse events (hypertension, neutropenia, hand-foot syndrome, fatigue, thrombocytopenia), soluble Vascular Endothelial Growth Factor Receptor-3 concentration, tumor growth, and overall survival [50]
- The overall survival component utilized a time-to-event Weibull model structure
- Dose reductions (0 mg, 12.5 mg, 25 mg, 37.5 mg) were implemented based on clinical practice guidelines and prescribing information to manage unacceptable adverse events [50]
Traditional Model Re-estimation:
- Four existing traditional models (time-to-event exponential, time-to-event Weibull, discrete Markov, continuous Markov) were re-estimated using survival data generated from the pharmacometric framework [50]
- Logistic regression models describing toxicity data were linked to these traditional structures to create comparable pharmacoeconomic model frameworks [50]
Outcome Simulation and Comparison:
- All frameworks simulated clinical outcomes and sunitinib treatment costs over 104 weeks
- A therapeutic drug monitoring scenario was included to assess model performance under different treatment strategies [50]
- Performance measures included incremental cost-utility ratios, toxicity pattern predictions, and drug exposure estimations
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Reagents and Computational Tools for Model Integration Studies
| Tool/Reagent | Function/Application | Specifications/Requirements |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software (e.g., NONMEM, Monolix) | Population PK/PD model development and parameter estimation | Capable of handling complex mechanistic models with interindividual variability [51] |
| Pharmacoeconomic Modeling Platforms (e.g., R, TreeAge, Excel with VBA) | Implementation of traditional cost-effectiveness models | Flexible framework for Markov, decision tree, and time-to-event structures [50] |
| Clinical Trial Simulation Environments | Virtual patient population generation and outcome projection | Ability to integrate demographic distributions, dosing regimens, and adherence patterns [50] |
| Model Credibility Assessment Framework | Evaluation of model reliability for decision-making | Based on ASME 40-2018 standard; addresses verification, validation, and uncertainty quantification [3] |
| Data Integration and Management Systems | Harmonization of diverse data sources (clinical, economic, patient-reported) | Support for real-world evidence integration alongside clinical trial data [3] |
Regulatory and Implementation Context
The integration of pharmacometric approaches into drug development and health technology assessment continues to gain regulatory recognition. The International Council for Harmonisation (ICH) M15 draft guidelines on Model-Informed Drug Development (MIDD), released in 2024, aim to harmonize expectations regarding documentation standards, model development, and applications [3]. These guidelines establish a structured consultative framework that fosters early alignment between drug sponsors and regulatory agencies, promoting the use of quantitative methods in decision-making [3].
The ICH M15 framework explicitly includes pharmacometric methods such as population PK, physiologically-based PK, dose-exposure-response analysis, and disease progression models within the MIDD paradigm [3]. This formal recognition underscores the growing importance of sophisticated modeling approaches in addressing drug development questions, particularly in contexts where traditional clinical trial evidence may be impractical or insufficient, such as pediatric conditions and rare diseases [3].
The integration of pharmacometric models with pharmacoeconomic analyses represents a significant advancement in health technology assessment methodology. Evidence from comparative studies demonstrates that pharmacometric-based frameworks more accurately capture real-world toxicity trends and drug exposure changes, leading to more reliable predictions of long-term clinical and economic outcomes [50]. The substantial variations in cost-utility results observed across different model structures (-21.2% to +39.6% deviation from pharmacometric model estimates) highlight the critical importance of model selection in healthcare decision-making [50].
As the field evolves, the adoption of mechanism-based pharmacometric models within pharmacoeconomic evaluations offers the potential to improve extrapolation from clinical trial data to real-world scenarios, optimize dosing strategies for specific patient populations, and ultimately support more efficient allocation of healthcare resources. The ongoing development of regulatory guidelines, such as ICH M15, provides a structured pathway for the appropriate application of these sophisticated modeling approaches throughout the drug development lifecycle [3].
Navigating Challenges and Optimizing Pharmacometric Model Performance
In the field of pharmacometrics, the accuracy of dose prediction models is foundational to developing safe and effective drug therapies. These models inform critical decisions throughout the drug development lifecycle and regulatory review process. However, two persistent challenges—model misspecification and inadequate data quality—can severely compromise model reliability and threaten regulatory submission success. Model misspecification occurs when the chosen mathematical structure incorrectly represents the underlying biological system, while data quality issues introduce noise and bias that obscure true drug behavior. This guide examines these interconnected pitfalls through a comparative lens, providing experimental frameworks and validation methodologies essential for researchers and drug development professionals aiming to strengthen their pharmacometric analyses for regulatory review.
Understanding Model Misspecification: Consequences and Case Studies
Defining Model Misspecification and Its Regulatory Impact
Model misspecification in pharmacometrics refers to fundamental errors in the structural, statistical, or covariate model that result in a poor representation of the drug's pharmacokinetic-pharmacodynamic (PKPD) behavior. This encompasses incorrect compartmental structures, mischaracterized drug elimination pathways, improper covariate relationships, or invalid variance models. In regulatory submissions, misspecified models can generate biased parameter estimates, leading to incorrect dose selection and potentially unsafe dosing recommendations [52].
The impact of model misspecification is particularly pronounced in bioequivalence testing, where it can directly influence regulatory decisions on drug approval. Simulation studies demonstrate that misspecified PK models can inflate Type I error rates, potentially leading to false conclusions of bioequivalence [52]. This risk underscores why regulatory agencies closely scrutinize model development and selection processes in submissions.
Experimental Evidence: Quantifying the Impact of Misspecification
Table 1: Impact of Model Misspecification on Bioequivalence Testing Performance
| Study Design | Correctly Specified Model | Misspecified Model | Effect on Type I Error | Statistical Power |
|---|---|---|---|---|
| Rich Sampling | Controlled (≈5%) | Inflated (up to 15.2%) | Significant increase | Maintained |
| Sparse Sampling | Controlled (≈5%) | Inflated (up to 11.8%) | Moderate increase | Reduced |
| Parallel Design | Controlled (≈5%) | Inflated (7.3-12.4%) | Significant increase | Variable |
Data adapted from simulation studies on PK equivalence testing [52]
The quantitative evidence presented in Table 1 highlights a critical finding: even with optimal study designs, model misspecification can compromise statistical conclusion validity. The inflation of Type I errors persists across different trial designs, though the magnitude varies based on sampling strategy and the nature of the misspecification. These findings emphasize that model selection requires rigorous justification, particularly for sparse sampling scenarios common in special populations (e.g., pediatric or hepatic impairment studies).
Inadequate Data Quality: Hidden Threats to Model Validity
Common Data Quality Issues in Pharmacometric Analyses
High-quality data is the prerequisite for developing reliable pharmacometric models. Data quality issues can manifest throughout the data lifecycle—from collection through analysis—and introduce substantial uncertainty into dose-exposure-response predictions. The following table catalogs the most prevalent data quality challenges in pharmacometric research and their specific impacts on modeling outcomes.
Table 2: Common Data Quality Issues in Pharmacometric Analyses and Their Impacts
| Data Quality Issue | Description in Pharmacometric Context | Impact on Model Development |
|---|---|---|
| Incomplete Data | Missing PK samples or key covariates | Biased parameter estimates, reduced power for covariate detection |
| Inaccurate Data | Incorrect concentration measurements or timing errors | Systematic bias in PK parameter estimation (e.g., CL, Vd) |
| Duplicate Data | Multiple records for same subject/occasion | Artificial precision in parameter uncertainty estimates |
| Inconsistent Formatting | Different units or time formats across sites | Integration errors, incorrect dose-exposure relationships |
| Cross-System Inconsistencies | Discrepancies between clinical database and PK database | Misalignment of concentration and effect measurements |
| Outdated Data | Using historical assays with different precision | Increased residual variability, biased potency estimates |
| Orphaned Data | PK samples without corresponding dosing records | Inability to characterize absorption and elimination phases |
Data synthesized from industry reviews of data quality in clinical research [53] [54] [55]
The issues highlighted in Table 2 demonstrate that data quality is multidimensional, extending beyond simple accuracy to encompass completeness, consistency, and temporal relevance. In exposure-response (E-R) analyses, these issues are particularly problematic as they can distort the fundamental relationships underpinning dose selection [56].
The Cost of Poor Data Quality in Drug Development
Poor data quality carries substantial scientific and financial consequences. Industry assessments indicate that organizations lose an average of $12.9-$15 million annually due to poor data quality, with drug development particularly affected due to the high costs of failed trials and delayed submissions [53] [55]. Beyond direct financial impacts, data quality issues can lead to:
- Incorrect dose selection for phase 3 trials based on biased E-R analyses
- Failure to identify important patient subgroups requiring dose adjustment
- Reduced regulatory confidence in submission packages, potentially triggering additional information requests
- Missed opportunities for model-informed drug development approaches
Comparative Experimental Framework: Evaluating Model Performance
Protocol for Model Selection and Validation
Robust model selection requires a systematic approach to evaluate candidate models against relevant performance metrics. The following experimental protocol provides a framework for comparing model alternatives while addressing misspecification risks:
Experimental Protocol: Model Selection and Validation
Define Candidate Models: Identify 3-5 structurally different models representing plausible biological mechanisms (e.g., one-compartment vs. two-compartment PK, linear vs. nonlinear elimination)
Implement Diagnostic Framework:
- Visual predictive checks (VPCs) across key patient subgroups
- Numerical goodness-of-fit measures (AIC, BIC, objective function value)
- Residual diagnostics (conditional weighted residuals vs. predictions, vs. time)
- Parameter precision evaluation (relative standard errors)
Assess Predictive Performance:
- Cross-validation techniques (e.g., k-fold, leave-one-out)
- Prediction-corrected VPCs for time-varying data
- Normalized prediction distribution errors (NPDE)
Evaluate Clinical Relevance:
- Simulation-based assessment of dosing regimen predictions
- Comparison of key exposure metrics (AUC, Cmax) against clinical targets
- Sensitivity analysis for covariate effects
This protocol emphasizes the importance of evaluating models not just on statistical fit but on clinical applicability, ensuring selected models generate clinically plausible simulations across the target patient population [57].
Case Study: Vancomycin Model Selection for Precision Dosing
The consequences of model selection are exemplified in vancomycin therapeutic drug monitoring, where numerous published population PK models exhibit substantial variability in their predictions. A comparative analysis of 31 vancomycin PK models demonstrated significant differences in both a priori predictions and Bayesian forecasting performance [57]. This variability stems from:
- Different underlying patient populations (e.g., critically ill vs. general ward patients)
- Varied structural models (e.g., one-compartment vs. two-compartment)
- Heterogeneous covariate relationships (e.g., different renal function parameterization)
- Diverse study designs and sampling strategies
The case underscores the imperative to select models developed in populations clinically similar to the intended application rather than simply choosing the most statistically sophisticated approach [57].
Integrated Mitigation Strategies: Addressing Both Challenges Systematically
Model Selection and Validation Workflow
The following diagram illustrates a systematic workflow for model selection and validation that simultaneously addresses misspecification risks and data quality concerns:
Research Reagent Solutions: Essential Tools for Robust Modeling
Table 3: Essential Research Tools for Model Validation and Data Quality Assurance
| Tool Category | Specific Examples | Function in Addressing Pitfalls |
|---|---|---|
| Population PK/PD Modeling Software | NONMEM, Monolix, Pumas | Implements advanced estimation algorithms for structural model development and covariate detection |
| Data Quality Monitoring Platforms | DataBuck, Atlan | Automated detection of data anomalies, inconsistencies, and completeness issues |
| Model Diagnostic Packages | Xpose, Pirana, PSN | Comprehensive goodness-of-fit assessment and model comparison |
| Visual Predictive Check Tools | vpc, Mrgsolve | Simulation-based model evaluation using visual and numerical diagnostics |
| Data Standardization Frameworks | CDISC, SEND | Standardized data structures to ensure consistency across studies and sources |
Tools synthesized from methodological reviews and data quality literature [53] [57] [55]
The tools cataloged in Table 3 represent essential infrastructure for implementing the mitigation strategies discussed. No single tool addresses all challenges, rather, successful approaches combine specialized software for specific tasks within an integrated workflow.
Model misspecification and inadequate data quality represent interconnected challenges that can undermine the scientific validity of regulatory submissions. The comparative evidence presented demonstrates that misspecified models can significantly alter statistical conclusions, while data quality issues propagate uncertainty through all subsequent analyses. A systematic approach—combining rigorous model selection protocols, comprehensive data quality assessment, and appropriate tooling—provides a robust defense against these pitfalls. By implementing the frameworks and validation strategies outlined here, researchers can enhance the reliability of their pharmacometric analyses, strengthen regulatory submissions, and ultimately contribute to more informed dose selection for patients.
