Population Pharmacokinetic Modeling for Anti-infective Dose Optimization: A Comprehensive Guide for Researchers
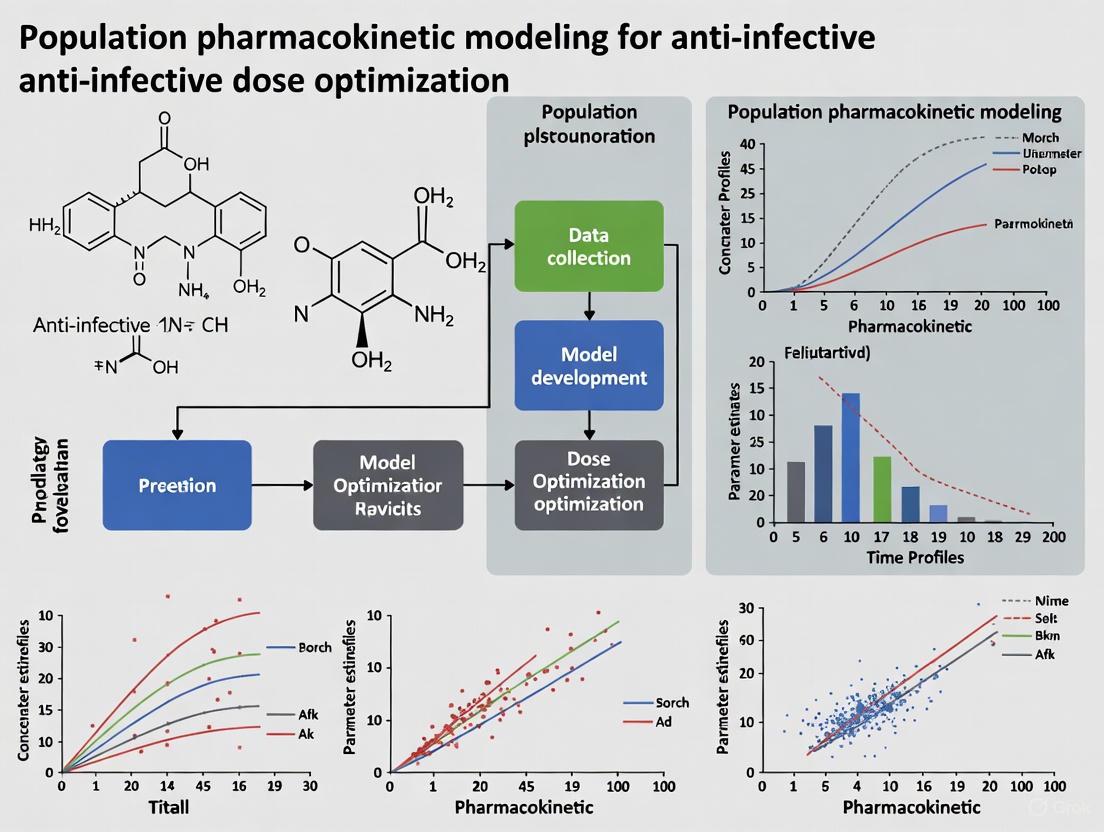
This article provides a comprehensive overview of population pharmacokinetic (PopPK) modeling and its critical application in optimizing anti-infective therapy, particularly in challenging patient populations like the critically ill.
Population Pharmacokinetic Modeling for Anti-infective Dose Optimization: A Comprehensive Guide for Researchers
Abstract
This article provides a comprehensive overview of population pharmacokinetic (PopPK) modeling and its critical application in optimizing anti-infective therapy, particularly in challenging patient populations like the critically ill. It covers foundational principles, methodological approaches using nonlinear mixed-effects models (NLMEM), and software tools like NONMEM and Phoenix NLME. The content further addresses troubleshooting common issues, model validation strategies, and explores emerging trends such as machine learning automation and exposure-response analysis to achieve precise, personalized dosing that improves clinical outcomes and combats antimicrobial resistance.
Understanding Population PK Fundamentals and Its Critical Role in Anti-infective Therapy
Population pharmacokinetics (PopPK) is a critical discipline that studies the sources and correlates of pharmacokinetic variability in patient populations [1]. It utilizes nonlinear mixed-effects models (NLMEM) to simultaneously analyze data from all individuals in a study population, providing a powerful framework for understanding how drugs are absorbed, distributed, metabolized, and excreted across diverse patient groups [2] [1]. This approach is particularly valuable in anti-infective dose optimization research, where optimizing drug exposure is essential for ensuring efficacy while minimizing toxicity and resistance development.
The "nonlinear" aspect of NLMEM refers to the fact that the dependent variable (e.g., drug concentration) is nonlinearly related to the model parameters and independent variables, while "mixed-effects" refers to the model parameterization that includes both fixed effects (population parameters assumed to be constant) and random effects (sample-dependent random variables) [1]. This modeling framework provides a robust solution for analyzing sparse, unbalanced data commonly encountered in clinical trials, where it may not be feasible to obtain extensive sampling from each patient [2]. By quantifying and explaining variability, PopPK models enable model-informed precision dosing, which is especially crucial for anti-infective drugs with narrow therapeutic windows.
Theoretical Foundations: Fixed Effects, Random Effects, and NLMEM
Fixed Effects
Fixed effects represent population-typical parameters that are assumed to remain constant each time data is collected [2]. These parameters describe the typical pharmacokinetic profile for the population, such as typical clearance (CL) or typical volume of distribution (Vd). Fixed effects can also include the influence of patient characteristics (covariates) on pharmacokinetic parameters. For example, a PopPK analysis of voriconazole identified that covariates such as continuous renal replacement therapy (CRRT), C-reactive protein, and specific liver enzymes significantly influence drug clearance [3]. Similarly, a piperacillin/tazobactam PopPK model identified estimated glomerular filtration rate (eGFR) adjusted by body surface area and body weight as significant covariates affecting drug clearance and distribution [4].
Random Effects
Random effects account for the unpredictable variability in pharmacokinetic parameters between individuals, between occasions, and within the residual error [1]. These effects are modeled as random variables with distributions that must be specified, typically assuming a normal distribution with mean zero and variance ω² [2]. Random effects act as additional error terms that capture:
- Between-subject variability (BSV): Differences in parameters between individuals
- Between-occasion variability (BOV): Differences within the same individual on different occasions
- Residual unexplained variability (RUV): Remaining variability not accounted for by other model components
Nonlinear Mixed-Effects Models (NLMEM)
NLMEM integrates both fixed and random effects to provide a comprehensive framework for population analysis [1]. The mixed-effects approach offers a strategic compromise between ignoring data groupings entirely—which sacrifices valuable information—and fitting each group with a separate model, which requires significantly larger sample sizes [2]. This makes NLMEM particularly suitable for analyzing sparse data sets, such as those collected during routine therapeutic drug monitoring in clinical practice [3].
Table 1: Key Components of Nonlinear Mixed-Effects Models in Pharmacokinetics
| Component | Description | Examples |
|---|---|---|
| Structural Model | Describes the typical concentration-time course | One-compartment, two-compartment models [4] |
| Fixed Effects | Population typical parameters | Typical clearance, volume of distribution [3] |
| Random Effects | Unexplained variability components | Between-subject, residual variability [1] |
| Covariate Models | Explain variability via patient factors | Renal function, body weight, genetic polymorphisms [3] [4] |
| Statistical Model | Accounts for random variability | Interindividual, interoccasion, residual error [1] |
Applications in Anti-Infective Dose Optimization Research
Voriconazole in COVID-19-Associated Pulmonary Aspergillosis
A recent PopPK study of voriconazole in patients with COVID-19-associated pulmonary aspergillosis (CAPA) demonstrated the clinical utility of NLMEM for dose optimization in complex patient populations [3]. The study developed a one-compartment model with first-order elimination to characterize voriconazole disposition, estimating an apparent clearance (CL/F) of 3.17 L/h and an apparent volume of distribution (V/F) of 135 L for a standard patient. Covariate analysis identified that CRRT, C-reactive protein, gamma-glutamyl transpeptidase, aspartate aminotransferase, and platelet count significantly influenced voriconazole clearance. Monte Carlo simulations based on the final model revealed that patients on CRRT required both higher loading doses and increased maintenance doses compared to those not on CRRT, providing evidence-based guidance for personalized dosing in this high-risk population [3].
Aztreonam-Avibactam Optimization through PopPK/PD
A population pharmacokinetic/pharmacodynamic modeling approach was used to optimize aztreonam-avibactam dose regimens for adult patients with serious gram-negative infections [5]. The final model, developed using data from 2,635 subjects, identified time-varying creatinine clearance as a key covariate on clearance for both drugs. The model was used to simulate exposures by infection type and renal function, estimating the joint probability of pharmacodynamic target attainment for phase 3 patients. Simulations demonstrated that the approved aztreonam-avibactam dose regimens achieved a joint probability of target attainment between 89% to >99% at steady state across renal function groups, confirming the adequacy of the proposed dosing strategy [5].
Piperacillin/Tazobactam Dosing Strategies
A PopPK analysis of piperacillin/tazobactam in healthy adults highlighted potential limitations in current dosing recommendations [4]. The study found that while the standard dosing regimen (4/0.5 g q6h with 30-minute infusion) achieved a 90% probability of target attainment for 50% fT>MIC at MIC values up to 4 mg/L in patients with normal renal function, this regimen often failed to achieve 90% PTA for more stringent targets (100% fT>MIC, 100% fT>4×MIC) or higher MICs, particularly in patients with enhanced renal function (eGFR ≥ 130 mL/min). These findings suggest that alternative strategies such as extended or continuous infusion may be necessary to optimize therapeutic outcomes, especially for less susceptible pathogens [4].
Table 2: Key Parameters from Recent Anti-Infective PopPK Studies
| Drug | Population | Structural Model | Key Covariates | Dosing Implications |
|---|---|---|---|---|
| Voriconazole [3] | CAPA patients | One-compartment | CRRT, CRP, GGT, AST, PLT | Higher doses needed for CRRT patients |
| Aztreonam-Avibactam [5] | Adults with gram-negative infections | Two-compartment | Time-varying CrCl | Optimized regimens across renal function |
| Piperacillin/Tazobactam [4] | Healthy adults | Two-compartment | eGFR, Body weight | Standard dosing inadequate for enhanced renal function |
Experimental Protocols for Population PK Model Development
Data Collection and Preprocessing
The initial step in PopPK model development involves comprehensive data collection and preprocessing. Data should be scrutinized to ensure accuracy, with graphical assessment performed to identify potential problems or outliers [1]. During data cleaning, erroneous records may be identified and excluded if justified as outliers that would impair model development. Common data components include:
- Dosing information: Drug, dose, route, frequency, and duration
- Concentration measurements: Plasma, serum, or blood samples with precise timing
- Patient demographics: Age, sex, weight, height, body surface area
- Laboratory values: Renal function (creatinine, eGFR), liver function (ALT, AST, bilirubin)
- Clinical covariates: Disease status, concomitant medications, genetic polymorphisms
- Special circumstances: Renal replacement therapy, extracorporeal membrane oxygenation [3]
For voriconazole PopPK analysis, researchers collected extensive clinical data including demographic characteristics, biochemical indicators, concomitant medications, and CYP2C19 and CYP3A4 genotypes [3]. Drug concentrations were quantified using validated high-performance liquid chromatography (HPLC) methods with calibration curves demonstrating acceptable linearity over 0.1–30 mg/L [3].
Structural Model Development
The structural model describes the typical concentration-time course within the population [1]. For pharmacokinetic data, mammillary compartment models are predominant, with the number of compartments determined by the distinct exponential phases observed when plotting log concentration versus time [1]. Common structural models include:
- One-compartment model: Suitable for drugs with simple disposition characteristics
- Two-compartment model: Appropriate for drugs with distinct distribution and elimination phases
- Three-compartment model: Necessary for drugs with complex distribution patterns
Model selection is guided by diagnostic plots, objective function value (OFV) comparisons, and information criteria such as Akaike information criterion (AIC) and Bayesian information criterion (BIC) [1]. The piperacillin/tazobactam PopPK analysis found that two-compartment models best described the concentration-time profiles for both drugs [4].
Statistical Model Development
The statistical model quantifies the random variability in the data, including between-subject variability, between-occasion variability, and residual unexplained variability [1]. Modelers must specify:
- IIV model: Typically exponential, proportional, or additive error models
- Residual error model: Additive, proportional, or combined error structures
Parameter estimation is typically performed using maximum likelihood methods, with the objective function value (OFV) providing a summary of how closely model predictions match the observed data [1].
Covariate Model Development
Covariate analysis identifies patient factors that explain variability in pharmacokinetic parameters [6]. This process typically involves:
- Identification of potential covariates based on biological plausibility
- Covariate screening using statistical methods and graphical analysis
- Model building with forward inclusion and backward elimination
- Model validation using diagnostic plots and statistical criteria
In the voriconazole PopPK analysis, covariates were tested using a stepwise approach with significance levels of p < 0.05 for forward inclusion and p < 0.01 for backward elimination [3].
Model Validation
Model validation evaluates the performance and predictive ability of the final PopPK model. Common techniques include:
- Goodness-of-fit plots: Observed vs. predicted concentrations, conditional weighted residuals vs. time or predictions [4]
- Visual predictive checks: Comparing the variability of simulations from the model against the variability observed in the data [7]
- Bootstrap analysis: Assessing the stability and precision of parameter estimates
- Prediction-corrected visual predictive checks: Accounting for variability in dosing regimens and sampling schedules
PopPK Model Development Workflow
Table 3: Essential Tools for Population Pharmacokinetic Research
| Category | Tool/Resource | Function/Application |
|---|---|---|
| Modeling Software | NONMEM [1] | Industry-standard for population PK/PD modeling |
| Monolix [7] | User-friendly interface for mixed-effects modeling | |
| Berkeley Madonna [7] | Model visualization and interactive simulation | |
| Statistical Platforms | R [8] | Data preprocessing, visualization, and diagnostics |
| SAS [8] | Data management and statistical analysis | |
| Analytical Methods | HPLC [3] | Drug concentration quantification |
| UV detection [3] | Detection method for chromatographic analysis | |
| Genotyping Tools | Sangon Biotech kits [3] | Genomic DNA isolation and purification |
| Sanger sequencing [3] | CYP450 polymorphism identification | |
| Visualization Tools | Graphviz/DOT [7] | Diagram creation for model workflows |
| ColorBrewer [8] | Accessible color palette selection for scientific figures |
Visualization Principles for Effective Communication
Effective visualization is crucial for communicating PopPK model results to multidisciplinary teams [7]. Key principles include:
- Provide a clear message: Focus on the main insight or relationship
- Show the quantity of interest: Display the placebo-corrected treatment effect rather than separate effects
- Use intuitive colors: Apply colors consistently (e.g., green for positive response, red for adverse effects)
- Ensure accessibility: Select color palettes with sufficient contrast for colorblind readers [8]
- Indicate thresholds of interest: Mark clinical relevance thresholds (e.g., target concentrations, efficacy thresholds)
For PopPK visualizations specifically:
- Show model components individually to facilitate understanding
- Display both estimated responses and confidence intervals
- Illustrate the percentage of patients crossing efficacy or safety thresholds
- Use appropriate time intervals and indicate dosing events [7]
NLMEM Components Relationship
Population pharmacokinetics using nonlinear mixed-effects modeling provides a powerful framework for understanding drug disposition variability in patient populations. By integrating fixed effects (population-typical parameters), random effects (unexplained variability), and covariate relationships, PopPK models enable evidence-based dose optimization for anti-infective therapies. The continued advancement of PopPK methodologies, coupled with appropriate visualization and communication strategies, will further enhance model-informed precision dosing in clinical practice, ultimately improving therapeutic outcomes for patients with infectious diseases.
Critically ill patients represent a population with some of the highest risks for treatment failure and drug-related toxicity. The pathophysiological changes associated with critical illness significantly alter antimicrobial disposition, creating substantial challenges for achieving effective drug concentrations at the site of infection [9]. Failure of antimicrobial therapy in this vulnerable population has a direct impact on survival, making dose optimization a critical determinant of clinical outcomes [9]. The complex interplay of multiple factors observed in critically ill patients poses a significant challenge in predicting the pharmacokinetics of antimicrobials, rendering standard dosing regimens frequently inadequate [9] [10].
The foundation of precision dosing rests upon the relationship between pharmacokinetic (PK) and pharmacodynamic (PD) properties of antimicrobial agents. The optimal PK/PD parameter depends on the antimicrobial's bacterial activity pattern: (1) peak plasma concentration (Cpeak)/minimum inhibitory concentration (MIC) for antimicrobials with concentration-dependent activity; (2) cumulative percent of time that free drug concentration remains above the MIC (fT>MIC) for time-dependent antimicrobials; and (3) area under the concentration-time curve (AUC)/MIC for antimicrobials with both concentration- and time-dependent activity [9]. Understanding these relationships is essential for designing regimens that maximize bacterial killing while minimizing toxicity and resistance development.
Quantitative Foundations: Pathophysiological Factors Altering PK/PD
The pathophysiological changes occurring during critical illness profoundly impact all aspects of drug disposition. Table 1 summarizes the primary factors and their effects on key pharmacokinetic parameters.
Table 1: Pathophysiological Factors Altering Antimicrobial Pharmacokinetics in Critically Ill Patients
| Factor | Impact on Volume of Distribution (Vd) | Impact on Clearance (CL) | Most Affected Antimicrobial Classes | Clinical Implications |
|---|---|---|---|---|
| Systemic Inflammation/SIRS | Increased Vd for hydrophilic antibiotics due to capillary leakage and edema [9] | Reduced metabolic clearance due to cytokine-mediated downregulation of metabolic enzymes [9] | Hydrophilic antibiotics (β-lactams, glycopeptides, aminoglycosides); Voriconazole [9] | Higher initial loading doses often required; Altered maintenance dosing for hepatically cleared drugs [9] |
| Augmented Renal Clearance (ARC) | Minimal direct effect | Markedly increased renal clearance (CrCl >130 mL/min/1.73m²) [9] | Renally eliminated hydrophilic antibiotics (β-lactams, glycopeptides, aminoglycosides) [9] | Subtherapeutic exposure common; Requires higher doses or more frequent administration [9] |
| Hypoalbuminemia | Increased Vd for highly protein-bound drugs [9] | Increased clearance of highly protein-bound drugs [9] | Highly protein-bound antibiotics (ceftriaxone, ertapenem, teicoplanin) [9] | Increased free fraction may enhance efficacy but also increase toxicity risk [9] |
| Acute Kidney Injury (AKI) | Minimal direct effect (unless fluid overload) | Markedly decreased renal clearance [9] | Renally eliminated antibiotics [9] | Drug accumulation and toxicity risk; Requires dose reduction or extended dosing intervals [9] |
| Extracorporeal Therapies (CRRT, ECMO) | Variable effects depending on circuit components and flow rates [9] | Enhanced clearance during CRRT; Variable effects with ECMO [9] | hydrophilic antibiotics with low protein binding [9] | Highly variable drug removal; Therapeutic drug monitoring essential [9] |
Site-Specific Penetration Challenges
The primary infection site introduces additional variability in antibiotic exposure due to differing physiology that affects drug penetration. Table 2 summarizes key infection sites and their implications for dosing strategy.
Table 2: Infection Site Considerations and Dosing Implications
| Infection Site | PK Alteration | Representative Penetration Data | Dosing Strategy Adaptation |
|---|---|---|---|
| Bloodstream | Expanded Vd, Enhanced CL in sepsis [11] | Central compartment for distribution | Loading dose often required; Higher maintenance doses or continuous infusion [11] |
| Lung (ELF) | Variable penetration based on drug properties [11] | Piperacillin ELF:plasma ~0.50; Cefepime ELF:plasma ~1.04 [11] | Dose increase for hydrophilic agents with poor penetration [11] |
| CNS | Impaired permeability due to blood-brain barrier [11] | Limited penetration for many antibiotics | Maximal dosing regimens; Consider higher doses or alternative routes [11] |
| Soft Tissue | Variable based on perfusion and composition [11] | Contingent on body composition and drug properties | Consider obesity and tissue perfusion in dosing [11] |
Methodological Framework: Population PK Modeling Approaches
Core Components of Population PK Analysis
Population pharmacokinetic (popPK) modeling represents the methodological cornerstone of precision dosing by quantifying and explaining variability in drug concentrations [12] [13]. These models integrate data from multiple individuals, often pooled from several studies, to characterize typical population parameters while quantifying between-subject and residual variability [13]. The nonlinear mixed-effects modeling (NONMEM) approach first demonstrated by Sheiner et al. enables analysis of sparse clinical data, making it particularly valuable for critically ill populations where rich sampling is often impractical [14].
The structural model forms the foundation, typically employing compartmental approaches to describe the drug's ADME processes [13]. For example, piperacillin/tazobactam kinetics are optimally described by a two-compartment model, with parameters for clearance (CL), volumes of distribution (V1, V2), and intercompartmental clearance (Q) [4]. The statistical model then accounts for variability through between-subject variability (BSV), between-occasion variability (BOV), and residual unexplained variability (RUV) [13]. Covariate analysis identifies patient-specific factors (e.g., renal function, body size, inflammatory markers) that explain portions of the BSV, enabling more precise individualized predictions [13].
Population PK modeling follows a systematic process from data collection through model validation and simulation, with key considerations for critically ill patient covariates.
Experimental Protocol: Population PK Model Development
Protocol Title: Development of a Population Pharmacokinetic Model for Anti-infective Agents in Critically Ill Adults
Objective: To construct and validate a population PK model that characterizes the disposition of [Anti-infective Agent] in critically ill patients, identifying significant covariates that explain pharmacokinetic variability.
Materials and Requirements:
- Patient Population: Critically ill adults receiving [Anti-infective Agent] as part of standard care
- Sample Size: Typically 20-100 patients depending on expected variability [4] [3]
- Ethical Considerations: Approval from institutional review board with waiver of informed consent if using opportunistic sampling design
Methodology:
- Blood Sampling Protocol: Employ sparse sampling strategy (2-6 samples per patient) timed around drug administration. Collect demographic and clinical data including:
- Age, weight, height, body composition metrics
- Serum creatinine, albumin, C-reactive protein (CRP)
- Organ support modalities (CRRT, ECMO, vasopressors)
- Relevant genetic polymorphisms (e.g., CYP450 enzymes for voriconazole) [3]
Bioanalytical Methods:
- Quantify drug concentrations using validated method (e.g., HPLC, LC-MS/MS)
- Establish calibration curves and quality control samples
- Document precision and accuracy according to regulatory guidelines
Model Building:
- Develop structural model using nonlinear mixed-effects modeling (NONMEM)
- Test one-, two-, and three-compartment models
- Incorporate statistical model for between-subject and residual variability
- Perform stepwise covariate analysis evaluating clinical and demographic factors
Model Validation:
- Conduct bootstrap analysis to evaluate parameter precision
- Perform visual predictive checks to assess predictive performance
- Consider external validation if independent dataset available
Output Applications:
- Monte Carlo simulations to determine probability of target attainment (PTA) across patient subgroups [4]
- Development of model-informed precision dosing algorithms
- Identification of patient subgroups requiring alternative dosing strategies
Applied Research Tools: The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Antimicrobial PK/PD Research
| Research Tool | Function/Application | Representative Use in Critical Care PK |
|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Quantification of drug concentrations in biological matrices | High-sensitivity measurement of antimicrobial concentrations in plasma and tissue specimens [3] |
| Population PK Software (NONMEM, Monolix, R) | Nonlinear mixed-effects modeling | Development of population PK models from sparse clinical data [4] [3] |
| Monte Carlo Simulation Software | Prediction of probability of target attainment | Simulation of dosing regimens across virtual patient populations [4] |
| In Vitro Infection Models | Simulation of human PK profiles in laboratory setting | Assessment of bacterial killing and resistance prevention with human-simulated dosing regimens |
| Biomarker Assays (CRP, Procalcitonin, Cytokines) | Quantification of inflammatory response | Correlation of inflammatory status with altered drug clearance [9] [3] |
| Genetic Typing Platforms | Identification of pharmacogenetic variants | CYP2C19 genotyping for voriconazole metabolism prediction [3] |
| Protein Binding Assays | Determination of free drug fractions | Assessment of protein binding changes in hypoalbuminemia [9] [11] |
Experimental Protocol: Target Attainment Analysis
Protocol Title: Assessment of Pharmacodynamic Target Attainment for Anti-infective Regimens in Critically Ill Populations
Objective: To evaluate the probability of achieving pharmacokinetic/pharmacodynamic targets for [Anti-infective Agent] across different renal function subgroups and dosing regimens.
Methods:
- Population PK Model: Utilize previously developed population PK model for [Anti-infective Agent] with key covariates including estimated glomerular filtration rate (eGFR) and body size [4].
Monte Carlo Simulations:
- Generate virtual population (n=10,000) representing the target critically ill patient demographic
- Incorporate distributions for key covariates (renal function, body size, albumin)
- Simulate concentration-time profiles for standard and alternative dosing regimens
PD Target Definition:
Probability of Target Attainment (PTA) Calculation:
- Calculate PTA for each regimen across MIC distribution
- Determine cumulative fraction of response (CFR) for relevant pathogen populations
Output Analysis:
- Identify regimens achieving PTA >90% at relevant MIC values
- Recommend optimal dosing strategies for specific renal function subgroups
- Highlight patient populations at risk of subtherapeutic exposure
Case Applications and Clinical Translation
Exemplar Implementation: β-lactam Dosing Optimization
Recent research with piperacillin/tazobactam demonstrates the power of population PK approaches to identify suboptimal dosing in specific subpopulations. A 2025 study developed a population PK model in healthy adults to establish a baseline free from critical illness confounders, then performed Monte Carlo simulations across renal function subgroups [4]. The standard regimen (4g/0.5g q6h, 30-minute infusion) achieved a 90% probability of target attainment (PTA) for 50% fT>MIC at MIC values up to 4 mg/L in patients with normal renal function. However, this regimen frequently failed to achieve 90% PTA for more stringent targets (100% fT>MIC, 100% fT>4×MIC) or higher MICs, particularly in patients with augmented renal clearance (eGFR ≥130 mL/min) [4].
The precision dosing optimization workflow progresses from standard regimens through population PK analysis to targeted recommendations for at-risk subgroups.
Voriconazole Precision Dosing in Critically Ill Populations
Voriconazole exemplifies the challenges of antimicrobial dosing in critical illness, with its complex pharmacokinetics featuring significant interindividual variability, non-linear kinetics, and multiple influencing factors including inflammation and genetic polymorphisms [3]. A 2025 study of COVID-19-associated pulmonary aspergillosis (CAPA) patients developed a population PK model identifying voriconazole's apparent clearance (CL/F) at 3.17 L/h and volume of distribution (V/F) at 135 L for a standard patient [3]. Covariates significantly influencing clearance included continuous renal replacement therapy (CRRT), C-reactive protein (CRP), gamma-glutamyl transpeptidase, aspartate aminotransferase, and platelet count [3]. Monte Carlo simulations demonstrated that patients on CRRT required both higher loading doses and increased maintenance doses compared to those not on CRRT [3].
The integration of therapeutic drug monitoring (TDM) with model-informed precision dosing represents the most effective approach for addressing the extreme pharmacokinetic variability observed in critically ill patients [9]. Proactive TDM is recommended for vancomycin, teicoplanin, aminoglycosides, voriconazole, β-lactams, and linezolid in this population [9]. When combined with population PK models and Bayesian forecasting, TDM enables real-time dose individualization that accounts for each patient's unique and dynamic pathophysiology.
The imperative for precision dosing in critically ill patients stems from the profound alterations in antimicrobial pharmacokinetics that render standard dosing regimens inadequate. Population PK modeling provides the methodological foundation for understanding and predicting this variability, enabling the development of individualized dosing strategies that maximize therapeutic efficacy while minimizing toxicity. The integration of covariate data, therapeutic drug monitoring, and model-informed precision dosing represents the future standard for antimicrobial therapy in this vulnerable population. As drug development continues to address multidrug-resistant infections, these approaches will become increasingly essential for preserving the efficacy of new antimicrobial agents.
Critically ill patients present profound challenges for pharmacotherapy, particularly anti-infective dosing, due to extensive pathophysiological alterations that disrupt normal drug pharmacokinetics (PK). The complex interplay of haemodynamic, metabolic, and biochemical derangements significantly impacts drug absorption, distribution, metabolism, and excretion (ADME) [15]. Understanding these changes is paramount for developing effective population pharmacokinetic (popPK) models and optimizing dosing strategies for anti-infectives. This application note details the key challenges and provides structured experimental protocols for investigating these phenomena within anti-infective dose optimization research.
The core challenge lies in the hyperdynamic and highly variable nature of critical illness. Pathophysiological changes include endothelial dysfunction causing capillary leak, fluid shifts from aggressive resuscitation, altered protein binding, and organ dysfunction that collectively modify drug disposition [15] [16]. Furthermore, therapies like renal replacement therapy (RRT) and extracorporeal membrane oxygenation (ECMO) add another layer of complexity, contributing to significant inter- and intra-patient variability [15]. This document synthesizes current evidence to provide a framework for quantifying these alterations and integrating them into robust popPK models.
Core Pathophysiological Changes and Their Impact on PK
Altered Volume of Distribution and Fluid Shifts
The volume of distribution (Vd) is significantly perturbed in critically ill patients, primarily due to fluid shifts and altered tissue perfusion. The systemic inflammatory response in conditions like sepsis leads to widespread endothelial damage, increased capillary permeability, and fluid extravasation into the interstitial space [17] [16]. Resuscitation with intravenous fluids, while necessary for hemodynamic support, exacerbates this by expanding the extracellular fluid compartment.
Impact on Drug Classes:
- Hydrophilic Drugs (e.g., beta-lactams, aminoglycosides, glycopeptides): These drugs primarily distribute in the vascular and extracellular fluid compartments. The expansion of this space leads to a marked increase in Vd, resulting in lower plasma concentrations and a high risk of subtherapeutic exposure if standard loading doses are administered [17] [16] [18]. For instance, the Vd of vancomycin is reported to double in critical illness, and a 3 mg/kg loading dose of aminoglycosides fails to achieve target peak levels in 50% of patients [16] [18].
- Lipophilic Drugs (e.g., fentanyl, propofol, midazolam): The impact is more complex. While the vascular compartment may be expanded, reduced peripheral perfusion in the early "rescue" phase of critical illness can impede distribution into deep tissue and adipose compartments, potentially leading to higher initial plasma concentrations [16].
Table 1: Impact of Critical Illness on Volume of Distribution for Select Anti-infectives
| Drug Class | Example Drugs | Physicochemical Property | Direction of Vd Change | Clinical Implication | Supporting Evidence |
|---|---|---|---|---|---|
| Aminoglycosides | Gentamicin, Tobramycin | Hydrophilic | ↑ Increased by ~34% [18] | Standard 3 mg/kg load inadequate; consider 4-5 mg/kg [18] | [17] [16] [18] |
| Beta-lactams | Piperacillin, Meropenem | Hydrophilic | ↑ Significantly Increased | Subtherapeutic levels; increased loading dose required [15] [16] | [15] [16] [19] |
| Glycopeptides | Vancomycin | Hydrophilic | ↑ Can double [16] | Higher loading doses (e.g., 25-35 mg/kg) needed [16] | [15] [16] |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | Variable (Moderate lipophilicity) | ↑ Moderate Increase | Requires dose adjustment; TDM recommended [20] | [20] |
| Azoles | Voriconazole | Lipophilic | Variable (Influenced by protein binding) | Altered levels; TDM essential, especially with ECMO [20] | [20] |
Organ Dysfunction and Impact on Clearance
Organ dysfunction, particularly of the liver and kidneys, is a hallmark of critical illness and a major determinant of drug clearance.
Hepatic Dysfunction: Liver metabolism is compromised by reduced perfusion (shock, vasopressors) and direct cellular injury (hypoxic hepatitis, cholestasis) [15] [17]. The clearance of drugs is affected differently based on their extraction ratio (ER):
- High-ER Drugs (e.g., fentanyl, propofol): Clearance is blood flow-dependent. Reduced hepatic blood flow decreases clearance, increasing the risk of accumulation and toxicity [15] [17] [16].
- Low-ER Drugs (e.g., phenytoin, caspofungin): Clearance is dependent on enzyme function and protein binding. Systemic inflammation and cytokines (e.g., IL-6, TNF-α) downregulate cytochrome P450 (CYP450) enzyme activity, reducing metabolic clearance [15] [17] [21].
Renal Dysfunction and Augmented Renal Clearance (ARC):
- Acute Kidney Injury (AKI): Reduces the clearance of renally eliminated drugs (e.g., most beta-lactams, vancomycin, aminoglycosides), necessitating dose reduction to prevent toxicity [15].
- Augmented Renal Clearance (ARC): A hyperdynamic state in some critically ill patients (e.g., trauma, sepsis) leads to enhanced renal drug elimination, resulting in subtherapeutic concentrations if standard doses are used [22]. This is a key covariate in popPK models of beta-lactams [22].
