Overcoming Stability Challenges in Antimicrobial Peptide Formulations: From Molecular Design to Clinical Translation
Antimicrobial peptides (AMPs) represent a promising class of therapeutics to combat the rising tide of antibiotic-resistant infections.
Overcoming Stability Challenges in Antimicrobial Peptide Formulations: From Molecular Design to Clinical Translation
Abstract
Antimicrobial peptides (AMPs) represent a promising class of therapeutics to combat the rising tide of antibiotic-resistant infections. However, their clinical translation is significantly hampered by inherent stability issues, including susceptibility to proteolytic degradation, short half-life, and low bioavailability. This article provides a comprehensive analysis of contemporary strategies to enhance AMP stability, covering foundational challenges, advanced formulation methodologies like liposomal and nanoparticle systems, optimization techniques including AI-driven design, and the current clinical landscape. Tailored for researchers, scientists, and drug development professionals, this review synthesizes the latest advances to guide the rational development of stable, efficacious, and clinically viable AMP-based therapeutics.
The Stability Conundrum: Understanding the Core Challenges Plaguing Antimicrobial Peptides
Frequently Asked Questions (FAQs)
Q1: What are the primary reasons for the short half-life of antimicrobial peptides (AMPs) in biological systems? The short half-life of AMPs is primarily due to two inherent vulnerabilities: proteolytic degradation and rapid renal clearance [1]. AMPs are composed of natural L-amino acids joined by amide bonds, which are susceptible to cleavage by a wide array of proteases and enzymes present in plasma, tissues, and serum [1] [2]. Furthermore, their relatively small size makes them susceptible to rapid filtration and elimination by the kidneys, leading to a short circulation time in vivo [2].
Q2: How does the proteolytic stability of a peptide in serum differ from its stability in whole blood? Peptide stability can vary significantly between different biological fluids. Research shows that peptides are generally degraded faster in serum than in plasma [3]. Surprisingly, peptides are often more stable in fresh whole blood than in serum derived from the same animal [3]. This is because the process of preparing serum activates coagulation factors, which are primarily calcium-dependent serine proteases (e.g., thrombin) that cleave C-terminal to lysine or arginine residues, thereby increasing proteolytic activity [3]. Therefore, stability in commercial serum may not accurately predict in vivo performance.
Q3: What are the most common chemical modifications used to improve AMP stability? Several chemical modification strategies are effectively employed to enhance the metabolic stability of AMPs:
- D-Amino Acid Substitution: Replacing natural L-amino acids with their D-isomers makes the peptide sequence unrecognizable to many proteases [2]. For example, replacing L-Val and L-Pro with D-amino acids in the peptide N6 improved its stability against proteases [2].
- Cyclization: Creating cyclic peptides, either through disulfide bridges or head-to-tail cyclization, makes them more rigid and less accessible to proteases [2]. Marketed AMPs like bacitracin A, daptomycin, and polymyxins are cyclic [2].
- PEGylation: Attaching polyethylene glycol (PEG) chains to the peptide can improve its biocompatibility, increase its effective size to reduce renal clearance, and shield it from proteolytic enzymes [2]. This has been successfully applied to peptides like OM19r-8 and N6NH2 [2].
- Terminal Modification: N-terminal acetylation or C-terminal amidation can block the action of exopeptidases like aminopeptidases and carboxypeptidases [4].
Q4: Beyond chemical modification, what formulation approaches can protect AMPs from degradation? Advanced delivery systems can shield AMPs from the biological environment and provide controlled release:
- Nanoparticles: Encapsulating AMPs in nanoparticles can protect them from proteolytic degradation, enhance their bioavailability, and allow for targeted delivery to the site of infection [5].
- Hydrogels: These networks can act as reservoirs for AMPs, providing a sustained and localized release that minimizes systemic exposure and degradation [5].
Troubleshooting Guides
Diagnosing Instability in Preclinical Models
If your AMP shows promising in vitro activity but fails in in vivo models, follow this diagnostic pathway to identify the root cause.
Problem: The antimicrobial peptide exhibits potent activity in laboratory assays but demonstrates significantly reduced efficacy during in vivo animal studies.
Investigation Procedure:
- Perform an Ex Vivo Stability Assay: Collect blood via cardiac puncture directly into a syringe containing your peptide solution to prevent clotting. Incubate this fresh whole blood at 37°C [3].
- Conduct a Comparative Stability Analysis: In parallel, incubate your peptide in commercially obtained serum and plasma from the same animal species [3].
- Sample and Analyze: Take aliquots from each mixture at set time points (e.g., 0, 10, 30, 60 minutes). Precipitate proteins with trichloroacetic acid (TCA), centrifuge, and analyze the supernatants using Reversed-Phase High-Performance Liquid Chromatography (RP-HPLC) to quantify the remaining intact peptide [3].
- Identify Degradation Fragments: Use Mass Spectrometry (MS) to analyze the degradation products from each biological fluid. This will pinpoint the specific cleavage sites within your peptide sequence [3].
Interpretation & Solutions:
- If degradation is slow in fresh blood but fast in commercial serum: The instability is likely linked to proteases activated during the serum clotting process (e.g., thrombin). Consider modifying lysine and arginine residues or using D-amino acid substitutes [3] [2].
- If degradation is rapid across all fluids: Your peptide is broadly susceptible to various proteases. Implement broad-stability strategies like cyclization or PEGylation [2].
- If degradation is minimal but in vivo efficacy is low: The issue may be rapid renal clearance or poor distribution to the target site. Consider PEGylation to increase hydrodynamic size or reformulate using a delivery system for targeted release [5] [2].
Optimizing Peptide Stability Through Design
This guide helps you systematically improve peptide stability through iterative design and testing.
Problem: Your lead AMP candidate is effective against pathogens but is rapidly degraded by proteases, limiting its therapeutic potential.
Optimization Procedure:
- Baseline Stability Profiling: Begin by incubating your lead peptide with specific proteases (e.g., trypsin, chymotrypsin) or in 10-50% serum. Use HPLC and MS to determine the half-life and identify the primary cleavage sites [3] [1].
- Iterative Modification:
- For cleavage near termini: Implement N-terminal acetylation or C-terminal amidation to block exopeptidases [4].
- For cleavage after basic residues (Lys/Arg): Replace L-lysine or L-arginine with D-enantiomers or other cationic, non-proteinogenic amino acids [2].
- For broad, non-specific degradation: Introduce cyclization via disulfide bridges or head-to-tail synthesis to confer conformational rigidity [2]. Alternatively, incorporate synthetic aromatics that provide steric hindrance and enhance helicity through non-covalent π-π interactions [4].
- Functional Validation: After each modification cycle, re-test the peptide's stability using the assays from Step 1. Crucially, confirm that the antimicrobial activity is retained via minimum inhibitory concentration (MIC) assays [2].
- Advanced Validation: Before moving to costly in vivo studies, validate the stability of your optimized peptide in the ex vivo fresh whole blood model described in Section 2.1 [3].
Quantitative Data on Peptide Stability
Table 1: Comparative Half-Life of Peptides in Different Biological Fluids
This table summarizes data on how different model peptides degrade in various media, highlighting the importance of choosing the right stability assay. [3]
| Peptide Family / Name | Sequence (Cleavage Site) | Half-life in Fresh Blood (Ex Vivo) | Half-life in Commercial Serum | Half-life in Commercial Plasma | Key Proteases Involved |
|---|---|---|---|---|---|
| Api88 | (Proprietary) | ~30 minutes | < 10 minutes | ~60 minutes | Coagulation factors (e.g., Thrombin) |
| Model Peptide A | ...KK↓AR... | > 60 minutes | ~15 minutes | > 60 minutes | Trypsin-like serine proteases |
| Model Peptide B | ...AA↓GP... | > 60 minutes | ~45 minutes | > 60 minutes | Nonspecific proteases |
Table 2: Impact of Chemical Modifications on Peptide Stability and Properties
This table outlines common stabilization strategies and their effects on peptide characteristics. [1] [2] [4]
| Modification Strategy | Mechanism of Stabilization | Effect on Proteolytic Half-Life | Potential Trade-offs / Considerations |
|---|---|---|---|
| D-Amino Acid Substitution | Renders peptide unrecognizable to proteases | Increase of several fold | Must verify that target receptor binding is not disrupted |
| Cyclization | Restricts conformational flexibility, shielding cleavage sites | Significant increase | Can be complex synthetically; may affect membrane interaction |
| PEGylation | Shields peptide via steric hindrance; reduces renal clearance | Moderate to significant increase | Can reduce antimicrobial activity; requires optimization of PEG size |
| Terminal Modification (Acetylation/Amidation) | Blocks action of exopeptidases | Moderate increase | Only protects termini; does not prevent endoprotease cleavage |
| Conjugation with Synthetic Aromatics | Provides steric hindrance and enhances α-helicity | Significant increase (as shown in model peptides) | A novel strategy; long-term toxicity profile may be less established |
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Studying Peptide Stability
| Reagent / Material | Function in Experiment | Key Considerations |
|---|---|---|
| Pooled Mouse/Human Serum | Provides a complex mix of active proteases for stability screening. | Be aware: Protease composition differs from fresh blood due to coagulation activation [3]. |
| K₂EDTA or Lithium Heparin Plasma | Provides a protease profile closer to circulating blood by inhibiting coagulation. | EDTA chelates Ca²⁺, inhibiting metalloproteases and coagulation factors [3]. |
| Trichloroacetic Acid (TCA) | Precipitates proteins and peptides to stop enzymatic reactions in stability assays. | The supernatant contains small peptide fragments for HPLC analysis after neutralization [3]. |
| RP-HPLC System with C18 Column | Separates and quantifies the intact peptide from its degradation products. | The primary tool for determining degradation half-life [3]. |
| Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF/TOF-MS) | Identifies the molecular weights of intact peptides and their degradation fragments to pinpoint cleavage sites. | Crucial for informing rational design and modification strategies [3]. |
| Trypsin, Chymotrypsin, Elastase | Used for targeted stability studies to understand susceptibility to proteases with specific cleavage preferences. | Trypsin cleaves after Lys/Arg; Chymotrypsin after aromatic residues; Elastase after small neutral residues [6]. |
| Synthetic Aromatic Compounds (e.g., NDI) | Conjugated to peptides via disulfide bridges to provide steric hindrance against proteases and enhance helicity. | A tool for non-covalent, structure-based stabilization as described in research [4]. |
Troubleshooting Guides
Common Experimental Challenges and Solutions
Table 1: Troubleshooting Common AMP Experimental Issues
| Problem | Potential Causes | Recommended Solutions | References |
|---|---|---|---|
| High Hemolytic Activity | Excessive peptide hydrophobicity; overly positive charge leading to non-specific membrane disruption. | Reduce hydrophobicity by substituting with less hydrophobic amino acids (e.g., Ala to Gly); Introduce cationic residues like Dap to reduce hemolysis while maintaining activity [7]. | [8] [7] |
| Poor Plasma Stability | Susceptibility to proteolytic degradation by serum proteases. | Introduce disulfide bonds via cysteine residues; Conjugate with mPEG to shield from enzymatic breakdown; Use D-amino acids to create protease-resistant analogs [8] [9]. | [8] [9] |
| Low Antimicrobial Efficacy | Insufficient interaction with bacterial membranes; suboptimal hydrophobicity/charge balance. | Increase net positive charge to enhance binding to anionic bacterial membranes; Optimize hydrophobicity to a "sweet spot" (neither too high nor too low); Utilize hybrid peptide strategy to combine active fragments [9]. | [9] [10] |
| Cytotoxicity to Mammalian Cells | Lack of selectivity for bacterial vs. mammalian cells. | Employ a "Safe-by-Design" approach by incorporating specific residues (e.g., Dap) shown to lower cytotoxicity; Use targeted delivery systems (e.g., nanoparticles) to concentrate peptide at infection site [7] [10]. | [10] [7] |
| Loss of Activity Post-Modification | Structural changes disrupt the active conformation or membrane-binding motif. | When cyclizing or dimerizing, ensure the active face of the peptide remains accessible; For point mutations, use helical wheel projections to predict impact on amphipathicity [8]. | [8] |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental cause of the Toxicity-Stability Paradox in Antimicrobial Peptides (AMPs)?
The paradox arises because the physicochemical properties that enhance an AMP's antimicrobial efficacy—such as a high net positive charge and appropriate hydrophobicity—are often the same properties that contribute to non-specific interactions with eukaryotic cell membranes (like red blood cells), leading to hemolysis and cytotoxicity [8] [9]. Furthermore, a linear, bioactive structure is often susceptible to rapid proteolytic degradation in plasma, forcing a trade-off between stability and inherent activity [10] [11].
Q2: What are the most effective strategies to reduce the hemolytic activity of a promising AMP?
Two highly effective strategies are:
- Charge Engineering: Substituting lysine with other cationic amino acids like L-2,3-diaminopropionic acid (Dap) has been shown to effectively decrease hemolytic activity while maintaining or even improving antimicrobial potency [7].
- PEGylation: Conjugating the AMP with methoxy polyethylene glycol (mPEG) can significantly shield its hydrophobic regions, reducing non-specific interactions with red blood cell membranes and thereby lowering hemolysis [8].
Q3: How can I improve the plasma stability of my AMP without completely compromising its function?
Introducing structural constraints is a key approach. This includes:
- Cyclization: Creating disulfide bonds through the introduction of cysteine residues can dramatically enhance stability against proteases [8].
- Using D-Amino Acids: Incorporating D-enantiomers of amino acids makes the peptide sequence unrecognizable to many natural proteases, thereby increasing its half-life in biological fluids [9].
- Nano-encapsulation: Formulating AMPs within nanoparticles or hydrogels can protect them from degradation and provide controlled release, improving bioavailability and stability at the infection site [10].
Q4: Are there specific amino acid substitutions known to improve the therapeutic index (TI) of AMPs?
Yes, research indicates that substitutions with certain non-canonical amino acids are beneficial. For instance, in the antimicrobial peptide Polybia-MPII, replacing lysine with L-2,3-diaminopropionic acid (Dap) not only enhanced its stability against tryptic digestion but also effectively decreased its hemolytic activity and cytotoxicity, leading to an overall improved therapeutic index [7].
Q5: What is a key consideration when designing experiments to assess AMP cytotoxicity?
It is critical to use multiple, complementary assays. A common approach is to pair a membrane integrity-based assay (e.g., using a dye like trypan blue or a fluorescent DNA-binding dye like SYTOX Green that penetrates only dead cells) with a metabolic activity assay (e.g., ATP detection) [12]. This helps distinguish between true cytotoxicity and cytostatic effects, providing a more comprehensive safety profile.
Experimental Protocols & Data
Key Quantitative Data on AMP Modifications
Table 2: Impact of Structural Modifications on AMP Properties
| Modification Type | Example / Residue | Effect on Antimicrobial Activity | Effect on Hemolysis | Effect on Plasma Stability | Key Finding / Rationale |
|---|---|---|---|---|---|
| Amino Acid Substitution | Lysine (Lys) | Baseline | Baseline | Baseline | Control reference [7]. |
| Arginine (Arg) | Improved | No improvement | No improvement | Enhanced activity but poor stability [7]. | |
| Dap (L-2,3-diamino-propionic) | Maintained | Decreased | Improved | Improved therapeutic index and tryptic stability [7]. | |
| Conjugation | mPEG | Decreased | Significantly Reduced | Significantly Improved | Trade-off: stability gained, but intrinsic activity often lowered [8]. |
| Structural | Cysteine (for cyclization) | Variable | Increased (due to hydrophobicity) | Enhanced conspicuously | Stability is improved, but increased hydrophobicity can raise hemolysis [8]. |
| Sequence Alteration | Altered sequence (same composition) | Little impact | Little impact | Little impact | Changing order of amino acids alone is insufficient [8]. |
Detailed Methodologies
Protocol 1: Assessing Hemolytic Activity This protocol measures the damage AMPs cause to red blood cells, a key indicator of toxicity.
- Preparation of RBCs: Collect fresh human or animal (e.g., sheep) blood in heparinized tubes. Centrifuge at 1,000-2,000 × g for 10 minutes. Remove plasma and buffy coat. Wash the pelleted red blood cells three times with phosphate-buffered saline (PBS).
- Peptide Incubation: Prepare a 2-4% (v/v) suspension of the washed RBCs in PBS. Incubate this suspension with a serial dilution of your AMP (typical concentration range 1-256 µg/mL) for 1 hour at 37°C. Include controls: PBS only (0% hemolysis) and 1% Triton X-100 (100% hemolysis).
- Measurement: After incubation, centrifuge the samples. Transfer the supernatant to a 96-well plate and measure the absorbance of released hemoglobin at 540 nm using a plate reader.
- Calculation: Calculate the percentage of hemolysis for each peptide concentration:
% Hemolysis = [(Abs_sample - Abs_PBS) / (Abs_TritonX - Abs_PBS)] × 100. The HC50 (concentration causing 50% hemolysis) is a standard metric for comparison [8] [7].
Protocol 2: Evaluating Tryptic Stability (Plasma Stability) This protocol tests an AMP's resistance to protease degradation, simulating in vivo conditions.
- Reaction Setup: Dissolve the AMP in a suitable buffer (e.g., Tris-HCl, pH 7.4-8.0). Add trypsin to the solution at a specific enzyme-to-substrate ratio (e.g., 1:20 to 1:50 w/w). Incubate the mixture at 37°C.
- Sampling: Withdraw aliquots at regular time intervals (e.g., 0, 5, 15, 30, 60, 120 minutes). Immediately stop the enzymatic reaction by adding a stop solution, such as trifluoroacetic acid (TFA) or by heating at 95°C for 5 minutes.
- Analysis: Analyze the samples using Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC). Monitor the disappearance of the intact peptide peak over time.
- Data Interpretation: Calculate the half-life (t1/2) of the peptide. A longer half-life indicates superior stability. Studies have shown that modifications like incorporating Dap can significantly slow the degradation rate compared to the native peptide [7].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent / Material | Function / Explanation | Example Use Case |
|---|---|---|
| SYTOX Green / Propidium Iodide | Fluorescent, membrane-impermeant DNA dyes that selectively enter dead cells with compromised membranes, used to quantify cytotoxicity [12]. | Distinguishing live from dead cells in a cytotoxicity assay via fluorescence microscopy or flow cytometry. |
| Trypan Blue | A vital dye excluded by live cells but taken up by dead cells, allowing for manual counting of cell viability [12]. | Quick and routine assessment of cell viability and concentration before seeding for an experiment. |
| mPEG (methoxy PEG) | A polymer conjugated to AMPs to shield them from proteolytic enzymes and reduce non-specific binding to host cells, thereby improving stability and reducing toxicity [8]. | Creating a PEGylated AMP derivative to test for improved plasma stability and reduced hemolysis in serum assays. |
| Cysteine | An amino acid used to introduce disulfide bonds into the peptide structure, conferring rigidity and resistance to proteolysis [8]. | Designing a cyclic AMP analog to test the hypothesis that constrained structures have enhanced stability. |
| Non-Canonical Amino Acids (Dap, Dab) | Synthetic counterparts of lysine that can be incorporated during peptide synthesis to fine-tune charge, hydrophobicity, and stability without altering the sequence length drastically [7]. | Systematically replacing lysine residues in a parent AMP to identify analogs with a lower hemolytic profile. |
Visualization of Workflows and Relationships
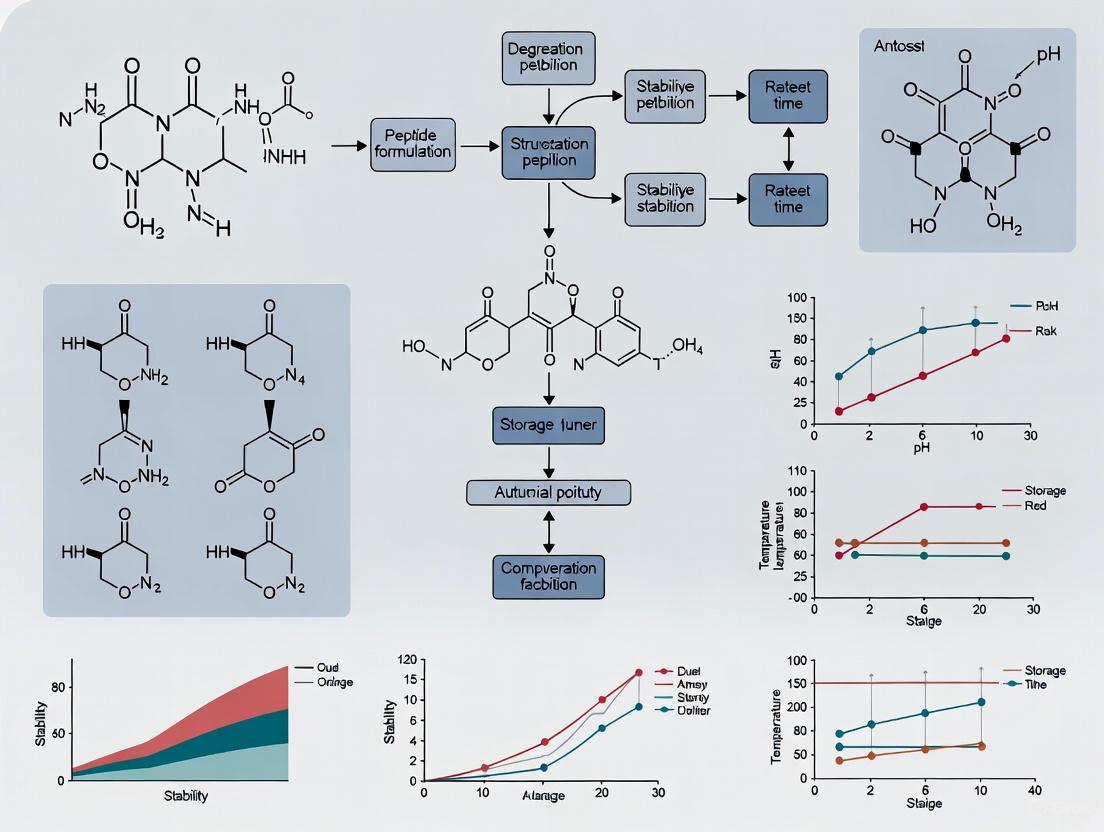
AMP Optimization Workflow
AMP Optimization Workflow
Toxicity-Stability Paradox Mechanism
Paradox Mechanism & Resolution
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary factors that limit the systemic bioavailability of Antimicrobial Peptides (AMPs)? The systemic bioavailability of AMPs is limited by a combination of factors, including susceptibility to proteolytic degradation by host proteases in serum and blood cells, cytotoxicity (particularly hemolytic activity), rapid systemic clearance, and poor permeability across biological membranes [10] [13] [11]. These inherent limitations often result in a short half-life and loss of activity before the peptide reaches its microbial target.