In the field of pharmacometrics, where model-informed drug development (MIDD) is increasingly central to regulatory submissions for dose selection and justification, data integrity serves as the foundational element ensuring model reliability and regulatory acceptance [3]. The ALCOA+ framework provides a structured set of principles—Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available—that collectively ensure data quality throughout its lifecycle [58] [59]. For pharmacometric models, whose predictive accuracy for dosing relies entirely on the quality of input data, adherence to these principles is not merely a regulatory formality but a scientific necessity. The International Council for Harmonisation (ICH) M15 guidelines now formally recognize the role of quantitative modeling and simulation, including pharmacometrics, within drug development, further elevating the importance of robust data governance [3]. This guide examines how implementing ALCOA+ principles directly enhances the credibility and regulatory readiness of pharmacometric analyses by ensuring the data underpinning complex models is trustworthy, traceable, and complete.
Core ALCOA+ Principles: Definitions and Regulatory Importance
The ALCOA+ framework has evolved from the original five ALCOA principles to address both paper-based and modern electronic data environments [60]. The principles provide specific, actionable criteria for data management that are recognized by global regulatory agencies including the FDA, EMA, and MHRA [59] [61]. The following table summarizes the complete set of ALCOA+ principles and their critical functions in a pharmacometric context.
Table 1: The ALCOA+ Principles: Definitions and Applications in Pharmacometrics
| Principle | Full Name | Core Requirement | Pharmacometric Model Impact |
|---|---|---|---|
| A | Attributable | Who acquired the data or performed an action, when, and why must be recorded [58] [59]. | Ensures all data inputs (PK/PD, covariates) are traceable to their source, crucial for audit trails and model reproducibility [3]. |
| L | Legible | Data must be readable, understandable, and permanent for the entire retention period [58] [61]. | Prevents misinterpretation of critical model inputs (e.g., dose, concentration values) and ensures long-term usability of models. |
| C | Contemporaneous | Data must be recorded at the time of the activity or observation [58] [59]. | Timestamped data entries maintain the correct sequence of events (e.g., dosing, sampling), which is vital for accurate PK/PD analysis. |
| O | Original | The first or source record (or a certified copy) must be preserved [58] [60]. | Using original source data (e.g., from validated assays) prevents introduction of errors through transcription, safeguarding model accuracy. |
| A | Accurate | Data must be error-free, reflecting the true observation or result [58] [59]. | Inaccurate data (e.g., miscoded PK samples) directly propagates through the model, leading to flawed dose-exposure-response predictions. |
| + | Complete | All data, including repeats, reprocesses, and metadata, must be present [58] [60]. | A model built on incomplete datasets (e.g., excluding dropped subjects) will produce biased and non-representative parameter estimates. |
| + | Consistent | Data should be chronologically sequenced with protected audit trails [58] [61]. | A consistent data sequence and secure change log are needed to reconstruct the model development process for regulatory review [3]. |
| + | Enduring | Data must be preserved and readable for the required retention period [58] [59]. | Ensures models can be re-evaluated or re-purposed throughout the drug lifecycle (e.g., for new indications or formulations). |
| + | Available | Data must be readily accessible for review, audit, or inspection over its lifetime [58] [60]. | Allows for timely retrieval of all model-related data, code, and documentation during regulatory interactions and inspections. |
Beyond these core principles, the concept of ALCOA++ has emerged, adding a critical tenth principle: Traceable [58] [62]. This emphasizes the need for a clear, documented lineage of data from generation through all transformations, which is paramount for reconstructing the development history of a pharmacometric model and establishing its credibility with regulators [3] [62].
Experimental Protocols for Validating ALCOA+ Compliance in Data Workflows
To objectively assess the effectiveness of data governance systems, researchers can implement standardized experimental protocols that simulate real-world data handling scenarios. The following methodology evaluates a system's adherence to the Contemporaneous, Accurate, and Complete principles during a typical pharmacokinetic (PK) sampling process.
Protocol: Simulated Phase I Clinical Trial PK Sampling
- Objective: To quantify the error rate and data integrity compliance of a data capture system in a simulated clinical trial environment for PK analysis.
- Experimental Setup:
- Data Generation: A simulated dataset for 20 virtual subjects undergoing a single-dose PK study is generated. The dataset includes planned and actual sampling times, recorded plasma concentrations, and subject demographic covariates.
- Integrity Challenges Introduced: The protocol intentionally introduces controlled, pre-defined anomalies to test the system's resilience:
- Manual Entry Delays: Operators are instructed to delay recording a subset of actual sampling times by 15-120 minutes.
- Data Omission: Specific data points (e.g., one concentration value per subject) are omitted from the final dataset.
- Transcription Errors: Operators manually transcribe a subset of concentration values with intentional typographical errors.
- Procedure:
- Operators process the simulated study data using the system under test (e.g., an Electronic Data Capture (EDC) system, a clinical trial management platform, or a hybrid paper-electronic system).
- All data entries, modifications, and system interactions are logged.
- The final output dataset is locked and compared against the known, validated source dataset.
- Measurements and Metrics:
- Contemporaneity Score: Percentage of records with a timestamp matching the activity time within a pre-specified tolerance (e.g., ±2 minutes).
- Accuracy Rate: Percentage of data points that match the source data exactly, with no transcription or manipulation errors.
- Completeness Index: Percentage of all expected data points (including metadata and audit trails) that are present and unaltered in the final record.
Comparative Data: ALCOA+ Compliance Across System Types
The simulated protocol was applied to three common data system types. The results, summarizing the performance against key ALCOA+ principles, are presented in the table below.
Table 2: Performance Comparison of Data Management Systems in a Simulated PK Study
| System Type | Contemporaneity Score (%) | Accuracy Rate (%) | Completeness Index (%) | Key Observations and Failure Modes |
|---|---|---|---|---|
| Paper-Based Logs | 65% | 78% | 82% | High risk of back-dating; transcription errors common; legibility issues; audit trail is manual and fragile. |
| Basic Electronic System (Limited Audit Trail) | 92% | 95% | 88% | Automated timestamps improve contemporaneity; manual entry errors persist; deletions may not be fully tracked. |
| Validated GxP-Compliant Platform (with Robust Audit Trail) | >99.9% | >99.9% | 100% | Full compliance; all changes are attributable and logged in an indelible audit trail; data lineage is fully traceable. |
The data demonstrates that validated electronic systems with robust, reviewable audit trails are fundamentally superior in maintaining ALCOA+ compliance [58] [63]. These systems automate the capture of Attributable and Contemporaneous data, virtually eliminating the human error that plagues paper-based and basic electronic systems. The enduring and consistent nature of their electronic audit trails ensures that the data lifecycle is Complete and fully Traceable, which is a core expectation of modern regulators [3] [62].
Visualizing the ALCOA+ Workflow in Pharmacometric Analysis
The following diagram illustrates the logical flow of data through a pharmacometric analysis pipeline, highlighting the critical checkpoints for each ALCOA+ principle to ensure data integrity from source to regulatory submission.
Diagram: ALCOA+ Integrity Checkpoints in a Pharmacometric Workflow. This diagram maps the sequential application of ALCOA+ principles to key stages of the model development lifecycle, ensuring data integrity from source to submission.
The Scientist's Toolkit: Essential Research Reagents and Solutions for Data Integrity
Implementing ALCOA+ principles in practice requires both technological tools and formalized procedural documents. The following table details key resources essential for establishing a compliant data integrity framework in pharmacometric research.
Table 3: Essential Research Reagents and Solutions for Data Integrity
| Tool/Solution | Category | Primary Function | Relevant ALCOA+ Principle(s) |
|---|---|---|---|
| Validated EDC System | Software Platform | Electronically capture clinical trial data with user authentication and timestamps [58]. | Attributable, Contemporaneous, Original |
| Laboratory Information Management System (LIMS) | Software Platform | Manage and track sample-related data (e.g., bioanalytical PK concentrations), ensuring data lineage [58]. | Attributable, Complete, Traceable |
| Audit Trail Repository | Software Feature | Automatically log all user actions, data changes, and reasons for change in a secure, reviewable file [58] [59]. | Complete, Consistent, Enduring, Traceable |
| Electronic Signature (21 CFR Part 11 Compliant) | Software Feature | Provide a legally binding signature equivalent for approvals, reviews, and data modifications [61]. | Attributable, Accurate |
| Standard Operating Procedure (SOP) on Data Governance | Document | Define roles, responsibilities, and standardized procedures for data handling, review, and archiving [61] [60]. | Consistent, Accurate, Available |
| Model Analysis Plan (MAP) | Document | Pre-specify the objectives, data sources, and methods for pharmacometric model development per ICH M15 [3]. | Consistent, Accurate, Traceable |
| Validated Data Archive | System/Service | Provide long-term, secure storage for all trial and model-related data in readable formats [58] [60]. | Enduring, Available |
The rigorous application of ALCOA+ principles is a critical enabler for the acceptance of pharmacometric models by regulatory agencies. In the context of the ICH M15 guidelines, the credibility of a model is inextricably linked to the integrity of the data upon which it is built [3]. Principles like Traceable and Complete ensure that the entire data lineage is documented, allowing for the reconstruction of the model development process, which is a core aspect of regulatory assessment [62]. As the industry moves toward greater use of artificial intelligence and machine learning in drug development, the role of ALCOA+ as a foundational framework for data quality becomes even more pronounced [64] [63]. By embedding these principles into every stage of data handling—from the initial patient measurement to the final model submission—sponsors can significantly strengthen the scientific rigor of their dose-justification strategies, thereby accelerating the development of safe and effective therapies for patients.
The efficacy and safety of a drug are fundamentally tied to its dosing regimen, a challenge that becomes exponentially complex when tailoring these regimens for specific patient subpopulations. Pharmacometric models, particularly population pharmacokinetic (PopPK) models, are indispensable tools in this endeavor, using nonlinear mixed-effects models (NLMEMs) to quantify and predict drug exposure in diverse patient groups [65] [66]. However, the predictive accuracy and regulatory acceptance of these models are critically dependent on the adequacy of the input data used for their development. A model is only as reliable as the data that informs it. The "data hurdle" refers to the multifaceted challenges in collecting, curating, and integrating data of sufficient quality, granularity, and representativeness to build models that are truly "fit-for-purpose" [65] [67]. Within the context of model validation, overcoming this hurdle is the foremost prerequisite for ensuring dose prediction accuracy, especially when the model's context of use extends to supporting regulatory decisions, such as waiving a dedicated clinical trial in an unstudied subpopulation [65].
This guide objectively compares different methodologies and data strategies employed to ensure input data adequacy, providing researchers with a framework to evaluate and improve their own approaches to subpopulation dosing.
Comparative Analysis of Data Adequacy Strategies
A robust strategy for ensuring data adequacy encompasses study design, data collection, analytical techniques, and reporting. The table below compares traditional approaches with more advanced, model-informed strategies that directly address common data hurdles.
Table 1: Comparison of Traditional vs. Advanced Data Adequacy Strategies for Subpopulation Dosing
| Strategy Component | Traditional Approach | Advanced/Model-Informed Approach | Key Advantage for Data Adequacy |
|---|---|---|---|
| Study Design & Sampling | Intensive, consecutive sampling from a limited number of subjects [67]. | Population PK Design: Sparse sampling from a large number of subjects, optimized using D-optimal design to determine the most informative sampling times [67]. | Enables feasible PK studies in vulnerable populations (e.g., neonates) by minimizing sample volume/burden per patient while maximizing information gain [67]. |
| Handling Data Sparsity | Reliance on limited data, leading to potentially ungeneralizable models for subpopulations. | Mixed-Effects Modeling: Uses the population as the unit of analysis, characterizing variability with fixed (e.g., weight, age) and random effects. Allows covariate identification (e.g., renal function) to explain variability [67]. | Quantifies and explains inter-subject variability, enabling prediction of PK parameters in individuals not directly studied, based on their covariates. |
| Subpopulation Identification | Pre-defined subgroups based on broad demographics; static analysis [68]. | Sub-population Optimization & Modeling Solution (SOMS): A data-driven, AI-powered analysis of multiple variables to identify patient subgroups with differential treatment response or safety profiles [68]. | Dynamically identifies responsive subpopulations from complex trial data, rescuing trials and optimizing dosing for groups with higher efficacy or risk [68]. |
| Data Representativeness | Single-center studies, potentially lacking diversity in key covariates [67]. | Multi-site Collaborations & Data Federation: Standardizing protocols and leveraging centralized data platforms to pool data across institutions [69] [67]. | Ensures a sufficiently broad range of covariates (age, organ function, genetics) are represented, allowing for generalized conclusions for subpopulations [65]. |
| Analytical Sensitivity | High Performance Liquid Chromatography with Ultraviolet Detection (HPLC-UV), requiring larger sample volumes (1-2 mL) [67]. | HPLC with Tandem Mass Spectrometry (HPLC-MS/MS) & Dried Blood Spot (DBS) Sampling. Enables highly sensitive measurement from very small volume samples (10-100 μL) [67]. | Makes PK studies feasible in neonates and children by adhering to the recommended maximum blood volume of 3 mL/kg [67]. |
Experimental Protocols for Model Evaluation and Data Assessment
The validation of a pharmacometric model's dose prediction is a multi-faceted process that relies on rigorous experimental and graphical protocols. The following methodologies are central to assessing whether a model and its underlying data are adequate for their intended purpose.
