Time-Kill Kinetics Assay: A Comprehensive Protocol Guide for Antimicrobial Evaluation
This article provides a comprehensive guide for researchers and drug development professionals on the time-kill kinetics assay, a crucial in vitro method for characterizing the bactericidal or bacteriostatic activity of...
Time-Kill Kinetics Assay: A Comprehensive Protocol Guide for Antimicrobial Evaluation
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the time-kill kinetics assay, a crucial in vitro method for characterizing the bactericidal or bacteriostatic activity of antimicrobial agents over time. The content spans from foundational principles and standardized protocols, including CLSI and ASTM guidelines, to advanced applications in pharmacodynamic modeling and biofilm studies. It further addresses common troubleshooting scenarios, data optimization strategies, and comparative analyses with other antimicrobial susceptibility testing methods. By integrating current methodologies with practical validation techniques, this resource aims to enhance the accuracy and reproducibility of time-kill studies in the discovery and development of novel antimicrobials.
Understanding Time-Kill Kinetics: Core Principles and Significance in Antimicrobial Development
Time-kill kinetics represents a sophisticated in vitro pharmacodynamic method used to quantify the rate and extent of antimicrobial killing over time. Unlike endpoint determinations such as Minimum Inhibitory Concentration (MIC), time-kill assays provide a dynamic profile of antimicrobial activity, capturing the complex interaction between a pharmaceutical agent and microorganisms across a temporal landscape [1] [2]. This methodology is particularly valuable in antimicrobial drug development because it reveals the kinetic characteristics of antimicrobial action—whether an agent exerts bactericidal (killing) or bacteriostatic (growth-inhibiting) effects—and can identify potential synergistic combinations of drugs [2].
The fundamental principle underlying time-kill kinetics is the establishment of the rate at which a microorganism population is reduced when exposed to an antimicrobial agent. By measuring survival data at multiple exposure time points, researchers can model the decline in microbial population to potential extinction, providing critical insights for determining optimal dosing regimens and predicting clinical efficacy [3]. This approach offers a more comprehensive understanding of antimicrobial activity compared to single-time-point measurements, as it characterizes the entire progression of microbial kill rates [1].
Key Concepts and Definitions
Bactericidal vs. Bacteriostatic Activity
The classification of antimicrobial activity derived from time-kill kinetics is fundamentally based on the magnitude of microbial reduction:
- Bactericidal Activity: Defined as a greater than 3 log₁₀ decrease in colony-forming units (CFU) of surviving bacteria, which equates to 99.9% killing of the initial inoculum. This level of reduction demonstrates substantial killing capability that is considered clinically significant for eradication of pathogens [2].
- Bacteriostatic Activity: Characterized by a reduction in bacterial growth that does not achieve the 3 log₁₀ threshold, typically maintaining the bacterial population near the starting inoculum level. This indicates inhibition of growth without substantial killing [2].
Table 1: Classification of Antimicrobial Effects Based on Time-Kill Kinetics
| Effect Type | Log Reduction | Percentage Killing | Definition |
|---|---|---|---|
| Bactericidal | ≥ 3.0 log₁₀ | ≥ 99.9% | Substantial killing considered clinically significant |
| Bacteriostatic | < 3.0 log₁₀ | < 99.9% | Inhibition of growth without substantial killing |
| Ineffective | No reduction or growth | 0% or negative | No antimicrobial activity demonstrated |
Quantitative Measures in Time-Kill Assays
The quantitative framework of time-kill kinetics relies on logarithmic reductions in viable bacterial counts:
- A 1 log₁₀ reduction represents a 90% decrease in viable organisms (from 1,000,000 to 100,000 CFU/mL)
- A 2 log₁₀ reduction represents a 99% decrease (from 1,000,000 to 10,000 CFU/mL)
- The critical 3 log₁₀ reduction represents a 99.9% decrease (from 1,000,000 to 1,000 CFU/mL) [3]
These quantitative measurements provide a standardized approach to comparing the potency of different antimicrobial agents and regimens, enabling researchers to make precise comparisons between test compounds and establish concentration-effect relationships [2] [4].
Experimental Design and Methodology
Standard Time-Kill Assay Protocol
The execution of a robust time-kill assay requires meticulous attention to protocol details to ensure reproducible and meaningful results. The following workflow outlines the core procedures:
Critical Protocol Steps:
Inoculum Preparation: Challenge bacteria or fungi are suspended generally in 0.9% saline and standardized to a concentration of approximately 1.5 × 10⁶ CFU/mL to ensure consistent starting populations across experimental conditions [1] [3].
Antimicrobial Exposure: The standardized microbial suspension is introduced into the test product, which can be either undiluted (99%) or as a 10% dilution, depending on the experimental design. Multiple treatment modes should be considered, including single agents and combinations to evaluate potential synergistic effects [1].
Sampling and Neutralization: At predetermined time intervals (typically 0, 4, 8, 16, and 24 hours), samples are collected from the suspension and transferred to a validated neutralizing fluid that effectively eliminates the antimicrobial properties of the product without harming surviving microorganisms. This neutralization step is critical for accurate quantification of viable organisms [3].
Viability Assessment: The neutralized suspension undergoes serial dilution (usually 1:10 increments), followed by plating on appropriate agar media. After incubation at 37°C for 24 hours, resulting colonies are counted, with each colony representing a single microorganism that survived antimicrobial exposure [1] [3].
Research Reagent Solutions
Table 2: Essential Materials and Reagents for Time-Kill Assays
| Reagent/Material | Function/Purpose | Specifications |
|---|---|---|
| Bacterial Inoculum | Test organism | Standardized to ~1.5 × 10⁶ CFU/mL in 0.9% saline [1] [3] |
| Antimicrobial Agent | Test compound | Diluted to multiple concentrations (neat or diluted) [3] |
| Neutralizing Fluid | Inactivates antimicrobial agent | Validated for effectiveness per ASTM E1054 [3] |
| Agar Media | Supports microbial growth | Appropriate for test organism (e.g., Nutrient Agar, Sabouraud Dextrose Agar) [5] |
| Dilution Buffers | Serial dilution | Typically 0.9% saline or appropriate buffer [3] |
Data Analysis and Interpretation
Quantitative Analysis of Time-Kill Data
The analytical phase of time-kill kinetics transforms raw colony counts into meaningful pharmacodynamic parameters:
Calculation of Viable Bacteria: The number of viable bacteria at each time point is calculated according to the dilution ratio and the counted colonies on the plate. The formula for this calculation is:
[ \text{CFU/mL} = \frac{\text{Number of colonies counted} \times \text{Dilution factor}}{\text{Volume plated (mL)}} ]
These values are then converted to log₁₀ CFU/mL to facilitate comparison and plotting of the time-kill curves [1].
Data Interpretation Framework: The log CFU/mL values for all treatment groups are determined at time 0 and subsequent intervals, enabling the construction of kill curves that visualize the dynamics of antimicrobial activity. The interpretation of these curves follows specific criteria [2]:
- Bactericidal: Reduction of ≥3 log₁₀ CFU/mL from the initial inoculum
- Bacteriostatic: Reduction of <3 log₁₀ CFU/mL, with values remaining near the starting concentration
- Ineffective: No reduction or continued bacterial growth similar to control groups
Visualization and Curve Interpretation
Time-kill data are typically presented as semi-logarithmic plots with time on the x-axis and log₁₀ CFU/mL on the y-axis. The following diagram illustrates the decision-making process for interpreting time-kill kinetics results:
Advanced Analytical Approaches
Contemporary time-kill assay methodologies may incorporate multiple readout systems for enhanced data robustness. Recent protocols describe simultaneous quantification using both colony-forming units (CFU) and most probable number (MPN) techniques, particularly for challenging organisms like Mycobacterium tuberculosis [4]. This dual-method approach provides complementary datasets that strengthen the reliability of kill kinetics assessment, especially when dealing with slow-growing or fastidious microorganisms where traditional plating efficiency may be suboptimal.
Longitudinal data from time-kill assays reflect the dynamics of antibiotic effects over time against planktonic cultures and enable quantification of the concentration-effect relationship, which is fundamental to pharmacodynamic modeling and dose optimization [4].
Applications in Antimicrobial Research
Time-kill kinetics assays have become indispensable tools across multiple domains of antimicrobial research and development:
Natural Product Evaluation: Time-kill kinetics has been extensively employed to characterize antimicrobial properties of natural products. For example, in a study investigating mushroom extracts, time-kill kinetics revealed that methanol extracts of Trametes gibbosa, Trametes elegans, Schizophyllum commune, and Volvariella volvacea exhibited primarily bacteriostatic action against test organisms, providing crucial information about their mechanism of antimicrobial activity [5].
Novel Antimicrobial Peptide Assessment: In the development of antimicrobial peptides (AMPs), time-kill assays have confirmed rapid bactericidal action of promising candidates. For instance, the peptide Hel-4K-12K demonstrated complete bacterial elimination within one hour at its MIC concentration, highlighting its potential as a therapeutic agent against resistant bacteria [6].
Synergistic Combination Studies: Time-kill kinetics is particularly valuable for evaluating potential synergistic effects between antimicrobial agents. Studies designed with multiple treatment modes (single agents alone versus combinations) can identify enhanced killing kinetics that support combination therapy approaches for multidrug-resistant infections [1].
Regulatory Considerations and Guidelines
The execution of time-kill assays for regulatory purposes must adhere to established methodological standards:
- CLSI Guidelines: The Clinical and Laboratory Standards Institute provides standardized methodology for time-kill kinetics assays of antimicrobial agents through document M26 [2].
- ASTM Standards: For antimicrobial agents requiring shorter time-kill analysis (seconds/minutes), such as antiseptics, the ASTM E2315 guideline provides appropriate methodology [2].
- Neutralization Validation: Critical to assay validity, neutralization methods must be properly validated according to standards such as ASTM E1054 to ensure accurate assessment of microbial survival [3].
These standardized approaches ensure that time-kill data generated in different laboratories maintain comparability and reliability, supporting informed decisions in antimicrobial drug development and regulatory evaluations.
Table 3: Regulatory Guidelines for Time-Kill Assays
| Guideline | Scope/Application | Key Specifications |
|---|---|---|
| CLSI M26 | Antimicrobial agents | Standardized methodology for time-kill kinetics [2] |
| ASTM E2315 | Antimicrobial agents with short kill times | Methodology for seconds/minutes kill time analysis [2] |
| ASTM E1054 | Neutralization validation | Standards for validating neutralization methods [3] |
| EN Methods | General time-kill aqueous suspension tests | European standardized methodology [3] |
In antimicrobial research, the classification of agents as either bactericidal or bacteriostatic is fundamental for understanding their mode of action and potential clinical application. Bactericidal agents directly kill bacteria, leading to a irreversible reduction in bacterial viability, while bacteriostatic agents reversibly inhibit bacterial growth and reproduction, relying on the host's immune system to clear the infection [7] [8]. The time-kill kinetics assay serves as a critical in vitro tool for characterizing this activity over time, providing dynamic data beyond what is available from endpoint measurements like Minimum Inhibitory Concentration (MIC) [2] [9].
The interpretation of a ≥3 log₁₀ (99.9%) reduction in Colony Forming Units per milliliter (CFU/mL) is the established laboratory benchmark for defining bactericidal activity [7] [2]. This quantitative measure distinguishes agents that kill from those that merely inhibit. However, this classification is not always absolute; it can be influenced by factors such as bacterial species, inoculum size, antimicrobial concentration, and exposure time [7]. For instance, some antibiotics like linezolid exhibit bactericidal activity against Streptococcus pneumoniae but are bacteriostatic against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) [7].
Theoretical Framework and Definitions
Key Parameters and Quantitative Measures
The following table summarizes the core laboratory parameters used to define and distinguish bactericidal and bacteriostatic activity.
Table 1: Key Definitions and Quantitative Measures for Antimicrobial Activity
| Parameter | Definition | Interpretation and Significance |
|---|---|---|
| Minimum Inhibitory Concentration (MIC) | The lowest concentration of an antimicrobial that inhibits visible bacterial growth after 24 hours of incubation in specific media [7]. | Defines the potency of an antimicrobial. It is a primary measure for both bacteriostatic and bactericidal agents. |
| Minimum Bactericidal Concentration (MBC) | The minimum concentration of an antimicrobial required to achieve a ≥99.9% (3 log₁₀) reduction in the initial bacterial inoculum after 24 hours [7]. | Confirms bactericidal activity. The MBC/MIC ratio is used to classify an agent's action. |
| MBC/MIC Ratio | A ratio comparing the MBC to the MIC of an antimicrobial agent [7]. | ≤4: Classified as Bactericidal. >4: Classified as Bacteriostatic [7]. |
| ≥3 log₁₀ Reduction in CFU/mL | Equivalent to a 99.9% kill rate of the initial bacterial inoculum [2] [3]. | The standard threshold for defining bactericidal activity in time-kill kinetics assays. |
The Logic of Classifying Antimicrobial Action
The decision tree below outlines the standard workflow for classifying an antimicrobial agent as bactericidal or bacteriostatic based on data from time-kill kinetics assays and MBC/MIC ratios.
Time-Kill Kinetics Assay: A Detailed Protocol
The time-kill kinetics assay is a suspension test that measures the rate and extent of killing of a microorganism by an antimicrobial agent over a defined period, typically 24 hours [3]. It provides a time-course profile of antimicrobial effect, which is more informative than a single time-point test.
Materials and Reagents
Table 2: Research Reagent Solutions for Time-Kill Kinetics Assay
| Item | Function and Specification |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for the assay, ensuring consistent ion concentration for antibiotic activity [9]. |
| Sterile Saline (0.9%) | Diluent for preparing bacterial suspensions and performing serial dilutions [3]. |
| Antimicrobial Stock Solutions | Solutions of test compounds at high concentration (e.g., 1-10 mg/mL) in appropriate solvent (e.g., water, DMSO) [9] [10]. |
| Neutralizing Fluid | Used to terminate antimicrobial action at specific time points; must be validated for the specific antimicrobial being tested (e.g., Dey-Engley broth) [3]. |
| Agar Plates (e.g., Mueller-Hinton Agar) | Used for pour-plating or spread-plating to enumerate viable bacteria (CFU) [5] [3]. |
Step-by-Step Methodology
Step 1: Preparation of Inoculum
- Grow the bacterial strain of interest to the mid-logarithmic phase (typically 4-6 hours of growth) [9].
- Adjust the turbidity of the bacterial suspension to a 0.5 McFarland standard, which corresponds to approximately 1-2 x 10⁸ CFU/mL [9] [10].
- Dilute the suspension in the chosen broth to achieve a final inoculum density of approximately 5 x 10⁵ to 1 x 10⁶ CFU/mL in the test vessel [10].
Step 2: Preparation of Antimicrobial Solutions
- Prepare working solutions of the test antimicrobial at concentrations that are multiples of the predetermined MIC (e.g., 0.5x, 1x, 2x, 4x MIC) [9].
- Include two essential controls:
- Growth Control: Inoculated broth without any antimicrobial agent.
- Vehicle Control: Inoculated broth with the solvent used to dissolve the antimicrobial (e.g., DMSO) to rule out solvent toxicity [10].
Step 3: Incubation and Sampling
- Combine the standardized inoculum with the antimicrobial solutions in flasks and incubate at 37°C with constant shaking [9].
- At predetermined time points (e.g., 0, 2, 4, 6, 8, and 24 hours), aseptically remove aliquots (e.g., 1 mL) from each flask [2] [9].
Step 4: Quantification of Viable Bacteria
- Immediately after sampling, serially dilute the aliquots in sterile saline or a neutralizing broth to stop the antimicrobial action [3].
- Plate appropriate dilutions (e.g., 100 µL) onto agar plates via spread-plating or pour-plating [5] [3].
- Incubate the plates for 18-24 hours at 37°C and count the resulting colonies.
Step 5: Data Analysis and Interpretation
- Calculate the bacterial density (log₁₀ CFU/mL) for each sample at each time point.
- Plot the log₁₀ CFU/mL against time to generate time-kill curves for each concentration of the antimicrobial and for the controls.
- Interpretation:
- Bactericidal Activity: A decrease of ≥3 log₁₀ CFU/mL from the initial inoculum at any time point [2].
- Bacteriostatic Activity: The log₁₀ CFU/mL remains relatively unchanged or decreases by less than 3 log₁₀ CFU/mL compared to the initial inoculum [5] [2].
- Bacterial Regrowth: An initial decrease followed by an increase in CFU, which may indicate degradation of the antibiotic or the emergence of resistance.
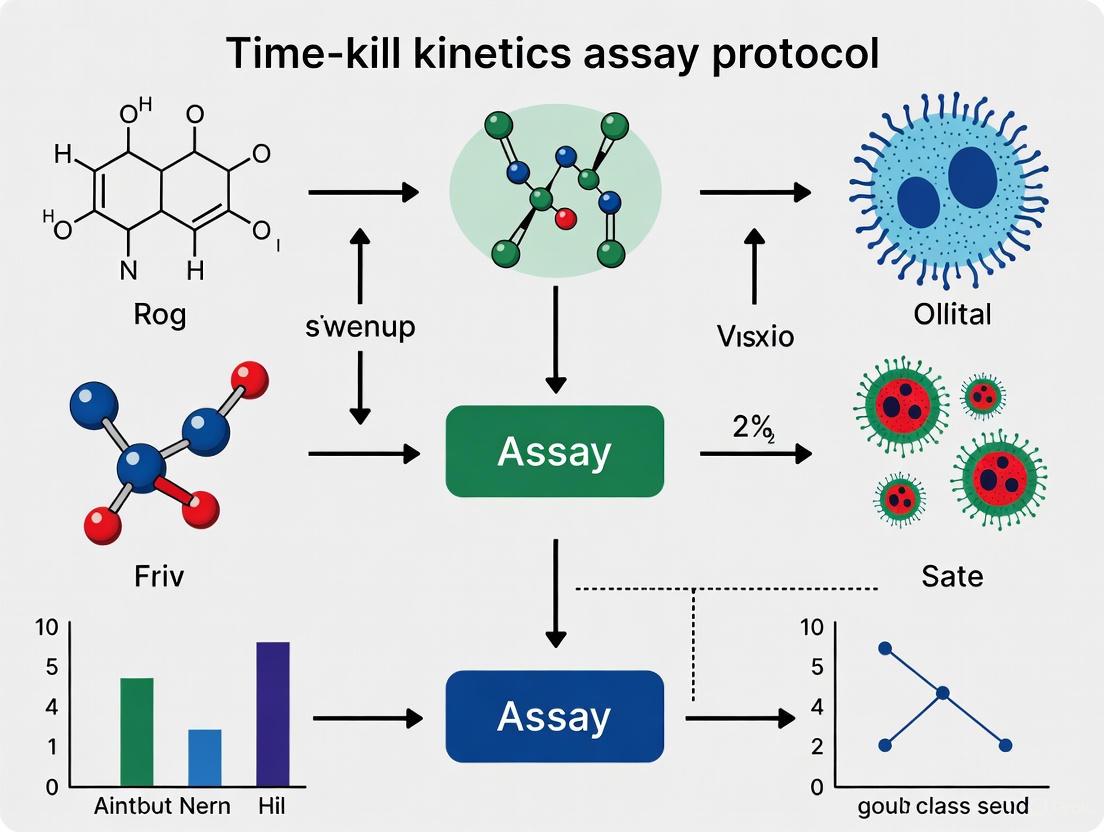
The following diagram visualizes the key stages of the experimental protocol and the subsequent data analysis pathway.
Data Interpretation and Analysis
Practical Examples from Research
Time-kill kinetics provide concrete data for classifying antimicrobials. The following table summarizes findings from recent studies, illustrating how this assay determines an agent's action.
Table 3: Empirical Data from Time-Kill Kinetics Studies
| Antimicrobial Agent / Extract | Test Organism(s) | Key Findings from Time-Kill Assay | Classification | Reference |
|---|---|---|---|---|
| Methanol extract of Trametes gibbosa | Various Gram-positive and Gram-negative bacteria | The extracts limited bacterial growth but did not achieve a ≥3 log₁₀ reduction in viable cell count. | Bacteriostatic [5] | [5] |
| Ciprofloxacin (CIP) | Klebsiella pneumoniae | Achieved ≥99.9% (3 log₁₀) reduction in the number of viable cells at 24 hours post-inoculation at 1x MIC concentration. | Bactericidal [9] | [9] |
| Levofloxacin (LEV) | Salmonella typhi ST07 | Achieved a 3 log₁₀-fold reduction in CFU/mL at 30 hours post-inoculation at 1x MIC concentration. | Bactericidal [9] | [9] |
| Ofloxacin (OFL) | Enterobacter aerogenes EA01 | Achieved a 3 log₁₀-fold reduction in CFU/mL at 30 hours post-inoculation at 1x MIC concentration. | Bactericidal [9] | [9] |
| Phosphanegold(I) Dithiocarbamate (Compound 4) | MRSA and Bacillus sp. | Showed varying degrees of bactericidal and bacteriostatic activities against different susceptible strains. | Context-Dependent [10] | [10] |
Factors Influencing Activity and Clinical Translation
It is critical to recognize that the classification derived from in vitro time-kill assays does not always directly translate to clinical superiority. The in vitro activity can be influenced by several factors [7]:
- Bacterial Strain and Species: An antibiotic may be bactericidal against one species but bacteriostatic against another (e.g., linezolid is bactericidal against Streptococcus pneumoniae but bacteriostatic against enterococci) [7].
- Antibiotic Concentration and Dosing: The achieved concentration at the site of infection, dictated by pharmacokinetics (PK), is a major determinant of in vivo efficacy.
- Inoculum Effect: A high density of bacteria can significantly reduce the apparent efficacy of some antimicrobials.
- Interaction with the Host Immune System: Bacteriostatic agents work in concert with the host's immune defenses to clear an infection, which is not a factor in in vitro assays [7] [8].
Furthermore, the long-held dogma that bactericidal drugs are inherently superior to bacteriostatic ones, especially in severe infections, is being re-evaluated. Specific bacteriostatic agents like linezolid and tigecycline have demonstrated clinical non-inferiority to bactericidal agents for infections such as pneumonia, intra-abdominal infections, and skin and soft tissue infections [7].
In the field of antimicrobial research, the Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) serve as fundamental in vitro parameters for evaluating the potency of antimicrobial agents. The MIC is defined as the lowest concentration of an antimicrobial agent that inhibits visible growth of a microorganism after a standard incubation period (typically 16-20 hours for fast-growing bacteria), while the MBC represents the lowest concentration that kills ≥99.9% of the initial bacterial inoculum [11] [12]. These parameters provide a crucial foundation for understanding antimicrobial efficacy; MIC distinguishes between growth inhibition and resistance, whereas MBC helps differentiate bacteriostatic (inhibitory) from bactericidal (lethal) effects [11] [13]. Concurrently, time-kill curve (TKC) analysis extends beyond these static endpoint measurements by characterizing the rate and extent of microbial killing over time, providing dynamic, time-dependent pharmacokinetic-pharmacodynamic (PK/PD) data that more accurately reflects antimicrobial action under conditions mimicking in vivo environments [14] [15].
The relationship between these parameters forms a hierarchical framework for antimicrobial assessment: MIC establishes the threshold for biological activity, MBC confirms lethal potential, and time-kill curves elucidate the kinetics of the entire interaction, from initial inhibition to ultimate eradication or regrowth. This integrated approach is particularly valuable for profiling novel antimicrobial candidates, optimizing dosing regimens, and identifying combinations that overcome resistance mechanisms [11] [14].
Theoretical Framework and Relationships
Conceptual Hierarchy of Antimicrobial Testing Parameters
The evaluation of antimicrobial agents follows a logical progression from simple threshold determinations to complex kinetic profiling. MIC testing serves as the initial screening step, identifying whether a compound possesses any inhibitory activity and establishing the concentration required to suppress visible growth [16]. This binary classification (growth vs. no growth) provides a practical foundation for further investigation but reveals nothing about the temporal dynamics or killing efficiency of the antimicrobial agent.
Building upon MIC data, MBC determination differentiates between compounds that merely inhibit growth (bacteriostatic agents) and those that achieve microbial death (bactericidal agents). The MBC/MIC ratio provides valuable insights into an agent's killing characteristics – a ratio ≤4 generally indicates bactericidal activity, while higher ratios suggest bacteriostatic activity [13]. This distinction has profound clinical implications, as bactericidal agents are often preferred for treating endocarditis, meningitis, and infections in immunocompromised patients where host defenses may be inadequate to eliminate pathogens.
Time-kill curve analysis represents the most comprehensive of these approaches, capturing the temporal dynamics of microbial killing that static endpoint measurements cannot reveal. Unlike MIC/MBC determinations that provide single-timepoint snapshots, TKCs generate a continuous profile of microbial response to antimicrobial exposure, enabling researchers to distinguish between concentration-dependent killing (where higher concentrations produce greater killing rates) and time-dependent killing (where the duration of exposure above MIC correlates with efficacy) [14] [15]. This kinetic information proves invaluable for establishing optimal dosing strategies and identifying compounds with persistent effects that continue to suppress regrowth even after concentrations fall below MIC.
Figure 1: The hierarchical relationship between MIC, MBC, and time-kill curves in antimicrobial evaluation, progressing from basic inhibition assessment to dynamic killing profiling and resistance prediction.
Methodological Synergies and Information Complementarity
These parameters exhibit significant methodological synergy, with each approach compensating for limitations in the others. While MIC testing offers high-throughput screening capability, it cannot distinguish between bactericidal and bacteriostatic effects, potentially overlooking compounds with slow but ultimately complete killing kinetics [11]. MBC testing addresses this limitation but remains vulnerable to artifacts from drug carryover during subculturing and provides no information about killing rates [12]. Time-kill curves overcome these constraints by directly monitoring microbial viability throughout the exposure period, enabling detection of biphasic killing patterns (indicating heteroresistance or persistence) and delayed regrowth that signals emerging resistance [14].
The integration of these approaches creates a powerful framework for comprehensive antimicrobial characterization. MIC values guide appropriate concentration selection for time-kill studies, while MBC determinations validate whether observed inhibition translates to meaningful microbial death. Conversely, time-kill curves provide context for interpreting MIC/MBC results – for instance, explaining why two agents with identical MIC values might demonstrate markedly different clinical efficacy due to variations in their killing kinetics or post-antibiotic effects [15].
Experimental Protocols and Methodologies
Broth Microdilution for MIC Determination
The broth microdilution method represents the gold standard for MIC determination, providing reproducible, quantitative results that align with clinical microbiology practices [16]. The following protocol, adapted from EUCAST guidelines, details the procedure for non-fastidious organisms:
Day 1: Bacterial Strain Preparation
- Using a sterile 1 μL loop, streak all test strains on LB agar (or appropriate rich medium supplemented with necessary antibiotics for selection).
- Incubate plates statically overnight at 37°C.
Day 2: Inoculum Standardization
- Gently vortex the overnight cultures.
- Mix 100 μL of overnight culture with 900 μL growth media and measure OD600 using a spectrophotometer.
