Mastering CLSI M07 Broth Microdilution: A Complete Guide for Antimicrobial Susceptibility Testing in 2024
This comprehensive guide details the CLSI M07 broth microdilution standard method for determining Minimum Inhibitory Concentrations (MICs) of antimicrobial agents against bacteria.
Mastering CLSI M07 Broth Microdilution: A Complete Guide for Antimicrobial Susceptibility Testing in 2024
Abstract
This comprehensive guide details the CLSI M07 broth microdilution standard method for determining Minimum Inhibitory Concentrations (MICs) of antimicrobial agents against bacteria. It provides researchers, scientists, and drug development professionals with foundational principles, a step-by-step methodological walkthrough, troubleshooting strategies for common pitfalls, and insights into method validation and comparison with other techniques like agar dilution (M07) and disk diffusion (M02). The article covers recent updates from the Clinical and Laboratory Standards Institute (CLSI), practical applications in drug discovery and clinical trials, and best practices for ensuring accurate, reproducible, and compliant results.
What is CLSI M07 Broth Microdilution? Core Principles and Standards Explained
Defining Broth Microdilution and the Role of CLSI Standard M07
Introduction
Within the rigorous framework of antimicrobial susceptibility testing (AST) research, broth microdilution (BMD) stands as the reference quantitative method for determining the minimum inhibitory concentration (MIC) of antimicrobial agents. This in-depth technical guide defines the BMD method and elaborates on the critical role of the Clinical and Laboratory Standards Institute (CLSI) standard M07, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," in ensuring the accuracy, reproducibility, and clinical relevance of this foundational technique. This discussion is framed within the context of advancing thesis research on the M07 standard, focusing on its methodological specifics, interpretative criteria, and its position as the benchmark against which novel diagnostic technologies are validated.
1. Defining Broth Microdilution
Broth microdilution is a standardized laboratory technique where a bacterial inoculum of defined density is exposed to serial two-fold dilutions of an antimicrobial agent in a liquid growth medium, typically within a 96-well microtiter plate. After a defined incubation period (usually 16-20 hours at 35°C ± 2°C), the MIC is determined as the lowest concentration of the antimicrobial that completely inhibits visible growth of the organism.
2. The Role and Scope of CLSI Standard M07
CLSI document M07 provides the definitive procedural and quality control framework for performing BMD for aerobic bacteria. Its primary role is to standardize all variables to ensure results are reliable, comparable across laboratories, and clinically actionable. Key areas standardized by M07 include:
- Preparation of antimicrobial stock solutions: Specifies solvents, diluents, and storage conditions.
- Panel preparation: Details the formulation of cation-adjusted Mueller-Hinton Broth (CA-MHB) as the standard medium and the methodology for creating serial dilutions.
- Inoculum preparation: Mandates the use of the 0.5 McFarland standard and subsequent dilution to achieve a final bacterial density of ~5 x 10⁵ CFU/mL in each well.
- Incubation conditions: Defines time, temperature, and atmosphere.
- Reading and interpretation: Provides guidelines for determining endpoints and correlating MICs with clinical breakpoints (found in CLSI M100).
3. Detailed Experimental Protocol: Reference BMD per CLSI M07
The following protocol is a synthesis of the core methodology from CLSI M07-Ed13.
Materials:
- Cation-Adjusted Mueller Hinton Broth (CA-MHB)
- Sterile 96-well, U-bottom microtiter plates
- Antimicrobial agents of known potency
- Bacterial isolates, freshly subcultured
- 0.5 McFarland turbidity standard or densitometer
- Sterile saline or broth for inoculum preparation
- Multichannel pipettes and sterile reservoirs
- 35°C ± 2°C ambient air incubator
Procedure:
- Antimicrobial Stock Solution Preparation: Prepare a stock solution of the antimicrobial agent at a high concentration (e.g., 5120 µg/mL or 10x the highest concentration to be tested) using the appropriate solvent and diluent as specified in M07 Table 6A.
- Microdilution Panel Preparation: Using CA-MHB as the diluent, perform serial two-fold dilutions of the antimicrobial stock directly in the microtiter plate wells. Typically, a volume of 50 µL per well is used. One column of wells serves as a growth control (antimicrobial-free broth). Final well volumes before inoculation are 50 µL.
- Inoculum Standardization: Adjust the turbidity of a log-phase bacterial broth culture or saline suspension to match a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL).
- Inoculum Dilution: Dilute the standardized suspension 1:150 in sterile saline or broth to achieve a concentration of ~1 x 10⁶ CFU/mL.
- Plate Inoculation: Add 50 µL of the diluted inoculum to each well of the microtiter plate containing the 50 µL of antimicrobial dilutions. This step achieves the target final inoculum of ~5 x 10⁵ CFU/mL per well in a total volume of 100 µL.
- Incubation: Cover the plate and incubate at 35°C ± 2°C in ambient air for 16-20 hours.
- Endpoint Determination: Examine the plate visually or with an automated reader. The MIC is the lowest antimicrobial concentration that completely inhibits visible growth.
4. Key Quantitative Data from M07-Based Studies
Table 1: Acceptable Ranges for Quality Control (QC) Organisms in BMD (Excerpt)
| QC Organism | Antimicrobial Agent | Acceptable MIC Range (µg/mL) |
|---|---|---|
| Staphylococcus aureus ATCC 29213 | Oxacillin | 0.12 - 0.5 |
| Vancomycin | 0.5 - 2 | |
| Escherichia coli ATCC 25922 | Ciprofloxacin | 0.004 - 0.015 |
| Meropenem | 0.004 - 0.015 | |
| Pseudomonas aeruginosa ATCC 27853 | Tobramycin | 0.5 - 2 |
| Ceftazidime | 1 - 4 |
Table 2: Impact of Critical Variables on MIC Results
| Variable | CLSI M07 Specification | Consequence of Deviation |
|---|---|---|
| Cation Concentration | Ca²⁺: 20-25 mg/L; Mg²⁺: 10-12.5 mg/L in CA-MHB | Alters MICs of aminoglycosides (Mg²⁺) and daptomycin (Ca²⁺). |
| Inoculum Density | Final: 5 x 10⁵ CFU/mL (± 1 log) | Higher density can falsely elevate MIC; lower density can falsely lower MIC. |
| Incubation Time | 16-20 hours | Prolonged incubation can lead to trailing growth or degradation of labile drugs. |
| Incubation Atmosphere | Ambient Air (for non-fastidious aerobes) | Altered O₂/CO₂ can affect growth rate and MIC for some species. |
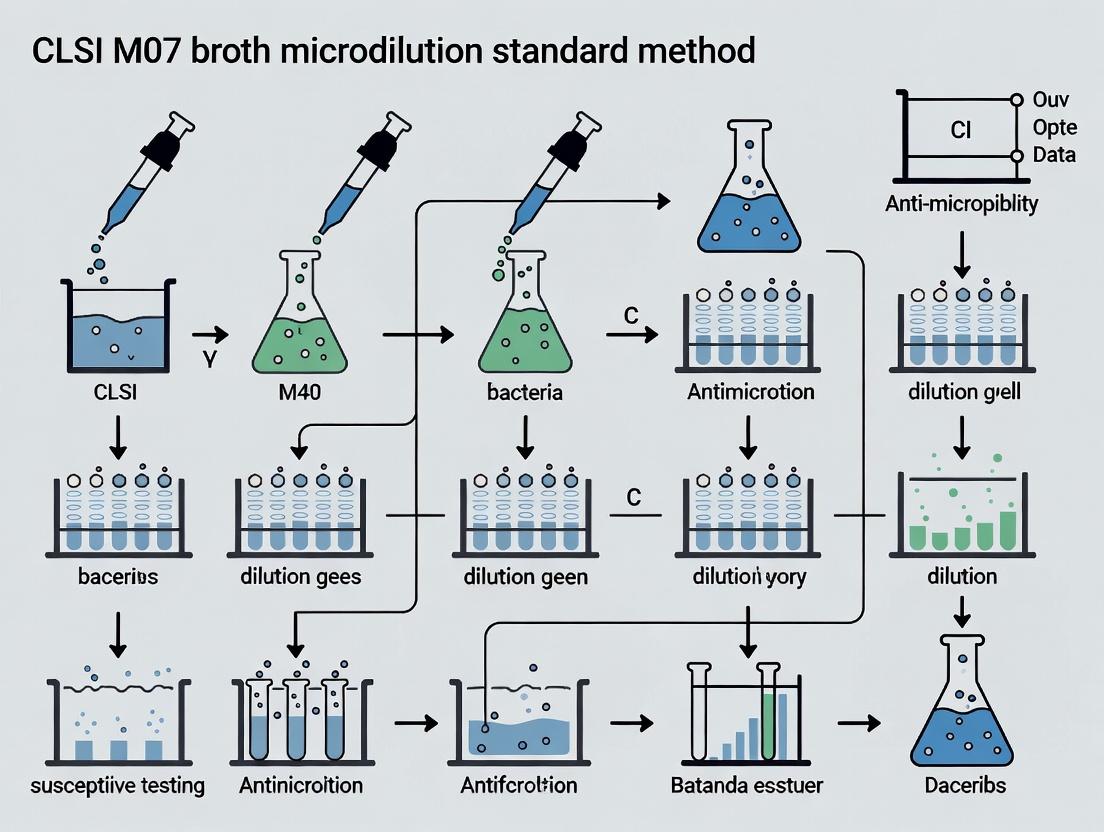
5. Experimental Workflow Diagram
Diagram 1: CLSI M07 Reference Broth Microdilution Workflow
6. The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for CLSI M07-Compliant BMD
| Item | Function | Critical Specification |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CA-MHB) | Standardized growth medium for non-fastidious aerobes. | Must contain defined levels of calcium (20-25 mg/L) and magnesium (10-12.5 mg/L) ions. |
| Microtiter Plates (96-well, U-bottom) | Reaction vessel for housing dilutions and inoculum. | Must be non-cytotoxic, sterile, and have low protein binding. |
| 0.5 McFarland Turbidity Standard | Primary standard for inoculum density preparation. | Can be commercial latex suspension or verified in-house barium sulfate standard. |
| CLSI QC Strains (e.g., ATCC 29213, 25922, 27853) | Quality control organisms to verify reagent performance and technique. | Must be obtained from a reputable source, stored properly, and subcultured per M07. |
| Antimicrobial Reference Powders | For preparation of primary stock solutions. | Must be of known and high potency (>90%), with purity verified. |
| Sterile Dimethyl Sulfoxide (DMSO) or Water | Solvents for initial dissolution of antimicrobial powders. | Choice dictated by M07 Table 6A; must be sterile and of reagent grade. |
Conclusion
The CLSI M07 standard is not merely a procedural manual; it is the cornerstone of robust, defensible research in antimicrobial susceptibility. For thesis research, a deep understanding of M07's tenets allows for the precise execution of the reference BMD method, enabling valid comparisons with novel AST platforms, investigations into resistance mechanisms, and studies on the pharmacokinetic/pharmacodynamic (PK/PD) correlates of efficacy. Adherence to M07 ensures that generated MIC data is of the highest quality, forming a reliable foundation for scientific discovery and clinical interpretation.
The Significance of MIC (Minimum Inhibitory Concentration) in Antimicrobial Testing
Within the framework of Clinical and Laboratory Standards Institute (CLSI) document M07 research, the Minimum Inhibitory Concentration (MIC) remains the foundational quantitative measure for assessing antimicrobial susceptibility. This in-depth technical guide explores the pivotal role of MIC determination via the standardized broth microdilution method, its interpretation in the context of pharmacokinetic/pharmacodynamic (PK/PD) indices, and its critical function in antimicrobial stewardship and drug development.
The MIC is defined as the lowest concentration of an antimicrobial agent that completely inhibits visible growth of a microorganism under standardized incubation conditions. In the research context of CLSI M07, broth microdilution is established as the reference method for MIC determination due to its reproducibility, scalability, and capacity for high-throughput testing essential for research and drug development.
Methodology: CLSI M07 Broth Microdilution Standard Protocol
Core Experimental Protocol
This detailed protocol is adapted from CLSI M07-A11 (2023) and subsequent updates.
Step 1: Preparation of Antimicrobial Stock Solutions
- Weigh the antimicrobial reference powder using an analytical balance.
- Dissolve in the appropriate solvent (specified by CLSI Appendix B).
- Filter sterilize (0.22 µm pore size).
- Aliquot and store at -70°C or below (unless stability data indicates otherwise).
Step 2: Preparation of Dilution Series
- Perform serial two-fold dilutions in cation-adjusted Mueller-Hinton broth (CAMHB) or other appropriate medium.
- Dilution range typically spans from 0.008 µg/mL to 128 µg/mL, encompassing expected clinical breakpoints.
Step 3: Inoculum Preparation
- Select 3-5 well-isolated colonies from an overnight agar plate.
- Suspend in sterile saline or broth to achieve a 0.5 McFarland standard (approx. 1-2 x 10^8 CFU/mL for Enterobacterales).
- Dilute the suspension in broth to achieve a final inoculum density of 5 x 10^5 CFU/mL in the test well.
Step 4: Microdilution Plate Setup
- Dispense 100 µL of each antimicrobial dilution into the wells of a sterile 96-well microtiter plate.
- Add 100 µL of the standardized inoculum to each test well.
- Include controls: Growth control (broth + inoculum), sterility control (broth only), and quality control (reference strain with known MIC).
Step 5: Incubation and Reading
- Incubate plates under atmospheric conditions (non-fastidious organisms) at 35°C ± 2°C for 16-20 hours.
- Read MIC visually or with automated readers. The MIC is the lowest concentration with no visible turbidity.
Key Quantitative Data and Clinical Breakpoints
The interpretation of raw MIC data relies on correlation with clinical breakpoints established by CLSI and EUCAST.
Table 1: Example MIC Interpretive Criteria (CLSI M100, 2024) for Pseudomonas aeruginosa vs. Ciprofloxacin
| MIC (µg/mL) | Interpretation (S/I/R) | Clinical Implication |
|---|---|---|
| ≤ 0.5 | Susceptible (S) | Standard dosing regimen likely effective |
| 1 | Intermediate (I) | May be effective at higher doses or at body sites where drug concentrates |
| ≥ 2 | Resistant (R) | High likelihood of clinical failure with standard dosing |
Table 2: Key PK/PD Indices Linked to MIC for Efficacy Prediction
| PK/PD Index | Target for Bactericidal Activity (Typical) | Description & Significance |
|---|---|---|
| %T > MIC (Time-dependent) | 40-70% of dosing interval (e.g., β-lactams) | Time the free drug concentration exceeds the MIC |
| AUC(_{0-24}) / MIC (Concentration-dependent) | 25-400 (e.g., Fluoroquinolones: ~125) | Area Under the Curve of free drug over 24h relative to MIC |
| C(_{max}) / MIC (Concentration-dependent) | 8-12 (e.g., Aminoglycosides) | Peak free drug concentration relative to MIC |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for Broth Microdilution MIC Testing
| Item | Function & Critical Specifications |
|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standard medium ensuring reproducible cation concentrations (Ca2+, Mg2+) that affect aminoglycoside and tetracycline activity. |
| 96-Well Sterile Microtiter Plths | Polystyrene plates with low protein binding; U-bottom for easier visual reading, flat-bottom for spectrophotometric reading. |
| Reference Antimicrobial Powder | USP-grade powder of known potency, used for preparing in-house stock solutions for research. |
| Frozen or Lyophilized Panels | Pre-made panels with serial dilutions of multiple drugs, essential for high-throughput screening in development. |
| Quality Control Strains | E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213. Used to validate test performance. |
| Densitometer or Spectrophotometer | For standardizing inoculum to precisely 0.5 McFarland (optical density ~0.08-0.13 at 625 nm). |
| Multichannel Pipettes & Reagent Reservoirs | For accurate and efficient dispensing of broth, inoculum, and antimicrobial solutions. |
Advanced Applications in Drug Development
MIC data feeds into critical development decisions:
- Determination of In Vitro Potency: Establishes baseline activity against target pathogens.
- Resistance Frequency Studies: Informs on the mutational prevention concentration (MPC).
- Combination Synergy Testing: Checkerboard MIC assays quantify fractional inhibitory concentration (FIC) indices.
Visualizing the Role of MIC in Research and Clinical Decision Pathways
Diagram Title: MIC Data Flow from Lab Experiment to Research and Clinical Application
Diagram Title: Integration of MIC with PK/PD to Predict Outcome
Within the rigorous framework of CLSI M07, the MIC is not a standalone number but the essential link between in vitro antimicrobial testing, research into resistance mechanisms, and clinical efficacy. Its accurate determination via standardized broth microdilution is fundamental for robust surveillance data, rational drug development, and the informed application of PK/PD principles to combat antimicrobial resistance.
The Clinical and Laboratory Standards Institute (CLSI) document M07 outlines standardized broth microdilution methods for the in vitro susceptibility testing of aerobic bacteria. As part of a broader thesis on refining and applying M07 methodology, this whitepaper details the critical foundational components: the formulation and preparation of broth media, the precise preparation of the bacterial inoculum, and the rigorous specifications of the microdilution plate format. Mastery of these three elements is fundamental to generating reproducible, accurate, and clinically relevant minimum inhibitory concentration (MIC) data.
Broth Media: The Growth Environment
Broth media must support consistent, rapid growth of non-fastidious aerobic bacteria without interfering with antimicrobial activity. Cation-adjusted Mueller-Hinton Broth (CAMHB) is the standard medium, with specific adjustments to ensure reproducibility.
Critical Components of CAMHB
The formulation is designed to control variables that significantly affect MIC results, particularly cation concentrations.