Protocol for Visual Predictive Check (VPC)
The VPC is a simulation-based graphical tool used to assess the model's ability to simulate data that matches the observed data, evaluating the overall model structure, parameter variability, and residual error model [66].
- Objective: To evaluate the adequacy of the model's structural and stochastic components by comparing the distribution of observed data with model-simulated data.
- Procedure:
- Using the final population model parameter estimates, simulate several hundred (e.g., 500-1000) replicate datasets under the same conditions as the original study design.
- For each replicate dataset, calculate the percentiles (e.g., 5th, 50th, and 95th) of the observed or simulated concentrations at each time point or within binned time intervals.
- Calculate the median and a confidence interval (e.g., 95% CI) for the simulated percentiles across all the replicates.
- On the same graph, overlay the corresponding percentiles calculated from the original observed data.
- Interpretation: A model is considered adequate if the observed percentiles fall within the confidence intervals of the simulated percentiles, with no systematic trends. Trends or observed percentiles consistently outside the confidence intervals suggest a model misspecification, such as an incorrect structural model or residual error model [66].
Protocol for Covariate Model Evaluation
This protocol assesses the relationship between individual model parameters (Empirical Bayes Estimates, EBEs) and patient covariates to identify unexplained relationships that should be incorporated into the model to improve subpopulation predictions [66].
- Objective: To diagnose missing covariate relationships in the model, which are critical for accurate subpopulation dosing.
- Procedure:
- Following model development, extract the EBEs for key pharmacokinetic parameters (e.g., Clearance - CL, Volume of Distribution - V).
- Create scatter plots of these EBEs against continuous covariates (e.g., body weight, age) and boxplots for categorical covariates (e.g., sex, genotype).
- Statistically, this can be supplemented by testing for correlations (e.g., Spearman's rank) or differences (e.g., t-test, ANOVA).
- Interpretation: The absence of a strong trend or statistical relationship between an EBE and a covariate supports the model's adequacy. A significant trend suggests that the covariate should be formally tested for inclusion in the model, as it explains a portion of the inter-individual variability, leading to more precise dosing recommendations for subpopulations defined by that covariate [66]. It is crucial to perform this diagnostic when the "eta-shrinkage" is low, as high shrinkage can mask these relationships [66].
Visualization of Workflows and Conceptual Frameworks
The Data Adequacy Assessment Workflow
The following diagram illustrates a logical workflow for ensuring and evaluating input data adequacy throughout the model development and validation lifecycle.
Data Adequacy Workflow
The Risk-Informed Credibility Framework for Data
This diagram maps the conceptual relationships within a risk-informed credibility framework, which provides a holistic link from the initial question to the model-informed decision, emphasizing data's role [65].
Risk-Informed Credibility Framework
The Scientist's Toolkit: Essential Research Reagents and Solutions
The experimental and modeling work described relies on a suite of specialized tools, software, and platforms. The table below details key solutions that form the modern toolkit for overcoming data hurdles in subpopulation dosing.
Table 2: Key Research Reagent Solutions for Advanced Pharmacometric Analysis
| Tool/Solution | Type | Primary Function | Role in Ensuring Data Adequacy |
|---|---|---|---|
| HPLC-MS/MS Systems [67] | Analytical Instrument | High-sensitivity measurement of drug concentrations in biological samples. | Enables accurate PK profiling from micro-volume samples (10-100 µL), crucial for studies in neonates and children where blood volume is limited [67]. |
| Dried Blood Spot (DBS) [67] | Sampling Technique | Collection of a small blood sample on filter paper via heel or finger prick. | Minimizes patient burden and simplifies sample logistics, facilitating larger and more diverse study recruitment and richer data collection [67]. |
| NONMEM / MONOLIX / Phoenix NLME [65] [66] | Software Platform | Gold-standard software for non-linear mixed effects modeling (NLMEM) and population PK/PD analysis. | Provides the computational engine for developing and evaluating complex models that quantify variability and identify subpopulation-specific covariate effects [65]. |
| DXRX - The Diagnostic Network [70] | Data Analytics Platform | A global repository of diagnostic testing data, lab mappings, and physician profiling. | Provides real-world data on biomarker testing rates and lab readiness, helping to ensure that patient recruitment for targeted therapies is feasible and representative [70]. |
| SOMS (Sub-population Optimization & Modeling Solution) [68] | AI & Analytics Software | Uses algorithms (e.g., SIDES) to perform data-driven identification of patient subgroups with differential treatment responses. | Analyzes complex trial data to "rescue" trials and identify subpopulations for whom dosing adjustments are most critical, turning failed trials into targeted successes [68]. |
The journey toward precise and safe subpopulation dosing is paved with data. Overcoming the "data hurdle" requires a conscious shift from traditional methods to a more holistic, model-informed strategy that prioritizes data adequacy from the outset. This involves implementing advanced study designs like population PK with D-optimal sampling, leveraging sensitive analytical techniques like HPLC-MS/MS, and utilizing sophisticated AI-driven tools like SOMS for subpopulation discovery. Furthermore, the credibility of the resulting models must be rigorously established through comprehensive evaluation protocols, including VPCs and covariate model diagnostics, all framed within a risk-informed perspective. By systematically adopting these compared strategies and tools, researchers and drug developers can ensure that their pharmacometric models are built on a foundation of robust, representative, and adequate data, thereby delivering on the promise of personalized medicine with accurate and reliable dose predictions for all patient subgroups.
In the modern pharmaceutical landscape, ensuring robust method development and accurate dose prediction is paramount. Within the context of validating pharmacometric models for dose prediction accuracy research, two systematic methodologies stand out: Quality-by-Design (QbD) and Design of Experiments (DoE). QbD is a holistic, systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and control, based on sound science and quality risk management [71]. In contrast, DoE is a statistical technique used to systematically investigate and analyze the relationship between process variables (factors) and the output (response) of a process [72]. While QbD provides the overarching strategic framework for building quality in from the beginning, DoE serves as a critical tactical tool within this framework to efficiently achieve process and product understanding. This guide objectively compares their roles, integration, and application in method development, particularly supporting the rigorous validation of pharmacometric models used in model-informed drug development (MIDD).
Core Concepts: QbD vs. DoE
Defining the Methodologies
Quality-by-Design (QbD) QbD is a comprehensive, proactive approach to product and process development. Its core philosophy, pioneered by Dr. Joseph M. Juran, is that quality must be designed into a product, not tested into it [71]. In pharmaceuticals, QbD involves defining a desired target product profile and then using scientific understanding and risk management to design a formulation and process that reliably delivers that profile [71] [72]. The key elements of pharmaceutical QbD include [71]:
- A Quality Target Product Profile (QTPP) that identifies the Critical Quality Attributes (CQAs) of the drug product.
- Product design and understanding including identification of Critical Material Attributes (CMAs).
- Process design and understanding including identification of Critical Process Parameters (CPPs).
- A control strategy.
- Process capability and continual improvement.
Design of Experiments (DoE) DoE is a structured statistical method for simultaneously investigating the effects of multiple factors on a process output. Instead of the traditional one-factor-at-a-time (OFAT) approach, DoE varies all relevant factors in a predetermined pattern to efficiently identify main effects, interactions, and optimal conditions [72]. Key aspects of DoE include [72]:
- Factorial designs to study the effects of multiple factors.
- Response surface methodologies to model and optimize processes.
- Identification of critical factors and their interactions that significantly impact the CQAs.
Comparative Analysis: Strategic Framework vs. Tactical Tool
Table 1: A direct comparison of QbD and DoE
| Aspect | Quality-by-Design (QbD) | Design of Experiments (DoE) |
|---|---|---|
| Core Objective | Build quality into product and process design from the outset [71] [72] | Systematically explore and optimize the relationship between input variables and outputs [72] |
| Scope | Holistic, covering the entire product lifecycle from development to commercial manufacturing [71] | Focused on specific experiments for process and product understanding [72] |
| Primary Role | A strategic, overarching development framework [72] | A statistical tool used within the QbD framework [72] |
| Key Outputs | QTPP, CQAs, CMA, CPPs, Design Space, Control Strategy [71] | Mathematical models, factor effects, interaction plots, optimized parameter settings [72] |
| Regulatory Impact | Enhances root cause analysis and post-approval change management [71] | Provides scientific evidence and data to support the defined design space and control strategy [72] |
Integration in Method Development and Validation
The QbD Workflow and the Role of DoE
A typical QbD-based method development process is sequential and iterative, with DoE playing a crucial role in specific stages. The flowchart below illustrates this integrated workflow.
Diagram 1: QbD-Driven Method Development Workflow.
As shown in Diagram 1, the process begins with defining the QTPP and identifying CQAs. A risk assessment is then conducted to link material and process parameters to the CQAs. It is at this stage that DoE is deployed to systematically generate data and build predictive models, which directly informs the establishment of a robust design space and control strategy.
The Iterative Cycle of Design of Experiments
The application of DoE itself is a structured, iterative process. The following diagram details the key stages of a DoE cycle within a QbD framework.
Diagram 2: The Iterative Cycle of Design of Experiments (DoE).
Experimental Protocols and Data Presentation
Protocol for a DoE Study in Analytical Method Validation
The following protocol outlines a generalized procedure for employing a DoE to optimize an analytical method, a critical step in building a QbD-validated pharmacometric model.
Objective: To optimize and validate a High-Performance Liquid Chromatography (HPLC) method for the quantification of a drug substance in plasma, identifying the design space for critical method parameters.
Materials:
- Analytical Standard: Drug substance of known purity.
- Internal Standard: Structurally similar analog for normalization.
- Biological Matrix: Drug-free human plasma.
- Mobile Phase Components: HPLC-grade solvents and buffers.
- Equipment: HPLC system with UV/DAD detector, analytical column, data acquisition software.
Methodology:
- Define Critical Method Attributes (CMAs - Responses): Identify the key outputs determining method quality. These typically include:
- Peak Resolution (Rs): Must be >2.0 between the analyte and closest eluting interference.
- Tailing Factor (Tf): Must be ≤2.0.
- Theoretical Plates (N): A measure of column efficiency.
Identify Critical Method Parameters (CMPs - Factors): Via risk assessment (e.g., Fishbone diagram), select factors for DoE. For an HPLC method, this often includes:
- pH of the aqueous buffer in the mobile phase.
- Percentage of Organic Solvent (e.g., %Acetonitrile) in the mobile phase.
- Column Temperature.
Select and Execute DoE: A Central Composite Design (CCD) is suitable for this response surface methodology.
- Define low and high levels for each of the three factors.
- The software-generated design will require 18-20 experimental runs, including center points to estimate curvature and pure error.
- Execute runs in a randomized order to avoid bias.
Data Analysis:
- Use multiple linear regression to fit mathematical models to each response (Rs, Tf, N).
- Perform Analysis of Variance (ANOVA) to determine the statistical significance of each factor and their interactions.
- Generate contour plots and 3D response surface plots to visualize the relationship between factors and responses.
Establish Method Design Space:
- Using the models and plots, identify the region of the operational parameter space (pH, %Organic, Temperature) where all CMA responses meet their predefined criteria.
- This region constitutes the method design space.
Verify the Model: Perform confirmation experiments at a set of conditions within the design space (not originally in the DoE) to verify the model's predictive accuracy.
Quantitative Data Presentation
The data generated from a DoE is best summarized in structured tables for objective comparison.
Table 2: Example DoE Results from an HPLC Method Optimization (ANOVA Summary)
| Factor | Effect on Resolution (p-value) | Effect on Tailing (p-value) | Effect on Plate Count (p-value) | Conclusion |
|---|---|---|---|---|
| pH | 0.85 (<0.001) | -0.22 (0.003) | 450 (0.012) | Critical, affects all responses |
| %Organic | -1.10 (<0.001) | 0.15 (0.045) | -3500 (<0.001) | Critical, strong effect on efficiency |
| Column Temp. | 0.05 (0.510) | -0.03 (0.410) | 200 (0.210) | Not a critical parameter |
| pH * %Organic | -0.35 (0.005) | 0.08 (0.080) | - | Significant interaction for resolution |
Table 3: Comparison of Method Performance: QbD/DoE vs. Traditional One-Factor-at-a-Time (OFAT) Approach
| Performance Metric | QbD/DoE Approach | Traditional OFAT Approach |
|---|---|---|
| Number of Experiments to Optimize | 20 (via CCD) | ~40-50 (estimated) |
| Understanding of Factor Interactions | Yes (e.g., pH*%Organic) | No |
| Robustness to Variation | High (established design space) | Low (single-point optimization) |
| Ease of Troubleshooting | High (based on mechanistic understanding) | Low (limited knowledge base) |
| Regulatory Flexibility | High (within design space) | Low (fixed parameters) |
Application in Pharmacometric Model Validation
The principles of QbD and DoE are directly applicable to the thesis context of validating pharmacometric models for dose prediction accuracy. Model-Informed Drug Development (MIDD) is defined as "the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [3].
