Resistance-Proofing Therapies: Novel Strategies to Prevent Antibiotic Resistance Development During Treatment
This article provides a comprehensive analysis of innovative strategies designed to counteract the development of antibiotic resistance during therapeutic interventions.
Resistance-Proofing Therapies: Novel Strategies to Prevent Antibiotic Resistance Development During Treatment
Abstract
This article provides a comprehensive analysis of innovative strategies designed to counteract the development of antibiotic resistance during therapeutic interventions. Aimed at researchers, scientists, and drug development professionals, it synthesizes the latest scientific advances, from foundational resistance mechanisms to cutting-edge clinical applications. The review covers the molecular drivers of resistance, explores emerging 'resistance-resistant' therapeutic modalities such as evolutionary steering and combination therapies, and addresses the significant translational challenges in the current antibiotic development pipeline. Furthermore, it evaluates validation frameworks and comparative effectiveness of these novel approaches, offering a critical perspective on future directions for preserving antibiotic efficacy in an era of escalating antimicrobial resistance.
Understanding the Enemy: Foundational Mechanisms of Antibiotic Resistance Emergence
Antimicrobial resistance (AMR) is a critical global health threat, undermining the effectiveness of life-saving treatments and placing populations at heightened risk from common infections and routine medical interventions [1]. According to the World Health Organization's (WHO) 2025 Global Antibiotic Resistance Surveillance Report (GLASS), which draws on data from more than 23 million laboratory-confirmed infections across 110 countries, the situation is escalating rapidly [1]. The data reveals that one in six bacterial infections worldwide is now resistant to antibiotic treatments [2]. Between 2018 and 2023, antibiotic resistance increased in over 40% of the pathogen-antibiotic combinations monitored by the WHO, with an average annual rise of 5–15% [2]. This technical brief outlines the scope of the crisis and provides actionable guidance for researchers developing new therapeutic strategies.
Quantifying the Global Burden: Key Surveillance Data
The following tables summarize the core quantitative findings from the latest WHO surveillance, providing a snapshot of resistance levels for critical pathogen-antibiotic combinations.
Table 1: Global Resistance Prevalence for Key Pathogen-Antibiotic Combinations (2023)
| Pathogen | Antibiotic Class | Global Resistance Prevalence | Key Regional Variance |
|---|---|---|---|
| Escherichia coli | Third-generation cephalosporins | >40% [2] | Exceeds 70% in the African Region [2] |
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% [2] | Exceeds 70% in the African Region [2] |
| Klebsiella pneumoniae | Carbapenems | Increasing, narrowing treatment options [2] | Becoming more frequent globally [2] |
| Staphylococcus aureus | Methicillin (MRSA) | ~27% (widespread) [3] | |
| All bacterial pathogens | All treatments | 1 in 6 infections (global average) [2] | 1 in 3 in SE Asia & Eastern Mediterranean; 1 in 5 in African Region [2] [4] |
Table 2: Surveillance Capacity and Its Impact (2023) [2] [3] [4]
| Surveillance Metric | Status | Implication |
|---|---|---|
| Country participation in GLASS | 104 reporting countries (4x increase since 2016) [3] | Improved but incomplete global picture |
| Non-reporting countries | 48% of countries did not report data [2] | Critical data gaps persist, especially in underserved areas |
| Data quality | ~50% of reporting countries lack systems for reliable data [2] | Resistance may be over- or underestimated in some regions |
FAQs & Troubleshooting Guides for AMR Research
FAQ 1: Which bacterial pathogens currently pose the most urgent threat for therapeutic research?
Answer: Based on WHO 2025 data, drug-resistant Gram-negative bacteria represent the most dangerous and escalating threat [2]. The highest priority pathogens include:
- E. coli and K. pneumoniae: These are leading causes of drug-resistant bloodstream infections, with resistance to first-line treatments (third-generation cephalosporins) exceeding 40% and 55%, respectively, globally [2]. Resistance to last-resort carbapenems is also rising [2].
- Acinetobacter spp.: Noted for increasing resistance to essential antibiotics like carbapenems and fluoroquinolones, severely limiting treatment options [2].
- Staphylococcus aureus (MRSA): Methicillin resistance remains widespread at approximately 27%, sustaining its status as a major priority for research [3].
FAQ 2: My research on a novel compound is based on older resistance data. How can I ensure my experimental design reflects current real-world resistance patterns?
Troubleshooting Guide: A disconnect between historical data and current resistance trends is a common pitfall that can invalidate a compound's perceived efficacy.
- Problem: Novel compound shows high efficacy in vitro against lab-evolved resistant strains, but fails against contemporary clinical isolates.
- Solution:
- Source Recent Clinical Isolates: Actively collaborate with clinical microbiology laboratories in diverse geographical locations to obtain recent, clinically relevant isolates. The WHO report highlights significant regional variations (e.g., >70% resistance for E. coli in Africa vs. global average of >40%) [2]. Your test panel should reflect this diversity.
- Consult Real-Time Surveillance Data: Utilize the WHO GLASS dashboard and other national AMR surveillance databases to inform the selection of antibiotic comparators in your assays. Ensure you test against antibiotics known to have high failure rates in the region you are modeling.
- Validate with Genotypic Analysis: Use Whole Genome Sequencing (WGS) on your clinical isolates to confirm the presence of contemporary, clinically relevant resistance mechanisms (e.g., ESBL, carbapenemase genes) [5] [6]. This moves beyond phenotypic results alone and provides mechanistic insight.
FAQ 3: What are the best practices for incorporating rapid diagnostics into my therapeutic efficacy study protocols?
Troubleshooting Guide: Integrating rapid diagnostics can significantly reduce the Turnaround Time (TAT), a critical factor in combating AMR.
- Problem: Reliance on conventional culture-based AST (taking 48-72 hours) delays critical data in animal models or in vitro systems, slowing down the research pipeline.
- Solution: Implement a tiered diagnostic strategy.
- For Rapid Pathogen ID & Resistance Screening: Use MALDI-TOF Mass Spectrometry for rapid pathogen identification and FTIR Spectroscopy for preliminary typing and resistance detection [5]. These can provide data within hours.
- For Comprehensive Resistance Gene Profiling: Employ Next-Generation Sequencing (NGS). Techniques like Whole Genome Sequencing (WGS) or targeted Hybrid Capture panels can detect known and novel resistance genes from a sample without the need for prior cultivation, offering a complete resistome profile [5] [6].
- For Phenotypic Confirmation: Use automated broth microdilution systems (e.g., VITEK 2, Sensititre) or gradient diffusion tests (e.g., E-test) for gold-standard Minimum Inhibitory Concentration (MIC) determination, but with the prior knowledge gained from rapid methods to focus your testing [5].
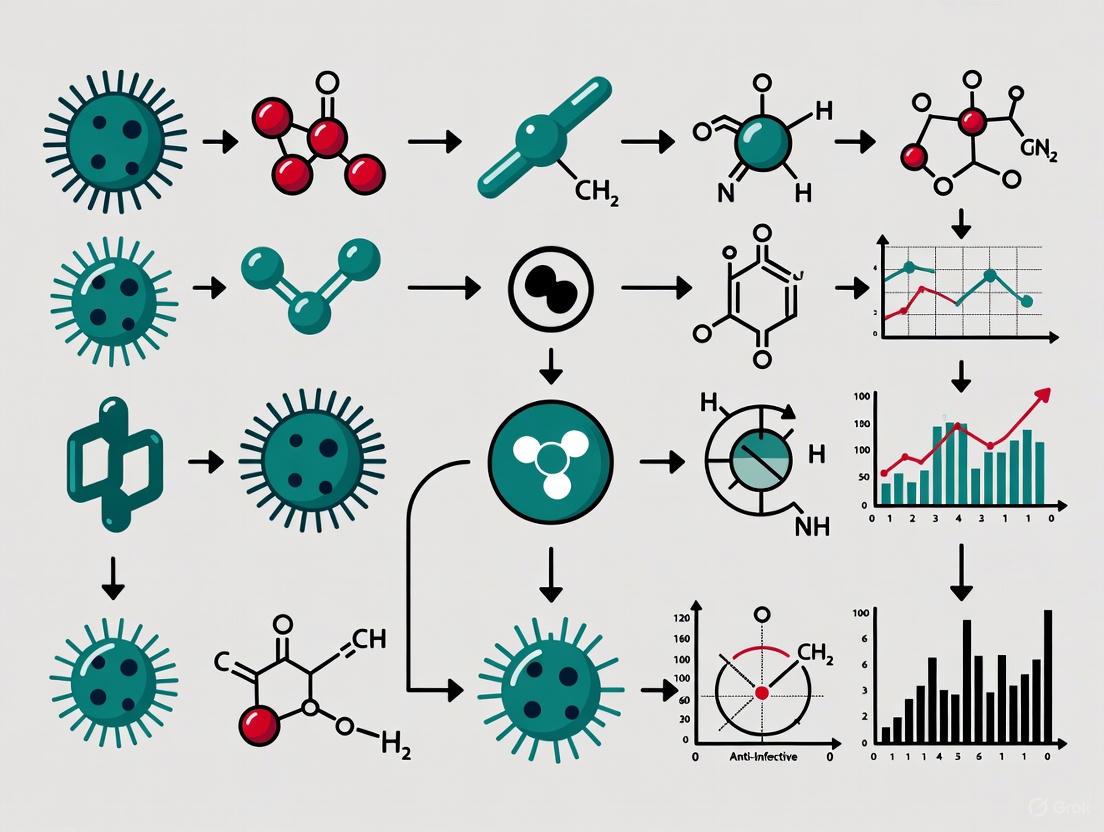
Diagram: Integrated Workflow for Rapid AMR Diagnostics in Research. This workflow combines rapid identification and genotypic methods with phenotypic confirmation to provide a comprehensive AMR profile faster than conventional methods alone [5].
The Scientist's Toolkit: Essential Reagents & Methods for AMR Research
Table 3: Key Research Reagent Solutions for AMR Studies
| Reagent / Tool | Function in AMR Research | Example Application |
|---|---|---|
| Sensititre Broth Microdilution Panels | Gold-standard for determining Minimum Inhibitory Concentration (MIC) [5]. | Quantifying resistance levels of clinical isolates against a novel compound panel. |
| Whole Genome Sequencing Kits (e.g., Illumina DNA Prep) | Comprehensive genomic analysis to identify known and novel resistance mechanisms [6]. | Characterizing the resistome of a bacterial pathogen and detecting horizontal gene transfer events. |
| Targeted AMR Panels (e.g., AmpliSeq for Illumina AMR Panel) | Focused sequencing of 478+ AMR genes for efficient screening [6]. | Rapidly screening a large collection of isolates for a wide array of known resistance determinants. |
| MALDI-TOF MS Reagents | Ultra-rapid microbial identification to species level [5]. | Confirming pathogen identity in animal infection models prior to efficacy testing. |
| Urinary/Respiratory Pathogen ID/AMR Panels | Multiplexed detection of pathogens and resistance markers from complex samples [6]. | Studying polymicrobial infections and their impact on resistance emergence in vivo. |
| DL-erythro-Dihydrosphingosine | DL-erythro-Dihydrosphingosine, CAS:6036-76-6, MF:C18H39NO2, MW:301.5 g/mol | Chemical Reagent |
| Byakangelicol | Byakangelicol, CAS:61046-59-1, MF:C17H16O6, MW:316.30 g/mol | Chemical Reagent |
Advanced Experimental Protocols
Protocol 1: Using Whole Genome Sequencing (WGS) for Resistome Analysis
Methodology: This protocol outlines the steps for using WGS to comprehensively identify antimicrobial resistance genes (ARGs) in bacterial isolates [5] [6].
- Genomic DNA Extraction: Use a validated kit (e.g., Illumina DNA Prep) to extract high-quality, high-molecular-weight genomic DNA from a pure bacterial culture. Quantify DNA using fluorometry.
- Library Preparation: Fragment the gDNA and attach sequencing adapters compatible with your NGS platform. For large-scale studies, incorporate unique dual indices (UDIs) to multiplex multiple samples in a single sequencing run.
- Sequencing: Perform sequencing on an Illumina platform (e.g., MiSeq, NextSeq) to achieve sufficient coverage (e.g., 50x-100x) for high-confidence variant calling and gene detection.
- Bioinformatic Analysis:
- Quality Control: Use tools like FastQC to assess raw read quality. Trim adapters and low-quality bases with Trimmomatic.
- Assembly: De novo assemble quality-filtered reads into contigs using assemblers like SPAdes.
- Resistance Gene Identification: Annotate the assembled genome by querying contigs against curated ARG databases (e.g., CARD, ResFinder) using BLAST or dedicated analysis pipelines (e.g., ARIBA).
Protocol 2: Implementing a High-Throughput qPCR Screen for ARGs
Methodology: This protocol describes a high-throughput method to screen a large number of bacterial isolates or environmental DNA extracts for a predefined set of ARGs [5].
- DNA Template Preparation: IsDNA from single bacterial colonies or directly from complex samples (e.g., stool, wastewater). Normalize all DNA concentrations to a standard value (e.g., 10 ng/μL).
- Primer/Probe Design: Select primers and TaqMan probes targeting a comprehensive panel of ARGs (e.g., blaKPC, mecA, vanA). Ensure probes are labeled with different fluorophores for multiplexing.
- qPCR Setup: Use a 384-well plate format. Each reaction should contain: 1X master mix, forward and reverse primers, TaqMan probe, template DNA, and nuclease-free water. Include no-template controls (NTCs) and positive controls (plasmids containing target ARG) on each plate.
- Amplification and Detection: Run the plate on a high-throughput real-time PCR instrument. Use the following cycling conditions: 95°C for 10 min (polymerase activation), followed by 40 cycles of 95°C for 15 sec (denaturation) and 60°C for 1 min (annealing/extension).
- Data Analysis: Determine cycle threshold (Ct) values. A sample is considered positive for an ARG if its Ct value is below a predetermined threshold (established using positive controls) and the amplification curve is sigmoidal.
Diagram: Implementation Research (IR) Continuum for AMR Interventions. Successfully moving an intervention from the lab to widespread use requires navigating a three-phase continuum, all while accounting for critical context domains that influence real-world adoption and impact [7].
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: My bacterial strains are showing resistance to multiple, structurally unrelated antibiotics. What is the most likely mechanism, and how can I confirm it? A1: This multi-drug resistance (MDR) pattern strongly suggests the overexpression of efflux pumps [8]. To confirm:
- Inhibitor Assays: Use a broad-spectrum efflux pump inhibitor (e.g., Phe-Arg β-naphthylamide, PAβN) in combination with your antibiotics. A significant decrease in the Minimum Inhibitory Concentration (MIC) of the antibiotics in the presence of the inhibitor confirms efflux pump activity [8].
- Genetic Analysis: Perform PCR or whole-genome sequencing to identify and quantify the expression of genes encoding known MDR pumps, such as those from the RND superfamily (e.g., AcrAB-TolC in E. coli or MexAB-OprM in P. aeruginosa) [8] [9].
Q2: My β-lactam antibiotics are failing against clinical isolates. How do I distinguish between enzymatic degradation and target site modification? A2: Both mechanisms can affect β-lactams, but they can be differentiated experimentally.
- For Enzymatic Degradation (e.g., by β-lactamases):
- Test: Use a β-lactamase inhibitor (e.g., clavulanic acid, sulbactam) in combination with the antibiotic. A restored antibiotic effect (synergy) indicates the presence of a susceptible β-lactamase (e.g., ESBLs) [9] [10].
- Molecular Detection: Perform specific PCR tests for prevalent resistance genes like blaNDM (metallo-β-lactamase) or blaKPC (serine carbapenemase) [9] [10].
- For Target Site Modification (e.g., PBP alteration):
- This is common in Gram-positives like MRSA (Methicillin-Resistant Staphylococcus aureus).
- Test: Detect the mecA gene, which codes for an alternative penicillin-binding protein (PBP2a) with low affinity for β-lactams [11].
Q3: My research involves combating efflux-mediated resistance. What are the latest innovative approaches beyond traditional inhibitors? A3: Research is moving beyond simple inhibition to more sophisticated strategies:
- "Resistance Hacking": A proof-of-concept study on Mycobacterium abscessus used a structurally modified antibiotic (florfenicol) that is activated by a bacterial resistance protein (Eis2). This creates a perpetual cascade where the bacterium's own resistance mechanism amplifies the drug's effect, effectively turning resistance against itself [12].
- CRISPR-Cas9 Gene Editing: This technology can be used to precisely target and disrupt genes encoding efflux pumps, potentially reversing the resistant phenotype. Phage-delivered CRISPR systems are being explored for this purpose [8] [10].
Q4: According to recent surveillance data, which drug-pathogen combinations currently pose the most severe threat? A4: The WHO's 2025 report highlights critical threats, largely driven by the mechanisms discussed here [2] [13]:
- Gram-negative bacteria, particularly E. coli and K. pneumoniae, are the most concerning.
- Over 40% of E. coli and 55% of K. pneumoniae isolates are resistant to third-generation cephalosporins (a first-line treatment), often due to ESBL production (enzymatic degradation) [2].
- Carbapenem resistance, once rare, is becoming more frequent in these pathogens, largely due to the spread of carbapenemase enzymes (e.g., NDM, KPC), severely limiting treatment options [2] [10].
Troubleshooting Common Experimental Issues
Problem: Inconsistent results in efflux pump inhibition assays.
- Potential Cause: Degradation or instability of the efflux pump inhibitor in the growth medium.
- Solution: Prepare fresh inhibitor stock solutions for each experiment. Verify the stability profile of your specific inhibitor and ensure it is compatible with your assay conditions (e.g., pH, temperature) [8].
Problem: Failure to detect a known resistance gene via PCR in a phenotypically resistant strain.
- Potential Cause: The resistance may be due to a previously unidentified mutation or a novel resistance gene.
- Solution: Move beyond targeted PCR to whole-genome sequencing. This allows for the discovery of new resistance mutations (e.g., in promoter regions that upregulate efflux pumps) or novel horizontally acquired genes [8] [9].
Problem: Investigating a new compound, but unable to determine its primary resistance mechanism.
- Solution: Implement a systematic workflow:
- Check for Enzymatic Degradation: Incubate the compound with bacterial cell lysates and use HPLC/MS to look for degradation products.
- Check for Efflux: Perform the accumulation/efflux assay with a fluorescent substrate (see protocol below) in the presence of your compound.
- Check for Target Modification: Select for resistant mutants in vitro, then sequence the putative target gene(s) to identify mutations [8] [11].
Experimental Protocols
Protocol 1: Detecting β-Lactamase Activity via Nitrocefin Hydrolysis Assay
Principle: Nitrocefin is a chromogenic cephalosporin that changes color from yellow to red upon hydrolysis by β-lactamase enzymes. This is a quick, qualitative test for β-lactamase production [9].
Materials:
- Nitrocefin solution (0.5 mg/mL in phosphate-buffered saline or DMSO)
- Test bacterial culture (fresh, late-logarithmic phase)
- Sterile loop or swab
- Microfuge tubes or a microtiter plate
- 37°C incubator
Method:
- Suspend several bacterial colonies in 100 µL of PBS to create a dense suspension.
- Add 50 µL of the nitrocefin solution to the bacterial suspension.
- Incubate the mixture at 37°C and observe for color change within 5-15 minutes.
- Interpretation: A rapid color change to red indicates a positive result for β-lactamase production.
Protocol 2: Evaluating Efflux Pump Activity Using an Ethidium Bromide Accumulation Assay
Principle: Ethidium bromide (EtBr) is a fluorescent substrate for many broad-specificity efflux pumps. Inhibiting these pumps leads to increased intracellular EtBr accumulation and higher fluorescence [8].
Materials:
- Bacterial culture in mid-log phase
- Ethidium Bromide (EtBr) stock solution (1 mg/mL)
- Efflux pump inhibitor (e.g., PAβN, 25-100 µg/mL)
- HEPES or PBS buffer (pH 7.0)
- Spectrofluorometer or fluorescence microplate reader
- 37°C water bath or incubator
Method:
- Harvest bacterial cells by centrifugation, wash twice, and resuspend in buffer to an OD~600~ of ~0.5.
- Divide the cell suspension into two aliquots:
- Test: Pre-incubate with an efflux pump inhibitor for 10 minutes.
- Control: Pre-incubated with buffer only.
- Add EtBr to both tubes to a final concentration of 1-2 µg/mL.
- Immediately transfer the mixtures to a cuvette or microplate and measure fluorescence at excitation/emission wavelengths of ~530/600 nm every minute for 30-60 minutes.
- Interpretation: A steeper increase in fluorescence in the test sample compared to the control indicates that the inhibitor successfully blocked efflux activity, leading to EtBr accumulation.
Data Presentation: Global Resistance Prevalence
The table below summarizes key quantitative data from the WHO's 2025 Global Antimicrobial Resistance Surveillance Report, illustrating the severe and widespread nature of resistance driven by these core molecular mechanisms [2] [13].
Table 1: Global Prevalence of Antibiotic Resistance in Key Bacterial Pathogens (WHO GLASS 2025 Report)
| Bacterial Pathogen | Antibiotic Class | Resistance Prevalence (%) | Primary Molecular Mechanism(s) | Key Geographic Concern |
|---|---|---|---|---|
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% globally (exceeds 70% in Africa) | Enzymatic degradation (ESBLs) | Worldwide, highest in SE Asia, E. Mediterranean, Africa [2] [13] |
| Escherichia coli | Third-generation cephalosporins | >40% globally | Enzymatic degradation (ESBLs) | Worldwide, high in SE Asia, E. Mediterranean, Africa [2] [13] |
| Acinetobacter spp. | Carbapenems | Increasing, specific rates vary | Enzymatic degradation (Carbapenemases), Efflux pumps | A major concern in healthcare settings worldwide [2] [10] |
| Various Gram-negative bacteria | Carbapenems | Rising | Enzymatic degradation (e.g., blaKPC, blaNDM, blaOXA-48) | Documented regional spread in Europe (e.g., Moldova, Ukraine) [10] |
Research Reagent Solutions
The table below lists key reagents and their applications for studying the core molecular mechanisms of antibiotic resistance.
Table 2: Essential Research Reagents for Investigating Antibiotic Resistance Mechanisms
| Research Reagent | Function / Target | Specific Application Example |
|---|---|---|
| Nitrocefin | Chromogenic β-lactamase substrate | Qualitative and kinetic assessment of β-lactamase enzyme activity [9] |
| Phe-Arg β-naphthylamide (PAβN) | Broad-spectrum efflux pump inhibitor | Used in combination assays to confirm efflux-mediated resistance and study pump kinetics [8] |
| Clavulanic Acid | β-lactamase inhibitor (primarily for ESBLs) | Used in combination disk tests or broth microdilution to confirm Extended-Spectrum Beta-Lactamase (ESBL) production [9] [10] |
| CRISPR-Cas9 System | Genome editing tool | Precise knockout of resistance genes (e.g., efflux pump genes, beta-lactamase genes) to study function and reverse resistance [8] [10] |
| Specific PCR Primers (e.g., for blaKPC, blaNDM, mecA) | Molecular detection of resistance genes | Rapid genotypic identification and surveillance of specific resistance mechanisms in bacterial isolates [9] [10] |
Mechanism and Workflow Visualization
Efflux Pump Resistance and Inhibition
Resistance Mechanism Identification Workflow
Antimicrobial resistance (AMR) is a escalating global health crisis, directly causing an estimated 1.27 million deaths annually and contributing to nearly 5 million more [14]. A core mechanism driving the evolution of resistance in bacteria is their innate capacity for rapid adaptation under pressure. This technical resource center focuses on two critical components of bacterial evolvability: stress-induced mutagenesis and the SOS response. These interconnected systems allow bacterial populations to increase their genetic diversity when faced with stressors like antibiotics, accelerating the development of resistance [15] [16]. Understanding and experimentally disrupting these pathways is essential for developing novel therapeutic strategies to curb the rise of resistant superbugs.
FAQs: Core Concepts for Researchers
Q1: What is the fundamental difference between the SOS response and stress-induced mutagenesis?
The SOS response is a specific, inducible DNA repair network activated by DNA damage. It is a defined regulon controlled by the LexA repressor and RecA inducer [17] [18]. In contrast, stress-induced mutagenesis is a broader phenomenon describing a transient increase in mutation rates under stress, which can be fueled by multiple mechanisms, including the SOS response [15]. The SOS response is a key driver of stress-induced mutagenesis, but other stress pathways, like the general stress response (RpoS) and the stringent response, also contribute [15] [19].
Q2: How does antibiotic treatment itself promote resistance via these mechanisms?
Many antibiotic classes directly or indirectly cause DNA damage. For example, ciprofloxacin (a fluoroquinolone) inhibits topoisomerases, leading to double-strand breaks [18]. This damage activates the SOS response. Subsequently, SOS-induced error-prone DNA polymerases (like Pol IV and Pol V) perform translesion synthesis, which is inherently mutagenic [17] [20]. This creates genetic diversity, including mutations that can confer antibiotic resistance, precisely when the bacterial population is under selection pressure from the drug [18] [19].
Q3: Why do we observe heterogeneous responses to DNA damage in clonal bacterial populations?
Recent single-cell studies using fluorescent SOS reporters (e.g., GFP under control of recA or umuDC promoters) have revealed that the SOS response oscillates in individual cells [18]. Instead of a simple on/off switch, cells exhibit one, two, or even three successive peaks of SOS gene expression after damage. This digital pulsating suggests that the SOS response is tuned to cope with a certain level of damage per pulse. The heterogeneity may arise from stochastic fluctuations in key limiting factors, such as RecA nucleoprotein filament dynamics or UmuD cleavage [18].
Q4: What is the connection between the SOS response, biofilms, and antimicrobial tolerance?
Biofilms are hotbeds for SOS induction. The dynamic biofilm environment generates endogenous DNA-damaging factors, such as reactive oxygen species and metabolic byproducts [19]. Furthermore, the SOS response plays a significant role in biofilm formation itself. Biofilms are highly recalcitrant to antimicrobials, sheltering persistent cells. The induction of the SOS response within this protected environment fuels bacterial adaptation and diversification, making biofilms a key reservoir for the emergence of resistance [19].
Troubleshooting Common Experimental Challenges
Table 1: Common Experimental Issues and Solutions in SOS and Mutagenesis Research
| Challenge | Potential Cause | Solution |
|---|---|---|
| Low mutation frequency in stress assays. | Insufficient stressor dose/duration; repair pathways overwhelming mutagenesis. | - Titrate stressor (e.g., antibiotic concentration) to find sub-lethal but inducing levels [16].- Use mutants deficient in high-fidelity repair (e.g., uvrB). |
| High background mutation rate in controls. | Pre-existing mutator alleles (e.g., in mutS, mutL) in your strain. |
Resuscitate strains from single colonies and verify genotype; use whole-genome sequencing to check for mutator phenotypes. |
| No SOS induction detected via reporter. | Non-cleavable LexA repressor; defective RecA; insufficient DNA damage. | - Use a positive control (e.g., low-dose UV irradiation, mitomycin C) [18].- Verify genotype of recA and lexA genes. |
| Inconsistent results in persister cell assays. | Cell population heterogeneity; variations in culture growth phase. | - Ensure cultures are grown to the exact same optical density and phase (e.g., mid-log vs. stationary) [19].- Use high-resolution, single-cell reporter systems to capture heterogeneity [18]. |
Quantitative Data on Mutagenesis and Resistance
Table 2: Key Stress-Induced Mutagenesis Systems and Their Genetic Dependencies
| System Name | Organism | Mutation Type | Selected Phenotype | Key Genetic Requirements | References |
|---|---|---|---|---|---|
| Adaptive Mutation (Lac+) | E. coli | Frameshifts | Growth on lactose | Pol IV, RecA, RecBCD, RpoS, Ppk | [15] |
| ROSE Mutagenesis | E. coli | Base substitutions | Rifampicin resistance | CyaA, RecA, LexA*, Pol I | [15] |
| Mutagenesis in Aging Colonies (MAC) | E. coli | Base substitutions | Rifampicin resistance | RpoS, Pol II, MMR* | [15] |
| SOS-Dependent Spontaneous Mutagenesis | E. coli | Base substitutions | Tryptophan prototrophy | RecA, Pol V | [15] |
| Stationary-Phase Mutagenesis | P. putida | Frameshifts, base substitutions | Growth on phenol | Pol IV, Pol V, RpoS | [15] |
Note: An asterisk () denotes loss or inactivation of the gene. MMR: Mismatch Repair.*
Standard Experimental Protocols
Protocol 1: Inducing and Quantifying the SOS Response
Principle: Measure SOS induction by quantifying the derepression of a reporter gene (e.g., sfiA::lacZ or recA::gfp) after controlled DNA damage [18].