Table 2: Impact of Organ Dysfunction and Inflammation on Drug Clearance Pathways
| Clearance Pathway | Pathophysiological Change | Impact on Drug PK | Example Drugs Affected | Key Inflammatory Biomarkers Linked to Change [21] |
|---|---|---|---|---|
| Hepatic Metabolism (CYP450) | Cytokine-mediated downregulation of enzyme activity & cellular hypoxia | ↓ Reduced metabolic clearance of Low-ER drugs | Phenytoin, Voriconazole, Valproic Acid | IL-6, TNF-α, CRP |
| Hepatic Blood Flow | Reduced perfusion from shock, vasopressors, ventilation | ↓ Reduced clearance of High-ER drugs | Fentanyl, Propofol, Midazolam | - |
| Renal Elimination | Acute Kidney Injury (AKI) | ↓ Reduced renal clearance | Vancomycin, Piperacillin, Meropenem | CRP, Procalcitonin |
| Augmented Renal Clearance (ARC) | ↑ Increased renal clearance | Beta-lactams, Vancomycin [22] | - | |
| Organ Cross-Talk | Acute Kidney Injury reducing CYP450 activity (reno-hepatic crosstalk) | ↓ Reduced non-renal clearance | Multiple drugs metabolized by CYP450 [17] | IL-6, TNF-α |
Experimental Protocols for PopPK Model Development
Protocol for a PopPK Study of Beta-Lactams in Critically Ill Adults
1. Study Objective: To develop a popPK model for (e.g., meropenem) in critically ill patients, identifying and quantifying the impact of covariates like fluid balance, organ function, and inflammatory biomarkers on drug exposure.
2. Patient Population:
- Inclusion: Adults (≥18 years) admitted to the ICU receiving meropenem for proven or suspected infection.
- Exclusion: Known hypersensitivity; pregnancy.
- Stratification: Plan to enroll patients across a spectrum of renal function (including those on CRRT) and fluid balance states.
3. Blood Sampling Strategy:
- Employ sparse sampling designed for popPK analysis (e.g., 2-4 samples per patient per dosing interval at random time points).
- Collect samples pre-dose (trough), and at various time points post-infusion (e.g., 0.5h, 2h, 4h after the start of infusion).
- Align sampling with routine clinical blood draws where possible.
4. Data Collection (Covariates): Systematically collect the following potential covariates, as they are frequently tested and often significant in popPK models [22]:
- Patient Characteristics: Age, sex, actual body weight, ideal body weight, BMI.
- Physiological Parameters & Biomarkers: Serum creatinine, Albumin, C-Reactive Protein (CRP), Procalcitonin.
- Organ Function & Support: Estimated CLCR (e.g., Cockcroft-Gault), need for RRT/CRRT, SOFA score.
- Fluid Dynamics: Cumulative fluid balance (24-hour and total), use of vasopressors.
5. Bioanalysis: Quantify meropenem plasma concentrations using a validated method (e.g., LC-MS/MS or HPLC-UV).
6. Modelling Workflow:
- Use non-linear mixed-effects modelling (NONMEM or equivalent).
- Develop a base model (structural + statistical).
- Perform stepwise covariate model building to identify significant relationships (e.g., between CLCR and drug clearance, fluid balance and volume of distribution).
- Validate the final model internally and, if possible, with an external dataset [19].
Figure 1: Workflow for a Population Pharmacokinetic (PopPK) Study in Critically Ill Patients.
Protocol for Assessing the Impact of Inflammation on CYP450 Metabolism
1. Study Objective: To evaluate the correlation between longitudinal inflammatory biomarker levels and the metabolic clearance of a CYP450 probe drug in critically ill patients.
2. Study Design: Prospective, observational pharmacokinetic study.
3. Methodology:
- Probe Drug: Administer a microdose or a therapeutic dose of a specific CYP substrate (e.g., midazolam for CYP3A4 activity).
- PK Sampling: Collect serial blood samples over a dosing interval to characterize the clearance of the probe drug.
- Biomarker Analysis: Measure plasma concentrations of inflammatory biomarkers (e.g., CRP, IL-6, TNF-α) concurrently with PK sampling [21].
- Data Analysis: Use non-linear regression or popPK modelling to quantify the relationship between the level of each biomarker and the clearance of the probe drug.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for PopPK Research in Critical Care
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| LC-MS/MS System | Gold-standard for quantitative bioanalysis of drugs and metabolites in biological matrices. | Essential for measuring antibiotic plasma concentrations (e.g., meropenem, vancomycin) with high sensitivity and specificity. |
| CRP / IL-6 ELISA Kits | Quantification of inflammatory biomarkers to correlate with altered PK parameters. | Useful for investigating cytokine-mediated downregulation of CYP enzymes [21]. |
| NONMEM Software | Industry-standard for non-linear mixed-effects modelling of population PK/PD data. | Used for model development, covariate analysis, and simulation. |
| R or Python with PopPK Libraries | Open-source environment for data preparation, model diagnostics, and visualization. | Packages like 'nlmixr' (R) facilitate model evaluation and comparison. |
| Certified Bioanalytical Standards | Reference standards for drugs and internal standards for method development and validation. | Critical for ensuring the accuracy and reproducibility of concentration data. |
The pathophysiological triad of altered volume of distribution, profound fluid shifts, and evolving organ dysfunction creates a highly dynamic and unpredictable pharmacokinetic environment in critically ill patients. Success in anti-infective dose optimization research hinges on the systematic collection of high-quality PK data and the integration of clinically relevant covariates—such as fluid balance, renal function, and inflammatory biomarkers—into robust popPK models. The experimental protocols and frameworks outlined herein provide a foundation for generating evidence that can be translated into model-informed precision dosing strategies, ultimately improving therapeutic outcomes in this vulnerable population.
Population pharmacokinetic (PopPK) modeling is a cornerstone of model-informed drug development (MIDD), enabling researchers to quantify and understand the sources of variability in drug exposure among individuals in a target population [13] [12]. For anti-infective drugs, which often possess narrow therapeutic windows and are used in diverse patient populations, this approach is particularly vital for optimizing dosing regimens to ensure both efficacy and safety [23] [24]. By integrating patient-specific covariates—such as age, weight, and organ function—PopPK models move beyond the "one dose fits all" paradigm toward personalized medicine, allowing for more informed dosing decisions in clinical practice [25]. The foundation of a PopPK analysis rests on three core model components: the structural model, the statistical model, and the covariate model. These components work in concert to describe the typical drug behavior in a population, quantify the random variability, and explain predictable sources of variability through patient characteristics [13] [1]. This article details these core components and provides practical protocols for their implementation in anti-infective dose optimization research.
Core Components of a PopPK Analysis
Structural Model
The structural model represents the theoretical, "platonic ideal" of how a drug is expected to behave in the body, describing the typical concentration-time course for a population [13] [1]. It is a mathematical representation of the pharmacokinetic (PK) processes of absorption, distribution, metabolism, and excretion (ADME) [13].
- Function and Purpose: The structural model acts as the scaffolding around which the observed data vary. Its primary purpose is to describe the central tendency of the PK data without accounting for variability between individuals [13] [26].
- Common Forms: The most prevalent structural models are mammillary compartmental models [1]. These models conceptualize the body as a series of compartments between which the drug flows.
- A one-compartment model describes the body as a single, homogenous unit and is suitable for drugs that distribute rapidly and evenly.
- Multi-compartment models (e.g., two or three compartments) are used when drug distribution occurs at different rates to various tissues. A central compartment (e.g., plasma and highly perfused organs) is typically connected to one or more peripheral compartments (e.g., less perfused tissues) [1].
- Key Parameters: The structural model is parameterized using fundamental PK parameters:
- Clearance (CL): The volume of plasma cleared of the drug per unit time, representing the body's efficiency in eliminating the drug [1].
- Volume of Distribution (V): The apparent volume in which a drug distributes in the body. Multi-compartment models will have a central volume (Vc or V1) and peripheral volume(s) (Vp or V2) [1].
- Inter-compartmental Clearance (Q): The flow rate of drug between the central and peripheral compartments in a multi-compartment model [27].
- Absorption Rate Constant (Ka): For extravascularly administered drugs (e.g., oral), this describes the rate of drug absorption into the systemic circulation [13].
Table 1: Common Structural Model Types and Their Applications in Anti-Infective PK
| Model Type | Description | Typical Use Case in Anti-Infectives |
|---|---|---|
| One-Compartment | Single, homogeneous unit with first-order elimination. | Drugs with simple, rapid distribution; initial model screening. |
| Two-Compartment | A central compartment (e.g., plasma) and one peripheral tissue compartment. | Most common model for drugs showing bi-phasic decline (e.g., Vancomycin [28]). |
| Three-Compartment | A central compartment with two peripheral compartments with different distribution rates. | Drugs with complex, multi-phasic distribution (e.g., some antibiotics in critically ill patients). |
| Transit Compartment | A series of compartments to model delayed absorption. | Drugs with complex absorption phases (e.g., Rifampicin [23]). |
Statistical Model
The statistical model quantifies the random variability that is not explained by the structural model alone. It accounts for the "noise" in the data and the differences between individuals [13] [1]. This component is essential because it formally recognizes that individuals in a population are not identical to the "typical" patient.
- Function and Purpose: To characterize and partition the different sources of random variability in the observed data, including differences between subjects, between occasions, and measurement error [13] [26].
- Types of Variability:
- Between-Subject Variability (BSV): Also known as Inter-individual Variability (IIV), this is the variability of a PK parameter (e.g., CL, V) between different individuals in the population. It is modeled by assuming that an individual's parameter value (Pᵢ) deviates from the typical population value (Pₚₒₚ) by a random effect (ηᵢ). This is typically assumed to follow a log-normal distribution to prevent physiologically impossible negative parameter values [13] [26]. The magnitude of BSV is often reported as a variance or coefficient of variation.
- Example:
CLᵢ = TVCL × exp(ηᵢ^CL), where ηᵢ^CL ~ N(0, ω²)
- Example:
- Between-Occasion Variability (BOV): This accounts for variability within the same individual when the drug is administered on different occasions (e.g., different cycles of therapy) [13].
- Residual Unexplained Variability (RUV): Also known as the residual error, this captures the discrepancy between an individual's model-predicted concentration and their actual observed concentration. This variability arises from assay error, model misspecification, timing inaccuracies, and within-subject fluctuations [13] [26]. Common statistical models for RUV include proportional, additive, or combined error structures.
- Between-Subject Variability (BSV): Also known as Inter-individual Variability (IIV), this is the variability of a PK parameter (e.g., CL, V) between different individuals in the population. It is modeled by assuming that an individual's parameter value (Pᵢ) deviates from the typical population value (Pₚₒₚ) by a random effect (ηᵢ). This is typically assumed to follow a log-normal distribution to prevent physiologically impossible negative parameter values [13] [26]. The magnitude of BSV is often reported as a variance or coefficient of variation.
Table 2: Components of the Statistical Model in PopPK
| Component | Symbol | Description | Common Model Form |
|---|---|---|---|
| Between-Subject Variability (BSV) | η (eta) | Random deviation of an individual's parameter from the population typical value. | Log-normal: Pᵢ = Pₚₒₚ × exp(ηᵢ) |
| Residual Unexplained Variability (RUV) | ε (epsilon) | Random difference between an individual's predicted and observed concentration. | Additive: Cₒᵦₛ = Cₚᵣₑ𝒹 + ε Proportional: Cₒᵦₛ = Cₚᵣₑ𝒹 × (1 + ε) Combined: Cₒᵦₛ = Cₚᵣₑ𝒹 × (1 + ε₁) + ε₂ |
Covariate Model
While the statistical model quantifies random variability, the covariate model aims to explain a portion of the BSV by identifying patient-specific characteristics (covariates) that have a systematic, predictable influence on PK parameters [13] [25].
- Function and Purpose: To establish quantitative relationships between clinically relevant patient factors and PK parameters, thereby reducing the unexplained BSV and enabling more precise, individualized dosing [13] [26].
- Common Covariates in Anti-Infective Research:
- Demographic: Body size (weight, fat-free mass), age (including postmenstrual age in pediatrics), sex [13] [23].
- Organ Function: Creatinine clearance (CRCL) or serum creatinine for renal function; liver enzyme levels or bilirubin for hepatic function [24] [27].
- Clinical Status: Serum albumin levels, disease status (e.g., HIV, diabetes), APACHE-II score in critically ill patients [23] [27].
- Genetic Factors: Polymorphisms in drug transporter genes (e.g., SLCO1B1 for Rifampicin) or metabolizing enzymes [23].
- Modeling Relationships: Covariates are incorporated into the model using mathematical functions. For example, the effect of body weight on clearance is often modeled using a power function:
CLᵢ = TVCL × (Weightᵢ / 70)^θᶜᴸ × exp(ηᵢ^CL)where TVCL is the typical clearance for a 70 kg individual, and θᶜᴸ is the estimated exponent describing the strength of the relationship.
Table 3: Examples of Covariate Effects on Anti-Infective PK Parameters
| Drug | Covariate | Effect on PK Parameter | Clinical Implication |
|---|---|---|---|
| Rifampicin [23] | Fat-free mass (FFM) | Increases Clearance (CL) | Dosing based on FFM may be more rational than total body weight. |
| Polymyxin B [27] | Albumin (ALB) Level | Explains variability in CL | Critically ill patients with low ALB may have altered clearance. |
| Polymyxin B [27] | Age | Explains variability in Volume of Distribution (Vd) | Older patients may have a different volume of distribution. |
| Vancomycin [28] | Creatinine Clearance (CLcr) | Primary determinant of CL | Dosing must be adjusted based on renal function. |
| Colistin [24] | Renal Function | Significantly impacts CL | Dosing optimization required in lung transplant recipients. |
The following workflow diagram illustrates the integration of these three core components in a typical PopPK model development process.
PopPK Model Development Workflow
Experimental Protocols for PopPK Model Development
Protocol for Structural Model Development
Objective: To identify the compartmental model that best describes the typical concentration-time profile of the anti-infective drug in the population.
- Data Preparation: Assemble a dataset containing all drug concentration measurements and corresponding sampling times. For drugs administered extravascularly (e.g., orally), include the dose and dosing time [1].
- Exploratory Data Analysis: Create semi-logarithmic plots of concentration versus time for all individuals. Visually inspect the plots to identify the number of distinct exponential phases in the concentration decline, which provides an initial indication of the required number of compartments [1].
- Base Model Building:
- Start by fitting a one-compartment model with first-order elimination.
- Progress to more complex models (e.g., two-compartment, three-compartment) if the data support the additional complexity.
- For oral drugs, test different absorption models: first-order, zero-order, or transit compartment models to handle complex absorption patterns, as was beneficial for Rifampicin [23].
- Model Comparison: Compare competing structural models using objective function value (OFV), Akaike Information Criterion (AIC), and Bayesian Information Criterion (BIC). A decrease in OFV of >3.84 (p<0.05, χ² distribution, 1 degree of freedom) for a nested model, or a lower AIC/BIC, suggests a significantly better fit [1]. Additionally, use goodness-of-fit plots to assess model performance visually.
Protocol for Covariate Model Building
Objective: To systematically identify and validate patient covariates that significantly explain the between-subject variability in key PK parameters.
- Covariate Selection: Based on physiological knowledge of the drug's disposition (ADME) and the patient population, compile a list of potential covariates. Common candidates for anti-infectives include weight, age, creatinine clearance, and albumin levels [13] [27].
- Stepwise Covariate Modeling (SCM):
- Forward Inclusion: Add each pre-specified covariate to the base model one at a time. Use the Likelihood Ratio Test (LRT), where a reduction in OFV > 3.84 (p<0.05) for 1 degree of freedom, indicates a significant improvement in the model fit. Retain all covariates that meet the significance criterion.
- Backward Elimination: Create a full model containing all covariates identified in the forward inclusion step. Then, remove each covariate from the full model one by one. A covariate is retained in the final model only if its removal causes a statistically significant increase in OFV (e.g., >6.63 for p<0.01, 1 df), ensuring only the most influential covariates are included [13].
- Model Evaluation: After identifying the final covariate model, perform a thorough evaluation. This includes:
- Goodness-of-Fit Plots: Observed vs. Population Predicted Concentrations; Observed vs. Individual Predicted Concentrations; Conditional Weighted Residuals vs. Time/Predictions.
- Visual Predictive Check (VPC): Simulating multiple datasets using the final model and comparing the simulated percentiles with the observed data to assess the model's predictive performance [23] [28].
- Bootstrap Analysis: Performing a non-parametric bootstrap to evaluate the stability and precision of the final parameter estimates [29].
Protocol for Model Validation and Dosing Simulation
Objective: To validate the final PopPK model and utilize it for clinical dosing optimization via Monte Carlo simulations.
- Model Validation:
- Internal Validation: Use techniques like bootstrap (as mentioned above) and data-splitting, where the model is developed on a training set and tested on a validation set [25].
- External Validation: If possible, test the model's predictive performance on a completely new, independent dataset from a different study or clinical center [23]. This is the strongest form of validation.
- Monte Carlo Simulation:
- Define the target patient population and their covariate distributions (e.g., range of weights, renal function) [23] [27].
- Using the final PopPK model (parameter estimates and their variances), simulate concentration-time profiles for a large number of virtual patients (e.g., 1000-5000) for a given dosing regimen [23] [27].
- Target Attainment Analysis:
- For anti-infectives, define a PK/PD target associated with efficacy. Common targets include the ratio of the area under the concentration-time curve to the minimum inhibitory concentration (AUC/MIC) or the time that free drug concentration remains above the MIC (fT>MIC) [27].
- Calculate the Probability of Target Attainment (PTA) as the proportion of virtual patients who achieve the predefined PK/PD target for a given dosing regimen.
- Repeat the simulation for multiple dosing regimens (e.g., different doses, intervals) to identify the regimen that achieves the desired PTA (e.g., ≥90%) in the target population [27].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for PopPK Analysis
| Tool Category | Specific Examples | Function in PopPK Analysis |
|---|---|---|
| Modeling Software | NONMEM, Monolix, Pmetrics (for R), Phoenix NLME | Industry-standard software for performing nonlinear mixed-effects modeling and parameter estimation [26] [27]. |
| Programming Languages | R, Python | Used for data preparation, visualization, simulation, and result analysis. R is particularly dominant in pharmacometrics. |
| Statistical Packages | mrgsolve (R package), xpose (R package) |
mrgsolve is used for simulating from PK/PD models; xpose is used for diagnostics and model evaluation [23]. |
| Bioanalytical Assays | LC-MS/MS | The gold standard for precise and accurate quantification of drug and metabolite concentrations in biological matrices (e.g., plasma) [27]. |
| Simulation Tools | Built-in simulators in Monolix/NONMEM, mrgsolve, Shiny applications |
Used for performing Monte Carlo simulations and creating user-friendly interfaces for model-based dosing [23]. |
Population pharmacokinetic (PopPK) analysis is a critical component of modern model-informed drug development (MIDD), enabling researchers to quantify and explain the variability in drug exposure among individuals from a target patient population. Regulatory agencies worldwide, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), recognize PopPK as a powerful tool for guiding drug development decisions and informing therapeutic individualization through tailored dosing strategies [30]. By integrating drug, disease, and trial information, PopPK analyses help support more efficient drug development and regulatory decisions, particularly for anti-infective agents where appropriate dosing is crucial for clinical efficacy and preventing resistance [31] [32].
The FDA's Division of Pharmacometrics (DPM) has established PopPK analyses as fundamental to its regulatory review process, with a strategic focus on improving drug dosing decisions for all patients [31]. Similarly, the EMA provides specific guidelines on reporting PopPK results to ensure sufficient detail for regulatory assessment [33]. The integration of PopPK analyses in marketing applications has in some cases alleviated the need for postmarketing requirements or commitments, accelerating patient access to novel therapies [30].
Regulatory Framework and Guidelines
FDA Guidance on Population Pharmacokinetics
The FDA's guidance document "Population Pharmacokinetics" represents the agency's current thinking on the application of PopPK analysis in drug development. Issued in February 2022 as a Level 1 guidance, this document assists sponsors and applicants of new drug applications (NDAs), biologics license applications (BLAs), abbreviated new drug applications (ANDAs), and investigational new drugs (IND) applications [30]. The guidance emphasizes the importance of PopPK analysis in guiding drug development and informing recommendations on therapeutic individualization, particularly through tailored dosing regimens [30].
The FDA's structured approach to PopPK review is managed through the Division of Pharmacometrics, which employs a multidisciplinary team including quantitative clinical pharmacologists, statisticians, engineers, and data management experts [31]. This division has developed standardized formats for PopPK reports to facilitate regulatory review and has made the integration of quantitative clinical pharmacology summaries a standard practice in NDA/BLA submissions [31]. The FDA also actively supports international harmonization of pharmacometrics standards through quarterly cluster meetings with global regulatory agencies and participation in ICH guidance development [31].
EMA Guidelines and Reporting Standards
The European Medicines Agency provides complementary guidance on how to present PopPK analysis results to enable secondary evaluation by regulatory authorities [33]. The EMA emphasizes that reporting should provide sufficient detail to allow assessment of the conducted analysis and conclusions drawn, with a focus on transparent methodology and results interpretation [33]. The EMA's scientific guidelines on clinical pharmacology and pharmacokinetics help medicine developers prepare marketing authorization applications for human medicines, establishing a comprehensive framework for PopPK integration in drug development [34].
Recently, the EMA has been preparing to release draft guidance on mechanistic models in Model-Informed Drug Development (MIDD), including PopPK models, with a concept paper released for public consultation from February to May 2025 [35]. This initiative aims to encourage wider use of these models and promote a standardized approach to their application in drug development [35].
Table 1: Comparative Overview of FDA and EMA PopPK Regulatory Guidance
| Aspect | FDA Approach | EMA Approach |
|---|---|---|
| Primary Guidance Document | Population Pharmacokinetics Guidance for Industry (February 2022) [30] | Reporting the results of population pharmacokinetic analyses [33] |
| Regulatory Scope | NDAs, BLAs, ANDAs, IND applications [30] | Marketing Authorization Applications for human medicines [34] |
| Key Emphasis | Therapeutic individualization through tailored dosing [30] | Transparency and secondary evaluability of analyses [33] |
| Review Structure | Division of Pharmacometrics [31] | Committee for Medicinal Products for Human Use (CHMP) |
| Recent Developments | Standardized templates for PopPK reviews [31] | Draft guidance on mechanistic models in MIDD (2025) [35] |
PopPK Applications in Anti-infective Drug Development
Case Study: Aztreonam-Avibactam Dose Optimization
A recent application of PopPK in anti-infective development illustrates its critical role in dose optimization and regimen selection. A 2024 population pharmacokinetic/pharmacodynamic modeling study aimed to optimize aztreonam-avibactam dose regimens for adult patients [5]. The researchers developed a simultaneous aztreonam and avibactam PopPK model using pharmacokinetic data from two phase 3 trials, creating a two-compartment model with zero-order infusion and first-order elimination [5].
The final model incorporated 4,914 aztreonam plasma samples from 431 subjects and 18,222 avibactam plasma samples from 2,635 subjects, identifying time-varying creatinine clearance as a key covariate on clearance for both drugs [5]. Infection type also significantly influenced clearance and volume, with the lowest exposures observed in patients with complicated intra-abdominal infections (cIAI) [5]. The PopPK analysis demonstrated that the final aztreonam-avibactam dose regimens achieved joint pharmacodynamic target attainment (PTA) of 89% to >99% at steady state across renal function groups, while ceftazidime-avibactam plus aztreonam regimens proposed by the Infectious Diseases Society of America achieved joint PTA below 85% due to insufficient avibactam exposures [5].
Case Study: Teicoplanin Dosing Optimization
Another compelling example comes from a 2022 study that developed a PopPK model for unbound teicoplanin in Chinese adult patients [36]. This research highlights the importance of PopPK in optimizing dosing regimens for anti-infective agents with complex pharmacokinetic properties. The study collected 103 unbound teicoplanin concentrations from 72 patients and established a one-compartment pharmacokinetic model with first-order elimination [36].
The analysis identified that clearance and volume of distribution of unbound teicoplanin were positively correlated with estimated glomerular filtration rate (eGFR) and serum albumin concentrations, respectively [36]. Dosing simulation results demonstrated that standard dosing regimens failed to meet the treatment needs of all patients, requiring optimization based on eGFR and serum albumin concentrations [36]. The study found that high eGFR and serum albumin concentration were associated with reduced probability of achieving target unbound trough concentrations, providing critical insights for personalized teicoplanin therapy [36].
Table 2: Key Covariates Identified in Anti-infective PopPK Case Studies
| Drug | Population | Key Covariates | Clinical Impact |
|---|---|---|---|
| Aztreonam-Avibactam [5] | Adult patients with various infections | Time-varying creatinine clearance, infection type | Dosing optimization across renal function groups and infection types |
| Teicoplanin (unbound) [36] | Chinese adult patients | eGFR, serum albumin concentrations | Personalized dosing based on renal function and protein binding status |
| Aztreonam-Avibactam [5] | Patients with cIAI | Infection type (cIAI) | Identified subpopulation requiring special consideration for exposure targets |
Experimental Protocols for PopPK Analysis
PopPK Model Development Workflow
The standard methodology for developing PopPK models follows a structured workflow that integrates data collection, model development, validation, and simulation. The following diagram illustrates this process:
Protocol for PopPK Analysis in Anti-infective Development
1. Data Collection and Preparation
- Collect rich or sparse pharmacokinetic samples from clinical trials, ensuring appropriate timing relative to dosing [36]
- Record demographic data (age, weight, sex), physiological parameters (serum creatinine, albumin), and clinical laboratory values [36]
- Document precise dosing information (dose, frequency, infusion duration) and sampling times [36]
- For anti-infective agents, record pathogen susceptibility and infection site details [5]
2. Analytical Method Validation
- Employ validated bioanalytical methods (e.g., UPLC-MS/MS) for drug concentration measurement [36]
- For highly protein-bound drugs, implement ultrafiltration methods to determine unbound concentrations [36]
- Establish calibration curves and validate precision, accuracy, and recovery rates according to regulatory standards [36]
3. Model Development
- Utilize specialized software (e.g., NONMEM, R) for nonlinear mixed-effects modeling [36]
- Test structural models (one-compartment, two-compartment) to describe drug disposition [32]
- Implement statistical models to account for interindividual variability, interoccasion variability, and residual unexplained variability [32]
- Incorporate covariate relationships using forward addition/backward elimination procedures [5] [36]
4. Model Validation
- Apply goodness-of-fit plots to assess model performance [32]
- Conduct visual predictive checks to evaluate model predictive performance [32]
- Perform bootstrap analysis to assess parameter uncertainty and model stability [32]
- When applicable, use external validation with independent datasets [32]
5. Model Application and Simulation
- Execute Monte Carlo simulations to evaluate probability of target attainment for various dosing regimens [5] [36]
- Simulate drug exposure metrics under different clinical scenarios (various renal functions, albumin levels) [36]
- Identify optimal dosing strategies to maximize efficacy while minimizing toxicity [5]
Table 3: Essential Research Reagents and Tools for PopPK Analysis
| Tool/Reagent | Function | Application Example |
|---|---|---|
| NONMEM Software [36] | Nonlinear mixed-effects modeling platform | Primary software for PopPK model development and parameter estimation |
| R Statistical Environment [36] | Data assembly, exploratory analysis, and visualization | Data preprocessing, model diagnostics, and graphical presentation of results |
| UPLC-MS/MS System [36] | High-sensitivity drug concentration measurement | Quantification of drug concentrations in biological matrices |
| Centrifree Ultrafiltration Device [36] | Separation of unbound drug fraction | Determination of pharmacologically active unbound drug concentrations |
| Wings for NONMEM [36] | NONMEM execution and assistance | Streamlining model execution and output management |
| Clinical Data Standards [30] [33] | Regulatory-compliant data collection | Ensuring data quality and integrity for regulatory submissions |
Covariate Analysis in PopPK Modeling
The identification of clinically relevant covariates is essential for understanding sources of pharmacokinetic variability. The relationship between key covariates and PopPK parameters can be visualized as follows:
Population pharmacokinetic modeling represents a cornerstone of modern anti-infective drug development, providing a robust framework for understanding drug behavior in target patient populations. The regulatory frameworks established by the FDA and EMA emphasize the importance of PopPK analyses in supporting dosing recommendations and therapeutic individualization [30] [33]. As demonstrated by the case studies on aztreonam-avibactam and teicoplanin, PopPK approaches enable model-informed dose optimization that accounts for patient-specific factors such as renal function, serum albumin levels, and infection characteristics [5] [36].
The continued evolution of regulatory guidelines, including the EMA's upcoming guidance on mechanistic models [35] and the FDA's ongoing refinement of PopPK review standards [31], ensures that PopPK methodologies will remain essential tools for advancing anti-infective therapy. By implementing the experimental protocols and utilizing the research tools outlined in this document, scientists and drug development professionals can generate high-quality PopPK data to support regulatory submissions and optimize anti-infective dosing strategies for diverse patient populations.
Building and Applying PopPK Models: From Data to Clinical Decision-Making
In population pharmacokinetic (PopPK) modeling for anti-infective dose optimization, the quality of analytical outcomes is fundamentally dependent on rigorous data preparation. Critical issues including sparse sampling, outlier observations, and data below the quantification limit present significant analytical challenges that can substantially influence model development and subsequent dosing recommendations. This application note provides structured protocols and evidence-based solutions for addressing these pervasive data challenges, with specific emphasis on applications within antimicrobial pharmacometrics. The systematic approaches outlined herein enable researchers to transform complex, real-world data into reliable analytical datasets for robust population modeling and precision dosing strategies.
Handling Sparse Data in Pharmacokinetic Studies
Background and Challenges
Sparse sampling designs, where only a limited number of blood samples are collected per subject, are frequently necessary in clinical settings where intensive sampling is impractical, such as in critically ill patients, pediatric populations, or outpatient studies. Traditional pharmacokinetic analysis methods like standard two-stage (STS) approaches often fail to provide reliable parameter estimates from sparse data, potentially leading to biased results and suboptimal dosing recommendations [37].
Evidence-Based Protocol for Sparse Data Analysis
Protocol Title: Population Pharmacokinetic Modeling of Sparse Data Using Non-Parametric Adaptive Grid Algorithm
Experimental Validation: A post-hoc analysis of morphine pharmacokinetics demonstrated that sparse sampling with as few as three samples per subject could accurately characterize a complex 3-compartment model when analyzed with appropriate population methods [37]. The study compared traditional STS modeling with nonparametric adaptive grid (NPAG) population modeling in 14 healthy volunteers, with validation in 5 surgical patients.
Key Experimental Findings on Sparse Data Sufficiency:
Table 1: Predictive Performance of Sparse vs. Intensive Sampling for Morphine PK
| Sampling Strategy | Analysis Method | Mean Error (ME) | Root-Mean-Square Error | Model Structure Identified |
|---|---|---|---|---|
| 9 samples/subject | NPAG | 0.76 ng/mL | 25.8 ng/mL | 3-compartment |
| 3 samples/subject | NPAG | -1.0 ng/mL | 26.2 ng/mL | 3-compartment |
| Intensive sampling | STS | 4.43 ng/mL | Not reported | Inaccurate |
Methodological Workflow:
- Study Design Phase: Implement optimal sampling theory principles to identify informative time points for sparse sampling
- Data Collection: Collect a minimum of 3 strategically timed samples per subject based on optimal design calculations
- Model Development: Utilize NPAG or other nonlinear mixed-effects modeling software capable of handling sparse data
- Model Validation: Apply bootstrap methods and prediction-corrected visual predictive checks to evaluate model performance
- Dosing Optimization: Use final model parameters to simulate exposure profiles and optimize dosing regimens
Critical Considerations: The successful application of sparse sampling methodologies requires careful structural model identification from more intensively sampled pilot data before implementation in sparse sampling designs [37] [38].
Outlier Detection and Analysis in Clinical Datasets
Theoretical Framework for Outlier Characterization
Outliers in clinical and pharmacokinetic data can be systematically classified by three primary attributes: root cause, type, and measure. Proper characterization is essential for determining appropriate handling strategies [39].
Table 2: Classification Framework for Outliers in Pharmacometric Data
| Characteristic | Category | Description | Clinical Example |
|---|---|---|---|
| Root Cause | Error-based | Human or instrument errors | Entry of additional digit in weight field in electronic record |
| Fault-based | Underlying system breakdown | Congestive heart failure causing symptoms | |
| Natural deviation | Chance-based extreme values | Extremely tall individual with no pathology | |
| Novelty-based | New generative mechanism | Unexpected drug effect for unrelated indication | |
| Type | Point | Single anomalous observation | Patient with disease relative to healthy population |
| Collective | Cluster of related anomalies | Rare infectious disease cluster in geographic area | |
| Contextual | Abnormal in specific context | Pregnancy changes abnormal in general population but normal in pregnancy context | |
| Measure | Distance-based | Degree of deviation from expected | Systolic blood pressure relative to hypertension threshold |
| Probability-based | Statistical rarity of observation | Rare adverse event during therapeutic management | |
| Information-based | Novel patterns not in traditional descriptions | Novel signs/symptoms not part of traditional disease description |
Augmented Intelligence Protocol for Outlier Analysis
Protocol Title: Five-Step Augmented Intelligence Framework for Clinical Discovery Through Outlier Analysis
Methodology Overview: This protocol reframes clinical discovery as an outlier detection problem within a structured augmented intelligence framework, enabling systematic identification of novel observations that may lead to scientific breakthroughs [39].
Experimental Workflow:
Implementation Details:
- Define Patient Population: Establish clear inclusion criteria and clinical outcomes of interest for the target population
- Build Predictive Model: Develop multivariate models predicting expected outcomes using available clinical covariates
- Identify Outliers: Calculate inconsistency scores expressing deviation between model predictions and actual observations
- Expert Investigation: Subject matter experts review identified outliers to distinguish meaningful anomalies from noise
- Hypothesis Generation: Formulate testable scientific hypotheses based on investigated outliers
Application Note: This approach is particularly valuable in antimicrobial resistance research, where outlier patients with unexpected treatment responses may reveal novel resistance mechanisms or therapeutic opportunities [39] [40].
High-Throughput Screening Outlier Mining
Protocol Adaptation for Pharmaceutical Screening: In high-throughput screening for anti-infective compounds, outlier mining techniques enable identification of false negatives and structure-activity relationship (SAR) borderline compounds that may contribute substantially to robust SAR understanding [41].