In this context:
- QbD provides the framework: The model itself is the "product." The QTPP is a model with predefined accuracy for predicting human dose-exposure-response relationships. The CQAs are the model's performance metrics (e.g., prediction error, robustness).
- DoE provides the tools: Experimental and clinical data used to build and validate the model should be generated and evaluated using sound statistical principles, akin to DoE. This includes [3]:
- Planning modeling activities with a defined Question of Interest (QOI) and Context of Use (COU).
- Using a Model Analysis Plan (MAP).
- Systematically evaluating model credibility, verifying the model's technical performance, and validating its predictive power against external datasets.
For example, a PopPK model's accuracy can be validated by comparing its predictions of drug concentrations to real-world observed data [8]. A systematic, QbD-like approach to this validation, planning the comparison methodology and acceptance criteria (e.g., mean prediction error within 15%) in advance, ensures the model is fit for its intended purpose in dose prediction.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for QbD/DoE-Based Method Development
| Item / Solution | Function in Development & Validation |
|---|---|
| Certified Reference Standards | Provides the known quantity of analyte with high purity and traceability, essential for accurate calibration, determining recovery, and establishing method accuracy [71]. |
| Stable Isotope-Labeled Internal Standards | Used in bioanalytical methods (e.g., LC-MS/MS) to correct for analyte loss during sample preparation and matrix effects, significantly improving precision and accuracy. |
| Biologically Relevant Matrices | (e.g., human plasma, tissue homogenates). Critical for assessing method selectivity, matrix effects, and recovery in a realistic context, ensuring the method is suitable for its intended biological application [71]. |
| Forced Degradation Samples | Samples of the drug substance stressed under various conditions (heat, light, acid, base, oxidation). Used to demonstrate the method's stability-indicating properties and its ability to separate the analyte from potential degradation products [71]. |
| Quality Control (QC) Materials | Samples with known concentrations of the analyte (low, mid, high) in the relevant matrix. Used throughout method validation and routine application to monitor the method's performance, precision, and accuracy over time. |
| Advanced Statistical Software | Software capable of executing DoE (factorial designs, CCD), performing regression analysis, ANOVA, and generating optimization plots. This is the computational engine for data analysis and model building in a QbD framework [72]. |
Frameworks for Rigorous Model Validation and Comparative Analysis
The risk-informed credibility framework represents a paradigm shift in how regulatory agencies evaluate computational models used in drug development and medical device submissions. This systematic approach provides a structured methodology for assessing whether a model's outputs are sufficiently credible to inform regulatory decisions, from first-in-human studies to post-market surveillance. As recognized by the International Council for Harmonisation (ICH) in its M15 guidelines on Model-Informed Drug Development (MIDD), the framework aims to "align the expectations of regulators and sponsors, support consistent regulatory decisions, and minimize errors in the acceptance of modeling and simulation" [3]. The foundation of this approach lies in its risk-informed nature – the level of evidence required to establish model credibility is directly proportional to the regulatory impact of the decisions the model supports [3] [73].
The framework's origins can be traced to the ASME V&V 40-2018 standard, which provides technical requirements for evaluating verification and validation activities of computational models [3]. This standard was subsequently adapted by regulatory agencies, including the U.S. Food and Drug Administration (FDA), which published guidelines in 2023 incorporating categories of credibility evidence [3]. The European Medicines Agency (EMA) similarly emphasizes that MIDD approaches "should adhere to the highest standards and regulatory guidance especially when of high regulatory impact" [74]. This harmonized perspective ensures that model credibility assessment follows consistent principles across international regulatory bodies, providing sponsors with clear expectations for model submission requirements.
Core Components of the Credibility Framework
The risk-informed credibility framework operates on several foundational components that work in concert to provide a comprehensive assessment strategy. These elements ensure that models are evaluated consistently based on their intended use and potential impact on regulatory decisions.
Key Elements and Their Relationships
The diagram below illustrates the core components of the risk-informed credibility framework and their relationships:
Framework Component Definitions
Table 1: Core Components of the Risk-Informed Credibility Framework
| Component | Definition | Regulatory Significance |
|---|---|---|
| Context of Use (COU) | A detailed statement describing how the model will be applied and the specific decisions it will inform [3] [1] | Serves as the foundation for all subsequent credibility assessment activities |
| Question of Interest (QOI) | The specific scientific or clinical question the model aims to address [1] [14] | Determines the model's scope and boundaries |
| Model Risk Analysis | Evaluation of potential impact of incorrect model outputs on decision-making [73] [75] | Directly determines the level of evidence needed for credibility |
| Decision Consequences | Assessment of potential impact on patient safety, product efficacy, or public health [3] | Determines the risk level of the modeling application |
| Credibility Evidence | Collective body of verification, validation, and uncertainty quantification activities [73] | Provides objective basis for establishing trust in model predictions |
The framework operates hierarchically, beginning with clear definition of the COU and QOI. These definitions then inform a model risk analysis that considers the decision consequences associated with the modeling application [73]. As noted in FDA guidance on computational modeling, "an ISCT is a virtual representation of the real world that has to be shown to be credible before being relied upon to make decisions that have the potential to cause patient harm" [73]. This risk analysis directly dictates the amount and rigor of credibility evidence required, creating a proportional approach where higher-risk applications demand more extensive evidence.
Framework Comparison with Traditional Approaches
The risk-informed credibility framework differs substantially from traditional model evaluation approaches in pharmaceutical development. Where traditional methods often applied standardized checklists regardless of context, the risk-informed approach creates a flexible, adaptive evaluation structure tailored to specific regulatory needs.
Comparative Analysis of Evaluation Approaches
Table 2: Risk-Informed Framework vs. Traditional Model Evaluation
| Evaluation Aspect | Traditional Approach | Risk-Informed Credibility Framework |
|---|---|---|
| Evaluation Standardization | One-size-fits-all checklists | Risk-proportional evidence requirements |
| Regulatory Flexibility | Limited flexibility based on model type | Adapts to model complexity and decision impact |
| Validation Requirements | Fixed validation protocols regardless of impact | Tiered validation based on risk analysis |
| Documentation Standards | Standardized documentation templates | Documentation depth proportional to risk level |
| Uncertainty Handling | Often qualitative or minimal | Structured uncertainty quantification required |
| Cross-Agency Acceptance | Variable acceptance across regions | Harmonized through ICH M15 guidelines [3] |
The fundamental differentiator lies in the framework's explicit linkage between model risk and evidence requirements. As detailed in assessments of in silico clinical trials, "establishing the credibility of each ISCT submodel is challenging, but is nonetheless important because inaccurate output from a single submodel could potentially compromise the credibility of the entire ISCT" [73]. This perspective acknowledges that not all models require the same level of validation, while simultaneously recognizing that critical applications demand rigorous assessment.
The framework also introduces a more nuanced understanding of model purpose through the "fit-for-purpose" principle [1] [14]. A model is considered fit-for-purpose when it successfully defines the COU, data quality, model verification, calibration, validation, and interpretation [1]. Conversely, "oversimplification, lack of data with sufficient quality or quantity, or unjustified incorporation of complexities, might also render the model not fit-for-purpose" [1]. This represents a more sophisticated evaluation paradigm than simple accuracy metrics alone.
Implementation Workflow and Process
Implementing the risk-informed credibility framework follows a structured workflow that aligns with regulatory expectations. This process transforms theoretical framework components into actionable assessment activities.
Credibility Assessment Workflow
The following diagram illustrates the sequential workflow for implementing the risk-informed credibility framework:
Key Implementation Steps
The implementation workflow consists of several critical phases:
Definition Phase: The process begins with comprehensive definition of the COU and QOI. The ICH M15 guidelines emphasize that MIDD activities start with "planning that defines the Question of Interest (QOI), Context of Use (COU), Model Influence, Decision Consequences, Model Risk, Model Impact, Appropriateness, and Technical Criteria" [3]. This foundational stage must produce precise specifications, as all subsequent activities reference these definitions.
Risk Assessment Phase: This phase involves evaluating "Model Influence, Decision Consequences, Model Risk, Model Impact" [3]. For medical device in silico trials, this includes assessing how model inaccuracies might "potentially compromise the credibility of the entire ISCT" [73]. The risk assessment directly determines the "level of evidence required" for credibility establishment [73].
Evidence Generation Phase: This phase encompasses verification, validation, and uncertainty quantification activities. Verification ensures the model is implemented correctly, while validation confirms the model accurately represents reality [73]. Uncertainty quantification characterizes the reliability of model predictions. As demonstrated in tuberculosis treatment modeling, this includes "the definition of all the verification and validation activities and related acceptability criteria" [75].
Decision Phase: The collected evidence is evaluated against pre-specified acceptability criteria to determine whether the model achieves sufficient credibility for its intended use. This decision is documented comprehensively for regulatory review [73] [75].
Experimental Validation and Case Studies
The practical application of the risk-informed credibility framework is best illustrated through experimental validations and case studies across therapeutic areas. These examples demonstrate how the framework functions in real-world regulatory evaluations.
Pharmacogenomic Dose Prediction Validation
A 2025 study validating mathematical model-based pharmacogenomics dose prediction exemplifies framework application [8]. The research aimed to "verify the usage of mathematical modeling in predicting patients' medication doses in association with their genotypes versus real-world data" [8], with a specific focus on CYP2D6 and CYP2C19 gene polymorphisms.
Table 3: Experimental Protocol for Pharmacogenomic Model Validation
| Protocol Component | Implementation Details |
|---|---|
| Data Sources | Real-world data from 1,914 subjects across 26 studies [8] |
| Genomic Focus | CYP2D6 and CYP2C19 gene polymorphisms [8] |
| Validation Approach | Comparison of model-predicted dosing against clinically reported optimal dosing [8] |
| Key Metrics | Predictive accuracy for optimal dosing across genotype subgroups |
| Outcome Measures | Ability to circumvent trial-and-error in patient treatments [8] |
The study concluded that "the mathematical model was able to predict the reported optimal dosing of the values provided in the considered studies" [8], thus establishing credibility for this specific context of use. The researchers recommended "that researchers and healthcare professionals use simple descriptive metabolic activity terms for patients and use allele activity scores for drug dosing rather than phenotype/genotype classifications" [8], providing specific guidance for framework implementation.
AI-PBPK Model for Aldosterone Synthase Inhibitors
Another application demonstrates the framework's utility for emerging modeling approaches, specifically an artificial intelligence-physiologically based pharmacokinetic (AI-PBPK) model for aldosterone synthase inhibitors [76]. This case highlights how the framework adapts to complex, multi-component modeling strategies.
Table 4: Experimental Protocol for AI-PBPK Model Validation
| Protocol Component | Implementation Details |
|---|---|
| Model Architecture | Integration of machine learning with classical PBPK modeling [76] |
| Compound Selection | Baxdrostat (model compound), Dexfadrostat, Lorundrostat, BI689648, LCI699 [76] |
| Validation Approach | Four-step process: model construction, calibration, validation, simulation [76] |
| Data Sources | Published clinical trial data and literature sources [76] |
| Predictive Focus | PK/PD properties and selectivity index (SI) for enzyme inhibition [76] |
The researchers developed a comprehensive workflow where "the model was then calibrated by adjusting key parameters based on the comparison" [76], followed by external validation using clinical PK data. This systematic approach to credibility establishment enabled the conclusion that "the PK/PD properties of an ASI could be inferred from its structural formula within a certain error range" [76], demonstrating the framework's utility for early drug discovery.
Regulatory Applications and Impact
The risk-informed credibility framework has significant implications for regulatory evaluation processes across the product development lifecycle. Its application spans multiple domains and therapeutic areas, providing a consistent approach for assessing model-based evidence.
Pediatric Drug Development
The framework plays a particularly valuable role in pediatric drug development, where "practical and ethical limitations" constrain data collection [74]. The EMA emphasizes that MIDD approaches "can serve as the basis for dose/regimen selection, clinical trial optimisation, and extrapolation" in pediatric populations [74]. The framework enables credibility assessment for these applications through defined evaluation criteria, such as:
- Presentation of "exposure ranges predicted for the proposed doses for the subsets of the paediatric population" visualized with boxplots [74]
- Comparison of "proposed doses to the doses resulting from the underlying function" [74]
- Inclusion of "body weight relationships when describing pharmacokinetic (PK) in paediatric patients" with appropriate allometric scaling [74]
Medical Device In Silico Clinical Trials
For medical devices, the framework enables credibility assessment of in silico clinical trials (ISCTs) that "can be used to refine, reduce, or in some cases to completely replace human participants in a clinical trial" [73]. The hierarchical approach involves "systematically gathering credibility evidence for each ISCT submodel before demonstrating credibility of the full ISCT" [73]. This is particularly important because "ISCTs can integrate many different submodels that potentially use different modeling types" [73], each requiring specialized assessment strategies.
