Pharmacometric Modeling and Simulation: Revolutionizing Anti-Infective Drug Development and Precision Dosing
This article provides a comprehensive overview of the critical role pharmacometric modeling and simulation (M&S) plays in the development and optimization of anti-infective therapies.
Pharmacometric Modeling and Simulation: Revolutionizing Anti-Infective Drug Development and Precision Dosing
Abstract
This article provides a comprehensive overview of the critical role pharmacometric modeling and simulation (M&S) plays in the development and optimization of anti-infective therapies. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles of pharmacokinetic/pharmacodynamic (PK/PD) modeling, its methodological applications in designing effective dosage regimens against resistant pathogens, and its utility in troubleshooting therapy failures and optimizing treatment for special populations. Further, the article examines the validation of these models and their growing acceptance by regulatory agencies, highlighting how this quantitative discipline accelerates timelines, reduces development costs, and paves the way for more personalized and effective antimicrobial pharmacotherapy.
The Essential Primer: Core Principles of Pharmacometrics in Anti-Infective Therapy
Pharmacometrics represents a critical, quantitative discipline in modern drug development, integrating pharmacokinetics (PK), pharmacodynamics (PD), and disease biology to inform decision-making. It employs mathematical models to characterize and predict the time-course of drug effects, accounting for variability in patient populations [1] [2]. Within anti-infective development, these model-informed approaches are transformative, enabling optimized dosing regimens for vulnerable populations, overcoming clinical trial recruitment challenges, and supporting regulatory strategies for accelerated approval [1] [3]. This article details core pharmacometric components and provides applicable protocols for integrating these methods into anti-infective research pipelines.
Pharmacometrics is defined as a science focused on developing and applying mathematical and statistical methods to characterize, understand, and predict the pharmacokinetic and pharmacodynamic behavior of drugs [2]. It serves as a quantitative framework that bridges diverse data sources—from pre-clinical studies, clinical trials, and real-world evidence—to translate drug and disease knowledge into actionable development strategies [3]. In the context of anti-infective therapeutics, pharmacometrics is indispensable for tackling the unique challenges of rapid pathogen evolution, narrow therapeutic windows, and the need for combination therapies to prevent resistance. By integrating models of disease progression, host-pathogen interactions, and drug effects, pharmacometrics provides a powerful toolkit for designing more efficient and informative clinical trials and for tailoring treatments to specific patient subpopulations [2].
Core Components of Pharmacometrics
The practice of pharmacometrics is built upon several interconnected modeling approaches. The table below summarizes the key model types, their definitions, and primary applications in anti-infective development.
Table 1: Core Pharmacometric Modeling Approaches in Anti-Infective Development
| Model Type | Definition | Primary Application in Anti-Infectives |
|---|---|---|
| Population PK (PopPK) [1] | Uses nonlinear mixed-effects models to analyze PK data from all individuals in a study population, quantifying between-subject variability (BSV). | Characterizing drug exposure variability in patients with differing organ function, ages, or disease states to identify covariates for dose adjustment. |
| Physiologically-Based PK (PBPK) [1] [2] | Mechanistic model incorporating physiological, genetic, and biochemical parameters to simulate a drug's ADME (Absorption, Distribution, Metabolism, Excretion). | Predicting drug-drug interaction potential in complex HAART regimens; extrapolating PK from adults to pediatric populations. |
| PK/PD Modeling [2] | Mathematical relationship linking PK (drug concentration) to PD (pharmacological effect), often using an indirect-response or Emax model. | Quantifying the exposure-response relationship for efficacy (e.g., microbial kill) and safety (e.g., QT prolongation) to establish a therapeutic window. |
| Disease Progression (DisP) Modeling [2] | A model that mathematically characterizes the natural time-course of a disease and how a therapeutic intervention alters that trajectory. | Modeling bacterial load dynamics or viral replication in untreated patients and the modifying effect of antimicrobial agents. |
| Quantitative Systems Pharmacology (QSP) [2] | A highly mechanistic framework integrating drug action with systems-level disease biology, often involving multiple interconnected pathways. | Simulating the emergence of antimicrobial resistance and evaluating the efficacy of novel combination therapies to suppress resistant subpopulations. |
| Model-Based Meta-Analysis (MBMA) [2] | A quantitative analysis that integrates and compares data from multiple clinical studies to understand the competitive landscape and drug class effects. | Informing dose selection and trial endpoints by analyzing historical data on standard-of-care anti-infectives. |
Essential Research Reagents and Computational Tools
Successful pharmacometric analysis relies on a combination of high-quality data and sophisticated software. The following table details the essential "toolkit" for researchers in this field.
Table 2: Research Reagent Solutions and Key Resources for Pharmacometric Analysis
| Category / Item | Function and Description |
|---|---|
| Clinical Data | |
| Richly-Sampled PK/PD Data | Provides the foundational data for building and validating PK, PD, and PK/PD models. Crucial for characterizing time-dependent processes. |
| Sparse PopPK Data from Clinical Trials | Used for population analysis to quantify variability and identify patient factors (covariates) influencing drug exposure and response. |
| Biomarker Data (e.g., Viral Load, Bacterial Counts) | Serves as a quantitative PD endpoint for modeling drug effect on the pathogen and disease progression. |
| Software & Computational Tools | |
| NONMEM (Nonlinear Mixed Effects Modeling) | The industry-standard software for population PK/PD analysis using nonlinear mixed-effects models. |
| R or Python | Open-source programming languages used for data preparation, exploratory analysis, model diagnostics, and visualization (e.g., using the xpose and ggplot2 packages in R) [4]. |
| PBPK Software (e.g., GastroPlus, Simcyp) | Specialized platforms containing physiological and demographic libraries to develop and simulate PBPK models. |
| Graphviz (DOT language) | An open-source graph visualization tool used to create clear diagrams of model structures, workflows, and biological pathways, as utilized in this document. |
Experimental Protocol for an Integrated PopPK/PD Analysis
This protocol outlines a standardized workflow for conducting a population PK/PD analysis to support anti-infective development.
Objective: To develop a PopPK model for a novel anti-infective drug, followed by a PD model linking drug exposure to a biomarker of efficacy (e.g., viral load), and to perform clinical trial simulations to evaluate proposed dosing regimens.
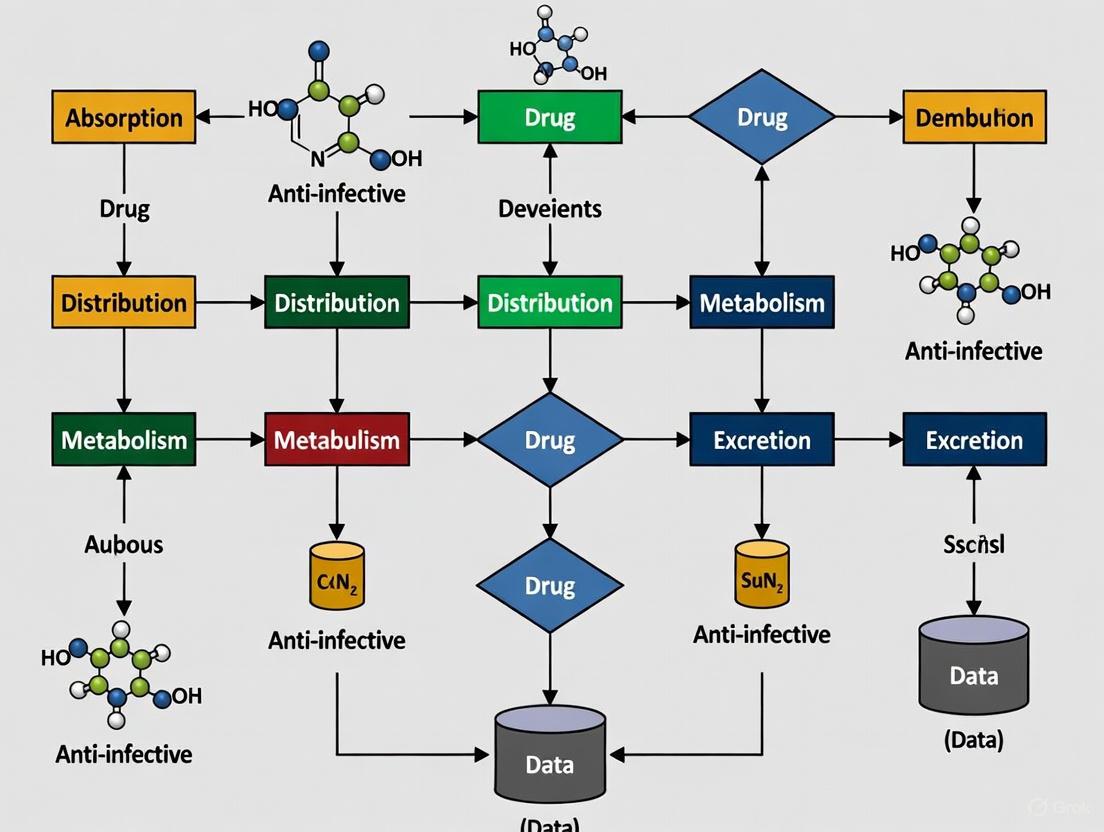
Workflow Overview: The following diagram illustrates the integrated, iterative nature of a pharmacometric analysis.
Stepwise Detailed Protocol
Step 1: Planning and Regulatory Interaction (Stage 1 of MIDD)
- Action: Define the Question of Interest (QOI) and Context of Use (COU). Document the planned analysis in a Model Analysis Plan (MAP) [1].
- Example QOI: "What is the influence of renal impairment on drug exposure, and what dose adjustment is recommended for patients with severe renal impairment?"
- Documentation: The MAP should include sections on Introduction, Objectives, Data Sources, and planned Methods for model development and evaluation.
Step 2: Data Assembly and Exploratory Analysis
- Action: Collate all PK/PD data, dosing records, and patient covariates from clinical trials. Perform data cleaning and exploratory graphical analysis (e.g., concentration-time profiles, empirical Bayesian estimates vs. covariates) [4].
- Software: R or Python for data preparation and visualization.
- Key Outputs: A consolidated dataset suitable for nonlinear mixed-effects modeling and initial hypotheses on covariate relationships.
Step 3: Base Population PK Model Development
- Action: Develop a structural PK model (e.g., 1-, 2-, or 3-compartment) using nonlinear mixed-effects modeling. Estimate between-subject variability (BSV) on key parameters (e.g., Clearance - CL, Volume - V) and characterize residual error.
- Software: NONMEM, Monolix, or equivalent.
- Model Selection: Use diagnostic plots and statistical criteria (e.g., drop in objective function value - OFV) to select the best structural model.
Step 4: Covariate Model Building
- Action: Identify patient-specific factors (e.g., weight, renal function, age) that explain a portion of the BSV. Use a stepwise forward addition/backward elimination procedure.
- Technical Criteria: A drop in OFV of >3.84 (p<0.05, χ², 1 df) for forward inclusion and >6.63 (p<0.01) for backward deletion.
- Output: A final PopPK model that can simulate drug exposure for virtual patients with different demographic and pathophysiological characteristics.
Step 5: PK/PD Model Development
- Action: Link the final PopPK model to a PD endpoint. For anti-infectives, this often involves an indirect-response model or a direct-effect model to characterize the drug's effect on pathogen load.
- Common Models:
- Direct Effect Emax Model:
Effect = E0 - (Emax * C) / (EC50 + C) - Indirect Response Model (Inhibition of Growth):
dR/dt = Kin * (1 - (Imax * C)/(IC50 + C)) - Kout * R - Viral Dynamics Model: A system of differential equations modeling target cells, infected cells, and virus.
- Direct Effect Emax Model:
- Objective: Quantify the exposure-response relationship and identify a target exposure for efficacy.
Step 6: Model Evaluation and Validation
- Action: Assess the model's robustness and predictive performance.
- Visual Predictive Check (VPC): Simulate multiple trials using the final model and compare the simulation intervals with the observed data [4]. Advanced methods like V2ACHER-transformed VPC (V3PC) can improve interpretability for models with multiple covariates [4].
- Bootstrap: Re-estimate model parameters on multiple resampled datasets to evaluate parameter precision.
- Goodness-of-Fit Plots: Examine observed vs. population-predicted and individual-predicted values, and conditional weighted residuals.
Step 7: Clinical Trial Simulation and Decision Making
- Action: Use the qualified PopPK/PD model to simulate virtual clinical trials.
- Process: Simulate drug exposure and response for thousands of virtual subjects under various dosing regimens and patient population scenarios.
- Application: Compare the probability of achieving a target efficacy/safety metric across different doses to support dose justification and label recommendations.
Advanced Integration: Quantitative Systems Pharmacology (QSP) in Anti-Infectives
For more complex questions, such as predicting the emergence of resistance, a QSP approach is warranted. The following diagram outlines the structure of a simplified QSP model for an antiviral drug.
QSP Protocol Outline:
- Model Scope Definition: Define the key biological system components (e.g., host immune cells, different viral subpopulations, intracellular drug kinetics).
- System Assembly: Construct a network of ordinary differential equations (ODEs) based on known pathophysiology and drug mechanisms.
- Parameterization: Gather system parameters from literature and pre-clinical data. Use optimization techniques to estimate unknown parameters.
- Validation: Challenge the model by comparing its simulations to clinical trial outcomes not used for model building.
- Scenario Exploration: Use the validated model to simulate the long-term outcomes of various combination therapies and dosing strategies on resistance suppression.
Pharmacometrics provides the formal, quantitative framework essential for integrating PK, PD, and disease biology into a cohesive model-informed drug development strategy. The application notes and protocols detailed herein offer a practical roadmap for implementing these powerful methodologies in anti-infective research. By adopting these approaches—from foundational PopPK/PD to advanced QSP modeling—researchers can significantly de-risk development, optimize therapy for individual patients, and combat the ever-present threat of antimicrobial resistance more effectively. The ongoing integration of artificial intelligence and machine learning promises to further refine these models, enhancing their predictive power and solidifying their role as a cornerstone of modern therapeutics development [2] [5].
Application Note: Pharmacometric Modeling in Anti-Infective Development
Background and Rationale
The global antimicrobial resistance (AMR) crisis represents one of the most significant public health threats of the 21st century, projected to cause 10 million deaths annually by 2050 if unmitigated [6]. The development of anti-infective therapies faces unique challenges, including the rapid evolution of resistant pathogens and economic disincentives for traditional antibiotic development [7]. Quantitative approaches, particularly pharmacometric modeling and simulation (M&S), have emerged as indispensable tools to optimize anti-infective drug development and combat AMR through data-driven decision support [8].
Pharmacometrics integrates mathematical models based on biology, pharmacology, physiology, and disease to quantify drug-patient interactions [8]. This application note outlines how pharmacometric approaches address key challenges in anti-infective development, including optimizing dosage regimens, predicting resistance development, and supporting regulatory decisions across the drug development continuum [8].
Quantitative Framework Implementation
The pharmacometric workflow integrates data from multiple sources to characterize pharmacokinetic-pharmacodynamic (PK/PD) relationships and predict clinical outcomes. Table 1 summarizes the primary quantitative modeling approaches employed in anti-infective development.
Table 1: Pharmacometric Modeling Approaches in Anti-Infective Development
| Model Type | Primary Application | Key Outputs | Software Platforms |
|---|---|---|---|
| Population PK (popPK) | Characterize drug exposure variability in patient populations | Parameter variability estimates, Covariate effects | NONMEM, Monolix, Phoenix WinNonlin |
| PK/PD Modeling | Establish exposure-response relationships for efficacy and safety | Target attainment analysis, Dose optimization | NONMEM, R, Phoenix WinNonlin |
| Mechanistic Systems Models | Predict resistance development and population dynamics | Resistance probability, Optimal combination therapies | MATLAB, R, Custom implementations |
| Transational PK/PD | Bridge preclinical findings to human predictions | First-in-human dosing, Therapeutic window estimation | Simulx, PK-Sim, GastroPlus |
Key Quantitative Parameters and Targets
Table 2 outlines critical PK/PD indices and their target values for major anti-infective classes, derived from pharmacometric analyses [8].
Table 2: Key PK/PD Targets for Anti-Infective Agents
| Anti-Infective Class | Primary PK/PD Index | Target Value | Pathogen Example | Clinical Application |
|---|---|---|---|---|
| Fluoroquinolones | fAUC/MIC | 100-250 | Streptococcus pneumoniae | Community-acquired pneumonia |
| β-Lactams | fT>MIC | 30-70% (varies by agent) | Staphylococcus aureus | Nosocomial infections |
| Glycopeptides | AUC/MIC | ≥400 | Staphylococcus aureus | Gram-positive infections |
| Aminoglycosides | Cmax/MIC | 8-12 | Gram-negative bacilli | Serious infections |
| Oxazolidinones | fAUC/MIC | 80-120 | MRSA | Skin and soft tissue infections |
Protocol: Development and Validation of Pharmacometric Models for Anti-Infectives
Protocol: Population PK Model Development
Objective
To develop a population pharmacokinetic (popPK) model that characterizes drug disposition and identifies sources of variability in target patient populations.
Materials and Equipment
- Pharmacokinetic concentration-time data
- Patient demographic data (age, weight, renal/hepatic function)
- Concomitant medication records
- NONMEM, Monolix, or equivalent modeling software
- R or Python for data preparation and diagnostics
Experimental Procedure
- Data Assembly: Compile PK samples with accurate recording of sampling times, doses, and administration routes. Include relevant patient covariates.
- Structural Model Development:
- Plot concentration-time data and evaluate appropriate structural models (1-, 2-, 3-compartment)
- Test absorption models (zero/first-order, transit compartments)
- Estimate parameters (clearance, volume, absorption rate)
- Statistical Model Development:
- Characterize between-subject variability using exponential error models
- Model residual variability using proportional, additive, or combined error structures
- Covariate Model Development:
- Evaluate relationships between parameters and physiologic covariates
- Use stepwise forward inclusion (p<0.05) and backward elimination (p<0.01)
- Validate final model using visual predictive checks and bootstrap analysis
Data Analysis
- Generate parameter estimates with precision (relative standard error)
- Calculate shrinkage for empirical Bayesian estimates
- Perform model qualification using diagnostic plots and simulation-based evaluations
Protocol: PK/PD Target Attainment Analysis
Objective
To determine the probability of achieving predefined PK/PD targets across a population using Monte Carlo simulations.
Materials and Equipment
- Final popPK model with parameter distributions
- Pathogen MIC distributions from surveillance data
- Preclinical PK/PD targets (e.g., fT>MIC, fAUC/MIC)
- R, SAS, or other simulation software
Experimental Procedure
- Define PK/PD Target: Identify relevant index and target value based on preclinical infection models (refer to Table 2).
- Set Up Simulation:
- Simulate concentration-time profiles for 10,000 subjects using final popPK model
- Incorporate parameter uncertainty and covariate distributions
- Calculate PK/PD Index:
- For each simulated subject, compute the relevant PK/PD index
- Compare to preclinical target value
- Determine Probability of Target Attainment (PTA):
- Calculate percentage of subjects achieving target at each MIC
- Plot PTA versus MIC to determine susceptibility breakpoints
Data Analysis
- Identify MIC where PTA falls below 90% (susceptibility breakpoint)
- Generate PTA curves for multiple dosing regimens to support dose selection
- Integrate epidemiologic MIC data to estimate cumulative fraction of response
Signaling Pathways and Workflows
Pharmacometric Modeling Workflow
Anti-Infective PK/PD Relationship Pathway
Research Reagent Solutions
Table 3: Essential Research Tools for Anti-Infective Pharmacometrics
| Tool Category | Specific Solution | Function | Application Context |
|---|---|---|---|
| Modeling Software | NONMEM | Nonlinear mixed-effects modeling | Population PK/PD model development |
| Modeling Software | Monolix | Parameter estimation using SAEM algorithm | PK/PD model development and diagnostics |
| Modeling Software | R with packages (nlme, ggplot2) | Data visualization and statistical analysis | Exploratory data analysis and plotting |
| Simulation Tools | Simulx | Clinical trial simulation | Study design optimization |
| Simulation Tools | Phoenix WinNonlin | Non-compartmental analysis | Initial PK parameter estimation |
| Data Standards | CDISC SEND | Nonclinical data standardization | Regulatory submission preparation |
| Data Standards | CDISC SDTM/ADaM | Clinical data standardization | Regulatory submission preparation |
| Bioanalytical | LC-MS/MS systems | Drug concentration quantification | PK sample analysis |
| Microbiological | Broth microdilution | MIC determination | PD input parameter generation |
| Clinical Data | Electronic Data Capture (EDC) | Clinical trial data management | Efficient data collection and cleaning |
Advanced Applications: Integrating AI and Machine Learning
Recent advances have integrated artificial intelligence with traditional pharmacometric approaches to address AMR [9]. The novel BARDI framework (Brokered data-sharing, AI-driven Modelling, Rapid diagnostics, Drug discovery, and Integrated economic prevention) exemplifies this integration, using machine learning to enhance predictive modeling of resistance development and optimize combination therapies [9].
Quantitative modeling of population dynamics using both mechanistic models and machine learning approaches shows particular promise for predicting AMR emergence and spread [10]. These integrated models can account for non-genetic heterogeneity in microbial populations, which contributes to the development of resistance through fluctuations in gene expression even in clonal populations [11].
The application of these quantitative tools represents a paradigm shift in anti-infective development, enabling more efficient dose selection, optimized clinical trial designs, and ultimately, more effective strategies for combating antimicrobial resistance through data-driven approaches.
In the face of increasing antimicrobial resistance, the optimization of anti-infective therapy through Pharmacokinetic/Pharmacodynamic (PK/PD) principles has become paramount. PK/PD integration comprehensively analyzes the relationships between drug exposure, microbial response, and clinical outcome, providing a scientifically robust framework for rational dosage regimen design and treatment optimization [12] [13]. These models are indispensable tools in pharmaceutical development, academia, and regulatory agencies for bridging preclinical findings and clinical application [13]. The core indices that predict antibiotic efficacy—fAUC/MIC, T>MIC, and fCmax/MIC—serve as critical guides for maximizing bacterial kill and suppressing resistance emergence. This article details these fundamental PK/PD indices within the context of pharmacometric modeling and simulation, providing structured data and experimental protocols for their application in anti-infective development.
Core PK/PD Indices: Definitions and Target Values
Antibiotics are traditionally categorized based on their pattern of bacterial killing and the PK/PD index most predictive of their efficacy. The "f" prefix denotes the unbound, pharmacologically active fraction of the drug [12].
Table 1: Core PK/PD Indices and Their Characteristics
| PK/PD Index | Definition | Antibiotic Classes | Primary Goal of Therapy |
|---|---|---|---|
fAUC/MIC |
Ratio of the area under the unbound drug concentration-time curve to the MIC [12]. | Fluoroquinolones, Vancomycin, Tetracyclines, Azithromycin, Tigecycline, Daptomycin, Colistin [14] [15] [16] | Maximize the overall drug exposure over time. |
%T > MIC |
Percentage of the dosing interval that the unbound drug concentration exceeds the MIC [12]. | β-lactams (Penicillins, Cephalosporins, Carbapenems), Erythromycin, Linezolid [14] [15] | Maximize the duration of contact between the drug and the bacterium. |
fCmax/MIC |
Ratio of the maximum unbound drug concentration to the MIC [12]. | Aminoglycosides, Metronidazole, likely Rifampin [15] | Maximize the peak drug concentration. |
Table 2: Representative PK/PD Target Values for Efficacy
| Antibiotic / Class | PK/PD Index | Target for Efficacy | Notes / Clinical Context |
|---|---|---|---|
| Aminoglycosides | Cmax/MIC |
8-10 [14] | Target associated with preventing resistance. |
| Vancomycin | AUC/MIC |
≥400 [14] | Target for MRSA; associated with reduced mortality and treatment failure [14]. |
| Fluoroquinolones (vs S. pneumoniae) | AUC/MIC |
>33.7 [14] | Linked to 100% microbiological response [14]. |
| β-Lactams | %T > MIC |
60-70% of dosing interval [14] | For maximum killing; newer evidence suggests benefit of 100% coverage [15]. |
| Colistin (vs A. baumannii) | fAUC/MIC |
Stasis: 1.57-7.41; 1-log kill: 6.98-42.1 [17] [16] | Target varies by strain and infection site (thigh vs. lung) [17]. |
| Daptomycin | AUC/MIC |
>600 [15] | Requires doses of 6-12 mg/kg/day depending on MIC [15]. |
| Linezolid | AUC/MIC |
100 [15] | May require increased dosing frequency for strains with MICs at the breakpoint [15]. |
Diagram 1: A workflow for selecting the primary PK/PD index and corresponding dosing strategy based on antibiotic classification. (PAE: Post-Antibiotic Effect).
Experimental Protocols for PK/PD Index Determination
Determining which PK/PD index best predicts an antibiotic's efficacy requires well-designed experiments. The following protocols outline the key methodologies.
In Vitro PK/PD Model (Hollow Fiber/Peristaltic Pump System)
This system simulates human PK in a controlled environment to characterize the exposure-response relationship without host immune interference [12].
Key Reagent Solutions:
- Hollow Fiber Bioreactor: A cartridge with semi-permeable membranes simulating a central compartment; allows for dynamic drug concentration changes and bacterial sampling without dilution [12].
- Cation-Adjusted Mueller Hinton Broth (CAMHB): Standardized growth medium ensuring robust and reproducible bacterial growth [17].
- Test Organism: Prepared early logarithmic-phase bacterial suspension (e.g., ~10⁷ CFU/mL) to simulate active infection [17].
Procedure:
- Inoculation: Inject the bacterial suspension into the central compartment of the hollow fiber system.
- Drug Administration: Simulate human PK profiles by administering antibiotic regimens into the system's central compartment. For dose-fractionation studies, administer the same total daily dose using different dosing intervals (e.g., Q24h, Q12h, Q8h) [17].
- Sampling: Collect samples from the central compartment at predetermined time points over 24-48 hours for both:
- Data Analysis: Plot time-kill curves. Use non-linear regression analysis to correlate the observed antibacterial effect (e.g., change in log₁₀ CFU at 24h) with the three PK/PD indices (
fAUC/MIC,%fT>MIC,fCmax/MIC). The index with the highest coefficient of determination (R²) is the most predictive [17].
In Vivo PK/PD Model (Murine Thigh/Lung Infection)
This model studies the complex interplay between host, pathogen, and drug, providing critical data for translating in vitro findings to a living system [17] [12].
Key Reagent Solutions:
- Immunocompromised Host: Female Swiss albino mice rendered neutropenic via intraperitoneal cyclophosphamide (150 mg/kg 4 days prior, 100 mg/kg 1 day prior) to blunt innate immune response [17].
- Infection Inoculum: Prepare early logarithmic-phase bacterial suspension in sterile saline (~10⁷ CFU/mL for thigh; ~10⁸ CFU/mL for lung infection) [17].
- Test Article: Colistin sulphate solution, freshly prepared in water and filter-sterilized (0.2 µm) before each experiment [17].
Procedure:
- Infection Establishment:
- Treatment Initiation: Commence therapy (e.g., subcutaneous injections) 2 hours post-inoculation [17].
- Dose Fractionation Design: Administer a range of total daily doses (e.g., 1-160 mg/kg/day for colistin) fractionated into different intervals (e.g., every 6, 8, 12, or 24 hours) [17].
- Endpoint Analysis: Humanely euthanize mice 24 hours after treatment initiation. Aseptically remove and homogenize target organs (thighs/lungs). Perform quantitative cultures on homogenates to determine the bacterial burden [17].
- PK/PD Integration & Population Analysis:
- Integration: Use previously established plasma PK profiles to calculate the
fAUC/MIC,%fT>MIC, andfCmax/MICfor each regimen. Correlate these values with the measured bacterial burden to identify the predictive index [17]. - Resistance Monitoring: Spiral plate tissue homogenates onto agar plates containing increasing concentrations of colistin (e.g., 0.5 to 10 mg/L) to generate Population Analysis Profiles (PAPs) and monitor the amplification of resistant subpopulations [17].
- Integration: Use previously established plasma PK profiles to calculate the
Diagram 2: A side-by-side comparison of the experimental workflows for determining the predictive PK/PD index using in vitro and in vivo models. (PAPs: Population Analysis Profiles).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Instruments for PK/PD Experiments
| Item | Function / Application | Example Usage |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized medium for broth microdilution MIC determination and in vitro PK/PD model inoculum preparation [17]. | Ensuring reproducible bacterial growth and reliable MIC results [17]. |
| Hollow Fiber Infection Model (HFIM) | In vitro system that simulates human PK profiles for antibiotics against bacteria in a dynamic, closed system [12]. | Performing robust dose-fractionation studies to identify the PK/PD driver without animal use [12]. |
| Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) | Highly sensitive and specific analytical technique for quantifying drug concentrations in complex biological matrices [18]. | Measuring antibiotic concentrations in plasma, tissue homogenates, and in vitro samples for PK analysis [18]. |
| Confocal Raman Spectroscopy | Label-free, non-destructive technique for measuring local drug concentration distributions in tissues and gels [18]. | Mapping drug penetration and gradients in tissue specimens, complementing LC-MS/MS data [18]. |
| Tissue Homogenizer (e.g., Polytron) | Instrument for homogenizing solid tissues into a uniform suspension for subsequent analysis. | Preparing homogeneous samples from infected murine thighs or lungs for CFU counting and drug assay [17]. |
| Spiral Plater (e.g., WASP2) | Automated instrument for depositing liquid samples in an Archimedean spiral on agar plates for bacterial counting. | Performing rapid and accurate quantitative cultures on serial dilutions of tissue homogenates or in vitro samples [17]. |
The strategic application of PK/PD principles is fundamental to modern anti-infective development and therapy. A deep understanding of the core indices—fAUC/MIC, %T>MIC, and fCmax/MIC—enables researchers and clinicians to design dosing regimens that maximize efficacy and minimize the potential for resistance. As the field evolves, integrating these principles with advanced pharmacometric modeling and novel experimental approaches, such as physiologically-based pharmacokinetic (PBPK) models and enhanced in vitro systems, will be crucial for optimizing the use of existing antibiotics and guiding the development of new agents against multidrug-resistant pathogens.
