Tiny Messengers, Mighty Weapons
How Immune Cell "Bubbles" Could Revolutionize COVID-19 Treatment
The Covert Messengers in Our Blood
Imagine a world where our own cells produce microscopic bubbles capable of carrying life-saving messages or blocking a deadly virus. This isn't science fiction—it's the cutting-edge science of exosomes. Amid the COVID-19 pandemic, scientists discovered that these nano-sized vesicles (30–150 nm) secreted by immune cells play a dual role: they can worsen viral infection or become powerful therapeutic allies 1 2 .
With the potential to deliver targeted treatments, suppress deadly cytokine storms, and even outsmart viral evolution, immune cell-derived exosomes represent a paradigm shift in combating SARS-CoV-2 and future pandemics 4 6 .

Decoding the Exosome Enigma
What Are Exosomes?
Exosomes are lipid-bound nanovesicles produced by nearly all cell types, including immune cells like T cells, B cells, and macrophages. They form inside cellular compartments called multivesicular bodies (MVBs) and are released into bodily fluids (blood, saliva, etc.) when MVBs fuse with the cell membrane 1 9 . Their cargo includes:
- Proteins (e.g., ACE2, tetraspanins)
- Nucleic acids (miRNA, dsRNA)
- Lipids that stabilize their structure 1
Key Exosome Markers and Their Roles
| Marker | Role in Exosomes | Relevance to COVID-19 |
|---|---|---|
| CD9/CD63 | Tetraspanin surface proteins | Exosome identification and isolation |
| ACE2 | Angiotensin-converting enzyme 2 | Binds SARS-CoV-2 spike protein |
| HSP70 | Heat shock protein | Promotes immune cell activation |
| Viral dsRNA | Double-stranded RNA | Triggers inflammatory responses |
The Double-Edged Sword in COVID-19
Exosomes' similarity to viruses—both in size and composition—makes them formidable players in infection:
Viral Accomplices
SARS-CoV-2 hijacks exosome pathways to spread viral RNA and proteins. Exosomes from infected cells carry viral dsRNA and spike protein, amplifying inflammation and immune evasion 2 .
Therapeutic Heroes
Exosomes from mesenchymal stem cells (MSCs) or engineered immune cells can neutralize the virus, deliver anti-inflammatory miRNAs, and repair lung damage. For example, exosomes loaded with ACE2 (evACE2) act as "decoys," binding to SARS-CoV-2 and blocking cellular entry with 135× greater efficiency than soluble ACE2 1 4 .
Breakthrough Experiment: How COVID-19 Exosomes Ignite Inflammation
The Pivotal Study
A landmark 2022 study revealed how exosomes from COVID-19 patients fuel systemic inflammation and long-term complications . Here's how researchers unraveled this phenomenon:
Methodology: Step by Step
- Exosome Isolation: Plasma from 50 hospitalized COVID-19 patients (early and late hospitalization phases) was ultracentrifuged to isolate exosomes. Samples were heat-treated (57°C for 30 min) to inactivate virions without damaging exosomes.
- Cargo Analysis: RNA sequencing detected SARS-CoV-2 dsRNA (a viral replication intermediate) in 82% of exosomes from early-phase patients.
- Immune Stimulation: Purified exosomes were incubated with healthy donor peripheral blood mononuclear cells (PBMCs). Controls used exosome-depleted plasma.
- Response Monitoring: Cytokine production (IL-6, TNF-α, etc.) and Toll-like receptor (TLR) expression were measured via flow cytometry and ELISA. TLR3 inhibition was tested using the drug CU-CPT-4a .
Immune Cell Responses to COVID-19 Exosomes
| Immune Cell Type | Response to Exosomes | Key Cytokines Produced |
|---|---|---|
| CD4⁺ T cells | Hyperactivation | IL-6, TNF-α |
| CD8⁺ T cells | Proinflammatory shift | IFN-γ, Granzyme B |
| CD14⁺ monocytes | Inflammatory polarization | IL-8, MCP-1 |
| Regulatory T cells | Minimal change | TGF-β (unchanged) |
Results and Analysis
- Cytokine Surge: COVID-19 exosomes triggered a 6–12-fold increase in IL-6, IL-8, and TNF-α from PBMCs. Depleting exosomes abolished this response.
- Cell-Specific Effects: CD4⁺/CD8⁺ T cells and CD14⁺ monocytes were hyperactivated, while regulatory T cells remained unaffected.
- TLR Link: Exosomes upregulated TLR3/7/8/9 in immune cells. Inhibiting TLR3 slashed cytokine production in T cells by 70% but had minimal effect on monocytes, highlighting divergent pathways .
Why This Matters
This study proved that SARS-CoV-2 transforms exosomes into "danger carriers" that disseminate inflammation beyond the lungs. Even after active infection, exosomal dsRNA persists—explaining long-term immune dysregulation in Long COVID 3 .