Essential Research Toolkit
Implementing the risk-informed credibility framework requires specific methodological tools and approaches. The table below outlines key "research reagent solutions" essential for conducting credibility assessments.
Table 5: Essential Research Toolkit for Credibility Assessment
| Tool/Resource | Function in Credibility Assessment | Application Context |
|---|---|---|
| ASME V&V 40-2018 Standard | Provides technical framework for risk-informed credibility assessment [3] | Foundation for regulatory evaluation across multiple agencies |
| ICH M15 Guidelines | Offers harmonized principles for Model-Informed Drug Development [3] | Global drug development applications |
| PBPK Modeling Platforms | Enable prediction of drug behavior across populations [1] [76] | Drug-drug interaction prediction, special populations |
| Population PK/PD Modeling | Characterizes variability in drug exposure and response [3] [1] | Dose selection, special population dosing |
| AI/ML Prediction Tools | Generate parameters when experimental data is limited [8] [76] | Early discovery, pharmacogenomic prediction |
| Verification & Validation Protocols | Standardized methods for model verification and validation [73] [75] | Credibility evidence generation across all domains |
| Uncertainty Quantification Methods | Characterize reliability of model predictions [73] | Risk assessment for decision-making |
This toolkit provides the methodological foundation for implementing the risk-informed credibility framework across various regulatory contexts. The selection of appropriate tools depends on the specific model type, context of use, and regulatory requirements for the submission.
The risk-informed credibility framework represents a significant advancement in regulatory science, providing a structured, transparent, and proportional approach for evaluating computational models across the therapeutic development spectrum. By linking evidence requirements to decision consequences, the framework creates an efficient yet rigorous assessment paradigm that aligns regulator and sponsor expectations. As model-informed approaches continue to expand through artificial intelligence, mechanistic modeling, and in silico trials, this framework provides the necessary foundation for establishing model credibility while maintaining flexibility for innovation. The ongoing harmonization through ICH M15 guidelines ensures consistent application across global regulatory agencies, ultimately supporting more efficient development of safe and effective medical products.
Modern drug development faces unprecedented complexity, requiring the integration of diverse scientific fields to solve challenging problems. Traditionally, statistical methods have served as the primary tool for designing and analyzing clinical trials, providing the framework for hypothesis testing and validity. Increasingly, pharmacometric approaches utilizing physiology-based drug and disease models are being applied in this context. Rather than existing in isolation, these two quantitative disciplines possess more common ground than divisive territory, and their collective synergy can generate significant advances in clinical research and development [77] [78]. This integration is transforming the landscape of model-informed drug development, leading to more efficient processes and more effective therapies for patients with medical needs.
The paradigm is shifting from a traditional, sequential statistical testing approach to a more dynamic, model-informed strategy that leverages the strengths of both disciplines. This article examines how this synergy enhances decision-making in drug development, with a specific focus on validating pharmacometric models for dose prediction accuracy. We will explore concrete examples, compare methodological approaches, and detail the experimental protocols that demonstrate how this collaboration is advancing therapeutic precision.
The Synergistic Framework: Concepts and Definitions
Core Disciplines Defined
- Pharmacometrics: A quantitative science that utilizes mathematical models based on biology, pharmacology, physiology, and disease processes to describe and quantify the interaction between drugs and patients. It employs physiologically-based pharmacokinetic (PBPK) models and pharmacodynamic (PD) models to simulate drug behavior and effects within the body.
- Statistics: The science of collecting, analyzing, interpreting, and presenting data. In drug development, it provides the principles for study design, randomization, hypothesis testing, and uncertainty quantification, ensuring robust and valid conclusions from clinical trials.
The Interface of Methodologies
The synergy emerges at the intersection of these fields. Pharmacometrics provides mechanistic models that describe the underlying biological system, while statistics provides the framework for parameter estimation, model uncertainty quantification, and design optimization. Together, they enable model-based adaptive optimal designs that can learn from accumulating data and adjust trial parameters in a statistically sound manner [77]. This collaborative approach is particularly powerful for addressing complex questions about dose-exposure-response relationships, patient variability, and optimal dosing strategies – all critical elements in the quest for personalized medicine.
Quantitative Evidence: Validating Model-Based Dose Prediction
The true test of any model lies in its predictive accuracy when confronted with real-world data. Recent research provides compelling quantitative evidence validating pharmacometric approaches for precise dose prediction.
Pharmacogenomic Dose Prediction Validation
A 2025 study conducted a direct verification of mathematical modeling for predicting optimal medication doses based on patient genetics. The research utilized real-world data from 1,914 subjects across 26 studies, focusing on polymorphisms in the CYP2D6 and CYP2C19 genes, which encode drug-metabolizing enzymes [8].
Table 1: Validation of Model-Based Pharmacogenomic Dose Prediction
| Validation Metric | Results | Clinical Implications |
|---|---|---|
| Prediction Accuracy | Mathematical model successfully predicted reported optimal dosing values from studies | Circumvents traditional trial-and-error in patient treatment |
| Data Source | Real-world data on dosing and genotypes from 1,914 subjects | Enhances generalizability of findings |
| Key Genes | CYP2D6 and CYP2C19 polymorphisms | Critical for metabolism of many commonly prescribed drugs |
| Clinical Utility | Supports better-informed decision-making in clinical settings and R&D | Facilitates personalized medicine approaches |
The study concluded that mathematical models could successfully predict reported optimal dosing, providing a robust alternative to the traditional trial-and-error approach in patient treatment [8]. This validation is particularly significant for drugs with narrow therapeutic windows, where dosing precision is critical for both efficacy and safety.
AI-Enhanced PBPK Modeling for Aldosterone Synthase Inhibitors
Further demonstrating the evolution of these approaches, a 2025 study developed an artificial intelligence-physiologically based pharmacokinetic (AI-PBPK) model to predict PK/PD properties of aldosterone synthase inhibitors (ASIs) at the drug discovery stage [76]. The model integrated machine learning with classical PBPK modeling to predict pharmacokinetic parameters and pharmacodynamic effects directly from a compound's structural formula.
The workflow involved:
- Inputting the compound's structural formula into an AI model to generate key ADME parameters
- Using these parameters in a PBPK model to predict pharmacokinetic profiles
- Developing a PD model to predict inhibition rates of target enzymes based on plasma free drug concentrations [76]
This approach demonstrated that PK/PD properties of an ASI could be inferred from its structural formula within a reasonable error range, providing a powerful tool for early compound screening and optimization before extensive laboratory testing [76].
Figure 1: Synergistic Workflow Between Statistics and Pharmacometrics
Comparative Analysis: Pharmacometrics vs. Traditional Statistics in Drug Development
To fully appreciate the synergy between pharmacometrics and statistics, it is valuable to compare their distinct but complementary roles in the drug development process.
Table 2: Comparison of Statistical vs. Pharmacometric Approaches in Drug Development
| Aspect | Traditional Statistics | Pharmacometrics | Synergistic Integration |
|---|---|---|---|
| Primary Focus | Group averages, hypothesis testing, p-values | Drug and disease system behavior, time-course | Model-informed adaptive designs with statistical rigor |
| Data Approach | Primarily empirical, data-driven | Primarily mechanistic, model-driven | Integration of mechanistic understanding with empirical validation |
| Dose Selection | Based on statistical significance between fixed doses | Based on modeling exposure-response and variability | Optimal dose selection informed by models with statistical validation |
| Patient Variability | Controlled through inclusion/exclusion criteria | Quantified and explained through covariate modeling | Prediction of individual patient responses with confidence intervals |
| Trial Design | Fixed designs with predetermined sample sizes | Model-based adaptive designs that learn from accumulating data | More efficient trials through continuous learning and adjustment |
This comparison reveals how the two disciplines address different but complementary aspects of the drug development challenge. Statistics provides the rigorous framework for inference, while pharmacometrics offers the mechanistic context for interpretation. When integrated, they enable a more comprehensive approach that leverages both empirical evidence and biological understanding [77] [79].
Experimental Protocols and Methodologies
Protocol for Validating Pharmacogenomic Dose Prediction
The validation of mathematical models for pharmacogenomic dose prediction followed a rigorous protocol [8]:
Data Collection and Curation:
- Collected real-world data on drug dosing and patient genotypes from 26 published studies
- Focused on CYP2D6 and CYP2C19 gene polymorphisms due to their established role in drug metabolism
- Standardized data across studies to ensure comparability
Model Development:
- Constructed mathematical models relating genotype to metabolic activity
- Used allele activity scores rather than traditional phenotype/genotype classifications for more precise quantification
Validation Approach:
- Compared model-predicted optimal dosing against empirically determined optimal doses from the literature
- Assessed predictive accuracy across different drug classes and patient populations
Analysis of Clinical Utility:
- Evaluated potential for circumventing trial-and-error dosing in clinical practice
- Assessed implications for drug development and personalized medicine
This protocol demonstrates the integration of statistical principles (data standardization, validation against empirical evidence) with pharmacometric approaches (mathematical modeling of genotype-phenotype relationships).
Protocol for AI-PBPK Model Development and Validation
The development of the AI-PBPK model for aldosterone synthase inhibitors followed a structured workflow [76]:
Model Construction:
- Selected Baxdrostat as the model compound due to extensive available clinical data
- Developed a web-based platform (B2O Simulator) integrating PBPK with machine learning
- Used structural formulas as input for predicting ADME parameters
Model Calibration:
- Compared initial predictions with published clinical trial data for Baxdrostat
- Adjusted key parameters to improve model accuracy
- Ensured physiological plausibility of all parameters
External Validation:
- Tested model predictions against clinical PK data for two additional ASIs (Dexfadrostat and Lorundrostat)
- Assessed predictive performance across different compound structures
Simulation and Application:
- Predicted PK profiles for five compounds (Baxdrostat, BI689648, Dexfadrostat, Lorundrostat, and LCI699)
- Developed PD models predicting inhibition of aldosterone synthase versus 11β-hydroxylase based on plasma free concentrations
- Calculated selectivity indices (ratio of IC50 toward 11β-hydroxylase to IC50 toward AS)
Figure 2: AI-PBPK Modeling Workflow for Drug Discovery
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing the synergistic approach between pharmacometrics and statistics requires specialized tools and methodologies. The following table details key resources essential for research in this field.
Table 3: Essential Research Reagents and Computational Tools
| Tool/Resource | Type | Function/Purpose | Example Applications |
|---|---|---|---|
| Population PK/PD Modeling Software | Computational Tool | Quantifies drug behavior and effects in populations, identifying sources of variability | Dose optimization for special populations, drug-drug interaction assessment |
| PBPK Platforms | Computational Tool | Simulates ADME processes using physiological parameters and drug-specific data | Prediction of first-in-human doses, formulation optimization |
| AI-PBPK Integrative Platforms | Computational Tool | Combines machine learning with PBPK modeling to predict PK from molecular structure | Early candidate screening before synthetic chemistry [76] |
| Model-Informed Precision Dosing Software | Clinical Decision Tool | Translates popPK models into clinical dose recommendations for individual patients | Bayesian forecasting for drugs with narrow therapeutic windows [80] |
| Real-World Evidence Databases | Data Resource | Provides clinical data from routine practice for model validation | Validation of pharmacogenomic dose prediction models [8] |
| Multi-Output Gaussian Process Models | Statistical Tool | Simultaneously predicts all dose-response relationships and identifies biomarkers | Biomarker discovery, drug repositioning [17] |
Applications in Precision Oncology
The synergy between pharmacometrics and statistics has shown particular promise in oncology, where narrow therapeutic windows and significant inter-individual variability make dosing particularly challenging.
Model-Informed Precision Dosing in Cancer Therapy
A 2025 review identified 16 different oncology drugs for which prospective model-informed precision dosing (MIPD) validation or implementation has been performed [80]. This approach uses population pharmacokinetic (popPK) models to inform individualized dosing decisions, with demonstrated benefits:
- Busulfan: Prospective MIPD implementation resulted in decreased rates of veno-occlusive disease (24.1% vs. 3.4%) and increased rates of engraftment after 90 days (64.0% vs. 92.9%) in pediatric patients undergoing hematopoietic stem cell transplantation [80].
- Cyclophosphamide: MIPD led to a 38% reduction in the hazard of acute kidney injury and lower post-conditioning peak total serum bilirubin [80].
- High-dose methotrexate: MIPD demonstrated improved clinical outcomes through optimized exposure [80].
The review highlighted that MIPD is particularly valuable when there is a well-established narrow therapeutic window predictive of efficacy and/or toxicity, combined with significant inter-individual variability in drug exposure [80].
Advanced Statistical Approaches for Dose-Response Prediction
Beyond traditional pharmacometric approaches, advanced statistical methods like Multi-output Gaussian Process (MOGP) models are enhancing dose-response prediction in oncology. These models simultaneously predict all dose-response relationships and uncover biomarkers by describing the relationship between genomic features, chemical properties, and every response at every dose [17].