- Ca²⁺ Concentration: Adjusted to 20–25 mg/L (as Ca²⁺). Critical for testing aminoglycosides and tetracyclines, as excess Ca²⁺ can antagonize aminoglycoside activity.
- Mg²⁺ Concentration: Adjusted to 10–12.5 mg/L (as Mg²⁺). Excess Mg²⁺ can antagonize the activity of aminoglycosides against Pseudomonas aeruginosa.
- pH: Final pH must be 7.2–7.4 at room temperature. pH variations can drastically alter the activity of certain agents (e.g., macrolides, aminoglycosides).
- Thymidine/Thymine Content: Must be low to prevent antagonism of sulfonamides and trimethoprim.
Protocol for CAMHB Preparation:
- Rehydrate commercial Mueller-Hinton broth powder according to manufacturer's instructions.
- Adjust divalent cation levels by adding sterile solutions of CaCl₂ and MgCl₂ as needed. Confirm concentrations via atomic absorption spectroscopy or using commercial broth with verified levels.
- Adjust pH to 7.2–7.4 using 1N NaOH or 1N HCl.
- Filter sterilize (0.22 µm pore size) and store at 2–8°C.
Quantitative Specifications for Broth Media
Table 1: CLSI M07 Specifications for Cation-Adjusted Mueller-Hinton Broth
| Parameter | Target Specification | Rationale |
|---|---|---|
| Calcium (Ca²⁺) | 20 – 25 mg/L | Standardizes aminoglycoside & tetracycline activity |
| Magnesium (Mg²⁺) | 10 – 12.5 mg/L | Prevents false resistance in P. aeruginosa with aminoglycosides |
| pH | 7.2 – 7.4 (at 25°C) | Maintains optimal & reproducible drug activity |
| Thymidine Content | Low (<0.1 µg/mL) | Prevents antagonism of trimethoprim/sulfamethoxazole |
Inoculum Preparation: Standardizing the Challenge
Inoculum density is a primary source of variability in MIC testing. The M07 method standardizes this to approximately 5 x 10⁵ CFU/mL in each well of the final microdilution plate.
Protocol for Inoculum Preparation via Direct Colony Suspension Method:
- Select 3–5 well-isolated colonies of the target organism from an overnight (18–24 hour) non-selective agar plate.
- Transfer colonies to a tube containing 4–5 mL of sterile saline (0.85–0.9%) or Mueller-Hinton Broth.
- Vortex thoroughly to create a homogeneous suspension.
- Adjust the turbidity of the suspension to match a 0.5 McFarland standard using a densitometer or visual comparator.
- A 0.5 McFarland standard yields a suspension containing approximately 1–2 x 10⁸ CFU/mL for E. coli.
- Within 15 minutes of adjustment, dilute the standardized suspension 1:150 in sterile saline or broth to achieve a working inoculum of ~5 x 10⁵ CFU/mL.
- Example: Add 0.5 mL of the 0.5 McFarland suspension to 74.5 mL of CAMHB.
Protocol for Inoculum Preparation via Growth Method:
- Make a direct colony suspension as above, but adjust to a 0.5 McFarland standard using CAMHB.
- Incubate the suspension with shaking at 35 ± 2°C until it reaches the turbidity of a 0.5 McFarland standard (typically 2–6 hours).
- Dilute the actively growing culture as needed in CAMHB to achieve a working inoculum of ~5 x 10⁵ CFU/mL.
Verification: Inoculum density should be verified periodically by performing viable plate counts on the working suspension.
Plate Format and Testing Procedure
Microdilution plates are typically 96-well U-bottom plates, which facilitate the observation of small pellets of precipitated growth. Each well contains a serial two-fold dilution of an antimicrobial agent in a defined volume (typically 50–100 µL) of CAMHB.
Protocol for Plate Preparation and Inoculation:
- Plate Formatting: Antimicrobial stock solutions are serially diluted in CAMHB and dispensed into the plate. Columns 1-11 contain decreasing concentrations of drug. Column 12 is a growth control well (broth + inoculum, no drug).
- Inoculation: Add an equal volume (e.g., 50 µL) of the prepared working inoculum (~5 x 10⁵ CFU/mL) to each well of the plate, doubling the volume and halving the drug concentration. The final target inoculum is ~2.5–5 x 10⁵ CFU/mL per well.
- Sealing & Incubation: Seal the plate with a non-permeable lid or adhesive film. Incubate aerobically at 35 ± 2°C for 16–20 hours.
- Reading Results: Read the MIC as the lowest concentration of antimicrobial agent that completely inhibits visible growth of the organism. Use a reading mirror for accuracy. The growth control must show confluent turbidity, and the sterility control (broth only) must be clear.
Table 2: Standardized Parameters for M07 Microdilution Testing
| Parameter | Specification | Notes |
|---|---|---|
| Final Inoculum Density | 5 x 10⁵ CFU/mL (± 1 log) | Verified by plate count |
| Well Volume (Final) | 100 µL | 50 µL drug + 50 µL inoculum common |
| Antibiotic Dilution Series | Two-fold serial dilutions | Covers CLSI breakpoint range |
| Incubation Conditions | 35 ± 2°C, Ambient Air, 16–20 hrs | Extended times for certain drugs |
| Plate Type | 96-well, U-bottom | Facilitates pellet visualization |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CLSI M07 Broth Microdilution
| Item | Function & Specification |
|---|---|
| Cation-Adjusted MH Broth (CAMHB) | Standard growth medium with controlled Ca²⁺ & Mg²⁺ levels. |
| Mueller-Hinton Agar (MHA) Plates | For subculturing and maintaining test isolates prior to testing. |
| 0.5 McFarland Standard | Turbidity standard for inoculum preparation (latex particle or BaSO₄). |
| Sterile Saline (0.85–0.9%) | For making initial bacterial suspensions and dilutions. |
| 96-Well Microdilution Plates | Sterile, U-bottom plates for housing the dilution series and inoculum. |
| Antimicrobial Reference Powders | High-purity, potency-certified powders for preparing stock solutions. |
| Multichannel Pipettes & Sterile Tips | For accurate and efficient transfer of inoculum across the plate. |
| Plate Sealing Film | Non-permeable adhesive film to prevent evaporation and contamination. |
| MIC Reading Mirror/Viewer | Aids in visualizing small amounts of growth or pellets in wells. |
Workflow and Pathway Visualizations
Title: M07 Broth Microdilution Core Workflow
Title: Critical Factors Influencing MIC Result Reliability
The Clinical and Laboratory Standards Institute (CLSI) M07 standard, “Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically,” is the definitive reference for broth microdilution (BMD) methods. Within a broader thesis on CLSI M07 method research, recent updates (2023-2024) refine critical procedural details, acceptance criteria, and quality control (QC) parameters to address emerging challenges in antimicrobial susceptibility testing (AST). This review synthesizes these technical revisions and their implications for research and drug development.
Key Quantitative Updates in M07 (2023-2024)
The following tables summarize the primary quantitative changes and clarifications introduced.
Table 1: Updated QC Ranges for Key Antimicrobial Agents
| Organism (QC Strain) | Antimicrobial Agent | Previous MIC Range (μg/mL) | Updated MIC Range (μg/mL) | CLSI Document Reference |
|---|---|---|---|---|
| E. coli ATCC 25922 | Cefiderocol | 0.03-0.12 | 0.015-0.06 | M100-Ed34 |
| P. aeruginosa ATCC 27853 | Ceftolozane-Tazobactam | 0.5-4 | 0.25-2 | M100-Ed34 |
| S. aureus ATCC 29213 | Delafloxacin | 0.008-0.03 | 0.004-0.015 | M100-Ed34 |
| E. faecalis ATCC 29212 | Daptomycin | 1-4 | 0.5-4 (Ca²⁺ adj.) | M100-Ed34 |
Table 2: Clarified Technical Specifications for BMD
| Parameter | Previous Guidance (Pre-2023) | Refined Guidance (2023-2024) |
|---|---|---|
| Inoculum Preparation (McFarland) | 0.5 McFarland standard | Emphasizes direct colony suspension and verification via colony count or photometric methods. |
| Incubation Time for Staphylococcus spp. | 16-20 hours | Specifies 20-24 hours for oxacillin and cefoxitin against S. aureus to ensure mecA expression. |
| Cation Adjustment for Daptomycin Testing | Mueller-Hinton Broth (MHB) with Ca²⁺ | Mandates final Ca²⁺ concentration of 50 µg/mL and provides detailed preparation protocol. |
| Quality Control Frequency | Daily (or with each run) | Allows for weekly QC if established criteria are met (≥30 consecutive days of acceptable results). |
Detailed Experimental Protocols
Updated Broth Microdilution for Daptomycin (Ca²⁺-Adjusted)
Objective: To determine the MIC of daptomycin against Enterococcus spp. and Staphylococcus spp. Methodology:
- Broth Preparation: Prepare Ca²⁺-adjusted MHB. Dissolve MHB powder in distilled water, autoclave, and cool. Aseptically add a sterile 1% CaCl₂ solution to achieve a final concentration of 50 µg/mL Ca²⁺. Verify concentration if needed.
- Antimicrobial Dilution: Prepare a stock solution of daptomycin in sterile water. Perform two-fold serial dilutions in the Ca²⁺-adjusted MHB across the 96-well microdilution tray (final volume: 50 µL/well).
- Inoculum Standardization: Using a direct colony suspension method, adjust a bacterial suspension to a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL). Dilute this suspension 1:100 in sterile saline or water, then further dilute 1:20 in Ca²⁺-adjusted MHB to achieve ~5 x 10⁵ CFU/mL.
- Inoculation: Add 50 µL of the adjusted inoculum to each well of the antimicrobial-containing tray. Final inoculum: ~2.5 x 10⁵ CFU/well. Include growth (antimicrobial-free) and sterility (broth-only) controls.
- Incubation & Reading: Seal tray and incubate aerobically at 35±2°C for 16-20 hours. The MIC is the lowest concentration that completely inhibits visible growth.
QC Procedure Using Weekly Monitoring Protocol
Objective: To implement the optional weekly QC testing after establishing performance. Methodology:
- Initial Daily QC: For a minimum of 30 consecutive test days, perform QC using appropriate ATCC strains (E. coli 25922, S. aureus 29213, etc.) with each batch of clinical or research isolates.
- Data Logging: Record all MIC results. All results for each drug-organism pair must fall within the published QC range for the 30-day period.
- Transition to Weekly QC: After successful validation, QC testing for that specific drug-organism-strain combination may be performed weekly. Each test run must still include the required growth controls.
- Failure Action: If any weekly QC result is out of range, revert to daily QC for that agent until the problem is identified, corrected, and another 30-day period of in-control results is documented.
Visualizing Key Methodological Updates
Title: Updated Broth Microdilution Inoculum Prep Workflow
Title: Decision Tree for QC Testing Frequency (CLSI M07)
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for CLSI M07-Compliant BMD
| Item | Function/Brief Explanation |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium containing optimal levels of Ca²⁺ and Mg²⁺ ions for AST. |
| Sterile 1% Calcium Chloride (CaCl₂) Solution | Used to supplement MHB to the precise 50 µg/mL final concentration required for reliable daptomycin MICs. |
| Frozen or Lyophilized Microdilution Panels | Pre-manufactured 96-well panels containing serial dilutions of antimicrobials, ensuring standardization and reproducibility. |
| Tryptic Soy Agar (TSA) or Blood Agar Plates | For sub-culture and preparation of pure, 18-24 hour old bacterial colonies for inoculum. |
| 0.5 McFarland Turbidity Standard | Reference for standardizing bacterial inoculum density either visually or via densitometer. |
| ATCC Quality Control Strains (e.g., E. coli 25922, S. aureus 29213) | Essential for validating the accuracy and precision of the test system as per CLSI guidelines. |
| Sterile Saline (0.85-0.9% NaCl) | For making bacterial suspensions and performing critical dilution steps. |
| Multichannel Pipettes (e.g., 50 µL volume) | Enables rapid, accurate, and reproducible inoculation of microdilution trays. |
| Microdilution Tray Sealing Film | Prevents evaporation and cross-contamination during the 16-24 hour incubation period. |
The Clinical and Laboratory Standards Institute (CLSI) M07 standard, formally titled "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," is the definitive reference broth microdilution (BMD) method for antimicrobial susceptibility testing (AST). Its global importance stems from its adoption and citation by major regulatory and standard-setting bodies, which use it to ensure the accuracy, reproducibility, and clinical relevance of AST data critical for drug development and patient care.
Table 1: M07 Citation in Global Guidelines
| Regulatory Body | Guideline Document | Primary Role of M07 | Status |
|---|---|---|---|
| U.S. FDA | Various Drug-Specific Guidance, e.g., "Acute Bacterial Skin and Skin Structure Infections: Developing Drugs for Treatment" | Defines the reference method for establishing in vitro susceptibility of drug candidates and for validating commercial AST devices. Cited for MIC determination of comparator agents. | Mandatory for regulatory submissions. |
| EUCAST | EUCAST Definitive Document (EDef) 3.1 & 7.1 (Method for MIC determination) | Forms the methodological basis. EUCAST has harmonized its BMD methodology with CLSI M07, with minor modifications (e.g., inoculum preparation, some media specifications). | Foundational. EUCAST describes its method as "based on" the CLSI standard. |
| CLSI | M07 (current edition: M07-A11/EUCAST 7.1) | The source document. Provides the comprehensive, detailed procedural standard for performing reference BMD. | The core standard. |
| Ph. Eur./USP | General Chapter 5.1.4 (Microbiological assay of antibiotics) & various monographs | Referenced as the standard method for determining minimum inhibitory concentrations (MICs) for potency assays and quality control. | Referenced standard. |
| Japanese PMDA | Various, including "Microbiological Data for Antimicrobial Products" | Recognized as an acceptable reference method for clinical trials and drug approval submissions. | Accepted standard. |
Core Methodological Protocols from CLSI M07
The following is a synthesized workflow of the critical experimental protocols defined in CLSI M07.
Protocol 1: Preparation of Antimicrobial Stock Solutions
- Purpose: To create standardized, high-concentration solutions of antimicrobial agents for subsequent dilution in microdilution trays.
- Materials: Analytical-grade antimicrobial powder, precise balance, appropriate solvent (as specified in M07 Table 6A), diluent (often sterile distilled water or buffer), sterile vials.
- Method:
- Calculate the required mass of powder to achieve a stock concentration of at least 1000 µg/mL (or higher, e.g., 5120 µg/mL).
- Dissolve the powder in the specified solvent. For poorly water-soluble drugs, a small volume of alternative solvent (e.g., dimethyl sulfoxide, acidic/basic buffer) may be used initially.
- Dilute to final volume with the appropriate diluent.
- Filter-sterilize (0.22 µm pore size) if not prepared aseptically.
- Aliquot and store at -70°C or below (unless stability data support less stringent conditions).
Protocol 2: Broth Microdilution Panel Preparation
- Purpose: To create a serial two-fold dilution series of the antimicrobial agent in cation-adjusted Mueller-Hinton Broth (CAMHB) within a 96-well microdilution tray.
- Materials: Antimicrobial stock solution, CAMHB, sterile 96-well trays, multichannel pipettes, automated dilutor/dispenser.
- Method:
- Prepare CAMHB according to manufacturer instructions. For testing Streptococcus pneumoniae or other fastidious organisms, supplement with 2.5-5% lysed horse blood.
- Using a multichannel pipette or automated system, dispense 50 µL of CAMHB into all wells of the tray.
- Add 50 µL of the antimicrobial stock solution to the first well (highest concentration).
- Serially dilute by transferring 50 µL from well 1 to well 2, mixing, and continuing across the plate. Discard 50 µL from the final well.
- The final volume in each well is 50 µL, containing the antimicrobial at the desired final concentration range (e.g., 64 to 0.03 µg/mL).
Protocol 3: Inoculum Preparation and Standardization
- Purpose: To prepare a standardized bacterial inoculum of approximately 5 x 10⁵ CFU/mL in the final test well.
- Materials: Fresh overnight bacterial culture on non-selective agar, sterile saline or broth, spectrophotometer, adjustable pipettes.
- Method (Direct Colony Suspension):
- Select 3-5 well-isolated colonies from an 18-24 hour agar plate.
- Suspend colonies in sterile saline or broth.
- Adjust the turbidity to a 0.5 McFarland standard using a spectrophotometer (optical density of 0.08-0.13 at 625 nm). This yields a suspension of ~1-2 x 10⁸ CFU/mL.
- Dilute this suspension 1:100 in sterile saline or water to create a "working suspension" of ~1-2 x 10⁶ CFU/mL.
- Further dilute this 1:20 by adding 10 µL to 190 µL of CAMHB in a tube or well. The final test inoculum is ~5 x 10⁵ CFU/mL in a total volume of 100 µL per well (50 µL drug + 50 µL inoculated broth).
Protocol 4: Inoculation, Incubation, and MIC Reading
- Purpose: To conduct the test and determine the Minimum Inhibitory Concentration (MIC).
- Materials: Prepared microdilution tray, standardized inoculum, multichannel pipette, sterile reservoir, incubator set to 35°C ± 2°C.
- Method:
- Add 50 µL of the standardized inoculum (from Protocol 3, step 4) to each well of the drug-containing microdilution tray. Use a growth control well (CAMHB + inoculum) and a sterility control well (CAMHB only).
- Seal the tray with a lid or adhesive seal.
- Incubate under ambient air at 35°C ± 2°C for 16-20 hours (standard organisms). Incubate S. pneumoniae and other fastidious organisms for 20-24 hours in ambient air.
- Read the MIC visually. The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth as observed with the unaided eye.