FAQ 2: How can the stability of AMPs against proteolytic degradation be improved? A common and effective strategy is amino acid substitution. This involves partially or wholly replacing L-amino acids in the peptide sequence with their D-amino acid counterparts [14]. Such modifications make the AMP resistant to protease degradation, as demonstrated by peptides maintaining their activity after incubation with trypsin and fetal calf serum, whereas their all-L-amino acid counterparts were degraded [14]. Other strategies include chemical modification (e.g., cyclization, N-methylation) and encapsulation within protective delivery systems [15] [10].
FAQ 3: What is the significance of "bioavailability as a microbial system property" in environmental bioremediation? This concept emphasizes that bioavailability is not just a chemical property but is fundamentally shaped by the biological system, including the physiology, ecology, and mobility of the degrading microorganisms [16]. In contexts like biodegradation of pollutants, bioavailability depends on microbial processes such as chemotaxis, production of biosurfactants, and the formation of transport networks (e.g., fungal mycelia), which enhance access to substrates [16]. This ecological perspective is crucial for predicting and enhancing bioremediation success.
FAQ 4: Which delivery systems show promise for enhancing AMP bioavailability and targeted delivery? Several advanced delivery systems are being investigated to overcome bioavailability hurdles:
- Nanoparticles: Inorganic (e.g., gold, silica) and organic (e.g., liposomes, micelles) nanoparticles can protect AMPs from degradation and reduce toxicity [15] [10].
- Hydrogels: These networks allow for controlled release of AMPs at the site of infection, such as in wound dressings, improving local bioavailability [15] [10].
- Targeted Systems: Some strategies involve conjugating AMPs to targeting moieties or designing systems that respond to specific environmental triggers (e.g., pH) at the infection site, enabling precise delivery [15].
FAQ 5: Beyond microbial membranes, what other mechanisms contribute to AMP activity? While many AMPs act by disrupting microbial membranes (membrane-targeting), a significant number exert their effects through non-membrane-targeting mechanisms [10]. These include:
- Inhibition of cell wall synthesis by binding to essential components like lipid II [10].
- Intracellular targeting of vital processes such as nucleic acid synthesis (e.g., indolicidin), protein folding, and enzyme activity [10] [17].
Troubleshooting Guides
Problem 1: Rapid Loss of Antimicrobial Activity in Biological Fluids
Potential Cause: Proteolytic degradation of the AMP by proteases present in serum, plasma, or host cell cytosols [14] [13].
Solutions and Experimental Protocols:
Solution A: Incorporate D-Amino Acids
- Principle: Proteases are stereospecific and primarily target L-amino acids. Substituting with D-isomers confers resistance.
- Experimental Protocol:
- Synthesis: Synthesize the parent all-L-amino acid peptide (L-peptide) and one or more variants with partial or complete D-amino acid substitution (D-peptide, All-D-peptide) [14].
- Stability Assay:
- Incubate each peptide (e.g., at 20 µM) with the biological fluid of interest (e.g., 2% serum in PBS) or with washed human erythrocyte cytosolic extracts at 37°C with agitation [14] [13].
- Withdraw samples at various time points (e.g., 0, 30, 60, 120 minutes).
- Analyze samples via reversed-phase HPLC. Monitor the disappearance of the parent peptide peak and the emergence of degradation fragments [13].
- Use MALDI-TOF mass spectrometry to identify the cleavage products [13].
- Activity Validation: Confirm that the D-amino acid substituted peptides retain antimicrobial activity against target microbes using a standard MIC (Minimum Inhibitory Concentration) or killing assay [14].
Solution B: Utilize Protective Delivery Systems
- Principle: Encapsulate the AMP within a carrier that acts as a physical barrier against proteases.
- Experimental Protocol:
- Formulation: Formulate the AMP into a delivery system such as a liposome, polymeric nanoparticle (e.g., PLGA), or hydrogel [15] [10].
- In Vitro Release and Stability:
- Incubate the free AMP and the AMP-loaded formulation in serum or a protease solution.
- At predetermined time points, separate the released/degraded fraction (e.g., via centrifugation or filtration).
- Measure the intact AMP content using HPLC or a bioassay to compare the stability profile of the formulated vs. free AMP.
The following workflow outlines the core experimental strategies for troubleshooting AMP stability and cytotoxicity:
Problem 2: Unacceptable Cytotoxicity (e.g., Hemolysis) at Therapeutic Concentrations
Potential Cause: The inherent amphipathicity and cationic charge that enable AMPs to disrupt microbial membranes can also cause non-specific lysis of host cells, particularly red blood cells [11] [17].
Solutions and Experimental Protocols:
Solution A: Optimize Peptide Sequence
- Principle: Systematically modify the peptide's physicochemical properties (e.g., hydrophobicity, charge, helicity) to increase its therapeutic index (selectivity for microbes vs. host cells).
- Experimental Protocol:
- Design: Create a library of peptide analogs with variations in key parameters. For instance, reduce overall hydrophobicity or introduce proline residues to disrupt alpha-helical structure.
- Hemolysis Assay:
- Prepare a suspension of fresh human or animal red blood cells (RBCs) in PBS [13].
- Incubate the RBCs with a range of peptide concentrations (and a positive control like Triton X-100 for 100% lysis, and a negative PBS control for 0% lysis) for a set time (e.g., 1 hour) at 37°C.
- Centrifuge the samples and measure the hemoglobin release in the supernatant by absorbance at 540 nm.
- Calculate the percentage hemolysis and determine the HC50 (concentration causing 50% hemolysis). The goal is to significantly increase the HC50 relative to the MIC [11].
Solution B: Formulate with Liposomes
- Principle: Encapsulation in liposomes can shield the AMP from direct contact with host cells until it reaches the target site, thereby reducing systemic cytotoxicity.
- Experimental Protocol:
- Formulation: Prepare liposomes (e.g., from phosphatidylcholine/cholesterol) containing the AMP using a method like thin-film hydration or extrusion.
- Cytotoxicity Testing:
- Perform the hemolysis assay as described above, comparing free AMP with liposome-encapsulated AMP.
- Additionally, test cytotoxicity against other mammalian cell lines (e.g., HEK293) using assays like MTT or LDH release.
- Confirm that the formulation retains antimicrobial efficacy in a co-culture or infection model.
Problem 3: Low Bioavailability at the Specific Site of Infection
Potential Cause: The AMP is distributed systemically but fails to accumulate or remain active at the required local site due to non-specific distribution, clearance, or an unfavorable microenvironment [15] [18] [16].
Solutions and Experimental Protocols:
Solution A: Develop Targeted Delivery Systems
- Principle: Conjugate the AMP or its carrier to ligands (e.g., antibodies, sugars) that bind specifically to receptors at the infection site, such as on microbial surfaces or inflamed host tissues [15].
- Experimental Protocol:
- Conjugation and Formulation: Chemically conjugate the targeting moiety to the AMP or the surface of a nanoparticle carrier.
- In Vitro Binding Test:
- Use techniques like surface plasmon resonance (SPR) or fluorescence microscopy to demonstrate enhanced binding of the targeted formulation to the target microbes or relevant cells, compared to a non-targeted control.
- In Vivo Validation:
- Use an animal model of infection. Administer the targeted and non-targeted formulations and, after a period, quantify the AMP concentration at the infection site and non-target organs (e.g., via HPLC-MS or fluorescence imaging) to demonstrate improved targeting and retention.
Solution B: Engineer Stimuli-Responsive Release
- Principle: Design a delivery system that releases its AMP payload in response to stimuli unique to the infection site, such as low pH, specific enzymes (e.g., lipases, hyaluronidases), or elevated lactate levels [15].
- Experimental Protocol:
- Formulate Responsive Carrier: Create a nanoparticle or hydrogel that degrades or changes structure under the specific stimulus (e.g., a pH-sensitive polymer or an enzyme-cleavable cross-linker).
- In Vitro Release Study:
- Place the AMP-loaded formulation in release buffers mimicking physiological (pH 7.4) and pathological (e.g., pH 5.5-6.5) conditions, or in the presence of the target enzyme.
- Sample the release medium over time and quantify the released AMP. The system should show minimal release under normal conditions and triggered release under pathological conditions.
The Scientist's Toolkit: Key Reagent Solutions
Table 1: Essential reagents and materials for addressing AMP bioavailability challenges.
| Reagent/Material | Function/Benefit | Example Use Cases |
|---|---|---|
| D-Amino Acids | Confers resistance to proteolytic degradation by host proteases, thereby increasing peptide stability and half-life [14]. | Synthesis of stable AMP analogs for in vivo applications. |
| Protease Inhibitors | Used in in vitro assays to confirm the role of proteolysis in AMP inactivation and to stabilize peptides during experimental processing [14]. | Added to serum or cell lysate incubations to protect the AMP. |
| Human Erythrocytes | Critical for assessing hemolytic activity (cytotoxicity) and for studying host cell-associated AMP degradation via cytosolic proteases [13]. | Hemolysis assays; preparation of cytosolic extracts for stability testing. |
| Liposome Formulation Kits | Provide a ready-to-use system for encapsulating AMPs, which can reduce cytotoxicity and protect the peptide from degradation [15] [10]. | Creating nanoparticle-based delivery systems for in vivo studies. |
| Cytosolic Extracts | Used to directly screen for susceptibility to intracellular proteases present in host cells, a key degradation pathway beyond serum proteases [13]. | In vitro stability assays under conditions mimicking intracellular environment. |
Table 2: Quantitative data on the effect of D-amino acid substitutions on AMP stability and activity. Data adapted from [14].
| Peptide Type | Sequence (Example) | Stability in Trypsin | Stability in Fetal Calf Serum | Antimicrobial Activity Post-Serum Incubation |
|---|---|---|---|---|
| All L-amino acid (L-peptide) | GRRGRRGRRGRR | Susceptible (Degraded) | Susceptible (Activity Lost) | Low/None |
| Partial D-amino acid (D-peptide) | GrRGRrGRrGRR (lowercase = D-form) | Resistant | Partially Resistant | Partially Retained |
| All D-amino acid (AD-peptide) | grrgrrgrrgrr (all lowercase = D-form) | Resistant | Resistant | Fully Retained |
The relationship between AMP properties, optimization strategies, and the resulting bioavailability outcomes can be visualized as follows:
Economic and Manufacturing Barriers in Large-Scale Production
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary economic challenges in scaling up Antimicrobial Peptide (AMP) production? The high cost of AMP development and manufacturing is a major barrier to their widespread clinical application. These costs are driven by complex synthesis and purification processes, low yields from natural extraction, and the expensive raw materials required for production. Furthermore, the inherent instability of peptides necessitates costly formulation technologies to ensure sufficient shelf-life and efficacy, making large-scale production economically challenging [11] [19].
FAQ 2: Why are AMPs inherently unstable and how does this impact manufacturing? AMPs face significant stability issues that complicate their manufacturing and storage. They are susceptible to proteolysis (degradation by enzymes), physical instability like aggregation, and chemical instability such as deamidation and oxidation. These undesirable properties lead to a short half-life, low bioavailability, and potential cytotoxicity, which severely limit their clinical application. Overcoming these instabilities requires advanced formulation or delivery systems, adding complexity and cost to the manufacturing process [15] [10] [19].
FAQ 3: What formulation strategies can mitigate the instability of AMPs during storage and delivery? Advanced drug delivery systems are being developed to protect AMPs from degradation and enhance their stability. These include:
- Nanocarriers: Systems like liposomes, polymeric nanoparticles, and micelles encapsulate AMPs, shielding them from proteolytic enzymes and enabling controlled release at the target site [15] [19].
- Hydrogels: These networks can entrap AMPs and provide a sustained release profile, which is particularly useful for topical applications like wound healing [15].
- Chemical Conjugation: Attaching AMPs to polymers or other molecules can improve their stability and pharmacokinetic profile [15].
FAQ 4: How can production costs be reduced for AMPs? Several approaches can help manage the high production costs of AMPs:
- Heterologous Expression: Using engineered microorganisms to produce AMPs can be more cost-effective than chemical synthesis or extraction from natural sources [19].
- Process Optimization: Implementing smart manufacturing technologies and leveraging economies of scale can improve production efficiency and output [20].
- Structural Optimization: Designing shorter or more stable peptide analogs (e.g., incorporating D-amino acids) can reduce synthesis costs and improve the peptide's stability, thereby lowering downstream processing expenses [21] [11].
Troubleshooting Guides
Problem 1: Low Yield or High Cost in Production
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low yield from natural source extraction. | Natural AMPs are often found in complex biological matrices in low quantities. | Shift to synthetic production methods like solid-phase peptide synthesis or recombinant expression in bacterial/yeast systems [11] [19]. |
| High raw material costs for synthesis. | Use of expensive protected amino acids and coupling reagents. | Optimize synthesis protocols and scale up purchasing to benefit from bulk pricing economies [20] [19]. |
| Inefficient purification process. | Multiple chromatography steps are needed to achieve pharmaceutical-grade purity. | Explore single-step or platform purification methods and invest in continuous manufacturing technology to improve efficiency [22]. |
Problem 2: Peptide Instability and Aggregation
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Peptide aggregates in solution during storage. | Exposure to stress conditions like elevated temperature, pH shifts, or mechanical shear forces [23]. | Reformulate with stabilizers such as sucrose, mannitol, or surfactants (e.g., polysorbate) to suppress molecular interactions [23]. |
| Loss of antimicrobial activity over time. | Chemical degradation (e.g., deamidation or oxidation of amino acids) [23]. | Modify buffer conditions (pH, ionic strength) and consider lyophilization (freeze-drying) for long-term storage. Use inert gas headspace to prevent oxidation [10]. |
| Short half-life in vivo. | Susceptibility to proteolysis by serum proteases [10]. | Incorporate AMPs into a delivery system like nanoparticles or liposomes to protect them from enzymatic degradation [15] [19]. |
Problem 3: Cytotoxicity (e.g., Hemolysis)
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| AMP causes red blood cell lysis (hemolysis). | The peptide's hydrophobicity and cationic charge lead to non-selective interaction with mammalian cell membranes [11] [10]. | Use structure-activity relationship (SAR) studies to optimize the peptide sequence. Reduce overall hydrophobicity or introduce D-amino acids to enhance selectivity for bacterial membranes [11]. |
| Cytotoxicity observed in cell-based assays. | Explore targeted delivery systems (e.g., with surface ligands) to concentrate the AMP at the site of infection and reduce systemic exposure [15]. |
Experimental Data and Protocols
Key Stability and Formulation Data
The data below summarizes common challenges and formulation strategies for AMPs, derived from recent research.
Table 1: Common AMP Instabilities and Mitigation Strategies
| Instability Type | Impact on AMP | Formulation Strategy | Reported Outcome |
|---|---|---|---|
| Proteolytic Degradation | Shortens half-life, reduces bioavailability [10]. | Encapsulation in nanoparticles (e.g., PLGA, gold) [15]. | Enhanced stability in serum; prolonged activity [15] [19]. |
| Aggregation | Loss of activity, increased immunogenicity [23]. | Addition of stabilizers (sucrose, surfactants) [23]. | Improved shelf-life and reduced particle formation. |
| Cytotoxicity | Hemolysis, nephrotoxicity [19]. | Sequence modification (e.g., cyclization) [21]. | Reduced hemolysis while retaining antimicrobial activity [21]. |
| Rapid Clearance | Inefficient dosing, requires frequent administration [15]. | PEGylation or fusion with albumin-binding domains [15]. | Increased circulation half-life [15]. |
Essential Experimental Protocol: Evaluating AMP Stability in Formulation
This protocol is used to assess the physical and chemical stability of an AMP in a chosen formulation under stress conditions.
Protocol Title: Forced Degradation Study for AMP Formulation Screening
1. Objective: To evaluate the stability of an AMP under various stress conditions (heat, light, agitation, pH) to identify the optimal formulation for long-term storage.
2. Materials and Reagents:
- Purified AMP
- Candidate formulations (e.g., buffers with different excipients)
- HPLC vials and system with UV/VIS or MS detector
- Thermostated water baths or stability chambers
- Centrifuge
3. Methodology:
- Step 1: Sample Preparation. Prepare identical aliquots of the AMP in each candidate formulation.
- Step 2: Stress Application. Subject the aliquots to different stress conditions:
- Thermal Stress: Incubate at 4°C (refrigerator control), 25°C (room temperature), and 40°C (accelerated testing) for 1-4 weeks [23].
- Agitation Stress: Place samples on an orbital shaker for 24-48 hours to simulate transportation forces [23].
- pH Stress: Incubate samples at a range of pH values (e.g., 3, 7, 9) for a set period.
- Step 3: Analysis. At predetermined time points, analyze samples by:
- HPLC: To quantify the percentage of intact AMP remaining and identify degradation peaks [23].
- Mass Spectrometry (MS): To characterize the chemical nature of the degradation products (e.g., deamidation, oxidation) [23].
- Dynamic Light Scattering (DLS): To monitor for aggregation and particle size changes.
4. Data Interpretation: The formulation that retains the highest percentage of intact AMP with the lowest levels of aggregates and degradation products across all stress conditions is considered the most stable and should be selected for further development.
Workflow Diagram: AMP Stability Optimization Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for AMP Formulation and Stability Research
| Item | Function/Application |
|---|---|
| Liposomes (e.g., DPPC, Cholesterol) | Versatile nanocarriers for encapsulating AMPs to reduce toxicity and protect against protease degradation [15] [19]. |
| Polymeric Nanoparticles (e.g., PLGA) | Biodegradable particles for sustained release of AMPs, improving pharmacokinetics and bioavailability [19]. |
| Hydrogels (e.g., Chitosan, Alginate) | 3D polymer networks for topical delivery of AMPs, providing a moist wound-healing environment and controlled release [15]. |
| Amino Acids (Fmoc/Derived) | Building blocks for solid-phase peptide synthesis (SPPS) of native or modified AMP sequences [19]. |
| Stabilizers (Sucrose, Trehalose) | Excipients that protect AMPs from aggregation and surface-induced denaturation during storage and lyophilization [23]. |
| Surfactants (Polysorbate 20/80) | Agents that minimize adsorption to containers and reduce shear-induced aggregation during manufacturing [23]. |
Advanced Delivery Systems and Formulation Strategies for Enhanced Stability
Troubleshooting Guides
Low Encapsulation Efficiency
Problem: The percentage of successfully encapsulated antimicrobial peptide (AMP) within liposomes is unacceptably low, leading to wasted API and compromised therapeutic potential.
Solutions:
- For Hydrophilic AMPs (e.g., LL-37): Utilize techniques that maximize the aqueous internal volume of liposomes. The Freezing, Annealing, and Thawing (FAT) method is highly effective, as the freezing step disrupts lamellae and promotes the formation of larger vesicles with greater aqueous space, resulting in higher encapsulation efficiency for water-soluble compounds [24].
- For Hydrophobic AMPs: Employ the Reverse-Phase Evaporation (REV) method. This technique is favorable for lipophilic compounds as it creates a environment where the antibiotic can partition into the forming lipid bilayers, leading to improved encapsulation [24].
- Optimize the Lipid-to-Drug Ratio: A poorly balanced ratio can lead to drug crystallization or leakage. Use Design of Experiments (DoE) to systematically identify the optimal molar ratio for your specific AMP, ensuring sufficient lipid is present to encapsulate the drug without excessive waste [25].
- Implement Remote Loading: For weakly basic amphipathic peptides, establish a transmembrane pH or ion gradient (e.g., ammonium sulfate). This "active loading" technique drives the uncharged drug across the bilayer, where it becomes ionized and trapped, achieving efficiencies over 90% [25].
Poor Physical Stability and Drug Leakage
Problem: Liposomes aggregate, fuse, or leak their encapsulated AMP payload during storage or in physiological media, reducing shelf-life and efficacy.
Solutions:
- Modulate Membrane Rigidity: Incorporate cholesterol (up to 50 mol%) into the phospholipid bilayer. Cholesterol condenses the lipid packing, reduces membrane fluidity, and decreases permeability to water-soluble molecules, thereby minimizing passive leakage [26] [25].
- Select High-Tm Lipids: Use saturated phospholipids with high gel-to-liquid crystalline phase transition temperatures (Tm), such as DSPC. These lipids form more rigid and stable bilayers at physiological temperatures [25].
- Enhance Electrosteric Stabilization:
- Surface Charge: Incorporate charged lipids (e.g., DMPG for negative, DPTAP for positive) to increase the zeta potential (typically >|±30| mV), preventing aggregation via electrostatic repulsion [27] [28].
- PEGylation: Graft polyethylene glycol (PEG) onto the liposome surface to create a "stealth" effect. The hydrated PEG layer sterically inhibits aggregation and opsonization, prolonging circulation time and enhancing stability [29] [25].
- Apply Protective Coatings: For oral delivery, use a dual-coating system with biopolymers like pectin and whey protein isolate (WPI). The polyelectrolyte layers protect the liposome from degradation in the gastrointestinal tract and provide controlled release [28].
- Utilize Lyophilization: Add cryoprotectants like trehalose and perform freeze-drying to create a stable solid powder. This process removes water and prevents lipid bilayer degradation, vastly extending shelf-life [26] [30].
Inefficient Targeting and Cellular Uptake
Problem: Liposomes fail to deliver AMPs effectively to the target site (e.g., intracellular M. tuberculosis), limiting antimicrobial efficacy.
Solutions:
- Create Ligand-Mediated "Stealth" Liposomes: Conjugate target-specific ligands (e.g., antibodies, peptides, sugars) to the liposome surface, often via a PEG spacer. This "molecular homing" allows for precise targeting of infected cells or tissues, minimizing off-target effects [31].
- Leverage the Lymphatic System: Design formulations that preferentially utilize the lymphatic system for distribution. This natural detour bypasses first-pass metabolism in the liver, reduces systemic toxicity, and provides a mechanism for prolonged release [31].
- Develop Stimuli-Responsive Liposomes: Use lipids or polymers that change structure in response to specific triggers at the infection site, such as lower pH or specific enzymes. This "intelligent" design ensures the AMP is released primarily at the target site [29] [31].
Frequently Asked Questions (FAQs)
Q1: What is the most critical factor in choosing a liposome preparation method for my antimicrobial peptide? The hydrophilicity/hydrophobicity of your peptide is the primary deciding factor. For hydrophilic AMPs like Vancomycin hydrochloride, methods that maximize aqueous volume (e.g., FAT) are superior. For hydrophobic AMPs like Rifampin, solvent-based methods like Reverse-Phase Evaporation (REV) are more effective. For moderate lipophilicity, techniques like thin film hydration can be suitable, but efficiency must be carefully evaluated [24].
Q2: How can I protect my liposomal formulation from degradation by gastrointestinal enzymes and bile salts? Applying a dual-coating of food-grade biopolymers, such as pectin and whey protein isolate (WPI), has been proven effective. The polyelectrolyte complex formed on the liposome surface acts as a physical barrier, shielding it from proteolytic enzymes and detergent-like bile salts, thereby improving stability for oral delivery [28].
