INT Colorimetric Assay for MIC Determination: A Comprehensive Guide from Principle to Precision
This article provides a thorough exploration of the p-iodonitrophenyltetrazolium violet (INT) colorimetric assay for determining the Minimum Inhibitory Concentration (MIC) of antimicrobial agents.
INT Colorimetric Assay for MIC Determination: A Comprehensive Guide from Principle to Precision
Abstract
This article provides a thorough exploration of the p-iodonitrophenyltetrazolium violet (INT) colorimetric assay for determining the Minimum Inhibitory Concentration (MIC) of antimicrobial agents. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of the assay, including its mechanism where INT is reduced by metabolically active bacterial cells to a colored formazan product, enabling visual or spectrophotometric MIC reading. The scope extends to detailed methodological protocols for essential oils and antibiotics, strategies for troubleshooting common sources of variability like analyst technique and reagent stability, and rigorous validation procedures against reference methods such as Etest. By synthesizing these four core intents, this guide serves as a definitive resource for implementing a robust, accurate, and reproducible INT colorimetric MIC assay in both research and development settings.
Understanding the INT Colorimetric Assay: Principles, Mechanisms, and Advantages over Traditional MIC Methods
The 2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride (INT) is a tetrazolium salt that serves as a critical colorimetric viability indicator in microbiological assays. Its core principle of operation is based on its reduction by metabolically active bacterial cells into an intensely colored, insoluble formazan product. In the presence of active dehydrogenase enzyme systems within viable bacteria, the colorless, water-soluble INT is reduced to iodonitrotetrazolium formazan, which is characterized by its reddish-purple or pink color [1]. This color change provides a clear, visual endpoint for determining bacterial growth and, by extension, the efficacy of antimicrobial compounds. The INT assay is particularly valuable in Minimum Inhibitory Concentration (MIC) determination, a fundamental test in antimicrobial susceptibility testing. It offers a solution to the challenges of visual turbidity reading, which can lead to underestimation of bacterial growth, by providing a more objective, color-based signal that is directly proportional to the quantity of viable cells [1].
Application Note: INT in MIC Determination
Core Principle and Mechanism
The INT assay functions as a biochemical marker for cellular respiration. Metabolically active bacteria possess an intact electron transport chain. INT acts as an artificial electron acceptor in this chain. When bacterial cells are viable, their dehydrogenase enzymes reduce the INT molecule, cleaving the tetrazolium ring. This biochemical reduction reaction transforms the colorless INT into a vividly colored, water-insoluble formazan precipitate [1]. The intensity of the color developed is directly correlated with the number of metabolically active cells in the test system. In the context of MIC determination, a lack of color change after incubation indicates that bacterial growth has been successfully inhibited by the antimicrobial agent at that specific concentration.
Comparison with Other Viability Indicators
INT is one of several tetrazolium salts used for viability indication. Research has compared its performance against other common indicators, noting that different salts have varying properties, including toxicity and the nature of the formazan product [1]. The following table summarizes key tetrazolium salts and their characteristics:
Table 1: Comparison of Tetrazolium Salts Used as Viability Indicators
| Tetrazolium Salt | Full Name | Reduced Product (Formazan) Color | Key Characteristics |
|---|---|---|---|
| INT | 2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride | Reddish-Purple / Pink | Mentioned as a common choice; properties compared in validation studies [1]. |
| TTC | 2,3,5-Triphenyltetrazolium Chloride | Red | Selected in a validated method for lower toxicity compared to INT and MTT; colorless when solubilized in water [1]. |
| MTT | 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide | Purple | Noted to exhibit higher toxicity in comparative studies [1]. |
| XTT | 2,3-bis(2-Methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5-carboxanilide | Orange | Undergoes color alteration upon reduction [1]. |
| Resazurin | 7-Hydroxy-3H-phenoxazin-3-one-10-oxide | Blue (Oxidized) to Pink (Resorufin) | Used in Resazurin Microtiter Assay (REMA); color change indicates bacterial growth [2]. |
Experimental Protocol: MIC Determination Using the INT Assay
This protocol describes a standardized broth microdilution method for determining the Minimum Inhibitory Concentration of antimicrobial compounds against aerobic bacteria, using INT as a visual growth indicator.
Research Reagent Solutions and Essential Materials
Table 2: Key Reagents and Materials for INT-based MIC Assay
| Item | Function / Description |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized broth medium for susceptibility testing of non-fastidious aerobic bacteria [3] [4]. |
| INT Solution | 2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride, prepared at 0.2% (w/v) in sterile water. Filter-sterilize and store protected from light [1]. |
| Microdilution Panels | Sterile 96-well U-bottom plates. |
| Standardized Bacterial Inoculum | Bacterial suspension adjusted to a turbidity equivalent to a 0.5 McFarland standard, then diluted to yield a final concentration of ~5 x 10^5 CFU/mL in each well [3] [4]. |
| Antimicrobial Stock Solutions | Solutions of the test antimicrobial agent at a known, high concentration (e.g., 1280 µg/mL) for serial dilution. |
| Multichannel Pipettes | For accurate and efficient reagent distribution. |
| Microplate Incubator | Capable of maintaining 35 ± 2 °C for aerobic incubation [3]. |
| Dey-Engley (D/E) Neutralizing Broth | Contains neutralizers to inactivate residual disinfectant or antiseptic in the sample for accurate MIC determination [2]. |
Step-by-Step Procedure
Step 1: Preparation of Antimicrobial Serial Dilutions 1.1. Dispense 100 µL of CAMHB into all wells of the 96-well microdilution panel, except for the first well in each row. 1.2. In the first well, add 200 µL of the antimicrobial stock solution. 1.3. Perform a two-fold serial dilution using a multichannel pipette. Transfer 100 µL from the first well to the second, mix thoroughly, and continue this process to the penultimate well. Discard 100 µL from the penultimate well. The final well serves as the growth control (no antimicrobial) [3] [1].