- Calculate the volume of overnight culture needed to prepare standardized inoculum using the formula: Volume (μL) = 1000 μL ÷ (10 × OD600 measurement)/(target OD600)
- Pipette the calculated volume into a sterile 1.5 mL microtube and add 0.85% w/v sterile saline solution to 1 mL total volume.
- Use inoculum within 30 minutes of preparation [16].
MIC Assay Setup
- Prepare serial two-fold dilutions of the antimicrobial agent in Mueller-Hinton broth (or appropriate medium) in 96-well microtiter plates. Cation-adjusted Mueller-Hinton broth is recommended for testing cationic antimicrobials like polymyxins [16].
- Add standardized bacterial inoculum (5 × 10^5 CFU/mL final concentration) to all wells except sterility controls.
- Include growth control wells (inoculum without antimicrobial) and sterility controls (medium only).
- Incubate plates at 37°C for 16-20 hours (adjust for slow-growing organisms if necessary).
- Record MIC as the lowest antimicrobial concentration showing no visible turbidity [16] [12].
Quality Control
- Perform CFU enumeration to verify inoculum density by serial dilution and spot plating.
- Include quality control strains with known MIC ranges (e.g., E. coli ATCC 25922) in each assay run.
- Conduct tests in biological triplicate on different days to ensure reproducibility for research purposes [16].
MBC Determination Protocol
The MBC determination builds directly upon MIC results:
Subculturing Procedure
- From all clear wells in the MIC plate (showing no visible turbidity), subculture 100 μL onto appropriate non-selective agar plates (e.g., blood agar for fastidious organisms).
- Use a sterile bent rod to evenly spread the aliquot across the agar surface.
- Incubate subculture plates at 37°C for 24 hours.
MBC Interpretation
- Examine subculture plates for bacterial growth.
- The MBC is defined as the lowest antimicrobial concentration that results in no visible colony formation or yields ≤0.1% of the original inoculum (equivalent to ≥99.9% killing) [12] [13].
- Calculate the MBC/MIC ratio to classify antimicrobial activity: ratio ≤4 suggests bactericidal activity, while ratio >4 indicates bacteriostatic activity [13].
Time-Kill Curve Assay Methodology
Time-kill curves provide kinetic data on bacterial killing and are essential for comprehensive antimicrobial characterization:
Experimental Setup
- Prepare antimicrobial solutions at multiple concentrations (typically 0.5×, 1×, 2×, and 4× MIC) in appropriate culture medium.
- Inoculate flasks containing antimicrobial solutions with standardized bacterial suspension (5 × 10^5 CFU/mL final concentration).
- Include growth control flasks (inoculum without antimicrobial).
- Incubate at 37°C with constant shaking.
Sampling and Enumeration
- Remove samples (e.g., 100 μL) from each flask at predetermined timepoints (e.g., 0, 2, 4, 6, 8, 24 hours).
- Perform serial 10-fold dilutions in neutralizer solution or saline to minimize antibiotic carryover.
- Plate appropriate dilutions onto agar media and incubate for 18-24 hours at 37°C.
- Enumerate colony-forming units (CFU/mL) and plot log10 CFU/mL versus time [14] [15].
Data Interpretation
- Bactericidal activity: ≥3 log10 reduction (99.9% killing) in CFU/mL compared to initial inoculum.
- Bacteriostatic activity: <3 log10 reduction in CFU/mL.
- Regrowth: Initial reduction followed by increase in bacterial counts, suggesting emerging resistance or adaptive tolerance.
Figure 2: Experimental workflow for time-kill curve assays, illustrating the sequential steps from bacterial preparation through data visualization for kinetic analysis of antimicrobial activity.
Data Presentation and Interpretation
Quantitative Comparison of Antimicrobial Parameters
Table 1: MIC and MBC values for representative antimicrobial agents against bacterial pathogens
| Antimicrobial Agent | Bacterial Strain | MIC Value | MBC Value | MBC/MIC Ratio | Interpretation | Reference |
|---|---|---|---|---|---|---|
| Hyper-branched poly-L-lysine (HBPL) | MRSA ATCC 43300 | 0.5 mg/mL | 1.0 mg/mL | 2 | Bactericidal | [13] |
| Methylene Blue (MB) with photoactivation | E. faecalis ATCC 29212 | 66.67 ± 28.87 μg/mL | 266.67 ± 115.47 μg/mL | 4 | Bactericidal | [12] |
| MB-rGO with photoactivation | E. faecalis ATCC 29212 | 50.00 ± 0.00 μg/mL | 200.00 ± 0.00 μg/mL | 4 | Bactericidal | [12] |
| Grapefruit Extract | S. aureus | 0.25 ± 0.08 mg/mL | ND | - | - | [11] |
| Erythromycin | S. aureus | 0.0008 ± 0.0003 mg/mL | ND | - | - | [11] |
Table 2: Time-kill curve parameters for antimicrobial agents in different media conditions
| Antimicrobial Agent | Bacterial Strain | Media Condition | Time to 99.9% Killing | Regrowth Observed | Key Findings | Reference |
|---|---|---|---|---|---|---|
| Cefazolin | Model pathogen | Pure MHB | 6h | No | Standard growth | [14] |
| Cefazolin | Model pathogen | MHB + 20% plasma | Delayed by 0.25h | No | Growth delay observed | [14] |
| Cefazolin | Model pathogen | MHB + 70% plasma | Delayed by 2.90h | No | Significant growth delay | [14] |
| Clindamycin | Model pathogen | Pure MHB | 8h | No | Standard growth | [14] |
| Clindamycin | Model pathogen | MHB + 20% plasma | Delayed by 0.64h | No | Growth delay observed | [14] |
| Clindamycin | Model pathogen | MHB + 70% plasma | Delayed by 1.40h | No | Significant growth delay | [14] |
Advanced Applications and Integration with Novel Technologies
Bioluminescence-Based Real-Time Monitoring Recent advances in antimicrobial susceptibility testing incorporate bioluminescent bacterial strains engineered with reporter genes (e.g., bacterial luciferase) for real-time viability assessment. This approach offers several advantages over traditional methods:
- Continuous monitoring without manual sampling
- Enhanced sensitivity to sublethal effects
- Non-invasive measurement preserving sample integrity
- Reduced assay time through early detection of inhibition or killing
Studies demonstrate strong correlation between bioluminescence signals and classical CFU enumeration in MIC/MBC determinations, validating this approach for rapid antimicrobial screening [15]. The methodology involves:
- Using naturally luminescent bacteria or strains transformed with lux operons
- Measuring bioluminescence kinetics alongside optical density
- Establishing correlation between light emission and viable counts
- Applying real-time data for pharmacokinetic/pharmacodynamic modeling
Addressing Methodological Limitations Standard MIC/MBC methods face challenges when testing non-conventional antimicrobials with unique physicochemical properties (e.g., natural extracts, ionic liquids, ozonated oils, nanoparticulate systems). These substances may exhibit:
- Poor solubility in aqueous testing media
- Interaction with medium components
- High viscosity affecting diffusion
- Volatility impacting concentration stability
For such compounds, a combined methodological approach is recommended, integrating broth microdilution with agar dilution and disk diffusion to confirm activity despite methodological limitations [11]. Additionally, modifications to standard protocols may be necessary, such as:
- Using cation-adjusted media for testing cationic antimicrobial peptides
- Incorporating solubilizing agents for hydrophobic compounds
- Implementing low-volume assays for scarce investigational compounds
- Applying specialized detection methods for turbidity-masking substances [16]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for MIC, MBC, and time-kill curve assays
| Reagent/Material | Specification | Application/Function | Reference |
|---|---|---|---|
| Mueller-Hinton II Broth | Cation-adjusted | Standardized growth medium for susceptibility testing | [15] |
| 96-well Microtiter Plates | Sterile, polystyrene | Broth microdilution MIC assays | [16] [12] |
| Diode Laser | 660 nm wavelength | Photoactivation of photosensitizers in aPDT studies | [12] |
| Bioluminescent Bacterial Strains | e.g., P. aeruginosa Xen41, S. aureus SAP229 | Real-time viability assessment without sampling | [15] |
| Sheep Blood Agar | 5% defibrinated sheep blood | Subculturing for MBC determination and purity checks | [12] |
| Hyper-branched Poly-L-lysine | MW 3,114-4,532 Da, PDI 1.46 | Synthetic antimicrobial polymer for novel agent studies | [13] |
| Reduced Graphene Oxide Functionalized MB | 12.5-400 μg/mL range | Enhanced photosensitizer for antimicrobial photodynamic therapy | [12] |
| Human Plasma | 20-70% concentration in MHB | Physiologically relevant media for improved in vitro-in vivo correlation | [14] |
The integrated application of MIC, MBC, and time-kill curve analyses provides a comprehensive framework for antimicrobial efficacy assessment that transcends the limitations of any single approach. While MIC establishes fundamental inhibitory concentrations and MBC confirms lethal potential, time-kill curves elucidate the kinetic profile essential for predicting in vivo efficacy and designing optimal dosing regimens. The continued refinement of these methodologies – through incorporation of physiologically relevant media conditions, advanced detection technologies like bioluminescence reporting, and adaptations for non-conventional antimicrobial agents – will enhance their predictive value in the translational pipeline. For researchers engaged in antimicrobial discovery and development, this multi-parametric approach offers the robust dataset necessary to advance promising candidates from laboratory characterization to clinical application in an era of escalating antimicrobial resistance.
The Minimum Inhibitory Concentration (MIC) is a cornerstone of antimicrobial susceptibility testing, defined as the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism after overnight incubation [17]. Despite its widespread use and high reproducibility, the static nature of MIC determination presents significant limitations. As a single endpoint measurement, MIC fails to capture the dynamic interactions between antibiotics and bacteria over time, obscuring critical pharmacodynamic (PD) information such as the rate and extent of bacterial killing, which are essential for predicting clinical efficacy [18] [19].
Time-kill kinetics assays address these limitations by providing a comprehensive, dynamic profile of antimicrobial activity against bacterial populations over time. This method quantifies the rate and extent of bactericidal or bacteriostatic activity, enabling researchers to distinguish between different killing patterns and understand the time- and concentration-dependent characteristics of antimicrobial agents [2] [19]. Unlike static MIC determinations, time-kill kinetics can identify whether an antimicrobial exhibits concentration-dependent killing (where higher concentrations result in greater killing) or time-dependent killing (where the duration of exposure is more critical than peak concentration), thereby facilitating the optimization of dosing regimens for pre-clinical development [20] [18].
Limitations of Static MIC Determinations
Fundamental Constraints of the MIC Assay
The MIC value, while simple to determine, provides an incomplete picture of antimicrobial efficacy due to several inherent constraints. Firstly, MIC testing employs a fixed incubation period (typically 16-20 hours) and static antibiotic concentrations, which do not reflect the constantly changing drug levels experienced by pathogens in vivo due to pharmacokinetic processes of absorption, distribution, metabolism, and excretion [19]. This static exposure fails to model the dynamic nature of antibiotic concentrations in human tissues and bodily fluids, potentially leading to inaccurate predictions of clinical effectiveness.
Secondly, the MIC represents a population-level threshold that obscures heterogeneous responses within bacterial populations. It does not account for the presence of persister cells or resistant subpopulations that may influence treatment outcomes, particularly with bactericidal agents [18]. Furthermore, the MIC endpoint is based on visible growth inhibition, which lacks precision in quantifying the extent of bacterial killing or determining whether the antimicrobial effect is primarily bactericidal (killing) or bacteriostatic (growth inhibition) [19].
Clinical Relevance and Predictive Value Gaps
The clinical translation of MIC data is complicated by numerous factors that limit its predictive value for treatment success. MIC testing in artificial media often fails to account for the influence of host factors, including immune system interactions, protein binding, and site-specific penetration barriers that alter antibiotic bioavailability at the infection site [19]. Additionally, the inoculum effect, where high bacterial densities can significantly reduce antibiotic effectiveness, is not routinely assessed in standard MIC determinations but can profoundly impact therapeutic outcomes [19].
Perhaps most importantly, MIC values alone provide insufficient information for optimizing dosing regimens, as they do not characterize the kinetics of antimicrobial activity [18]. Different antibiotics with similar MIC values may exhibit dramatically different time-kill profiles, necessitating distinct dosing strategies to maximize efficacy and minimize resistance development. This limitation becomes particularly critical when treating infections in immunocompromised patients, where rapid bactericidal activity is essential for successful outcomes [19].
Advantages of Time-Kill Kinetics
Capturing Dynamic Antimicrobial Effects
Time-kill kinetics assays provide a comprehensive temporal profile of antimicrobial activity that reveals critical pharmacodynamic information unavailable through static MIC testing. This methodology enables researchers to quantitatively monitor the progression of bacterial killing over time, characterizing both the rate of kill and the extent of kill at various antibiotic concentrations [2] [19]. By capturing these dynamic effects, time-kill kinetics can distinguish between bactericidal agents (which achieve ≥3 log₁₀ reduction in colony-forming units [CFU]/mL) and bacteriostatic agents (which inhibit growth without achieving this level of killing) [2] [3].
This approach is particularly valuable for identifying concentration-dependent killing patterns, where increased antibiotic concentrations result in enhanced killing rates and extent, as seen with aminoglycosides and fluoroquinolones [20] [18]. Conversely, time-kill kinetics also reveals time-dependent killing patterns, where antibacterial activity primarily depends on the duration of exposure above a threshold concentration, characteristic of β-lactams and macrolides [20]. This discrimination is crucial for designing optimal dosing regimens, as concentration-dependent antibiotics benefit from higher peak concentrations, while time-dependent antibiotics require prolonged exposure above the MIC [20] [18].
Enhanced Predictive Capability for In Vivo Efficacy
The dynamic nature of time-kill kinetics data enables more accurate predictions of in vivo efficacy by facilitating the development of mechanistic pharmacokinetic/pharmacodynamic (PK/PD) models [21]. These models integrate time-kill data with pharmacokinetic parameters to simulate bacterial response under fluctuating antibiotic concentrations, mirroring the dynamic environment encountered in infected patients [18] [21]. Such modeling approaches have demonstrated that bacterial susceptibility to an antibiotic cannot be adequately described by MIC alone, as isolates with identical MIC values may exhibit different maximal kill rates (Emax) and concentration-response relationships (Hill coefficient) [18].
Time-kill kinetics also provides critical insights for suppressing resistance emergence by characterizing the mutant selection window and identifying concentrations that prevent the amplification of resistant subpopulations [19]. Furthermore, this approach is indispensable for evaluating antibiotic combination therapies, as it can detect synergistic, additive, or antagonistic interactions between drugs that would remain undetected in static MIC assays [19]. The enhanced predictive capability of time-kill kinetics makes it particularly valuable for guiding antibiotic therapy in immunocompromised patients and for infections requiring rapid bactericidal activity, such as meningitis and endocarditis [19].
Experimental Protocols
Standard Time-Kill Kinetics Assay Protocol
The time-kill kinetics assay evaluates the bactericidal or bacteriostatic activity of antimicrobial agents over a defined period, typically 24 hours. The following protocol adheres to guidelines established by the Clinical and Laboratory Standards Institute (CLSI) and incorporates best practices from current literature [2] [19].
Materials and Reagents:
- Test microorganisms (freshly cultured, 18-24 hours)
- Antimicrobial agents (pure substances of known potency)
- Appropriate culture media (e.g., Mueller-Hinton Broth [MHB])
- Sterile saline (0.9% NaCl) for dilutions
- Neutralizing solution (e.g., Dey-Engley neutralizing broth)
- Agar plates for colony counting
- Incubator set at appropriate temperature (e.g., 35±2°C)
- Water bath (for temperature control)
Procedure:
- Inoculum Preparation: Adjust the turbidity of a fresh bacterial culture in logarithmic growth phase to approximately 1×10⁸ CFU/mL (0.5 McFarland standard), then dilute in culture medium to achieve a final inoculum of 1×10⁶ CFU/mL in the test system.
Antibiotic Solution Preparation: Prepare serial dilutions of the antimicrobial agent in culture medium to achieve test concentrations, typically including multiples of the MIC (e.g., 0.5×, 1×, 2×, 4×, 8×MIC).
Experimental Setup: Combine equal volumes of standardized inoculum and antibiotic solutions in sterile tubes. Include growth control tubes (inoculum without antibiotic) and sterility control tubes (media only).
Incubation and Sampling: Inculate all tubes at the appropriate temperature. Remove samples (e.g., 1 mL) from each tube at predetermined time points (e.g., 0, 2, 4, 6, 8, 12, 24 hours).
Viable Count Determination: Serially dilute each sample in neutralizing broth to stop antimicrobial action. Plate appropriate dilutions onto agar plates in duplicate. Incubate plates for 18-24 hours, then enumerate colonies.
Data Analysis: Calculate CFU/mL at each time point and plot log₁₀ CFU/mL versus time to generate time-kill curves.
Data Interpretation and Analysis
Bactericidal Activity: Defined as a ≥3 log₁₀ decrease (99.9% reduction) in CFU/mL compared to the initial inoculum [2] [3].
Bacteriostatic Activity: Defined as maintenance of the initial inoculum level or a <3 log₁₀ decrease in CFU/mL [2].
Synergy Evaluation: For combination studies, synergy is typically defined as a ≥2 log₁₀ decrease in CFU/mL with the combination compared to the most active single agent [19].
The time-kill curves generated from this protocol provide visual representation of the rate and extent of antimicrobial activity, enabling classification of antibiotics based on their killing patterns and facilitating comparisons between different agents or regimens.
Quantitative Data Comparison
Table 1: Comparative Features of Static MIC and Time-Kill Kinetics Assays
| Feature | Static MIC Determination | Time-Kill Kinetics |
|---|---|---|
| Temporal Resolution | Single endpoint (16-20 hours) | Multiple time points (0-24 hours) |
| Killing Dynamics | Not determined | Quantifies rate and extent of killing |
| Classification Ability | Limited bactericidal/bacteriostatic distinction | Clear bactericidal (≥3 log₁₀ kill) vs. bacteriostatic differentiation [2] [3] |
| Pattern Recognition | No time- or concentration-dependent pattern identification | Identifies concentration-dependent vs. time-dependent killing [20] [18] |
| Resistance Detection | Limited to homogeneous resistance | Can detect heteroresistance and evaluate resistance suppression [19] |
| Combination Therapy Assessment | Limited to fractional inhibitory concentration (FIC) | Comprehensive synergy/additivity/antagonism evaluation [19] |
| PK/PD Modeling Utility | Limited to time above MIC (T>MIC) calculations | Enables development of sophisticated PK/PD models [18] [21] |
Table 2: Key Pharmacodynamic Parameters Obtainable from Time-Kill Kinetics
| Parameter | Description | Clinical Significance |
|---|---|---|
| Maximal Kill Rate (Emax) | Maximum rate of bacterial killing achieved at high antibiotic concentrations [18] | Predicts efficiency of bacterial eradication at optimal concentrations |
| EC₅₀ | Antibiotic concentration producing 50% of maximal kill rate [18] | Indicates potency relative to killing efficiency |
| Hill Coefficient | Steepness of the concentration-effect relationship [18] | Predicts responsiveness to dose increases; higher values indicate steeper concentration-effect relationships |
| Bactericidal Threshold | Concentration required for ≥3 log₁₀ reduction in CFU/mL [2] | Guides target concentration for bactericidal efficacy |
| Post-Antibiotic Effect (PAE) | Persistent suppression of bacterial growth after antibiotic removal [19] | Informs dosing interval optimization |
Visualization of Experimental Workflows
Time-Kill Kinetics Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Time-Kill Kinetics
| Item | Function/Purpose | Specifications/Examples |
|---|---|---|
| Culture Media | Supports bacterial growth during experiment | Mueller-Hinton Broth (MHB) for most organisms; supplemented media for fastidious organisms [17] |
| Neutralizing Solution | Stops antimicrobial action during sampling | Dey-Engley neutralizing broth; specific neutralizers for different antimicrobial classes [3] |
| Reference Antibiotics | Positive controls for antimicrobial activity | Certified reference standards of known potency [5] |
| Quality Control Strains | Verifies experimental conditions | ATCC strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) [17] |
| Sterile Saline | Diluent for bacterial suspensions | 0.9% sodium chloride, isotonic solution [3] |
| Agar Plates | Colony counting and viability assessment | Mueller-Hinton Agar; blood agar for fastidious organisms [2] |
The implementation of time-kill kinetics assays represents a significant advancement over static MIC determinations, providing critical insights into the dynamic interactions between antimicrobial agents and bacterial pathogens. By capturing both time- and concentration-dependent effects, this methodology enables more accurate predictions of in vivo efficacy and supports the optimization of dosing regimens for improved clinical outcomes.
The relentless rise of antimicrobial resistance (AMR) is a formidable global challenge, rendering a growing number of infectious diseases difficult to treat and increasing mortality rates [22] [23] [24]. In the urgent quest for new anti-infective agents, time-kill kinetics assays have emerged as a vital tool for the sophisticated evaluation of novel compounds. This method provides dynamic, time-dependent data on the interaction between antimicrobial agents and microbial strains, offering insights far beyond those available from standard static minimum inhibitory concentration (MIC) tests [22] [2] [25]. Within drug development pipelines, time-kill kinetics are indispensable for characterizing the rate and extent of microbial killing, determining whether a novel agent is bacteriostatic/fungistatic or bactericidal/fungicidal, and providing essential data for pharmacodynamic modeling to optimize dosing strategies [2] [26] [25]. These applications make the assay particularly valuable for evaluating candidates from diverse sources—including natural products like plumbagin from Plumbago zeylanica, mushroom extracts, and synthetic compounds—against priority pathogens [22] [5] [25].
Core Principles and Definitions
The time-kill kinetics assay measures the rate at which a microorganism is killed by a test product by tracking the number of surviving bacteria or fungi over a specified time period [2] [3]. The fundamental measure in these assays is the log10 reduction in colony-forming units (CFU) per milliliter relative to the initial inoculum [3].
A key distinction in these assays is the classification of antimicrobial activity:
- Bactericidal/Fungicidal Activity: Defined as a greater than 3 log10 decrease in CFU/mL, equating to 99.9% killing of the initial inoculum [2].
- Bacteriostatic/Fungistatic Activity: The agent inhibits growth but does not achieve the 3 log10 reduction threshold, with the CFU count over time remaining roughly similar to the starting concentration [2] [26].
The assay can monitor the effect of various antimicrobial concentrations over time in relation to the different growth phases of microorganisms (lag, exponential, and stationary phases), providing a comprehensive profile of antimicrobial action [2].
Critical Applications in Drug Development
Profiling Novel Antimicrobial Compounds
Time-kill kinetics are crucial for the initial characterization of novel antimicrobial entities. For instance, research on plumbagin isolated from Plumbago zeylanica roots demonstrated its bacteriostatic and fungistatic activity against a panel of test organisms through time-kill studies, providing essential information for its development as a lead compound [22]. Similarly, studies on methanol extracts of Ghanaian mushrooms, including Trametes gibbosa and Schizophyllum commune, used time-kill kinetics to confirm their bacteriostatic action, supporting their potential as sources of new antimicrobial agents [26] [5].
Resistance Modulation and Combination Therapy
With multidrug-resistant (MDR) pathogens on the rise, combination therapy has become a promising strategy to extend antimicrobial lifespan and combat resistance [27] [24]. Time-kill kinetics serve as a gold standard method for evaluating in vitro synergy between drug candidates and existing antibiotics [27]. In resistance modulation studies, plumbagin at a subinhibitory concentration (4 μg/mL) was found to potentiate the activity of ketoconazole against Candida albicans by up to 12-fold, as revealed through follow-up kill-kinetic analyses [22]. Research on crude alkaloids from Phyllanthus fraternus also employed time-kill kinetics to demonstrate their bactericidal effects against specific pathogens and their potential to enhance the effectiveness of tetracycline [24].
Pharmacodynamic Modeling for Dosing Optimization
Time-kill curve data are frequently used in pharmacodynamic modeling to establish relationships between antimicrobial concentration and microbial killing rates [25]. These models help predict optimal dosing regimens for clinical applications. For example, a study on Neisseria gonorrhoeae used a pharmacodynamic model to analyze time-kill curves, generating parameters such as the maximal bacterial growth rate (ψmax), minimal growth rate (ψmin), Hill coefficient (к), and pharmacodynamic MIC (zMIC). This approach revealed gradual decreases in bactericidal effects across different antibiotics and identified purely bacteriostatic agents, providing critical information for improving future dosing strategies to treat gonorrhea [25].
Detailed Experimental Protocol
Research Reagent Solutions
Table 1: Essential Reagents and Materials for Time-Kill Kinetics Assay
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Culture Media | Supports microbial growth during assay | Mueller-Hinton Broth (MHB) [24], Graver-Wade (GW) medium for fastidious organisms [25], Nutrient broth [22] |
| Standard Antibiotics | Reference controls for comparison | Ciprofloxacin, ketoconazole, tetracycline, ceftriaxone [22] [24] [25] |
| Test Compounds | Investigational antimicrobial agents | Natural extracts (plumbagin, mushroom alkaloids) or synthetic compounds [22] [5] [24] |
| Saline Solution (0.9%) | Diluent for microbial suspension preparation | Used as a suspension medium for challenge organisms [3] |
| Dimethyl Sulfoxide (DMSO) | Solvent for poorly water-soluble compounds | Used to dissolve compounds like plumbagin before dilution in culture medium [22] |
| Neutralizing Buffer | Halts antimicrobial action at sampling time points | Validated neutralizing fluid to stop antimicrobial activity for accurate plating [3] |
| Solid Agar Media | Enumeration of surviving microorganisms | Muller Hinton Agar (MHA), GCBA plates, Sabouraud dextrose agar [23] [25] |
Step-by-Step Methodology
The following workflow outlines the core procedures for conducting a time-kill kinetics assay, from sample preparation through data analysis:
Sample Preparation and Inoculum Standardization
Begin by preparing a standardized microbial inoculum from fresh overnight cultures. Adjust the suspension in saline or appropriate medium to match a 0.5 McFarland standard, typically resulting in approximately 1-5 × 108 CFU/mL. Further dilute this suspension in the chosen assay medium (e.g., Mueller-Hinton Broth or chemically defined GW medium for fastidious organisms) to achieve a final working concentration of approximately 106 CFU/mL [22] [25]. For pre-incubation, transfer the diluted bacteria to microtiter plates and incubate for approximately 4 hours with shaking (e.g., 150 rpm) at 35-37°C to synchronize the culture in the early- to mid-logarithmic growth phase before antimicrobial exposure [25].
Antimicrobial Preparation and Exposure
Prepare serial dilutions of the test and reference antimicrobial compounds in the appropriate solvent, typically covering a concentration range from below to above the MIC (e.g., 0.016× to 16× MIC) [25]. Add the antimicrobial solutions to the pre-incubated bacterial cultures. Include appropriate controls: a growth control (bacteria without antimicrobial), a vehicle control (bacteria with solvent alone), and a negative control (sterile medium only) [22] [2]. Maintain the assay system under optimal growth conditions throughout the exposure period.