Model-Informed Drug Development (MIDD) is defined as the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence [1]. In the critical field of anti-infective research, pharmacometric modeling and simulation has emerged as an indispensable tool for addressing the global challenge of antimicrobial resistance and optimizing treatment regimens for established antimicrobials [8] [19]. The International Council for Harmonisation (ICH) M15 guidelines, released for public consultation in November 2024, establish a harmonized framework for MIDD applications, aiming to align expectations between regulators and sponsors while supporting consistent regulatory decisions [1].
The model-based continuum spans from early preclinical discovery through clinical development and into lifecycle management, with pharmacometrics serving as the backbone that connects knowledge across stages. This approach is particularly valuable for anti-infective development, where it facilitates the integration of preclinical and clinical data to provide a scientifically rigorous framework for rational dosage regimen design and treatment optimization [8]. By leveraging quantitative approaches such as population pharmacokinetic-pharmacodynamic (PopPK-PD) modeling and quantitative systems pharmacology (QSP), researchers can characterize the complex relationships between drug exposure, microbial killing, and resistance emergence, ultimately accelerating the delivery of novel anti-infective therapies to patients [8] [20].
Theoretical Framework and Key Methodologies
The Pharmacometric Modeling Spectrum
The MIDD framework encompasses a diverse spectrum of modeling approaches, each with distinct applications across the drug development continuum. Population PK-PD (PopPK-PD) modeling, typically leveraging nonlinear mixed-effects modeling of compartmental PK and PD models, has emerged as a preeminent methodology for dose-exposure-response (E-R) predictions in MIDD [1]. These models are particularly effective for characterizing variability in drug concentrations and effects between subjects, as well as for performing clinical trial simulations [1].
Physiologically based PK (PBPK) modeling represents another crucial methodology, with approximately 70% of its applications in drug development and regulatory settings focused on predicting drug-drug interactions with enzymes and transporters [1]. For anti-infectives, this is particularly relevant for complex combination therapies used for drug-resistant infections. More recently, Quantitative Systems Pharmacology (QSP) has gained prominence as a mechanistic modeling approach that incorporates the (patho)physiology of interest, mechanistic links between target modulation and key endpoints, overall system dynamics, population variability, and pharmacological interventions [20].
The International Society of Pharmacometrics (ISoP) special interest groups (SIGs) have articulated how these diverse modeling approaches integrate into MIDD decision-making [20]. The selection of the appropriate model class begins with understanding the specific research question and available data, ranging from simple statistical models to complex mechanistic models depending on the development stage and decision context [20].
Key Pharmacodynamic Parameters for Anti-Infectives
For anti-infective drugs, specific pharmacokinetic-pharmacodynamic (PK-PD) indices have been established as critical predictors of efficacy. These parameters form the foundation of exposure-response modeling in antimicrobial development and are summarized in the table below.
Table 1: Key PK-PD Parameters for Anti-Infective Efficacy
| PK-PD Index | Drug Class | Target Value | Biological Significance |
|---|---|---|---|
| fAUC/MIC | Fluoroquinolones | 30-100 | Predicts concentration-dependent killing |
| %T>MIC | β-Lactams | 30-70% | Time-dependent bacterial killing |
| fCmax/MIC | Aminoglycosides | 8-10 | Concentration-dependent killing and post-antibiotic effect |
The application of these PK-PD targets is well illustrated by garenoxacin, where a pharmacometric analysis determined that a fAUC₀⁻²⁴/MIC₉₀ ratio >200 supported a 400 mg QD oral dosing regimen as safe and effective for community-acquired pneumonia [8]. Similarly, moxifloxacin demonstrated target attainment rates exceeding 95% for respiratory tract infections when the fAUC₀⁻²⁴/MIC₉₀ ratio reached 120 in epithelial lining fluid [8].
Application Notes: Implementing MIDD Across the Development Continuum
Preclinical to Clinical Translation
The transition from preclinical models to first-in-human studies represents a critical juncture in anti-infective development. Model-based approaches significantly enhance this translation by integrating in vitro and animal model data to inform human dosing predictions. For instance, PK-PD models that incorporate data from murine thigh and lung infection models can establish exposure targets for human efficacy, effectively bridging the gap between preclinical results and clinical trial design [8].
The integration of QSP and clinical pharmacometrics occurs through three primary paradigms: (1) parallel synchronization, where independent efforts serve as cross-validation; (2) cross-informative use, where one approach informs the other; and (3) sequential integration, where one approach precedes the other, creating a framework that can inform decisions along the entire research and development continuum [20]. This integration is particularly valuable for novel therapies with limited clinical data, such as those targeting multidrug-resistant pathogens.
A notable example of successful translation involves the dose selection of pembrolizumab, where cross-validation efforts between modeling approaches strengthened confidence in the recommended dosing strategy [20]. Similarly, a large QSP model of the cardio-renal system helped explain the unexpected cardioprotective effect of SGLT2 inhibitors in patients with heart failure, demonstrating how mechanistic modeling can provide insights into drug effects beyond the primary indication [20].
Clinical Development Optimization
During clinical development, PopPK-PD modeling becomes indispensable for characterizing variability in drug exposure and response across diverse patient populations. These analyses are particularly important for anti-infectives, which are often used in patients with organ dysfunction, critical illness, or other comorbidities that alter drug pharmacokinetics. For example, population PK analyses of norvancomycin identified that clearance was correlated with creatinine clearance (CL=2.54(CLCr/50)) in patients with renal dysfunction, enabling optimized dosing in this special population [8].
The use of modeling and simulation in clinical development enables the quantitative integration of knowledge across the development program and compounds, addressing a broader range of dose-exposure responses, product design, special populations, and disease-related questions than traditional statistical approaches alone [1]. This approach has proven particularly valuable in special populations such as pediatric patients, where MIDD has enabled accelerated approvals of drugs for pediatric conditions and rare diseases where recruiting sufficient patients for efficacy studies is challenging [1].
Table 2: Clinical Pharmacometrics Case Studies in Anti-Infective Development
| Drug | Population | Key Analysis | Outcome/Recommendation |
|---|---|---|---|
| Cefditoren | Lower respiratory tract infections | PD profiling & probability of target attainment (PTA) | PTA <80% at T>MIC of 33% (MIC=0.06mg/L) with 400 mg QD [8] |
| Ceftobiprole | Nosocomial pneumonia | PD profiling & renal dose adjustments | 500 mg BID optimal for CrCl ≤50 mL/min [8] |
| Oseltamivir | Neonates and infants | Population PK modeling | 3 mg/kg BID in infants; 1.7 mg/kg BID in neonates [8] |
| Piperacillin/Tazobactam | Gram-negative infections | PK/PD parameters & in vivo effectiveness | Doses of 3.375g Q4h-Q6h and 4.5g Q6h-Q8h provided adequate target attainment [8] |
The ICH M15 guidelines formalize the MIDD process through defined stages: Planning and Regulatory Interaction, Implementation, Evaluation, and Submission [1]. This structured approach begins with planning that defines the Question of Interest (QOI), Context of Use (COU), Model Influence, Decision Consequences, Model Risk, Model Impact, Appropriateness, and Technical Criteria – all documented in a Model Analysis Plan (MAP) [1].
Experimental Protocols
Protocol: Integrated PopPK-PD Model Development for Anti-Infectives
Objective: To develop a population PK-PD model that characterizes the relationship between drug exposure, microbial killing, and resistance emergence for a novel anti-infective compound.
Materials and Reagents:
- Nonlinear Mixed-Effects Modeling Software: NONMEM, Monolix, or equivalent for parameter estimation [1]
- Data Assembly Tools: R, Python, or SAS for dataset creation and exploratory analysis [8]
- Pharmacometric Dataset: Including drug concentrations, pathogen MIC values, patient demographics, and clinical outcomes [8]
- Model Diagnostic Tools: Visual predictive checks, goodness-of-fit plots, bootstrap analyses [1]
Methodology:
- Data Compilation: Assemble rich or sparse PK sampling data from phase 1 and phase 2 trials, including patient covariates (weight, renal/hepatic function, age) and pathogen-specific MIC values [8].
- Structural Model Development:
- Test compartmental PK models (1-, 2-, 3-compartment) with first-order or Michaelis-Menten elimination
- Develop PD model linking plasma concentrations to microbial killing using Emax models or similar functions
- Incorporate natural disease progression and placebo effects where applicable
- Stochastic Model Building:
- Characterize between-subject variability on key parameters using exponential error models
- Define residual error models (additive, proportional, or combined)
- Implement correlation between random effects if supported by data
- Covariate Model Development:
- Evaluate relationship between patient factors (e.g., renal function) and PK parameters using stepwise covariate modeling
- Validate final covariate relationships using visual predictive checks and bootstrap procedures
- Model Validation:
- Conduct internal validation through data splitting, bootstrap, or cross-validation techniques
- Perform external validation with independent datasets when available
- Evaluate predictive performance through visual predictive checks and numerical predictive checks
Output Applications:
- Simulation of various dosing regimens to determine probability of target attainment
- Identification of patient subgroups requiring dose adjustments
- Optimization of sampling schedules for future trials
Protocol: QSP Model for Resistance Development in Antibacterial Drugs
Objective: To develop a mechanistic QSP model that predicts the emergence of bacterial resistance under different drug exposure scenarios.
Materials and Reagents:
- Systems Modeling Software: MATLAB/Simulink, Julia, or specialized QSP platforms [20]
- Biological Data: In vitro time-kill curves, resistance frequency measurements, genomic data on resistance mechanisms
- Physiological Parameters: Bacterial growth rates, mutation rates, fitness costs of resistance
Methodology:
- Model Scope Definition:
- Define the biological system: bacterial population dynamics, drug-target interactions, resistance mechanisms
- Establish model boundaries and level of mechanistic detail based on the QOI
- Virtual Patient Population:
- Create virtual patients (VPs) representing credible observations in the parameter space
- Ensure VPs are consistent with observed pathophysiology and response to therapies [20]
- Mathematical Model Implementation:
- Implement bacterial subpopulations (susceptible, resistant) with different growth and killing rates
- Incorporate drug pharmacokinetics and PD effects on bacterial killing
- Include mutation rates between subpopulations and fitness costs of resistance
- Model Calibration and Validation:
- Calibrate model parameters against in vitro time-kill data and resistance emergence studies
- Validate model predictions using in vivo data from preclinical infection models
- Conduct sensitivity analyses to identify key parameters driving resistance emergence
- Simulation and Scenario Testing:
- Simulate various dosing regimens and their impact on resistance development
- Identify exposure thresholds associated with rapid resistance emergence
- Optimize dosing strategies to suppress resistance while maintaining efficacy
Output Applications:
- Guidance on optimal dosing strategies to minimize resistance emergence
- Identification of pharmacological properties desirable for resistance suppression
- Support for regulatory submissions regarding resistance risk management
Visualization of Workflows and Signaling Pathways
MIDD Workflow in Anti-Infective Development
MIDD Development Cycle
This diagram illustrates the iterative knowledge integration throughout the model-based drug development continuum, from preclinical data generation through regulatory submission.
Anti-Infective PK-PD Modeling Framework
PK-PD Modeling Framework
This workflow depicts the fundamental relationships in anti-infective pharmacometrics, connecting drug administration to pharmacological effects through measurable exposure parameters and their resulting biological responses.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of model-based approaches in anti-infective development requires specialized tools and methodologies. The following table summarizes key resources essential for pharmacometric analyses in this field.
Table 3: Essential Research Reagent Solutions for Anti-Infective Pharmacometrics
| Tool Category | Specific Solutions | Function/Application | Key Features |
|---|---|---|---|
| Modeling & Simulation Software | NONMEM, Monolix, Phoenix NLME | Population PK-PD model development and parameter estimation | Nonlinear mixed-effects modeling, covariate analysis, simulation capabilities [1] |
| Systems Modeling Platforms | MATLAB/Simulink, Julia, R | QSP model implementation and simulation | Differential equation solving, parameter estimation, model calibration [20] |
| Data Management & Analysis | R, Python, SAS | Dataset creation, exploratory analysis, model diagnostics | Data visualization, statistical analysis, automated reporting [8] |
| PBPK Modeling Platforms | GastroPlus, Simcyp, PK-Sim | Prediction of drug absorption, distribution, and drug-drug interactions | Physiology-based parameters, special population modules [1] |
| Clinical Trial Simulation | Trial Simulator, East | Design and simulation of clinical trials | Power analysis, sample size estimation, adaptive design evaluation |
The integration of these tools creates a comprehensive ecosystem for model-based anti-infective development. As noted in the ICH M15 guidelines, the MIDD framework encompasses a broad range of quantitative methods, including PopPK, PBPK, dose-exposure-response analysis, model-based meta-analysis, QSP, and increasingly, AI/ML methods [1]. The selection of specific tools should be guided by the Question of Interest (QOI) and Context of Use (COU) defined in the Model Analysis Plan (MAP) as recommended by the ICH M15 guidelines [1].
The model-based drug development continuum represents a transformative approach to anti-infective research, integrating knowledge from preclinical discoveries through clinical applications. By implementing pharmacometric modeling and simulation strategies, researchers can optimize dosage selection, identify patient factors influencing drug exposure and response, and develop strategies to combat antimicrobial resistance. The standardized methodologies and protocols outlined in these application notes provide a framework for implementing MIDD in anti-infective development programs, with the potential to accelerate the delivery of novel therapies to patients facing resistant infections.
The adoption of model-based approaches continues to gain regulatory endorsement, as evidenced by the ICH M15 guidelines and the successful case studies across various therapeutic areas [1]. As the field advances, the integration of emerging technologies such as AI/ML with traditional pharmacometric methods promises to further enhance the efficiency and predictive performance of model-based strategies in anti-infective drug development [1] [20].
From Model to Medicine: Methodologies and Real-World Applications in Anti-Infectives
Model-informed drug development (MIDD) has a long and rich history in infectious diseases, playing a pivotal role in the development of anti-infective therapies by quantitatively integrating pharmacokinetic (PK) and pharmacodynamic (PD) data. Pharmacometric modeling transforms complex biological systems into mathematical frameworks that describe the complete time course of the dose-response relationship, enabling more efficient drug development and optimized dosing regimens for clinical practice [21] [22]. In anti-infective research, these models are particularly valuable as they allow researchers to characterize and translate antibiotic effects, ultimately supporting the development of new therapeutic agents and treatment strategies against resistant pathogens [23].
The foundational principle of pharmacokinetic/pharmacodynamic (PK/PD) modeling lies in establishing mathematical relationships between administered doses, resulting drug concentrations in the body (pharmacokinetics), and the subsequent pharmacological effects (pharmacodynamics). This integrated approach provides a quantitative framework for predicting drug behavior and effects across different patient populations and dosing scenarios, making it an indispensable tool in the clinical pharmacologist's arsenal [21] [24]. For anti-infective agents, PK/PD modeling has become particularly crucial for designing effective dosing strategies that maximize efficacy while minimizing the development of antimicrobial resistance [25].
Compartmental Pharmacokinetic (PK) Modeling
Fundamental Principles and Model Types
Compartmental pharmacokinetic modeling is a mathematical approach that describes the absorption, distribution, metabolism, and excretion (ADME) of drugs within the body by grouping tissues and fluids with similar pharmacokinetic properties into hypothetical compartments [26] [27]. These compartments do not necessarily represent specific anatomical tissues but rather functional spaces with distinct kinetic characteristics. The primary objective of compartmental modeling is to simplify the body's complexity into manageable, quantifiable systems that can predict drug behavior based on various structural configurations [27].
Table 1: Types of Compartmental Pharmacokinetic Models
| Model Type | Structural Components | Key Characteristics | Typical Applications |
|---|---|---|---|
| One-Compartment | Single central compartment | Assumes instantaneous, uniform drug distribution; first-order elimination | Preliminary PK analysis; drugs with rapid distribution [26] [27] |
| Two-Compartment | Central + Peripheral compartments | Accounts for distribution phase; more accurately reflects tissue distribution | Drugs showing biphasic elimination; many antibiotics and antivirals [26] [27] |
| Three-Compartment | Central + Two Peripheral compartments | Further subdivision of distribution phases; complex kinetics | Drugs with deep tissue distribution; specialized anti-infectives [26] [27] |
| Physiologically-Based PK (PBPK) | Multiple organ- and tissue-specific compartments | Grounded in biological and physiological data; highly mechanistic | First-in-human dose prediction; drug-drug interaction studies [26] [25] |
Mathematical Foundation
The one-compartment model with intravenous administration represents the simplest form, where the entire body is treated as a single homogeneous unit. The differential equation describing this model is:
dA/dt = -k × A
where A is the amount of drug in the body, and k is the first-order elimination rate constant. The integrated form yields:
C = (Dose/V) × e^(-k×t)
where C is the drug concentration at time t, and V is the apparent volume of distribution [26].
For a two-compartment model with intravenous administration, the system is described by two differential equations:
dA₁/dt = k₂₁ × A₂ - k₁₂ × A₁ - k₁₀ × A₁ dA₂/dt = k₁₂ × A₁ - k₂₁ × A₂
where A₁ and A₂ represent the amount of drug in the central and peripheral compartments, respectively; k₁₂ and k₂₁ are distribution rate constants between compartments; and k₁₀ is the elimination rate constant from the central compartment [26].
Application Protocol: Establishing a Compartmental PK Model
Objective: To develop and validate a compartmental PK model for a novel anti-infective compound.
Materials and Reagents:
- Test compound (API)
- Animal model (e.g., mice, rats) or human subjects
- Appropriate formulation vehicles
- Blood collection tubes (containing anticoagulant)
- Analytical standards for calibration
- LC-MS/MS system for bioanalysis
- PK modeling software (e.g., NONMEM, Monolix, Phoenix WinNonlin)
Procedure:
- Study Design: Administer the test compound via relevant route (IV for complete bioavailability assessment, plus other intended routes). Implement dense sampling strategy (10-15 timepoints) during the elimination phase to characterize distribution and elimination.
- Bioanalytical Method: Validate a sensitive and specific analytical method (typically LC-MS/MS) for quantifying compound concentrations in plasma. Ensure the calibration curve covers the expected concentration range with acceptable accuracy and precision.
- Sample Collection and Analysis: Collect blood samples at predetermined timepoints, process to plasma, and analyze using the validated method.
- Data Preparation: Prepare dataset containing compound concentrations, sampling times, dose information, and relevant subject covariates.
- Model Development:
- Begin with structural model identification using one-, two-, or three-compartment models.
- Incorporate appropriate absorption models for extravascular administration (e.g., first-order, zero-order, or more complex absorption models).
- Implement statistical model to account for interindividual variability and residual error.
- Model Evaluation: Assess model performance using diagnostic plots, visual predictive checks, and precision of parameter estimates.
- Model Application: Utilize the final model for simulations to predict exposure under different dosing regimens and in specific populations.
Diagram 1: Structure of a Two-Compartment Pharmacokinetic Model
Pharmacodynamic (PD) Modeling: Emax and Sigmoid Emax Models
Theoretical Basis and Mathematical Formulation
Pharmacodynamic modeling quantitatively describes the relationship between drug concentration at the effect site and the pharmacological response. For anti-infective drugs, this typically represents the relationship between antimicrobial concentrations and the reduction in bacterial populations [22]. The most fundamental PD models include the fixed-effect, linear, log-linear, maximum effect (Emax), and sigmoid Emax models, with the latter two being most prevalent in anti-infective PK/PD modeling [22].
The sigmoid Emax model is particularly valuable as it can describe a wide range of concentration-effect relationships, from shallow to steep curves, making it applicable to various anti-infective mechanisms. The mathematical equation for the sigmoid Emax model is:
E = E₀ + (Emax × Cⁿ) / (EC₅₀ⁿ + Cⁿ)
where E is the measured effect, E₀ is the baseline effect in the absence of drug, Emax is the maximum possible effect, C is the drug concentration at the effect site, EC₅₀ is the drug concentration that produces 50% of the maximum effect, and n is the Hill coefficient that determines the steepness of the concentration-effect curve [22].
Table 2: Parameters of the Sigmoid Emax Model
| Parameter | Definition | Biological Interpretation | Typical Units |
|---|---|---|---|
| E₀ | Baseline effect | Effect in absence of drug | Variable (e.g., CFU/mL) |
| Emax | Maximum effect | Maximum achievable drug effect | Same as E₀ |
| EC₅₀ | Half-maximal effective concentration | Drug potency; lower value indicates higher potency | Concentration (e.g., mg/L) |
| n | Hill coefficient | Steepness of concentration-effect relationship; reflects cooperative binding | Unitless |
Application Protocol: Implementing PD Models for Anti-Infective Agents
Objective: To characterize the concentration-effect relationship of an antimicrobial agent using the sigmoid Emax model.
Materials and Reagents:
- Test antimicrobial agent
- Reference bacterial strains with known MIC values
- Mueller-Hinton broth or other appropriate culture media
- Sterile 96-well plates or test tubes
- Incubator
- Spectrophotometer for turbidity measurements
- Colony counting equipment (agar plates, colony counter)
Procedure:
- Preparation of Drug Dilutions: Prepare a range of drug concentrations (typically 0.25× to 64× MIC) using serial dilution methods in appropriate culture media.
- Inoculum Preparation: Adjust bacterial suspensions to approximately 10⁵-10⁶ CFU/mL in fresh culture media.
- Exposure and Incubation: Combine equal volumes of drug dilutions and bacterial suspensions in sterile plates or tubes. Include growth controls (no drug) and sterility controls (no bacteria).
- Effect Measurement: Incubate under appropriate conditions for a predetermined time (typically 18-24 hours for bacteria). Measure the antibacterial effect using viable count methods (determining CFU/mL) or optical density for growth inhibition.
- Data Analysis:
- Calculate the percentage of growth inhibition or log reduction in CFU/mL compared to growth controls.
- Plot effect measures against drug concentrations.
- Fit the sigmoid Emax model to the data using nonlinear regression.
- Estimate model parameters (E₀, Emax, EC₅₀, n) with associated measures of precision.
- Model Validation: Assess model goodness-of-fit through residual analysis, visual inspection, and comparison with simpler models (e.g., linear, Emax without sigmoidicity).
Diagram 2: Pharmacodynamic Modeling Approaches
Time-Kill Curve Modeling
Conceptual Framework and Advantages
Time-kill curve analysis represents a dynamic approach to characterizing antimicrobial effects by measuring changes in bacterial density over time when exposed to varying antibiotic concentrations [28]. Unlike static MIC-based approaches, time-kill curves capture the kinetics of microbial killing and growth as a function of both time and antibiotic concentration, providing a more comprehensive assessment of the pharmacokinetic-pharmacodynamic relationship [28] [29].
The primary advantage of time-kill curve approaches lies in their ability to characterize the rate and extent of bactericidal activity, detect regrowth due to resistance emergence, and identify concentration-dependent versus time-dependent killing patterns [28]. This method allows researchers to directly compare the effects of various concentration profiles and provides a more detailed assessment of the PK/PD relationship than simple MIC-based determinations [28].
Mathematical Implementation
Mechanism-based PK/PD models for antimicrobial effects can generally be derived from a common framework premised on bacterial growth and kill rate processes. The fundamental differential equation describing bacterial growth and drug-induced killing is:
dN/dt = k₉ʳᵒʷᵗʰ × N - kₖᵢₗₗ(C) × N
where N is the bacterial density, k₉ʳᵒʷᵗʰ is the first-order growth rate constant, and kₖᵢₗₗ(C) is the drug concentration-dependent kill rate, which can be described by various models including the sigmoid Emax model [30].
More sophisticated models may incorporate additional components such as:
- Adaptation phases accounting for initial growth delay
- Subpopulations with different susceptibility profiles
- Post-antibiotic effects
- Immune system contributions to bacterial clearance
Application Protocol: Time-Kill Curve Experiments
Objective: To characterize the time-dependent killing activity of an antimicrobial agent against a target pathogen.
Materials and Reagents:
- Test antimicrobial agent (stock solutions at appropriate concentrations)
- Bacterial strains (reference and clinical isolates)
- Culture media (Mueller-Hinton broth or other appropriate media)
- Sterile flasks or tubes for time-kill experiments
- Water bath or shaking incubator for temperature control
- Phosphate buffered saline (PBS) for serial dilutions
- Agar plates for viable counting
- Colony counter or automated enumeration system
Procedure:
- Preparation: Prepare antibiotic solutions at multiple concentrations (e.g., 0.5×, 1×, 2×, 4×, 8× MIC) in appropriate culture media.
- Inoculation: Add standardized bacterial inoculum (approximately 10⁵-10⁶ CFU/mL) to each antibiotic-containing flask and to growth control flasks (no antibiotic).
- Incubation: Incubate under appropriate conditions with shaking if necessary.
- Sampling: Remove samples at predetermined timepoints (e.g., 0, 2, 4, 6, 8, 24 hours) for viable counting.
- Viable Counting: Perform serial dilutions of samples in PBS, plate onto appropriate agar media, incubate, and enumerate colonies.
- Data Collection: Record CFU/mL values for each timepoint and antibiotic concentration.
- Modeling: Fit appropriate mathematical models to the time-kill data using nonlinear regression. Start with a simple growth/kill model and incorporate additional components as needed to describe the data adequately.
Table 3: Time-Kill Curve Characterization of Antimicrobial Activity
| Antibiotic Class | Killing Pattern | Regrowth Potential | PAE Duration | Typical Model Components |
|---|---|---|---|---|
| β-lactams | Time-dependent | Common with sub-MIC concentrations | Short (0-2 hours) | Growth rate, maximum kill rate, resistance emergence |
| Aminoglycosides | Concentration-dependent | Less common with adequate Cmax/MIC | Moderate (1-3 hours) | Growth rate, high maximum kill rate, adaptive resistance |
| Fluoroquinolones | Concentration-dependent | Can occur with resistant subpopulations | Prolonged (1-5 hours) | Multi-population model, resistant subpopulation |
| Glycopeptides | Time-dependent | Slow, often observed at 24-48 hours | Short to moderate | Slow bacterial killing, heterogeneous populations |
Integrated PK/PD Modeling Approaches
Integration Methodologies and Applications
Integrated PK/PD modeling combines the mathematical frameworks describing drug exposure (PK) and drug effect (PD) into a unified model that can predict the complete time course of pharmacological response to dosing [21] [22]. For anti-infective agents, these integrated models are particularly valuable for identifying optimal dosing regimens that maximize efficacy while minimizing resistance development [25].
The integration can be accomplished through different approaches:
- Direct Link Models: Where the effect is directly related to the plasma or effect site concentration
- Indirect Response Models: Where the drug acts indirectly by inhibiting the production or stimulating the loss of response mediators
- Transduction Models: Which incorporate delays between plasma concentrations and effects through series of transit compartments
For anti-infective agents, the most common approach involves linking a compartmental PK model with a kill curve PD model, often incorporating an effect compartment to account for hysteresis when necessary [21].
Application Protocol: Developing Integrated PK/PD Models
Objective: To develop an integrated PK/PD model for a novel anti-infective agent using both plasma concentration data and microbial kill curve data.
Materials and Reagents:
- All materials listed in Protocols 2.3 and 4.3
- PK/PD modeling software (e.g., NONMEM, Monolix, Berkeley Madonna)
- Dataset containing both concentration-time and effect-time data
Procedure:
- Data Assembly: Compile a comprehensive dataset containing dose administration times, plasma concentration measurements, and corresponding effect measurements (e.g., bacterial density over time).
- Structural Model Identification:
- Develop the structural PK model based on concentration-time data
- Develop the structural PD model based on effect-concentration relationships
- Select appropriate link model (direct, indirect, effect compartment)
- Stochastic Model Development: Incorporate interindividual variability and residual error models to account for variability in PK and PD parameters.
- Model Fitting: Simultaneously fit all model parameters to the combined PK/PD dataset using appropriate estimation algorithms.
- Model Evaluation: Assess model performance using diagnostic plots, visual predictive checks, and bootstrap analysis.
- Model Simulation: Utilize the validated model to simulate bacterial killing under different dosing regimens and for different bacterial subpopulations.