Visualizing the Regulatory and Methodological Ecosystem
Diagram 1: M07 as the Foundational Hub for Global AST
Diagram 2: Core Broth Microdilution Experimental Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents & Materials for M07-Compliant BMD
| Item | Function & Specification | Critical Notes |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | The standard medium for non-fastidious organisms. Contains controlled levels of Ca²⁺ and Mg²⁺ cations, which critically affect the activity of aminoglycosides and polymyxins. | Must meet lot-to-lot performance standards using CLSI QC strains. |
| CAMHB with Lysed Horse Blood (LHB) | Supplemented (2.5-5%) for testing fastidious organisms like S. pneumoniae, Haemophilus spp., and other streptococci. | Lysis removes inhibitors and provides necessary growth factors (X and V factors for Haemophilus). |
| Reference Antimicrobial Powders | High-purity, potency-certified powders for preparing in-house stock solutions. Used for investigational drug testing or validating commercial panels. | Source from reputable suppliers (e.g., USP, Sigma). Potency must be accounted for in concentration calculations. |
| Quality Control (QC) Strains | Frozen stocks of well-characterized strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213). | Used daily to verify the precision and accuracy of the entire test system (media, inoculum, drugs, incubation). |
| 96-Well Microdilution Trays | Sterile, non-pyrogenic, U-bottom or flat-bottom polystyrene trays. U-bottom is standard for easier visual reading. | Must be compatible with automated inoculators and readers if used. |
| McFarland Standards (0.5) | Provides the optical reference for standardizing the bacterial inoculum turbidity. Can be physical tubes or a calibrated densitometer. | Critical for achieving the target final inoculum of ~5 x 10⁵ CFU/mL. |
| Sterile Saline (0.85-0.9%) | Isotonic solution for suspending bacterial colonies and preparing inoculum dilutions. | Prevents osmotic shock to the bacterial cells during suspension. |
| Multichannel/Micro-volume Pipettes | For accurate, reproducible dispensing of small volumes (50-100 µL) of broth, drugs, and inoculum across 96-well plates. | Regular calibration is essential for data integrity. |
| Automated Plate Reader (Optional) | Spectrophotometric or imaging device to objectively determine MIC endpoints, improving reproducibility and enabling high-throughput. | Must be validated against visual reading per CLSI guidelines. |
Step-by-Step Protocol: Executing the CLSI M07 Broth Microdilution Method
The reliability of any antimicrobial susceptibility testing (AST) study hinges upon the foundational steps of reagent and stock solution preparation. Within the framework of CLSI standard M07 for broth microdilution method research, precision in these initial stages dictates the validity of Minimum Inhibitory Concentration (MIC) data, which informs critical decisions in drug development and resistance monitoring. This guide details the technical protocols and considerations essential for robust, reproducible research.
Core Reagent Preparation for Broth Microdilution
The growth medium must support robust growth of control organisms while not interfering with the antimicrobial's activity. Cation-adjusted Mueller Hinton Broth (CAMHB) is the standard medium specified by CLSI M07.
Protocol: Preparation of CAMHB
- Weigh the appropriate quantity of commercially available Mueller Hinton Broth powder as per manufacturer's instructions (typically 21g/L for the base broth).
- Dissolve in distilled or deionized water with gentle heating and stirring.
- Autoclave at 121°C for 15 minutes. Allow to cool to room temperature.
- Aseptically supplement with cations to achieve final concentrations of:
- Calcium (Ca²⁺): 20-25 mg/L (50-100 µM)
- Magnesium (Mg²⁺): 10-12.5 mg/L (20-50 µM)
- This is typically done using filter-sterilized stock solutions of CaCl₂ and MgCl₂.
- Adjust pH to 7.2-7.4 at room temperature using sterile acid or base. Verify pH after adjustment and storage.
Table 1: Critical Quality Control Parameters for CAMHB
| Parameter | Target Specification | Rationale & Impact |
|---|---|---|
| pH | 7.2 - 7.4 (at 25°C) | pH affects antimicrobial stability and activity (e.g., aminoglycosides more active at alkaline pH, tetracyclines at acidic pH). |
| Divalent Cations | Ca²⁺: 20-25 mg/L; Mg²⁺: 10-12.5 mg/L | Standardizes conditions; affects activity of aminoglycosides (enhanced by Mg²⁺) and tetracyclines (chelated by cations). |
| Thymidine/Thymine Content | Minimal to absent | Prevents antagonism of trimethoprim and sulfonamide activity. |
| Sterility | No growth after 72h incubation | Prevents contamination of test panels. |
| Performance Check | MICs for QC strains within published ranges | Validates the entire medium preparation system. |
Antimicrobial Stock Solution Preparation
Accurate stock solutions are paramount. Errors at this stage are multiplicative and invalidate subsequent dilutions.
Protocol: Standard Preparation of a 1280 µg/mL (or 2560 µg/mL) Primary Stock
- Calculate Mass: Determine the mass of antimicrobial powder required using the formula: Mass (mg) = (Desired Concentration (µg/mL) * Desired Volume (mL)) / Potency (µg/mg). Potency is specific to each batch, as stated on the Certificate of Analysis.
- Weighing: Use an analytical balance (minimum 4 decimal places) in a controlled environment. Pre-weigh an appropriate vessel to correct for tare weight.
- Solubilization: Dissolve the powder in the correct solvent (see Table 2). Vortex or sonicate as needed.
- Dilution to Final Volume: Transfer to a volumetric flask and dilute to the final mark with the appropriate diluent (often sterile water or buffer). Mix thoroughly.
- Aliquoting & Storage: Aseptically aliquot into sterile, tightly sealed vials. Label with compound name, concentration, date, batch number, and storage conditions. Store per stability data (typically ≤ -60°C for long-term).
Table 2: Common Solvents and Diluents for Antimicrobial Stock Solutions
| Antimicrobial Class | Recommended Solvent | Primary Diluent | Stability Considerations (Approx.) |
|---|---|---|---|
| β-lactams (Penicillins, Cephalosporins) | Phosphate Buffer (pH 6.0, 0.1M) | Sterile Water or Buffer | Unstable; prepare fresh weekly; store at -60°C or below. |
| Aminoglycosides | Sterile Water or Phosphate Buffer | Sterile Water | Stable for 1 year at -60°C; avoid repeated freeze-thaw. |
| Fluoroquinolones | Water with 0.1N NaOH (if needed) | Sterile Water | Stable for 1 year at -60°C. |
| Macrolides | Methanol or Ethanol (small volume) | Sterile Water | Stable for 1 year at -60°C; ensure ethanol ≤1% final in test. |
| Tetracyclines | Water with 0.1N HCl (if needed) | Sterile Water | Light sensitive; stable for 1 year at -60°C in dark. |
| Glycopeptides (Vancomycin) | Sterile Water | Sterile Water | Stable for 1 year at -60°C. |
| Azoles (Fluconazole) | Sterile Water | Sterile Water | Stable for 1 year at -60°C or 6 months at -20°C. |
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Analytical Balance (0.0001g) | Precise weighing of antimicrobial powders is non-negotiable for accurate stock concentrations. |
| Certified Reference Standard Powder | High-purity antimicrobial with a known potency and assigned expiry date, traceable to a national/international standard. |
| pH Meter (Calibrated) | Ensures CAMHB and any buffers are within the strict pH range (7.2-7.4) required by CLSI M07. |
| Class A Volumetric Glassware | Provides the highest accuracy for preparing standard solutions and final broth volumes. |
| Sterile, Low-Binding Microcentrifuge Tubes & Vials | For aliquoting and storing stock solutions to prevent adsorption to container walls and maintain sterility. |
| Ultra-Low Temperature Freezer (≤ -60°C) | For long-term storage of stock solutions to maintain antimicrobial stability. |
| Solvent Filter Units (0.22 µm) | For sterilizing solvents, diluents, and cation supplements that cannot be autoclaved. |
| QC Strain Panels | Frozen stocks of reference strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) for validating medium and test performance. |
Workflow and Quality Control Integration
AST Reagent Preparation and QC Workflow
Detailed Broth Microdilution Panel Preparation Protocol
Protocol: Two-Fold Serial Dilution in 96-Well Trays
- Thaw Stock: Thaw the primary antimicrobial stock solution (e.g., 2560 µg/mL) and warm to room temperature. Vortex briefly.
- Prepare Intermediate Dilution: In a sterile tube, dilute the primary stock in CAMHB to create an intermediate concentration that is twice the desired highest test concentration (e.g., for a high test concentration of 64 µg/mL, prepare 128 µg/mL in 10 mL CAMHB).
- Panel Loading: Aseptically add 100 µL of CAMHB to all wells of a sterile 96-well tray (columns 2-12).
- Serial Dilution: Add 100 µL of the intermediate antimicrobial solution to all wells of column 1. Perform a two-fold serial dilution by transferring 100 µL from column 1 to column 2, mixing thoroughly, then from column 2 to column 3, and so on through column 11. Discard 100 µL from column 11. Column 12 serves as the growth control (no antimicrobial).
- Inoculum Addition: Prepare a standardized bacterial inoculum of 5 x 10⁵ CFU/mL in CAMHB. Add 100 µL of this inoculum to each well of columns 1-11. Add 100 µL of inoculated broth to column 12. This results in a final volume of 200 µL/well and a final antimicrobial concentration range (e.g., 64, 32, 16,... µg/mL) with ~5 x 10⁵ CFU/mL.
- Incubation: Seal the tray and incubate at 35±2°C for 16-20 hours (as per organism and CLSI guidelines).
- MIC Determination: The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth.
Adherence to these critical first steps in reagent and stock solution preparation establishes the foundation for generating data that is precise, reproducible, and compliant with the rigorous standards of CLSI M07, ultimately driving meaningful research in antimicrobial drug development.
Within the framework of CLSI standard M07 for broth microdilution antimicrobial susceptibility testing, accurate inoculum preparation is the critical first step. The reliability of Minimum Inhibitory Concentration (MIC) endpoints depends entirely on the precision of the initial bacterial inoculum. This guide details the technical procedures for achieving a standardized 0.5 McFarland suspension and performing the subsequent dilutions required for testing, as mandated by CLSI M07.
The 0.5 McFarland Standard: Principles and Specifications
The McFarland standard is a turbidity benchmark. A 0.5 McFarland standard provides a reproducible optical density corresponding to a known approximate cell density, essential for creating a consistent starting inoculum.
Table 1: McFarland Standard Specifications
| McFarland Standard | Approximate Bacterial Density (CFU/mL) | % Transmittance | Absorbance (625 nm) |
|---|---|---|---|
| 0.5 | 1.5 x 10^8 | 74.3 - 77.4 | 0.08 - 0.13 |
| 1.0 | 3.0 x 10^8 | 55.6 - 60.2 | 0.22 - 0.27 |
| 2.0 | 6.0 x 10^8 | 35.0 - 40.7 | 0.39 - 0.46 |
CFU: Colony Forming Units. Data sourced from current CLSI M07 guidelines and instrument manuals.
Core Experimental Protocol: Inoculum Preparation per CLSI M07
Direct Colony Suspension Method (Primary Method)
Objective: To prepare a bacterial suspension directly from isolated colonies, adjusted to a 0.5 McFarland standard.
Materials: See "The Scientist's Toolkit" below. Procedure:
- Select 3-5 well-isolated, morphologically identical colonies from an 18-24 hour agar plate.
- Using a sterile loop or swab, transfer the colonies to a tube containing 4-5 mL of sterile saline (0.85% NaCl) or Mueller-Hinton Broth.
- Vortex the suspension vigorously for 15-20 seconds to achieve a homogeneous, clump-free suspension.
- Adjust the turbidity: a. Using a densitometer: Measure and add broth or saline until the reading is 0.08-0.13 at 625 nm. b. Using visual comparators: Compare against a 0.5 McFarland standard under appropriate lighting against a white background with a contrasting black line.
- Critical: The adjusted suspension must be used within 15 minutes of preparation.
Inoculum Dilution for Broth Microdilution
Objective: To dilute the 0.5 McFarland suspension to the final testing inoculum of approximately 5 x 10^5 CFU/mL.
Procedure:
- Perform a 1:150 dilution of the adjusted 0.5 McFarland suspension into cation-adjusted Mueller-Hinton Broth (CAMHB).
- Example: Add 0.1 mL of suspension to 14.9 mL of CAMHB (or proportionally smaller volumes).
- This yields a "turbidity-adjusted inoculum" with a target density of ~1 x 10^6 CFU/mL.
- Dispense this diluted inoculum into the wells of a microdilution tray. The act of adding an equal volume of this inoculum to wells containing an equal volume of 2X drug solution (or broth for growth control) results in a final 1:2 dilution.
- Final Result: Each test well contains ~5 x 10^5 CFU/mL in a total volume of 100 µL (typical).
Table 2: Dilution Scheme for Broth Microdilution
| Step | Suspension | Diluent | Dilution Factor | Approximate CFU/mL |
|---|---|---|---|---|
| 1 | Colonies | Saline | N/A | Adjusted to 1.5 x 10^8 |
| 2 | 0.5 McFarland | CAMHB | 1:150 | 1 x 10^6 |
| 3 | Diluted Inoculum | 2X Drug in Well | 1:2 (Final) | 5 x 10^5 |
Quality Control and Validation
- Purity Check: Subculture the adjusted suspension to confirm purity.
- Quantitative Verification: Perform colony counts on the final diluted inoculum. Plate 10 µL of the 1:150 dilution onto an agar plate. After incubation, the number of colonies x 100 = CFU/mL in the diluted inoculum. Target: 0.5 - 2 x 10^6 CFU/mL.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Inoculum Standardization
| Item | Function | Key Specifications |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for susceptibility testing. | Contains controlled levels of Ca2+ and Mg2+ ions as per CLSI. |
| Sterile 0.85% Saline | Suspension fluid for initial colony suspension. | Isotonic to prevent osmotic shock to bacterial cells. |
| McFarland Standards (0.5) | Primary turbidity reference. | Sealed tubes or latex particle suspensions; replaced periodically. |
| Turbidity Densitometer | Instrument for precise optical density measurement. | Wavelength: 625 nm; requires regular calibration. |
| Sterile Polystyrene Tubes | For preparing and adjusting suspension. | Non-inhibitory, clear for turbidity reading. |
| Digital Dispensers/Pipettes | For accurate volume transfers during dilution. | Calibrated regularly; capable of dispensing 10 µL - 10 mL. |
| Vortex Mixer | To create homogenous bacterial suspensions. | Must provide sufficient agitation to break up clumps. |
Visualized Workflows
The Clinical and Laboratory Standards Institute (CLSI) document M07, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," serves as the authoritative protocol for broth microdilution (BMD) testing. A cornerstone of the method's reproducibility and clinical relevance is the precise establishment of the drug dilution series and appropriate controls within the microdilution tray. This whitepaper details the technical execution of this critical step, providing an in-depth guide for researchers and drug development professionals to ensure data integrity, support antibiotic discovery, and generate results compliant with CLSI M07 standards.
Core Principles: Drug Dilution Series Design
The BMD method quantifies the Minimum Inhibitory Concentration (MIC) by testing a series of drug concentrations against a standardized bacterial inoculum. The series is typically a two-fold serial dilution, yielding a concentration range that brackets the expected MIC of target organisms.
Quantitative Parameters for Drug Preparation
Stock Solution Preparation: A primary stock solution of the test antimicrobial agent is prepared at a high concentration (e.g., 1280 µg/mL or 10× the highest test concentration). Solubility, stability, and solvent choice must be justified and documented per CLSI M07 guidelines. Appropriate safety data sheets (SDS) must be consulted.
Dilution Series Calculation: The final test concentrations in the broth are achieved through a serial dilution workflow. The following table summarizes a standard 96-well plate layout for a single antimicrobial agent.
Table 1: Example Two-Fold Serial Dilution Scheme for a 96-Well Plate
| Well Row | Dilution Step | Volume Transfer | Diluent Volume | Relative Final Concentration (µg/mL) | Purpose |
|---|---|---|---|---|---|
| A1-A12 | Primary Stock | N/A | N/A | 128 (Highest) | Test series start |
| B1-B12 | 1:2 from Row A | 100 µL → | 100 µL | 64 | Two-fold dilution |
| C1-C12 | 1:2 from Row B | 100 µL → | 100 µL | 32 | Two-fold dilution |
| D1-D12 | 1:2 from Row C | 100 µL → | 100 µL | 16 | Two-fold dilution |
| E1-E12 | 1:2 from Row D | 100 µL → | 100 µL | 8 | Two-fold dilution |
| F1-F12 | 1:2 from Row E | 100 µL → | 100 µL | 4 | Two-fold dilution |
| G1-G12 | 1:2 from Row F | 100 µL → | 100 µL | 2 | Two-fold dilution |
| H1-H12 | 1:2 from Row G | 100 µL → | 100 µL | 1 (Lowest) | Test series end |
Note: After final transfer, 100 µL is discarded from the last row (H) to maintain equal volumes. The actual concentration values are example placeholders.
Essential Controls in BMD per CLSI M07
Controls validate the entire test system. Their inclusion is non-negotiable for CLSI-compliant research.
Table 2: Mandatory and Recommended Controls for BMD Trays
| Control Type | Well Position Example | Composition | Acceptable Result | Function |
|---|---|---|---|---|
| Growth Control | Column 11, All Rows | Broth + Inoculum (No drug) | Visible Growth | Confirms organism viability and adequate incubation. |
| Sterility Control | Column 12, All Rows | Broth Only (No drug, No inoculum) | No Growth | Confirms media sterility and aseptic technique. |
| Solvent Control | As Needed | Broth + Inoculum + Max [Solvent] | Growth equal to Growth Control | Rules out solvent toxicity. |
| Reference Strain Control | Separate Tray/Plate | Broth + QC Strain + Drug Series | MIC within published QC range | Verifies drug potency and procedure accuracy. |
Detailed Experimental Protocol: Tray Setup
Protocol 1: Manual Preparation of Drug Dilution Series in a 96-Well Tray Materials: Sterile 96-well U-bottom microtiter plate, multichannel pipettes, sterile reservoirs, antimicrobial stock solution, cation-adjusted Mueller-Hinton Broth (CAMHB), sterile pipette tips. Procedure:
- Labeling: Label the plate with drug name, date, batch, and organism identifiers.