Sampling, Viable Count Determination, and Data Analysis
Sample the cultures at predetermined time intervals (e.g., 0, 2, 4, 6, 8, 10, 12, and 24 hours). At each time point, remove aliquots and immediately dilute in a validated neutralizing solution to stop antimicrobial action [3]. Perform serial 1:10 dilutions in sterile phosphate-buffered saline or appropriate diluent. Plate aliquots from appropriate dilutions onto solid agar media using spread-plating or pour-plating techniques. Incubate plates for 18-24 hours at optimal growth conditions, then enumerate the colonies to determine CFU/mL at each time point [3] [25].
Calculate the log10 CFU/mL for each sample and plot these values against time to generate time-kill curves. Compare the reduction in viable counts against the initial inoculum and the growth control to determine the killing kinetics. A ≥3 log10 decrease in CFU/mL compared to the initial inoculum indicates bactericidal activity, while lesser reductions that maintain or slow growth suggest bacteriostatic activity [2].
Data Interpretation and Analysis
Quantitative Analysis of Time-Kill Kinetics
Table 2: Key Parameters for Interpretation of Time-Kill Kinetics Data
| Parameter | Description | Interpretation Guidelines |
|---|---|---|
| Log10 Reduction | Decrease in viable count from initial inoculum | ≥3 log10 (99.9% killing): Bactericidal [2]<3 log10: Bacteriostatic [26] |
| Killing Rate | Slope of the kill curve | Steep slope: Rapid killingGradual slope: Slow killing |
| Post-Antibiotic Effect | Continued suppression after removal | Prolonged suppression: Persistent effectRapid regrowth: Limited persistent effect |
| Concentration Dependency | Effect of increasing antimicrobial concentrations | Increased killing with higher concentrations: Concentration-dependent killingSimilar killing despite concentration: Time-dependent killing |
| Regrowth | Increase in CFU after initial decline | Suggests potential resistance development or incomplete killing |
Pharmacodynamic Modeling
For advanced analysis, time-kill data can be fitted to pharmacodynamic models. The model described by Regoes et al. uses four key parameters to characterize antimicrobial action: the maximal growth rate without antimicrobial (ψmax), the minimal growth rate at high concentrations (ψmin), the Hill coefficient (κ) indicating steepness of the concentration-effect relationship, and the pharmacodynamic MIC (zMIC) representing the concentration where the growth rate is half of ψmax [25]. This modeling approach allows for quantitative comparison between different antimicrobial agents and supports optimized dosing regimen design.
Comparison with Other Antimicrobial Susceptibility Methods
Table 3: Comparison of Time-Kill Kinetics with Other Antimicrobial Susceptibility Testing Methods
| Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Time-Kill Kinetics | Time-dependent measurement of microbial killing in liquid medium | Provides dynamic killing profileDistinguishes bactericidal vs. bacteriostaticGold standard for synergy studies [27] | Time-consuming and labor-intensive [27]Requires significant technical expertise [27] |
| Broth Microdilution | Determination of MIC in liquid medium using dilution series | Quantitative resultsStandardized and reproducibleSuitable for multiple isolates | Static endpoint (single time point)Does not distinguish cidal vs. static [28] |
| Disk Diffusion | Measurement of inhibition zones around antibiotic disks on agar | Simple and inexpensiveWell-standardizedSuitable for routine testing | Qualitative/semi-quantitativeNot suitable for slow-growing organisms [23] |
| Agar Gradient Diffusion (Etest) | MIC determination using predefined antibiotic gradient on strips | Flexible for single drugsQuantitative MICsEasy to perform | Expensive for routine useLimited to available gradients [28] |
Time-kill kinetics assays represent a powerful, information-rich methodology that provides critical insights into the dynamics of antimicrobial action essential for drug development. The ability to distinguish between bactericidal and bacteriostatic activity, evaluate synergistic combinations for overcoming resistance, and generate data for pharmacodynamic modeling makes this approach invaluable for advancing novel antimicrobial candidates from discovery through preclinical development. While the method demands specialized expertise and resources, its comprehensive output justifies its application in characterizing promising therapeutic agents, particularly as we face the escalating threat of antimicrobial resistance worldwide.
Executing the Assay: A Step-by-Step Protocol from Inoculum to Analysis
Time-kill kinetics assays represent a cornerstone methodology in antimicrobial research, providing a dynamic and quantitative assessment of an antimicrobial agent's bactericidal or bacteriostatic activity over time. Unlike endpoint determinations such as the minimum inhibitory concentration (MIC), time-kill kinetics reveal the rate and extent of microbial killing, offering critical insights into the pharmacodynamics of antimicrobial agents [2]. This methodology is particularly valuable for characterizing novel antimicrobial compounds, studying combination therapies, and evaluating agents for treatment of serious infections where rapid bactericidal activity is essential [29].
Two principal standardized guidelines govern the execution of time-kill kinetics assays: the Clinical and Laboratory Standards Institute (CLSI) M26 document, "Methods for Determining Bactericidal Activity of Antimicrobial Agents," and the ASTM International E2315, "Standard Guide for Assessment of Antimicrobial Activity Using a Time-Kill Procedure" [29] [30]. These protocols, while sharing a common objective, are optimized for different applications within antimicrobial research and development. CLSI M26 is primarily oriented toward clinical correlation and predicting bacterial eradication in patients, especially in scenarios involving compromised host immune defenses [29]. In contrast, ASTM E2315 is widely applied in the industrial sector for disinfectant product development, providing a rapid and reproducible means to measure the biocidal potential of liquid antimicrobial formulations [31].
Table 1: Core Applications and Characteristics of CLSI M26 and ASTM E2315
| Feature | CLSI M26 | ASTM E2315 |
|---|---|---|
| Primary Application | Clinical therapeutic development; predicting in vivo efficacy [29] | Disinfectant and antiseptic product development [2] [31] |
| Typical Test Duration | Up to 24 hours [2] | Shorter contact times (seconds to minutes) or up to 24 hours [2] |
| Defining Bactericidal Activity | ≥3 log10 (99.9%) reduction in CFU/mL [2] | Percentage killed over time [31] |
| Testing Model | Predictive model for systemic treatment | "Best-case" suspension model for liquid contact [31] |
| Key Outcome | Bactericidal vs. bacteriostatic classification [2] | Death curve (kill-rate) for biocidal potential [31] |
Theoretical Foundations of Time-Kill Kinetics
Principles of Bactericidal Activity
The fundamental principle underlying time-kill kinetics is the direct quantification of viable microorganisms after exposure to an antimicrobial agent at specified time intervals. The assay monitors the effect of various antimicrobial concentrations throughout the different growth phases of bacteria (lag, exponential, and stationary phase), providing a time-course profile of microbial survival [2]. Bactericidal activity is stringently defined as a ≥3 log10-fold decrease in colony-forming units (CFU) per milliliter, which corresponds to a 99.9% killing of the initial inoculum [2]. An agent that inhibits growth but does not achieve this level of killing is classified as bacteriostatic.
The post-antibiotic effect and the inhibitory effects of sub-MIC antibiotic concentrations are other critical factors that influence the microbiologic response of patients and can be informed by time-kill studies [29]. It is crucial to recognize that clinical cure depends largely upon host factors, and while bactericidal tests provide a rough prediction of bacterial eradication, they are one component of a comprehensive efficacy assessment [29].
Signaling Pathways and Antimicrobial Mechanisms
Antimicrobial agents exert their effects through diverse mechanisms of action, many of which involve targeting specific bacterial pathways. The following diagram illustrates the primary cellular targets and the consequential lethal pathways activated in bacterial cells upon antimicrobial exposure.
CLSI M26 Protocol: Detailed Workflow
Experimental Design and Preparation
The CLSI M26 guideline provides a standardized framework for assessing the bactericidal activity of antimicrobial agents, with a focus on ensuring accurate and reproducible testing that can predict bacterial eradication in clinical settings [29]. The protocol is intended primarily for testing aerobic bacteria that grow in adjusted Mueller-Hinton broth, which may be supplemented with human serum or its ultrafiltrate to simulate certain in vivo conditions [29].
Key preparatory steps include:
- Organism Selection and Inoculum Preparation: Select well-isolated colonies (3-5) from a fresh culture (18-24 hours) to prepare a bacterial suspension. The turbidity of this inoculum must be standardized to a 0.5 McFarland standard, which corresponds to approximately 1-2 x 10^8 CFU/mL [32].
- Antimicrobial Agent Preparation: Prepare serial dilutions of the antimicrobial agent in the chosen broth medium. Testing typically includes concentrations at, above, and below the MIC, as well as a growth control without antimicrobial agent.
- Quality Control Strains: Include appropriate quality control strains to ensure testing conditions, media, and reagents are performing within acceptable limits [32].
Step-by-Step Procedural Workflow
The following diagram outlines the critical stages in the CLSI M26 time-kill kinetics assay, from initial preparation to final data interpretation.
Detailed Protocol:
- Inoculum Standardization: Prepare a bacterial suspension directly from colonies and adjust to a 0.5 McFarland standard [32]. Confirm the initial viable count by serial dilution and plating.
- Reaction Mixture Setup: Combine equal volumes of the standardized inoculum and antimicrobial solution in sterile tubes, resulting in a final bacterial density of approximately 5 x 10^7 CFU/mL. Include a growth control (inoculum + broth without antimicrobial).
- Incubation and Sampling: Incubate the test tubes at 35°C under ambient atmosphere. At predetermined time points (e.g., 0, 4, 8, and 24 hours), remove aliquots from each tube [2].
- Viable Count Determination: Perform serial 10-fold dilutions of each aliquot in a neutralizing solution to stop antimicrobial action. Plate appropriate dilutions onto agar media and incubate for 18-24 hours. Count the resulting colonies and calculate the CFU/mL for each sample and time point.
- Data Analysis and Interpretation: Plot the log10 CFU/mL against time for each antimicrobial concentration and the growth control. A decrease of ≥3 log10 CFU/mL compared to the initial inoculum defines bactericidal activity. A <3 log10 reduction with suppression of growth relative to the control indicates bacteriostatic activity [2].
ASTM E2315 Protocol: Detailed Workflow
Experimental Design and Preparation
The ASTM E2315 standard guide is designed as a flexible framework for measuring the reduction of a microbial population in a liquid suspension after exposure to a test material over time [30]. This method is particularly valuable for disinfectant product developers as a fast, relatively inexpensive, and reproducible way to measure biocidal potential [31].
Key preparatory steps include:
- Test Microorganism Preparation: Prepare microbial cultures as specified. For most bacteria, a 24-hour culture in nutrient broth is suitable. For fungi, a spore preparation from a saline wash is typically used [31].
- Test Substance and Controls: Place equal volumes of the liquid test product in sufficient sterile test vessels. Include a saline control vessel spiked with the same microbial culture to measure initial microbial concentrations and appropriate neutralization controls.
- Contact Time Determination: Pre-determine contact times based on the expected use of the antimicrobial product. These can range from very brief intervals (seconds/minutes) for disinfectants to longer periods (hours) [2] [31].
Step-by-Step Procedural Workflow
The ASTM E2315 procedure focuses on direct interaction between microorganisms and antimicrobials in a liquid suspension, modeling scenarios like disinfectant rinses.
Detailed Protocol:
- Culture Preparation: Grow the test microorganisms under optimal conditions to achieve a high cell density. Adjust the concentration if necessary.
- Test Inoculation: Add a volume of microbial culture (typically 1/10 of the product volume) to the test vessel containing the antimicrobial product and mix immediately. This step marks time zero [31].
- Sampling and Neutralization: After predetermined contact times, remove small aliquots from the mixture and transfer them to a solution containing an appropriate neutralizer to stop the antimicrobial action effectively.
- Viable Count Determination: Perform serial dilutions of the neutralized samples and plate onto appropriate agar media. Incubate plates and count the resulting colonies to determine the surviving CFU/mL at each time point.
- Data Analysis: Plot the number of surviving microorganisms (log10 CFU/mL) against time to generate a "death curve." Calculate the percentage reduction in viability at each time point compared to the initial concentration determined from the saline control [31].
Comparative Analysis and Data Interpretation
Key Differences and Applications
While both CLSI M26 and ASTM E2315 assess antimicrobial activity over time, their design philosophies reflect their distinct applications. CLSI M26 establishes uniform test procedures to permit comparison of different datasets with a focus on clinical correlation, especially for situations like endocarditis where bactericidal activity is crucial [29]. The methodology is evolving and requires more work on methodological aspects and clinical correlations [29]. In contrast, ASTM E2315 offers a more flexible framework that is particularly suited for industrial product development, providing a "best-case" scenario for evaluating liquid antimicrobial formulations [31].
A critical methodological difference lies in the neutralization step. ASTM E2315 explicitly requires immediate neutralization of the antimicrobial agent upon sampling to precisely define the contact time [31]. While CLSI M26 also implies this step, its emphasis is on the standardized growth conditions and the definition of bactericidal activity. Furthermore, the growth medium in CLSI M26 is specifically defined as adjusted Mueller-Hinton broth, potentially supplemented with human serum, to better simulate certain in vivo conditions [29].
Table 2: Direct Comparison of CLSI M26 and ASTM E2315 Methodologies
| Parameter | CLSI M26 | ASTM E2315 |
|---|---|---|
| Inoculum Standardization | 0.5 McFarland Standard [32] | Broth culture or spore suspension [31] |
| Typical Inoculum Size | ~5 x 10^7 CFU/mL (final) | High concentration (volume: 1/10 of product) [31] |
| Growth Medium | Adjusted Mueller-Hinton Broth (± human serum) [29] | Not specified (liquid test substance as environment) [31] |
| Incubation Atmosphere | Ambient air [32] | Not specified (dependent on test system) |
| Sampling Time Points | e.g., 0, 4, 8, 24 hours [2] | Pre-determined contact times (flexible) [30] |
| Neutralization | Implied for accurate counts | Explicitly required post-sampling [31] |
| Key Data Output | Log10 CFU/mL reduction over time [2] | Percentage killed over time; Death curve [31] |
Data Interpretation and Quality Control
Robust data interpretation and quality assurance are fundamental to both protocols. For CLSI M26, the primary endpoint is the classification of an agent as bactericidal (≥3 log10 reduction), bacteriostatic, or inactive based on the reduction from the initial inoculum [2]. The growth control must show adequate growth to validate the test conditions.
In ASTM E2315, results are often presented as kill curves showing the rate of microbial death, and the percentage reduction is calculated for each contact time. The method's strength is its ability to study the impact of a disinfectant on microorganisms over time with relative ease and under controlled parameters [31].
For both standards, implementation of a robust quality assurance program is critical. This includes using quality control strains to verify testing conditions, ensuring staff competency, and participating in proficiency testing programs to maintain accuracy and consistency [32]. Furthermore, all materials and reagents must be of verified quality to ensure reliable and reproducible results.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of time-kill kinetics assays requires carefully selected and quality-controlled materials. The following table details the essential components of the researcher's toolkit for these studies.
Table 3: Key Research Reagent Solutions for Time-Kill Kinetics Assays
| Reagent/Material | Function & Purpose | Specification & Notes |
|---|---|---|
| Adjusted Mueller-Hinton Broth | Standard growth medium for CLSI M26; ensures reproducible ion concentration and pH [29]. | Must be formulated according to CLSI specifications; may be supplemented with human serum or ultrafiltrate [29]. |
| Quality Control Strains | Verifies performance of test systems, media, and reagents [32]. | Strains with established zone/MIC ranges (e.g., S. aureus ATCC 29213); used for periodic QC testing. |
| McFarland Standards | Turbidity standard for inoculum preparation and standardization [32]. | 0.5 McFarland standard (~1.5 x 10^8 CFU/mL) is typically used for broth inoculation. |
| Neutralizing Solution | Inactivates antimicrobial agent at specific time points to stop killing action [31]. | Critical for accurate contact times in ASTM E2315; composition depends on test agent (e.g., polysorbate, lecithin, thiosulfate). |
| Agar Media for Enumeration | Supports growth of survivors for viable counting via colony formation. | Non-selective media like Tryptic Soy Agar; must be validated for recovery of test organisms. |
| Antimicrobial Reference Powders | Provides known active agents for comparison and control. | High-purity, potency-certified materials for preparing stock solutions and serial dilutions. |
Within the framework of a thesis investigating time-kill kinetics assays for antimicrobial evaluation, the integrity of the research data is fundamentally dependent on the precise selection and preparation of critical reagents. The time-kill kinetics assay is a powerful method used to study the bactericidal or bacteriostatic activity of an antimicrobial agent over time, characterizing the rate and extent of microbial killing [2]. Its reliability, however, is profoundly influenced by foundational elements: the growth medium supporting the microorganisms, the accurately prepared antimicrobial stock solutions, and the effective neutralizers that halt antimicrobial action at specified time points. Missteps in these preparatory stages can introduce significant variability, compromising the validity of kinetic profiles. This protocol provides detailed methodologies for the preparation of these critical reagents, ensuring the generation of reproducible, high-quality data essential for robust antimicrobial research and drug development.
Media Selection for Time-Kill Assays
The Role of Growth Media
The culture medium serves as the physicochemical environment for the test microorganisms, directly influencing their growth rate, metabolic state, and, consequently, their susceptibility to antimicrobial agents. An inappropriate medium can lead to poor bacterial growth, sub-inhibitory concentrations of the antimicrobial due to binding or inactivation, or chemical interactions that alter the agent's effective concentration. The primary goal is to select a medium that supports robust, standardized growth of the inoculum without interfering with the activity of the compound being tested.
Common Media and Selection Criteria
Mueller Hinton Broth (MHB) is frequently the medium of choice for time-kill assays against bacteria, particularly when following Clinical & Laboratory Standards Institute (CLSI) guidelines [2] [33]. Its widespread use is attributed to its well-defined composition and reproducibility, providing a reliable baseline for comparative studies.
Table 1: Common Media for Bacterial Cultivation in Antimicrobial Assays
| Media Name | Common Applications | Key Characteristics | Considerations for Time-Kill Assays |
|---|---|---|---|
| Mueller Hinton Broth (MHB) | Standard for antibacterial susceptibility testing (CLSI) | Well-defined composition, low antagonist levels | Supports consistent growth; may require supplementation for fastidious organisms. |
| Nutrient Broth | General cultivation of non-fastidious bacteria | Complex, undefined mixture | Cost-effective; batch-to-batch variability may affect reproducibility. |
| Iso-Sensitest Broth | Alternative for susceptibility testing | Defined formulation aimed at reducing variability | Can be used for enhanced reproducibility in research settings. |
| SYP Agar/Mannitol Soybean Agar | Screening for antimicrobial production [34] | Supports secondary metabolite production | May be used in specialized contexts for producer organisms. |
Researchers must also consider the requirements of specific microbial strains. For instance, evaluating antimicrobial production from bacterial strains may require screening on specialized media like SYP or mannitol soybean agar to optimize compound production [34]. The medium must not only support growth but also maintain the stability and activity of the antimicrobial agent throughout the experiment.
Preparation of Antimicrobial Stock Solutions
Solvent Selection and Preparation
The choice of solvent is critical for dissolving the antimicrobial agent without inactivating it or being toxic to the test microorganisms. A common practice is to use a small volume of a high-quality solvent to dissolve the compound fully before diluting it to the working stock concentration in a more biocompatible solvent like sterile water or culture media.
- Common Solvents: Dimethyl sulfoxide (DMSO) is widely used for its ability to dissolve a broad spectrum of organic compounds [22]. Sterile water is suitable for water-soluble compounds, while dilute acids or bases may be needed for others.
- Concentration: Stock solutions are typically prepared at high concentrations (e.g., 1-10 mg/mL) to minimize the final solvent concentration in the assay.
- Quality Control: Use high-purity, sterile solvents. The chemical stability of the stock solution under storage conditions (e.g., -20°C or -80°C) must be verified.
- Vehicle Controls: Every assay must include a vehicle control (e.g., the same final concentration of DMSO in broth) to account for any effects of the solvent on microbial growth [2].
A documented example is the dissolution of plumbagin in DMSO for antimicrobial testing, demonstrating a standard approach for hydrophobic natural products [22].
Determining Test Concentrations
The concentrations tested in a time-kill assay are often anchored to the Minimum Inhibitory Concentration (MIC). A typical assay might evaluate concentrations at 0.5x, 1x, 2x, and 4x the MIC to characterize concentration-dependent effects [22]. The MIC is pre-determined using standardized methods like broth microdilution in 96-well plates, with growth indicated by colorimetric dyes like MTT [22].
Neutralizers in Time-Kill Kinetics
The Principle of Neutralization
A fundamental challenge in time-kill assays is ensuring that the reduction in viable count at a specific time point reflects killing by the antimicrobial agent and not merely transient inhibition. If a small amount of the antimicrobial is carried over during the plating process, it can continue to act in the agar plate, preventing the growth of viable but stressed cells and leading to an overestimation of killing efficacy. Neutralizers are substances that chemically inactivate residual antimicrobial agents in a sample, allowing an accurate quantification of surviving colony-forming units (CFU) [35].
Selecting an Appropriate Neutralizing System
The choice of neutralizer depends entirely on the chemical nature of the antimicrobial agent being tested. No single universal neutralizer exists, so a system must be selected to match the test compound.
Table 2: Common Neutralizers and Their Applications
| Neutralizing Agent / Medium | Target Antimicrobials/Chemicals | Mechanism of Action |
|---|---|---|
| Lecithin | Quaternary ammonium compounds, Ethanol (in combination with Polysorbate 80) | Binds and inactivates surfactants and disinfectants. |
| Polysorbate 80 (Tween 80) | Phenolics, Hexachlorophene, Formalin, Ethanol | Acts as a dispersing agent, sequestering phenolic and other molecules. |
| Letheen Media | Contains Lecithin and Polysorbate 80; neutralizes quaternaries, phenolics, ethanol, formalin, hexachlorophene. | Combined action of its components provides broad neutralization. |
| D/E Neutralizing Media | Broad-spectrum: quaternary ammonium compounds, phenols, iodine, chlorine, mercurials, formaldehyde, glutaraldehyde. | Formulated with multiple agents to inactivate a wide array of germicides. |
| Sodium Thiosulfate | Halogens (Iodine, Chlorine) | Reduces and inactivates halogen-based compounds. |
| Histidine / Cysteine | Aldehydes (Formaldehyde, Glutaraldehyde) | Reacts with and neutralizes aldehyde groups. |
The CDC guidelines recommend employing neutralizing media like Letheen Media or D/E Neutralizing Media to overcome the problem of disinfectant carryover during subculturing [35]. It is crucial to validate that the chosen neutralizer effectively inactivates the antimicrobial agent and is not toxic to the test microorganism.
Integrated Experimental Workflow
The following diagram illustrates the logical relationship and workflow between the three critical reagent systems discussed in this protocol, within the context of a time-kill kinetics assay.
The Scientist's Toolkit: Research Reagent Solutions
The following table details the essential materials and reagents required for executing a time-kill kinetics study, as discussed in this application note.
Table 3: Essential Reagents for Time-Kill Kinetics Assays
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Culture Media | Mueller Hinton Broth (MHB), Nutrient Broth | Provides nutrients for microbial growth; standardizes physiological state of inoculum. |
| Antimicrobial Solvents | Dimethyl Sulfoxide (DMSO), Sterile Water | Dissolves test compounds for preparation of stock solutions; must be non-inhibitory. |
| Neutralizing Media | Letheen Media, D/E Neutralizing Media | Inactivates carried-over antimicrobial agent during plating, ensuring accurate CFU counts. |
| Reference Standards | Ciprofloxacin, Amoxicillin, Ketoconazole | Provides benchmark for antimicrobial activity and validates assay performance. |
| Viability Indicators | MTT dye, Resazurin | Used in preliminary MIC tests to indicate microbial growth metabolically. |
| Buffers & Diluents | Phosphate Buffered Saline (PBS), Saline | Used for serial dilutions of samples for CFU plating and inoculum preparation. |
Concluding Remarks
The meticulous preparation of media, antimicrobial stock solutions, and neutralizers is not merely a preliminary step but the cornerstone of a reliable and reproducible time-kill kinetics assay. Proper media selection ensures optimal and consistent microbial growth, accurate stock solution preparation guarantees that the tested concentrations are precise, and effective neutralization confirms that the measured kill kinetics are genuine and not an artifact of the methodology. By adhering to the detailed protocols outlined in this document, researchers can significantly reduce variability, enhance data quality, and contribute robust findings to the critical field of antimicrobial discovery and development.
This application note provides a detailed protocol for standardizing bacterial inocula to achieve a precise starting concentration of 1–5 × 10^5 CFU/mL, a critical prerequisite for reliable time-kill kinetics assays in antimicrobial evaluation research. We outline robust methodologies for preparing mid-log phase cultures, standardizing turbidity, and verifying colony counts, supplemented by technical insights on calibration and quality control to ensure data reproducibility and accuracy for research scientists and drug development professionals.
In antimicrobial research, the physiological state and initial concentration of the microbial inoculum are fundamental variables that significantly influence the outcome of time-kill kinetics studies. A standardized inoculum ensures that the observed antimicrobial effect is attributable to the agent being tested rather than experimental variability. Time-kill kinetics assays, which plot the log10 CFU/mL against time, require a starting inoculum within a specific range (e.g., 1–5 × 10^5 CFU/mL) to accurately distinguish between bactericidal (≥3 log10 reduction) and bacteriostatic activity [2]. This protocol details the steps to achieve a reproducible mid-log phase culture and accurately standardize it to the target concentration, forming a cornerstone for reliable antimicrobial efficacy testing.
Theoretical Background: The Bacterial Growth Cycle
Understanding the bacterial growth cycle is essential for harvesting cells at the correct physiological state.
- Lag Phase: A period of metabolic adaptation and preparation for rapid growth following inoculation into fresh medium. Cells are metabolically active but not yet dividing [36].
- Exponential (Log) Phase: The period of balanced growth characterized by constant, maximal cell division rates. Cells in this phase are uniformly metabolically active and are considered the standard for most antimicrobial susceptibility tests [36].
- Stationary Phase: Growth ceases due to nutrient depletion and/or accumulation of waste products. Cells undergo significant physiological changes and may exhibit increased stress resistance [36].
The objective of this protocol is to consistently harvest cells during the mid-log phase, where they are most uniform and predictable.
Materials and Equipment
Research Reagent Solutions
Table 1: Essential reagents and materials for inoculum standardization.
| Item | Function/Application |
|---|---|
| Non-selective Agar Plates (e.g., Tryptic Soy Agar, Mueller-Hinton Agar) | For cultivation and isolation of test organisms from pure stocks. |
| Sterile Broth Media (e.g., Mueller-Hinton Broth, Tryptic Soy Broth) | For growing liquid cultures for inoculum preparation and dilution. |
| Sterile Saline (0.85-0.9% NaCl) | For making serial dilutions of bacterial suspensions without causing osmotic shock. |
| McFarland Standards (0.5) | The gold-standard reference for visually or spectrophotometrically standardizing turbidity to ~1.5 x 108 CFU/mL [37]. |
| Barium Chloride Dihydrate (BaCl₂·2H₂O) & Sulfuric Acid (H₂SO₄) | Reagents for the laboratory preparation of McFarland standards [37]. |
Experimental Protocol
Preparation of a Mid-Log Phase Culture
The following workflow outlines the complete process for obtaining a standardized mid-log phase inoculum.