Diagram 3: Integrated PK/PD Modeling Framework
Research Reagent Solutions
Table 4: Essential Research Reagents for Pharmacometric Modeling Studies
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Culture Media | Mueller-Hinton Broth, Cation-adjusted MH Broth | Support bacterial growth in PD studies | Standardized composition critical for reproducible MIC and time-kill results [29] |
| Analytical Standards | Certified reference standards, Stable isotope-labeled internal standards | Bioanalytical method calibration and quantification | Essential for accurate PK concentration measurements; should be of highest purity |
| Protein Binding Assays | Equilibrium dialysis devices, Ultrafiltration devices | Determination of free drug fraction | Critical for PK/PD correlations as only free drug is pharmacologically active [28] |
| Enzymatic Assays | β-lactamase detection kits, Metabolic activity assays | Assessment of resistance mechanisms and bacterial viability | Complementary to CFU counting for understanding antibacterial mechanisms |
| Animal Disease Models | Murine thigh infection, Lung infection models | In vivo PK/PD correlation | Provide host-pathogen-drug interactions for translational modeling [29] |
| Hollow Fiber Systems | Hollow fiber infection models | Simulation of human PK profiles in vitro | Enable complex multi-dose regimen simulations without animal use [25] |
| Automated Colony Counters | Protocol 3, Scan 1200 | Accurate enumeration of bacterial colonies | Reduce variability in PD endpoint measurements |
The integration of compartmental PK modeling with mechanism-based PD approaches, particularly time-kill curve analysis and sigmoid Emax models, provides a powerful framework for optimizing anti-infective therapy and combating antimicrobial resistance. These modeling approaches enable researchers to characterize complex exposure-response relationships, identify optimal dosing strategies, and predict clinical efficacy based on preclinical data. As antibiotic resistance continues to threaten global health, sophisticated pharmacometric approaches will play an increasingly vital role in accelerating the development of novel anti-infective agents and preserving the efficacy of existing therapeutics through model-informed precision dosing.
Pharmacometric modeling and simulation have become cornerstones of modern anti-infective drug development, providing a quantitative framework to link drug exposure to pharmacological effect. Pharmacokinetic/pharmacodynamic (PK/PD) modeling integrates mathematical models to describe the complete time course of the dose-response relationship, moving beyond traditional isolated approaches where pharmacokinetics described only plasma concentrations and pharmacodynamics described only the intensity of the response [22]. This integration has proven particularly valuable for optimizing dose regimens for antibacterial and antifungal agents, especially given the expanding crisis of antimicrobial resistance [22] [31]. In the context of a broader thesis on pharmacometric modeling, PK/PD approaches enable more efficient drug development by supporting candidate selection, dose regimen definition, and clinical outcome simulation across all phases of drug development [22].
The fundamental rationale behind PK/PD modeling is to unite the time course of drug concentrations with the resultant effect on pathogens, thereby establishing a robust dose-concentration-response relationship [22]. For anti-infectives, this relationship is uniquely complex as it involves three distinct entities: the host (who receives the drug), the pathogen (which the drug targets), and the drug itself. PK/PD models typically consist of a pharmacokinetic component (often using compartmental models) linked to a pharmacodynamic component that relates drug concentration to antimicrobial effect using mathematical functions such as the sigmoid Emax model [22].
Foundational PK/PD Concepts and Indices
Core PK/PD Parameters and Their Significance
PK/PD modeling for anti-infectives relies on several key parameters that integrate drug exposure with measures of pathogen susceptibility. The minimum inhibitory concentration (MIC) represents the lowest concentration of an antimicrobial that prevents visible growth of a microorganism under standardized conditions and serves as a fundamental measure of drug potency [22] [32]. However, the MIC alone provides limited information as it is a static measure that doesn't account for dynamic concentration-time relationships.
Three primary PK/PD indices have been established to correlate pharmacokinetic parameters with MIC values, each particularly relevant for different classes of antimicrobial agents [33] [34]:
- Area Under the Curve to MIC ratio (AUC/MIC): Integrates both concentration and time aspects of drug exposure, most commonly applied to concentration-dependent antimicrobials like fluoroquinolones and azoles.
- Time Above MIC (%T>MIC): Represents the percentage of a dosing interval that drug concentrations remain above the MIC, particularly critical for time-dependent antimicrobials like β-lactams.
- Peak Concentration to MIC ratio (Cmax/MIC): Relates the maximum drug concentration to the MIC, important for concentration-dependent drugs like aminoglycosides and polyenes.
These indices serve as critical predictors of therapeutic efficacy and form the basis for optimizing dosing strategies across different patient populations and pathogen profiles [34].
Table 1: Key PK/PD Indices and Their Clinical Applications
| PK/PD Index | Definition | Primary Drug Classes | Target Values |
|---|---|---|---|
| AUC/MIC | Area under the concentration-time curve over 24h divided by MIC | Fluoroquinolones, Azoles, Glycopeptides | Variable by drug: e.g., >100-400 for fluoroquinolones |
| %T>MIC | Percentage of dosing interval that concentration exceeds MIC | β-lactams, Carbapenems | 30-70% depending on pathogen and drug |
| Cmax/MIC | Peak concentration divided by MIC | Aminoglycosides, Polyenes | ≥8-10 for optimal efficacy |
Advanced PD Concepts: Resistance Prevention and Combination Therapy
Beyond standard efficacy parameters, advanced PD concepts address the critical issue of antimicrobial resistance. The mutant prevention concentration (MPC) defines the drug concentration that prevents the growth of resistant mutants, while the mutant selection window (MSW) represents the concentration range between MIC and MPC where resistant subpopulations are selectively enriched [34]. Targeting drug concentrations above the MPC through optimized dosing represents a key strategy for suppressing resistance emergence.
For complex infections and multidrug-resistant pathogens, combination therapy leverages PK/PD principles to achieve synergistic effects. The primary methodologies for evaluating combinations include time-kill studies for dynamic assessment and in vitro PK/PD models like the hollow fiber infection model (HFIM) that simulate human pharmacokinetics [23] [32]. These approaches allow researchers to identify combinations that enhance bacterial killing, prevent resistance, and improve clinical outcomes.
Experimental Approaches in PK/PD Research
In Vitro Methodologies
In vitro PK/PD models serve as the initial platform for characterizing antimicrobial pharmacodynamics, ranging from simple static systems to complex dynamic models that simulate human pharmacokinetic profiles [33] [32].
Protocol 3.1.1: Static Time-Kill Curve Assay
- Purpose: To characterize the time- and concentration-dependent antibacterial activity of an antimicrobial agent against a specific pathogen.
- Materials: Cation-adjusted Mueller-Hinton broth (for bacteria) or RPMI-1640 (for fungi), standardized microbial inoculum (approximately 5×10^5 CFU/mL), antimicrobial stock solutions, sterile tubes or microtiter plates, water bath or incubator.
- Procedure:
- Prepare serial dilutions of the antimicrobial in growth medium to achieve target concentrations (typically 0.25× to 4× MIC).
- Inoculate tubes with standardized microbial suspension.
- Incubate at appropriate temperature (35±2°C for bacteria; 35°C for yeasts).
- Sample at predetermined timepoints (0, 2, 4, 6, 8, 12, 24 hours).
- Perform viable counts by serial dilution and plating on appropriate agar.
- Count colonies after 18-24 hours incubation and calculate CFU/mL.
- Data Analysis: Plot log10 CFU/mL versus time for each concentration. Determine bactericidal activity (≥3-log reduction from initial inoculum) and bacteriostatic activity (<3-log reduction).
Protocol 3.1.2: Hollow Fiber Infection Model (HFIM)
- Purpose: To simulate human pharmacokinetics of antimicrobial agents in vitro and study bacterial killing and resistance emergence over extended periods.
- Materials: Hollow fiber bioreactor system, growth medium, antimicrobial stock solutions, peristaltic pumps, reservoir bottles, standardized microbial inoculum.
- Procedure:
- Load the central reservoir with growth medium containing the antimicrobial at a concentration calculated to simulate human PK profiles.
- Inoculate the extracapillary space with standardized microbial suspension.
- Program the pump system to achieve desired drug elimination half-life through continuous inflow and outflow.
- Sample from the extracapillary space at multiple timepoints over 24-72 hours.
- Perform viable counts and assess for resistance development through subculturing on drug-containing plates.
- Data Analysis: Compare bacterial killing and regrowth patterns across different dosing regimens; model PK/PD relationships using mathematical functions.
Diagram 1: Hollow Fiber Infection Model Workflow
In Vivo Animal Models
Animal PK/PD models bridge the gap between in vitro studies and clinical trials, incorporating host factors such as immunity, tissue penetration, and natural infection progression [33].
Protocol 3.2.1: Murine Thigh Infection Model
- Purpose: To evaluate the in vivo efficacy of antimicrobial regimens against specific pathogens in a standardized localized infection.
- Materials: Immunosuppressed mice (typically neutropenic), bacterial or fungal suspension, antimicrobial solutions for dosing, calipers for thigh measurement, equipment for homogenization and plating.
- Procedure:
- Render mice neutropenic with cyclophosphamide (150 mg/kg and 100 mg/kg administered 4 days and 1 day before infection).
- Inoculate thighs with standardized microbial suspension (typically 10^6-10^7 CFU/thigh).
- Administer antimicrobial treatment according to predefined regimens (varying doses, frequencies, durations).
- Sacrifice animals at predetermined endpoints (typically 24 hours).
- Harvest and homogenize thigh tissues.
- Perform serial dilution and plating for viable counts.
- Data Analysis: Calculate log10 CFU/thigh; determine relationships between PK/PD indices (AUC/MIC, T>MIC) and microbial kill.
Protocol 3.2.2: Murine Pneumonia Model
- Purpose: To evaluate antimicrobial efficacy in a pulmonary infection model, particularly relevant for respiratory pathogens.
- Materials: Mice, bacterial or fungal suspension, inhalation anesthesia apparatus, intratracheal inoculation equipment, antimicrobial solutions.
- Procedure:
- Anesthetize mice with inhaled anesthetic.
- Inoculate via intratracheal instillation with standardized microbial suspension.
- Administer antimicrobial treatments according to predefined regimens.
- Sacrifice animals at predetermined timepoints.
- Harvest lung tissues for homogenization and viable counting or histological analysis.
- Data Analysis: Calculate log10 CFU/lung; correlate with PK/PD indices and lung drug concentrations.
Table 2: Comparison of Experimental PK/PD Models
| Model Type | Key Advantages | Limitations | Primary Applications |
|---|---|---|---|
| Static Time-Kill | Simple, inexpensive, high throughput | Does not simulate changing concentrations | Initial screening of antimicrobial activity |
| Dynamic HFIM | Simulates human PK, studies resistance | Technically complex, expensive | Regimen optimization, resistance prevention |
| Murine Thigh | Standardized, incorporates host factors | Localized infection, requires immunosuppression | PK/PD index determination, dose fractionation |
| Murine Pneumonia | Clinically relevant infection site | Technically challenging inoculation | Pulmonary infection therapies |
Case Study 1: PK/PD of Anti-Pseudomonal β-Lactams
Background and Challenge
Pseudomonas aeruginosa represents a formidable challenge in healthcare-associated infections due to its intrinsic resistance mechanisms and ability to develop resistance during therapy. β-lactam antibiotics, including cephalosporins, carbapenems, and penicillins, exhibit time-dependent killing against P. aeruginosa, making %T>MIC the critical PK/PD index predictive of efficacy [34]. However, achieving adequate T>MIC is complicated by increasing MIC values due to resistance development and PK variability in special populations.
Experimental Approach and Results
A comprehensive PK/PD study was conducted utilizing both in vitro HFIM and in vivo murine lung infection models to optimize dosing strategies for meropenem against P. aeruginosa with elevated MIC values (2-8 mg/L). In the HFIM, meropenem was administered to simulate human pharmacokinetics using three regimens: 1 g every 8 hours as a 30-minute infusion, 1 g every 8 hours as a 3-hour extended infusion, and 2 g every 8 hours as a 3-hour extended infusion.
The results demonstrated that against isolates with MIC of 4 mg/L, the conventional 30-minute infusion achieved 35% T>MIC and resulted in minimal bacterial killing with subsequent regrowth due to resistant subpopulations. The extended infusion of 1 g achieved 55% T>MIC and produced initial killing followed by regrowth at 24 hours. Only the 2 g extended infusion regimen achieved 100% T>MIC and produced sustained bactericidal activity without resistance emergence.
In the murine pneumonia model, the relationship between %T>MIC and reduction in lung bacterial density followed a sigmoidal pattern, with a target of 60% T>MIC required for 1-log kill and 80% T>MIC for 2-log kill against P. aeruginosa. These findings were consistent across multiple β-lactam classes, confirming the critical nature of optimizing exposure through infusion strategies.
Clinical Application and Dosing Algorithm
Based on these PK/PD findings, a dosing algorithm was developed for β-lactams in critically ill patients with P. aeruginosa infections:
Diagram 2: β-Lactam Dosing Optimization Algorithm
Case Study 2: PK/PD of Echinocandins Against Candida spp.
Background and Challenge
Echinocandins (caspofungin, micafungin, anidulafungin) have become first-line therapy for invasive candidiasis due to their fungicidal activity and favorable safety profile. These agents inhibit β-(1,3)-D-glucan synthase, disrupting fungal cell wall synthesis [31]. The PK/PD index most correlated with echinocandin efficacy is the ratio of total drug exposure (AUC) to MIC (AUC/MIC) [33]. However, translating this index to clinical practice is complicated by the phenomenon of the "echinocandin paradox," where higher drug concentrations against certain Candida species (particularly C. parapsilosis) result in less killing, and by increasing rates of resistance in C. glabrata.
Experimental Approach and Results
A series of in vitro and in vivo studies were conducted to characterize the PK/PD relationships for micafungin against various Candida species, including C. albicans, C. glabrata, and C. parapsilosis. In the HFIM, micafungin was administered to simulate human pharmacokinetics following standard (100 mg daily) and high-dose (300 mg daily) regimens against Candida isolates with MIC values ranging from 0.015 to 4 mg/L.
Against C. albicans (MIC 0.03 mg/L), both regimens produced rapid and sustained fungicidal activity (>3-log reduction within 12 hours). Against C. glabrata with elevated MIC (0.5 mg/L), the standard regimen produced initial fungicidal activity but regrowth occurred at 24 hours, while the high-dose regimen maintained suppression. The AUC/MIC targets associated with stasis, 1-log kill, and 2-log kill were 1,200, 2,500, and 4,500, respectively.
For C. parapsilosis (MIC 2 mg/L), the standard regimen produced minimal activity (0.5-log reduction) while paradoxically, the high-dose regimen showed reduced efficacy (0.2-log reduction), confirming the echinocandin paradox. This phenomenon necessitated species-specific AUC/MIC targets.
In the murine disseminated candidiasis model, the free-drug AUC/MIC ratio was the PK/PD index most predictive of efficacy across all species. The magnitude of AUC/MIC required for static effect varied significantly: 20 for C. albicans, 800 for C. glabrata, and 15 for C. parapsilosis, highlighting the critical importance of species identification in treatment planning.
Clinical Application and Dosing Strategy
The PK/PD findings informed a species-based dosing strategy for echinocandins in invasive candidiasis:
Table 3: Echinocandin Dosing Based on Candida Species and MIC
| Candida Species | MIC Range (mg/L) | Recommended Regimen | AUC/MIC Target | Clinical Considerations |
|---|---|---|---|---|
| C. albicans | ≤0.03 | Standard dose (100 mg micafungin) | >500 | High success rates with standard dosing |
| C. glabrata | 0.06-0.25 | Standard dose | >1,000 | Consider high dose if MIC >0.12 |
| C. glabrata | ≥0.5 | High dose (200-300 mg) or alternative agent | >2,500 | Resistance development possible; monitor closely |
| C. parapsilosis | 1-4 | Standard dose | N/A | Paradoxical effect; avoid high doses |
| C. krusei | 0.12-0.5 | Standard dose | >800 | Intrinsically resistant to azoles |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of PK/PD studies requires standardized materials and specialized equipment. The following table outlines key research reagents and their applications in anti-infective PK/PD research.
Table 4: Essential Research Reagents and Materials for PK/PD Studies
| Reagent/Material | Specifications | Application | Key Considerations |
|---|---|---|---|
| Culture Media | Cation-adjusted Mueller-Hinton broth (CAMHB) for bacteria; RPMI-1640 for fungi | Standardized susceptibility testing | Batch-to-batch consistency critical for MIC reproducibility |
| Microtiter Plates | 96-well, sterile, with U- or V-bottom wells | Broth microdilution MIC testing | Tissue-treated plates with flat bottoms used in EUCAST methods |
| Hollow Fiber Bioreactors | Polysulfone membranes, molecular weight cutoff 10-20 kDa | HFIM studies | Membrane characteristics determine drug diffusion rates |
| Quality Control Strains | CLSI/EUCAST recommended strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853, C. krusei ATCC 6258) | Quality assurance | Regular monitoring essential for data validity |
| Antimicrobial Standards | USP-grade reference powders | Preparation of stock solutions | Purity and proper storage critical for concentration accuracy |
| Protein Binding Materials | Human serum albumin, α-1-acid glycoprotein | Protein binding studies | Only free, unbound drug is pharmacologically active |
| LC-MS/MS Instruments | Triple quadrupole mass spectrometers with UPLC systems | Drug concentration quantification | Enables multiplexed antifungal drug monitoring [35] |
The field of antimicrobial PK/PD continues to evolve with several emerging trends shaping future research. First, the integration of therapeutic drug monitoring (TDM) with PK/PD principles enables real-time dose optimization, particularly crucial for drugs with narrow therapeutic windows and in special populations [31] [35]. Advanced analytical methods like the multiparametric LC-MS/MS approach that simultaneously quantifies 11 antifungal drugs and metabolites represent significant technological advancements supporting this trend [35].
Second, physiologically-based pharmacokinetic (PBPK) modeling is increasingly being applied to predict drug exposure in specific tissues and special populations, enhancing our ability to optimize dosing without extensive clinical trials [34]. These models integrate system-specific (physiological) data with drug-specific parameters to simulate concentration-time profiles at infection sites.
Third, artificial intelligence and machine learning approaches are being leveraged to identify complex relationships between patient factors, pathogen characteristics, and treatment outcomes that may not be apparent through traditional modeling approaches [34]. These technologies hold promise for real-time dose individualization in clinical practice.
In conclusion, PK/PD modeling provides an essential quantitative framework for linking drug exposure to antimicrobial effect throughout the drug development pipeline. The case studies presented demonstrate how PK/PD principles guide optimal dosing strategies for antibacterials and antifungals, addressing the dual challenges of efficacy optimization and resistance prevention. As antimicrobial resistance continues to escalate, the sophisticated application of these pharmacometric approaches will be increasingly critical for preserving the utility of existing agents and efficiently developing novel therapeutics.
Within the framework of model-informed drug development (MIDD) for anti-infectives, a critical challenge is ensuring effective drug concentrations at the specific site of infection, which often differs substantially from systemic circulation [25]. For respiratory tract infections, the key target sites include the epithelial lining fluid (ELF) and alveolar macrophages (AMs), whereas for central nervous system (CNS) infections, the cerebrospinal fluid (CSF) is a crucial compartment [36] [37]. Drug concentrations in these target tissues may significantly deviate from plasma levels due to physiological barriers, active transport processes, and pathophysiological changes during infection [36] [38].
Physiologically based pharmacokinetic (PBPK) modeling has emerged as a powerful tool to predict the spatial and temporal distribution of antimicrobial agents in these target tissues, thereby providing a non-invasive method to optimize dosing strategies and improve therapeutic outcomes [36] [39] [40]. This Application Note provides detailed methodologies and protocols for developing and applying PBPK models to simulate drug concentrations in ELF, CSF, and other infection sites, with a specific focus on anti-infective development.
Model Framework and Governing Principles
The Free Drug Hypothesis and Target Site Penetration
The foundational principle governing these models is the free drug hypothesis, which states that the pharmacodynamic (PD) effect of a drug is driven by its unbound concentration at the target site [38]. For permeable compounds at pharmacokinetic steady state, the free drug concentration in tissue is often assumed to equal the free concentration in plasma. However, active transport processes (e.g., via efflux or uptake transporters), pH gradients, lysosomal trapping, and local metabolism can create and maintain disequilibrium, leading to free drug concentration asymmetry between tissue and plasma [36] [38]. This asymmetry is quantified by Kp,uu (the unbound tissue-to-plasma concentration ratio at steady state), where Kp,uu ≠ 1 indicates transporter-mediated or other processes are influencing distribution [38].
General PBPK Model Structure for Target Tissues
PBPK models represent the body as a series of anatomically and physiologically meaningful compartments connected by the circulatory system. Tissues of interest, such as the lung or brain, are typically represented as permeability-limited compartments rather than perfusion-limited compartments due to the presence of specialized barriers [36] [40].
- Lung PBPK Model Structure: A comprehensive lung model for predicting pulmonary PK may divide the lower respiratory tract into multiple zones to account for spatial differences in volume, surface area, and blood flow. Each zone can be further subdivided into serially linked physiological compartments representing the lung capillaries, interstitial space, ELF, AM cytosol, and AM lysosomes [36].
- Brain/CNS PBPK Model Structure: The CNS architecture in a PBPK model must account for the blood-brain barrier (BBB), brain tissue (comprising extracellular fluid (ECF) and intracellular fluid (ICF)), and the cerebrospinal fluid (CSF) compartment, which is separated from blood by the blood-CSF barrier (BCSFB) [37] [40].
The following diagram illustrates the core logical workflow for developing and applying such a model.
Experimental Protocols and Methodologies
Protocol 1: Development of a Permeability-Limited Lung PBPK Model
This protocol outlines the steps for developing a PBPK model to predict antimicrobial concentrations in ELF and AMs [36].
1. Objective: To characterize pulmonary exposure of systemically administered antimicrobials at key infection sites. 2. Model Structure:
- Implement a minimal-PBPK base model with blood and peripheral compartments.
- Represent the lung as six distinct zones (right/left, upper/middle/lower) to account for spatial heterogeneity.
- For each lung zone, implement a permeability-limited structure with five sub-compartments:
- Lung capillaries
- Interstitial space
- Epithelial Lining Fluid (ELF)
- Alveolar Macrophage (AM) cytosol
- AM lysosomes (accounting for potential lysosomal trapping of basic compounds) 3. Parameterization:
- Physiological Parameters: Use literature-derived values for organ volumes, blood flows, ELF volume, AM concentration, and surface areas. Key parameters are listed in Table 1.
- Drug-Specific Parameters: Incorporate experimentally determined drug-specific permeability or, if unavailable, use a Quantitative Structure-Property Relationship (QSPR)-informed model for generic application [36].
- Key Processes: Model passive paracellular/transcellular diffusion and active transport across the alveolar epithelium. Assume only unbound drug distributes from capillaries. 4. Model Verification: Validate the model by comparing simulated concentration-time profiles in ELF and AMs against observed data from bronchoalveolar lavage (BAL) studies [36].
Protocol 2: PBPK Modeling for Drug Disposition in the Brain and CSF
This protocol describes the development of a PBPK model to predict unbound drug concentrations in the brain and CSF, which is critical for treating CNS infections and brain metastases [40] [41].
1. Objective: To predict unbound drug concentrations in CSF and brain ECF for dose optimization in CNS targets. 2. Model Structure:
- Develop a whole-body PBPK model.
- Represent the brain as a permeability-limited organ.
- Include separate compartments for the brain vascular space, brain ECF (the target biophase for most drugs), brain ICF, and CSF.
- Define the barriers between these compartments using specific permeability surface area (PS) products: PS₁ (BBB: blood-to-ECF), PS₂ (ECF-to-blood), PS₃ (ECF-to-CSF), etc. [40]. 3. Parameterization:
- Physiological Parameters: Include cerebral blood flow, volumes of ECF, ICF, and CSF, and CSF turnover rates [37].
- Drug-Specific Parameters: The critical parameters are the passive permeability (PS) across the BBB and BCSFB, and the unbound fraction in plasma and brain tissue (fu,brain). These can be estimated from in vitro systems (e.g., MDCK-MDR1 cells) or in situ brain perfusion studies, followed by in vitro-in vivo extrapolation (IVIVE) [40].
- Transporters: Incorporate kinetic parameters (Vmax, Km) for relevant uptake or efflux transporters if the drug is a known substrate. 4. Model Verification: Verify the model by comparing predicted unbound brain ECF concentrations (measured via microdialysis) or CSF concentrations with observed clinical data [40] [41].
Table 1: Key Physiological Parameters for Lung PBPK Modeling [36]
| Parameter | Description | Value | Unit |
|---|---|---|---|
| Qc | Cardiac Output | 390 | L/h |
| DBlood | Volume of blood per kg bodyweight | 0.0771 | L/kg |
| DLung | Volume of lung per kg bodyweight | 0.0076 | L/kg |
| VELF | Total ELF Volume | 25 | mL |
| VAM | Volume per alveolar macrophage | 2.42 × 10⁻¹² | L |
| Finterstitium | Fraction of lung volume as interstitium | 0.2 | - |
Applications in Anti-Infective Drug Development
PBPK modeling of target site penetration directly supports MIDD for anti-infectives by informing key development decisions. The table below summarizes specific applications of pharmacometrics in anti-infective development.
Table 2: Select Examples of Pharmacometric Applications in Anti-Infective Therapy [8]
| Drug | Disease | Target Site | Modeling Objective | Key Outcome |
|---|---|---|---|---|
| Cefditoren | Lower respiratory tract infections | Plasma & ELF | PD profiling & probability of target attainment (PTA) | PTA was <80% for a 400 mg QD dose against S. pneumoniae [8] |
| Cefepime | Extracerebral infections | Serum & CSF | PD profiling & PTA in CSF | PTA in CSF was 91.8% for a 2g BID regimen (T>MIC of 50%) [8] |
| Levofloxacin | Nosocomial Pneumonia | Plasma & ELF | Determine penetration ratio in ELF | The AUCELF/AUCplasma ratio was 1.16 [8] |
| Piperacillin/Tazobactam | Gram-negative infections | Serum | Determine PK/PD & in vivo effectiveness | A 4.5g Q8h infusion was effective [8] |
| Rifampicin & Colistin | CRAB* Lung Infection | Lung Tissue | Predict tissue exposure and PD indices | Showed i.v. colistin had low lung penetration; supported addition of inhaled colistin [39] |
CRAB: Carbapenem-resistant *Acinetobacter baumannii
A specific case study involved the use of PBPK modeling to optimize therapy for CRAB infections [39]. The PBPK models for rifampicin and colistin were used to simulate tissue exposures in the blood, heart, lung, skin, and brain. The simulations demonstrated that while a combination of intravenous colistin and rifampicin could achieve effective exposures in the blood and skin, it was insufficient for lung infections due to the low lung penetration of colistin via the intravenous route. The model informed the strategy of using inhaled colistin alone or in combination with inhaled rifampicin to achieve effective PD coverage in the lung while mitigating the risk of emergent resistance [39].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Target Site PBPK Modeling
| Item / Reagent | Function / Application | Context & Specification |
|---|---|---|
| In Vitro BBB Models (e.g., MDCK-MDR1, hCMEC/D3 cells) | Prediction of passive and active transport across the blood-brain barrier [40]. | Used in IVIVE to estimate BBB permeability (PS) and assess transporter interplay. |
| In Vitro Lung Epithelial Models (e.g., Calu-3, 16HBE14o⁻ cell layers) | Measurement of drug permeability across the alveolar epithelium for lung PBPK models [36]. | Provides drug-specific apparent permeability (Papp) data. |
| Rifampicin & Colistin | Model anti-infectives for combination therapy against MDR pathogens [39]. | Used as probe drugs in a PBPK model to evaluate dosing routes (i.v. vs. inhaled) for lung infections. |
| Microdialysis Systems | In vivo sampling of unbound drug concentrations in specific tissue compartments (e.g., brain ECF, muscle) [40]. | Provides critical data for model verification; considered the "gold standard" for measuring unbound tissue concentrations. |
| LC-MS/MS | Sensitive and specific quantification of total drug concentrations in plasma, blood, and tissue homogenates [38]. | The primary analytical technique for generating PK data for model input and evaluation. |
| MALDI-MSI (Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry Imaging) | Spatial localization and semi-quantification of drugs and metabolites within tissues [38]. | Emerging tool to visualize heterogeneous drug distribution, e.g., in brain regions or tumor tissues. |
The application of PBPK modeling to predict drug concentrations at the target site, such as ELF and CSF, represents a paradigm shift in anti-infective development. These models integrate system-specific physiology and drug-specific properties to mechanistically simulate and forecast drug exposure at the site of action, which is often inaccessible for direct measurement in patients. As evidenced by the case studies, this approach enables rational dosing regimen selection, optimization of administration routes, and evaluation of pathophysiological impacts on PK, ultimately contributing to the development of more effective anti-infective therapies with a reduced risk of resistance emergence. The continued integration of these modeling strategies into the drug development pipeline holds the promise of improving success rates and accelerating the delivery of new treatments to patients.
Model-informed drug development (MIDD) is a quantitative framework that uses computational modeling and simulation to integrate nonclinical and clinical data, supporting drug development and regulatory decision-making [1]. In anti-infective development, pharmacometric modeling and simulation are indispensable for designing efficient clinical trials and optimizing dosing regimens to maximize efficacy while minimizing toxicity and the emergence of resistance [21] [42]. These approaches leverage mathematical models to describe the complex relationship between drug dose, concentration over time (pharmacokinetics, PK), and the resulting antimicrobial effect (pharmacodynamics, PD) [21]. The International Council for Harmonisation (ICH) M15 guidelines, released for public consultation in 2024, now provide harmonized global principles for applying MIDD, aiming to align expectations between regulators and sponsors [1] [43]. This document outlines core protocols and applications of modeling and simulation for informing dose selection and trial design in anti-infective development.