This approach was tested across ten cancer types and demonstrated effectiveness in accurately predicting dose-responses even with limited training data. Additionally, it identified EZH2 gene mutation as a novel biomarker of BRAF inhibitor response – a finding that was not detected through traditional ANOVA analysis of IC50 values [17]. This highlights how integrated statistical and modeling approaches can uncover novel biological insights that might be missed by conventional methods.
The synergy between pharmacometrics and statistics represents a paradigm shift in drug development, moving beyond traditional statistical hypothesis testing to a more integrated, model-informed approach. The evidence demonstrates that this collaboration enhances decision-making across the development continuum – from early candidate selection to clinical dose optimization.
Validated against real-world data, pharmacometric models have demonstrated remarkable accuracy in predicting optimal dosing based on patient characteristics, including genetics [8]. When enhanced with artificial intelligence and machine learning, these models show potential to further accelerate early drug discovery [76]. In clinical practice, particularly in challenging areas like oncology, model-informed precision dosing has begun to demonstrate tangible improvements in patient outcomes [80].
As these fields continue to converge, the future of drug development will be increasingly characterized by multidisciplinary collaboration, with teams of statisticians, pharmacometricians, clinicians, and biologists working together to develop more effective medicines more efficiently. This synergy promises not only to enhance the drug development process but ultimately to deliver more personalized, effective, and safer therapies to patients in need.
Assessing the fit and predictive performance of pharmacometric models is a critical step in model-informed drug development (MIDD), directly impacting the accuracy of dose prediction and the success of drug development programs [3] [1]. This guide provides a comparative analysis of the key tools and methodologies used by scientists to evaluate model quality, grounded in experimental data and protocols.
The evaluation of pharmacometric models employs a diverse toolkit, ranging from graphical diagnostics to quantitative metrics. The table below summarizes the primary tools and their applications.
Table 1: Key Tools for Pharmacometric Model Evaluation
| Tool Category | Specific Tool | Primary Function | Key Metric/Output | What to Expect if the Model is Correct |
|---|---|---|---|---|
| Goodness-of-Fit (GOF) Diagnostics | Observations vs. Population Predictions (OBS vs PRED) [66] | Assess structural model adequacy | Scatter plot of observed data (OBS) against model predictions (PRED) | Data points are scattered around the identity line [66]. |
| Conditional Weighted Residuals (CWRES) vs. Time [66] | Detect systematic bias in structural or error models | Scatter plot of residuals against time or predictions | Data points are scattered evenly around the horizontal zero-line [66]. | |
| Individual Weighted Residuals (IWRES) vs. Individual Predictions (IPRED) [66] | Evaluate structural model and residual error at individual level | Scatter plot | Data points are scattered evenly around zero; cone-shaped pattern suggests error model misspecification [66]. | |
| Predictive Performance & Simulation | Visual Predictive Check (VPC) [66] | Evaluate model's ability to simulate new data matching observations | Graph comparing percentiles of observed data with prediction intervals from simulated data | Observed percentiles are not systematically different from predicted percentiles and lie within confidence intervals [66]. |
| Normalized Prediction Distribution Errors (NPDE) [66] | Quantify discrepancies between model predictions and observations | Distribution of NPDE vs. time or predictions; should be normally distributed | NPDE are scattered evenly around zero; most values lie within (-1.96, 1.96) [66]. | |
| Posterior Predictive Check [81] | Bayesian method for model evaluation | Comparison of observed data statistics with posterior predictive distribution | - | |
| Parameter Identifiability | Sensitivity Matrix Method (SMM) [82] | Assess local parameter identifiability a priori | Skewing angle; Minimal Parameter Relation (MPR) | A skewing angle of 0 indicates formal unidentifiability; values near 1 indicate better identifiability [82]. |
| Fisher Information Matrix Method (FIMM) [82] [83] | Assess parameter identifiability and inform optimal design | Expected Fisher Information Matrix (FIM) | A non-singular FIM suggests local identifiability; used for calculating parameter standard errors [83]. | |
| Robustness & Uncertainty | Bootstrap [84] | Evaluate parameter uncertainty and model stability | Distributions of parameter estimates from resampled datasets | Used to calculate confidence intervals and assess covariate selection stability [84]. |
| Log-Likelihood Profiling (LLP) [84] | Calculate confidence intervals for parameters without normality assumptions | Profile of -2 log-likelihood vs. parameter value | Confidence interval limits are where the log-likelihood is 3.84 units higher than at the maximum estimate [84]. | |
| Case-deletion Diagnostics (CDD) [84] | Identify influential individuals/observations | Cook's score, Covariance ratio | Identifies subjects with the greatest impact on parameter estimates [84]. |
Experimental Protocols for Key Evaluation Methods
Implementing these tools requires standardized methodologies. Below are detailed protocols for three critical experimental approaches.
Protocol for Visual Predictive Check (VPC)
The VPC is a simulation-based tool that visually compares the distribution of observed data with model-based simulations [66].
Methodology:
- Simulation: Using the final model and its parameter estimates, simulate a large number (e.g., 1000) of replicate datasets matching the structure of the original dataset (same subjects, dosing, and sampling times).
- Calculation of Percentiles: For each time point (or prediction bin), calculate the median and specific percentiles (e.g., 5th, 50th, and 95th) of both the observed data and the simulated data.
- Calculation of Confidence Intervals: Calculate the confidence intervals (e.g., 95%) around the simulated percentiles to account for simulation uncertainty.
- Visualization: Create a graph where the x-axis is time (or the independent variable). Overlay the following:
- The observed data percentiles (e.g., as points or a solid line).
- The simulated data percentiles (e.g., as a solid line).
- The confidence intervals around the simulated percentiles (e.g., as shaded areas).
Interpretation: A model is considered adequate if the observed percentiles generally fall within the confidence intervals of the corresponding simulated percentiles. Systematic deviations outside the intervals suggest model misspecification [66].
Protocol for Parameter Identifiability Analysis using Sensitivity Matrix
This analysis determines if model parameters can be uniquely estimated from the available data and study design [82].
Methodology:
- Input Definition: Define the model (as a set of differential equations), nominal parameter values, and the study design (dosing, observation times).
- Sensitivity Matrix Calculation: Compute the sensitivity matrix ( S ), where each element ( S{ij} = \frac{dyi}{dp_j} ) represents the sensitivity of the i-th model output (prediction) to the j-th parameter.
- Continuous Indicator Calculation:
- Skewing Angle (( \alpha )): Calculate this metric based on the determinant and column norms of ( S^T S ). The formula is: ( \alpha = \sqrt[k]{\frac{\det(S^T S)}{\prod{i=1}^k \|si\|^22}} ) where ( k ) is the number of parameters and ( si ) is the i-th column of ( S ) [82].
- Interpretation: A value of ( \alpha = 0 ) indicates the model is formally unidentifiable. Values closer to 1 indicate stronger identifiability.
- Identification of Unidentifiable Directions: Perform singular value decomposition on the sensitivity matrix to identify the linear combinations of parameters that are least informed by the data [82].
Protocol for Robust Handling of Outliers and Censored Data
This protocol uses full Bayesian inference with robust error models to manage data irregularities [85].
Methodology:
- Model Specification:
- Parameter Estimation: Employ full Bayesian inference (e.g., Markov Chain Monte Carlo) to estimate the posterior distribution of parameters. This does not rely on asymptotic approximations and provides a full characterization of uncertainty [85].
- Performance Assessment: In a simulation study, compare the performance of this approach (Student's t + M3) against traditional methods (Normal + M1 omission) by assessing the bias and precision of the resulting parameter estimates [85].
The Scientist's Toolkit: Essential Research Reagents and Software
The following tools are fundamental for conducting the experiments and analyses described above.
Table 2: Essential Research Reagent Solutions for Model Evaluation
| Tool Name | Type | Primary Function |
|---|---|---|
| NONMEM [85] [84] | Software | The industry-standard software for nonlinear mixed-effects modeling, used for parameter estimation and simulation. |
| Perl-speaks-NONMEM (PsN) Toolkit [84] | Software Suite | A collection of computer-intensive statistical methods for NONMEM, automating tasks like bootstrapping, VPC, and case-deletion diagnostics. |
| R Project | Software | A statistical programming environment widely used for data processing, plotting evaluation graphics (e.g., VPC, NPDE plots), and custom analysis [66]. |
| Monolix | Software | An integrated modeling and simulation platform for nonlinear mixed-effects models, providing advanced diagnostics and graphical outputs [66]. |
| Fisher Information Matrix (FIM) [82] [83] | Mathematical Object | Used in optimal design to predict the precision of parameter estimates before data collection; the inverse of the FIM approximates the parameter variance-covariance matrix. |
Workflow for Comprehensive Model Evaluation
A robust model evaluation strategy integrates multiple tools in a logical sequence. The diagram below outlines a recommended workflow.
Model Evaluation Workflow for Dose Prediction Accuracy
This workflow begins with an a priori Parameter Identifiability Analysis to ensure the model structure and design can support parameter estimation [82]. Following model fitting, Goodness-of-Fit Diagnostics are used to check for systematic bias [66]. If these are failed, the model must be refined. Predictive performance is then tested using Visual Predictive Checks (VPC) and related methods [66]. Finally, Robustness & Uncertainty analyses quantify the reliability of parameter estimates [84]. A model successfully completing these stages can be considered qualified for informing dose predictions.
Model-Informed Drug Development (MIDD) is a transformative framework that leverages quantitative modeling and simulation to integrate nonclinical and clinical data, informing critical decisions in drug development and regulatory evaluation [3]. As defined by the emerging International Council for Harmonisation (ICH) M15 guidelines, MIDD encompasses the "strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [3]. At the heart of this framework lies pharmacometrics, which applies mathematical models to characterize and predict drug pharmacokinetics (PK) and pharmacodynamics (PD). The credibility of these models hinges on rigorous validation against real-world clinical outcomes, ensuring their accuracy for dose prediction and therapy optimization [3] [86].
This guide objectively compares the performance of pharmacometric modeling approaches against conventional statistical methods, providing supporting experimental data to illustrate their transformative potential in modern drug development.
Comparative Performance: Pharmacometric vs. Conventional Approaches
Pharmacometric models demonstrate superior efficiency and statistical power compared to conventional analysis methods, particularly in early-phase clinical trials. The tables below summarize quantitative comparisons from simulated proof-of-concept (POC) trials.
Table 1: Sample Size Comparison for Proof-of-Concept Trials (80% Power)
| Therapeutic Area | Trial Design | Conventional Analysis | Pharmacometric Analysis | Fold Reduction |
|---|---|---|---|---|
| Acute Stroke [87] | Placebo vs. Active Dose | 388 patients | 90 patients | 4.3 |
| Type 2 Diabetes [87] | Placebo vs. Active Dose | 84 patients | 10 patients | 8.4 |
| Acute Stroke [87] | Dose-Ranging (4 arms) | 776 patients | 184 patients | 4.2 |
| Type 2 Diabetes [87] | Dose-Ranging (4 arms) | 168 patients | 12 patients | 14.0 |
Table 2: Key Advantages of Pharmacometric Modeling
| Feature | Conventional Analysis (e.g., t-test) | Pharmacometric Model-Based Analysis |
|---|---|---|
| Data Utilization | Often uses only endpoint data, discarding longitudinal information [87] | Uses all available data (repeated measurements, multiple endpoints) [87] |
| Dose-Response Insight | Limited; difficult to interpolate between treatment arms [87] | Characterizes full exposure-response relationship, enabling extrapolation [87] |
| Mechanistic Interpretation | Statistical inference only [87] | Parameters often relate to biological processes (e.g., clearance, volume) [88] |
| Trial Design Flexibility | Limited to pre-specified comparisons [87] | Enables clinical trial simulations for optimizing future study designs [87] |
The dramatic reduction in required sample size, as shown in Table 1, stems from the model's ability to leverage all longitudinal data and characterize the underlying biological system, rather than relying on a single, static endpoint comparison [87]. This efficiency is crucial in therapeutic areas like acute stroke and rare diseases, where patient recruitment is challenging [3].
Experimental Protocols for Model Validation
Workflow for Integrated Model Validation
The following diagram illustrates a robust workflow for developing and validating pharmacometric models against real-world outcomes, integrating principles from the ICH M15 guidelines [3] and modern diagnostic practices [66].
Model Validation Workflow
Protocol 1: Proof-of-Concept Trial Simulation
Objective: To compare the statistical power of a pharmacometric model-based analysis versus a conventional t-test for detecting a defined drug effect [87].
- Therapeutic Areas: Acute Stroke and Type 2 Diabetes.
- Model Structure:
- Methodology:
- Data Simulation: Use previously developed and qualified pharmacometric models to simulate clinical trial data under predefined drug effect scenarios.
- Analysis Comparison:
- Conventional: Apply a two-sided t-test to the change from baseline to study endpoint (e.g., day 90 for stroke).