Q3: My liposomes are forming aggregates during storage. How can I prevent this? Aggregation is often a sign of insufficient surface charge or steric hindrance. To prevent this:
- Increase Zeta Potential: Incorporate charged lipids to achieve a zeta potential above |±30| mV, which provides strong electrostatic repulsion between vesicles [27].
- PEGylate: Use PEGylated lipids to create a steric barrier that prevents vesicles from coming close enough to aggregate [29].
- Control Size: Ensure a narrow, uniform particle size distribution via extrusion or microfluidics, as polydisperse samples are more prone to aggregation [25].
Q4: What are the best analytical methods to accurately determine encapsulation efficiency? The choice of method is critical, as some can introduce significant bias. Ultrafiltration followed by bursting the liposomes with methanol is a recommended method for minimal bias. Techniques that rely on dialysis or simple centrifugation can lead to underestimation or overestimation of the encapsulated drug due to non-encapsulated drug binding or incomplete separation [24].
Q5: Can liposomal encapsulation really improve the biocompatibility of antimicrobial peptides like LL-37? Yes. Studies have demonstrated that encapsulating cationic AMPs like LL-37 and IDR-1018 in liposomes (e.g., based on soy lecithin) can significantly reduce their cytotoxicity against human cells (e.g., macrophages, epithelial cells) while maintaining their potent antimicrobial activity against pathogens like Mycobacterium tuberculosis [32].
Quantitative Data for Formulation Optimization
Table 1: Impact of Preparation Method on Encapsulation Performance for Different Antibiotics
Table based on data from [24]
| Antibiotic | Hydrophilicity | Preparation Method | Encapsulation Efficiency (%) | Mass Yield (%) | Key Takeaway |
|---|---|---|---|---|---|
| Vancomycin HCl | High | FAT | 33.4 ± 3 | 93.4 ± 7 | Best mass yield, suitable for hydrophilic drugs. |
| Reverse-Phase Evaporation | 39.4 | <50 | Higher efficiency but poor yield; significant API loss. | ||
| Teicoplanin | Moderate | Reverse-Phase Evaporation | ~74 (Max) | 93.4 ± 3.4 | Optimal method for moderately lipophilic drugs. |
| Rifampin | High (Lipophilic) | Reverse-Phase Evaporation | ~15.5 (Max) | 79.5 ± 3 | Optimal method for highly hydrophobic drugs. |
| Thin Film | 0 | <10 | Unsuitable for this hydrophobic drug. |
Table 2: Lipid Composition and Its Impact on Critical Quality Attributes
Data synthesized from [26] [31] [25]
| Lipid Component | Function | Impact on Liposome Properties | Recommended Use | ||
|---|---|---|---|---|---|
| Saturated Phospholipids (e.g., DSPC, DPPC) | Forms main bilayer structure. | ↑ Rigidity, ↑ Tm, ↑ Stability, ↓ Permeability. | Core lipid for stable formulations; high-Tm lipids for reduced leakage. | ||
| Cholesterol | Membrane modulator. | ↑ Rigidity, ↓ Fluidity, ↓ Permeability, ↑ Stability against aggregation. | 30-50 mol% to enhance mechanical stability and drug retention. | ||
| Charged Lipids (e.g., DMPG, DPTAP) | Confers surface charge. | ↑ Zeta Potential, ↑ Electrostatic Stability, prevents aggregation. | 5-20 mol% to achieve zeta potential > | ±30 | mV. |
| PEGylated Lipids | Creates steric shield. | ↑ Circulating half-life, ↑ Steric stability, ↓ RES uptake. | 1-10 mol% for "stealth" properties and enhanced stability in biological fluids. |
Experimental Protocols
Protocol 1: Freezing, Annealing, and Thawing (FAT) for Hydrophilic Peptides
Adapted from [24]
Objective: To encapsulate hydrophilic antimicrobial peptides with high efficiency by creating large unilamellar vesicles with maximized aqueous volume.
Materials:
- Lipids: DPPC, Cholesterol (3:1 molar ratio)
- Aqueous phase: Buffer containing the hydrophilic AMP (e.g., Vancomycin HCl)
- Equipment: Rotary evaporator, liquid nitrogen or -80°C freezer, water bath, extruder.
Procedure:
- Thin Film Formation: Dissolve the lipid mixture in chloroform in a round-bottom flask. Remove the organic solvent using a rotary evaporator under reduced pressure to form a thin, uniform lipid film on the flask walls.
- Primary Hydration: Hydrate the dry lipid film with the aqueous solution containing the AMP above the phase transition temperature (Tm) of the lipids (e.g., 50°C for DPPC) with vigorous stirring for 1 hour. This will form multilamellar vesicles (MLVs).
- Freezing and Thawing: Subject the MLV suspension to 5-10 rapid cycles of freezing in liquid nitrogen (or -80°C) and complete thawing in a warm water bath (above Tm).
- Extrusion: Pass the FAT-treated suspension through polycarbonate membranes of defined pore size (e.g., 100-200 nm) using an extruder for 10-20 passes to homogenize the vesicle size and reduce lamellarity, forming oligo- or unilamellar vesicles.
- Purification: Purify the resulting liposomes from non-encapsulated AMP using gel filtration chromatography or dialysis.
Protocol 2: Dual-Coating of Liposomes for Enhanced GI Stability
Adapted from [28]
Objective: To coat liposomes with layers of pectin and whey protein to protect against gastrointestinal degradation and enable controlled release.
Materials:
- Pre-formed liposomes (e.g., anionic liposomes from DMPC/DMPG)
- Pectin solution (e.g., 0.1-0.5% w/w in buffer)
- Whey Protein Isolate (WPI) solution (e.g., 1-2% w/w in buffer)
Procedure:
- First Layer Coating (Pectin): Under constant mild stirring, add the pectin solution dropwise to the liposome suspension. Continue stirring for 30-60 minutes to allow the anionic pectin to adsorb onto the cationic or anionic liposome surface via electrostatic and weak interactions.
- Second Layer Coating (Whey Protein): Similarly, add the WPI solution dropwise to the pectin-coated liposome suspension. Stir for an additional 30-60 minutes to allow the formation of a secondary layer stabilized by ionic interactions.
- Characterization: Confirm successful coating by measuring the change in zeta potential after each layer addition and by using techniques like FTIR and TEM. Perform in vitro release studies in simulated gastric and intestinal fluids to validate the protective effect.
Workflow and Mechanism Diagrams
Diagram 1: Liposome Formulation Optimization Workflow
Diagram Title: Liposome Formulation Decision Workflow
Diagram 2: Dual-Coated Liposome Protection Mechanism
Diagram Title: Protective Mechanism of Dual-Coated Liposomes
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Liposomal Formulation Research
| Reagent / Material | Function / Rationale | Example Application in AMP Research |
|---|---|---|
| Soy Lecithin | Natural, food-grade phospholipid mixture; forms the primary liposome bilayer. | Base lipid for creating biocompatible, clinically translatable formulations for peptides like LL-37 [32]. |
| High-Tm Phospholipids (e.g., DSPC, DPPC) | Synthetic saturated lipids; provide a rigid, stable bilayer with low passive permeability. | Core component for formulations requiring high drug retention and long-term stability [25]. |
| Cholesterol | Membrane stabilizer; inserts into the bilayer to reduce fluidity and prevent drug leakage. | Essential additive (30-50 mol%) in most formulations to enhance mechanical stability [26] [25]. |
| PEGylated Lipids (e.g., DSPE-PEG) | Steric stabilizer; creates a hydrophilic corona that reduces opsonization and extends circulation half-life. | Key for creating "stealth" liposomes that evade the immune system for targeted delivery [29] [25]. |
| Pectin & Whey Protein Isolate (WPI) | Biopolymer coating materials; form a protective polyelectrolyte shell via layer-by-layer deposition. | Used to create dual-coated liposomes that resist enzymatic degradation and bile salts in the GI tract [28]. |
| Ammonium Sulfate | Gradient agent; used in remote loading to create a transmembrane pH gradient for active drug encapsulation. | Enables high encapsulation efficiency (>90%) for weakly basic amphipathic compounds [25]. |
| Trehalose | Cryoprotectant; protects liposome integrity during the freeze-drying process by forming a glassy matrix. | Added before lyophilization to ensure long-term shelf stability and easy reconstitution [26] [30]. |
FAQs: Nanoparticle Formulation for Antimicrobial Peptide (AMP) Delivery
Q1: What are the main strategies to improve the circulation time of nanoparticle-based AMP carriers?
A1: The primary strategies involve surface functionalization to create "stealth" nanoparticles and the use of biomimetic coatings.
- PEGylation: Covalently attaching poly(ethylene glycol) (PEG) to the nanoparticle surface creates a hydrophilic layer that reduces opsonization (the adsorption of blood proteins) and uptake by the mononuclear phagocyte system (MPS), leading to prolonged circulation half-life [33] [34].
- Biomimetic Coating: Coating inorganic nanoparticles with biological membranes (e.g., red blood cell membranes, leukocyte membranes, or platelet membranes) confers the nanoparticles with the same biological functions as their parent cells. This includes superior biocompatibility, immune evasion, and prolonged circulation time [35].
Q2: Our encapsulated AMPs often show burst release instead of sustained release. How can we achieve better-controlled release kinetics?
A2: Burst release is often caused by weak surface adsorption or inadequate encapsulation. The following approaches can promote sustained release:
- Polymer Selection: Use biodegradable polymers with slower degradation kinetics, such as PLGA (poly(lactic-co-glycolic acid) or PCL (poly(ε-caprolactone)). The release rate can be tuned by adjusting the polymer's molecular weight and lactide-to-glycolide ratio in PLGA [33] [36].
- Stimuli-Responsive Design: Incorporate materials that release their cargo in response to specific stimuli found in the target microenvironment, such as:
Q3: We are experiencing aggregation and instability with our inorganic nanoparticle formulations. What are the key factors for improving colloidal stability?
A3: Colloidal stability is achieved by providing sufficient electrostatic or steric repulsion between particles.
- Surface Charge (Zeta Potential): A high absolute value of zeta potential (typically > ±30 mV) indicates strong electrostatic repulsion that prevents aggregation. This can be controlled by using specific surfactants or stabilizers during synthesis, such as citrate or CTAB (cetyltrimethylammonium bromide) [38].
- Surface Functionalization: Coating inorganic nanoparticles with a stable polymeric or silica shell provides a physical barrier and steric stabilization [35] [38]. For example, coating iron oxide nanoparticles with a silica layer prevents oxidation and aggregation [38].
Q4: How can we enhance the targeting efficiency of nanoparticles to specific bacterial infections?
A4: Active targeting can be achieved by conjugating targeting moieties to the nanoparticle surface.
- Ligand Conjugation: Attach antibodies, aptamers, or specific peptides that recognize and bind to antigens or receptors on the surface of the target bacterial cells [15]. This requires prior functionalization of the nanoparticle surface with reactive groups (e.g., carboxyl, amine, thiol) for bioconjugation [38].
- Biomimetic Approaches: Using membranes derived from specific cells, such as macrophages, can inherit their inherent ability to target infection sites [35].
Troubleshooting Guides
Table 1: Troubleshooting Common Issues in Nanoparticle Synthesis and Formulation
| Problem | Possible Causes | Suggested Solutions |
|---|---|---|
| Low AMP Encapsulation Efficiency | - Hydrophilic AMP partitioning into aqueous phase during emulsion.- Rapid diffusion of AMP during solvent removal.- Poor interaction between AMP and nanoparticle matrix. | - Use a double emulsion (W/O/W) method for hydrophilic AMPs [33] [36].- Optimize the organic-to-aqueous phase ratio.- Incorporate charged polymers to promote ionic interaction with charged AMPs. |
| Large Polydispersity (Heterogeneous Size) | - Inadequate homogenization or sonication energy.- Uncontrolled nucleation and growth during synthesis.- Aggregation during purification or storage. | - Increase homogenization speed/sonication power and time [33].- Use microfluidic reactors for precise mixing control [39].- Optimize the type and concentration of stabilizers/surfactants. |
| Poor Colloidal Stability (Aggregation) | - Low surface charge (low zeta potential).- Inadequate steric stabilization.- Storage conditions (e.g., temperature, ionic strength). | - Purify nanoparticles to remove unbound stabilizers.- Introduce PEG or other steric stabilizers [33].- Store nanoparticles in deionized water at 4°C and avoid freeze-thaw cycles. |
| Unexpected Cytotoxicity | - Cytotoxicity of unreacted reagents or solvents.- Cationic surface charge causing membrane disruption.- Rapid release of high local doses of AMP. | - Improve purification (dialysis, tangential flow filtration) to remove residuals [33].- Modify surface charge to neutral or slightly negative.- Reformulate to achieve a more sustained release profile. |
Table 2: Troubleshooting Functional Performance Issues
| Problem | Possible Causes | Suggested Solutions |
|---|---|---|
| Short Circulation Time | - Rapid clearance by the immune system (MPS).- Large nanoparticle size (>200 nm).- Opsonization. | - PEGylate the nanoparticle surface [34].- Use a biomimetic red blood cell membrane coating [35].- Ensure nanoparticle size is optimally between 10-150 nm. |
| Insufficient Targeted Release | - Lack of specific targeting ligands.- Stimuli-responsive mechanism not activated in target microenvironment.- Ligand density too high or too low. | - Conjugate specific targeting moieties (e.g., antibodies, peptides) [15].- Characterize the target site's pH, enzyme, or redox conditions and tailor the responsive material accordingly [37].- Optimize ligand density during conjugation chemistry. |
| Loss of AMP Bioactivity | - Harsh synthesis conditions (organic solvents, sonication) denature AMP.- Undesirable interactions with the nanoparticle matrix. | - Use mild preparation methods like nanoprecipitation or ionic gelation where possible [36].- Consider pre-loading stabilizers (e.g., albumin) to protect the AMP. |
Experimental Protocols
Protocol 1: Preparation of AMP-Loaded PLGA Nanoparticles via Double Emulsion (W/O/W) Solvent Evaporation
This method is ideal for encapsulating hydrophilic antimicrobial peptides [33] [36].
1. Materials:
- Polymer: PLGA (e.g., 50:50 lactide:glycolide, MW 10-30 kDa).
- Solvent: Dichloromethane (DCM) or Ethyl Acetate.
- Aqueous Phases: Primary (W1): AMP dissolved in deionized water. Secondary (W2): Surfactant solution (e.g., 1-5% PVA, polyvinyl alcohol) in water.
- Equipment: Probe sonicator, magnetic stirrer, centrifugation.
2. Step-by-Step Workflow:
- Primary Emulsion (W1/O): Dissolve 100 mg PLGA in 2 mL DCM. Add 0.5 mL of the aqueous AMP solution (W1). Probe sonicate this mixture on ice (e.g., 50-100 W for 30-60 sec) to form a stable water-in-oil (W1/O) emulsion.
- Secondary Emulsion (W1/O/W2): Immediately pour the primary emulsion into 20 mL of the external aqueous PVA solution (W2). Vigorously stir or sonicate again to form a double emulsion (W1/O/W2).
- Solvent Evaporation: Stir the double emulsion at room temperature for 4-6 hours to allow the organic solvent to evaporate and the nanoparticles to harden.
- Collection & Purification: Centrifuge the nanoparticle suspension (e.g., 20,000 rpm, 30 min) to pellet the nanoparticles. Wash the pellet 2-3 times with deionized water to remove PVA and unencapsulated AMP.
- Storage: Re-suspend the final nanoparticle pellet in a suitable buffer (e.g., PBS) and store at 4°C.
The following diagram illustrates the key stages of this synthesis method.
Protocol 2: Biomimetic Coating of Inorganic Nanoparticles with Cell Membranes
This protocol describes coating pre-synthesized inorganic nanoparticles (e.g., gold, silica) with a natural cell membrane to prolong circulation [35].
1. Materials:
- Source Cells: Red blood cells (RBCs) or macrophages.
- Inorganic Nanoparticles: Pre-synthesized and characterized nanoparticles (e.g., ~100 nm).
- Buffers: Hypotonic lysing buffer, PBS (phosphate-buffered saline).
- Equipment: Extruder with polycarbonate membranes, centrifugation.
2. Step-by-Step Workflow:
- Membrane Derivation: Isolate the desired cells (e.g., from whole blood). Lyse the cells in a hypotonic buffer and centrifuge to separate the membrane fraction from intracellular contents. Wash the derived membranes repeatedly.
- Membrane Vesicle Formation: Sonicate the membrane fragments and extrude them through a porous membrane (e.g., 400 nm) to form cell-membrane-derived vesicles.
- Fusion/Coating: Co-incubate the cell membrane vesicles with the inorganic nanoparticles. Subject the mixture to repeated extrusion through a smaller pore membrane (e.g., 100-200 nm). The mechanical force induces fusion, resulting in the cell membrane forming a continuous lipid bilayer around the nanoparticle core.
- Purification: Use density gradient centrifugation to isolate the successfully coated nanoparticles from free membrane fragments and uncoated nanoparticles.
Visualization: Nanoparticle Engineering and Characterization Workflow
The following diagram outlines a logical workflow for developing and evaluating advanced nanoparticle formulations for targeted AMP delivery, integrating key concepts from stability enhancement and targeted release.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Formulation and Functionalization
| Category & Item | Function/Benefit | Key Considerations |
|---|---|---|
| Polymers | ||
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable, biocompatible synthetic polymer; allows sustained release; degradation rate tunable by LA:GA ratio [33] [36]. | Acidic degradation products may affect some AMPs. |
| PCL (Poly(ε-caprolactone)) | Slower degrading polyester than PLGA; suitable for long-term delivery [33]. | Slower drug release profile. |
| Chitosan | Natural, mucoadhesive polymer; promotes penetration at mucosal surfaces; cationic for complexation with nucleic acids or negative charges [36]. | Requires dissolution in acidic conditions; solubility varies with degree of deacetylation. |
| Lipids & Surfactants | ||
| DSPE-PEG | Phospholipid-PEG conjugate; used for PEGylation to create stealth nanoparticles and prolong circulation [35] [34]. | PEG chain length (e.g., PEG-2000, PEG-5000) impacts stealth properties. |
| CTAB (Cetyltrimethylammonium bromide) | Cationic surfactant; commonly used as a stabilizing and shape-directing agent in gold nanorod synthesis [38]. | Requires careful removal due to cytotoxicity. |
| PVA (Polyvinyl Alcohol) | Stabilizer and emulsifying agent in solvent evaporation methods; prevents nanoparticle aggregation during formation [33]. | Residual PVA can affect surface properties and cellular interactions. |
| Functionalization Agents | ||
| EDC/NHS (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide / N-Hydroxysuccinimide) | Carboxyl-to-amine crosslinkers; standard chemistry for conjugating targeting ligands (peptides, antibodies) to nanoparticle surfaces [38] [15]. | Reaction must be performed in aqueous buffers at controlled pH. |
| Maleimide-PEG-NHS | Heterobifunctional crosslinker; allows coupling between amine-containing nanoparticles and thiol-containing ligands (e.g., cysteine-terminated peptides) [15]. | Thiol groups must be reduced and free for reaction. |
| Characterization Tools | ||
| Dynamic Light Scattering (DLS) | Instrument for measuring nanoparticle hydrodynamic size, size distribution (PDI), and aggregation state in solution [33]. | Sensitive to dust and impurities in sample. |
| Zeta Potential Analyzer | Measures surface charge of nanoparticles; key indicator of colloidal stability and potential for protein adsorption [33] [38]. | Measurement is sensitive to pH and ionic strength of the medium. |
Antimicrobial peptides (AMPs) are considered potent tools for combating resistant bacterial infections due to their broad-spectrum antibacterial effects and unique membrane-disrupting mechanisms [40] [10]. However, their clinical translation faces significant challenges, including limited stability, susceptibility to enzymatic degradation, cytotoxicity, and poor pharmacokinetic properties [40] [10] [2]. These limitations result in a narrow therapeutic window and reduced in vivo efficacy, despite promising in vitro activity [2].
Hydrogel-based delivery systems present a promising strategy to overcome these challenges by providing localized, sustained release of AMPs directly at infection sites [41] [42]. These highly hydrated polymer networks protect labile AMPs from degradation, reduce systemic toxicity, and maintain therapeutic concentrations within the therapeutic window for extended periods [41] [42]. This technical resource provides practical guidance for researchers developing hydrogel-AMP formulations, addressing common experimental challenges through troubleshooting guides and detailed methodologies.
Mechanisms of Hydrogel Protection and Sustained Release
Hydrogels protect AMPs and control their release through several interconnected mechanisms:
Molecular Stabilization
Anionic polysaccharides in hydrogel formulations (e.g., xanthan gum, hyaluronic acid, propylene glycol alginate) significantly decrease the degradation rate of AMPs like vancomycin and daptomycin by electrostatic interactions between the ionizable amine groups of the drugs and the anionic carboxylate groups of the polysaccharides [43]. This creates a microenvironment where water molecules have lower mobility and reduced thermodynamic activity, thereby slowing hydrolytic degradation [43].
Controlled Release Mechanisms
- Diffusion-Controlled Release: Drug molecules diffuse from regions of high concentration through the gel matrix, with release rates dependent on mesh size and porosity [44] [42].
- Swelling-Controlled Release: The drug is dispersed within glassy hydrogel polymers that swell upon contact with biofluids, releasing the drug during chain relaxation [44].
- Affinity-Based Release: Specific interactions (electrostatic, hydrophobic, covalent) between the AMP and polymer chains provide additional control over release kinetics [42].