Step 2: Inoculation of the Test Panel 2.1. Prepare a standardized bacterial inoculum as described in Section 3.1. 2.2. Add 10 µL of the standardized inoculum to all test wells, resulting in a final volume of 110 µL and a target inoculum of ~5 x 10^5 CFU/mL per well [1]. 2.3. Include a sterility control well (broth only) to confirm medium sterility.
Step 3: Incubation 3.1. Cover the microdilution panel and incubate at 35 ± 2 °C for 16-20 hours under aerobic conditions [3].
Step 4: Addition of INT Indicator and Final Incubation 4.1. After the initial incubation, add 20 µL of the 0.2% INT solution to each well. 4.2. Re-incubate the plate for 1-4 hours, or until a distinct color development is observed in the growth control well [1].
Step 5: Reading and Interpretation of Results 5.1. Examine the plate for a color change from colorless to reddish-purple.
- Viable Bacteria (Positive Result): Reddish-purple formazan precipitate indicates bacterial growth.
- Non-Viable Bacteria (Negative Result): No color change indicates inhibition of growth. 5.2. The Minimum Inhibitory Concentration (MIC) is defined as the lowest concentration of the antimicrobial agent that completely prevents a color change, indicating no visible bacterial growth [1].
Experimental Workflow Visualization
The following diagram illustrates the logical workflow for the INT-based MIC determination protocol:
Data Presentation and Analysis
Quantitative Data from INT-Based MIC Assays
The data generated from an INT-based MIC assay can be systematically recorded for analysis. The table below provides a hypothetical example of results for a single bacterial isolate tested against an antimicrobial agent.
Table 3: Example MIC Test Results and Interpretation Using INT
| Well Number | Antimicrobial Concentration (µg/mL) | Visual Turbidity | INT Color Reaction | Interpretation |
|---|---|---|---|---|
| 1 (Growth Control) | 0 | Turbid | Reddish-Purple | Growth |
| 2 | 1 | Clear | No Color Change | No Growth |
| 3 | 2 | Clear | No Color Change | No Growth |
| 4 | 4 | Clear | No Color Change | No Growth |
| 5 | 8 | Clear | No Color Change | No Growth |
| 6 | 16 | Slightly Turbid | Faint Pink | Partial Inhibition |
| 7 | 32 | Turbid | Reddish-Purple | Growth |
| 8 | 64 | Turbid | Reddish-Purple | Growth |
| MIC Result | 8 µg/mL |
Advanced Quantitative Applications
Beyond the qualitative MIC endpoint, the INT assay can be adapted for more advanced quantitative analysis. The formazan product can be dissolved in an organic solvent (e.g., DMSO or ethanol), and its absorbance can be measured spectrophotometrically. This absorbance value can be correlated with the number of viable cells (CFU/mL), allowing for the determination of inhibitory concentrations that cause a 50% or 90% reduction in viability (IC50% and IC90%), providing a more precise measure of an antimicrobial agent's potency [1].
Within antimicrobial drug discovery, the minimum inhibitory concentration (MIC) serves as a fundamental quantitative measure, defining the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism [5] [6]. Accurate and rapid MIC determination is critical for evaluating the efficacy of new compounds and for guiding clinical treatment strategies in the face of rising antimicrobial resistance [1] [6]. Colorimetric assays using tetrazolium salts, such as INT (2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium Chloride), have emerged as powerful tools to streamline this process. These assays leverage a vivid color change—from violet tetrazolium to red formazan—as a metabolic indicator of viable cells, enabling clearer and more objective endpoint determination than traditional turbidity measurements [1]. This application note details the biochemical mechanism of this reaction and provides a standardized protocol for employing the INT assay in MIC determination, a methodology highly relevant for research framed within the context of antibiotic susceptibility testing.
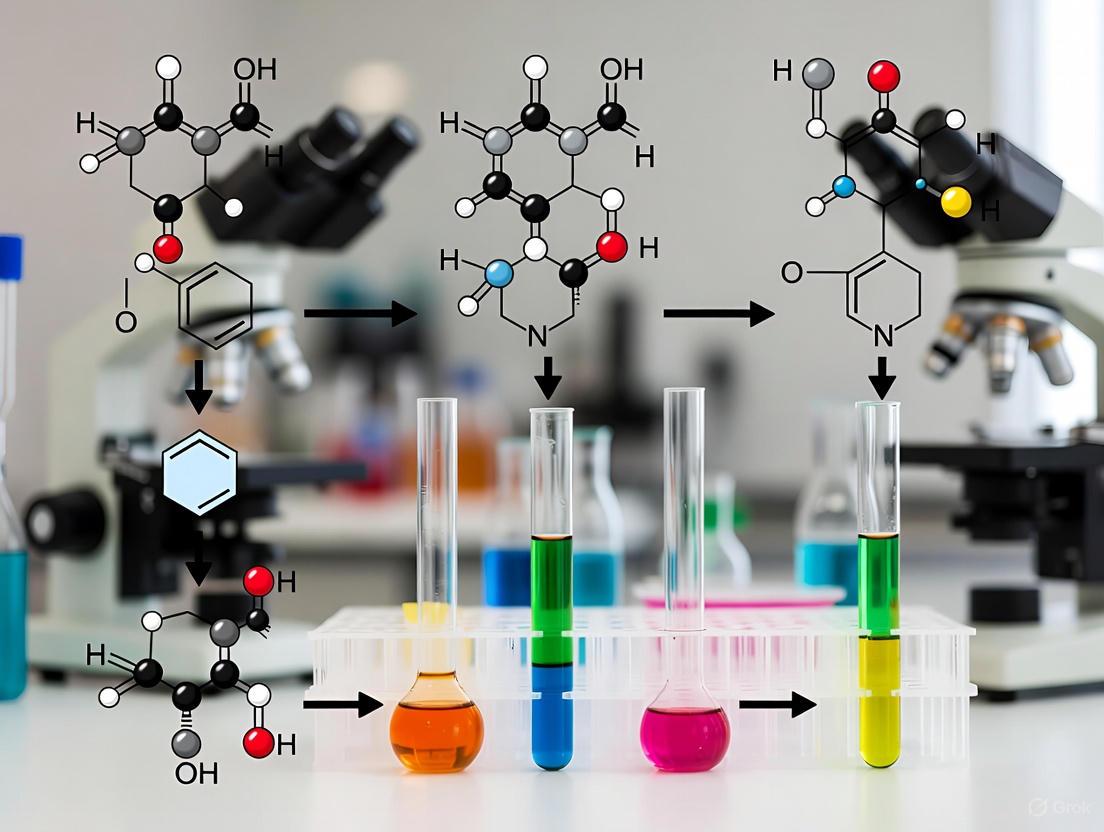
Biochemical Mechanism of Tetrazolium Reduction
The core principle of the INT colorimetric assay rests on the enzymatic reduction of a tetrazolium salt into a corresponding formazan product. The distinct violet color of the INT tetrazolium compound is transformed into a red-colored, water-insoluble formazan crystal in the presence of metabolically active microbial cells [1].