- Diluent Addition: Using a multichannel pipette, add 100 µL of CAMHB to wells B12 through H12 (sterility control column) and wells B1 through H11 (all test columns except the first row).
- Initial Drug Addition: Add 200 µL of the prepared antimicrobial stock solution to wells A1 through A11.
- Serial Dilution: Mix the contents of row A thoroughly. Transfer 100 µL from row A to row B. Mix row B thoroughly. Continue this two-fold serial dilution through row G, transferring 100 µL each time.
- Final Volume Adjustment: After mixing row G, transfer 100 µL from row G to row H. Mix row H and discard 100 µL from row H to leave a final volume of 100 µL in all wells.
- Inoculum Addition: Prepare a 0.5 McFarland standard suspension of the test organism and dilute it in CAMHB to achieve a final inoculum of ~5 × 10⁵ CFU/mL. Using a multichannel pipette, add 100 µL of this adjusted inoculum to all wells in columns 1-11 (drug and growth control wells).
- Sterility Control Setup: Add 100 µL of sterile CAMHB (no inoculum) to all wells in column 12.
- Incubation: Cover the plate, place it in a sealed container or plastic bag to prevent evaporation, and incubate aerobically at 35 ± 2 °C for 16-20 hours as per CLSI M07.
Protocol 2: Using Pre-prepared, Frozen Microdilution Trays Materials: Commercially prepared or laboratory-made frozen trays, water bath at 35-40°C, calibrated inoculum delivery system. Procedure:
- Thawing: Remove tray from frozen storage (-70°C or lower) and thaw at room temperature or in a 35-40°C water bath for ≤30 minutes.
- Drying: Place the thawed tray in a laminar flow hood with the lid slightly ajar for 10-15 minutes to eliminate condensation on the lid.
- Inoculation: Following CLSI M07 inoculum preparation standards, use a replicator or multichannel pipette to deliver 0.005-0.01 mL (5-10 µL) of the adjusted inoculum (~5 × 10⁵ CFU/mL) directly onto the surface of the broth in each well. This results in a 1:10 to 1:20 final dilution.
- Mixing: Gently tap or vortex the tray to mix.
- Incubation: Incubate as described in Protocol 1, Step 8.
Visualization: BMD Tray Setup and Testing Workflow
Diagram Title: Broth Microdilution Tray Setup and Testing Workflow
Diagram Title: 96-Well Plate Layout for MIC Testing and Controls
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for BMD Tray Setup
| Item | Function | Technical Specification / Notes |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for susceptibility testing. | Must contain Ca²⁺ (20-25 mg/L) and Mg²⁺ (10-12.5 mg/L) as per CLSI M07. Ensures reproducible cation-dependent drug activity (e.g., aminoglycosides, polymyxins). |
| Sterile, U-Bottom 96-Well Microtiter Plates | Reaction vessel for the dilution series and incubation. | Polystyrene, non-tissue-culture-treated. U-bottom facilitates pellet formation for clear visual endpoint reading. Must be lid-compatible to prevent evaporation. |
| Precision Multichannel Pipettes | Enables accurate, high-throughput liquid handling for serial dilutions and inoculation. | Typically 8- or 12-channel, volumes 1-50 µL and 30-300 µL. Regular calibration is essential for volumetric accuracy. |
| McFarland Standard (0.5) | Visual or densitometric reference for standardizing bacterial inoculum density. | Corresponds to ~1-2 x 10⁸ CFU/mL for E. coli. Use commercial latex standards or a calibrated densitometer for accuracy. |
| Quality Control (QC) Strains | Validates drug potency and procedural accuracy. | CLSI M07 specifies strains (e.g., S. aureus ATCC 29213, P. aeruginosa ATCC 27853). Their MICs must fall within published QC ranges. |
| Sterile Dilution Buffers/Solvents | For solubilizing antimicrobial agents. | Common solvents include sterile water, dimethyl sulfoxide (DMSO), or specific pH buffers. Must be validated for non-interference with bacterial growth. |
| Automated Plate Inoculation System (e.g., replicator) | Alternative to manual pipetting for high-throughput studies. | Delivers a precise, small volume (5-10 µL) of inoculum simultaneously to all wells, improving speed and reproducibility. |
| Plate Sealing Film or Humidified Chamber | Prevents evaporation during incubation. | Critical for maintaining well volume and drug concentration over the 16-20 hour incubation period. |
Incubation Conditions, Timing, and Environmental Controls
The Clinical and Laboratory Standards Institute (CLSI) document M07, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," is the definitive standard for broth microdilution (BMD) testing. While M07 defines critical procedural parameters, the optimization of incubation conditions, timing, and environmental controls remains a focal point of ongoing research. This whitepaper delves into the technical nuances of these variables, framed within the broader thesis that precise, reproducible, and clinically predictive BMD results are contingent upon strict, evidence-based incubation protocols beyond the foundational M07 guidelines. For drug development professionals and researchers, mastering these elements is paramount for generating robust data for novel antimicrobial agents and understanding resistance mechanisms.
Core Incubation Parameters: A Quantitative Analysis
The standard incubation conditions per CLSI M07 (11th Edition, 2018) for non-fastidious aerobic bacteria are 35°C ± 1°C in ambient air for 16-20 hours. However, research into specific organism-antimicrobial combinations and resistance phenotypes necessitates deviations and precise controls.
Table 1: Standard and Research-Based Incubation Conditions
| Organism Category | Temperature (°C) | Atmosphere | Duration (Hours) | Rationale & Research Context |
|---|---|---|---|---|
| Non-fastidious Aerobes (Standard) | 35 ± 1 | Ambient Air | 16-20 | CLSI M07 baseline. Critical for reproducibility of MIC endpoints. |
| Staphylococcus spp. (MRSA detection) | 35 ± 1 | Ambient Air | Full 24 | Research indicates ≤20h may miss inducible resistance (e.g., mecA). Essential for cefoxitin screening. |
| Streptococcus pneumoniae & Viridans Group | 35 ± 1 | 5% CO₂ | 20-24 | Enhanced growth in CO₂. CO₂ can acidify media, affecting aminoglycoside/tetracycline MICs. Must be controlled. |
| Haemophilus influenzae | 35 ± 1 | 5% CO₂ | 20-24 | Standard for fastidious organisms. Requires HTM broth, validated for CO₂ incubation. |
| Neisseria gonorrhoeae | 35 ± 1 | 5% CO₂ | 20-24 | CO₂ essential. Use GC agar base supplement. Duration may extend for some antimicrobials. |
| Non-tuberculous Mycobacteria (e.g., M. avium) | 30-35 (species-dependent) | Ambient Air | 3-7 days (up to 14) | Research area: Slow growth requires extended incubation. Temperature optima vary. Mueller-Hinton broth with OADC enrichment. |
| Carbapenemase-Producing Enterobacterales (CPE) | 35 ± 1 | Ambient Air | 16-20 + Reading at 4h/8h | Early-read studies for rapid phenotypic detection (e.g., colorimetric methods) alongside standard MIC. |
Environmental Controls & Their Impact on MIC
Temperature Uniformity and Calibration
A deviation of >1°C can significantly alter bacterial growth kinetics and MIC results. Research-grade incubators must have:
- Continuous Monitoring: Data-logging probes independent of incubator display.
- Mapping Studies: Validation of temperature uniformity across all shelf positions.
- Calibration: Traceable to national standards, performed at least annually.
Atmospheric Composition
- CO₂ Incubation: Lowers pH of unbuffered media (e.g., standard Mueller-Hinton Broth). This can increase MICs of aminoglycosides, macrolides, and tetracyclines, and decrease MICs of beta-lactams. CLSI-approved media for CO₂ incubation (e.g., CAMHB with TES buffer) mitigates this.
- Humidity: High humidity (>95%) is maintained in CO₂ incubators to prevent evaporation from microdilution wells, which can falsely elevate antimicrobial concentration and MIC.
Timing and Endpoint Determination
The incubation duration is intrinsically linked to the defined MIC endpoint: the lowest concentration that inhibits visible growth after a specified time.
- Early Reading: Research protocols for rapid resistance detection may use spectrophotometric or fluorometric readings at 4-8 hours, correlating to standard 16-20h MICs.
- Late Reading (>20h): Risks "skipped wells" or trailing endpoints, particularly with bacteriostatic agents. M07 advises against over-incubation but mandates it for specific agents (e.g., Staphylococcus with cefoxitin).
Detailed Experimental Protocols from Key Research
Protocol 1: Evaluating Incubation Time on Inducible Resistance Detection (e.g., MRSA)
Objective: To determine the optimal incubation time for reliable detection of methicillin-resistant Staphylococcus aureus (MRSA) using cefoxitin in BMD. Methodology:
- Strains: Use a panel of 50 S. aureus strains, including 20 confirmed MRSA (mecA+), 25 MSSA (mecA-), and 5 borderline oxacillin-resistant S. aureus (BORSA).
- Inoculum & Plating: Prepare 0.5 McFarland suspension in saline, dilute in CAMHB to achieve ~5x10⁵ CFU/mL. Aliquot 100 µL per well into a custom cefoxitin panel (range: 0.25-16 µg/mL).
- Incubation: Place panels in ambient air incubator at 35°C ± 0.5°C.
- Reading:
- Read MICs (complete inhibition) at 16h, 18h, 20h, 22h, and 24h.
- Record any well with >80% growth inhibition.
- Analysis: Compare MRSA detection rates (MIC ≥4 µg/mL) at each time point against mecA PCR as gold standard. Calculate sensitivity and specificity.
Protocol 2: Assessing CO₂-Induced MIC Shifts for Aminoglycosides
Objective: To quantify the effect of 5% CO₂ incubation on gentamicin MICs for Pseudomonas aeruginosa. Methodology:
- Media: Prepare two sets of BMD panels: Standard CAMHB and CAMHB buffered with 25mM TES.
- Strains: 30 clinical isolates of P. aeruginosa.
- Inoculum: Standardized per CLSI M07.
- Incubation Conditions: Duplicate panels are incubated in:
- Condition A: Ambient Air, 35°C.
- Condition B: 5% CO₂, 35°C. Both for 16-20h.
- Measurement & Analysis:
- Read MICs visually.
- Measure final pH of one control well per panel using a micro-pH electrode.
- Determine essential agreement (EA) and categorical agreement (CA) between conditions. A >2-fold MIC increase in CO₂ is significant.
Visualization of Experimental Workflows
Diagram 1: Comparative Incubation Condition Study Workflow
Diagram 2: CLSI M07 Incubation Timing Decision Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials for Incubation Condition Research
| Item | Function in Research | Technical Notes |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standard medium for BMD of non-fastidious aerobes. Provides consistent cation levels (Ca²⁺, Mg²⁺) critical for aminoglycoside/polymyxin testing. | Must be validated for CO₂ incubation if used; often supplemented with TES buffer. |
| TES Buffer (N-Tris[Hydroxymethyl]methyl-2-aminoethanesulfonic acid) | Biological buffer added to CAMHB (20-25mM) to stabilize pH during incubation in CO₂ atmospheres. | Prevents false-high MICs for pH-sensitive drugs. Essential for reliable CO₂ studies. |
| HTM Broth (Haemophilus Test Medium) | Enriched medium for H. influenzae susceptibility testing. Contains NAD, hematin, and yeast extract. | Validated for incubation in 5% CO₂ per CLSI. |
| GC Broth Base with Supplement | For N. gonorrhoeae BMD. Requires IsoVitaleX or similar growth supplement. | CO₂ incubation is mandatory. |
| Precision Data-Logging Thermometer/Hygrometer | To continuously monitor and validate incubator temperature and humidity uniformity. | Independent probe(s) placed in liquid-filled flask simulate microplate conditions. |
| Microtiter Plate Reader (Spectrophotometric/Fluorometric) | For objective, high-throughput MIC reading and early-timepoint kinetic studies. | Allows research into rapid phenotypic resistance detection (e.g., carbapenemase activity). |
| pH Micro-Electrode | To measure final pH in control wells after incubation, quantifying CO₂-induced media acidification. | Confirms buffer capacity and identifies pH-related MIC outliers. |
Within the framework of CLSI M07 standard method research for broth microdilution, the determination of the Minimum Inhibitory Concentration (MIC) remains the definitive quantitative measure of antimicrobial susceptibility. The endpoint, the lowest concentration that inhibits visible growth, can be interpreted through two primary modalities: traditional visual reading and automated instrument reading. This technical guide examines the methodologies, validation criteria, and comparative performance of these two approaches, providing a detailed protocol for researchers and drug development professionals.
Core Methodologies and Protocols
Visual Reading Protocol (CLSI M07 Reference Method)
Principle: Trained technologists observe microdilution wells under controlled lighting against a non-reflective background.
- Panel Preparation: Prepare cation-adjusted Mueller-Hinton broth (CAMHB) according to CLSI M07. Dispense serial two-fold dilutions of antimicrobial agent into a 96-well microtiter plate.
- Inoculum Standardization: Adjust microbial suspension to a 0.5 McFarland standard (~1-5 x 10^8 CFU/mL). Further dilute in broth to achieve a final inoculum of ~5 x 10^5 CFU/mL in each well.
- Incubation: Incubate plates at 35°C ± 2°C in ambient air for 16-20 hours (standard bacteria; some fastidious organisms require extended time or specific conditions).
- Visual Endpoint Determination: Examine each well. The MIC is the lowest concentration where there is no visible growth, indicated by a clear well or a barely visible button of cells. Use an inverted reading mirror for enhanced visualization. Growth control must show turbidity, and sterility control must remain clear.
Automated Reading Protocol
Principle: Instruments determine optical density (OD) or turbidimetric measurements to calculate growth inhibition.
- Panel Preparation & Inoculation: Identical to visual method (Steps 1-3 above). Commercially prepared panels are often used.
- Instrument Calibration: Calibrate the automated reader (e.g., Sensititre Vizion, MicroScan, Vitek 2) using manufacturer-defined standards and control organisms.
- Automated Scanning: The reader scans each well at a specified wavelength (e.g., 405-660 nm depending on system). It measures OD for each well.
- Algorithmic Endpoint Determination: Proprietary software compares the OD of test wells to growth control wells. A threshold (e.g., ≥90% inhibition) is applied to determine the MIC. The software flags results requiring visual verification (e.g., skipped wells, trailing endpoints).
Comparative Performance Data
Table 1: Essential Criteria for MIC Endpoint Determination
| Criterion | Visual Reading | Automated Reading |
|---|---|---|
| Primary Detection Signal | Human eye perception of turbidity | Photometric absorbance/turbidity |
| Endpoint Threshold | No visible growth (subjective, trained eye) | Pre-defined % inhibition (e.g., ≥90%) |
| Read Time per Plate | 1-2 minutes | < 30 seconds |
| Susceptibility to Trailing | Manual assessment of slight growth across dilutions | Algorithmic interpretation, may require overrides |
| Essential Quality Control | Technologist competency testing, control strains | Daily instrument calibration, control strains |
Table 2: Agreement Rates Between Visual and Automated Methods (Representative Data)
| Organism Group (n studies) | Essential Agreement (% within ±1 dilution) | Categorical Agreement (%) | Major Error Rate (%) |
|---|---|---|---|
| Enterobacterales (3) | 95.2 - 98.7 | 97.1 - 99.0 | 0.1 - 0.5 |
| Non-fermenters (2) | 92.5 - 96.0 | 94.8 - 97.2 | 0.3 - 1.2 |
| Gram-positive Cocci (3) | 94.8 - 98.1 | 96.5 - 98.8 | 0.2 - 0.8 |
| Fastidious Organisms (2) | 90.1 - 94.3 | 92.0 - 95.5 | 0.5 - 1.5 |
Essential Agreement: MICs agree within ±1 two-fold dilution. Categorical Agreement: Interpretive category (S/I/R) matches. Major Error: False-resistant result.
Signaling and Decision Pathways
Diagram Title: MIC Endpoint Determination Workflow: Visual vs. Automated Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Broth Microdilution MIC Studies
| Item | Function & Specification |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standard medium for non-fastidious aerobes; divalent cation adjustment ensures consistency in tetracycline/aminoglycoside activity. |
| Sterile 96-Well Microtiter Plates | U-bottom or flat-bottom plates for holding broth dilutions and inoculum. Must be non-cytotoxic and compatible with reader. |
| Antimicrobial Agent Stock Solutions | High-purity reference powders dissolved in appropriate solvent (water, DMSO, ethanol) per CLSI M100. |
| Turbidity Standard (0.5 McFarland) | Pre-made latex suspension or densitometer to standardize inoculum density to ~1.5 x 10^8 CFU/mL. |
| Multichannel & Automated Pipettes | For accurate, high-throughput transfer of broth, antimicrobials, and inoculum. |
| Automated MIC Reader (e.g., Sensititre Vizion) | Photometric instrument for measuring well turbidity; includes software for MIC calculation. |
| Quality Control Strains | CLSI-recommended strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) for daily validation of test conditions. |
| Inverted Reading Mirror & Light Box | Essential for visual reading; provides uniform, glare-free background to assess well turbidity. |
Validation and Quality Assurance Protocol
To validate an automated system against the reference visual method per CLSI guidelines:
- Strain Selection: Test a panel of 100-300 recent clinical isolates, encompassing target species and resistance phenotypes.
- Parallel Testing: Inoculate identical panels from the same preparation. Incubate and read one set visually (by two independent readers, blinded) and one set by the automated system.