Method:
- Culture and Stressor: Grow an E. coli strain containing the SOS reporter to mid-log phase. A common inducing stressor is UV irradiation at 254 nm.
- Induction: Harvest cells, wash, and resuspend in saline. Expose to a calibrated UV dose (e.g., 10-50 J/m²). Keep a non-irradiated control in the dark.
- Incubation and Measurement: Post-irradiation, dilute cells in fresh medium and incubate with shaking. For
lacZfusions, measure β-galactosidase activity at timed intervals (0, 30, 60, 90 mins) [18]. Forgfpfusions, monitor fluorescence via microscopy or flow cytometry to capture single-cell, oscillatory induction patterns [18]. - Controls: Include a
recAorlexAdeficient mutant as a negative control.
Protocol 2: Measuring Stress-Induced Mutagenesis Using the Lac+ System
Principle: Quantify the rate of reversion mutations that allow Lac- cells to utilize lactose as a sole carbon source during starvation [15].
Method:
- Starvation Setup: Plate a large number of Lac- E. coli cells (e.g., FC40 strain) onto minimal media plates with lactose as the only carbon source. Include a low concentration of a poor carbon source (e.g., 0.05% glycerol) to allow limited growth before starvation sets in.
- Incubation: Incubate plates for several days. Visible colonies are Lac+ revertants that arose during starvation.
- Quantification: Count the number of Lac+ revertants that appear over time. Mutation rates can be calculated using the Ma-Sandri-Sarkar maximum likelihood method or fluctuation analysis on parallel cultures.
- Validation: Confirm the genetic dependencies of the observed mutagenesis by repeating the assay with isogenic strains lacking key genes like
dinB(Pol IV) orrecA[15].
Signaling Pathway & Experimental Workflow Diagrams
Diagram Title: SOS Response Signaling Pathway
Diagram Title: Workflow for SOS and Mutagenesis Assays
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOS and Mutagenesis
| Reagent / Tool | Category | Key Function in Research | Example Use Case |
|---|---|---|---|
recA::gfp / lexA::gfp transcriptional fusions |
Reporter Strain | Visualizes SOS induction dynamics in real-time at single-cell resolution. | Detecting oscillatory SOS pulses after UV damage [18]. |
ΔrecA / ΔlexA mutant strains |
Genetic Control | Confirms SOS-dependence of an observed phenotype (e.g., mutagenesis). | Determining if antibiotic-induced mutagenesis requires a functional SOS response [18]. |
ΔdinB (Pol IV) / ΔumuDC (Pol V) mutants |
Genetic Tool | Dissects the specific role of error-prone TLS polymerases in mutagenesis. | Identifying the polymerase responsible for specific mutation signatures under stress [15] [17]. |
| UV Crosslinker (254 nm) | Laboratory Equipment | Provides a controlled, reproducible DNA-damaging stimulus to induce the SOS response. | Standardized induction of the SOS pathway for mechanistic studies [20]. |
| Error-Prone Polymerase Inhibitors | Pharmacological Agent | Experiments with novel therapeutics aimed at suppressing stress-induced mutagenesis. | Testing if inhibiting Pol IV/V reduces the emergence of antibiotic resistance [16]. |
| Cedryl Acetate | Cedryl Acetate, CAS:61789-42-2, MF:C17H28O2, MW:264.4 g/mol | Chemical Reagent | Bench Chemicals |
| Pantethine | Pantethine, CAS:644967-47-5, MF:C22H42N4O8S2, MW:554.7 g/mol | Chemical Reagent | Bench Chemicals |
Horizontal Gene Transfer (HGT) acts as a molecular "conveyor belt," enabling the rapid spread of antibiotic resistance genes among bacterial populations. Unlike vertical gene transfer (from parent to offspring), HGT allows for the movement of genetic information between organisms, a process that includes the spread of antibiotic resistance genes among bacteria, fueling pathogen evolution [21]. This continuous flow of genetic material is a primary driver of the antimicrobial resistance (AMR) crisis, making it a critical focus for therapeutic research.
Mechanisms of the HGT Conveyor Belt
The HGT conveyor belt operates through three well-understood genetic mechanisms, each with distinct functionalities. The table below summarizes these core processes.
Table 1: Core Mechanisms of Horizontal Gene Transfer
| Mechanism | Description | Key Components | Primary Role in AMR Spread |
|---|---|---|---|
| Transformation [21] [22] | Bacteria take up and integrate free environmental DNA from dead, degraded bacteria. | Competence-specific proteins, DNA binding proteins, RecA proteins | Allows for the acquisition of resistance genes from the environment, including from non-pathogenic bacteria. |
| Conjugation [21] [22] [23] | Direct cell-to-cell transfer of genetic material via a conjugative pilus. | Conjugative plasmids, conjugative transposons, mobilizable plasmids | The most common mechanism for inter-species transfer of resistance plasmids (R-plasmids). |
| Transduction [21] [22] | Bacteriophages (bacterial viruses) accidentally package and transfer bacterial DNA from one cell to another. | Bacteriophages (lytic and temperate) | Transfers resistance genes between bacteria of the same or closely related species. |
To elucidate the logical relationships between these mechanisms and their collective impact on antimicrobial resistance, the following diagram outlines the HGT pathway.
The Scientist's Toolkit: Key Research Reagents & Materials
Research into HGT mechanisms requires specific reagents and tools. The following table details essential materials for studying the conveyor belt of resistance genes.
Table 2: Essential Research Reagents for HGT Experiments
| Research Reagent / Material | Function in HGT Research |
|---|---|
| Competence-Inducing Media [22] | Stimulates natural competence in bacteria (e.g., Streptococcus pneumoniae, Neisseria gonorrhoeae) for transformation studies. |
| Selective Antibiotics [21] [22] | Used in growth media to select for and isolate transformants/transconjugants that have acquired a resistance marker. |
| Conjugative Plasmids (e.g., F-factor, R-plasmids) [22] [23] | Serve as mobile genetic elements to study the mechanism, efficiency, and regulation of conjugation. |
| Bacteriophage Lysates [22] [24] | Used in transduction experiments to infect donor and recipient strains for generalized or specialized transduction. |
| DNA Binding Dyes (e.g., Ethidium Bromide, DAPI) | Visualize DNA uptake during transformation or track the location of plasmids within cells. |
| Anti-SprB Antibody [25] | Used in tethered-cell analysis to study the mechanics of gliding motility and the Type IX Secretion System (T9SS) in certain Bacteroidetes. |
| PCR Reagents & Primers | Amplify and detect specific resistance genes before and after HGT events to confirm successful transfer. |
| 1-Tetradecanol | 1-Tetradecanol, CAS:67762-30-5, MF:C14H30O, MW:214.39 g/mol |
| Chrysosplenetin | Chrysosplenetin, CAS:69234-29-3, MF:C19H18O8, MW:374.3 g/mol |
Troubleshooting Common HGT Experimental Challenges
This section addresses specific issues researchers might encounter during experiments related to HGT and antibiotic resistance.
FAQ 1: Why is my conjugation experiment yielding no transconjugants?
Problem: Despite setting up a conjugation between a donor strain (with an R-plasmid) and a recipient strain, no antibiotic-resistant transconjugant colonies are growing on the selective plates.
Solution:
- Verify Strain Viability: Ensure both donor and recipient strains are viable and in the correct growth phase (typically mid- to late-log phase) for optimal pilus formation and mating efficiency [22].
- Optimize Mating Conditions: Increase the mating time (e.g., from 1 hour to 4-18 hours) and use a non-selective, nutrient-rich solid or liquid medium for the conjugation step. Gently resuspend cells without vortexing to avoid shearing the conjugation pili.
- Check Antibiotic Selectivity: Confirm that the selective antibiotics in your plate effectively kill the donor and recipient controls. The recipient must be resistant to an antibiotic that inhibits the donor, and the selective plate must contain an antibiotic for which the R-plasmid confers resistance to the recipient.
- Confirm Plasmid Mobility: Ensure the plasmid in the donor strain is indeed a conjugative plasmid, not a non-mobilizable one [23].
FAQ 2: How can I confirm that resistance was acquired via natural transformation and not spontaneous mutation?
Problem: After co-incubating a sensitive strain with DNA from a resistant strain, resistant colonies appear, but you need to rule out spontaneous mutation as the cause.
Solution:
- Include Critical Controls:
- DNA Control: Plate the naked DNA on the selective medium to confirm it cannot grow.
- Recipient Control: Plate the recipient strain without added DNA on the selective medium to check for pre-existing resistant mutants.
- DNase Control: Treat the DNA with DNase before adding it to the recipient. This should completely abolish the appearance of resistant colonies, confirming that the resistance is DNA-dependent [22].
- Molecular Confirmation: Use PCR to amplify the specific resistance gene from the transformed colonies. Sanger sequencing of the amplicon can confirm it is identical to the gene from the donor DNA, not a mutated version.
FAQ 3: What methods can I use to quantify the rate of HGT in my experimental system?
Problem: You need to move beyond a qualitative "yes/no" for HGT and measure the frequency of transfer events.
Solution:
- Standard Calculation: For conjugation and transformation, the transfer frequency is typically calculated as the number of transconjugants or transformants divided by the number of recipient cells (or total viable count) at the end of the mating/transformation period [23].
- Experimental Workflow: The process involves performing the HGT experiment, plating appropriate dilutions on selective media to count transconjugants/transformants, and plating on non-selective media to determine the total recipient cell count.
- Use of Fluorescent Reporters: Engineer donor and recipient strains with fluorescent proteins (e.g., GFP, RFP). The transfer of a plasmid carrying a fluorescence gene can be quantified over time using flow cytometry, providing a high-throughput method to measure HGT dynamics.
The following workflow diagram illustrates the key steps for a standard HGT quantification experiment.
Advanced Techniques & Novel Interventional Strategies
Beyond basic HGT study, current research focuses on disrupting this conveyor belt to combat AMR. The table below summarizes several advanced strategies.
Table 3: Novel Strategies to Combat Horizontal Gene Transfer of Resistance
| Strategy | Mechanism of Action | Experimental Protocol Highlights |
|---|---|---|
| Phage Therapy [24] | Use of bacteriophages to specifically infect and lyse antibiotic-resistant bacteria, reducing the reservoir of resistance genes. | "Training" phages via experimental evolution for 30 days to expand host range against multi-drug resistant pathogens like Klebsiella pneumoniae [24]. |
| CRISPR-Cas Gene Editing [26] | Delivery of CRISPR-Cas systems to specifically target and cleave resistance genes in bacterial populations, "re-sensitizing" them to antibiotics. | Design of sgRNAs to target specific resistance gene sequences (e.g., blaNDM-1) and delivery via plasmids or phages to bacterial communities. |
| Antibiotic Potentiators [27] | Use of non-antibiotic compounds that impair bacterial resistance mechanisms (e.g., efflux pump inhibition, enzyme blockade), restoring efficacy of existing antibiotics. | Checkerboard assays to measure synergy (FIC Index) between a potentiator (e.g., a natural terpene) and an antibiotic against a resistant strain. |
| Precision Prescribing [28] | Computerized alerts using EHR data to guide clinicians toward narrow-spectrum antibiotics for low-risk patients, reducing selective pressure. | Implementation of clinical decision support systems that use hospital-specific data to assess individual patient risk for resistant infections. |
Global Resistance Data & The Imperative for Action
Understanding the scale of the AMR problem underscores the importance of HGT research. Recent data from the World Health Organization (WHO) quantifies the threat.
Table 4: WHO Global Prevalence of Antibiotic Resistance (2025 Report) [2]
| Pathogen | Key Resistance Finding | Clinical Impact |
|---|---|---|
| Klebsiella pneumoniae | Over 55% are resistant to third-generation cephalosporins (first-choice treatment) globally. | Leads to untreatable pneumonia and sepsis; a prime carrier of transmissible resistance plasmids. |
| Escherichia coli | Over 40% are resistant to third-generation cephalosporins globally. Resistance to fluoroquinolones and carbapenems is rising. | A major cause of drug-resistant urinary tract and bloodstream infections. |
| Acinetobacter spp. | Increasing carbapenem resistance, narrowing treatment options to last-resort antibiotics. | Notorious for causing hard-to-treat hospital-acquired infections. |
| Aggregate | 1 in 6 laboratory-confirmed bacterial infections in people worldwide were resistant to antibiotic treatments in 2023. | Illustrates the pervasive and systemic nature of the AMR crisis, driven largely by HGT. |
Technical Support Center: FAQs & Troubleshooting Guides
My bacterial isolates are showing unexpectedly high resistance rates in my assay. What could be the cause?
Answer: Unexplained spikes in resistance can often be traced to contamination or undisclosed antibiotic exposure in your research model. First, verify the purity of your bacterial stocks through re-streaking and single-colony isolation. For in vivo studies, investigate potential environmental sources. In one comprehensive study, high resistance rates of 27.95% were noted, particularly against pathogens like Staphylococcus aureus and Klebsiella pneumoniae [29]. Implement stricter environmental controls and audit animal feed and water for antimicrobial agents, as uncontrolled antibiotic use in livestock can contribute to resistance that enters the research setting [30].
What is the best way to model environmental antibiotic residue exposure in my research?
Answer: To accurately model environmental exposure, simulate real-world conditions. Prepare sub-inhibitory concentrations of antibiotics based on concentrations reported in agricultural runoff or wastewater effluent. In laboratory settings, studies show that exposing bacteria to concentrations as low as 1/10 the MIC in chemostats over serial passages can effectively simulate the selection pressure found in contaminated environments. This approach aligns with the One Health principle that environmental contamination is a key driver of resistance [31] [32].
How can I improve the translational value of my antibiotic therapy study from animals to humans?
Answer: Adopt a pharmacokinetic/pharmacodynamic (PK/PD) modeling approach that integrates data across species. Ensure your animal model accounts for the interconnectedness of human and animal health, a core tenet of the One Health approach [31] [30]. Furthermore, incorporate host immune response metrics and gut microbiome analysis into your endpoints. Surveillance data coordinated by institutions like the University of Nairobi shows that common bacteria in animals and humans, such as E. coli and S. aureus, exhibit similar resistance patterns (e.g., 60-70% for E. coli), highlighting the shared resistance landscape [30].
My research on a new drug combination is being confounded by pre-existing resistances in my clinical isolates. How can I screen for this more effectively?
Answer: Implement a pre-screening protocol using genomic and phenotypic characterization. Begin with rapid molecular techniques like PCR to detect common resistance genes (e.g., NDM-1, ESBLs). Follow this with phenotypic confirmation using minimum inhibitory concentration (MIC) testing. National policies, such as India's AMR containment policy, recommend establishing robust AMR surveillance systems that combine these methods to generate reliable data for informing empirical therapy [33]. This two-tiered approach helps clarify whether observed treatment failures are due to pre-existing resistance or other experimental factors.
Quantitative Data on Resistance and Therapy
Table 1: Documented Resistance Rates of Common Pathogens (Surveillance Data)
| Pathogen | Common Resistance Profile | Documented Resistance Rate | Key Context |
|---|---|---|---|
| Klebsiella pneumoniae | Resistance to commonly used treatments in newborns [30] | 70-80% [30] | A major concern for neonatal infections [30] |
| Escherichia coli | Resistance to frequently used antibiotics [30] | 60-70% [30] | Prevalent in community and healthcare settings [30] |
| Staphylococcus aureus | Resistance to available antibiotics (e.g., MRSA) [29] [30] | ~50% [30] | A serious problem in hospital settings; MRSA prevalence in India was 41% [33] |
| Overall Resistance (across various classes and pathogens) | Highest rates noted in penicillins and cephalosporins [29] | 27.95% (average in a study of 1,050 observations) [29] | Resistance varies widely across antibiotic classes [29] |
Table 2: Key Findings from a Comparative Study on Antibiotic Therapy
| Study Parameter | Findings from 1,050 Patient Records [29] |
|---|---|
| Most Prescribed Broad-Spectrum Antibiotic | Ceftriaxone (27.9%) |
| Patients with History of Previous Infection | 67.5% |
| Patients Receiving High-Dose Drugs | 36.5% |
| Average Treatment Effectiveness | 77.43% |
| Average Treatment Safety Rate | 84.77% |
| Average Diagnosis Delay | 4 days |
| Statistical Correlation | Significant associations were found between prior antibiotic use and the development of resistance across different antibiotic classes. |
Experimental Protocols for One Health Research
Protocol 1: Integrated One Health AMR Surveillance
Objective: To establish a methodology for tracking antimicrobial resistance patterns across human, animal, and environmental samples in a defined region.
Methodology:
- Sample Collection: Concurrently collect clinical isolates from human healthcare settings, livestock (e.g., poultry, cattle), and environmental sources (e.g., soil, water bodies near farms).
- Laboratory Analysis:
- Isolate and identify major bacterial pathogens (E. coli, K. pneumoniae, S. aureus) using standard microbiological and biochemical methods.
- Perform Antimicrobial Susceptibility Testing (AST) using Kirby-Bauer disk diffusion or broth microdilution to determine MICs for a core panel of antibiotics (e.g., penicillins, cephalosporins, carbapenems, fluoroquinolones).
- Preserve isolates for genetic analysis.
- Data Integration and Analysis:
- Create a centralized database to log resistance profiles from all three sectors.
- Use spatial mapping to visualize hotspots of specific resistance patterns.
- Perform genetic sequencing (e.g., whole-genome sequencing) on a subset of isolates with similar resistance profiles from different sectors to investigate the genetic relatedness and potential transmission of resistance genes.
This protocol operationalizes the collaborative, multisectoral approach recommended by the One Health strategy [31] [30] [32].
Protocol 2: Evaluating the Impact of Sub-therapeutic Antibiotic Exposure
Objective: To determine how sub-inhibitory concentrations of antibiotics in the environment, mimicking agricultural runoff, select for resistant bacterial populations.
Methodology:
- Strain Preparation: Select environmental or commensal bacterial strains (e.g., E. coli).
- Exposure Model:
- Set up continuous-culture bioreactors (chemostats) with low-nutrient media to simulate natural aquatic environments.
- Continuously introduce a sub-therapeutic dose (e.g., 1/10 to 1/100 of the MIC) of a target antibiotic (e.g., tetracycline, used in agriculture).
- Maintain control chemostats without antibiotic pressure.
- Monitoring and Endpoint Analysis:
- Sample populations at regular intervals over several weeks.
- Quantify the MIC of the population over time to track resistance development.
- Use selective plating to enumerate the proportion of resistant bacteria.
- At endpoint, sequence the genomes of evolved populations to identify acquired resistance mutations or genes.
This methodology directly addresses the environmental dimension of One Health, where contamination exerts selective pressure for AMR [31] [32].
Visualizing the One Health Approach to AMR
Diagram 1: One Health AMR Drivers
Diagram 2: AMR Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AMR Research
| Item | Function / Application in AMR Research |
|---|---|
| Mueller-Hinton Agar/Broth | The standardized medium recommended by CLSI and EUCAST for performing Antimicrobial Susceptibility Testing (AST) to ensure reproducible and comparable MIC results. |
| Antimicrobial Powder Standards | High-purity antibiotic powders used to prepare custom solutions for creating concentration gradients in MIC assays and for use in disk diffusion tests. |
| CRISPR-Cas9 Gene Editing Systems | Molecular tools used for precise knockout or modification of specific bacterial resistance genes to study their function and contribution to the resistant phenotype. |
| Whole Genome Sequencing Kits | Reagents for preparing bacterial DNA libraries to sequence entire genomes, allowing for the identification of known and novel resistance mutations and genes. |
| Biofilm Reactors & Stains | Systems (e.g., flow cells, Calgary biofilm devices) and dyes (e.g., crystal violet, LIVE/DEAD stains) to grow and quantify biofilms, which are key to understanding chronic, resistant infections. |
| Animal Infection Models | Specific pathogen-free (SPF) rodent models (e.g., mouse, rat) used to study the in vivo efficacy of new therapeutic agents and the pathogenesis of resistant infections. |
| Data Integration Software | Bioinformatics platforms (e.g., CLC Genomics Workbench, Geneious) and statistical software (e.g., R, SPSS) essential for analyzing complex datasets from integrated One Health surveillance [33] [29]. |
| 2-Hydroxyquinoline | 2-Hydroxyquinoline, CAS:104534-80-7, MF:C9H7NO, MW:145.16 g/mol |
| 1-Tetradecanol | 1-Tetradecanol (Myristyl Alcohol) Supplier for Research |
Resistance-Resistant Therapeutics: From Conceptual Frameworks to Clinical Applications
The escalating crisis of antimicrobial resistance (AMR) represents one of the most pressing challenges in modern medicine. According to recent WHO data, one in six laboratory-confirmed bacterial infections globally were resistant to antibiotic treatments in 2023, with resistance rising in over 40% of monitored pathogen-antibiotic combinations [2]. This alarming trend has stimulated research into innovative approaches that move beyond directly killing bacteria to instead inhibit their evolutionary capacity to develop resistance. A prime target in this endeavor is the bacterial SOS response—an inducible DNA repair network that promotes genetic diversity and adaptability under stress [34] [17]. When antibiotics trigger DNA damage, either directly or indirectly through metabolic byproducts like reactive oxygen species (ROS), bacteria activate this sophisticated emergency response system [35] [19]. The SOS pathway not only facilitates repair of damaged DNA but also regulates error-prone DNA polymerases that introduce mutations, thereby accelerating the evolution of resistance mechanisms [34] [17]. This technical resource provides troubleshooting guides, experimental protocols, and strategic insights for researchers developing interventions that target bacterial evolvability through disruption of mutagenic stress responses.
Core Mechanism: The SOS Response Pathway
The SOS response is a highly regulated bacterial stress adaptation mechanism. Understanding its components and activation dynamics is fundamental to developing effective inhibitors.
Molecular Regulation
The SOS response is primarily regulated by two key proteins: LexA (repressor) and RecA (inducer) [17] [19]. During normal growth, LexA forms a dimer that binds to operator sequences (SOS boxes) in the promoter regions of more than 50 genes, maintaining the SOS regulon in a repressed state [17]. When DNA damage occurs, single-stranded DNA (ssDNA) gaps accumulate, providing a platform for RecA nucleation. RecA binds to ssDNA, forming nucleoprotein filaments (RecA*) that activate LexA's self-cleavage capacity [17]. This cleavage inactivates LexA, reducing its affinity for DNA and leading to derepression of SOS genes [17] [19].
The following diagram illustrates the core SOS response pathway and potential inhibition points:
Temporal Regulation of SOS Genes
SOS gene expression follows a precise temporal sequence that reflects their functional priorities [17]. Early-phase genes include those involved in error-free repair mechanisms, such as nucleotide excision repair (uvrA, uvrB) and homologous recombination (recA, recN). Mid-phase genes include those encoding DNA polymerase II (polB) and polymerase IV (dinB), along with the cell division inhibitor sulA. The late-phase response features the error-prone DNA polymerase V (umuC, umuD), which facilitates translesion synthesis at the cost of increased mutagenesis [17]. This temporal regulation ensures that error-prone mechanisms are deployed only when damage is extensive and persistent.
Research Reagent Solutions: Key Molecular Targets and Inhibitors
The table below summarizes prime targets for inhibiting SOS-mediated evolvability and characterized inhibitor compounds:
Table 1: Key Research Reagents for SOS Pathway Inhibition
| Target Protein | Known Inhibitors | Mechanism of Action | Research Application |
|---|---|---|---|
| RecA [34] | Suramin, suramin-like agents [34] | Disassembles RecA-ssDNA filaments [34] | Block SOS induction; reduce recombination |
| 2-amino-4,6-diarylpyridine [34] | ATPase inhibition [34] | Prevent RecA activation | |
| Zinc acetate [34] | Inhibits LexA cleavage [34] | Indirect SOS suppression | |
| Peptide 4E1 (RecX-like) [34] | Filament disassembly [34] | Targeted RecA disruption | |
| LexA [34] | 5-amino-1-(carbamoylmethyl)-1H-1,2,3-triazole-4-carboxamide [34] | Inhibits self-cleavage [34] | Block SOS derepression |
| Boron-containing compounds [34] | Interacts with catalytic Ser-119 [34] | LexA cleavage inhibition | |
| Pol V (UmuD2C) [34] | RecA D112R/N113R mutant [34] | Disrupts RecA-PolV interaction [34] | Study mutasome formation |
| SSB Protein [34] | Small molecules [34] | Disrupt SSB protein interfaces [34] | Impair replication/repair |
| RecBCD [34] | Sulfanyltriazolobenzimidazole NSAC1003 [34] | Binds RecB ATP-binding site [34] | Inhibit DNA end resection |
Experimental Protocols: Key Methodologies
Protocol: Measuring SOS Inhibition in Pseudomonas aeruginosa
Background: This protocol adapts methodology from studies investigating SOS function in P. aeruginosa during ciprofloxacin exposure [36]. It enables quantification of how SOS inhibition affects competitive fitness and resistance development.
Materials:
- Wild-type P. aeruginosa PAO1 (WT)
- Isogenic SOS-uninducible LexA S125A mutant (prevents autocleavage) [36]
- M9KB broth medium
- Ciprofloxacin (stock solution: 1 mg/mL in water/DMSO)
- Gentamicin (for selection)
- Luminescence plate reader (if using reporter strain)
Method:
- Strain Preparation: Inoculate separate colonies of WT and LexA mutant into M9KB broth. Grow overnight at 37°C with shaking [36].
- Competition Setup: Combine exponential-phase cultures at varying initial ratios (e.g., 70:30, 50:50, 30:70 WT-to-mutant). Use gentamicin resistance (present in the LexA mutant) as a selectable marker [36].
- Antibiotic Exposure: Dilute mixed cultures 100-fold into fresh M9KB containing sublethal ciprofloxacin (e.g., 48 µg/L, which induces ~50% mortality and maximal SOS response) [36]. Include antibiotic-free controls.
- Growth and Plating: Incubate cultures for 24 hours at 37°C. Dilute and plate on M9KB agar with and without gentamicin to enumerate each strain [36].
- Fitness Calculation: Calculate wild-type fitness as the ratio of Malthusian parameters for WT versus mutant: m = [ln(Nf/N0)]WT / [ln(Nf/N0)]LexA where N0 and Nf are initial and final densities [36].
- SOS Expression Monitoring: For temporal analysis, use a luminescent SOS reporter (e.g., plexA::lux) to measure induction kinetics under treatment [36].
Troubleshooting: If fitness differences are minimal, verify ciprofloxacin concentration and ensure proper marker selection. The LexA S125A mutation provides a clean genetic SOS blockade without pleiotropic effects [36].
Protocol: Assessing SOS-Independent Resistance Evolution in E. coli
Background: Recent findings demonstrate that RecA deletion can unexpectedly accelerate β-lactam resistance through SOS-independent mechanisms involving ROS accumulation and impaired DNA repair [37]. This protocol quantifies this alternative evolutionary path.
Materials:
- E. coli MG1655 (WT) and isogenic ΔrecA mutant (JW2669-1 from CGSC) [37]
- LB broth and agar
- Ampicillin (stock: 50 mg/mL in water)
- ROS detection dye (e.g., H2DCFDA)
- Rifampicin plates for mutation frequency
- 96-well deep culture plates
Method:
- Strain Validation: Confirm RecA deletion phenotype via UV sensitivity compared to WT [37].
- Single Exposure Resistance: Grow overnight cultures of WT and ΔrecA. Dilute 1:100 into fresh LB containing ampicillin (50 µg/mL, ~10× MIC). Incubate 8 hours at 37°C with shaking [37].
- MIC Determination: Measure post-exposure MIC using broth microdilution. Compare to pre-exposure MIC [37].
- Mutation Rate Analysis: Distribute 96 independent cultures of WT and ΔrecA in 96-well plates. Grow with/without ampicillin for 8 hours. Plate on rifampicin to select resistant mutants. Use maximum likelihood estimation to calculate mutation rates [37].