The Reduction Reaction
This color change is a visual manifestation of cellular metabolic activity. Viable microorganisms with active electron transport chains possess dehydrogenase enzymes. These enzymes, often acting in concert with the cofactor NADH, transfer electrons from metabolic substrates to the tetrazolium compound [7] [8]. The INT molecule acts as an artificial electron acceptor, becoming reduced in the process. This reduction disrupts the tetrazole ring structure, leading to the formation of the formazan dye [7]. The amount of formazan produced is directly proportional to the number of viable, metabolically active cells present [9].
Diagram 1: The biochemical pathway of INT reduction to formazan.
Application in Susceptibility Testing
In the context of antimicrobial susceptibility testing, this mechanism is harnessed to determine the MIC. When a microorganism is exposed to an effective antibiotic, its metabolic activity is inhibited or the cell is killed. Consequently, the electron transport chain is disrupted, and the reduction of INT to formazan ceases or is significantly diminished [8]. In a microdilution plate containing serial dilutions of an antibiotic, wells with concentrations below the MIC will show metabolic activity and turn red, while wells at or above the MIC will remain violet, indicating no bacterial growth [1]. This provides a clear, color-based visual endpoint for determining the MIC.
Research Reagent Solutions
The following table details the essential reagents and materials required to perform the INT colorimetric MIC assay.
Table 1: Key research reagents and their functions in the INT assay.
| Reagent/Material | Function/Description | Example/Comment |
|---|---|---|
| INT Tetrazolium Salt | Colorimetric indicator; reduced to red formazan by metabolically active cells [1]. | Prepare as a 0.2 mg/mL stock solution in water; filter-sterilize [1]. |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized culture medium for antimicrobial susceptibility testing [6]. | Ensures reproducible and accurate MIC results [6]. |
| 96-Well Microtiter Plate | Platform for broth microdilution testing [1] [6]. | U-bottom plates are commonly used. |
| Antibiotic Stock Solutions | Source of the antimicrobial agent for serial dilution [6]. | Typically prepared at high concentration (e.g., 10 mg/mL) in appropriate solvent [6]. |
| Inoculum Standard | Standardized microbial suspension for inoculation [1] [6]. | Adjusted to 0.5 McFarland standard (~1-2 x 10⁸ CFU/mL for bacteria). |
Detailed Experimental Protocol for MIC Determination
This protocol is adapted from standardized methods for broth microdilution and colorimetric assessment [1] [6] [10].
Pre-Assay Preparation
- INT Solution Preparation: Dissolve INT powder in sterile distilled water to a concentration of 0.2 mg/mL. Filter-sterilize the solution using a 0.2 µm membrane filter. The solution can be stored protected from light at 4°C [1].
- Antibiotic Serial Dilution:
- Prepare a stock solution of the test antibiotic. Common solvents include water, methanol, or DMSO, chosen based on the compound's solubility [6].
- Perform two-fold serial dilutions of the antibiotic in CAMHB across the wells of a 96-well microtiter plate. A typical volume is 100 µL per well. The concentration range should encompass the expected MIC and clinical breakpoints [6].
- Inoculum Preparation:
- Grow the test microorganism on an appropriate solid medium for 18-24 hours.
- Suspend colonies in a sterile saline solution and adjust the turbidity to match a 0.5 McFarland standard (approximately 1-2 x 10⁸ CFU/mL for bacteria) [1] [6].
- Further dilute this suspension in CAMHB to achieve a final working inoculum, which is typically around 5 x 10⁵ CFU/mL.
Assay Procedure and Incubation
- Inoculation: Add 100 µL of the prepared working inoculum to each well of the microtiter plate containing the antibiotic dilutions. This step brings the final test volume to 200 µL per well and the final bacterial concentration to approximately 5 x 10⁵ CFU/mL.
- Controls:
- Growth Control: Include a well containing 100 µL of CAMHB and 100 µL of inoculum (no antibiotic).
- Sterility Control: Include a well containing 200 µL of CAMHB only (no inoculum, no antibiotic).
- Incubation: Seal the microtiter plate and incubate at 35±2°C for 16-20 hours, unless testing slow-growing organisms [6].
Colorimetric Development and MIC Reading
- INT Addition: After the initial incubation period, add 20-30 µL of the 0.2 mg/mL INT solution to each well [1].
- Secondary Incubation: Re-incubate the plate for 1-4 hours at 35±2°C. Monitor the plate periodically for color development.