- Data Analysis: Calculate essential agreement (EA) and categorical agreement (CA). Investigate all discrepancies (major/very major errors) by repeat testing using both methods and reference broth macrodilution if needed.
- Acceptance Criteria: For FDA/CLSI validation, EA should be ≥90% for non-fastidious organisms, with CA ≥90% and major error rates <3%.
This whitepaper provides an in-depth technical guide for determining the Minimum Inhibitory Concentration (MIC) of novel antimicrobial compounds, a cornerstone of in vitro efficacy assessment in drug development. The content is explicitly framed within the ongoing research and validation context of the Clinical and Laboratory Standards Institute (CLSI) standard M07, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically." Mastery of this standardized broth microdilution method is critical for generating reproducible, reliable, and clinically predictive data that can bridge the gap between early discovery and clinical trials.
The MIC is defined as the lowest concentration of an antimicrobial agent that completely inhibits visible growth of a microorganism under defined in vitro conditions. For novel compounds, establishing a baseline of activity against reference strains is the first critical step. The following table summarizes typical MIC data for control agents against CLSI-recommended quality control strains, which must be included in every run to validate the procedure.
Table 1: CLSI QC Ranges for Reference Antimicrobials (Broth Microdilution, CAMHB)
| QC Strain (ATCC #) | Antimicrobial | QC MIC Range (µg/mL) | Purpose in Novel Compound Testing |
|---|---|---|---|
| Staphylococcus aureus 29213 | Oxacillin | 0.12 - 0.5 | Control for β-lactamase stability |
| Escherichia coli 25922 | Ciprofloxacin | 0.004 - 0.016 | Control for fluoroquinolone/DNA gyrase targeting |
| Pseudomonas aeruginosa 27853 | Tobramycin | 0.5 - 2 | Control for aminoglycoside/efflux pump activity |
| Enterococcus faecalis 29212 | Vancomycin | 1 - 4 | Control for cell wall synthesis inhibition |
Table 2: Example MIC Data Interpretation for a Novel Compound
| Result Pattern | MIC (µg/mL) vs. QC Strain | Interpretation & Action |
|---|---|---|
| Within QC Range | Ciprofloxacin vs. E. coli 25922 = 0.008 | Run Valid. Novel compound data is reliable. |
| Out of QC Range | Ciprofloxacin vs. E. coli 25922 = 0.5 | Run Invalid. Investigate media, inoculation, compound stability. |
| Novel Compound Result | Novelexocin vs. S. aureus 29213 = 2.0 | Potency Benchmark. Compare to standard-of-care agents. |
Detailed Experimental Protocol: CLSI M07 Broth Microdilution
Protocol Title: Determination of MIC for a Novel Compound Against Aerobic Bacteria
1. Preparation of Antimicrobial Stock Solution:
- Weigh the novel compound precisely using an analytical balance.
- Dissolve in the appropriate solvent (e.g., DMSO, water, 0.1N NaOH/HCl) as per stability data to create a primary stock solution (e.g., 5120 µg/mL). Filter-sterilize (0.22 µm pore size).
- Prepare a working stock in sterile water or CAMHB at 10x the highest final test concentration.
2. Preparation of Microdilution Trays:
- Using a multichannel pipette, dispense 50 µL of cation-adjusted Mueller-Hinton broth (CAMHB) into each well of a sterile 96-well plastic tray (rows A-G, columns 1-12).
- Add 100 µL of the novel compound working stock to the first well of the designated row (e.g., column 1).
- Perform two-fold serial dilutions: Transfer 50 µL from column 1 to column 2, mix thoroughly, and continue through column 11. Discard 50 µL from column 11. Column 12 serves as the growth control (broth + inoculum, no drug).
3. Preparation of Inoculum:
- Streak the test organism from a frozen stock onto a non-selective agar plate. Incubate to obtain isolated colonies.
- Select 3-5 colonies to suspend in saline or broth. Adjust the turbidity to a 0.5 McFarland standard (~1-2 x 10^8 CFU/mL).
- Dilute the suspension in CAMHB to achieve a final concentration of ~5 x 10^5 CFU/mL (typically a 1:150 dilution).
4. Inoculation and Incubation:
- Add 50 µL of the adjusted inoculum to each well in the test rows (columns 1-12). This brings the total volume to 100 µL and achieves the final target inoculum of ~5 x 10^5 CFU/mL, with drug concentrations now at their intended 1x level.
- Seal the tray with a sterile lid or adhesive film. Incubate aerobically at 35±2°C for 16-20 hours.
5. Reading and Interpretation:
- After incubation, examine the wells visually or with a reading mirror. The MIC is the lowest concentration of the novel compound that completely inhibits visible growth.
- Compare the growth in the growth control (well 12) and sterility control (broth only) to ensure valid conditions. QC results for standard antibiotics must be within published ranges.
Title: Broth Microdilution MIC Protocol Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for CLSI-Compliant MIC Testing
| Item | Function & Critical Specification |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium with controlled divalent cation (Ca2+, Mg2+) levels, ensuring consistent activity of cationic antimicrobials. |
| Sterile 96-Well U-Bottom Microdilution Trays | Non-binding, inert plastic trays for holding test volumes; U-bottom facilitates reading of bacterial pellets. |
| Automated Liquid Handler / Multichannel Pipette | Essential for accurate, high-throughput dispensing and serial dilution to minimize human error. |
| Densitometer (McFarland Standard) | Provides precise optical standardization of bacterial inoculum density for reproducible inoculum size. |
| Quality Control Strains (e.g., ATCC) | Frozen or lyophilized stocks of reference organisms with well-characterized MICs to validate each test run. |
| Sterile Dimethyl Sulfoxide (DMSO) | Primary solvent for water-insoluble novel compounds; must be at lowest possible final concentration (typically ≤1% v/v) to avoid toxicity. |
Advanced Considerations: Signaling Pathways & Resistance Mechanisms
Understanding the mechanism of action (MOA) of a novel compound contextualizes its MIC. For a new compound targeting bacterial cell wall synthesis (e.g., inhibiting penicillin-binding proteins, PBPs), the pathway and potential resistance mechanisms can be visualized as follows:
Title: Beta-lactam MOA and Resistance Impact on MIC
Integrating robust, CLSI M07-compliant MIC determination early in the drug development pipeline provides an indispensable, standardized metric for lead compound selection, structure-activity relationship (SAR) analysis, and pre-clinical efficacy profiling.
Common Challenges and Solutions: Optimizing Your M07 Assay for Reliable Results
The Clinical and Laboratory Standards Institute (CLSI) document M07, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," is the foundational standard for broth microdilution (BMD) testing. Reliable, reproducible bacterial growth is paramount for generating accurate Minimum Inhibitory Concentration (MIC) data, a critical endpoint in both clinical diagnostics and drug discovery research. This guide provides an in-depth, technical troubleshooting framework for resolving poor growth in BMD assays, a common yet critical failure point that can invalidate results and compromise research integrity.
I. Media-Related Issues: Composition and Preparation
Proper media is the non-negotiable foundation for successful BMD. Deviations from CLSI M07 specifications directly impact growth kinetics and antibiotic activity.
Key Media Parameters to Troubleshoot:
| Parameter | CLSI M07 Specification | Impact of Deviation | Corrective Action |
|---|---|---|---|
| Cation Concentrations (Ca²⁺, Mg²⁺) | CAMHB (Ca: 20-25 mg/L; Mg: 10-12.5 mg/L) | Alters aminoglycoside & polymyxin activity; can inhibit growth. | Use commercial, validated CAMHB lots. Verify with atomic absorption if needed. |
| pH | 7.2 ± 0.1 at room temperature | Affects antibiotic stability & uptake; suboptimal for bacterial enzymes. | Calibrate pH meter daily. Adjust after all additions (e.g., blood, supplements). |
| Thymidine/Thymine Content | Minimal (in "HTM" or "supplemented" media) | High levels can antagonize trimethoprim/sulfonamides; may spuriously elevate MICs. | Use thymidine-free media or add thymidine phosphorylase for specific agents. |
| Supplementation (e.g., lysed horse blood) | 2-5% for fastidious organisms (S. pneumoniae, H. influenzae) | Insufficient leads to poor growth; excessive can alter antibiotic binding. | Use fresh, sterile supplements. Adhere strictly to organism-specific guidelines. |
| Storage & Shelf Life | 2-8°C, protected from light; use within expiry. | Degradation produces toxic byproducts; CO2 absorption lowers pH. | Prepare smaller batches. Record opening dates. Never use discolored media. |
Experimental Protocol: Media Quality Control Check
- Prepare Control Plates: Use a batch of previously validated CAMHB as a positive control. Prepare test plates from the new media batch.
- Select QC Strains: Inoculate E. coli ATCC 25922, S. aureus ATCC 29213, and P. aeruginosa ATCC 27853 according to CLSI M07.
- Incubate & Compare: Perform BMD with a panel of relevant antibiotics. Incubate at 35±1°C for 16-20 hours.
- Analyze: MICs for all QC strains in the test media must be within one doubling dilution of the control media MICs. Growth in the positive control wells (no antibiotic) must be equivalent (turbidity match).
II. Inoculum Preparation and Standardization
Inoculum density is the single most critical variable in BMD. CLSI M07 specifies a target of 5 x 10⁵ CFU/mL in each well, achieved by diluting a standardized suspension.
Quantitative Analysis of Inoculum Effects:
| Inoculum Preparation Step | Target / Method | Typical Error Range | Consequence of Error |
|---|---|---|---|
| Colony Selection | 3-5 isolated colonies from an 18-24 hr non-selective plate. | +/- 0.5 log CFU if colonies are too old or from selective media. | Inconsistent growth rate; heteroresistance may be missed. |
| Direct Colony Suspension | Adjust to 0.5 McFarland standard in saline or broth. | 0.5 McFarland = 1-2 x 10⁸ CFU/mL. Variability can be +/- 50%. | Primary source of final inoculum error. |
| Spectrophotometric Verification | OD₆₂₅ of 0.08-0.13 for E. coli correlates to ~1x10⁸ CFU/mL. | Strain-dependent; mucoid or chain-forming organisms are inaccurate. | Over-inoculation: Falsely low MICs (esp. β-lactams). Under-inoculation: Falsely high MICs or no growth. |
| Final Dilution | 1:150 dilution of 0.5 McFarland into cation-adjusted Mueller Hinton Broth (CAMHB). | Pipetting error ±5-10%. | Directly propagates to final well density. |
| Viability Verification (CFU plating) | Plate 10 µL of 1:1000 final dilution. Target: 50-100 colonies. | Gold standard for accuracy. | Confirms true inoculum size; essential for troubleshooting. |
Experimental Protocol: Viable Count Verification
- After preparing the working inoculum per M07, perform a serial 1:10 dilution in sterile saline to a theoretical 10⁻⁵.
- Plate 10 µL spots of the 10⁻⁴ and 10⁻⁵ dilutions onto non-selective agar (e.g., TSA). Perform in duplicate.
- Incubate plates overnight at 35°C.
- Count colonies: (Colony count) x (Dilution Factor) x 100 = CFU/mL in the working inoculum.
- Acceptance Criterion: Result must be 2-8 x 10⁵ CFU/mL. If outside range, adjust the initial McFarland standardization process.
III. Incubation and Environmental Conditions
Incubation parameters directly influence growth rate, which must be optimized for the method, not necessarily for maximal yield.
Critical Incubation Parameters Table:
| Parameter | CLSI M07 Standard | Impact of Deviation | Monitoring & Control |
|---|---|---|---|
| Temperature | 35±1.0°C for non-fastidious bacteria. | Higher: Can accelerate growth but alter antibiotic stability. Lower: Slows growth, can falsely elevate MICs. | Use calibrated, independent thermometer with continuous logging. |
| Atmosphere | Ambient air for most; CO₂ for fastidious organisms (e.g., S. pneumoniae). | CO₂ for non-fastidious: Acidifies media, affects pH-sensitive drugs (e.g., macrolides). | Use airtight incubators with calibrated CO₂ sensors for required tests. |
| Duration | 16-20 hours for most; 20-24 hours for oxacillin vs. Staph or Enterococcus. | Short: Inadequate growth in slow wells. Long: Can mask trailing endpoints or cause overgrowth. | Read plates at strict, standardized times. Use a time-stamped reader. |
| Humidity | High humidity to prevent evaporation in microtiter wells. | Evaporation concentrates antibiotics, falsely elevating MICs. | Place plates in a humidified chamber or use sealed containers with wet towels. |
Experimental Protocol: Incubator Mapping and Validation
- Place calibrated temperature probes in multiple locations within the incubator (shelves, corners, center, near door).
- Log temperatures every 15 minutes over a 24-48 hour period under normal operating conditions (with plates/baffles inside).
- Analyze data for spatial and temporal variability. All locations must maintain 35±1.0°C.
- Repeat quarterly and after any servicing. For CO₂ incubators, also validate CO₂ concentration with a secondary analyzer.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Cation-Adjusted Mueller Hinton II Broth (CAMHB) | Standardized growth medium with controlled Ca²⁺ and Mg²⁺ levels to ensure reproducible antibiotic activity, especially for cationic agents like aminoglycosides. |
| Adjustable Volume Electronic Pipettes (8-channel) | For accurate, high-throughput dispensing of inoculum into 96-well microtiter plates. Reduces repetitive strain and volumetric error. |
| Digital McFarland Densitometer | Provides objective, reproducible measurement of initial bacterial suspension density, reducing the visual error associated with manual comparators. |
| Pre-defined, Dried Microtiter Panels | Commercial panels offer consistency in antibiotic concentration gradients and are essential for standardized, high-throughput screening in drug development. |
| Automated Plate Reader (Spectrophotometer) | For objective determination of well turbidity (OD600-630). Enplicates reading, detects subtle growth (trailing), and facilitates data export. |
| Quality Control Strains (ATCC) | Standard reference organisms (E. coli 25922, S. aureus 29213, etc.) used daily to validate the entire test system—media, inoculum, incubation, and antibiotics. |
| Sterile, Indelible Plate Sealers | Prevents cross-contamination and evaporation during incubation, critical for maintaining well volume and drug concentration. |
| Precision Incubator with Data Logging | Maintains constant 35°C temperature and, if needed, 5% CO₂. Data logging provides an audit trail for troubleshooting aberrant results. |
Visualizing the Troubleshooting Workflow
Title: Systematic Troubleshooting Workflow for BMD Growth Issues
Achieving consistent, optimal bacterial growth in broth microdilution is a foundational technical skill underpinning reliable MIC data. Within the framework of CLSI M07 research, systematic troubleshooting must sequentially interrogate media composition, inoculum density, and incubation conditions. By adhering to standardized QC protocols, employing precise measurement tools, and maintaining rigorous environmental controls, researchers can isolate and resolve growth anomalies, ensuring the integrity of susceptibility data critical for antimicrobial drug development and resistance surveillance.
Addressing Trailing Endpoints and Indistinct MIC Values
The Clinical and Laboratory Standards Institute (CLSI) M07 standard, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," is the definitive guide for broth microdilution (BMD) testing. A persistent analytical challenge within this methodology is the accurate interpretation of wells exhibiting "trailing endpoints" and "indistinct" minimum inhibitory concentration (MIC) values. Trailing endpoints are characterized by a gradual, often incomplete reduction in bacterial growth across a series of increasing antimicrobial concentrations, while indistinct MICs arise when there is no clear demarcation between growth and inhibition. Within the broader thesis of refining M07 for novel antimicrobial agents and resistant phenotypes, addressing these ambiguities is critical for ensuring reproducible, accurate, and clinically meaningful susceptibility data. This guide delves into the technical origins, standardized interpretive approaches, and advanced protocols for managing these phenomena.
Etiology and Impact on MIC Determination
Trailing and indistinct endpoints are not random errors but phenomena with specific biological and technical causes.
| Phenomenon | Primary Causes | Typical Drug Classes | Impact on MIC Readability |
|---|---|---|---|
| Trailing Endpoint | - Phenotypic tolerance / persister cell formation.- Partial inhibition of a target without cell death.- Drug degradation during incubation.- Inoculum density effects. | Azoles (e.g., Fluconazole), Cationic peptides, Some bacteriostatic agents. | Creates a gradient of turbidity, making the "80-90% inhibition" rule (CLSI M07) subjective. |
| Indistinct MIC | - Heteroresistance within the population.- Narrow margin between MIC and minimum bactericidal concentration (MBC).- Poor solubility or binding of drug in medium.- Automated reader calibration issues. | Glycopeptides (e.g., Vancomycin), Lipopeptides, Some β-lactams. | No single well shows a sharp drop in growth; multiple wells appear partially inhibited. |
Standardized Methodological Approaches (CLSI M07-Ed12)
The current CLSI M07 standard provides essential guidance for managing these challenges.
Key Experimental Protocol: The "Significant Reduction" Method for Trailing
This protocol is applied when a clear, sharp endpoint is absent.
- Preparation: Perform standard BMD per CLSI M07 (inoculum ~5 x 10⁵ CFU/mL, cation-adjusted Mueller-Hinton broth [CAMHB], 35°C ± 2°C, 16-20 hours incubation).
- Visual Reading: Examine the microdilution tray against a non-reflective, black-white background with indirect lighting.
- Identification: Identify the well with a significant, abrupt reduction in growth compared to the growth control. This is often more pronounced than an 80% reduction.
- Comparison: Compare the turbidity in this well to subsequent higher concentration wells. If turbidity does not decrease further (or decreases only minimally), the well with the initial abrupt reduction is designated the MIC.
- Recording: If no significant reduction is observed, the MIC is reported as ">" (greater than) the highest concentration tested.