- Pharmacometric: Use a likelihood ratio test (LRT) within the nonlinear mixed-effects modeling framework, utilizing all longitudinal data points.
- Power Calculation: Perform repeated simulations and analyses (e.g., using Monte-Carlo Mapped Power) across a range of sample sizes to construct power curves [87].
- Key Output: The sample size required for each method to achieve 80% statistical power.
Protocol 2: Integrated Real-World Evidence Validation
Objective: To prospectively validate a model's predictive performance by comparing its simulations with real-world clinical outcomes [86].
- Application Example: Predicting bleeding risk for generic direct-acting oral anticoagulants (DOACs) like dabigatran and apixaban [86].
- Methodology:
- Model Development: Integrate Physiologically-Based Pharmacokinetic (PBPK) absorption models with Population PK/Pharmacodynamic (PD) models.
- Simulation: Use the integrated model to simulate clinical outcomes (e.g., bleeding event rates) for soon-to-be-marketed generic products under real-world usage conditions.
- Real-World Data Collection: Conduct pharmacoepidemiologic analyses using healthcare databases to observe actual comparative event rates post-market.
- Comparison: Statistically compare the model-predicted outcomes with the real-world observed outcomes.
- Iterative Learning: Use discrepancies to refine and improve the mechanistic model, enhancing its biological plausibility and predictive capability [86].
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Tools for Pharmacometric Model Development and Validation
| Tool Category | Specific Examples | Function & Application |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software [88] | NONMEM, Monolix, R (nlmixr), Phoenix NLME | Industry-standard platforms for estimating population PK/PD parameters and their variability. |
| Model Diagnostic Tools [66] | Conditional Weighted Residuals (CWRES), Normalized Prediction Distribution Errors (NPDE), Visual Predictive Check (VPC) | Graphical and numerical methods for evaluating model goodness-of-fit and identifying misspecifications. |
| Data Management & Visualization | R, Python (pandas, Matplotlib) | Critical for data cleaning, exploratory analysis, and creating publication-quality diagnostic plots [66]. |
| Credibility Assessment Framework [3] | ASME 40-2018 Standard | Provides a structured process for evaluating model verification and validation activities, as referenced in ICH M15. |
| Real-World Data Platforms [86] | Electronic Health Records (EHR), Insurance Claims Databases | Enable external validation of model predictions against observed clinical outcomes in diverse populations. |
Visualizing the Integration of Modeling and Real-World Evidence
The synergy between M&S and real-world evidence creates a powerful, iterative cycle for validating and refining pharmacometric models, as shown in the following workflow.
M&S and RWE Integration
This integrated approach combines the internal validity of mechanistic models with the external validity of real-world evidence, creating a robust framework for demonstrating model accuracy and informing regulatory and clinical decision-making [86].
The accuracy of dose prediction is a critical determinant of success in drug development, directly impacting both therapeutic efficacy and patient safety. Traditional pharmacometric models, while foundational, often struggle with the complexity and variability of human physiology. The emergence of Artificial Intelligence (AI) and Digital Twin technologies represents a paradigm shift in model validation, moving from static, population-average predictions to dynamic, individualized forecasting. AI models excel at identifying complex, non-linear patterns from large datasets, while digital twins—virtual replicas of physiological systems—provide a mechanistic framework for simulating drug behavior in silico. This review objectively compares the performance of these innovative approaches against traditional methods, focusing on their application in pharmacometric models for dose prediction accuracy. As regulatory agencies like the FDA begin to accept alternative methods, understanding the capabilities and limitations of these technologies becomes imperative for researchers, scientists, and drug development professionals [89].
Artificial Intelligence and Machine Learning Models
AI in pharmacometrics primarily utilizes machine learning (ML) algorithms to learn patterns from historical data and predict pharmacokinetic (PK) parameters such as absorption, distribution, metabolism, and excretion (ADME). These models fall into several categories:
- Supervised Learning Algorithms: Including regression models (linear, lasso, ridge), tree-based methods (Random Forests, XGBoost), support vector machines, and neural networks. These are used when both input and output data are known, making them suitable for predicting plasma concentrations based on patient characteristics and dosage [90].
- Deep Learning Models: Including convolutional neural networks (CNNs) and recurrent neural networks (RNNs), which handle large, complex datasets and capture intricate relationships between molecular structures and their PK properties [91].
- Ensemble Methods: Such as Stacking Ensembles, which combine multiple models to improve prediction accuracy and robustness [92].
These AI techniques are particularly valuable for their speed, efficiency in handling large datasets, and ability to identify complex relationships that might be missed by traditional approaches [90].
Digital Twin Technologies (PBPK Modeling)
Physiologically Based Pharmacokinetic (PBPK) modeling serves as the foundation for digital twins in pharmacology. These are mechanistic models that simulate drug disposition by incorporating:
- Physiological Parameters: Organ sizes, blood flow rates, and tissue compositions.
- Drug-Specific Properties: Solubility, permeability, and binding characteristics.
- Patient-Specific Factors: Age, organ function, genetics, and disease states.
Unlike purely data-driven AI models, PBPK models are built on established biological mechanisms, facilitating mechanistic understanding, biological interpretability, and the ability to conduct in silico experiments through model simulations [90]. The "digital twin" concept extends PBPK models to create virtual patient replicas that can be used to predict individual responses to medications, optimizing personalized dosing strategies.
The Validation Workflow
The integration of AI and digital twins follows a systematic validation workflow to ensure predictive accuracy and reliability:
Figure 1: Integrated AI-Digital Twin Validation Workflow
Performance Comparison: Quantitative Analysis of Predictive Accuracy
Table 1: Comparative Performance of Dose Prediction Technologies
| Technology Category | Specific Model/Approach | Prediction Accuracy (R²) | Mean Absolute Error (MAE) | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| AI/ML Models | Stacking Ensemble | 0.92 [92] | 0.062 [92] | Handles complex nonlinear relationships; rapid predictions | Limited mechanistic interpretability |
| Graph Neural Networks (GNN) | 0.90 [92] | Not specified | Captures molecular structure-property relationships | Requires substantial computational resources | |
| Transformer Models | 0.89 [92] | Not specified | Excellent with sequential data | High parameter complexity | |
| XGBoost | 0.85-0.89 [90] | Varies by application | Handles missing data well; robust to outliers | Limited extrapolation capability | |
| Neural Networks | 0.84-0.88 [90] | Varies by application | High representation flexibility | Prone to overfitting without regularization | |
| Digital Twin | PBPK Modeling | 0.80-0.87 [93] | Varies by application | Strong mechanistic interpretability | Requires extensive compound-specific data |
| Traditional Methods | Population PK (PopPK) | 0.75-0.82 [90] | Varies by application | Regulatory familiarity; well-established | Limited handling of complex covariates |
| IVIVE | 0.70-0.79 [93] | Varies by application | Based on in vitro-in vivo correlation | Limited accuracy for high-binding drugs |
Antibiotic Dose Prediction Performance
Table 2: Performance in Antibiotic Therapeutic Drug Monitoring
| Antibiotic | AI/ML Model Used | Comparative Traditional Method | Performance Advantage | Study Details |
|---|---|---|---|---|
| Vancomycin | XGBoost [90] | Population PK Models | Improved accuracy in AUC prediction | 7 studies; particularly beneficial for critical care patients |
| Neural Networks [90] | Population PK Models | Better handling of nonlinear kinetics | Larger datasets (>1000 patients) showed greatest benefit | |
| Aminoglycosides | Ensemble Methods [90] | Therapeutic Drug Monitoring | Reduced prediction error for trough concentrations | Particularly valuable in pediatric populations |
| Beta-lactams | Multiple Algorithms [90] | Population PK Models | More accurate in critically ill patients | Improved prediction in rapidly changing renal function |
| Rifampicin | Custom ML Algorithm [90] | Population PK Models | Comparable accuracy with less data requirement | Potential for resource-limited settings |
Experimental Protocols and Methodologies
AI Model Development and Validation Protocol
The development and validation of AI models for pharmacometric applications follow a rigorous, multi-stage process:
Data Curation and Preprocessing
- Collect retrospective patient data including demographic information, laboratory values, dosing history, and drug concentrations [90].
- Handle missing data using appropriate imputation techniques (e.g., multivariate imputation by chained equations).
- Split data into training (60-80%), validation (10-20%), and test sets (10-20%) using stratified sampling to maintain distribution of key covariates [94].
Feature Engineering and Selection
- Extract relevant features including patient demographics, clinical characteristics, genetic markers, and concomitant medications.
- Apply domain knowledge to create meaningful derived features (e.g., renal function estimates, liver function indices).
- Use techniques like recursive feature elimination or SHAP analysis to identify the most predictive features [91].
Model Training with Cross-Validation
Model Validation and Testing
- Evaluate final model performance on held-out test set using metrics including R², MAE, root mean square error (RMSE), precision, and recall [91].
- Assess fairness and bias across different demographic subgroups [91].
- Perform external validation when possible using data from different institutions or patient populations.
Digital Twin (PBPK) Development Protocol
The development of PBPK-based digital twins follows a mechanistic, physiology-focused approach:
System Parameters Specification
- Define physiological parameters including organ weights, blood flows, and tissue compositions based on literature values for specific populations [93].
- Incorporate age-dependent changes in physiology for pediatric or geriatric applications.
- Account for disease-specific pathophysiological changes when modeling special populations.
Drug Parameters Estimation
Model Verification and Validation
- Verify model coding and structure by comparing simulations with known physiological principles.
- Validate model performance against clinical data from early-phase trials.
- Evaluate predictive performance using goodness-of-fit plots, prediction-corrected visual predictive checks, and other pharmacometric diagnostics.
Integrated AI-Digital Twin Protocol
The most advanced approaches combine AI with digital twin technologies:
Figure 2: AI-Enhanced Digital Twin Development Protocol
Research Reagent Solutions: Essential Tools for Model Validation
Computational and Software Tools
Table 3: Essential Research Tools for AI and Digital Twin Validation
| Tool Category | Specific Tool/Platform | Primary Function | Application in Validation |
|---|---|---|---|
| AI Testing Frameworks | RAGAS [95] | Evaluation of LLM predictions | Assesses faithfulness, answer correctness, and relevance of AI-generated insights |
| MLflow [95] | Experiment tracking and model management | Logs model predictions, parameters, and metrics across versions | |
| Pytest [95] | Functional testing framework | Validates model responses against expected outputs | |
| SHAP/LIME [91] | Model interpretability | Provides explanations for model predictions, enhancing trustworthiness | |
| Model Development Platforms | GastroPlus [93] | PBPK modeling and simulation | Predicts human PK parameters using IVIVE and mechanistic modeling |
| Transformer Libraries [91] | Deep learning model implementation | Builds and trains advanced neural network architectures | |
| XGBoost [90] | Gradient boosting framework | Implements tree-based ensemble models for structured data | |
| Data Management Tools | Great Expectations [91] | Data validation and profiling | Ensures data quality and consistency during model training |
| k-fold Cross-Validation [94] | Data resampling method | Reduces overfitting and provides robust performance estimates |
- Bioactive Compound Databases: Curated databases like ChEMBL (containing over 10,000 bioactive compounds) provide essential training data for AI models predicting PK parameters [92].
- In Vitro Assay Systems: Caco-2 cells for permeability assessment, human liver microsomes, and hepatocytes for metabolic stability provide critical input parameters for both PBPK models and AI algorithms [93].
- Clinical Data Repositories: Electronic health records, therapeutic drug monitoring databases, and clinical trial data serve as the foundation for training and validating data-driven models [90].
The comprehensive comparison of AI and digital twin technologies for pharmacometric model validation reveals a complementary relationship rather than a competitive one. AI models demonstrate superior predictive accuracy for complex, nonlinear relationships within large datasets, with Stacking Ensemble methods achieving remarkable R² values of 0.92 [92]. Meanwhile, digital twin approaches (PBPK modeling) provide crucial mechanistic understanding and biological interpretability that pure data-driven approaches lack [90].
For researchers and drug development professionals, the strategic integration of both technologies offers the most promising path forward. AI can enhance digital twins by optimizing parameters and identifying previously unrecognized covariates, while digital twins can ground AI predictions in physiological reality, ensuring clinically relevant outputs. This synergistic approach aligns with the FDA's evolving perspective on alternative methods, which emphasizes a "complementary enhancement" model where new approach methodologies augment rather than entirely replace established techniques [89].
As these technologies continue to evolve, their role in dose prediction accuracy will expand, potentially transforming drug development from an experience-driven to a data-driven enterprise. The validation frameworks, performance metrics, and experimental protocols outlined in this review provide a foundation for researchers to critically evaluate and implement these powerful technologies in their pharmacometric workflow.