- ROS Detection: Load parallel cultures with H2DCFDA (10 µM). Measure fluorescence intensity during ampicillin exposure to quantify ROS accumulation [37].
Expected Results: ΔrecA strains typically show ≥20-fold ampicillin MIC increase after single exposure, correlated with elevated ROS and increased mutation supply [37].
Troubleshooting Guide: Common Experimental Challenges
Table 2: Troubleshooting SOS Inhibition Experiments
| Problem | Potential Cause | Solution |
|---|---|---|
| No fitness cost with SOS inhibition | Suboptimal antibiotic concentration; insufficient DNA damage induction | Titrate antibiotic to achieve ~50% mortality; use known SOS inducers (e.g., ciprofloxacin) [36] |
| High variability in competition assays | Inconsistent initial ratios; cross-contamination | Use multiple independent colonies; verify mixing ratios by plating; maintain sterile technique [36] |
| Unexpected resistance in SOS-deficient strains | SOS-independent pathways; ROS-mediated mutagenesis | Include ROS scavengers (e.g., thiourea); complement with functional RecA; test multiple replicates [37] |
| Poor inhibitor potency in vivo | Limited cellular uptake; efflux pump activity | Use chemical analogs with improved permeability; employ efflux pump deficient strains [34] |
| Toxicity of SOS inhibitors | Off-target effects on host/human cells | Determine selective index (bacterial vs. mammalian cell toxicity); use targeted delivery approaches [34] |
Advanced Concepts: Resistance Beyond SOS
While the SOS response represents a prime target, recent research reveals additional evolutionary pathways that can complicate therapeutic strategies:
SOS-Independent Resistance Mechanisms: Studies demonstrate that E. coli lacking RecA can rapidly develop stable, multi-drug resistance after a single β-lactam exposure through SOS-independent pathways [37]. This occurs through a two-step process: (1) RecA deficiency impairs DNA repair and represses antioxidant defenses, leading to ROS accumulation and increased mutational supply; and (2) antibiotic pressure selectively enriches resistant variants from this hypermutable population [37]. This highlights the importance of combinatorial approaches that target both specific resistance pathways and general mutational mechanisms.
Alternative Evolutionary Strategies: Research in P. aeruginosa indicates that the SOS response primarily provides short-term fitness advantages under antibiotic stress rather than accelerating long-term adaptation [36]. During 200-generation selection experiments with ciprofloxacin, SOS-proficient and deficient strains showed similar resistance evolution trajectories, with SOS expression actually decreasing during adaptation [36]. This suggests bacteria may downreginate mutagenic pathways once initial resistance is acquired.
Exploiting Resistance Mechanisms: Innovative approaches are exploring how to "hack" bacterial resistance mechanisms for therapeutic benefit. In Mycobacterium abscessus, researchers engineered a florfenicol prodrug that is activated by Eis2, a WhiB7-regulated resistance protein [12]. This creates a perpetual cascade where antibiotic activation induces more resistance proteins, which in turn generate more active drug, effectively turning the resistance mechanism against the bacterium [12].
Frequently Asked Questions (FAQs)
Q1: Why target bacterial evolvability rather than simply developing new antibiotics?
A: Inhibiting evolvability addresses the fundamental problem of resistance development rather than playing "catch-up" with resistant strains. By suppressing mutagenic stress responses like the SOS pathway, we can potentially extend the therapeutic lifespan of existing antibiotics and reduce the emergence of multi-drug resistant strains [34] [33].
Q2: What is the relationship between SOS response and bacterial persistence?
A: The SOS response contributes to bacterial persistence through multiple mechanisms. It can induce toxin-antitoxin systems (like TisB/IstR in E. coli) that promote dormancy and regulate biofilm formation, which provides physical protection and creates heterogeneous microenvironments that stimulate SOS induction [19]. Persisters exhibit transient tolerance to antibiotics and can serve as a reservoir for resistance development.
Q3: Are there species-specific differences in SOS regulation that might affect inhibitor design?
A: Yes, significant variations exist. While E. coli and P. aeruginosa have canonical LexA/RecA systems, Mycobacterium tuberculosis utilizes a different mutagenic polymerase (DnaE2) under LexA control [34]. Some species like Streptococcus pneumoniae lack LexA entirely and use alternative regulatory cascades [34]. Effective inhibitor design must consider these species-specific differences.
Q4: What are the main challenges in developing SOS inhibitors for clinical use?
A: Key challenges include: (1) achieving sufficient specificity to avoid host toxicity, particularly given RecA's structural similarities to eukaryotic RAD51; (2) ensuring bacterial permeability and retention; (3) preventing rapid resistance to the inhibitors themselves; and (4) navigating complex regulatory pathways that may vary between bacterial species [34] [17].
Q5: How do sublethal antibiotic concentrations influence resistance development?
A: Sublethal antibiotic exposure can induce stress responses (including SOS) that increase mutation rates and promote horizontal gene transfer [36] [19]. This emphasizes the importance of maintaining adequate dosing regimens and complete treatment courses to minimize the emergence of resistance.
Conceptual Framework: FAQs on Core Principles
FAQ 1: What are evolutionary steering and collateral sensitivity in the context of antibiotic resistance?
Answer: Evolutionary steering is a therapeutic strategy that aims to control the evolution of a pathogen population by deliberately applying selective pressure with one drug. The goal is to direct the evolutionary trajectory of the population in a predictable way, steering it toward a state of vulnerability [38]. Collateral sensitivity (CS) is a specific, exploitable evolutionary trade-off where resistance to one antibiotic concurrently causes increased sensitivity to a second, unrelated antibiotic [39] [40]. When combined, these approaches can trap pathogens in an "evolutionary double bind," making it difficult for multidrug resistance to emerge [38] [39].
FAQ 2: What are the common genetic and physiological mechanisms behind collateral sensitivity?
Answer: Collateral sensitivity arises from pleiotropic mutations, where a single genetic change impacts multiple traits. The table below summarizes key mechanisms identified in bacterial pathogens.
Table 1: Common Mechanisms of Collateral Sensitivity
| Mechanism | Description | Example Consequence |
|---|---|---|
| Altered Membrane Permeability | Mutations that decrease uptake of one drug may increase uptake of another [40]. | Increased sensitivity to a second antibiotic due to enhanced import. |
| Efflux Pump Regulation | Overexpression of a efflux pump to remove one drug can be energetically costly or alter transport of other compounds [40]. | Hypersensitivity to drugs not expelled by the overexpressed pump. |
| Modification of Drug Targets | A mutation that alters the target of drug A may destabilize its interaction with drug B [40]. | Resistance to drug A but sensitivity to drug B. |
| Resistance Enzyme Hijacking | A resistance enzyme that normally inactivates one drug can activate a prodrug, turning the resistance mechanism against the cell [12]. | perpetual amplification of the antibiotic's effect within the cell. |
FAQ 3: Why is the order of drug administration (drug sequence) so critical?
Answer: Collateral sensitivity networks are often directional. Resistance to Drug A may cause sensitivity to Drug B, but resistance to Drug B might not cause sensitivity to Drug A—it could even cause cross-resistance [39]. The effectiveness of evolutionary steering depends on using the correct sequence that creates a sustained vulnerability. Using the wrong sequence can select for multidrug-resistant clones and lead to therapeutic failure [38] [39].
Experimental Protocols & Workflows
This section provides a detailed methodology for setting up and analyzing evolution experiments to identify and validate collateral sensitivity pairs.
Core Experimental Protocol: Laboratory Evolution and Sensitivity Profiling
Objective: To evolve resistance to a primary antibiotic and systematically identify collateral sensitivity to a panel of secondary antibiotics.
Materials:
- Bacterial Strain: e.g., Pseudomonas aeruginosa or other relevant pathogen [39].
- Antibiotics: Stock solutions of the primary selective antibiotic and a panel of secondary antibiotics for profiling.
- Growth Media: Appropriate liquid and solid media (e.g., Mueller-Hinton Broth).
- Equipment: Microplate readers, automated liquid handlers, incubators.
Procedure:
- Passage and Selection:
- Propagate multiple replicate populations of the bacterial strain in the presence of a sub-inhibitory concentration of the primary antibiotic (Drug A).
- Over successive generations, linearly increase the concentration of Drug A to select for highly resistant populations [39].
- Include control populations passaged without antibiotics.
Resistance Validation:
- After resistance stabilizes, isolate single clones from the evolved populations.
- Determine the Minimum Inhibitory Concentration (MIC) of Drug A for both the evolved clones and the ancestral strain to quantify the level of resistance.
Collateral Sensitivity Screening:
- Perform dose-response assays of the evolved clones and the ancestor against a panel of secondary antibiotics (Drugs B, C, D, etc.).
- Calculate the fold-change in MIC for each secondary drug. Collateral sensitivity is defined as a significant decrease (e.g., ≥ 4-fold) in the MIC of the secondary drug in the evolved clone compared to the ancestor [39].
Genomic Analysis:
- Sequence the whole genomes of clones showing strong collateral sensitivity.
- Identify mutations (SNPs, indels, amplifications) responsible for the primary resistance.
- Use genetic techniques (e.g., gene knockouts, complementation) to validate the role of identified mutations in causing both resistance and collateral sensitivity [39].
Figure 1: Experimental workflow for identifying collateral sensitivity.
Protocol for Testing Evolutionary Stability
Objective: To determine if a identified collateral sensitivity relationship is stable or if pathogens can easily escape the trade-off.
Procedure:
- Evolutionary Challenge:
- Take a clone that is resistant to Drug A and collaterally sensitive to Drug B.
- Subject this clone to a second round of evolution, this time under pressure from Drug B. Start at sub-inhibitory concentrations and escalate over time [39].
- Outcome Analysis:
- Monitor populations for extinction, which indicates a stable trade-off that cannot be overcome.
- If populations survive, isolate clones and re-measure MICs for both Drug A and Drug B.
- A favorable outcome is re-sensitization, where resistance to Drug B causes renewed sensitivity to Drug A, maintaining the trade-off [39].
Table 2: Quantitative Data from a Model CS Study with P. aeruginosa
| Evolutionary Step | Strain / Population | MIC Piperacillin/Tazobactam (µg/mL) | MIC Streptomycin (µg/mL) | Interpretation |
|---|---|---|---|---|
| Baseline | Ancestral Strain | X | Y | Wild-type susceptibility |
| After 1st Evolution | PIT-Resistant Clone | >X (e.g., 32-fold increase) | Collateral Sensitivity to Streptomycin | |
| After 2nd Evolution | STR-Adapted Clone | ~X (returns near baseline) | >Y | Re-sensitization to Piperacillin |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Evolutionary Steering Experiments
| Item | Function/Description | Key Consideration |
|---|---|---|
| High-Complexity Barcoded Libraries | Uniquely tags individual bacterial cells to track clonal dynamics in large, heterogeneous populations [38]. | Essential for distinguishing pre-existing resistant clones from those acquiring de novo mutations. |
| Large-Capacity Culture Vessels (e.g., HYPERflask) | Supports growth of very large populations (10^8 – 10^9 cells) without re-plating bottlenecks [38]. | Maintains intra-tumour heterogeneity and allows selection of pre-existing resistant subclones. |
| Morbidostat / Evolver | Automated continuous culture devices that dynamically adjust antibiotic concentration to maintain a constant selective pressure [39]. | Ideal for conducting controlled, long-term evolution experiments. |
| Phenotypic Microarray Plates | Pre-configured 96-well plates with different antibiotics for high-throughput collateral sensitivity screening. | Dramatically speeds up the process of profiling evolved clones against a broad drug panel. |
| Clinical Isolate Panels | Collections of clinically relevant, multidrug-resistant bacterial pathogens (e.g., CRKP, MRSA). | Ensures research findings are translationally relevant and reflect real-world resistance threats. |
| Pteryxin | Pteryxin, CAS:737005-97-9, MF:C21H22O7, MW:386.4 g/mol | Chemical Reagent |
| Imazalil | Imazalil, CAS:73790-28-0, MF:C14H14Cl2N2O, MW:297.2 g/mol | Chemical Reagent |
Troubleshooting Common Experimental Challenges
Problem 1: Inconsistent or non-repeatable collateral sensitivity effects between replicate populations.
- Potential Cause: Stochastic evolution, where different mutations conferring resistance to the first drug arise in different replicates, and these distinct mutations have different collateral effects [39] [40].
- Solution:
- Increase the number of biological replicates.
- Use larger population sizes to ensure a more consistent representation of pre-existing genetic variation [38].
- Perform whole-genome sequencing on clones from all replicates to correlate specific resistance mutations with their resulting collateral sensitivity profiles.
Problem 2: Evolved populations develop multidrug resistance instead of showing collateral sensitivity.
- Potential Cause: The selected antibiotic pair does not have a strong trade-off, or the population size is large enough to allow for very rare double-resistant mutants to emerge [39].
- Solution:
- Re-screen for new antibiotic pairs that show stronger, ideally reciprocal, collateral sensitivity.
- Use higher concentrations of the second drug to more effectively eliminate singly-resistant cells.
- Consider applying both drugs in combination after initial steering to prevent outgrowth of doubly-resistant mutants [40].
Problem 3: Failure to contain resistance in an in vivo model despite success in vitro.
- Potential Cause: The complex host environment (immune system, spatial heterogeneity, pharmacokinetics) alters selective pressures and evolutionary dynamics.
- Solution:
- Optimize dosing schedules in animal models to match the timing of selective windows identified in vitro.
- Monitor bacterial population dynamics directly from the infection site over time, if possible.
- Account for pathogen physiology in vivo, which may differ from laboratory conditions.
Figure 2: Logical pathways showing optimal and suboptimal evolutionary steering.
What are antibiotic adjuvants and why are they a critical tool in combating antimicrobial resistance (AMR)?
Antibiotic adjuvants are non-antibiotic compounds that enhance the effectiveness of antibiotics when administered together. They represent a promising strategy to combat multi-drug resistant (MDR) pathogens by rescuing the efficacy of existing antibiotics rather than developing new ones from scratch. The primary value of adjuvants lies in their ability to overcome specific bacterial resistance mechanisms, thereby restoring the activity of antibiotics against resistant strains. This approach is particularly vital given the declining pipeline of new antibiotics and the rapid global spread of resistance [41] [42].
How is "synergy" defined and measured in antibiotic combination therapies?
In the context of antibiotic combinations, "synergy" occurs when the combined effect of two or more agents is greater than the sum of their individual effects. Several mathematical models and associated metrics are used to quantify this phenomenon:
- Fractional Inhibitory Concentration Index (FICI): Based on the Loewe additivity model, where doses are assumed to be additive. An FICI of ≤0.5 is generally considered synergistic [43].
- Bliss Independence Model: Assumes drugs act independently and probabilistically. Synergy is declared when the observed combined effect exceeds the expected independent effect [43].
- Highest Single Agent (HSA) Model: The effect of the combination should be equal to the maximum of the effects of each drug used individually; any effect above this maximum indicates synergy [43].
- Minimax Effective Concentration Index (MECI): A newer metric designed for efficient identification of synergistic combinations, especially in high-dimensional screens involving many drugs [43].
Frequently Asked Questions (FAQs) for Researchers
A. Screening and Identification
What are the primary experimental designs for screening synergistic combinations?
The table below summarizes common screening approaches:
| Method Name | Key Principle | Best Use Case | Sample Requirement |
|---|---|---|---|
| Full Factorial (Checkerboard) | Tests all possible concentration combinations of drugs [43]. | Gold standard for 2-drug combinations. | Grows exponentially with drug count (e.g., 10^d for d drugs) [43]. |
| Normalized Diagonal Sampling (NDS) | Samples along diagonals in concentration space where ratios are fixed [43]. | High-throughput screening of multi-drug (≥3) combinations. | Scales linearly with drug count (e.g., m ⋅ 2^d samples) [43]. |
| Library Screening (Repurposing) | Tests approved drugs or known bioactives as potential adjuvants [44]. | Identifying non-obvious adjuvants from existing compound libraries. | Varies by library size. |
What computational tools can predict synergistic interactions?
Computational models can significantly reduce the experimental burden:
- Parametric Models (Dose, Pairs): Assume no higher-order interactions beyond pairs of drugs [43].
- Mechanistic Models: Utilize knowledge of underlying drug targets or gene expression data [43].
- MAGENTA Model: Leverages phenotypic information about the cell's response to antibiotics [43].
- Data-Driven Predictive Models: Trained on pair-wise data to predict higher-order combination effects [43].
B. Mechanisms and Reagents
What are the major classes of antibiotic adjuvants and their mechanisms?
Adjuvants are broadly classified based on their target and mechanism of action [42]:
| Adjuvant Class | Mechanism of Action | Representative Examples | Target Antibiotic/Pathway |
|---|---|---|---|
| Class I.A: Inhibitors of Active Resistance | Block specific resistance enzymes [42]. | β-lactamase inhibitors (e.g., clavulanic acid) [44] [42] | β-lactam antibiotics |
| Class I.B: Inhibitors of Passive Resistance | Overcome physiologic barriers like membrane permeability or efflux pumps [42]. | Efflux pump inhibitors [41] | Various (e.g., tetracyclines) |
| Class I.B (Extended) | Disrupt protective bacterial communities. | Biofilm disruptors [41] | Antibiotics used against chronic infections |
| Class II: Immunomodulators | Enhance the host's immune response to infection [42]. | Immunomodulatory peptides (e.g., LL-37) [42] | Used in combination with standard antibiotics |
Can you provide a specific example of a non-antibiotic adjuvant discovery?
Yes. A screen of a compound library identified the antiplatelet drug ticlopidine as a potent adjuvant. While it had no inherent antibiotic activity, it strongly synergized with the cephalosporin cefuroxime against Methicillin-resistant Staphylococcus aureus (MRSA). Its molecular target was identified as TarO, an enzyme in the early stage of wall teichoic acid biosynthesis in the S. aureus cell wall. Inhibiting TarO sensitizes MRSA to β-lactam antibiotics [44].
C. Troubleshooting Common Experimental Issues
We are not identifying synergistic combinations in our high-throughput screens. What could be wrong?
- Problem: The experimental design or synergy metric might not be appropriate for the number of drugs being tested.
- Solution: For screens involving more than three antibiotics, consider moving from a full factorial design (which becomes infeasible) to a Normalized Diagonal Sampling (NDS) design. This method provably identifies the Minimax Effective Concentration Index (MECI) with exponentially fewer samples [43].
- Example: Screening 8 drugs at 10 concentrations each would require 10^8 samples exhaustively but only about 2,560 samples with NDS [43].
Our identified synergistic pair shows efficacy in growth inhibition assays but not in bacterial killing (clearance) assays. Why?
- Problem: Growth inhibition (e.g., MIC, optical density) does not always correlate with bacterial cell death (cidal activity). A combination may be synergistic in inhibiting growth but not in killing, particularly against tolerant or persistent sub-populations [45].
- Solution: Supplement standard growth inhibition assays (like checkerboard) with time-kill curve experiments. This measures the reduction in viable bacterial count (CFU/mL) over time and is a more clinically relevant metric for evaluating clearance efficacy [45].
The synergistic effect we observed in a reference strain is not conserved in clinical isolates. How can we improve translational potential?
- Problem: Collateral sensitivity and synergy networks can be highly dependent on the genetic background. A mutation that confers resistance to drug A may cause sensitivity to drug B in one strain, but not in another [45].
- Solution:
- Validate Robustness: Screen for synergies that are robust across a diverse panel of clinical isolates, not just a single lab strain [45].
- Exploit Conserved Mechanisms: Focus on adjuvants that target highly conserved and horizontally spread resistance mechanisms, such as mobile β-lactamases. For instance, expression of certain β-lactamases creates robust collateral sensitivity to colistin and azithromycin in diverse E. coli strains [45].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and their applications in adjuvant and synergy research.
| Reagent / Material | Primary Function in Research | Example Application |
|---|---|---|
| β-lactamase Enzymes | Target for Class I.A adjuvants; used in biochemical inhibition assays [42]. | Evaluating the potency of novel β-lactamase inhibitors (e.g., against NDM-1) [44]. |
| Engineered Efflux Pump Strains | Tool for identifying and characterizing Class I.B efflux pump inhibitors [41] [42]. | Screening compound libraries for agents that increase intracellular accumulation of fluorescent substrates or antibiotics. |
| Biofilm Culturing Equipment (e.g., flow cells, peg lids) | Enables the study of adjuvants that disrupt bacterial biofilms, a major cause of chronic infections [41]. | Testing the ability of compounds to enhance antibiotic penetration and efficacy against biofilm-encased bacteria. |
| Standardized Bacterial Panels (e.g., ESKAPE pathogens) | Provides a clinically relevant set of strains for validating the spectrum of activity of new synergistic combinations [45]. | Ensuring a candidate adjuvant-antibiotic pair is effective against a range of multi-drug resistant pathogens. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing (e.g., broth microdilution, checkerboard) [45]. | Ensures reproducible and comparable results for MIC and FICI determinations. |
| Metaflumizone | Metaflumizone, CAS:852403-68-0, MF:C24H16F6N4O2, MW:506.4 g/mol | Chemical Reagent |
| Methyl salicylate | Methyl Salicylate Research Grade|RUO | Research-grade Methyl Salicylate for scientific study. Used in pain relief, plant science, and chemical research. For Research Use Only. Not for human consumption. |
Workflow and Mechanism Visualization
A. Experimental Workflow for Identifying Synergistic Combinations
The following diagram outlines a logical workflow for a synergy screening project, integrating both computational and experimental steps.
B. Mechanisms of Action for Major Adjuvant Classes
This diagram illustrates the logical relationships between different adjuvant classes, their mechanisms, and their effects on bacteria and antibiotics.
FAQs: Core Principles of Bacteriophage-Antibiotic Synergy (PAS)
Q1: What is the fundamental principle behind Phage-Antibiotic Synergy (PAS)? PAS describes a phenomenon where bacteriophages and antibiotics work together to produce a combined antibacterial effect that is greater than the sum of their individual effects. This synergy can manifest through several mechanisms. Antibiotics can induce physiological or morphological changes in bacteria, such as cell filamentation, that enhance phage replication and efficacy. Conversely, phages can compromise bacterial cell envelope integrity, thereby increasing the uptake of antibiotics or disrupting bacterial efflux pumps, re-sensitizing resistant bacteria to the antibiotic's action [46] [47].
Q2: Why is PAS considered a promising strategy to combat antibiotic resistance? PAS addresses the global crisis of antimicrobial resistance (AMR), which was associated with an estimated 4.95 million deaths in 2019 [48]. This approach offers a "one-two punch" that can more effectively eradicate multidrug-resistant (MDR) pathogens, including critical ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.) [48]. By using phages and antibiotics in concert, PAS can reduce the likelihood of bacteria developing resistance to either agent, prolonging the usefulness of existing antibiotics and providing new therapeutic options for otherwise untreatable infections [49] [46].
Q3: What are the primary molecular and cellular mechanisms that drive PAS? Research has identified several key mechanisms of PAS:
- Antibiotic-Induced Morphological Changes: Sub-inhibitory concentrations of certain antibiotics (e.g., β-lactams) can cause bacterial cells to filament, increasing their physical size and the number of phage replication cycles, thereby boosting phage production and lysis [46].
- Restoration of Antibiotic Sensitivity: Some phages use bacterial structures involved in antibiotic resistance, such as efflux pumps, as their receptor for infection. Infection by these phages can select for or force bacteria to downregulate these resistance mechanisms, making them vulnerable to antibiotics again [48].
- Biofilm Disruption: Phages excel at degrading the extracellular matrix of bacterial biofilms, which are inherently resistant to antibiotics. By disrupting biofilms, phages allow antibiotics to penetrate and kill the underlying bacteria [48] [47].
Q4: How can I design a phage-antibiotic cocktail with broad-spectrum activity? A systematic approach involves grouping phages into Complementarity Groups (CGs) based on the bacterial receptors they target. Phages within the same CG use the same receptor, so resistance to one often confers cross-resistance to others. An effective cocktail should combine phages from different CGs to target non-redundant receptors, thereby minimizing the chance for bacteria to develop complete resistance. This strategy, combined with specific antibiotic pairings, has been used to create cocktails effective against over 96% of clinical isolates of P. aeruginosa and S. aureus in experimental models [50].
Troubleshooting Common Experimental Challenges
Table 1: Troubleshooting PAS Experiments
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| No observed synergy | Antagonistic interaction between the specific phage and antibiotic [46]. | Systematically screen different classes of antibiotics paired with your phage [47]. |
| Incorrect antibiotic concentration (e.g., bactericidal vs. sub-inhibitory) [46]. | Perform checkerboard assays with a range of antibiotic and phage concentrations (MOI) [47]. | |
| Rapid emergence of phage-resistant bacteria | Cocktail is too narrow, targeting a single receptor [50]. | Develop a cocktail using phages from different Complementarity Groups (CGs) that use non-redundant receptors [50]. |
| Phage population is too low to overwhelm the bacteria (insufficient MOI). | Optimize the Multiplicity of Infection (MOI) through kinetic killing assays [51]. | |
| Inconsistent results in biofilm assays | Inefficient phage penetration into the biofilm matrix. | Select phages with documented biofilm-degrading enzymes (e.g., depolymerases) [48]. |
| Inadequate contact time between phage and biofilm before antibiotic addition. | Pre-treat the biofilm with phages for 2-4 hours before introducing the antibiotic [47]. | |
| Difficulty in interpreting synergy | Lack of quantitative metrics for synergy. | Calculate metrics like the Suppression Index (growth inhibition) and Resistance Index (growth upon re-challenge) to quantify effects [50]. Use standardized models like the Bliss independence model to evaluate interactions [46]. |
Standardized Experimental Protocols
Protocol 1: Initial PAS Screening Using Checkerboard Assay
This protocol is used for the initial identification of synergistic phage-antibiotic pairs.
Materials:
- Fresh log-phase culture of the target bacterial strain.
- Purified, high-titer lytic phage stock.
- Antibiotic stock solution.
- 96-well cell culture plates.
- Liquid growth medium (e.g., Mueller-Hinton Broth).
Method:
- Prepare Antibiotic Dilutions: Serially dilute the antibiotic in growth medium along the rows of the 96-well plate, typically covering a range from below the MIC to above the MIC.
- Prepare Phage Dilutions: Serially dilute the phage stock along the columns of the same plate, covering a range of MOIs.
- Inoculate Bacteria: Add a standardized inoculum of bacteria (~10^5 CFU/well) to each well.
- Incubate and Measure: Incubate the plate with shaking at the appropriate temperature (e.g., 37°C) for 16-20 hours. Measure the optical density (OD600) at regular intervals using a plate reader.
- Analyze Data: Determine the combination effects. Synergy is concluded if the observed inhibitory effect of the combination is significantly greater than the expected additive effect of the two agents alone [46] [47].
Protocol 2: Quantifying PAS with Kinetic Growth Curves
This protocol provides a dynamic view of the interaction between phages and antibiotics over time.
Materials:
- Spectrophotometer with temperature-controlled shaking for culture tubes or a plate reader for 96-well plates.
- The same materials as Protocol 1.
Method:
- Set Up Cultures: In a culture tube or well, combine bacteria, phage (at a defined MOI, e.g., 1 or 10), and a sub-inhibitory concentration of antibiotic.
- Monitor Growth: Continuously measure the OD600 for a prolonged period (e.g., 24-30 hours) to create a kinetic growth curve.
- Calculate Indices:
- Suppression Index: The percentage of bacterial growth inhibition caused by the phage within a set time (e.g., first 30 hours) [50].
- Resistance Index: The percentage of bacterial growth observed upon re-exposing a previously phage-treated culture to the same phage, quantifying the level of resistance that has emerged [50].
- Interpret Results: A synergistic combination will show a deep and prolonged suppression of growth compared to either agent alone.