Table 1: Hydrogel Mechanisms for Addressing AMP Limitations
| AMP Limitation | Hydrogel Protection Mechanism | Technical Outcome |
|---|---|---|
| Enzymatic degradation | Physical barrier against proteases | Increased half-life in biological environments |
| Rapid clearance | Sustained, controlled release | Maintained therapeutic concentration |
| Cytotoxicity | Localized delivery | Reduced systemic exposure |
| Chemical instability | Protective microenvironment | Enhanced shelf-life and in vivo stability |
Quantitative Stabilization Data: Polysaccharide Hydrogels
Recent research has quantified the stabilization effects of various anionic polysaccharides on AMP degradation:
Table 2: Stabilization of Antimicrobial Peptides by Polysaccharide Hydrogels
| Polysaccharide | Antimicrobial Peptide | Degradation Rate Constant (kobs, day⁻¹) | Half-Life (days) | Stabilization Effect |
|---|---|---|---|---|
| Buffer (pH 7.4) | Vancomycin | 5.5 × 10⁻² | 13.9 | Baseline |
| Xanthan Gum | Vancomycin | 2.1 × 10⁻² | 33.0 | 2.6-fold improvement |
| Hyaluronic Acid | Vancomycin | 2.3 × 10⁻² | 30.1 | 2.3-fold improvement |
| PGA | Vancomycin | 2.2 × 10⁻² | 31.5 | 2.4-fold improvement |
| Dextran | Vancomycin | 4.4 × 10⁻² | 15.8 | Minimal effect |
| Alginic Acid | Vancomycin | 5.4 × 10⁻² | 12.8 | No effect |
| Buffer (pH 7.4) | Daptomycin | 5.6 × 10⁻² | 12.4 | Baseline |
| Xanthan Gum | Daptomycin | 2.1 × 10⁻² | 33.0 | 2.7-fold improvement |
| PGA | Daptomycin | 2.3 × 10⁻² | 30.1 | 2.4-fold improvement |
| Hyaluronic Acid | Daptomycin | 7.2 × 10⁻² | 9.6 | Destabilization |
Data adapted from research on anionic polysaccharides for stabilization and sustained release of antimicrobial peptides [43].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Hydrogel-AMP Formulation Development
| Reagent Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Natural Polymers | Alginate, Chitosan, Hyaluronic Acid, Collagen, Gelatin | Biocompatible hydrogel base materials | Provide innate bioactivity; may require chemical modification for optimal controlled release [41] |
| Synthetic Polymers | Poly(ethylene glycol), Poly(vinyl alcohol), Poly(acrylic acid) | Tunable hydrogel matrices with controlled properties | Offer precise control over mechanical properties and degradation rates [41] [42] |
| Crosslinkers | Glutaraldehyde, Genipin, Methacrylates, EDAC | Create 3D network structure | Crosslinking density directly controls mesh size and drug release kinetics [41] |
| Stabilizing Agents | Xanthan Gum, Propylene Glycol Alginate | Enhance AMP stability in formulation | Electrostatic interactions with AMPs reduce degradation rates [43] |
| Characterization Reagents | Triton X-100, PBS, Enzymes (e.g., lysozyme) | Assess release profiles and stability | Simulate physiological conditions for in vitro testing [41] |
Experimental Protocol: Hydrogel Formulation and Characterization
Hydrogel Preparation with AMP Encapsulation
Materials: Selected polymer (e.g., alginate, PEG), crosslinker, AMP solution, buffer (PBS, pH 7.4), mixing apparatus.
Method:
- Polymer Solution Preparation: Dissolve polymer in buffer at 2-10% (w/v) with continuous stirring until fully hydrated and clear [41].
- Drug Incorporation: Add AMP solution (1-10 mg/mL final concentration) to polymer solution under gentle mixing to avoid denaturation [44].
- Crosslinking:
- Curing: Maintain at room temperature for 1-24 hours based on crosslinking kinetics [41].
Troubleshooting Tip: If AMP activity decreases significantly after encapsulation, verify that crosslinking chemistry doesn't modify critical amino acid residues in the peptide sequence.
In Vitro Release Kinetics Assessment
Materials: Phosphate buffered saline (PBS), protease solutions (e.g., trypsin), Franz diffusion cells, UV-Vis spectrophotometer or HPLC.
Method:
- Sample Preparation: Precisely cut hydrogel discs (e.g., 10mm diameter × 2mm thickness) [41].
- Release Study Setup: Immerse samples in release medium (PBS, pH 7.4, 37°C) with mild agitation (50-100 rpm) [41].
- Sampling Protocol: Withdraw aliquots (200-500 μL) at predetermined intervals (0.5, 1, 2, 4, 8, 12, 24, 48, 72 hours) and replace with fresh medium [41].
- Drug Quantification:
- Data Analysis: Calculate cumulative release and fit to kinetic models (zero-order, first-order, Higuchi, Korsmeyer-Peppas) [41].
Diagram 1: Experimental workflow for hydrogel formulation and characterization
Troubleshooting Guide: Common Challenges and Solutions
FAQ 1: How can I reduce burst release from my hydrogel system?
Problem: Initial rapid drug release (burst release) depletes a significant portion of the AMP before sustained release begins, potentially causing local toxicity and reducing long-term efficacy [45].
Solutions:
- Increase crosslinking density to reduce mesh size and slow diffusion (e.g., increase crosslinker concentration by 25-50%) [44] [42].
- Implement composite systems by pre-encapsulating AMPs in nanocarriers (e.g., liposomes) before incorporating into hydrogels [45].
- Utilize affinity-based interactions between AMP and polymer chains (e.g., heparin-binding peptides with sulfated polysaccharides) [42].
- Apply coating layers with lower porosity on the hydrogel surface to create a diffusion barrier [44].
FAQ 2: What approaches improve encapsulation efficiency for hydrophobic AMPs?
Problem: Conventional hydrogels primarily encapsulate hydrophilic compounds, leading to low loading capacity for hydrophobic AMPs [45].
Solutions:
- Use liposomal hydrogels where hydrophobic AMPs are loaded into lipid bilayers before hydrogel incorporation [45].
- Employ polymer-drug conjugates where hydrophobic AMPs are covalently attached to hydrogel polymers via cleavable linkers [44].
- Implement mixed micelle-hydrogel systems that solubilize hydrophobic AMPs in micelle cores within the hydrogel matrix [45].
- Modify hydrogel polymers with hydrophobic domains that interact with hydrophobic AMPs through affinity interactions [42].
FAQ 3: How can I enhance the stability of AMPs in hydrogel formulations?
Problem: AMPs may degrade during storage or after administration, reducing therapeutic efficacy [43] [2].
Solutions:
- Select appropriate polysaccharide stabilizers based on quantitative stabilization data (see Table 2) [43].
- Modify peptide structure by incorporating D-amino acids or cyclization to reduce protease susceptibility before encapsulation [2].
- Optimize storage conditions including pH control, antioxidants, and temperature based on the specific AMP's degradation pathways [41].
- Use desiccated hydrogels that are rehydrated immediately before application to minimize hydrolysis during storage [41].
FAQ 4: How do I control release duration for different infection timelines?
Problem: Release kinetics need matching to specific infection types, ranging from acute (days) to chronic (weeks) [42].
Solutions:
- Modulate hydrogel degradation rate by selecting polymers with appropriate hydrolysis profiles (e.g., fast-degrading: gelatin; slow-degrading: PEG) [44] [42].
- Utilize multi-mechanism systems that combine diffusion-controlled release initially with degradation-controlled release later [44].
- Implement layered hydrogels with sequential degradation profiles for programmed pulsatile release [42].
- Incorporate stimulus-responsive elements that accelerate release in response to infection biomarkers (e.g., pH, enzymes) [44].
Diagram 2: Troubleshooting guide for common hydrogel-AMP formulation challenges
Advanced Applications: Nanocarrier-Hydrogel Composite Systems
For challenging AMP delivery scenarios, composite systems offer enhanced functionality:
Liposome-Hydrogel Composites
These systems provide hierarchical control over drug release, where the hydrogel sustains liposome diffusion, followed by drug release from liposomes [45]. This approach significantly extends release duration - in one study, cumulative release from liposomal scaffolds plateaued 144 hours longer than scaffolds containing the drug alone [45].
3D-Printed Hydrogel Systems
Additive manufacturing enables precise spatial control over AMP distribution within hydrogels, allowing for:
- Geometric control of release kinetics through designed macroporous structures [45].
- Multi-drug combinations with independent release profiles for combination therapies [45].
- Patient-specific implants customized to infection site anatomy [45].
Characterization Techniques for Hydrogel-AMP Systems
Essential Analytical Methods:
- Rheological Analysis: Measures storage (G') and loss (G") moduli to characterize mechanical properties and crosslinking density [43] [41].
- Mesh Size Determination: Calculated from swelling ratio and polymer volume fraction, or measured directly by NMR techniques [42].
- Drug Release Kinetics: Quantified using UV-Vis, HPLC, or fluorescence spectroscopy with appropriate calibration curves [41].
- Stability Assessment: Monitor AMP integrity after encapsulation and release using HPLC-MS or gel electrophoresis [41].
- Antimicrobial Activity Testing: Compare MIC values before and after encapsulation to confirm maintained efficacy [10].
When developing hydrogel-based delivery systems for antimicrobial peptides, methodical optimization of formulation parameters is essential. By applying the troubleshooting strategies and experimental protocols outlined in this technical resource, researchers can systematically address the stability challenges that have impeded clinical translation of AMP therapeutics, paving the way for more effective treatments against antibiotic-resistant infections.
Fusion Protein Technologies and Molecular Engineering for Improved Pharmacokinetics
Within antimicrobial peptide (AMP) research, a significant translational challenge lies in overcoming inherent instability and pharmacokinetic shortcomings. Fusion protein technologies have emerged as a powerful molecular engineering strategy to address these issues. By genetically fusing AMPs to carrier protein domains, researchers can markedly enhance peptide stability, reduce proteolytic degradation, and improve bioavailability. This technical support center provides targeted guidance for troubleshooting experimental hurdles in developing these advanced therapeutic constructs, directly supporting the broader thesis of achieving stable, clinically viable AMP formulations.
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: Which fusion tag should I select to minimize antimicrobial peptide toxicity during heterologous expression?
Challenge: The inherent toxicity of AMPs to microbial expression hosts (e.g., E. coli) leads to poor cell viability and low protein yields.
Solution: The choice of fusion tag is critical for shielding the host from the AMP's activity. Below is a comparison of commonly used tags:
Table 1: Comparison of Fusion Tags for AMP Expression
| Fusion Tag | Mechanism to Reduce Toxicity | Key Advantages | Reported Yield in AMP Production |
|---|---|---|---|
| DAMP4 | Forms a stable, soluble helical bundle that sequesters the AMP [46]. | Enables non-chromatographic purification via heat/salt precipitation; allows acid cleavage [46]. | ~29.3 mg/L of Kiadin peptide [46]. |
| SUMO | Enhances solubility and correct folding, masking the AMP's activity [47]. | Highly specific cleavage by SUMO proteases; improves solubility and yield [47]. | Information Missing |
| TrxA | Acts as a solubility enhancer, reducing AMP aggregation and toxicity. | Widely used in E. coli; can improve disulfide bond formation [46]. | Information Missing |
| GST | Large, soluble tag that dilutes the local concentration of the toxic AMP. | Allows purification via glutathione-affinity chromatography. | Information Missing |
Troubleshooting Guide:
- If host cell growth is still impaired: Consider using a tighter, inducible promoter system (e.g., T7 lac) to prevent leaky expression before induction.
- If the fusion protein is insoluble: Screen different tags (e.g., from GST to SUMO or DAMP4), lower the expression temperature, or use a host strain engineered for disulfide bond formation.
FAQ 2: How can I efficiently cleave and purify the AMP from the fusion tag without using expensive proteases?
Challenge: Enzymatic cleavage (e.g., with TEV or SUMO protease) is highly specific but adds significant cost, especially for large-scale production.
Solution: Integrate acid-cleavable linkers into your fusion construct. The peptide bond between Aspartic Acid (D) and Proline (P) is uniquely labile under mild acidic conditions.
Detailed Protocol: Acid Cleavage of DPS Linker Fusion Proteins [46]
- Construct Design: Genetically fuse your AMP to the carrier protein (e.g., DAMP4) via a DPS (Asp-Pro-Ser) tripeptide linker sequence.
- Purify Fusion Protein: First, purify the intact fusion protein using standard methods (e.g., affinity or the heat/salt precipitation method enabled by the DAMP4 tag).
- Acid Cleavage Reaction:
- Resuspend the purified fusion protein in an acidic buffer. Formic acid (e.g., 70-75% v/v) is commonly used and effective [46].
- Incubate the mixture at an elevated temperature (e.g., 37-45°C) for a defined period (e.g., 4-24 hours). Optimization of time and temperature is required for maximum yield.
- Separate and Recover AMP:
- The DAMP4 carrier protein is highly stable and will precipitate under these acidic conditions.
- Separate the precipitated carrier from the soluble AMP by centrifugation.
- The supernatant containing the released AMP can be further purified, often via isoelectric precipitation or reverse-phase HPLC, to achieve high purity (>96%) [46].
Troubleshooting Guide:
- If cleavage efficiency is low: Systematically optimize the acid concentration, temperature, and incubation time. Ensure the linker sequence is correctly encoded and accessible.
- If the AMP is degraded: Test shorter incubation times or milder acid conditions. Some AMPs are inherently stable across a wide pH and temperature range, making them ideal for this method [46].
FAQ 3: What strategies can I use to extend the plasma half-life of my therapeutic AMP beyond fusion tags?
Challenge: Even after successful expression and cleavage, small AMPs can be rapidly cleared by renal filtration and proteolysis in vivo.
Solution: Fusion and conjugation strategies that increase the hydrodynamic radius of the peptide are highly effective. The table below compares key technologies:
Table 2: Strategies for Prolonging the Plasma Half-Life of Proteins and Peptides
| Strategy | Mechanism of Action | Key Considerations | Clinical Example |
|---|---|---|---|
| Fc Fusion | Binds to the neonatal Fc receptor (FcRn), recycling the protein back into circulation and reducing degradation [48] [49]. | Significantly increases half-life; can confer effector functions. | Etanercept (TNF-R/Fc) [50] [49]. |
| PEGylation | Covalent attachment of polyethylene glycol (PEG) increases size and sterically shields from proteases and kidneys [51] [52]. | Risk of losing bioactivity; can induce anti-PEG antibodies leading to "accelerated blood clearance" [51]. | PEGylated interferon alpha-2a [52]. |
| HSA Fusion | Fusion to Human Serum Albumin (HSA) exploits its long native half-life via FcRn recycling [52]. | A large tag that may affect the bioactivity of the fused partner. | Albiglutide (GLP-1/HSA fusion) [48]. |
| PASylation | Fusion with a polypeptide chain of Pro, Ala, and Ser (PAS) creates a "cloud-like" hydrodynamic volume [52]. | Unstructured, flexible tag that avoids pre-existing immunity. | In clinical development. |
Troubleshooting Guide:
- If the fusion protein loses antimicrobial activity: The large size of Fc or HSA may sterically block the AMP's interaction with microbial membranes. Consider using a flexible or cleavable linker to improve accessibility.
- If immunogenicity is a concern: PEGylation can sometimes trigger an immune response. PASylation or human protein-based fusions (like HSA) may be less immunogenic alternatives.
Experimental Workflow and Protocol
This section provides a detailed, citable protocol for the biosynthesis and purification of an AMP using the DAMP4 fusion and acid-cleavage system, a method highlighted for its cost-effectiveness and high yield [46].
Title: Workflow for AMP Biosynthesis via DAMP4 Fusion
Diagram Specification:
Title: AMP Action Mechanisms
Diagram Specification:
Protocol: High-Level Biosynthesis of Kiadin Antimicrobial Peptide [46]
Objective: To express, cleave, and purify the antimicrobial peptide Kiadin using a DAMP4 fusion system in E. coli, achieving high purity and yield while mitigating host toxicity.
Construct Design and Cloning:
- Design a synthetic gene encoding the fusion protein: M-(EPS-MKQLADSLHQLARQVSRLEHA)₄-D-P-S-Kiadin-HH.
- The C-terminal histidine residues mitigate hydrolysis risks. Clone this gene into a standard expression vector (e.g., pET-28a).
Expression in E. coli:
- Transform the construct into an appropriate E. coli host strain (e.g., BL21(DE3)).
- Induce expression with 1 mM IPTG. The DAMP4 tag sequesters the Kiadin domain, preventing host toxicity and allowing high-level expression.
Non-Chromatographic Purification of Fusion Protein:
- Lyse the cells and centrifuge to obtain the soluble fraction.
- Utilize the thermal and saline stability of DAMP4: incubate the lysate at high temperature and salt concentration. This precipitates host proteins while the DAMP4–DPS–Kiadin fusion remains soluble.
- Centrifuge to recover the soluble fusion protein from the precipitate of host contaminants.
Acid Cleavage and Final Purification:
- Resuspend the purified fusion protein in 70% (v/v) formic acid.
- Incubate at 37-45°C for 4-24 hours to cleave the acid-labile Asp-Pro (D-P) bond in the DPS linker.
- The DAMP4 tag will precipitate under these conditions. Separate it from the soluble Kiadin peptide by centrifugation.
- Subject the supernatant containing Kiadin to isoelectric precipitation or reverse-phase HPLC to achieve final purity (>96%). The reported yield using this method is 29.3 mg/L of bacterial culture [46].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Fusion Protein Development for AMPs
| Reagent / Material | Function / Purpose | Key Considerations |
|---|---|---|
| DAMP4 Tag | Fusion partner for toxicity mitigation and non-chromatographic purification [46]. | Enables cost-effective, scalable production via heat/salt precipitation and acid cleavage. |
| SUMO Tag | Fusion partner for enhancing solubility and enabling high-specificity cleavage [47]. | Requires costly SUMO protease for cleavage but often provides high yields of soluble protein. |
| Acid-Cleavable Linker (DPS) | A specific peptide sequence (Asp-Pro-Ser) that allows tag release under mild acidic conditions [46]. | A low-cost alternative to enzymatic cleavage; requires optimization of acid concentration and temperature. |
| pET Expression Vectors | A family of high-expression plasmids for use in E. coli with T7/lac promoter system. | Standard workhorse for recombinant protein expression; offers tight control over induction. |
| E. coli BL21(DE3) | A robust and widely used host strain for protein expression, deficient in proteases. | Suitable for a wide range of fusion proteins; other strains may be needed for disulfide-rich proteins. |
| Formic Acid | Acidic reagent used to cleave the DPS linker and release the target AMP from the fusion tag [46]. | Handling requires appropriate personal protective equipment (PPE) in a fume hood. |
| Nickel-NTA Resin | Affinity chromatography resin for purifying polyhistidine (His)-tagged proteins. | Useful for initial capture if a His-tag is incorporated into the fusion construct. |
Rational Design and Cutting-Edge Optimization of Stable AMPs
Welcome to this technical support center, dedicated to sequence-based engineering of peptides, with a specific focus on modulating two critical parameters: amphipathicity and hydrophobicity. This resource is framed within the broader thesis of addressing pervasive stability issues in antimicrobial peptide (AMP) formulations. A primary challenge in AMP development lies in balancing potent antibacterial activity with low toxicity toward host cells and sufficient stability in biological environments. This guide provides researchers, scientists, and drug development professionals with targeted troubleshooting advice and detailed methodologies to overcome common experimental hurdles in the rational design of more stable and effective therapeutic peptides.
Frequently Asked Questions (FAQs) & Troubleshooting
Design and Property Calculation
Q1: How can I quickly estimate the key physicochemical properties of a newly designed peptide sequence?
A: Computational tools are essential for initial property estimation before synthesis.
- Problem: Manual calculation of mean hydrophobicity and amphipathic moment is prone to error.
- Solution: Utilize established online servers.
- HeliQuest: This server is highly recommended for α-helical peptides. It calculates mean hydrophobicity
, the amphipathic moment <µH>, and generates a helical wheel diagram to visualize the spatial distribution of hydrophobic and hydrophilic residues [53] [54]. - NSP@ Server: Use this server for predicting secondary structure, such as helicity, from the amino acid sequence [53].
- HeliQuest: This server is highly recommended for α-helical peptides. It calculates mean hydrophobicity
- Troubleshooting: If your peptide shows poor amphipathicity in the helical wheel projection, consider mutating residues to improve the segregation of hydrophobic and hydrophilic faces. Substituting with residues of higher helical propensity (e.g., Glu over Thr) can also enhance stability [54].
Q2: My peptide is designed to be amphipathic but shows low experimental helicity. What could be the reason?
A: This is a common issue often related to sequence-specific "helix breakers" or terminal charge effects.
- Problem: The presence of residues like proline (Pro) or multiple glycine (Gly) residues can disrupt α-helical formation [54].
- Solution:
- Sequence Mutation: Identify and mutate helix-breaking residues (e.g., Pro to Leu or Ala) with residues known for high helical former propensity [54].
- Terminal Capping: Modify the peptide termini. N-terminal acetylation and C-terminal amidation can shield the charged terminal groups, which stabilizes the helical dipole and significantly increases helical content [54].
Activity and Selectivity
Q3: My peptide has strong antimicrobial activity but is also highly hemolytic. How can I improve its selectivity?
A: This indicates a poor selectivity window, often due to excessive hydrophobicity or unbalanced amphipathicity.
- Problem: High hydrophobicity can lead to non-selective interaction with neutral mammalian membranes (e.g., red blood cells) [55].
- Solution:
- Reduce Hydrophobicity: Systematically replace highly hydrophobic residues in the non-polar face (e.g., Phe, Leu) with less hydrophobic ones (e.g., Ala, Ser). Note that this must be balanced to maintain sufficient activity [56].
- Increase Positive Charge: Incorporating more arginine (Arg) residues has been shown to be superior to lysine (Lys) in enhancing bactericidal activity and selectivity, likely due to improved interaction with bacterial membranes [53].
- Post-Translational Modification: Phosphorylation is a recently demonstrated strategy that can significantly reduce hemolytic activity and cytotoxicity (e.g., 19-fold reduction in hemolysis) while maintaining or only slightly reducing antimicrobial efficacy [57].
- Computational Prediction: Use machine learning tools like HEPAD to predict the hemolytic potential of your peptide sequences early in the design process, allowing you to filter out problematic candidates before synthesis [55].
Q4: How can I enhance the conformational stability of my AMP in biological fluids?
A: Poor stability leads to rapid degradation and short half-lives.
- Problem: Unmodified linear peptides are often susceptible to proteolytic degradation [58].
- Solution:
- Terminal Modifications: As in Q2, N-terminal acetylation and C-terminal amidation not only enhance helicity but also protect against exoproteases [54].
- Introduce Disulfide Bonds: For peptides with β-sheet or specific loop structures, engineering disulfide bonds can rigidify the structure and improve stability [58].
- Phosphorylation: This modification has been shown to dramatically improve serum stability, with one study reporting a 6.3-fold longer serum half-life for a phosphorylated peptide analog [57].
- Nanoparticle Incorporation: Encapsulating or conjugating AMPs onto nanoparticles can shield them from enzymatic degradation and improve their pharmacokinetics [58].
Experimental Characterization
Q5: What is a direct method to confirm that my peptide interacts with and disrupts bacterial membranes?
A: Atomic force microscopy (AFM) is a powerful technique for this purpose.
- Problem: Indirect assays (e.g., viability) do not confirm the mechanism of action.
- Solution: Atomic Force Microscopy (AFM). This technique allows for the high-resolution imaging of bacterial cells before and after peptide treatment. A successful membrane-disruptive action will manifest as visible pits, cracks, or full-scale rupture on the bacterial surface, providing direct physical evidence of the peptide's effect [53].