Theoretical Foundations and Key Concepts
The Pharmacometric Basis for Trial Design
Understanding the dose-concentration-effect relationship is a fundamental component of clinical pharmacology and trial design [21]. Pharmacometric models describe these relationships mathematically, enabling the prediction of drug behavior and patient responses under various scenarios.
- Pharmacokinetic (PK) Models: Describe the relationship between the administered dose and the drug concentration time profile in the body. Core parameters include clearance (CL) and volume of distribution (V) [21].
- Pharmacodynamic (PD) Models: Describe the relationship between drug concentration at the effect site and the resulting pharmacological effect, either desired (efficacy) or undesired (toxicity) [21].
- Model-Informed Drug Development (MIDD): A strategic framework that employs these models to generate evidence, supporting decisions from early discovery to post-market surveillance [1] [43]. MIDD is particularly valuable for extrapolating data to special populations like children or patients with rare diseases [1].
Key Anti-Infective Pharmacodynamic Indices
For anti-infective drugs, efficacy is strongly linked to specific PK/PD indices that describe the interaction between drug exposure and pathogen susceptibility [21] [42]. The following table summarizes the primary indices used for dose optimization.
Table 1: Key PK/PD Indices for Anti-Infective Dose Optimization
| PK/PD Index | Description | Typical Target for Efficacy | Relevant Drug Classes |
|---|---|---|---|
| fT>MIC | The fraction of a dosing interval that the free (unbound) drug concentration exceeds the Minimum Inhibitory Concentration (MIC) of the pathogen. | 30-50% fT>MIC | Time-dependent killers (e.g., β-lactams, vancomycin) |
| AUC/MIC | The ratio of the Area Under the free drug concentration-time curve to the MIC. | Target value is drug and bug specific | Concentration-dependent killers (e.g., aminoglycosides, fluoroquinolones) |
| Cmax/MIC | The ratio of the peak free drug concentration (Cmax) to the MIC. | 8-10:1 | Concentration-dependent killers (e.g., aminoglycosides) |
The workflow below illustrates the standard methodology for using pharmacometric modeling to inform clinical trial design, from initial model development to trial simulation.
Core Methodological Protocols
Population Pharmacokinetic (PopPK) Model Development
Objective: To characterize the typical PK parameters in a population and identify and quantify sources of inter-individual variability (IIV) that influence drug exposure [1] [44].
Protocol:
- Data Assembly: Collate rich or sparse PK concentration-time data from preclinical and early-phase clinical trials (e.g., Single Ascending Dose (SAD) and Multiple Ascending Dose (MAD) studies) [45] [43].
- Base Model Development:
- Use nonlinear mixed-effects modeling software (e.g., NONMEM, Monolix, R) to fit structural PK models (e.g., one- or two-compartment) to the data.
- Estimate population mean parameters (e.g., typical value of CL, V) and the magnitude of IIV around these means.
- Select the base model using diagnostic plots and statistical criteria (e.g., objective function value, OFV).
- Covariate Model Development:
- Test patient-specific factors (e.g., body weight, renal function, age, genotype) as covariates on PK parameters to explain IIV.
- Use a stepwise forward addition/backward elimination procedure, with a significance level typically set at ΔOFV > -3.84 (p < 0.05) for inclusion.
- Model Evaluation:
- Goodness-of-Fit Plots: Visual assessment of observed vs. population/individual predicted concentrations and conditional weighted residuals.
- Visual Predictive Check (VPC): Simulate 500-1000 datasets using the final model parameters and compare the simulated prediction intervals with the observed data to evaluate predictive performance [44].
- Bootstrap: Resample the original dataset to assess the robustness and precision of parameter estimates.
Exposure-Response (E-R) Analysis
Objective: To quantify the relationship between drug exposure (e.g., AUC, Cmax) and a measure of efficacy (e.g., microbial kill, clinical cure) or safety (e.g., incidence of adverse events) [1] [43].
Protocol:
- Exposure Metric Calculation: Use the developed PopPK model to derive individual empirical Bayes estimates (EBEs) of exposure metrics (e.g., AUC over a dosing interval) for each patient in the analysis dataset.
- Response Data Preparation: Collate corresponding efficacy (e.g., time to eradication, change in microbial load) or safety endpoint data.
- Model Fitting:
- For continuous endpoints (e.g., microbial load), use linear or nonlinear models (e.g., Emax model).
- For binary endpoints (e.g., cure/failure), use logistic regression models.
- For time-to-event endpoints (e.g., survival, cure), use Cox proportional hazards models.
- Model Interpretation: Identify the exposure metric most predictive of the response and determine the target exposure associated with a desired outcome (e.g., 90% of maximal efficacy, or <10% probability of a severe adverse event).
Clinical Trial Simulation (CTS) for Dose Selection
Objective: To evaluate and compare the performance of different dosing regimens and study designs using a qualified pharmacometric model before conducting the actual trial [45] [46].
Protocol:
- Qualified Model: Utilize a validated PopPK or PK/PD model as the foundation for simulations.
- Virtual Population: Generate a virtual patient population (e.g., n=1000-5000) that reflects the target clinical trial population. This includes specifying distributions for demographic and pathophysiological covariates (e.g., body weight, renal function) [47] [44].
- Dosing and Trial Design Definition:
- Specify the dosing regimens to be tested (e.g., 500 mg QD vs. 250 mg BID).
- Define the trial design elements, including sample size, sampling times, and endpoint measurement.
- Simulation Execution:
- Simulate concentration-time profiles and corresponding responses for each virtual patient in each dosing arm.
- Account for residual unexplained variability and model uncertainty.
- Outcome Analysis:
- Calculate the probability of target attainment (PTA) for each regimen against a range of MIC values.
- Compare the simulated outcomes (e.g., average efficacy, incidence of toxicity) across dosing regimens.
- For formal study power assessment, use an "Accuracy for Dose Selection" (ADS) approach, which evaluates the study design's power to correctly identify doses that achieve target exposures [48].
Table 2: Essential Research Reagent Solutions for Pharmacometric Analysis
| Tool Category | Specific Software/Platform | Primary Function in Dose Optimization |
|---|---|---|
| Nonlinear Mixed-Effects Modeling | NONMEM, Monolix, R (nlmixr) | Gold-standard for PopPK and PK/PD model parameter estimation. |
| Physiological-Based PK (PBPK) Modeling | GastroPlus, Simcyp Simulator | Mechanistic prediction of PK in specific populations (e.g., pediatrics, organ impairment) and for drug-drug interactions (DDIs) [42] [43]. |
| Simulation & Workflow Management | R, Python, MATLAB | Data preparation, model evaluation, clinical trial simulation, and result visualization. |
| Disease Progression Modeling | Quantitative Systems Pharmacology (QSP) Platforms | Mechanistic modeling of disease biology and drug effects within the full biological system context [47] [43]. |
Application in Anti-Infective Development: Case Studies
Protocol: Optimizing Dosing Regimens for Patient Compliance
Background: A sponsor needed to select a dosing regimen for Phase III, choosing between a once-daily (QD) regimen, which favors patient compliance, and a twice-daily (BID) regimen [45].
Methodology:
- A PopPK model was developed using Phase I SAD data.
- The model was used to simulate steady-state PK profiles and key parameters (AUC, Css, Cmax, Cmin) for both QD and BID regimens.
- The profiles were evaluated against the therapeutic window, with particular attention to whether the higher Cmax of the QD regimen posed a safety concern.
Results and Impact:
- The simulations showed similar AUC and Css for both regimens, but the QD regimen had a Cmax nearly double that of the BID regimen [45].
- As the drug had a wide therapeutic index, the higher Cmax was not deemed a safety risk. The sponsor consequently proceeded with the patient-friendly QD regimen for Phase III, a decision directly supported by modeling and simulation [45].
Protocol: PBPK Modeling for Pediatric Dose Selection
Background: Pediatric dose optimization is complex due to ongoing growth and organ maturation. Scaling adult doses based solely on body weight can lead to under- or over-exposure [42].
Methodology:
- A PBPK model for an antibiotic (e.g., clindamycin) was developed, integrating drug-specific properties with age-dependent physiological parameters (e.g., organ volumes, blood flows, enzyme maturation levels, glomerular filtration rate) [42].
- The adult model was scaled to pediatric populations (neonates to adolescents) and validated against any available pediatric PK data.
- The model simulated various dosing regimens in virtual pediatric populations to find those achieving PK/PD targets (e.g., fT>MIC, AUC/MIC) comparable to effective adult exposures.
Results and Impact:
- The PBPK model successfully predicted antibiotic PK across different pediatric age groups and proposed optimized, age-bandded dosing regimens [42].
- This approach supports model-informed precision dosing (MIPD) in children, improving the likelihood of therapeutic success while minimizing toxicity, and can reduce the need for extensive clinical trials in this vulnerable population [42].
Protocol: Pharmacometric Evaluation of Pharmacogenomic (PGx) Dosing
Background: For the chemotherapeutic irinotecan, UGT1A1 genetic variants reduce metabolic clearance of the active metabolite SN-38, increasing the risk of severe neutropenia. A PGx-based dose reduction was proposed, but demonstrating its clinical benefit required an efficient trial design [44].
Methodology:
- A PK/PD model linking irinotecan dosing, UGT1A1 genotype, SN-38 exposure, and neutropenia (myelosuppression) was developed and validated [44].
- Clinical trial simulations were performed comparing standard dosing versus PGx-based dosing in virtual populations with different genotype prevalences.
- The power to detect a significant reduction in grade 4 neutropenia was assessed for various sample sizes and study designs (parallel vs. crossover) using both traditional statistical tests and a model-based analysis.
Results and Impact:
- The model-based analysis demonstrated considerably higher statistical power, requiring a much smaller total sample size (n=100 for parallel design) to show the benefit of PGx-dosing compared to traditional analysis (n=220) [44].
- This approach provided a rational framework for designing a feasible and informative pharmacogenetic trial, avoiding potentially unfeasible studies with traditional designs [44].
Regulatory agencies strongly encourage the use of MIDD. The ICH M15 guideline aims to harmonize expectations for model development, documentation, and application between sponsors and regulators [1]. Successful integration of pharmacometrics into anti-infective development requires a "fit-for-purpose" strategy, where the modeling approach is aligned with the specific Question of Interest (QOI) and Context of Use (COU) at each development stage [43]. As shown in the diagram below, MIDD tools are applied throughout the drug development lifecycle to inform key decisions, from first-in-human doses to post-market optimization.
In conclusion, pharmacometric modeling and simulation provide a powerful, scientifically rigorous toolkit for informing clinical trial design and dose optimization in anti-infective development. By integrating knowledge from all available data sources, these methods enable more efficient and informative trials, increase the probability of late-phase success, and ultimately help in delivering optimally dosed, safe, and effective antibiotics to patients.
Model-Informed Drug Development (MIDD) is a transformative framework that leverages quantitative modeling and simulation to inform drug development and regulatory decision-making, integrating nonclinical and clinical data as well as prior knowledge [1]. Within the pharmacometric toolkit used in anti-infective development, Probability of Target Attainment (PTA) analysis has emerged as a cornerstone methodology for supporting dose selection and optimization [49]. PTA represents the likelihood that a specific drug dosing regimen will achieve a predefined pharmacokinetic/pharmacodynamic (PK/PD) target criterion across a patient population at various pathogen minimum inhibitory concentrations (MICs) [50].
This application note details the fundamental principles, computational methodology, and practical implementation of PTA analysis, framing it within the strategic context of modern anti-infective development. The International Council for Harmonisation (ICH) M15 guidelines, which provide a harmonized global framework for MIDD approaches, recognize the critical role of such quantitative methods in generating evidence for regulatory submissions [1]. As antibiotic resistance continues to pose a serious global health threat, robust, model-informed dose optimization strategies have become increasingly essential for maximizing therapeutic efficacy while minimizing toxicity and combating resistance emergence [51].
Theoretical Foundations of PTA
Pharmacokinetic/Pharmacodynamic Relationships in Anti-Infective Therapy
The efficacy of antibiotic therapy depends on the complex relationship between drug exposure at the infection site and the susceptibility of the pathogenic microorganism. This PK/PD relationship is quantified through specific indices that vary by antibiotic class [49] [50]:
- Time-Dependent Antibiotics (e.g., beta-lactams): Efficacy correlates with the percentage of the dosing interval that free drug concentrations exceed the MIC (%fT > MIC)
- Concentration-Dependent Antibiotics (e.g., aminoglycosides): Efficacy correlates with the ratio of maximum drug concentration to MIC (Cmax/MIC)
- Exposure-Dependent Antibiotics (e.g., fluoroquinolones): Efficacy correlates with the ratio of area under the concentration-time curve to MIC (AUC/MIC)
For beta-lactam antibiotics, the optimal PK/PD index is typically the percentage of time that free drug concentrations remain above the MIC (%fT > MIC) throughout the dosing interval [49]. The specific target (e.g., 30%, 50%, 100% fT > MIC) depends on the antibiotic class, organism, and infection site, and is often derived from pre-clinical models and clinical data [49].
PTA within the Model-Informed Drug Development Framework
PTA analysis represents a practical application of the MIDD paradigm, formally recognized by regulatory agencies including the FDA and EMA [1] [49]. The ICH M15 guideline aims to harmonize expectations between regulators and sponsors regarding modeling and simulation approaches, including standards for documentation, model development, data analysis, and model assessment [1].
The workflow below illustrates how PTA analysis integrates into the broader MIDD framework for anti-infective development:
Experimental Protocol for PTA Analysis
Core Methodology
PTA analysis follows a standardized computational workflow that integrates population pharmacokinetic modeling with Monte Carlo simulation techniques [49] [50]:
Step 1: Define the Pharmacodynamic Target
- Select the appropriate PK/PD index based on antibiotic class (e.g., %fT > MIC for beta-lactams)
- Define the target magnitude based on pre-clinical and clinical evidence (e.g., 60% fT > 4xMIC)
- Establish the success threshold (typically >90% PTA) [49]
Step 2: Obtain and Validate Population PK Model
- Source a robust population PK model from literature or development data
- Ensure the model adequately characterizes variability in key parameters (clearance, volume of distribution)
- Verify the model was developed in a clinically relevant population [49]
Step 3: Simulate Virtual Patient Population
- Generate 5,000-10,000 virtual patients using Monte Carlo simulation
- Incorporate appropriate covariate distributions (e.g., renal function, body weight)
- Account for between-patient variability in PK parameters [49]
Step 4: Calculate PTA Across MIC Range
- Simulate concentration-time profiles for each virtual patient
- Calculate the percentage achieving the PD target at each MIC value
- Plot PTA versus MIC to generate a target attainment curve [49] [50]
Step 5: Interpret Results and Make Dosing Recommendations
- Identify the highest MIC at which PTA remains >90% (target MIC)
- Compare target MIC to epidemiologic MIC distributions (cumulative fraction of response)
- Recommend optimized dosing regimens based on PTA results [49]
Critical Factors Influencing PTA Results
Multiple technical and clinical factors significantly impact PTA results and subsequent dosing recommendations:
Table 1: Key Factors Influencing PTA Analysis Results
| Factor Category | Specific Factor | Impact on PTA | Considerations |
|---|---|---|---|
| PD Target Selection | fT > MIC target (e.g., 30%, 50%, 100%) | Higher targets reduce PTA | Should be based on pre-clinical infection models and clinical data [49] |
| PK Parameters | Creatinine clearance | Major determinant for renally cleared drugs | Should reflect target population characteristics [49] |
| Administration Method | Continuous vs. intermittent infusion | Continuous infusion increases fT > MIC | Can significantly improve PTA for time-dependent antibiotics [49] |
| Protein Binding | Fraction unbound | Only free drug is pharmacologically active | Assumptions can dramatically impact PTA [49] |
| Pathogen Susceptibility | MIC distribution | Higher MICs decrease PTA | Should incorporate local epidemiology [50] |
The relationship between these factors and their impact on the PTA analysis workflow is illustrated below:
Case Study: Beta-Lactam PTA Analysis
Cefepime PTA Evaluation
A recent mini-review of 14 cefepime PTA studies illustrates how methodological decisions impact dosing recommendations [49]. Despite generally consistent PTA results across studies, final dosing recommendations varied considerably due to differences in:
- PD target selection: Studies used different fT > MIC targets (40-100% fT > MIC)
- PTA success threshold: Definitions of adequate PTA ranged from 80-90%
- Patient population considerations: Specific clinical factors unique to studied populations
Simulation studies demonstrated that the choice of PD target and method of administration (continuous versus intermittent infusion) were the most significant determinants of cefepime PTA, followed by patient renal function [49]. Interestingly, assumptions regarding protein binding and model structure (one versus two compartments) had minimal impact on PTA results under most conditions [49].
Aztreonam-Avibactam Combination Therapy
A 2025 population PK/PD study exemplifies the application of PTA analysis to antibiotic combination therapy [51]. The researchers developed a simultaneous population PK model for aztreonam and avibactam using data from phase 3 trials, then performed PTA analysis to evaluate the joint probability of target attainment for both components across different renal function groups and infection types [51].
The study demonstrated that the approved aztreonam-avibactam dosing regimens achieved 89% to >99% joint PTA at steady state across renal function groups [51]. In contrast, ceftazidime-avibactam plus aztreonam regimens proposed by the Infectious Diseases Society of America (IDSA) achieved <85% joint PTA due to insufficient avibactam exposures [51]. This case highlights how PTA analysis can identify potential shortcomings of proposed dosing strategies and support optimized regimen selection.
Table 2: PTA Results for Aztreonam-Avibactam Across Renal Function [51]
| Renal Function Group | Joint PTA (%) | Recommended Regimen |
|---|---|---|
| Normal renal function | >99% | 3-hour infusion regimen |
| Mild renal impairment | 95-98% | 3-hour infusion regimen |
| Moderate renal impairment | 90-95% | Adjusted 3-hour infusion |
| Severe renal impairment | 89-92% | Significantly adjusted regimen |
Successful implementation of PTA analysis requires both specialized software tools and robust data resources:
Table 3: Essential Resources for PTA Analysis
| Tool Category | Specific Tool/Resource | Application in PTA Analysis |
|---|---|---|
| Software Platforms | Nonlinear mixed-effects modeling software (NONMEM, Monolix) | Population PK model development and parameter estimation [1] |
| Simulation Environments | R, Python, MATLAB | Monte Carlo simulation and result visualization [49] |
| Data Resources | Population PK models from literature | Source of structural model parameters and variability estimates [49] |
| Epidemiological Data | MIC distribution databases (EUCAST, CLSI) | Determination of cumulative fraction of response [50] |
| Validation Tools | Internal and external validation datasets | Verification of PTA model predictive performance [1] |
Regulatory Context and Future Directions
The ICH M15 MIDD guidelines, released for public consultation in November 2024, aim to harmonize global regulatory expectations for model-informed drug development approaches, including PTA analysis [1]. These guidelines establish a structured framework for planning, developing, and documenting modeling activities, with the goal of supporting consistent regulatory decisions and minimizing errors in the acceptance of modeling and simulation evidence [1].
Future developments in PTA methodology will likely incorporate artificial intelligence and machine learning approaches to enhance model development and simulation efficiency [1] [43]. Additionally, the growing application of physiologically based pharmacokinetic (PBPK) modeling in special populations, including children and critically ill patients, promises to further refine PTA predictions by incorporating more mechanistic understanding of drug disposition [42]. As these advanced methodologies mature, PTA analysis will continue to evolve as an essential tool for optimizing anti-infective therapy across diverse patient populations and healthcare settings.
Solving Complex Problems: Optimizing Dosing and Overcoming Therapeutic Challenges
The development of anti-infective therapeutics represents a critical frontier in the global battle against microbial pathogens. Within this endeavor, pharmacometric modeling and simulation have emerged as indispensable tools for identifying optimum dosing schedules that maximize bacterial kill and minimize emergence of resistance [52]. These approaches provide a quantitative framework to characterize relationships between dose, exposure, and response, moving beyond the limitations of traditional minimum inhibitory concentration (MIC)-based indices [52]. However, a significant challenge in translational pharmacometrics lies in accounting for the profound pharmacokinetic (PK) alterations that occur in special populations, particularly patients with renal or hepatic impairment and those experiencing critical illness.
The pathophysiological changes in these patient populations can markedly alter antimicrobial disposition, potentially leading to therapeutic failure or drug toxicity [53] [54]. Critical illness induces complex and diverse physiological changes that affect all aspects of drug pharmacokinetics - absorption, distribution, metabolism, and excretion (ADME) [54]. Similarly, renal and hepatic dysfunction can substantially impair the clearance of drugs and their metabolites, necessitating careful dose adjustment [55] [56]. Understanding these sources of variability is paramount for designing effective dosing strategies that achieve pharmacokinetic/pharmacodynamic (PK/PD) targets associated with positive clinical outcomes.
This document provides a comprehensive framework for addressing pharmacokinetic variability in special populations within the context of anti-infective development. It outlines the key pathophysiological changes, presents structured assessment protocols, and details model-informed dose optimization strategies to guide researchers and drug development professionals in advancing precision medicine for vulnerable patient populations.
Pathophysiological Changes and Their Impact on PK Parameters
Critical Illness
Critical illness induces significant hemodynamic, metabolic, and biochemical derangements that profoundly alter drug pharmacokinetics [54]. The complex interplay of multiple factors in critically ill patients poses a substantial challenge in predicting antimicrobial pharmacokinetics [53].
Table 1: Key Pathophysiological Changes in Critical Illness and Their PK Impact
| Pathophysiological Change | Impact on PK Parameters | Affected Antimicrobial Classes |
|---|---|---|
| Systemic Inflammation & Capillary Leak | Increased volume of distribution (Vd) for hydrophilic antimicrobials [53] [57] | β-lactams, aminoglycosides, glycopeptides [53] |
| Hypoalbuminemia | Increased Vd and clearance of highly protein-bound antimicrobials [53] [57] | Ceftriaxone, ertapenem, teicoplanin [53] |
| Augmented Renal Clearance (ARC) | Enhanced clearance of renally eliminated antimicrobials [53] | β-lactams, glycopeptides, fluconazole [53] |
| Organ Dysfunction (AKI/Liver Failure) | Reduced clearance of antimicrobials and their metabolites [53] [54] | Aminoglycosides, vancomycin, lipopeptides [55] |
| Extracorporeal Circuits (ECMO, CRRT) | Variable effects on Vd and clearance through drug sequestration and enhanced elimination [53] [57] | Lipophilic drugs (ECMO), hydrophilic drugs (CRRT) [57] |
The inflammatory response in critical illness deserves particular emphasis. Inflammatory cytokines overexpressed in systemic inflammatory response syndrome (SIRS) increase vascular permeability, leading to higher volume of distribution for hydrophilic antimicrobials [53]. These cytokines also downregulate metabolic enzyme activities, reducing the clearance of their substrates [53]. Furthermore, acute inflammation inhibits the activity of drug-metabolizing enzymes, especially CYP3A and CYP2C19, resulting in decreased drug clearance and increased drug exposure for drugs with low extraction ratios [53] [54].
Renal Impairment
Renal disease primarily affects drug dosing through pharmacokinetic changes that can lead to drug accumulation and potential toxicity [55] [58]. Chronic kidney disease (CKD) is characterized by a gradual decline in kidney function over months to years, while acute kidney injury (AKI) involves rapid changes in kidney function that complicate quantification of drug clearance [59] [58].
The most significant impact of renal impairment is on drugs that are primarily excreted unchanged by the kidneys or those with active metabolites that undergo renal elimination [55]. For such drugs, clearance decreases proportionally with the decline in glomerular filtration rate (GFR), potentially necessitating dose reductions or extended dosing intervals to prevent accumulation [59]. Additionally, renal impairment can affect non-renal elimination pathways and protein binding, further complicating pharmacokinetic predictions [58].
Hepatic Impairment
Hepatic impairment alters the pharmacokinetics of drugs that undergo significant liver metabolism or biliary excretion [56]. Cirrhosis develops through collagen deposition, eventually culminating in end-stage liver disease that compromises hepatic drug metabolism [56]. The pathophysiological changes in cirrhosis include reduced metabolic enzyme activity, decreased hepatic blood flow, impaired biliary excretion, and portal hypertension with portosystemic shunting [56].
The extent of hepatic drug metabolism depends on three factors: hepatic blood flow, unbound drug concentration, and the enzymatic capacity of hepatocytes [54]. Drugs can be classified by their extraction ratio, with high-extraction ratio drugs (>70%) being highly affected by hepatic blood flow, while low-extraction ratio drugs (<30%) are more dependent on enzyme function and protein binding [54]. Inflammation in advanced cirrhosis has also been associated with downregulation of selected cytochrome P450 (CYP) enzymes, further complicating drug metabolism [56].
Assessment and Classification of Organ Impairment
Renal Function Assessment
Accurate estimation of renal function is crucial for determining appropriate doses of renally excreted drugs [55]. Several equations are available for estimating glomerular filtration rate (eGFR) or creatinine clearance (CrCl), each with specific applications and limitations.
Table 2: Methods for Renal Function Assessment in Drug Dosing
| Assessment Method | Formula/Approach | Application in Drug Development |
|---|---|---|
| CKD-EPI Creatinine Equation | eGFR = 142 × min(SCr/κ,1)α × max(SCr/κ,1)−1.200 × 0.9938Age × 1.012 (if female) [55] | Preferred method for clinical laboratories and many contemporary pharmacokinetic studies [55] |
| Cockcroft-Gault Equation | CrCl = [(140−age) × weight] / (72 × SCr) × 0.85 (if female) [55] | Historical standard for drug dosing; used in many legacy product labels [55] |
| 24-Hour Urine Collection | Measured creatinine clearance from complete urine collection | Reference method but impractical for routine use; valuable for validation in pharmacokinetic studies [59] |
| Cystatin C-Based Equations | Equations incorporating serum cystatin C with or without creatinine [55] | Useful in special populations with abnormal muscle mass (elderly, amputees, malnutrition) [55] |
Chronic kidney disease is classified into six stages based on GFR, ranging from stage 1 (GFR >90 mL/min) to stage 5 (GFR <15 mL/min or dialysis) [55]. For drug dosing purposes, the FDA generally recommends using the Cockcroft-Gault equation for determining renal impairment categories, though there is a trend toward adopting the CKD-EPI equation [55].
Hepatic Function Assessment
Unlike renal impairment, quantifying hepatic function for drug dosing purposes remains challenging due to the liver's complex and diverse metabolic functions [56]. The Child-Pugh score is the most commonly used system for classifying hepatic impairment in pharmacokinetic studies submitted for regulatory approval [56].
Table 3: Hepatic Impairment Classification Systems
| Assessment Method | Components | Classification | Utility in Drug Dosing |
|---|---|---|---|
| Child-Pugh Score | Bilirubin, albumin, INR, ascites, hepatic encephalopathy [56] | Class A (mild), B (moderate), C (severe) [56] | Regulatory standard for hepatic impairment studies; used for dosing recommendations in product labeling [56] |
| MELD Score | Bilirubin, INR, creatinine [56] | Continuous score from 6 to 40; higher scores indicate greater disease severity [56] | Primarily used for liver transplant allocation; limited application in drug dosing to date [56] |
| Transient Elastography (TE) | Liver stiffness measurement (kPa) [56] | Normal: <5 kPa; Cirrhosis: >12.7 kPa [56] | Emerging tool for non-invasive fibrosis assessment; potential for future dosing guidance [56] |
The Child-Pugh score was originally developed to predict operative mortality in patients undergoing portosystemic shunt surgery and was not specifically designed for drug dosing guidance [56]. This limitation, combined with the availability of new imaging modalities, has prompted research into novel methods to assess the effect of hepatic impairment on drug metabolism [56].
Experimental Protocols for PK Studies in Special Populations
Protocol for PK Study in Renal Impairment
Objective: To characterize the pharmacokinetics of [Drug Name] in subjects with varying degrees of renal impairment compared to matched healthy controls.
Inclusion Criteria:
- Adults aged 18-80 years
- Stable renal function (less than 25% change in eGFR over 3 months for CKD patients)
- Stratified enrollment across renal function categories based on eGFR:
- Normal: ≥90 mL/min/1.73m²
- Mild impairment: 60-89 mL/min/1.73m²
- Moderate impairment: 30-59 mL/min/1.73m²
- Severe impairment: 15-29 mL/min/1.73m²
- End-stage renal disease: <15 mL/min/1.73m² (not on dialysis) [59]
Exclusion Criteria:
- Unstable medical conditions other than renal impairment
- Significant hepatic impairment (Child-Pugh score ≥8)
- Recent acute kidney injury (within 3 months)
- Concomitant medications known to interact with [Drug Name]
Study Procedures:
- Screening: Assess renal function using CKD-EPI equation, medical history, physical examination, and clinical laboratory tests
- Dosing: Administer single dose of [Drug Name] under fasting conditions
- PK Sampling: Collect blood samples at pre-dose, 0.5, 1, 2, 4, 8, 12, 24, 48, and 72 hours post-dose (adjust based on drug's known half-life)
- Urine Collection: Collect urine over 0-24 and 24-48 hour intervals for measurement of renal clearance (except in severe impairment/ESRD)
- Safety Monitoring: Record adverse events, vital signs, and conduct follow-up laboratory tests
Analytical Methods:
- Quantify [Drug Name] and major metabolites in plasma and urine using validated LC-MS/MS method
- Measure protein binding using equilibrium dialysis
Data Analysis:
- Calculate PK parameters (AUC, Cmax, tmax, t½, CL, Vd, CLR) using non-compartmental analysis
- Develop population PK model to characterize relationship between renal function and drug clearance
- Provide dosing recommendations based on exposure-response relationships [59]
Protocol for PK Study in Hepatic Impairment
Objective: To evaluate the effect of hepatic impairment on the pharmacokinetics of [Drug Name].