Research Reagent Solutions
Table 2: Essential Reagents for PAS Research
| Reagent / Material | Function in PAS Research | Key Considerations |
|---|---|---|
| Lytic Bacteriophages | The viral agent that specifically infects and lyses the target bacterial host. | Must be thoroughly characterized (genome sequenced, absence of virulence/antibiotic resistance genes). Obligately lytic phages are preferred for safety [49] [52]. |
| Sub-inhibitory Antibiotics | Used to induce bacterial physiological changes that enhance phage replication and activity. | Concentration is critical; must be determined empirically for each bacterial strain [46]. |
| Phage DNA Isolation Kit (e.g., Norgen Biotek Cat. 46800) | To purify high-quality phage genomic DNA for sequencing and characterization. | High-quality DNA is essential for genome sequencing, ensuring the phage lacks lysogeny genes and is safe for therapeutic use [52]. |
| 96-well Microtiter Plates | The platform for high-throughput checkerboard assays and kinetic growth measurements. | Allows for systematic testing of multiple phage-antibiotic concentration combinations in replicate [47]. |
| Spectrophotometer / Plate Reader | To measure bacterial density (OD600) for quantifying growth, inhibition, and synergy. | Instruments with continuous shaking and temperature control are necessary for reliable kinetic growth curves [50]. |
| Transmission Electron Microscope (TEM) | For morphological characterization and classification of isolated bacteriophages. | Confirms phage family (e.g., Myoviridae, Siphoviridae, Podoviridae) based on tail and capsid structure [47]. |
Visualizing the Complementarity Group Strategy
The following diagram illustrates the core strategy of using Complementarity Groups (CGs) to design robust phage cocktails that prevent bacterial resistance. Phages are grouped based on the bacterial receptor they target (e.g., Type IV Pilus, LPS, Flagella). Using phages from different CGs simultaneously blocks multiple evolutionary escape routes for the bacterium.
Frequently Asked Questions (FAQs)
FAQ 1: What makes nanoparticles and antimicrobial peptides (AMPs) less likely to induce resistance compared to conventional antibiotics?
Both nanoparticles and AMPs employ multiple mechanisms of action against bacteria, making it difficult for bacteria to develop resistance through single genetic mutations.
- Nanoparticles: They often utilize a multi-mechanistic approach, including physical membrane disruption, generation of reactive oxygen species (ROS), and enzyme inhibition. This simultaneous attack means bacteria would require multiple, simultaneous gene mutations to survive, which is a statistically improbable event [53] [54].
- Antimicrobial Peptides: Most AMPs are cationic and amphiphilic. They primarily target the negatively charged bacterial membrane through electrostatic interactions, leading to membrane permeabilization and cell death. This mechanism targets the fundamental structure of the membrane, which is not easily altered by simple genetic changes [55] [56] [57].
FAQ 2: My nanoparticle formulation shows good efficacy in vitro but poor efficacy in an animal infection model. What could be the reason?
This is a common challenge in translating nanotherapeutics from the lab to the clinic. The issue often lies with the overall biodistribution of the nanoparticles. After systemic administration, a significant portion of the nanoparticle dose can be sequestered by the mononuclear phagocyte system (MPS), primarily in the liver and spleen, reducing the amount that reaches the infection site [58]. To troubleshoot:
- Consider incorporating "stealth" technology, such as PEGylation, to reduce opsonization and uptake by macrophages [58].
- Re-evaluate the size of your nanoparticles. Very small particles (<10 nm) are rapidly cleared by the kidneys, while larger particles are more likely to be taken up by the MPS [58].
- Explore active targeting strategies by functionalizing the nanoparticle surface with ligands that bind to receptors overexpressed at the infection site [58].
FAQ 3: The antimicrobial peptide I am testing is highly cytotoxic to mammalian cells. How can I improve its selectivity?
Cytotoxicity, particularly hemolytic activity, is a major limitation for many natural AMPs. This is often linked to the peptide's hydrophobicity [55] [57]. You can address this through rational design:
- Modify Hydrophobicity: Systematically alter the sequence to reduce overall hydrophobicity or adjust the hydrophobic moment. This can decrease non-specific interactions with neutral mammalian cell membranes while retaining activity against bacterial membranes [55] [56].
- Check Net Charge: Ensure the peptide has a sufficient positive charge (from lysine and arginine residues) for strong interaction with negative bacterial membranes [55].
- Utilize Delivery Systems: Encapsulating the AMP in nanoparticles or hydrogels can shield it from interaction with host cells until it reaches the infection site, thereby reducing systemic toxicity and improving pharmacokinetics [57].
Troubleshooting Guides
Issue 1: Nanoparticle Aggregation in Biological Fluids
Problem: Nanoparticles aggregate when introduced into culture media or physiological buffers, leading to inconsistent results and potential toxicity.
Solution:
- Surface Functionalization: Coat nanoparticles with stabilizing agents like polyethylene glycol (PEG) or polysorbates (Tween) to create a steric hindrance that prevents aggregation [58].
- Charge Stabilization: Ensure nanoparticles have a sufficient zeta potential (typically > ±30 mV) to create electrostatic repulsion between particles. Be cautious, as a highly positive charge may increase non-specific binding to cells and proteins [53] [54].
- Characterization: Use Dynamic Light Scattering (DLS) to monitor hydrodynamic size and Nanoparticle Tracking Analysis (NTA) for size and concentration in the actual dispersant you will use. NTA is particularly useful for polydisperse samples and provides number-weighted distributions [59].
Issue 2: AMPs are Degraded by Proteases in Serum
Problem: The antimicrobial activity of my AMP is significantly reduced in the presence of serum or plasma, likely due to proteolytic degradation.
Solution:
- Amino Acid Substitution: Replace natural L-amino acids with their D-enantiomers or use non-natural amino acids that are not recognized by proteases [57].
- Peptide Cyclization: Create cyclic analogs of the AMP, which are often more conformationally rigid and resistant to protease activity. For example, the clinical candidate NP213 (Novexatin) is a cyclic peptide designed for improved stability [57].
- Encapsulation: Formulate the AMP within a protective drug delivery system, such as polymeric nanoparticles or liposomes. This physically shields the peptide from degradative enzymes until it is released at the target site [57].
Issue 3: Inability to Penetrate Bacterial Biofilms
Problem: Neither my conventional antibiotics nor my experimental nano-AMP formulations are effective against established biofilms.
Solution:
- Exploit Nanoparticle Properties: Use small, metallic nanoparticles like silver (AgNPs) or zinc oxide (ZnO NPs). Their small size allows them to diffuse into the biofilm matrix, and they can generate ROS or release ions that disrupt the extracellular polymeric substance (EPS) and kill dormant bacteria [53] [54].
- Leverage AMP Mechanisms: Certain AMPs have inherent anti-biofilm activity. They can disrupt quorum sensing signals, a key communication system for biofilm maintenance, or directly damage the biofilm structure [60] [57].
- Combination Therapy: Design a nanoparticle that co-delivers an AMP and a conventional antibiotic. The AMP can permeabilize the biofilm and bacterial membranes, facilitating the entry of the antibiotic to its intracellular target [60] [53].
Experimental Protocols & Data Presentation
Protocol 1: Evaluating Bacterial Membrane Disruption by AMPs
Objective: To confirm and visualize the membrane-lytic activity of an AMP.
Materials:
- Bacterial culture (e.g., S. aureus, E. coli)
- AMP solution in appropriate buffer
- Propidium Iodide (PI) or SYTOX Green dye
- Fluorescence microscope or flow cytometer
Method:
- Grow bacteria to mid-log phase.
- Wash and resuspend in buffer.
- Incubate bacterial suspension with PI or SYTOX Green (membrane-impermeant dyes that fluoresce upon binding DNA).
- Add the AMP and monitor fluorescence increase immediately and over time using real-time kinetics.
- Controls: Include untreated bacteria (negative control) and bacteria treated with 70% isopropanol (positive control).
Expected Outcome: A rapid increase in fluorescence indicates that the AMP has compromised the cell membrane, allowing the dye to enter and bind to nucleic acids [55] [56].
Protocol 2: Assessing ROS Generation by Antimicrobial Nanoparticles
Objective: To quantify the production of reactive oxygen species induced by metal oxide nanoparticles.
Materials:
- Nanoparticle suspension (e.g., ZnO, TiOâ‚‚)
- Bacterial culture
- ROS-sensitive fluorescent dye (e.g., DCFH-DA, Dihydroethidium)
- Microplate reader or flow cytometer
Method:
- Prepare a bacterial suspension in PBS or a minimal buffer.
- Load the bacteria with the ROS-sensitive dye according to the manufacturer's protocol.
- Incubate the dye-loaded bacteria with different concentrations of nanoparticles.
- For TiOâ‚‚ nanoparticles, expose the sample to UVA light (e.g., 365 nm) to activate photocatalysis.
- Measure fluorescence at regular intervals (ex/em ~485/535 nm for DCF).
Expected Outcome: A concentration- and time-dependent increase in fluorescence indicates ROS generation, which contributes to oxidative stress and bacterial death [53] [54].
Table 1: Key Research Reagent Solutions
| Reagent/ Material | Function in Research | Key Considerations |
|---|---|---|
| Silver Nanoparticles (AgNPs) | Broad-spectrum antimicrobial agent; disrupts membranes, inhibits enzymes, damages DNA [53] [54]. | Size and surface coating critically affect efficacy and toxicity. Monitor for aggregation in biological fluids. |
| Zinc Oxide Nanoparticles (ZnO NPs) | Generates reactive oxygen species (ROS); effective against biofilms [53] [54]. | Antimicrobial activity is highly dependent on particle morphology and UV activation. |
| Cationic Lipids/Polymers | Form nanoparticles for AMP encapsulation; protect from degradation and enhance delivery [57]. | Positively charged surfaces can interact with anionic bacterial membranes but may also increase cytotoxicity. |
| LL-37 Antimicrobial Peptide | Human cathelicidin; studied for antibacterial, immunomodulatory, and wound-healing properties [55] [56]. | Prone to proteolysis. Its derivatives and analogs are often used to improve stability. |
| Daptomycin | Clinically approved lipopeptide antibiotic; targets the bacterial membrane in a calcium-dependent manner [57]. | A key positive control for experiments involving membrane-acting agents against Gram-positive bacteria. |
| Propidium Iodide / SYTOX Green | Membrane-impermeant fluorescent dyes; indicate loss of membrane integrity [55]. | Essential for validating the membrane-disruption mechanism of action for both AMPs and nanoparticles. |
Table 2: Minimum Inhibitory Concentration (MIC) Ranges for Selected Nanoparticles
| Nanoparticle Type | Target Bacterium | Typical MIC Range | Key Influencing Factors |
|---|---|---|---|
| Silver (AgNPs) | E. coli, S. aureus | Effective at low concentrations, varies by synthesis and coating [53] | Size, shape, surface charge, and coating material [53] [54]. |
| Zinc Oxide (ZnO NPs) | E. coli, S. aureus | Effective concentrations demonstrated in studies [53] | Particle morphology, presence of UV light, bacterial species [53] [54]. |
| Copper (Cu NPs) | E. coli, S. aureus | Shown to be effective in various studies [54] | Oxidation state, particle size, and delivery medium [54]. |
Mechanism and Workflow Visualizations
Diagram 1: Logical workflow for overcoming antibiotic resistance using nanoparticles and AMPs.
Diagram 2: Primary mechanisms of membrane disruption by antimicrobial peptides (AMPs).
FAQs: Core Concepts and Mechanisms of Action
Q1: How do microbiome-based interventions like FMT and probiotics help combat antibiotic-resistant pathogens?
These interventions primarily work through the principle of colonization resistance, which is the innate ability of a healthy gut microbiome to prevent the expansion and domination of opportunistic pathogens [61] [62]. The mechanisms include:
- Nutrient Competition: A diverse microbiota consumes available nutrients, leaving fewer resources for pathogens [62].
- Production of Inhibitory Metabolites: Beneficial bacteria produce metabolites like short-chain fatty acids (SCFAs) which lower gut pH, creating an unfavorable environment for many Gram-negative pathogens [61] [62].
- Niche Exclusion: By occupying physical niches in the gut lining, resident microbes prevent pathogens from establishing a foothold [62].
- Restoration of Microbial Diversity: FMT, in particular, aims to repair the broad microbial diversity damaged by antibiotics, thereby restoring the functional capacity of the microbiome that confers protection [63] [64].
Q2: What is the key regulatory and conceptual difference between Probiotics, FMT, and Live Biotherapeutic Products (LBPs)?
The table below summarizes the key distinctions:
| Intervention | Definition & Composition | Regulatory Status (in the U.S.) | Key Characteristics |
|---|---|---|---|
| Probiotics | Live microorganisms (e.g., Lactobacilli, Bifidobacteria) intended to confer a health benefit [64]. | Generally classified as dietary supplements [64]. | Not required to undergo pre-market approval for efficacy; evidence for benefits in disease treatment is often limited [64]. |
| Fecal Microbiota Transplantation (FMT) | Transfer of the entire microbial community from screened healthy donor stool [61]. | Regulated as a drug by the FDA. Approved for recurrent C. difficile under enforcement discretion [63] [64] [65]. | Aims to restore the entire gut ecosystem; highly effective for rCDI. Composition is complex and variable [63] [61]. |
| Live Biotherapeutic Products (LBPs) | A defined consortium of live microorganisms (bacteria or yeasts) produced under controlled laboratory conditions [63] [61]. | Regulated as biological products/drugs by the FDA [63] [61]. | Offer a standardized, targeted approach; designed to avoid the variability of donor-derived products [63]. |
Q3: What are the primary safety concerns associated with FMT, and how can they be mitigated in a clinical trial setting?
Key safety concerns include:
- Infectious Agent Transmission: The primary risk is the inadvertent transmission of undetected pathogens from donor to recipient [61] [65]. Mitigation requires a rigorous donor screening program including detailed medical history and testing for blood and enteric pathogens [61].
- Long-Term Unknowns: The long-term health effects of altering a recipient's microbiome are not fully known [65] [66].
- Off-Target Effects and "Mismatches": Recent research indicates that microbes from a fecal transplant (primarily from the colon) can persist in unintended regions of the gut (like the small intestine) for months, potentially "terraforming" the local environment and leading to changes in host metabolism and immune function [66]. Mitigation strategies under investigation include using "omni-microbial" transplants sourced from different gut regions [66].
Troubleshooting Common Experimental Challenges
Q4: We are observing inconsistent engraftment of donor microbes in our FMT studies. What factors could be influencing this?
Inconsistent engraftment is a common challenge and can be influenced by several recipient and methodological factors:
- Recipient's Pre-Existing Microbiome: The composition of the recipient's microbiome at baseline can create a permissive or resistant environment for incoming donor strains [64] [67].
- Recipient Antibiotic Preconditioning: The type and duration of antibiotic regimen used to precondition the recipient can significantly impact engraftment success. Stopping antibiotics 12-48 hours before FMT is a common practice, but protocols may need optimization [61].
- Donor-Recipient Matching: There is no standard for donor-recipient matching beyond safety screening. Incompatibility at the strain level may hinder engraftment.
- Delivery Method and Formulation: The route of administration (e.g., colonoscopy, enema, oral capsule) and the state of the product (fresh vs. frozen) can affect which parts of the gut are colonized and to what degree [61] [66].
Q5: Our team is developing a defined LBP. How can we track the persistence and functional activity of our bacterial strains in vivo?
Advanced genomic tools are now available for precise strain-level tracking:
- Long-Read Metagenomic Sequencing with Strain-Resolved Tracking: A recently developed method combines long-read DNA sequencing (which reads longer genetic fragments) with a computational tool called LongTrack [68]. This allows researchers to create a unique genetic "fingerprint" for each donor strain and track its fate and evolution in the recipient's gut over months or years with high reliability and scalability [68].
- Functional Metagenomics and Metabolomics: To assess functional activity, pairing genomic tracking with metabolomic profiling of stool samples can link the presence of specific strains to the production of key metabolites (e.g., SCFAs, bile acids) [67].
Q6: In models of antibiotic-induced dysbiosis, probiotic administration sometimes delays microbiome recovery. How should we interpret this finding?
This is a documented phenomenon. Studies show that administering a common probiotic consortium after antibiotics can delay the return of the gut microbiome to its pre-antibiotic state, whereas an autologous FMT (using the patient's own pre-antibiotic stool) accelerates it [64]. This suggests that:
- Probiotics Can Occupy Ecological Niches: The administered probiotic strains may temporarily fill the ecological space opened by antibiotics, potentially slowing the recovery of the more diverse indigenous microbiota [64].
- Interpretation Depends on the Goal: This finding highlights that the effect of a microbiome intervention is context-dependent. If the goal is rapid restoration of the host's native microbiome, probiotics post-antibiotics might not be optimal. However, if the goal is immediate introduction of specific beneficial functions, they may be useful [64].
Experimental Protocols & Workflows
Protocol 1: Assessing FMT Efficacy in a Murine Model of Antibiotic-InducedC. difficileInfection (CDI)
This protocol outlines key steps for establishing a robust in vivo model to study FMT against recurrent CDI.
1. Model Induction:
- Antibiotic Preconditioning: Administer a broad-spectrum antibiotic cocktail (e.g., kanamycin, gentamicin, colistin, metronidazole, vancomycin) in the drinking water for 3-7 days to disrupt the native microbiota [62].
- C. difficile Challenge: After a washout period, administer a defined dose of a toxigenic C. difficile strain (e.g., ribotype 027) via oral gavage [63].
2. Intervention Phase:
- Group Allocation: Randomize mice into treatment groups:
- FMT Group: Receive fecal microbiota transplant from a healthy donor mouse via oral gavage.
- Vehicle Control Group: Receive a vehicle control (e.g., saline with glycerol).
- Untreated Control Group.
- FMT Preparation: Prepare donor FMT from pooled fresh or frozen feces from specific pathogen-free healthy mice, suspended in anaerobic PBS with cryoprotectant [61].
3. Outcome Assessment:
- Clinical Scoring: Monitor and score daily for weight loss, diarrhea, and survival.
- Microbial Engraftment: Collect fecal samples pre- and post-FMT for 16S rRNA sequencing or shotgun metagenomics to assess changes in microbial diversity and donor strain engraftment [68].
- Functional Analysis: Perform metabolomic analysis (e.g., GC-MS for SCFAs) on cecal contents to correlate engraftment with functional restoration [62].
- Pathogen Burden: Quantify C. difficile load in feces using quantitative PCR for toxin genes or culture methods.
Protocol 2: In Vitro Co-culture Assay to Screen LBP Candidates Against Multi-Drug Resistant (MDR) Bacteria
This protocol provides a high-throughput method to identify bacterial strains that can inhibit the growth of MDR pathogens.
1. Pathogen and LBP Strain Preparation:
- Culture the target MDR pathogen (e.g., extended-spectrum beta-lactamase (ESBL)-producing E. coli or vancomycin-resistant Enterococcus faecium (VRE)) in appropriate broth to mid-log phase.
- Culture candidate LBP strains (e.g., from Bacteroides, Clostridium clusters, or other commensals) anaerobically to mid-log phase.
2. Co-culture Setup:
- In an anaerobic chamber, combine the prepared cultures in a defined ratio (e.g., 1:1) in fresh, pre-reduced medium.
- Include control wells containing only the pathogen and only the LBP candidate.
- Incubate the co-culture plates anaerobically at 37°C for 24-48 hours.
3. Inhibition Analysis:
- Viable Counts: After incubation, serially dilute the co-culture and plate on selective agars to enumerate the viable counts of the pathogen and the LBP candidate separately.
- Metabolite Profiling: Analyze the spent culture medium for pH changes and the production of inhibitory metabolites like lactic acid or SCFAs.
- Data Interpretation: A significant reduction in the pathogen count in the co-culture compared to the pathogen-only control indicates inhibitory activity of the LBP candidate.
The Scientist's Toolkit: Key Research Reagents & Materials
| Reagent / Material | Function / Application in Research |
|---|---|
| Gnotobiotic (Germ-Free) Mice | Essential for establishing causal links between a specific microbiome and a host phenotype. Allows for colonization with defined microbial communities [64]. |
| Anaerobic Chamber/Workstation | Creates an oxygen-free environment essential for the cultivation, manipulation, and processing of obligate anaerobic gut bacteria without loss of viability [61]. |
| Cryoprotectants (e.g., Glycerol) | Added to fecal and bacterial suspensions before freezing to maintain microbial viability during long-term storage at -80°C [61]. |
| Long-Read DNA Sequencer (e.g., PacBio, Nanopore) | Enables high-resolution, strain-level tracking of microbial communities after interventions like FMT, allowing researchers to follow donor strain engraftment and evolution over time [68]. |
| Selective Media & Agars | Used for the selective cultivation and enumeration of specific bacterial groups (e.g., MacConkey for Gram-negatives, BBE for Bacteroides) from complex communities like stool [62]. |
| Anti-CDI Antibiotics (Vancomycin, Fidaxomicin) | Used in both clinical and preclinical models as a standard-of-care control and to precondition subjects for FMT or LBP studies by clearing C. difficile vegetation [63]. |
| Triflumizole | Triflumizole, CAS:99387-89-0, MF:C15H15ClF3N3O, MW:345.75 g/mol |
| 3-Octanol | 3-Octanol, CAS:20296-29-1, MF:C8H18O, MW:130.23 g/mol |
Visualizing Workflows and Pathways
Colonization Resistance Mechanisms
Strain-Tracking Workflow Post-FMT
Navigating Development Challenges: Optimization and Translational Hurdles
Frequently Asked Questions (FAQs) on Antibiotic R&D Economics
FAQ 1: Why have large pharmaceutical companies largely exited antibiotic R&D?
Large pharmaceutical companies have abandoned antibiotic research primarily for economic reasons. The traditional market-based financing model, which relies on high sales volumes and premium pricing, fails for antibiotics. New antibiotics are typically used as last-resort treatments, necessitating low usage to preserve their efficacy. This results in low sales; the average revenue for a new antibiotic in its first eight years on the market is only about $240 million in total, far less than the estimated $300 million in annual revenue needed for sustainability. Furthermore, the high cost of clinical trials, particularly for resistant infections, makes development financially unsustainable under the current model [69].
FAQ 2: What are "pull incentives" and how can they revitalize the pipeline?
Pull incentives are financial mechanisms designed to reward successful development and availability of new antibiotics, decoupling revenue from the volume of sales. They are considered essential for revitalizing the R&D pipeline. The core concept is delinkage, where the cost of R&D is separated from the price and sales volume of the end-product. This can be achieved through models like substantial upfront prize payments or market-entry rewards upon antibiotic approval. These incentives ensure a return on investment for companies without creating pressure to oversell the new drug, thereby supporting both innovation and responsible use [70] [71].
FAQ 3: What are the major scientific challenges in early-stage antibiotic discovery?
Even before economic barriers, significant scientific challenges hamper early-stage R&D. Antibiotic discovery has a much lower yield compared to other drug classes. Key unresolved scientific hurdles include [69] [71]:
- Compound Penetration and Efflux: Getting potential drugs to accumulate inside bacterial cells, especially Gram-negative bacteria, is difficult due to their protective outer membranes and efflux pumps that actively expel toxins.
- Managing Toxicity: Finding compounds that are highly effective against bacterial targets but non-toxic to human cells remains a major challenge.
- The "Valley of Death": The transition from basic research to clinical development is particularly difficult for small biotechs and academics due to limited public funding for translational research and a lack of venture capital interest [71].
FAQ 4: How does environmental pollution from manufacturing drive antibiotic resistance?
Waste from antibiotic production sites can create local environmental "hotspots of resistance". When antibiotic residues enter waterways from manufacturing effluent, they exert selective pressure on environmental bacteria, favoring the survival and proliferation of resistant strains and promoting the horizontal gene transfer of resistance genes. This disproportionately affects low- and middle-income countries, where regulatory frameworks may be weaker. Addressing this requires transparent supply chains, stronger global environmental regulations, and the adoption of cleaner production technologies [72].
FAQ 5: What is the current state of the clinical antibacterial pipeline?
According to a 2025 WHO report, the clinical antibacterial pipeline is shrinking and fragile. As of early 2025, there are only 90 agents in clinical development, down from 97 in 2023. Of these, only 50 are traditional antibiotics, and the rest are non-traditional agents (e.g., bacteriophages, lysins). Critically, innovation is limited; only 15 agents are considered innovative, and a mere 5 of these target WHO critical priority pathogens. This highlights an urgent need for increased R&D investment and coordination [73].
Troubleshooting Guides for R&D Economic Challenges
Problem 1: Securing Sustainable Funding for Late-Stage Clinical Trials
Symptom: A promising antibiotic candidate has successfully completed early-phase trials, but the development team cannot secure funding for the large, costly Phase 3 trials required for regulatory approval.
Background: Phase 3 trials for antibiotics are expensive, often requiring thousands of patients across multiple sites. Trials targeting resistant infections are even more costly and challenging to enroll. One trial for an antibiotic against carbapenem-resistant Enterobacteriaceae (CRE) was estimated to cost $1 million per recruited patient [69].
Solution: Implement a delinked, publicly-funded pull incentive model.
Resolution Protocol:
- Advocate for Policy Change: Engage with policymakers and health technology assessment bodies to demonstrate the public health value of the new antibiotic, emphasizing its role in treating resistant infections and enabling modern medicine (e.g., surgery, cancer therapy).
- Pursue Market Entry Rewards: Lobby for governments to collectively fund substantial, upfront financial rewards (e.g., $1-1.5 billion per antibiotic) upon successful regulatory approval. This payment is delinked from sales volume and secures a return on investment.
- Partner with Non-Profit PDPs: Collaborate with not-for-profit Product Development Partnerships (PDPs) like the Global Antibiotic Research and Development Partnership (GARDP). These organizations can provide funding, expertise, and share the risk of late-stage development [71].
- Design Efficient Trials: Work with regulators to design innovative clinical trial protocols that may be smaller, faster, or use alternative endpoints, reducing overall costs while maintaining scientific and regulatory rigor.
Problem 2: Navigating the "Valley of Death" in Translational Research
Symptom: An academic research group has identified a promising novel compound with good in vitro activity against a priority pathogen, but lacks the resources and expertise to advance it into pre-clinical and clinical development.
Background: The "valley of death" refers to the gap between basic research and clinical application. With most large pharma having left the field, this gap has widened. The global pool of active AMR researchers is estimated to be only ~3,000, creating a major expertise gap [69] [71].
Solution: Establish a multi-stakeholder partnership to bridge the translational gap.
Resolution Protocol:
- Conduct Robust IP and Market Analysis: Perform a thorough analysis of the compound's intellectual property landscape and its potential fit within the WHO priority pathogen list to attract partners and funders.
- Seek Translational Grant Funding: Apply for public grants specifically aimed at translational research, such as those from the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) or similar national initiatives.
- Form a Strategic Partnership: License the asset to a specialized biotech company with antimicrobial development expertise or establish a joint venture with a contract research organization (CRO) that has antimicrobial experience.
- Access Specialist Networks: Leverage the expertise and networking opportunities provided by organizations like the BEAM Alliance (representing European biotechs in AMR) and attend specialized conferences (e.g., the AMR Conference, GAMRIC) to connect with potential partners and investors [73].
Quantitative Data on the Antibiotic R&D Landscape
Table 1: Economic Challenges in Antibiotic R&D
| Challenge | Metric / Data Point | Source / Reference |
|---|---|---|
| R&D Cost | Mean cost to develop a systemic anti-infective: $1.3 billion | [69] |
| Post-Approval Cost | Additional $240-622 million over 5 years | [69] |
| Revenue vs. Need | Average total revenue (first 8 years): $240 million; Sustainable annual revenue needed: >$300 million | [69] |
| Clinical Pipeline Size | 90 agents in clinical development (2025), down from 97 in 2023 | [73] |
| Innovation Gap | Only 5 innovative agents target WHO Critical Priority pathogens | [73] |
| Expertise Drain | Only ~3,000 active AMR researchers globally | [69] |
Table 2: Proposed Sustainable Economic Models for Antibiotic R&D
| Model | Core Principle | Key Advantage | Implementation Example |
|---|---|---|---|
| Full Delinkage | Completely separate R&D costs from price and sales volume via upfront rewards. | Removes incentive to oversell; preserves antibiotic efficacy. | A global fund that provides a $1 billion+ market entry reward upon successful drug approval [71]. |
| Transferable Exclusivity Vouchers (TEVs) | Grant a voucher for extended market exclusivity on another, more profitable drug in return for developing a new antibiotic. | Leverages existing market mechanisms without direct government expenditure. | Under discussion in Europe; a company that brings a new antibiotic to market receives a voucher it can use or sell to another company [73]. |
| Publicly Funded PDPs | Use public and philanthropic funds to drive R&D through non-profit product development partnerships. | Aligns R&D with public health needs rather than profit maximization. | The Global Antibiotic R&D Partnership (GARDP) partners with biotechs and academics to develop new treatments [71]. |
Experimental Protocols & Workflows
Protocol: Framework for Implementing a Delinked Pull Incentive
Objective: To establish a government-led, sustainable funding model that rewards the successful development of a new antibiotic targeting a WHO priority pathogen, without relying on sales revenue.