Key Experimental Protocol: The "Complete Inhibition" Overread for Indistinct Endpoints
For cases with generalized faint growth across multiple wells.
- Incubation Extension: After initial 20-hour incubation, re-incubate the tray for an additional 4 hours (total 24h).
- Re-examination: Read the tray again. The additional incubation often allows faint growth in wells with sub-inhibitory concentrations to become more pronounced.
- Endpoint Determination: The MIC is the lowest concentration that shows complete absence of visible growth after the extended incubation. Any persistent haziness or faint button is considered growth.
- Control Validation: Ensure the growth control remains robust and the sterility control remains clear. Report the extended incubation time with the MIC result.
Advanced and Investigative Protocols
For research requiring higher precision, supplementary methods are employed.
Protocol for Viability Staining (e.g., Resazurin)
This fluorescence-based method distinguishes between metabolic activity (trailing) and true inhibition.
- Post-Incubation: Following standard BMD incubation, add 10-20 µL of a 0.01% resazurin sodium salt solution to each well.
- Re-incubation: Incubate the tray for 1-2 hours at 35°C.
- Reading: Under normal or fluorescent light, observe color change. A shift from blue (non-fluorescent) to pink/colorless (fluorescent) indicates metabolic activity. The MIC is the lowest concentration well that remains blue.
- Quantification: Fluorescence can be quantified using a plate reader (Excitation 530-570 nm, Emission 590-620 nm) to generate more objective dose-response curves.
Protocol for Time-Kill Curve Synergy
To contextualize trailing endpoints within pharmacodynamic models.
- Setup: From the BMD tray, at time T=0 and at 2, 4, 6, 8, and 24 hours, remove a 10 µL aliquot from key wells (growth control, MIC well, 2xMIC, 4xMIC).
- Serial Dilution & Plating: Perform serial 10-fold dilutions in sterile saline and spot-plate 10 µL onto non-selective agar plates.
- Enumeration: After overnight incubation, count colony-forming units (CFU/mL).
- Analysis: Plot Log₁₀ CFU/mL vs. Time for each concentration. True bactericidal activity is defined as a ≥3-log₁₀ CFU/mL reduction from the initial inoculum. Trailing often shows initial killing followed by regrowth of a tolerant subpopulation.
Visualization of Workflows and Concepts
Title: MIC Determination Workflow for Ambiguous Endpoints
Title: Biological Basis of Trailing Endpoint Formation
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standard medium for BMD; ensures consistent cation levels (Ca²⁺, Mg²⁺) critical for aminoglycoside and polymyxin activity. |
| Polysorbate 80 (Tween 80) | Surfactant used to solubilize hydrophobic compounds (e.g., some novel antimicrobials) to prevent non-specific binding to plastic trays. |
| Resazurin Sodium Salt Solution | Viability stain; used to differentiate between static (metabolically active) and cidal (inactive) effects in trailing endpoints. |
| DMSO (Grade A, Sterile) | High-quality solvent for reconstituting stock solutions of experimental compounds without antimicrobial carryover effects. |
| Densitometer (e.g., McFarland Standard) | Critical for standardizing the bacterial inoculum to 0.5 McFarland, a primary variable affecting endpoint sharpness. |
| 96-Well Microtiter Plates (Treated, Sterile) | Tissue-culture treated plates minimize cell adhesion; U-bottom wells facilitate pellet formation for easier visual reading. |
| Automated Plate Reader (with shaking & incubation) | Enables kinetic (time-based) OD600 readings, generating growth curves for each well to algorithmically determine MICs. |
| CLSI M07-Ed12 and EUCAST Standards | Essential reference documents for protocol details, QC organism ranges, and interpretive criteria updates. |
Optimizing Assay Conditions for Fastidious Organisms
1. Introduction Within the framework of CLSI standard M07 (Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically), broth microdilution (BMD) is the reference methodology for antimicrobial susceptibility testing (AST). However, its application to fastidious organisms—those with complex nutritional requirements—presents significant challenges. This guide details the optimization of BMD conditions to ensure accurate and reproducible Minimum Inhibitory Concentration (MIC) determinations for these organisms, a critical step in drug development and stewardship.
2. Key Growth Variables & Optimization Data Optimization centers on supplementing cation-adjusted Mueller Hinton Broth (CAMHB), the standard medium in M07. The table below summarizes current, evidence-based recommendations.
Table 1: Optimized Supplementation Strategies for Common Fastidious Organisms
| Organism Group | Standardized Test Medium (per CLSI M07/ M100) | Critical Supplement(s) | Optimal Incubation Conditions | Typical MIC Impact vs. Unsupplemented CAMHB |
|---|---|---|---|---|
| Streptococcus pneumoniae & other Streptococci | CAMHB + 2.5-5% lysed horse blood (LHB) | LHB (provides NAD, hemin, growth factors) | 35±2°C, Ambient air, 20-24h | For S. pneumoniae: β-lactam MICs decrease significantly (≥2 dilutions) without LHB. |
| Haemophilus influenzae & H. parainfluenzae | Haemophilus Test Medium (HTM) | 15 µg/mL NAD + 15 µg/mL bovine hematin + 5 g/mL yeast extract in CAMHB | 35±2°C, Ambient air, 20-24h | Essential for growth. Trimethoprim-sulfa MICs are most affected by thymidine content. |
| Neisseria gonorrhoeae | GC Broth Base + 1% Defined Growth Supplement | 1% Supplement (contains vitamins, amino acids, ferric nitrate, glucose) | 35±2°C, 5% CO2, 20-24h | Failure to supplement results in no growth. CO2 is mandatory. |
| Campylobacter spp. | CAMHB + 5% LHB or defibrinated horse blood | Blood (scavenges toxic oxygen radicals) | 42±2°C, Microaerophilic (5% O2, 10% CO2, 85% N2), 48h | No growth under aerobic conditions. Incubation temperature is species-specific. |
| Moraxella catarrhalis | CAMHB + 2.5-5% LHB (historically used) | LHB (older methods); unsupplemented CAMHB may suffice for many strains. | 35±2°C, Ambient air, 20-24h | Most modern studies use unsupplemented CAMHB. LHB may slightly lower β-lactam MICs. |
3. Detailed Experimental Protocol: Optimization of Haemophilus Test Medium (HTM) This protocol exemplifies the systematic approach to medium optimization for a fastidious organism.
Objective: To prepare and quality-control HTM for BMD according to CLSI guidelines. Materials: Cation-adjusted Mueller Hinton Broth (CAMHB powder), β-Nicotinamide adenine dinucleotide (NAD), Bovine hematin powder, Yeast extract, Sterile distilled water, 0.5 McFarland turbidity standard, Haemophilus influenzae ATCC 49247, H. influenzae ATCC 49766, Sterile 96-well microdilution trays. Procedure:
- Medium Preparation: a. Prepare CAMHB according to manufacturer's instructions. b. Prepare supplement stock solutions: i. NAD: 15 mg in 10 mL sterile water. Filter sterilize (0.22 µm). ii. Hematin: Dissolve 60 mg in 10 mL of 0.01N NaOH. Heat gently. Filter sterilize. iii. Yeast extract: 5 g in 100 mL water. Autoclave. c. For 1L of HTM, add 15 mL of NAD stock, 2.5 mL of hematin stock, and 100 mL of yeast extract stock to 882.5 mL of sterile CAMHB.
- Inoculum Preparation: a. Subculture control strains on chocolate agar, incubate at 35°C in 5% CO2 for 20-24h. b. Suspend colonies in sterile saline to a 0.5 McFarland standard (~1-4 x 10^8 CFU/mL). c. Dilute the suspension 1:100 in HTM to achieve a final inoculum of ~5 x 10^5 CFU/mL in the test well.
- BMD Setup & Incubation: a. Dispense 50 µL of HTM into all wells of a microdilution tray. b. Perform serial two-fold dilutions of the antimicrobial agent in the first column. c. Add 50 µL of the adjusted inoculum to all test wells. Include growth control (inoculum, no drug) and sterility control (HTM only) wells. d. Seal tray and incubate at 35±2°C in ambient air for 20-24h.
- Quality Control: a. Read MIC endpoint as the lowest concentration inhibiting visible growth. b. Validate the medium batch by ensuring MICs for ATCC 49247 (e.g., ampicillin MIC 0.5-2 µg/mL) and ATCC 49766 (β-lactamase positive) fall within CLSI-specified QC ranges.
4. Visualizing the Optimization Workflow & Microbial Stress Response
5. The Scientist's Toolkit: Essential Reagents & Materials Table 2: Key Research Reagent Solutions for Fastidious Organism BMD
| Item | Function in Assay Optimization | Key Consideration |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) Powder | Standard base medium providing consistent levels of Ca2+, Mg2+, and pH. | Essential for reproducible MICs of cationic antimicrobials (e.g., aminoglycosides, polymyxins). |
| Lysed Horse Blood (LHB) | Provides essential growth factors (NAD, hemin) and inactivates inhibitors like trimethoprim and sulfonamides. | Preferred over whole blood for clearer MIC endpoints. Must be aseptically prepared or commercially sourced. |
| β-NAD (Nicotinamide Adenine Dinucleotide) | "V Factor" required by Haemophilus and some other species as a coenzyme. | Light and heat-sensitive. Use fresh, filter-sterilized stock solutions. |
| Bovine Hematin (or Protoporphyrin IX) | "X Factor" required by Haemophilus for cytochromes and catalase synthesis. | Dissolves in weak base (e.g., 0.01N NaOH). Do not autoclave the stock solution. |
| Defined Growth Supplements (e.g., for GC) | Chemically defined mix of vitamins, amino acids, and minerals for organisms with stringent needs (e.g., N. gonorrhoeae). | Eliminates batch variability associated with biological supplements like blood. |
| Microaerophilic & CO2 Generation Systems | Creates the reduced-oxygen, CO2-enriched atmosphere required by Campylobacter, Helicobacter, etc. | Use commercial gas-generating pouches or controlled atmosphere incubators for reliability. |
| Quality Control (QC) Strain Panels | Reference strains with well-characterized MIC ranges (e.g., ATCC 49247 for H. influenzae) used to validate each assay run. | Mandatory per CLSI guidelines to ensure medium, inoculum, and incubation conditions are optimal. |
| Sterile, Non-Toxic 96-Well Microdilution Trays | The physical platform for the BMD test. | Must be composed of polypropylene or polystyrene that does not bind antimicrobials. Pre-made frozen panels are commercially available. |
Within the framework of research on the Clinical and Laboratory Standards Institute (CLSI) M07 broth microdilution standard method, the implementation of robust quality control (QC) is paramount. This technical guide details the use of American Type Culture Collection (ATCC) reference strains and their associated acceptable ranges to ensure the precision, accuracy, and reproducibility of antimicrobial susceptibility testing (AST) data—a cornerstone of valid research and drug development.
The Role of ATCC Reference Strains in CLSI M07
ATCC reference strains are fully characterized, genotypically stable microorganisms with defined susceptibility profiles. In the context of CLSI M07, they serve as the primary QC tool to verify that every component of the broth microdilution test system—including media, inoculum density, incubation conditions, and antimicrobial agent potency—is functioning within specified parameters.
Essential QC Strains and Current Acceptable Ranges (CLSI M100)
The following table summarizes key ATCC reference strains and their current acceptable MIC ranges (in µg/mL) for select antimicrobial agents, as per the latest CLSI M100 performance standards document. Ranges are typically defined to encompass 95-99% of results from replicate testing.
Table 1: Key ATCC QC Strains and Acceptable MIC Ranges for Broth Microdilution (CLSI M07)
| ATCC Strain | Organism | Antimicrobial Agent | Acceptable MIC Range (µg/mL) |
|---|---|---|---|
| ATCC 25923 | Staphylococcus aureus | Oxacillin | 0.12 - 0.5 |
| ATCC 25923 | Staphylococcus aureus | Vancomycin | 1 - 4 |
| ATCC 35218 | Escherichia coli (β-lactamase +) | Amoxicillin-Clavulanate | 4/2 - 16/8 |
| ATCC 29212 | Enterococcus faecalis | Ampicillin | 0.5 - 2 |
| ATCC 29212 | Enterococcus faecalis | Gentamicin (HLR) | 4 - 16 |
| ATCC 27853 | Pseudomonas aeruginosa | Ceftazidime | 1 - 4 |
| ATCC 27853 | Pseudomonas aeruginosa | Ciprofloxacin | 0.25 - 1 |
| ATCC BAA-1705 | Klebsiella pneumoniae (KPC +) | Meropenem | 4 - 16 |
| ATCC BAA-1706 | Klebsiella pneumoniae (KPC +) | Meropenem | 0.25 - 1 |
Detailed Experimental Protocol: Performing QC with ATCC Strains
Materials Preparation (The Scientist's Toolkit)
Table 2: Research Reagent Solutions for CLSI M07 QC Testing
| Item | Function/Brief Explanation |
|---|---|
| ATCC QC Strains (Lyophilized) | Genetically defined reference organisms. Stored at ≤ -20°C or as specified. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for non-fastidious organisms. Provides consistent cation concentrations (Ca²⁺, Mg²⁺) critical for aminoglycoside and tetracycline activity. |
| Sterile 0.85% Saline or Tryptic Soy Broth | Used for bacterial suspension preparation and dilution to achieve the target inoculum density. |
| McFarland 0.5 Standard | Turbidity reference to standardize inoculum to ~1.5 x 10⁸ CFU/mL. |
| Broth Microdilution Trays | Pre-dried, 96-well plastic trays containing serial dilutions of antimicrobial agents. Store at ≤ -20°C. |
| Adjustable Volume Micropipettes (1-10µL, 10-100µL, 100-1000µL) | For precise transfer of inoculum and broth. Must be calibrated regularly. |
| Sterile Disposable Tips with Filters | Prevents aerosol contamination and carryover. |
| Multichannel Pipette (30-300µL) | For efficient inoculation of microdilution trays. |
| Incubator (35 ± 2°C, ambient air) | Provides standardized atmospheric and temperature conditions for growth. |
Step-by-Step Protocol
Strain Reconstitution & Storage: Rehydrate the lyophilized ATCC strain as per the Certificate of Analysis. Subculture onto non-selective agar (e.g., Blood Agar) to obtain isolated colonies. Maintain short-term stock on appropriate agar slants at 2-8°C for up to 2 weeks. Prepare long-term stocks in 10-20% glycerol broth and store at ≤ -60°C.
Inoculum Preparation: From a fresh (18-24 hour) agar plate, select 3-5 isolated colonies of the QC strain. Suspend colonies in sterile saline or broth. Vortex thoroughly. Adjust the suspension turbidity to match a 0.5 McFarland standard, which yields approximately 1-2 x 10⁸ CFU/mL.
Inoculum Dilution: Within 15 minutes of standardization, dilute the adjusted suspension 1:150 in sterile CAMHB. This results in a final inoculum of approximately 1 x 10⁶ CFU/mL in the test well.
Tray Inoculation: Using a multichannel pipette, transfer 100 µL of the 1:150 dilution into each well of the predried microdilution tray. This step simultaneously rehydrates and dilutes the antimicrobial agent to its final test concentration. Include a growth control well (broth + inoculum) and a sterility control well (broth only).
Incubation: Place inoculated trays in a non-CO₂ incubator at 35 ± 2°C for 16-20 hours (S. aureus ATCC 29213 requires a full 24 hours).
Reading & Interpretation: Examine trays over a white, non-reflective surface. The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth. Compare the MIC of the QC strain against the published acceptable range in the current CLSI M100 table.
QC Result Acceptance: If the observed MIC falls within the published acceptable range, the test system is considered in control. If the result is out of range, the test is invalid, and a systematic investigation of materials, methodology, and equipment must be initiated.
Workflow and Decision Logic
Diagram Title: QC Workflow for Broth Microdilution Using ATCC Strains
Troubleshooting Out-of-Range QC Results
Persistent QC failures require investigation. The following decision pathway guides the troubleshooting process.
Diagram Title: Troubleshooting Pathway for Failed QC Results
Integrating rigorous QC practices with defined ATCC reference strains and their CLSI-established acceptable ranges is non-negotiable for research adhering to the M07 standard. This systematic approach validates the entire test system, ensuring that subsequent MIC data generated for novel compounds or clinical isolates is reliable, reproducible, and suitable for informing critical decisions in the drug development pipeline. Consistent application of this protocol forms the bedrock of scientifically defensible AST research.
Automation and High-Throughput Optimization for Screening Programs
The Clinical and Laboratory Standards Institute (CLSI) M07 standard, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically," is the definitive guide for broth microdilution (BMD). Manual BMD, as described in M07, is labor-intensive, low-throughput, and prone to human error, creating a bottleneck in antimicrobial discovery and resistance surveillance. This whitepaper frames automation and high-throughput optimization as a critical evolution of the M07 standard, enabling its core principles—standardized inoculum preparation (~5 x 10⁵ CFU/mL), controlled growth conditions, and precise endpoint determination—to be executed at scale, accelerating screening programs in drug development.
Quantitative Data: Manual vs. Automated BMD
Table 1: Performance Comparison of BMD Methodologies
| Metric | Manual CLSI M07 BMD | Automated & HTP-Optimized BMD |
|---|---|---|
| Throughput (Plates/Technician/Day) | 10 - 20 | 200 - 500 |
| Inoculum Preparation Time | 45 - 60 minutes | 5 - 10 minutes |
| Plate Setup Time (96-well) | 20 - 30 minutes | 2 - 5 minutes |
| Volume Dispensing Accuracy (CV%) | 5% - 15% | < 2% |
| Data Recording & Transfer | Manual, error-prone | Automated, digital traceability |
| Estimated Error Rate | 3% - 5% | < 0.5% |
| Minimum Inhibitory Concentration (MIC) Determination | Visual, subjective | Spectrophotometric/Kinetic, objective |
Table 2: Impact of Automation on Screening Program Output
| Screening Phase | Traditional Timeline (Weeks) | HTP-Optimized Timeline (Weeks) | Fold Increase |
|---|---|---|---|
| Primary Screen (10,000 compounds) | 8 - 12 | 1 - 2 | ~8x |
| MIC Confirmation (500 hits) | 4 - 6 | 0.5 - 1 | ~8x |
| Mechanism of Action Studies | Manual, sequential | Parallelized assays | 5x - 10x |
Core Experimental Protocols
Protocol 1: Automated Broth Microdilution Plate Preparation
- Objective: To replicate CLSI M07 guidelines using automated liquid handlers for superior reproducibility.