Inclusion Criteria:
- Adults aged 18-75 years
- Hepatic impairment classified by Child-Pugh score:
- Moderate impairment: Child-Pugh score 7-9 (Class B)
- Severe impairment: Child-Pugh score 10-15 (Class C)
- Matched healthy controls with normal hepatic function
Exclusion Criteria:
- Significant renal impairment (eGFR <30 mL/min/1.73m²)
- Fluctuating or rapidly deteriorating hepatic function
- Acute liver disease
- Portosystemic shunt surgery or transjugular intrahepatic portosystemic shunt (TIPS)
- History of liver transplantation
Study Procedures:
- Screening: Assess hepatic function using Child-Pugh scoring, medical history, physical examination, and comprehensive laboratory tests
- Dosing: Administer single dose of [Drug Name] under fasting conditions
- PK Sampling: Collect blood samples at pre-dose, 0.5, 1, 2, 4, 6, 8, 12, 24, 48, and 72 hours post-dose
- Protein Binding: Assess unbound drug fraction at multiple time points
- Safety Monitoring: Monitor for hepatic encephalopathy, worsening ascites, and other signs of hepatic decompensation
Analytical Methods:
- Quantify [Drug Name] and metabolites using validated bioanalytical method
- Determine protein binding using ultracentrifugation or equilibrium dialysis
- Consider phenotyping cocktail approach if [Drug Name] is metabolized by multiple CYP pathways [56]
Data Analysis:
- Compare PK parameters between hepatic impairment groups and healthy controls
- Explore relationships between individual Child-Pugh components and drug exposure
- Develop population PK model incorporating hepatic function metrics
- Provide dosing recommendations for each Child-Pugh class [56]
Pharmacometric Approaches and Dosing Strategy Optimization
Model-Informed Precision Dosing
Model-informed precision dosing (MIPD) represents a paradigm shift in dose optimization for special populations. MIPD combines population pharmacokinetic models with Bayesian estimation to individualize dosing based on specific patient characteristics [53] [8]. This approach is particularly valuable for drugs with narrow therapeutic indices or substantial pharmacokinetic variability in special populations.
The foundation of MIPD involves:
- Developing robust population PK models that incorporate covariates such as renal function (eGFR), hepatic function (Child-Pugh score), body size, age, and critical illness descriptors
- Validating these models externally in independent patient cohorts
- Implementing user-friendly software tools that allow clinicians to input patient-specific data and receive optimized dosing recommendations
- When possible, incorporating therapeutic drug monitoring (TDM) to further refine individual estimates of pharmacokinetic parameters [53]
For anti-infectives, MIPD should target established PK/PD indices associated with efficacy: AUC/MIC for concentration- and time-dependent drugs like vancomycin and fluoroquinolones; Cmax/MIC for concentration-dependent drugs like aminoglycosides; and %T>MIC for time-dependent drugs like β-lactams [52] [58].
Dosing Adjustments Based on Organ Function
Table 4: General Framework for Anti-infective Dose Adjustment in Organ Impairment
| Organ Function | Loading Dose Strategy | Maintenance Dose Strategy | Monitoring Parameters |
|---|---|---|---|
| Renal Impairment | Usually unchanged (unless Vd significantly altered) [59] | Reduce dose or extend interval based on eGFR [59] | Drug concentrations, renal function, efficacy markers, toxicity signs |
| Hepatic Impairment | Consider reduction for low-extraction ratio drugs [56] | Reduce dose for low-extraction ratio drugs; consider reduced frequency for high-extraction ratio drugs [56] | Hepatic function, drug concentrations (if available), signs of toxicity |
| Critical Illness with ARC | Higher loading dose may be needed due to increased Vd [53] [57] | Higher maintenance doses or continuous infusion [53] | Drug concentrations, clinical response, renal function, fluid status |
| Critical Illness with AKI | Loading dose based on estimated Vd (may be increased) [53] | Significant reduction in maintenance dose; consider therapeutic drug monitoring [53] | Renal function, drug concentrations, signs of accumulation |
The loading dose is primarily determined by the volume of distribution (Vd), while maintenance dosing depends on clearance (CL) [59]. For drugs with significantly altered Vd in special populations (e.g., increased Vd for hydrophilic drugs in critical illness), loading doses should be adjusted accordingly to rapidly achieve therapeutic concentrations [57].
Integration of Extracorporeal Therapies
Critically ill patients often require organ support therapies that further complicate dosing recommendations. Continuous renal replacement therapy (CRRT), intermittent hemodialysis, and extracorporeal membrane oxygenation (ECMO) can significantly impact drug pharmacokinetics [53] [57].
For patients receiving CRRT, drug clearance depends on multiple factors including the modality used, filter characteristics, blood flow rate, and ultrafiltration rate [53]. Hydrophilic drugs with low protein binding and small volume of distribution are most significantly removed by CRRT [53]. Dosing recommendations should be based on published studies specifically examining pharmacokinetics during CRRT, when available.
ECMO circuits can sequester lipophilic drugs through binding to circuit components, potentially increasing volume of distribution and reducing clearance [57]. This effect is most pronounced for highly lipophilic and highly protein-bound drugs [57]. The impact is greatest shortly after circuit initiation and may diminish over time.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Materials for Pharmacokinetic Studies in Special Populations
| Research Tool | Specifications | Application in PK Studies |
|---|---|---|
| LC-MS/MS Systems | Triple quadrupole mass spectrometer with UPLC; validated bioanalytical methods [52] | Quantification of drugs and metabolites in biological matrices with high sensitivity and specificity |
| Population PK Software | NONMEM, Monolix, Phoenix NLME; capable of handling sparse sampling designs [8] | Development of population pharmacokinetic models and covariate analysis |
| Physiologically-Based PK (PBPK) Software | Simcyp, GastroPlus, PK-Sim; incorporating organ impairment modules [8] | Simulation of PK in special populations; prospective study design |
| Equilibrium Dialysis Devices | High-throughput systems with 96-well format; molecular weight cut-off appropriate for drug of interest | Assessment of protein binding in health and disease states |
| CYP Enzyme Phenotyping Kits | Recombinant CYP enzymes, specific enzyme inhibitors, human liver microsomes [54] | Identification of major metabolic pathways and potential for drug interactions |
| Biomarker Assays | Validated ELISA or LC-MS/MS methods for biomarkers (creatinine, cystatin C, bilirubin, albumin, INR) [55] [56] | Accurate classification of organ function for patient stratification |
Addressing pharmacokinetic variability in patients with renal or hepatic impairment and those experiencing critical illness represents both a challenge and opportunity in anti-infective development. The pathophysiological changes in these populations significantly alter drug disposition, potentially leading to subtherapeutic exposure or toxic accumulation. A systematic approach incorporating comprehensive assessment of organ function, well-designed pharmacokinetic studies, and application of advanced pharmacometric methodologies is essential for optimizing anti-infective therapy in these vulnerable populations.
Model-informed drug development and precision dosing strategies offer promising avenues for individualizing anti-infective therapy in special populations. By integrating population pharmacokinetic modeling, disease progression modeling, and clinical trial simulation, researchers can optimize dosing regimens across the spectrum of organ function, ultimately improving therapeutic outcomes while minimizing toxicity. As the field advances, the continued refinement of these approaches will be crucial for addressing the evolving challenges of antimicrobial resistance and improving care for patients with complex medical conditions.
Guiding Therapeutic Drug Monitoring (TDM) with Model-Informed Precision Dosing
Model-Informed Precision Dosing (MIPD) represents a paradigm shift in therapeutic drug monitoring (TDM), moving from traditional population-based dosing toward highly individualized antimicrobial therapy. Within pharmacometric modeling and anti-infective development, MIPD provides a virtual platform to integrate patient-specific information—including body size, age, genetic background, and disease characteristics—to evaluate clinical scenarios and determine actionable dosing recommendations tailored to individual patient needs [60]. This approach is particularly critical for anti-infectives given the escalating global threat of antimicrobial resistance (AMR), which is projected to cause 10 million deaths annually by 2050 if no effective countermeasures are implemented [34].
The MIPD framework enables the utilization of clinical feedback, such as blood concentrations and biomarkers, to further individualize medications throughout treatment [60]. For anti-infective drugs, this precision approach is essential not only for maximizing therapeutic efficacy but also for minimizing toxicity and preventing the emergence of resistant bacterial strains through precise exposure control at the infection site [34]. The integration of MIPD into antimicrobial TDM represents the cutting edge of pharmacometric applications in infectious diseases, leveraging advanced computational approaches to optimize drug exposure in complex patient populations.
Core Principles of Pharmacokinetics/Pharmacodynamics (PK/PD) in MIPD
Fundamental PK/PD Indices and Targets
The scientific foundation of MIPD rests upon robust pharmacokinetic/pharmacodynamic (PK/PD) principles that define the relationship between drug exposure and antimicrobial effect. Three primary PK/PD indices serve as critical indicators of therapeutic efficacy for anti-infective agents, each relevant to different antibiotic classes [34]:
- %T > MIC: The percentage of time that drug concentrations remain above the minimum inhibitory concentration (MIC) during a dosing interval
- AUC/MIC: The ratio of the 24-hour area under the concentration-time curve to the MIC
- Cmax/MIC: The ratio of the maximum drug concentration to the MIC
These indices vary significantly among antimicrobial classes, informing both empirical dosing strategies and MIPD-based individualization. Beyond traditional efficacy targets, the mutant prevention concentration (MPC) has emerged as a crucial threshold for suppressing resistant subpopulations. The concentration range between MIC and MPC defines the mutant selection window (MSW), where resistant bacterial mutants are most likely to be selected [34]. In managing AMR infections, the focus increasingly shifts from MIC-based to MPC-based indices to ensure optimal therapeutic outcomes while mitigating resistance development.
Advanced Pharmacodynamic Concepts
Several sophisticated PD concepts are integral to MIPD for anti-infectives, including the post-antibiotic effect (PAE), where bacterial growth remains suppressed even after antibiotic removal [32]. This phenomenon is particularly pronounced for antibiotics that inhibit protein and nucleic acid synthesis, such as aminoglycosides and fluoroquinolones [32]. The PAE permits extended dosing intervals while maintaining therapeutic efficacy, a consideration directly incorporated into MIPD simulations.
For bactericidal antibiotics, the minimum bactericidal concentration (MBC) represents the lowest concentration reducing pathogen count by ≥99.9% [32]. When the MBC/MIC ratio reaches 32 or higher, a phenomenon termed "tolerance" occurs, significantly impacting bactericidal efficacy [32]. MIPD approaches must account for such phenotypic variations in bacterial response to optimize dosing regimens against tolerant strains, particularly in immunocompromised patients.
Table 1: Key PK/PD Parameters for Anti-Infective MIPD
| Parameter | Definition | Clinical Significance in MIPD |
|---|---|---|
| MIC | Minimum inhibitory concentration | Lowest concentration inhibiting visible bacterial growth; primary efficacy benchmark |
| MPC | Mutant prevention concentration | Threshold preventing selective enrichment of resistant mutants |
| MSW | Mutant selection window | Concentration range between MIC and MPC where resistance emergence is favored |
| AUC/MIC | Area under curve to MIC ratio | Primary efficacy index for concentration-dependent antibiotics |
| %T > MIC | Time above MIC | Primary efficacy index for time-dependent antibiotics |
| PAE | Post-antibiotic effect | Persistent suppression of bacterial growth after antibiotic removal |
| MBC | Minimum bactericidal concentration | Concentration reducing bacterial inoculum by ≥99.9% |
Computational Frameworks for MIPD
Modeling Approaches in MIPD
MIPD leverages several complementary modeling methodologies to predict drug exposure and optimize dosing regimens [34]:
- Population PK (PopPK) Modeling: A "top-down" approach that characterizes drug disposition variability within target populations using nonlinear mixed-effects modeling
- Physiologically-Based PK (PBPK) Modeling: A "bottom-up" technique describing drug behavior based on drug-specific physicochemical properties and patient physiology
- Hybrid Modeling: Approaches combining population PK and PBPK methodologies for enhanced predictive performance
These modeling frameworks enable the prediction of drug exposure at the infection site, a critical advancement over traditional plasma concentration monitoring. For instance, recent research initiatives focus on developing PBPK models to characterize central nervous system (CNS) distribution of antibiotics with varying physicochemical properties, addressing the therapeutic challenge of nosocomial cerebro-meningeal infections in ICU patients [61].
Emerging Technologies in MIPD Implementation
The implementation of MIPD in clinical practice is being accelerated through several technological innovations [60] [34]:
- Artificial Intelligence and Machine Learning: Leveraging AI/ML approaches to support therapeutic optimization based on prediction of drug exposure, adverse reactions, and clinical outcomes by integrating real-world clinical data
- EHR-Integrated Clinical Decision Support: Developing user-friendly software integrated into electronic health record systems to disseminate model-informed precision dosing at the bedside
- Bayesian Estimation Platforms: Utilizing Bayesian algorithms to combine population priors with individual patient data for real-time dose optimization
These technologies are overcoming historical barriers to MIPD implementation, including computational complexity and limited clinical workflow integration. The ongoing development of machine learning models trained on data produced by Monte Carlo simulations generated from various population PK models represents a particularly promising frontier [61].
Diagram 1: MIPD Clinical Implementation Workflow. This workflow illustrates the integration of patient factors, modeling approaches, and TDM data to generate precision dosing recommendations.
MIPD Application in Special Populations
Pediatric Precision Dosing
Pediatric patients present unique challenges for MIPD implementation due to developmental changes affecting drug pharmacokinetics across the pediatric age spectrum [62]. Dosing recommendations are often split into categories accounting for different stages of child development as proxies for organ function maturation [62]. Recent comparisons of European pediatric formularies have revealed that while the majority of anti-infective dosing recommendations are consistent, significant variations exist in approximately 30-40% of cases, highlighting the need for MIPD approaches in this population [62].
In neonates, developmental pharmacology must account for gestational age, birth weight, and postnatal age, each significantly impacting drug disposition [34]. For instance, vancomycin—a hydrophilic drug—may not achieve sufficient trough concentrations after initial empirical dosing in neonates due to their high body water content increasing the volume of distribution [34]. Similarly, increases in volume of distribution have been reported for lipophilic drugs including fluoroquinolones, rifampicin, and linezolid, likely attributable to larger lipid-rich organs relative to body weight [34].
Complex Adult Populations
MIPD applications are particularly valuable in complex adult populations with altered PK profiles [34]:
- Elderly Patients: Age-related declines in renal and hepatic function can lead to prolonged drug half-life and increased toxicity risk
- Obese Patients: Physiological changes from obesity significantly impact antimicrobial PK, often requiring regimen modifications
- Critically Ill Patients: Pathophysiological changes in ICU patients, including organ dysfunction and fluid shifts, dramatically alter drug exposure
For example, population PK studies have demonstrated significant age-related differences in piperacillin clearance: healthy young adults (mean age 25.1 years) show clearance of 11.9 L/h, while elderly pneumonia patients over 75 years (mean age 86.5 years) demonstrate substantially reduced clearance of only 4.6 L/h [34]. These findings underscore the critical importance of MIPD in special populations with altered drug disposition.
Table 2: MIPD Considerations for Special Populations
| Population | Key PK Alterations | MIPD Application Examples |
|---|---|---|
| Pediatric | Maturing clearance mechanisms;Changing volume of distribution | Age- and weight-based dosing;PBPK modeling of development |
| Elderly | Reduced renal/hepatic function;Altered body composition | Renal function-based dosing;Reduced frequency regimens |
| Obese | Increased volume of distribution;Altered clearance | Weight-based dosing algorithms;Lean body weight considerations |
| Critically Ill | Organ dysfunction;Fluid shifts;Capillary leak | Therapeutic drug monitoring;Adaptive dosing strategies |
Experimental Protocols for MIPD Development
Protocol 1: Population PK Model Development
Objective: To develop a population pharmacokinetic model for characterizing variability in drug exposure and identifying significant covariates influencing PK parameters.
Materials and Methods:
- Patient Data Collection: Retrospective or prospective collection of demographic, clinical, and concentration-time data from patients receiving the target anti-infective
- Bioanalytical Methods: Validated chromatographic (LC-MS/MS) or immunoassay methods for drug concentration quantification [63]
- Software Tools: Nonlinear mixed-effects modeling software (NONMEM, Monolix, Phoenix NLME)
- Model Development:
- Develop structural PK model (1-, 2-, or 3-compartment)
- Identify and quantify interindividual variability
- Identify and quantify residual unexplained variability
- Covariate model building using stepwise forward inclusion/backward elimination
- Model Validation: Internal validation (bootstrap, visual predictive check) and external validation if possible
This protocol enables the quantification of PK variability and identification of patient factors significantly impacting drug exposure, forming the foundation for MIPD algorithms.
Protocol 2: Hollow Fiber Infection Model (HFIM) for PK/PD
Objective: To characterize the exposure-response relationship of anti-infectives against target pathogens and identify PK/PD indices correlating with efficacy and resistance suppression.
Materials and Methods:
- Bacterial Strains: Reference and clinical isolates with relevant resistance mechanisms
- Culture System: Hollow fiber bioreactor with semi-permeable membranes maintaining bacteria in the extracapillary space [32]
- Antibiotic Administration: Simulated human PK profiles in the central reservoir mimicking human dosing regimens
- Experimental Procedures:
- Inoculate HFIM system with target pathogen (~10⁶ CFU/mL)
- Administer antibiotic regimens simulating human PK profiles
- Sample at predetermined time points for:
- Bacterial density determination (CFU counts)
- Resistance emergence assessment (population analysis profiles)
- Antibiotic concentration quantification
- Continue experiments for 7-10 days to monitor resistance development
- Data Analysis: Link PK data with PD response using mathematical modeling (e.g., Emax models) to identify PK/PD targets
The HFIM system provides a dynamic in vitro model that closely mimics in vivo conditions, allowing for the study of bacterial responses to antibiotic exposure over time [32]. This approach is particularly valuable for evaluating resistance emergence and establishing PK/PD targets for resistance suppression.
MIPD Implementation Protocol for Anti-Infective TDM
Clinical Implementation Workflow
Objective: To provide a step-by-step protocol for implementing MIPD in clinical practice for anti-infective TDM.
Materials and Reagents:
- Bioanalytical Equipment: LC-MS/MS system or validated immunoassay for drug concentration measurement
- Software Platforms: MIPD software (e.g., TDMx, InsightRX, DoseMe) or custom Bayesian estimation algorithms
- Population PK Models: Previously developed and validated models for target anti-infectives
- Clinical Data: Patient demographics, serum creatinine, hepatic function tests, clinical status
Procedural Steps:
- Patient Assessment: Collect relevant patient characteristics (age, weight, height, serum creatinine, organ function, clinical status)
- Initial Dosing: Select initial regimen based on population guidelines or institutional protocols
- Blood Sampling: Collect samples at clinically appropriate times (trough, peak, or random timing with accurate documentation)
- Concentration Analysis: Quantify drug concentrations using validated analytical methods
- Model Application: Input patient data and concentration results into MIPD platform
- Regimen Optimization: Generate individualized dosing regimen to achieve target PK/PD exposure
- Therapeutic Monitoring: Repeat TDM as clinically indicated based on changing patient status
Interpretation and Decision Rules:
- For time-dependent antibiotics (β-lactams): Target %fT > MIC of 60-100% or %fT > 4xMIC of 50-70% for critically ill patients
- For concentration-dependent antibiotics (aminoglycosides): Target AUC/MIC ratios or Cmax/MIC ratios based on pathogen and infection site
- For vancomycin: Target AUC₂₄/MIC ratio of 400-600 for MRSA infections
This implementation protocol enables the translation of MIPD from research to clinical practice, facilitating personalized antimicrobial therapy across diverse patient populations and healthcare settings.
Diagram 2: Clinical MIPD Implementation Protocol. This protocol outlines the sequential steps for implementing MIPD in clinical practice, with feedback loops for regimen adaptation.
Essential Research Reagents and Computational Tools
Table 3: Essential Research Toolkit for MIPD Implementation
| Tool Category | Specific Tools/Reagents | Function in MIPD |
|---|---|---|
| Bioanalytical Equipment | LC-MS/MS systems;Immunoassay platforms;HPLC-UV systems | Quantitative drug concentration measurement for TDM and model validation |
| Software Platforms | NONMEM;Monolix;R with nlmixr;Phoenix NLME | Population PK model development and parameter estimation |
| MIPD Applications | TDMx;InsightRX;DoseMe;BestDose | Clinical decision support for model-informed precision dosing |
| PBPK Software | GastroPlus;Simcyp Simulator;PK-Sim | Physiologically-based pharmacokinetic modeling and simulation |
| Experimental Systems | Hollow fiber infection models (HFIM);Static time-kill assays;Chemostat systems | In vitro assessment of exposure-response relationships and resistance emergence |
| Data Management | R;Python;Electronic health record systems | Data analysis, visualization, and clinical implementation |
Model-Informed Precision Dosing represents a transformative approach to therapeutic drug monitoring of anti-infectives, integrating pharmacometric modeling with patient-specific data to optimize antimicrobial therapy. The frameworks and protocols outlined in this document provide a roadmap for implementing MIPD in both research and clinical settings, with particular relevance to pharmacometric modeling in anti-infective development. As antimicrobial resistance continues to escalate globally, these advanced approaches to dose individualization will play an increasingly critical role in preserving the efficacy of existing anti-infectives while minimizing toxicity and suppressing resistance emergence. The ongoing integration of artificial intelligence, machine learning, and EHR-embedded clinical decision support promises to further enhance the accessibility and implementation of MIPD across diverse healthcare settings.
Optimizing Dosing for Combination Therapies and Against Multi-Drug Resistant Pathogens
The rising prevalence of multi-drug resistant (MDR) pathogens and the complexity of combination therapies represent two critical challenges in modern therapeutics. Pharmacometric modeling and simulation provide powerful computational frameworks to address these challenges by quantitatively integrating pharmacokinetic (PK), pharmacodynamic (PD), and pathogen or disease progression data. For anti-infective development, these approaches enable rational optimization of dosing regimens for combination therapies against MDR pathogens, where traditional trial-and-error methods are often inefficient and clinically impractical [1] [64].
Model-Informed Drug Development (MIDD) has emerged as a transformative framework recognized by regulatory authorities, including the International Council for Harmonisation (ICH) M15 guidelines [1]. MIDD employs quantitative models to integrate nonclinical and clinical data, supporting more efficient drug development and regulatory decision-making. This application note outlines specific protocols and methodologies for applying pharmacometric approaches to optimize dosing strategies for combination therapies against MDR pathogens, with particular emphasis on Gram-negative bacteria identified as critical priorities by the World Health Organization [64] [65].
Computational Frameworks for Combination Therapy Optimization
Pharmacometric Modeling Approaches
Table 1: Pharmacometric Modeling Approaches for Combination Therapy Optimization
| Model Type | Key Application | Data Requirements | Software Tools |
|---|---|---|---|
| Population PK/PD (PopPK/PD) | Characterize dose-exposure-response relationships accounting for inter-patient variability | Serial PK samples; PD biomarkers; clinical outcomes | NONMEM, Monolix, R (mrgsolve) |
| Quantitative Systems Pharmacology (QSP) | Model networked biological systems and drug effects on pathways | Pathway information; drug-target binding; system parameters | MATLAB, SimBiology, R |
| Feedback System Control (FSC) | Phenotypically-driven optimization without requiring mechanistic knowledge | High-throughput drug combination screening data | Custom algorithms (e.g., Differential Evolution) |
| Multi-type Branching Process | Model resistance emergence in heterogeneous cell populations | Cell proliferation/death rates; mutation frequencies | ACESO R package |
Several advanced computational frameworks have been developed specifically for optimizing combination therapies. The ACESO (A Cancer Evolution Schedule Optimizer) R package implements a multi-type branching process with time-dependent rates to model how heterogeneous cell populations evolve under therapeutic pressure [66]. This approach incorporates pharmacokinetic profiles and drug interaction effects to identify administration schedules that minimize resistance emergence. The model structure includes sensitive type-0 cells that acquire resistance mutations at rate uᵢbᵢ(t) per cell division to generate resistant type-i cells, each with birth and death rates (bᵢ(t) and dᵢ(t)) that may exhibit concentration-dependent profiles [66].
For anti-infective applications, Feedback System Control (FSC) with population-based stochastic search algorithms enables efficient navigation through large parametric spaces of drug combinations. This iterative approach involves experimental testing followed by algorithm-based analysis to rapidly identify synergistic low-dose drug combinations. The method has successfully optimized angiostatic drug combinations containing erlotinib, BEZ-235, and RAPTA-C, demonstrating enhanced efficacy with reduced doses in preclinical models [67].
Protocol: Implementing a Pharmacometric Workflow for Combination Therapy Optimization
Objective: To establish a standardized protocol for developing and qualifying a pharmacometric model to optimize dosing regimens for combination therapies against MDR pathogens.
Materials and Software Requirements:
- R statistical software with mrgsolve package for PK/PD simulation [66]
- NONMEM or alternative population modeling software
- High-throughput screening data for individual drugs and combinations
- Pathogen susceptibility profiles (MIC distributions)
- Patient demographic and clinical characteristic data
Experimental Workflow:
Step 1: Structural Model Identification
- Conduct in vitro time-kill studies for individual drugs and combinations across clinically relevant concentration ranges
- Fit candidate PK models to concentration-time data using maximum likelihood or Bayesian methods
- Test various PD models (Emax, sigmoidal Emax, logistic) to characterize exposure-response relationships
Step 2: Covariate Model Development
- Collect patient factors (age, renal/hepatic function, comorbidities) that may influence PK/PD
- Implement stepwise covariate model building with statistical criteria (p<0.01 for forward inclusion, p<0.001 for backward elimination)
- Evaluate covariate-parameter relationships using visual predictive checks and goodness-of-fit plots
Step 3: Drug Interaction Characterization
- Quantify drug interactions using Bliss Independence or Loewe Additivity models [68]
- For Bliss Independence: S = EA+B − (EA + EB), where S>0 indicates synergy
- Incorporate interaction parameters into the combined PD model structure
Step 4: Model Qualification and Validation
- Perform visual predictive checks using 1000 simulated datasets
- Conduct bootstrap analysis (n=1000) to evaluate parameter precision
- Calculate prediction-corrected metrics for model performance evaluation
Step 5: Clinical Trial Simulation
- Simulate candidate dosing regimens in virtual populations representing target patient groups
- Evaluate probability of target attainment for various pharmacodynamic indices (AUC/MIC, Cmax/MIC, T>MIC)
- Optimize regimens to maximize therapeutic response while minimizing resistance amplification
Figure 1: Pharmacometric Model Development Workflow. QOI: Question of Interest; COU: Context of Use.
Application to Multi-Drug Resistant Gram-Negative Pathogens
Current Landscape of MDR Gram-Negative Infections
The treatment of MDR Gram-negative pathogens represents one of the most pressing challenges in anti-infective therapy. The Infectious Diseases Society of America (IDSA) 2024 guidance highlights the critical threat posed by carbapenem-resistant Enterobacterales (CRE), Pseudomonas aeruginosa with difficult-to-treat resistance (DTR P. aeruginosa), and carbapenem-resistant Acinetobacter baumannii (CRAB) [69]. These pathogens have been designated as critical priorities by the WHO due to their significant morbidity, mortality, and limited treatment options.
Gram-negative bacteria employ multiple resistance mechanisms, including drug inactivation by enzymes (e.g., β-lactamases), target alteration, metabolic pathway modification, and drug efflux pumps [65]. The complex cell envelope structure of Gram-negative bacteria, with its outer membrane and lipopolysaccharide layer, presents a particular challenge for antibiotic penetration and efficacy.
Table 2: Preferred Treatment Regimens for MDR Gram-Negative Pathogens (per IDSA 2024 Guidance)
| Pathogen | Infection Type | Preferred Regimens | Alternative Options | Pharmacometric Considerations |
|---|---|---|---|---|
| CRE | Invasive infections | Ceftazidime-avibactam + Aztreonam (for MBL producers) | Polymyxins, Tigecycline, Aminoglycosides | Simultaneous q8h dosing to facilitate coordination; prolonged infusions for β-lactams |
| CRAB | Various infections | Sulbactam-durlobactam + Meropenem or Imipenem | High-dose Ampicillin-sulbactam (27g daily) + additional agent | Combination therapy essential to prevent resistance |
| DTR P. aeruginosa | Pyelonephritis/cUTI | Traditional β-lactams (if susceptible) as high-dose extended infusion | Once-daily Tobramycin or Amikacin | Optimized dosing based on local susceptibility patterns |
| ESBL-E | Complicated UTIs | Cefiderocol (preserved for DTR P. aeruginosa) | Cefepime if MIC ≤ 2 µg/mL | Avoid piperacillin-tazobactam due to increased risk of failure |
Protocol: Optimizing Combination Regimens for CRAB Infections
Objective: To develop an optimized dosing strategy for sulbactam-durlobactam in combination with a carbapenem for the treatment of CRAB infections, accounting for resistance suppression and PK/PD target attainment.
Background: CRAB exhibits extensive drug resistance mechanisms, including enzymatic degradation, efflux pumps, and target site modifications. Combination therapy is essential to enhance bacterial killing and suppress resistance emergence [69] [65].