Methodology:
- Needs Assessment & Priority Setting:
- Convene a global coordination entity (e.g., under WHO auspices) with stable funding and appropriate expertise [71].
- Use the WHO Priority Pathogens List (PPL) to identify the most critical unmet needs.
- Define Target Product Profiles (TPPs) for desired antibiotics (e.g., oral formulation, activity against XDR Gram-negative bacteria).
Fund Establishment and Sizing:
- Governments and other funders collectively capitalise a global antibiotic reward fund.
- The size of the reward should be sufficient to provide a competitive return on investment, estimated to be in the range of $1 to $1.5 billion per approved antibiotic [71].
Application and Evaluation:
- Developers (biotechs, academia, PDPs) submit applications for projects, from late-stage preclinical to Phase 3-ready assets.
- An independent, scientific review board assesses applications based on:
- Alignment with the predefined TPPs and priority pathogens.
- Scientific innovation and clinical need.
- Potential to address cross-border health threats.
Contracting and Payment:
- Successful applicants enter into a contract with the fund.
- A significant portion of the reward is paid upon regulatory approval (e.g., by the FDA or EMA).
- Further conditions can be attached, such as commitments to affordable pricing, sustainable production, and responsible stewardship.
Post-Market Management:
- The developer may be required to maintain a baseline supply.
- Governments ensure responsible use through national stewardship programs and surveillance.
Visualizing the R&D Ecosystem and Solutions
Table 3: Research Reagent Solutions for Antibiotic Discovery
| Item / Resource | Function / Application | Relevance to Economic Challenge |
|---|---|---|
| WHO Priority Pathogens List (PPL) | A list of antibiotic-resistant bacteria to guide R&D priorities and resource allocation. | Ensures research targets the most pressing public health needs, improving the impact of R&D investment [71] [73]. |
| Non-Traditional Agents (e.g., Bacteriophages, Lysins) | Alternative therapeutic approaches that can bypass traditional resistance mechanisms. | Represents innovative pathways beyond small molecules, potentially offering new patent life and overcoming existing resistance [69] [73]. |
| Diagnostic-Guided 'Theranostics' | Using rapid diagnostics to identify specific pathogens and resistance markers to guide targeted therapy. | Enables more efficient clinical trials and supports responsible antibiotic use post-approval, preserving drug efficacy [69]. |
| Global R&D Coordination Platforms | Entities (e.g., proposed under WHO) that coordinate funding, priorities, and data sharing across countries. | Reduces duplication of effort, pools risk and resources, and creates economies of scale, making the overall R&D ecosystem more efficient [71]. |
| Public-Private Partnership Agreements | Legal and collaborative frameworks for partnerships between academia, biotech, and non-profit PDPs. | Mitigates risk for single entities by sharing costs, expertise, and infrastructure, bridging the "valley of death" [71]. |
Antimicrobial resistance (AMR) is an increasingly prevalent global health problem that undermines the efficacy of critical antimicrobial agents [10]. With one in six laboratory-confirmed bacterial infections worldwide now showing resistance to antibiotic treatments, the development of new therapeutic strategies is more urgent than ever [2]. Clinical trials for novel antimicrobial agents face significant methodological challenges, particularly in patient recruitment and the application of non-inferiority designs. This technical support guide addresses these complexities within the broader context of preventing antibiotic resistance development during therapy research.
Troubleshooting Guide: Patient Recruitment Challenges
Problem: Slow enrollment of eligible patients in antibiotic resistance trials
Diagnosis: Identifying specific bottlenecks in the recruitment pipeline for multidrug-resistant infection studies.
Solution: Implement a multi-faceted recruitment strategy
- Utilize centralized laboratory surveillance data to identify patients with resistant pathogens more efficiently [2]
- Establish screening partnerships with high-risk patient settings including intensive care units, oncology wards, and long-term care facilities [10]
- Develop predictive models using local resistance pattern data to anticipate patient populations likely to harbor resistant infections [74]
Prevention: Design trials with pragmatic eligibility criteria that reflect real-world patient populations while maintaining scientific validity [74].
Problem: High screen failure rates due to evolving resistance patterns
Diagnosis: Rapidly changing local resistance epidemiology renders pre-specified inclusion criteria obsolete.
Solution:
- Incorporate adaptive enrollment strategies that allow modification of microbiological inclusion criteria based on interim surveillance data [74]
- Implement molecular diagnostic screening to rapidly identify patients with specific resistance mechanisms of interest [10]
- Establish continuous resistance monitoring at participating sites to guide recruitment focus [2]
Troubleshooting Guide: Non-Inferiority Design Challenges
Problem: Determining appropriate noninferiority margins for antimicrobial trials
Diagnosis: The crucial but difficult step in designing noninferiority trials is prespecifying a margin that establishes the new drug is not worse than its active comparator while accounting for uncertainty in the effect size of the active control versus placebo [75].
Solution: Apply the fixed-margin method (95%-95% method)
- Determine M1: Conservative estimate (smallest effect size possible) of the active comparator's effect versus placebo, using the upper bound of the 95% confidence interval of the pooled effect size from historical placebo-controlled trials [75]
- Calculate M2: Largest clinically acceptable difference representing the degree of inferiority, typically preserving 50%-67% of M1 [75]
- Validate margin selection against serious outcomes and relative safety profiles of the investigational product and comparator [75]
Prevention: Conduct comprehensive meta-analysis of historical placebo-controlled trials with similar designs, populations, and outcome measures before finalizing the noninferiority margin [75].
Problem: Insufficient statistical power due to unexpectedly high placebo rates
Diagnosis: Historical effect sizes of active comparator may not reflect current clinical practice.
Solution:
- Incorporate adaptive features such as sample-size re-estimation using interim data [74]
- Use group-sequential designs with pre-specified alpha-spending functions for early stopping [74]
- Consider hybrid designs that combine noninferiority and superiority testing frameworks [74]
Frequently Asked Questions (FAQs)
Q: What are the key considerations when choosing a noninferiority margin for trials of antibiotics targeting multidrug-resistant organisms?
A: The margin must account for both clinical and statistical considerations. For serious infections caused by multidrug-resistant organisms, it is crucial to preserve a substantial portion of the active comparator's effect, often 67% or higher, particularly when studying last-resort antibiotics like carbapenems [75]. The margin should also reflect the clinical seriousness of the outcome and the benefit-risk profile of both the investigational product and the active comparator.
Q: How can we improve the generalizability of trial results while maintaining internal validity in antibiotic resistance studies?
A: Consider incorporating pragmatic trial features that align procedures with routine clinical care, such as broader eligibility criteria and flexible visit schedules [74]. This approach enhances generalizability while rigorous randomization, blinding, and prespecified analyses maintain internal validity. Hybrid explanatory-pragmatic designs are particularly valuable for effectiveness assessment in real-world settings [74].
Q: What operational safeguards are essential for antimicrobial trials targeting high-risk populations?
A: Implement a Data and Safety Monitoring Board (DSMB) when conducting trials in critically ill patients with multidrug-resistant infections [74]. Additionally, employ risk-based monitoring focused on errors that impact patient safety and primary endpoints, and predefine protocol deviation handling and safety signal escalation paths [74].
Q: How can we address the challenge of microbiome disruption assessment in long-term antibiotic trials?
A: Incorporate microbiome analysis as a secondary or exploratory endpoint using standardized sampling protocols. Consider adaptive designs that allow for protocol modifications based on emerging microbiome data while preserving trial integrity [10].
Experimental Protocols for Antibiotic Resistance Studies
Protocol 1: Assessing Resistance Development During Therapy
Objective: To evaluate the potential for resistance emergence during investigational antibiotic treatment.
Methodology:
- Obtain serial isolates from patients throughout treatment course at days 0, 3, 7, and end of therapy [10]
- Perform minimum inhibitory concentration (MIC) testing using broth microdilution methods according to CLSI guidelines
- Conduct whole-genome sequencing on paired isolates showing MIC changes to identify resistance mechanisms [10]
- Assess fitness cost of potential resistance mutations through growth curve analysis
Endpoint: Proportion of patients with emergent resistance defined as ≥4-fold increase in MIC during treatment.
Protocol 2: Evaluating "Resistance Hacking" Approaches
Objective: To test strategies that exploit bacterial resistance mechanisms for enhanced efficacy.
Methodology:
- Engineer prodrug analogs designed to be activated by bacterial resistance enzymes (e.g., Eis2 in Mycobacterium abscessus) [12]
- Compare activity against wild-type and resistance gene knockout strains
- Assess potential for auto-amplification through resistance pathway activation (e.g., WhiB7 regulon) [12]
- Evaluate specificity through testing against human mitochondrial ribosomes [12]
Endpoint: Demonstration of enhanced potency specifically in resistant strains through resistance pathway exploitation.
Quantitative Data on Antibiotic Resistance
Table 1: Global Prevalence of Antibiotic Resistance in Key Pathogens (WHO GLASS Report 2023) [2]
| Pathogen | Antibiotic Class | Global Resistance Prevalence | Notes |
|---|---|---|---|
| Escherichia coli | Third-generation cephalosporins | >40% | First-choice treatment for bloodstream infections |
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% | Exceeds 70% in African Region |
| Acinetobacter spp. | Carbapenems | Increasing | Narrowing treatment options significantly |
| Multiple pathogens | Fluoroquinolones | Increasing | Essential life-saving antibiotics losing effectiveness |
Table 2: Noninferiority Margin Determination Examples from Antimicrobial Trials [75]
| Trial Type | Active Comparator | M1 (Control Effect) | Preservation | M2 (Margin) | Rationale |
|---|---|---|---|---|---|
| Venous thromboembolism prophylaxis | Enoxaparin | RD: -0.26 (95% CI: -0.33 to -0.19) | 50% | RD: 0.130 | Fixed-margin method |
| Venous thromboembolism prophylaxis | Enoxaparin | RD: -0.26 (95% CI: -0.33 to -0.19) | 67% | RD: 0.086 | Higher preservation for serious outcome |
Research Reagent Solutions
Table 3: Essential Materials for Antibiotic Resistance Mechanism Studies
| Reagent | Function | Application Example |
|---|---|---|
| CRISPR/Cas-based systems | Gene editing to study resistance mechanisms | Investigating genetic basis of resistance [10] |
| Molecular diagnostic probes | Rapid detection of resistance genes | Screening for blaKPC, blaNDM, blaOXA-48 genes [10] |
| Prodrug analogs | Exploiting resistance enzymes for activation | Florfenicol analogs activated by Eis2 in M. abscessus [12] |
| Phage susceptibility testing | Assessing alternative therapeutic approaches | Evaluating bacteriophage K activity against S. aureus [10] |
| Biofilm formation assays | Studying resistance in bacterial communities | Assessing S. aureus biofilm-related resistance [10] |
Visualizations
Noninferiority Trial Design Logic
Resistance Hacking Mechanism
Patient Recruitment Strategy
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What types of data are most critical for training accurate AI models to predict antibiotic resistance evolution? The most critical data includes antibiotic susceptibility test (AST) results (e.g., MIC values, zone diameters), patient demographic data, sample collection details, and bacterial genotype data, such as the presence or absence of resistance markers like β-lactamase genes (CTXM, TEM, AMPC) [76]. For models focusing on population dynamics, data on bacterial growth, death rates, and horizontal gene transfer frequencies are essential [77]. The quality, granularity, and standardization of this data are paramount; models like XGBoost have achieved high performance (AUC 0.96) using such comprehensive, curated datasets [76].
FAQ 2: My model's predictions are inaccurate for bacterial communities beyond simple, clonal populations. What strategies can improve performance for complex communities? This is a common challenge. Mechanistic models often fail in complex communities because they require complete knowledge of all interactions [77]. A recommended strategy is to use Machine Learning to augment mechanistic modeling. ML can identify key interaction patterns from large, high-throughput community data without requiring a full mechanistic understanding. Techniques include using neural networks to learn from time-series abundance data of community members or employing random forests to identify the most influential species interactions driving resistance dynamics [77].
FAQ 3: How can I handle significant missing data in my genomic surveillance datasets without compromising clinical relevance? While imputation techniques can be applied to increase prediction accuracy, they must be used with extreme caution in a clinical context [76]. It is crucial to assess the imputation method's reliability and potential to mislead. From a clinical decision-making perspective, a more robust approach is to use models that can handle missing data natively or to perform analysis only on the available data, clearly communicating the associated uncertainty. Experts recommend developing systems that "know when they don't know" to avoid overconfident predictions from incomplete data [78].
FAQ 4: What are the most promising non-traditional AI approaches for combating resistance beyond small-molecule discovery? AI is enabling several innovative strategies. These include:
- "Resistance Hacking": Using AI to design prodrugs that are selectively activated by a bacterium's own resistance enzymes, turning its defense mechanisms against it [12].
- Bacteriophage Therapy: AI can help identify and engineer phages that target resistant bacteria [79] [78].
- Microbiome Modulation: AI models can predict how interventions like fecal microbiota transplantation (FMT) can reduce the burden of resistant pathogens [80] [81].
- CRISPR-Cas Systems: AI aids in designing targeted gene drives to eliminate resistance genes from bacterial populations [79].
Troubleshooting Guides
Issue 1: Poor Model Performance and Low Predictive Accuracy
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Low AUC/accuracy on test set | Biased training data from geographic or socioeconomic underrepresentation [76]. | Apply data balancing techniques (e.g., SMOTE) to increase recall for minority classes. Actively seek out diverse data sources [76]. |
| Model fails to generalize | Inability to convey uncertainty; model gives overconfident answers on novel data [78]. | Implement modeling frameworks that provide confidence intervals or Bayesian uncertainty estimates. Do not remove phenotypic testing validation [78]. |
| High performance on training data but not on new isolates | Data fragmentation and lack of standardization across different labs and sources [78]. | Prioritize data curation and standardization. Use federated learning approaches where models are trained across institutions without sharing raw proprietary data [78]. |
Issue 2: Technical and Computational Hurdles in Model Implementation
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Generative AI designs molecules that are impossible to synthesize | Unconstrained generative models invent compounds that are not synthetically tractable [82]. | Use generative models constrained to libraries of known molecular "building blocks" that can be feasibly assembled using standard chemical reactions [82]. |
| Mechanistic models become intractable with increasing community complexity | The number of parameters and interactions grows exponentially with community size [77]. | Replace or augment mechanistic models with ML predictors (e.g., Random Forests, CNNs) trained on high-throughput experimental data to predict community dynamics [77]. |
| Difficulty integrating heterogeneous data types (e.g., genomic, clinical, phenotypic) | Data integration issues from non-standardized formats and missing values [76] [78]. | Develop and use structured data pipelines and ontologies. Employ AI-driven data integration tools and focus on creating unified, granular datasets for training [76]. |
Experimental Protocols & Methodologies
Protocol 1: Building a Predictive Model for Antibiotic Resistance from Surveillance Data
This protocol is based on a study that used the Pfizer ATLAS dataset to predict resistance phenotypes [76].
1. Data Acquisition and Curation
- Source: Obtain a comprehensive surveillance dataset, such as the Pfizer ATLAS Antibiotics dataset, which includes 917,049 bacterial isolates with AST results, patient demographics, and for a subset, genotype data [76].
- Curation: Rigorously clean the data. Hold variables like temperature, pH, and media constant to ensure MIC results are comparable. This standardization is critical for model performance [82].
2. Exploratory Data Analysis (EDA) and Preprocessing
- EDA: Use libraries like
matplotlib,pandas, andseabornto understand data distributions, global resistance patterns, and temporal trends. Generate heatmaps to visualize missing data [76]. - Preprocessing: Address the missing data problem. For genotype data with significant absence, consider creating two subsets: one with and one without these features. For model training, employ imputation methods with caution, assessing their impact clinically [76].
3. Model Training, Validation, and Optimization
- Algorithm Selection: Train and compare multiple machine learning models, including XGBoost, Random Forest, and Support Vector Classifiers [76] [83].
- Validation: Use robust cross-validation techniques. XGBoost has been shown to consistently outperform others, achieving AUC values of 0.96 for phenotype-only prediction [76].
- Optimization: Perform hyperparameter tuning for slight accuracy improvements. Apply data balancing techniques to notably increase recall for resistant classes [76].
4. Model Interpretation
- Feature Importance: Determine which features most influenced the prediction. In the referenced study, the specific antibiotic used emerged as the most influential feature [76].
- SHAP Analysis: Generate SHAP (SHapley Additive exPlanations) summary plots to provide insights into model interpretability and understand the direction and magnitude of each feature's effect [76].
The workflow for this protocol is summarized in the diagram below:
Protocol 2: AI-Driven Discovery of Novel Antibiotic Candidates
This protocol outlines the process for using AI to mine or generate new antibiotic molecules, as pioneered by researchers like de la Fuente and Stokes [82].
1. Assembling Training Data
- Action: Curate a high-quality dataset linking chemical structures to biological activity. This requires measuring Minimum Inhibitory Concentrations (MICs) for thousands of molecules across diverse bacterial strains under standardized conditions [82].
- Data Types: Use proteomic and genomic sequencing data from public databases or novel sources (e.g., ancient organisms). For generative AI, datasets of known active and inactive compounds are essential [82].
2. Model Selection and Training
- For Mining: Use machine learning models to parse biological sequence data (proteomes, genomes) and identify snippets that encode products with predicted antimicrobial activity [82].
- For Generation: Employ generative AI models. Train these models on known active/inactive antibiotics, then task them with drawing brand-new molecular structures predicted to be active. To ensure synthesizability, constrain models to use libraries of known molecular "building blocks" [82].
3. Experimental Validation
- Synthesis: Chemically synthesize the top candidate molecules suggested by the AI models.
- In Vitro Testing: Test the synthesized molecules against a panel of target bacteria in the lab to determine MICs and assess antibacterial activity [82].
- In Vivo Testing: Progress the most promising candidates to animal models (e.g., mice with skin abscess or thigh infections) to evaluate efficacy and toxicity in a living system [82].
The workflow for this protocol is summarized in the diagram below:
Protocol 3: Exploiting Resistance Mechanisms via "Resistance Hacking"
This proof-of-concept protocol is based on the work from St. Jude Children's Research Hospital that turned a bacterium's resistance genes against it [12].
1. Identify a Key Resistance Regulator
- Action: Focus on a bacterial pathogen with high intrinsic resistance. Identify a master regulator of the resistance response (e.g., WhiB7 in Mycobacterium abscessus, which controls over 100 proteins involved in antimicrobial resistance) [12].
2. Rational Prodrug Design
- Action: Develop a prodrug—an inactive chemical compound—that is structurally similar to an existing antibiotic known to activate the resistance regulator. The prodrug should be designed to be a substrate for a resistance enzyme induced by the master regulator [12].
3. Establish the Self-Amplifying Cycle
- Validation: Test the prodrug against wild-type bacteria and a mutant strain lacking the resistance regulator.
- Mechanism Confirmation: Confirm that the prodrug's activation is dependent on the resistance enzyme (e.g., Eis2). The active drug should then inhibit its target (e.g., the ribosome), leading to further activation of the master regulator, which in turn produces more of the activating enzyme, creating a perpetual, self-amplifying cycle of antibiotic activation [12].
The logical relationship of this mechanism is summarized in the diagram below:
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in AI-AMR Research |
|---|---|
| Surveillance Datasets (e.g., Pfizer ATLAS) | Provides large-scale, granular data on antibiotic susceptibility test results, patient demographics, and genotype data essential for training and validating predictive ML models [76]. |
| Standardized Bacterial Strain Panels | Curated collections of bacterial isolates, including resistant and susceptible strains, used for generating consistent, high-quality MIC data for AI model training and validation [82]. |
| Whole Genome Sequencing (WGS) Kits | Enable the generation of genomic data from bacterial pathogens, allowing researchers to identify resistance genes and mutations for genotype-phenotype correlation in ML models [76] [78]. |
| High-Throughput Screening Assays | Robotic and automated systems that allow for the rapid experimental testing of thousands of AI-predicted antibiotic candidates against bacterial targets, compressing the discovery timeline [82]. |
| β-lactamase Activity Assays | Used to measure the enzymatic hydrolysis of β-lactam antibiotics and the efficacy of inhibitors. Critical for validating AI predictions on resistance mechanisms for specific drug classes [77]. |
| Federated Learning Platforms | Software solutions that enable brokered data-sharing across institutions, allowing AI models to be trained on decentralized data without transferring proprietary clinical or research data [78]. |
| SHAP (SHapley Additive exPlanations) | A game-theoretic approach to explain the output of any ML model. Used for interpreting feature importance in resistance prediction models, crucial for clinical trust and biological insight [76]. |
| Methyl Salicylate | Methyl Salicylate|High-Purity Research Compound |
Frequently Asked Questions (FAQs)
1. What are the core PK/PD indices used to suppress antimicrobial resistance? The core indices are the ratio of the area under the concentration-time curve to the minimum inhibitory concentration (AUC/MIC), the maximum concentration to MIC ratio (Cmax/MIC), and the percentage of time that the drug concentration exceeds the MIC (%T > MIC). Targeting the mutant prevention concentration (MPC) and minimizing the time that drug concentrations reside within the mutant selection window (MSW)—the range between the MIC and MPC—is a key strategy for suppressing the emergence of resistant subpopulations [84].
2. How do patient-specific factors influence PK/PD target attainment? Patient physiology significantly alters antibiotic pharmacokinetics. Key considerations include:
- Pediatric Patients: High body water content increases the volume of distribution for hydrophilic drugs; renal and hepatic clearance are immature and change rapidly with gestational and postnatal age [84].
- Elderly Patients: Reduced renal and hepatic function are common, leading to prolonged drug half-life. For example, piperacillin clearance can be more than 50% lower in patients over 85 compared to young adults [84].
- Obesity: Altered body composition can affect the volume of distribution and clearance, often necessitating dose adjustments for drugs like levofloxacin [84].
- Organ Dysfunction: Renal impairment drastically reduces the clearance of renally excreted drugs (e.g., meropenem), while hepatic impairment affects metabolized drugs [84].
3. Should I use monotherapy or combination therapy to prevent resistance? Current evidence does not definitively demonstrate a routine benefit of combination therapy over monotherapy for novel drugs when the goal is to prevent resistance. Available studies are limited, and resistance emergence has rarely been a primary endpoint. Prevention currently relies more heavily on optimized PK/PD dosing and infusion strategies than on routine combination regimens [81] [80].
4. What non-antibiotic approaches can support resistance suppression? Non-antimicrobial strategies can reduce the pathogen load and transmission, thereby preserving the effectiveness of antibiotics. These include:
- Phage Therapy: Uses bacteriophages to specifically target and lyse resistant bacteria [81] [85].
- Fecal Microbiota Transplantation (FMT): Can help restore a healthy microbiome and reduce the burden of multidrug-resistant organisms [81].
- Vaccination: Prevents infections, thereby reducing the need for antibiotic use and the risk of resistance emerging [85].
Troubleshooting Guides
Problem 1: Failure to Achieve PK/PD Targets in Special Populations
Issue: Simulated or measured drug exposures are consistently below the target PK/PD index (e.g., AUC/MIC or %T > MIC) in a specific patient group.
Solution:
- Action 1: Identify the primary source of PK variability. Use population PK models to determine if the issue is an increased volume of distribution (Vd) or reduced clearance (CL). For example, in critically ill patients, Vd is often larger, requiring a higher loading dose, while augmented renal clearance may require more frequent dosing or continuous infusion [84].
- Action 2: Implement a dose optimization strategy. The table below summarizes common approaches based on the PK/PD driver of efficacy [84]:
| PK/PD Index | Antibiotic Class | Dosing Strategy | Example |
|---|---|---|---|
| %T > MIC | Beta-lactams (Penicillins, Cephalosporins, Carbapenems) | • Increased frequency• Extended (e.g., 3-4 hours) or continuous infusion | Continuous infusion of meropenem to maintain concentrations above the MIC for 100% of the dosing interval [81]. |
| AUC/MIC | Fluoroquinolones, Glycopeptides, Oxazolidinones | • Increased dose• Altered frequency (note: for concentration-dependent killers) | Higher dose of levofloxacin (750 mg) in morbidly obese patients to achieve target AUC/MIC [84]. |
| Cmax/MIC | Aminoglycosides | • Large, once-daily dosing | Single daily dose of amikacin to maximize concentration-dependent killing. |
- Action 3: Utilize therapeutic drug monitoring (TDM) and Bayesian estimation software when available to individualize dosing in real-time, especially for drugs with a narrow therapeutic index [84].
Problem 2: Emergence of Resistance On-Therapy
Issue: Bacterial isolates from a patient show a progressive increase in MIC during or after a course of antibiotic treatment, indicating the selection of resistant mutants.
Solution:
- Action 1: Re-evaluate the dosing regimen against the Mutant Selection Window (MSW) hypothesis. The goal is to adjust dosing so that drug concentrations do not linger within the MSW. This can be achieved by [84]:
- Increasing the dose to push the Cmax above the MPC.
- Using a loading dose to rapidly achieve concentrations outside the MSW.
- Switching to prolonged/continuous infusion to minimize the Time inside the MSW (TMSW) for time-dependent antibiotics.
- Action 2: For highly resistant pathogens like Mycobacterium abscessus, consider novel strategies such as "resistance hacking." This approach, demonstrated with a modified florfenicol prodrug, exploits the bacterium's own resistance machinery (the WhiB7 regulon and Eis2 protein) to perpetually amplify the antibiotic's effect, effectively reversing resistance [12].
- Action 3: Consider adjunctive non-antibiotic therapies. Phage therapy can be specifically tailored to target the resistant subpopulation that has emerged, while FMT may help decolonize the gut of resistant organisms [81] [85].
Experimental Protocols
Protocol 1: Establishing a PK/PD Model for Resistance Suppression
Objective: To determine the dosing regimen that maximizes efficacy and minimizes the emergence of resistance in an in vitro pharmacokinetic model.
Materials:
- Research Reagent Solutions:
- Glass chemostat or bioreactor to simulate dynamic drug concentrations.
- Pre-calibrated syringe pumps for precise control of antibiotic infusion and elimination.
- Cation-adjusted Mueller-Hinton broth for bacterial growth.
- Reference bacterial strain with a well-defined MIC and MPC.
- Drug stock solution of the antibiotic under investigation.
Methodology:
- Inoculum Preparation: Grow the bacterial strain to mid-log phase and standardize the inoculum to ~10^8 CFU/mL.
- PK Simulation: Set up the bioreactor with fresh broth. Program syringe pumps to simulate human single- or multi-dose pharmacokinetic profiles (e.g., half-life, Cmax) of the test antibiotic.
- Dosing Regimens: Test multiple regimens (e.g., bolus vs. extended infusion, high dose vs. standard dose) in separate experiments.
- Sampling: Collect samples at predetermined time points over 24-72 hours for:
- Total Bacterial Density: Serially dilute and plate on drug-free agar to determine total CFU/mL.
- Resistant Subpopulation: Plate undiluted samples on agar containing the antibiotic at 2x, 4x, and 8x the MIC.
- Drug Concentration: Analyze broth samples via HPLC or bioassay to verify the target PK profile was achieved.
- Data Analysis: Plot time-kill curves and calculate the following for each regimen:
- The change in log10 CFU/mL.
- The duration of time the drug concentration spent within the MSW (TMSW).
- The probability of achieving specific PK/PD targets (AUC/MPC, T>MPC).
Protocol 2: Validating a "Resistance Hacking" Prodrug Approach
Objective: To demonstrate that a modified antibiotic prodrug is selectively activated by a bacterial resistance enzyme, leading to amplified killing in the resistant pathogen.
Materials:
- Research Reagent Solutions:
- Wild-type and isogenic mutant strains (e.g., ΔwhiB7 or Δeis2 for M. abscessus).
- Prodrug and active drug compounds (e.g., engineered florfenicol analog and native florfenicol) [12].
- Cell lysis reagents and protein assay kit for enzyme preparation.
- HPLC-MS system to quantify prodrug activation and drug levels.
Methodology:
- In Vitro Activation Assay:
- Prepare cell-free extracts from wild-type and mutant strains.