- Endpoint Determination: The MIC is defined as the lowest concentration of antibiotic that completely prevents a color change to red. Wells with viable, growing bacteria will turn pink/red due to formazan production, while wells with inhibited growth will remain colorless (or the color of the original medium) [1].
Diagram 2: Experimental workflow for the INT microdilution assay.
Data Interpretation and Quantitative Analysis
The INT assay provides qualitative and quantitative data for determining antimicrobial activity.
Visual and Spectrophotometric Reading
The primary readout is visual: a clear well indicates no growth (inhibited), and a red well indicates growth. For a more objective and quantitative analysis, the optical density (OD) of each well can be measured using a microplate reader. Formazan production can be quantified at 570 nm, and the absorbance values are correlated with the number of viable cells [1]. This allows for the calculation of IC50% and IC90% (the concentrations inhibiting 50% and 90% of growth, respectively) in addition to the standard MIC [1].
Table 2: Example of MIC results and interpretation for a hypothetical antibiotic against S. aureus.
| Antibiotic Concentration (µg/mL) | Visual Color | OD570 nm | Growth Interpretation | MIC Determination |
|---|---|---|---|---|
| 16 | Colorless | 0.05 | No Growth | |
| 8 | Colorless | 0.06 | No Growth | MIC = 4 µg/mL |
| 4 | Faint Pink | 0.25 | Inhibited Growth | |
| 2 | Red | 0.85 | Growth | |
| 1 | Red | 0.89 | Growth | |
| 0.5 | Red | 0.91 | Growth | |
| Growth Control | Red | 0.90 | Growth | |
| Sterility Control | Colorless | 0.04 | No Growth |
Validation and Comparison with Reference Methods
The performance of the INT assay should be validated against reference strains with known MIC values. Studies on similar tetrazolium and colorimetric assays have shown excellent correlation with standard broth microdilution and molecular methods (e.g., mecA gene detection for MRSA), with category agreement often exceeding 99% [9] [10]. A key advantage of the INT method is its speed, providing results in 5-7 hours post-inoculation for many fast-growing bacteria, compared to the 16-20 hours required for a standard visual MIC readout [9] [10].
The colorimetric assay for Minimum Inhibitory Concentration (MIC) determination represents a significant advancement in antimicrobial susceptibility testing (AST). By utilizing redox indicators like INT (Iodonitrotetrazolium chloride) or colorimetric pH sensors, these assays transform the visual interpretation of bacterial growth and metabolic activity into a simple color change output [11] [12]. This document details the application and protocol for INT colorimetric assays, highlighting their key advantages—simplicity, accuracy, and reproducibility—within modern research and drug development pipelines. The integration of such methods addresses the growing need for rapid, reliable diagnostics in the face of increasing antimicrobial resistance [11].
Key Advantages and Quantitative Performance
The INT colorimetric assay offers a compelling alternative to traditional AST methods like broth microdilution. Its performance is characterized by the following advantages:
- Simplicity: The assay requires minimal specialized equipment compared to reference methods. The color change endpoint is visually interpretable, facilitating use in various settings [11].
- Accuracy: The method demonstrates high categorical agreement with reference standards. For instance, similar colorimetric principles have shown sensitivity and specificity values exceeding 95% in related diagnostic applications [12].
- Reproducibility: The use of stable chemical indicators and standardized protocols ensures consistent results across different operators and laboratories [13].
Table 1: Comparative Analysis of AST Methods
| Method Feature | INT Colorimetric Assay | Reference Broth Microdilution [11] | Disk Diffusion [11] |
|---|---|---|---|
| Turnaround Time | 2 - 6 hours (with rapid metabolic indicator) | 18 - 24 hours | 18 - 24 hours |
| Result Output | Quantitative (MIC) | Quantitative (MIC) | Qualitative/Semi-quantitative (S/I/R) |
| Equipment Cost | Low (spectrophotometer optional) | Moderate (requires dedicated trays, reader) | Low |
| Ease of Automation | High (suitable for microtiter plates) | High | Low |
| Per-test Cost | Low | Moderate to High | Low ($2 - $5) |
Table 2: Performance Metrics of Colorimetric Assays in Related Applications
| Assay Type | Target | Reported Sensitivity | Reported Specificity | Linear Range / LOD |
|---|---|---|---|---|
| ColorPhAST [12] | Phage susceptibility in E. coli | 95.6% | 100% | N/A |
| GSH Detection [14] | Glutathione | N/A | N/A | 0–152.7 μM (LOD: 0.74 μM) |
| Tyrosinase Assay [15] | Tyrosinase | N/A | N/A | LOD: 4.13 x 10⁻⁵ U/mL |
Experimental Protocol: INT Colorimetric MIC Determination
This protocol is adapted for a 96-well microtiter plate format, enabling high-throughput screening of compounds against bacterial pathogens.
Materials and Reagents
Table 3: Research Reagent Solutions
| Item | Function/Description |
|---|---|
| Cation-adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for AST as per EUCAST/CLSI guidelines [4]. |
| INT (Iodonitrotetrazolium chloride) Solution | Redox indicator. Prepared as a 2 mg/mL stock solution in sterile water and filter-sterilized. |
| Test Compound/Antibiotic | Serial dilutions prepared in CAMHB. |
| Bacterial Inoculum | Adjusted to a 0.5 McFarland standard, then diluted to ~1-5 x 10⁵ CFU/mL in CAMHB. |
| Sterile 96-Well Microtiter Plates | Platform for broth microdilution assay. |
| Multichannel Pipettes | For efficient reagent and inoculum dispensing. |
| Microplate Spectrophotometer (Optional) | For objective measurement of absorbance at 490-520 nm. |
Procedure
Day 1: Preparation
- Compound Dilution Series: In a sterile 96-well plate, perform a two-fold serial dilution of the antibiotic or test compound in CAMHB across the rows (e.g., 100 μL/well). Leave the last column without antibiotic for growth control wells.