Detailed Procedure:
- Subculture Initiation: Using a sterile loop, select 3-5 well-isolated colonies of identical morphology from a fresh agar plate (incubated for 18-24 hours) [37].
- Inoculation: Transfer the colonies into a flask containing 10-50 mL of appropriate sterile broth medium (e.g., Mueller-Hinton Broth). The flask volume should be at least 5 times the medium volume to ensure proper aeration.
- Incubation and Monitoring: Incubate the flask at the optimal temperature for the test organism (typically 35±2°C) with constant, vigorous shaking. Monitor the optical density at 600 nm (OD600) periodically.
- Harvesting: Once the OD600 reaches approximately 0.1 to 0.3, the culture is in the mid-log phase. Proceed immediately to standardization. Delays can allow the culture to progress into late-log or stationary phase, altering cell physiology.
Inoculum Standardization via Turbidity
The mid-log phase culture must now be diluted to the target concentration for the time-kill assay.
Detailed Procedure:
- Turbidity Adjustment:
- Vortex the mid-log phase culture thoroughly.
- Transfer a portion to a sterile tube and compare its turbidity against a 0.5 McFarland standard against a Wickerham card with black lines [37].
- If the suspension is too light, add more cellular material. If it is too turbid, dilute with sterile saline or broth.
- A properly standardized 0.5 McFarland suspension corresponds to approximately 1.5 x 108 CFU/mL for bacteria like E. coli [37].
- Dilution to Target Concentration:
- Perform an aseptic dilution of the 0.5 McFarland suspension to achieve the final target of 1–5 x 105 CFU/mL.
- A 1:1500 dilution is typically effective. For example, adding 10 µL of the standardized suspension to 15 mL of broth yields a theoretical concentration of 1 x 105 CFU/mL.
Verification by Colony Forming Units (CFU) Count
Theoretical calculations must be confirmed empirically.
- Serial Dilution: Perform a serial 10-fold dilution of the final inoculum in sterile saline (e.g., 10-1 to 10-5).
- Plating: Spread-plate 100 µL aliquots from appropriate dilutions (e.g., 10-3 and 10-4) onto agar plates in duplicate.
- Incubation and Counting: Incubate plates for 18-24 hours. Count the colonies on plates bearing 30-300 colonies.
- Calculation: Calculate the CFU/mL using the formula: [ \text{CFU/mL} = \text{Number of colonies} \times \text{Dilution Factor} \times 10 ] (The factor of 10 accounts for plating 0.1 mL instead of 1 mL). The result must fall within the 1–5 x 105 CFU/mL range for the inoculum to be valid.
Data Presentation and Calibration
Critical Calibration Parameters
Table 2: Key considerations for accurate optical density measurements and inoculum calibration.
| Parameter | Consideration & Impact |
|---|---|
| Cell Size & Morphology | The relationship between OD and cell concentration is highly dependent on cell size. For a given OD, smaller cells yield a higher concentration. Filamentation or other morphological changes under stress can drastically alter this relationship [38]. |
| Growth Conditions | The calibration curve (OD vs. CFU/mL) can change with media composition, leading to different cell sizes [38]. |
| Instrumentation | Different spectrophotometers and microplate readers can yield different OD readings for the same sample due to variations in detector geometry and light path [38]. |
| Correlation Method | Direct cell counting (microscopy) is more accurate for generating calibration curves than CFU plating, as the latter only counts viable cells [38]. |
Table 3: Example calibration data for E. coli under different growth conditions.
| Growth Condition | Approx. Cell Size (µm) | OD₆₀₀ | Corresponding Concentration (CFU/mL) |
|---|---|---|---|
| Minimal Media | 1 x 2 | 0.1 | ~2.5 x 10⁷ |
| Rich Media (LB) | 1.2 x 2.5 | 0.1 | ~1.8 x 10⁷ |
| LB + Sub-MIC Ampicillin | Filamentous (>10) | 0.1 | ~3.0 x 10⁶ |
Troubleshooting and Best Practices
- Inconsistent Lag Times: Ensure the pre-culture is always prepared from fresh colonies and incubated for a standardized duration to achieve a consistent physiological state [36].
- Inoculum Too High/Low After Standardization: Verify the preparation and mixing of the McFarland standard. Confirm the accuracy of pipettes used for dilution. Always perform CFU verification for critical assays.
- Subjectivity in Turbidity Comparison: For high-precision work, replace visual McFarland comparison with a spectrophotometer. Calibrate the OD600 reading against a CFU count for your specific organism and growth conditions to create a custom standard curve [38].
- Quality Control of McFarland Standards: Store laboratory-prepared standards in the dark at room temperature and check their absorbance spectrophotometrically at 625 nm before use. The acceptable range for a 0.5 McFarland standard is typically 0.08 - 0.10 [37].
The time-kill kinetics assay is a fundamental in vitro method used to characterize the bactericidal or bacteriostatic activity of an antimicrobial agent over time [2]. In the context of antimicrobial resistance (AMR), a formidable global challenge, this assay provides critical insights beyond the static endpoint data provided by minimum inhibitory concentration (MIC) determinations [23]. By quantifying the rate and extent of microbial killing, researchers can determine the pharmacodynamic profile of a novel compound, essential for predicting its in vivo efficacy and for guiding dosage regimen design in subsequent drug development stages. This protocol details the establishment of antimicrobial concentration ranges and the indispensable control groups required for a robust and interpretable time-kill kinetics study, framed within a comprehensive antimicrobial evaluation thesis.
Theoretical Basis of the Assay
Key Definitions and Parameters
- Minimum Inhibitory Concentration (MIC): The lowest concentration of an antimicrobial agent that completely inhibits visible growth of a microorganism under defined in vitro conditions. This value serves as the benchmark for setting the concentration range in a time-kill study.
- Bactericidal Activity: Defined as a ≥3 log₁₀ (99.9%) reduction in the colony-forming units (CFU/mL) of the original inoculum over a specified time [2]. Agents demonstrating this level of killing are considered cidal.
- Bacteriostatic Activity: Defined as a <3 log₁₀ reduction in CFU/mL, where the agent inhibits growth but does not kill a significant portion of the inoculum [5] [2].
- Minimum Bactericidal Concentration (MBC): The lowest concentration of an antimicrobial agent that results in a 99.9% reduction (≥3 log₁₀ kill) of the initial inoculum at a specified time, typically 24 hours [2].
Experimental Design and Setup
Determining Antimicrobial Concentration Ranges
The concentration range should be carefully selected to bracket the MIC and elucidate the concentration-dependent nature of the antimicrobial's effect. A typical range is a serial dilution of the test agent, prepared in a suitable broth medium.
Table 1: Suggested Antimicrobial Concentration Range for Time-Kill Kinetics Assays
| Concentration Multiples of MIC | Final Concentration | Purpose and Expected Outcome |
|---|---|---|
| 16× MIC | [Calculated Value] | To evaluate potential tidal activity at high concentrations and assess the impact of concentration on the killing rate. Often used for agents with concentration-dependent killing. |
| 8× MIC | [Calculated Value] | |
| 4× MIC | [Calculated Value] | A key concentration to confirm tidal activity (if achieved). |
| 2× MIC | [Calculated Value] | To determine if the effect is tidal or static just above the inhibitory threshold. |
| 1× MIC | [Calculated Value] | The inhibitory threshold; growth should be statistically equivalent to the initial inoculum (static effect) if the agent is purely bacteriostatic. |
| 0.5× MIC | [Calculated Value] | A sub-inhibitory concentration where some limited growth may occur, useful for understanding sub-MIC effects. |
| 0.25× MIC | [Calculated Value] | |
| 0.125× MIC | [Calculated Value] | |
| 0.063× MIC | [Calculated Value] | |
| 0.032× MIC | [Calculated Value] | Lower end of the range to study potential post-antibiotic effects or other phenomena at very low concentrations. |
| 0.016× MIC | [Calculated Value] | The lowest concentration tested, helping to define the full pharmacodynamic curve. |
- Preparation: Prepare a stock solution of the antimicrobial agent. Perform a two-fold serial dilution in the appropriate broth (e.g., Mueller-Hinton Broth) to achieve the final desired concentrations in the test tubes or wells. The final volume must accommodate sampling at each time point without significant volume loss.
Essential Control Groups
Inclusion of proper controls is non-negotiable for validating the experimental results. Each control serves a specific purpose in data interpretation.
Table 2: Required Control Groups for Time-Kill Kinetics Assays
| Control Group | Preparation | Purpose and Interpretation |
|---|---|---|
| Growth Control | Inoculated broth medium without any antimicrobial agent. | Serves as the baseline for uninhibited microbial growth. A steady increase in CFU/mL over time confirms organism viability and proper growth conditions. The killing in test groups is calculated relative to the initial inoculum and compared to this control. |
| Vehicle Control | Inoculated broth medium with the highest concentration of the solvent used (e.g., DMSO, ethanol). | Ensures that any observed antimicrobial effect is due to the agent itself and not the solvent. The growth curve should closely resemble the Growth Control. |
| Time-Zero Control | Sample taken immediately after inoculation and addition of the antimicrobial agent (Time = 0 hours). | Precisely defines the baseline CFU/mL from which all subsequent killing is measured. This is the reference point for calculating log reduction. |
| Reference Control | Inoculated broth medium with a known standard antibiotic (e.g., ciprofloxacin). | Validates the methodology and the sensitivity of the microbial strain. Provides a benchmark for comparing the killing kinetics of the test agent. |
| Sterility Control (Blank) | Uninoculated broth medium, with and without the antimicrobial agent. | Confirms the aseptic preparation of media and reagents. The absence of growth throughout the experiment verifies that no contamination occurred. |
Workflow and Data Interpretation
Experimental Workflow
The following diagram outlines the key steps in a time-kill kinetics assay:
Interpreting Time-Kill Curves
The data from colony counts is used to generate time-kill curves, which are critical for determining the agent's mode of action.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions and Materials
| Item | Function / Purpose | Examples / Notes |
|---|---|---|
| Broth Dilution Media | Provides nutrients for microbial growth during the assay. The standard medium for most bacteria is Mueller-Hinton Broth (MHB). | Cation-adjusted MHB is used for Pseudomonas aeruginosa and other non-fastidious organisms [23]. |
| Agar Media | Solid medium used for determining viable colony counts (CFU/mL) via the plate count method. | Mueller-Hinton Agar (MHA); Blood Agar for fastidious organisms. |
| Reference Antibiotics | Used as a positive control to validate the test system and provide a benchmark for the test agent's activity. | Ciprofloxacin (for Gram-negatives), Vancomycin (for Gram-positives), Ketoconazole (for fungi) [5]. Purity should be high (e.g., ≥98% HPLC). |
| Sterile Solvents/Diluents | For reconstituting and diluting hydrophobic or solid antimicrobial agents. The solvent must be non-toxic to the test organism at the concentrations used. | Dimethyl Sulfoxide (DMSO), Ethanol, Water. A Vehicle Control is mandatory [5]. |
| Saline or Phosphate Buffered Saline (PBS) | Used for making serial dilutions of samples taken at various time points to achieve a countable number of colonies (typically 30-300 CFU per plate). | Must be sterile and isotonic to prevent osmotic shock to the cells during dilution. |
| Automated Colony Counter / Imaging System | For accurate and efficient enumeration of colony-forming units on agar plates. Reduces human error and increases throughput. | Alternatively, manual counting with a pen tally and a dark-field colony counter can be used. |
| Microplate Reader (Spectrophotometer) | Can be used to monitor microbial growth turbidimetrically (OD600) in parallel with the gold-standard CFU count, providing supplementary data on growth dynamics. | CFU plating remains the definitive method for determining viable counts in time-kill studies. |
Protocol and Best Practices
Detailed Procedural Steps
- Preparation: Determine the MIC of the test agent against the target strain using CLSI or EUCAST broth microdilution methods. Prepare all control groups as described in Table 2.
- Inoculum Standardization: Grow the test organism to mid-log phase and adjust the turbidity to a 0.5 McFarland standard, resulting in a final inoculum density of approximately 1-5 x 10⁸ CFU/mL. Further dilute the suspension in broth to achieve a final test concentration of ~5 x 10⁵ CFU/mL in each test tube or well.
- Assay Initiation: Add the standardized inoculum to the pre-diluted antimicrobial solutions and control tubes. This is Time Zero. Immediately remove a sample (e.g., 100 µL) from the growth control and one from each antimicrobial concentration for the Time-Zero control.
- Incubation and Sampling: Inculate the test tubes at the appropriate temperature (e.g., 35±2°C) with constant shaking. Remove samples from all tubes at predetermined time intervals (e.g., 0, 2, 4, 6, 8, and 24 hours).
- Viable Count Determination: Perform serial 10-fold dilutions of each sample in sterile saline or PBS. Plate a fixed volume (e.g., 10-100 µL) of each dilution onto pre-dried agar plates in duplicate. Incubate the plates for 18-24 hours (or as required) and count the colonies.
- Data Analysis: Calculate the log₁₀ CFU/mL for each sample. Plot the mean log₁₀ CFU/mL versus time for each concentration and control. Determine if the antimicrobial effect is bactericidal (≥3 log₁₀ kill) or bacteriostatic at each concentration and time point.
Critical Considerations for Reproducibility
- Inoculum Viability: The initial inoculum must be from a fresh, actively growing culture to ensure consistent results across experiments.
- Sampling Frequency: The choice of time points should capture the critical phases of killing—the initial rapid kill phase and any potential regrowth.
- Methodology Adherence: All testing should follow established guidelines, such as those from the Clinical & Laboratory Standards Institute (CLSI M26 document) or ASTM [2].
- Data Reporting: Clearly report the starting inoculum density, the specific concentrations tested (as multiples of MIC), and the data from all control groups to provide context for the kill curves.
Within the framework of antimicrobial evaluation research, the time-kill kinetics assay is a cornerstone method for characterizing the dynamic, concentration-dependent bactericidal activity of novel therapeutic agents [39] [4]. This assay provides longitudinal data that surpasses the static snapshot offered by the Minimum Inhibitory Concentration (MIC), revealing the rate and extent of microbial killing over time [1]. The critical component of this assay—the accurate quantification of bacterial burden at sequential time points—relies heavily on the precise techniques of serial dilution and viable count enumeration. This protocol details the methodologies for these supporting techniques, which are essential for generating reliable data on the concentration-effect relationship of antimicrobial compounds against planktonic cultures [4].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential materials and reagents required for executing serial dilution and viable plate counts in the context of time-kill studies.
Table 1: Essential Materials and Reagents for Serial Dilution and Viable Count Enumeration
| Item | Function/Explanation |
|---|---|
| Mueller-Hinton (MH) Broth | A standardized, non-fastidious growth medium recommended for antimicrobial susceptibility testing, ensuring reproducible bacterial growth conditions [40]. |
| Sterile Diluent (e.g., Water or Saline) | A sterile, isotonic solution used to systematically reduce the concentration of the bacterial sample without causing cell lysis or osmotic shock [41]. |
| Nutrient Agar Plates | Solid culture media used to support the growth of viable microorganisms after the dilution process, enabling the formation of countable colonies [42]. |
| Sterile L-shaped Cell Spreaders | Also known as "hockey sticks," these tools are used to evenly distribute a small volume of the diluted sample across the surface of an agar plate, promoting the growth of well-isolated colonies [42]. |
| Reference Bacterial Strains | Quality control strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) with known antimicrobial susceptibility profiles, used to validate assay performance [40]. |
| Calibrated Pipettes and Sterile Tips | Essential for the accurate and aseptic transfer of specific liquid volumes during the serial dilution process, minimizing experimental error [42] [41]. |
Quantitative Data from Antimicrobial Evaluation
The following table summarizes exemplary quantitative data obtained from a recent study investigating the efficacy of a novel antimicrobial peptide, SK1260, against a panel of bacterial pathogens using MIC and time-kill assays [39].
Table 2: In vitro Antimicrobial Activity and Efficacy of SK1260 [39]
| Bacterial Strain | MIC (µg/mL) | Time-Kill Assay Result (at ≥1× MIC) |
|---|---|---|
| S. aureus ATCC 6538 | 3.13 - 12.5 | Complete bacterial clearance, comparable to ciprofloxacin |
| MRSA ATCC 43300 | 3.13 - 12.5 | Complete bacterial clearance, comparable to ciprofloxacin |
| E. coli ATCC 8739 | 3.13 - 12.5 | Complete bacterial clearance, comparable to ciprofloxacin |
| K. pneumoniae ATCC 700603 | 3.13 - 12.5 | Complete bacterial clearance, comparable to ciprofloxacin |
| P. aeruginosa ATCC 9027 | 3.13 - 12.5 | Complete bacterial clearance, comparable to ciprofloxacin |
Experimental Protocols
Protocol for Broth Microdilution for MIC Determination
This procedure is based on international standards (CLSI, ISO 20776-1:2020) for determining the Minimum Inhibitory Concentration [39] [40].
Preparation of Antimicrobial Stock Solution:
- Weigh the antimicrobial agent using a pre-calibrated analytical balance [40].
- Dissolve the powder in a suitable solvent to create a high-concentration stock solution (e.g., ≥ 1 g/L). For commercial antibiotics, factor in the powder potency to calculate the correct mass using the formula:
m = (V * c) / P, wheremis mass (mg),Vis volume (mL),cis concentration (µg/mL), andPis potency (µg/mg) [40]. - For experimental compounds with unknown potency, determine the stock concentration spectrophotometrically using the Beer-Lambert law if the molar extinction coefficient is known [40].
Preparation of Bacterial Inoculum:
- Pre-culture the sourced bacteria in Mueller-Hinton (MH) Broth at 35 ± 1°C for 18-24 hours [40].
- Adjust the optical density of the culture at 625 nm to match that of a 0.5 McFarland Standard (OD625 ~0.1), corresponding to approximately 1-2 × 10^8 Colony-Forming Units per milliliter (CFU/mL) [40].
- Further dilute this suspension in MH broth to a final concentration of about 10^6 CFU/mL for testing [40].
- CRITICAL: Perform purity checks and viable colony counts to ensure the accuracy of the inoculum and avoid contamination [40].
Microdilution and Incubation:
- Prepare a series of two-fold dilutions of the antimicrobial agent in a 96-well microtiter plate, covering a concentration range (e.g., 0.75 to 100 µg/mL) [39] [40].
- Add the prepared bacterial inoculum to each well, resulting in a final testing concentration of approximately 10^5 CFU/mL [39].
- Include a positive growth control (bacteria without antimicrobial) and a negative sterility control (broth only) on each plate.
- Incubate the plate under suitable conditions (e.g., 35 ± 1°C for 18-24 hours) [40].
Determination of MIC:
Protocol for Serial Dilution and Viable Plate Count
This protocol describes the steps for performing serial dilutions and spread plating to quantify viable bacteria from time-kill assay samples [42] [41].
Preparation:
Serial Dilution Process:
- Aseptically transfer 1.0 mL from the initial bacterial sample (e.g., a sample taken from a time-kill assay) into the first tube containing 9.0 mL of diluent. This creates a 10^-1 dilution [41].
- Mix the tube thoroughly, ensuring a homogeneous suspension. A vortex mixer can be used [42] [41].
- Change the pipette tip to prevent carryover of a high concentration of cells [42].
- Transfer 1.0 mL from the 10^-1 dilution tube to the next tube (9.0 mL diluent), creating a 10^-2 dilution. Mix thoroughly [41].
- Continue this process sequentially to achieve the desired range of dilutions. A cumulative dilution of 10^-6 to 10^-8 is often necessary for samples from time-kill assays [39] [42].
Spread Plating and Incubation:
- Using a new pipette tip for each dilution, transfer 100 µL (0.1 mL) from selected dilution tubes onto the center of the correspondingly labeled agar plates [42].
- Use a sterile, L-shaped cell spreader to distribute the liquid evenly across the agar surface. Allow the liquid to be fully absorbed by the agar [42].
- Invert the plates and incubate them at the appropriate temperature (e.g., 37°C) for 24-48 hours [42] [1].
Enumeration and Calculation:
- After incubation, select plates that contain between 30 and 300 well-isolated colonies for counting [42].
- Count the colonies and calculate the viable bacterial concentration in the original sample using the formula:
CFU/mL = (Number of colonies counted) / (Dilution factor × Volume plated in mL)[42]. - For example, if 85 colonies are counted on the 10^-6 dilution plate, and 0.1 mL was plated: CFU/mL = 85 / (10^-6 × 0.1) = 8.5 × 10^8 [42].
Workflow and Data Analysis Visualization
Experimental Workflow for Time-Point Sampling and Enumeration
The following diagram illustrates the logical sequence and key steps involved in processing samples from a time-kill assay to obtain quantitative viable count data.
Serial Dilution Scheme and Calculations
This diagram outlines the procedural steps and corresponding calculations for a standard serial dilution, which is fundamental to achieving countable colonies.
Time-kill kinetics assays are a cornerstone of antimicrobial evaluation, providing dynamic, longitudinal data on the interaction between a potential antimicrobial agent and a microorganism. Unlike static endpoints such as the minimum inhibitory concentration (MIC), time-kill kinetics reveal the rate and extent of microbial lethality over time, offering critical insights into whether an agent exerts bacteriostatic (growth-inhibiting) or bactericidal (lethal) activity [5] [43]. This protocol details the methodology for quantifying bacterial burden via Colony Forming Units (CFU), generating Log CFU/mL versus time graphs, and analytically determining kill rates, forming an essential component of a comprehensive thesis on antimicrobial evaluation.
Experimental Protocol for Time-Kill Assay and Sampling
Materials and Reagent Preparation
Table 1: Essential Research Reagents and Materials
| Item | Function/Description |
|---|---|
| Luria-Bertani (LB) Broth | Standard liquid growth medium for bacterial culture [44]. |
| LB Agar Plates | Solidified medium (1.5% w/v agar) in Petri dishes for CFU enumeration [44]. |
| Phosphate Buffered Saline (PBS) | Sterile diluent for creating serial dilutions of bacterial culture [44]. |
| Test Antimicrobial Agent | The compound under investigation (e.g., Thymoquinone [43] or mushroom extracts [5]). |
| Sterile Erlenmeyer Flasks | For bulk culture growth; use a 1:5 ratio of media volume to flask volume [44]. |
| Spectrophotometer | For measuring optical density (OD₆₀₀) to approximate cell density [44]. |
Procedural Workflow
The following diagram outlines the core workflow for executing a time-kill kinetics assay.
Detailed Methodology
- Culture Inoculation: Prepare an overnight liquid culture of the test organism from a single colony [44]. On the experiment day, dilute the overnight culture into fresh, pre-warmed media within an Erlenmeyer flask to a standard starting density (e.g., ~5 × 10⁵ CFU/mL) [43].
- Agent Addition and Sampling: At time zero, add the antimicrobial agent at the desired concentration (e.g., the Minimum Biocidal Concentration, MBC). Maintain an untreated control flask. From both flasks, aseptically withdraw samples (e.g., 1 mL) at predefined time intervals (e.g., 0, 1, 2, 4, 6, 8, 12, 24 hours) [43] [4].
- Serial Dilution and Plating: For each sample, perform a 1:10 serial dilution series in sterile PBS. The number of dilutions required depends on the expected bacterial density; for early time points, 10⁻⁴ to 10⁻⁷ may suffice, while for later time points, 10⁻⁶ to 10⁻⁹ may be necessary [45] [44]. From selected dilution tubes, plate 100 µL onto labeled agar plates and spread evenly using a sterile spreader.
- Colony Counting and Calculation: After overnight incubation, count the plates containing between 30 and 250 colonies. Calculate the CFU/mL for that time point using the formula [46]: CFU/mL = (Number of colonies) / (Dilution factor × Volume plated in mL).
Data Analysis and Kill Rate Determination
Generating the Log CFU/mL vs. Time Graph
- Data Transformation: Convert all calculated CFU/mL values to logarithmic (Log₁₀) scale. This linearizes exponential growth and allows for clear visualization of killing trends [45].
- Plotting: Plot time (hours) on the x-axis and Log₁₀(CFU/mL) on the y-axis. Use a scatter plot to represent the actual data points. This creates the classic time-kill curve [44].
- Curve Fitting: Draw a smooth curve or a series of straight lines connecting the data points to visualize the trend. Do not simply "connect the dots"; instead, draw the best-fit line through the distinct phases of the curve [45].
Interpreting Kill Kinetics from the Curve
Table 2: Classification of Antimicrobial Action from Time-Kill Curves
| Kill Curve Profile | Description | Interpretation |
|---|---|---|
| Bactericidal | A decrease in Log CFU/mL of ≥ 3 (99.9% reduction) from the initial inoculum [43]. | The agent is lethal and kills the bacteria. |
| Bacteriostatic | The curve remains relatively flat or shows less than a 3 Log decrease from the initial inoculum. | The agent inhibits growth but does not kill. |
| Time-Dependent Killing | The rate and extent of killing are dependent on the duration of exposure. | Characteristic of agents like beta-lactams. |
| Concentration-Dependent Killing | The rate and extent of killing increase as the antimicrobial concentration increases. | Characteristic of agents like aminoglycosides. |
The kill rate can be directly determined from the slope of the linear, declining portion of the Log CFU/mL vs. time curve. A steeper negative slope indicates a faster kill rate [45].
Data Visualization and Presentation Standards
Color Palette for Scientific Figures
Effective data visualization is critical for communicating results. The following color palette, defined by HEX codes, ensures clarity and accessibility, including for individuals with color vision deficiencies (CVD) [47].
- Primary Blue:
#4285F4 - Alert Red:
#EA4335 - Warning Yellow:
#FBBC05 - Success Green:
#34A853 - Neutral White:
#FFFFFF - Light Background Gray:
#F1F3F4 - Dark Text Gray:
#202124 - Mid Text/Line Gray:
#5F6368
Always test your color choices using tools like Viz Palette to check for conflicts and ensure accessibility for audiences with CVD [47].
Workflow for Data Visualization and Analysis
The final stage involves a rigorous process of data compilation, graphical representation, and kinetic analysis.
Time-kill kinetics assays represent a cornerstone methodology in antimicrobial research, providing dynamic, time-dependent data on the bactericidal or bacteriostatic activity of potential therapeutic agents. Unlike endpoint measurements, these assays quantify how rapidly a microbial population is reduced over time, offering critical insights into the rate and extent of killing activity [3]. Within the broader context of antimicrobial evaluation research, this protocol focuses on the sophisticated application of time-kill assays to biofilm communities and combination therapies. Biofilms, which are structured communities of microorganisms encased in a self-produced extracellular matrix, demonstrate dramatically increased antibiotic resistance (10 to 1,000-fold) compared to their planktonic (free-floating) counterparts [48]. This inherent recalcitrance makes biofilm-related infections particularly challenging to treat and a significant focus for novel therapeutic strategies.