Experimental Design:
Step 1: In Vitro Time-Kill Studies
- Prepare bacterial inoculum of CRAB clinical isolates at ~10⁶ CFU/mL
- Test sulbactam-durlobactam alone and in combination with meropenem across concentration gradients
- Sample at 0, 2, 4, 8, and 24 hours for quantitative culture
- Define synergy as ≥2-log₁₀ CFU/mL reduction compared to the most active single agent
Step 2: Resistance Prevention Studies
- Conduct serial passage experiments over 5 days at sub-inhibitory concentrations
- Determine mutant prevention concentration (MPC) for individual drugs and combinations
- Calculate mutant selection window (MSW) to identify dosing strategies that restrict resistant mutant amplification
Step 3: Population PK Model Development
- Collect plasma concentration-time data from phase 1-3 clinical trials
- Develop a two-compartment population PK model with between-subject variability on clearance and volume parameters
- Identify covariates (renal function, body size) influencing PK variability
Step 4: PK/PD Target Identification
- Determine the PK/PD index (AUC/MIC, %T>MIC) most predictive of efficacy
- Establish PK/PD target values for stasis and 1-log kill using in vitro and in vivo data
- Identify PK/PD thresholds for resistance suppression
Step 5: Monte Carlo Simulations
- Simulate 10,000 virtual patients receiving candidate regimens
- Calculate probability of target attainment (PTA) for each regimen
- Determine cumulative fraction of response (CFR) against CRAB populations
- Recommend optimal dosing based on PTA ≥90% and CFR ≥90%
Figure 2: CRAB Combination Therapy Optimization Protocol
Advanced Applications: Digital Twins and Adaptive Dosing
The integration of pharmacometric approaches with digital twin technology represents a cutting-edge application in optimizing combination therapies. A recent study demonstrated a refined quantitative systems pharmacology model of cancer-angiogenesis crosstalk that served as a digital twin for personalizing combination therapy administration timing [47]. This approach enabled the development of adaptive regimens scheduled by monitoring vessel normalization windows, using tumor microenvironment biomarkers predictive of treatment outcome.
In the context of anti-infective therapy, similar digital twin approaches can be applied to optimize dosing of combination regimens against MDR pathogens. By creating virtual patient representations that incorporate pathogen-specific characteristics, host immune responses, and drug properties, clinicians can simulate various combination strategies and identify patient-specific optimal regimens.
Protocol: Implementing a Digital Twin Framework for Adaptive Dosing
Objective: To develop a digital twin framework for adaptive dosing of combination antibiotics in individual patients with MDR infections.
Methodology:
Step 1: Virtual Patient Model Development
- Create a library of virtual patients representing population variability in PK parameters
- Incorporate pathogen-specific PD parameters based on MIC distributions
- Include models of host immune function and disease progression
Step 2: Bayesian Forecasting for Individualization
- Collect sparse therapeutic drug monitoring data from the patient
- Use Bayesian estimation to derive patient-specific PK parameters
- Update the digital twin with individual parameter estimates
Step 3: Adaptive Dosing Optimization
- Simulate various dosing regimens in the updated digital twin
- Identify regimens that optimize target attainment while minimizing toxicity
- Implement the optimized regimen in the actual patient
Step 4: Continuous Feedback and Model Refinement
- Monitor clinical response and drug concentrations
- Refine the digital twin based on ongoing patient data
- Adjust dosing as needed based on changing patient status
Table 3: Key Research Reagent Solutions for Combination Therapy Studies
| Reagent/Resource | Function | Application Examples | Key Features |
|---|---|---|---|
| ACESO R Package | Optimizes combination treatment scheduling using evolutionary modeling | Identifying administration schedules that minimize resistance in cancer therapy | Incorporates PK profiles, flexible drug interaction models [66] |
| mrgsolve R Package | Rapid simulation of ODE-based PK models | Implementing complex PK models with different routes of administration | Flexible model specification, efficient simulation [66] |
| Differential Evolution Algorithm | Population-based stochastic search algorithm | Navigating large parametric spaces of drug combinations in FSC | Global optimization, handles non-linear responses [67] |
| Bliss Independence Model | Quantifies drug synergy/antagonism | Evaluating combination effects in high-throughput screens | Simple calculation: S = EA+B - (EA + EB) [68] |
| Ceftazidime-Avibactam + Aztreonam | Combination against MBL-producing CRE | Treating NDM, VIM, IMP carbapenemase-producing infections | Simultaneous q8h administration recommended [69] |
| Sulbactam-Durlobactam | Targeted therapy for CRAB infections | Treatment of carbapenem-resistant Acinetobacter baumannii | Used in combination with carbapenems [69] |
Pharmacometric modeling and simulation provide powerful methodologies for optimizing dosing strategies for combination therapies against multi-drug resistant pathogens. The protocols outlined in this application note demonstrate systematic approaches to address the complex challenges posed by MDR Gram-negative infections, with particular relevance to CRE, CRAB, and DTR P. aeruginosa. By integrating in vitro data, population PK/PD modeling, and clinical trial simulation, researchers can identify optimized combination regimens that maximize efficacy while minimizing resistance emergence.
The field continues to evolve with emerging technologies such as digital twins and artificial intelligence approaches offering new opportunities for personalizing combination therapy. As noted in the ICH M15 guidelines on MIDD, these model-informed approaches are increasingly recognized by regulatory agencies as valid strategies for supporting drug development and approval [1]. The ongoing challenge of antimicrobial resistance necessitates continued refinement and application of these pharmacometric approaches to ensure optimal use of existing agents and guide development of novel therapeutic strategies.
Model-Informed Drug Development (MIDD) leverages quantitative methods to streamline drug development and regulatory decision-making. Within the pharmacometrics toolkit, Physiologically-Based Pharmacokinetic (PBPK) modeling has emerged as a powerful mechanistic tool to predict drug absorption, distribution, metabolism, and excretion (ADME) by integrating drug-specific properties with population-specific physiological parameters [70] [71]. Unlike traditional data-driven pharmacokinetic models, PBPK models employ a "middle-out" approach, combining bottom-up prediction from in vitro data with top-down verification using available in vivo data [72]. This capability is particularly valuable for simulating drug exposure in special populations, such as pediatrics, the elderly, and patients with organ dysfunction, where clinical trials are often ethically and practically challenging [73] [74]. This article details the application and protocols for using PBPK modeling to optimize anti-infective therapies in these populations, providing a critical component to a broader thesis on pharmacometric modeling in anti-infective development.
Core Concepts and Value of PBPK Modeling
The PBPK Framework and Its Advantages
PBPK models consist of a series of anatomical compartments representing key organs and tissues, interconnected by the circulatory system. The models are parameterized using:
- Drug-dependent parameters: Physicochemical properties (e.g., lipophilicity, molecular weight, pKa) and in vitro data (e.g., permeability, metabolic clearance) [71] [72].
- System-dependent parameters: Physiological information (e.g., organ volumes and blood flows, tissue composition, enzyme/transporter abundance) specific to a population or disease state [71] [72].
A major paradigm shift enabling the modern resurgence of PBPK modeling has been the integration of In Vitro-In Vivo Extrapolation (IVIVE). IVIVE allows for the separation of drug properties from system parameters, facilitating "bottom-up" prediction of human pharmacokinetics from preclinical data and the extrapolation of drug behavior to untested clinical scenarios [70]. This represents a move from a conventional "learn-confirm" cycle to a more powerful "predict-learn-confirm-apply" cycle in drug development [70].
Key Applications in Special Populations and Anti-infective Development
For special populations, PBPK models are used to simulate the impact of age- or disease-related physiological changes on drug PK, thereby informing dose selection and optimization without resorting to extensive clinical testing [73] [71] [74]. In the context of anti-infective development, pharmacometric approaches are invaluable for determining the appropriate dosage regimen to achieve pharmacokinetic/pharmacodynamic (PK/PD) targets linked to efficacy, such as the time that drug concentration exceeds the minimum inhibitory concentration (T>MIC) for antibiotics [8]. PBPK modeling enhances this by providing robust, mechanistic predictions of drug exposure at the site of infection (e.g., epithelial lining fluid, prostate) in these vulnerable patient groups [8].
Application in Pediatric and Geriatric Populations
Physiological Changes and PBPK Modeling Strategies
The physiological parameters governing drug ADME undergo significant changes from preterm neonates to the oldest elderly patients. Table 1 summarizes the key age-dependent physiological changes and the corresponding PBPK modeling strategies for pediatrics and geriatrics.
Table 1: Age-Dependent Physiological Changes and PBPK Modeling Strategies
| Physiological Parameter | Change in Pediatrics | Change in Geriatrics | PBPK Modeling Strategy |
|---|---|---|---|
| Organ Volumes (e.g., Liver, Kidney) | Increases with growth and development [73] | Decreases (e.g., liver volume ~70% in 90s vs. 20s) [73] | Use of population-specific equations to scale organ sizes [73] [74] |
| Organ Blood Flow (e.g., Hepatic, Renal) | Increases with cardiac output [73] | Decreases (e.g., liver blood flow ~57% in 90s vs. 20s) [73] | Adjustment of cardiac output and fractional blood flows [73] [74] |
| Enzyme Activity (e.g., CYP3A4) | Maturational change from low activity at birth [73] | Conflicting data; may decline in advanced age [73] [74] | Incorporation of ontogeny functions for pediatrics; sensitivity analysis for geriatrics [73] [74] |
| Renal Function (GFR) | Maturational increase after birth [73] | Linear decline with age [73] [74] | Use of age-appropriate GFR estimation equations [73] [74] |
| Body Composition (Adipose, Lean Mass) | Variable changes with developmental stage [73] | Increased adipose, decreased lean body mass [74] | Adjustment of tissue volumes and composition to predict Vd [74] |
| Gastric pH & Motility | Higher, less acidic at birth; matures postnatally [73] | Conflicting reports on gastric emptying [74] | Application of age-dependent pH profiles; often assumes adult absorption in elderly [73] [74] |
Case Studies and Quantitative Predictions
Pediatrics: A 2025 study developed a dynamic age-dependent PBPK model for CYP3A4-metabolized drugs (midazolam, fentanyl, alfentanil, sufentanil). The model, validated in adults, was extrapolated to pediatrics by replacing physiological and pharmacokinetic parameters. The predicted AUC~0–t~ and C~max~ for these drugs in children were within 0.5 to 2 times the observed values, demonstrating high predictive accuracy and enabling dose optimization [73].
Geriatrics: The same study successfully predicted the increased exposure to midazolam in elderly populations, facilitating visualization of dose transitions from adults to geriatrics [73]. Furthermore, a 2024 analysis highlighted the use of PBPK models to simulate drug exposure in older adults, even with comorbidities like renal or hepatic impairment, though it noted knowledge gaps regarding transporter function changes and ethnic diversity in existing virtual populations [74].
Application in Organ Dysfunction
Modeling Hepatic and Renal Impairment
Organ dysfunction, particularly of the liver and kidneys, significantly alters drug clearance. PBPK models can incorporate disease-specific physiological changes to predict these effects.
- Renal Impairment (RI): Models account for the reduced glomerular filtration rate (GFR) and its impact on the clearance of renally excreted drugs. Advanced models may also include the dysfunction of specific renal transporters. For example, a PBPK model for rivaroxaban incorporated the disproportionate deterioration of hOAT3-mediated secretion compared to GFR during RI [74].
- Hepatic Impairment (HI): Changes in liver blood flow, liver volume, and metabolic capacity can be integrated into the model. Virtual populations with HI can be generated from healthy population models by adjusting parameters corresponding to the severity of impairment [74].
Integrated Workflow for Complex Cases
Geriatric patients often present with multiple comorbidities, leading to complex disease-drug-drug interactions (D-DDIs). A robust workflow for modeling these patients involves:
- Starting with a virtual healthy geriatric population.
- Superimposing disease-specific pathophysiological changes (e.g., for RI or HI).
- Incorporating known drug-drug interactions.
- Refining the model using available clinical data, including those from population PK (popPK) analyses, to identify key covariates of variability [74].
Experimental Protocols for PBPK Model Development and Application
General Workflow for Developing a Dynamic Age-Dependent PBPK Model
The following protocol, adapted from a study on CYP3A4-metabolized drugs, outlines the key steps for building a PBPK model for special populations [73].
Objective: To develop and qualify a PBPK model for predicting drug pharmacokinetics across the human age range (preterm neonates to elderly). Drugs: Anti-infectives or other drugs with known disposition pathways. Software: PBPK platforms (e.g., Simcyp, GastroPlus, PK-Sim).
Procedure:
- Model Architecture Definition: Define a multi-compartment model (e.g., stomach, intestine, liver, kidney, muscle, adipose) connected by the circulatory system.
- Data Collection:
- System Parameters: Gather population-specific anatomical and physiological data (organ volumes, blood flows, GFR, enzyme ontogeny) from integrated databases or literature.
- Drug Parameters: Input drug-specific physicochemical properties (molecular weight, logP, pKa) and in vitro data (solubility, permeability, plasma protein binding, CL~int~ from hepatocyte or microsomal assays).
- Model Building and Verification in Adults:
- Develop the model using data from healthy young adults.
- Simulate clinical PK studies and compare predictions (e.g., plasma concentration-time profile, AUC, C~max~) against observed data.
- Qualify the model by ensuring key metrics fall within pre-defined acceptance criteria (e.g., predicted/observed ratios for AUC and C~max~ between 0.5-2.0) [73].
- Model Extrapolation to Special Populations:
- Replace the system parameters in the verified adult model with those of the target special population (pediatric, geriatric, or organ impairment).
- For pediatrics, incorporate validated ontogeny profiles for relevant enzymes and transporters.
- For organ dysfunction, adjust parameters like GFR or liver function according to disease severity.
- Simulation and Validation:
- Run simulations in the virtual special population (e.g., n=1000 virtual individuals) to predict PK parameters and dose-exposure relationships.
- Compare simulation outcomes with any available clinical data in that population for external validation.
- Dose Optimization:
- Use the validated model to simulate various dosing regimens.
- Identify the regimen that achieves drug exposure (e.g., AUC) comparable to the safe and effective exposure in healthy adults or that meets a predefined PK/PD target (e.g., T>MIC).
Figure 1: Workflow for PBPK model development and application in special populations.
Protocol for Predicting Drug-Drug Interactions (DDIs) in Special Populations
PBPK modeling is extensively used for DDI prediction, which is critical for polypharmacy patients, especially the elderly [74] [75].
Objective: To predict the magnitude of DDI when an anti-infective (object drug) is co-administered with another drug (perpetrator). Software: PBPK platforms with DDI modules (e.g., Simcyp).
Procedure:
- Develop and Verify the Perpetrator Model:
- Build a PBPK model for the perpetrator drug (e.g., itraconazole, a CYP3A4 inhibitor) using its physicochemical and in vitro data.
- Verify the model's ability to predict its own PK and the magnitude of its inhibition against a sensitive index substrate (e.g., midazolam).
- Develop and Verify the Object Drug Model:
- Build and verify the PBPK model for the anti-infective drug (object drug) as described in Protocol 5.1.
- DDI Simulation:
- Simulate the co-administration of the object and perpetrator drugs in a virtual population.
- The platform will mechanistically simulate the inhibition (or induction) process, altering the clearance of the object drug.
- DDI Analysis:
- Calculate the geometric mean ratio of the object drug's AUC and C~max~ with and without the co-administered perpetrator.
- Classify the DDI risk based on the calculated ratios and recommend dose adjustments or clinical monitoring as needed [75].
The Scientist's Toolkit: Essential Reagents and Software
Table 2: Key Research Reagent Solutions and Software for PBPK Modeling
| Item / Resource | Function / Application | Relevance to PBPK Modeling |
|---|---|---|
| Simcyp Simulator (Certara) | A PBPK software platform with built-in virtual populations. | Features libraries for pediatric, geriatric, and organ impairment populations; used for DDI and PK prediction in special populations [74]. |
| GastroPlus (Simulations Plus) | A PBPK software focusing on absorption and PK/PD modeling. | Used for mechanistic modeling of oral absorption, formulation design, and prediction of drug exposure in different populations [72]. |
| PK-Sim (Open Systems Pharmacology) | An open-source whole-body PBPK modeling platform. | Enables cross-species extrapolation and includes a database for generating virtual European and geriatric populations [74]. |
| Human Liver Microsomes / Hepatocytes | In vitro system to study drug metabolism. | Used to obtain experimental data for intrinsic clearance (CL~int~), which is extrapolated via IVIVE to inform in vivo hepatic clearance in the model [73] [72]. |
| Caco-2 Cell Assay | In vitro model of the human intestinal mucosa. | Provides data on drug permeability, a critical parameter for predicting oral absorption in the PBPK model [72]. |
| Assays for Plasma Protein Binding | Determines the fraction of drug unbound in plasma (f~u~). | Essential for predicting the volume of distribution and clearance, as only the unbound fraction is considered pharmacologically active [73] [72]. |
PBPK modeling represents a cornerstone of modern pharmacometrics, providing a mechanistic, predictive framework for optimizing drug therapy in special populations. Within anti-infective development, it allows researchers and clinicians to bridge the knowledge gap created by the ethical and practical limitations of conducting clinical trials in pediatrics, the elderly, and patients with organ dysfunction. By leveraging in vitro data and existing clinical knowledge through a "predict-learn-confirm-apply" cycle, PBPK models enable quantitative, evidence-based dose selection and DDI risk assessment, ultimately accelerating the development of safe and effective anti-infective regimens for these vulnerable patients. As the field evolves, addressing current gaps—such as the characterization of transporter ontogeny and the development of more diverse virtual populations—will further enhance the robustness and regulatory acceptance of these powerful models.
Using Models to Define Breakpoints and Combat the Emergence of Resistance
The relentless rise of antimicrobial resistance (AMR) poses a critical threat to global public health, rendering once-effective therapies obsolete. Antimicrobial breakpoints, which are predefined criteria classifying bacterial isolates as susceptible, intermediate, or resistant to a drug, are cornerstone concepts in guiding effective antimicrobial therapy [76]. Traditionally, these breakpoints were established using a limited set of in vitro and clinical data. However, this approach has significant limitations in an era of rapidly evolving resistance mechanisms.
A major challenge in monitoring AMR trends is "breakpoint drift"—where observed increases in resistance rates may stem not only from genuine microbial evolution but also from revisions to the interpretive standards and breakpoints themselves [76]. For instance, an isolate classified as susceptible under older guidelines might be reclassified as resistant under updated criteria, creating the illusion of rapidly spreading resistance without a true biological change in the pathogen population [76]. This phenomenon complicates longitudinal surveillance and can skew public health narratives and responses.
Pharmacometric modeling and simulation offers a powerful, paradigm-shifting approach to this problem. By integrating mathematical models of drug pharmacokinetics (PK, what the body does to the drug) and pharmacodynamics (PD, what the drug does to the body and the pathogen), this discipline provides a mechanistic, quantitative framework for defining more robust and clinically relevant breakpoints and for optimizing dosing strategies to suppress the emergence of resistance [77] [78].
The Breakpoint Challenge and the Pitfalls of Traditional Methods
The Consequence of Evolving Interpretive Criteria
Breakpoints are not static; standards-setting organizations like the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) periodically revise them to incorporate new pharmacokinetic/pharmacodynamic (PK/PD), microbiologic, and clinical data [76]. While scientifically justified, these revisions can profoundly impact reported resistance rates.
Table 1: Impact of Updated CLSI Breakpoints on Zone Diameter Interpretive Criteria (2015 vs. 2025) [76]
| Bacteria | Antimicrobial | CLSI-2015 (S) ≥ | CLSI-2025 (S) ≥ | CLSI-2015 (R) ≤ | CLSI-2025 (R) ≤ |
|---|---|---|---|---|---|
| Enterobacterales | Ciprofloxacin | 21 mm | 26 mm | 15 mm | 21 mm |
| Enterobacterales | Levofloxacin | 17 mm | 21 mm | 13 mm | 16 mm |
| Pseudomonas aeruginosa | Ciprofloxacin | 21 mm | 25 mm | 15 mm | 18 mm |
| Staphylococcus aureus | Ceftaroline | 24 mm | 25 mm | 20 mm | 19 mm |
| Acinetobacter spp. | Ampicillin-sulbactam | 15 mm | 22 mm | 11 mm | 16 mm |
As shown in Table 1, a bacterial isolate with a ciprofloxacin zone diameter of 22 mm would have been categorized as "Susceptible" in 2015 but would be classified as "Resistant" under the 2025 criteria. This reclassification, while improving the clinical predictive value of the test, artificially inflates resistance rates in surveillance reports if not properly accounted for, potentially leading to misguided policy and premature abandonment of older agents [76].
Limitations of the MIC-Centric View
The Minimum Inhibitory Concentration (MIC) is a fundamental PD measurement. However, using a single, static MIC value to define breakpoints ignores the dynamic interplay between the drug concentration time-profile at the infection site (PK) and the time-course of its antibacterial effect (PD) [77] [78]. The traditional approach often fails to:
- Capture Dynamic Drug-Pathogen Interactions: It does not account for the changing bacterial population, including the emergence of resistant subpopulations during therapy [77].
- Inadequately Inform Combination Therapy: For drug combinations like β-lactam/β-lactamase inhibitors (e.g., ceftazidime/avibactam), traditional methods may not optimally define the exposure target for the inhibitor, potentially leading to suboptimal dosing and treatment failure [77].
The Pharmacometric Solution: Mechanism-Based PK/PD Modeling
Pharmacometric models integrate in vitro and in vivo data to create a unified mathematical representation of the entire system, from drug administration to bacterial killing. This allows for a more sophisticated "model-informed" definition of breakpoints and dosing strategies.
Core PK/PD Concepts and Indices for Efficacy
The antibacterial effect of a drug is best described by one of three PK/PD indices that link the drug's PK to a meaningful PD measure (the MIC) [79]. The specific index depends on the antibiotic's mode of action:
Table 2: Key Pharmacokinetic/Pharmacodynamic (PK/PD) Indices for Antibacterial Efficacy [79]
| PK/PD Index | Definition | Applies To | Typical Target |
|---|---|---|---|
| %fT >MIC | Percentage of the dosing interval that the free (unbound) drug concentration exceeds the MIC. | Time-dependent antibiotics (e.g., β-lactams like meropenem) [80]. | e.g., 40% fT>MIC for bacteriostasis [80]. |
| fAUC/MIC | Ratio of the area under the free concentration-time curve to the MIC. | Concentration-dependent antibiotics (e.g., aminoglycosides, fluoroquinolones) and drugs with mixed activity. | Varies by drug and desired effect (e.g., bacteriostasis vs. eradication). |
| fC~max~/MIC | Ratio of the maximum free drug concentration to the MIC. | Concentration-dependent antibiotics (e.g., aminoglycosides). | Target depends on drug and infection. |
Mechanism-based PK/PD models move beyond these summary indices by mathematically describing the bacterial growth and killing kinetics in response to changing drug concentrations over time. These models can incorporate features like the emergence of pre-existing resistant subpopulations and the phenomenon of bacterial tolerance [77].
The Model-Informed Drug Development (MIDD) Framework
The application of pharmacometrics in drug development is formalized in the Model-Informed Drug Development (MIDD) framework. The International Council for Harmonisation (ICH) M15 guideline defines MIDD as "the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [81] [43]. This framework ensures that models are developed and applied with rigorous planning, evaluation, and documentation, making them suitable for regulatory decision-making, including the support of breakpoint definitions and optimized dosing regimens [81].
Diagram 1: The MIDD workflow for anti-infective development. This process, aligned with ICH M15 guidelines, ensures quantitative models are rigorously developed and applied to inform critical decisions like breakpoint setting and dose optimization [81] [43].
Application Notes & Protocols
Protocol 1: Developing a Mechanism-Based PK/PD Model to Inform Breakpoints
This protocol outlines the steps for building a mechanism-based model from in vitro time-kill data, which can subsequently be used to simulate human dosing regimens and identify PK/PD targets for breakpoint setting [77].
Objective: To characterize the time-course of antibacterial effect and identify the most predictive PK/PD index and target value for a new antibiotic against a resistant pathogen.
Materials & Reagents:
- Bacterial Strain: A well-characterized, β-lactamase-producing, drug-resistant strain (e.g., Klebsiella pneumoniae NCTC 13438) [77].
- Antibiotic Stock Solutions: Prepare fresh solutions according to CLSI guidelines for MIC and time-kill assays.
- Growth Medium: Cation-adjusted Mueller-Hinton Broth (CAMHB).
- Equipment: Automated broth microdilution system, incubator, spectrophotometer for measuring optical density (OD), and viable count plating equipment.
Experimental Procedure:
- Determine Baseline Parameters: Conduct static time-kill studies over 24 hours at multiple antibiotic concentrations (e.g., 0x, 0.5x, 1x, 2x, 4x, 8x MIC). Sample at 0, 2, 4, 6, 8, and 24 hours. Serially dilute and plate samples for viable counting (CFU/mL). This data will characterize the natural growth rate of the bacteria and the concentration-dependent killing rate of the drug.
- Model Building: Use non-linear mixed-effects modeling software (e.g., NONMEM, Monolix, R) to fit a mathematical model to the time-kill data. A typical model structure might include:
- A differential equation for bacterial growth (e.g., logistic growth).
- A term for drug-induced killing (e.g., a maximum killing rate, ( K{max} ), and a concentration to achieve 50% of ( K{max} ), ( KC_{50} )).
- A compartment for a pre-existing resistant subpopulation with reduced drug susceptibility [77].
- Model Validation: Validate the final model by assessing its ability to predict data not used in the model-building process (e.g., from a different strain or a dynamic in vitro model).
Integration and Human Simulation:
- Link to Human PK: Integrate the validated PD model with a population PK (PopPK) model for the antibiotic in humans [77] [79].
- Run Clinical Trial Simulations: Simulate thousands of virtual patients receiving various dosing regimens (e.g., different doses, infusion durations). For each regimen, calculate the traditional PK/PD indices (fT>MIC, fAUC/MIC) and the resultant bacterial density at 24 hours.
- Identify PK/PD Target: Determine which PK/PD index (e.g., fAUC/MIC) best predicts success (e.g., bacteriostasis or 1-log kill) and the magnitude of that target required for a high (>90%) probability of success [77]. This target, combined with population PK variability and the MIC distribution of wild-type and resistant pathogens, forms the quantitative basis for proposing a new, evidence-based breakpoint.
Protocol 2: Optimizing Combination Therapy Dosing Using a PK/PD Model
This protocol is specific to combinations like ceftazidime/avibactam, where the inhibitor (avibactam) has multiple roles [77].
Objective: To determine the optimal dosing ratio and infusion strategy for a β-lactam/β-lactamase inhibitor combination to maximize bacterial killing against resistant strains.
Materials & Reagents: As in Protocol 1, with both the antibiotic (e.g., ceftazidime) and the inhibitor (e.g., avibactam).
Experimental & Modeling Procedure:
- Conduct Combination Time-Kill Studies: Perform time-kill studies with varying concentrations of both the antibiotic and the inhibitor in a factorial design. This is critical to capture their synergistic interaction [77].
- Develop a Mechanism-Based Interaction Model: Build a PD model that explicitly includes the mechanisms of action:
- β-lactam antibiotic: Kills bacteria but is degraded by β-lactamases.
- β-lactamase inhibitor: Inhibits the β-lactamase enzyme (protecting the antibiotic) and may have a direct potentiating or bactericidal effect [77].
- Human Simulations and Optimization: Link the interaction model to PopPK models for both drugs. Simulate clinical scenarios to evaluate different dosing ratios (e.g., 1:1, 2:1, 4:1 ceftazidime:avibactam) and infusion modes (intermittent vs. prolonged infusion). The outcome measure is the probability of attaining a predefined PK/PD target for the combination. A study on ceftazidime/avibactam found that increasing the relative dose of avibactam and using continuous infusion improved the probability of target attainment against Pseudomonas aeruginosa [77].
Diagram 2: The logic flow from PK/PD modeling to breakpoint determination. The integration of population PK, mechanism-based PD, and pathogen MIC data via clinical trial simulations allows for the calculation of PTA, which directly informs the rationale for a new breakpoint.
The Scientist's Toolkit: Essential Reagents and Models
Table 3: Research Reagent Solutions for Pharmacometric Breakpoint Studies
| Item | Function & Application in Breakpoint Research |
|---|---|
| Reference Bacterial Strains | Well-characterized strains with known resistance mechanisms (e.g., KPC-2 producing K. pneumoniae) are essential for validating PD models against relevant phenotypes [77]. |
| In Vitro Pharmacodynamic Models | Such as hollow-fiber infection models, which can simulate human PK profiles in vitro to generate rich time-kill data for model building under dynamic drug concentrations. |
| Population PK (PopPK) Models | Mathematical models describing drug disposition and variability in the target human population. These are integrated with PD models for clinical simulations [77] [79]. |
| Non-Linear Mixed-Effects Modeling Software | Software platforms (e.g., NONMEM, Monolix, R with mrgsolve or nlmixr) are used to develop and run PK/PD models and clinical trial simulations [77]. |
| Machine Learning (ML) Algorithms | Emerging ML techniques can identify complex patterns in large datasets to enhance model-informed precision dosing and improve predictions of individual patient PK [79]. |
The paradigm for defining antimicrobial breakpoints and combating resistance is shifting from a static, MIC-centric view to a dynamic, model-informed one. Pharmacometric modeling and simulation, conducted within a rigorous MIDD framework, provides a powerful toolset to:
- Decouple true biological resistance from breakpoint drift by establishing more scientifically robust and stable breakpoints.