- Materials: See Scientist's Toolkit.
- Method:
- Compound Dilution Series: Using a 384-channel liquid handler, perform twofold serial dilutions of antimicrobial agents in cation-adjusted Mueller Hinton Broth (CAMHB) across a 384-well polypropylene master plate. Transfer 2 µL from each well of the master plate to the corresponding well of a 384-well assay plate.
- Inoculum Standardization: Adjust a mid-log phase bacterial suspension to a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL) using a spectrophotometer. Use an automated dispenser to dilute this suspension in CAMHB to achieve the target inoculum of 5 x 10⁵ CFU/mL in a reservoir.
- Plate Inoculation: Dispense 98 µL of the standardized inoculum into each well of the assay plate containing pre-dried compound, resulting in a final test volume of 100 µL and final compound concentrations per CLSI M07.
- Controls: Include growth control (no antibiotic) and sterility control (no inoculum) wells, automated by the same method.
- Sealing & Incubation: Automatically apply a breathable sealing film. Incubate statically at 35°C ± 2°C for 16-20 hours.
Protocol 2: High-Throughput, Kinetic MIC Determination
- Objective: To replace subjective visual MIC reads with objective, growth-kinetic data.
- Materials: Automated plate reader/imager, integrated data analysis software.
- Method:
- Kinetic Reading: Place assay plates in a robotic-equipped plate reader. Measure optical density (OD₆₀₀) or fluorescence (if using resazurin) every 15-30 minutes over the 16-20 hour incubation period.
- Growth Curve Analysis: For each well, software generates a bacterial growth curve. The MIC is determined as the lowest concentration where the area under the growth curve (AUC) or the maximum growth rate (µ_max) is statistically indistinguishable from the sterility control (typically ≥90% inhibition).
- Data Integration: MIC values, growth parameters, and quality control metrics are automatically compiled into a database, linked to compound identifiers.
Visualizations
Title: HTP Automated Screening Workflow
Title: Drug-Target-Phenotype Link in BMD
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HTP BMD Screening
| Item | Function in HTP BMD | Key Consideration |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium as per CLSI M07. Ensures consistent cation concentrations (Ca²⁺, Mg²⁺) critical for aminoglycoside & tetracycline activity. | Must be sourced as a ready-to-use, quality-controlled liquid for automation. |
| Pre-sterilized, Assay-Ready Microplates (384/1536-well) | Polypropylene or polystyrene plates with low binding surfaces. Enable direct compound drying and automated inoculation. | Plate geometry must be compatible with liquid handler heads and readers. |
| Liquid Handling Systems (e.g., Beckman Coulter Biomek, Hamilton STAR) | Automate serial dilutions, plate replication, and high-accuracy inoculum dispensing. | Integrated with scheduling software for walk-away operation. |
| Automated Plate Readers/Imagers (e.g., BMG LabTech CLARIOstar, Molecular Devices SpectraMax) | Provide kinetic OD or fluorescence reads for objective, high-resolution growth curves. | Must have temperature-controlled incubation and stacker integration. |
| Resazurin (AlamarBlue) Cell Viability Reagent | Fluorescent/colorimetric redox indicator. Adds a secondary, more sensitive endpoint to OD measurements. | Added after initial incubation or kinetically for time-to-kill analyses. |
| Laboratory Information Management System (LIMS) | Tracks samples, compounds, protocols, and results. Creates an auditable data trail from strain to MIC value. | Must be configurable to encode CLSI M07 quality control rules. |
| Automated Colony Picker & Inoculation System | Selects and transfers individual colonies from agar plates to liquid culture, initiating the inoculum prep workflow. | Essential for fully automated, hands-off initiation of screening runs. |
Validating M07 Results and Comparing Methods: Agar Dilution, Disk Diffusion, and EUCAST
Establishing a Validation Framework for In-House M07 Procedures
Within the broader thesis on CLSI M07 broth microdilution standard method research, this whitepaper presents a comprehensive technical guide for establishing a robust validation framework for in-house M07 antimicrobial susceptibility testing (AST) procedures. This framework ensures the reliability, reproducibility, and accuracy of results, which are critical for drug development and resistance surveillance.
The CLSI M07 standard is the definitive reference method for broth microdilution susceptibility testing of bacteria. For drug development, especially for novel antimicrobial agents, laboratories must adapt and validate in-house versions of the M07 method. Validation confirms that the modified procedure performs equivalently to the reference standard, ensuring data integrity for regulatory submissions and research conclusions.
Core Validation Parameters & Performance Standards
Validation of an in-house M07 procedure requires evaluation against predefined acceptance criteria, benchmarked against the CLSI M07 reference method and published quality control (QC) ranges.
Table 1: Essential Validation Parameters & Acceptance Criteria
| Validation Parameter | Definition | Recommended Acceptance Criterion (for in-house M07) |
|---|---|---|
| Accuracy | Proximity of test results to the reference (true) value. | For QC strains, ≥95% of results within CLSI-established QC ranges. |
| Precision (Repeatability) | Agreement among independent test results under identical conditions (within-lab, same day, same analyst). | Standard Deviation (SD) of replicate MICs for a strain ≤1 two-fold dilution step. |
| Intermediate Precision | Agreement under varied conditions (different days, analysts, equipment). | ≥90% of results within ±1 two-fold dilution of the modal (most common) MIC. |
| Linearity | Ability to obtain test results directly proportional to analyte concentration. | Demonstrated through a standard curve (e.g., for colorimetric indicators). R² ≥ 0.98. |
| Range | Interval between upper and lower concentrations where accuracy, precision, and linearity are acceptable. | Must cover all clinical breakpoints and QC ranges for the drug(s) tested. |
| Robustness | Capacity to remain unaffected by small, deliberate variations in procedural parameters. | MIC variation ≤1 two-fold dilution when key parameters (inoculum density, incubation time) are altered within a specified range. |
Table 2: Example QC Ranges for Validation (CLSI M07-Ed13 2024)
| QC Strain | Antimicrobial Agent | CLSI QC MIC Range (µg/mL) |
|---|---|---|
| Staphylococcus aureus ATCC 29213 | Vancomycin | 0.5 – 2 |
| Escherichia coli ATCC 25922 | Ciprofloxacin | 0.004 – 0.016 |
| Pseudomonas aeruginosa ATCC 27853 | Meropenem | 0.25 – 1 |
| Enterococcus faecalis ATCC 29212 | Ampicillin | 0.5 – 2 |
Detailed Experimental Validation Protocol
This protocol outlines the systematic validation of an in-house broth microdilution procedure.
Materials & Preparation
- Broth Medium: Cation-adjusted Mueller Hinton Broth (CAMHB), prepared and supplemented per CLSI M07.
- Antimicrobial Stock Solutions: Prepared from USP Reference Standards or certified materials. Stocks are serially two-fold diluted in sterile water or broth as specified.
- Inoculum: Bacterial suspensions adjusted to a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL), then diluted in broth to achieve a final inoculum of ~5 x 10⁵ CFU/well.
- Microdilution Trays: Sterile, 96-well polypropylene trays. Trays are pre-dispensed with antimicrobial dilutions and stored at ≤ -60°C if not used immediately.
Validation Procedure
- QC Strain Selection: A panel of at least 3-4 CLSI-recommended QC strains representing different bacterial groups.
- Testing Replicates: Each QC strain is tested in replicates of 3-6 per run. The validation should include a minimum of 3 independent runs performed on different days.
- Parallel Testing: For accuracy assessment, the in-house procedure is run in parallel with a method that strictly adheres to the literal CLSI M07 document (if available), using the same inoculum preparation.
- Incubation: Trays are incubated at 35±2°C in ambient air for 16-20 hours (Enterobacteriaceae, Pseudomonas, staphylococci) or 20-24 hours (Streptococcus, Haemophilus).
- Endpoint Determination: MIC is read as the lowest concentration that completely inhibits visible growth. Use a mirrored reader box to aid visualization.
- Data Analysis: MICs are recorded and analyzed against the parameters in Table 1.
Workflow and Data Analysis Logic
Title: M07 In-House Validation Workflow
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for M07 Validation
| Item | Function / Purpose | Critical Specifications |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for AST. Provides consistent divalent cation levels (Ca²⁺, Mg²⁺) critical for aminoglycoside & tetracycline activity. | Must meet CLSI cation content: Ca²⁺ 20-25 mg/L, Mg²⁺ 10-12.5 mg/L. pH 7.2-7.4. |
| ATCC Quality Control Strains | Reference organisms with well-defined MIC ranges. Used to validate accuracy and precision of the test system. | Must be obtained from reputable source (e.g., ATCC). Stored and subcultured per CLSI M07-A13 guidelines. |
| USP Grade Antimicrobial Reference Standards | High-purity compounds used to prepare accurate stock solutions for microdilution trays. | Certified purity and potency. Stored appropriately (often desiccated, frozen). |
| Sterile, U-bottom 96-Well Microdilution Trays | Vessels for holding broth, antimicrobial dilutions, and inoculum during incubation. | Non-binding surface, low evaporation lid, compatible with automated dispensing systems. |
| McFarland Standard (0.5) | Turbidity standard for calibrating bacterial inoculum density to ~1-2 x 10⁸ CFU/mL. | Can be commercial latex standards or prepared barium sulfate solution. Must be verified spectrophotometrically. |
| Multichannel Pipettes & Automated Dispensers | For accurate and precise dispensing of inoculum and broth into microdilution trays. | Regularly calibrated. Tips must be sterile and aerosol-resistant. |
| MIC Reading Device (Mirrored Box) | Provides consistent, reflected light to accurately determine growth endpoints (turbidity). | Standardized design to minimize subjective reading differences. |
| Data Logging & Analysis Software | Records MICs, calculates essential statistics (mode, SD, % agreement), and compares to QC ranges. | Should be 21 CFR Part 11 compliant for regulated environments. |
This whitepaper provides a comparative analysis of two cornerstone antimicrobial susceptibility testing (AST) methods: Broth Microdilution and Agar Dilution. This analysis is framed within ongoing research on the Clinical and Laboratory Standards Institute (CLSI) M07 standard, "Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically." The CLSI M07 standard primarily details the reference broth microdilution (BMD) method, while agar dilution (AD), often referenced in M07-related documents, remains a critical method for specific applications. This document serves as a technical guide for researchers validating new antimicrobials, developing diagnostic tests, or investigating resistance mechanisms, where understanding the nuances between these reference methods is paramount.
Methodological Protocols
Broth Microdilution (CLSI M07 Core Method)
Principle: Determination of the Minimum Inhibitory Concentration (MIC) by testing bacterial growth in serial two-fold dilutions of an antimicrobial agent in a liquid growth medium within a microtiter plate.
Detailed Protocol:
- Inoculum Preparation: From a fresh (18-24 hour) agar plate, select 3-5 colonies to prepare a suspension in saline or broth. Adjust the suspension to a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL) using a densitometer.
- Inoculum Standardization: Dilute the standardized suspension in a suitable broth (e.g., cation-adjusted Mueller-Hinton Broth, CAMHB) to achieve a final concentration of approximately 5 x 10⁵ CFU/mL. This is the "working inoculum."
- Plate Inoculation: Using a multichannel pipette, transfer 100 µL of the working inoculum into each well of a pre-prepared microdilution tray containing serial two-fold dilutions of antimicrobials. Include growth control (no drug) and sterility control (no inoculum) wells.
- Incubation: Seal the tray and incubate at 35°C ± 2°C in ambient air for 16-20 hours.
- Reading and Interpretation: Examine the plate visually or with an automated reader. The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth.
Agar Dilution (M07-Related Method)
Principle: Determination of the MIC by incorporating antimicrobial agents into agar plates at serial two-fold concentrations and spotting a standardized inoculum onto the agar surface.
Detailed Protocol:
- Agar Plate Preparation: Prepare a series of Mueller-Hinton Agar plates containing serial two-fold dilutions of the antimicrobial agent. One plate without antimicrobial serves as the growth control.
- Inoculum Preparation: Prepare bacterial suspensions as in BMD, adjusting to a 0.5 McFarland standard. This suspension is used directly without further dilution.
- Inoculum Application: Using a replicating device (e.g., Steers replicator) or a multipoint inoculator, deliver a spot (~1-2 µL) of each bacterial suspension (containing ~10⁴ CFU) onto the surface of each agar plate in the dilution series. Typically, multiple isolates (32-36) are tested per plate.
- Incubation: Allow spots to dry, then incubate plates inverted at 35°C ± 2°C in ambient air for 16-20 hours.
- Reading and Interpretation: The MIC is the lowest concentration of antimicrobial agent that prevents visible growth or yields a marked reduction in growth (≥80% inhibition) compared to the growth control plate.
Comparative Data Analysis
Table 1: Core Comparative Analysis of BMD and AD Methods
| Feature | Broth Microdilution (CLSI M07) | Agar Dilution (M07-Related) |
|---|---|---|
| Format | Liquid broth in 96-well microtiter plate. | Solid agar in Petri dishes. |
| Throughput | High-throughput for a single drug against multiple isolates. | High-throughput for multiple isolates against a single drug concentration series. |
| Inoculum Density | ~5 x 10⁵ CFU/mL (final in well). | ~10⁴ CFU/spot. |
| Volume Tested | 100 µL total volume. | 1-2 µL spot volume. |
| Key Advantage | Automation-friendly; gold standard for MIC; suitable for synergy testing. | Ideal for testing fastidious or anaerobic organisms; reduces risk of cross-contamination; best for testing many isolates against one drug. |
| Key Limitation | More susceptible to cation concentration effects; not ideal for mucoid or anaerobic organisms. | Labor-intensive plate preparation; less flexible for testing multiple drugs. |
| Cost per Test | Lower for commercial pre-made panels. | Lower for in-house preparation when testing many isolates with one drug. |
| Reproducibility | Excellent intra-laboratory; requires strict quality control of broth components. | Excellent inter-laboratory; considered the reference method for many fastidious bacteria. |
| Primary CLSI Reference | M07 (Core Standard) | Referenced in M07, detailed in M11 for anaerobes, and M100 for specific organisms. |
Table 2: Quantitative Performance Metrics (Generalized Data)
| Metric | Broth Microdilution | Agar Dilution |
|---|---|---|
| Typical Incubation Time | 16-20 hrs | 16-20 hrs (up to 48h for fastidious organisms) |
| Standard Number of Isolates per Run | 1-4 per plate (multiple drugs) | 32-36 per plate (single drug) |
| Essential Quality Control Ranges | Narrow, defined for each drug-organism pair in CLSI M100. | Similar to BMD, but may differ slightly due to format. |
| Agreement with Reference Method | Self is the reference. | Generally >95% essential agreement (±1 dilution) with reference BMD for non-fastidious bacteria. |
Visualized Workflows and Relationships
Title: Broth Microdilution Experimental Workflow
Title: Agar Dilution Experimental Workflow
Title: AST Method Selection Decision Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Broth and Agar Dilution AST
| Item | Function | Critical Consideration |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for BMD. Provides consistent concentrations of Ca²⁺ and Mg²⁺, critical for aminoglycoside and tetracycline activity. | Must comply with CLSI specifications; lot-to-lot verification required. |
| Mueller Hinton Agar (MHA) | Standardized solid medium for AD. Must be poured to a uniform depth of 4 mm. | pH must be 7.2-7.4; should be free of thymidine and excessive cations. |
| Microtiter Trays (96-well) | Disposable plastic plates for BMD. Can be prepared in-house or purchased as commercial frozen or lyophilized panels. | Wells must be non-binding for antimicrobials; sterility is essential. |
| Multipoint Inoculator (Steers replicator) | Device for delivering standardized bacterial spots to multiple AD plates simultaneously. | Prongs must deliver 1-2 µL; must be flamed between inoculations to prevent carryover. |
| Turbidity Standard (0.5 McFarland) | Reference for standardizing bacterial inoculum density. Can be physical (latex) or optical (densitometer). | Must be verified and replaced regularly to ensure accurate inoculum size. |
| Quality Control (QC) Strains | Reference bacterial strains with well-defined MIC ranges (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853). | Used daily to verify the accuracy and precision of the entire test system (drug, medium, incubation). |
| Dimethyl Sulfoxide (DMSO) | Common solvent for reconstituting and diluting hydrophobic antimicrobial stock solutions. | Must be high-grade, sterile; final concentration in test system should be ≤1% (v/v) to avoid toxicity. |
Correlating M07 MICs with Disk Diffusion (M02) Zone Diameters
1. Introduction Within the broader research on the Clinical and Laboratory Standards Institute (CLSI) M07 broth microdilution standard method, establishing accurate correlations with the M02 disk diffusion method remains a critical task for antimicrobial susceptibility testing (AST). This technical guide details the principles, methodologies, and analytical approaches required to generate and validate robust interpretive correlations between Minimum Inhibitory Concentrations (MICs) determined by M07 and zone diameters from M02.