Technical Implementation:
- Utilize one- and two-dimensional molecular descriptors to encode structural information
- Apply logistic regression to calculate hit/nonhit probability scores
- Compute inconsistency scores to identify outliers for validation experiments
- Prioritize false-negative outliers and SAR-compliant borderline compounds for follow-up
Management of Below Lower Limit of Quantification (BLQ) Data
Analytical and Clinical Significance of BLQ Values
BLQ data points occur when analyte concentrations fall below the lower limit of quantification (LLOQ) of bioanalytical methods. Traditional approaches that simply exclude these values can introduce significant bias in pharmacokinetic parameter estimation, particularly for drugs with complex elimination profiles or when characterizing terminal elimination phases [42].
Regulatory Context: While FDA Guidance on Bioanalytical Method Validation states that use of measurements below the LLOQ is "not recommended," senior FDA pharmacometricians have acknowledged that "from a pharmacometrics point of view one should use good scientific judgment to decide whether to include BLOQ observations or not. We are open to all reasonable approaches" [42].
Comprehensive Protocol for BLQ Data Handling
Protocol Title: Strategic Handling of BLQ Values in Pharmacokinetic Analysis
Experimental Validation: Research has demonstrated that meaningful drug disposition information can be extracted from values between the LLOQ and limit of detection (LOD), particularly when supported by companion pharmacokinetic and pharmacodynamic profiles [42]. The Beal "Method M3" implemented in NONMEM, which treats BLQ measurements as censored observations, has been widely adopted in pharmacometrics and shown to reduce parameter estimation bias.
Method Selection Framework:
Software Implementation in PumasNCA: The PumasNCA package provides sophisticated BLQ handling capabilities through the concblq argument, allowing different strategies based on BLQ location in the concentration-time profile [43]:
- First BLQ values: Measurements before first non-BLQ value (default: keep)
- Middle BLQ values: Measurements between non-BLQ values (default: drop)
- Last BLQ values: Measurements after last non-BLQ value (default: keep)
Practical Decision Framework:
Table 3: Strategic Approaches for BLQ Data Handling Based on Profile Position
| BLQ Location | Handling Method | Rationale | Potential Impact |
|---|---|---|---|
| Early timepoints | Set to missing | May represent absorption lag time | Potential impact on Cmax estimation |
| Between observed concentrations | Impute with LLOQ/2 or use M3 method | Maintains profile shape | Prevents AUC overestimation from linear interpolation |
| Terminal phase | Set to zero | Allows accurate terminal slope estimation | Prevents AUC overestimation from premature truncation |
| All values BLQ | Consider more sensitive assay | Data may be insufficient for PK characterization | Exclusion of subject from analysis may be necessary |
Advanced Integration Approaches: For complex modeling scenarios, incorporate companion pharmacodynamic data to inform the validity of drug concentration measurements falling below the LLOQ. When drug effects outlast measurable concentrations above the LLOQ, a systems PK/PD approach can supplement analytical uncertainty [42].
Integrated Data Cleaning Workflow for Anti-Infective PopPK Modeling
Comprehensive Quality Control Framework
Protocol Title: End-to-End Data Quality Assessment for Antimicrobial Population PK/PD
Workflow Implementation:
Case Study: Voriconazole in COVID-19-Associated Pulmonary Aspergillosis
Experimental Context: A recent PopPK study of voriconazole in patients with COVID-19-associated pulmonary aspergillosis (CAPA) demonstrated the critical importance of integrated data handling approaches in special populations [3]. The study developed a one-compartment model with first-order elimination using data from critically ill patients.
Key Covariate Findings:
- Voriconazole apparent clearance (CL/F) estimated at 3.17 L/h for standard CAPA patient
- Continuous renal replacement therapy (CRRT) significantly influenced voriconazole clearance
- C-reactive protein, gamma-glutamyl transpeptidase, aspartate aminotransferase, and platelet count identified as significant covariates
- Monte Carlo simulations supported higher loading and maintenance doses in patients on CRRT
Methodological Insights: The successful characterization of voriconazole pharmacokinetics in this complex population required appropriate handling of sparse sampling, potential outliers in critically ill patients, and BLQ values in the concentration-time data.
Table 4: Essential Research Reagents and Computational Tools for PopPK Data Preparation
| Tool/Resource | Function | Application Context |
|---|---|---|
| NONMEM | Nonlinear mixed-effects modeling | Population PK/PD model development with sparse data and BLQ handling |
| PumasNCA | Noncompartmental analysis | Sophisticated BLQ handling with location-specific rules |
| NPAG Algorithm | Nonparametric population modeling | Robust parameter estimation from sparse data designs |
| Logistic Regression | Hit probability scoring | Outlier identification in high-throughput screening |
| "Method M3" | Censored data handling | Maximum likelihood approach for BLQ data in NONMEM |
| HPLC/LC-MS/MS | Bioanalytical quantification | Drug concentration measurement with defined LLOQ |
| CYP Genotyping Assays | Metabolic phenotype characterization | Source of variability identification in outlier analysis |
| Optimal Design Software | Informative time point identification | Sparse sampling scheme optimization |
Robust data preparation methodologies for handling sparse data, outliers, and BLQ values are fundamental to successful population pharmacokinetic modeling and dose optimization in anti-infective research. The protocols and frameworks presented in this application note provide structured approaches for transforming challenging, real-world data into reliable analytical datasets. By implementing these evidence-based strategies, researchers can enhance the quality of PopPK models, leading to more precise dosing recommendations and improved therapeutic outcomes for anti-infective treatments, particularly in complex patient populations with limited sampling opportunities.
Structural model development forms the cornerstone of population pharmacokinetic (PopPK) modeling, a critical discipline in anti-infective dose optimization research. The selection of an appropriate compartmental model and the accurate characterization of absorption processes directly influence the predictive performance of models guiding therapeutic decisions [44] [45]. This protocol provides detailed methodologies for developing structural models, with specific application to anti-infective agents, to support robust PopPK analysis in drug development.
The process involves identifying a mathematical model that best describes the time course of drug concentrations in the body, comprising two fundamental components: the structural model, which defines the pharmacokinetic (PK) parameters and their relationship, and the stochastic model, which accounts for variability [46]. For anti-infectives, this is further integrated with pharmacodynamic (PD) indices to optimize dosing regimens against pathogenic targets [44] [45].
Theoretical Framework and Key Concepts
Fundamentals of Compartmental Modeling
Compartmental models are mechanistic models that simulate the movement of a drug between different physiological states or "compartments" [47]. These models are based on a system of ordinary differential equations (ODEs) that express the dynamics of drug absorption, distribution, and elimination [48] [47]. The compartments do not necessarily represent specific anatomical entities but rather groups of tissues with similar blood flow and drug affinity.
The most common compartmental structures used in PK modeling include:
- One-compartment model: Assumes instantaneous distribution throughout the body
- Two-compartment model: Considers a central compartment (blood and well-perfused organs) and a peripheral compartment (poorly perfused tissues)
- Multi-compartment models: Account for more complex distribution patterns
For anti-infective drugs, the selection of an appropriate compartmental structure is crucial for accurately predicting drug exposure at the infection site, which may be a specific tissue compartment [46].
Absorption Process Mechanisms
Drug absorption represents the transportation of the unmetabolized drug from the site of administration to the systemic circulation [49]. The primary mechanisms include:
- Passive diffusion: The drug moves according to the concentration gradient from higher to lower concentration without energy expenditure; this is governed by Fick's law of diffusion and is the most common absorption mechanism [49]
- Carrier-mediated membrane transport: Specialized transporter systems including active transport (energy-dependent) and facilitated diffusion (carrier-mediated but without energy requirement) [49]
- Paracellular transport: Passive movement through intercellular spaces
For anti-infective drugs, the absorption process can be influenced by physicochemical properties (solubility, permeability, pKa), formulation factors, and patient-specific physiological variables [49]. Understanding these mechanisms is essential for predicting bioavailability, particularly when extrapolating from intravenous to oral dosing regimens [45].
Selection of Compartmental Models
Model Selection Criteria
The process of selecting an appropriate compartmental model involves evaluating statistical criteria and physiological plausibility. Key considerations include:
Table 1: Criteria for Compartmental Model Selection
| Criterion | Description | Application to Anti-Infectives |
|---|---|---|
| Goodness-of-fit plots | Observed vs. predicted concentrations, residual plots | Assess model predictability across therapeutic range [46] |
| Akaike Information Criterion (AIC) | Compares model fit with penalty for parameters | Lower values indicate better parsimonious model [50] |
| Bayesian Information Criterion (BIC) | Similar to AIC with stronger penalty for complexity | Prevents overparameterization in population models [50] |
| Physiological plausibility | Parameter values consistent with known physiology | Volume of distribution related to body composition; clearance aligned with elimination pathways [46] [45] |
| Precision of parameter estimates | Relative standard errors of estimated parameters | RSE <30-50% for fixed effects, <50% for random effects [50] |
Types of Compartmental Models
The following diagram illustrates the decision pathway for selecting appropriate compartmental models in structural model development:
The workflow begins with analyzing the concentration-time profile to determine the appropriate model structure. Key model types include:
- One-compartment model: Appropriate when drug distribution is rapid and homogeneous, characterized by monoexponential decline in concentrations [51]. Suitable for drugs with limited tissue distribution.
- Two-compartment model: Characterized by biexponential decline, with an initial rapid distribution phase (α) followed by a slower elimination phase (β) [47]. Commonly used for anti-infectives with significant tissue distribution.
- Multi-compartment model: Necessary for drugs with complex distribution patterns, such as accumulation in deep tissues, characterized by polyexponential decline [46].
For anti-infectives, tissue distribution is particularly important as infection sites may be in peripheral compartments. Physiologically-based pharmacokinetic (PBPK) models represent a specialized approach that incorporates actual physiological and anatomical data to predict drug disposition [46].
Absorption Process Characterization
Modeling Absorption Kinetics
Accurate characterization of absorption processes is essential for predicting drug exposure, especially for orally administered anti-infectives. The following diagram illustrates the key processes in drug absorption and conversion:
The absorption process can be modeled using several mathematical approaches:
Table 2: Absorption Models for Anti-Infective Drugs
| Absorption Model | Mathematical Form | Application Context |
|---|---|---|
| First-order absorption | dA/dt = -ka × A | Most common approach for immediate-release formulations [50] |
| Zero-order absorption | dA/dt = k0 | Constant absorption rate over fixed duration; appropriate for controlled-release formulations |
| Transit compartment models | Series of compartments representing absorption sites | Delayed absorption; mimics complex gastrointestinal transit [51] |
| Mixed-order absorption | Combination of zero and first-order processes | Complex absorption patterns with simultaneous rapid and slow components |
Special Considerations for Anti-Infectives
For anti-infective drugs, several factors require special consideration in absorption modeling:
- First-pass metabolism: Orally administered drugs may undergo significant gut wall and hepatic metabolism before reaching systemic circulation, reducing bioavailability [49]
- Food effects: Co-administration with food can enhance (e.g., albendazole with lipids) or reduce (e.g., levodopa with proteins) absorption [49]
- Site-specific absorption: The small intestine, particularly the duodenum with its villi and microvilli, provides the largest surface area for absorption [49]
- Active metabolites: Many anti-infectives (e.g., artemisinin derivatives) are converted to active metabolites that contribute to efficacy [51]
Experimental Protocols
Protocol for Structural Model Development
Title: Systematic Development of Structural PK Models for Anti-Infective Agents
Objective: To develop and qualify a structural pharmacokinetic model comprising compartmental and absorption components for anti-infective drugs.
Materials and Reagents:
- PK concentration-time data from pre-clinical or clinical studies
- Pharmacometric modeling software (e.g., NONMEM, Monolix, Phoenix NLME)
- Computing resources for numerical integration of differential equations
Procedure:
- Data Preparation:
- Compile concentration-time data following single and multiple dosing
- Include relevant covariate information (demographics, pathophysiological factors)
- Ensure appropriate handling of below quantification limit (BQL) values
Base Model Development:
- Begin with simple one-compartment model with first-order absorption and elimination
- Progress to more complex models if simple model demonstrates inadequate fit
- Implement models using differential equations when closed-form solutions are insufficient
Model Implementation (Example for two-compartment model with first-order absorption):
Where A represents amount in each compartment, Vc and Vp are volumes of distribution, CL is clearance, Q is intercompartmental clearance, and ε is residual error
Model Selection:
- Compare objective function values (-2 log-likelihood) between nested models
- Utilize visual predictive checks to assess predictive performance
- Evaluate physiological plausibility of parameter estimates
Model Qualification:
- Perform bootstrap analysis to assess parameter precision
- Conduct visual predictive check to evaluate model simulation properties
- Apply cross-validation techniques where appropriate
Protocol for Absorption Time Lag and Conversion
Title: Characterization of Absorption Time Lag and Metabolic Conversion for Anti-Infective Drugs
Objective: To model delayed absorption and conversion to active metabolites for anti-infective agents with complex PK profiles.
Materials and Reagents:
- Concentration-time data for parent drug and major metabolites
- Information on administration conditions (fasting/fed state)
- In vitro metabolism data (if available)
Procedure:
- Data Requirements:
- Collect rich sampling during absorption phase (0-8 hours post-dose)
- Include metabolite concentrations when pharmacologically active
- Document administration conditions that may affect absorption
Model Structure (Adapted from [51]):
- Implement absorption lag time (tlag) when visual inspection shows delayed absorption
- For prodrugs requiring metabolic activation, include conversion compartment:
Parameter Estimation:
- Estimate absorption rate constant (ka) and lag time (tlag)
- For drugs with active metabolites, estimate conversion rate (k_conv) and metabolite elimination
- Incorporate known physiological information as Bayesian priors when appropriate
Model Evaluation:
- Compare observed and predicted concentrations for parent and metabolite
- Evaluate absorption phase with dedicated diagnostic plots
- Assess impact of absorption model structure on overall model performance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Structural Model Development
| Tool/Category | Specific Examples | Function in Model Development |
|---|---|---|
| Modeling Software | NONMEM, Monolix, Phoenix NLME, R with nlmixr | Platform for implementing and estimating PK models using nonlinear mixed-effects approaches [50] [46] |
| PBPK Platforms | GastroPlus, Simcyp, PK-Sim | Mechanistic modeling incorporating physiological and drug-specific data [46] |
| Data Management | R, Python, SAS | Data preparation, visualization, and diagnostic plotting [48] |
| Statistical Criteria | AIC, BIC, Likelihood Ratio Test | Objective comparison of competing models [50] |
| Visualization Tools | Xpose, ggplot2, vpc | Diagnostic plotting and model evaluation [48] |
Application to Anti-Infective Dose Optimization
The integration of structural PK models with PD targets is essential for anti-infective dose optimization. Key PK/PD indices include [44] [45]:
- AUC/MIC: Area under the concentration-time curve to minimum inhibitory concentration ratio
- Cmax/MIC: Peak concentration to MIC ratio
- %T>MIC: Percentage of dosing interval that concentrations exceed the MIC
For population PK modeling in special populations, such as pediatrics, the structural model must account for developmental changes in physiology. For example, in neonates and infants, increased body water content can increase the volume of distribution of hydrophilic drugs, while immature renal and hepatic function can reduce clearance [46] [45]. Similar considerations apply to elderly patients and those with organ dysfunction [45].
The structural model serves as the foundation for subsequent covariate model development, where patient factors such as body size, renal function, and age are incorporated to explain interindividual variability [50] [46]. This comprehensive approach enables model-informed precision dosing (MIPD) for anti-infective therapies, optimizing efficacy while minimizing toxicity and resistance development [46] [45].
In anti-infective dose optimization research, population pharmacokinetic (PopPK) modeling serves as a critical methodology for quantifying drug exposure-response relationships and identifying optimal dosing regimens across diverse patient populations. PopPK integrates classical pharmacokinetic compartment models with statistical principles to analyze drug behavior in populations, accounting for inter-individual variability and the influence of patient-specific factors [52]. This approach is particularly valuable for anti-infective development, where achieving target drug exposures at the site of infection is essential for clinical efficacy and preventing antimicrobial resistance.
The software tools used for PopPK analysis—including NONMEM, MATLAB/SimBiology, and ADAPT—provide specialized environments for building, validating, and simulating mathematical models that describe the time course of drug concentrations in biological systems. These platforms enable researchers to implement nonlinear mixed-effects models (NONMEM), which account for both fixed effects (population typical values and covariate relationships) and random effects (inter-individual and residual variability) [53]. By leveraging these tools, scientists can identify patient characteristics (e.g., weight, renal function, genetic polymorphisms) that significantly influence drug pharmacokinetics, thereby facilitating personalized dose optimization for anti-infective therapies.
Table 1: Core Software Platforms for Population Pharmacokinetic Modeling
| Software Platform | Primary Developer | Core Modeling Approach | Key Application in Anti-infectives |
|---|---|---|---|
| NONMEM | ICON PLC | Nonlinear Mixed-Effects Modeling (NONMEM) | Population PK/PD analysis and covariate screening [53] [52] |
| MATLAB/SimBiology | MathWorks | Graphical and programmatic modeling of biochemical systems [54] | Integrated PK modeling and systems pharmacology for anti-infectives |
| ADAPT | USC Biomedical Simulations Resource | Maximum likelihood and Bayesian estimation [52] | Experimental PK/PD model fitting and simulation |
NONMEM: Industry Standard for Population PK/PD
NONMEM (Nonlinear Mixed Effects Model) represents the gold standard software for population pharmacokinetic and pharmacodynamic analysis in pharmaceutical development and academic research. Initially developed by Beal and Sheiner, NONMEM utilizes FORTRAN-based programming to implement nonlinear mixed-effects modeling, which allows simultaneous analysis of sparse data collected from diverse patient populations [52]. This capability is particularly valuable in anti-infective research, where opportunistic sampling designs are often implemented in critically ill patients with variable physiological states. The software provides a flexible framework for estimating fixed effects (population typical values), random effects (inter-individual and residual variability), and covariate relationships that explain variability in drug exposure.
NONMEM's estimation methods include First Order (FO), First Order Conditional Estimation (FOCE), and Bayesian estimation methods, which enable robust parameter estimation even with complex model structures and sparse data structures [52]. The software has been extensively validated through decades of use in regulatory submissions, with numerous examples of PopPK analyses supporting drug approval and labeling recommendations. For anti-infective dose optimization, NONMEM facilitates the development of models that identify patient factors (e.g., renal impairment, obesity, critical illness) significantly influencing drug clearance and volume of distribution, thereby enabling precision dosing strategies.
Experimental Protocol for PopPK Analysis
Protocol Title: Population Pharmacokinetic Analysis of Anti-infective Agents Using NONMEM
Objective: To develop a population pharmacokinetic model for [Drug Name] that characterizes typical population parameter values, identifies significant covariates explaining inter-individual variability, and enables model-based simulation of optimized dosing regimens.
Materials and Equipment:
- NONMEM software (version 7.5 or higher)
- Dataset containing drug concentration-time points, dosing records, and patient covariates
- Pirana or PsN (Perl-Speaks-NONMEM) for workflow management [52]
- R or Xpose for diagnostic graphics and model evaluation
- High-performance computing cluster for computationally intensive runs
Methodology:
- Data Preparation and Assembly: Compile concentration-time data, dosing histories, and patient covariates (e.g., weight, serum creatinine, albumin, age) into a suitable dataset format (e.g., CSV). Ensure appropriate coding of missing data and verification of data consistency.
Base Model Development:
- Implement a structural pharmacokinetic model (e.g., one-compartment, two-compartment) using NONMEM control files
- Estimate population typical values for clearance (CL), volume of distribution (V), and inter-compartmental clearances (Q) if applicable
- Identify appropriate statistical model for inter-individual variability (exponential, proportional, or additive error models)
- Select residual error model that adequately describes variability between observed and predicted concentrations
Covariate Model Building:
- Conduct stepwise forward addition (p<0.05) of potential covariates (e.g., weight on CL and V, creatinine clearance on CL) based on physiological plausibility
- Perform backward elimination (p<0.001) to establish final covariate model
- Evaluate continuous covariates using power relationships and categorical covariates using fractional change parameterization
Model Evaluation:
- Generate standard goodness-of-fit plots: observations vs population predictions, observations vs individual predictions, conditional weighted residuals vs time/predictions
- Perform visual predictive checks (VPC) to assess model predictive performance
- Conduct bootstrap analysis to evaluate parameter precision and model stability
Model Application and Simulation:
- Execute Monte Carlo simulations to evaluate probability of target attainment for various dosing regimens [55]
- Generate exposure-response analyses linking PK parameters to efficacy or safety endpoints
- Recommend optimized dosing regimens based on simulation results for specific patient subpopulations
MATLAB/SimBiology: Integrated Modeling Environment
Platform Capabilities and Framework
MATLAB with the SimBiology extension provides a comprehensive computational environment for pharmacokinetic modeling, system biology analyses, and quantitative systems pharmacology (QSP) applications in anti-infective research. Unlike traditional command-line driven PK software, SimBiology offers both graphical and programmatic modeling tools that enable construction of complex reaction networks, integration of pharmacokinetic models with biochemical pathways, and exploration of system dynamics through simulation [54]. This integrated approach is particularly valuable for anti-infective dose optimization, where drug action involves complex interactions between host, pathogen, and drug components.
The SimBiology platform supports a range of modeling approaches, including mechanism-based PK/PD models that explicitly represent biological processes governing drug distribution to infection sites, bacterial killing kinetics, and emergence of resistance. Researchers can import external data from multiple sources (e.g., databases, Excel files), identify PK models using built-in PK fitting tools, and perform parameter estimation using maximum likelihood or Bayesian methods. For anti-infective applications, this enables development of sophisticated models that incorporate bacterial growth dynamics, time-dependent killing, and post-antibiotic effects—features essential for optimizing dosing regimens to maximize eradication and suppress resistance.
Experimental Protocol for Mechanism-Based PK/PD Modeling
Protocol Title: Mechanism-Based PK/PD Modeling of Anti-infectives Using MATLAB/SimBiology
Objective: To develop and validate an integrated pharmacokinetic-pharmacodynamic model for [Drug Name] that characterizes antimicrobial activity against target pathogens and supports dose regimen optimization.
Materials and Equipment:
- MATLAB R2020a or later with SimBiology toolbox installed
- Experimental data: concentration-time profiles, bacterial killing kinetics, protein binding measurements
- High-performance computing resources for parallel processing of simulations
- Custom MATLAB scripts for data preprocessing and results visualization
Methodology:
- Model Structure Definition:
- Construct structural PK model using SimBiology graphical interface or programmatic commands
- Define PD component using mechanism-based terms: bacterial growth, natural death, drug-induced killing, adaptive resistance development
- Implement relevant PK/PD index linking approach (e.g., %T>MIC, AUC/MIC, Cmax/MIC) based on drug characteristics [55]
Parameter Estimation:
- Load and preprocess experimental data (in vitro time-kill curves, in vivo PK profiles)
- Specify model parameters to be estimated (e.g., maximum killing rate, EC50, hysteresis parameters)
- Configure estimation algorithm (maximum likelihood, Markov chain Monte Carlo)
- Execute parameter estimation and assess convergence diagnostics
Model Validation:
- Conduct internal validation using data splitting or cross-validation techniques
- Perform external validation using independent datasets not used for model building
- Evaluate predictive performance through simulation-based calibration diagnostics
Clinical Translation and Simulation:
- Scale preclinical model to human physiology using allometric principles or physiologically-based pharmacokinetic (PBPK) approaches
- Execute Monte Carlo simulations to account for variability in PK parameters and MIC distributions [55]
- Calculate probability of target attainment (PTA) and cumulative fraction of response (CFR) for candidate dosing regimens
- Identify optimal dosing strategies that maximize PTA/CFR while minimizing toxicity risk
Figure 1: Workflow for Mechanism-Based PK/PD Modeling in MATLAB/SimBiology
ADAPT: Computational Tools for Pharmacokinetic Analysis
Software Framework and Methodologies
ADAPT (Automated Data Analysis and Parameter Estimation) is a software system developed at the University of Southern California Biomedical Simulations Resource that provides comprehensive tools for pharmacokinetic-pharmacodynamic modeling and simulation. The platform supports multiple estimation methods, including maximum likelihood approaches, Bayesian estimation, and nonparametric adaptive grid algorithms [52]. ADAPT's strength lies in its flexibility for handling complex experimental designs and its implementation of advanced algorithms for model identification and parameter estimation, making it particularly useful for pre-clinical anti-infective research where rich data sets are often available.
The software system consists of several interconnected programs, including ADAPT II and newer versions, which offer user-friendly interfaces for data entry, model specification, and results visualization. For anti-infective applications, ADAPT enables development of complex PK/PD models that incorporate factors such as tissue distribution to infection sites, protein binding effects, and time-dependent antimicrobial activity. The Bayesian estimation capabilities are especially valuable for incorporating prior information from in vitro studies or previous clinical trials, thereby improving parameter precision when analyzing limited data from special populations.
Experimental Protocol for Bayesian PK/PD Analysis
Protocol Title: Bayesian Population Pharmacokinetic Analysis Using ADAPT Software
Objective: To develop a Bayesian population pharmacokinetic model for [Drug Name] that incorporates prior knowledge and quantifies parameter uncertainty for precision dosing of anti-infectives.
Materials and Equipment:
- ADAPT software suite installed on Windows workstation
- Prior parameter distributions from pre-clinical studies or literature
- Patient concentration-time data with associated dosing records
- Covariate data (demographics, laboratory values, clinical characteristics)
Methodology:
- Data Configuration and Model Specification:
- Prepare dataset in appropriate format for ADAPT input
- Define structural PK model using differential equations or analytical solutions
- Specify prior distributions for key parameters based on previous studies or physiological constraints
Bayesian Parameter Estimation:
- Configure Markov Chain Monte Carlo (MCMC) sampling parameters (number of chains, iterations, burn-in period)
- Implement Metropolis-Hastings algorithm or Gibbs sampling for posterior parameter estimation
- Monitor convergence using trace plots and Gelman-Rubin statistics
Posterior Distribution Analysis:
- Extract and summarize posterior distributions for PK parameters
- Calculate credibility intervals for parameter estimates
- Evaluate shrinkage and other diagnostics for random effects
Model-Based Dose Individualization:
- Develop Bayesian forecasting algorithms for dose individualization
- Implement maximum a posteriori (MAP) Bayesian estimation for therapeutic drug monitoring
- Generate patient-specific dosing recommendations based on posterior parameter distributions and target exposure metrics
Table 2: Key Research Reagent Solutions for PopPK Modeling
| Reagent/Resource | Function in PopPK Analysis | Application Context |
|---|---|---|
| NONMEM Software | Nonlinear mixed-effects modeling for population analysis [52] | Population PK model development across all clinical phases |
| Pirana Model Manager | NONMEM run management and workflow organization [52] | Streamlining PopPK analysis and facilitating model diagnostics |
| R/Xpose Packages | Model diagnostic graphics and statistical evaluation [52] | Visualization of goodness-of-fit and model performance metrics |
| PsN (Perl-Speaks-NONMEM) | Automated covariate screening and model validation [52] | Efficient PopPK model development and robust model qualification |
| Monte Carlo Simulation | Assessment of probability of target attainment [55] | Dose regimen optimization and susceptibility breakpoint evaluation |
Comparative Analysis and Applications in Anti-infective Development
Software Selection Considerations
The selection of appropriate software for population pharmacokinetic modeling in anti-infective research depends on multiple factors, including study objectives, data characteristics, and analytical requirements. NONMEM remains the industry standard for population PK analysis in regulatory submissions, with extensive documentation in peer-reviewed literature and established workflows for model development and validation [52]. Its robustness for analyzing sparse data from clinical trials and identifying covariate effects makes it particularly valuable for late-stage anti-infective development. MATLAB/SimBiology offers superior flexibility for mechanism-based modeling and integration with systems biology approaches, making it ideal for early research phases where understanding biological mechanisms is paramount. ADAPT provides accessible Bayesian modeling capabilities that are especially useful for therapeutic drug monitoring applications and analysis of rich data from pre-clinical studies.
For anti-infective dose optimization specifically, the software platforms enable critical analyses including the determination of PK/PD targets such as %fT>MIC for beta-lactams, AUC/MIC for fluoroquinolones, and Cmax/MIC for aminoglycosides [55]. Through Monte Carlo simulations, researchers can evaluate the probability of achieving these targets across a population of virtual patients, thereby identifying dosing regimens most likely to achieve clinical success while suppressing resistance emergence. The integration of these computational approaches throughout drug development has become increasingly important for optimizing anti-infective therapies and addressing the growing challenge of antimicrobial resistance.
Figure 2: Population PK Modeling Process for Anti-infective Dose Optimization
Regulatory and Clinical Implementation
The application of population pharmacokinetic modeling in anti-infective development has gained significant recognition from global regulatory agencies, with model-informed drug development approaches now playing pivotal roles in dosing recommendations and label claims. The U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and other regulatory bodies have incorporated PopPK analyses into review processes, particularly for justifying dosing adjustments in special populations and supporting alternative dosing strategies [53] [52]. Software platforms like NONMEM and Phoenix have been specifically adopted by regulatory agencies for evaluating sponsor submissions, creating a clear pathway for model-based anti-infective development.
In clinical practice, PopPK models developed using these software tools have enabled precision dosing of anti-infectives through several mechanisms: (1) identification of patient characteristics (e.g., renal function, body size) that significantly impact drug exposure; (2) development of Bayesian forecasting algorithms for therapeutic drug monitoring; and (3) creation of model-informed dosing guidelines for special populations such as critically ill patients, pediatrics, and obese individuals. The continuous refinement of these models with real-world clinical data further enhances their predictive performance and extends their utility in optimizing anti-infective therapies across diverse healthcare settings.
In population pharmacokinetic (PopPK) modeling, understanding and quantifying the impact of patient-specific covariates is fundamental to optimizing drug therapy, particularly for anti-infective agents. Covariates are patient characteristics—such as renal function, body weight, age, or clinical status—that explain a portion of the inter-individual variability in drug exposure and response [22]. The primary goal of covariate analysis is to develop models that can inform precision dosing, ensuring that patients achieve drug concentrations sufficient for efficacy while minimizing toxicity [56]. This is especially critical in anti-infective therapy, where suboptimal exposure can lead to treatment failure and the development of antimicrobial resistance [22].
The process of covariate analysis is built upon a foundation of biological plausibility. For renally cleared drugs like many anti-infectives, renal function is a pre-specified, biologically justified covariate for clearance. Similarly, body size is often a key determinant of a drug's volume of distribution. The systematic identification and validation of these relationships allow for the creation of robust, generalizable models that improve dosing predictions across diverse patient populations [22].
Key Covariates and Their Quantitative Impact
Established Covariates in Anti-infective PopPK
Extensive research has identified a consistent set of covariates that significantly influence the pharmacokinetics of anti-infective drugs. A systematic review of PopPK studies for β-lactam antimicrobials in critically ill patients categorized 1,083 covariate instances, with patient characteristics, biomarkers, and physiological parameters being the most frequently investigated [22].
The table below summarizes the most commonly reported significant covariates and their typical effects on pharmacokinetic parameters.
Table 1: Key Covariates in Anti-infective PopPK Models
| Covariate Category | Specific Covariate | PK Parameter Most Affected | Typical Effect Direction | Example from Literature |
|---|---|---|---|---|
| Renal Function | Creatinine Clearance (CrCl)Estimated Glomerular Filtration Rate (eGFR) | Clearance (CL) | Positive Correlation | Piperacillin CL increases with higher eGFR [56]. Balcinrenone exposure (AUC) increases 1.44-fold as eGFR drops from 60 to 25 mL/min/1.73m² [57]. |
| Body Size & Composition | Total Body WeightLean Body MassBody Mass Index (BMI) | Volume of Distribution (V)Clearance (CL) | Positive Correlation | In critically ill patients, weight is a common covariate for V and CL [22]. In obesity, CL via glomerular filtration and active secretion increases with BMI [58]. |
| Clinical Status & Support | Continuous Renal Replacement Therapy (CRRT)Extracorporeal Membrane Oxygenation (ECMO) | Clearance (CL)Volume of Distribution (V) | Variable | CRRT was associated with a lower V for teicoplanin [59]. |
| Demographics | AgeGender | CLV | Variable | Gender was associated with a higher V for teicoplanin [59]. |
| Laboratory Biomarkers | Serum Albumin | CL (for high-extraction-ratio drugs)V (for highly protein-bound drugs) | Negative Correlation | Serum albumin is a commonly tested covariate [22]. |
Quantitative Impact of Renal Function and Weight
The impact of covariates is not merely qualitative but can be precisely quantified to guide dose adjustments.
Renal Function: For piperacillin/tazobactam, Monte Carlo simulations demonstrated that a standard regimen (4/0.5 g q6h) achieved a 90% probability of target attainment (PTA) for an MIC of 4 mg/L in patients with normal renal function. However, this PTA dropped significantly in patients with an eGFR ≥ 130 mL/min, indicating underdosing in those with augmented renal clearance [56]. This highlights that a one-size-fits-all dosing strategy for patients with a CrCl > 40 mL/min is often inadequate.
Body Weight and Obesity: A physiologically based pharmacokinetic (PBPK) analysis systematically evaluated the impact of obesity on renal drug clearance (CLr). The study found that CLr through both glomerular filtration and active tubular secretion increases with body mass index (BMI), though the extent depends on specific drug properties [58]. The analysis concluded that for individuals with a BMI above 30 kg/m², simple allometric scaling methods are not systematically accurate, and more sophisticated, model-informed dosing is required [58].
Experimental Protocols for Covariate Analysis
PopPK Model Development Workflow
The following diagram illustrates the standard workflow for developing a PopPK model, including the identification and testing of covariates.