The Scientist's Toolkit: Key Reagents in Exosome Research
| Reagent/Method | Function | Application Example |
|---|---|---|
| Ultracentrifugation | Isolates exosomes via high-speed spins | Purifying plasma exosomes for cargo analysis |
| TLR3 Inhibitors (e.g., CU-CPT-4a) | Blocks dsRNA-sensing pathways | Testing inflammation mechanisms in T cells |
| Tetraspanin Antibodies (anti-CD9/63) | Binds exosome surface markers | Flow cytometry exosome identification |
| RT-ddPCR | Detects low-abundance viral RNA | Quantifying SARS-CoV-2 dsRNA in exosomes |
| Nanoparticle Tracking (NTA) | Measures exosome size/concentration | Confirming exosome integrity post-isolation |
From Lab to Clinic: The Therapeutic Frontier
Exosomes as Next-Gen Therapeutics
Engineered immune cell exosomes are advancing toward clinical use:
Vaccine Platforms
"Exosome mimetics" displaying SARS-CoV-2 spike protein elicited stronger antibody responses than mRNA vaccines in preclinical models 5 .
Challenges Ahead
Scalable production, standardized isolation, and targeted delivery remain hurdles. However, trials like NCT04798716 (MSC exosomes for COVID-19) are paving the way 7 .
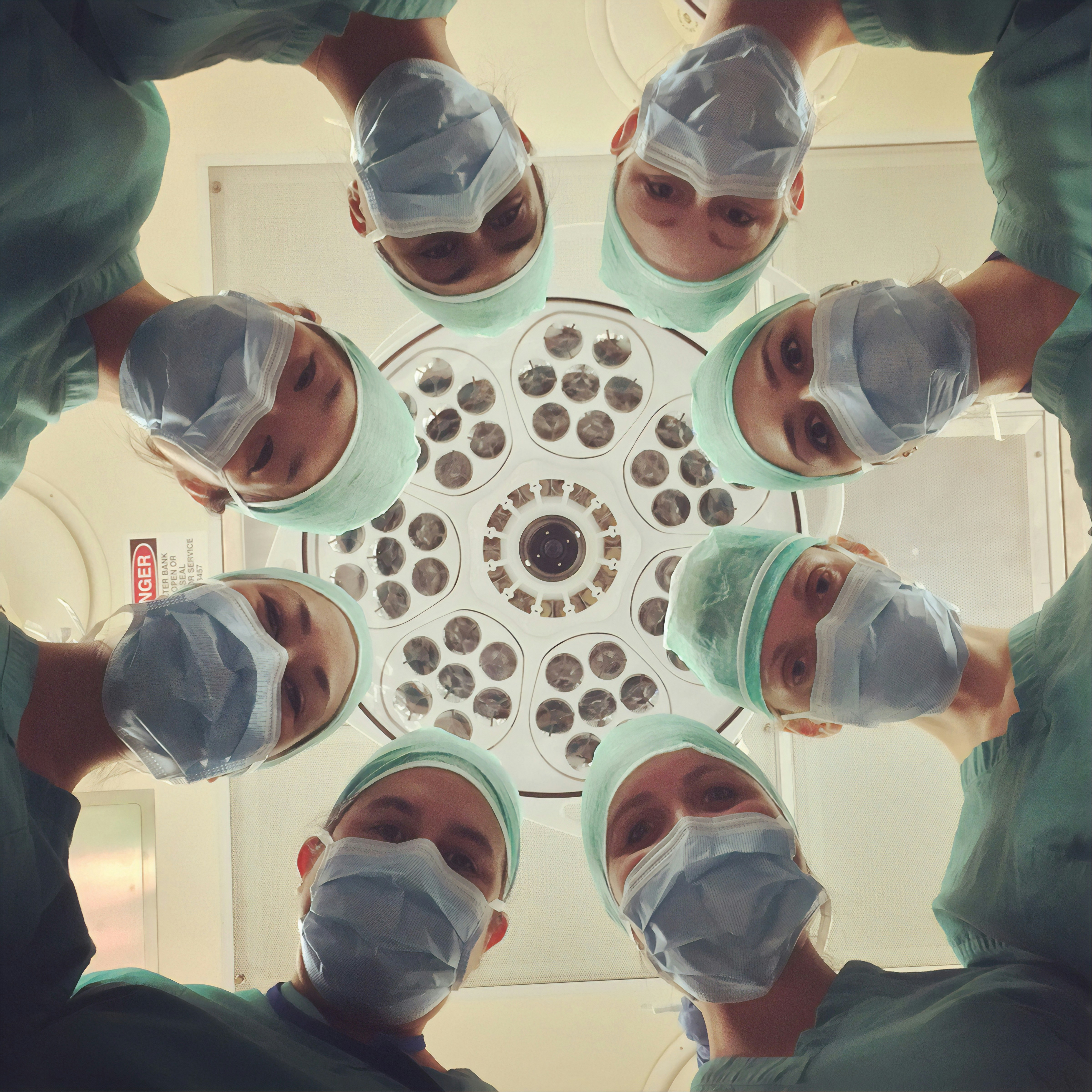
Researchers working on exosome-based therapies in a laboratory setting.
Conclusion: The Future in a Nanovesicle
Exosomes embody a biological paradox: natural accomplices of SARS-CoV-2 yet engineered to become precision-guided therapeutics. By leveraging their innate roles in immunity and intercellular communication, scientists are developing exosome-based solutions that could outmaneuver viral evolution and address Long COVID's lingering inflammation 3 6 . As research advances, these "tiny messengers" may well redefine how we combat not just COVID-19, but future viral threats.
"Exosomes are the body's own nanotechnology—we're just learning to harness it."