- Mechanistically optimize dosing regimens, especially for combination therapies, maximizing efficacy and suppressing the emergence of resistance.
- Accelerate the development of new anti-infectives and refine the use of existing ones through quantitative, evidence-based decision-making.
Widespread adoption of these approaches, coupled with standardized reporting of breakpoint metadata in surveillance studies, is critical for accurately tracking AMR trends and preserving the efficacy of existing antimicrobials for future generations.
Evidence and Impact: Validating Models and Comparing Outcomes in Drug Development
Model-Informed Drug Development (MIDD) represents a transformative framework that leverages quantitative modeling and simulation to integrate nonclinical and clinical data, enhancing decision-making throughout drug development and regulatory evaluation [1]. For anti-infective drug development, MIDD provides powerful tools to optimize dosing regimens, predict efficacy against pathogenic organisms, and support regulatory approvals, particularly when patient recruitment for traditional clinical trials is challenging [82] [1]. Regulatory agencies including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have increasingly endorsed MIDD approaches, culminating in recent harmonized guidelines that establish clear standards for model development, assessment, and application [1] [83].
The International Council for Harmonisation (ICH) M15 guideline, released for public consultation in November 2024, defines MIDD as "the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [1]. This guideline harmonizes expectations between regulators and sponsors, supporting consistent regulatory decisions and minimizing errors in the acceptance of modeling and simulation to inform drug labels [1]. For anti-infective researchers, these developments create unprecedented opportunities to leverage pharmacometric approaches for addressing key development challenges, from first-in-human dose selection to post-approval lifecycle management.
Regulatory Framework and Guidelines
Evolution of Regulatory Guidance
The regulatory foundation for MIDD has evolved significantly over the past decade. The FDA's Division of Pharmacometrics (DPM) established a 10-year strategic plan in 2010, which has subsequently trained 91 pharmacometricians and developed 14 disease models to enhance regulatory review capabilities [84]. The Prescription Drug User Fee Act (PDUFA) VI and VII have further catalyzed regulatory acceptance by incorporating biomarkers, real-world evidence, and alternative clinical trial designs into the drug approval process [1].
The ICH M15 draft guideline, endorsed in November 2024, represents the current regulatory standard for MIDD applications [1] [83]. This guideline provides a harmonized framework for assessing evidence derived from MIDD and aims to facilitate multidisciplinary understanding and appropriate use of these approaches [83]. The EMA has paralleled these developments with specific guidelines on pharmacokinetic-pharmacodynamic (PK-PD) analyses for antibacterial agents, addressing the use of these analyses to identify potentially efficacious dose regimens [82].
Key Regulatory Programs and Initiatives
The FDA has established specific programs to facilitate MIDD implementation, including the MIDD Paired Meeting Program, which continues through fiscal years 2023-2027 under PDUFA VII [85]. This program provides sponsors with opportunities to discuss MIDD approaches with Agency staff, with priority given to submissions focusing on dose selection or estimation, clinical trial simulation, and predictive or mechanistic safety evaluation [85].
Regulatory agencies have also developed specialized frameworks for specific modeling approaches. The FDA issued guidance on Physiologically Based Pharmacokinetic (PBPK) Analyses in September 2018, formally recognizing PBPK's role in drug-drug interaction (DDI) assessments [86]. The EMA published its first PBPK-specific guideline in December 2018, marking international regulatory recognition of this technology [86].
Key MIDD Methodologies and Applications in Anti-Infective Development
Quantitative Modeling Approaches
Table 1: Essential MIDD Modeling Approaches for Anti-Infective Development
| Modeling Approach | Key Application in Anti-Infectives | Regulatory Application Examples |
|---|---|---|
| Population PK (PopPK) | Characterizes variability in drug exposure among patients with infections | Dose justification for special populations (renally/hepatically impaired) |
| Physiologically Based PK (PBPK) | Predicts drug-drug interactions and tissue penetration at infection sites | DDI assessment (81.9% of PBPK applications), organ impairment dosing (7.0%) [86] |
| Exposure-Response (E-R) | Links antibiotic exposure to microbiological and clinical outcomes | Probability of target attainment analysis for dose justification [82] |
| Quantitative Systems Pharmacology (QSP) | Models host-pathogen-drug interactions for combination therapies | Mechanistic safety evaluation, identification of critical biomarkers [43] |
| Model-Based Meta-Analysis (MBMA) | Integrates historical trial data to contextualize new drug performance | Benchmarking against standard of care antibiotics [1] |
Application to Anti-Infective Specific Challenges
For anti-infective agents, MIDD approaches specifically address the unique challenges of infectious disease therapeutics. The EMA guideline explicitly addresses the use of PK-PD analyses to identify efficacious dose regimens for antibacterial, antimycobacterial, and antifungal agents [82]. Key concepts include the epidemiologic cut-off value, exposure-response relationship, minimal inhibitory concentration (MIC), PK-PD index magnitude, target, probability of target attainment, and wild-type distribution analysis [82].
These approaches are particularly valuable for optimizing dosing against resistant pathogens, where patient populations may be limited and traditional clinical trials impractical. MIDD has enabled accelerated approvals of drugs for pediatric infectious conditions and rare diseases, where recruiting sufficient patients for efficacy studies is challenging [1]. Additionally, MIDD has contributed to clinical pharmacology strategies that successfully allow dose extrapolation to related disease indications and clinical populations without additional clinical trials [1].
Experimental Protocols for MIDD in Anti-Infective Development
Protocol 1: Population PK-PD Model Development for Antibacterial Agents
Objective: To develop a PopPK-PD model that characterizes the relationship between drug exposure, microbiological response, and clinical outcomes in patients with bacterial infections.
Materials and Reagents:
- Plasma/Serum Samples: For drug concentration determination (PK)
- Microbiological Data: MIC values against clinical isolates
- Clinical Response Data: Microbiological eradication and clinical cure rates
- Patient Covariates: Demographics, organ function, comedications
- Software Platforms: NONMEM, Monolix, or R for population modeling
Methodology:
- Data Collection: Collect rich or sparse PK samples during clinical trials. Determine MIC values for baseline pathogens using standardized methods.
- Structural Model Development: Develop a structural PK model using compartmental approaches. Integrate a PD model linking drug concentrations to bacterial killing using Emax or similar models.
- Covariate Analysis: Identify patient factors (renal/hepatic function, age, weight) influencing PK-PD parameters using stepwise covariate modeling.
- Model Validation: Validate the final model using visual predictive checks, bootstrap analysis, and external validation if possible.
- Probability of Target Attainment (PTA): Conduct Monte Carlo simulations to determine PTA for various dosing regimens against MIC distributions.
Regulatory Considerations: The model should be developed following ICH M15 guidelines, with clearly defined Context of Use (COU) and Question of Interest (QOI) [1]. Documentation should include a Model Analysis Plan (MAP) created prior to analysis.
Protocol 2: PBPK Model for Antifungal Drug-Drug Interactions
Objective: To develop a PBPK model predicting DDIs between a novel antifungal agent and commonly co-administered medications.
Materials and Reagents:
- In Vitro Metabolism Data: CYP enzyme inhibition/induction parameters (IC50, KI, kinact)
- Physicochemical Properties: LogP, pKa, solubility, permeability
- Physiological Parameters: Organ sizes, blood flows, enzyme/transporter abundances
- Software Platforms: Simcyp, GastroPlus, or PK-Sim
Methodology:
- Model Building: Develop a base PBPK model using in vitro and physicochemical data. Verify model performance against observed single-agent PK data.
- Enzyme/Transporter Characterization: Incorporate parameters for CYP inhibition/induction or transporter interactions from in vitro studies.
- DDI Prediction: Simulate interactions with probe substrates (e.g., midazolam for CYP3A4). Compare predictions with observed clinical DDI data if available.
- Sensitivity Analysis: Conduct sensitivity analyses on key uncertain parameters.
- Dosing Recommendation: Propose dose adjustments for combinations with interacting drugs.
Regulatory Considerations: Follow FDA and EMA PBPK guidelines regarding model verification and validation [86]. Document the model using the standardized format described in regulatory guidance, including a complete chain of evidence from in vitro parameters to clinical predictions.
Visualization of MIDD Workflows
MIDD Process Flow in Anti-Infective Development
Probability of Target Attainment Analysis
Research Reagent Solutions for MIDD in Anti-Infectives
Table 2: Essential Research Tools for MIDD in Anti-Infective Development
| Tool Category | Specific Solutions | Function in MIDD |
|---|---|---|
| PK Modeling Software | NONMEM, Monolix, Phoenix NLME | Population PK and PK-PD model development |
| PBPK Platforms | Simcyp, GastroPlus, PK-Sim | Prediction of DDIs and special population dosing |
| Clinical Data Management | R, Python, SAS | Data preparation, exploration, and visualization |
| Statistical Tools | R, Stan, WinBUGS | Bayesian analysis, model diagnostics, simulation |
| Clinical Trial Simulators | Trial Simulator, MIDD customized tools | Prediction of trial outcomes and optimization of study designs |
| Database Resources | EUCAST, CLSI MIC distributions | Wild-type and epidemiologic cut-off values for PTA analysis |
Regulatory Submission Framework
Documentation Requirements
Successful regulatory submission of MIDD evidence requires comprehensive documentation aligned with ICH M15 expectations. The Model Analysis Plan (MAP) serves as the foundational document, containing Introduction, Objectives, Data, and Methods sections [1]. This should be developed early in the process, ideally with regulatory feedback through the MIDD Paired Meeting Program [85].
The submission should clearly articulate the Context of Use (COU), Question of Interest (QOI), Model Influence, Decision Consequences, Model Risk, Model Impact, Appropriateness, and Technical Criteria [1]. For anti-infective applications, specific attention should be paid to the epidemiological relevance of MIC distributions and the clinical validity of PK-PD targets [82].
Model Validation and Credibility Assessment
Regulatory agencies employ credibility assessment frameworks based on standards such as ASME 40-2018 for evaluating computational models [1]. Model credibility is established through verification (ensuring correct implementation), validation (ensuring accuracy for intended use), and uncertainty quantification [1].
For PBPK models in particular, regulatory reviews focus on whether the model establishes "a complete and credible chain of evidence from in vitro parameters to clinical predictions" [86]. Even models with limitations may demonstrate practical value in critical applications if their strengths and limitations are properly characterized [86].
The regulatory endorsement of MIDD by the FDA and EMA represents a fundamental shift in drug development paradigms, offering powerful approaches for addressing the unique challenges of anti-infective development. The recent harmonization of guidelines through ICH M15 provides clarity and consistency for sponsors seeking to implement these approaches [1] [83].
For anti-infective researchers, MIDD enables more efficient dose optimization, particularly for special populations and resistant pathogens where traditional clinical trials are impractical. The continued evolution of MIDD, including integration with artificial intelligence and multi-omics data, promises to further enhance predictive accuracy and support the development of novel anti-infective therapies [86].
By adopting the structured frameworks, experimental protocols, and documentation standards outlined in this article, anti-infective researchers can successfully navigate regulatory expectations and leverage MIDD to accelerate the delivery of effective treatments to patients.
Within the modern anti-infective development pipeline, Model-Informed Drug Development (MIDD) has emerged as an indispensable tool for optimizing therapy and informing regulatory decisions [87]. Pharmacometrics, the science of using mathematical models to quantify drug, disease, and trial characteristics, provides a scientifically rigorous framework to integrate preclinical and clinical data [8]. This application note details the successful application of Modeling & Simulation (M&S) strategies in the development of novel anti-infectives, providing a structured comparative analysis and detailed experimental protocols for implementation.
Comparative Analysis of M&S Applications
Table 1: Overview of M&S Applications in Anti-Infective Development
| Anti-Infective / Class | Development Challenge | M&S Approach Applied | Key Outcome / Success Story |
|---|---|---|---|
| Novel Triaryl Antimicrobials [88] | Optimization of a hit compound with weak antimicrobial activity (MIC: 128–256 µg/mL) | Structure-Based Design & Scaffold Hopping: Replacement of a linear linker with a benzene ring to minimize molecular energy and maintain active conformation, informed by docking models. | Achieved MIC of 1–2 µg/mL against drug-resistant Streptococcus pneumoniae, superior to some marketed antibiotics [88]. |
| Ceftobiprole (Cephalosporin) [8] | Dose optimization for nosocomial pneumonia and patients with renal impairment | Population PK/PD & PTA Analysis: Modeling to determine pharmacodynamic target attainment (PTA) for various dosing regimens in special populations. | Established 500 mg BID as the optimal dose for patients with renal clearance (CLCr) ≤ 50 mL/min [8]. |
| Garenoxacin (Fluoroquinolone) [8] | Optimizing dosing for community-acquired pneumonia (CAP) | Exposure-Response Relationship & PTA: Integration of population PK with PD data from serum and epithelial lining fluid (ELF). | Confirmed 400 mg QD as a safe and adequate dose, with PTA >95% for a target fAUC0-24/MIC90 ratio [8]. |
| AI-Discovered Halicin [89] | Efficiently screening vast chemical space for novel, effective antibiotics | Graph Neural Network (GNN) & Predictive Modeling: Trained on chemical structures to predict efficacy, then scored for novelty, stability, and toxicity. | Identification of a novel antibiotic candidate (Halicin) with activity against resistant strains via a new mechanism, from a screen of tens of millions of compounds [89]. |
Table 2: Quantitative Pharmacodynamic (PD) Targets for Anti-Infectives
| Pharmacokinetic/Pharmacodynamic (PK/PD) Index | Typical Target Value for Efficacy | Anti-Infective Case Study |
|---|---|---|
| fT>MIC (Time free drug concentration exceeds MIC) | 30-50% of dosing interval for β-lactams [8] | Cefepime: PTA of 91.8% for 50% T>MIC in CSF for extracerebral infections [8]. |
| fAUC/MIC (Area Under the free concentration curve over MIC) | ~100-200 for Fluoroquinolones [8] | Moxifloxacin: PTA >95% for fAUC0-24/MIC90 of 120 in ELF for CAP [8]. |
| Cmax/MIC (Peak free drug concentration over MIC) | >10 for Aminoglycosides [8] | Moxifloxacin: Cmax/MIC90 >10 associated with efficacy [8]. |
Detailed Experimental Protocols
Protocol 1: MIDD for Dose Optimization and Registrational Support
This protocol outlines the application of M&S to support the late-stage development and registration of an anti-infective, using ceftobiprole for nosocomial pneumonia as an example [8].
1. Objective: To determine the optimal dosing regimen of ceftobiprole (500 mg BID vs. TID, 1-2 hour infusion) for patients with nosocomial pneumonia, including those with renal impairment.
2. Materials and Software:
- Software: Nonlinear mixed-effects modeling software (e.g., NONMEM, Monolix)
- Data: Rich and sparse PK data from Phase I and Phase II/III trials, patient demographic data, renal function markers (e.g., serum creatinine)
- In Vitro Data: MIC distributions for target pathogens (e.g., Staphylococcus aureus, Streptococcus pneumoniae)
3. Methodology:
- Step 1: Population Pharmacokinetic (PopPK) Model Development
- Develop a structural PK model (e.g., 2- or 3-compartment) to describe the concentration-time profile.
- Identify and quantify sources of inter-individual variability (e.g., on clearance, volume) and residual unexplained variability.
- Covariate model building to identify patient factors (e.g., creatinine clearance, body weight) that significantly influence PK parameters. Use stepwise covariate modeling.
- Step 2: Pharmacodynamic (PD) Target Identification
- Select a relevant PD index from the literature (e.g., %fT>MIC for β-lactams).
- Define the target magnitude for the index required for efficacy (e.g., 50% fT>MIC for 1-log10 CFU reduction).
- Step 3: Pharmacodynamic Target Attainment (PTA) Analysis
- Perform Monte Carlo simulations (e.g., n=5000 virtual patients) using the final PopPK model and its parameter distributions.
- For each virtual patient and dosing regimen, calculate the probability of achieving the PD target across a range of MIC values (e.g., 0.06 to 32 mg/L).
- Generate PTA curves (PTA vs. MIC).
- Step 4: Cumulative Fraction of Response (CFR) Analysis
- Integrate the PTA with the MIC distribution of relevant bacterial pathogens from surveillance studies.
- Calculate the CFR, which predicts the expected population PTA for the given regimen and pathogen mix.
- Step 5: Dose Recommendation
- Recommend the dosing regimen that achieves a PTA of ≥90% at the MIC breakpoint and a high CFR (e.g., >80-90%) for the target infections.
Protocol 2: AI-Guided Discovery of Novel Anti-Infective Pharmacophores
This protocol describes a modern, AI-driven approach for the de novo discovery of novel antibiotic candidates, as exemplified by the discovery of Halicin and other compounds [89].
1. Objective: To efficiently screen ultra-large chemical libraries in silico to identify novel chemical structures with predicted antibacterial activity and desirable drug-like properties.
2. Materials and Software:
- Software: Graph Neural Network (GNN) libraries (e.g., PyTorch Geometric, DGL), molecular docking software, cheminformatics toolkits (e.g., RDKit)
- Data: Training dataset of chemical structures with associated MIC values or growth inhibition data against target bacteria (can be relatively small, e.g., a few thousand compounds)
- Hardware: Standard GPU workstations or compute clusters
3. Methodology:
- Step 1: Model Training
- Represent molecules as graphs (atoms as nodes, bonds as edges).
- Train a Graph Neural Network (GNN) or a Convolutional Neural Network on the molecular graphs to predict antibacterial activity from the chemical structure.
- Step 2: In Silico Screening and Hit Prioritization
- Use the trained model to predict the activity of millions of compounds from a virtual chemical library (e.g., ZINC, PubChem).
- Apply a multi-step filtering pipeline to the top-predicted hits:
- Efficacy Filter: Select compounds with predicted high activity.
- Novelty Filter: Remove compounds structurally similar to known antibiotics (to ensure new mechanisms).
- Toxicity Filter: Use pre-trained models or structural alerts to flag potentially toxic compounds.
- Synthesizability Filter: Prioritize compounds that are chemically feasible to synthesize.
- Step 3: In Vitro Validation
- Synthesize or procure the top candidate molecules.
- Test the compounds in vitro against a panel of Gram-positive and Gram-negative bacteria to determine Minimum Inhibitory Concentrations (MICs).
- For confirmed hits, proceed to mechanistic studies (e.g., whole-genome sequencing of resistant mutants) to identify the mode of action.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Software for M&S in Anti-Infective R&D
| Category | Item / Solution | Function / Application |
|---|---|---|
| Software & Computational Tools | NONMEM, Monolix, R | Gold-standard software for population PK/PD model development and simulation [8] [87]. |
| Molecular Docking Software (e.g., AutoDock Vina, GOLD) | Structure-based virtual screening to predict ligand binding to target proteins (e.g., RNAP, enzymes) [88]. | |
| Graph Neural Network (GNN) Libraries (e.g., PyTorch Geometric) | AI-driven in silico screening for de novo drug discovery and scaffold hopping [89] [90]. | |
| Chemical & Biological Resources | Predefined Chemical Fragment Libraries | Used in fragment splicing methods (e.g., DeepFrag, FREED) for rational structure-based design [91]. |
| Cation-Adjusted Mueller-Hinton Broth | Standardized medium for performing MIC assays according to CLSI guidelines to determine antimicrobial activity [88]. | |
| Panel of WHO Priority Pathogens | Reference bacterial strains for essential antimicrobial susceptibility testing during lead compound evaluation [88] [92]. | |
| Analytical & Synthesis | Palladium Catalysts (e.g., Tetrakis(triphenylphosphine)palladium(0)) | Essential for key synthetic steps, such as Suzuki-Miyaura coupling, in the synthesis of novel scaffolds (e.g., triaryl compounds) [88]. |
| LC-MS/MS Systems | For quantitative bioanalysis of drug concentrations in complex biological matrices (plasma, ELF, CSF) for PK studies [8]. |
The relentless rise of antimicrobial resistance (AMR), projected to cause 10 million deaths annually by 2050, underscores a critical need for efficient antibiotic development [64]. However, the anti-infective pipeline remains perilously thin, hampered by scientific challenges and, critically, by economic barriers that make it difficult for companies to recoup development costs [64] [93]. In this high-stakes environment, pharmacometrics has emerged as a transformative discipline. As the core of Model-Informed Drug Development (MIDD), it employs quantitative modeling and simulation to integrate nonclinical and clinical data, informing key development and regulatory decisions [1]. This application note details how the strategic application of pharmacometric principles directly addresses the economic and timeline challenges in anti-infective research, providing structured protocols and quantitative evidence of its impact.
Quantitative Evidence of Impact
The following tables synthesize data on how pharmacometrics mitigates specific, costly challenges in drug development, particularly within the anti-infective domain.
Table 1: How Pharmacometrics Addresses Major Cost Drivers in Anti-Infective Development
| Cost Driver | Traditional Approach | Pharmacometric Solution | Quantifiable Impact |
|---|---|---|---|
| Late-Stage Failure | Reliance on Phase 3 trial outcomes for all decisions [1]. | Early Go/No-Go decisions using exposure-response and disease progression models [1]. | Reduces resource expenditure on doomed candidates; improves probability of technical success. |
| Patient Recruitment | Large, lengthy trials for rare diseases or specific resistant infections [1]. | Extrapolation of efficacy from source to target population (e.g., adults to pediatrics) using PopPK/PD [1]. | Can potentially eliminate the need for dedicated clinical trials in certain populations [1]. |
| Inefficient Dosing | Empirical, frequent dose-finding trials. | PopPK/PD models identify optimal dosing regimens, including for special populations [1]. | Prevents costly post-market corrections and maximizes therapeutic potential. |
| Regulatory Delays | Inconsistent regulatory expectations for model submissions [1]. | ICH M15 guidelines provide a harmonized framework for MIDD, aligning regulators and sponsors [1]. | Minimizes errors in submission acceptance, streamlining the approval pathway [1]. |
Table 2: Pharmacometrics Contribution to Timeline Acceleration
| Development Stage | Application | Reported Timeline Impact |
|---|---|---|
| Preclinical to Clinical Translation | Physiologically Based Pharmacokinetic (PBPK) models predict human PK and drug-drug interactions [1]. | Informs first-in-human dose selection, reducing early trial iterations. |
| Clinical Phase Bridging | Using models to support extrapolation across indications, populations, or formulations [1]. | Can obviate the need for duplicate clinical trials, saving several years of development time. |
| Regulatory Submission & Review | Model-based meta-analysis and exposure-response data supporting evidence of effectiveness [1]. | Enables accelerated approvals, especially for pediatric conditions and rare diseases [1]. |
Detailed Experimental Protocols
Protocol 1: Population PK/PD (PopPK/PD) Model for a Novel Antibiotic
This protocol outlines the development of a PopPK/PD model to characterize drug exposure and its relationship to bactericidal effect in a patient population, which is fundamental for determining an optimal dosing regimen.
1. Objective: To develop a PopPK/PD model that describes the plasma concentration-time profile of a novel antibiotic and links its exposure to the reduction in bacterial burden, identifying key sources of variability (e.g., renal function, weight).
2. Research Reagent Solutions & Materials: Table 3: Essential Materials for PopPK/PD Modeling
| Item | Function/Description |
|---|---|
| Clinical PK-PD Dataset | The core data source, containing drug concentration measurements, patient demographic data, clinical lab values, and longitudinal pathogen counts. |
| NONMEM Software | Industry-standard software for nonlinear mixed-effects modeling, used for model parameter estimation [94]. |
| PsN (Perl Speaks NONMEM) | A toolkit for model diagnostics, validation, and automation, facilitating robust model development [94]. |
| R Software with Xpose Package | Open-source environment for data preparation, statistical analysis, and comprehensive graphical model diagnostics [94]. |
| Structural PK Model | A mathematical representation (e.g., one- or two-compartment model) of the drug's disposition in the body [94]. |
| PD Model (e.g., Emax) | A model (e.g., ( E = E0 - (E{max} * C) / (EC_{50} + C) )) describing the drug's effect on bacterial killing [95]. |
3. Methodology:
- Data Collection: Collect rich or sparse blood samples for drug concentration assay. Simultaneously, measure bacterial counts (e.g., from in vitro time-kill studies or patient samples) at predetermined time points [95].
- Structural Model Development:
- Begin with a base structural PK model (e.g., one-compartment with first-order absorption).
- Integrate a PD model, linking plasma concentration (C) to the bacterial killing rate. An indirect response model is often applicable for antibiotics.
- Stochastic Model Development:
- Introduce inter-individual variability (IIV) on key PK/PD parameters (e.g., Clearance, EC₅₀) using an exponential error model:
Pi = θ * exp(ηi), where ηi is the random effect [94]. - Define a residual error model (e.g., combined additive and proportional) to account for unexplained variability:
Yij = Cij * (1 + ε1ij) + ε2ij[94].
- Introduce inter-individual variability (IIV) on key PK/PD parameters (e.g., Clearance, EC₅₀) using an exponential error model:
- Covariate Model Building:
- Evaluate the influence of patient covariates (e.g., creatinine clearance on clearance, albumin on volume of distribution) using stepwise forward addition/backward elimination.
- The final model should explain a substantial portion of the IIV, leading to more precise dosing recommendations for sub-groups.
- Model Evaluation:
- Use Goodness-of-Fit (GOF) plots: observed vs. population/individual predictions, conditional weighted residuals vs. time [94].
- Perform bootstrap analysis (e.g., 1000 runs) to assess parameter precision and model stability [94].
- Conduct Visual Predictive Check (VPC) to evaluate the model's predictive performance by comparing simulated data with observed data [94].
Diagram 1: PopPK/PD Model Development Workflow
Protocol 2: Model-Based Trial Simulation for Dose Selection
This protocol uses an established PopPK/PD model to simulate virtual clinical trials, comparing the efficacy of different dosing regimens to select the most promising one for a Phase 3 study.
1. Objective: To simulate the clinical outcome (e.g., microbial eradication) for multiple candidate dosing regimens of a novel anti-infective, leveraging a previously validated PopPK/PD model to select the regimen with the highest probability of success.
2. Methodology:
- Define Question of Interest (QOI) & Context of Use (COU): Explicitly state the goal: "To identify the dose that achieves >90% probability of target attainment (PTA) for a /fAUC/MIC ratio of 100 against the target pathogen."
- Develop Model Analysis Plan (MAP): Document the objectives, input models (the final PopPK/PD model), simulation scenarios (doses, patient demographics), and outcomes to be measured, as guided by ICH M15 [1].
- Set Up Virtual Patient Population: Simulate a virtual population (e.g., n=1000) that reflects the target clinical trial population, including distributions of covariates identified in the PopPK/PD model.
- Run Simulations:
- For each virtual patient and each candidate regimen, simulate the full time-course of drug concentration and bacterial burden.
- Calculate the outcome metric (e.g., rate of eradication at end of therapy).
- Analyze Results & Make Decision:
- Summarize the probability of efficacy for each regimen.
- Select the dose with the optimal benefit-risk profile (highest efficacy, lowest risk of toxicity) for progression.
Diagram 2: Model-Based Trial Simulation Process
Case Study: Model-Informed Development of a Novel Anti-Infective
The development of zosurabalpin, the first new class of antibiotic in 50 years targeting carbapenem-resistant Acinetobacter baumannii (CRAB), exemplifies MIDD principles in action [96]. While not all details are public, the pathway illustrates key applications:
- Challenge: Developing a drug for a critical priority pathogen with a novel mechanism (inhibiting lipopolysaccharide transport) and no existing clinical efficacy benchmarks [96].
- MIDD Application: Preclinical PK/PD models in infected mice were used to establish the exposure-response relationship linking drug concentrations to bacterial killing in the lung and thigh infection models. These models were pivotal in transitioning from animal efficacy studies to predicting effective human dosing regimens [96].
- Impact: This model-informed strategy de-risked early clinical development and supported the design of the ongoing Phase 3 trial, which compares zosurabalpin with standard-of-care, accelerating the path for this critically needed therapy [96].
The integration of pharmacometrics into anti-infective development is no longer a luxury but a necessity in the face of AMR. As detailed in these application notes, the quantitative power of MIDD provides a structured, evidence-based approach to confront the field's most pressing economic and timeline challenges. By enabling smarter, faster decisions—from lead optimization to regulatory submission—pharmacometrics directly reduces late-stage attrition, optimizes trial designs, and facilitates regulatory agreement. The ongoing harmonization of guidelines like ICH M15 further solidifies its role as a cornerstone of modern drug development [1]. For researchers and developers in the anti-infective space, building pharmacometric capabilities is a strategic investment essential for revitalizing the pipeline and securing future therapies against drug-resistant infections.
Model-Informed Drug Development (MIDD) represents a transformative framework that uses quantitative modeling and simulation to integrate data and inform decision-making in drug development [1]. Within anti-infective development, pharmacometric modeling and simulation approaches have demonstrated significant advantages over traditional methods for dose prediction and risk management [97] [79]. These approaches enable more precise dosing strategies that account for inter-patient variability and pathogen susceptibility, which is particularly crucial in an era of increasing antimicrobial resistance [7] [79]. This application note details the quantitative evidence, experimental protocols, and practical implementation strategies for benchmarking MIDD against traditional drug development methods, with specific focus on anti-infective therapeutics.