Step-by-Step Protocol for Non-Linear Mixed-Effects Modeling
This protocol details the methodology for incorporating covariates into a PopPK model using non-linear mixed-effects modeling (NONMEM), as exemplified in recent studies [56] [57] [59].
Objective: To identify patient factors that significantly explain inter-individual variability (IIV) in PK parameters and quantify their impact.
Materials and Software:
- Software: NONMEM, R (with
xpose,ggplot2packages), Phoenix NLME, or other NLME software. - Data: Rich or sparse drug concentration-time data from the target patient population.
- Covariates: Patient demographics, clinical lab values, and physiologic parameters.
Procedure:
Data Assembly and Preparation:
- Compile a dataset where each row represents an observed concentration with corresponding time, dose, and patient ID.
- Merge all potential covariate data (e.g., weight, eGFR, serum albumin) into the dataset, keyed by patient ID.
- Explore data graphically (e.g., plots of PK parameters vs. covariates from a prior base model) to identify potential relationships.
Base Model Development:
- Develop a structural PK model (e.g., one- or two-compartment) without covariates.
- Estimate IIV for each PK parameter (e.g., CL, V) using an exponential error model:
P_i = TVP * exp(η_i), whereP_iis the parameter for individuali,TVPis the typical population value, andη_iis the random effect for IIV. - Select the base model using objective function value (OFV), goodness-of-fit plots, and precision of parameter estimates.
Covariate Model Building:
- Pre-specification: Define a list of biologically plausible covariate-parameter relationships to test based on the drug's properties (e.g., eGFR on CL, body weight on V).
- Forward Addition: Systematically test each pre-specified relationship by incorporating it into the base model. For a continuous covariate like weight, use a power model:
CL_i = TVCL * (WT_i / WT_median)^θ. For a categorical covariate like CRRT, use a proportional model:CL_i = TVCL * (1 + θ * CRRT_i). - A covariate relationship is considered statistically significant if its inclusion results in a reduction in the OFV (e.g., > 3.84 for 1 degree of freedom, p < 0.05).
- Backward Elimination: After adding all significant covariates in the forward step, refine the model by removing each covariate one at a time. A covariate is retained if its removal causes a large increase in OFV (e.g., > 6.63 for 1 degree of freedom, p < 0.01), ensuring a stringent final model.
Model Evaluation:
- Use bootstrapping to assess the robustness and precision of the final parameter estimates.
- Perform visual predictive checks (VPC) to simulate concentrations from the final model and compare them to the observed data, ensuring the model accurately captures the central trend and variability.
Model Application (Simulation):
- Use the final model to perform Monte Carlo simulations [56]. Simulate concentration-time profiles for thousands of virtual patients under different dosing regimens, covariate values, and pathogen MICs.
- Calculate the probability of target attainment (PTA) for each scenario, based on a predefined pharmacodynamic target (e.g., %fT>MIC).
- Recommend optimal dosing regimens that achieve a high PTA (e.g., ≥90%) across the range of relevant covariates.
Successful execution of a PopPK analysis requires a combination of software, data, and methodological rigor.
Table 2: Essential Resources for PopPK Covariate Analysis
| Category | Item | Function & Application |
|---|---|---|
| Software & Platforms | NONMEMPhoenix NLMER/Python | Industry-standard for NLME modeling.Commercial platform with GUI for PK/PD analysis.For data preparation, visualization, and model diagnostics. |
| Analytical Tools | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)Validated Bioanalytical Assay | Quantifies drug concentrations in biological samples (e.g., plasma) with high sensitivity and specificity [59]. |
| Key Methodologies | First-Order Conditional Estimationwith Interaction (FOCE-I)Monte Carlo Simulation (MCS) | A common estimation algorithm in NLME modeling to obtain accurate parameter estimates [59].Used to predict PK outcomes and PTAs for various dosing scenarios in diverse populations [56] [28]. |
| Data Prerequisites | Patient Covariate DatasetConcentration-Time Data | A curated dataset containing demographic, laboratory, and clinical parameters for each study subject.Serial or sparse drug concentration measurements linked to dosing history. |
The rigorous incorporation of covariates such as renal function and body weight is not an optional step but a cornerstone of robust population pharmacokinetic modeling. The methodologies outlined here—from systematic model building to simulation-based validation—provide a framework for moving beyond one-size-fits-all dosing. For anti-infective drugs, this approach is paramount to achieving precision dosing, improving patient outcomes, and combating the global threat of antimicrobial resistance. Future work will continue to refine these models, exploring novel covariates and integrating them into clinical decision support tools to bring model-informed precision dosing to the bedside.
The integration of Pharmacokinetic (PK) and Pharmacodynamic (PD) principles represents a cornerstone in modern anti-infective drug development and dose optimization research. PK/PD analysis describes the complex relationship between the time course of drug concentrations in the body (pharmacokinetics) and the resulting pharmacological effect (pharmacodynamics). This approach has proven invaluable for establishing rational dosage regimens, particularly for antimicrobial agents in both human and veterinary medicine [60]. In the context of population pharmacokinetic modeling for anti-infective dose optimization, exposure-response analysis provides the critical link between drug exposure at the infection site and the resulting antibacterial effect, enabling researchers to maximize efficacy while minimizing toxicity and the emergence of resistance [60] [61].
The fundamental importance of PK/PD analysis is underscored by its inclusion in regulatory guidelines, such as those from the European Medicines Agency (EMA), for the evaluation of medicinal products [60]. Furthermore, the approach aligns with the World Health Organization's global action plan on antimicrobial resistance, which identifies optimizing antimicrobial use as one of five strategic objectives [60]. From a clinical perspective, appropriate PK/PD understanding is essential for achieving optimal outcomes, especially in challenging patient populations such as critically ill patients where physiological alterations can significantly impact drug disposition and response [62].
Fundamental PK/PD Principles and Parameters
Core PK/PD Concepts and Terminology
The foundation of exposure-response analysis rests on several key concepts that bridge pharmacokinetics and pharmacodynamics:
- Minimum Inhibitory Concentration (MIC): The lowest concentration of an antimicrobial that inhibits visible growth of a microorganism under standardized conditions. This serves as the primary PD marker for antibacterial activity [63] [64].
- Pharmacodynamic Target (PDT): The magnitude of the PK/PD index required to achieve a desired level of predicted response, typically derived from animal models and in vitro studies during drug development [60].
- Probability of Target Attainment (PTA): The probability that a specific value of the PK/PD index associated with efficacy is achieved at a certain MIC, calculated as the percentage of simulated patients with an estimated PK/PD index equal to or higher than the value related to efficacy [60].
- Cumulative Fraction of Response (CFR): The expected population PTA given a population of microorganisms for a specific dosing regimen, representing the expected probability of success of a dosing regimen against bacteria in the absence of a specific MIC value [60].
PK/PD Indices for Anti-Infective Agents
Anti-infective drugs are categorized based on their pattern of antimicrobial activity, which determines the most appropriate PK/PD index for predicting efficacy [60] [63]:
Table 1: PK/PD Indices for Different Antibacterial Classes
| Activity Pattern | Primary PK/PD Index | Antibacterial Classes | Typical Target Values |
|---|---|---|---|
| Concentration-Dependent | fCmax/MIC or fAUC24/MIC | Aminoglycosides, Fluoroquinolones | fCmax/MIC: 8-10 (Aminoglycosides); fAUC/MIC: 125-250 (Fluoroquinolones) |
| Time-Dependent | %fT>MIC | β-lactams (Penicillins, Cephalosporins, Carbapenems) | 30-70% of dosing interval depending on pathogen and infection site |
| Concentration-Dependent with Time-Dependence | fAUC24/MIC | Vancomycin, Linezolid, Daptomycin, Colistin | Variable by drug (e.g., Vancomycin: fAUC/MIC ≥400) |
For concentration-dependent antibiotics, the antibacterial effect increases with higher drug concentrations, making the ratio of peak concentration (fCmax) to MIC or the area under the concentration-time curve (fAUC) to MIC the most predictive indices [63]. In contrast, for time-dependent antibiotics, the duration of exposure is more critical than the peak concentration, making the percentage of time that drug concentrations exceed the MIC (%fT>MIC) the most predictive index [60] [63]. It is essential to note that all PK/PD indices should be calculated using free (unbound) drug concentrations rather than total plasma concentrations, as MIC is a free concentration value [64].
Experimental Models for PK/PD Analysis
In Vitro PK/PD Models
In vitro PK/PD models provide a controlled environment for studying the dynamic interaction between drugs and pathogens without host variables. The two primary systems are:
- Peristaltic Pump Models: These systems simulate one-compartment, two-compartment, or multiple-compartment PK models. The basic setup consists of a storage compartment (blank medium), a central compartment (containing drug, bacteria, and medium), and an elimination compartment (waste medium) connected by rubber tubing [64]. A peristaltic pump controls the flow rate to simulate drug elimination, while a magnetic stirrer maintains homogeneous mixing, and a thermostat ensures optimal bacterial growth temperature.
- Hollow Fiber Models: These more sophisticated systems consist of thousands of hollow fiber tubes that simulate multiple compartments and allow for better simulation of in vivo conditions [64]. They enable researchers to study concentration-time profiles similar to those observed in humans or animals and can run for extended periods (days to weeks), making them suitable for studying resistance emergence.
Table 2: Comparison of Primary PK/PD Experimental Models
| Model Type | Key Components | Applications | Advantages | Limitations |
|---|---|---|---|---|
| In Vitro | Peristaltic pumps, hollow fiber systems, bacterial cultures, growth media | Initial PK/PD characterization, resistance studies, dose fractionation | Cost-effective, controlled conditions, high throughput | Lacks host immune factors, may not reflect tissue penetration |
| Ex Vivo | Drug-containing body fluids (serum, plasma, tissue cage fluid), bacterial inoculum | Assessment of protein binding effects, bacterial killing in biological matrices | Incorporates host protein binding, more physiologically relevant | Static drug concentrations, limited sampling volume |
| In Vivo | Animal models (mice, rats, pigs), infection models, sampling systems | Comprehensive host-drug-pathogen interactions, translational research | Includes all host factors, most clinically predictive | Ethical considerations, cost, interspecies differences |
Ex Vivo and In Vivo PK/PD Models
Ex vivo PK/PD models utilize drug-containing body fluids (such as plasma, serum, or tissue cage fluid) collected at various time points after drug administration to assess bacterial killing in a more physiologically relevant matrix than artificial media [64]. The tissue cage fluid (TCF) model is particularly valuable as it represents extracellular fluid that is often the target site for bacterial infections. This model involves surgically implanting a perforated chamber between muscle and skin, allowing granulation tissue to form and produce TCF that can be sampled over time [64].
In vivo PK/PD models provide the most comprehensive assessment of host-drug-pathogen interactions. The tissue cage infection model (TCIM) involves adding pathogens to implanted tissue cages and administering various dosage regimens, followed by sampling TCF for drug concentration and bacterial density measurements [64]. The target organ infection model (TOIM) involves direct inoculation of bacteria into target organs, administration of test drugs, and subsequent sampling of infected tissues for drug concentrations and bacterial counts [64]. These models most closely simulate clinical infections and provide data that typically correlate well with clinical treatment outcomes.
Research Reagent Solutions and Essential Materials
Table 3: Key Research Reagents and Materials for PK/PD Studies
| Category | Specific Items | Function/Application |
|---|---|---|
| Bacterial Culture Components | Mueller-Hinton Broth (MHB), Iso-Sensitest agar, specific bacterial strains (e.g., S. pyogenes, E. coli ATCC 25922) | Standardized medium for MIC determination and time-kill curve experiments; reference strains for PK/PD model development |
| PK/PD Model Systems | Hollow fiber infection models, peristaltic pumps, tissue cages (for animal models), multi-compartmental chambers | Simulation of human PK profiles in vitro; creation of biological fluid compartments for ex vivo studies |
| Analytical Tools | HPLC systems, mass spectrometers, automated bacterial cell counters, Etest strips, microdilution panels | Drug concentration measurement; bacterial population quantification; MIC determination |
| Specialized Reagents | Protein binding filters, tissue cage implants, serum/plasma collection tubes, specialized growth media | Assessment of free drug concentrations; creation of biological sampling compartments; sample processing and storage |
Methodological Workflow for Exposure-Response Analysis
The following diagram illustrates the comprehensive workflow for conducting PK/PD exposure-response analysis in anti-infective development:
Experimental Protocol: In Vitro Time-Kill Curve Assay
Purpose: To characterize the time- and concentration-dependent antibacterial activity of a compound against specific bacterial strains.
Materials:
- Test compound (reference standard)
- Bacterial strains (wild-type and clinically relevant mutants)
- Mueller-Hinton Broth or appropriate medium
- Sterile tubes or microplates
- Incubator at 35±2°C
- Colony counting equipment (automated or manual)
Procedure:
- Prepare logarithmic dilutions of the test compound in appropriate medium to achieve concentrations ranging from 0.25× to 64× MIC.
- Standardize the bacterial inoculum to approximately 5×10^5 to 1×10^6 CFU/mL in the test solutions.
- Incubate the samples at 35±2°C with constant shaking if necessary.
- Sample at predetermined time points (e.g., 0, 2, 4, 6, 8, 12, 24 hours).
- Perform viable counts by plating serial dilutions on appropriate agar plates.
- Include growth control (bacteria without antibiotic) and sterility control (medium only).
- Plot time-kill curves (log10 CFU/mL versus time) for each concentration.
Data Analysis:
- Determine bactericidal activity (typically defined as ≥3-log reduction in CFU/mL)
- Calculate bactericidal concentrations (MBC)
- Assess presence of adaptive resistance or paradoxical effects
- Fit data to mathematical models (e.g., Emax models) to estimate parameters like EC50 and Emax [65]
Experimental Protocol: Population PK Model Development
Purpose: To characterize the pharmacokinetics of a drug in a target population, accounting for between-subject variability and covariate effects.
Materials:
- Drug concentration data from preclinical and clinical studies
- Patient demographic and clinical data (covariates)
- Nonlinear mixed-effects modeling software (e.g., NONMEM, Monolix, R)
- Diagnostic plotting tools
Procedure:
- Prepare dataset including dosing records, concentration measurements, and patient covariates.
- Develop structural PK model (e.g., one-, two-, or three-compartment) using standard estimation methods.
- Identify and quantify between-subject variability on PK parameters.
- Identify and quantify residual unexplained variability.
- Conduct covariate analysis to identify patient factors (e.g., weight, renal function) influencing PK parameters.
- Validate the final model using internal (e.g., bootstrap, visual predictive check) and external validation techniques.
Data Analysis:
- Evaluate model goodness-of-fit using diagnostic plots
- Calculate precision of parameter estimates
- Perform model comparison using objective function values and information criteria
- Simulate concentration-time profiles for various dosing regimens and patient subgroups
Advanced PK/PD Modeling Approaches
Mechanism-Based PK/PD Modeling
Traditional PK/PD indices (fAUC/MIC, fCmax/MIC, %fT>MIC) are summary endpoints that lose detailed information about the time course of individual PK and PD processes [65]. Mechanism-based (or semimechanistic) PK/PD models provide a more comprehensive approach by characterizing the full time course of drug effects and incorporating prior knowledge of the biological system [65]. These models typically include components for:
- Bacterial growth kinetics (including different bacterial states)
- Drug-induced bacterial killing
- Adaptation mechanisms and resistance development
- Host immune system effects
The mathematical representation typically includes differential equations that describe the rate of change in bacterial populations in response to drug exposure, allowing for more accurate predictions of antibacterial effects under different dosing scenarios [65].
Innovative PD Parameters Beyond MIC
While MIC remains the most common PD parameter in PK/PD analyses, several limitations have prompted exploration of alternative approaches [64]:
- Mutant Prevention Concentration (MPC)-based PK/PD models: MPC defines the antimicrobial concentration that prevents the growth of the least susceptible single-step mutant in a large bacterial population. PK/PD models based on MPC aim to suppress resistance development by maintaining drug concentrations within the mutant selection window [64].
- Kill rate-based PK/PD models: These models use the bacterial kill rate constant as the primary PD parameter instead of MIC, providing a more dynamic representation of antibacterial activity that can be linked to PK profiles through direct effect models or more complex indirect response models [64].
- Multiple PD parameter-based models: These approaches integrate multiple PD parameters (e.g., MIC, MBC, post-antibiotic effect duration) to provide a more comprehensive characterization of the concentration-effect relationship [64].
The following diagram illustrates the relationship between different modeling approaches and their applications in drug development:
Application to Dose Optimization and Clinical Translation
The ultimate goal of PK/PD analysis in anti-infective development is to optimize dosing regimens for clinical use. This process typically involves:
Target Attainment Analysis: Using Monte Carlo simulation to estimate the probability of target attainment (PTA) for various dosing regimens against pathogens with different MIC values [60]. A regimen is generally considered adequate if it provides PTA >90% for the target PK/PD index [60].
Cumulative Fraction of Response (CFR) Calculation: Estimating the expected population probability of success against a population of microorganisms, which accounts for the local MIC distribution [60].
Dose Selection and Rationale: Integrating PTA/CFR results with safety considerations to propose optimal dosing regimens for different patient populations (e.g., critically ill patients, those with renal impairment) [62].
Susceptibility Breakpoint Determination: Using PK/PD analysis to establish epidemiological cutoffs (ECOFFs) and clinical breakpoints that define susceptible, intermediate, and resistant categories [60].
In special populations such as critically ill patients, additional considerations are necessary due to altered PK parameters. These patients often exhibit increased volume of distribution for hydrophilic antibiotics (due to fluid resuscitation and capillary leak) and augmented renal clearance (in early sepsis), which can lead to subtherapeutic antibiotic concentrations if standard dosing regimens are used [62]. In these cases, PK/PD analysis supports dose optimization through loading doses, extended or continuous infusions (for time-dependent antibiotics), and therapeutic drug monitoring.
The integration of PK/PD principles into anti-infective development represents a powerful approach for maximizing therapeutic efficacy, minimizing toxicity, and preserving the utility of existing antibiotics in the face of escalating antimicrobial resistance challenges.
Population pharmacokinetic (PopPK) modeling is a fundamental tool for optimizing anti-infective therapy in critically ill patients, a population characterized by significant physiological alterations and pharmacokinetic variability [66]. These models use a limited sampling strategy to quantify drug exposure and its variability, identifying patient-specific factors (covariates) that influence pharmacokinetic parameters [25]. This approach enables model-informed precision dosing (MIPD) and Bayesian forecasting, moving beyond the "one dose fits all" paradigm to tailor therapy for narrow therapeutic index antibiotics like vancomycin and beta-lactams [25]. In the intensive care unit (ICU), pathophysiological changes such as augmented renal clearance, capillary leak syndrome, and organ dysfunction profoundly alter antibiotic pharmacokinetics, increasing the risk of therapeutic failure or toxicity [67] [68]. This article details practical applications and protocols for implementing PopPK strategies to optimize anti-infective dosing in this vulnerable population.
PopPK for Vancomycin in the ICU
Clinical Context and Rationale
Vancomycin, a glycopeptide antibiotic, remains a cornerstone for treating serious Gram-positive infections, including methicillin-resistant Staphylococcus aureus (MRSA). Its efficacy is best correlated with the ratio of the area under the concentration-time curve to the minimum inhibitory concentration (AUC/MIC), with a target of 400–600 mg·h/L recommended to ensure efficacy while minimizing nephrotoxicity [69]. Traditionally, trough concentrations of 15–20 mg/L were used as a surrogate, but this approach has shown limited correlation with the optimal AUC/MIC target [69]. Critically ill patients present additional challenges due to fluctuating renal function and fluid status, making personalized dosing through PopPK and Bayesian software essential.
Key Study Findings and Data
A recent prospective cohort study investigated the minimum number of vancomycin levels (VLs) required for accurate AUC estimation using Bayesian software (PrecisePK) in critically ill patients [69]. The study compared five estimation methods against a reference AUC calculated via the trapezoidal rule.
Table 1: Accuracy and Bias of Different Vancomycin AUC Estimation Methods in Critically Ill Patients [69]
| AUC Estimate | Vancomycin Levels Used | Relative Accuracy (Mean ± SEM) | Bias (Mean ± SEM) |
|---|---|---|---|
| AUC-Ref | Peak, Beta, Trough (Trapezoidal) | Reference | Reference |
| AUC-1 | Peak, Beta, Trough | 0.976 ± 0.012 | 0.053 ± 0.009 |
| AUC-2 | Beta, Trough | Not Reported | Not Reported |
| AUC-3 | Peak, Trough | 0.976 ± 0.012 | 0.053 ± 0.009 |
| AUC-4 | Trough only | 1.072 ± 0.032 | 0.134 ± 0.026 |
| AUC-5 | None (Bayesian prior only) | 1.150 ± 0.071 | 0.270 ± 0.060 |
The study concluded that using two vancomycin levels (specifically peak and trough, AUC-3) provided a more accurate and less biased AUC estimation than methods using a single trough level or no levels [69]. This finding is critical for designing efficient and effective TDM protocols.
Detailed Experimental Protocol: Vancomycin PopPK Sampling and AUC Estimation
Objective: To accurately estimate the vancomycin AUC/MIC in a critically ill patient using a limited sampling strategy and Bayesian forecasting.
Materials:
- Therapeutic drug monitoring service access
- Bayesian software (e.g., PrecisePK)
- Standard phlebotomy equipment
- Vancomycin assay equipment (e.g., KIMS COBAS, Roche)
Procedure:
- Vancomycin Administration: Administer vancomycin via intermittent infusion. For a central venous catheter, infuse a dose of ≤1 g over at least 60 minutes and doses >1 g over at least 120 minutes, not exceeding an infusion rate of 10 mg/min [69].
- Blood Sampling: Obtain blood samples at strategically timed points:
- Peak Level: Draw sample 20 minutes after the end of the infusion.
- Trough Level: Draw sample 1 hour before the next scheduled dose.
- (Optional) Beta Level:* Draw sample 2 hours after the end of the infusion for a three-point estimation [69].
- Sample Analysis: Quantify vancomycin plasma concentrations using a validated method (e.g., kinetic interaction of microparticles in a solution - KIMS).
- Data Input and Bayesian Estimation: Enter the following into the Bayesian software:
- Patient demographics (age, weight, height, sex).
- Serum creatinine and calculated creatinine clearance.
- Dose administration history (dose, start/end times).
- Vancomycin plasma levels and their sampling times.
- Output and Dose Adjustment: The software will generate an individualized PK model and calculate the estimated AUC/MIC. Adjust the vancomycin dosing regimen to achieve the target AUC/MIC of 400–600 mg·h/L (assuming a MIC of 1 mg/L if unknown) [69].
Workflow Visualization
PopPK for Beta-Lactams in the ICU
Clinical Context and Rationale
Beta-lactam antibiotics (penicillins, cephalosporins, carbapenems) exhibit time-dependent killing, where the primary pharmacodynamic index for efficacy is the percentage of the dosing interval that the free drug concentration exceeds the pathogen's MIC (%fT > MIC) [68]. Critically ill patients are at high risk of subtherapeutic beta-lactam exposure due to expanded volume of distribution and augmented renal clearance [68]. While a target of 100% fT > MIC is often recommended, some evidence suggests more aggressive targets (e.g., 100% fT > 4xMIC) may be needed for critically ill patients or resistant pathogens, though this risks toxicity [68]. PopPK models help define the sources of variability and facilitate dosing individualization, often through prolonged infusions and TDM.
Key Study Findings and Data
International surveys show a significant evolution in beta-lactam dosing practices. Extended or continuous infusions are increasingly used to maximize the %fT > MIC target [70]. Meropenem and piperacillin/tazobactam are now administered as extended infusions by 51% and 42% of respondents, respectively [70]. TDM for these drugs is also growing, though availability is not universal [70]. A critical challenge is the external validation of existing PopPK models. One study evaluating eight meropenem PopPK models found considerable variability in their predictive performance in an independent ICU cohort, underscoring the necessity for local model validation before clinical implementation [19].
Table 2: International Survey Data on Beta-Lactam Dosing and TDM Practices in the ICU [70]
| Antibiotic | Preferred Infusion Method | % Using Extended/Continuous Infusion | % Using TDM |
|---|---|---|---|
| Meropenem | Extended Infusion | 51% | 39% |
| Piperacillin/Tazobactam | Extended Infusion | 42% | 43% |
| Vancomycin | Intermittent Infusion | N/A | 90% |
Detailed Experimental Protocol: Beta-Lactam TDM and PopPK Application
Objective: To achieve and maintain a target beta-lactam exposure (e.g., 100% fT > MIC) in a critically ill patient using TDM and PopPK principles.
Materials:
- Beta-lactam antibiotic (e.g., meropenem, piperacillin/tazobactam).
- Infusion pump capable of prolonged infusion.
- HPLC-UV or other validated drug assay.
- PopPK model or TDM guidance protocol.
Procedure:
- Initial Dosing: Administer a loading dose (e.g., meropenem 1-2 g over 30 min) followed by a maintenance dose via extended (e.g., over 3 hours) or continuous infusion.
- Steady-State Sampling: After at least 24 hours of therapy (to approach steady-state), collect a blood sample. For continuous infusion, a single random concentration is sufficient. For extended infusions, a trough sample taken just before the next dose is most practical [68].
- Sample Analysis: Determine the free (unbound) drug concentration using a validated method (e.g., high-performance liquid chromatography - HPLC).
- Target Attainment Analysis: Compare the free drug concentration to the MIC of the causative pathogen.
- For Continuous Infusion: The steady-state concentration (Css) should be ≥1-4 times the MIC (e.g., fCss ≥ 4xMIC) [68].
- For Extended/Intermittent Infusion: The goal is 100% fT > MIC. Using the measured concentration and knowledge of the dosing regimen, software can simulate whether this target is met.
- Dose Adjustment: If the drug concentration is subtherapeutic, increase the infusion dose or rate. If supratherapeutic and concern for toxicity exists, decrease the dose. Dosing software using PopPK models can provide precise adjustment recommendations.
Table 3: Key Research Reagent Solutions for PopPK of Anti-infectives
| Item | Function/Application | Examples / Notes |
|---|---|---|
| PopPK Software | Non-linear mixed-effects modeling to develop and validate PopPK models. | NONMEM, Pmetrics, Monolix, Phoenix NLME [71] [72]. |
| Bayesian Forecasting Software | Clinical decision support for real-time, model-informed precision dosing. | PrecisePK, TDMx [69] [66]. |
| Drug Assay Platforms | Quantification of drug concentrations in biological samples (plasma, microdialysate). | UPLC-MS/MS (gold standard), HPLC-UV, KIMS [69] [72]. |
| Covariate Data | Patient factors that explain PK variability; essential for model building. | Demographics, renal function (CrCL, eGFR), illness severity scores (APACHE II), clinical chemistry (albumin, bilirubin) [71] [72]. |
| Validation Datasets | Independent patient data used to test the predictive performance of a developed PopPK model. | Crucial for establishing model robustness and generalizability before clinical use [19]. |
Population pharmacokinetic modeling has transitioned from a research tool to a critical component of anti-infective stewardship in the ICU. For vancomycin, Bayesian software utilizing two drug concentrations provides a superior method for AUC estimation compared to traditional trough-only monitoring. For beta-lactams, PopPK models support the trend toward prolonged infusions and growing use of TDM to achieve time-dependent targets. The successful clinical application of these models requires careful attention to sampling protocols, model validation, and the integration of patient-specific covariates. As the field advances, the focus must remain on external validation of models and demonstrating that these sophisticated, individualized approaches ultimately improve patient outcomes in critically ill populations.
Optimizing Models and Overcoming Common PopPK Challenges in Anti-infective Development
In population pharmacokinetic (PopPK) modeling for anti-infective dose optimization, selecting the appropriate model is a critical step that directly impacts dosing recommendations and therapeutic outcomes. PopPK analyzes pharmacokinetic data at the population level, using nonlinear mixed-effects models to simultaneously evaluate data from all individuals in a study population [1]. These models describe the typical concentration-time course (structural model), account for random variability (statistical model), and identify patient characteristics (covariates) that explain variability in drug exposure [1]. The primary goal of most PopPK analyses is to identify population pharmacokinetic parameters and sources of variability, ultimately relating observed concentrations to administered doses through predictive covariates in a target population [1].
Model selection criteria provide a rigorous framework for comparing competing models during this process. In PopPK, model building is an iterative process where increasingly complex models are compared to simpler ones. Selection criteria help balance the trade-off between model complexity and goodness-of-fit, preventing both underfitting (poor predictive performance) and overfitting (model describes noise rather than underlying relationship) [1]. The objective function value (OFV), expressed as minus twice the log-likelihood (-2LL), serves as the foundation for comparison, with lower values indicating better model fit [1]. This application note focuses on the practical implementation of Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and Likelihood Ratio Tests (LRT) within PopPK workflows for anti-infective research.
Foundational Concepts and Mathematical Formulations
The Likelihood Ratio Test Framework
The Likelihood Ratio Test (LRT) is a fundamental statistical tool for comparing two nested models in PopPK analysis. Nested models occur when one model (the reduced model) is a special case of another (the full model), typically through restrictions on parameter values [1]. The LRT evaluates whether the additional parameters in the full model provide a statistically significant improvement in fit compared to the simpler reduced model.
The test statistic is calculated as: D = -2 × (log-likelihoodreduced - log-likelihoodfull) = OFVreduced - OFVfull
where D follows an approximate χ² distribution with degrees of freedom equal to the difference in the number of parameters between the two models [73]. In PopPK, the objective function value (OFV) is minus twice the log-likelihood of the model, making computation straightforward [1]. A significant p-value (typically < 0.05) indicates that the full model provides a better fit to the data than the reduced model.
Table 1: Critical Values for Likelihood Ratio Test (Chi-Square Distribution)
| Δdf | α=0.05 | α=0.01 | α=0.005 | α=0.001 |
|---|---|---|---|---|
| 1 | 3.84 | 6.63 | 7.88 | 10.83 |
| 2 | 5.99 | 9.21 | 10.6 | 13.82 |
| 3 | 7.81 | 11.34 | 12.84 | 16.27 |
| 4 | 9.49 | 13.28 | 14.86 | 18.47 |
| 5 | 11.07 | 15.09 | 16.75 | 20.52 |
The LRT is particularly suitable for comparing covariate models to base models in PopPK, as these models are naturally nested [1]. For instance, when evaluating whether renal function significantly affects drug clearance, the base model (without the renal function covariate) is nested within the full model (with the renal function covariate). This application enables structured, hypothesis-driven model development.
Information-Theoretic Criteria: AIC and BIC
Unlike LRT, information criteria like AIC and BIC can compare both nested and non-nested models, providing greater flexibility in model selection [74] [75]. These criteria balance model fit with complexity, penalizing the inclusion of unnecessary parameters.
The Akaike Information Criterion (AIC) is formulated as: AIC = -2 × log(L) + 2 × (k+1)
where L is the maximized likelihood of the model, and k is the number of parameters [74] [75]. The AIC rewards goodness-of-fit (as measured by the likelihood) but penalizes model complexity, thus helping to avoid overfitting [75]. The model with the lowest AIC value is generally preferred.
The Bayesian Information Criterion (BIC), also known as the Schwarz Bayesian Criterion, applies a stronger penalty for model complexity: BIC = -2 × log(L) + (k+1) × log(n)
where n is the sample size [74]. The stronger penalty term makes BIC more conservative than AIC, particularly with larger sample sizes, often resulting in the selection of simpler models [75] [76].
Table 2: Comparison of AIC and BIC for Model Selection
| Criterion | Formula | Penalty Term | Model Preference | Primary Strength |
|---|---|---|---|---|
| AIC | -2log(L) + 2(k+1) |
2(k+1) |
Larger, more predictive models | Predictive accuracy |
| BIC | -2log(L) + (k+1)log(n) |
(k+1)log(n) |
Simpler, more parsimonious models | Identifying "true" model |
For linear models with normally distributed errors, AIC can be simplified to: AIC ≈ n × log(SSE) - n × log(n) + 2(k+1)
where SSE is the sum of squared errors [74]. This formulation highlights the relationship between AIC and error minimization.
Practical Implementation in PopPK Workflows
Interpretation Guidelines and Decision Rules
Effective application of model selection criteria requires clear interpretation guidelines. For LRT, the difference in OFV between two nested models is compared against critical values from the χ² distribution (Table 1). A reduction in OFV of 3.84 points (for 1 degree of freedom, α=0.05) is considered statistically significant [73] [1].
For information criteria, Kass and Raftery [1] provide evidence strength categorizations for BIC differences: 0-2 points indicates "weak" evidence, 2-6 points indicates "positive" evidence, 6-10 points indicates "strong" evidence, and >10 points indicates "very strong" evidence in favor of the model with the lower BIC [1]. In practice, a drop in AIC or BIC of 2 points is often used as a threshold for considering one model superior to another [1].
When AIC and BIC provide conflicting recommendations, the modeling objectives should guide selection. AIC is generally preferred when the goal is predictive accuracy, as it favors models with better forecasting performance [75] [76]. BIC is often preferred when the goal is identifying the true underlying data structure, as it more strongly penalizes complexity and favors parsimonious models [75] [76]. This is particularly relevant in PopPK, where interpretable models with biological plausibility are valued over black-box predictors.