Conclusion
The rigorous validation of pharmacometric models is fundamental to their credibility and utility in predicting accurate, individualized drug doses. As demonstrated, a successful validation strategy integrates foundational principles, robust methodological application, proactive troubleshooting, and a comprehensive evaluation using modern frameworks. The synergy between pharmacometrics and statistics, coupled with the adoption of risk-informed credibility assessments, provides a powerful approach for regulatory acceptance and clinical implementation. Future directions will be shaped by the increased integration of artificial intelligence, the use of real-world evidence for continuous model refinement, and the application of these models to support the development of personalized medicines and complex therapies. Embracing these advancements will ensure that pharmacometric models continue to enhance drug development efficiency and improve patient outcomes through precise and safe dosing strategies.
References
- 1. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 2. Applications of pharmacometrics in drug development [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24003259]
- 3. Scoping review of the role of pharmacometrics in model- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528282/]
- 4. Scoping review of the role of pharmacometrics in model ... [https://link.springer.com/article/10.1007/s10928-025-10005-8]
- 5. Model-guided development of pharmacokinetic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1476158/full]
- 6. Clinical Pharmacokinetics [https://link.springer.com/article/10.1007/s40262-025-01540-1]
- 7. CTTI Recommendations: Disease Progression Modeling [https://ctti-clinicaltrials.org/about/ctti-projects/disease-progression-modeling/ctti-recommendations-disease-progression-modeling/]
- 8. Validating the accuracy of mathematical model-based ... [https://pubmed.ncbi.nlm.nih.gov/39832006/]
- 9. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 10. Perspective on model‐informed drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8520742/]
- 11. Good Practices in Model‐Informed Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4809625/]
- 12. Impact of Model‐Informed Drug Development on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272314/]
- 13. Validating the accuracy of mathematical model–based ... [https://www.semanticscholar.org/paper/Validating-the-accuracy-of-mathematical-model-based-Saab-Nakad/3e5b891ead68d996977c3b5eb49e8908e9d0e185]
- 14. Advancing drug development with “Fit-for-Purpose” ... [https://link.springer.com/article/10.1007/s10928-025-09995-2]
- 15. Essentials of Model-informed Drug Development in Oncology [https://www.certara.com/blog/essentials-of-model-informed-drug-development-midd-top-down-vs-bottom-up-approaches/]
- 16. Building Hybrid Pharmacometric-Machine Learning ... [https://pubmed.ncbi.nlm.nih.gov/41104621/]
- 17. Multi-output prediction of dose–response curves enables ... [https://www.nature.com/articles/s41698-024-00691-x]
- 18. Nonlinear mixed-effects models for modeling in vitro drug ... [https://www.nature.com/articles/s41598-019-50936-0]
- 19. Nonlinear Mixed‐Effects Model Development and Simulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6765694/]
- 20. Nonlinear mixed-effects models for pharmacokinetic data ... [https://pubmed.ncbi.nlm.nih.gov/28194555/]
- 21. Applying exposure-response analysis to enhance ... [https://www.sciencedirect.com/science/article/pii/S0928098725001459]
- 22. Integrated modeling of biomarkers, survival and safety in ... [https://www.sciencedirect.com/science/article/pii/S0169409X24002989]
- 23. Nonlinear Mixed-Effects Modeling of Population ... [https://www.mathworks.com/company/technical-articles/nonlinear-mixed-effects-modeling-of-population-pharmacokinetics-data.html]
- 24. Pharmacometric Generative Stochastic Modeling of Patient ... [https://www.medrxiv.org/content/10.1101/2025.03.12.25323869v1.full-text]
- 25. How to use real-world clinicogenomic data to fuel drug ... [https://cotahealthcare.com/news/tech-developments/how-to-use-real-world-clinicogenomic-data-to-fuel-drug-development-2/]
- 26. Polygenic and pharmacogenomic contributions to medication ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06782-y]
- 27. a reality for future health care | The Pharmacogenomics ... [https://www.nature.com/articles/s41397-024-00326-1]
- 28. Real-World Impact of a Pharmacogenomics-Enriched ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8949247/]
- 29. Real‐World Utilization of Medications With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836345/]
- 30. An Assessment of Real-World Evidence and Other Sources ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12194790/]
- 31. An Assessment of Real-World Evidence and Other Sources ... [https://www.mdpi.com/2075-4426/15/6/232]
- 32. A retrospective study: establishment and validation of the ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1600936/full]
- 33. Development and externally validated prediction model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11983488/]
- 34. Deep learning-based prediction of individualized Real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079934/]
- 35. Comparison of different methods for predicting customized ... [https://www.sciencedirect.com/science/article/abs/pii/S0098135414002257]
- 36. Predicting the FSH threshold dose in women with WHO Group ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2387217/]
- 37. Comparison of different stimulation protocols used in in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4486909/]
- 38. Effective Visualizations Using “vachette” to Assess and ... [https://link.springer.com/article/10.1208/s12248-025-01131-9]
- 39. Effective Visualizations Using “vachette” to Assess and ... [https://www.certara.com/publication/effective-visualizations-using-vachette-to-assess-and-communicate-pharmacometric-model-results/]
- 40. New Visualization Method for Pharmacometric Modeling ... [https://www.linkedin.com/posts/certara_%F0%9D%97%95%F0%9D%97%BF%F0%9D%97%B6%F0%9D%97%B1%F0%9D%97%B4%F0%9D%97%B6%F0%9D%97%BB%F0%9D%97%B4-%F0%9D%98%81%F0%9D%97%B5%F0%9D%97%B2-%F0%9D%97%96%F0%9D%97%BC%F0%9D%97%BA%F0%9D%97%BA%F0%9D%98%82%F0%9D%97%BB%F0%9D%97%B6%F0%9D%97%B0%F0%9D%97%AE%F0%9D%98%81%F0%9D%97%B6%F0%9D%97%BC%F0%9D%97%BB-activity-7384664600757055488-kEyC]
- 41. Help for package vachette [https://cran.r-project.org/web/packages/vachette/refman/vachette.html]
- 42. Continued process verification [https://en.wikipedia.org/wiki/Continued_process_verification]
- 43. Enhance Continuous Manufacturing with Digital CPV ... [https://www.valgenesis.com/blog/enhancing-continuous-manufacturing-with-digital-cpv-integration]
- 44. The Path Toward Digital CPV: Why and How to Take It [https://www.fiercepharma.com/sponsored/path-toward-digital-cpv-why-and-how-take-it]
- 45. How Mareana CPV Prepares Your Pharma Team for ... [https://mareana.com/blog/prepare-pharma-teams-future-challenges-mareana-connect-cpv/]
- 46. How To Integrate Continued Process Verification Annual ... [https://www.outsourcedpharma.com/doc/how-to-integrate-continued-process-verification-annual-product-review-for-biologics-0001]
- 47. The clinical utility of pharmacometric models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6005593/]
- 48. The importance of Continued Process Verification [https://www.koerber-pharma.com/en/blog/successfully-managing-your-bioprocess-the-importance-of-continued-process-verification]
- 49. A guide to integrating continued process verification and ... [https://www.biophorum.com/download/continued-process-verification-cpv-a-guide-to-integrating-continued-process-verification-cpv-and-annual-product-review-apr/]
- 50. Comparative Analysis of Traditional and Pharmacometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724784/]
- 51. Understanding and applying pharmacometric modelling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5237699/]
- 52. Impact of model misspecification on model-based tests in ... [https://link.springer.com/article/10.1007/s10928-022-09821-z]
- 53. 10 Common Data Quality Issues (And How to Solve Them) [https://firsteigen.com/blog/10-common-data-quality-issues-and-how-to-solve-them/]
- 54. 14 Most Common Data Quality Issues and How to Fix Them [https://lakefs.io/data-quality/data-quality-issues/]
- 55. Data Quality Problems? 8 Ways to Fix Them in 2025 [https://atlan.com/data-quality-problems/]
- 56. A comprehensive regulatory and industry review of modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10169901/]
- 57. Tutorial on model selection and validation of model input into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725261/]
- 58. The ALCOA++ Principles for Data Integrity in Clinical Trials [https://www.quanticate.com/blog/alcoa-principles]
- 59. Alcoa Validation Data | NNIT [https://www.nnit.com/insights/articles/alcoa-validation-data]
- 60. ALCOA+ Principles & Data Integrity In Pharma [https://apotechconsulting.com/alcoa-principles-data-integrity/]
- 61. ALCOA, ALCOA+ and ALCOA++ Principles | Ensuring Data ... [https://www.pharmaguideline.com/2018/12/alcoa-to-alcoa-plus-for-data-integrity.html]
- 62. Dynamic Data Integrity: Why Alcoa Keeps Evolving [https://ispe.org/pharmaceutical-engineering/ispeak/dynamic-data-integrity-why-alcoa-keeps-evolving]
- 63. SCDM 2025 Regulatory Town Hall: Aligning Global ... [https://clinicalresearch.io/blog/scdm-2025-regulatory-town-hall-aligning-global-standards-for-ich-e6r3-and-artificial-intelligence/]
- 64. Artificial Intelligence in Pharmaceutical Technology and Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10385763/]
- 65. Scientific and regulatory evaluation of empirical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8592505/]
- 66. Model Evaluation of Continuous Data Pharmacometric Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC5321813/]
- 67. Barriers and Challenges in Performing Pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7151681/]
- 68. Solving Clinical Trial Challenges Through Sub-Population ... [https://drug-dev.com/clinical-trials-solving-clinical-trial-challenges-through-sub-population-optimization-modeling-solution/]
- 69. Conquering Data Management Challenges in the Pharma ... [https://hitconsultant.net/2024/10/14/best-practices-for-conquering-data-management-challenges-in-the-pharma-industry/]
- 70. The Data Pharma Needs to Overcome Testing Hurdles in ... [https://www.diaceutics.com/articles/nov-30-blog-on-data-pharma-benes]
- 71. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 72. Quality by Design (QbD) vs. Design of Experiments (DoE) ... [https://www.linkedin.com/pulse/understanding-difference-quality-design-qbd-vs-doe-basavaraju-phd]
- 73. Toward trustworthy medical device in silico clinical trials [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1433372/full]
- 74. Modelling and simulation: questions and answers [https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/modelling-simulation-questions-answers]
- 75. A Credibility Assessment Plan for an In Silico Model that ... [https://link.springer.com/article/10.1007/s10439-022-03078-w]
- 76. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 77. Pharmacometrics meets statistics-A synergy for modern drug ... [https://pubmed.ncbi.nlm.nih.gov/34318621/]
- 78. Pharmacometrics meets statistics—A synergy for modern ... [https://researchoutput.ncku.edu.tw/en/publications/pharmacometrics-meets-statisticsa-synergy-for-modern-drug-develop]
- 79. Practical Perspectives on Enhancing Predictive Modeling ... [https://link.springer.com/article/10.1007/s40495-025-00426-x]
- 80. Model-Informed Dose Optimization in Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946950/]
- 81. Model Evaluation of Continuous Data Pharmacometric ... [https://www.semanticscholar.org/paper/Model-Evaluation-of-Continuous-Data-Pharmacometric-Nguyen-Mouksassi/4b84d6579f2edee4afad4443d267791ff875f2ed]
- 82. Two new user‐friendly methods to assess pharmacometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11247123/]
- 83. Pharmacometric estimation methods for aggregate data ... [https://link.springer.com/article/10.1007/s10928-021-09760-1]
- 84. PsN-Toolkit—A collection of computer intensive statistical ... [https://www.sciencedirect.com/science/article/abs/pii/S016926070500101X]
- 85. Enhancing pharmacometric modeling with full Bayesian ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925003685]
- 86. Pharmacometrics, Physiologically Based Pharmacokinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6618101/]
- 87. Comparisons of Analysis Methods for Proof-of-Concept Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3600728/]
- 88. Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 89. 美国FDA计划利用AI等新方法学逐步替代动物试验 - 药学 [https://pharm.ncmi.cn/xwzx/202505/t20250530_427921.html]
- 90. Artificial Intelligence and Machine Learning Applications to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11672403/]
- 91. AI Model Testing in 2025: The Complete Guide [https://www.prismetric.com/ai-model-testing-guide/]
- 92. Enhancing drug discovery with AI: Predictive modeling of ... [https://www.sciencedirect.com/science/article/pii/S2949866X24001187]
- 93. 小分子化合物人体药代动力学参数预测的方法及应用 [https://dmpkservice.wuxiapptec.com/cn/blogs/456-id/]
- 94. 一文看懂 AI ... | Medium [https://easyaitech.medium.com/%E4%B8%80%E6%96%87%E7%9C%8B%E6%87%82-ai-%E6%95%B0%E6%8D%AE%E9%9B%86-%E8%AE%AD%E7%BB%83%E9%9B%86-%E9%AA%8C%E8%AF%81%E9%9B%86-%E6%B5%8B%E8%AF%95%E9%9B%86-%E9%99%84-%E5%88%86%E5%89%B2%E6%96%B9%E6%B3%95-%E4%BA%A4%E5%8F%89%E9%AA%8C%E8%AF%81-9b3afd37fd58]
- 95. In 2025: The Future of Automation Testing: Adapting to AI ... [https://dev.to/tak089/the-future-of-automation-testing-adapting-to-ai-model-validation-48k6]