Quantitative Benchmarking of MIDD vs Traditional Approaches
Portfolio-Level Time and Cost Savings
Table 1: Quantitative Benefits of MIDD Implementation in Drug Development
| Metric | Traditional Approach | MIDD Approach | Improvement | Source |
|---|---|---|---|---|
| Average Development Time per Program | Baseline | ~10 months reduction | Significant acceleration | [97] |
| Average Cost Savings per Program | Baseline | ~$5 million annually | Substantial cost reduction | [97] |
| Clinical Trial Budget Impact | Historical levels | $70-100 million reduction | Major efficiency gains | [97] |
| Phase 1 Study Waivers | Required for all standard scenarios | Possible via PBPK modeling | Direct time and cost savings | [97] |
| Sample Size Requirements | Fixed, often larger numbers | Reduced via population PK/PD | Lower trial cost and duration | [97] |
The implementation of MIDD approaches across a drug development portfolio demonstrates substantial advantages over traditional methods. A comprehensive analysis of pharmaceutical industry practices revealed that systematic application of MIDD yielded annualized average savings of approximately 10 months of cycle time and $5 million per program [97]. These efficiencies stem from multiple factors including clinical trial waivers, sample size reductions, and more informed "No-Go" decisions [97].
Antimicrobial Development Specific Considerations
Table 2: MIDD Applications in Anti-Infective Dose Optimization and Risk Management
| Application Area | Traditional Method | MIDD Approach | Advantages |
|---|---|---|---|
| Dose Individualization | Fixed dosing, TDM with therapeutic ranges | Model-Informed Precision Dosing (MIPD) | Accounts for inter-patient PK variability and specific pathogen MIC [79] |
| PK/PD Target Attainment | Empirical dosing | Population PK modeling and Monte Carlo simulations | Quantifies probability of target attainment for specific patient populations and pathogens [79] |
| Overcoming Resistance | Standard susceptibility testing | Integrated PK/PD and resistance modeling | Identifies dosing strategies to suppress resistance emergence [7] |
| Special Populations | Limited studies or exclusion | PBPK and population PK models | Optimizes dosing in critically ill, pediatric, and other special populations [79] |
| Trial Design | Large non-inferiority trials | Adaptive designs and clinical trial simulations | Reduces sample size requirements and development costs [97] [7] |
In antimicrobial development, MIDD enables more rational dose selection based on pharmacokinetic/pharmacodynamic (PK/PD) principles and probability of target attainment [79]. This is particularly valuable given the unique challenges in antibiotic development, including escalating resistance and difficult enrollment in traditional non-inferiority trials [7].
Experimental Protocols for MIDD Implementation
Protocol 1: Model-Informed Precision Dosing for Anti-Infectives
Objective: To implement model-informed precision dosing for optimized antimicrobial therapy in individual patients.
Materials and Methods:
- Patient Data Collection: Demographics (age, weight, height), clinical laboratory values (serum creatinine, albumin), clinical condition (ICU vs. non-ICU), organ function information [79]
- Pathogen Data: Minimum Inhibitory Concentration (MIC) for target pathogen [79]
- Drug Concentration Assay: Validated bioanalytical method for drug concentration measurement [79]
- Software Tools: Appropriate modeling software (e.g., NONMEM, Monolix, R) for parameter estimation and Bayesian forecasting [79]
Procedure:
- Select Appropriate Population PK Model: Choose a previously developed and validated population PK model specific to the patient population and antimicrobial [79]
- Collect Patient-Specific Data: Gather relevant patient covariates and, if available, drug concentration measurements (trough, peak, or AUC-based) [79]
- Perform Bayesian Estimation: Use maximum a posteriori (MAP) Bayesian estimation to derive individual PK parameters [79]
- Simulate Dosing Regimens: Project drug exposure for various dosing regimens using individual PK parameters [79]
- Calculate PK/PD Target Attainment: Determine fAUC/MIC, fC~max~/MIC, or %fT>MIC based on drug characteristics [79]
- Recommend Optimized Dose: Select dosing regimen that maximizes probability of target attainment while minimizing toxicity risk [79]
Validation:
- Compare predicted vs. measured drug concentrations
- Assess clinical outcomes (clinical cure, microbiological eradication)
- Monitor toxicity indicators [79]
Figure 1: MIDD Workflow for Anti-Infective Development - This diagram illustrates the systematic approach for implementing model-informed drug development in anti-infective programs, from defining key questions to informed decision-making.
Protocol 2: PBPK Modeling to Support Clinical Trial Waivers
Objective: To utilize Physiologically-Based Pharmacokinetic (PBPK) modeling to support waivers for dedicated clinical studies.
Materials and Methods:
- PBPK Software Platform: Qualified PBPK platform (e.g., GastroPlus, Simcyp, PK-Sim) [97] [43]
- Compound Parameters: Physicochemical properties, in vitro metabolism and transport data [43]
- System Data: Population-specific physiological parameters [43]
Procedure:
- Model Development: Develop and verify PBPK model using available in vitro and in vivo data [43]
- Model Qualification: Qualify model performance against available clinical data [97]
- Special Population Simulation: Simulate drug exposure in specific populations (renal/hepatic impairment, elderly, pediatric) [97] [43]
- Drug-Drug Interaction Assessment: Predict magnitude of interactions with commonly co-administered drugs [1]
- Dose Recommendation: Propose optimized dosing for special populations [97]
- Regulatory Submission: Prepare comprehensive model validation report and justification for study waiver [97]
Application Contexts:
- Renal impairment studies
- Hepatic impairment studies
- Drug-drug interaction studies
- Pediatric extrapolation [97]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for MIDD in Anti-Infective Development
| Category | Specific Tools | Function and Application |
|---|---|---|
| Modeling Software | NONMEM, Monolix, R with specific packages (nlmixr, PopED) | Population PK/PD model development and parameter estimation [1] [79] |
| PBPK Platforms | GastroPlus, Simcyp, PK-Sim | Physiologically-based pharmacokinetic modeling and simulation [97] [43] |
| Clinical Trial Simulation | Trial simulator, mrgsolve, PKPDsim | Clinical trial simulation and adaptive design evaluation [1] [43] |
| Bioanalytical Assays | LC-MS/MS, HPLC-UV validated methods | Quantification of drug concentrations in biological matrices for TDM and model validation [79] |
| Data Management | Electronic data capture systems, CDISC standards | Collection and standardization of clinical trial data for modeling purposes [97] |
| Susceptibility Testing | Broth microdilution, Etest, Automated systems | Determination of Minimum Inhibitory Concentration (MIC) for PK/PD target attainment analysis [79] |
Figure 2: MIDD-Driven Dose Optimization Strategy - This diagram outlines the integrated approach for optimizing anti-infective dosing strategies using patient, pathogen, and drug properties to inform model-based dosing recommendations.
Regulatory and Implementation Framework
The regulatory landscape for MIDD has evolved significantly, with the International Council for Harmonisation (ICH) releasing the M15 guideline on "General Principles for Model-Informed Drug Development" to harmonize expectations regarding documentation standards, model development, and applications [1]. Regulatory agencies recognize MIDD as a valuable tool for supporting drug development and review, particularly in challenging areas such as anti-infective development [97] [1].
Successful implementation requires:
- Early engagement with regulatory agencies through mid-development cycles [1]
- Comprehensive Model Analysis Plans (MAP) documenting context of use, model validation, and decision consequences [1]
- Adherence to "fit-for-purpose" principles, ensuring model complexity aligns with the question of interest [43]
- Multidisciplinary collaboration among pharmacometricians, clinicians, microbiologists, and statisticians [79]
Benchmarking studies demonstrate that MIDD approaches provide substantial advantages over traditional methods for dose prediction and risk management in anti-infective development. The quantitative evidence shows significant reductions in development timelines and costs, while improving precision in dosing strategies. The experimental protocols and research tools outlined in this application note provide a practical framework for implementation of these approaches. As antimicrobial resistance continues to pose serious threats to global health, the adoption of MIDD strategies becomes increasingly critical for optimizing anti-infective therapy and advancing novel treatments through efficient drug development pathways.
Model-informed drug development (MIDD) is a quantitative framework that uses modeling and simulation to integrate nonclinical and clinical data, informing drug development and regulatory decisions [1]. In anti-infective research, pharmacometric models—encompassing pharmacokinetics (PK), pharmacodynamics (PD), and their integration (PK/PD)—are paramount for determining optimal dosing regimens to maximize efficacy and curb resistance [98] [7]. The traditional development of these models can be labor-intensive, slow, and limited in its exploration of the vast model parameter space [99].
Artificial intelligence (AI) and machine learning (ML) are now revolutionizing this field by enhancing model predictivity, automating complex workflows, and enabling the integration of diverse data sources. This integration addresses critical challenges in anti-infective development, such as the rapid emergence of antimicrobial resistance (AMR) and the stark economic disincentives for creating new antibiotics [7] [96]. This document provides application notes and detailed experimental protocols for leveraging AI/ML to build more predictive pharmacometric models in anti-infective research.
The table below summarizes key performance data from recent studies applying AI/ML to pharmacometric challenges, demonstrating tangible improvements in efficiency and predictive power.
Table 1: Performance Metrics of AI/ML in Pharmacometric Applications
| Application Area | AI/ML Technique | Key Performance Outcome | Reference / Context |
|---|---|---|---|
| Population PK Model Automation | Bayesian Optimization with Random Forest (pyDarwin) | Identified model structures comparable to expert models in <48 hours on average, evaluating <2.6% of the total model space. | [99] |
| PK/PD Modeling (Irregular Time Series) | Neural-ODE (Neural Ordinary Differential Equations) | Superior extrapolation ability for predicting temporal PK data outside of training data compared to LightGBM and LSTM networks. | [98] |
| Exposure-Response Modeling | Artificial Neural Networks (ANN) | Produced less biased predictions of treatment effects compared to traditional multinomial logistic regression. | [98] |
| Clinical Trial Efficiency | AI-generated Digital Twins | Potential to significantly reduce control arm size in Phase 3 trials, lowering costs and speeding patient recruitment. | [100] |
| Pharmacogene Prioritization for African Populations | Knowledge Embedding & Large Language Models (LLMs) | Pipeline to systematically identify drug-gene pairs for dose optimization in malaria/TB treatments, addressing a major data scarcity issue. | [101] |
Application Note 1: Automated Population PK Model Development
3.1 Background Population PK (PopPK) model development is typically a manual, sequential process where a modeler tests structures from simple to complex. This is time-consuming, can lead to local minima, and introduces subjective variation [99]. Automation accelerates this process, ensures a more systematic exploration of the model space, and improves reproducibility.
3.2 Research Reagent Solutions
Table 2: Essential Tools for Automated PopPK Development
| Item | Function |
|---|---|
| pyDarwin Library | A Python library implementing global optimization algorithms (e.g., Bayesian optimization, genetic algorithms) for automated model selection. |
| NONMEM | Industry-standard software for non-linear mixed effects modeling, used for model fitting and parameter estimation. |
| Pre-defined PopPK Model Space | A structured library of plausible model components (compartments, absorption models, error structures) for the algorithm to search. |
| Penalty Function | A custom function that balances model fit (e.g., objective function value) with model plausibility (e.g., parameter precision, shrinkage). |
3.3 Experimental Protocol: Automated PopPK Structure Identification
Diagram 1: Automated PopPK Workflow
Procedure:
- Define the Model Search Space: Construct a comprehensive but biologically plausible set of structural models. This should include:
- Compartments: 1-, 2-, and 3-compartment models.
- Absorption Models: First-order, zero-order, and complex models (e.g., dual, sequential zero-first order) for extravascular drugs.
- Elimination Models: Linear and Michaelis-Menten (non-linear) elimination.
- Error Models: Additive, proportional, and combined residual error models.
Configure the Optimization Engine: Initialize the pyDarwin framework, specifying the optimization algorithm (e.g., Bayesian Optimization with a Random Forest surrogate). Set computational constraints (e.g., 40 CPUs, 40 GB RAM, max 72-hour runtime).
Implement the Penalty Function: Define a multi-objective penalty function to guide the search. This function should incorporate:
- Goodness-of-Fit: The model objective function value (OFV).
- Akaike Information Criterion (AIC): To penalize over-parameterization.
- Parameter Plausibility: Penalties for high relative standard errors (>50%), abnormally high or low inter-individual variability, or high shrinkage (>30%) [99].
Run the Automated Search: The algorithm will iteratively:
- Generate a set of candidate model structures from the search space.
- Execute NONMEM to fit each candidate model to the PK dataset.
- Calculate the penalty score for each fitted model.
- Use the optimization algorithm to select the next, most promising set of candidates based on the scores.
- Continue until a convergence criterion is met or computational limits are reached.
Output and Validation: The process outputs the top-ranked model structure(s). The final model must undergo standard validation procedures (e.g., visual predictive checks, bootstrap) as with any manually developed model.
Application Note 2: AI-Enhanced PK/PD Modeling for Predicting Efficacy
4.1 Background Traditional PK/PD modeling relies on pre-specified structural models derived from mechanistic understanding. ML approaches, particularly Neural-ODEs, can learn the underlying governing equations of PK/PD relationships directly from data, offering advantages in handling complex, irregularly sampled time-series data [98].
4.2 Research Reagent Solutions
Table 3: Essential Tools for AI-Enhanced PK/PD
| Item | Function |
|---|---|
| Neural-ODE Framework | A neural network architecture that learns the derivative of a system, effectively discovering the underlying ODEs from data. (e.g., using PyTorch or TensorFlow). |
| Long Short-Term Memory (LSTM) / Gated Recurrent Unit (GRU) | Recurrent neural networks designed for sequence prediction, useful for modeling time-dependent processes. |
| Pharmacometric Data Simulator | Software (e.g., mrgsolve, R) to generate synthetic PK/PD data for training and testing model extrapolation capabilities. |
4.3 Experimental Protocol: Building a Neural-ODE PK/PD Model
Diagram 2: Neural-ODE PK/PD Modeling
Procedure:
- Data Preparation and Simulation: Use a known PK/PD model (e.g., a one-compartment PK model with an indirect response PD model) to simulate dense and sparse time-series data for training and validation. Ensure the data covers a wide range of doses to test extrapolation.
Model Architecture Definition: Construct a Neural-ODE model where a neural network parameterizes the derivatives of the system.
- Input Layer: Current state (e.g., drug concentration in central compartment, drug effect) and time.
- Hidden Layers: Fully connected layers with activation functions (e.g., ReLU, Tanh).
- Output Layer: The derivatives of the state variables (e.g., dC/dt, dE/dt).
Model Training: Train the Neural-ODE using an adaptive ODE solver (e.g., Runge-Kutta 4th order, Dormand-Prince).
- Loss Function: Use mean squared error (MSE) between the predicted and observed PK and PD values.
- Optimizer: Use Adam or stochastic gradient descent.
- Training: Feed the initial conditions and dosing regimen, and let the ODE solver and neural network jointly predict the full time course.
Model Validation and Extrapolation:
- Internal Validation: Compare the model's fit to the training data against a traditional NLME model.
- Extrapolation Test: Challenge the trained model to predict PK/PD profiles for dosing regimens not included in the training data (e.g., predict BID profiles after training on QD data) [98]. Compare its performance against other ML models like LSTM or LightGBM, which often fail at this task.
Application Note 3: Integrating AI/ML and Pharmacometrics for Global Health
5.1 Background Infectious diseases like malaria and tuberculosis display varied treatment responses across populations due to high genetic diversity, a challenge particularly acute in Africa. AI can bridge the data gap by prioritizing pharmacogenes for investigation, which are then formally evaluated using physiologically-based pharmacokinetic (PBPK) and NLME models [101].
5.2 Experimental Protocol: A Pipeline for Tailoring Anti-Infective Dosing in Africa
Diagram 3: AI-Driven Dosing Optimization
Procedure:
- Knowledge-Based Pharmacogene Prioritization:
- Data Curation: Gather drug-target interaction data, chemical structures, bioactivity data, and known PGx associations from public resources like PharmGKB.
- Model Training: Use knowledge graph embedding techniques or other ML models to learn patterns from known drug-gene pairs. The model is trained to predict novel, high-probability drug-pharmacogene interactions for anti-infectives.
Large Language Model (LLM) Refinement: Feed the top-ranked drug-gene pairs and relevant scientific literature into a domain-specific LLM to further contextualize and refine the hypotheses, filtering out spurious associations.
PBPK Model Sensitivity Analysis:
- For the top-prioritized gene (e.g., CYP2B6 for artemether), incorporate its functional impact (e.g., enzyme activity levels for different genotypes) into a whole-body PBPK model.
- Run sensitivity analyses to quantify how variation in the enzyme's activity affects key PK parameters (e.g., AUC, C~max~). This identifies genes with potential clinical relevance.
NLME Dose Optimization:
- Develop a PopPK model that includes the identified genetic polymorphism as a covariate on the relevant PK parameter.
- Use this final model to perform clinical trial simulations. Test various dosing regimens in virtual populations with different genotype distributions to identify a regimen that maximizes efficacy and minimizes toxicity across the major genetic subgroups in the target African population [101].
Regulatory and Operational Considerations
The integration of AI/ML into regulatory submissions is being harmonized globally. The International Council for Harmonisation (ICH) M15 draft guideline on MIDD explicitly includes AI/ML methods within its scope [1]. Successful application requires:
- Structured Planning: A Model Analysis Plan (MAP) should pre-specify the Question of Interest (QOI), Context of Use (COU), and the AI/ML approach.
- Model Credibility: Demonstrating model validity through rigorous verification (is the model implemented correctly?) and validation (is the model right for its intended purpose?) is critical [1].
- Early Regulatory Interaction: Engaging with regulators early in the drug development process to align on the proposed AI/ML strategy is highly recommended to ensure acceptability of the generated evidence [5] [1].
Conclusion
Pharmacometric modeling and simulation has unequivocally transformed the landscape of anti-infective drug development and applied pharmacotherapy. By providing a quantitative, scientifically rigorous framework, it enables more efficient and rational decision-making from the lab to the clinic. The integration of PK/PD principles allows for the optimization of dosage regimens, improves the management of drug-resistant infections, and facilitates personalized dosing in diverse patient populations, thereby enhancing efficacy and minimizing toxicity. As the field evolves, the convergence of pharmacometrics with artificial intelligence, machine learning, and quantitative systems pharmacology promises even greater predictive power. This progression will be pivotal in accelerating the delivery of novel, life-saving anti-infective therapies to patients and strengthening the global fight against antimicrobial resistance.
References
- 1. Scoping review of the role of pharmacometrics in model- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528282/]
- 2. The Role of Pharmacometrics in Advancing the Therapies ... [https://www.mdpi.com/1999-4923/16/12/1559]
- 3. Pharmacometrics, Physiologically Based Pharmacokinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6618101/]
- 4. Visualization of complex trial data in pharmacometric analyses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8452296/]
- 5. Artificial Intelligence in Drug & Biological Product Development [https://ctti-clinicaltrials.org/2025-ai-in-drug-biological-product-development/]
- 6. Current approaches and tools for combating antibiotic ... [https://link.springer.com/article/10.1007/s42452-025-07108-9]
- 7. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 8. Applications of Pharmacometrics in the Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3809903/]
- 9. Mitigating antimicrobial resistance by innovative solutions ... [https://www.nature.com/articles/s44259-025-00150-y]
- 10. Predicting population dynamics of antimicrobial resistance ... [https://pubmed.ncbi.nlm.nih.gov/40763873/]
- 11. Advancing Antimicrobial Resistance Research Through ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.583415/full]
- 12. Pharmacodynamic Parameters of Pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8989418/]
- 13. Applications of pharmacometrics in the clinical development ... [https://pubmed.ncbi.nlm.nih.gov/23473593/]
- 14. PK/PD Approach to Antibiotic Therapy Review [https://www.rxkinetics.com/antibiotic_pk_pd.html]
- 15. The pharmacodynamic bases of the prescription ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6755362/]
- 16. fAUC/MIC is the most predictive pharmacokinetic ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/20573659/]
- 17. fAUC/MIC is the most predictive pharmacokinetic/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2920176/]
- 18. Quantitative Analysis of Microbicide Concentrations in Fluids ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0085124]
- 19. Applications of pharmacometrics in the clinical ... [https://www.ovid.com/journals/excp/pdf/10.1586/ecp.13.6~applications-of-pharmacometrics-in-the-clinical-development]
- 20. a cross-SIG perspective on improving drug development [https://link.springer.com/article/10.1007/s10928-024-09960-5]
- 21. Understanding and applying pharmacometric modelling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5237699/]
- 22. Pharmacokinetic/Pharmacodynamic Modeling and Application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9330032/]
- 23. Pharmacokinetic/pharmacodynamic models for time ... [https://www.sciencedirect.com/science/article/pii/S0924857922001285]
- 24. Application of Pharmacokinetic-Pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00997/full]
- 25. Model‐Informed Drug Development for Anti‐Infectives [https://pmc.ncbi.nlm.nih.gov/articles/PMC8014105/]
- 26. Pharmacokinetics & Compartmental Modeling [https://www.allucent.com/resources/blog/compartmental-modeling-pharmacokinetics]
- 27. What Is Compartment Modelling in Pharmacokinetics? [https://www.cusabio.com/c-21197.html?srsltid=AfmBOoqus8F1pLhkOi9Ql8g8_bEnjMqveVy2jrzGzvunDUJVFFIcd1e9]
- 28. Kill Curves versus MIC - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC321563/]
- 29. Pharmacodynamic Parameters of Pharmacokinetic ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2022.860472/full]
- 30. Mechanism-based pharmacokinetic-pharmacodynamic ... [https://pubmed.ncbi.nlm.nih.gov/17906920/]
- 31. Antifungals: From Pharmacokinetics to Clinical Practice [https://www.mdpi.com/2079-6382/12/5/884]
- 32. Enhancing antibiotic therapy through comprehensive ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1521091/full]
- 33. Antifungal Pharmacokinetics and Pharmacodynamics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4448584/]
- 34. PK/PD-Guided Strategies for Appropriate Antibiotic Use in ... [https://www.mdpi.com/2079-6382/14/1/92]
- 35. Multiparametric LC-MS/MS method for simultaneous ... [https://www.sciencedirect.com/science/article/pii/S0731708524005995]
- 36. Physiologically Based Modelling Framework for Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9676785/]
- 37. The need for mathematical modelling of spatial drug ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-019-0133-x]
- 38. Drug Concentration Asymmetry in Tissues and Plasma for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6756291/]
- 39. Physiologically-based pharmacokinetic modeling to inform ... [https://www.sciencedirect.com/science/article/pii/S092809872300074X]
- 40. Physiologically Based Pharmacokinetic Modelling of Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3787211/]
- 41. Prediction of trough concentration and ALK occupancy in ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1234262/full]
- 42. Physiologically Based Pharmacokinetic Modeling of ... [https://www.mdpi.com/2079-6382/14/6/541]
- 43. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 44. Pharmacometrics-Based Considerations for the Design of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8057977/]
- 45. Pharmacokinetic Modeling & Simulation to Optimize ... [https://premier-research.com/perspectives/increasing-clinical-trial-success-pharmacokinetic-modeling-simulation-to-optimize-dosing-regimens/]
- 46. Modeling Successful Phase III Trials [https://www.appliedclinicaltrialsonline.com/view/modeling-successful-phase-iii-trials]
- 47. Pharmacometric and Digital Twin modeling for adaptive ... [https://www.sciencedirect.com/science/article/pii/S0169260725003360]
- 48. A Novel Approach to Evaluating the Design of Pediatric ... [https://link.springer.com/article/10.1007/s40262-025-01542-z]
- 49. Beta-Lactam Probability of Target Attainment Success [https://pmc.ncbi.nlm.nih.gov/articles/PMC10044207/]
- 50. Probability of target attainment (PTA) [https://revive.gardp.org/resource/probability-of-target-attainment-pta/?cf=encyclopaedia]
- 51. Population pharmacokinetic/pharmacodynamic modeling ... [https://pubmed.ncbi.nlm.nih.gov/40530972/]
- 52. Translational PK/PD of anti-infective therapeutics [https://www.sciencedirect.com/science/article/abs/pii/S1740674916300312]
- 53. Pharmacokinetic variability and significance of therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912797/]
- 54. Pharmacokinetic Alterations Associated with Critical Illness [https://pmc.ncbi.nlm.nih.gov/articles/PMC9894673/]
- 55. Renal Failure Drug Dose Adjustments - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK560512/]
- 56. Assessment of Hepatic Impairment and Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5859945/]
- 57. How critical illness impacts drug pharmacokinetics and ... [https://pharmaceutical-journal.com/article/ld/how-critical-illness-impacts-drug-pharmacokinetics-and-pharmacodynamics]
- 58. Clinical Pharmacokinetics in Kidney Disease: Fundamental Principles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6032582/]
- 59. Clinical Pharmacokinetics in Kidney Disease: Application to Rational Design of Dosing Regimens [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6086693/]
- 60. Mizuno Lab Projects [https://www.cincinnatichildrens.org/research/divisions/p/pharmacology-clinical-translational/labs/mizuno/projects]
- 61. ISAP [https://www.isap.org/]
- 62. How Consistent are Anti-Infective Drug Dosing ... [https://link.springer.com/article/10.1007/s40272-024-00674-2]
- 63. Proactive Therapeutic Drug MONiToring to Guide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311387/]
- 64. Current economic and regulatory challenges in developing ... [https://www.nature.com/articles/s44259-025-00123-1]
- 65. Current Treatment Strategies Against Multidrug-Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9633024/]
- 66. Pharmacokinetic profiles determine optimal combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7442591/]
- 67. Rapid optimization of drug combinations for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4473022/]
- 68. Computational frameworks transform antagonism to ... [https://www.nature.com/articles/s41746-025-01435-2]
- 69. IDSA 2024 Guidance on the Treatment of Antimicrobial ... [https://www.idsociety.org/practice-guideline/amr-guidance/]
- 70. Where Do PBPK Models Stand in Pharmacometrics ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7020319/]
- 71. Physiologically-based Pharmacokinetic Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC5204363/]
- 72. Application of Physiologically-Based Pharmacokinetic ... [https://link.springer.com/article/10.1007/s40495-025-00427-w]
- 73. Prediction of Pharmacokinetics for CYP3A4-Metabolized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860008/]
- 74. Application of physiologically‐based pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11646931/]
- 75. Physiologically Based Pharmacokinetic (PBPK) Modeling ... [https://www.sciencedirect.com/science/article/pii/S2773216925000339]
- 76. Breakpoint drift: a hidden confounder in antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12426181/]
- 77. A model-based evaluation of the pharmacokinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11894798/]
- 78. Pharmacokinetic/Pharmacodynamic Modeling and ... [https://www.mdpi.com/2079-6382/11/8/986]
- 79. Dose Individualisation of Antimicrobials from a ... [https://link.springer.com/article/10.1007/s40265-024-02084-7]
- 80. PK/PD modelling and simulation of longitudinal ... [https://www.sciencedirect.com/science/article/pii/S0924857924003054]
- 81. Scoping review of the role of pharmacometrics in model- ... [https://link.springer.com/article/10.1007/s10928-025-10005-8]
- 82. Use of pharmacokinetics and pharmacodynamics in the ... [https://www.ema.europa.eu/en/use-pharmacokinetics-pharmacodynamics-development-antibacterial-medicinal-products-scientific-guideline]
- 83. M15 General Principles for Model-Informed Drug ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m15-general-principles-model-informed-drug-development]
- 84. Division of Pharmacometrics [https://www.fda.gov/about-fda/cder-offices-and-divisions/division-pharmacometrics]
- 85. Model-Informed Drug Development Paired Meeting Program [https://www.fda.gov/drugs/development-resources/model-informed-drug-development-paired-meeting-program]
- 86. The Evolution and Future Directions of PBPK Modeling in ... [https://www.mdpi.com/1999-4923/17/11/1413]
- 87. Application of MIDD to accelerate the development of anti- ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24002692]
- 88. Development of triaryl antimicrobials by scaffold hopping from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12364105/]
- 89. AI Discovered Antibiotics: How Small Data & Small GNNs Led ... [https://www.cognitiverevolution.ai/ai-discovered-antibiotics-how-small-data-small-gnns-led-to-big-results-w-mit-prof-jim-collins/]
- 90. Accelerating discovery of bioactive ligands with ... [https://www.nature.com/articles/s41467-025-56349-0]
- 91. Bridging chemical space and biological efficacy: advances ... [https://link.springer.com/article/10.1007/s13659-025-00521-y]
- 92. Antibiotics in the clinical pipeline as of December 2022 [https://www.nature.com/articles/s41429-023-00629-8]
- 93. Without Federal Funding, Antibiotics Research May Lag [https://undark.org/2025/07/30/antibiotics-funding-lag/]
- 94. Model-informed drug development of novel ROCK2 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1477607/full]
- 95. A pharmacometric model assessing the in vitro synergistic ... [https://www.sciencedirect.com/science/article/pii/S0924857925001839]
- 96. First antibiotic in 50 years to tackle superbug nears approval [https://www.labiotech.eu/trends-news/antibiotic-development-landscape/]
- 97. Impact of Model‐Informed Drug Development on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272314/]
- 98. Machine Learning for Pharmacokinetic/Pharmacodynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354923000126]
- 99. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 100. How AI will reshape pharma in 2025 [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 101. Artificial intelligence coupled to pharmacometrics ... [https://www.nature.com/articles/s41467-025-64304-2]