- Incubate the prodrug with each extract and necessary co-factors.
- Use HPLC-MS to measure the conversion rate of prodrug to active drug over time.
- Microbiological Susceptibility Testing:
- Determine the MIC of both the prodrug and the active drug against wild-type and mutant strains.
- A key indicator of success is the prodrug having high activity against the wild-type strain but little to no activity against the mutant strain lacking the activating enzyme [12].
- Mechanistic Validation:
- Use RNA sequencing or RT-qPCR to confirm that exposure to the active drug generated by the prodrug leads to upregulation of the resistance regulon (e.g., WhiB7) [12].
- Measure intracellular drug concentrations to confirm the perpetual amplification cycle.
Research Reagent Solutions
| Item | Function/Benefit in PK/PD Resistance Studies |
|---|---|
| Population PK Modeling Software (e.g., NONMEM, Monolix) | Identifies sources of PK variability in a population and facilitates the design of optimized dosing regimens for different patient subgroups [84]. |
| HPLC-MS System | Precisely quantifies antibiotic concentrations in complex biological matrices (e.g., plasma, broth) for accurate PK profiling and TDM [84]. |
| Lytic Bacteriophages | Provides a targeted, non-antibiotic tool to reduce the bacterial burden of specific resistant pathogens, often used in combination with antibiotics [85]. |
| Recombinant Resistance Enzymes | Used in biochemical assays to screen for and characterize prodrug candidates designed to be activated by specific bacterial resistance mechanisms [12]. |
| Biofilm Reactors | Models chronic infections where bacteria are highly tolerant to antibiotics, allowing testing of PK/PD regimens for their ability to penetrate and eradicate biofilms. |
Workflow for PK/PD-Driven Resistance Suppression
The following diagram illustrates the logical workflow and key decision points for designing a dosing regimen aimed at suppressing antimicrobial resistance.
Frequently Asked Questions (FAQ)
Q1: What are the primary advantages of using rapid diagnostic tests (RDTs) in antimicrobial therapy research? RDTs offer several key advantages for research settings. They provide real-time, point-of-care diagnoses, which is crucial for timely decision-making. When enhanced with smartphone-based readers and data capture systems, they can streamline data acquisition for large-scale studies. Furthermore, RDTs designed with Open Guidelines (OGs) can improve data uniformity and integration with laboratory and surveillance systems, maximizing the utility of the information collected for analysis [86].
Q2: My research involves tracking antimicrobial resistance (AMR) trends. How can AI enhance traditional diagnostic methods? Artificial Intelligence (AI) can significantly augment AMR surveillance. Machine learning models can analyze complex datasets from sources like electronic health records (EHRs) to predict sepsis hours before clinical onset, allowing for earlier intervention [87]. AI also excels at analyzing Raman spectroscopy data or bacterial cell images for rapid, culture-independent pathogen identification. Furthermore, AI can process large volumes of genomic and antibiotic susceptibility testing (AST) data to uncover novel resistance mechanisms and patterns that might be missed by conventional analysis [87].
Q3: What are common data-related challenges when integrating rapid diagnostics into existing research information systems? The main challenges stem from a lack of data standards and heterogeneity in form factors. Different RDTs from various manufacturers often have non-uniform hardware and software, creating significant barriers to seamless data integration. This lack of interoperability requires extensive, analytics-intensive tasks to convert and recode data for use in central systems, which can impede real-time analysis and response [86].
Q4: Are there non-invasive diagnostic methods suitable for longitudinal studies on antibiotic resistance? Yes, liquid biopsies are an emerging non-invasive method. These tests analyze blood samples to detect diseases, and their application is expanding. While prominently used in oncology for early cancer detection, research into their use for other diseases, including infectious diseases, is growing. Their non-invasive nature makes them highly suitable for longitudinal studies where repeated sampling is required [88].
Technical Troubleshooting Guides
Issue: Inconsistent Results from Lateral Flow Rapid Diagnostic Tests
Problem: Users report variable or unreliable test line intensities when using immunochromatographic RDTs, leading to difficulties in interpretation.
Solution:
- Step 1: Verify Storage Conditions: Ensure the RDTs have been stored as per the manufacturer's instructions, typically in a cool, dry place. Do not use tests that have been exposed to extreme temperatures or humidity.
- Step 2: Check Expiry Dates: Confirm that all test kits and reagents are within their valid expiration dates.
- Step 3: Standardize Sample Application: Use calibrated pipettes to ensure the exact volume of sample and buffer is applied. Inconsistent volumes are a common source of variation.
- Step 4: Control for Timing: Adhere strictly to the recommended development time for reading the result. Reading too early or too late can lead to false negatives or positives.
- Step 5: Implement a Digital Reader: To eliminate subjective visual interpretation, use a smartphone-based RDT reader. These systems use computer vision to provide an objective, quantitative measurement of the test and control lines, dramatically improving result consistency and data quality [86].
Issue: Poor Integration of Diagnostic Data with Research Databases
Problem: Data generated from diagnostic devices cannot be easily exported or structured for analysis in central research databases or electronic health record (EHR) systems.
Solution:
- Step 1: Advocate for Open Standards: When selecting RDTs for a study, prioritize those that adhere to Open Guidelines (OGs) or similar standards. These guidelines are designed to standardize data capture and output, facilitating horizontal (between manufacturers) and vertical (between system levels) integration [86].
- Step 2: Utilize Interoperability Protocols: Implement data schemas such as Fast Healthcare Interoperability Resources (FHIR). Using these standardized protocols allows diagnostic data to be structured in a consistent format that is readily ingested by other clinical and research information systems [86].
- Step 3: Develop a Middleware Interface: If standard RDTs must be used, create a custom software interface to automatically parse, code, and recode the output data into a standardized format (e.g., CSV, JSON) compatible with your database.
Experimental Protocols for Key Methodologies
Protocol: Experimental Evolution of Bacteriophages to Combat Resistant Bacteria
This protocol details a method to expand the host range of bacteriophages, enabling them to target antibiotic-resistant bacterial strains [24].
- Principle: By co-culturing phages with bacteria over multiple generations, the phages are forced to adapt to bacterial defense mechanisms, potentially evolving an enhanced ability to infect resistant strains.
- Materials:
- Target bacterial strain (e.g., multidrug-resistant Klebsiella pneumoniae)
- Bacteriophage stock specific to the bacterial species
- Liquid growth medium (e.g., Lysogeny Broth)
- Solid agar plates
- Incubator shaker
- Centrifuge and filters (0.22 µm)
- Procedure:
- Day 1: Inoculate a flask of liquid medium with the target bacteria and incubate until mid-log phase growth is achieved.
- Infection: Introduce the initial bacteriophage stock to the bacterial culture at a pre-determined multiplicity of infection (MOI).
- Co-incubation: Allow the phage and bacteria to interact for a set period (e.g., 24 hours) in the incubator shaker.
- Harvesting: Centrifuge the culture to pellet bacterial debris. Pass the supernatant through a 0.22 µm filter to collect the phage lysate, which now contains phages that have successfully infected the host.
- Serial Passage: Use a portion of the filtered lysate to infect a fresh, mid-log phase culture of the same bacterial strain. Repeat steps 3-4.
- Cycle Continuation: Continue this serial passage process for an extended period (e.g., 30 days). This constitutes one round of experimental evolution.
- Plaque Assay: Periodically, plaque assay the evolved phage populations on the original bacterial strain and on other drug-resistant strains to monitor changes in host range and killing efficacy.
- Analysis:
- Compare the plaque-forming ability of the evolved phages versus the ancestral phage on a panel of resistant clinical isolates.
- Sequence the genomes of evolved phages to identify mutations acquired in genes related to host recognition and binding.
Protocol: AI-Assisted Sepsis Prediction from Electronic Health Records
This protocol outlines the use of a deep learning model, such as COMPOSER, for early sepsis prediction using structured EHR data [87].
- Principle: AI models can learn complex, non-linear patterns from sequential patient data to predict the risk of sepsis onset before it is clinically apparent.
- Materials:
- De-identified EHR database (e.g., containing vital signs, lab results, timing data)
- Computational environment with GPU acceleration (e.g., Python with TensorFlow/PyTorch)
- Defined sepsis labels based on clinical criteria (e.g., Sepsis-3)
- Procedure:
- Data Curation: Extract and clean structured data from EHRs. Key features include heart rate, temperature, white blood cell count, and respiratory rate.
- Handle Irregular Timing: Implement a time-encoding strategy to manage the irregular intervals at which clinical measurements are taken.
- Model Architecture:
- Module 1 (Feature Processing): Use a Feedforward Neural Network (FFNN) to generate unified representations from the clinical and timing data.
- Module 2 (Conformal Prediction): Integrate a conformal predictor to identify and flag patient data that significantly deviates from the training set distribution, ensuring the model only makes predictions on reliable data.
- Module 3 (Risk Prediction): The processed features are fed into a final FFNN, which outputs a sepsis risk score between 0 and 1.
- Training: Train the model on a large dataset of patient EHR records, both with and without sepsis.
- Validation: Validate the model on a held-out test set from different hospital sites to assess generalizability. Key metrics include Area Under the Receiver Operating Characteristic Curve (AUROC).
- Analysis:
- Evaluate model performance using AUROC and precision-recall curves.
- In a clinical implementation, monitor outcomes such as relative reduction in in-hospital mortality and increase in sepsis bundle compliance.
Workflow and Pathway Diagrams
RDT-OG System Integration Workflow
This diagram illustrates the flow of information in a Rapid Diagnostic Test-Open Guideline system, from test administration to public health action.
AI-Powered Sepsis Prediction Dataflow
This diagram shows how different types of EHR data are processed by a multi-component AI model like COMPOSER to generate a sepsis risk score.
"Resistance Hacking" Prodrug Mechanism
This diagram visualizes the mechanism by which a prodrug exploits a bacterial resistance system to achieve targeted activation and perpetual amplification.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Key Research Reagents and Materials for Advanced Diagnostic and AMR Studies
| Item | Function/Application in Research | Key Characteristic |
|---|---|---|
| Open Guideline (OG) RDTs | Standardized rapid tests for pathogen detection. Facilitates seamless data integration into research databases. | High "Information Utilization Index (IUI)" for data interoperability [86]. |
| Smartphone-based RDT Reader | An accessory and app that uses a smartphone's camera and processing power to objectively read RDT results. | Eliminates subjective interpretation; enables quantitative data capture and geotagging [86]. |
| Bacteriophages | Viruses that infect and lyse specific bacteria. Used as therapeutic alternatives to antibiotics or in experimental evolution studies. | Can be "trained" to expand host range against resistant strains [24]. |
| Florfenicol Prodrug | A modified antibiotic that acts as a "resistance hacker." Inactive until activated by a specific bacterial resistance enzyme (Eis2). | Exploits the WhiB7 resistome of Mycobacterium abscessus for targeted, amplified killing with reduced off-target toxicity [12]. |
| FHIR (Fast Healthcare Interoperability Resources) Standards | A standards framework for exchanging healthcare information electronically. | Enables interoperability between diagnostic devices, electronic lab notebooks, and clinical data systems [86]. |
| Multiplex PCR Assays | Molecular diagnostic tests that simultaneously detect multiple pathogens or resistance genes from a single sample. | Drastically reduces turnaround time for identifying resistance mutations compared to culture (hours vs. weeks) [88]. |
FAQs: Foundational Concepts and Safety Profiles
Q1: What are the primary safety concerns associated with traditional antibiotics that novel therapies aim to mitigate?
Traditional antibiotics drive antimicrobial resistance (AMR), a top global health threat causing an estimated 1.27 million deaths annually [79]. Safety concerns include:
- C. diff Infection: Antibiotic use disrupts gut microbiota, increasing risk of Clostridioides difficile, which causes severe diarrhea and is linked to nearly 48,000 U.S. deaths annually [89].
- Allergic Reactions: Antibiotics cause 1 in 5 medication-related emergency room visits; reactions range from rash to life-threatening anaphylaxis [90].
- Toxicity: Antibiotics can cause side effects like diarrhea, and harmful effects on kidneys and liver [91].
- Accelerated Resistance: Misuse and overuse of antibiotics allows resistant bacteria to survive and multiply, making drugs ineffective [91] [90].
Q2: How do novel, non-antibiotic therapeutic modalities potentially reduce the risk of fostering antimicrobial resistance?
Novel modalities employ diverse mechanisms that pose a significantly lower selective pressure for resistance compared to traditional antibiotics, which directly target essential bacterial processes [92]. These approaches include:
- Precision Targeting: Bacteriophages and lysins specifically target pathogenic bacteria without harming beneficial microbiota, reducing ecological pressure for resistance [79] [92].
- Immune Potentiation: Therapies that modulate the host immune system (e.g., adaptive and innate immune modulators) help the body clear infections without directly exerting selective pressure on bacteria [79].
- Multi-component Action: Strategies like antimicrobial peptides (AMPs) often target fundamental bacterial structures (e.g., cell membranes), making it more difficult for bacteria to develop resistance through single mutations [92].
- Microbiome Preservation: Modalities such as probiotics, prebiotics, and fecal microbiota transplantation (FMT) work to restore a protective microbial community, thereby outcompeting pathogens and reducing the need for antibiotics [92].
Q3: What are the critical regulatory and clinical development challenges for these novel therapies?
The unique nature of non-antibiotic therapies necessitates the development of alternative regulatory and clinical pathways [79]. Key challenges include:
- Defining Efficacy Endpoints: Traditional antibiotic trials often use non-inferiority designs. For novel modalities (e.g., phage therapy, immune modulators), new endpoints and trial designs must be established to demonstrate clinical value [79].
- Manufacturing and Quality Control: Ensuring consistent, reproducible, and pure batches is complex, especially for biologics like bacteriophages and live microbial consortia (e.g., FMT) [92].
- Demonstrating Superiority: For diseases with existing treatments, proving superiority over standard of care can be difficult and require large, costly trials. For plazomicin, a trial against carbapenem-resistant Enterobacteriaceae (CRE) was stopped after screening 2000 patients yielded only 39 enrollees, at an estimated cost of $1 million per patient [79].
Troubleshooting Guides for Common Experimental Issues
Guide 1: Bacteriophage Therapy
| Symptom | Possible Cause | Troubleshooting Action | Preventive Measures |
|---|---|---|---|
| Reduced lytic activity in subsequent passages. | Emergence of phage-resistant bacterial mutants. | 1. Isolate new bacterial colonies and re-test phage susceptibility.2. Develop a cocktail of multiple phages with different receptor targets.3. Combine phage therapy with sub-inhibitory concentrations of antibiotics for synergistic effect [92]. | Use well-characterized phage cocktails from the outset to target multiple bacterial receptors simultaneously. |
| Inconsistent results in animal infection models. | Rapid clearance of phage by the host immune system. | 1. Modify phage pharmacokinetics using encapsulation techniques.2. Administer a higher multiplicity of infection (MOI).3. Route of administration; consider local/topical application vs. systemic [92]. | Pre-screen phages for stability in target biological fluids (e.g., serum, BALF). |
| Bacterial contamination of phage stocks. | Improper sterile technique during amplification or storage. | Re-purify phage stock via plaque isolation and filtration (0.22 µm). | Always use a double-agar layer method for phage propagation and store stocks with glycerol at -80°C. |
Guide 2: Antimicrobial Peptides (AMPs) and Nanoparticles (NPs)
| Symptom | Possible Cause | Troubleshooting Action | Preventive Measures |
|---|---|---|---|
| High cytotoxicity against mammalian cells. | Non-specific membrane disruption due to low selectivity. | 1. Modify the peptide sequence to increase net positive charge and amphipathicity.2. Switch to D-amino acids to improve proteolytic stability and reduce immune recognition.3. For NPs, adjust surface charge (zeta potential) and functionalization to enhance targeting [92]. | Perform early-stage hemolysis assays and cytotoxicity screens (e.g., against HEK293 or HepG2 cells) during design. |
| Loss of activity in biological fluids (e.g., serum). | Proteolytic degradation of AMPs or protein corona formation on NPs. | 1. Cyclize the AMP or incorporate non-natural amino acids.2. PEGylate NPs or AMPs to shield from enzymatic attack and reduce opsonization.3. Use liposomal or polymeric NP encapsulation for protection [92]. | Include protease inhibitors in in vitro assays or pre-test stability in relevant biological matrices. |
| Poor solubility or aggregation of AMPs/NPs. | High hydrophobicity or inappropriate formulation buffer. | 1. Change solvent system (e.g., use weak acids or organic solvents like DMSO).2. Redesign AMP with fewer hydrophobic residues.3. Use surfactants during NP synthesis to improve dispersion. | During peptide synthesis, incorporate solubilizing tags or charged residues. Characterize NP hydrodynamic diameter and PDI using DLS. |
Guide 3: Microbiome-Based Therapies (e.g., FMT, Probiotics)
| Symptom | Possible Cause | Troubleshooting Action | Preventive Measures |
|---|---|---|---|
| Highly variable efficacy in pre-clinical models. | Donor-to-donor variability or unstable microbial consortium. | 1. Use a defined consortium of bacterial strains instead of a complex, undefined community.2. Standardize donor screening and sample processing protocols.3. Co-administer prebiotics (synbiotics) to support engraftment of beneficial strains [92]. | Bank and quality-control a single, well-characterized donor sample for an entire study series. |
| Failure of probiotic strains to colonize the gut. | Host immune clearance or competition with resident microbiota. | 1. Pre-condition the host with a brief antibiotic regimen to create a niche (in animal models).2. Use engineered strains with adherence factors.3. Utilize targeted delivery systems (e.g., acid-resistant capsules) [92]. | Select probiotic strains with known adherence capabilities and test in vitro for mucin binding. |
| Unexpected inflammatory response post-treatment. | Presence of pathobionts in the donor material or immune reactivity to new antigens. | 1. Re-screen donor material for a broader range of pathogens and immune markers.2. Use a filtered microbial preparation that removes live bacteria but retains active molecules (postbiotics) [92]. | Implement rigorous donor screening that includes metagenomic sequencing and immunoassays. |
Experimental Protocols for Key Assays
Protocol 1: Assessing Resistance Development Potential
Aim: To evaluate the frequency with which bacteria develop resistance to a novel therapeutic compared to a conventional antibiotic.
Methodology:
- Serial Passage Assay: Inoculate a high-density bacterial culture (e.g., ~10^9 CFU/mL) in the presence of a sub-lethal concentration (e.g., 0.5x MIC) of the test compound (novel therapeutic) and a control antibiotic.
- Daily Passage: Incubate for 24 hours, then transfer a sample of the culture into fresh medium containing the same or a slightly increased concentration of the compound. Repeat for 20-30 passages.
- MIC Determination: Every 5 passages, determine the Minimum Inhibitory Concentration (MIC) for the passaged populations and a naive, unpassaged control strain using broth microdilution according to CLSI guidelines.
- Analysis: Plot the fold-change in MIC over time. A slow, gradual increase suggests a low potential for resistance, while a sharp, rapid increase indicates a high risk.
Diagram: Resistance Development Workflow
Protocol 2: Evaluating Host Cell Cytotoxicity
Aim: To determine the selectivity index (SI) of a novel therapeutic by comparing its toxicity to mammalian cells against its antimicrobial activity.
Methodology:
- Cell Culture: Maintain relevant mammalian cell lines (e.g., HEK 293, THP-1, or primary fibroblasts) in appropriate media.
- Cytotoxicity Assay: Seed cells in a 96-well plate. After adherence, treat with a serial dilution of the novel therapeutic. Incubate for 24-48 hours. Include a vehicle control (0% toxicity) and a lysis buffer (100% toxicity).
- Viability Measurement: Use a standard cell viability assay like MTT or AlamarBlue. Measure absorbance/fluorescence and calculate the percentage of cell viability.
- Data Calculation:
- Calculate the 50% cytotoxic concentration (CCâ‚…â‚€), the concentration that reduces cell viability by 50%.
- Determine the Minimum Inhibitory Concentration (MIC) against the target pathogen.
- Compute the Selectivity Index (SI) = CCâ‚…â‚€ / MIC. An SI > 10 is generally considered to indicate a promising, selective compound.
Diagram: Cytotoxicity & Selectivity Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Investigating Novel Anti-infective Modalities
| Item | Function | Example Application |
|---|---|---|
| Caco-2/HEK 293 Cell Lines | Models for in vitro assessment of host cell cytotoxicity and epithelial barrier integrity. | Determining the Selectivity Index (SI) for Antimicrobial Peptides (AMPs) [92]. |
| Standard Animal Models | In vivo evaluation of efficacy, pharmacokinetics, and preliminary safety. | Mouse thigh infection or neutropenic lung infection models for testing novel antibiotics and phage therapy efficacy [79]. |
| Biofilm Assay Kits | Quantifying the ability of therapeutics to prevent or disrupt bacterial biofilms. | Testing the anti-biofilm activity of nanoparticles or enzymes (lysins) [92]. |
| Matched Isogenic Strain Pairs | Comparing drug activity against wild-type vs. specific resistance mutant strains. | Elucidating the mechanism of action and assessing potential for cross-resistance [79]. |
| Human Feces Microbiota | Sourcing complex microbial communities for ex vivo or in vivo microbiome studies. | Evaluating the impact of novel therapies on commensal microbiota and for FMT research [92]. |
| Automated Liquid Handlers & AI Software | Enabling high-throughput screening and advanced data analysis for hit identification and optimization. | Supercharging the discovery of new antibiotics; GSK/Fleming Initiative uses AI/ML models to design drugs for multi-drug-resistant Gram-negative infections [93] [94]. |
Bench to Bedside: Validation Frameworks and Comparative Effectiveness Analysis
FAQs: Navigating Preclinical Models for Antibiotic Therapy Development
What are the main limitations of traditional preclinical models in antimicrobial research?
Traditional models have significant drawbacks in predicting human outcomes. Two-dimensional (2D) cell cultures lack the physiological complexity of human tissues, with fewer than 10% of leads from these in vitro studies progressing to successful clinical trials [95]. Animal models face fundamental anatomical, metabolic, and immunological disparities that cause poor translation; for example, over 90% of drugs fail in clinical stages due to unforeseen toxicity or lack of efficacy that animal testing did not predict [95] [96]. Additionally, a study attempting to confirm 53 "landmark" preclinical studies succeeded in only 6 cases [97].
Which advanced in vitro models can better predict human-specific antibiotic responses?
Complex In Vitro Models (CIVMs) better mimic human physiology. Key types are in the table below [96]:
| Model Type | Key Features | Applications in Antibiotic Research |
|---|---|---|
| Static Models (e.g., 3D organoids, spheroids) | 3D cell structures; more realistic cell-to-cell interaction than 2D cultures [95]. | Disease modeling (e.g., bacterial infection in biofilms); initial efficacy screening [98]. |
| Static Microphysiological Systems (MPS) | Incorporate advanced sensors but lack dynamic fluid flow [96]. | High-throughput screening of compound libraries [98]. |
| Dynamic MPS (e.g., Organ-Chips) | Replicate functional human organ units with dynamic fluid flow and mechanical forces [95] [96]. | Study drug metabolism, tissue-specific toxicity, and human-specific immune responses to antibiotics [96]. |
For instance, a human Liver-Chip model correctly identified 87% of drugs that cause drug-induced liver injury (DILI) in humans, despite having passed animal testing [96].
How can I address the reproducibility crisis in my preclinical experiments?
The "reproducibility crisis" in biomedical research stems from factors like selective reporting, low statistical power, and poor experimental design [97]. To enhance reproducibility:
- Pre-specify Data Analysis Plans: Define your data analysis strategy before conducting experiments to decrease selective reporting [97].
- Implement Rigorous Data Management: Maintain an auditable record of original raw data, all data management programs, and the final analysis files. Avoid non-auditable methods like cutting and pasting from Excel [97].
- Use Detailed Experimental Protocols: Write protocols that are so detailed a trustworthy colleague from another lab could run the experiment correctly from the script alone. The checklist below provides essential data elements for a reproducible protocol [99] [100].
The table below lists essential reagents and materials for establishing advanced preclinical models:
| Research Reagent / Material | Function in Preclinical Validation |
|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Source for deriving patient-specific human tissues (e.g., hepatocytes, immune cells) for disease modeling [98]. |
| Organ-Chips (e.g., Gut-Liver-Chip) | Microfluidic devices that simulate inter-organ crosstalk (e.g., gut absorption followed by liver metabolism) to study antibiotic absorption and toxicity [98]. |
| Extracellular Matrix (ECM) Hydrogels | Provide a 3D, physiologically relevant scaffold to support complex tissue architecture and cell function in 3D cultures and MPS [95] [98]. |
| Humanized Mouse Models (e.g., FcRn) | Provide an in vivo model with humanized drug metabolism pathways (e.g., for Fc-based biologics) to better predict human pharmacokinetics (PK) [101]. |
| Bacterial Resistance Gene Reporters | Genetically engineered systems to monitor the activation of bacterial resistance pathways (e.g., WhiB7 "resistome") in real-time during antibiotic treatment [12]. |
Troubleshooting Common Experimental Issues
Problem: Inconsistent Results in Animal Models of Infection
Potential Causes and Solutions:
Cause 1: Species-Specific Differences in Immune Response.
- Solution: Incorporate "humanized" mouse models that carry human genes, cells, or tissues. For example, FcRn humanized models are validated for assessing the pharmacokinetics of therapeutic antibodies, providing more clinically relevant data [101]. For infectious disease research, models with human immune components can better simulate the human response to pathogens [98].
Cause 2: Underpowered Studies and Uncontrolled Variables.
- Solution: Implement rigorous experimental protocols. A detailed protocol should cover all aspects of the experiment [99]:
- Setting up: Specific computer settings, equipment checks, and workspace arrangement.
- Animal handling: Standardized procedures for greeting, consent (if applicable), and acclimation.
- Monitoring: Clear guidelines for researcher behavior during data collection and criteria for intervention.
- Data saving and breakdown: Precise steps for data recording, storage, and lab shutdown.
- Solution: Implement rigorous experimental protocols. A detailed protocol should cover all aspects of the experiment [99]:
Problem: Poor Translation from In Vitro Killing to In Vivo Efficacy
Potential Causes and Solutions:
- Cause: Standard 2D Cultures Do Not Replicate the In Vivo Microenvironment.
- Solution: Transition to 3D co-culture systems or Organ-Chips. These models can incorporate multiple cell types (e.g., epithelial cells and immune cells) and physiological fluid flow, creating a more realistic environment for studying antibiotic penetration and efficacy against biofilms [95] [96]. A proof-of-concept study successfully used a gut-liver-on-a-chip to model the first-pass metabolism of orally administered drugs, a key factor in antibiotic bioavailability [98].
Problem: My Antibiotic Candidate is Effective but Causes High Toxicity
Potential Causes and Solutions:
- Cause: Failure to Predict Human-Specific Toxicity (e.g., DILI).
- Solution: Integrate human-specific Organ-Chip toxicology data into your preclinical package. For example, before advancing to non-human primate (NHP) studies, you can screen candidates for liver toxicity using a human Liver-Chip. One group screened 35 novel lipid nanoparticles this way over 18 months for $325,000, a process that would have cost over $5,000,000 and taken over 60 months using NHP studies [96].
Detailed Experimental Protocols
Protocol 1: Reporting a Reproducible Experimental Protocol
To ensure your experiments can be replicated by your team and the broader scientific community, use this checklist of essential data elements when writing your methods [100]:
- Objective: A clear statement of the protocol's purpose.
- Hypothesis: The specific hypothesis the experiment is designed to test.
- Biosafety Level: The required biosafety level for the experiment.
- Expertise: Necessary skills and training for personnel.
- Duration & Scheduling: Timeline for setup, execution, and breakdown.
- Input Materials & Reagents: A complete list of materials, including source, catalog numbers, and unique identifiers (RRIDs) where available.
- Input Equipment & Instruments: A complete list of equipment, including manufacturer and model.
- Workflow Steps: Sequential, detailed steps of the procedure.
- Parameters & Conditions: Specific settings, concentrations, temperatures, and time points.
- Hints & Troubleshooting: A section addressing common problems and their solutions.
- Output Data & Results: A description of the expected raw data and results.
- Analysis: The planned methods for data analysis.
- Validation: The method for validating the protocol and its results.
Protocol 2: A Workflow for Integrating Advanced Preclinical Models
The following diagram outlines a strategic workflow for leveraging advanced models in antibiotic development, from initial screening to regulatory submission.