Data Presentation: Quantitative Effects of Sequence Engineering
Table 1: Impact of Residue Substitutions on Peptide Self-Assembly Propensity
Data derived from systematic substitution in an Ac-(AKAE)2-NH2 peptide, which does not self-assemble on its own [56].
| Substituted Residues | Hydrophobicity / Side Chain Size | Self-Assembly Outcome | Key Insight |
|---|---|---|---|
| Double Phe | Moderate / Aromatic | Failed to assemble | Hydrophobicity of Phe is insufficient in this context. |
| Double 1-Nal / 2-Nal | High / Large Aromatic | Readily assembled | Larger, more hydrophobic aromatic rings promote assembly. |
| Double Cha | High / Aliphatic | Effective assembly | High hydrophobicity (aliphatic) is sufficient, even without aromaticity. |
| Double F5-Phe | Very High / Aromatic | Most efficient assembly | Extreme hydrophobicity and electronic properties enhance assembly. |
Table 2: Rational Design of a Peptide Series to Enhance Helical Stability and Activity
Data showing the step-wise improvement of a parent peptide (P01) through mutations and terminal capping [54].
| Peptide | Sequence Modifications | Net Charge | <µH> (Amphipathic Moment) | MIC vs S. aureus (μg/mL) | |
|---|---|---|---|---|---|
| P01 (Parent) | Native sequence | +2 | 0.550 | 0.246 | >250 |
| P01.1 | Mutations (N3I, T6I, A8K, P9K) + C-term amidation | +6 | 0.396 | 0.746 | >250 |
| P01.2 | P01.1 + N-term acetylation | +5 | 0.396 | 0.746 | 125 |
| P01.3 | P01.2 + T5E mutation | +4 | 0.321 | 0.821 | 15.63 |
Experimental Protocols
Protocol 1: Measuring Peptide Secondary Structure via Circular Dichroism (CD) Spectroscopy
Principle: CD measures the differential absorption of left- and right-handed circularly polarized light, providing information on a peptide's secondary structure in solution.
Methodology [54]:
- Sample Preparation:
- Dissolve the purified peptide in a suitable buffer (e.g., 10 mM sodium phosphate buffer, pH 7.0-7.4).
- Prepare a sample for a baseline scan containing only buffer.
- A common practice is to perform a Titration with Trifluoroethanol (TFE). Prepare a series of samples with increasing TFE concentrations (0%, 10%, 20%, 30%, 50% v/v). TFE mimics a membrane-like environment and can induce/intensify helical signals.
- Instrumentation and Data Acquisition:
- Use a spectropolarimeter calibrated with a standard (e.g., ammonium d-10-camphorsulfonate).
- Use a quartz cuvette with a short path length (e.g., 0.1 cm or 1 mm).
- Set the temperature (e.g., 25°C).
- Scan from 260 nm to 190 nm (or as low as the instrument permits) with appropriate bandwidth, step resolution, and speed.
- Perform multiple scans and average them to improve the signal-to-noise ratio.
- Data Analysis:
- Subtract the buffer baseline from the peptide spectrum.
- For α-helical structures, look for characteristic minima at 222 nm (n-π* transition) and 208 nm (π-π* transition), and a maximum around 190 nm.
- The mean residue ellipticity (MRE) at 222 nm, [θ]222, is a key indicator of helical content.
- Calculate the fractional helicity (fH) using the formula:
fH = (-[θ]222 + 3000) / 39000where [θ]222 is the measured mean residue ellipticity at 222 nm in deg·cm²·dmol⁻¹.
Protocol 2: Evaluating Bactericidal Activity and Mammalian Cell Toxicity
A. Bactericidal Assay [53]
- Bacterial Culture: Grow test bacteria (e.g., E. coli, S. aureus) to mid-logarithmic phase in an appropriate broth.
- Cell Washing: Harvest bacteria by centrifugation (e.g., 5,000 rpm), wash twice with phosphate-buffered saline (PBS, pH 7.4), and resuspend in PBS.
- Peptide Treatment: Incubate the bacterial inoculum (e.g., 5 x 10⁵ CFU/mL) with serial dilutions of the peptide (e.g., 6.25 to 50 µM) for a set time (e.g., 2 hours) at 37°C.
- Viability Assessment: After incubation, dilute the samples and spread them on LB-agar plates. Incubate overnight at 37°C and count the resulting colonies.
- Calculation:
- % Survival = (Colonies from peptide-treated sample / Colonies from negative control) x 100%
B. Hemolysis Assay [53]
- Erythrocyte Preparation: Collect fresh whole blood and centrifuge to separate red blood cells (RBCs). Wash the RBCs with PBS until the supernatant is clear.
- Peptide Treatment: Prepare a 1-5% (v/v) suspension of RBCs in PBS. Mix with the peptide to the desired final concentration (e.g., 50 µM). Incubate at 37°C with gentle shaking (e.g., 35 minutes).
- Measurement: Centrifuge the samples (e.g., 2,000 rpm for 10 minutes) to pellet intact RBCs.
- Analysis: Carefully transfer the supernatant to a new plate and measure its absorbance at 540 nm (the Soret band of hemoglobin).
- Controls and Calculation:
- Negative Control (0% Hemolysis): RBCs in PBS only.
- Positive Control (100% Hemolysis): RBCs in 1% Triton X-100.
- % Hemolysis = [(Abssample - Absnegative) / (Abspositive - Absnegative)] x 100%
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Computational Tools for AMP Engineering
| Item / Reagent | Function / Application | Example / Specification |
|---|---|---|
| F-moc Solid-Phase Synthesis | Standard method for chemical peptide synthesis. | Automated peptide synthesizer (e.g., Applied Biosystems 433A). |
| Reverse-Phase HPLC | Purification of synthetic peptides. | C18 column with water/acetonitrile gradient. Purity should be >95% [53]. |
| Trifluoroethanol (TFE) | Helix-inducing solvent for CD spectroscopy. | Used to mimic membrane environment and assess helical propensity [54]. |
| Langmuir Trough | Study peptide-lipid monolayer interactions. | Measures binding to model bacterial membranes [54]. |
| HeliQuest Server | Computational calculation of |
Critical for in silico design of amphipathic helices [53] [54]. |
| HEPAD Predictor | Machine learning-based identification of hemolytic peptides. | Used to filter out toxic candidates early in the design pipeline [55]. |
| N-terminal Acetyl Group | Chemical modification to stabilize helix and improve stability. | Protects from aminopeptidases and neutralizes positive charge [54]. |
| C-terminal Amide Group | Chemical modification to stabilize helix and improve stability. | Protects from carboxypeptidases and neutralizes negative charge [54]. |
Workflow and Relationship Visualizations
Diagram 1: Rational Peptide Design and Optimization Workflow
Diagram 2: Troubleshooting Guide for Common AMP Issues
Frequently Asked Questions (FAQs)
Q1: What are the primary goals of chemically modifying antimicrobial peptides (AMPs)?
The primary goals are to overcome the inherent limitations of natural AMPs for clinical application. These limitations include:
- Low Proteolytic Stability: Susceptibility to degradation by proteases in serum and tissues, leading to a short half-life [14] [59] [60].
- High Toxicity: Undesirable hemolytic activity (damage to red blood cells) and cytotoxicity to host cells [59] [61].
- Low Metabolic Stability: Rapid clearance from the body, often by the kidneys [60].
- Instability of Secondary Structure: Inability to maintain the bioactive conformation (e.g., alpha-helix) required for activity [62].
Chemical modifications are employed to enhance metabolic stability, increase target selectivity, reduce toxicity, and improve overall pharmacokinetic properties [63] [59] [60].
Q2: How does substituting L-amino acids with D-amino acids improve AMP properties?
D-amino acids are the mirror-image enantiomers of naturally occurring L-amino acids. Their incorporation enhances AMPs by:
- Increasing Proteolytic Resistance: Proteases have high substrate specificity for L-amino acids. Substituting them with D-isomers makes the peptide unrecognizable to many proteases, drastically improving stability in serum and other biological fluids [14] [60]. Studies have shown this can extend peptide half-life in plasma by more than 12-fold [61].
- Maintaining Antimicrobial Activity: Peptides with partial or full D-amino acid substitutions can often lyse bacteria as efficiently as their all-L-parent peptides [14].
Q3: What are "stapled peptides" and what advantages do they offer?
Stapled peptides are a class of modified peptides locked into their bioactive secondary structure (often an alpha-helix) through a synthetic brace, known as a "staple" [62] [64]. This staple is typically an all-hydrocarbon crosslink formed between side chains using ring-closing metathesis [62] [64]. The advantages include:
- Enhanced Helical Structure and Stability: The staple stabilizes the helical conformation, preventing unraveling [62].
- Protease Resistance: The stabilized structure and introduction of unnatural elements shield the peptide from proteolytic degradation [62].
- Improved Cellular Penetration: The staple can enhance the ability of the peptide to enter cells [62].
- Increased Biological Activity: By preserving the active conformation, stapling can improve binding affinity to the target and thus potency [62].
Q4: What are non-canonical amino acids (ncAAs) and how are they incorporated into peptides?
Non-canonical amino acids (ncAAs) are amino acids beyond the standard 20 proteinogenic amino acids. They can contain side chains that are chemically and structurally distinctive, introducing novel properties [63]. Key methods for their incorporation are:
- Solid-Phase Peptide Synthesis (SPPS): This is the major chemical strategy, allowing for complete control over peptide assembly and the incorporation of multiple, distinct ncAAs at any desired position [63] [65].
- Genetic Code Expansion (GCE): A biosynthetic technique that allows for the site-specific incorporation of ncAAs into proteins and peptides during translation by engineering aminoacyl-tRNA synthetase/tRNA pairs [63].
Q5: Besides stapling and D-amino acids, what other chemical modifications are useful for AMPs?
Several other modifications are commonly used to enhance AMP performance:
- N-terminal Acetylation and C-terminal Amidation: These modifications remove charged termini, mimicking natural peptides, increasing stability against exopeptidases, and improving cell permeability [65] [61] [60].
- PEGylation: Covalent attachment of polyethylene glycol (PEG) polymers. This increases the peptide's hydrodynamic size, slowing renal clearance and protecting it from proteolytic enzymes. It can also reduce immunogenicity [64] [60].
- Lipidation: The addition of fatty acid chains (e.g., myristic, palmitic acid) can enhance membrane interaction and increase half-life by promoting binding to serum albumin [61] [60].
- Cyclization: Creating a cyclic structure by linking the peptide's N- and C-termini or side chains can enhance conformational stability and resistance to proteolysis [65] [64].
Troubleshooting Guides
Issue 1: AMP is Unstable in Serum
Problem: Your antimicrobial peptide is rapidly degraded when incubated in serum or plasma, leading to a loss of activity.
Possible Causes and Solutions:
| Cause | Solution | Experimental Example to Try |
|---|---|---|
| Susceptibility to proteases | Incorporate D-amino acids at specific cleavage sites or use a full D-enantiomer approach. | Synthesize a variant where L-amino acids at predicted protease-sensitive sites are replaced with their D-enantiomers. Test stability in fetal calf serum compared to the parent peptide [14]. |
| Susceptibility to exopeptidases | Protect the peptide termini via N-terminal acetylation and C-terminal amidation. | Synthesize the peptide with an acetylated N-terminus and an amidated C-terminus. Compare half-life in plasma to the unmodified version [61] [60]. |
| Low inherent conformational stability | Apply a stapling technique to stabilize the peptide's secondary structure. | Design a peptide with olefin-bearing ncAAs (e.g., S-pentenylalanine) at i, i+4 or i, i+7 positions. Perform ring-closing metathesis to form the staple. Analyze helicity by CD spectroscopy and test protease resistance [62]. |
Decision Diagram:
Issue 2: AMP has High Hemolytic Activity
Problem: Your peptide shows strong antimicrobial activity but also causes significant lysis of red blood cells, indicating high toxicity.
Possible Causes and Solutions:
| Cause | Solution | Experimental Example to Try |
|---|---|---|
| Excessive hydrophobicity | Reduce overall hydrophobicity by substituting hydrophobic residues with polar/charged ones or shortening the peptide. | Create a truncated version of the peptide. Compare the hemolytic activity (IC50 for red blood cells) and antimicrobial activity (MBC) to calculate an improved selectivity index [61]. |
| Poor charge/hydrophobicity balance | Fine-tune amphipathicity by increasing the net positive charge or redistributing hydrophobic residues. | Replace a neutral residue with a cationic one (e.g., Lysine or Arginine) to increase charge without altering hydrophobicity. Measure hemolysis and antimicrobial activity [59] [61]. |
| Specific residue toxicity | Avoid modifications that are known to increase hemolysis, such as very long N-terminal acyl chains or certain substitutions. | If a peptide with a long-chain N-terminal acyl group (e.g., myristylation) shows high hemolysis, revert to an acetyl group or shorter chain [61]. |
Decision Diagram:
Issue 3: Low Bioavailability and Rapid Clearance
Problem: The peptide is effective in vitro but shows poor in vivo efficacy due to rapid clearance from the bloodstream.
Possible Causes and Solutions:
| Cause | Solution | Experimental Example to Try |
|---|---|---|
| Rapid renal clearance of small peptides | Increase the peptide's effective size by PEGylation or conjugation to larger proteins like albumin. | Conjugate a linear PEG polymer (e.g., 5-40 kDa) to the N-terminus of the peptide. Compare the pharmacokinetic profile and half-life in an animal model to the unmodified peptide [64] [60]. |
| Instability in physiological buffers | Improve enzymatic and chemical stability through backbone N-methylation or cyclization. | Synthesize a cyclic version of the peptide via a disulfide bond between cysteine residues or a lactam bridge. Test stability in various pH buffers and in serum [60]. |
Table 1: Impact of Common Modifications on Key AMP Properties
This table summarizes quantitative data from research findings on how different modifications affect AMP performance.
| Modification Type | Proteolytic Stability (Half-Life) | Antimicrobial Activity (MBC in μg/mL) | Hemolytic Activity (HC50 in μg/mL) | Key Reference Findings |
|---|---|---|---|---|
| D-Amino Acid Substitution | >12-fold increase in plasma half-life [61] | Unchanged or slightly improved (e.g., 4 μg/mL for A. baumannii) [14] [61] | Generally unchanged or improved (reduced hemolysis) [14] | Peptides with D-amino acids were highly stable to trypsin and serum proteases [14]. |
| Stapling (Hydrocarbon) | Significantly increased resistance to tryptic degradation [62] | Maintained or enhanced; dependent on staple position [62] | Variable; can be optimized by staple design [62] | Stapling locks alpha-helical structure, enhancing proteolytic resistance and target binding [62]. |
| N-acetylation / C-amidation | Moderate increase via exopeptidase protection [60] | Maintained [61] | Maintained [61] | Standard modification to mimic native peptides and block terminal degradation [65] [61]. |
| PEGylation | 5.86-fold increase in half-life reported for HM-3 peptide [60] | May slightly decrease due to steric hindrance | Generally decreased (reduced hemolysis) [64] | Increases molecular size, reducing renal filtration and shielding from proteases [64] [60]. |
| Peptide Shortening | Not directly assessed | Maintained (e.g., PepD3 vs. PepD2) [61] | Increased IC50 (reduced toxicity); SI improved from 4.7 to 8.5 [61] | Shorter peptides can reduce synthetic complexity and unwanted hydrophobicity [61]. |
Table 2: Research Reagent Solutions for Peptide Modification
| Reagent / Material | Function / Role | Application Example |
|---|---|---|
| Fmoc-protected D-amino acids | Building blocks for SPPS to create protease-resistant sequences [14]. | Substituting L-Lys and L-Leu with D-enantiomers to enhance plasma stability [61]. |
| Olefinic ncAAs (e.g., S-pentenylalanine) | Incorporated into peptide chains for subsequent stapling via RCM [62] [64]. | Creating i, i+4 or i, i+7 staples in alpha-helical peptides to stabilize structure [62]. |
| Ring-Closing Metathesis (RCM) Catalyst (e.g., Grubbs' Catalyst) | Facilitates the formation of the all-hydrocarbon staple between olefinic side chains [62]. | Used in solid-phase or solution-phase to macrocyclize the resin-bound or free peptide [62]. |
| PEG Reagents (e.g., mPEG-ald) | Covalently linked to peptides to increase hydrodynamic radius and stability [64] [60]. | N-terminal PEGylation of the HM-3 peptide to extend its circulatory half-life [60]. |
| N-terminal Acylation Reagents (e.g., Acetic Anhydride, Myristic Acid) | Blocks N-terminus, increases hydrophobicity, or promotes albumin binding [61]. | Acetylation with acetic anhydride is standard; long-chain acids (myristic) can enhance half-life but may increase hemolysis [61]. |
Detailed Experimental Protocols
Protocol 1: Enhancing Proteolytic Stability via D-Amino Acid Substitution using SPPS
This protocol outlines the synthesis of a D-amino acid-containing AMP analog.
- Peptide Design: Identify protease-sensitive sites (e.g., via mass spectrometry analysis of degradation products) or select key residues for substitution. Decide on partial or global D-substitution.
- Solid-Phase Synthesis:
- Use a peptide synthesizer and Rink Amide AM resin to achieve a C-terminal amidation [61].
- Employ the Fmoc-protection strategy. Use standard Fmoc-L-amino acids for unmodified positions and Fmoc-D-amino acids for the targeted substitutions.
- Perform iterative cycles of: a. Deprotection: Remove the Fmoc group with 30% (v/v) piperidine in DMF [61]. b. Coupling: Activate the next Fmoc-amino acid (4 equivalents) with HBTU (4 equivalents) in the presence of N-methyl morpholine. Couple to the free amine on the resin [61].
- N-terminal Modification: After the final deprotection, acetylate the N-terminus using acetic anhydride (4 equivalents) instead of an Fmoc-amino acid [61].
- Cleavage and Deprotection: Cleave the peptide from the resin and remove side-chain protecting groups by treating with a cocktail of trifluoroacetic acid (TFA)/water/ethanedithiol (95/2.5/2.5% v/v/v) for 2-4 hours at room temperature [61].
- Precipitation and Purification:
- Precipitate the crude peptide in cold methyl tert-butyl ether (MTBE).
- Centrifuge and wash the pellet.
- Purify the peptide using reversed-phase high-performance liquid chromatography (RP-HPLC) with a C18 column [61].
- Characterization: Verify the identity and purity of the final product using matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry [61].
Protocol 2: Stabilizing Alpha-Helical Structure via Hydrocarbon Stapling
This protocol describes the process of creating a stapled peptide.
- Peptide Design and Synthesis:
- Design the peptide sequence to include olefin-bearing ncAAs (e.g., (S)-N-Fmoc-2-(4'-pentenyl)alanine) at i and i+4 or i and i+7 positions to stabilize an alpha-helix.
- Synthesize the linear, resin-bound peptide using standard Fmoc-SPPS, incorporating the olefinic ncAAs at the designated positions.
- Ring-Closing Metathesis (RCM):
- While the peptide is still on the resin, swell the peptide-resin in an inert solvent (e.g., dichloroethane, DCE).
- Add a solution of a Grubbs metathesis catalyst (e.g., Grubbs 1st or 2nd generation catalyst) under an inert atmosphere (e.g., nitrogen or argon).
- Agitate the reaction mixture for 2-24 hours at room temperature to facilitate the staple formation [62] [64].
- Cleavage and Purification:
- Cleave the stapled peptide from the resin using a standard TFA-based cocktail.
- Precipitate, purify via RP-HPLC, and characterize by MALDI-TOF MS as described in Protocol 1.
- Validation:
- Use Circular Dichroism (CD) Spectroscopy to confirm the increase in alpha-helicity compared to the unstapled control.
- Perform a tryptic stability assay by incubating both stapled and unstapled peptides with trypsin and analyzing the degradation over time by HPLC or MS.
Workflow Diagram: Stapled Peptide Synthesis
Leveraging AI and Machine Learning for Predictive Peptide Design
Antimicrobial peptides (AMPs) are short amino acid sequences, typically 12 to 50 residues long, that serve as a first-line defense in the innate immune response of all classes of life [66] [67]. These cationic and amphiphilic molecules demonstrate broad-spectrum activity against various bacteria, viruses, and fungi, primarily through mechanisms that disrupt microbial membranes [68] [67]. Their potential as next-generation therapeutics is particularly valuable in an era of rising antimicrobial resistance, which accounts for over 1.27 million deaths globally each year [69].
Despite this promise, the translation of AMPs from laboratory research to clinical applications has been slow. A major hindrance is their inherent instability under physiological conditions [21] [70]. Bare AMPs often show limited activity following topical application due to their susceptibility to environmental factors like hydrolysis, oxidation, and photolysis, as well as wound-specific conditions such as alkaline pH and proteolysis [70]. Furthermore, their short elimination half-life and potential toxicity, including severe hemolytic activity, have limited the number of FDA-approved AMPs [68] [21]. Overcoming these stability issues is a central challenge that modern research, powered by artificial intelligence (AI) and machine learning (ML), aims to solve.
AI and ML Fundamentals for Peptide Design
Machine learning, a subset of AI, provides a suite of computational techniques that can learn patterns from complex datasets. In the context of AMP design, these approaches are broadly categorized into three learning types [69]:
- Supervised Learning: Used when the outputs (labels) are known for the input data. For AMPs, this includes:
- Classification: Predicting a category, such as whether a peptide is antimicrobial or not.
- Regression: Predicting a continuous value, such as the minimum inhibitory concentration (MIC).
- Unsupervised Learning: Used to discern patterns in inputs without pre-existing labels. This includes clustering to group similar peptide sequences or representation learning to extract meaningful features from raw sequences.
- Reinforcement Learning (RL): An agent (ML model) generates peptide sequences and receives continuous feedback (reward), such as predicted antimicrobial activity. The model dynamically adjusts its strategy to maximize future rewards, gradually learning to generate sequences with more desirable properties [69].
These methods enable the rapid in-silico exploration of a vast peptide sequence space, which is impractical to test empirically. AI models can predict biomolecular properties and structures, and generate novel peptide candidates with optimized stability, reduced toxicity, and enhanced efficacy [69] [71].
Key AI Model Architectures and Workflows
The following diagram illustrates a generalized workflow for AI-driven predictive peptide design, integrating the core ML categories and validation steps.
Troubleshooting Guide: Common Experimental Issues and AI-Driven Solutions
This section addresses specific challenges researchers may encounter during AMP development and outlines how AI methodologies can provide solutions.
FAQ 1: How can I improve the proteolytic stability of my lead AMP candidate?
The Problem: Your peptide shows good in-vitro antimicrobial activity but degrades rapidly in biological fluids (e.g., serum), leading to a short half-life and diminished efficacy.
AI-Driven Solutions:
- Strategic Peptide Engineering: Use ML models trained on protease cleavage sites and peptide stability data. These models can identify unstable motifs (e.g., susceptible amide bonds) in your sequence and suggest stabilising modifications [21].
- Incorporation of Non-Canonical Amino Acids: Reinforcement learning algorithms can guide the substitution of L-amino acids with D-amino acids or other non-canonical residues. This strategy makes the peptide less recognizable to proteases without compromising its antimicrobial activity [21].
- Cyclization: AI can help design cyclic peptide scaffolds, which are inherently more rigid and resistant to proteolytic degradation compared to their linear counterparts [21].
Experimental Protocol: Simulated Gastric Fluid (SGF) Stability Assay
- Preparation: Dissolve pepsin in 0.1 M HCl (pH ~1.2) to create SGF.
- Incubation: Add your AMP candidate to the SGF at 37°C. Use a control sample in a neutral pH buffer.
- Sampling: Withdraw aliquots at regular time intervals (e.g., 0, 15, 30, 60, 120 minutes).