- Inoculum Preparation: Pick 3-5 colonies from an overnight agar plate and suspend in sterile saline. Adjust the turbidity to a 0.5 McFarland standard (approx. 1-2 x 10⁸ CFU/mL). Dilute this suspension 1:100 in CAMHB to achieve a working inoculum of ~1-5 x 10⁶ CFU/mL.
Day 1: Inoculation and Incubation
- Plate Inoculation: Add 100 μL of the bacterial inoculum to all test and growth control wells. Add 100 μL of sterile CAMHB to the sterility control wells.
- Incubation: Seal the plate with a lid or parafilm and incubate at 35±2°C for 16-20 hours under normal atmospheric conditions.
Day 2: INT Staining and MIC Reading
- INT Addition: After incubation, add 20-40 μL of the sterile INT stock solution (2 mg/mL) to each well.
- Re-incubation: Re-incubate the plate for 30 minutes to 4 hours. Monitor periodically for color development.
- Endpoint Determination:
- Visual: The MIC is defined as the lowest concentration of the antibiotic that prevents a color change to pink/red. A color change indicates bacterial metabolic activity and reduction of INT to formazan.
- Spectrophotometric: Read the absorbance at 490-520 nm. The MIC is the lowest concentration where the absorbance is statistically indistinguishable from the sterility control.
Signaling Principle and Workflow Visualization
The INT assay is based on a straightforward biochemical principle. Metabolically active bacterial cells reduce the tetrazolium compound INT, which is colorless or yellow, into an intracellular, colored formazan product (pink/red). Inhibition of bacterial growth by an effective antibiotic prevents this reduction, thus inhibiting the color change [11].
Diagram 1: INT Colorimetric Signaling Principle.
The experimental workflow, from plate preparation to data analysis, is streamlined for efficiency and reliability, as outlined below.
Diagram 2: INT MIC Assay Workflow.
This application note provides a detailed comparative analysis of the p-iodonitrotetrazolium chloride (INT) colorimetric assay against the established agar dilution and broth macrodilution methods for determining the Minimum Inhibitory Concentration (MIC) of antimicrobial agents. MIC is defined as the lowest concentration of an antimicrobial agent that completely inhibits visible growth of a microorganism under controlled conditions [16]. We present standardized protocols, comparative performance data, and practical considerations to assist researchers in selecting the appropriate methodology for their antimicrobial susceptibility testing requirements. The INT colorimetric assay offers a rapid, sensitive alternative to traditional methods, particularly valuable in high-throughput screening environments and when evaluating colored substances that complicate visual interpretation.
Determining the Minimum Inhibitory Concentration (MIC) is a fundamental practice in microbiology for assessing the efficacy of antimicrobial compounds. While dilution methods are considered the gold standard, colorimetric assays have emerged as efficient alternatives addressing specific limitations of traditional approaches.
Agar dilution involves incorporating the antimicrobial agent into molten agar medium, pouring plates with serial concentrations, and spotting standardized inocula onto the agar surface. The MIC is the lowest concentration preventing visible growth after incubation [17] [18] [19]. It is regarded as a reference method with excellent reproducibility and is cost-effective for testing numerous bacterial isolates against a limited set of antimicrobial agents [17] [19].
Broth macrodilution employs a series of test tubes containing broth with two-fold serial dilutions of the antimicrobial agent. After inoculation with a standardized microbial suspension and incubation, the MIC is determined as the tube with the lowest concentration showing no visible turbidity [16] [20]. This method, while foundational, is resource-intensive and less suited for high-throughput applications.
The INT colorimetric assay utilizes the metabolic indicator p-iodonitrotetrazolium chloride, which is reduced by metabolically active bacteria from a colorless compound to a pink-red formazan derivative. The MIC is identified as the lowest concentration of antimicrobial agent where no color change occurs, indicating complete inhibition of microbial metabolism [21]. This method is particularly advantageous for its objectivity and rapid readout.
Comparative Methodologies: Protocols and Procedures
Agar Dilution Protocol
The agar dilution method is a robust, standardized technique recommended for testing large batches of bacterial isolates [17] [19].
Materials:
- Mueller-Hinton Agar (MHA) or appropriate supplemented medium (e.g., MHA with 5% sheep blood for fastidious organisms)
- Antimicrobial stock solution
- Bacterial strains adjusted to 0.5 McFarland standard (~1 x 10⁸ CFU/mL)
- Replicator device delivering 1-5 μL (final inoculum ~5 x 10⁴ CFU/spot)
Procedure:
- Prepare a series of two-fold dilutions of the antimicrobial agent in sterile water or an appropriate solvent [16].
- Incorporate each dilution into separate batches of molten agar, mixing thoroughly.
- Pour the antimicrobial-supplemented agar into Petri dishes and allow to solidify.
- Apply the standardized bacterial inocula (30-36 spots per plate) using a replicator device.
- Incubate the plates under optimal conditions (e.g., 35°C for 16-20 hours in ambient air or CO₂ for fastidious bacteria).
- Read the MIC as the lowest antimicrobial concentration that completely inhibits visible growth [18] [19].
Broth Macrodilution Protocol
This method determines MIC in a liquid medium system, often performed in tubes [20].
Materials:
- Mueller-Hinton Broth (MHB) or appropriate supplemented medium
- Antimicrobial stock solution
- Test tubes
- Bacterial suspension adjusted to 0.5 McFarland standard, further diluted to yield ~5 x 10⁵ CFU/mL in the final test volume
Procedure:
- Prepare a series of two-fold dilutions of the antimicrobial agent in MHB within test tubes.
- Inoculate each tube with the standardized bacterial suspension.
- Incubate the tubes under optimal conditions (e.g., 35°C for 16-20 hours).
- Read the MIC as the lowest antimicrobial concentration that completely inhibits visible turbidity [16] [20].
INT Colorimetric Assay Protocol
The INT assay provides a metabolic endpoint for growth inhibition, enhancing objectivity [21].