Integrated Model Selection Protocol for PopPK
A structured approach to model selection in PopPK studies ensures consistent and defensible decisions. The following protocol outlines a comprehensive workflow:
Protocol: Structured Model Selection for Population Pharmacokinetics
Establish Structural Base Model
- Begin with developing the structural model without covariates
- Compare one-, two-, and three-compartment models using OFV, diagnostic plots, and physiological plausibility [1]
- Select the base structural model that adequately describes the concentration-time profile
Covariate Model Building Using LRT
- For each potential covariate (e.g., body weight, renal function, age), test its inclusion using LRT
- Use a significance level of α=0.05 (ΔOFV > 3.84 for 1 parameter) for forward inclusion [73]
- Employ backward elimination with stricter criteria (α=0.01) to build a parsimonious final model
- Ensure all models are estimated using the same estimation method and data set
Final Model Selection Using Information Criteria
- Compile all biologically plausible models identified during covariate testing
- Calculate AIC and BIC for each candidate model
- Rank models by each criterion and identify top contenders
- When AIC and BIC disagree, prioritize based on study objectives: AIC for predictive accuracy, BIC for parsimony and theoretical interpretation [75] [76]
Final Model Validation
This protocol was applied in a systematic review of teicoplanin PopPK studies, where model selection criteria helped identify body weight, postmenstrual age, renal function, and albumin levels as key covariates influencing clearance in pediatric populations [77].
Research Reagents and Computational Tools
Table 3: Essential Software Tools for Population PK Model Selection
| Tool Category | Specific Software | Model Selection Implementation | Key Applications in PopPK |
|---|---|---|---|
| Professional PopPK Software | NONMEM, Monolix, Phoenix NLME | Automatic OFV calculation, LRT support | Gold-standard for PopPK model development and covariate testing |
| General Statistical Platforms | R, Python, Stata | AIC(), BIC() functions, various PK libraries | Model diagnostics, visualization, and comparative analysis |
| Specialized Pharmacometric Tools | PSN, Xpose, Pirana | Automated model candidate comparison | Workflow management and visualization of PopPK model selection |
Application in Anti-Infective Dose Optimization
In anti-infective research, model selection criteria directly impact dosing recommendations through their influence on the final PopPK model. For example, in a systematic review of tigecycline PopPK, model selection procedures identified hepatic function indicators, renal function markers, and body weight as key covariates influencing pharmacokinetics [78]. These findings directly informed dosing recommendations, including high-dose tigecycline (100mg, q12h) for drug-resistant bacterial infections and individualized dosing based on liver function [78].
The probabilistic interpretation of BIC differences is particularly valuable in this context, as it provides a quantitative measure of evidence for one model over another [1]. When coupled with clinical expertise, this evidence-based approach to model selection enhances confidence in the resulting dosing recommendations.
Model selection criteria also play a crucial role in evaluating predictive performance through visual predictive checks and Monte Carlo simulations [77]. In teicoplanin PopPK studies, model-based simulations assessed the probability of target attainment (PTA) against methicillin-resistant Staphylococcus aureus (MRSA), revealing that current dosing regimens may be inadequate when the minimum inhibitory concentration (MIC) is 2 mg/L [77]. These findings directly inform clinical practice and highlight the real-world impact of rigorous model selection.
AIC, BIC, and LRT provide complementary approaches to model selection in population pharmacokinetics for anti-infective dose optimization. LRT offers a hypothesis-testing framework for nested models, particularly during covariate selection, while AIC and BIC enable broader comparison of both nested and non-nested models based on information-theoretic principles. AIC tends to favor models with stronger predictive ability, making it suitable for forecasting applications, while BIC favors more parsimonious models, potentially offering better identification of the true data-generating mechanism. By implementing a structured model selection protocol that integrates these criteria with physiological plausibility and clinical relevance, researchers can develop robust PopPK models that reliably inform anti-infective dosing strategies across diverse patient populations.
In population pharmacokinetic (PPK) modeling, the assessment of model goodness-of-fit (GOF) is a critical step in developing a robust model that accurately represents drug behavior in the target population. For anti-infective dose optimization research, where precise exposure-response relationships directly impact therapeutic efficacy and safety, rigorous model evaluation is particularly crucial [79]. GOF diagnostics help determine how well the model describes the observed data, identify potential model misspecifications, and guide model improvement strategies. These evaluations rely heavily on visual inspection of diagnostic plots and statistical analysis of residual patterns, which together provide comprehensive insights into model performance [80] [4]. This protocol outlines standardized approaches for conducting and interpreting these essential diagnostic analyses within the context of anti-infective drug development.
Core Principles of Goodness-of-Fit Assessment
Fundamental Concepts
Goodness-of-fit evaluation in PPK modeling serves to verify that the structural model, inter-individual variability model, residual error model, and covariate relationships adequately describe the observed concentration-time data. The process involves both quantitative metrics and qualitative visual assessments to identify systematic trends that may indicate model deficiency [80]. In anti-infective research, where optimal dosing is paramount for overcoming infections while minimizing resistance development, a well-fitted model ensures accurate exposure estimates for pharmacodynamic target attainment [4].
The principle of parsimony guides much of model selection in pharmacokinetic analysis, favoring the simplest model that sufficiently represents the data without overparameterization [81]. This balance between complexity and explanatory power is particularly relevant when modeling anti-infective agents across diverse patient populations with varying physiological and pathological characteristics.
Diagnostic Workflow
The following workflow represents the standard process for conducting comprehensive goodness-of-fit evaluations in population pharmacokinetic modeling:
Key Diagnostic Plots and Their Interpretation
Primary Goodness-of-Fit Plots
GOF plots provide visual assessments of how well model predictions align with observed data. The following table summarizes the key diagnostic plots used in PPK model evaluation:
Table 1: Primary Goodness-of-Fit Diagnostic Plots in Population Pharmacokinetic Modeling
| Plot Type | Variables | Interpretation Guidelines | Common Patterns Indicating Deficiency |
|---|---|---|---|
| Observed vs. Population Predictions (PRED) | Y-axis: Observed concentrationsX-axis: Population predictions | Points should scatter randomly around the identity line (y=x) | Systematic trends (curvilinear patterns), funnel-shaped scatter (increasing variance with predictions) |
| Observed vs. Individual Predictions (IPRED) | Y-axis: Observed concentrationsX-axis: Individual predictions | Closer agreement with identity line expected compared to PRED | Significant deviations from identity line, systematic over/under-prediction in specific ranges |
| Conditional Weighted Residuals vs. Time (CWRES) | Y-axis: CWRESX-axis: Time after dose | Should scatter randomly around zero with uniform variance | Trends over time, unequal variance (heteroscedasticity), excessive outliers (>±4) |
| Conditional Weighted Residuals vs. Predictions | Y-axis: CWRESX-axis: Population predictions | Should show random scatter around zero across all prediction values | Funnel-shaped patterns, systematic over/under-prediction at high or low concentrations |
In the PPK analysis of ASC10, a double prodrug for COVID-19 treatment, researchers employed these standard GOF plots alongside visual predictive checks to validate their two-compartment model with transit compartment absorption [80]. The diagnostic plots confirmed appropriate model fit, supporting the conclusion that an 800 mg twice-daily dosing regimen would provide desirable exposure associated with clinical response.
Residual Analysis Methods
Residual analysis quantifies the differences between observed and model-predicted values, with specific types serving distinct diagnostic purposes:
Table 2: Residual Types and Their Applications in Model Diagnostics
| Residual Type | Calculation | Primary Application | Acceptance Criteria |
|---|---|---|---|
| Conditional Weighted Residuals (CWRES) | Normalized difference incorporating interindividual variability | Most powerful for detecting model misspecification | Random scatter between -4 and +4, with approximately 95% between -2 and +2 |
| Individual Weighted Residuals (IWRES) | Weighted based on individual predictions | Assessment of structural model adequacy | Similar distribution to CWRES but with individual focus |
| Normalized Prediction Distribution Errors (NPDE) | Non-parametric approach using simulation | More robust for sparse data situations | Should follow N(0,1) distribution; QQ-plots should align with identity line |
In the vancomycin PPK external validation study, researchers utilized NPDE alongside prediction error calculations to evaluate model performance across different patient populations [82]. The NPDE results demonstrated that all evaluated models showed obvious bias, highlighting the importance of thorough residual analysis before clinical application.
Advanced Diagnostic Approaches
Visual Predictive Check (VPC)
The Visual Predictive Check compares the distribution of observed data with model-based simulations to assess predictive performance. Prediction-corrected VPC (pcVPC) accounts for variability in dosing regimens and covariates, providing a normalized comparison [83] [84]. In anti-infective modeling, VPCs are particularly valuable for verifying that the model accurately captures the central tendency and variability of drug concentrations across the dosing interval, which directly impacts pharmacodynamic target attainment [4].
Partial Residual Plots (PRPs)
Partial residual plots serve as an integrated diagnostic tool that shows the relationship between response and a specific covariate after controlling for other covariates in the model [83]. In PPK modeling, PRPs help visualize whether covariate relationships have been appropriately captured in the final model. The process involves:
- Calculating partial residuals for the covariate of interest
- Normalizing observations to reference values for other covariates
- Plotting partial residuals against the covariate values
- Comparing the relationship with the model-predicted covariate effect
This approach enables "like-to-like" comparisons between observed data and model predictions, making it particularly valuable for identifying missed covariate relationships or inappropriate parameterization of included covariates [83].
Protocol: Comprehensive Goodness-of-Fit Assessment
Experimental Setup and Software Requirements
Table 3: Research Reagent Solutions for PPK Model Evaluation
| Tool Category | Specific Tools/Software | Primary Function | Application Notes |
|---|---|---|---|
| Modeling Software | NONMEM (v7.4+), Monolix, Phoenix NLME | Parameter estimation and model simulation | NONMEM remains industry standard; first-order conditional estimation with interaction (FOCEI) recommended |
| Statistical Programming | R (v4.0+), Python, SAS | Data preparation, diagnostic plotting, result analysis | R provides comprehensive packages (e.g., xpose, ggplot2) for diagnostic visualization |
| Diagnostic Packages | xpose4 (R), Pirana, Perl-speaks-NONMEM | Automated generation of diagnostic plots | xpose4 facilitates creation of standard GOF plots and calculation of various residuals |
| Visual Predictive Check | vpc (R package), custom simulation scripts | Predictive performance assessment | Prediction-correction essential for unbalanced designs or multiple dosing |
Step-by-Step Diagnostic Procedure
Phase 1: Initial Model Assessment
- Generate basic goodness-of-fit plots (observed vs. PRED, observed vs. IPRED, CWRES vs. time, CWRES vs. PRED)
- Examine plots for systematic trends and outliers
- Calculate numerical summary statistics (mean prediction error, root mean square error)
- Assess shrinkage for parameters and residuals
Phase 2: Residual Analysis
- Calculate conditional weighted residuals (CWRES) and individual weighted residuals (IWRES)
- Plot residuals against all covariates (continuous and categorical)
- Perform statistical tests on residual distributions (e.g., Shapiro-Wilk for normality)
- Identify patterns suggesting model misspecification
Phase 3: Predictive Check
- Perform visual predictive check with 500-1000 simulations
- Generate prediction-corrected VPC for unbalanced designs
- Compare observed percentiles (10th, 50th, 90th) with simulated confidence intervals
- Stratify VPC by key covariates when appropriate
Phase 4: Specialized Diagnostics
- Generate partial residual plots for all included covariates
- Perform case deletion diagnostics (e.g., COVSEARCH in NONMEM)
- Conduct leverage analysis to identify influential individuals
- Perform bootstrap analysis to assess parameter stability
The following workflow illustrates the relationship between different diagnostic techniques and how they inform model refinement decisions:
Interpretation Guidelines
Structural Model Deficiencies:
- Curvilinear patterns in observed vs. predictions plots suggest incorrect structural model
- Systematic trends in CWRES vs. time indicate misspecified absorption or elimination processes
- Unexplained bias in specific concentration ranges may require alternative clearance or volume models
Covariate Model Issues:
- Trends in residuals vs. covariates indicate missing covariate relationships
- Partial residual plots showing nonlinear relationships suggest incorrect parameterization
- Differences in residual patterns across subgroup strata require covariate inclusion
Variability Model Problems:
- Overdispersed residuals (excessive values outside ±4) suggest underestimated variability
- Heteroscedastic patterns (changing variance across predictions) require residual error model refinement
- High shrinkage (>30%) indicates insufficient information for estimating interindividual variability
In the piperacillin/tazobactam PPK analysis, researchers utilized these interpretation guidelines to identify body surface area-adjusted eGFR and body weight as significant covariates influencing drug clearance and volume of distribution [4]. The diagnostic plots confirmed the adequacy of the two-compartment model and identified opportunities for model refinement in specific patient subgroups.
Application in Anti-infective Dose Optimization
For anti-infective agents, appropriate goodness-of-fit is particularly crucial as model-informed dosing decisions directly impact pharmacodynamic target attainment and clinical outcomes [4] [82]. The exposure-response relationship for anti-infectives often features steep curves, where small changes in drug exposure can significantly impact bacteriological eradication or viral suppression.
In the PPK analysis of HIV antiretroviral therapies, including lenacapavir, bictegravir, and tenofovir alafenamide, researchers employed comprehensive goodness-of-fit assessments to validate a complex semi-mechanistic model incorporating viral dynamics and CD4+ T cell counts [84]. The model successfully characterized the exposure-response relationships, enabling optimization of dosing regimens for novel combination therapies. The diagnostic approach included prediction-corrected visual predictive checks stratified by drug class, which confirmed the model's ability to capture key aspects of viral dynamics and treatment response.
Similarly, in the population pharmacokinetic modeling of ASC10 for COVID-19 treatment, thorough goodness-of-fit evaluation supported the identification of food intake and body weight as influential covariates on ASC10-A pharmacokinetics [80]. The validated model enabled simulations demonstrating that an 800 mg twice-daily regimen provided desirable exposure associated with clinical response, highlighting the critical role of model diagnostics in anti-infective dose optimization.
Rigorous evaluation of goodness-of-fit through diagnostic plots and residual analysis is fundamental to developing robust population pharmacokinetic models for anti-infective drugs. The systematic application of these techniques ensures that models accurately characterize drug behavior across target populations, providing a reliable foundation for dose optimization decisions. As model-informed precision dosing continues to gain prominence in anti-infective therapy [79], standardized approaches to model evaluation become increasingly important for maximizing therapeutic efficacy while minimizing toxicity and resistance development.
Addressing Overparameterization and Model Stability
Overparameterization poses a significant threat to model stability and predictive performance in population pharmacokinetic (PopPK) modeling, particularly within anti-infective dose optimization research. An overparameterized model, possessing more parameters than can be justified by the available data, often leads to unstable parameter estimates, high estimation uncertainty, and poor generalizability to external datasets. This application note details standardized protocols for identifying and mitigating overparameterization, thereby enhancing the robustness of PopPK models critical for guiding anti-infective therapy. The implementation of model selection tools and machine learning-driven automation has demonstrated potential to improve prediction precision by 6–12% in some clinical applications, underscoring the tangible value of these methodologies [85].
The following tables consolidate key quantitative findings from recent investigations into model performance and stability.
Table 1: Performance Comparison of Model Selection Tools in Vancomycin MIPD
| Model Type | Data Set | Mean PAPE (%) | Mean PPE (%) | Key Improvement |
|---|---|---|---|---|
| Universally Best Model (UBM) | Training | 26.0 | 5.8 | Baseline |
| Model Selection Tool (MST) | Training | 22.8 | 4.7 | Precision ↑ 12% |
| Universally Best Model (UBM) | Validation | 30.2 | -2.8 | Baseline |
| Model Selection Tool (MST) | Validation | 28.4 | -1.5 | Precision ↑ 6% |
| MST (2 prior concentrations) | Validation | 18.9 | -1.0 | Optimal forecasting |
Table 2: Predictive Accuracy of ML-Enhanced PK Modeling Platforms
| Modeling Platform | Input Data Source | 2-fold AUC Prediction Accuracy | Key Feature |
|---|---|---|---|
| Traditional Bottom-up PBPK | In vitro experiments | 47.5% | Requires experimental inputs |
| ML-PBPK Platform | In silico ML predictions | 65.0% | Eliminates need for experiments |
| Automated PopPK Search (pyDarwin) | Clinical datasets | Evaluates <2.6% of model space | Identifies structures comparable to expert models |
Core Methodological Protocols
Protocol: Development of a Model Selection Tool (MST) to Prevent Overparameterization
This protocol outlines the creation of an MST, which selects the most appropriate pre-existing model for a patient subgroup rather than building a new, potentially overparameterized model from scratch [85].
Experimental Workflow:
Procedure Details:
- Data Curation: Collect retrospective data from patients receiving the target anti-infective (e.g., vancomycin in ICU adults). Divide the data into training and validation cohorts. For ICU patients, further subdivide data based on dynamic factors like renal replacement therapy status [85].
- Model Library Construction: Identify and curate all relevant published PopPK models for the drug. To minimize overparameterization risk, prioritize one-compartment models, which have been shown to perform comparably to more complex models when data are sparse [85].
- Universal Best Model (UBM) Identification: Calculate population predictions from each model in the library for all patient timeframes. Select the UBM based on the lowest sum of absolute values of Mean Percentage Prediction Error (PPE, for bias) and Mean Percentage Absolute Prediction Error (PAPE, for precision) [85].
- Model Selection Tool (MST) Development: Use a genetic algorithm to configure a Classification and Regression Tree (CART). The algorithm iteratively creates subsets of models and uses 10-fold cross-validation to find an optimal subset that minimizes the fitness function (mean PAPE of the cross-validation sets) [85] [86].
- Performance Evaluation: Compare the final MST against the UBM in the validation dataset. Key performance metrics include prediction precision (Mean PAPE) and bias (Mean PPE). Assess the MST's ability to forecast future drug concentrations based on prior measurements [85].
Protocol: Automated PopPK Model Search with Integrated Penalty Functions
This protocol uses an automated, out-of-the-box approach for PopPK development that explicitly penalizes overparameterization and implausible parameter values, ensuring model stability [86].
Experimental Workflow:
Procedure Details:
- Define Model Search Space: Propose a generic model search space for the drug administration route (e.g., extravascular). This space can contain over 12,000 unique model structures but is designed to be comprehensive yet constrained to biologically plausible configurations [86].
- Configure Optimization Algorithm: Implement optimization using a framework like pyDarwin, which employs Bayesian optimization with a random forest surrogate combined with an exhaustive local search. This hybrid strategy efficiently explores the vast parameter space while avoiding local minima [86].
- Apply Penalty Function for Model Selection: The core of ensuring stability is a dual-term penalty function that mimics expert modeler decisions:
- Term 1 (AIC Penalty): Discourages overparameterization by penalizing models with an excessive number of parameters, following the Akaike Information Criterion [86].
- Term 2 (Plausibility Penalty): Penalizes models with abnormal parameter values, such as high relative standard errors (RSE%), abnormally high or low inter-subject variability, or high shrinkage values. This term is critical for excluding models that are unstable or biologically implausible [86].
- Model Evaluation and Selection: Run the automated search, which typically evaluates fewer than 2.6% of the models in the search space. The final selected model is the one with the best objective function value that also satisfies the constraints of the penalty function, ensuring a parsimonious and stable structure [86].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Reagents and Software for Stable PopPK Modeling
| Item Name | Function/Brief Explanation | Example/Note |
|---|---|---|
| NONMEM | Industry-standard software for non-linear mixed effects modeling, used for PopPK model parameter estimation. | Gold-standard software requiring technical expertise [86] [80]. |
| Genetic Algorithm | An optimization algorithm that imitates evolutionary mechanisms to find optimal model subsets or parameters. | Used for developing Model Selection Trees (MSTs) to avoid building new complex models [85]. |
| pyDarwin Library | A library containing global optimization algorithms for automating the PopPK model structure search. | Employs Bayesian optimization with a random forest surrogate to efficiently navigate the model space [86]. |
| Akaike Information Criterion (AIC) | A metric used in model selection that balances model fit with complexity, penalizing overparameterization. | Incorporated into penalty functions during automated model search to favor parsimonious models [86]. |
| Visual Predictive Check (VPC) | A graphical technique for model evaluation that compares simulated data from the model with observed data. | Used to validate the final PopPK model's predictive performance and stability [80]. |
| M3 Method | A likelihood-based method in NONMEM for handling data below the quantification limit (BQL). | Prevents bias in parameter estimates that can contribute to model instability, especially with high BQL proportions [80]. |
Diagram: The Problem of Overparameterization in PopPK
The following diagram illustrates how overparameterization arises from complex model structures and its consequences for model stability and clinical application.
In population pharmacokinetic (PK) and pharmacodynamic (PD) modeling, the Fisher Information Matrix (FIM) provides a powerful mathematical framework for evaluating and optimizing study designs before a single subject is enrolled. The FIM quantifies the amount of information that observable data carries about unknown model parameters. According to the Cramér-Rao inequality, the inverse of the FIM establishes a lower bound for the variance of any unbiased parameter estimator [87]. This relationship means that maximizing the FIM directly leads to minimizing the expected uncertainty in parameter estimates, resulting in more precise and reliable models.
For nonlinear mixed-effects models (NLMEMs) commonly used in pharmacometrics, analytical solutions for the FIM are not available, necessitating the use of approximations. The application of FIM-based methods enables researchers to answer critical design questions related to sample size, number and timing of samples, cohort allocation, and the value of collecting covariate information. Within anti-infective dose optimization research, where understanding drug exposure-response relationships is critical for defeating resistant infections, efficient study design is particularly valuable. It allows for the maximum information to be extracted from a limited number of patients, which is often the case in clinical trials involving critically ill populations.
Theoretical Foundations of the Fisher Information Matrix
The Cramér-Rao Bound and Optimal Design Criteria
The foundational principle of FIM-based design optimization rests on the Cramér-Rao inequality. Formally, this relationship can be expressed as FIM⁻¹(q,Θ) ≤ COV(q,y,Θ), where y represents the observed data, q are the design variables, and Θ are the model parameters [87]. This inequality confirms that the inverse of the FIM is a lower bound for the covariance matrix of any unbiased estimator. Therefore, by maximizing the FIM, one minimizes the lower bound of the parameter estimate variances, leading to more precise estimates.
Several optimality criteria have been developed to guide the maximization of the FIM, each with a specific statistical interpretation:
- D-optimality: Perhaps the most widely used criterion, it focuses on maximizing the determinant of the FIM (
|FIM|). This is equivalent to minimizing the volume of the confidence ellipsoid around the parameter estimates, thereby providing the best overall joint precision for all parameters [88] [89]. - ED-optimality: A variant that aims to minimize the expected determinant of the parameter variance-covariance matrix.
- A-optimality: Seeks to minimize the trace of the inverse of the FIM, which corresponds to minimizing the average variance of the parameter estimates.
- C-optimality: Designed to minimize the variance of a specific function of the parameters.
In the context of population PK/PD models, the FIM must account for both fixed effects (population typical values) and random effects (inter-individual and residual variability). The calculation involves a first-order (FO) linearization of the model around the random effects [87]. More advanced approximations, such as the First-Order Conditional Estimation (FOCE) method, which linearizes the model around the empirical Bayes estimates of the random effects, can offer improved accuracy for highly nonlinear models [87].
FIM for Discrete and Covariate Data
The application of FIM has been successfully extended beyond continuous data models to include the design of studies with discrete data responses, such as dichotomous, count, or ordinal PD measurements [90]. This is crucial for pharmacodynamic endpoints that are often categorical. Furthermore, recent advancements have enabled the use of FIM to predict uncertainty in covariate effects and the statistical power to detect their relevance [91]. This allows researchers to plan studies that are adequately powered to identify patient factors that significantly impact drug pharmacokinetics and pharmacodynamics, a core objective in personalized anti-infective therapy.
Software Implementation: PFIM and PopED
PFIM: A Dedicated R Package
PFIM is a robust R program specifically developed for design evaluation and optimization in NLMEMs. The latest version, PFIM 4.0, includes several sophisticated features relevant to pharmacometric analyses [88]:
- A comprehensive PK/PD model library and the ability to accommodate user-defined models via R functions.
- Support for models incorporating inter-occasion variability and the influence of discrete covariates.
- Capabilities for adaptive design, where previously obtained results (summarized in a FIM) can be incorporated to optimize subsequent study stages.
- Implementation of the Bayesian individual FIM, which is valuable for designing studies focused on therapeutic drug monitoring (TDM) and model-informed precision dosing (MIPD). This feature predicts both the estimation precision for individual parameters and the expected shrinkage, a key metric in empirical Bayes estimation [88].
The software is freely available and has been proven effective for optimizing population PK studies and Bayesian individual designs, helping to ensure precise parameter estimation while minimizing required sample sizes [88].
PopED: A Versatile MATLAB/R Toolbox
PopED (Population Experimental Design) is another powerful, open-source tool for optimal design in population and individual studies. It is accessible both as a MATLAB toolbox and an R package, offering a broad range of functionalities [92] [87]:
- Multiple FIM approximation methods, including FO, FOCE, and a full likelihood-based (FULL) FIM for certain models.
- Various optimization algorithms for design variables, such as the line search, random search, and stochastic greedy algorithms.
- A parallelized computation engine that significantly speeds up the evaluation of complex designs, making extensive optimization feasible.
- A graphical user interface (GUI) that facilitates use for those less proficient in programming, though all features are accessible via code for full flexibility [87].
PopED can handle a wide array of design optimization tasks, including group size optimization, cost optimization with constraints, and the optimization of sampling times and dose levels [87].
Table 1: Comparison of PFIM and PopED Software Features
| Feature | PFIM | PopED |
|---|---|---|
| Primary Environment | R | R, MATLAB |
| Key Strengths | Adaptive designs, Bayesian individual FIM, covariate handling | Flexible FIM approximations, parallel computing, GUI |
| Optimality Criteria | D-optimality [88] | D-optimality, ED-optimality [89] [87] |
| FIM Approximations | First-order [88] | First-order, FOCE, FULL [87] |
| Design Scope | Population & Individual [88] | Population & Individual [92] |
Figure 1: A generalized workflow for optimal design evaluation and optimization using FIM-based software tools.
Application Notes and Protocols
Protocol 1: Optimizing a Population Pharmacokinetic Study
Objective: To evaluate and optimize a sampling design for a population PK study of a new anti-infective agent to precisely estimate clearance (CL) and volume of distribution (V).
Materials and Software:
- Software: PFIM 4.0 installed in R [88].
- Model: A one-compartment IV bolus model with first-order elimination.
- Parameters:
- Fixed effects: Typical value of CL = 2 L/h, Typical value of V = 30 L.
- Random effects: Inter-individual variability (IIV) on CL and V (ω²CL = 0.1, ω²V = 0.1), proportional residual error (σ²prop = 0.05).
Procedure:
- Define the Model in PFIM: Use the built-in PK model library to select the one-compartment intravenous model.
- Specify the Initial Design: Propose an initial design, for example, 3 samples per subject from 50 subjects, with sampling times at 1, 6, and 12 hours post-dose.
- Evaluate the Initial Design: Run the evaluation in PFIM to obtain the expected relative standard errors (RSE%) for each parameter.
- Optimize the Sampling Times: Using the D-optimality criterion in PFIM, optimize the three sampling times for a single subject. The software will adjust the timing to maximize the determinant of the FIM.
- Assess the Impact of Sample Size: Evaluate the RSE% for parameters using the optimized sampling schedule with different total sample sizes (e.g., N=30, 50, 100) to determine the minimal sample size required for a target precision (e.g., RSE% < 30% for CL).
Table 2: Example Output of RSE% for Different Designs in a Population PK Study
| Design Scenario | RSE% CL | RSE% V | D-criterion |
|---|---|---|---|
| Initial design (1, 6, 12h; N=50) | 8.5% | 10.2% | 1.00 (Reference) |
| Optimized times (2, 8, 24h; N=50) | 6.1% | 7.5% | 1.85 |
| Optimized times, N=30 | 7.9% | 9.7% | 1.83 |
Protocol 2: Bayesian Individual Dosing for Therapeutic Drug Monitoring
Objective: To design an optimal limited sampling strategy for precise estimation of individual PK parameters (e.g., CL) to support TDM of an anti-infective drug like cefepime [93] or vancomycin.
Materials and Software:
- Software: PFIM 4.0 with its Bayesian individual FIM functionality [88].
- Model: A pre-established population PK model from the literature (e.g., a two-compartment model for cefepime [93]).
- Parameters: The population parameters are considered fixed. The goal is to estimate individual empirical Bayes estimates.
Procedure:
- Input the Prior Model: Load the pre-existing population PK model and its parameter estimates (fixed and random effects) into PFIM.
- Define the TDM Context: Specify the patient's dosing regimen and the potential sampling windows (e.g., within one dosing interval).
- Evaluate Sampling Strategies: Compare the predictive performance for individual CL for different sparse sampling schemes (e.g., trough only, peak+trough, midpoint only) [93]. The Bayesian FIM will output the predicted relative standard error for the individual parameter and the expected shrinkage.
- Select the Optimal Strategy: Choose the sampling strategy that provides the best precision (lowest RSE) for the individual CL with the fewest samples, ensuring it is clinically feasible.
Protocol 3: Power Analysis for Covariate Detection
Objective: To determine the sample size required to achieve 90% power for detecting a clinically relevant effect of renal function on drug clearance.
Materials and Software:
- Software: PFIM 6.1 or higher, which includes methods for power analysis of covariate effects [91].
- Model: The population PK model, including a parameter for the covariate relationship (e.g., effect of creatinine clearance (CrCL) on CL).
Procedure:
- Specify the Covariate Model: Define the full model, including the parameter for the effect of CrCL on CL.
- Define the Null and Alternative Hypotheses: The null hypothesis is that the covariate effect is zero. The alternative is that it is different from zero, with a specific magnitude (e.g., a 0.75 power relationship between CrCL and CL).
- Simulate Covariate Distribution: Use the built-in method to simulate a distribution of CrCL in the target population.
- Run Power Analysis: Use the FIM to compute the expected uncertainty of the covariate effect parameter. Calculate the power to reject the null hypothesis for a range of sample sizes.
- Determine Sample Size: Identify the sample size at which the predicted power reaches the 90% target.
Figure 2: Workflow for designing an optimal Bayesian TDM strategy using the Bayesian individual FIM in PFIM.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Software and Methodological Tools for FIM-Based Optimization
| Tool / Concept | Function in Optimal Design | Example Application |
|---|---|---|
| PFIM Software | Evaluates & optimizes designs for NLMEMs in R [88]. | Optimizing sampling schedules for a population PK study. |
| PopED Software | Evaluates & optimizes designs with multiple FIM approximations in R/MATLAB [92] [87]. | Comparing FO vs. FOCE approximations for a PD model. |
| D-Optimality Criterion | A design criterion that maximizes the determinant of the FIM [88]. | Selecting the best overall design for precise parameter estimation. |
| Bayesian Individual FIM | Predicts precision of individual parameter estimates and shrinkage [88]. | Designing a limited sampling strategy for TDM. |
| Covariate Power Analysis (PFIM 6.1) | Predicts power to detect statistically significant covariate effects [91]. | Calculating sample size needed to detect a renal impairment effect. |
| FOCE Approximation | A more accurate FIM approximation for nonlinear models [87]. | Improving design reliability for a saturable PK/PD model. |
Population pharmacokinetic (PopPK) modeling is a cornerstone of anti-infective dose optimization research, enabling the quantification of drug exposure and its variability within target patient populations [94] [66]. In the face of escalating antimicrobial resistance (AMR) and a dwindling antibiotic pipeline, optimizing the use of existing and new anti-infectives through precise PK/pharmacodynamic (PD) modeling has become a critical imperative [95] [94]. Traditional model selection methods, such as Forward Addition/Backward Elimination (FABE), have been the standard for nearly half a century. However, these methods are often manual, time-consuming, susceptible to local minima, and risk missing significant interactions between model features because they typically examine only one feature at a time [96].
The integration of artificial intelligence (AI) and machine learning (ML) is poised to transform this landscape. AI encompasses a spectrum of techniques, including machine learning and deep learning, which can analyze vast, complex datasets to identify patterns and generate predictive models [95] [97]. In pharmacometrics, ML algorithms are now being deployed to automate and enhance the model selection process, offering a more efficient, robust, and objective approach to PopPK model development [98] [96]. This shift is part of a broader movement in pharmaceutical research, where AI is accelerating everything from initial drug discovery and target identification to the optimization of treatment regimens for personalized medicine [97].
This application note focuses on pyDarwin, an open-source Python package specifically designed for automated NONMEM-based PK/PD model selection using machine learning [99] [98]. We will explore its pivotal role in advancing anti-infective drug research by providing detailed protocols, visualizing its workflow, and summarizing its performance in comparative studies.
pyDarwin is an open-source software tool developed to automate the process of PopPK model selection. It provides a framework for defining a model "search space" and employs various ML algorithms to navigate this space efficiently to identify the optimal model [98]. The package has been integrated into the Pirana modeling workbench, offering a graphical user interface (GUI) that simplifies the setup, execution, and post-processing of automated model searches, making this advanced methodology more accessible to pharmacometricians [99] [98].
The core of pyDarwin's functionality lies in its implementation of several machine learning algorithms, each with distinct mechanisms and advantages for navigating the discrete model structure search space [96].
- Genetic Algorithm (GA): This algorithm mimics the process of natural selection. It begins with a random population of models (genomes). Models are selected as "parents" based on their fitness (e.g., lowest objective function value -2LL). Through operations called "crossover" and "mutation," new candidate models (offspring) are generated for the next generation. This process repeats, evolving the population towards an optimal solution [96].
- Gaussian Process (GP): This method models the fitness landscape as a probability distribution. It starts with an uninformative prior and iteratively updates this distribution as models are run and their fitness is evaluated. The algorithm intelligently selects new models to test based on where it believes the most information can be gained about the location of the optimum, making it a very efficient searcher [96].
- Random Forest (RF) and Gradient Boosted Random Tree (GBRT): These are ensemble methods that use decision trees to predict model fitness. RF builds multiple independent decision trees from random samples of the model data, while GBRT builds trees additively, with each new tree correcting errors from the previous ones. Both methods use these ensembles to predict which model features are likely to yield high fitness [96].