- Analysis: Quench the reaction and analyze the samples using Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) or Mass Spectrometry (MS) to quantify the intact peptide remaining.
- Validation: Compare the degradation profile of the original peptide with its AI-redesigned variants.
FAQ 2: My AMP is highly hemolytic. Can AI help reduce its toxicity while retaining potency?
The Problem: The peptide's hydrophobicity, which often correlates with membrane disruption, also causes unwanted lysis of human red blood cells.
AI-Driven Solutions:
- Multi-Objective Optimization: Employ ML frameworks that simultaneously optimize for multiple properties. You can train a model to maximize antimicrobial activity (low MIC) while minimizing hemolytic activity [69] [71].
- Charge and Hydrophobicity Fine-Tuning: AI models can learn the complex relationship between a peptide's net charge, hydrophobic moment, and selectivity for bacterial vs. mammalian membranes. They can then suggest mutations that fine-tune these physicochemical properties to enhance selectivity [69] [21].
Experimental Protocol: Hemolysis Assay
- Cell Preparation: Collect fresh human red blood cells (RBCs) and wash them with phosphate-buffered saline (PBS) until the supernatant is clear.
- Treatment: Incubate a 2-4% RBC suspension with a serial dilution of your AMP (e.g., 1-200 µM) for 1 hour at 37°C. Include controls: PBS for 0% hemolysis (negative) and 1% Triton X-100 for 100% hemolysis (positive).
- Measurement: Centrifuge the samples and measure the hemoglobin release in the supernatant by absorbance at 540 nm.
- Calculation: Calculate the percentage hemolysis for each concentration and determine the HC50 (concentration causing 50% hemolysis). The goal is to have an HC50 significantly higher than the therapeutic MIC.
FAQ 3: My AMP loses activity in the presence of serum or salts. What can I do?
The Problem: Serum and physiological salt concentrations can neutralize the electrostatic interactions between the cationic peptide and the anionic bacterial membrane, a phenomenon known as salt sensitivity.
AI-Driven Solutions:
- Feature Analysis for Salt Resistance: Train ML classifiers to identify sequence-level features and patterns that distinguish salt-resistant AMPs from salt-sensitive ones in curated databases [72].
- De Novo Design of Salt-Resistant Peptides: Use generative models, like variational autoencoders (VAEs) or generative adversarial networks (GANs), to create entirely new peptides that are intrinsically more stable in high-salt and serum conditions, as informed by the features learned [69].
Experimental Protocol: Serum & Salt Sensitivity MIC Assay
- Media Preparation: Prepare Mueller-Hinton Broth (MHB) supplemented with different concentrations of NaCl (e.g., 0, 50, 100, 150 mM) or with various percentages of serum (e.g., 0%, 10%, 25%, 50%).
- MIC Determination: Perform a standard broth microdilution MIC assay against your target bacteria in the prepared media.
- Analysis: Compare the MIC values in the presence and absence of salt/serum. A significant increase in MIC indicates sensitivity. Use this data to validate and retrain your AI models.
FAQ 4: How can I formulate my AMP for topical delivery to enhance its stability and residence time?
The Problem: The bare peptide is unstable and gets cleared too quickly from the wound site when applied topically.
AI-Driven Solutions:
- Predicting Peptide-Material Compatibility: While an emerging field, ML can help select optimal biomaterials for formulation by predicting interactions between peptide sequences and polymer/excipient chemistries.
- Optimizing Release Kinetics: Data-driven models can help design nanoparticle or hydrogel formulations that provide controlled, sustained release of the AMP, thereby enhancing its stability and prolonging its action at the wound site [71] [70].
Experimental Protocol: Formulation in Hydrogel and Release Kinetics
- Hydrogel Preparation: Incorporate your AMP into a biocompatible hydrogel (e.g., chitosan, alginate, or enzyme-responsive hydrogels).
- Release Study: Immerse the peptide-loaded hydrogel in a release buffer (e.g., PBS, pH 7.4) at 37°C under gentle agitation.
- Sampling and Analysis: Collect release medium at predetermined time points and replenish with fresh buffer. Quantify the released peptide using HPLC or a fluorescence-based assay.
- Efficacy Testing: Test the antimicrobial efficacy of the formulated AMP directly against biofilms in an in-vitro wound model.
The table below lists key reagents, databases, and computational tools essential for AI-driven AMP research.
Table 1: Research Reagent Solutions for AI-Driven AMP Development
| Category | Item/Resource | Function & Application in AMP Research |
|---|---|---|
| Databases | APD3, DBAASP, CAMP [69] | Curated repositories of known AMP sequences, structures, and activity data for model training and validation. |
| In-Vitro Assay Kits | Hemolysis Assay Kit | Standardized kit for quantifying peptide toxicity against red blood cells. |
| LAL Endotoxin Assay Kit | Critical for detecting and quantifying endotoxins in peptide samples for in-vivo studies. | |
| Live/Dead Bacterial Staining Kit | Fluorescence-based kit to visualize and quantify bactericidal effects of AMPs. | |
| Formulation Materials | Chitosan, Alginate, Hyaluronic Acid [70] | Natural polymers used to create hydrogels for topical AMP delivery, enhancing stability and residence time. |
| PLGA Nanoparticles [70] | Biocompatible, biodegradable nanoparticles for encapsulating AMPs to control release and protect from degradation. | |
| Computational Tools | AlphaFold [73] | Protein structure prediction tool for understanding peptide 3D conformation. |
| PepPrCLIP, RFDiffusion [74] | Examples of AI platforms specifically designed for peptide-protein interaction prediction and de novo peptide design. |
Data Presentation: Quantitative Insights from Research and Clinical Trials
Quantitative data is crucial for benchmarking and setting realistic goals for AMP development. The tables below summarize key metrics from recent AI-driven discoveries and approved peptide therapeutics.
Table 2: Experimentally Validated AMPs Discovered via AI/ML Approaches
| Reference (Method) | Number of Validated AMPs | Antimicrobial Activity (MIC Range) | Studied Bacteria | Toxicity Range |
|---|---|---|---|---|
| Nagarajan et al. (Neural Language Model) [69] | 10 (in vitro) / 1 (in mice) | ≤128 µg/mL | 30 pathogens including A. baumannii | LD50 ~213–224 µg/g in mice |
| Porto et al. (Genetic Algorithm) [69] | 8 (in vitro) / 1 (in mice) | 6.25–100 µg/mL | E. coli, S. aureus, P. aeruginosa | HC50 & CC50 >200 µM |
| Tucs et al. (Generative Adversarial Network) [69] | 5 (in vitro) | 3.1–50 µg/mL | E. coli | Not Tested (N.T.) |
| Capecchi et al. (Neural Language Model) [69] | 8 (in vitro) | ≤64 µg/mL | E. coli, S. aureus, P. aeruginosa | ≥500 µg/mL (Min. Hemolytic Conc.) |
Table 3: Properties of Selected FDA-Approved Antimicrobial Peptides
| Peptide Name (FDA Approval Year) | Sequence Length (Amino Acids) | Net Charge | Hydrophobic Content | Elimination Half-Life | Primary Indication |
|---|---|---|---|---|---|
| Daptomycin (2003) [21] | 13 | 0 (neutral) | High (Lipopeptide) | 8-9 hours | Complicated skin infections, S. aureus bacteremia |
| Oritavancin (2014) [21] | N/A (Lipoglycopeptide) | N/A | N/A | 14 days | Acute bacterial skin and skin structure infections |
| Telavancin (2009) [21] | N/A (Lipoglycopeptide) | N/A | N/A | ~195 hours (8 days) | Complicated skin and skin structure infections |
| Colistin (1962) [21] | 10 | +6 | 20% | 5 hours | Infections caused by Gram-negative bacteria |
High-Throughput Screening Methods for Assessing Stability and Toxicity
Frequently Asked Questions: Core Concepts
What is High-Throughput Screening (HTS) and how is it applied in toxicology? High-Throughput Screening (HTS) is a method that uses automated equipment, robotics, data processing software, and sensitive detectors to quickly conduct millions of chemical, genetic, or pharmacological tests [75]. In toxicology, HTS allows researchers to rapidly test thousands of environmental chemicals, pharmaceutical compounds, and industrial chemicals for various toxicological endpoints such as genotoxicity, cytotoxicity, and endocrine disruption [76]. This approach provides a cost-effective and time-saving alternative to traditional animal-based toxicity testing methods [77] [76].
How does HTS support chemical prioritization for regulatory decisions? HTS assays are used as tools for chemical prioritization rather than direct replacements for regulatory guideline animal-based tests [78]. Under the assumption that only a minority of chemicals will cause any specific adverse effect, HTS assays identify chemicals most likely to cause particular adverse effects. These chemicals can then be prioritized for more expensive, low-throughput animal-based guideline bioassays [78]. The U.S. EPA employs this approach through programs like ToxCast (Toxicity Forecaster), which uses high-throughput bioactivity profiling to predict toxicity potential [77] [79].
What are the key advantages of HTS over traditional toxicity testing methods? HTS offers several significant advantages over traditional toxicity testing methods, which are summarized in the table below:
Table: Advantages of High-Throughput Screening Over Traditional Methods
| Aspect | High-Throughput Screening | Traditional Methods |
|---|---|---|
| Throughput | Can test 10,000-100,000 compounds per day [75] [80] | Limited to much smaller numbers of compounds over longer timeframes |
| Cost | More cost-effective due to automation and miniaturization [76] [80] | Resource-intensive and expensive [78] |
| Animal Use | Reduces reliance on animal testing [77] [76] | Primarily rely on animal studies [78] |
| Mechanistic Insight | Provides clear mechanistic insight into toxicity pathways [78] | Often limited in providing mechanistic clarity [78] |
| Data Generation | Generates quantitative, reproducible read-outs [78] | Results may be more qualitative and variable |
What are New Approach Methods (NAMs) and how do they relate to HTS? New Approach Methods (NAMs) are broadly defined as any technology, methodology, approach, or combination that does not use vertebrate animals to provide information on chemical hazard and risk assessment [77]. HTS research develops and applies these NAMs to reduce animal use for testing thousands of chemicals, including Chemicals of Immediate and Emerging Concern such as per- and polyfluoroalkyl substances (PFAS) and chemical mixtures [77]. The EPA's Safer Chemicals Researchers use high-throughput toxicology, including high-throughput phenotypic profiling and high-throughput transcriptomics, to test hundreds of PFAS for potential toxicity [77].
Troubleshooting Common Experimental Issues
How can I address false positives and false negatives in HTS assays?
Table: Common HTS Artifacts and Resolution Strategies
| Problem Type | Common Causes | Solutions |
|---|---|---|
| False Positives | Assay interference, compound impurities, non-specific effects [76] | Use orthogonal assays, test compounds at multiple concentrations, apply more stringent hit selection criteria [76] |
| False Negatives | Low compound solubility, instability, sub-optimal assay conditions [76] | Optimize compound solubility, ensure proper storage conditions, validate assay conditions [76] |
| Assay Interference | Compound fluorescence, quenching, chemical reactivity with assay components [81] | Include appropriate controls, use counter-screens, employ multiple detection methods [81] |
What quality control metrics should I implement to ensure HTS assay reliability? Implement robust quality control metrics to identify assays with inferior data quality. The Z'-factor has become a widely accepted criterion for evaluation and validation of high-throughput screening assays [82]. Other quality-assessment measures include signal-to-background ratio, signal-to-noise ratio, signal window, assay variability ratio, and strictly standardized mean difference (SSMD) [75]. These metrics measure the degree of differentiation between positive controls and negative references, which is an index for good quality [75]. For HTS assays used in prioritization, relevance is demonstrated through the ability to detect key events with documented links to adverse outcomes and the ability to reproduce data and respond appropriately to carefully selected reference compounds [78].
How can I optimize assay conditions for better HTS performance? Assay conditions such as cell density, reagent concentrations, and incubation times must be optimized to ensure optimal performance in the high-throughput format [76]. Optimization involves testing different assay parameters and evaluating their impact on assay sensitivity, signal-to-background ratio, and reproducibility. Design of experiments (DOE) approaches can be used to systematically optimize assay conditions and minimize the number of experiments required [76]. Additionally, proper plate design helps identify systematic errors (especially those linked with well position) and determines what normalization should be used to remove/reduce the impact of systematic errors on both quality control and hit selection [75].
Experimental Protocols & Methodologies
What are the essential components of an HTS workflow? A typical HTS workflow consists of several integrated components that enable efficient and reliable testing of large numbers of compounds [75] [76]:
HTS Experimental Workflow
What specific HTS assays are available for different toxicological endpoints?
Table: HTS Assays for Key Toxicological Endpoints
| Toxicological Endpoint | HTS Assay Examples | Application in Stability & Toxicity Assessment |
|---|---|---|
| Cytotoxicity | Cell viability assays (e.g., Promega CellTiter-Glo Luminescent Cell Viability Assay) [76] | Measures cellular metabolic activity as an indicator of cell viability and compound cytotoxicity |
| Genotoxicity | Ames II and Ames Liquid Format Mutagenicity Screening Assays [79], Vitotox Assay [79] | Detects DNA damage and mutagenic potential of chemical compounds |
| Skin Sensitization | Keratinosens Assay [79] | Assesses chemical potential to cause skin sensitization |
| Developmental Toxicity | Embryonic Stem Cell Test (EST) [79], ReProGlo Assay [79] | Predicts embryotoxic potential of chemicals using stem cells |
| Endocrine Disruption | DR-CALUX reporter gene assay [79] | Detects dioxin and dioxin-like compounds that disrupt endocrine function |
| Phototoxicity | High-throughput screening assays for chemical phototoxicity [79] | Evaluates compound toxicity enhanced by light exposure |
| Receptor-Mediated Toxicity | High-throughput yeast-based assays [79] | Studies toxicity mediated through specific receptor interactions |
How do I implement dose-response experiments for hit confirmation? After initial screening, conduct dose-response experiments to determine the potency and efficacy of selected hits by measuring their activity across a range of concentrations [76]. Compounds are typically tested in a 10-point, 3-fold dilution series, spanning several orders of magnitude in concentration [76]. Dose-response curves are fitted to the data using nonlinear regression models, such as the four-parameter logistic equation, to estimate key parameters including IC50 (half-maximal inhibitory concentration) or EC50 (half-maximal effective concentration) [76]. Quantitative HTS (qHTS), developed by scientists at the NIH Chemical Genomics Center, represents an advanced paradigm that pharmacologically profiles large chemical libraries through the generation of full concentration-response relationships for each compound [75].
Data Analysis & Hit Selection Protocols
What statistical methods are appropriate for hit selection in HTS? The analytic methods for hit selection in screens without replicates differ from those with replicates [75]. For primary screens without replicates, the z-score method or SSMD is appropriate, though these methods are sensitive to outliers [75]. As a consequence, robust methods such as the z-score method, SSMD, B-score method, and quantile-based method have been proposed and adopted for hit selection [75]. In screens with replicates, you can directly estimate variability for each compound and should use SSMD or t-statistic that doesn't rely on the strong assumption that z-score methods require [75]. For hit selection, the major interest is the size of effect in a tested compound, and SSMD directly assesses the size of effects [75].
How should I handle and normalize large HTS datasets? Raw screening data must be normalized to account for plate-to-plate variability and systematic errors, such as edge effects or signal drift [76]. Common normalization methods include percent of control, Z-score, and robust Z-score, which express compound activity relative to positive and negative controls [76]. Data management software is crucial for organizing, analyzing, and interpreting the large amounts of data generated by HTS experiments [76]. These software tools can automatically extract data from plate readers, perform quality control checks, and apply statistical analyses to identify hits and evaluate assay performance [76]. Examples of data management software include Genedata Screener and Dotmatics Studies [76].
What is the pathway from HTS hit to confirmed lead compound? The process from initial screening to confirmed lead involves multiple stages of validation and testing, as illustrated below:
HTS Hit Confirmation Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Research Reagent Solutions for HTS in Stability & Toxicity Testing
| Reagent/Material | Function | Examples & Specifications |
|---|---|---|
| Microtiter Plates | Testing vessel for HTS assays | 96, 384, 1536-well plates; proper surface treatment for cell adherence when needed [75] [80] |
| Compound Libraries | Collections of small molecules for screening | Diversity libraries, targeted libraries, natural product libraries; quality controlled via LC-MS/NMR [76] |
| Cell Lines | Biological systems for toxicity assessment | Human cell lines (primary cells or cell lines); stem cell-derived models for organ-specific toxicity [78] [80] |
| Detection Reagents | Enable measurement of biological responses | Fluorescence, luminescence, absorbance-based reagents (e.g., Promega CellTiter-Glo) [76] [83] |
| Enzymes & Proteins | Targets for biochemical assays | High-purity enzymes (e.g., tyrosine kinase); quality controlled to prevent contamination [80] |
| Automated Liquid Handlers | Precise dispensing of reagents and compounds | Tecan Freedom EVO, Beckman Coulter Biomek FX; handle nanoliter to microliter volumes [76] |
| Plate Readers | Detect signals from assay plates | Fluorescence, luminescence, absorbance capabilities; compatible with high-density microplates [76] |
Advanced Applications & Emerging Technologies
How can I implement high-content screening for cytotoxicity assessment? High-content screening (HCS) combines HTS with high-resolution imaging and automated image analysis to extract multiple parameters from cell-based assays at a single-cell level [79] [83]. Implement HCS using the following workflow:
- Cell Preparation: Seed cells in 384-well imaging-compatible microplates at optimized density
- Compound Treatment: Use automated liquid handling to treat cells with test compounds across desired concentration ranges
- Staining: Apply fluorescent dyes or antibodies to mark cellular structures or specific targets
- Image Acquisition: Use automated high-content imagers such as the Molecular Devices ImageXpress Micro system [76]
- Image Analysis: Extract multiparametric data including cell morphology, protein localization, and subcellular changes
HCS enables the assessment of multiple toxicity pathways simultaneously, providing richer data than single-endpoint assays [79].
What emerging technologies are shaping the future of HTS in toxicity testing? The field of HTS continues to evolve with several emerging technologies. Quantitative HTS (qHTS) generates full concentration-response relationships for entire chemical libraries, enabling more robust pharmacological profiling [75]. Drop-based microfluidics allows screening that is 1,000 times faster and one-millionth the cost of conventional techniques by using drops of fluid separated by oil to replace microplate wells [75]. Advances in stem cell biology, particularly human embryonic stem cells (hESC) and induced pluripotent stem cells (iPSC), introduce new opportunities for toxicity testing using human-derived models that are compatible with industrial HTS formats [80]. Additionally, CRISPR/dCas-based screens provide powerful new tools for target deconvolution after hit discovery using phenotypic screens [83].
Bench to Bedside: Evaluating Efficacy and Clinical Translation Status
In Vitro and In Vivo Models for Assessing Formulation Stability and Efficacy
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: What are the fundamental differences between in vitro and in vivo models, and why are both necessary in AMP development?
Answer: In vitro and in vivo models serve complementary roles in the drug development pipeline. In vitro models involve experiments conducted outside a living organism, such as in petri dishes or test tubes, using isolated cells, tissues, or organs [84]. In vivo models involve testing within a whole, living organism to study complex biological interactions in real-time [84] [85].
The table below summarizes their key differences:
| Aspect | In Vitro Models | In Vivo Models |
|---|---|---|
| Definition | Studies in a controlled lab environment [85] | Studies within a living organism [85] |
| System Complexity | Simplified, isolated components (cells, tissues) [84] | Whole-organism, multi-system interactions [84] [85] |
| Cost & Resources | Lower cost; fewer resources required [85] | High cost due to animal care and specialized facilities [84] [85] |
| Time to Results | Quicker, high-throughput screening possible [84] [85] | Longer duration for studies and analysis [85] |
| Physiological Relevance | Limited; cannot replicate full organism response [84] | High; provides holistic, clinically relevant data [84] [85] |
| Ethical Considerations | Lower; no live animals involved [85] | Higher; involves animal testing and ethical oversight [84] [85] |
Both models are necessary because they answer different questions. In vitro models are excellent for early-stage screening, mechanistic studies, and assessing basic drug characteristics in a controlled, cost-effective manner [84]. In vivo models are indispensable for understanding a drug's systemic effects, including its pharmacokinetics (absorption, distribution, metabolism, and excretion), overall efficacy, and safety profile in a complex living system [84] [85]. Relying solely on in vitro data can be misleading, as it may not predict in vivo outcomes.
FAQ 2: Our AMP shows excellent in vitro efficacy and stability, but fails in animal models. What are the common causes?
Answer: This is a common hurdle in AMP development. Promising in vitro results often do not translate to in vivo success due to the vastly increased complexity of a living organism. The primary causes and their troubleshooting strategies are outlined below.
Troubleshooting Guide: From In Vitro Promise to In Vivo Success
| Problem Area | Common Causes | Troubleshooting Strategies |
|---|---|---|
| Proteolytic Degradation | Susceptibility to proteases in biological fluids (e.g., serum), leading to short half-life [86] [15]. | - Incorporate D-amino acids to create protease-resistant topoisomers (e.g., retroenantio forms) [86].- Use N-terminal acetylation and C-terminal amidation to block exopeptidase action [61]. |
| Systemic Toxicity | Unexpected cytotoxicity or hemolytic activity in a physiological context, not apparent in isolated cell assays [86]. | - Systemically evaluate toxicity in different cell types (e.g., HEK293 cells, red blood cells) during design [61].- Modify peptide sequence to reduce hydrophobicity or cationicity, which can correlate with hemolytic activity [61]. |
| Poor Pharmacokinetics | Rapid clearance from the bloodstream, inability to reach the target site at effective concentrations [21]. | - Optimize peptide length and sequence; shorter peptides may have better selectivity and reduced toxicity [61].- Employ drug delivery systems (e.g., nanoparticles, hydrogels) to improve stability and bioavailability [15] [10]. |
| Lack of Efficacy | The infection microenvironment (e.g., immune components, pH, mucin) can inhibit AMP activity [86]. | - Use infection models that include immunosuppressive agents like mucin to better simulate in vivo conditions [86].- Validate in vivo efficacy in established murine infection models [86]. |
Case Study Example: A study on the snake venom-derived peptide Ctn[15-34] and its retroenantio (re) analog demonstrated this challenge clearly. While the re version showed improved in vitro stability, it was toxic in vivo, causing animal deaths within minutes. In contrast, the native Ctn[15-34] sequence was effective at reducing bacterial loads in a murine infection model without toxicity, underscoring the critical importance of in vivo validation [86].
FAQ 3: What are the key experimental protocols for assessing AMP stability and efficacy across models?
Answer: A systematic, multi-stage approach is required to comprehensively evaluate AMP candidates.
Experimental Protocol 1: In Vitro Plasma/Serum Stability Assay
- Objective: To determine the half-life of an AMP in biological fluids.
- Methodology:
- Incubation: Dilute the synthetic peptide in human or mouse plasma/serum (e.g., at a 1:1 ratio) and incubate at 37°C [61].
- Sampling: Withdraw aliquots at predetermined time points (e.g., 0, 30, 60, 120, 240, 480 minutes).