The synergy testing component addresses the growing importance of combination therapies in overcoming resistance mechanisms. The fundamental goal of synergy testing is to identify drug interactions where the combined effect is significantly greater than the expected additive effect of individual agents, potentially allowing for dosage reduction and decreased toxicity [49]. This application note provides detailed, actionable protocols for researchers to quantitatively evaluate both the biofilm-eradicating potential of antimicrobials and the synergistic potential of combination therapies, thereby advancing the development of more effective treatment regimens against persistent infections.
Theoretical Foundations and Key Concepts
The Biofilm Lifecycle and Intrinsic Resistance Mechanisms
The robust resistance exhibited by biofilms is intrinsically linked to their structured lifecycle, which comprises five main stages: (1) initial attachment, (2) irreversible attachment, (3) micro-colony formation, (4) biofilm maturation, and (5) dispersion [50]. During maturation, cells secrete an extracellular matrix that can constitute over 90% of the biofilm's mass, creating a formidable barrier to antimicrobial penetration [50]. This extracellular polymeric substance (EPS) matrix, composed of polysaccharides, lipids, proteins, and extracellular DNA (eDNA), acts as a primary defense mechanism by hindering antibiotic absorption, inactivating antimicrobial agents through binding or enzymatic degradation, and creating chemical gradients that limit drug diffusion [50] [48].
Beyond physical barrier functions, the biofilm microenvironment induces physiological changes in resident cells. Nutrient and oxygen gradients within the biofilm structure create zones of slow growth or metabolic dormancy, rendering bacteria less susceptible to antibiotics that target active cellular processes [48]. Furthermore, biofilms harbor "persister" cells—dormant subpopulations that exhibit extreme, non-genetic tolerance to antimicrobials. Upon cessation of treatment, these persister cells can repopulate the biofilm, leading to recurrent infections [50] [48]. A comprehensive understanding of these mechanisms is prerequisite to designing effective biofilm eradication strategies and accurately interpreting time-kill assay results.
Defining Synergy in Combination Therapy
In combination therapy, synergistic activity is formally defined as a combined effect that is significantly greater than the expected additive effect of the individual drugs. In practical terms for time-kill assays, synergism is often quantified as a ≥ 2 log10 decrease in colony-forming units per milliliter (CFU/mL) of the combination compared to the most active single agent [51]. This quantitative definition provides a clear and standardized threshold for identifying promising combination treatments.
It is critical to distinguish between synergy and overall treatment sensitivity. A highly synergistic combination does not guarantee that the treatment will be highly effective in an absolute sense; it merely indicates that the combination performs better than anticipated based on monotherapy responses [52]. This distinction is crucial for drug development, as a mildly synergistic combination of two weak drugs may be less therapeutically valuable than a strongly effective monotherapy. Therefore, synergy should be evaluated alongside absolute measures of bacterial reduction.
Table 1: Key Concepts in Combination Therapy Synergy
| Concept | Definition | Application in Research |
|---|---|---|
| Synergism | A ≥ 2 log10 decrease in CFU/mL for a combination vs. its most active component [51]. | Primary endpoint for identifying promising combinations. |
| Additivity | The combined effect equals the sum of individual drug effects. | The baseline model against which synergy is measured. |
| Antagonism | The combined effect is less than the additive effect. | Identifies combinations to be avoided. |
| Indifference | The combined effect is no greater than the most effective single agent. | Suggests no benefit from combination. |
Experimental Protocols
Protocol 1: Biofilm Time-Kill Assay
This protocol is adapted from established methods for evaluating the efficacy of antimicrobial agents against pre-formed biofilms, such as those found on medical device surfaces [53].
Research Reagent Solutions and Essential Materials
Table 2: Essential Materials for Biofilm Time-Kill Assay
| Item | Function/Description | Example/Specification |
|---|---|---|
| Sintered Porous Glass Beads | Provides a high-surface-area substrate for robust biofilm formation. | 4 mm diameter, sterile [53]. |
| Culture Media | Supports bacterial growth and biofilm development. | Tryptic Soy Broth (TSB) or LB Broth [51] [53]. |
| Antimicrobial Agent | The test compound for biofilm eradication. | Phage suspension, antibiotic, or natural extract [53] [5]. |
| Saline Solution (0.9%) | Used for washing beads to remove non-adhered planktonic cells. | Phosphate-buffered saline (PBS) can also be used [53]. |
| Neutralizing Fluid | Halts antimicrobial action at specified time points to allow accurate CFU counting. | Validated for the specific antimicrobial tested [3]. |
| Ultrasound Bath (Sonicator) | Dislodges biofilm-embedded cells from the bead substrate for quantification. | e.g., BactoSonic, 40 kHz, 0.2 W/cm² [53]. |
| Agar Plates | Provides solid surface for colony growth and enumeration. | Tryptic Soy Agar (TSA) or Mueller-Hinton Agar (MHA) [51] [53]. |
Detailed Procedural Steps
- Biofilm Formation: Place sterile sintered porous glass beads into the wells of a 24-well plate. Cover each bead with 1 mL of TSB inoculated with a 1:100 dilution of an overnight bacterial culture. Incubate the plate at 37°C with moderate shaking (e.g., 150 rpm) for 24 hours under humid conditions to facilitate biofilm development [53].
- Washing: After incubation, carefully dip-wash each bead in sterile 0.9% saline to remove loosely attached, planktonic cells. This step is critical for isolating the biofilm population for testing.
- Antimicrobial Exposure: Transfer the washed, biofilm-coated beads into microcentrifuge tubes containing 1 mL of fresh TSB inoculated with the antimicrobial agent at the desired test concentration (e.g., 108 PFU/mL for phage therapy) [53]. For combination therapy, add all agents simultaneously.
- Sampling and Neutralization: Incubate the tubes at 37°C. At predetermined time points (e.g., 0, 2, 4, 6, and 24 hours), remove selected tubes. Transfer a measured volume of the suspension to a tube containing a validated neutralizing fluid to stop the antimicrobial activity [3].
- Biofilm Harvesting and Quantification:
- Sonicate the bead in the neutralizer for 10 minutes to dislodge the biofilm cells.
- Remove the bead and centrifuge the sonication fluid.
- Wash the bacterial pellet multiple times (e.g., four times) with PBS to ensure removal of residual antimicrobial agents.
- Perform ten-fold serial dilutions of the final resuspended fluid and spread-plate aliquots onto TSA plates.
- Incubate plates for 18-24 hours at 37°C and enumerate the colonies to determine the CFU/mL [53].
The following workflow diagram summarizes the key stages of this protocol:
Diagram 1: Biofilm Time-Kill Assay Workflow
Protocol 2: Combination Therapy Synergy Testing
This protocol outlines a standard time-kill procedure for evaluating the synergistic interaction between two or more antimicrobial agents against planktonic bacteria [51].
Research Reagent Solutions and Essential Materials
Table 3: Essential Materials for Combination Synergy Testing
| Item | Function/Description | Example/Specification |
|---|---|---|
| Inoculum | Standardized population of challenge bacteria. | Prepared at ~1 × 10^6 CFU/mL in growth broth [51]. |
| Antimicrobial Stock Solutions | Individual agents for mono- and combination therapy. | Prepared at precise concentrations in solvent or water. |
| Growth Broth | Liquid medium supporting bacterial growth during assay. | Cation-adjusted Mueller Hinton Broth or LB Broth [51]. |
| Control Tubes | Essential for result normalization and interpretation. | Tubes containing broth alone (growth control) [51]. |
| Agar Plates | For final enumeration of surviving bacteria. | Mueller-Hinton Agar (MHA) [51]. |
Detailed Procedural Steps
- Inoculum Preparation: Grow the bacterial strain of interest to the mid-logarithmic phase. Adjust the suspension to a density of approximately 1 × 106 CFU/mL in a suitable broth like LB [51].
- Experimental Setup: Distribute the inoculated broth into sterile tubes and add antimicrobials as follows:
- Growth Control: LB broth alone.
- Monotherapy A: Final concentration of drug A (e.g., thymol at 32-64 mg/L).
- Monotherapy B: Final concentration of drug B (e.g., colistin at 0.5-2 mg/L).
- Combination Therapy: Both drugs A and B at the same concentrations used in monotherapy [51].
- Incubation and Sampling: Incubate all tubes at 37°C with moderate shaking. Sample from each tube at specified time intervals (e.g., 0, 2, 4, 6, 12, and 24 hours).
- Viable Count Determination: At each time point, perform ten-fold serial dilutions of the samples in a neutralizer or saline. Spread-plate appropriate dilutions onto MHA plates. After incubating the plates for 18-24 hours at 37°C, count the colonies and calculate the CFU/mL for each sample and time point [51].
Data Analysis and Interpretation
Quantifying Results and Defining Synergy
The primary raw data from a time-kill assay is a table of CFU/mL values for each experimental condition across all time points. These values are typically converted to log10 and plotted against time to generate time-kill curves, which visually represent the killing kinetics of each treatment.
To quantify synergy, compare the log10 CFU/mL reduction of the combination against the most active single drug at the 24-hour time point. A ≥ 2 log10 decrease conferred by the combination is the standard benchmark for declaring synergism [51]. This represents a 99% greater reduction in the bacterial population than the best single agent alone.
Table 4: Sample Time-Kill Data Analysis (CFU/mL, log10)
| Time (h) | Growth Control | Monotherapy A | Monotherapy B | Combination A+B |
|---|---|---|---|---|
| 0 | 6.0 | 6.0 | 6.0 | 6.0 |
| 2 | 6.2 | 5.8 | 5.5 | 4.0 |
| 4 | 6.5 | 5.5 | 5.0 | 2.5 |
| 6 | 6.8 | 5.2 | 4.8 | 1.8 |
| 24 | 7.0 | 4.5 (Δ = 1.5) | 3.0 (Δ = 3.0) | 0.5 (Δ = 5.5) |
| Synergy Check | — | — | — | 5.5 - 3.0 = 2.5 (Synergistic) |
Note: Δ represents the change from the initial count at 0h. The combination shows a 2.5 log10 greater reduction than the most active monotherapy (Monotherapy B), confirming synergy.
Conceptual Workflow for Data Interpretation
The process of analyzing time-kill data involves transforming raw colony counts into actionable information about the antimicrobial interaction, guiding decisions on future therapeutic development.
Diagram 2: Data Analysis and Interpretation Workflow
The protocols detailed in this application note provide a robust framework for assessing the efficacy of antimicrobial agents against resilient biofilm communities and for identifying synergistic drug combinations. The integration of biofilm time-kill assays with systematic synergy testing enables a more translational research pathway, bridging the gap between standard planktonic susceptibility testing and the complex reality of chronic, difficult-to-treat infections. As the field advances, the application of these kinetic assays, combined with sophisticated data analysis and a deep understanding of biofilm biology and pharmacodynamic interactions, will be instrumental in developing the next generation of antimicrobial therapies to combat the growing threat of antimicrobial resistance.
Optimizing Assay Performance: Troubleshooting Common Pitfalls and Technical Challenges
Within antimicrobial research, the integrity of the time-kill kinetics assay is paramount for accurately evaluating the bactericidal activity of new therapeutic candidates. This assay relies heavily on robust growth in control samples—untreated bacterial suspensions—to serve as a baseline for determining the rate and extent of killing in treated samples. Poor bacterial growth in these controls introduces significant variability, compromises data validity, and can ultimately lead to erroneous conclusions about a compound's efficacy. The complexity of bacterial cultivation means that growth failures can stem from interrelated factors, primarily involving the culture medium, atmospheric conditions, and the viability of the bacterial strain itself. This application note provides a structured, experimental framework for diagnosing and remediating poor growth in control samples, specifically contextualized within the workflow of time-kill kinetics research [39] [1] [43].
Troubleshooting Poor Growth: A Systematic Workflow
A systematic approach is required to diagnose the root cause of insufficient growth. The following workflow guides the researcher through a series of checks and validation experiments. The diagram below outlines the logical decision-making process for troubleshooting poor bacterial growth in control samples.
Core Checks and Validation Protocols
Strain Viability and Preparation
The viability of the bacterial stock and the physiological state of the inoculum are foundational to successful growth in controls.
- Potential Issue: The bacterial stock may be non-viable, have diminished viability due to improper storage or repeated sub-culturing, or may have entered a "Viable But Not Culturable" (VBNC) state [54]. The inoculum may not be prepared from mid-log phase cells, leading to extended lag phases.
- Verification Protocol:
- Revive from Stock: Always initiate experiments by reviving the bacterial strain from a preserved, master stock (e.g., frozen at -80°C in glycerol) rather than relying on repeatedly sub-cultured working stocks [55].
- Growth Curve Analysis: Perform a full growth curve analysis to determine the optimal incubation time for harvesting mid-log phase cells. Measure the optical density at 600 nm (OD₆₀₀) at regular intervals (e.g., every 30-60 minutes) and plot the data to identify the logarithmic phase [54].
- Viability Staining: Use a LIVE/DEAD BacLight bacterial viability kit or similar staining method. This kit contains two dyes, Syto 9 (stains all cells green) and propidium iodide (stains cells with compromised membranes red), allowing for the quantification of the viable fraction via fluorescence microscopy or flow cytometry [56]. A low ratio of green to red fluorescence indicates a viability problem.
Culture Medium Optimization
The culture medium must provide all essential nutrients in the correct proportions and be free from inhibitory substances.
- Potential Issue: The medium may be prepared incorrectly, have degraded during storage, or may be suboptimal for supporting the robust growth required for time-kill assays [55].
- Verification Protocol:
- Fresh Medium Preparation: Prepare a fresh batch of culture medium from its basic components, strictly following the recipe for a non-selective, rich medium like Tryptic Soy Broth (TSB) or Luria-Bertani (LB) Broth [39] [54]. Autoclave or filter-sterilize appropriately.
- pH Verification and Adjustment: After preparation and sterilization, measure the pH of the medium at the incubation temperature. Adjust to the optimal pH for the strain (typically pH 7.0 - 7.4 for many pathogens) using sterile acid or base [57]. Note that bacterial metabolism can alter the pH of the media over time [57].
- Growth Promotion Test: Inoculate the fresh medium with a low inoculum (e.g., 10⁵ CFU/mL) of the target strain and monitor the growth curve. Compare the growth rate and maximum cell density against a previously accepted batch of medium. Robust growth should be observed within the expected time frame.
Atmospheric Conditions
Many bacterial species, including common pathogens, have specific requirements for oxygen and carbon dioxide levels for optimal growth.
- Potential Issue: The incubator may not be maintaining the correct atmosphere. Some bacteria are strict aerobes, others facultative anaerobes, and some require microaerophilic (low oxygen) or capnophilic (elevated CO₂) conditions [55].
- Verification Protocol:
- Atmosphere Validation: Use independent, calibrated sensors to verify the O₂ and CO₂ levels inside the incubator. Do not rely solely on the incubator's display.
- Use of Chemical Indicators: Employ resazurin color indicators within anaerobic chambers to confirm the absence of oxygen [56].
- Comparative Growth Test: Incurate identical inocula of the target strain under different atmospheric conditions (aerobic, anaerobic, microaerophilic with ~5% O₂ and 10% CO₂) [55]. Compare the growth yields and rates after a set period (e.g., 24 hours) to identify the optimal condition.
Essential Research Reagent Solutions
The table below catalogues key reagents and materials critical for executing the troubleshooting protocols and ensuring reliable time-kill assays.
Table 1: Key Research Reagents for Bacterial Growth Troubleshooting and Time-Kill Assays
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Rich Culture Media | Supports robust, non-selective growth for controls and inoculum preparation. | Tryptic Soy Broth (TSB) [39], Luria-Bertani (LB) Broth [57], Brain Heart Infusion (BHI) [56]. |
| Solid Agar Media | Colony isolation, purity checks, and CFU enumeration. | Tryptic Soy Agar (TSA), LB Agar, Blood Agar for fastidious species [55]. |
| Viability Stains | Differentiates viable from non-viable cells in a population. | LIVE/DEAD BacLight kit (Syto 9/PI) [56], Syto 13/Hexidium Iodide for Gram-staining [56]. |
| Atmosphere Generation Systems | Creates and maintains specific incubation conditions. | Anaerobic chambers (e.g., 90% N₂, 5% H₂, 5% CO₂) [56], CO₂ incubators, gas-generating sachets for jars. |
| Sterile Physiological Solution | Used for bacterial suspension and dilution without osmotic shock. | 0.9% Sodium Chloride (NaCl) solution [54]. |
| Quality Control Strains | Verifies performance of media and assay conditions. | E. coli ATCC 8739, S. aureus ATCC 6538 [39]. Use standard reference strains from culture collections. |
Integrated Validation Protocol: Time-Kill Kinetics Setup
Before commencing a time-kill kinetics assay, the following integrated protocol ensures that control samples are primed for optimal growth. The workflow diagram below visualizes the key steps in this preparation and validation process.
Procedure:
- Inoculum Preparation: Revive the bacterial strain from a frozen glycerol stock by streaking onto a fresh agar plate. Incubate under optimal conditions to obtain single colonies [55].
- Starter Culture: Pick a well-isolated colony and inoculate it into a flask containing fresh, pre-warmed liquid culture medium (e.g., TSB). The volume of medium should be large enough to ensure adequate aeration (typically a 1:5 flask-to-medium ratio) [54].
- Controlled Incubation: Incubate the flask with shaking (e.g., 180 rpm) at the optimal temperature and in a verified atmosphere to promote uniform growth and aeration [56].
- Harvesting: Monitor the OD₆₀₀ every 30 minutes. Once the culture reaches the mid-log phase (OD₆₀₀ typically between 0.4 and 0.6, pre-determined by growth curve analysis), harvest the cells [54].
- Cell Washing and Standardization: Centrifuge the bacterial suspension (e.g., at 3000-5000 rpm for 10 minutes) and resuspend the pellet in sterile physiological saline (0.9% NaCl) or a non-growth buffer. Repeat this washing step once. Adjust the optical density of the suspension to match a 0.5 McFarland standard or use a hemocytometer to achieve a target density of approximately 10⁸ CFU/mL. Perform a serial dilution and plate count to confirm the precise initial bacterial concentration for the time-kill assay [1] [43].
- Positive Control Setup: In the time-kill assay, the control sample (without antimicrobial) should be diluted in fresh culture medium at a ratio that yields a starting concentration of approximately 10⁵ to 10⁶ CFU/mL. This sample is then incubated under the same conditions as the test samples, and viable counts are determined at time zero and at predetermined intervals (e.g., 0, 4, 8, 16, and 24 hours) [39] [1]. A successful control will show a consistent increase in CFU/mL over the first few hours, demonstrating active growth.
Achieving consistent and robust bacterial growth in control samples is a critical prerequisite for generating reliable time-kill kinetics data. By systematically addressing the three pillars of bacterial cultivation—strain viability, culture medium, and atmospheric conditions—researchers can effectively troubleshoot and prevent growth failures. The application of the detailed protocols and reagent solutions provided herein will enhance the robustness of antimicrobial evaluations, ensuring that findings related to the bactericidal activity of new compounds, such as novel antimicrobial peptides [39] or natural compounds like thymoquinone [43], are built upon a foundation of reliable and reproducible control data.
In the context of antimicrobial evaluation research, the time-kill kinetics assay is a cornerstone method for characterizing the bactericidal or bacteriostatic activity of a potential antimicrobial agent over time [2]. A core challenge in this assay, however, is the high degree of variability observed between experimental replicates. Such variability can obscure true concentration-effect relationships and compromise the reliability of data used for critical decisions in drug development [23]. The root causes of this variability often trace back to two fundamental technical aspects: the consistency of the initial inoculum and the precision of the sampling technique [4] [58]. This Application Note details standardized protocols for these key steps, providing a framework for generating robust, reproducible, and high-quality time-kill data.
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials and reagents essential for executing a reproducible time-kill kinetics assay, particularly focusing on inoculum preparation and sampling.
Table 1: Key Research Reagent Solutions for Time-Kill Assays
| Item | Function/Application | Key Considerations for Reproducibility |
|---|---|---|
| Mueller-Hinton Broth (MHB) | Standardized growth medium for susceptibility testing [32]. | Use the same lot and supplier for a series of experiments to minimize medium-induced variability. |
| McFarland Standards | Visual or densitometric reference for standardizing bacterial suspension turbidity [32]. | Ensure standards are properly mixed and not expired. Verify suspension density spectrophotometrically if possible. |
| Sterile Saline (0.85-0.9%) | Diluent for preparing bacterial suspensions and performing serial dilutions during sampling [3]. | Must be sterile to avoid contamination of samples and inoculum. |
| Antimicrobial Neutralizers | Components of the neutralizing solution (e.g., in D/E Neutralizing Broth) to halt antimicrobial action immediately upon sampling [3]. | The neutralizing solution must be validated for the specific antimicrobial agent being tested to ensure complete inactivation [3]. |
| Agar Plating Media | Solid medium for enumerating viable bacteria via Colony Forming Units (CFU) [4]. | Use the same type and lot of agar throughout a study. Ensure even pouring for consistent colony counting. |
Core Protocols for Enhanced Reproducibility
Protocol 1: Standardized Inoculum Preparation
A standardized inoculum is the most critical factor in minimizing variability in the final results of antimicrobial susceptibility testing, including time-kill assays [32] [58].
Principle: The goal is to prepare a bacterial suspension of a defined and reproducible density, typically targeting a final concentration of approximately 5 x 10^5 CFU/mL in the test vessel, as this concentration is within the recommended range for standard antimicrobial susceptibility testing and helps avoid the "inoculum effect" [32] [59].
Detailed Methodology:
- Colony Selection: From a fresh overnight agar plate (incubated 18-24 hours), select 3-5 well-isolated colonies of the target organism [32].
- Initial Suspension: Transfer the colonies into a tube containing sterile saline or a suitable broth (e.g., Mueller-Hinton Broth).
- Turbidity Standardization: Vortex the suspension thoroughly and adjust its turbidity to match that of a 0.5 McFarland standard [32].
- Visual Comparison: Compare the tube against the McFarland standard against a card with a white background and contrasting black lines.
- Spectrophotometric Verification (Recommended): Measure the optical density at 600 nm (OD600). A 0.5 McFarland standard typically corresponds to an OD600 of 0.08 to 0.13 (approximately 1 x 10^8 CFU/mL) [32] [59]. This provides an objective quality check.
- Final Dilution: Perform a 1:100 dilution of the standardized suspension in the growth medium used for the assay. For example, add 0.1 mL of the suspension to 9.9 mL of broth. This yields a theoretical starting inoculum of ~1 x 10^6 CFU/mL [32]. Further dilution within the test tube containing the antimicrobial agent will achieve the final target concentration.
Table 2: Critical Quality Control Parameters for Inoculum Preparation
| Parameter | Target | Acceptance Criteria | Corrective Action |
|---|---|---|---|
| Source Material | 3-5 well-isolated colonies | Colonies from an 18-24 hour culture | Do not use colonies from older plates. |
| McFarland Standard | 0.5 | Visual match or OD600 of 0.08-0.13 | Add more bacteria or more diluent to adjust turbidity. |
| Final Assay Concentration | ~5 x 10^5 CFU/mL | Confirm by viable count (CFU/mL) | Adjust dilution factor based on viable count results. |
The workflow for this standardized process is outlined below.
Protocol 2: Aseptic and Quantitative Sampling
Precise sampling at each time point is essential for accurately tracking the change in viable bacterial count over time.
Principle: At predetermined time intervals (e.g., 0, 2, 4, 6, 24 hours), a sample is withdrawn from the test mixture and the antimicrobial action is immediately neutralized. The number of viable bacteria in this sample is then quantified, typically by serial dilution and plating for Colony Forming Unit (CFU) enumeration [2] [4].
Detailed Methodology:
- Pre-Sampling Mixing: Gently vortex or mix the test tube immediately before sampling to ensure a homogeneous distribution of bacteria.
- Sample Volume: Withdraw a defined volume, typically 100 μL to 1 mL, using a calibrated pipette. Using a consistent volume across all samples and time points is critical.
- Immediate Neutralization: Transfer the sample directly into a pre-prepared tube containing a suitable neutralizing solution [3]. The neutralizing solution (e.g., D/E Neutralizing Broth) must be validated for its ability to completely inactivate the antimicrobial agent being tested. Vortex to mix.
- Serial Dilution:
- Plating for Enumeration:
- From selected dilutions, plate a precise volume (e.g., 10-100 μL) onto labeled agar plates. For greater accuracy, especially for low counts, 100 μL is recommended for spread-plating [4].
- Alternatively, a 2.5 μL micro-droplet plating technique can be used for higher throughput, provided it is validated for consistency [4].
- Spread the aliquot evenly over the surface of the agar.
- Incubation and Counting: Incubate the plates under appropriate conditions for the test organism (typically 35±2°C for 18-24 hours). After incubation, count the colonies on plates that contain between 30 and 300 CFUs for statistical reliability. Calculate the original CFU/mL for each time point.
The logical sequence for quantitative sampling and data analysis is as follows.
High variability between replicates in time-kill kinetics assays can be systematically reduced through meticulous attention to inoculum preparation and sampling technique. The protocols detailed herein—emphasizing turbidity standardization, use of qualified neutralizing agents, and precise volumetric handling—provide a robust framework for generating reliable and reproducible data. Adherence to these standardized methodologies is fundamental for accurate assessment of antimicrobial efficacy and supports the development of robust, data-driven decisions in the drug development pipeline.
In antimicrobial evaluation research, particularly in time-kill kinetics assays, the drug carryover effect presents a significant methodological challenge that can compromise data integrity. This phenomenon occurs when antimicrobial agents are inadvertently transferred from the original incubation medium to the subculture or plating medium, inhibiting microbial growth not as a result of prior lethal activity but due to continued presence in the test system [60] [61]. The consequence is a potential overestimation of a drug's in vivo efficacy, as the carryover effect can cause falsely low minimum bactericidal concentration (MBC) determinations or overstate killing kinetics in time-kill studies [61]. This application note details proven methodologies for identifying, quantifying, and neutralizing antimicrobial carryover effects to ensure accurate assessment of antimicrobial activity within time-kill kinetics protocols.
Understanding and Quantifying the Carryover Effect
The Fundamental Challenge
Carryover effects pose the greatest risk when evaluating antimicrobial agents that combine high tissue penetration (large volumes of distribution) with exceptionally low MICs [60]. Studies have demonstrated that compounds such as the diarylquinoline TMC207 can achieve tissue concentrations that exceed their MIC against Mycobacterium tuberculosis by more than 100-fold, creating substantial risk for carryover effects when culturing treated samples [60]. Similarly, recent research highlights that residual antibiotics like penicillin in conditioned medium from tissue culture systems can produce bacteriostatic effects against sensitive bacterial strains, potentially leading to misinterpretation of cellular antimicrobial properties [62].