- Particle Swarm Optimization (PSO): Inspired by the social behavior of bird flocking or fish schooling, PSO initializes a population (swarm) of candidate models (particles). These particles move through the search space, with their trajectories influenced by their own best-known position and the best-known position of the entire swarm, converging over time on an optimal solution [96].
A critical component that enhances the robustness of these ML algorithms in pyDarwin is the incorporation of a local downhill search. This search systematically changes one or two "features" of a promising model identified by the ML algorithm (a one-bit or two-bit local search) to ensure that no simple, superior model is overlooked in the immediate neighborhood of the current best candidate [96].
Application Protocol: Implementing pyDarwin for a PopPK Analysis
The following protocol outlines the steps for setting up and executing a machine learning-based model search for a PopPK analysis of an anti-infective agent using the pyDarwin interface in Pirana.
Pre-Modeling Setup
- Data Preparation: Curate a dataset suitable for PopPK analysis. This includes individual patient dosing records, drug concentration measurements, and candidate covariates (e.g., weight, serum creatinine, age). The dataset should be formatted according to the requirements of the NONMEM software.
- Define the Base Model Structure: Develop a preliminary base PK structural model (e.g., one- or two-compartment) with an initial estimate of inter-individual and residual variability. This model will serve as the template for the
pyDarwinsearch.
Configuring the Darwin Workspace in Pirana
- Initiate Darwin: Within the Pirana workbench, create a new "Darwin" job to access the model search interface [98].
- General Setup:
- Data Setup: Select the analysis dataset and map the relevant data columns (e.g., ID, TIME, DV, AMT) to their corresponding model variables. Optionally, specify if continuous covariates should be centered [98].
- Model Template Setup:
- ADVAN Selection: Choose the PK model solution method (e.g.,
ADVAN1for one-compartment models). - Parameterization: Set the basic parameterization for clearance (CL) and volume of distribution (V).
- Covariates: Enable the specific covariates (e.g., WT, SCR, AGE) to be included in the model search [98].
- ADVAN Selection: Choose the PK model solution method (e.g.,
- ADVAN Setup: For each structural parameter (CL, V), define the set of potential model features to be searched. For example, for Clearance (CL):
- Structural Model: Specify the initial estimate and bounds for CL.
- Covariate Model: For each covariate (e.g., WT on CL), define the possible relationship forms to be tested:
None(no relationship),Linear, orPowermodel [98].
- Sigma Setup: Specify the forms of the residual error models to be searched (e.g., additive, proportional, combined) and provide initial estimates [98].
- Downhill Search Setup: Activate and configure the one-bit or two-bit local downhill search to run after the ML algorithm, ensuring a thorough local exploration [96].
- Penalties: Set penalties for model fitness calculations, such as criteria for covariate inclusion based on statistical significance (e.g., p-value threshold) or penalties for model complexity [98].
Execution and Post-Processing
- Run the Search: Execute the configured
pyDarwinjob. The system will automatically generate, run, and evaluate hundreds to thousands of candidate NONMEM models based on the defined search space and selected algorithm. - Monitor Progress: Track the progress and current best model through the Pirana interface.
- Post-Processing and Reporting: Upon completion, use Pirana's tools to generate diagnostic plots and reports for the final model selected by the automated search. Validate the model according to standard pharmacometric practices [98].
Workflow Visualization
The diagram below illustrates the integrated workflow of an AI-assisted PopPK analysis using pyDarwin.
Performance Comparison of ML Algorithms in pyDarwin
A key study evaluated the efficiency and robustness of five ML algorithms within the pyDarwin framework against an exhaustive search (evaluating all 1,572,864 possible models) as the gold standard [96]. The metrics for comparison were robustness (the ability to identify the known optimal model) and efficiency (the number of model evaluations required to find it).
Table 1: Performance Comparison of Machine Learning Algorithms in pyDarwin Model Selection [96]
| Algorithm | Robustness (Found Optimal Model) | Efficiency (Models Evaluated) | Elapsed Time (Minutes) | Local Search Requirement |
|---|---|---|---|---|
| Exhaustive Search | Yes (Gold Standard) | 1,572,864 | Not Specified | Not Applicable |
| Gaussian Process (GP) | Yes | 495 | 2975.6 | One-bit |
| Genetic Algorithm (GA) | Yes | Not Specified | 321.8 | One-bit |
| Random Forest (RF) | Yes | Not Specified | Not Specified | One-bit |
| Gradient Boosted Random Tree (GBRT) | Yes | Not Specified | Not Specified | One-bit |
| Particle Swarm Optimization (PSO) | Yes | 1,710 | Not Specified | Two-bit |
Key Findings:
- Robustness: All ML algorithms, when combined with a local downhill search, successfully identified the optimal model, demonstrating their robustness [96].
- Efficiency: The Gaussian Process algorithm was the most efficient, finding the optimal model after evaluating only 495 unique candidates—a fraction of the total search space. In contrast, Particle Swarm Optimization was the least efficient, requiring 1,710 models [96].
- Computational Time: A trade-off exists between efficiency and computational time. While GP was highly efficient in model count, it required the longest elapsed time (~49.6 hours). The Genetic Algorithm was notably faster, completing its search in just over 5 hours [96].
- Local Search Necessity: The one-bit local search was sufficient for GA, RF, GBRT, and GP to locate the optimum. However, PSO required the more comprehensive two-bit local search to achieve the same result [96].
The Scientist's Toolkit: Essential Research Reagents and Software
The following table details key software and methodological components essential for conducting AI-assisted PopPK analyses with pyDarwin.
Table 2: Essential Research Reagents and Software Solutions
| Item Name | Type | Function/Brief Explanation |
|---|---|---|
| pyDarwin | Software Package | An open-source Python package that automates NONMEM PK/PD model selection using machine learning algorithms [98]. |
| Pirana | Software Workbench | A pharmacometric analysis platform that provides a graphical user interface (GUI) for pyDarwin, streamlining the setup and management of automated model searches [99] [98]. |
| NONMEM | Software Engine | The industry-standard software for performing nonlinear mixed-effects modeling (NLMEM) that pyDarwin uses to execute and evaluate candidate models [98]. |
| Genetic Algorithm | Methodological Tool | An ML search strategy inspired by natural selection, effective for global exploration of the model space and efficiently identifying promising regions [96]. |
| Gaussian Process | Methodological Tool | A Bayesian optimization method that models the fitness landscape, making it highly efficient in terms of the number of models evaluated to find the optimum [96]. |
| Local Downhill Search | Methodological Tool | A systematic local search (one-bit or two-bit) used in conjunction with ML algorithms to verify that no superior model exists in the immediate neighborhood of the current best model [96]. |
Case Study: Integration with Anti-Infective Research
The drive towards AI-assisted model development is particularly relevant for anti-infectives like vancomycin, a drug with a narrow therapeutic index that requires careful therapeutic drug monitoring (TDM) [100] [101]. Traditional PopPK models for vancomycin, while valuable, often perform best in homogenous patient populations and can struggle with the significant heterogeneity seen in critically ill patients in Intensive Care Units (ICUs) [100] [101].
ML models have been developed to directly recommend vancomycin dosage, showing superior performance in achieving target trough levels compared to classical PK models and existing dosing nomograms [100]. These models can process large amounts of patient data to provide direct dosing suggestions for both initial and subsequent doses, applicable to a wide patient population without restrictions on renal function or weight [100].
In this context, pyDarwin can accelerate the development of robust, population-specific PopPK models for vancomycin. For instance, a PopPK study in Chinese ICU patients identified covariates like total body weight, serum creatinine, age, and continuous renal replacement therapy (CRRT) status as critical factors influencing vancomycin clearance and volume of distribution [101]. Using pyDarwin, a researcher could define a search space that includes all these potential covariates and their interactions. The ML algorithms would then efficiently and objectively sift through the countless possible model combinations to identify the most parsimonious and predictive model, ultimately supporting more precise and personalized vancomycin dosing in this vulnerable population.
The automation of PopPK model selection through AI and machine learning represents a significant leap forward for pharmacometrics and anti-infective research. pyDarwin stands as a powerful tool in this evolution, offering a suite of robust and efficient algorithms that overcome key limitations of traditional FABE methods. By providing a structured, objective, and comprehensive approach to model development, it enables researchers to build better models faster. The integration of pyDarwin into user-friendly platforms like Pirana makes this advanced methodology accessible, promising to enhance the efficiency and robustness of PopPK analyses. As the pharmaceutical industry continues to embrace AI-driven approaches, tools like pyDarwin will play an increasingly pivotal role in optimizing anti-infective therapy, combating antimicrobial resistance, and advancing the goals of personalized medicine.
The increased emergence of multidrug-resistant (MDR) microbial strains has created an urgent need to optimize anti-infective therapy through sophisticated quantitative approaches [102]. Pharmacometrics, particularly pharmacokinetic/pharmacodynamic (PK/PD) modeling and simulation, has emerged as a formidable tool that bridges microbiology, clinical expertise, and drug development sciences [102]. This discipline uses mathematical models based on biology, pharmacology, physiology, and disease characteristics to quantify drug-patient interactions, providing a scientific framework throughout the drug development continuum and in clinical applications [102] [103].
PK/PD modeling integrates two fundamental components: pharmacokinetics (what the body does to the drug, describing its absorption, distribution, metabolism, and excretion) and pharmacodynamics (what the drug does to the body, characterizing its biological and physiological effects) [104] [103]. By combining models of both processes, PK/PD modeling describes the complete time course of the dose-response relationship, enabling more informed decision-making in dosage selection and regimen design [103]. For anti-infective agents, this approach is particularly valuable for maximizing therapeutic efficacy while minimizing toxicity and the development of antimicrobial resistance [11] [45].
The application of model-informed drug development (MIDD) approaches has been strongly promoted by regulatory agencies, including the U.S. Food and Drug Administration, and has become increasingly essential in optimizing antibiotic dosing regimens for diverse patient populations [102] [105]. These methodologies are particularly crucial for addressing the unique challenges presented by special populations, including critically ill patients, pediatric and elderly patients, and those with organ dysfunction or obesity, who exhibit distinct PK profiles that significantly impact drug exposure and response [11] [45].
Theoretical Foundations of PK/PD Modeling
Basic PK/PD Concepts and Model Structures
The rationale behind PK/PD modeling establishes a continuous relationship between the administered dose, resulting drug concentrations in the body, and the subsequent pharmacological response [103]. This relationship is typically characterized using compartmental models to describe PK and direct effect models to describe PD [103]. Compartmental models represent the body as one or more compartments, with the monocompartmental model being the simplest approach that assumes homogeneous and rapid distribution to all tissues [103]. For many drugs, bicompartmental models provide a more appropriate kinetic description by incorporating a peripheral compartment in addition to the central compartment (plasma) [103].
The most frequently used pharmacodynamic model is the sigmoid Emax model, which theoretically reflects the increasing interactions between drug molecules and their receptors [103]. This model is described by the equation:
[ E = \frac{E{max} \times C^n}{EC{50} + C^n} ]
where (E) represents the measured effect, (E{max}) is the maximum possible effect, (C) is the drug concentration, (EC{50}) is the concentration producing 50% of the maximum effect, and (n) is the slope factor that determines the steepness of the concentration-effect relationship [103].
PK/PD Indices for Anti-Infective Agents
For anti-infective agents, the relationship between pharmacokinetics and microbiological activity is quantified using specific PK/PD indices that correlate with clinical efficacy [11] [45]. These indices vary among antimicrobial classes and serve as critical indicators for therapeutic optimization:
Table 1: Key PK/PD Indices for Major Anti-Infective Classes
| Anti-Infective Class | PK/PD Index | Typical Target Value | Bactericidal Pattern |
|---|---|---|---|
| Beta-lactams [11] | %T > MIC | 40-100% fT > MIC | Time-dependent |
| Vancomycin [11] | AUC₂₄/MIC | ≥400 | Time-dependent |
| Aminoglycosides [11] | Cₘₐₓ/MIC | 8-10 | Concentration-dependent |
| Fluoroquinolones [11] | AUC₂₄/MIC | 125-250 | Concentration-dependent |
These indices integrate drug exposure parameters (Cₘₐₓ, AUC, T > MIC) with bacterial susceptibility measures (MIC) to establish quantitative targets for optimal dosing [45]. The Probability of Target Attainment (PTA) is a crucial metric that predicts the likelihood of achieving these therapeutic targets in a specific population, enabling informed empiric dosing decisions [45].
Application Notes: Case Studies in Dose Optimization
Meropenem in Critically Ill Patients
Critically ill patients present significant challenges for antibiotic dosing due to pathophysiological alterations that profoundly affect drug PK [11] [106]. A population PK study of meropenem in critically ill patients established a model using creatinine clearance (CrCl) and adjusted body weight as key covariates [106]. The elimination rate constant (K₁₀) was described by the equation: K₁₀ = 0.3922 + 0.0025 × CrCl, demonstrating the significant impact of renal function on drug clearance [106].
Monte Carlo simulations (n=5,000) were employed to determine optimal dosing regimens across different renal function categories, comparing traditional 0.5-hour infusions with prolonged 3-hour infusions [106]. The results demonstrated that prolonged infusions significantly improved target attainment across all renal function categories, particularly at higher MICs:
Table 2: Probability of Target Attainment (40% fT > MIC) for Meropenem Regimens [106]
| Creatinine Clearance (mL/min) | Dosing Regimen | Infusion Duration | PTA at MIC = 8 mg/L |
|---|---|---|---|
| ≥50 | 2 g q8h | 0.5 h | 75% |
| ≥50 | 2 g q8h | 3 h | 96% |
| 30-49 | 1 g q8h | 0.5 h | 65% |
| 30-49 | 1 g q8h | 3 h | 90% |
| 10-29 | 1 g q12h | 0.5 h | 44% |
| 10-29 | 1 g q12h | 3 h | 61% |
These findings highlight the critical importance of both dosage selection and infusion strategy in optimizing antimicrobial therapy for critically ill patients, particularly those with impaired renal function [106].
Cefazolin in CNS Infections
Cefazolin, a first-generation cephalosporin with excellent activity against methicillin-susceptible Staphylococcus aureus (MSSA), has traditionally not been recommended for CNS infections due to its low penetration into the CNS [107]. However, recent approaches have utilized cerebrospinal fluid (CSF) PK modeling and simulation to evaluate the potential of high-dose regimens for MSSA meningitis [107].
A recently developed CSF PK model incorporated a mean CSF/serum ratio of 0.0525, estimated from patient data after 1-3 g doses, to predict cefazolin concentrations in the CSF [107]. The model was then used to simulate various dosing regimens and calculate the probability of achieving 100% T > MIC in the CSF, with the PK/PD breakpoint defined as the highest MIC at which target attainment probability exceeded 90% [107].
Table 3: Cerebrospinal PK/PD Breakpoints for Cefazolin Against MSSA Meningitis [107]
| Renal Function (CLcr) | Dosing Regimen | Cerebrospinal PK/PD Breakpoint (μg/mL) |
|---|---|---|
| 90 mL/min | 2 g q4h (0.5 h infusion) | 0.25 |
| 90 mL/min | 2 g q4h (4 h infusion) | 0.5 |
| 90 mL/min | 6 g continuous infusion | 0.5 |
| 90 mL/min | 12 g continuous infusion | 1.0 |
| 30 mL/min | 2 g q12h (0.5 h infusion) | 0.25 |
| 30 mL/min | 2 g q12h (4 h infusion) | 0.5 |
| 30 mL/min | 4 g continuous infusion | 1.0 |
| 30 mL/min | 6 g continuous infusion | 2.0 |
The simulations demonstrated that high-dose continuous infusion regimens (6-12 g/day) could achieve PK/PD breakpoints sufficient to inhibit the growth of 90% of the MSSA population (MIC₉₀ = 0.5 μg/mL) in patients with normal renal function [107]. Conversely, patients with renal impairment (CLcr = 30 mL/min) required dose reduction (4 g/day) to avoid excessive drug exposure while maintaining efficacy, highlighting the importance of individualized dosing based on renal function [107].
Experimental Protocols
Population PK Model Development
Objective: To develop a population pharmacokinetic model that characterizes drug disposition and identifies sources of variability in target populations.
Materials and Methods:
Data Collection: Collect rich or sparse PK sampling data from clinical studies, including drug concentration measurements, dosing history, and sampling times [108] [103].
Covariate Data: Document potential covariates including demographic factors (age, weight, body mass index), physiological parameters (renal function via creatinine clearance, hepatic function), clinical conditions (disease severity scores such as APACHE II or SOFA), and concomitant treatments [108] [45] [106].
Base Model Development:
- Use nonlinear mixed-effects modeling software (e.g., NONMEM, Monolix) to estimate population parameters and interindividual variability [108].
- Test different structural models (e.g., one-compartment, two-compartment) to best describe the concentration-time data [103].
- Evaluate various residual error models (additive, proportional, combined) [108].
Covariate Model Building:
- Identify potential relationships between model parameters and patient covariates using graphical exploration [108].
- Implement stepwise covariate modeling (forward inclusion p<0.05, backward elimination p<0.01) to establish final relationships [108] [106].
- For renally cleared drugs, incorporate creatinine clearance using established equations (e.g., Cockcroft-Gault, CKD-EPI) [45] [106].
Model Validation:
Monte Carlo Simulation for Target Attainment
Objective: To simulate the probability of achieving PK/PD targets across a population for various dosing regimens.
Materials and Methods:
Final Population PK Model: Utilize the validated population PK model with fixed and random effect parameters [106].
Patient Population: Define the virtual patient population (typically n=5,000-10,000) with distributions of key covariates (e.g., creatinine clearance, body weight, age) representative of the target clinical population [106].
Dosing Regimens: Specify the dosing regimens to be simulated, including dose amount, frequency, and infusion duration [107] [106].
PK/PD Targets: Define relevant PK/PD targets based on the antimicrobial class (e.g., 40% fT > MIC for carbapenems, AUC/MIC for fluoroquinolones) [11] [106].
Simulation Procedure:
Output Analysis:
- Generate probability of target attainment (PTA) curves showing the percentage of patients achieving the target across the MIC range [107] [106].
- Determine the PK/PD breakpoint as the highest MIC at which target attainment remains ≥90% [107].
- Compare different dosing regimens to identify optimal strategies for various patient subgroups [107] [106].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for PK/PD Modeling
| Tool/Resource | Function | Application Notes |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software (NONMEM, Monolix) [108] | Population PK/PD model development and parameter estimation | Enables implementation of complex structural models and covariate relationships; industry standard for population modeling |
| Monte Carlo Simulation Software (R, Matlab) [106] | Stochastic simulations of dosing regimens in virtual populations | Allows assessment of probability of target attainment; essential for dose selection and regimen optimization |
| CDISC Standards (SDTM, ADaM) [104] | Standardized data structures for regulatory submission | Ensures compliance with FDA requirements; facilitates integration of data across studies |
| Physiologically-Based PK (PBPK) Modeling Software (GastroPlus, Simcyp) [45] | Mechanistic prediction of drug disposition based on physiological parameters | Particularly valuable for special populations (pediatrics, organ impairment) where clinical data are limited |
| Microbial Susceptibility Data (MIC distributions) [103] [45] | Quantification of pathogen susceptibility for PK/PD target setting | Critical for establishing clinically relevant targets; should incorporate local epidemiology and resistance patterns |
| Therapeutic Drug Monitoring Assays [103] | Measurement of drug concentrations in biological matrices | Supports model validation and precision dosing; essential for drugs with narrow therapeutic indices |
Implementation Considerations
Special Population Considerations
Successful implementation of PK/PD-guided dosing requires careful consideration of specific patient factors that significantly alter drug disposition [45]. Pediatric patients present unique challenges due to developmental changes that affect drug absorption, distribution, metabolism, and excretion [45]. For instance, vancomycin may not achieve sufficient trough concentrations after the first empirical dose in neonates due to their high body water content, which increases the volume of distribution of hydrophilic drugs [45]. Similarly, lipophilic drugs like fluoroquinolones may also exhibit increased volume of distribution in neonates due to larger lipid-rich organs relative to body weight [45].
Elderly patients often experience alterations in PK parameters due to age-related decline in renal and hepatic function, though the rate and extent of these changes vary significantly among individuals [45]. Population PK analyses have demonstrated clear age-related reductions in drug clearance, as exemplified by piperacillin, which shows significantly lower clearance in elderly pneumonia patients (4.6 L/h in patients >75 years) compared to healthy young adults (11.9 L/h) [45].
Obese patients require special consideration as obesity-related physiological changes can substantially impact antimicrobial pharmacokinetics [45]. The updated 2022 guideline provides specific dosage recommendations for antimicrobials in obese patients, though many drugs still have "insufficient data" listed, highlighting the need for further research in this population [45].
Infection Site Penetration
A critical consideration in PK/PD modeling is the penetration of antimicrobial agents to the actual site of infection [11]. The physicochemical properties of antibiotics, particularly their relative solubility and protein binding characteristics, significantly influence their ability to reach different anatomical sites [11]. Hydrophilic agents (beta-lactams, vancomycin, aminoglycosides) typically demonstrate impaired permeability to sites like the lung and central nervous system, often necessitating higher doses or alternative administration strategies [11]. Conversely, lipophilic agents (fluoroquinolones) generally exhibit better tissue penetration due to their ability to cross biological membranes more readily [11].
For CNS infections, the challenge of achieving adequate antibiotic concentrations is particularly pronounced due to the blood-brain barrier [11] [107]. As demonstrated in the cefazolin example, even with high-dose regimens, CSF concentrations may only reach 5-12% of plasma concentrations, necessitating substantial dose escalation or continuous infusion strategies to achieve therapeutic targets at the site of infection [107].
PK/PD modeling and simulation represents a powerful approach for optimizing anti-infective dosing strategies across diverse patient populations. Through the integration of pharmacokinetic principles, microbiological data, and patient factors, these quantitative methods enable more rational dose selection and regimen design, ultimately improving therapeutic outcomes while mitigating the development of resistance. The case studies presented demonstrate the practical application of these methodologies in addressing complex clinical scenarios, from critically ill patients with variable renal function to challenging infection sites like the central nervous system. As antimicrobial resistance continues to escalate, the strategic implementation of model-informed dose optimization will become increasingly essential in preserving the utility of our existing anti-infective arsenal.
Ensuring Robustness: Model Validation, Comparison, and Regulatory Confidence
Population pharmacokinetic (PopPK) modeling is a powerful tool for quantifying the sources and magnitude of variability in drug exposure among individuals. For anti-infective agents, which often possess narrow therapeutic windows and face escalating resistance challenges, robust PopPK models are indispensable for optimizing dosing regimens. However, a model's predictive value is not inherent; it must be rigorously demonstrated through comprehensive validation. Validation transforms a mathematical construct into a reliable tool for clinical decision-making, ensuring that model-informed precision dosing (MIPD) improves patient outcomes rather than leading to erroneous dose adjustments [109]. This document outlines the core principles and detailed protocols for the internal and external evaluation of PopPK models, framed within the critical context of anti-infective drug development and use.
The process of PopPK model validation is broadly categorized into internal and external validation. Internal validation assesses the model's robustness and self-consistency using the very data from which it was derived. Its primary goal is to verify that the model structure, parameter estimates, and covariate relationships are stable and well-supported by the underlying dataset. External validation, a more stringent test, evaluates the model's generalizability and transportability by applying it to an entirely independent dataset not used during model development [19]. This step is crucial for confirming the model's utility in real-world settings, across different patient populations, and clinical practices. As highlighted in a recent external evaluation of meropenem PopPK models, the predictive ability of models often fails to generalize to broader populations, underscoring the necessity of this process [19].
Internal Validation Techniques
Internal validation is a multi-faceted process that employs both numerical and graphical techniques to ensure the model is a plausible representation of the data.
Core Techniques and Diagnostics
Table 1: Key Internal Validation Techniques and Their Interpretation
| Technique | Description | Interpretation of Success |
|---|---|---|
| Goodness-of-Fit Plots | Graphical comparisons of observed (DV) vs. population-predicted (PRED) and individual-predicted (IPRED) concentrations. | Points scatter randomly around the line of identity (y=x), with no systematic trends. |
| Conditional Weighted Residuals (CWRES) Plots | Plots of CWRES vs. PRED or time. Used to detect model misspecification. | Residuals are randomly scattered around zero, with the majority (95%) within ±4 [110]. |
| Bootstrap | A resampling technique where the model is repeatedly fitted to hundreds of new datasets generated by random sampling with replacement from the original dataset. | The original parameter estimates fall within the 2.5th to 97.5th percentiles (95% confidence interval) of the bootstrap estimates, indicating stability. |
| Visual Predictive Check (VPC) | A simulation-based diagnostic where the model is used to simulate hundreds of new datasets. The distribution of the observed data is compared to the distribution of the simulated data. | The observed data percentiles (e.g., 10th, 50th, 90th) fall within the confidence intervals of the corresponding simulated percentiles. |
Detailed Protocol: Conducting a Nonparametric Bootstrap
A bootstrap analysis was performed to evaluate the stability and precision of the final model parameters [110].
Objective: To assess the robustness of the final PopPK model parameter estimates and their associated standard errors.
Materials and Software:
- Software: NONMEM (Version 7.5), Pirana, Perl Speaks NONMEM (PSN, Version 5.4.0), or R (with nlmixr2 package) [110].
- Input Data: The final model file (.ctl or .txt) and the original dataset (.csv).
Procedure:
- Dataset Generation: Use the
bootstraptool in PSN or an equivalent function to generate a specified number (e.g., 1000) of new datasets. Each dataset is created by random sampling with replacement from the original dataset, maintaining the same total number of subjects. - Model Execution: Fit the final PopPK model to each of the 1000 bootstrap datasets.
- Results Compilation: Extract the parameter estimate (e.g., THETA, OMEGA, SIGMA) from each successful model run.
- Analysis: Calculate the median and the 2.5th and 97.5th percentiles for each parameter. Compare the original model estimates to this bootstrap confidence interval.
Success Criteria: The original parameter estimate is considered stable if it lies within the 2.5th and 97.5th percentiles of the bootstrap estimates. A high success rate (e.g., >90%) of successful model minimizations indicates a stable model.
External Validation Techniques
External validation is the ultimate test of a model's predictive performance and clinical applicability, particularly when the model is intended for use in MIPD.
Predictive Performance Evaluation
The predictive performance of a model on an external dataset is typically assessed using metrics of bias (accuracy) and precision [19].
Table 2: Key Metrics for External Predictive Performance
| Metric | Formula | Interpretation |
|---|---|---|
| Prediction Error (PE) | ( PE = C{obs} - C{pred} ) | Positive values indicate under-prediction; negative values indicate over-prediction. |
| Mean Prediction Error (MPE) | ( MPE = \frac{1}{n} \sum PE ) | Measures bias. An MPE close to zero indicates minimal systematic bias. |
| Root Mean Square Error (RMSE) | ( RMSE = \sqrt{\frac{1}{n} \sum PE^2} ) | Measures precision. A lower RMSE indicates higher predictive precision. |
A recent external validation of meropenem models stratified patients into subgroups, such as those receiving continuous renal replacement therapy (CRRT) and non-CRRT patients, with further stratification by obesity [19]. This approach revealed that model performance was highly variable across subgroups, emphasizing that a model valid for one patient population may not be suitable for another.
Detailed Protocol: External Validation with an Independent Dataset
Objective: To evaluate the predictive performance and generalizability of a published PopPK model using an independent dataset from a new clinical study or a different clinical site.
Materials and Software:
- Software: Modeling software (e.g., NONMEM, Monolix) or statistical software (e.g., R, Python).
- Inputs: The published PopPK model (parameter estimates and model structure) and the independent validation dataset.
Procedure:
- Dataset Curation: Prepare the external validation dataset according to the covariate requirements of the model. This may involve retrospective data collection from electronic health records or prospective data gathering [19] [111].
- Model Implementation: Code the published model and its fixed parameter estimates (THETAs) into your software. The inter-individual variability (OMEGA) and residual error (SIGMA) are typically retained.
- Prediction Generation: Use the implemented model to generate population predictions for each observation in the external dataset. Do not re-estimate the model parameters.
- Metric Calculation: For each observation, calculate the Prediction Error (PE). Then, compute the MPE (bias) and RMSE (precision) for the entire external cohort and for clinically relevant subgroups (e.g., by renal function, obesity status) [19].
- Graphical Assessment: Create plots of observed vs. predicted concentrations and plots of PE vs. time or predicted concentration to identify any systematic trends.
Success Criteria: A model is considered to have adequate predictive performance if the MPE is close to zero (minimal bias) and the RMSE is low (good precision). The absence of systematic trends in the diagnostic plots further supports the model's validity.
The PopPK Validation Workflow
The following diagram illustrates the integrated, sequential process of PopPK model development and validation.
Table 3: Key Research Reagent Solutions for PopPK Model Validation
| Category / Item | Specific Examples / Functions |
|---|---|
| Modeling Software | NONMEM (industry standard), Monolix, R (with nlmixr2, mrgsolve packages) [23] [110]. Used for model fitting, simulation, and estimation of parameters. |
| Scripting & Automation | Pirana (NONMEM run management), Perl Speaks NONMEM (PSN) [110], R/Python scripts. Automates tasks like bootstrapping and VPC. |
| Simulation & Visualization | R package mrgsolve [23] [28], ggplot2. Used for simulating concentration-time profiles and creating diagnostic plots. |
| Model Repository | Curated collections of published models (e.g., rifampicin PopPK model repository [23]). Provides a basis for external validation and MIPD. |
| Real-World Data Platforms | Web applications for TDM data pooling (e.g., PAT for vancomycin [111]). Sources large-scale, independent data for external validation. |
Regulatory and Advanced Considerations
The ICH M15 draft guidelines on Model-Informed Drug Development (MIDD) harmonize expectations for model development, documentation, and assessment [112]. These guidelines emphasize a credibility framework, which is directly addressed through rigorous internal and external validation. Furthermore, emerging technologies like machine learning (ML) are being developed to assist with tasks such as model selection or initial dose prediction [109] [113]. However, the principles of validation remain paramount; any ML-based approach must itself undergo external validation in independent datasets before it can be trusted for clinical use [113].
For anti-infective drugs, successful validation must also consider the pharmacodynamic (PD) target. A model is not truly "valid" for dose optimization unless its predictions can reliably achieve a target exposure (e.g., fAUC/MIC or %fT>MIC) associated with clinical efficacy and minimized resistance [109]. Therefore, the ultimate validation of a PopPK model for anti-infectives is its successful integration into a MIPD system that improves patient outcomes.
Diagnostic plots are indispensable tools in population pharmacokinetic (PopPK) modeling, providing critical assessments of model performance and validity. For anti-infective dose optimization research, these visual diagnostics enable researchers to verify that models accurately capture drug behavior, identify potential model misspecifications, and ensure robust simulations for dose selection. Within the model evaluation framework, three diagnostic approaches form a complementary hierarchy: individual fits examine agreement between model predictions and observed data at the participant level; residual analyses identify systematic biases in model performance; and visual predictive checks assess model simulation properties against the original dataset. This protocol details the application of these essential diagnostic tools, with specific emphasis on their role in anti-infective drug development.
Diagnostic Plot Fundamentals in PopPK Modeling
Theoretical Framework and Hierarchy of Diagnostics
In PopPK model development, diagnostic plots serve as the primary means for evaluating model adequacy prior to clinical application. The diagnostic process follows a structured approach that progresses from basic goodness-of-fit assessments to predictive performance evaluation [80] [103]. The hierarchy begins with individual fits, which provide the most granular assessment of how well the structural model recapitulates observed concentration-time profiles for each study participant. The analysis then progresses to residual-based diagnostics, which systematically quantify and visualize patterns in the discrepancies between observed and predicted values. The diagnostic sequence culminates with visual predictive checks, which evaluate the model's ability to simulate data that statistically resemble the original dataset [80] [114].
For anti-infective drugs specifically, appropriate model diagnostics are crucial due to the exposure-response relationships that drive efficacy and the emergence of resistance [103] [115]. Proper diagnostic evaluation ensures that model-based simulations used for dose selection accurately reflect the drug's pharmacokinetic profile across diverse patient populations, which is particularly important for drugs with narrow therapeutic indices or significant interindividual variability [114] [103].