Protocol 3: Exploiting Bacterial Resistance Mechanisms
A novel strategy to combat antibiotic resistance involves "hacking" the bacterium's own defense systems. The study below demonstrates how a prodrug can be designed to be activated by a bacterial resistance protein, creating a lethal feedback loop [12].
Quantitative Data: The Scale of Antimicrobial Resistance (AMR)
To underscore the critical need for robust preclinical models in antibiotic development, the table below summarizes key global surveillance data on resistance rates. This highlights the specific pathogens and drugs that require urgent attention [2].
| Bacterial Pathogen | Antibiotic Class | Global Resistance Prevalence (%) | Key Regional Concern |
|---|---|---|---|
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% | Global threat, >70% resistance in African Region [2]. |
| Escherichia coli | Third-generation cephalosporins | >40% | Leading cause of resistant bloodstream infections [2]. |
| Various Gram-negative bacteria (E. coli, K. pneumoniae, Salmonella, Acinetobacter) | Carbapenems (last-resort) | Rising rapidly | Carbapenem resistance, once rare, is becoming more frequent [2]. |
| All reported bacterial infections | Various (aggregate) | 1 in 6 (17%) | Highest in South-East Asia & Eastern Mediterranean (1 in 3) [2]. |
FAQs and Troubleshooting Guides
FAQ: Novel Therapeutic Strategies
Q1: What novel antibiotic strategies can help prevent resistance development? Several novel strategies show promise in preventing antibiotic resistance. Immuno-antibiotics represent a new class that interacts with host immunity, leading to potent indirect effects that improve antibacterial activities and can result in more swift and complete bactericidal effects [102]. Other emerging approaches include:
- Inhibition of bacterial SOS response: This targeting of biochemical resistance pathway components can combat antibiotic resistance in bacteria [102].
- Bacteriophage Therapy: Researchers are developing methods using "trained" bacteriophages (viruses that infect bacteria) that have evolved in laboratory settings to enhance their ability to kill a wide variety of bacterial strains, including multidrug-resistant pathogens [24].
- Long-acting antimicrobial formulations: Novel agents like lipoglycopeptides (e.g., dalbavancin, oritavancin) exhibit prolonged half-lives and sustained drug exposure, enabling shorter overall treatment durations and reducing selective pressure for resistance [103].
Q2: How do the pharmacokinetic properties of novel antibiotics support shorter therapy durations? Novel antibiotics with distinct pharmacokinetic (PK) and pharmacodynamic (PD) profiles challenge traditional, prolonged treatment paradigms [103]. The table below summarizes the key PK/PD characteristics that enable this shift.
| Antimicrobial Class | Example Agents | Key PK/PD Characteristics | Impact on Therapy Duration |
|---|---|---|---|
| Lipoglycopeptides [103] | Dalbavancin, Oritavancin | Long half-life (>7 days), sustained drug exposure, high tissue penetration | Enables single-dose or infrequent dosing, reducing treatment duration [103] |
| Novel Cephalosporins [103] | Ceftolozane-Tazobactam, Cefiderocol | Enhanced activity against MDR organisms, high tissue concentrations | May allow shorter therapy for MDR infections [103] |
| Long-Acting Aminoglycosides [103] | Liposomal Amikacin, Plazomicin | Improved intracellular penetration, prolonged drug release | Higher AUC/MIC ratios enable reduced dosing frequency [103] |
| Beta-Lactam/Beta-Lactamase Inhibitors [103] | Meropenem-Vaborbactam | Broad-spectrum activity against carbapenem-resistant pathogens | Potential to shorten therapy for multidrug-resistant infections [103] |
Q3: What are the primary pharmacodynamic indices used to optimize novel antibiotic therapies? Optimizing novel antibiotics relies on understanding key pharmacodynamic indices that predict efficacy and guide dosing. The following table outlines the critical indices.
| Pharmacodynamic Index | Definition | Clinical Implication for Novel Agents |
|---|---|---|
| T > MIC [103] | Duration drug concentration remains above the Minimum Inhibitory Concentration (MIC) | Higher values correlate with improved bacterial eradication for time-dependent antibiotics (e.g., beta-lactams) [103]. |
| AUC/MIC [103] | Ratio of the Area Under the concentration-time curve to the MIC | Critical for concentration-dependent antibiotics (e.g., aminoglycosides); optimizing this ratio allows for extended dosing intervals [103]. |
| Post-Antibiotic Effect (PAE) [103] | Persistent suppression of bacterial growth after antibiotic exposure | A longer PAE allows for extended dosing intervals and can support shorter overall treatment courses [103]. |
Troubleshooting Guide: Addressing Challenges in Novel Therapy Research
Problem: No bactericidal activity detected for a novel antimicrobial peptide (AMP) in vitro. This is a common issue in early-stage antimicrobial research. Follow this systematic troubleshooting guide to identify the cause.
Step-by-Step Diagnosis and Solution:
Identify the Problem: The assay shows no reduction in bacterial viability after exposure to the novel AMP. Confirm the result with a viability stain (e.g., propidium iodide) in addition to measuring optical density.
List Possible Explanations:
- Experimental Conditions: Incorrect buffer pH or salt concentration affecting AMP charge and interaction; use of growth media that inhibit AMP activity (e.g., high serum content).
- AMP Integrity: Peptide degradation due to improper storage or handling; peptide aggregation leading to reduced active monomer concentration; inaccurate concentration calculation.
- Bacterial Strain: The test strain is inherently resistant to the AMP; the bacterial inoculum was not viable or at the wrong growth phase (e.g., stationary phase).
- Measurement System: Malfunctioning spectrophotometer or plate reader; incorrect loading of viability dyes.
Collect Data & Eliminate Explanations:
- Controls: Run a positive control with a known bactericidal AMP and a negative control (buffer only). If the positive control works, it validates your experimental system.
- AMP Analysis: Characterize the AMP using mass spectrometry or HPLC to check for degradation and confirm identity. Repeat the concentration measurement.
- Strain Verification: Test the AMP on a standard, susceptible control strain (e.g., from the ATCC). Check the inoculum density using colony-forming unit (CFU) plating.
- Equipment Check: Calibrate instruments and confirm the measurement protocol with a known standard.
Check with Experimentation:
- Test the AMP in a different, standardized buffer (e.g., low-salt, neutral pH).
- Perform a time-kill assay with CFU plating, which is more definitive than optical density for assessing bactericidal activity.
- Use a fluorescence-based viability assay to cross-verify results.
Identify the Cause: Based on the experiments, pinpoint the specific issue. For instance, if activity is restored in a different buffer, the original buffer composition was the cause. If the AMP is degraded, synthesize a new batch with proper storage.
Problem: Evolved bacteriophages show reduced host range than expected. Troubleshooting Workflow:
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their functions for researching novel anti-resistance strategies, drawing on current methodologies.
| Research Reagent / Material | Function in Experimentation |
|---|---|
| Long-acting Lipoglycopeptides (e.g., Dalbavancin) [103] | Used in PK/PD studies to model sustained drug exposure and evaluate the feasibility of abbreviated treatment courses for complex infections like osteomyelitis [103]. |
| Trained/Bacteriophages [24] | Employed in phage therapy research to target and kill multidrug-resistant bacterial strains (e.g., Klebsiella pneumoniae); these are evolved in the lab to expand host range [24]. |
| Machine Learning-Identified Antimicrobial Peptides (AMPs) [104] | Serve as novel candidate therapeutic agents screened computationally for potent activity against multidrug-resistant (MDR) ESKAPE pathogens and biofilms [104]. |
| Beta-lactamase Inhibitor Combinations (e.g., Avibactam, Vaborbactam) [103] | Used in resistance mechanism studies to restore the efficacy of beta-lactam antibiotics against pathogens producing extended-spectrum and carbapenem-resistant beta-lactamases [103]. |
| SOS Response Inhibitors (e.g., potential small molecules) [102] | Utilized in biochemical assays to investigate and block bacterial stress response pathways, a emerging strategy to combat the evolution of antibiotic resistance [102]. |
Antimicrobial resistance (AMR) poses a critical threat to global health, causing an estimated 2.8 million illnesses and 35,000 deaths annually in the United States alone [91]. This technical support center provides researchers and drug development professionals with practical resources for evaluating novel therapeutic approaches that combat resistant pathogens. The following guides, protocols, and data summaries focus on two promising strategies: targeted bacteriocins and resistance-exploiting prodrugs, providing a framework for comparing their efficacy against conventional antibiotics.
Table 1: Comparative Efficacy of Traditional vs. Novel Antimicrobial Approaches
| Therapeutic Approach | Target Pathogen | Efficacy Metric | Impact on Microbiota | Research Model |
|---|---|---|---|---|
| Traditional Antibiotic (Ciprofloxacin) | Klebsiella pneumoniae | Equivalent pathogen reduction to KvarM [105] | Significant decrease in microbial diversity [105] | Murine intestinal model [105] |
| Bacteriocin KvarM | Klebsiella pneumoniae | 99% reduction in bacterial load [105] | No significant changes in microbial composition [105] | Murine intestinal model [105] |
| Modified Florfenicol Prodrug | Mycobacterium abscessus | Exploits bacterial resistance mechanisms for perpetual effect [12] | Minimizes microbiome disruption [12] | In vitro bacterial culture [12] |
| Ciprofloxacin (for UTI) | E. coli | Resistance rates: 8.4% to 92.9% across regions [106] | N/A (broad-spectrum) | Clinical isolates [106] |
| Ciprofloxacin (for UTI) | K. pneumoniae | Resistance rates: 4.1% to 79.4% across regions [106] | N/A (broad-spectrum) | Clinical isolates [106] |
| Third-generation Cephalosporins | E. coli (bloodstream) | >40% global resistance [2] | N/A (broad-spectrum) | Clinical isolates [2] |
| Third-generation Cephalosporins | K. pneumoniae (bloodstream) | >55% global resistance [2] | N/A (broad-spectrum) | Clinical isolates [2] |
Table 2: Global Antibiotic Resistance Trends (WHO GLASS Report 2025)
| Pathogen | Antibiotic Class | Global Resistance Prevalence | Regional Variation |
|---|---|---|---|
| E. coli | Third-generation cephalosporins | >40% [2] | Highest in African Region (>70%) [2] |
| K. pneumoniae | Third-generation cephalosporins | >55% [2] | Highest in African Region (>70%) [2] |
| Multiple bacterial pathogens | Multiple classes | 1 in 6 infections resistant globally [2] | 1 in 3 resistant in SE Asian & Eastern Mediterranean Regions [2] |
Experimental Protocols
Protocol 1: Evaluating Bacteriocin Efficacy in Murine Intestinal Models
Application: Testing targeted antimicrobials against Gram-negative pathogens in the gastrointestinal tract [105].
Materials:
- C57BL/6J mice (8-10 weeks old)
- Klebsiella pneumoniae subsp. pneumoniae 43816 (ATCC)
- LB nutrient medium with ampicillin (25 μg/mL)
- Purified bacteriocin (e.g., KvarM)
- Eudragit L100 and S100 polymers (Evonik Industries)
- 50 mM Phosphate buffer
- 2M NaOH and 2M HCl solutions
Methodology:
- Bacteriocin Formulation:
- Prepare 5% Eudragit L100 solution: Dissolve 100 mg in 2 mL phosphate buffer, adjust to pH 6-7 with NaOH
- Prepare 5% Eudragit S100 solution: Dissolve 100 mg in 2 mL phosphate buffer, adjust to pH 8 with NaOH
- Mix 0.25 mg lyophilized KvarM with 250 μL of each Eudragit solution
- Acidify mixtures to pH 4-5 with HCl to induce Eudragit polymerization
- Lyophilize coated KvarM and reconstitute in dHâ‚‚O before administration [105]
Infection Model:
- Culture K. pneumoniae in LB medium with ampicillin
- Inoculate mice on two consecutive days to establish intestinal colonization [105]
Treatment Groups:
- Positive control: Infected, no treatment
- Vehicle control: Infected, Eudragit only
- Experimental: Infected, Eudragit-coated KvarM
- Antibiotic control: Infected, ciprofloxacin [105]
Analysis:
- Assess bacterial load reduction using selective media
- Perform 16S rRNA gene sequencing of V1-V2 hypervariable region to evaluate microbiota impact [105]
Protocol 2: Assessing Resistance-Exploiting Prodrug Mechanisms
Application: Investigating antibiotics that hijack bacterial resistance pathways for enhanced efficacy [12].
Materials:
- Mycobacterium abscessus strains (wild-type and WhiB7 knockout)
- Modified florfenicol prodrug
- Standard bacterial culture media
- Equipment for RNA and protein analysis
Methodology:
- Strain Validation:
- Confirm WhiB7 "resistome" activation in wild-type M. abscessus
- Verify WhiB7 knockout strain lacks resistome response [12]
Prodrug Susceptibility Testing:
- Compare prodrug efficacy against wild-type vs. WhiB7 knockout strains
- Use standard MIC determination methods [12]
Mechanism Elucidation:
- Monitor Eis2 protein induction following WhiB7 activation
- Quantify conversion of prodrug to active form in both strains
- Assess ribosomal inhibition and subsequent WhiB7 activation [12]
Toxicity Assessment:
- Compare mitochondrial toxicity of prodrug vs. conventional phenicols
- Evaluate microbiome impact using diversity metrics [12]
Frequently Asked Questions (FAQs)
Q: What are the key advantages of bacteriocins like KvarM over traditional antibiotics? A: Bacteriocins offer targeted activity against specific bacterial species, typically without disrupting commensal microbiota. In murine models, KvarM achieved 99% reduction in K. pneumoniae load while preserving gut microbial diversity, whereas ciprofloxacin significantly reduced diversity [105].
Q: How do resistance-exploiting approaches differ from traditional antibiotics? A: Rather than avoiding resistance mechanisms, these approaches hijack them. The modified florfenicol prodrug is activated by Eis2, a resistance protein induced by WhiB7. This creates a perpetual cascade where antibiotic activation amplifies itself, effectively turning resistance against the bacterium [12].
Q: When should oral versus intravenous antibiotic administration be considered in research models? A: For stable subjects, oral antibiotics show equivalent efficacy to IV for many infections including pneumonia, bacteremia, and skin infections. Oral administration improves patient experience, reduces healthcare costs, and generates a lower carbon footprint. Reserve IV therapy for critically ill subjects or when oral administration isn't feasible [107].
Q: What factors contribute to the development of antibiotic resistance? A: Resistance develops through natural selection when bacteria are exposed to antibiotics. Key factors include excessive and inappropriate antibiotic use in healthcare and agriculture, inadequate treatment duration, and transmission of resistant strains in healthcare settings [91] [10].
Q: How can researchers accurately detect antibiotic-resistant bacteria? A: Traditional culture-based methods (disk diffusion, broth microdilution) remain foundational. Molecular techniques can rapidly identify resistance mechanisms. Emerging technologies include CRISPR/Cas-based systems, biosensors, and aptamer-based detection, which offer faster turnaround times for susceptibility testing [106].
Troubleshooting Guides
Problem: Inconsistent Bacteriocin Efficacy in GI Models
Potential Cause: Degradation of bacteriocin in the harsh GI environment before reaching the target site. Solution: Utilize pH-dependent coating strategies with Eudragit polymers. Eudragit L100 dissolves above pH 5.5 (small intestine), while S100 dissolves in alkaline environments (large intestine), protecting the bacteriocin until it reaches the target region [105].
Problem: Resistance Development During Therapy Studies
Potential Cause: Inappropriate antibiotic selection or dosing regimens. Solution:
- Implement antibiotic stewardship principles: use narrow-spectrum agents when possible
- Ensure adequate dosing duration and concentration
- Consider combination therapies for persistent infections
- Utilize rapid diagnostics to guide targeted treatment [91] [108]
Problem: Unexpected Toxicity in Novel Antimicrobial Testing
Potential Cause: Off-target effects on host mitochondria or beneficial microbiota. Solution:
- Explore prodrug approaches that minimize host toxicity, like modified florfenicol which avoids mitochondrial damage [12]
- Assess microbiome impact using 16S rRNA sequencing
- Include appropriate toxicity controls in study design
Problem: Poor Bioavailability of Oral Antibiotics in Animal Models
Potential Cause: Impaired absorption during acute infection phase. Solution: Note that research shows febrile subjects who are not critically ill do not have impaired absorption of oral antibiotics. The inflammatory response does not reduce total antibiotic exposure (AUC). Consider that vomiting, not systemic illness, may necessitate parenteral administration [107].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Antimicrobial Resistance Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Eudragit L100/S100 | pH-dependent polymer coating for targeted GI delivery | Protecting bacteriocins from degradation until reaching target intestinal regions [105] |
| Modified Florfenicol Prodrug | Resistance-exploiting antimicrobial | Hijacking bacterial WhiB7 resistome for perpetual antibiotic activation [12] |
| 16S rRNA Gene Sequencing Reagents | Microbiome composition analysis | Evaluating impact of antimicrobials on commensal microbiota [105] |
| WhiB7 Knockout Strains | Control for resistance mechanism studies | Verifying specificity of resistance-exploiting compounds [12] |
| Ciprofloxacin Reference Standard | Broad-spectrum antibiotic control | Comparing novel agents against conventional therapy [105] |
Experimental Workflows and Mechanisms
Bacteriocin KvarM Experimental Workflow
Resistance-Hacking Mechanism
Troubleshooting Guides
Guide 1: Addressing Data Inconsistencies in GLASS Reporting
Problem: Submitted surveillance data is flagged for inconsistencies or incompleteness by the GLASS IT Platform.
- Step 1: Verify data against GLASS case definitions. Confirm that all reported cases are from bacteriologically confirmed infections and that pathogen-antibiotic combinations are among the 93 tracked combinations [1].
- Step 2: Utilize WHONET software to re-analyze and validate laboratory data. This free WHO-supported application standardizes microbiology data analysis and is used in over 130 countries to ensure data comparability [109].
- Step 3: Check your national data against the GLASS dashboard's "completeness of national data" scoring framework to identify and rectify common gaps in reporting [1].
Problem: Inability to generate reliable national AMR estimates from collected data.
- Step 1: Assess laboratory capacity using WHO GLASS strengthening tools. Nearly half of reporting countries faced similar challenges in 2023 [110] [2].
- Step 2: Implement the GLASS-supported methodology for moving from laboratory-based data to a system that includes epidemiological and clinical data to improve representativeness [109].
- Step 3: Partner with WHO Collaborating Centres for external quality assurance and quality management of AMR testing procedures [109].
Guide 2: Overcoming Technical Barriers in Surveillance System Implementation
Problem: Establishing or expanding national AMR surveillance systems, particularly in resource-limited settings.
- Step 1: Leverage the stepwise approach outlined in the GLASS framework, which supports capacity building and monitors the status of both existing and new surveillance systems [109].
- Step 2: Engage with regional AMR surveillance networks (e.g., ReLAVRA in Latin America, CAESAR in Europe and Central Asia) for technical support and regional data harmonization [109] [110].
- Step 3: Utilize the GLASS IT Platform, which serves as a common environment for data submission and supports implementation of One Health AMR surveillance at the national level [109].
Frequently Asked Questions (FAQs)
Q1: What are the most critical pathogen-antibiotic combinations to monitor in therapy research? Based on 2023 GLASS data from 104 countries, the most urgent threats involve Gram-negative bacteria, particularly E. coli and K. pneumoniae [110] [2]. The table below summarizes critical combinations for research prioritization.
Table: Critical Pathogen-Antibiotic Resistance Patterns for Research Focus
| Pathogen | Antibiotic Class | Resistance Rate | Regional Variation |
|---|---|---|---|
| Escherichia coli | Third-generation cephalosporins | >40% globally | Exceeds 70% in African Region [110] [2] |
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% globally | Exceeds 70% in African Region [110] [2] |
| Klebsiella pneumoniae | Carbapenems | Increasing (once rare) | Narrowing treatment options worldwide [110] [2] |
| Acinetobacter spp. | Carbapenems | Rising | Major concern in healthcare settings [110] |
| Neisseria gonorrhoeae | Extended-spectrum cephalosporins | Tracked in GLASS | Compromising STI treatment [1] |
Q2: How can researchers ensure their AMR data is comparable to GLASS global estimates? Adhere to the standardized GLASS methodology for the collection, analysis, and interpretation of data [109]. This includes:
- Using WHONET software for data management and analysis [109].
- Reporting data on the eight common bacterial pathogens and 22 antibiotics covered in the GLASS 2025 report [1] [2].
- Participating in external quality assurance programs offered by WHO Collaborating Centres for AMR surveillance [109].
Q3: What is the current global trajectory of AMR, and how should this influence research directions? Between 2018 and 2023, antibiotic resistance rose in over 40% of monitored pathogen-antibiotic combinations, with an average annual increase of 5-15% [110] [2]. This persistent rise underscores the urgent need for research into:
- Novel antimicrobial agents: The development pipeline for new antibiotics remains limited, with few new classes discovered since the 1980s [111].
- Rapid diagnostic tools: To enable targeted therapy and reduce unnecessary antibiotic use [2].
- Alternative therapies: Including vaccines and non-antibiotic treatments to prevent and manage bacterial infections [112].
Experimental Protocols for AMR Surveillance and Intervention Testing
Protocol 1: National AMR Surveillance Baseline Assessment
Objective: To establish a national baseline of AMR prevalence for key pathogen-antibiotic combinations.
- Methodology:
- Case Ascertainment: Collect data from a nationally representative sample of laboratories on bacteriologically confirmed cases of bloodstream infections, urinary tract infections, gastrointestinal infections, and urogenital gonorrhoea [1].
- Laboratory Testing: Perform antimicrobial susceptibility testing (AST) for the 22 antibiotics specified in the GLASS report. Standardize AST methods according to WHO recommendations [1] [109].
- Data Analysis: Calculate resistance proportions for each pathogen-antibiotic combination. Analyze trends over time where data is available (2018-2023) [1].
- Data Validation: Use the GLASS scoring framework to assess data completeness and representativeness. Submit validated data to the GLASS IT Platform [1] [109].
Protocol 2: Evaluating the Impact of a Stewardship Intervention
Objective: To measure the effect of a hospital-based antibiotic stewardship program on resistance rates.
- Methodology:
- Design: Implement a pre-post intervention study design in a healthcare network.
- Intervention: Introduce an antibiotic stewardship program including prescriber education, guidelines based on local AMR patterns, and audit with feedback [112] [108].
- Data Collection: Pre- and post-intervention, collect data on antibiotic consumption (Defined Daily Doses) and resistance rates in key pathogen-antibiotic combinations (e.g., third-generation cephalosporin-resistant E. coli) [109].
- Analysis: Use statistical process control charts to detect significant changes in resistance rates following intervention implementation. Compare your findings to regional trends reported in GLASS [110].
Surveillance System Workflow and Data Integration
One Health AMR Context
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for AMR Surveillance and Intervention Research
| Resource / Tool | Function / Application | Source / Reference |
|---|---|---|
| WHONET Software | Free software for management and analysis of microbiology laboratory data; supports standardized AMR surveillance in over 130 countries. | WHO Collaborating Centre [109] |
| GLASS IT Platform | Web-based platform for global data sharing on AMR; serves as common environment for data submission for several technical modules. | World Health Organization [109] |
| External Quality Assurance (EQA) Programs | Programs to ensure quality and reliability of antimicrobial susceptibility testing (AST) results in national reference laboratories. | WHO Collaborating Centres [109] |
| GLASS Manual & Guidelines | Provide standardized protocols for case definitions, data collection, analysis, and interpretation to ensure global data comparability. | World Health Organization [1] [109] |
| One Health Surveillance Frameworks | Integrated approaches and tools for surveillance coordinating across human health, animal health, and environmental sectors. | UNGA Political Declaration 2024 [110] [2] |
FAQs: Regulatory and Development Pathways
Q1: What regulatory designations can accelerate the development of new antibacterial therapies? The U.S. Food and Drug Administration (FDA) offers several designations to expedite the development and review of drugs for serious conditions [113].
- Fast Track: Facilitates development and expedites review of drugs to treat serious conditions and fill an unmet medical need [113].
- Breakthrough Therapy: Expedites development and review for drugs where preliminary clinical evidence indicates substantial improvement over available therapy [113].
- Priority Review: Designates that the FDA aims to take action on a drug application within six months, compared to the standard ten months [113].
- Accelerated Approval: Allows approval based on a surrogate endpoint that is reasonably likely to predict clinical benefit, requiring post-marketing trials to verify the benefit [113].
Q2: How is the regulatory landscape adapting to non-traditional antimicrobials, like phage therapy? Regulatory agencies are beginning to create new pathways for adaptive therapies. A key example is France's authorization of a personalized phage therapy platform for veterinary use [114]. Unlike approving a single, fixed formulation, this platform approach establishes a validated framework for producing tailored phage combinations. This allows the medicine to evolve as bacteria develop resistance, without requiring a new, lengthy approval process for each modification [114]. This model is a pioneering step for regulating living, evolving medicines.
Q3: What are the key elements of an Expanded Access Policy required for investigational drugs? The 21st Century Cures Act requires manufacturers to publicly post their expanded access policies [115]. These policies must include [115]:
- Contact information for the sponsor or representative.
- Procedures for requesting access.
- The general criteria the sponsor uses to evaluate requests.
- The expected time for acknowledging receipt of requests.
- A link to the clinical trial record on ClinicalTrials.gov.
Q4: What are the major economic challenges in developing new antibiotics? The traditional economic model for drug development is failing for antibiotics [79]. Key challenges include:
- Low Financial Return: The direct net present value of a new antibiotic is close to zero, making it an unattractive investment compared to drugs for chronic conditions [79].
- High Development Costs: The mean cost to develop a systemic anti-infective is approximately $1.3 billion, similar to other drug classes [79].
- Low Sales Volume: To preserve efficacy, new antibiotics must be used sparingly. Most new antibiotics generate only $15-$50 million in annual U.S. sales, far less than the estimated $300 million needed to be sustainable [79].
Troubleshooting Guides: Overcoming Research and Development Hurdles
Challenge: Clinical Trial Design for Antibacterial Agents
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| Difficulty enrolling enough patients for a superiority trial. | The target drug-resistant infection is too rare. | Design a non-inferiority trial to demonstrate the new drug is not unacceptably worse than the current standard of care [79]. |
| Trial costs become prohibitively high. | Need to screen thousands of patients to find a few with the specific resistant infection. | Explore innovative trial designs and leverage collaborative networks. Note: One trial spent an estimated $1 million per recruited patient [79]. |
| Resistance emerges during a clinical trial. | Rapid bacterial evolution under selective pressure. | Implement stringent stewardship within the trial protocol and consider combination therapies to reduce the emergence of resistance [79]. |
Challenge: Implementing an Effective Antimicrobial Stewardship Program (AMS)
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| High use of extended-spectrum antibiotics despite low incidence of resistant infections. | Diagnostic uncertainty and lack of patient-specific risk information at the point of care. | Implement automated clinical decision support. The INSPIRE trials used computerized prompts providing patient-specific risk data, reducing unnecessary extended-spectrum antibiotic use by 28-35% [116]. |
| Failure to meet national AMS standards for hospital formulary access to new antimicrobials. | Lack of a functional AMS committee, inadequate diagnostic capacity, or failure to report AMR surveillance data. | Develop a documented AMS and Infection Prevention and Control (IPC) program. Hospitals should have a functional AMS committee, in-house pharmacy, clinical pharmacist, and diagnostic capacity, and must commit to reporting AMR data to national surveillance platforms [117]. |
Quantitative Data on Antimicrobial Resistance
Table 1: Documented Resistance Rates in Key Bacterial Pathogens (India, 2023)
Data from the Indian Council of Medical Research (ICMR) surveillance network highlights the critical nature of the AMR threat [117].
| Pathogen | Antibiotic | Resistance Rate | Notes |
|---|---|---|---|
| Klebsiella pneumoniae | Carbapenem (Meropenem) | 62.3% | Significantly limits treatment options [117]. |
| Escherichia coli | Imipenem | 37% (Declined from 81% in 2017) | Shows a disturbing trend of increasing resistance [117]. |
| Escherichia coli | Piperacillin-tazobactam | 57.6% (Declined from 43.2% in 2017) | Sensitivity has dropped significantly [117]. |
| Klebsiella pneumoniae | Piperacillin-tazobactam | 73.5% | Very low susceptibility to a key antibiotic [117]. |
| Escherichia coli | Ceftazidime-avibactam | 37.6% | Newer drug facing rapid resistance development [117]. |
| Klebsiella pneumoniae | Ceftazidime-avibactam | 74.9% | High resistance to a recently introduced drug [117]. |
| Pseudomonas aeruginosa | Ceftazidime-avibactam | 54.4% | Highlights cross-pathogen resistance challenges [117]. |
Table 2: Global Burden of Antimicrobial Resistance (WHO Data)
A global perspective on the impact of AMR [118].
| Metric | Figure | Context |
|---|---|---|
| Global deaths directly attributable to bacterial AMR (2019) | 1.27 million | Demonstrates the significant direct health impact [118]. |
| Global deaths associated with bacterial AMR (2019) | 4.95 million | Shows the broader burden where AMR was a contributing factor [118]. |
| Projected annual deaths due to AMR by 2050 | 10 million | A widely cited projection underscoring the future threat [102]. |
| Projected additional healthcare costs by 2050 (World Bank) | US$ 1 trillion | Highlights the massive economic burden [118]. |
| Projected annual GDP losses by 2030 (World Bank) | US$ 1-3.4 trillion | AMR threatens overall economic stability [118]. |
Experimental Protocols for Stewardship and Diagnostics
Protocol: Automated Clinical Decision Support to Reduce Unnecessary Antibiotic Prescribing
Based on the INSPIRE Trials [116]
Objective: To reduce the use of extended-spectrum antibiotics in non-critically ill hospitalized patients with common infections where the risk of resistant pathogens is low.