Materials:
- Mueller-Hinton Broth (MHB)
- 96-well microtiter plates
- Antimicrobial stock solution and/or plant extracts
- Bacterial suspension adjusted to ~10⁶ CFU/mL in MHB
- INT solution (0.2 mg/mL of p-iodonitrotetrazolium chloride, filter-sterilized)
Procedure:
- Serially dilute the antimicrobial agent or plant extract two-fold in MHB within the wells of a 96-well microtiter plate.
- Inoculate each well with the standardized bacterial suspension.
- Incubate the plate at 37°C for 20 hours.
- Add INT solution (e.g., 40 μL per well) and incubate for an additional 30 minutes.
- Read the MIC as the lowest concentration of the antimicrobial agent in a well that remains clear (no pink-red color formation) after the addition and incubation with INT [21].
Comparative Performance Data
The following tables summarize key characteristics and performance metrics of the three MIC determination methods.
Table 1: Method Characteristics and Operational Comparison
| Parameter | INT Colorimetric Assay [21] | Agar Dilution [17] [19] | Broth Macrodilution [16] [20] |
|---|---|---|---|
| Principle | Metabolic activity (color change) | Visible growth on solid medium | Visible growth (turbidity) in liquid medium |
| Throughput | High (96-well format) | High for isolates, low for agents | Low |
| Subjectivity | Low (colorimetric endpoint) | Moderate (visual growth) | Moderate (visual turbidity) |
| Turnaround Time | ~20.5 hours | 16-48 hours | 16-20 hours |
| Cost per Test | Low | Cost-effective for batch testing | High (resource-intensive) |
| Ease of Automation | High | Low | Low |
Table 2: Reported Method Agreement in Literature
| Comparison | Agreement | Context / Organisms | Source |
|---|---|---|---|
| Broth Microdilution vs. Etest | 88% within ±1 log₂ dilution | Doripenem vs. Gram-positive and Gram-negative bacteria | [22] |
| Broth Microdilution vs. Agar Dilution | 94% within ±1 log₂ dilution | Doripenem vs. Gram-positive and Gram-negative bacteria | [22] |
| Broth Microdilution vs. Agar Dilution | 78.7% within 1 log₂ MIC | Campylobacter jejuni and C. coli | [23] |
| REMA vs. D/E Neutralizer (Colorimetric) | 90.3% overall agreement | Povidone-Iodine vs. S. aureus and K. aerogenes | [2] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for MIC Determination
| Reagent | Function & Application | Key Considerations |
|---|---|---|
| p-Iodonitrotetrazolium Chloride (INT) | Colorimetric indicator of cellular metabolic activity. Used in the INT assay, it is reduced from colorless to pink-red formazan in the presence of growing bacteria [21]. | Filter sterilize. Optimize concentration and incubation time to prevent background color development. |
| Mueller-Hinton Agar/Broth | Standardized, nutritionally adequate medium for antimicrobial susceptibility testing of non-fastidious bacteria [19] [16]. | For fastidious organisms, supplementation (e.g., 5% sheep blood) is required as per CLSI/EUCAST guidelines. |
| Dey-Engley (D/E) Neutralizing Broth | Contains neutralizing agents (e.g., Tween, lecithin) to inactivate disinfectants and antimicrobials during testing, preventing carry-over effect. Can include a colorimetric indicator [2]. | Critical for evaluating antiseptics and disinfectants to ensure accurate MIC results. |
| Resazurin Sodium Salt | Oxidation-reduction indicator used in assays like REMA. It changes from blue to pink/colorless upon reduction by metabolically active cells [2]. | Can be more sensitive than INT but may require fluorescence measurement for optimal detection. |
| Dimethyl Sulfoxide (DMSO) | Common solvent for dissolving hydrophobic antimicrobial compounds, plant extracts, or synthetic drugs prior to dilution in aqueous media [16]. | Use the lowest possible concentration as high levels can be toxic to test microorganisms. |
The selection of an MIC method depends on the specific research objectives, sample type, and available resources.
For high-throughput screening of novel compounds or plant extracts, the INT colorimetric assay in a 96-well microplate format is highly recommended. Its objective endpoint, speed, and minimal reagent requirements make it ideal for processing large numbers of samples [21]. It is particularly useful for testing colored plant extracts that can obscure visual growth reading in traditional methods.
For reference testing and batch analysis of multiple bacterial isolates against a few agents, agar dilution remains the gold standard. Its high reproducibility and capacity to test up to 30 isolates simultaneously per plate make it cost-effective for surveillance studies [17] [19].
Broth macrodilution, while foundational, is now primarily used when other methods are not feasible or for specific organism-drug combinations. Its labor-intensive and resource-heavy nature limits its use in modern high-volume laboratories [20].
In conclusion, while agar dilution provides a benchmark for accuracy, the INT colorimetric assay offers a reliable, rapid, and efficient alternative for quantitative MIC determination, especially within the context of drug discovery and resistance monitoring. Researchers should validate any non-reference method against a standard dilution method for their specific microbial strains to ensure result reliability.
The rising threat of antimicrobial resistance necessitates the continuous discovery and evaluation of new antimicrobial agents, including natural products like essential oils (EOs) and novel synthetic antibiotics [24]. Fastidious organisms, with their complex nutritional requirements and slow growth rates, present a significant challenge for conventional antimicrobial susceptibility testing (AST) [25] [26]. The INT colorimetric assay for minimum inhibitory concentration (MIC) determination offers a robust, sensitive, and quantitative solution for screening compounds against these demanding microorganisms. This application note details standardized protocols integrating this colorimetric method, framed within broader research on optimizing MIC determinations for fastidious bacteria.