Quantitative Assessment of Carryover
Researchers should first establish the Maximal Non-Inhibitory Concentration (MNIC) for their antimicrobial-agent system, defined as the highest concentration of an antimicrobial that can be transferred during subculturing without inhibiting growth of the test organism [60]. The table below summarizes key quantitative findings from carryover studies:
Table 1: Efficacy of Protein-Enriched Media in Preventing Carryover Effects for TMC207
| Culture Medium | Average MIC (μg/mL) | Average MNIC (μg/mL) | Carryover Prevention Efficacy |
|---|---|---|---|
| 7H11 Agar (Unsupplemented) | 0.03 | 0.97 | Baseline (Low) |
| 7H11 Agar + 5% BSA | 1.00 | 32.33 | High |
| Lowenstein-Jensen Medium | 14.33 | 96.33 | Very High |
Data adapted from PMC2446915 [60]
These findings demonstrate that protein supplementation significantly increases the MNIC, thereby reducing carryover effects. For TMC207, adding 5% Bovine Serum Albumin (BSA) to 7H11 agar increased the MNIC by approximately 33-fold compared to unsupplemented medium [60].
Neutralization Methodologies and Protocols
Protein Binding and Media Supplementation
Principle: Antimicrobial binding proteins in the culture medium sequester drug molecules, reducing their free concentration and bioavailable fraction below inhibitory thresholds [60].
Protocol: Protein-Enriched Media Preparation
- Prepare double-concentrated 7H11 agar by dissolving 12.6 g in 240 mL distilled water with 3 mL glycerol.
- Heat with continuous stirring, boil for 1 minute, and autoclave at 121°C for 15 minutes.
- Cool to 55°C and add 60 mL Middlebrook OADC enrichment.
- For 7H11 + 5% BSA medium, mix 200 mL double-concentrated 7H11 agar with 200 mL of 10% BSA solution.
- For Lowenstein-Jensen medium, dissolve 18.6 g base in 300 mL distilled water with 6 mL glycerol, autoclave, cool to 55°C, and add 200 mL fresh, uniform egg suspension.
- Distribute into plates and coagulate for 45 minutes at 85°C [60].
Considerations: This method is particularly effective for highly protein-bound antimicrobials like TMC207, which demonstrates >99.9% plasma protein binding [60].
Physical Removal Techniques
Principle: Physical separation methods eliminate antimicrobial agents from bacterial cells before subculturing through washing procedures or mechanical separation.
Protocol: Centrifugation-Wash Technique
- Following antimicrobial exposure in time-kill experiments, transfer a 1 mL aliquot to a sterile microcentrifuge tube.
- Centrifuge at 10,000 × g for 5 minutes to pellet bacterial cells.
- Carefully decant the supernatant containing the antimicrobial agent.
- Resuspend the pellet in 1 mL of appropriate antimicrobial-free buffer (e.g., phosphate-buffered saline) or growth medium.
- Repeat centrifugation and resuspension steps for a total of two washes.
- Perform final resuspension in antimicrobial-free medium before serial dilution and plating [61].
Protocol: Strategic Agar Streaking
- Following antimicrobial exposure, subculture a 10-100 μL aliquot onto appropriate agar medium.
- Using a sterile loop, streak the aliquot over at least one-half of the surface of a 100 mm agar plate.
- Employ a streaking pattern that progressively dilutes the antimicrobial agent across the plate surface.
- Incubate plates under appropriate conditions and examine for isolated colonies in areas of highest dilution [61].
Cell Culture Pre-Washing for Conditioned Medium Studies
Principle: Remove residual antibiotics retained on tissue culture plastic surfaces before collecting conditioned medium for antimicrobial testing.
Protocol: Pre-Washing Procedure
- Grow cells to 70-80% confluency in antibiotic-containing medium.
- Aspirate culture medium and wash cell monolayer twice with sterile, pre-warmed phosphate-buffered saline (PBS).
- Add antibiotic-free basal medium for the conditioning period (typically 72 hours).
- Collect conditioned medium and clarify by centrifugation if necessary [62].
Table 2: Impact of Pre-Washing on Antimicrobial Activity of Conditioned Medium
| Experimental Condition | Residual Antimicrobial Activity | Recommended Application |
|---|---|---|
| No Pre-Wash | High | Not recommended for accurate assessment |
| Single PBS Wash | Significantly Reduced | Minimum requirement |
| Multiple PBS Washes | Effectively Eliminated | Optimal for sensitive applications |
Data adapted from Scientific Reports 2025 [62]
Integration with Time-Kill Kinetics Assays
Time-kill kinetics assays evaluate the rate and extent of antimicrobial killing over time, typically measuring a ≥3 log10 (99.9%) reduction in colony-forming units (CFU) to demonstrate bactericidal activity [2] [3]. Proper carryover control is essential throughout this process.
The following workflow diagram illustrates the integration of carryover control methods into a standard time-kill kinetics protocol:
Figure 1: Integration of carryover control methods into time-kill kinetics workflow. Critical neutralization steps highlighted in green.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for Carryover Neutralization
| Reagent/Material | Function in Carryover Control | Application Notes |
|---|---|---|
| Bovine Serum Albumin (BSA) | Binds protein-reactive antimicrobials; increases MNIC | Use at 5% concentration in agar media [60] |
| Egg-Enriched Media (L-J) | Provides natural protein binding capacity | Effective for highly lipophilic antibiotics [60] |
| Protein-Free Buffer (PBS) | Washing medium for physical antibiotic removal | Essential for pre-washing cell cultures [62] |
| Antimicrobial Neutralizers | Inactivates disinfectants/antiseptics in suspension tests | Validated neutralizers required for specific compounds [3] |
| Centrifugation Equipment | Physical separation of cells from antimicrobials | Effective for non-filamentous bacteria [61] |
Effective management of antimicrobial carryover effects requires careful methodological planning and implementation. Protein-enriched media, particularly 7H11 agar supplemented with 5% BSA, provides a practical solution for highly protein-bound antimicrobials, while physical removal methods including centrifugation-washing and strategic streaking offer broad-spectrum applicability. Integration of these controls into time-kill kinetics protocols ensures accurate determination of bactericidal activity and prevents overestimation of antimicrobial efficacy. Researchers should validate the effectiveness of their chosen neutralization method for specific antimicrobial-bacterial systems to generate reliable, reproducible data in antimicrobial evaluation studies.
Neisseria gonorrhoeae presents a formidable challenge in antimicrobial research due to its fastidious nature and escalating antibiotic resistance. As the causative agent of gonorrhea, it is classified as an urgent global public health threat by the World Health Organization due to progressively developing resistance to all commonly used antibiotics [63] [64]. The shift toward molecular diagnostic testing has further complicated resistance monitoring by reducing the availability of viable isolates for phenotypic susceptibility testing [65] [64]. This application note details optimized methodologies for cultivating and evaluating antimicrobial susceptibility of this fastidious pathogen within the context of time-kill kinetics assays, utilizing defined media to enhance reproducibility and reliability in antimicrobial evaluation research.
Current Resistance Landscape and Therapeutic Challenges
Epidemiology and Clinical Significance
N. gonorrhoeae disproportionately affects gay, bisexual, and other men who have sex with men, young people aged 15-24 years, and certain ethnic minority groups [63]. The bacterium exhibits specificity for columnar epithelium, infecting mucous membranes of the urethra, endocervix, rectum, pharynx, and conjunctiva [63]. While urogenital infections often present with symptoms, most rectal and pharyngeal infections are asymptomatic, facilitating silent transmission [63].
Antimicrobial Resistance Patterns
Table 1: Documented Resistance Profiles of N. gonorrhoeae
| Antimicrobial Agent | Resistance Prevalence | Key Resistance Mechanisms | Clinical Implications |
|---|---|---|---|
| Penicillin | 87.7% resistance reported [66] | PPNG production (24.6% of isolates) [66] | No longer recommended for treatment |
| Tetracycline | 82.5% resistance reported [66] | High-level TRNG (28.1% suspected) [66] | Excluded from treatment guidelines |
| Ciprofloxacin | 71.9% resistance reported [66] | Chromosomal mutations in gyrA and parC | Not suitable for empirical therapy |
| Azithromycin | Increasing resistance globally [64] | Mutations in 23S rRNA and mtrR efflux pump | Removed from dual therapy recommendations |
| Ceftriaxone | 3.5-5.3% resistance emerging [66] | Alterations in penA, mtrR, ponA | Now the primary recommended monotherapy [63] |
| Spectinomycin | Rare resistance detected [66] [67] | Mutations in rpsE gene (80_82 delTTA) [67] | Remains an alternative regimen |
The progressive resistance development underscores the critical need for ongoing surveillance and novel antimicrobial development. Current guidelines recommend ceftriaxone 1g intramuscularly as first-line treatment, with alternative regimens including cefixime plus azithromycin, gentamicin plus azithromycin, or azithromycin alone for specific cases [63].
Methodological Framework for Susceptibility Testing
Gold Standard and Novel Approaches
Traditional antimicrobial susceptibility testing for N. gonorrhoeae relies heavily on agar dilution methods, which, while accurate, are labor-intensive and resource-demanding [65]. Recent innovations have focused on developing high-throughput alternatives that maintain accuracy while improving efficiency.
Table 2: Comparison of Susceptibility Testing Methodologies
| Method | Principle | Time Requirement | Advantages | Limitations |
|---|---|---|---|---|
| Agar Dilution | Serial antimicrobial dilutions in agar | 24-48 hours | Gold standard, reproducible | Labor-intensive, resource-heavy |
| Disc Diffusion | Zone of inhibition measurement | 24 hours | Simple, cost-effective | Qualitative or semi-quantitative only |
| E-test | Gradient diffusion on strip | 24 hours | Quantitative MIC determination | Higher cost, variable results for some drugs [65] |
| 96-well Microtiter Assay | Broth microdilution in plate format | 20-24 hours | High-throughput, scalable [65] | Requires standardization |
| Pheno-molecular Assay | qPCR detection post-incubation with antibiotics | 4-6 hours [64] | Rapid, sensitive, specific | Requires specialized equipment and reagents |
Defined Media Formulations for Optimized Growth
The fastidious nature of N. gonorrhoeae necessitates rich media supplemented with specific growth factors. Recent research has validated simplified supplement formulations that maintain efficacy while reducing complexity and cost.
Media Composition and Preparation
Gonococcal (GC) agar base serves as the foundation, supplemented with either:
- Kellogg's Supplement: Contains glucose, L-glutamine, cocarboxylase, and ferric nitrate [65]
- Complex-Defined Growth Supplement (IsoVitaleX): More expensive alternative with additional components [65]
Research demonstrates that Kellogg's supplement performs comparably to the complex-defined growth supplement recommended by CLSI and EUCAST, providing a cost-effective alternative without compromising reliability [65].
Defined Media for Reproducible Results
Chemically defined media offer significant advantages for standardized antimicrobial testing by eliminating batch-to-batch variability associated with complex components like protein digests [68]. These media typically contain:
- Amino acids: 19-21 proteinogenic amino acids
- Energy sources: Glucose and pyruvate
- Vitamins and cofactors: Thiamine, niacin, cocarboxylase
- Salts and buffers: Maintaining ionic balance and pH
- Fatty acids: As nutritional components and potential permeabilizers [68]
Application Protocol: Time-Kill Kinetics Assay for N. gonorrhoeae
Strain Selection and Preparation
- Quality Control Strains: Include ATCC 49226 as recommended by CLSI/EUCAST [65]
- Clinical Isolates: Select strains with characterized resistance profiles (e.g., WHO reference panel) [64]
- Culture Conditions:
- Revive from glycerol stocks on chocolate agar with 1% Kellogg's supplement
- Incubate at 37°C in 5% CO₂ with 95% humidity for 18-24 hours
- Perform second passage to ensure logarithmic growth phase
Inoculum Standardization
- Prepare bacterial suspension in sterile PBS to 0.5 McFarland standard (~1.5 × 10⁸ CFU/mL)
- Dilute 1:9 in appropriate broth medium to achieve ~1 × 10⁷ CFU/mL
- Verify inoculum density by quantitative culture
Antimicrobial Preparation
- Stock Solutions: Prepare antimicrobial stocks at highest concentration (e.g., 25-50 mg/mL) [65]
- Working Concentrations: Create serial two-fold dilutions encompassing expected MIC range and higher multiples for kill kinetics
- Lyophilized Antibiotics: Recent studies show equivalent performance of lyophilized antibiotics in pheno-molecular assays [64]
Experimental Setup and Sampling
Figure 1: Experimental workflow for time-kill kinetics assay
High-Throughput 96-Well Microtiter Method
The adapted 96-well method offers significant advantages for time-kill kinetics studies:
Plate Preparation:
- Add 10μL of antimicrobial dilutions to first 10 wells of each row
- Add 190μL of 1% supplemented GC agar, mix gently
- Include positive (no antibiotic) and negative (no inoculum) controls
- Store plates at 4°C for maximum of 2 weeks [65]
Inoculation and Incubation:
- Apply 1μL of standardized inoculum (~1 × 10⁴ CFU) to prewarmed plates
- Incubate with lids ajar until drops absorb
- Continue incubation for 20-24 hours at 37°C with 5% CO₂ [65]
Automated Reading:
- Measure optical density or utilize automated imaging systems
- Alternatively, employ pheno-molecular approaches with qPCR detection [64]
Data Analysis and Interpretation
Time-Kill Curve Generation
Figure 2: Data analysis workflow for time-kill kinetics
Interpretation Criteria
- Bactericidal Activity: ≥3-log₁₀ reduction in CFU/mL compared to initial inoculum at 24 hours
- Bacteriostatic Activity: <3-log₁₀ reduction but no growth compared to initial inoculum
- Antibiotic Tolerance: Initial killing followed by regrowth
- Persister Cells: Subpopulation surviving high antibiotic concentrations
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for N. gonorrhoeae Antimicrobial Studies
| Reagent Category | Specific Products | Function/Application | Performance Notes |
|---|---|---|---|
| Growth Media | GC Agar Base | Solid support for growth | Requires supplementation for optimal growth |
| Nutritional Supplements | Kellogg's Supplement | Provides essential growth factors | Cost-effective alternative to IsoVitaleX [65] |
| Antibiotic Standards | Ceftriaxone, Azithromycin, Ciprofloxacin | Reference antimicrobials | Prepare fresh stocks or use lyophilized formats [64] |
| Quality Control Strains | ATCC 49226, WHO Reference Panel | Method validation and QC | Essential for verifying assay performance [65] [64] |
| Detection Systems | qPCR Master Mixes, Viability Stains | Quantification of bacterial viability | Enables pheno-molecular approaches [64] |
| Resistance Detection | rpsE Mutation-specific Primers [67] | Identification of spectinomycin resistance | Enables molecular confirmation of resistance mechanisms |
Troubleshooting and Technical Considerations
Common Challenges and Solutions
- Poor Growth: Verify supplement freshness and CO₂ concentration; pre-warm media before inoculation
- Variable MIC Results: Standardize inoculum preparation precisely; use logarithmic phase cultures
- Antibiotic Degradation: Prepare fresh stock solutions or verify stability of lyophilized forms
- Contamination: Implement strict sterile technique; include negative controls
Advantages of Pheno-Molecular Approaches
Recent advances in pheno-molecular testing combine short cultivation (4-6 hours) with quantitative PCR, offering:
- Rapid Results: 4 hours for most antibiotics, 6 hours for ceftriaxone [64]
- High Agreement: 92.4% categorical agreement with gold standard methods [64]
- Sensitivity: Detection at densities as low as 10² CFU/mL [64]
- Automation Potential: Adaptable to high-throughput screening platforms
The progressive resistance development in N. gonorrhoeae demands sophisticated research methodologies for evaluating novel antimicrobials. The protocols outlined herein, utilizing defined media and adapted for high-throughput applications, provide robust frameworks for time-kill kinetics studies. Integration of pheno-molecular approaches with traditional culture methods enhances the speed and precision of antimicrobial evaluation, accelerating the development of urgently needed therapeutic interventions for this multidrug-resistant pathogen.
Within antimicrobial evaluation research, the time-kill kinetics assay stands as a cornerstone method for characterizing the rate and extent of microbial killing by a potential therapeutic agent [2]. This protocol is framed within a broader thesis investigating the optimization of time-kill kinetics to generate robust, reliable, and clinically relevant data. Accurately defining bactericidal endpoints is a critical component of this process, ensuring that the data generated truly reflects the potency and killing dynamics of the compound under investigation. This document provides detailed application notes and protocols, focusing on the strategic selection of time points and the precise calculation of log reductions, to standardize the determination of bactericidal activity against challenging pathogens.
Theoretical Foundation: Log Reduction and Bactericidal Definitions
A fundamental understanding of log reduction is essential for accurately determining bactericidal endpoints. In microbiology, a log reduction represents the logarithmic relative change in the number of live microorganisms, calculated by comparing the colony-forming units per milliliter (CFU/mL) before and after treatment [69].
Mathematical Calculation
The log reduction is calculated using the following formula [69]:
Log Reduction = log10(Initial CFU / Final CFU)
This logarithmic value directly corresponds to a percentage reduction in the microbial population, providing a clear measure of an antimicrobial's efficacy [70]. The table below outlines the direct relationship between log reduction, percentage reduction, and the fraction of the original population that remains.
Table 1: Interpretation of Log Reduction Values
| Log Reduction | Percent Reduction | Fraction Remaining | CFU Remaining from 1,000,000 |
|---|---|---|---|
| 1 | 90% | 1/10 | 100,000 |
| 2 | 99% | 1/100 | 10,000 |
| 3 | 99.9% | 1/1,000 | 1,000 |
| 4 | 99.99% | 1/10,000 | 100 |
| 5 | 99.999% | 1/100,000 | 10 |
Defining Bactericidal Activity
The standard criterion for bactericidal activity is defined as a ≥ 3 log₁₀ (99.9%) reduction in the viable cell count of the original inoculum [2] [3]. This benchmark, equivalent to a 99.9% kill rate, is a critical endpoint that distinguishes a truly lethal agent from one that merely inhibits growth (bacteriostatic effect). In a time-kill assay, achieving this level of reduction at any time point confirms the bactericidal nature of the agent.
Experimental Design for Accurate Endpoint Determination
Strategic Selection of Time Points
A well-designed sampling schedule is crucial for capturing the full kinetic profile of microbial killing. The following time points are recommended to accurately define the endpoint:
- Early Phase (Rapid Killing): 5, 10, and 20 minutes [71]. These early intervals are critical for capturing the initial rate of kill, which is particularly important for fast-acting agents or antiseptics.
- Mid Phase (Progression): 60 minutes [71]. This point helps track the progression of killing activity as the agent continues to act.
- Late Phase (Prolonged Effect): Additional points up to 24 hours [2]. For many antibiotic agents, a 24-hour profile is standard to assess whether regrowth occurs due to agent degradation or the emergence of resistance.
This multi-phase approach ensures that the point of maximum kill (the bactericidal endpoint) is not missed and provides a comprehensive view of the agent's pharmacodynamics.
Workflow for Time-Kill Kinetics Assay
The following diagram illustrates the logical workflow of a time-kill kinetics assay, from experimental setup to data interpretation.
Detailed Protocol: Time-Kill Kinetics Assay
This protocol follows guidelines from the Clinical and Laboratory Standards Institute (CLSI) and is adapted from published methodologies [71] [2].
Materials and Reagents
Table 2: Research Reagent Solutions
| Item | Function / Description | Example / Specification |
|---|---|---|
| Mueller-Hinton Broth (MHB) | Standardized growth medium for susceptibility testing. | Commercially available, prepared according to manufacturer's instructions [71]. |
| Phthalate Buffer (pH 4.5) | Reconstitution and dilution of test substances to maintain stability. | Used for preparing stock solutions of test compounds like pomegranate rind extract [71]. |
| Neutralizing Buffer | Halts antimicrobial action at specified time points to prevent carryover. | Universal Quenching Agent (UQA); validation required per ASTM E1054 [71] [3]. |
| Mueller-Hinton Agar (MHA) | Solid medium for enumerating surviving colonies after treatment. | Used for pour- or spread-plating of neutralized samples [71]. |
Step-by-Step Procedure
- Inoculum Preparation: Adjust a fresh culture of the test organism to a turbidity equivalent to a 0.5 McFarland standard (approximately 1-5 x 10^8 CFU/mL for bacteria) in a suitable broth like MHB [71].
- Agent Addition: Add a standardized volume of the prepared inoculum (e.g., 10 µL) to tubes containing the antimicrobial agent at the desired test concentration(s), typically prepared in a vehicle like phthalate buffer. Include a vehicle-only control and a growth control (inoculum without agent) [71] [2].
- Incubation and Sampling: Incubate the test tubes under appropriate conditions (e.g., 37°C). At each predetermined time point (e.g., 0, 5, 10, 20, 60 minutes, and up to 24 hours), aseptically remove a 100 µL aliquot [71].
- Neutralization: Immediately transfer the aliquot into a tube containing 900 µL of a validated neutralizing solution. Vortex mix thoroughly to stop the antimicrobial action [71] [3].
- Viable Count Enumeration:
- Perform serial 10-fold dilutions of the neutralized sample in saline or broth.
- Plate 10 µL drops or spread 100 µL volumes from appropriate dilutions onto MHA plates in triplicate [71].
- Incubate plates for 18-24 hours at the requisite temperature.
- Data Collection: Count the colonies on plates with 30-300 colonies and calculate the CFU/mL for each sample at each time point using the formula [71]:
CFU/mL = (Number of colonies × Dilution Factor) / Volume plated
Data Analysis and Interpretation
Calculating Log Reduction and Generating the Kill Curve
For each time point, calculate the log reduction using the formula in Section 2.1, where "Initial CFU" is typically the count from the growth control at time zero. Plot the mean log₁₀ CFU/mL for each test condition and control against time to generate the time-kill curve [2].
Interpreting the Kill Curve
- Bactericidal: A decrease of ≥3 log₁₀ CFU/mL from the initial inoculum at any time point [2].
- Bacteriostatic: A reduction of <3 log₁₀ CFU/mL, where the agent inhibits growth but does not achieve substantial killing. The curve may remain near the starting inoculum level.
- Regrowth: An initial decrease in CFU followed by an increase at later time points, which may indicate degradation of the agent or the emergence of resistance.
Table 3: Key Criteria for Bactericidal Endpoint Determination
| Criterion | Description | Significance |
|---|---|---|
| Magnitude of Kill | ≥ 3 log10 reduction (99.9% killing). | Definitive benchmark for bactericidal action [2]. |
| Time to Endpoint | The specific time point at which the ≥3 log10 reduction is first achieved. | Indicates the speed of killing; critical for dosing regimens. |
| Rate of Killing | The slope of the kill curve between time points. | Reveals how rapidly the agent kills the population. |
| Regrowth Presence | Increase in CFU after an initial decline. | Suggests potential resistance or agent instability. |
Adherence to this detailed protocol for time-kill kinetics ensures the accurate and reproducible determination of bactericidal endpoints. The strategic selection of frequent, early time points, combined with precise log reduction calculations against the standardized 3-log benchmark, provides a robust framework for evaluating the killing dynamics of novel antimicrobial agents. This rigorous approach is indispensable for generating high-quality data that can reliably inform subsequent stages of drug development, ultimately contributing to the fight against antimicrobial resistance.
Ensuring Robust Data: Validation Strategies and Comparative Analysis with Other Methods
Within antimicrobial evaluation research, time-kill kinetics assays are fundamental for characterizing the rate and extent of antimicrobial activity against target microorganisms. However, the reliability of these assays hinges on rigorous validation of three core components: repeatability (intra-laboratory precision), reproducibility (inter-laboratory precision), and neutralization efficacy (accurate termination of antimicrobial action). This document provides detailed application notes and protocols to standardize these validation processes, ensuring data generated are robust, reliable, and suitable for regulatory submissions and scientific publication.
Determining Repeatability and Reproducibility
Definitions and Quantitative Measures
Repeatability refers to the precision of a method under the same operating conditions over a short interval of time, quantified by the repeatability standard deviation (Sr) [72]. Reproducibility assesses the precision of a method when the same protocol is applied in different laboratories, quantified by the reproducibility standard deviation (SR) [72]. For time-kill kinetics, the primary efficacy outcome is the log10 reduction (LR) in colony-forming units (CFU), with a reduction of ≥3 log10 (99.9% killing) typically defined as bactericidal activity [2] [3].
Table 1: Key Statistical Metrics for Assay Validation
| Metric | Definition | Interpretation | Ideal Value |
|---|---|---|---|
| Repeatability SD (Sr) | Standard deviation of LRs from replicate tests within a single laboratory [72]. | Measures within-laboratory precision. | As low as possible. |
| Reproducibility SD (SR) | Standard deviation of LRs from tests conducted across multiple laboratories [72]. | Measures between-laboratory precision. | SR ≤ SR,max. |
| SR,max | The maximum acceptable SR, determined by stakeholder specifications [72]. | Objective benchmark for reproducibility. | Dependent on μ, γ, and δ. |
A Statistical Decision Process for Reproducibility
An evidence-based decision process determines if a method's reproducibility is acceptable for a given application [72]. This process requires stakeholder-defined specifications:
- μ: The target (ideal true) log reduction value for the antimicrobial agents of interest.
- γ: The percentage of test results that must fall within an acceptable error margin of μ (e.g., 90%).
- δ: The maximum acceptable error (deviation from μ) for the proportion of tests defined by γ (e.g., 1, 2, or 3 log units).
A method is deemed acceptably reproducible if the SR estimated from a multi-laboratory study is less than or equal to the calculated SR,max [72]. The relationship between SR and the mean LR often follows a "frown-shaped" curve, where variability is highest for agents with moderate efficacy [72].
Figure 1: Workflow for the statistical decision process assessing assay reproducibility.
Protocol: Evaluating Repeatability and Reproducibility
Objective: To determine the repeatability and reproducibility standard deviations (Sr and SR) of a time-kill kinetics assay for a given antimicrobial agent.
Materials:
- Standardized antimicrobial agent(s) at specified concentrations.
- Reference microbial strains (e.g., Pseudomonas aeruginosa ATCC 15442, Staphylococcus aureus ATCC 6538).
- Validated growth media and neutralization solution.
Procedure:
- Study Design: A minimum of 3-5 independent laboratories participate. Each laboratory tests at least 2 replicate samples of the antimicrobial agent against each target microorganism on three separate days [72] [73].
- Testing: Each laboratory performs the time-kill kinetics assay per a standardized protocol. The log reduction (LR) is calculated at specified time points (e.g., 0, 1, 2, 4, 6, 24 hours) [2].
- Data Analysis:
- For each laboratory, calculate the mean LR and standard deviation for replicate tests to assess repeatability.
- Calculate the repeatability standard deviation (Sr) by pooling within-laboratory variances [72].
- Across all laboratories, calculate the overall mean LR and the reproducibility standard deviation (SR) [72].
- Decision: Using the stakeholder specifications (μ, γ, δ), calculate SR,max. The method is validated for reproducibility if SR ≤ SR,max [72].