- Reaction Termination: Precipitate proteins by adding trichloroacetic acid or acetonitrile, then centrifuge to obtain a clear supernatant.
- Analysis: Use reversed-phase high-performance liquid chromatography (RP-HPLC) to quantify the remaining intact peptide. The half-life (t1/2) is calculated from the degradation curve [61].
- Troubleshooting: If stability is low, consider peptide modifications. For example, a study showed that substituting L-amino acids with D-amino acids extended the peptide half-life in plasma by more than 12-fold [61].
Experimental Protocol 2: In Vivo Murine Infection Model for Efficacy
- Objective: To evaluate the therapeutic efficacy of an AMP in a live organism.
- Methodology (Based on an Acinetobacter baumannii model) [86]:
- Infection: Immunosuppress mice by injecting 5% porcine mucin intraperitoneally. Subsequently, inject a standardized inoculum of the pathogen (e.g., 108 CFU/kg of A. baumannii).
- Treatment: Administer the AMP candidate (e.g., via intraperitoneal injection) at a specific dose (e.g., 30 mg/kg for Ctn[15-34]) and schedule post-infection. Include control groups (vehicle-only and a positive control like colistin).
- Monitoring: Observe animals for clinical symptoms (e.g., piloerection, reduced mobility, weight loss) and survival rates over several days.
- Endpoint Analysis: Euthanize animals at the endpoint and harvest target organs (e.g., spleen, liver). Homogenize the organs and plate serial dilutions to quantify bacterial loads (CFU/organ).
- Troubleshooting: If the peptide shows toxicity (e.g., rapid death, severe weight loss), conduct a separate maximum tolerance dose study to establish a safe dosing range before efficacy testing [86].
Visual Guide: The AMP Preclinical Development Workflow
The diagram below summarizes the key stages and decision points in a typical preclinical assessment of an Antimicrobial Peptide.
Visual Guide: Key Stability Challenges for AMPs
This diagram illustrates the primary stability challenges that Antimicrobial Peptides encounter and the corresponding formulation strategies to overcome them.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and reagents used in the featured experiments for AMP development.
| Research Reagent | Function/Application | Example in Context |
|---|---|---|
| Porcine Mucin | An immunosuppressive agent used in murine infection models to enhance susceptibility to bacterial infection [86]. | Added to the bacterial inoculum of A. baumannii in a mouse model to establish a successful infection [86]. |
| Rink Amide AM Resin | A solid support used for Fmoc-based solid-phase peptide synthesis (SPPS), yielding C-terminal amidated peptides [61]. | Used for the synthesis of de novo designed peptides like pepD2; C-terminal amidation protects against exopeptidase degradation [61]. |
| Fmoc-Amino Acid Derivatives | Building blocks for the step-wise synthesis of custom peptide sequences in SPPS [61]. | Used to construct peptides with specific sequences (e.g., W, K, L only) or to incorporate non-canonical or D-amino acids [61]. |
| Matrigel | A tissue-derived extracellular matrix (ECM) hydrogel used for cultivating 3D organoids and complex in vitro models (CIVMs) [87]. | Provides a 3D environment that supports the self-organization of stem cells into organ-specific structures for more physiologically relevant screening [87]. |
| Colistin (Polymyxin E) | A last-resort, FDA-approved cyclic AMP used as a positive control in in vivo efficacy studies against Gram-negative bacteria [86] [21]. | Served as the positive control treatment in a murine A. baumannii infection model, demonstrating a 100% survival rate [86]. |
FAQ 4: What advanced formulation strategies can improve the clinical translation of AMPs?
Answer: To overcome the limitations of natural AMPs, several advanced formulation and delivery strategies are being employed:
| Strategy | Description | Benefit | Clinical Example/Status |
|---|---|---|---|
| Nanoparticles | Inorganic (gold, silica) or organic (lipid, polymer) carriers that encapsulate or conjugate AMPs [15]. | Protects from degradation, improves bioavailability, enables targeted and controlled release [15] [10]. | Melittin-loaded nanoparticles showed reduced hemolysis and controlled release in early cancer trials [10]. |
| Hydrogels | Polymer networks that can absorb aqueous solutions and provide a scaffold for AMP incorporation [15]. | Ideal for topical application (wound dressings); provides sustained release at the infection site [15]. | AMC-109 impregnated in wound dressings/gels showed superior bacterial reduction in skin infection models [88]. |
| Amino Acid Substitution | Replacing L-amino acids with D-amino acids or other unnatural amino acids in the peptide sequence [86] [61]. | Dramatically increases resistance to protease degradation, extending plasma half-life [86] [61]. | Retroenantio topoisomers of Ctn peptides showed >12-fold increased stability in serum [86]. |
| Peptide Cyclization | Creating a circular peptide structure by linking the N- and C-termini or side chains. | Enhances structural rigidity, proteolytic stability, and often improves target binding affinity [21]. | Daptomycin is an FDA-approved cyclic lipopeptide with an elimination half-life of 8-9 hours [21]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Our Antimicrobial Peptide (AMP) shows excellent in vitro efficacy but poor in vivo performance. What could be the cause? A1: This common discrepancy is often due to low bioavailability and poor stability of AMPs in complex physiological environments. In vivo, AMPs face challenges like proteolytic degradation by serum proteases, interaction with serum proteins, and rapid renal clearance. To address this, consider nanoencapsulation strategies. Lipid- or polymer-based nanoparticles can shield AMPs, protect them from degradation, and improve their pharmacokinetic profile [15] [5].
Q2: The AMP formulation we are developing shows signs of cytotoxicity, such as hemolytic activity. How can this be mitigated? A2: Cytotoxicity, particularly hemolysis, is a frequent hurdle with membrane-active AMPs and is often concentration-dependent [2]. Mitigation strategies include:
- Optimizing Hydrophobicity: Reformulate the AMP using a delivery system that allows for a lower effective dose. High hydrophobicity correlates with increased hemolytic activity, which can be managed through careful carrier selection [59] [89].
- Using Targeted Delivery Systems: Employ functionalized nanocarriers (e.g., ligand-targeted liposomes or polymeric nanoparticles) that enhance accumulation at the infection site, thereby reducing systemic exposure and off-target toxicity [15] [90].
Q3: We are encountering rapid degradation of our lead AMP candidate by proteases. What formulation strategies can improve its stability? A3: Protease susceptibility is a major limitation for linear peptides. Effective formulation strategies include:
- Chemical Modification via Delivery Systems: Incorporation into hydrogels or solid lipid nanoparticles provides a physical barrier against proteases [5] [89].
- PEGylation: Conjugating polyethylene glycol (PEG) to the peptide or the nanoparticle surface can sterically hinder protease access and improve biocompatibility [2].
Q4: How can we achieve targeted delivery of AMPs to a specific infection site to improve efficacy and reduce systemic side effects? A4: Targeted delivery can be engineered into your delivery system in several ways:
- Active Targeting: Functionalize the surface of your nanocarrier (e.g., liposome, polymeric NP) with ligands like antibodies or peptides that recognize specific receptors on the target bacterial cells or at the infected tissue [15].
- Stimuli-Responsive Release: Design delivery systems (e.g., certain hydrogels or nanoparticles) that release their AMP payload in response to unique stimuli at the infection site, such as a specific pH or enzyme presence [15].
Q5: What are the key scalability challenges when moving from lab-scale to industrial production of an AMP delivery system? A5: Scalability is a critical bridge between research and clinical application. Key challenges include:
- Reproducibility and Cost: Complex multi-step synthesis of some nanocarriers (e.g., core-shell nanoparticles) can be difficult to reproduce at a large scale and often involves high production costs [90] [5].
- Regulatory Hurdles: Sophisticated delivery systems are classified as "complex products." They require rigorous characterization of critical quality attributes (CQAs) like particle size, distribution, and drug release profile, which complicates the regulatory approval pathway [5].
Table 1: Comparative Analysis of AMP Delivery System Efficacy
This table summarizes the performance of different delivery systems in enhancing AMP efficacy against resistant bacteria, based on recent preclinical studies.
| Delivery System | Example AMP | Target Pathogen | Key Efficacy Outcome | Reported Limitations |
|---|---|---|---|---|
| Gold Nanoparticles (Au-NPs) | HuAL1 [90] | Staphylococcus aureus, Pseudomonas aeruginosa | Conjugated AMP showed higher antimicrobial activity at lower concentrations (1.0-1.2 mg·mL⁻¹) than free AMP [90]. | Potential long-term tissue accumulation; requires rigorous toxicity profiling [90]. |
| Silver Nanoparticles (Ag-NPs) | Lys AB2 P [90] | Multidrug-resistant bacteria | Synergistic action: Ag-NPs cause oxidative stress (ROS), while AMP disrupts membranes [90]. | Silver toxicity (cytotoxicity) is a concern; requires careful dosing [90]. |
| Polymeric Nanoparticles | Not specified (Various) | ESKAPE pathogens [89] | Protects AMP from proteolysis; allows controlled release; can be engineered for intracellular delivery [89]. | Complexity in polymer synthesis and biodegradability; potential polymer-specific inflammation [5] [89]. |
| Lipid Nanoparticles (LNPs) | Not specified (Various) | Systemic infections [89] | High biocompatibility; capable of fusing with bacterial membranes; suitable for mRNA-encoded AMP delivery [89]. | Stability issues during storage (e.g., fusion, drug leakage); scalability can be challenging [89]. |
| Hydrogels | Not specified (Various) | Wound infections [15] [5] | Excellent for topical application; maintains a moist environment; provides sustained release of AMP at the site [15]. | Limited suitability for systemic infections; diffusion rate of AMP can be difficult to control precisely [15]. |
Table 2: Safety and Scalability Profile of AMP Delivery Systems
This table compares the safety, stability, and manufacturing scalability of the primary delivery platforms.
| Delivery System | Safety / Toxicity Concerns | Stability Profile | Scalability & Manufacturing |
|---|---|---|---|
| Inorganic NPs (Au, Ag) | Cytotoxicity (especially Ag-NPs), potential for tissue accumulation, immunogenicity [90]. | High physical stability. Aggregation can be an issue without proper surface coating [90]. | Well-established synthesis methods, but cost of GMP-grade materials can be high [90]. |
| Polymeric NPs | Biocompatibility depends on polymer type (e.g., PLA, PLGA are preferred). Degradation products may cause mild inflammation [5] [89]. | Good shelf-life. Polymer degradation rate in storage must be monitored [89]. | Easily scalable (e.g., emulsion techniques). Reproducible particle size control is key [5]. |
| Lipid-based Systems | Generally low toxicity. High doses can cause transient immune reactions. Lipid composition determines hemocompatibility [89]. | Lower physical stability. Sensitive to temperature and oxidation; requires cold chain storage [89]. | Highly scalable (e.g., high-pressure homogenization). Technology is mature for pharmaceuticals [89]. |
| Hydrogels | Generally very safe. High biocompatibility with natural polymers (e.g., chitosan, alginate) [15]. | Swells with hydration. Mechanical strength and drug release rate can be temperature/pH dependent [15]. | Scaling production of sterile gels is straightforward; batch-to-batch consistency of natural polymers can vary [15]. |
Experimental Protocols
Protocol 1: Formulation and Evaluation of AMP-Loaded Polymeric Nanoparticles
This protocol details the preparation of AMP-encapsulated PLGA nanoparticles using a double emulsion solvent evaporation method, a standard technique for hydrophilic peptides [89].
1. Materials:
- AMP of interest (lyophilized powder)
- PLGA (50:50, acid-terminated)
- Dichloromethane (DCM)
- Polyvinyl Alcohol (PVA)
- Deionized Water
2. Methodology:
- Primary Emulsion (W1/O): Dissolve 100 mg PLGA in 4 mL DCM. Dissolve 10 mg of your AMP in 0.5 mL of deionized water. Add the aqueous AMP solution to the PLGA solution and probe-sonicate on ice for 60 seconds to form a primary water-in-oil (W1/O) emulsion.
- Secondary Emulsion (W1/O/W2): Pour the primary emulsion into 100 mL of a 2% w/v PVA solution under vigorous stirring. Homogenize this mixture for 2-3 minutes to form a double emulsion (W1/O/W2).
- Solvent Evaporation: Stir the double emulsion magnetically at room temperature for 4-6 hours to allow the organic solvent (DCM) to evaporate, solidifying the nanoparticles.
- Purification & Collection: Centrifuge the nanoparticle suspension at high speed (e.g., 20,000 x g for 30 minutes). Wash the pellet twice with deionized water to remove residual PVA and unencapsulated AMP.
- Lyophilization: Re-suspend the final nanoparticle pellet in a cryoprotectant solution (e.g., 5% trehalose) and lyophilize for long-term storage.
3. Key Characterization Experiments:
- Particle Size and Zeta Potential: Use Dynamic Light Scattering (DLS) to measure the hydrodynamic diameter and polydispersity index (PDI). Measure zeta potential using laser Doppler micro-electrophoresis.
- Encapsulation Efficiency (EE): Quantify the amount of AMP loaded by measuring the unencapsulated peptide in the supernatant after centrifugation via HPLC. EE% = (Total AMP added - Free AMP in supernatant) / Total AMP added * 100.
- In Vitro Release Kinetics: Incubate a known amount of AMP-NPs in phosphate-buffered saline (PBS) at 37°C under gentle agitation. At predetermined time points, centrifuge samples and measure the AMP released into the supernatant using a validated analytical method (e.g., HPLC or fluorescence assay).
Protocol 2: Assessing Stability to Proteolytic Degradation
This experiment evaluates the protective effect of a delivery system against protease attack [14].
1. Materials:
- Free AMP solution and AMP-loaded formulation (e.g., nanoparticles, liposomes)
- Trypsin or a relevant protease (e.g., Proteinase K)
- Fetal Calf Serum (FCS)
- HPLC system with C18 column
2. Methodology:
- Sample Preparation: Prepare two sets of tubes containing equal molar amounts of the free AMP and the AMP-loaded formulation.
- Protease Challenge: Add trypsin (at a defined enzyme-to-substrate ratio) or 10-50% (v/v) FCS to all tubes. Incubate at 37°C.
- Reaction Termination: At time points (e.g., 0, 30, 60, 120 minutes), remove aliquots and immediately heat them to 95°C for 5 minutes to denature the proteases, or add a protease inhibitor cocktail.
- Analysis: For nanoparticles, separate the released degradation products from the intact, encapsulated AMP by centrifugation and analyze the pellet (after dissolution) and supernatant via HPLC. For free AMP, analyze the solution directly. Monitor the disappearance of the intact AMP peak over time.
3. Data Interpretation: A slower degradation rate and a higher percentage of intact AMP remaining in the formulation group compared to the free AMP group demonstrate the system's protective capability.
Visualization Diagrams
Diagram 1: Decision Workflow for Selecting an AMP Delivery System
This diagram outlines a logical workflow to help researchers select the most appropriate delivery system based on their AMP's properties and the target application.
Diagram 2: Mechanism of Nano-Encapsulated AMP Action
This diagram illustrates the synergistic mechanisms by which nanoparticle-AMP conjugates combat bacterial infections.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AMP Delivery System Research
| Reagent / Material | Function / Role | Key Considerations for Selection |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer for forming nanoparticles that provide sustained/controlled release of AMPs [89]. | Ratio (e.g., 50:50, 75:25): Affects degradation rate and drug release kinetics. Molecular Weight: Influences nanoparticle size and mechanical strength. |
| PVA (Polyvinyl Alcohol) | Stabilizer & Emulsifier used in nanoparticle formulation (e.g., double emulsion methods) to control particle size and prevent aggregation [89]. | Grade & Hydrolysis Level: Affects biodegradability and residual content in the final product. Must be thoroughly washed post-synthesis. |
| DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | Phospholipid used as a primary component for constructing liposomes and lipid nanoparticles, offering high bilayer stability and biocompatibility [89]. | Transition Temperature: High Tm (~55°C) ensures bilayer stability at physiological temperatures. Often used with cholesterol to modulate fluidity. |
| Cholesterol | Membrane Stabilizer incorporated into liposomal bilayers to reduce fluidity, minimize drug leakage, and enhance in vivo stability [89]. | Purity: Essential for reproducible formulation and minimizing oxidative degradation. |
| PEGylated Lipids (e.g., DSPE-PEG) | Stealth Agent conjugated to the surface of liposomes or nanoparticles to reduce opsonization, prolong circulation half-life, and enhance passive targeting (EPR effect) [2]. | PEG Chain Length: Longer chains provide better steric protection but can inhibit cellular uptake. |
| Cationic Lipids (e.g., DOTAP) | Charge Modifier used to impart a positive surface charge to nanoparticles, promoting interaction with negatively charged bacterial membranes and enhancing cellular uptake [89]. | Cytotoxicity: Must be optimized and balanced; high positive charge can lead to increased cytotoxicity. |
| Chitosan | Natural Polysaccharide used in nanoparticles and hydrogels. It is mucoadhesive and can enhance penetration across mucosal barriers, useful for wound dressings [15]. | Molecular Weight & Degree of Deacetylation: Directly influences viscosity, biodegradability, and antimicrobial activity. |
FAQs: Antimicrobial Peptides in Clinical Development
What antimicrobial peptides are currently FDA-approved for clinical use?
Several Antimicrobial Peptides (AMPs) have received FDA approval and are in clinical use, primarily for bacterial infections. The table below summarizes key approved AMP-based drugs [17] [10].
| Peptide Name | Class/Type | Target Pathogens | Therapeutic Use |
|---|---|---|---|
| Polymyxin B | Cyclic lipopeptide | Gram-negative bacteria | Treatment of Gram-negative bacterial infections [10] |
| Daptomycin | Lipopeptide | Drug-resistant Staphylococcus aureus (e.g., MRSA) | Complicated skin infections, bacteremia [10] |
| Bacitracin | Cyclic peptide | Gram-positive bacteria | Topical application for skin and eye infections [91] |
| Gramicidin S | Cyclic peptide | Gram-positive and Gram-negative bacteria | Topical antibiotic formulations [91] |
Which AMP candidates are in clinical trials, and what are their targets?
Numerous novel AMPs are progressing through clinical trials, targeting a range of infections from bacterial and fungal to viral and oncological. The following table details notable candidates [17] [10].
| Peptide Name | Trial Phase | Mechanism of Action | Clinical Application | Status/Notes |
|---|---|---|---|---|
| NP213 (Novexatin) | Phase II | Water-soluble cyclic peptide; disrupts fungal membranes | Onychomycosis (fungal nail infection) | Shows significant efficacy and safety; penetrates human nails effectively [10] |
| Omiganan | Phase II | Synthetic indolicidin analog; disrupts microbial membranes | Genital lesions induced by human tumor virus | Superior safety and efficacy profile in patients [10] |
| Murepavadin | Phase III | Targets outer membrane protein of Pseudomonas aeruginosa | Multidrug-resistant P. aeruginosa infections | Reduces host virulence through specific targeting [10] |
| Melittin (in nanoparticles) | Early Phase | Disrupts cell membranes; combined with targeted nanoparticles | Solid tumors | Shows controlled release and reduced hemolytic toxicity [10] |
| LL-37-Derived Peptide | Phase I/II (Completed 2024) | Immunomodulatory and antitumor activity | Melanoma | Induces antitumor effects [10] |
What are the major stability challenges in AMP formulation, and how are they addressed?
A primary challenge in AMP development is their inherent instability in physiological conditions, including susceptibility to proteolytic degradation, short half-life, and potential cytotoxicity (e.g., hemolysis) [11] [10]. Researchers are employing several advanced strategies to overcome these hurdles [10] [92] [93]:
- Structural Modifications: Incorporating D-amino acids, peptide cyclization, and utilizing non-natural amino acids to enhance resistance to proteases.
- Advanced Delivery Systems: Encapsulating or conjugating AMPs with biomaterials like nanoparticles, liposomes, and hydrogels. These systems protect the peptide, enable controlled release at the infection site, and can significantly reduce toxic side effects.
- Sequence Optimization: Using computational and machine learning (ML) approaches to design optimized peptide sequences that maximize stability and antimicrobial activity while minimizing cytotoxicity [17] [91].
Troubleshooting Guides
Issue: Rapid Degradation of AMP in Biological Fluids DuringIn VitroTesting
Problem: Your AMP candidate shows promising activity in simple buffers but loses efficacy rapidly when tested in serum or other complex biological media, likely due to proteolysis.
Solution: Implement a combination of formulation and peptide engineering strategies to shield the AMP from degrading enzymes.
Experimental Protocol: Protease Stability Assay
This protocol helps evaluate and improve the stability of your AMP.
Prepare Peptide Solutions:
- Test Group: Your AMP, optionally modified (e.g., cyclized, D-amino acid substitution) or formulated (e.g., encapsulated in PLGA nanoparticles).
- Control Group: The native, unmodified AMP in the same buffer.
- Incubate both groups in 50% (v/v) human serum or plasma at 37°C.
Sample Collection: Withdraw aliquots from the incubation mixture at predetermined time points (e.g., 0, 15, 30, 60, 120 minutes).
Analyze Integrity:
- HPLC/MS: Use Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) coupled with Mass Spectrometry (MS) to quantify the remaining intact peptide and identify degradation fragments.
- Antimicrobial Activity Test: At each time point, dilute an aliquot and test its residual antimicrobial activity against a standard target bacterium (e.g., S. aureus) using a broth microdilution assay to determine the Minimum Inhibitory Concentration (MIC).
Expected Outcome: A successfully stabilized AMP (e.g., nanoparticle-encapsulated) will show a slower decay of the intact peptide peak in HPLC and retain antimicrobial activity for a significantly longer duration compared to the control.
Issue: Optimizing an AMP Lead with Machine Learning
Problem: You have a weakly active natural AMP template (like citropin 1.1) and need to design a shorter, more potent, and less toxic derivative efficiently, moving beyond low-throughput traditional methods.
Solution: Combine traditional peptide design principles with machine learning (ML)-backed sequence optimization to intelligently explore the vast sequence space, as demonstrated with the development of CIT-8 [91].
Experimental Protocol: ML-Guided AMP Optimization Workflow
This workflow outlines the key steps for integrating ML into your AMP design process.
Data Curation & Clustering:
- Gather a large, aggregated dataset of known functional AMPs from public databases (e.g., APD, DRAMP). Preprocess to ensure unique sequences.
- Calculate key physicochemical descriptors (e.g., molecular weight, GRAVY, hydrophobicity, helicity) for all peptides.
- Use an unsupervised ML algorithm like k-means clustering to group peptides based on these descriptors. This identifies clusters with properties (e.g., high hydrophobicity and helicity) desirable for your target.
Template Truncation & Target Identification:
- Apply traditional design: Truncate your lead peptide to its core active fragment (e.g., CIT-1 was a 13-residue truncation of citropin 1.1).
- Identify specific amino acid positions for substitution that are predicted to enhance interaction with bacterial membranes (e.g., replacing neutral/negative residues with positive ones, or small hydrophobic residues with bulkier ones).