The Challenge of Fastidious Organisms and Essential Oils in Susceptibility Testing
Fastidious bacteria, such as the HACEK group (Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella), Abiotrophia, Granulicatella, and Campylobacter spp., require specialized media, atmospheric conditions, and often extended incubation times for growth [25] [26]. The lack of standardized testing guidelines for many of these organisms further complicates the reliable assessment of their susceptibility [25].
Similarly, evaluating the antimicrobial properties of EOs is problematic due to their complex, hydrophobic, and volatile nature [27]. Conventional broth microdilution methods can be affected by the insolubility of EOs in aqueous media and the potential for vapor-phase activity, which may lead to cross-contamination between wells in a microtiter plate [27]. The INT colorimetric assay addresses key limitations of visual turbidity readings by providing a clear, objective color change linked to microbial metabolic activity, thereby enhancing the accuracy and reliability of MIC endpoints for both fastidious organisms and complex natural products [1].
The INT Colorimetric Assay: Principle and Advantages
The INT (2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride) assay is a colorimetric method used to determine cell viability and metabolic activity. Metabolically active bacteria reduce the colorless, water-soluble INT salt to a red-colored, water-insoluble formazan product [1]. The intensity of the red color is directly proportional to the number of viable cells.
Advantages of the INT assay include:
- Objectivity: Provides a clear, color-based endpoint, reducing the subjectivity associated with visual turbidity assessment [1].
- Sensitivity: Can detect low levels of microbial growth that are not visible to the naked eye [1].
- Quantification: The signal can be measured spectrophotometrically to determine inhibitory concentrations such as IC50% and IC90%, providing data on the potency of antimicrobial compounds [1].
The diagram below illustrates the signaling pathway and workflow for the INT colorimetric MIC assay.
Research Reagent Solutions for Fastidious Organism Testing
The table below outlines essential materials and their specific functions for conducting INT colorimetric MIC assays on fastidious organisms.
Table 1: Essential Research Reagents and Materials
| Item | Function & Application | Key Considerations |
|---|---|---|
| MH-F Broth | Enriched Mueller-Hinton broth for fastidious organisms [4]. Supports growth of streptococci, H. influenzae, etc. | Must be supplemented with lysed horse blood and beta-NAD [4]. |
| INT Solution | Cell viability indicator. Colorless INT is reduced to red formazan by metabolically active bacteria [1]. | Final concentration typically 0.02-0.2 mg/mL. Filter-sterilized before use. |
| Dimethyl Sulfoxide (DMSO) / Polysorbate 80 | Solvent/emulsifier for hydrophobic compounds like essential oils [27]. | Final solvent concentration must be non-inhibitory to bacterial growth (typically ≤1-2% v/v) [27]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standard broth for non-fastidious aerobic bacteria [28] [26]. Used for quality control strains. | Essential for reliable testing of antibiotics like polymyxins [28]. |
| Quality Control Strains | Verifies accuracy and precision of the AST procedure [28] [26]. | Examples: E. coli ATCC 25922, S. aureus ATCC 29213. Must be organism- and antibiotic-specific [28]. |
Quantitative MIC Data for Essential Oils and Antibiotics
The following tables summarize published MIC values for various essential oils and standard antibiotics, providing reference points for assay validation and result interpretation.
Table 2: MIC Values of Selected Essential Oils Against Reference Bacteria
| Plant Source (Essential Oil) | Microorganism | MIC Value | Reference |
|---|---|---|---|
| Cymbopogan citratus (Lemongrass) | Escherichia coli | 0.6 µL/mL | [24] |
| Staphylococcus aureus | 0.6 µL/mL | [24] | |
| Salmonella typhimurium | 2.5 µL/mL | [24] | |
| Thymus vulgaris (Thyme) | Clostridium perfringens | 1.25 mg/mL | [24] |
| Origanum vulgarae (Oregano) | Escherichia coli | 1600–1800 ppm | [24] |
| Staphylococcus aureus | 800–900 ppm | [24] | |
| Cinnamomum zeylanicum (Cinnamon) | Staphylococcus aureus | 0.5 mg/mL | [24] |
| Allium sativum (Garlic) | Escherichia coli | 15–1500 µg/mL | [24] |
Table 3: Example Clinical Breakpoints for Antibiotics (EUCAST)
| Antibiotic | Organism | Susceptible (S) MIC Breakpoint (≤ mg/L) | Resistant (R) MIC Breakpoint (> mg/L) | Reference |
|---|---|---|---|---|
| Ceftazidime | Escherichia coli | 1 mg/L | 4 mg/L | [28] |
| Benzylpenicillin | Streptococcus pneumoniae | 0.06 mg/L | 2 mg/L | [4] |
| Clarithromycin | Helicobacter pylori | 0.25 mg/L | 0.5 mg/L | [25] |
Detailed Experimental Protocols
Protocol 1: Broth Microdilution MIC Assay with INT Endpoint for Fastidious Organisms
This protocol is adapted from EUCAST guidelines and validated colorimetric methods [28] [1] [4].
Day 1: Preparation of Inoculum
- Using a sterile loop, streak the fastidious organism from a frozen stock onto an appropriate enriched agar plate (e.g., chocolate agar). Incubate at 35±1°C in 5% CO₂ for 18-24 hours [28] [26].
- Prepare a bacterial suspension in sterile saline (0.85% NaCl) directly from overnight colonies, adjusting the turbidity to a 0.5 McFarland standard. This results in a suspension of approximately 1-2 x 10⁸ CFU/mL [28] [1].
Day 2: MIC Assay Procedure
- Prepare Antimicrobial Stock Solutions: Dissolve antibiotics in appropriate solvents (e.g., water, methanol). For Essential Oils, prepare a stock solution in a non-inhibitory concentration of DMSO or polysorbate 80 (e.g., 1% v/v) [27].
- Dilution Scheme: In a sterile 96-well microtiter plate, perform two-fold serial dilutions of the antimicrobial agent in MH-F broth [4]. Include a growth control well (MH-F broth + inoculum) and a sterility control well (MH-F broth only).