2. Core Principles of Correlation The correlation is based on the linear inverse relationship between the log₂ MIC and the zone diameter for a given antimicrobial-organism combination. This relationship is described by the regression line: Zone Diameter = a + b(log₂ MIC), where a is the intercept and b is the slope (typically negative). The primary goal is to establish zone diameter breakpoints that correspond to the MIC-based breakpoints (Susceptible, Intermediate, Resistant) defined in CLSI M100.
3. Experimental Protocols for Correlation Studies
3.1. Strain Selection and Preparation
- Panel Composition: A minimum of 100 recent, clinically isolated, non-duplicate strains of a specific bacterial species are required. The panel must include a balanced distribution of MIC values across the range of interest, including a significant number (≥10%) of resistant isolates.
- QC Strains: Include appropriate CLSI quality control strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213).
- Inoculum Preparation: For both methods, prepare bacterial suspensions in saline or Mueller-Hinton Broth (MHB) adjusted to a 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL).
3.2. Concurrent Testing by M07 and M02 Methods All isolates must be tested simultaneously by both reference methods.
CLSI M07 Broth Microdilution Protocol:
- Prepare cation-adjusted Mueller-Hinton broth (CAMHB) as per M07.
- In a 96-well microdilution tray, perform two-fold serial dilutions of the antimicrobial agent in CAMHB.
- Dilute the standardized inoculum to achieve a final concentration of ~5 x 10⁵ CFU/mL in each well.
- Incubate at 35±2°C for 16-20 hours in ambient air.
- Read the MIC as the lowest concentration of antimicrobial that completely inhibits visible growth.
CLSI M02 Disk Diffusion Protocol:
- Inoculate a Mueller-Hinton agar (MHA) plate uniformly with the standardized suspension using a sterile swab.
- Apply the appropriate antimicrobial disk to the agar surface within 15 minutes.
- Incubate at 35±2°C for 16-18 hours in ambient air.
- Measure the diameter of the zone of complete inhibition (including the disk diameter) to the nearest millimeter using calipers or an automated system.
4. Data Analysis and Regression Modeling Scatterplots are generated with log₂ MIC on the X-axis and zone diameter on the Y-axis. The correlation is analyzed using statistical methods.
4.1. Regression Analysis
- Ordinary Least Squares (OLS) Regression: Commonly used but assumes no error in the MIC value.
- Deming Regression or Passing-Bablok Regression: Preferred as they account for measurement error in both variables. These methods generate the line of best fit for setting interpretive breakpoints.
4.2. Establishing Zone Diameter Breakpoints Vertical lines are drawn on the scatterplot at the CLSI MIC breakpoints (S≤X µg/mL, I=Y µg/mL, R≥Z µg/mL). Horizontal lines are then drawn from the intersections of the regression line with these vertical MIC lines to the Y-axis. These intersection points define the proposed zone diameter breakpoints.
5. Quantitative Correlation Data Summary
Table 1: Example Correlation Data for a Hypothetical Antimicrobial vs. Enterobacterales
| Statistic / Parameter | Value |
|---|---|
| Number of Isolates (N) | 100 |
| MIC Range (µg/mL) | 0.25 – 128 |
| Zone Diameter Range (mm) | 6 – 32 |
| Regression Method | Deming |
| Correlation Coefficient (r) | -0.92 |
| Regression Equation | Zone = 28 - 3.1(log₂ MIC) |
| Proposed Breakpoint (S≥) | 20 mm (corresponding to MIC ≤4 µg/mL) |
| Proposed Breakpoint (R≤) | 12 mm (corresponding to MIC ≥16 µg/mL) |
| Essential Agreement (±1 log₂) | 97% |
| Categorical Agreement | 95% |
| Very Major Error Rate | 1.2% |
| Major Error Rate | 0.8% |
6. Visualization of Correlation Workflow
Diagram 1: Correlation Study Workflow (100 chars)
Diagram 2: Breakpoint Derivation Logic (91 chars)
7. The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for M07-M02 Correlation Studies
| Item | Function & Specification |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Liquid medium for M07 microdilution. Must contain Ca²⁺ (20-25 mg/L) and Mg²⁺ (10-12.5 mg/L) for accurate aminoglycoside & polymyxin testing. |
| Mueller-Hinton Agar (MHA) | Solid medium for M02 disk diffusion. Must be 4±0.5 mm deep. pH 7.2-7.4. |
| Antimicrobial Standard Powder | High-purity reference standard for preparing in-house microdilution panels. Used to define exact test concentrations. |
| Antimicrobial Disks | Commercially available disks with specified potencies for M02 method. Must be stored desiccated at ≤ -20°C or 2-8°C. |
| Sterile 0.85% Saline or MHB | For standardizing bacterial inoculum turbidity to the 0.5 McFarland standard. |
| McFarland Standards (0.5) | Essential for visual or densitometric calibration of inoculum density. |
| 96-Well Microdilution Trays | Sterile, non-cytotoxic trays for M07 method. Can be prepared in-house or purchased as commercially frozen/lyophilized panels. |
| ATCC Quality Control Strains | Reference strains with defined MIC and zone diameter ranges for daily quality control of both test methods. |
Understanding Differences Between CLSI M07 and EUCAST MIC Methods
Introduction Within the context of advancing broth microdilution standard method research, as per the CLSI M07 standard, understanding the nuanced differences between the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) methodologies is critical for drug development and clinical research. While both aim to determine the minimum inhibitory concentration (MIC) of antimicrobial agents, key divergences in technical parameters, interpretation criteria, and underlying philosophies impact experimental outcomes and data comparability in global research.
1. Core Methodological Divergences The foundational broth microdilution procedures in CLSI M07 and EUCAST documents share a common principle but differ in specific parameters that can influence MIC endpoints.
Table 1: Key Technical Parameters for Broth Microdilution
| Parameter | CLSI M07 (11th Ed.) | EUCAST (v 14.0) |
|---|---|---|
| Inoculum Density | 5 x 10⁵ CFU/mL | 5 x 10⁵ CFU/mL |
| Inoculum Preparation | Direct colony suspension, 0.5 McFarland standard | Direct colony suspension, 0.5 McFarland standard |
| Incubation Time | 16-20 hours; 20-24 hours for Staphylococcus spp. & some non-fermenters | 16-20 hours (± 1 hour) |
| Incubation Atmosphere | Ambient air; CO₂ only if required for growth | Ambient air; CO₂ only if required for growth |
| Broth Medium | Cation-adjusted Mueller-Hinton Broth (CAMHB) | CAMHB, with defined Ca²⁺/Mg²⁺ & low thymidine |
| Quality Control Ranges | Defined organism-specific QC limits | Defined, often narrower than CLSI QC ranges |
| Result Reading | Visual or automated; ignore single skipped well (trailing) | Visual; specific rules for reading endpoints with trailing |
2. Interpretation: Breakpoints and Clinical Categorization The most impactful difference lies in the application of breakpoints. CLSI establishes its own breakpoints (Susceptible, Intermediate, Resistant) based on extensive data review. EUCAST establishes breakpoints independently, which often differ from CLSI's, leading to different categorical interpretations.
Table 2: Comparative MIC Interpretation Outcomes (Example: E. coli and Ciprofloxacin)
| MIC (mg/L) | CLSI M100 (2024) Category | EUCAST (v 14.0) Category |
|---|---|---|
| ≤0.25 | Susceptible | Susceptible |
| 0.5 | Susceptible (I) | Resistant (≥0.5) |
| 1 | Intermediate | Resistant |
| ≥2 | Resistant | Resistant |
3. Detailed Experimental Protocol for Comparative MIC Testing The following protocol is designed to generate data suitable for analysis under both frameworks.
Materials:
- Test organism, reference QC strains (E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213).
- CAMHB, prepared according to CLSI and EUCAST specifications (separately for rigorous comparison).
- Antimicrobial stock solutions.
- Sterile 96-well microdilution plates, multichannel pipettes, plate reader (if used).
Procedure:
- Inoculum Preparation: From an overnight agar plate, prepare a 0.5 McFarland suspension in saline (~1-2 x 10⁸ CFU/mL). Dilute this 1:100 in both CLSI-specified CAMHB and EUCAST-specified CAMHB to achieve ~5 x 10⁵ CFU/mL.
- Plate Inoculation: Aliquot 100 µL of the standardized inoculum into each well of the predried antibiotic dilution panels. Include growth control (no drug) and sterility control (broth only) wells.
- Incubation: Place panels in ambient air at 35±1°C for 16-20 hours. For specific organisms (e.g., Staphylococci), a CLSI arm may be incubated for 20-24 hours.
- Endpoint Determination:
- CLSI Reading: Read the MIC as the lowest concentration that completely inhibits visible growth. Ignore a single skipped well (trailing) or faint turbidity.
- EUCAST Reading: Read the MIC as the lowest concentration that inhibits growth by ≥90% (visually). Apply specific trailing rules: for some drug-bug combinations (e.g., azoles vs. Candida), read significant reduction at 80%.
- Quality Control: Verify results within published QC ranges for each standard.
- Categorization: Apply respective CLSI M100 and EUCAST breakpoint tables to the MIC values obtained.
4. Logical Workflow for Method Selection and Data Analysis
Title: Workflow for MIC Method Selection & Analysis
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Comparative MIC Studies
| Item | Function & Specification | Critical Note |
|---|---|---|
| CAMHB, CLSI Grade | Provides standardized cation concentrations for reliable MICs in CLSI framework. | Verify lot-to-lot consistency; supplement with cations if needed per M07. |
| CAMHB, EUCAST Grade | Formulated with strict, defined low thymidine/pyrimidine and cation levels per EUCAST. | Essential for accurate comparison; not interchangeable with CLSI broth for EUCAST work. |
| Pre-dried Microdilution Panels | Custom or commercial panels with serial antibiotic dilutions for high-throughput testing. | Must be prepared and stored per manufacturer specs to ensure antibiotic stability. |
| Frozen Inoculum Trays | Standardized, ready-to-thaw inoculum for daily QC and test setup. | Improves reproducibility and saves time in longitudinal studies. |
| Electronic Inoculum Density Meters (e.g., DensiCHEK) | Provides precise, digital verification of 0.5 McFarland standard. | Replaces subjective visual comparison, enhancing data precision. |
| Plate Reading Devices | Automated readers for optical density measurement of MIC endpoints. | Must be validated against visual reading, especially for trailing endpoints. |
Conclusion For researchers engaged in CLSI M07-centric studies, a precise understanding of EUCAST methodological differences is not merely academic but essential for data contextualization, regulatory submission in different regions, and collaborative global science. The choice of standard directly influences the MIC value through medium composition and the clinical interpretation via breakpoint application. Rigorous protocols that account for these variables, supported by appropriate reagent solutions, are fundamental to generating robust, reproducible data that can be critically evaluated across the scientific community.
This whitepaper provides a technical guide for interpreting Minimum Inhibitory Concentration (MIC) data in the context of established clinical breakpoints. This process is a critical output of research utilizing the Clinical and Laboratory Standards Institute (CLSI) standard method M07: Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically. The broader thesis posits that rigorous, standardized broth microdilution, as defined by M07, generates the foundational MIC data required to establish, validate, and revise clinical breakpoints. These breakpoints are the pivotal link between in vitro susceptibility testing and predicting in vivo therapeutic success.
Foundational Concepts: MICs, Breakpoints, and Their Determinants
The MIC is the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism under defined in vitro conditions. Clinical breakpoints are specific concentration thresholds, derived from a complex analysis of MIC distributions, pharmacokinetic/pharmacodynamic (PK/PD) indices, and clinical outcome data. They categorize bacterial isolates as Susceptible (S), Intermediate (I), or Resistant (R).
Table 1: Core Components for Breakpoint Establishment
| Component | Description | Data Source |
|---|---|---|
| MIC Distribution | Population distribution of MICs for a drug-bug combination from a large, genetically diverse set of isolates. | CLSI M07-compliant studies. |
| Pharmacokinetics (PK) | Absorption, distribution, metabolism, and excretion of the drug in humans (e.g., serum concentration over time). | Human clinical trials. |
| Pharmacodynamics (PD) | Relationship between drug concentration and microbial kill (e.g., Time above MIC, AUC/MIC). | In vitro models & animal infection studies. |
| Clinical Outcome Data | Correlation of patient outcomes with the MIC of the infecting pathogen. | Controlled clinical trials. |
| Epidemiological Cutoff (ECV/ECOFF) | The MIC that separates isolates without acquired resistance mechanisms from those with them. | Analysis of wild-type MIC distributions. |
The Standardized Experimental Protocol: CLSI M07 Broth Microdilution
The generation of reliable MIC data is contingent upon strict adherence to a standardized method.
Detailed Methodology (Summarized from CLSI M07):
- Inoculum Preparation: Fresh colonies are suspended in saline or broth to a 0.5 McFarland standard (~1-2 x 10^8 CFU/mL). This suspension is further diluted in cation-adjusted Mueller-Hinton Broth (CAMHB) to achieve a final inoculum of ~5 x 10^5 CFU/mL in each well.
- Plate Preparation: A 96-well microdilution tray is used. Each row contains a serial two-fold dilution series of a single antimicrobial agent (e.g., 128, 64, 32, ... 0.125 µg/mL). One well serves as a growth control (no drug), and one as a sterility control (no inoculum).
- Inoculation & Incubation: Each well is inoculated with the standardized bacterial suspension. Trays are sealed and incubated aerobically at 35±2°C for 16-20 hours.
- MIC Determination: The MIC is read as the lowest concentration of antimicrobial that completely inhibits visible growth as observed with the unaided eye. Automated readers may be used but must be validated against visual reading.
- Quality Control: QC strains with known MIC ranges (e.g., Staphylococcus aureus ATCC 29213, Escherichia coli ATCC 25922) are run in parallel to ensure reagent and procedural accuracy.
The Pathway from MIC Data to Clinical Breakpoints
The following diagram illustrates the integrative, multi-parameter analysis required to translate MIC data into clinically actionable breakpoints.
Diagram Title: Pathway from MIC Data to Clinical Breakpoints
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for M07-Compliant MIC Research
| Item | Function & Importance |
|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium ensuring consistent cation (Ca2+, Mg2+) levels, which critically affect the activity of aminoglycosides and polymyxins. |
| Reference QC Strains (e.g., ATCC 25922, 29213, 27853) | Validate accuracy of antimicrobial dilutions, media, and incubation conditions in each run. |
| Frozen or Lyophilized Microdilution Panels | Pre-prepared panels with serial dilutions of antimicrobials ensure standardization and reproducibility across labs. |
| Digital Colony Density Meter | Precisely standardizes inoculum to a 0.5 McFarland standard, a critical pre-analytical variable. |
| Multichannel Pipettes & Sterile Reservoirs | Ensures rapid, uniform, and sterile inoculation of 96-well microdilution trays. |
| Microdilution Tray Sealer | Prevents evaporation and cross-contamination during incubation. |
| Refrigerated Microplate Incubator | Maintains stable, uniform temperature at 35±2°C across all wells during incubation. |
| Validated MIC Reading System (Visual or Automated) | For accurate, reproducible endpoint determination. Automated systems must correlate with gold-standard visual reads. |
Quantitative Data Correlation in Practice
Table 3: Hypothetical Data Analysis for a Novel Cephalosporin vs.E. coli
| MIC (µg/mL) | Number of Isolates (n=200) | PK/PD Target Attainment* | Clinical Cure Rate* | Proposed Breakpoint Category |
|---|---|---|---|---|
| ≤0.25 | 85 | 99% | 96% | Susceptible |
| 0.5 | 50 | 95% | 92% | Susceptible |
| 1 | 35 | 85% | 85% | Susceptible |
| 2 | 15 | 70% | 75% | Intermediate |
| 4 | 10 | 40% | 60% | Resistant |
| ≥8 | 5 | <10% | <50% | Resistant |
| ECOFF Value | MIC ≤1 µg/mL |
Simulated data for illustration. Target attainment is based on probability of achieving free drug concentration above MIC for 60% of the dosing interval (fT>MIC).
Interpretation: The MIC distribution shows a clear wild-type population (≤1 µg/mL). PK/PD and clinical outcomes are excellent for MICs ≤1 µg/mL, decline at 2 µg/mL, and are poor at ≥4 µg/mL. This supports setting a Susceptible breakpoint at ≤1 µg/mL, an Intermediate at 2 µg/mL, and a Resistant breakpoint at ≥4 µg/mL. The ECOFF (≤1 µg/mL) aligns with the proposed susceptible breakpoint, confirming it separates wild-type from non-wild-type populations.
Advanced Workflow for MIC/Breakpoint Correlation Studies
Diagram Title: MIC-Breakpoint Correlation Research Workflow
The correlation of MICs with clinical breakpoints is a data-intensive, multi-disciplinary process. The CLSI M07 broth microdilution standard is the non-negotiable foundation, providing the reproducible, high-quality in vitro susceptibility data upon which all subsequent PK/PD and clinical analyses depend. For researchers and drug developers, mastery of M07 and a deep understanding of the integrative breakpoint-setting framework are essential for advancing new antimicrobial agents and ensuring their effective and appropriate clinical use.
Conclusion
The CLSI M07 broth microdilution method remains the cornerstone reference technique for quantitative antimicrobial susceptibility testing. Mastering its foundational principles, adhering to its detailed protocol, proactively troubleshooting common issues, and rigorously validating results against comparative standards are all essential for generating reliable MIC data. This data is critical for driving informed decisions in antimicrobial drug discovery, clinical trial design, and understanding resistance mechanisms. Future directions will likely involve greater integration of automation and digital plate reading, harmonization with international standards like EUCAST, and adaptations to address emerging challenges such as testing novel antimicrobial classes (e.g., phage therapy, antimicrobial peptides) and complex polymicrobial infections. Continued reliance on and proper implementation of M07 ensures the scientific integrity of the fight against antimicrobial resistance.