ML-Guided Substitution:
- Focus on the most relevant cluster from Step 1 (e.g., Cluster 1 for helical, hydrophobic peptides).
- Analyze this cluster to build "knowledge graphs" of the most frequently occurring amino acids at each position in potent, natural AMPs.
- Use these preferred amino acid patterns to guide which specific residues should replace the target positions identified in Step 2.
Synthesis & Validation:
- Synthesize the top ML-designed candidate peptides.
- Validate their properties through a standard battery of tests: antimicrobial activity (MIC), cytotoxicity (hemolysis), and mechanism-of-action studies (e.g., membrane depolarization).
The Scientist's Toolkit: Research Reagent Solutions
This table lists essential materials and their functions for key experiments in AMP development and stability research.
| Reagent / Material | Function in AMP Research |
|---|---|
| Proteases (e.g., Trypsin) | Used in stability assays to simulate enzymatic degradation in biological environments [93]. |
| Human Serum/Plasma | A complex medium for evaluating the stability and half-life of AMPs under physiologically relevant conditions [93]. |
| Cation-adjusted Mueller-Hinton Broth | Standardized growth medium for determining Minimum Inhibitory Concentration (MIC), ensuring reproducible antimicrobial activity results. |
| Sheep Red Blood Cells (RBCs) | Used in hemolysis assays to quantify the cytotoxicity of AMPs against mammalian cells, a critical safety parameter [11] [10]. |
| Lipopolysaccharide (LPS) | A key component of the Gram-negative outer membrane, used in studies to understand the initial electrostatic interaction of AMPs with bacteria [10]. |
| Lipid II | Essential precursor for bacterial cell wall synthesis; used in mechanistic studies to identify AMPs that inhibit cell wall formation (e.g., Nisin) [10]. |
| Fluorescent Dyes (e.g., DiSC₃(5)) | Membrane-potential sensitive dyes used in mechanism-of-action studies to detect AMP-induced membrane depolarization in real-time [91]. |
| PLGA Nanoparticles | A biodegradable and biocompatible polymer used to encapsulate AMPs, protecting them from degradation and enabling controlled release [10] [92]. |
Key Translational Challenges and Regulatory Considerations
Troubleshooting Guide: Common AMP Formulation Issues
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Stability & Degradation | Rapid loss of antimicrobial activity | Proteolytic degradation by host or bacterial proteases [5] [94]; Chemical instability (e.g., deamidation) [94] | Incorporate D-amino acids [5]; Use lipid or polymeric nanoparticle encapsulation [5]; Develop hydrogel-based sustained-release systems [5] |
| Toxicity | Hemolytic activity or cytotoxicity toward host cells | Non-specific interaction with mammalian cell membranes due to peptide's cationic/amphipathic nature [5] [94] | Optimize peptide sequence to enhance selectivity for bacterial membranes [5]; Conjugate with antibiotics to lower effective dose [94] |
| Manufacturing | High production costs and low yields | Complex synthesis and purification processes; Scalability challenges [94] | Explore recombinant expression systems; Optimize peptide sequences for more efficient production [94] |
| Bioavailability & Delivery | Poor pharmacokinetics; Ineffective delivery to target site | Rapid renal clearance; Inability to penetrate biological barriers (e.g., biofilms) [5] | Utilize targeted delivery systems (e.g., murepavadin targets specific outer membrane proteins) [5]; Employ self-assembling peptides to disrupt biofilms [94] |
Frequently Asked Questions (FAQs)
Q1: Why is my antimicrobial peptide highly effective in vitro but shows no efficacy in animal models? This common discrepancy is often due to proteolytic degradation of the peptide by enzymes in the host's body or poor penetration into the infection site [5]. The peptide may also be binding non-specifically to serum proteins, reducing its bioavailability. Solutions include formulating the peptide within a protective nanoparticle or hydrogel delivery system that shields it from degradation and allows for controlled release at the target site [5].
Q2: How can I reduce the cytotoxicity of my AMP formulation without completely losing its antimicrobial activity? Strategies focus on enhancing the selective toxicity of the peptide for bacterial over mammalian cells. This can be achieved by sequence modification to fine-tune the peptide's charge and hydrophobicity [5]. Another promising approach is creating AMP-antibiotic conjugates, which can enhance efficacy against the pathogen while potentially reducing the required AMP dose and its associated toxicity [94].
Q3: What are the critical stability parameters to monitor during AMP formulation development? Key parameters include:
- Susceptibility to Proteolysis: Assess stability in the presence of relevant proteases (e.g., trypsin, elastase) [5].
- Physical Stability: Monitor for aggregation or precipitation over time, especially in liquid formulations.
- Chemical Stability: Check for modifications like oxidation or deamidation under storage conditions (e.g., temperature, pH) [94].
Q4: My AMP works against planktonic bacteria but fails against biofilms. What can I do? Biofilms present a significant physical and physiological barrier. Consider using self-assembling peptides that can form nanostructures designed to penetrate and disrupt the biofilm matrix [94]. Another strategy is to combine your AMP with a delivery system, such as cubosomes, which have been shown to enhance the anti-biofilm activity of peptides like LL-37 by protecting them from degradation [5].
Experimental Protocol: Evaluating AMP Stability and Efficacy
Protocol 1: Assessing Proteolytic Stability of AMP Formulations
Objective: To determine the resistance of an antimicrobial peptide to enzymatic degradation, simulating the in vivo environment.
Materials:
- Purified AMP (lyophilized or in solution)
- Protease solution (e.g., Trypsin, Elastase at a defined activity)
- Appropriate buffer (e.g., PBS, Tris-HCl)
- Incubator or water bath
- HPLC system with a C18 column or MALDI-TOF Mass Spectrometer
Method:
- Preparation: Dissolve the AMP in the chosen buffer to a final concentration of 1 mg/mL.
- Reaction Setup: In a microcentrifuge tube, mix the AMP solution with the protease solution at a specific enzyme-to-substrate ratio (e.g., 1:100 w/w). Include a control tube with AMP and buffer only (no protease).
- Incubation: Incubate the reaction mixture at 37°C.
- Sampling: Withdraw aliquots from both the test and control tubes at predetermined time points (e.g., 0, 15, 30, 60, 120 minutes).
- Reaction Termination: Immediately inactivate the protease in the sampled aliquots, typically by heating at 95°C for 5 minutes or by adding a protease inhibitor.
- Analysis:
- HPLC Analysis: Inject the terminated samples into an HPLC system. Monitor the degradation by observing the decrease in the intact peptide peak area and the appearance of new peaks (degradation fragments) over time.
- Mass Spectrometry: Use MALDI-TOF to confirm the molecular weight of the intact peptide and identify the masses of degradation products.
- Data Interpretation: Calculate the half-life of the AMP by plotting the logarithm of the remaining intact peptide concentration against time.
Protocol 2: Time-Kill Assay to Evaluate Formulation Efficacy
Objective: To compare the bactericidal kinetics of a free AMP versus a formulated AMP (e.g., encapsulated in nanoparticles).
Materials:
- Bacterial culture (e.g., Staphylococcus aureus, Escherichia coli)
- Cation-adjusted Mueller-Hinton Broth (CAMHB)
- Free AMP solution
- AMP-loaded formulation (e.g., nanoparticles, cubosomes)
- Sterile phosphate-buffered saline (PBS)
- Shaking incubator
- Spectrophotometer
- Colony counter and agar plates
Method:
- Inoculum Preparation: Grow bacteria to mid-logarithmic phase (OD600 ≈ 0.5) and dilute in CAMHB to a final density of approximately 5 x 10^5 CFU/mL.
- Treatment: Add the free AMP and the formulated AMP to separate flasks containing the bacterial inoculum. The final AMP concentration should be at or above the predetermined MIC. Include a flask with no AMP as a growth control.
- Incubation: Incubate the flasks at 37°C with constant shaking.
- Viable Count: At time points 0, 1, 2, 4, 6, and 24 hours, remove 100 µL aliquots from each flask. Perform serial ten-fold dilutions in PBS and plate onto Mueller-Hinton agar plates in duplicate.
- Enumeration: After overnight incubation at 37°C, count the colonies on plates with 30-300 colonies. Calculate the CFU/mL for each sample and time point.
- Data Analysis: Plot Log10 CFU/mL versus time for the free AMP, formulated AMP, and growth control. The formulation is superior if it shows a faster or more sustained reduction in viable counts compared to the free peptide.
Research Reagent Solutions
| Reagent / Material | Function in AMP Research | Key Considerations |
|---|---|---|
| Cubosomes (Lipid-based Nanoparticles) | Protects AMPs (e.g., LL-37) from proteolytic degradation; enables sustained release [5]. | Monitor peptide loading efficiency and release kinetics. |
| Hydrogels | Provides a scaffold for controlled, localized delivery of AMPs at the infection site [5]. | Optimize cross-linking density to control release rate and maintain peptide stability. |
| Murepavadin | A targeted AMP in Phase III trials; specific against Pseudomonas aeruginosa; model for targeted delivery [5]. | Study its mechanism of targeting outer membrane proteins to reduce off-target effects. |
| Omiganan | Synthetic AMP in trials for skin conditions; useful for studying topical formulation challenges [5]. | An ideal candidate for developing and testing topical delivery systems. |
| Nisin | A bacteriocin; model AMP for studying "dual-mechanism" action (binds Lipid II and forms pores) [5]. | Useful for research on synergy with conventional antibiotics and food preservation. |
| Polymyxin B | Clinically approved AMP for Gram-negative infections; benchmark for toxicity and efficacy studies [5]. | Use to compare the safety profile of novel, less toxic AMP formulations. |
AMP Stability Optimization Workflow
AMP Stability Optimization Workflow
AMP Mechanism of Action and Degradation
AMP Mechanisms and Translational Barriers
Conclusion
The path to overcoming stability issues in antimicrobial peptide formulations is multifaceted, requiring an integrated approach that combines advanced delivery systems, intelligent molecular design, and robust validation. The progression from foundational understanding to sophisticated liposomal, polymeric, and hydrogel-based carriers demonstrates a clear path toward protecting AMPs from degradation and enhancing their therapeutic index. Furthermore, the emergence of AI-driven design and rational optimization strategies allows for the precise engineering of peptides with inherent stability. While challenges in cost-effective manufacturing and long-term pharmacokinetics remain, the growing clinical pipeline, including candidates in Phase II and III trials, underscores the tangible progress being made. Future success will hinge on interdisciplinary collaboration to refine these strategies, ensuring that the immense potential of AMPs is fully realized in the global fight against antimicrobial resistance.
References
- 1. Therapeutic peptides: current applications and future directions | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-022-00904-4]
- 2. Frontiers | Editorial: Antimicrobial and their druggability... peptides [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1425952/full]
- 3. Differential stability of therapeutic peptides with different proteolytic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5456363/]
- 4. of Stabilization against peptides through... proteolysis [https://pubs.rsc.org/en/content/articlelanding/2017/ob/c6ob02786e]
- 5. biological activity, delivery systems and clinical... Antimicrobial peptide [https://pmc.ncbi.nlm.nih.gov/articles/PMC11887333/]
- 6. - Wikipedia Proteolysis [https://en.wikipedia.org/wiki/Proteolysis]
- 7. The effects of incorporation of the counterparts and mimics of l-lysine... [https://link.springer.com/article/10.1007/s00726-021-03099-0]
- 8. The effect of structural modification of antimicrobial on their... peptides [https://pubmed.ncbi.nlm.nih.gov/33554385/]
- 9. Progress on the design and optimization of antimicrobial ... peptides [https://pmc.ncbi.nlm.nih.gov/articles/PMC9927193/]
- 10. Antimicrobial peptide biological activity, delivery systems and clinical translation status and challenges | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06321-9]
- 11. Frontiers | Progress in the classification, optimization, activity, and application of antimicrobial peptides [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1582863/full]
- 12. Cytotoxicity Assays: In Vitro Methods to Measure Dead Cells - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK540958/]
- 13. Antimicrobial Peptides are Degraded by the Cytosolic Proteases of Human Erythrocytes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659893/]
- 14. Antimicrobial activity and stability to proteolysis of small linear cationic peptides with D-amino acid substitutions - PubMed [https://pubmed.ncbi.nlm.nih.gov/12516770/]
- 15. towards clinical application: Delivery and... Antimicrobial peptides [https://pubmed.ncbi.nlm.nih.gov/34090965/]
- 16. as a Bioavailability System Property... | SpringerLink Microbial [https://link.springer.com/chapter/10.1007/698_2020_568]
- 17. Frontiers | Unlocking the power of antimicrobial peptides: advances in production, optimization, and therapeutics [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1528583/full]
- 18. Factors Influencing the Bioavailability of Organic Molecules to Bacterial Cells—A Mini-Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9570905/]
- 19. Frontiers | Antimicrobial and Nanotechnology, Recent... Peptides [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.00855/full]
- 20. Economies of scale - Wikipedia [https://en.wikipedia.org/wiki/Economies_of_scale]
- 21. Development and Challenges of Antimicrobial for... Peptides [https://pmc.ncbi.nlm.nih.gov/articles/PMC7168295/]
- 22. Technological and economic barriers of industrial-scale production of nanocellulose - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/B9780128232965000150]
- 23. Optimizing Antibody Stability and Formulation ... - Creative Peptides [https://www.creative-peptides.com/resources/optimizing-antibody-stability-and-formulation-studies-using-peptide-labeling.html]
- 24. Liposomal Nanovesicles for Efficient Encapsulation of Staphylococcal Antibiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6649299/]
- 25. How to Improve Drug Delivery with Liposome Encapsulation? - BOC Sciences [https://liposomes.bocsci.com/resources/liposome-encapsulation-strategies-overcoming-drug-delivery-barriers.html]
- 26. in Food Systems: A Review of Formulation... Liposomal Encapsulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321603/]
- 27. Study of Natural Dyes’ Liposomal Encapsulation in Food Dispersion Model Systems via High-Pressure Homogenization [https://www.mdpi.com/1420-3049/30/8/1845]
- 28. Frontiers | Dual Coating of Liposomes as Encapsulating Matrix of... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2017.00103/full]
- 29. Liposome Technology for Industrial Purposes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3065896/]
- 30. Exploring Liposomal Systems: Revolutionizing... | Clinikally Delivery [https://www.clinikally.com/blogs/news/exploring-liposomal-delivery-systems-revolutionizing-skincare]
- 31. Drug Liposome : The Future of Therapeutics by WBCIL Delivery [https://www.wbcil.com/blog/liposomal-technology-a-voyage-into-the-future-of-drug-delivery/]
- 32. Enhancing Stability and Biocompatibility of Antitubercular Peptides ... [https://link.springer.com/article/10.1007/s12247-025-10173-7]
- 33. Polymeric Nanoparticles: Production, Characterization, Toxicology and Ecotoxicology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7464532/]
- 34. Polymer Nanoparticles: Synthesis and Applications - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9781848/]
- 35. to tumors using biological... Targeting inorganic nanoparticles [https://pmc.ncbi.nlm.nih.gov/articles/PMC9732394/]
- 36. Applications of polymer -based nanoparticles in vaccine field [https://www.degruyterbrill.com/document/doi/10.1515/ntrev-2019-0014/html]
- 37. Engineered GLP-1R- targeting nanoplatforms: multimodal therapeutics... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03677-4]
- 38. Nanoparticles: synthesis and applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7151836/]
- 39. Intelligent Systems for Inorganic Nanomaterial Synthesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029268/]
- 40. Systems as Promising Tools Against... Antimicrobial Peptide Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC11591436/]
- 41. Hydrogels as Drug Delivery Systems: A Review of Current Characterization and Evaluation Techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7762425/]
- 42. Designing hydrogels for controlled drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5898614/]
- 43. Anionic polysaccharides for stabilization and sustained release of... [https://pubmed.ncbi.nlm.nih.gov/36889417/]
- 44. Hydrogel Biomaterials for Drug Delivery: Mechanisms, Design, and Drugs | IntechOpen [https://www.intechopen.com/chapters/80823]
- 45. Nanocarrier-Hydrogel Composite Delivery Systems for Precision Drug Release - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9811486/]
- 46. High-level biosynthesis and purification of the antimicrobial ... peptide [https://biotechnologyforbiofuels.biomedcentral.com/articles/10.1186/s13068-025-02607-8]
- 47. Unlocking the power of antimicrobial : advances in... peptides [https://pubmed.ncbi.nlm.nih.gov/40365533/]
- 48. Pharmacokinetics of Recombinant Bifunctional Fusion Proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3718553/]
- 49. Fusion Proteins Overview | Sino Biological [https://www.sinobiological.com/resource/protein-review/fusion-protein]
- 50. Fusion protein - Wikipedia [https://en.wikipedia.org/wiki/Fusion_protein]
- 51. Pegylation and formulation strategy of Anti-Microbial Peptide (AMP) according to the quality by design approach - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0928098719304701]
- 52. for Modulation of Strategies of Recombinant... Pharmacokinetics [https://link.springer.com/article/10.1134/S2079086418020093]
- 53. An engineered arginine-rich α-helical antimicrobial peptide exhibits... [https://www.nature.com/articles/s41598-018-32981-3?error=cookies_not_supported&code=bc71ed19-040d-4c34-9fe9-efcbaf655b6a]
- 54. Improving Conformational Stability and Bacterial... | Research Square [https://www.researchsquare.com/article/rs-7340189/v1]
- 55. HEPAD: enhancing hemolytic peptide prediction with adaptive feature engineering and diverse sequence descriptors | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06254-6]
- 56. Balancing hydrophobicity and sequence pattern to influence... [https://pubmed.ncbi.nlm.nih.gov/29292825/]
- 57. Phosphorylation as an Effective Tool to Improve Stability and Reduce... [https://pubmed.ncbi.nlm.nih.gov/39383315/]
- 58. Frontiers | Antimicrobial and their Druggability, Bio-safety... Peptides [https://www.frontiersin.org/research-topics/51944/antimicrobial-peptides-and-their-druggability-bio-safety-stability-and-resistance]
- 59. Design methods for antimicrobial peptides with improved performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802102/]
- 60. Improving enzymatic and chemical of stability by peptides ... chemical [https://www.novoprolabs.com/support/articles/improving-enzymatic-and-chemical-stability-of-peptides-by-chemical-modifications-202102261579.html]
- 61. Frontiers | A Systematic Study of the Stability, Safety, and Efficacy ... [https://www.frontiersin.org/articles/10.3389/fmicb.2021.678330/full]
- 62. Rational design of stapled | antimicrobial peptides Amino Acids [https://link.springer.com/article/10.1007/s00726-023-03245-w]
- 63. Incorporation of Non - Canonical into Amino ... Acids Antimicrobial [https://pmc.ncbi.nlm.nih.gov/articles/PMC9746297/]
- 64. Peptide Modifications | Bachem [https://www.bachem.com/articles/peptides/peptide-modifications/]
- 65. Peptide Design: Principles & Methods | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/peptide-design.html]
- 66. Frontiers | Antimicrobial Peptides: A New Hope in Biomedical and Pharmaceutical Fields [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2021.668632/full]
- 67. Antimicrobial peptides - Wikipedia [https://en.wikipedia.org/wiki/Antimicrobial_peptides]
- 68. The antimicrobial peptides and their potential clinical applications - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6684887/]
- 69. Machine learning for antimicrobial peptide identification and design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756916/]
- 70. Topical antimicrobial peptide formulations for wound healing: Current developments and future prospects - PubMed [https://pubmed.ncbi.nlm.nih.gov/31874224/]
- 71. Advances Precision Targeting in Next-Generation Antimicrobial... AI [https://bioengineer.org/ai-advances-precision-targeting-in-next-generation-antimicrobial-peptide-design/]
- 72. A Review of Antimicrobial Peptides and Their Therapeutic Potential as Anti-Infective Drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1497874/]
- 73. How AI is Revolutionizing Medicine: Designing Smarter Antibodies... [https://www.linkedin.com/pulse/how-ai-revolutionizing-medicine-designing-smarter-yunguo-yu-phd-md-n8vxe]
- 74. The advent of AI for peptide : An emerging field design [https://www.labiotech.eu/in-depth/ai-peptide-design/]
- 75. High-throughput screening - Wikipedia [https://en.wikipedia.org/wiki/High-throughput_screening]
- 76. - High | Toxicology Class Notes | Fiveable throughput screening [https://fiveable.me/toxicology/unit-10/high-throughput-screening/study-guide/EMKp0XEVa3Fq4ebu]
- 77. - High Toxicology | US EPA Throughput [https://www.epa.gov/chemical-research/high-throughput-toxicology]
- 78. Perspectives on Validation of High - Throughput Assays Supporting... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3934015/]
- 79. Wiley-VCH - High - Throughput in Screening Testing Methods Toxicity [https://www.wiley-vch.de/en/areas-interest/natural-sciences/high-throughput-screening-methods-in-toxicity-testing-978-1-118-06563-1]
- 80. Adaptation of High-Throughput Screening in Drug Discovery—Toxicological Screening Tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269696/]
- 81. - High (HTS): A Simple Throughput to Faster Drug... Screening Guide [https://www.chemcopilot.com/blog/hts-material-discovery]
- 82. Overview of high-throughput screening - PubMed [https://pubmed.ncbi.nlm.nih.gov/22294406/]
- 83. High-Throughput Screening: today's biochemical and cell-based approaches - PubMed [https://pubmed.ncbi.nlm.nih.gov/32801051/]
- 84. On In Vivo vs. In Vitro Models [https://phenovista.com/blog/on-in-vivo-vs.-in-vitro-models]
- 85. In Vivo vs. In Vitro Models: Key Differences and Applications in Preclinical Research – Home 1 [https://liveonbiolabs.com/in-vivo-vs-in-vitro-models/]
- 86. From In Promise to Vitro Reality: An Instructive Account of... In Vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC11431785/]
- 87. Complex in vitro model: A transformative model in drug development and precision medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10828975/]
- 88. and In antibacterial properties of vitro AMC-109... in vivo peptide [https://www.nature.com/articles/s41429-021-00406-5?error=cookies_not_supported&code=8d248a9d-83a6-41c1-acf1-aafd9529f2ff]
- 89. Advanced delivery systems for peptide antibiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10771258/]
- 90. Antimicrobial Peptide Delivery Systems as Promising Tools Against Resistant Bacterial Infections [https://www.mdpi.com/2079-6382/13/11/1042]
- 91. Antimicrobial peptide developed with machine learning sequence optimization targets drug resistant Staphylococcus aureus in mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165799/]
- 92. Advances in Antimicrobial Peptides: Mechanisms, Design Innovations, and Biomedical Potential [https://www.mdpi.com/1420-3049/30/7/1529]
- 93. Advances in the discovery, mechanism of action, optimization of activity and potential for clinical application of antimicrobial peptides - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1385894724104536]
- 94. A critical view of antimicrobial : exploring their potential and... peptides [https://research.manchester.ac.uk/en/publications/a-critical-view-of-antimicrobial-peptides-exploring-their-potenti]