Diagnostic Workflow and Interrelationships
The following diagram illustrates the integrated workflow for implementing diagnostic plots in PopPK analysis, highlighting the sequential relationship between different diagnostic classes and their specific roles in model evaluation:
Individual Fits: Protocol for Evaluation and Interpretation
Analytical Protocol
Individual fits display observed data points overlaid with individual predicted concentrations or population predictions for each study participant [80]. The following protocol ensures consistent generation and interpretation:
Step 1: Data Preparation
- Extract individual observed concentration-time data and corresponding predictions from the modeling software (e.g., NONMEM, Monolix)
- For drugs with complex kinetics, consider logarithmic transformation to better visualize wide concentration ranges
- Flag and document observations below the quantification limit (BQL) using appropriate handling methods (e.g., M3 method) [80]
Step 2: Plot Generation
- Create scatter plots of observed concentrations (Y-axis) versus individual predictions (X-axis)
- Generate observed versus population predictions for comparison
- Include a line of identity (y=x) to visualize perfect prediction
- For time-based evaluation, plot observed and predicted concentrations versus time for representative individuals
Step 3: Quantitative Assessment
- Calculate and record individual goodness-of-fit metrics: mean prediction error (MPE) for bias, root mean squared error (RMSE) for precision
- For anti-infective drugs, pay particular attention to fit quality at concentrations near the minimum inhibitory concentration (MIC) [103]
Step 4: Qualitative Evaluation
- Examine systematic deviations from the line of identity
- Identify individuals with consistently over- or under-predicted concentrations
- Assess whether misfits occur at specific time points or concentration ranges
Interpretation Guidelines
The table below summarizes key patterns in individual fits and their potential implications for model refinement:
Table 1: Interpretation Guide for Individual Fit Diagnostics
| Pattern Observed | Potential Implication | Model Refinement Consideration |
|---|---|---|
| Systematic over-prediction at low concentrations, under-prediction at high concentrations | Misspecified elimination process | Evaluate non-linear clearance; consider Michaelis-Menten kinetics |
| Consistent under-prediction during absorption phase | Incorrect absorption model | Test alternative absorption models: transit compartments, first-order with lag time [80] |
| Random scatter around line of identity with no systematic bias | Adequate structural model | No structural model changes needed |
| Specific subpopulations showing biased predictions | Unaccounted covariate effects | Evaluate demographic (weight, age) or pathophysiological factors (renal function) [114] [116] |
| Poor fits in patients with extreme characteristics | Inadequate covariate relationship | Test alternative parameterizations (allometric scaling, power functions) [114] |
Residual Diagnostics: Protocol for Analysis
Residual Calculation Methods
Residuals quantify the discrepancy between observed and model-predicted values, with different residual types serving complementary diagnostic purposes [80]:
Population Residuals
- Based on population parameter estimates (PRED)
- Useful for identifying structural model misspecification
- Calculated as: RES = OBS - PRED
Individual Residuals
- Utilize empirical Bayes estimates of individual parameters (IPRED)
- Sensitive to both structural model and interindividual variability specification
- Calculated as: IRES = OBS - IPRED
Normalized Residuals
- Weight residuals by their expected variability (WRES, NPRES)
- Facilitate comparison across concentration ranges and individuals
- Essential for identifying heteroscedasticity
Analytical Protocol
Step 1: Generate Residual Plots
- Create scatter plots of residuals versus population predictions
- Plot residuals versus time after dose
- Generate residuals versus continuous covariates (e.g., weight, age, renal function)
- For time-varying covariates, plot residuals versus covariate values
Step 2: Assess Residual Distributions
- Construct quantile-quantile (Q-Q) plots against the normal distribution
- Calculate skewness and kurtosis statistics
- Perform statistical tests for normality if needed (e.g., Shapiro-Wilk)
Step 3: Evaluate Patterns
- Identify systematic trends in residual distributions
- Assess homogeneity of residual variance across predictions (homoscedasticity)
- Document any correlation between residual magnitude and covariate values
Interpretation Framework
Table 2: Residual Diagnostic Patterns and Implications in Anti-infective PopPK
| Residual Pattern | Diagnostic Implication | Impact on Anti-infective PK |
|---|---|---|
| Funnel-shaped variability (increasing variance with predictions) | Heteroscedastic residual error | Proportional error model may be appropriate; common with anti-infectives with high clearance variability [114] |
| U-shaped or inverted U-shaped trend versus predictions | Structural model misspecification | May indicate incorrect clearance or volume parameterization; impacts AUC predictions crucial for efficacy [103] |
| Systematic trend versus time | Unmodeled time-dependent process | Could indicate autoinduction, enzyme inhibition, or circadian rhythms; particularly relevant for chronic anti-infective therapies |
| Correlation with specific covariates | Omitted covariate relationship | Missed opportunity for individualized dosing; critical for drugs with narrow therapeutic indices [114] [116] |
| Normally distributed around zero with constant variance | Appropriate error structure | Supports current model specification; proceed to predictive checks |
Visual Predictive Checks: Protocol for Implementation
Theoretical Basis
Visual Predictive Checks (VPC) evaluate whether model simulations can reproduce the statistical properties of the original dataset [80] [114]. Unlike goodness-of-fit diagnostics that assess agreement between model predictions and the data used for estimation, VPC assesses the model's predictive performance through simulation-based evaluation.
The fundamental VPC algorithm involves:
- Simulating multiple replicate datasets using the final parameter estimates and their uncertainty
- Calculating percentiles of the simulated data at each time point
- Overlaying percentiles from the observed data
- Assessing concordance between simulated and observed percentile bands
For anti-infective drugs, VPC is particularly valuable for verifying that the model adequately captures the variability in drug exposure metrics (AUC, Cmax) that drive efficacy and toxicity [103].
Computational Protocol
Step 1: Simulation Design
- Determine appropriate number of simulations (typically 500-1000) to ensure stable percentiles
- Maintain the original study design in simulations: dosing regimens, sampling times, covariate distributions
- For studies with rich data, consider stratification by relevant covariates (e.g., weight bands, renal function)
Step 2: Calculation of Percentiles
- For each time point, calculate the 5th, 50th, and 95th percentiles of simulated data
- Compute corresponding percentiles from the observed data
- For non-continuous data (e.g., BQL data), calculate the proportion of observations in each category
Step 3: Plot Generation
- Create shaded regions representing the 90% prediction intervals (5th-95th percentiles) from simulations
- Overlay the median (50th percentile) of simulated data as a line
- Plot the corresponding percentiles from observed data as points with error bars
- Use different colors or line styles to distinguish simulated from observed percentiles
Step 4: Numerical Assessment
- Calculate the proportion of observed data points falling outside the simulation prediction intervals
- For a well-calibrated model, approximately 10% of observations should fall outside the 90% prediction interval
- Perform statistical tests if needed (e.g., prediction-corrected VPC for sparse data)
VPC Interpretation Framework
Table 3: VPC Interpretation Guide for Anti-infective Dose Optimization
| VPC Pattern | Interpretation | Clinical Impact on Dose Optimization |
|---|---|---|
| Observed median within simulated prediction interval, observed variability matches simulations | Adequate model for simulation and dose selection | Supports proceeding to clinical trial simulations for dose justification |
| Observed median outside simulated prediction intervals at critical time points | Structural model deficiency | AUC predictions may be biased; dose recommendations potentially suboptimal |
| Observed variability exceeds simulated variability | Underestimation of interindividual variability | Risk of underdosing sensitive subpopulations; necessitates covariate identification |
| Observed variability less than simulated variability | Overparameterization or overestimation of variability | May lead to unnecessarily conservative dosing; consider model simplification |
| Systematic misfit at specific dosing intervals | Incorrect absorption or elimination model | Trough concentration predictions unreliable; impacts dosing interval selection |
Integrated Case Example: Anti-infective PopPK Application
ASC10 PopPK Model Diagnostic Evaluation
The PopPK analysis of ASC10 (an oral double prodrug for COVID-19 treatment) exemplifies comprehensive diagnostic assessment [80]. The model development utilized data from 57 healthy subjects with 1634 observations, employing a two-compartment model with transit compartment absorption.
Diagnostic Implementation:
- Individual fits confirmed the structural model adequately captured both single and multiple-dose pharmacokinetics
- Residual diagnostics employed the M3 method for BQL data handling and used the Laplacian algorithm for estimation
- VPC evaluation demonstrated the model could successfully simulate the central tendency and variability of observed ASC10-A concentrations
Covariate Impact Assessment: Diagnostic plots revealed food intake and body weight as influential covariates on ASC10-A pharmacokinetics. The VPC simulations confirmed that the 800 mg twice-daily regimen provided desirable exposure associated with clinical response across the studied population [80].
Diagnostic Workflow for Anti-infective Development
The following diagram illustrates the comprehensive diagnostic workflow integrated throughout the anti-infective PopPK model development process:
The Scientist's Toolkit: Essential Research Reagents and Software
Table 4: Essential Tools for PopPK Diagnostic Plot Implementation
| Tool Category | Specific Tools/Software | Application in Diagnostic Plotting | Key Features for Anti-infective PK |
|---|---|---|---|
| Modeling Software | NONMEM [80], Monolix [117], Phoenix NLME [114] | Primary estimation and simulation engine | Handles complex kinetics; BQL data methods; efficient covariance estimation |
| Visualization Platforms | R [80], Python (Matplotlib, Plotly) | Diagnostic plot generation and customization | Publication-quality graphics; interactive visualization; reproducible workflows |
| Diagnostic Algorithms | Xpose, Pirana, PSN | Automated diagnostic calculation and visualization | Streamlines diagnostic workflow; template-based plotting; model comparison |
| Data Management | SAS, R Data Frames, Python Pandas | Dataset preparation for diagnostics | Efficient handling of large PK datasets; merging of predictions with observations |
| Specialized Diagnostic Tools | VPC Algorithm [80], NPDE Calculation | Predictive check implementation | Robust percentile calculation; handling of sparse data; statistical evaluation |
| Reporting Tools | R Markdown, Jupyter Notebooks, LaTeX | Integrated reporting of diagnostics | Combines code, results, and interpretation; facilitates regulatory submission |
In the field of anti-infective dose optimization research, the challenge of obtaining rich pharmacokinetic (PK) data is ever-present. Sparse sampling designs, characterized by few samples per individual, are often a practical necessity in special populations like critically ill patients [118] [79]. This application note provides a comparative analysis of two methodological approaches for handling sparse data: Population Pharmacokinetic (PopPK) modeling and Traditional Individual Fitting.
PopPK, specifically using the Nonlinear Mixed-Effects Modeling (NLMEM) framework, has emerged as a robust solution for characterizing inter-individual variability in drug exposure when dense sampling is impractical [119] [120]. This analysis details the advantages, limitations, and practical protocols for implementing PopPK in anti-infective research, providing a structured framework for researchers and drug development professionals.
Theoretical Foundations and Key Differences
Fundamental Methodological Distinctions
Traditional Individual Fitting approaches, including non-compartmental analysis (NCA) and individual compartmental modeling, require sufficient data points per subject to independently estimate PK parameters for each individual [1] [121]. These methods typically need 3-4 samples after peak time and 2 points before peak for extravascular formulations to reliably characterize drug disposition [122]. In practice, this often means ≥6 samples per participant to establish individual PK profiles, which is frequently impractical in clinical settings involving critically ill patients or special populations [79] [1].
In contrast, PopPK modeling using NLMEM analyzes data from all individuals simultaneously, leveraging information across the entire population to inform individual parameter estimates [119] [120]. This approach explicitly quantifies and partitions variability into between-subject variability (BSV), within-subject variability (WSV), and residual unexplained variability (RUV) [79]. By borrowing strength from the population, PopPK can provide reliable parameter estimates even when individuals contribute as few as one or two sampling points [119] [120] [122].
Comparative Advantages and Limitations
Table 1: Comprehensive Comparison of PopPK vs. Traditional Individual Fitting Approaches
| Characteristic | Population PK (NLMEM) | Traditional Individual Fitting |
|---|---|---|
| Data Requirements | Handles both intensive and sparse data; robust to missing timepoints | Requires dense sampling (typically ≥6 points per subject); sensitive to missing data |
| Model Outputs | Population parameters + BSV/WSV + RUV; covariate effects | Individual PK parameters only (CL, Vd, t₁/₂, AUC) |
| Analytical Capabilities | PK/PD modeling; simulation of alternative regimens; covariate detection | Non-compartmental analysis; individual curve fitting |
| Computational Complexity | High; requires specialized software and expertise | Low to moderate; user-friendly software available |
| Regulatory Recognition | Well-established in FDA/EMA guidelines for drug development | Standard for early-phase clinical trials |
| Interpretation | Mechanistic understanding of variability sources | Descriptive individual exposure metrics |
| Predictive Utility | High for simulation and forecasting | Limited to observed data |
| Implementation Time | Longer development and validation time | Rapid analysis turnaround |
The primary advantage of PopPK lies in its ability to quantify variability and identify covariates that explain differences in drug exposure, ultimately supporting model-informed precision dosing (MIPD) [118] [123] [79]. For anti-infective agents like linezolid, this approach enables the identification of patient factors (e.g., age, renal function) that significantly impact pharmacokinetics and pharmacodynamic target attainment [118].
However, PopPK requires specialized expertise and advanced software tools, making it more computationally intensive and time-consuming than traditional approaches [120] [121]. Additionally, model development requires careful attention to structural model selection, covariate testing, and validation strategies [123] [1].
Practical Implementation Protocols
PopPK Workflow for Sparse Data Analysis
The following diagram illustrates the comprehensive workflow for implementing PopPK modeling with sparse data in anti-infective research:
Protocol 1: Data Preparation and Initial Analysis
Purpose: To properly structure sparse data and generate initial parameter estimates for PopPK model development.
Materials and Software:
- Patient concentration-time data with dosing records
- Demographic and clinical covariates
- Software: R with appropriate packages (e.g., nlmixr2, PKNCA) or specialized tools (Monolix, NONMEM)
Procedure:
- Data Assembly: Compile all concentration data with precise dosing times and sampling times relative to last dose
- Covariate Compilation: Collect potential covariates including age, weight, renal function (eGFR), hepatic function, concomitant medications
- Handling BLOQ Data: Implement appropriate methods for below limit of quantification values rather than simple imputation (e.g., LLOQ/2) [1]
- Naïve Pooled Analysis: Apply binning strategy using predefined time windows (default: 10 windows) to calculate median concentrations at median times for visual pattern recognition [122]
- Initial Parameter Estimation: Use adaptive single-point methods for clearance (CL) and volume of distribution (Vd) estimation:
- For intravenous administration:
CL = Dose / AUCwhere AUC is estimated from steady-state concentrations - For extravascular administration:
Vd = Dose / (F × C₀)where F is assumed bioavailability and C₀ is estimated initial concentration [122]
- For intravenous administration:
Quality Control: Generate exploratory plots of concentration versus time by key patient subgroups to identify potential covariate relationships and data anomalies.
Protocol 2: Base Model Development with Sparse Data
Purpose: To establish the structural and statistical model without covariate relationships.
Procedure:
- Structural Model Selection:
- Test one-, two-, and three-compartment models using likelihood-based criteria
- For anti-infectives with complex distribution, prioritize two-compartment models initially
- Evaluate absorption models (first-order, zero-order, transit compartments) for extravascular administration
Statistical Model Specification:
- Model between-subject variability using exponential error models:
Pᵢ = θₚ × exp(ηᵢ)where ηᵢ ~ N(0, ω²) - Test proportional, additive, and combined residual error models
- Model between-subject variability using exponential error models:
Parameter Estimation:
- Utilize maximum likelihood estimation with appropriate algorithms (SAEM, FOCE)
- Implement in software such as Monolix, NONMEM, or nlmixr2
Model Selection Criteria:
- Compare objective function value (OFV) for nested models (ΔOFV > -3.84 for p < 0.05)
- Use Akaike Information Criterion (AIC) or Bayesian Information Criterion (BIC) for non-nested models [1]
- Evaluate precision of parameter estimates and physiological plausibility
Validation Steps: Conduct visual predictive checks (VPC) and evaluate goodness-of-fit plots before proceeding to covariate modeling.
Protocol 3: Covariate Model Building and Validation
Purpose: To identify significant patient factors explaining pharmacokinetic variability and develop a final model for simulation.
Procedure:
- Covariate Screening:
- Create scatterplots of empirical Bayes estimates (EBEs) versus continuous covariates
- Generate boxplots of EBEs versus categorical covariates
- Identify potential relationships for formal testing
Stepwise Covariate Modeling:
- Forward inclusion (p < 0.05, ΔOFV > -3.84)
- Backward elimination (p < 0.01, ΔOFV > -6.63)
- Test typical covariate-parameter relationships using power models:
CL = θₛₜd × (WT/70)^θₑₓₚ × exp(ηᵢ)
Model Validation:
- Bootstrap analysis (n = 1000) to evaluate parameter precision
- Numerical predictive check (NPC) to assess predictive performance
- External validation if independent dataset available
Model Evaluation for Forecasting:
Application in Anti-Infective Research: Case Example
Linezolid PopPK in Hemato-Oncological Patients with Sepsis
A recent PopPK analysis of linezolid in hemato-oncological patients with sepsis demonstrates the practical application of these protocols [118]. The study developed a PopPK model using 197 serum concentrations from 22 patients (approximately 9 samples per patient), representing a sparse sampling scenario.
Table 2: Performance Comparison for Sparse Data Applications
| Performance Metric | PopPK with Sparse Data | Traditional Individual Fitting |
|---|---|---|
| Parameter Bias | Low (when properly specified) | High with very sparse data |
| Parameter Precision | Acceptable with adequate sample size | Poor with limited points per subject |
| Covariate Detection Power | Good with adequate population size | Limited to graphical exploration |
| Predictive Performance | Good for population, moderate for individuals | Limited without rich data |
| Optimal Sampling Design | 60 patients with 3 points or 20 patients with 5 points [124] | 6-8 points per patient required |
Key Findings:
- Patient age was identified as the most predictive covariate for linezolid clearance
- For a median age of 59 years, typical parameters were: Vd = 46.2 L, CL = 12.1 L/h
- Linezolid clearance decreased by 33% during the first 4 days of therapy
- Model-based simulations enabled the development of an age-stratified dosing nomogram
Clinical Impact: The PopPK approach enabled the identification of optimal dosing strategies that would have been undetectable using traditional methods due to sparse sampling constraints. The model demonstrated that probability of target attainment increased through age-based individualization, loading doses, and continuous infusion administration [118].
Table 3: Key Software Tools for PopPK Analysis
| Tool Name | Type | Primary Function | License |
|---|---|---|---|
| NONMEM | Standalone software | Gold standard for PopPK analysis | Commercial |
| Monolix | Standalone software | PopPK modeling with user-friendly interface | Commercial |
| nlmixr2 | R package | Open-source PopPK modeling | Open-source |
| Phoenix NLME | Standalone software | Integrated PK/PD modeling platform | Commercial |
| PKNCA | R package | Noncompartmental analysis for initial estimates | Open-source |
| xpose | R package | Model diagnostics and evaluation | Open-source |
| ggpmx | R package | Advanced graphics for pharmacometrics | Open-source |
Population pharmacokinetic modeling using NLMEM represents a superior analytical framework for sparse data scenarios commonly encountered in anti-infective dose optimization research. Compared to traditional individual fitting approaches, PopPK provides robust parameter estimation, meaningful covariate detection, and enhanced predictive capability through model-based simulations.
The implementation protocols outlined in this application note provide researchers with a structured approach for developing, evaluating, and applying PopPK models to optimize anti-infective therapy in special populations where sparse sampling is unavoidable. As model-informed precision dosing continues to gain traction in clinical practice, PopPK methodologies will play an increasingly vital role in tailoring anti-infective regimens to individual patient characteristics and maximizing the probability of therapeutic success.
In population pharmacokinetic (PopPK) modeling for anti-infective dose optimization, model uncertainty represents a critical challenge that can significantly impact dosing recommendations and therapeutic outcomes. PopPK models utilize the non-linear mixed-effects model (NONMEM) approach to characterize drug behavior across diverse patient populations, identifying sources of variability and quantifying their influence on drug exposure [125]. These models serve as the foundation for model-informed precision dosing (MIPD), which aims to optimize drug therapy by providing patient-tailored doses based on pharmacokinetic/pharmacodynamic (PK/PD) results [125]. However, the inherent variability in pharmacological data, coupled with complex model structures, introduces uncertainty that must be rigorously quantified to ensure reliable clinical applications.
The bootstrap and cross-validation techniques have emerged as essential methodologies for quantifying model uncertainty and evaluating predictive performance in pharmacometric analyses. Bootstrap methods provide robust approaches for estimating the uncertainty of parameters in NONMEM, offering advantages over traditional asymptotic methods, particularly for models with high nonlinearity [126]. Cross-validation, particularly bootstrap cross-validation (BS-CV), assesses the predictive ability of a model, allowing researchers to rank models according to their generalizability and stability [127]. Together, these methods form a critical framework for validating PopPK models in anti-infective development, where accurate quantification of uncertainty directly impacts the safety and efficacy of dosing regimens across diverse patient populations.
Theoretical Foundations
In PopPK analysis, model uncertainty arises from multiple sources, including parameter uncertainty, model structure uncertainty, and covariate selection uncertainty. Parameter uncertainty refers to the imprecision in estimating PK parameters such as clearance (CL) and volume of distribution (V), which are influenced by inter-individual variability and residual unexplained variability [128]. For instance, in a vancomycin PopPK model for pediatric patients, inter-individual variability was described using an exponential error model, while residual variability was accounted for using combined proportional and additive error models [128].
Model structure uncertainty encompasses the selection of an appropriate compartmental model and elimination characteristics. For example, in the development of a pyrazinamide PopPK model, a one-compartment model with allometric scaling for body size effect adequately described the pharmacokinetics, while for dexmedetomidine, a two-compartment model with first-order absorption and linear elimination was optimal [125] [129]. Covariate selection uncertainty arises when identifying patient factors that significantly influence PK parameters, such as body weight, renal function, or comorbidities like diabetes mellitus [125]. Each of these uncertainty sources must be addressed to ensure the developed PopPK model reliably supports dose optimization decisions.
Bootstrap Principles
Bootstrap methods are resampling techniques that estimate the sampling distribution of a statistic by repeatedly sampling with replacement from the original dataset. In PopPK, bootstrap methods are particularly valuable for estimating parameter uncertainty in NONMEM, especially for models with high nonlinearity and heteroscedastic error [126]. The fundamental principle involves creating multiple bootstrap datasets, each representing a potential alternative sample from the underlying population, and then refitting the model to each dataset to generate a distribution of parameter estimates.
Three primary bootstrap approaches are used in pharmacometrics: case bootstrap, nonparametric residual bootstrap, and parametric bootstrap. The case bootstrap resamples individuals with replacement, preserving both between-subject and residual variability in a single resampling step [126]. This method is computationally efficient and makes no assumptions about the underlying model structure. The nonparametric residual bootstrap resamples both random effects and residuals but may underperform in unbalanced designs due to failure to reflate variance before resampling [126]. The parametric bootstrap generates new datasets based on the assumed model structure and estimated parameter distributions, typically performing better when the true model and variance distribution are correctly specified [126].
Cross-Validation Foundations
Cross-validation assesses a model's predictive performance by systematically partitioning the data into training and testing sets. In pharmacometrics, this approach evaluates how well a PopPK model will generalize to independent datasets, providing crucial insights into model stability and reliability. The bootstrap cross-validation (BS-CV) method combines the strengths of both approaches by using bootstrap resampling as the basis for cross-validation [127]. In BS-CV, the items selected in a given bootstrap iteration constitute the training data, while the omitted items form the testing data, enabling efficient assessment of predictive performance across multiple resampling cycles.
Cross-validation is particularly valuable for model selection in PopPK, where multiple candidate models with different covariate relationships or structural components must be compared. By evaluating predictive performance rather than just goodness-of-fit metrics, cross-validation helps identify models that are overfitted to the specific dataset and may perform poorly when applied to new patient populations. This is especially critical in anti-infective dose optimization, where models must reliably predict exposures across diverse clinical scenarios.
Table 1: Comparison of Bootstrap Methods in PopPK
| Method | Key Features | Advantages | Limitations |
|---|---|---|---|
| Case Bootstrap | Resamples individuals with replacement | Simple, preserves between-subject and residual variability | May be suboptimal in highly unbalanced designs |
| Nonparametric Residual Bootstrap | Resamples both random effects and residuals | Makes minimal distributional assumptions | Fails to reflate variance in unbalanced designs |
| Parametric Bootstrap | Generates new data based on assumed model structure | Optimal when true model is known | Performance degrades with model misspecification |
Methodological Protocols
Bootstrap Implementation Protocol
Software and Tools
The implementation of bootstrap methods for PopPK model uncertainty requires specific computational tools. NONMEM (version 7.4.1 or higher) serves as the primary software for model fitting and parameter estimation [128]. Perl-speaks-NONMEM (PsN) provides a robust platform for automating bootstrap procedures, covariate screening, and model validation [128]. R software (version 4.3.1 or higher) is essential for data preparation, visualization, and statistical analysis, with specialized packages available for advanced bootstrap diagnostics [128].
Procedural Steps
The bootstrap implementation follows a systematic protocol:
Model Estimation: Fit the final PopPK model to the original dataset using appropriate estimation methods (e.g., first-order conditional estimation with interaction).
Bootstrap Dataset Generation: Generate a specified number of bootstrap datasets (typically 1000 or more) by sampling with replacement from the original dataset. For case bootstrap, sample individuals; for residual bootstrap, resample both random effects and residuals.
Model Re-estimation: Fit the PopPK model to each bootstrap dataset, recording parameter estimates for each run.
Results Aggregation: Calculate the median and percentiles (e.g., 2.5th and 97.5th) of the parameter distributions from successful bootstrap runs.
Bias Assessment: Compare the original parameter estimates with the median bootstrap estimates to evaluate potential estimation bias.
Uncertainty Quantification: Derive confidence intervals for parameters based on the bootstrap percentiles.
This protocol was successfully applied in a vancomycin PopPK study, where bootstrap results confirmed the stability and reliability of the final model [128]. Similarly, in a dexmedetomidine nasal spray PopPK analysis, bootstrap validation demonstrated model robustness, with the estimated population typical values for CL, V2, Q, Vp, KA, F1, and ALAG remaining consistent across resampled datasets [129].
Cross-Validation Implementation Protocol
Workflow Design
The cross-validation protocol employs the following structured approach:
Data Partitioning: Divide the dataset into k subsets of approximately equal size. For leave-one-out cross-validation, k equals the number of individuals.
Iterative Model Building: For each iteration:
- Retain one subset as the validation data
- Use the remaining k-1 subsets as training data
- Estimate model parameters using only the training data
- Predict concentrations for the validation individuals
- Calculate prediction error metrics
Performance Metrics Calculation: Compute overall performance metrics across all iterations, including mean prediction error (MPE) for bias and root mean squared prediction error (RMSPE) for precision.
For BS-CV, the process is modified to use bootstrap resampling, where each bootstrap sample serves as training data and the out-of-bag observations as validation data [127].
Model Selection Criteria
The cross-validation results guide model selection through several criteria:
- Predictive Performance: Models with lower prediction errors across validation sets are preferred.
- Stability: Consistent performance across different data partitions indicates model robustness.
- Parsimony: Among models with similar predictive performance, the simplest model is selected to enhance generalizability.
This approach was implicitly applied in a pyrazinamide PopPK study, where the dataset was divided into training and test sets at a 4:1 ratio, and the model demonstrated better predictive performance compared to previously published models when applied to the test set [125].
Integrated Uncertainty Assessment Protocol
For comprehensive model uncertainty evaluation, bootstrap and cross-validation methods should be integrated:
Bootstrap-Based Model Validation: Perform case bootstrap with 1000 samples to estimate parameter distributions and confidence intervals.
Bootstrap Cross-Validation: Implement BS-CV to assess predictive performance and model stability.
Visual Predictive Check: Simulate datasets based on the final model and compare the distribution of observed data with model predictions.
Covariate Impact Assessment: Use forest plots to visualize the effect of identified covariates on key PK parameters, as demonstrated in teicoplanin PopPK analyses [77].
This integrated approach was applied in a vancomycin PopPK study, where bootstrap validation, goodness-of-fit plots, and visual predictive checks collectively demonstrated model stability and reliability [128].
Applications in Anti-Infective Dose Optimization
PopPK Model Development for Anti-Infectives
Population pharmacokinetic modeling plays a pivotal role in anti-infective development by quantifying drug exposure and its relationship to patient factors. For anti-infectives, PK/PD indices such as the area under the concentration-time curve to minimum inhibitory concentration ratio (AUC/MIC) serve as critical predictors of efficacy [11] [77]. The European Medicines Agency emphasizes the use of PK/PD analyses to identify potentially efficacious dose regimens of antibacterial agents, including the determination of probability of target attainment (PTA) [130].
In PopPK model development for anti-infectives, bootstrap methods validate parameter estimates, while cross-validation ensures robust covariate selection. For instance, in a linezolid PopPK study, bootstrap techniques would be essential to quantify the uncertainty in clearance estimates, particularly given the identified influences of renal function and severe liver impairment on pharmacokinetics [131]. Similarly, in teicoplanin PopPK analyses, bootstrap methods help validate the impact of covariates such as body weight, postmenstrual age, and renal function on drug clearance [77].
Model-Informed Precision Dosing
Model-informed precision dosing (MIPD) represents a key application of PopPK models in anti-infective therapy, leveraging patient-specific factors to individualize dosing regimens. MIPD-based therapeutic drug monitoring (TDM) uses population PK models and prospective Bayesian forecasting to reduce variability in treatment responses and optimize anti-infective therapy [125]. However, the successful implementation of MIPD depends critically on the quantification and communication of model uncertainty.
Bootstrap methods support MIPD by providing confidence intervals around model-based dosing recommendations. For example, in a vancomycin PopPK model for pediatric patients, Monte Carlo simulations based on bootstrap-validated parameter estimates were used to explore trough concentrations under different dosing regimens in patients with varying renal function [128]. This approach enables clinicians to assess not only the recommended dose but also the certainty of this recommendation across the patient population.
Cross-validation further strengthens MIPD by ensuring that models maintain predictive accuracy when applied to new patients. In pyrazinamide therapy, where geriatric patients with diabetes mellitus demonstrated 30% higher apparent clearance, cross-validation would verify that this covariate relationship generalizes beyond the development cohort [125]. This is particularly important for anti-infectives, where suboptimal exposure can lead to treatment failure and antimicrobial resistance.
Table 2: Research Reagent Solutions for PopPK Uncertainty Analysis
| Tool Category | Specific Software/Platform | Primary Function | Application Example |
|---|---|---|---|
| Modeling Software | NONMEM (v7.4+) | Non-linear mixed-effects modeling | PopPK model development and parameter estimation [132] [128] |
| Automation Tools | Perl-speaks-NONMEM (PsN) | Automation of bootstrap, cross-validation | Covariate screening, model validation [128] |
| Statistical Analysis | R (v4.3.1+) with specialized packages | Data visualization, statistical diagnostics | Bootstrap diagnostics, visual predictive checks [128] |
| Simulation Platforms | Monte Carlo Simulation | Probability of target attainment | Dose regimen evaluation for anti-infectives [77] |
Case Study: Vancomycin PopPK in Pediatric Patients
A recent study established a vancomycin PopPK model for pediatric patients using a one-compartment model with first-order elimination [128]. The model identified body weight and glomerular filtration rate as significant covariates affecting clearance. To handle model uncertainty, the researchers implemented a comprehensive bootstrap validation procedure:
Bootstrap Implementation: 1000 bootstrap datasets were generated by case resampling, and the model was re-estimated for each dataset.
Parameter Distributions: The bootstrap results provided empirical distributions for all model parameters, enabling calculation of 95% confidence intervals.
Model Stability: The similarity between original parameter estimates and bootstrap medians confirmed model stability.
Predictive Performance: Visual predictive checks based on bootstrap simulations validated the model's predictive capabilities.
The bootstrap analysis revealed that the typical values for clearance and volume of distribution were 8.22 L/h and 113 L, respectively, with narrow confidence intervals indicating precise estimation [128]. This rigorous uncertainty quantification supported the subsequent Monte Carlo simulations, which evaluated trough concentrations across different renal function groups and dosing regimens, providing a robust foundation for clinical dosing recommendations.
Bootstrap and cross-validation methods provide essential methodologies for quantifying and addressing model uncertainty in population pharmacokinetic modeling for anti-infective dose optimization. Through rigorous implementation of these techniques, researchers can develop more robust PopPK models, validate covariate relationships, and generate reliable dosing recommendations with quantified uncertainty. The integration of bootstrap methods for parameter uncertainty estimation and cross-validation for predictive performance assessment creates a comprehensive framework for model evaluation that enhances the credibility of model-informed precision dosing in anti-infective therapy.
As PopPK modeling continues to evolve, advances in bootstrap cross-validation and other resampling techniques will further strengthen our ability to quantify model uncertainty, particularly for complex models with nonlinear kinetics and extensive covariate relationships. These methodological refinements will ultimately support more precise and individualized anti-infective dosing across diverse patient populations, improving therapeutic outcomes while minimizing toxicity risks.
Population pharmacokinetic (PopPK) modeling is an advanced quantitative analysis tool essential for characterizing the variability in drug exposure among individuals and optimizing dosing regimens [79]. In the critical field of anti-infective drug development, where overcoming resistance and ensuring efficacy is paramount, these models are particularly valuable for supporting dosing evaluation, setting clinical breakpoints, and dosing individualization [66]. The success of PopPK analyses heavily depends on the software tools employed, with NONMEM (Nonlinear Mixed Effects Model) and Certara's Phoenix Platform representing two of the most established and widely used standards in the pharmacometrics industry. This application note provides a detailed comparison of these two tools, framing their strengths within the context of anti-infective dose optimization research. We summarize their key features, present experimental protocols for their application, and visualize their workflows to guide researchers in selecting and implementing the appropriate tool for their projects.
NONMEM
NONMEM is one of the oldest and most widely recognized software tools for nonlinear mixed-effects modeling, forming the cornerstone of many published PopPK analyses [133] [134]. Its core strength lies in its powerful estimation algorithms, such as First Order Conditional Estimation with Interaction (FOCEI), which are capable of handling complex, hierarchical models typical in clinical pharmacology. A distinctive feature of NONMEM is its PRIOR subroutine, which allows for Bayesian and "frequentist" prior information to be incorporated into model parameters. This is particularly useful for analyzing sparse data from special populations, such as critically ill patients or children, by stabilizing parameter estimation and improving model convergence [135].
Phoenix
The Phoenix Platform is an integrated software suite that provides comprehensive tools for PK/PD modeling, from non-compartmental analysis (NCA) to PopPK and pharmacodynamic (PD) modeling [136]. A key component is Phoenix NLME, which performs population modeling. Phoenix is designed as an all-in-one decision support system, bridging the gap between discovery and clinical phases. Its strengths include a user-friendly graphical interface, and it is trusted by major regulatory agencies worldwide, including the US FDA [136]. It integrates various analysis types, such as NCA and IVIVC (In Vitro-In Vivo Correlation), within a single workflow.
The table below summarizes the quantitative data and key characteristics of NONMEM and Phoenix based on current literature and industry usage.