Table 2: Example Reproducibility Data from a Multi-Laboratory Study
| Antimicrobial Agent | Test Microorganism | Mean Log Reduction (μ) | Sr | SR | SR,max (for γ=90%, δ=2) | Reproducibility Decision |
|---|---|---|---|---|---|---|
| DDAC 0.04% [73] | Staphylococcus aureus | ~3.0 | 0.087 - 0.317 [73] | ~1.0 [72] | ~1.2 [72] | Accept |
| Benchmark Formulation | Pseudomonas aeruginosa | ~5.5 | Not Reported | >1.5 [72] | ~1.2 [72] | Reject |
Validation of Neutralization Efficacy
The Critical Role of Neutralization
In time-kill kinetics and other antimicrobial efficacy tests, residual antimicrobial agent in the sampling fluid can continue to kill microorganisms after the designated contact time, leading to a significant overestimation of efficacy [74] [75]. Effective neutralization is therefore not optional but essential for obtaining valid results, particularly for non-volatile agents like chlorhexidine and antimicrobial peptides (AMPs) [74] [75].
Protocol: Neutralizer Effectiveness and Toxicity Testing (Based on ASTM E1054)
Objective: To validate that a chosen neutralizing solution effectively stops antimicrobial activity without being toxic to the microorganisms being recovered [76] [75].
Materials:
- Test antimicrobial agent (e.g., 2% chlorhexidine digluconate [75]).
- Proposed neutralizing solution (e.g., 3% polysorbate 80, 0.3% lecithin, 0.1% L-histidine [75] or 0.05% Sodium Polyanethol Sulfonate (SPS) for AMPs [74]).
- Challenge microorganisms (e.g., Staphylococcus aureus, Pseudomonas aeruginosa, Candida albicans).
Procedure: The test consists of three main parts, run in triplicate [76].
Neutralizer Effectiveness:
- Prepare a suspension of the test microorganism in a neutralizer solution to yield a low number of CFUs (30-100 CFU/mL) [76] [75].
- Add a aliquot of the antimicrobial agent to the microorganism-neutralizer mixture.
- Mix and within 1 minute, plate aliquots in duplicate onto solid recovery medium containing a neutralizer.
- Repeat plating after a storage period (e.g., 3 hours at 2-8°C) to test for carry-over activity [75].
Neutralizer Toxicity:
- Add the test microorganism to a tube containing the neutralizer solution and a non-antimicrobial solution (e.g., Phosphate Buffered Saline) [76].
- Mix and plate as above. This controls for any inhibitory effects of the neutralizer itself on microbial growth.
Viability Control (Baseline Growth):
- Add the test microorganism to a tube containing only a non-antimicrobial solution (e.g., Saline Peptone Water) [75].
- Mix and plate as above. This establishes the baseline recovery of microorganisms without any antimicrobial or neutralizer present.
Validation Criteria: The neutralization method is considered effective and non-toxic if the number of CFUs recovered in the Effectiveness test is not significantly less than the number recovered in the Viability Control, and the number recovered in the Toxicity test is not significantly less than the Viability Control [76] [75]. Statistical analysis (e.g., t-test) should be applied, with a common criterion being a difference of less than 0.5 log10 CFU [75].
Figure 2: Experimental workflow for validating neutralization efficacy according to standards like ASTM E1054.
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Reagents for Neutralization Validation in Antimicrobial Testing
| Reagent / Solution | Function / Application | Example Use Case |
|---|---|---|
| Sodium Polyanethol Sulfonate (SPS) | Neutralizes cationic antimicrobials like aminoglycosides, polymyxins, and antimicrobial peptides (AMPs) [74]. | Inactivation of SAAP-148, pexiganan, and chlorhexidine in efficacy tests [74]. |
| Lecithin & Polysorbate 80 | Neutralizers for a wide range of agents including quaternary ammonium compounds, chlorhexidine, and phenolics [75]. | Standard component in many neutralizing formulations for disinfectant testing [75]. |
| Sodium Thiosulfate | Effective neutralizer for halogen-based antimicrobials like iodine and chlorine [75]. | Used in neutralizer broths for testing antiseptics and disinfectants containing halogens. |
| Dey-Engley Neutralizing Broth | A general-purpose, all-in-one neutralizing growth medium designed to inactivate a broad spectrum of antimicrobial chemicals. | Often used in the recovery of microorganisms from disinfected or antiseptic-treated surfaces. |
| Validated Neutralizer Cocktails | Custom mixtures of neutralizers prepared and validated according to standards like ASTM E1054 for specific test formulations [76] [75]. | Essential for complex formulations containing multiple active ingredients to prevent false-positive efficacy results. |
Integrated Workflow for Time-Kill Kinetics Assay Validation
Figure 3: Integrated workflow for the comprehensive validation of a time-kill kinetics assay, incorporating neutralization, repeatability, and reproducibility assessments.
Within antimicrobial evaluation research, selecting an appropriate susceptibility testing method is fundamental to accurately determining the efficacy of antimicrobial agents and their combinations. While the time-kill kinetics assay provides a gold standard for assessing the bactericidal or fungicidal activity of antimicrobials over time, it is labor-intensive and low-throughput. Researchers frequently rely on more accessible, though sometimes less dynamic, methods for initial screening and combination therapy assessment. This application note provides a detailed comparative analysis of three common in vitro techniques—Disk Diffusion (DD), Broth Microdilution (BMD), and the Checkerboard Assay—framed within the context of a broader thesis on time-kill kinetics. We evaluate the operational strengths, limitations, and specific protocols for each method to guide researchers and drug development professionals in selecting the optimal tools for their investigative pipeline.
The table below summarizes the core characteristics, strengths, and limitations of each method, providing a high-level overview for researchers.
Table 1: Comparative overview of antimicrobial susceptibility testing methods
| Feature | Disk Diffusion (DD) | Broth Microdilution (BMD) | Checkerboard Assay |
|---|---|---|---|
| Core Principle | Diffusion of antibiotic into agar to form a concentration gradient [77] | Dilution of antimicrobial in broth to determine the Minimum Inhibitory Concentration (MIC) [77] | Two-dimensional broth microdilution to test multiple drug combination ratios [78] |
| Primary Output | Zone of Inhibition (ZOI) diameter | Minimum Inhibitory Concentration (MIC) | Fractional Inhibitory Concentration Index (FICi) |
| Throughput | High [79] | Medium | Low [78] |
| Speed/Turnaround | 18-24 hours; Direct DD can provide results within 24h of positive culture [79] | 24-48 hours [77] | 48-72 hours [78] |
| Quantitative Output | Semi-quantitative | Quantitative | Quantitative (FICi) |
| Key Strengths | Low cost, easy to perform, suitable for screening large isolate numbers [79] | Gold standard for MIC, quantitative, can be automated [77] | Standardized method for quantifying synergy/antagonism [78] |
| Major Limitations | Lacks precise MIC, influenced by agar depth and diffusion coefficient [77] | Static system, cannot replicate complex in vivo dynamics [77] | Labor-intensive, high workload and variability [78] |
| Best Application | Rapid phenotypic AST and large-scale surveillance studies [79] [80] | Definitive MIC determination for clinical breakpoints and regulatory work | In-depth analysis of specific drug-drug interactions |
Detailed Experimental Protocols
Disk Diffusion (DD) Testing
The DD test is a cornerstone of phenotypic antimicrobial susceptibility testing (AST) due to its simplicity and cost-effectiveness.
Workflow: Disk Diffusion Assay
Protocol Steps:
- Agar Plate Preparation: Pour Mueller-Hinton Agar (MHA) into sterile Petri dishes to a uniform depth of 4 mm. For fastidious organisms, supplement with blood or other required nutrients.
- Inoculum Standardization: Prepare a microbial suspension from fresh overnight colonies in a saline or broth solution. Adjust the turbidity to match the 0.5 McFarland standard (approximately 1-2 x 10^8 CFU/mL for bacteria).
- Inoculation: Within 15 minutes of standardization, dip a sterile cotton swab into the inoculum, remove excess fluid, and swab the entire surface of the MHA plate in three directions (rotating the plate ~60° each time) to ensure a confluent lawn.
- Disk Application: Using sterile forceps or an automated dispenser, place antibiotic disks firmly onto the inoculated agar surface. Disks should be spaced evenly and at least 24 mm apart (center to center) to prevent overlapping inhibition zones.
- Incubation: Invert plates and incubate at 35±2°C for 16-18 hours in an ambient air incubator. Incubation time may be extended for slow-growing organisms.
- Reading and Interpretation: After incubation, use calipers or an automated zone scanner to measure the diameter of each inhibition zone (including the disk diameter) to the nearest millimeter. Interpret results as Susceptible (S), Intermediate (I), or Resistant (R) based on current CLSI M100 or EUCAST breakpoint tables [81].
Direct Disk Diffusion: For rapid testing from positive blood cultures, a sample of the broth can be used directly for inoculation after standardization, significantly reducing time to results [79].
Broth Microdilution (BMD) Testing
BMD is the reference method for determining the Minimum Inhibitory Concentration (MIC), providing a quantitative measure of antimicrobial potency.
Workflow: Broth Microdilution Assay
Protocol Steps:
- Panel Preparation: Prepare a two-fold serial dilution of the antimicrobial agent in cation-adjusted Mueller-Hinton Broth (CAMHB) within the wells of a sterile 96-well microtiter plate. This can be done manually or using pre-manufactured, commercially available panels (e.g., Sensititre systems [80]).
- Inoculum Standardization: Prepare a microbial suspension as for DD and further dilute it in broth to achieve a final concentration of approximately 5 x 10^5 CFU/mL in each well.
- Inoculation: Dispense the standardized inoculum into each well of the microdilution plate. Include growth control (inoculum without antibiotic) and sterility control (broth only) wells.
- Incubation: Cover the plate and incubate at 35±2°C for 16-20 hours.
- Reading the MIC: The MIC is defined as the lowest concentration of antimicrobial that completely inhibits visible growth of the organism. Examine the plates over a dark, non-reflective surface. The Minimum Bactericidal Concentration (MBC) can be determined by subculturing from clear wells onto agar plates to achieve >99.9% killing [77].
Checkerboard Assay
The checkerboard assay is the classical method for quantifying interactions (synergy, antagonism, additivity) between two antimicrobial agents.
Workflow: Checkerboard Assay
Protocol Steps:
- Panel Setup: In a 96-well microtiter plate, prepare a two-fold serial dilution of Drug A along the rows (e.g., from left to right, with decreasing concentrations). Independently, prepare a two-fold serial dilution of Drug B along the columns (e.g., from top to bottom). This creates a matrix where each well contains a unique combination of the two drugs [78].
- Inoculation: Add a standardized inoculum (5 x 10^5 CFU/mL final concentration) to all wells. Include controls for each drug alone, a growth control, and a sterility control.
- Incubation and MIC Determination: Incubate the plate at 35±2°C for 24 hours (or longer for fungi). Determine the MIC of each drug alone (MICA and MICB) and the MIC of each drug in combination (MICA,B and MICB,A).
- Calculation of FICi:
- Calculate the Fractional Inhibitory Concentration (FIC) for each drug in the combination:
- FICA = MIC of Drug A in combination / MIC of Drug A alone
- FICB = MIC of Drug B in combination / MIC of Drug B alone
- Calculate the FIC Index (FICi): FICi = FICA + FICB
- Calculate the Fractional Inhibitory Concentration (FIC) for each drug in the combination:
- Interpretation:
- Synergy: FICi ≤ 0.5 [78]
- Additivity/Indifference: 0.5 < FICi ≤ 4
- Antagonism: FICi > 4
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential materials and reagents for antimicrobial susceptibility testing
| Item | Function/Application | Key Considerations |
|---|---|---|
| Mueller-Hinton Agar/Broth | Standard medium for AST; provides reproducibility and consistent diffusion. | Must be cation-adjusted for broth (CAMHB). Supplementation required for fastidious organisms (e.g., S. pneumoniae). |
| Antibiotic Disks | Source of antibiotic for diffusion-based tests (DD). | Stable, predefined drug concentrations. Require proper storage (-20°C or 2-8°C) to maintain potency. |
| Sensititre Broth Microdilution Plates | Commercial BMD system with pre-dispensed, dried antibiotics. | Enables high-throughput, standardized MIC testing. Custom panels can be designed [80]. |
| 0.5 McFarland Standard | Reference for standardizing microbial inoculum density. | Ensures reproducible and accurate results across all methods. Can be prepared in-house or purchased. |
| 96-Well Microtiter Plates | Platform for performing BMD and checkerboard assays. | Must be sterile and non-cytotoxic. U-bottom wells are typically used for clearer visual endpoints. |
Integration with Time-Kill Kinetics Research
While the methods described above are excellent for determining inhibitory endpoints (MIC, ZOI, FICi), they provide a static snapshot and do not directly inform on the rate and extent of microbial killing, which is the domain of time-kill kinetics (TKK) assays. The strengths of DD, BMD, and checkerboard assays make them ideal for high-throughput screening and initial interaction profiling. For instance, a novel combination plate method for antifungal testing, which operates on a principle similar to DD but for three drugs simultaneously, can screen 92 isolates for multiple combinations overnight, identifying promising synergistic pairs for further study [78]. These synergistic pairs, once identified, become prime candidates for in-depth TKK analysis to characterize the killing dynamics over 24 hours, confirming whether the inhibitory synergy observed in the checkerboard assay translates to enhanced, concentration-dependent killing rates—a critical step for validating combination therapies intended for clinical use.
The transition from in vitro activity to in vivo efficacy is a critical challenge in antimicrobial drug development. Pharmacodynamic (PD) modeling, particularly when integrated with pharmacokinetic (PK) data, provides a powerful mathematical framework to bridge this gap. PD modeling quantitatively describes what the drug does to the body, defining the relationship between drug concentration and effect [82]. In the context of antimicrobial research, time-kill kinetics assays serve as a primary source of in vitro PD data, characterizing the rate and extent of antimicrobial killing over time [2]. This article details how these in vitro results can be correlated with in vivo efficacy through PK/PD modeling, providing researchers with structured protocols and visualization tools to enhance their antimicrobial development programs.
Quantitative Parameters from Time-Kill Kinetics Assays
Time-kill kinetics assays generate quantitative data on the rate and extent of microbial killing. The key parameters derived from these assays, summarized in the table below, form the foundation for building robust PD models.
Table 1: Key Quantitative Parameters from Time-Kill Kinetics Assays
| Parameter | Description | Interpretation |
|---|---|---|
| Bactericidal Activity | ≥ 3 log10 (99.9%) decrease in Colony Forming Units (CFU) from the starting inoculum [2]. | The agent is capable of killing the pathogen. |
| Bacteriostatic Activity | The log10 CFU over time remains roughly the same as the starting concentration [2]. | The agent inhibits growth but does not kill. |
| Minimum Inhibitory Concentration (MIC) | The lowest concentration of an antimicrobial that prevents visible growth. | A static endpoint of growth inhibition. |
| Minimum Bactericidal Concentration (MBC) | The lowest concentration that achieves a 99.9% (3 log10) reduction in the original bacterial inoculum at a specified time [2]. | A cidal endpoint of killing efficacy. |
The following diagram illustrates a typical outcome of a time-kill kinetics assay, demonstrating how these parameters are visualized and interpreted over time.
Experimental Protocol: Time-Kill Kinetics Assay
This protocol is adapted from standard CLSI guidelines (M26) and representative research methodologies [5] [2].
Materials and Reagents
Table 2: Research Reagent Solutions for Time-Kill Kinetics Assay
| Item | Function/Description | Example/Standard |
|---|---|---|
| Culture Media | Supports microbial growth. Nutrient broth and Sabouraud dextrose agar are common [5]. | Nutrient Broth, Sabouraud Dextrose Agar [5]. |
| Test Organisms | Standardized bacterial/fungal strains for consistent and reproducible testing. | Escherichia coli ATCC 25922, Staphylococcus aureus ATCC 25923 [5]. |
| Antimicrobial Agent | The compound under investigation. Prepared in an appropriate solvent. | Test extract dissolved in 70% v/v methanol [5]. |
| Neutralizing Fluid | Halts antimicrobial action at specific time points to enable accurate survivor counting [3]. | Validated per ASTM E1054 [3]. |
| Positive Control | A known antimicrobial agent to validate assay performance. | Ciprofloxacin (for bacteria), Ketoconazole (for fungi) [5]. |
| Saline (0.9%) | A balanced salt solution used for preparing microbial suspensions and dilutions [3]. | - |
Step-by-Step Procedure
- Preparation of Inoculum: Harvest test organisms from fresh agar plates and suspend in 0.9% saline. Adjust the turbidity of the suspension to match a 0.5 McFarland standard, yielding a starting inoculum of approximately 1-5 x 108 CFU/mL for bacteria [5] [3].
- Exposure Setup: In sterile tubes, combine the growth medium with the antimicrobial agent at predetermined concentrations (e.g., 1x, 2x, 4x MIC). Include a growth control (media + inoculum, no antimicrobial) and a vehicle control (media + inoculum + solvent) [2].
- Inoculation and Incubation: Inoculate each tube with the prepared microbial suspension. Incubate the tubes under appropriate conditions (e.g., 37°C with shaking for bacteria).
- Sampling: At specified time intervals (e.g., 0, 2, 4, 6, 8, and 24 hours), aseptically remove a measured sample aliquot from each tube [3].
- Neutralization and Serial Dilution: Immediately transfer the aliquot into a validated neutralizing fluid to stop the antimicrobial action [3]. Perform serial 10-fold dilutions of the neutralized sample in saline or broth.
- Viable Counting: Plate aliquots from appropriate dilutions onto agar plates. Incubate the plates for a predetermined time to allow colony formation.
- Data Calculation: Count the colonies and calculate the viable microbial density (log10 CFU/mL) for each sample at each time point. Plot the data as log10 CFU/mL versus time to generate time-kill curves like the one shown in the diagram above.
From In Vitro Data to In Vivo Prediction: The PK/PD Modeling Workflow
The workflow below outlines the process of integrating in vitro time-kill data with PK models to predict in vivo efficacy and optimize dosing regimens.
Developing the Pharmacodynamic (PD) Model
The quantitative parameters from the time-kill curve are used to develop a mathematical PD model. A fundamental concept is the sigmoid Emax model, which has its origins in receptor theory [82]. This model describes how the drug effect (E) changes with concentration (C):
E = E₀ + (Emax × Cγ) / (EC50γ + Cγ)
Where:
- E₀ is the baseline effect in the absence of drug.
- Emax is the maximum possible drug effect.
- EC50 is the concentration that produces 50% of Emax (a measure of drug potency).
- γ is the Hill coefficient, which describes the steepness of the concentration-effect curve [82].
Time-kill data at various concentrations can be fit to this model or its derivatives to estimate these critical PD parameters (Emax, EC50), which describe the drug's intrinsic efficacy and potency.
Accounting for Effect Delays: Hysteresis
A direct plot of observed in vivo effect versus plasma concentration may show a loop, known as hysteresis. This indicates a temporal disconnect between plasma concentration and effect [82].
- Counter-clockwise hysteresis occurs when the effect lags behind the concentration, which is common with antimicrobials due to factors like slow distribution to the target site [82].
- Clockwise hysteresis can indicate the development of tolerance [82].
To account for this, a hypothetical effect compartment is often incorporated into the model. This compartment is linked to the plasma PK and introduces a delay, allowing the model to accurately describe the observed effect-time profile rather than the effect-concentration relationship.
Application in Drug Development and Regulatory Science
PK/PD modeling is indispensable in modern antimicrobial development. It moves beyond simple MIC reporting to provide a dynamic understanding of drug action. These models can be used to simulate different dosing regimens, identify optimal PK/PD indices (e.g., T > MIC, Cmax/MIC), and support the justification of dosing strategies for clinical trials [83]. Furthermore, regulatory agencies recognize the value of modeling; the US FDA states that PD modeling can contribute to "substantial evidence of effectiveness" and add to the "weight of evidence supporting efficacy" [82]. By bridging in vitro time-kill kinetics with in vivo outcomes, PK/PD modeling provides a powerful, quantitative framework for advancing new antimicrobial agents from the bench to the bedside.
The rise of multidrug-resistant bacterial pathogens poses a significant challenge to global public health, necessitating the development of novel antibacterial agents. Sulopenem, a penem antibiotic with both intravenous and oral formulations, represents a promising therapeutic option for infections caused by resistant organisms, particularly in urinary tract and intra-abdominal infections [84] [85]. Unlike traditional carbapenems, sulopenem's distinct chemical structure allows for oral administration, facilitating step-down therapy and potentially reducing hospital stays.
This application note provides a detailed framework for evaluating the in vitro antimicrobial activity of sulopenem using time-kill kinetics and complementary methodologies. The data and protocols presented herein are framed within the broader context of antimicrobial evaluation research, offering scientists and drug development professionals a standardized approach for characterizing novel antibiotic agents. We demonstrate how time-kill kinetics, when integrated with post-antibiotic effect (PAE) studies and synergy testing, can provide comprehensive insights into the pharmacodynamic profile of sulopenem against clinically relevant pathogens, thereby supporting optimal dosing regimen design and further clinical development [85].
Theoretical Background and Key Concepts
Time-Kill Kinetics Fundamentals
Time-kill kinetics assays are essential pharmacodynamic tools that quantify the rate and extent of bactericidal or bacteriostatic activity of an antimicrobial agent over time. Unlike static minimum inhibitory concentration (MIC) measurements, which provide a single-time-point threshold value, time-kill kinetics capture the dynamic interaction between an antibiotic and a bacterial population, revealing the concentration-dependent killing characteristics of the drug [86]. This method allows researchers to determine whether an agent exhibits concentration-dependent killing (where higher concentrations result in increased killing rates) or time-dependent killing (where the duration of exposure is more critical than peak concentration).
The assay measures the viable bacterial count (in colony-forming units per milliliter, CFU/mL) at predetermined time points after exposure to various antibiotic concentrations. Bactericidal activity is formally defined as a ≥3 log10 (99.9%) reduction in viable organism counts compared to the initial inoculum, while bacteriostatic activity is defined as maintenance of the initial inoculum with less than a 99.9% reduction [33]. The resulting time-kill curves provide visual representation of the rate and extent of microbial killing, enabling researchers to identify potential regrowth phenomena due to adaptive resistance or the emergence of resistant subpopulations.
Complementary Methodologies for Comprehensive Profiling
A complete antimicrobial evaluation extends beyond time-kill kinetics to include several complementary assays:
Post-Antibiotic Effect (PAE): This parameter measures the persistent suppression of bacterial growth after brief exposure to an antimicrobial agent, followed by its removal or inactivation [85]. A prolonged PAE allows for less frequent dosing intervals in clinical practice.
Sub-Minimum Inhibitory Concentration Effect (PAE-SME): This measures the growth suppression when bacteria are re-exposed to sub-inhibitory concentrations of an antibiotic following initial exposure at higher concentrations [85].
Checkerboard Synergy Testing: This method evaluates potential interactions (synergistic, additive, indifferent, or antagonistic) between multiple antimicrobial agents by calculating the fractional inhibitory concentration (ΣFIC) index [85].
Experimental Design and Workflow
The comprehensive evaluation of a novel antibiotic requires a systematic approach integrating multiple in vitro methodologies. The workflow below outlines the key stages in characterizing the antimicrobial activity of sulopenem:
Bacterial Strains and Growth Conditions
The experimental design should include reference strains and clinically relevant isolates to ensure comprehensive assessment of the compound's spectrum of activity. For sulopenem evaluation, the following strains are recommended:
- Escherichia coli ATCC 25922, NCTC 13353, and ATCC 35218
- Klebsiella pneumoniae ATCC 700603
- Clinical isolates of E. coli and K. pneumoniae, including fluoroquinolone-resistant and extended-spectrum β-lactamase (ESBL)-producing strains [85]
Bacterial cultures should be prepared by inoculating a single colony into Mueller Hinton Broth (MHB) and incubating overnight at 37°C. A subculture (1:100 dilution) should then be incubated for 1.5-2 hours at 200 rpm to achieve mid-logarithmic growth phase (approximately 108 CFU/mL) [33]. The inoculum for all assays should be standardized to 1-5 × 105 CFU/mL to ensure consistent and reproducible results across experiments.
Research Reagent Solutions
Table 1: Essential research reagents and materials for time-kill kinetics evaluation of novel antibiotics
| Item | Specification/Recommended Type | Primary Function |
|---|---|---|
| Mueller Hinton Broth (MHB) | Standardized according to CLSI guidelines | Growth medium for bacterial cultivation and susceptibility testing [33] |
| Antibiotic Stock Solutions | High-purity reference standards | Preparation of working solutions at precise concentrations [85] |
| Comparator Agents | Amoxicillin, aztreonam, ceftriaxone, doxycycline, gentamicin, levofloxacin, nitrofurantoin, trimethoprim-sulfamethoxazole | Reference compounds for synergy testing and comparative activity assessment [85] |
| Quality Control Strains | E. coli ATCC 25922, E. coli ATCC 35218, K. pneumoniae ATCC 700603 | Verification of assay performance and reproducibility [85] |
| Sterile Phosphate Buffered Saline (PBS) | 0.1 M, pH 7.3 | Diluent for bacterial suspensions and serial dilutions |
| Agar Plates | Mueller Hinton Agar (MHA) | Enumeration of viable bacteria via colony counting |
Detailed Experimental Protocols
Time-Kill Kinetics Assay
The following protocol is adapted from established methodologies with specific modifications for sulopenem evaluation [33] [85]:
Preparation of Antibiotic Solutions: Prepare sulopenem working solutions in MHB at concentrations corresponding to 1×, 2×, 4×, and 8× the predetermined MIC for each test strain.
Inoculum Standardization: Adjust the mid-log phase bacterial culture to approximately 1-5 × 105 CFU/mL in fresh MHB.
Assay Setup: Combine equal volumes (250 μL each) of the standardized bacterial suspension and antibiotic working solution in sterile tubes. Include growth control tubes (bacteria without antibiotic) and sterility control tubes (media only).
Incubation and Sampling: Incubate all tubes at 37°C with constant shaking at 180 rpm. Remove samples (100 μL) at predetermined time points: 0, 30 min, 1, 3, 5, 8, and 24 hours.
Viable Count Determination: Perform serial 10-fold dilutions in sterile PBS for each sample. Plate 100 μL of appropriate dilutions onto Mueller Hinton Agar plates in duplicate. Incubate plates at 37°C for 18-24 hours, then enumerate colonies.
Data Analysis: Calculate log10 CFU/mL for each time point and plot time-kill curves. Bactericidal activity is defined as a ≥3 log10 reduction in CFU/mL compared to the initial inoculum, while bacteriostatic activity maintains the initial inoculum with <99.9% reduction [33].
Checkerboard Synergy Testing
Preparation of Drug Solutions: Prepare serial two-fold dilutions of sulopenem and comparator agents in MHB across 96-well microtiter plates.
Combination Setup: Arrange the plate such that each well contains a unique combination of sulopenem and the test agent at specific concentrations.
Inoculation and Incubation: Inoculate each well with the standardized bacterial suspension (final inoculum 5 × 105 CFU/mL). Incubate plates at 37°C for 18-24 hours.
Fractional Inhibitory Concentration (FIC) Calculation: Determine the MIC of each agent alone and in combination. Calculate the FIC index using the formula: ΣFIC = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone).
Interpretation: Classify interactions as follows: synergy (ΣFIC ≤0.5), indifference (ΣFIC >0.5 to ≤4), or antagonism (ΣFIC >4) [85].