Methodology:
- Algorithm Integration: Embed a predictive algorithm into the hospital's computerized provider order entry (CPOE) system.
- Patient Risk Stratification: The algorithm uses available patient data to estimate the individual patient's need for extended-spectrum antibiotics (e.g., those targeting Pseudomonas and multidrug-resistant gram-negative bacteria).
- Automated Prompt: When a physician prescribes an antibiotic that is discordant with the algorithm's risk assessment, the system triggers an automated, patient-specific prompt.
- Prompt Content: The prompt provides information on the estimated low risk for a resistant infection, encouraging the use of narrower-spectrum agents.
- Outcome Measurement: The primary outcome is the reduction in days of therapy with extended-spectrum antibiotics. Safety is monitored via ICU transfers and hospital length of stay.
Protocol: Implementing a Hospital Framework for Accessing New Antimicrobials
Based on ICMR Expert Recommendations [117]
Objective: To ensure responsible introduction and use of new, last-resort antimicrobials to preserve their efficacy.
Methodology:
- Restrict Availability: Limit new, potent antimicrobials (Watch and Reserve categories) to hospital formularies only; they should not be available in retail pharmacies.
- Hospital Pre-Qualification: Require hospitals to provide documentary evidence of:
- A functional Antimicrobial Stewardship Program (AMS) and Infection Prevention and Control (IPC) program, certified by a national body.
- A functional AMS committee that conducts prescription review and audit.
- In-house diagnostic capacity (e.g., for performing antibiograms).
- An in-house pharmacy and a clinical pharmacist.
- Mandate Reporting: Hospitals must periodically submit AMR surveillance data to a national platform and declare this data on their website.
- Enforcement: Non-compliance should result in punitive measures, such as temporary suspension of access to these restricted antimicrobials.
Signaling Pathways and Regulatory Workflows
Diagram 1: FDA Drug Development and Accelerated Pathways
Diagram 2: SOS Response Pathway and Resistance Inhibition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Investigating Novel Anti-Resistance Strategies
| Research Reagent / Tool | Primary Function in Research | Application in AMR Context |
|---|---|---|
| SOS Response Inhibitors | Chemical compounds that inhibit the bacterial SOS response pathway, a stress-induced DNA repair system [102]. | Prevents the emergence of new resistance mutations during antibiotic treatment by reducing error-prone repair [102]. |
| Immuno-antibiotics | A class of antibiotics designed to target bacterial pathways (e.g., MEP isoprenoid pathway) that also interact with or modulate host immunity [102]. | Creates a dual antibacterial effect: direct killing and enhanced clearance by the host's immune system [102]. |
| Hydrogen Sulfide (Hâ‚‚S) Inhibitors | Compounds that block the production or function of Hâ‚‚S, a key biochemical mediator of bacterial stress resistance and antibiotic tolerance [102]. | Sensitizes bacteria to existing antibiotics by disrupting a universal defense network [102]. |
| Phage Libraries | Curated collections of bacteriophages (viruses that infect bacteria) characterized for their host range and lytic activity [114]. | Used to create personalized phage cocktails to treat drug-resistant bacterial infections, especially as an alternative to antibiotics [114]. |
| Predictive Algorithm & CDS | Software integrated into clinical workflows (Computerized Provider Order Entry) that analyzes patient data to estimate infection risk [116]. | Supports antimicrobial stewardship by providing patient-specific prompts to guide empiric antibiotic selection, reducing unnecessary broad-spectrum use [116]. |
Technical Support Center: Troubleshooting Antibiotic Resistance in Therapy Research
Troubleshooting Guide: Addressing Common Experimental Challenges
Problem 1: Unexpected Treatment Failure in Efficacy Models
- Symptoms: Lower-than-expected cure rates in animal models or in vitro assays, even with previously effective antibiotic concentrations.
- Investigation & Resolution:
- Confirm Resistance Development: Perform antimicrobial susceptibility testing (AST) on re-isolated pathogens. A significant increase in Minimum Inhibitory Concentration (MIC) indicates resistance development [119].
- Check Drug Stability and Preparation: Verify drug storage conditions, solvent use, and preparation methodology. Chemical degradation can mimic treatment failure.
- Review Inoculum Preparation: Ensure the initial bacterial inoculum size is standardized. A high inoculum can lead to apparent resistance due to the presence of pre-existing resistant subpopulations or inoculum effect.
- Control for Contamination: Rule out contamination with other resistant environmental strains by using genotyping methods on pre- and post-treatment isolates.
Problem 2: High Variability in Preclinical Cost-Effectiveness Outcomes
- Symptoms: Widely varying results in simulated cost-effectiveness models using identical input parameters.
- Investigation & Resolution:
- Verify Model Structure: Ensure the decision tree or Markov model accurately reflects the patient journey and treatment pathways. Common errors include incorrect state transitions or double-counting of costs [120].
- Audit Input Parameters: Check for consistency in cost (e.g., drug acquisition, hospitalization, management of adverse events) and outcome data (e.g., cure rates, mortality). Use probabilistic sensitivity analysis to understand the impact of parameter uncertainty [120] [121].
- Validate Time Horizon and Discounting: Confirm that the model's time horizon is sufficient to capture long-term outcomes and that costs and benefits are discounted appropriately, typically at 3% as used in many analyses [120].
Problem 3: Inconsistent Data on Resistance Emergence Rates
- Symptoms: Literature reports highly variable rates of resistance emergence for the same antibiotic-pathogen combination.
- Investigation & Resolution:
- Scrutinize Methodology: Compare the experimental designs. Differences in dosing regimens, infection models (in vitro vs. in vivo), and the definition of "resistance emergence" (e.g., genetic mutation vs. phenotypic MIC shift) can cause major discrepancies.
- Standardize Testing Protocols: Adhere to established guidelines like those from the Clinical and Laboratory Standards Institute (CLSI) or European Committee on Antimicrobial Susceptibility Testing (EUCAST) for AST.
- Implement Sequencing: Use whole-genome sequencing on pre- and post-exposure isolates to identify specific resistance-conferring mutations, providing a more precise measure of emergence [118].
Frequently Asked Questions (FAQs)
Q1: What are the primary mechanisms by which bacteria become resistant to a new antibiotic during therapy research? Bacteria develop resistance through several mechanisms: (1) Enzymatic Inactivation: Producing enzymes like β-lactamases that degrade the antibiotic [120]. (2) Target Modification: Altering the drug's binding site so it can no longer interact effectively. (3) Efflux Pumps: Actively pumping the drug out of the cell [119]. (4) Reduced Permeability: Changing the cell wall or membrane to prevent drug entry.
Q2: How can we design in vitro experiments to better predict the potential for resistance development? Utilize serial passage experiments, where bacteria are repeatedly exposed to sub-inhibitory concentrations of the antibiotic over multiple generations. Monitor for increases in MIC. Additionally, use chemostat models to maintain bacteria in a steady state of growth under antibiotic pressure, which can simulate the conditions that select for resistant mutants in a clinical setting.
Q3: From a health economics perspective, how is the long-term benefit of a new antibiotic that limits resistance development quantified? The long-term benefit is often quantified using cost-effectiveness analysis, which calculates the Incremental Cost-Effectiveness Ratio (ICER). This metric compares the difference in costs between a new therapy and the standard of care to the difference in their health outcomes, typically measured in Quality-Adjusted Life-Years (QALYs) [120]. A therapy that slows resistance may have higher upfront costs but can lead to greater QALY gains by remaining effective longer, resulting in a favorable ICER.
Q4: What key parameters should be included in an economic model to capture the value of preventing resistance? A robust economic model should include [120] [121]:
- Rates of resistance emergence for all comparators.
- Associated costs of treating resistant infections (prolonged hospitalization, more expensive second-line drugs).
- Mortality and morbidity (quality of life) differences between successful treatment and treatment failure.
- Transmission dynamics, accounting for the spread of resistant strains within a community.
- Costs of managing drug-related adverse events (e.g., nephrotoxicity).
Quantitative Data in Antibiotic Resistance and Cost-Effectiveness
Table 1: Cost-Effectiveness Outcomes of Aztreonam-Avibactam vs. Colistin+Meropenem in Italy
| Infection Type | Incremental Cost-Effectiveness Ratio (ICER) | Key Outcome Summary |
|---|---|---|
| Complicated Intra-Abdominal Infection (cIAI) | Dominant (Cost-saving & more effective) | Higher cure rates, shorter hospital stays, and QALY gains compared to colistin-based therapy [120]. |
| Hospital-Acquired Pneumonia/Ventilator-Associated Pneumonia (HAP/VAP) | €1,552 per QALY | ICER well below the Italian willingness-to-pay threshold of €30,000, indicating high cost-effectiveness [120]. |
Table 2: Global Burden and Economic Impact of Antimicrobial Resistance (AMR)
| Metric | Estimated Value | Context |
|---|---|---|
| Global deaths attributable to bacterial AMR (2019) | 1.27 million direct deaths [118]. | Highlights the significant mortality burden of AMR. |
| Projected annual global economic cost of AMR by 2030 | USD 1–3.4 trillion in GDP losses [118]. | Demonstrates the massive macroeconomic impact. |
| Most studied AMR infections in LMICs | Tuberculosis (40%) and general bacterial infections (39%) [121]. | Identifies research focus areas in low- and middle-income countries. |
Experimental Protocols for Resistance Prevention Studies
Protocol 1: Assessing the Mutant Prevention Concentration (MPC)
- Objective: To determine the antibiotic concentration that suppresses the growth of resistant mutant subpopulations.
- Methodology:
- Prepare a high-density bacterial inoculum (>10^10 CFU) from multiple colonies to ensure a representative population of mutants.
- Plate the inoculum onto a series of agar plates containing the test antibiotic at concentrations ranging from the MIC to well above it (e.g., 0.5x, 1x, 2x, 4x, 8x, 16x MIC).
- Incubate the plates and observe for bacterial growth.
- The MPC is defined as the lowest antibiotic concentration that prevents the growth of any bacterial colonies.
- The Mutant Selection Window (MSW) is the concentration range between the MIC and the MPC, where selective amplification of resistant mutants is most likely.
Protocol 2: Combination Therapy Synergy Checkerboard Assay
- Objective: To identify synergistic antibiotic combinations that can enhance efficacy and delay resistance.
- Methodology:
- In a 96-well microtiter plate, prepare a two-dimensional dilution series of two antibiotics (Drug A and Drug B), creating a matrix where each well has a unique combination of concentrations.
- Inoculate each well with a standardized bacterial suspension.
- After incubation, measure the optical density to determine growth inhibition.
- Calculate the Fractional Inhibitory Concentration (FIC) Index for each combination:
- FIC Index = (MIC of Drug A in combination / MIC of Drug A alone) + (MIC of Drug B in combination / MIC of Drug B alone)
- Interpretation: An FIC Index ≤0.5 indicates synergy; >0.5 to 4 indicates indifference; and >4 indicates antagonism.
Visualizing Workflows and Relationships
Diagram Title: Integrated R&D and Health Economics Workflow
Diagram Title: Primary Antibiotic Resistance Mechanisms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Antibiotic Resistance Studies
| Item | Function/Application |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing (AST) as per CLSI guidelines. |
| 96-Well Microtiter Plates | For performing broth microdilution assays to determine MIC and for checkerboard synergy tests. |
| Quality Control Strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) | To ensure the accuracy and precision of AST results. |
| Agar Plates for MPC | Solid media for plating high-density bacterial inoculums to determine the Mutant Prevention Concentration. |
| DNA Extraction & Purification Kits | For extracting bacterial genomic DNA to perform sequencing and identify resistance mutations. |
Conclusion
The escalating crisis of antimicrobial resistance demands a paradigm shift from traditional antibiotic development toward innovative 'resistance-resistant' strategies that proactively manage evolutionary pressures. This synthesis demonstrates that future success lies in integrated approaches combining foundational understanding of resistance mechanisms with advanced therapeutic modalities like evolutionary steering, phage therapy, and targeted mutagenesis inhibition. The critical path forward requires overcoming significant translational challenges through enhanced economic models, AI-powered resistance prediction, and adaptive clinical trial designs. For researchers and drug development professionals, prioritizing these multifaceted approaches—validated through robust surveillance frameworks and comparative effectiveness research—offers the most promising pathway to outmaneuver bacterial adaptation and preserve the longevity of our antimicrobial arsenal. The future of infectious disease treatment depends on our collective ability to implement these strategies before conventional options are exhausted.
References
- 1. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 2. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 3. Global antibiotic resistance surveillance report 2025 [https://www.amr-insights.eu/global-antibiotic-resistance-surveillance-report-2025/]
- 4. WHO report highlights growing AMR crisis and urgent need ... [https://bsac.org.uk/who-report-highlights-growing-amr-crisis-and-urgent-need-for-stronger-global-surveillance/]
- 5. Rapid Methods for Antimicrobial Resistance Diagnostics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7924329/]
- 6. Antimicrobial Resistance | Detection with NGS [https://www.illumina.com/areas-of-interest/microbiology/public-health-surveillance/antimicrobial-resistance-detection.html]
- 7. Mitigating antimicrobial resistance (AMR) using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10041058/]
- 8. Exploring molecular mechanisms of drug resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11883354/]
- 9. Antimicrobial resistance: Linking molecular mechanisms to ... [https://www.sciencedirect.com/science/article/pii/S2472555225000255]
- 10. Combating Antimicrobial Resistance: Innovations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388624/]
- 11. Antimicrobial resistance: Linking molecular mechanisms to ... [https://pubmed.ncbi.nlm.nih.gov/40216324/]
- 12. Approach to combat antibiotic resistance turns bacterium's ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/approach-to-combat-antibiotic-resistance-turns-bacteriums-genes-against-it.html]
- 13. 世å«ç»„织è¦å‘Šç§°å…¨çƒæ™®éå˜åœ¨å¸¸ç”¨æŠ—ç”Ÿç´ è€è¯æ€§| | 1è”åˆå›½æ–°é—» [https://news.un.org/zh/story/2025/10/1140905]
- 14. What is antimicrobial resistance and how can we tackle it? [https://www.weforum.org/stories/2025/11/antimicrobial-resistance-superbugs-antibiotics/]
- 15. Stress-Induced Mutagenesis in Bacteria - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2747772/]
- 16. Evaluating evolutionary models of stress-induced ... [https://www.nature.com/articles/nrg3415]
- 17. The SOS system: A complex and tightly regulated response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590174/]
- 18. After 30 Years of Study, the Bacterial SOS Response Still ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1174825/]
- 19. The DNA Damage Inducible SOS Response Is a Key ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01785/full]
- 20. Model of SOS-induced mutagenesis in bacteria ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519309003865]
- 21. Horizontal Gene Transfer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4536854/]
- 22. 3.1: Horizontal Gene Transfer in Bacteria [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Kaiser)/Unit_2%3A_Bacterial_Genetics_and_the_Chemical_Control_of_Bacteria/3%3A_Bacterial_Genetics/3.1%3A_Horizontal_Gene_Transfer_in_Bacteria]
- 23. Horizontal gene transfer and adaptive evolution in bacteria [https://www.nature.com/articles/s41579-021-00650-4]
- 24. Researchers develop new method to combat antibiotic ... [https://www.news-medical.net/news/20251119/Researchers-develop-new-method-to-combat-antibiotic-resistant-bacteria-using-bacteriophages.aspx]
- 25. A molecular conveyor belt-associated protein controls the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239597/]
- 26. A comprehensive review of advanced strategies to combat ... [https://pubmed.ncbi.nlm.nih.gov/41003718/]
- 27. Antibiotic potentiators as a promising strategy for ... [https://www.nature.com/articles/s44259-025-00112-4]
- 28. Two large clinical trials find a better method to prescribe ... [https://www.ucihealth.org/about-us/news/2025/04/inspire-clinical-trials]
- 29. Current Trends in Antibiotic Therapy and Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063558/]
- 30. Integrated one health approach key to combating antimicrobial resistance, experts say [https://www.the-star.co.ke/news/2025-11-19-experts-integrated-one-health-approach-key-to-combating-antimicrobial-resistance]
- 31. About One Health [https://www.cdc.gov/one-health/about/index.html]
- 32. One health [https://www.who.int/health-topics/one-health]
- 33. Strategies to Combat Antimicrobial Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4149102/]
- 34. Targeting evolution of antibiotic resistance by SOS response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7843400/]
- 35. Antibiotic-induced stress responses in Gram-negative ... [https://pubmed.ncbi.nlm.nih.gov/40053699/]
- 36. The SOS response increases bacterial fitness, but not ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4614765/]
- 37. Fast evolution of SOS-independent multi-drug resistance in ... [https://elifesciences.org/articles/95058]
- 38. Exploiting evolutionary steering to induce collateral drug ... [https://www.nature.com/articles/s41467-020-15596-z]
- 39. Evolutionary stability of collateral sensitivity to antibiotics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6881144/]
- 40. Navigating collateral sensitivity: insights into the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11540712/]
- 41. synergistic tool to combat multi-drug resistant pathogens [https://pubmed.ncbi.nlm.nih.gov/38179424/]
- 42. Antibiotic Adjuvants: Rescuing Antibiotics from Resistance [https://www.sciencedirect.com/science/article/abs/pii/S0966842X16300725]
- 43. Sample-efficient identification of high-dimensional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9333450/]
- 44. Combination Approaches to Combat Multi-Drug Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3594660/]
- 45. Drug combinations targeting antibiotic resistance [https://www.nature.com/articles/s44259-024-00047-2]
- 46. The Current Landscape of Phage–Antibiotic Synergistic (PAS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190067/]
- 47. Phage-antibiotic synergy to combat multidrug resistant ... [https://www.nature.com/articles/s41598-025-01489-y]
- 48. Overcoming Antimicrobial Resistance: Phage Therapy as ... [https://www.sciencedirect.com/science/article/pii/S0924857925001955]
- 49. A targeted approach to overcoming antibiotic resistance [https://pubmed.ncbi.nlm.nih.gov/39477033/]
- 50. A blueprint for broadly effective bacteriophage-antibiotic ... [https://www.nature.com/articles/s41467-024-53994-9]
- 51. Phage Therapy—Challenges, Opportunities and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10747886/]
- 52. Phage Therapy: The Future of Fighting Antibiotic Resistance [https://norgenbiotek.com/blog/phage-therapy-future-fighting-antibiotic-resistance?srsltid=AfmBOop-1UJq6MbvEAPuCwJ_sdaqbuGT2KJm2cEkqUXlOQbSA2bMMYOd]
- 53. Advanced Nanoparticles in Combating Antibiotic Resistance [https://www.mdpi.com/2624-845X/6/2/9]
- 54. Antimicrobial nanoparticles: current landscape and future ... [https://pubs.rsc.org/en/content/articlehtml/2024/pm/d4pm00032c]
- 55. The antimicrobial peptides and their potential clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6684887/]
- 56. Antimicrobial Peptides: Classification, Design, Application ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.582779/full]
- 57. Antimicrobial peptide biological activity, delivery systems and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06321-9]
- 58. Critical questions in development of targeted nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4817320/]
- 59. Basic Principles of Nanoparticle Tracking Analysis - Q&A [https://www.malvernpanalytical.com/en/learn/knowledge-center/insights/basic-principles-of-nanoparticle-tracking-analysis-qa]
- 60. Combating Antimicrobial Resistance: Innovative Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389514/]
- 61. Gut microbiome therapy: fecal microbiota transplantation vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11469438/]
- 62. Exploring the role of gut microbiota in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11915737/]
- 63. What's New and What's Next in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377394/]
- 64. Targeting the microbiome: from probiotics to fecal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6208019/]
- 65. Fecal microbiota transplantation: Uses, questions, and ethics [https://www.sciencedirect.com/science/article/pii/S2590097820300240]
- 66. Fecal transplants: Promising treatment or potential health risk? [https://biologicalsciences.uchicago.edu/news/fecal-transplant-potential-health-risk]
- 67. challenges in translating microbiome research to clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550608/]
- 68. Scientists Develop a Way to Track Donor Bacteria After ... [https://www.mountsinai.org/about/newsroom/2025/scientists-develop-a-way-to-track-donor-bacteria-after-fecal-microbiota-transplants]
- 69. Antibiotics re-booted—time to kick back against drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125309/]
- 70. Revitalizing the antibiotic pipeline by implementing new ... [https://www.ifpma.org/publications/revitalizing-the-antibiotic-pipeline-by-implementing-new-rd-pull-incentives/]
- 71. 5 challenges that governments need to address in resolving ... [https://www.reactgroup.org/news-and-views/news-and-opinions/year-2022/five-challenges-that-governments-need-to-address-in-resolving-the-stagnation-in-antibiotic-development/]
- 72. ReAct Policy Brief: Sustainable antibiotic production – 2025 [https://www.reactgroup.org/news-and-views/news-and-opinions/year-2025/react-policy-brief-sustainable-antibiotic-production/]
- 73. WHO: Reviews of antibacterial therapeutics and ... [https://amr.solutions/2025/10/04/who-reviews-of-antibacterial-therapeutics-and-diagnostics/]
- 74. Common Questions in Clinical Trial Design [https://www.quanticate.com/blog/common-questions-in-clinical-trial-design]
- 75. The challenges of determining noninferiority margins: a case ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3576440/]
- 76. Prediction of antibiotic resistance from ... [https://www.nature.com/articles/s41598-025-14078-w]
- 77. Predicting population dynamics of antimicrobial resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X25001462]
- 78. Mitigating antimicrobial resistance by innovative solutions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402447/]
- 79. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 80. Avoiding resistance development to newer drugs [https://pubmed.ncbi.nlm.nih.gov/41241177/]
- 81. Avoiding resistance development to newer drugs [https://www.sciencedirect.com/science/article/pii/S1198743X25005609]
- 82. Harnessing AI to Revolutionize Antibiotic Discovery [https://asm.org/articles/2025/august/ai-next-frontier-antibiotic-discovery]
- 83. The role of artificial intelligence and machine learning in ... [https://www.sciencedirect.com/science/article/pii/S2001037025000078]
- 84. PK/PD-Guided Strategies for Appropriate Antibiotic Use in ... [https://www.mdpi.com/2079-6382/14/1/92]
- 85. Current approaches and tools for combating antibiotic ... [https://link.springer.com/article/10.1007/s42452-025-07108-9]
- 86. Transforming Rapid Diagnostic Tests for Precision Public ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041428/]
- 87. How AI can help us beat AMR | npj Antimicrobials and ... [https://www.nature.com/articles/s44259-025-00085-4]
- 88. What are the 2025 Trends in Diagnostics? [https://www.hartmannyoung.com/resources/blog/what-are-the-2025-trends-in-diagnostics-/]
- 89. Antibiotic Resistance - NFID [https://www.nfid.org/antibiotic-resistance/]
- 90. Antimicrobial Resistance: Causes and How It Spreads [https://www.cdc.gov/antimicrobial-resistance/causes/index.html]
- 91. Frequently Asked Questions (FAQs) About Antimicrobial ... [https://www.health.state.mn.us/diseases/antibioticresistance/basics/faq.html]
- 92. Beyond antibiotics: exploring multifaceted approaches to ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1493915/full]
- 93. GSK and Fleming Initiative scientists unite to target AMR ... [https://www.gsk.com/en-gb/media/press-releases/gsk-and-fleming-initiative-scientists-unite-to-target-amr-with-advanced-ai/]
- 94. 5 Drug Discovery and Development Challenges and How ... [https://www.srgtalent.com/blog/5-drug-discovery-and-development-challenges-and-how-to-solve-them]
- 95. Navigating the Complex Evolution of Preclinical Models - PharmaFeatures [https://pharmafeatures.com/navigating-the-complex-evolution-of-preclinical-models/]
- 96. The Role of Complex In Vitro Models in IND Submissions to the FDA ... [https://emulatebio.com/what-are-complex-in-vitro-models/]
- 97. A Guide to Reproducibility in Preclinical Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6314499/]
- 98. Advanced In Vitro Models for Preclinical Drug Safety: Recent Progress and Prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763796/]
- 99. Chapter 15 Experimental protocols | Lab Handbook [https://ccmorey.github.io/labHandbook/experimental-protocols.html]
- 100. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 101. Guide: Assessing preclinical PK in therapeutic antibodies [https://www.ddw-online.com/guide-assessing-preclinical-pk-in-therapeutic-antibodies-27434-202312/]
- 102. Antibiotic resistance: The challenges and some emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459344/]
- 103. The Changing Landscape of Antibiotic Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291801/]
- 104. Antibiotics, Volume 14, Issue 11 (November 2025) [https://www.mdpi.com/2079-6382/14/11]
- 105. Frontiers | Bacteriocin KvarM versus Conventional Antibiotics ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1559865/abstract]
- 106. Current and Future Technologies for the Detection of Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10606640/]
- 107. Therapeutics Initiative | [155] Oral vs IV antibiotics [https://www.ti.ubc.ca/2025/05/20/155-oral-vs-iv-antibiotics/]
- 108. Controlling the Emergence and Spread of Antimicrobial ... [https://www.cdc.gov/antimicrobial-resistance/prevention/index.html]
- 109. Global Antimicrobial Resistance and Use Surveillance ... [https://www.who.int/initiatives/glass]
- 110. WHO warns of widespread resistance to common ... [https://www.paho.org/en/news/13-10-2025-who-warns-widespread-resistance-common-antibiotics-worldwide]
- 111. Antimicrobial Resistance: A Growing Serious Threat for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10340576/]
- 112. æŠ—ç”Ÿç´ è€è¯æ€§ [https://www.who.int/zh/news-room/fact-sheets/detail/antibiotic-resistance]
- 113. Development & Approval Process | Drugs [https://www.fda.gov/drugs/development-approval-process-drugs]
- 114. Alternatives to antibiotics in the fight against superbugs [https://www.weforum.org/stories/2025/10/this-regulatory-shift-is-unlocking-alternatives-to-antibiotics-in-the-fight-against-superbugs/]
- 115. Let It Grow: FDA Revises Q&A Guidance to Support ... [https://www.jdsupra.com/legalnews/let-it-grow-fda-revises-q-a-guidance-to-4399947/]
- 116. April 14, 2025: In INSPIRE Trials, Automated Prompts ... [https://rethinkingclinicaltrials.org/news/april-14-2025-in-inspire-trials-automated-prompts-reduced-unnecessary-prescribing-of-extended-spectrum-antibiotics/]
- 117. A strategic approach to regulating new antimicrobials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363153/]
- 118. Antimicrobial resistance [https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance]
- 119. Antimicrobial Resistance: Definition, Causes & Prevention [https://my.clevelandclinic.org/health/articles/16142-antimicrobial-resistance]
- 120. Cost-Effectiveness Analysis of Aztreonam-Avibactam (ATM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602586/]
- 121. Economic costing methodologies for drug-resistant bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139254/]