Table 1: Key Comparison of NONMEM and Phoenix
| Feature | NONMEM | Phoenix |
|---|---|---|
| Primary Strength | Gold standard for NLME; Highly flexible and powerful estimation methods [134] | Integrated, user-friendly platform for end-to-end PK/PD analysis [136] |
| Key Distinctive Feature | PRIOR subroutine for incorporating prior information [135] |
Seamless workflow from NCA to population modeling and IVIVC [136] |
| Typical Use Case | Methodological research; Complex model development; Handling sparse data with priors [135] | Efficient, streamlined analysis from preclinical to clinical stages; Regulatory submissions [136] |
| Industry Adoption | Extensively published and cited over decades [79] | Used by 2,600 companies and 11 global regulatory agencies [136] |
| Handling of Sparse Data | Can use PRIOR subroutine to stabilize parameters [135] |
Naïve pooled and NLME engines available; performance can be sensitive to initial estimates in some cases [137] |
| Computational Approach | Maximum Likelihood (e.g., FOCE), Bayesian methods [135] [133] | True maximum likelihood estimators (Phoenix Model) and iterated weighted least squares (WNL Classic) [137] |
Table 2: Analysis of Suitable Application Contexts
| Research Scenario | Recommended Tool | Rationale |
|---|---|---|
| Analyzing sparse data from a special population (e.g., critically ill, pediatric) | NONMEM | The PRIOR subroutine allows integration of existing knowledge to stabilize parameter estimation, which is often necessary with limited data [135]. |
| Routine PopPK analysis as part of an integrated drug development workflow | Phoenix | The unified platform streamlines the process from raw data (NCA) to model building (NLME) and reporting, improving efficiency [136]. |
| Research requiring the most established and referenced tool | NONMEM | As the historical gold standard, NONMEM is backed by a vast body of literature and is deeply embedded in pharmacometrics research [79] [134]. |
| Leveraging Machine Learning/AI in PopPK | Emerging Area | Recent research shows AI/ML models can complement traditional tools; Neural ODEs show promise for large datasets and can be implemented in both NONMEM and Monolix [134]. |
Experimental Protocols for Anti-Infective Dose Optimization
This section outlines detailed methodologies for applying NONMEM and Phoenix to a typical PopPK analysis in anti-infective development, using the determination of an optimal dosing regimen as an objective.
Protocol 1: PopPK Model Development with NONMEM
Application Note: This protocol details the use of NONMEM's PRIOR subroutine to develop a PopPK model for a new anti-infective drug in a special population (e.g., critically ill patients) where data may be sparse, but prior information from healthy volunteer studies exists.
Materials and Software:
- Software: NONMEM (v7.4 or higher), Pirana (v2.8.0 or higher) or similar model management tool, PsN toolkit (v4.9.0 or higher), R (v3.5.1 or higher) with Xpose (v4.0 or higher) [138].
- Data: Patient demographic data, dosing records, and drug concentration-time data.
Procedure:
- Data Preparation: Prepare the dataset in a format suitable for NONMEM (e.g., CSV). Define all required columns ($INPUT) such as ID, TIME, AMT, DV, EVID, and relevant covariates (e.g., WT, AGE, renal function).
- Base Model Development:
- Select a structural model (e.g., one- or two-compartment) using the FOCE-I estimation algorithm.
- Parameterize inter-individual variability (IIV) on key parameters (e.g., CL, V) using an exponential model.
- Select a residual error model (e.g., combined additive and proportional).
- Evaluate model fit using goodness-of-fit (GOF) plots and the objective function value (OFV).
- Defining and Implementing the Prior:
- Select a Reference Model: Identify a previous PopPK model from a similar compound or a different population. Assess its relevance based on population similarity and parameter precision [135].
- Code the
$PRIORSubroutine: In the NONMEM control stream, use$PRIOR NWPRIto inform the subroutine that a prior will be used. Specify the prior parameter values (hyperparameters) and their variance (omega block) from the reference model.
- Model Estimation: Run the model with the
$PRIORsubroutine. The OFV will now be the sum of the likelihood from the data and a penalty function based on the deviation from the prior estimates [135]. - Model Evaluation:
- Check Similarity: Compare the final parameter estimates with those from the reference model.
- Sensitivity Analysis: Assess the model's sensitivity to the prior values.
- Standard Diagnostics: Perform visual predictive checks (VPC) and bootstrap analysis to evaluate predictive performance and model stability [138].
Troubleshooting: If the model fails to converge, check the adequacy of the prior information and its weighting. Vague (non-informative) priors can be used for parameters with sufficient information in the new data [135].
Protocol 2: Exposure-Response Analysis with Phoenix
Application Note: This protocol describes an integrated workflow in Phoenix to establish an exposure-response relationship for an anti-infective agent, linking drug exposure (e.g., AUC) to a biomarker of disease severity (e.g., SOFA score in sepsis) to support dose selection for a Phase IIb trial [138].
Materials and Software:
- Software: Certara Phoenix Platform (v7.0 or higher) with WinNonlin and NLME engines.
- Data: Patient PK concentration-time data, PD biomarker data (e.g., daily SOFA scores), and covariate data.
Procedure:
- Non-Compartmental Analysis (NCA):
- Use the Phoenix WinNonlin module to perform NCA on the PK data.
- Calculate key exposure metrics like
AUC0-8h,Cmax, andTmaxfor each individual. These can be used for initial exposure-response exploration or as inputs for the PopPK model [138].
- Population PK Model Development:
- Use the Phoenix NLME module to build a PopPK model.
- Import the structural model and parameter estimates from the NCA step as initial estimates to aid convergence [122].
- Use the graphical interface to define the model structure, IIV, and residual error.
- Run the model using the FOCE-ELS algorithm and evaluate using GOF plots.
- Exposure-Response Model Development:
- Link the individual PK parameters (e.g., AUC) from the final PopPK model to the PD biomarker using an appropriate model. For a sepsis drug, this could be an inhibitory indirect response model [138].
- The model should account for both the drug effect and the standard of care therapy effect. A latent-variable approach can be used to differentiate these effects [138].
- Model Validation and Simulation:
- Validate the final model using a prediction-corrected visual predictive check (pcVPC).
- Perform Monte Carlo simulations (e.g., 1000 times) based on the built model to simulate the PD response (e.g., SOFA score on day 7) across a range of doses or exposures [138].
- Identify the exposure target (e.g., AUC) that produces the maximal desired effect and recommend the corresponding dose for the next trial phase.
Troubleshooting: If the NLME model is sensitive to initial estimates, try using the naive pooled data analysis function in Phoenix to generate better starting values, or leverage the adaptive single-point methods discussed in recent literature [122] [137].
Workflow Visualization
The following diagram illustrates the logical workflow for a PopPK analysis, integrating steps and decision points from both the NONMEM and Phoenix protocols.
The Scientist's Toolkit: Essential Research Reagents and Software
The table below details key software and methodological "reagents" used in the PopPK experiments described in this note.
Table 3: Essential Tools for PopPK Modeling
| Tool / Method | Function | Application Context |
|---|---|---|
| PRIOR Subroutine (NONMEM) | Incorporates previous parameter estimates as Bayesian priors to stabilize estimation with new, sparse data [135]. | Essential for analyzing data from special populations (e.g., pediatrics, critically ill) where rich data collection is difficult. |
| Naïve Pooled Analysis | Treats all data as if from a single subject to generate initial parameter estimates [122]. | Used in Phoenix and other tools to overcome sensitivity to initial estimates and provide a starting point for NLME. |
| Visual Predictive Check (VPC) | A graphical diagnostic that compares simulated data from the model with the observed data to evaluate predictive performance [138] [139]. | Standard model evaluation step for both NONMEM and Phoenix models. |
| Monte Carlo Simulation | Uses the final model to simulate thousands of virtual patients to predict outcomes under different dosing scenarios [138]. | Critical for justifying dose selection for future clinical trials (e.g., Phase IIb). |
| Inhibitory Indirect Response Model | A pharmacodynamic model structure where the drug inhibits the production or loss of a response biomarker [138]. | Used to model the effect of anti-infective drugs on disease biomarkers like the SOFA score in sepsis. |
| Machine Learning / Neural ODEs | Emerging AI-based approaches for PK prediction that can handle complex patterns and may offer advantages with large datasets [134]. | A growing area of research to complement traditional PopPK, with implementations becoming available in standard software. |
Both NONMEM and Phoenix are powerful, industry-standard tools for PopPK modeling with distinct strengths. The choice between them should be guided by the specific research question and context. NONMEM, with its unparalleled flexibility and features like the PRIOR subroutine, is exceptionally well-suited for novel methodological research and for analyzing complex or sparse datasets. Phoenix, with its integrated and user-friendly platform, excels in streamlining the entire PK/PD workflow, from initial data exploration through final modeling and simulation, making it highly efficient for drug development projects. In the critical endeavor of anti-infective dose optimization, leveraging the strengths of either tool—or a combination thereof—enables robust quantification of drug behavior and supports the development of effective, personalized dosing regimens.
Building Reproducible and Standardized Workflows for Regulatory Submission
Within anti-infective drug development, population pharmacokinetic (PopPK) modeling is a cornerstone for informing dose selection, especially in critically ill patients who exhibit significant pharmacokinetic variability. The efficacy of this research is ultimately proven through successful regulatory submission and approval. This application note provides a detailed protocol for establishing reproducible and standardized workflows that integrate PopPK analysis for anti-infective dose optimization into regulatory submissions. It is framed within a broader research thesis on model-informed precision dosing (MIPD) of anti-infectives, addressing the critical need for robust, audit-ready processes that satisfy evolving regulatory expectations for transparency and computational reproducibility [140] [141].
Core Principles and Regulatory Context
Regulatory agencies are increasingly formalizing expectations for the use of model-informed approaches and artificial intelligence/machine learning (AI/ML) in drug development. A foundational shift towards a credibility framework is evident, where regulators require a documented chain linking the Context of Use (COU) of a model to its design, validation datasets, performance metrics, and monitoring plans [140]. For PopPK models supporting a dosing recommendation, the COU must be precisely defined.
Furthermore, the FDA's 2025 draft guidance emphasizes data quality, representativeness, and bias assessment. Sponsors must demonstrate that training and validation datasets are representative of the target population, requiring transparent data lineage and demographic analyses [140]. The guidance also formalizes Predetermined Change Control Plans (PCCPs), which are critical for managing planned model updates without a full resubmission, provided rigorous governance and validation workflows are in place [140] [142].
Finally, a hybrid programming environment using both SAS and R is becoming the operational standard. While SAS provides a proven, compliant framework for core data manipulation and standard statistical analysis, R offers superior flexibility for advanced statistical modeling, machine learning, and visualization [143]. A modern Statistical Computing Environment (SCE) is necessary to manage this coexistence, ensuring end-to-end traceability, version control, and reproducibility across both languages [143].
Experimental Protocols
Protocol for Developing a PopPK Model for Anti-Infectives
This protocol outlines the key steps for building a PopPK model, from study design through to model evaluation, ensuring data and processes are submission-ready.
1. Study Design and Data Collection
- Patient Population: Enroll patients representing the intended clinical population (e.g., critically ill, specific infection types). For example, a study on linezolid recruited hematooncological patients with sepsis [118], while a voriconazole study focused on patients with COVID-19-associated pulmonary aspergillosis [3].
- Dosing and Sampling: Administer the anti-infective and collect rich or sparse pharmacokinetic blood samples. Protocols may include sampling at 1, 2, 4, 6, and 8 hours after infusion initiation to capture the concentration-time profile [118].
- Data Recorded: Collect demographic (age, weight), clinical (e.g., disease state), laboratory (e.g., serum creatinine, C-reactive protein, liver enzymes), and genetic data (e.g., CYP450 genotypes for metabolized drugs) [118] [3].
2. Bioanalytical Method
- Quantify drug concentrations in plasma using a validated method, such as Ultra-Performance Liquid Chromatography–tandem mass spectrometry (UPLC-MS/MS) [118] or High-Performance Liquid Chromatography (HPLC) [3]. The method should be documented with details on calibration curves, precision, and accuracy.
3. Population PK Modeling
- Software: Use non-linear mixed-effects modeling (NONMEM) software or equivalent packages in R (e.g.,
nlmixr) within a validated SCE [118] [143]. - Structural Model: Test compartmental models (e.g., one- or two-compartment) to describe the drug's concentration-time profile. A two-compartment model is often found to be the best fit [4] [5].
- Statistical Model: Quantify inter-individual variability (IIV) and residual unexplained variability.
- Covariate Model: Identify patient factors that explain IIV using a stepwise approach. Common significant covariates include renal function (eGFR, CrCl) on clearance [4] [5], age [118], and body size on volume of distribution [4].
- Model Evaluation: Validate the final model using goodness-of-fit plots, visual predictive checks, and bootstrap analysis.
4. Model-Based Simulations for Dose Optimization
- Use the final PopPK model to perform Monte Carlo simulations [118] [4] [3].
- Simulate thousands of virtual patients receiving different dosing regimens (e.g., varying doses, infusion durations).
- Calculate the Probability of Target Attainment (PTA) for relevant pharmacokinetic/pharmacodynamic (PK/PD) indices (e.g., %fT>MIC for beta-lactams [4], AUC/MIC for linezolid [118]).
- Propose an optimized dosing regimen that maximizes PTA while minimizing toxicity risk across different patient subgroups.
Protocol for Ensuring Regulatory-Grade Reproducibility
This protocol supplements the scientific workflow with steps to ensure computational reproducibility and readiness for regulatory scrutiny.
1. Define Context of Use (COU)
- Before analysis, explicitly document the COU for the PopPK model. For example: "To recommend an optimized dosing regimen for levetiracetam in pediatric patients aged 0.5-12 years based on body weight and renal function" [144].
2. Establish a Statistical Computing Environment (SCE)
- Implement an SCE that supports both SAS and R, providing unified data access, version control (e.g., Git), automated execution, and immutable logging of all analyses [143].
3. Implement Code and Data Management
- Data: Use controlled terminologies and standard data structures (e.g., CDISC SDTM). Maintain immutable, versioned datasets with clear provenance.
- Code: Write modular, well-commented scripts. For R, use a controlled package repository (e.g.,
packratorrenv) to manage specific package versions and ensure dependency stability [143]. - Validation: Establish a process for validating R code and outputs, which may include cross-verification with SAS for key results [143].
4. Document the Workflow
- Generate a complete audit trail. This includes logs of all software versions, code executed, and outputs generated for the final analysis.
Data Presentation
Key Outputs from PopPK Dose Optimization Studies
The following table summarizes quantitative results and dosing recommendations from recent PopPK studies, illustrating the application of the described workflow.
Table 1: Summary of Recent PopPK Model-Based Dose Optimization Findings
| Anti-Infective Agent | Patient Population | Key Covariates | PK/PD Target | Proposed Optimized Regimen |
|---|---|---|---|---|
| Linezolid [118] | Hematooncological patients with sepsis | Age, Time-dependent clearance | AUC₂₄/MIC 80-120 | Age-scaled dosing, Loading dose, Continuous infusion |
| Piperacillin/Tazobactam [4] | Healthy adults (Baseline for patients) | BSA-adjusted eGFR, Body Weight | 50% fT>MIC & 100% fT>MIC | Standard regimen (4/0.5 g q6h) inadequate for high eGFR (≥130 mL/min); Extended/continuous infusion proposed |
| Aztreonam-Avibactam [5] | Adults with serious infections | Time-varying CrCl, Infection type | Joint PTA: Aztreonam 60% fT>8 mg/L & Avibactam 50% fT>2.5 mg/L | Approved regimen (loading + maintenance, 3h infusion) achieved 89->99% joint PTA across renal function |
| Voriconazole [3] | CAPA patients | CRRT, CRP, GGT, AST, Platelets | Trough Concentration 1-5 mg/L | Higher loading and maintenance doses required for patients on CRRT |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Software for PopPK/PD Workflows
| Item Name | Function/Brief Explanation |
|---|---|
| NONMEM | Industry-standard software for nonlinear mixed-effects modeling. |
R & nlmixr |
Open-source language and package for pharmacometric modeling, offering advanced flexibility [143]. |
| SAS | Validated software for clinical data manipulation, analysis, and reporting, ensuring regulatory compliance [143]. |
| Statistical Computing Environment (SCE) | A unified platform (e.g., Instem) that provides governance, traceability, and reproducibility for multi-language (SAS, R) workflows [143]. |
| Monolix Suite | User-friendly software utilizing the Stochastic Approximation Expectation-Maximization (SAEM) algorithm for PopPK analysis [118]. |
| UPLC-MS/MS | Ultra-Performance Liquid Chromatography-tandem Mass Spectrometry; a highly sensitive and specific bioanalytical method for quantifying drug concentrations in biological samples [118]. |
| Predetermined Change Control Plan (PCCP) | A regulatory document outlining planned future model updates and the validation controls that ensure safety, allowing for iterative improvement without full resubmission [140] [142]. |
Visualization of Workflows
End-to-End PopPK Analysis and Submission Workflow
PopPK to Regulatory Submission Workflow
AI-Enhanced Regulatory Review and Submission Process
AI in Regulatory Submission and Review
Conclusion
Population pharmacokinetic modeling has firmly established itself as an indispensable tool for optimizing anti-infective dose regimens, especially in complex and variable critically ill populations. By systematically understanding the foundations, applying rigorous methodologies, and adhering to robust validation practices, researchers can effectively characterize and account for PK variability. The future of PopPK is being shaped by increased automation through machine learning, which promises to accelerate model development and enhance reproducibility. The continued integration of these advanced modeling techniques into clinical practice is paramount for advancing personalized medicine, improving patient outcomes in severe infections, and effectively addressing the global challenge of antimicrobial resistance.
References
- 1. Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 2. Nonlinear Mixed-Effects Modeling of Population ... [https://www.mathworks.com/company/technical-articles/nonlinear-mixed-effects-modeling-of-population-pharmacokinetics-data.html]
- 3. Population pharmacokinetics and dose optimization of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1554370/full]
- 4. Population Pharmacokinetic Modeling of Piperacillin ... [https://www.mdpi.com/1424-8247/18/8/1124]
- 5. Population pharmacokinetic/pharmacodynamic modeling ... [https://pubmed.ncbi.nlm.nih.gov/40530972/]
- 6. Example of a Pharmacometrics Visualization [https://www.inetsoft.com/info/pharmacometrics-software-example/]
- 7. Visualization and Communication of Pharmacometric Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055786/]
- 8. Choosing color palettes for scientific figures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7040535/]
- 9. Pharmacokinetic variability and significance of therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912797/]
- 10. Understanding antimicrobial pharmacokinetics in critically ... [https://www.sciencedirect.com/science/article/pii/S2667100X24000094]
- 11. Pharmacokinetic and Pharmacodynamic Principles of Anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5039113/]
- 12. What Is Population Pharmacokinetic (popPK) Analysis? [https://www.allucent.com/resources/blog/what-population-pharmacokinetic-poppk-analysis]
- 13. Population PK (PopPK): The What, The How, and The Why [https://www.quantics.co.uk/blog/poppk-the-what-the-how-and-the-why/]
- 14. In the Cradle of Pharmacometric Methodology - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087688/]
- 15. Pharmacokinetic Alterations Associated with Critical Illness [https://pmc.ncbi.nlm.nih.gov/articles/PMC9894673/]
- 16. How critical illness impacts drug pharmacokinetics and ... [https://pharmaceutical-journal.com/article/ld/how-critical-illness-impacts-drug-pharmacokinetics-and-pharmacodynamics]
- 17. Pharmacokinetics in sepsis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7807908/]
- 18. Impact of altered aminoglycoside volume of distribution on ... [https://pubmed.ncbi.nlm.nih.gov/9663254/]
- 19. External validation of population pharmacokinetic models ... [https://www.sciencedirect.com/science/article/pii/S2213716525001195]
- 20. Clinical Pharmacokinetics and Dose Optimization of Anti ... [https://www.mdpi.com/journal/antibiotics/special_issues/7O743L01P9]
- 21. The relation between inflammatory biomarkers and drug ... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-024-05150-4]
- 22. Covariates in population pharmacokinetic studies of critically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10895699/]
- 23. Parametric Population Pharmacokinetics Model Repository of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009037/]
- 24. Population pharmacokinetic analysis and dosing ... [https://www.sciencedirect.com/science/article/pii/S0924857924002620]
- 25. Population Pharmacokinetic Models (PopPK) and Their ... [https://lajclinsci.com/vD-7-21]
- 26. Interpreting population pharmacokinetic-pharmacodynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3099367/]
- 27. Population pharmacokinetic analysis and dosing ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1122310/full]
- 28. Generating and Modeling Virtual Patient Data from ... [https://www.mdpi.com/1424-8247/18/11/1748]
- 29. Model-informed drug development in public health emergency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587539/]
- 30. Population Pharmacokinetics [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/population-pharmacokinetics]
- 31. Division of Pharmacometrics [https://www.fda.gov/about-fda/cder-offices-and-divisions/division-pharmacometrics]
- 32. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 33. Reporting the results of population pharmacokinetic analyses [https://www.ema.europa.eu/en/reporting-results-population-pharmacokinetic-analyses-scientific-guideline]
- 34. Clinical pharmacology and pharmacokinetics [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics]
- 35. EMA Draft Guidance on Mechanistic Models in ... [https://www.vph-institute.org/news/ema-draft-guidance-on-mechanistic-models-in-model-informed-drug-development-midd.html]
- 36. Population pharmacokinetics and dosing optimization of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.1045895/full]
- 37. a post hoc analysis of a pharmacokinetic study of morphine ... [https://pubmed.ncbi.nlm.nih.gov/22381713/]
- 38. Population approaches/sparse data analysis for human ... [https://www.sciencedirect.com/science/article/pii/S1382668996000555]
- 39. Outlier analysis for accelerating clinical discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC11111092/]
- 40. Combating Antimicrobial Resistance Through a Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584525/]
- 41. Outlier Mining in High Throughput Screening Experiments [https://www.sciencedirect.com/science/article/pii/S2472630322001273]
- 42. Use of Pharmacokinetic Data Below Lower Limit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3422429/]
- 43. Handling Missing and BLQ Data [https://docs.pumas.ai/stable/nca/blq_handling/]
- 44. In vitro pharmacokinetic/pharmacodynamic models in anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3042695/]
- 45. PK/PD-Guided Strategies for Appropriate Antibiotic Use in ... [https://www.mdpi.com/2079-6382/14/1/92]
- 46. Physiologically Based Pharmacokinetic Modeling of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189772/]
- 47. Compartmental models (epidemiology) [https://en.wikipedia.org/wiki/Compartmental_models_(epidemiology)]
- 48. Simulating Compartmental Models in Epidemiology using ... [https://medium.com/data-science/simulating-compartmental-models-in-epidemiology-using-python-jupyter-widgets-8d76bdaff5c2]
- 49. Drug Absorption - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557405/]
- 50. Oral Cephalexin Population Pharmacokinetics and Target ... [https://pubmed.ncbi.nlm.nih.gov/40995926/]
- 51. Improving Pharmacokinetic-Pharmacodynamic Modeling to ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1003151]
- 52. 群体药物动力学及其在新药研究中的应用 [https://html.rhhz.net/YXXB/html/20170305.htm]
- 53. 群体药代动力学及其在药物研发中的应用 [https://unionclin.com/News/193.html]
- 54. 计算生物学- MATLAB 和Simulink 解决方案 [https://ww2.mathworks.cn/solutions/computational-biology.html]
- 55. 直播回顾| Phoenix WinNonlin在抗菌药物PKPD建模和模拟 ... [https://www.tri-ibiotech.com/news/2243]
- 56. Population Pharmacokinetic Modeling of Piperacillin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389047/]
- 57. Population Pharmacokinetic Analysis of Balcinrenone in ... [https://link.springer.com/article/10.1007/s40262-025-01572-7]
- 58. A Systematic Analysis Using PBPK Modeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC12304071/]
- 59. Population pharmacokinetics of teicoplanin and dosage ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1621959/full]
- 60. The Role of PK/PD Analysis in the Development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8230268/]
- 61. Optimización del régimen de dosificación de antibióticos a ... [http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1609-91172024000300014]
- 62. Farmacocinética y farmacodinámica de los antibióticos ... [https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-63432022000300012&lng=es&nrm=iso&tlng=es]
- 63. Farmacocinética y farmacodinamia de antimicrobianos [https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0716-10182004021100008]
- 64. Pharmacodynamic Parameters of Pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8989418/]
- 65. Pharmacokinetic/Pharmacodynamic (PK/PD) Indices of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3186970/]
- 66. Clinical applications of population pharmacokinetic models ... [https://www.sciencedirect.com/science/article/pii/S1043661818307503]
- 67. Optimization of antimicrobial therapy in critically ill patients ... [https://www.sciencedirect.com/science/article/pii/S2352556825000931]
- 68. Beta-Lactam Dose Optimisation in the Intensive Care Unit [https://www.mdpi.com/2079-6382/12/5/870]
- 69. Vancomycin levels for Bayesian dose-optimization in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1575224/full]
- 70. International survey of antibiotic dosing and monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10278304/]
- 71. Population Pharmacokinetics of Imipenem in Critically Ill ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7329758/]
- 72. Population pharmacokinetics of polymyxin B in critically ill ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1511088/full]
- 73. What is the -2LL or the Log-likelihood Ratio? [https://www.certara.com/knowledge-base/what-is-the-2ll-or-the-log-likelihood-ratio/]
- 74. 3.1 Model selection criteria | Stat 340 Notes: Fall 2025 [https://bookdown.org/ltupper/340f25_notes/model-selection-criteria.html]
- 75. AIC BIC Model Selection: The Ultimate 2025 Guide Made Easy [https://econometriclinks.com/aic-bic-model-selection/]
- 76. AIC and BIC: Time Series Forecasting Model Selection [https://www.junglebot.app/en/aic-and-bic-time-series-forecasting-model-selection/]
- 77. A Comprehensive Analysis of Teicoplanin Population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577477/]
- 78. Population Pharmacokinetics of Tigecycline and ... [https://pubmed.ncbi.nlm.nih.gov/41244714/]
- 79. Global research on the utilization of population ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1548023/full]
- 80. Population Pharmacokinetic Modeling Analysis of ASC10, a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398292/]
- 81. Probabilistic nested model selection in pharmacokinetic ... [https://www.nature.com/articles/s41598-024-83306-6]
- 82. External validation of vancomycin population ... [https://www.sciencedirect.com/science/article/pii/S2213716522001217]
- 83. Partial Residual Plots as an Integrated Model Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11652818/]
- 84. Integrated Population Pharmacokinetic-pharmacodynamic ... [https://link.springer.com/article/10.1208/s12248-025-01136-4]
- 85. Subgroup-based model selection to improve the prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406661/]
- 86. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 87. PopED: An extended, parallelized, nonlinear mixed effects ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260712001319]
- 88. PFIM 4.0, an extended R program for design evaluation ... [https://pubmed.ncbi.nlm.nih.gov/29428073/]
- 89. POPED, a software for optimal experiment design in ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/14992824/]
- 90. Population Fisher information matrix and optimal design of ... [https://pubmed.ncbi.nlm.nih.gov/21660504/]
- 91. Using Fisher Information Matrix to predict uncertainty in ... [https://pubmed.ncbi.nlm.nih.gov/40659916/]
- 92. PopED [https://andrewhooker.github.io/PopED/]
- 93. Predictive performance of population pharmacokinetic ... [https://pubmed.ncbi.nlm.nih.gov/40353524/]
- 94. Clinical applications of population pharmacokinetic models ... [https://pubmed.ncbi.nlm.nih.gov/30033398/]
- 95. Advancing Anti-Infective Drug Discovery: The Pivotal Role ... [https://www.sciencedirect.com/science/article/pii/S3050787125001179]
- 96. pyDarwin machine learning algorithms application and ... [https://link.springer.com/article/10.1007/s10928-024-09932-9]
- 97. Artificial Intelligence (AI) Applications in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510778/]
- 98. Machine Learning Based Model Selection with pyDarwin in ... [https://www.page-meeting.org/?abstract=10417]
- 99. Machine learning model selection with Darwin in Pirana [https://www.certara.com/on-demand-webinar/machine-learning-model-selection-with-darwin-in-pirana/]
- 100. AI Models to Assist Vancomycin Dosage Titration [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.801928/full]
- 101. Population pharmacokinetic modeling and clinical ... [https://www.nature.com/articles/s41598-021-82312-2]
- 102. Applications of Pharmacometrics in the Clinical Development and Pharmacotherapy of Anti-Infectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3809903/]
- 103. Pharmacokinetic/Pharmacodynamic Modeling and Application in Antibacterial and Antifungal Pharmacotherapy: A Narrative Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9330032/]
- 104. Expert PK/PD Statistical Data Analysis Services for Trial ... [https://www.navitaslifesciences.com/expert-pk-pd-statistical-data-analysis-services-for-trial-efficiency]
- 105. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 106. Optimization of meropenem dosage in the critically ill population based on renal function - PubMed [https://pubmed.ncbi.nlm.nih.gov/21136037/]
- 107. Cerebrospinal Pharmacokinetic Modeling and Pharmacodynamic Simulation of High-Dose Cefazolin for Meningitis Caused by Methicillin-Susceptible Staphylococcus aureus [https://www.mdpi.com/2079-6382/14/10/1008]
- 108. Population Pharmacokinetics Analysis and Dosing ... [https://www.sciencedirect.com/science/article/pii/S0022354922000259]
- 109. Dose Individualisation of Antimicrobials from a ... [https://link.springer.com/article/10.1007/s40265-024-02084-7]
- 110. Population Pharmacokinetic Modeling of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1662364/abstract]
- 111. Validation and development of population pharmacokinetic ... [https://www.sciencedirect.com/science/article/abs/pii/S1341321X24001466]
- 112. Scoping review of the role of pharmacometrics in model- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528282/]
- 113. Development and external validation of a machine learning ... [https://pubmed.ncbi.nlm.nih.gov/39893767/]
- 114. A population pharmacokinetic model for individualised ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5739632/]
- 115. Artificial Intelligence and Machine Learning Applications to ... [https://www.mdpi.com/2079-6382/13/12/1203]
- 116. Clinical Pharmacokinetics [https://link.springer.com/article/10.1007/s40262-025-01540-1]
- 117. Population pharmacokinetics/pharmacodynamics analysis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1631034/full]
- 118. Population Pharmacokinetic Model‐Based Optimization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409655/]
- 119. Population pharmacokinetic modeling in ... [https://www.frontiersin.org/journals/nuclear-medicine/articles/10.3389/fnume.2025.1695332/full]
- 120. Population pharmacokinetic modeling in radiopharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546074/]
- 121. What is the Difference Between Individual and Population ... [https://www.certara.com/knowledge-base/what-is-the-difference-between-individual-and-population-pk/]
- 122. An automated pipeline to generate initial estimates for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592298/]
- 123. Pharmacokinetic Model Comparisons: How We Do It and Why ... [https://blog.insight-rx.com/resources/pharmacokinetic-model-comparisons-methods]
- 124. Random sparse sampling strategy using stochastic ... [https://www.sciencedirect.com/science/article/pii/S1319016413000133]
- 125. Development of a population pharmacokinetic model ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1116226/full]
- 126. Evaluation of bootstrap methods for estimating uncertainty ... [https://pubmed.ncbi.nlm.nih.gov/24317870/]
- 127. [PDF] Bootstrap Cross-validation Improves Model Selection ... [https://www.semanticscholar.org/paper/Bootstrap-Cross-validation-Improves-Model-Selection-Cavenaugh/aec2aae0d854bc24f0859737fce4ad732648fe3e]
- 128. Establishment of a Vancomycin Population ... [https://link.springer.com/article/10.1007/s40268-025-00523-8]
- 129. Population pharmacokinetic modeling of dexmedetomidine ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1662364/full]
- 130. Use of pharmacokinetics and pharmacodynamics in the ... [https://www.ema.europa.eu/en/use-pharmacokinetics-pharmacodynamics-development-antibacterial-medicinal-products-scientific-guideline]
- 131. Toward precision dosing of linezolid in critical ill patients [https://www.sciencedirect.com/science/article/abs/pii/S001429992500531X]
- 132. Population Pharmacokinetic and Pharmacodynamic Modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539412/]
- 133. Two general methods for population pharmacokinetic modeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC3630269/]
- 134. A Comparative Analysis of NONMEM and AI-based Models ... [https://link.springer.com/article/10.1208/s12248-025-01121-x]
- 135. Prior information for population pharmacokinetic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7520416/]
- 136. Phoenix® PK/PD Platform | PK/PD Analysis & Modeling [https://www.certara.com/software/phoenix-pkpd/]
- 137. Comparison with NONMEM - Phoenix WNL basics [https://forum.certara.com/t/comparison-with-nonmem/2556]
- 138. Exposure-Response Modeling to Support Dosing Selection for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8091127/]
- 139. Population Pharmacokinetic Modelling and Simulation to ... [https://www.mdpi.com/1999-4923/13/5/629]
- 140. What's new in the FDA's 2025 AI/ML draft guidance? [https://blogs.atlas-compliance.ai/whats-new-in-the-fdas-2025-ai-ml-draft-guidance/]
- 141. Faster regulatory submissions for pharma with AI [https://www.mckinsey.com/industries/life-sciences/our-insights/rewiring-pharmas-regulatory-submissions-with-ai-and-zero-based-design]
- 142. AI-Ready Regulatory Submissions for Medical Devices [https://www.regdesk.co/blog/building-ai-ready-submissions-and-future-proofing-regulatory-operations/]
- 143. How R and SAS Can Coexist in Clinical Study Reporting [https://www.instem.com/how_sas_and_r_can_coexist/]
- 144. Physiologically-based pharmacokinetic modeling and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1678960/full]