Post-Antibiotic Effect (PAE) and PAE-SME Assessment
Antibiotic Exposure: Expose logarithmic-phase bacteria (approximately 108 CFU/mL) to sulopenem at concentrations of 1×, 5×, and 10× MIC for 2 hours.
Antibiotic Removal: Dilute the culture 1:1000 in prewarmed fresh MHB to effectively remove the antibiotic.
PAE Determination: Monitor bacterial growth by measuring optical density at 600 nm or performing viable counts at regular intervals. Calculate PAE using the formula: PAE = T - C, where T is the time required for the antibiotic-exposed culture to increase 1 log10 CFU/mL after dilution, and C is the corresponding time for the untreated control.
PAE-SME Assessment: Following the initial antibiotic exposure and dilution, add sub-inhibitory concentrations (0.5× MIC) of sulopenem to the culture medium and measure the extended growth suppression (PAE-SME) using the same calculation method [85].
Key Findings and Data Interpretation
Sulopenem Time-Kill Kinetics Results
Table 2: Time-kill kinetics results for sulopenem against Escherichia coli and Klebsiella pneumoniae isolates [85]
| Antibiotic Concentration | Bactericidal Activity (≥3 log10 Reduction) | Time to Bactericidal Activity | Strains Tested |
|---|---|---|---|
| 1× MIC | Variable | >24 hours | 6/6 isolates |
| 8× MIC | 100% (6/6 isolates) | Within 8 hours (5/6 isolates) | 6/6 isolates |
| Growth Control | No reduction | Not applicable | 6/6 isolates |
Sulopenem demonstrated concentration-dependent bactericidal activity against all tested isolates. At 8× MIC, the antibiotic achieved a ≥3 log10 (99.9%) reduction in viable bacterial counts against all six isolates within 24 hours, with five of the six isolates showing this bactericidal activity within just 8 hours of exposure [85]. These findings suggest that sulopenem exhibits rapid and concentration-dependent killing against Enterobacterales, supporting the exploration of higher dosing regimens to achieve maximal bactericidal effect in clinical settings.
Complementary Assay Results
Table 3: Post-antibiotic effect and synergy testing results for sulopenem [85]
| Assay Type | Experimental Condition | Result | Interpretation |
|---|---|---|---|
| Post-Antibiotic Effect (PAE) | 1×, 5×, or 10× MIC | 0.0-0.7 hours | Minimal concentration-dependent PAE |
| PAE-Sub-MIC Effect (SME) | 0.5× MIC following 5× MIC | >4.8 hours | Prolonged growth suppression |
| Checkerboard Synergy | Sulopenem + TMP-SMX vs. E. coli | ΣFICmin = 0.38-0.5 | Synergistic interaction |
| Checkerboard Synergy | Sulopenem + Gentamicin vs. K. pneumoniae | ΣFICmin = 0.5 | Synergistic interaction |
| Checkerboard Testing | Majority of combinations | ΣFIC >0.5 to ≤4 | Indifference (no antagonism) |
The PAE and synergy testing results provide additional dimensions to sulopenem's pharmacodynamic profile. While the direct PAE was minimal (0.0-0.7 hours), the markedly prolonged PAE-SME (>4.8 hours) suggests that sub-inhibitory concentrations can effectively suppress bacterial regrowth following initial bactericidal exposure [85]. Checkerboard assays revealed no antagonism between sulopenem and comparator agents, with indifference observed in most combinations. Notably, synergistic interactions were identified with trimethoprim-sulfamethoxazole against E. coli and with gentamicin against K. pneumoniae, suggesting potential combination therapy approaches for difficult-to-treat infections [85].
The relationship between sulopenem concentration and its antimicrobial effects across different assays can be visualized as follows:
Regulatory Considerations and Standards
When conducting antimicrobial susceptibility testing, adherence to established standards is paramount for generating clinically relevant data. The Clinical and Laboratory Standards Institute (CLSI) guidelines, particularly M02, M07, and M100, represent the gold standard for antimicrobial susceptibility testing methodology and interpretation [87]. These standards are recognized by regulatory agencies including the U.S. Food and Drug Administration (FDA) [88].
For sulopenem specifically, the FDA has identified exceptions or additions to the recognized CLSI standards, underscoring the importance of consulting the most current regulatory guidance when designing studies and interpreting results [88]. Similarly, the European Committee on Antimicrobial Susceptibility Testing (EUCAST) provides regularly updated clinical breakpoint tables that are essential for categorizing microorganisms as susceptible, susceptible with increased exposure, or resistant to antimicrobial agents [89].
The comprehensive in vitro evaluation of sulopenem using time-kill kinetics and complementary methodologies reveals a promising pharmacodynamic profile characterized by:
Concentration-dependent bactericidal activity achieving ≥3 log10 reduction in viable counts within 8 hours at 8× MIC concentrations.
Favorable interaction profile with no observed antagonism when combined with other antimicrobial classes and synergistic activity with specific agents.
Prolonged sub-MIC effects (PAE-SME >4.8 hours) that may support less frequent dosing intervals in clinical practice.
These findings support the continued development of sulopenem for multidrug-resistant infections, particularly uncomplicated urinary tract infections where it has demonstrated efficacy against amoxicillin-clavulanate and in fluoroquinolone-resistant uUTI in phase 3 clinical trials [84] [85]. The oral dosing regimen of sulopenem etzadroxil/probenecid 500 mg/500 mg administered every 12 hours appears pharmacodynamically sound based on these in vitro parameters.
For researchers applying these protocols, we recommend:
- Adherence to CLSI guidelines for all susceptibility testing procedures
- Inclusion of appropriate quality control strains in each experiment
- Investigation of additional Gram-negative pathogens and resistant phenotypes
- Exploration of the relationship between in vitro time-kill results and in vivo efficacy through pharmacokinetic/pharmacodynamic modeling
The methodologies outlined in this application note provide a robust framework for the comprehensive evaluation of novel antimicrobial agents, contributing valuable data to support their clinical development and optimal use in practice.
The escalating threat of antimicrobial resistance (AMR) necessitates a renewed effort in the discovery and development of novel therapeutic agents [22]. Natural products, particularly plant-derived compounds, represent a promising source for new antimicrobials due to their complex chemical structures and diverse mechanisms of action [90] [91]. Time-kill kinetics assays are a cornerstone of in vitro antimicrobial evaluation, providing a dynamic, quantitative assessment of an agent's bactericidal or bacteriostatic activity over time, unlike static endpoints like the minimum inhibitory concentration (MIC) [92]. This case study focuses on evaluating the antibacterial efficacy of plumbagin (5-hydroxy-2-methyl-1,4-naphthoquinone), a bioactive naphthoquinone isolated from the roots of Plumbago zeylanica L., using a detailed time-kill kinetics protocol [22] [90]. The objective is to present a standardized framework for assessing the concentration- and time-dependent effects of plumbagin, thereby contributing to the preclinical evidence base for this potent natural product.
Plumbagin: A Potent Antimicrobial Natural Product
Plumbagin is a yellow pigment identified as the major active constituent of Plumbago zeylanica roots, a plant used in traditional medicine for treating wounds, tuberculosis, and rheumatic pains [22]. Its significance in antimicrobial research is underscored by its potent, broad-spectrum activity against a range of multidrug-resistant (MDR) Gram-positive and Gram-negative bacteria, including Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, and Klebsiella pneumoniae [22] [91].
Mechanisms of Action: Research indicates that plumbagin exerts its antibacterial effects through multiple mechanisms, making it a promising lead compound for overcoming resistance. Key mechanisms include:
- Disruption of Cell Membrane: Plumbagin impairs the structure and function of the bacterial cell membrane, leading to increased permeability, leakage of potassium ions (K+), and extrusion of nucleic acids [93].
- Induction of Oxidative Stress: Treatment with plumbagin increases intracellular levels of reactive oxygen species (ROS) and malondialdehyde (MDA), while reducing the activity of antioxidant enzymes like catalase (CAT) and superoxide dismutase (SOD), causing oxidative damage to bacterial cells [93].
- Inhibition of Biofilm Formation: Plumbagin demonstrates robust activity against biofilms, a key virulence factor. It significantly reduces the extracellular polymeric substances (EPS) in S. aureus biofilms, particularly targeting extracellular DNA (eDNA) at low concentrations, followed by polysaccharides and proteins [94].
- Disruption of Metabolism: Metabolomic studies reveal that plumbagin severely affects central metabolic pathways in E. coli, including the TCA cycle, glutathione metabolism, amino acid synthesis, and lipid metabolism [93].
Synergistic Potential: Plumbagin exhibits resistance modulation action, potentiating the effects of conventional antibiotics. For instance, a subinhibitory concentration of plumbagin (4 µg/mL) was shown to potentiate the activity of ketoconazole against Candida albicans by up to 12-fold [22].
The following table summarizes key efficacy data for plumbagin against various bacterial pathogens, providing a quantitative overview of its antimicrobial potential.
Table 1: Antibacterial and Anti-Biofilm Efficacy of Plumbagin Against Selected Pathogens
| Bacterial Strain | MIC (µg/mL) | MBC (µg/mL) | MBIC (µg/mL) | Key Findings | Source |
|---|---|---|---|---|---|
| Staphylococcus aureus | 0.5 - 4 | 0.235 - 0.94 | 16 | Disrupted biofilm EPS; eDNA most sensitive target (inhibited at 4 µg/mL). | [22] [94] [91] |
| Escherichia coli | 31.25 - 8 | Not Reported | Not Reported | Caused cell membrane damage, oxidative stress, and metabolic disruption. | [22] [93] |
| Pseudomonas aeruginosa | 8 | 0.94 | Not Reported | Growth inhibited; susceptible to plumbagin in MDR clinical isolates. | [22] [91] |
| Klebsiella pneumoniae | 8 | Not Reported | Not Reported | Growth inhibited at low concentrations. | [22] |
| Staphylococcus saprophyticus | 0.029 | 0.235 | Not Reported | Exhibited highest sensitivity among tested MDR clinical isolates. | [91] |
Experimental Protocol: Time-Kill Kinetics Assay
This protocol details the steps for conducting a time-kill kinetics study to evaluate the efficacy of plumbagin against a target bacterium, such as Staphylococcus aureus.
Principle
The time-kill kinetics assay measures the rate and extent of bactericidal or bacteriostatic activity of an antimicrobial agent over a defined period (typically 0-24 hours) [92]. It determines whether an agent's effect is concentration-dependent or time-dependent and classifies it as bactericidal (≥3-log10 reduction in CFU/mL) or bacteriostatic (<3-log10 reduction) [22] [92].
Materials and Reagents
Table 2: Research Reagent Solutions and Essential Materials
| Item | Function/Explanation |
|---|---|
| Plumbagin (from P. zeylanica) | The natural product compound under investigation; stock solution is typically prepared in Dimethyl Sulfoxide (DMSO) [22] [91]. |
| Dimethyl Sulfoxide (DMSO) | A common solvent for dissolving hydrophobic compounds like plumbagin; used at a final concentration that is non-toxic to bacteria (e.g., ≤1% v/v) [91]. |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | The standardized, nutrient-rich medium recommended by CLSI for antimicrobial susceptibility testing, supporting robust bacterial growth [15] [88]. |
| Sterile Phosphate Buffered Saline (PBS) | Used for serial dilution of bacterial samples to a countable range (typically 30-300 CFU per plate) for colony counting [4]. |
| Agar Plates (e.g., Mueller Hinton Agar) | A solid growth medium used for the determination of viable bacterial counts via the colony-forming unit (CFU) method [4]. |
| Bioluminescent Bacterial Strains (e.g., S. aureus SAP229) | Engineered strains expressing luciferase; provide a real-time, non-destructive measure of bacterial viability through light emission, complementing CFU counts [15]. |
Workflow Diagram
The following diagram illustrates the comprehensive experimental workflow for the time-kill kinetics assay.
Step-by-Step Procedure
Preparation of Inoculum:
- Grow the test organism (e.g., S. aureus ATCC 25923) overnight in Mueller Hinton Broth (MHB) at 37°C.
- Dilute the overnight culture in fresh, pre-warmed MHB to a turbidity equivalent to a 0.5 McFarland standard, which corresponds to approximately 1-2 x 10^8 CFU/mL.
- Further dilute this suspension in MHB to achieve a final working concentration of approximately 5 x 10^5 CFU/mL in the test vessel [4] [92].
Compound Preparation:
- Prepare a stock solution of plumbagin in DMSO. Serially dilute the stock in MHB to obtain working solutions that will yield the desired final concentrations (e.g., 0.5xMIC, 1xMIC, 2xMIC, 4xMIC) in the test tubes or wells. The final concentration of DMSO in the test system should not exceed 1% (v/v) and must be included in the solvent control [22] [91].
Assay Setup:
- In sterile culture tubes or a 96-well plate, combine the plumbagin working solutions with the standardized bacterial inoculum. The final volume and bacterial concentration should be 5 x 10^5 CFU/mL.
- Include the following controls:
- Growth Control: Inoculum + MHB + equivalent DMSO (no plumbagin).
- Sterility Control: MHB only (no inoculum, no compound).
- Vortex the mixtures thoroughly.
Incubation and Sampling:
- Incubate the test vessels at 37°C with constant shaking.
- At predetermined time intervals (e.g., 0, 2, 4, 6, 8, and 24 hours), remove a 100 µL aliquot from each vessel [4].
Viable Bacterial Count (CFU Enumeration):
- Serially dilute each aliquot (e.g., 10-fold dilutions) in sterile PBS to achieve a countable range [4].
- Plate 100 µL of each dilution onto pre-dried Mueller Hinton Agar plates. Spread the aliquot evenly.
- Incubate the plates at 37°C for 18-24 hours.
- Count the colonies on plates yielding 30-300 colonies and calculate the viable bacterial density (CFU/mL) for each sample and time point.
Real-Time Monitoring (Optional):
- If using bioluminescent reporter strains, measure the luminescence signal from dedicated wells at each time point alongside sampling for CFU counts. The reduction in light emission correlates with a decrease in metabolically active bacteria [15].
Data Analysis and Interpretation
Data Processing: Calculate the mean log10 CFU/mL for each test condition and time point. Plot the mean log10 CFU/mL versus time to generate time-kill curves for each concentration of plumbagin and the growth control.
Interpretation of Kill Curves: The resulting kill curves are interpreted based on the difference in bacterial reduction between the treated samples and the growth control.
- Bactericidal Activity: A ≥3-log10 (99.9%) reduction in the viable count of the test organism compared to the starting inoculum at a specific time point [92].
- Bacteriostatic Activity: A reduction in the growth of the test organism of <3-log10 compared to the starting inoculum, where the growth control shows a significant increase [92].
- Synergism/Antagonism: When testing combinations, synergism is typically defined as a ≥2-log10 decrease in CFU/mL by the combination compared to the most active single agent [92].
The following diagram outlines the logical pathway for analyzing time-kill data and classifying the antimicrobial effect.
Application to Plumbagin: In a prior study, plumbagin (at 4 µg/mL) was found to be bacteriostatic and fungistatic against the tested microorganisms, as observed from its time-kill kinetics profile [22]. This indicates that plumbagin inhibits cellular replication but does not directly kill the organisms at that concentration and within the experimental timeframe.
The time-kill kinetics assay is an indispensable tool for the comprehensive in vitro evaluation of novel antimicrobials like plumbagin. This case study provides a detailed protocol demonstrating that plumbagin exhibits potent, multi-mechanistic antibacterial and anti-biofilm activity against a spectrum of MDR pathogens, with its effects being characterized as bacteriostatic under the tested conditions. The integration of this dynamic assay into antimicrobial development workflows provides critical insights that static MIC tests cannot, enabling researchers to accurately determine the rate and extent of microbial killing. This protocol offers a robust framework for assessing plumbagin and other natural products, facilitating the translation of promising lead compounds into viable therapeutic strategies to combat the global AMR crisis.
Conclusion
The time-kill kinetics assay is an indispensable tool that provides dynamic, concentration-dependent data on antimicrobial action, far surpassing the static snapshot offered by MIC determinations. Its ability to distinguish between bactericidal and bacteriostatic effects and to model pharmacodynamic relationships is critical for optimizing dosing strategies and combating antimicrobial resistance. Future directions will likely involve greater integration with advanced techniques like microfluidics for real-time observation of biofilms, increased automation for higher throughput, and sophisticated PK/PD modeling to better translate in vitro findings into clinical success. By adhering to standardized protocols, implementing robust validation, and understanding its place within the broader toolkit of antimicrobial susceptibility testing, researchers can reliably leverage this powerful method to advance the development of much-needed novel antimicrobial therapies.
References
- 1. 4.5. Time–Kill Assay [https://bio-protocol.org/exchange/minidetail?id=9358262&type=30]
- 2. Time-Kill Kinetics Assay [https://emerypharma.com/solutions/cell-microbiology-services/time-kill-kinetics-assay/]
- 3. Time-Kill Evaluations [https://www.nelsonlabs.com/testing/time-kill-evaluations/]
- 4. Protocol to quantify bacterial burden in time-kill assays ... [https://www.sciencedirect.com/science/article/pii/S2666166725000498]
- 5. Antimicrobial Activities and Time-Kill Kinetics of Extracts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5682094/]
- 6. Designing Novel Antimicrobial Agents from the Synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195976/]
- 7. antibacterials: clinical significance... Bactericidal versus bacteriostatic [https://pmc.ncbi.nlm.nih.gov/articles/PMC11695898/]
- 8. Difference Between Bactericidal and Bacteriostatic | Definition... [https://pediaa.com/difference-between-bactericidal-and-bacteriostatic/]
- 9. Fluoroquinolone antibiotics: in vitro antibacterial and time-kill... [https://bnrc.springeropen.com/articles/10.1186/s42269-022-00826-9]
- 10. In vitro antibacterial and time-kill evaluation of phosphanegold... [https://link.springer.com/article/10.1007/s13404-014-0144-y]
- 11. Beyond One-Size-Fits-All: Addressing Methodological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382792/]
- 12. Determination of minimum inhibitory and bactericidal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616320/]
- 13. Antibacterial mechanism of hyper-branched poly-L-lysine ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1676135/full]
- 14. Plasma effects on bacterial time-kill dynamics: Insights from ... [https://www.sciencedirect.com/science/article/pii/S0924857924003509]
- 15. Real-time evaluation of antibacterial efficacy using ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1569217/full]
- 16. Antibiotic susceptibility testing using minimum inhibitory ... [https://www.nature.com/articles/s44259-024-00051-6]
- 17. The Minimum Inhibitory Concentration of Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913839/]
- 18. Limitations of MIC as sole metric of pharmacodynamic ... [https://www.nature.com/articles/srep37907]
- 19. Enhancing antibiotic therapy through comprehensive ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1521091/full]
- 20. Review Optimisation of antimicrobial therapy using ... [https://www.sciencedirect.com/science/article/pii/S1198743X14640489]
- 21. Pharmacokinetic/pharmacodynamic models for time ... [https://www.sciencedirect.com/science/article/pii/S0924857922001285]
- 22. Resistance Modulation Action, Time-Kill Kinetics Assay, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899278/]
- 23. Methods for screening and evaluation of antimicrobial activity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11097785/]
- 24. Crude alkaloids from Phyllanthus fraternus, Webster [https://www.sciencedirect.com/science/article/pii/S2950199725001727]
- 25. Time-kill curve analysis and pharmacodynamic modelling for ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-016-0838-9]
- 26. Antimicrobial Activities and Time-Kill Kinetics of Extracts ... [https://pubmed.ncbi.nlm.nih.gov/29234399/]
- 27. Comparison of methods for the detection of in vitro synergy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7161189/]
- 28. Conventional methods and future trends in antimicrobial ... [https://www.sciencedirect.com/science/article/pii/S1319562X2300027X]
- 29. M26 | Methods for Determining Bactericidal Activity of ... [https://clsi.org/shop/standards/m26/]
- 30. E2315 Standard Guide for Assessment of Antimicrobial ... [https://www.astm.org/e2315-16.html]
- 31. ASTM E2315 - Liquid Suspension Time-Kill Test [https://microchemlab.com/test/astm-e2315-liquid-suspension-time-kill-test/]
- 32. Antimicrobial Susceptibility Testing - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539714/]
- 33. 4.6. Time-Kill Kinetics Assay [https://bio-protocol.org/exchange/minidetail?id=9049708&type=30]
- 34. 2.7. Evaluation of Different Media for Antimicrobial Production [https://bio-protocol.org/exchange/minidetail?id=8817352&type=30]
- 35. Neutralization of Germicides | Infection Control [https://www.cdc.gov/infection-control/hcp/disinfection-sterilization/germicide-neutralization.html]
- 36. Lag Phase Is a Distinct Growth Phase That Prepares Bacteria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3264077/]
- 37. Inoculum Standardisation: Ensuring Reliable Antimicrobial ... [https://altuner.me/Blog1.php]
- 38. General calibration of microbial growth in microplate readers [https://www.nature.com/articles/srep38828]
- 39. Broad-spectrum antimicrobial activity and in vivo efficacy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019989/]
- 40. Protocol to analyze antimicrobial susceptibility data [https://pmc.ncbi.nlm.nih.gov/articles/PMC9641264/]
- 41. Serial Dilution | The Method | Ossila [https://www.ossila.com/pages/serial-dilution]
- 42. 5.3: Lab Procedures- Viable Plate count - Biology LibreTexts [https://bio.libretexts.org/Courses/North_Carolina_State_University/MB352_General_Microbiology_Laboratory_2021_(Lee)/05:_Enumeration_of_Bacteria/5.03:_Lab_Procedures-_Viable_Plate_count]
- 43. In Vitro and In Silico Approaches for the Evaluation of ... [https://www.mdpi.com/2079-6382/11/1/79]
- 44. Video: Growth Curves, CFU and Optical Density ... [https://www.jove.com/v/10511/growth-curves-cfu-and-optical-density-measurements]
- 45. 6-6 Generating a growth curve [https://instr.bact.wisc.edu/book/displayarticle?theme=Printer&aid=114]
- 46. Microbiology Writing Guide: Presenting Data [https://wic.oregonstate.edu/microbiology-writing-guide-presenting-data]
- 47. Best Color Palettes for Scientific Figures and Data ... [https://www.simplifiedsciencepublishing.com/resources/best-color-palettes-for-scientific-figures-and-data-visualizations]
- 48. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 49. Evaluation of synergism in drug combinations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9127325/]
- 50. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 51. Time-kill assays. [https://bio-protocol.org/exchange/minidetail?id=17515310&type=30]
- 52. How to predict effective drug combinations [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152377/]
- 53. 2.5. Biofilm Time-Killing Assay [https://bio-protocol.org/exchange/minidetail?id=17654192&type=30]
- 54. Viability studies of bacterial strains exposed to nitrogen ... [https://www.nature.com/articles/s41598-025-94898-y]
- 55. Current and Past Strategies for Bacterial Culture in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4284306/]
- 56. Assessment of Gram- and Viability-Staining Methods for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01469/full]
- 57. Accurate modeling and simulation of the effect of bacterial ... [https://www.nature.com/articles/s41598-025-16150-x]
- 58. Inoculum size-insensitive susceptibility determination of ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267023010796]
- 59. Effect of inoculum size and antibiotics on bacterial traveling ... [https://www.nature.com/articles/s41378-021-00309-3]
- 60. Prevention of Drug Carryover Effects in Studies Assessing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2446915/]
- 61. Evaluation of two methods for overcoming the antibiotic ... [https://link.springer.com/article/10.1007/BF01967095]
- 62. Antibiotic carry over is a confounding factor for cell-based ... [https://www.nature.com/articles/s41598-025-14186-7]
- 63. Gonorrhoea 2025: Updated Guideline [https://www.bashh.org/resources/136/gonorrhoea_2025_updated_guideline/]
- 64. Antimicrobial Susceptibility Testing of Neisseria gonorrhoeae ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9241851/]
- 65. Neisseria gonorrhoeae antimicrobial susceptibility testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210901/]
- 66. 男性淋病患者奈瑟球菌57株药敏分析 [https://xuebao.bbmu.edu.cn/article/id/171bbd5f-5e2e-412d-bb47-888f397e2c1e]
- 67. 淋病奈瑟菌大观霉素耐药基因检测方法的建立与评价 [https://ykxb.scu.edu.cn/cn/article/id/94bdb5bb-3fe2-41f7-9466-3489ff586c50]
- 68. 用于生长或检测微生物的化学成分确定的培养基 [https://patents.google.com/patent/CN108603163A/zh]
- 69. Log Reduction Calculator [https://www.omnicalculator.com/biology/log-reduction]
- 70. Log & Percent Reductions in Microbiology & Antimicrobial ... [https://microchemlab.com/information/log-and-percent-reductions-microbiology-and-antimicrobial-testing/]
- 71. A Time-Kill Assay Study on the Synergistic Bactericidal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8699308/]
- 72. Reproducibility of antimicrobial test methods [https://www.nature.com/articles/s41598-018-30282-3]
- 73. An enhanced, statistically repeatable method for screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11950432/]
- 74. SPS-neutralization in tissue samples for efficacy testing of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6937930/]
- 75. Pitfalls in efficacy testing – how important is the validation of ... [https://ann-clinmicrob.biomedcentral.com/articles/10.1186/1476-0711-7-20]
- 76. ASTM E1054 Neutralization Evaluation Test [https://microchemlab.com/test/astm-e1054-neutralization-evaluation-test/]
- 77. Effect of host microenvironment and bacterial lifestyles on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12095824/]
- 78. Fast detection of synergy and antagonism in antifungal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528425/]
- 79. Direct Disk Diffusion Testing and Antimicrobial Stewardship ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291970/]
- 80. Comparison of disc diffusion and Sensititre® Broth ... [https://pubmed.ncbi.nlm.nih.gov/40339735/]
- 81. Major updates to FDA-recognized Clinical and Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077184/]
- 82. Part 3—Introduction to Pharmacodynamic Modeling Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC3917320/]
- 83. Application of Pharmacokinetic-Pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00997/full]
- 84. Characterization of sulopenem antimicrobial activity using ... [https://pubmed.ncbi.nlm.nih.gov/39907459/]
- 85. Characterization of sulopenem antimicrobial activity using in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878024/]
- 86. A Simple in vitro PK/PD Model System to Determine Time- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2783979/]
- 87. M100 | Performance Standards for Antimicrobial ... [https://clsi.org/shop/standards/m100/]
- 88. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria]
- 89. Clinical Breakpoint Tables [https://www.eucast.org/bacteria/clinical-breakpoints-and-interpretation/clinical-breakpoint-tables/]
- 90. The antibacterial and antioxidant activities of plumbagin- ... [https://www.sciencedirect.com/science/article/pii/S2950194625000615]
- 91. Antibacterial and anti-biofilm activity of plumbagin against ... [https://smj.org.sa/content/43/11/1224]
- 92. Enhancing antibiotic therapy through comprehensive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893874/]
- 93. Antibacterial activity and potential mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12148597/]
- 94. Antibiofilm activity of Plumbagin against Staphylococcus ... [https://www.nature.com/articles/s41598-025-92435-5]