- Inoculate Plate: Dilute the 0.5 McFarland standard suspension 1:100 in MH-F broth to achieve a final inoculum of ~5 x 10⁵ CFU/mL. Add 100 µL of this standardized inoculum to all test and growth control wells. Add 100 µL of sterile MH-F broth to the sterility control well. The final volume in each test well is 200 µL.
- Incubate: Seal the microtiter plate with a lid and incub at 35±1°C for 16-20 hours under appropriate atmospheric conditions (e.g., 5% CO₂ if required) [26] [4].
- Add INT and Re-incubate: After initial incubation, add 20 µL of a filter-sterilized INT solution (0.125% w/v) to each well. Re-incubate the plate for 1-4 hours [1].
- Determine MIC Endpoint:
- Visual Reading: The MIC is the lowest concentration of the antimicrobial agent that prevents a color change to red. A pink/red color indicates bacterial growth and metabolic activity [1].
- Spectrophotometric Reading: Measure the absorbance at 490 nm using a microplate reader. The MIC is the lowest concentration that results in an optical density (OD) below a predefined threshold (e.g., 90% inhibition compared to the growth control) [1]. This allows for calculation of IC50 and IC90 values.
Protocol 2: Quality Control and Data Interpretation
- Quality Control: Each assay run must include approved quality control (QC) strains with known MIC ranges [28] [26]. Results are valid only if the MIC for the QC strain falls within the accepted reference range.
- Interpretation: For antibiotics, compare the obtained MIC value to the current clinical breakpoints published by EUCAST or CLSI to categorize the isolate as Susceptible (S), Intermediate (I), or Resistant (R) [28]. For essential oils or investigational compounds, the MIC value itself is the primary result, though it can be compared to Epidemiologic Cutoff Values (ECVs) if available [26].
The integration of the INT colorimetric assay into standardized broth microdilution provides a powerful, quantitative tool for screening the efficacy of essential oils and antibiotics against fastidious organisms. This method enhances the objectivity and sensitivity of MIC determinations, facilitating reliable data generation for antimicrobial discovery and resistance surveillance. The protocols outlined herein, utilizing specialized media like MH-F broth, offer researchers a robust framework to advance studies within the broader context of developing novel strategies to combat multidrug-resistant infections.
Step-by-Step Protocol: Developing and Executing a Robust INT Colorimetric MIC Assay
The p-Iodonitroterazolium Chloride (INT) colorimetric assay is a vital tool in microbiological research for rapidly determining the Minimum Inhibitory Concentration (MIC) of antimicrobial agents [29]. The assay functions as a bacterial viability indicator; viable bacteria reduce the yellow, water-soluble INT dye to a pink, water-insoluble formazan product, providing a clear visual or spectrophotometric endpoint for growth [29]. This method is particularly valued for its speed and simplicity compared to traditional broth dilution methods. However, the reliability of the INT assay is critically dependent on the stability of the prepared INT solution. Degradation of the reagent can lead to diminished colorimetric response, resulting in false negatives or an overestimation of antimicrobial activity. This application note details the preparation, storage, and stability testing protocols for INT solution to ensure data integrity within MIC determination research.
Key Research Reagent Solutions
The following table outlines the essential reagents and materials required for the preparation and use of the INT colorimetric assay in MIC studies.
Table 1: Essential Reagents for INT Colorimetric MIC Assays
| Reagent/Material | Function/Description | Application Notes |
|---|---|---|
| p-Iodonitroterazolium Chloride (INT) | Colorimetric viability indicator. Reduced by bacterial dehydrogenases from yellow to pink formazan [29]. | Critical to prepare at specified concentration (e.g., 0.2 µg/mL) [29]. Stability of prepared solution is a key focus of this document. |
| Dimethyl Sulfoxide (DMSO) | Common solvent for preparing stock solutions of antimicrobials or dyes like INT [29]. | Must be tested to ensure no inherent antibacterial activity at concentrations used in the assay [29]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution susceptibility testing [30]. | Provides essential nutrients and controlled ion concentration for reproducible bacterial growth. |
| Resazurin Dye | Alternative colorimetric viability indicator. Reduced from blue to pink [2] [30]. | Used in Resazurin Microplate Assay (REMA); serves as a comparative method for INT [2] [30]. |
| Dey-Engley (D/E) Neutralizer Broth | Growth medium containing neutralizing agents to inactivate disinfectants/antiseptics during testing [2]. | Contains bromcresol purple as a pH-based colorimetric indicator for bacterial growth [2]. |
INT Solution Preparation and Quality Control
Stock Solution Preparation Protocol
A standardized protocol is essential for consistent and reliable INT assay performance.
- Step 1: Weighing. Accurately weigh the required mass of INT powder to prepare a 0.02% (w/v) stock solution (e.g., 0.02 g in 100 mL of solvent) [30].
- Step 2: Reconstitution. Dissolve the INT powder in an appropriate sterile solvent, such as deionized water or phosphate-buffered saline (PBS). The Resazurin protocol suggests sterile filtration for sterilization [30].
- Step 3: Sterilization. Sterilize the prepared 0.02% INT stock solution by passing it through a 0.22 µm membrane filter into a sterile container [30]. This step is critical to prevent microbial contamination.
- Step 4: Aliquoting. Dispense the sterile stock solution into single-use, light-protected vials (e.g., amber vials) to minimize freeze-thaw cycles and light exposure.
Working Solution Preparation
- The stock solution is typically diluted for use in assays. The referenced protocol uses a final concentration of 0.2 µg/mL, which is achieved by adding 50 µL of the 0.02% stock to the test well [29].
Initial Quality Control Assessment
- Positive Control: Validate each new batch of INT solution by testing with a known viable bacterial strain (e.g., E. coli ATCC 25922). A distinct color change from yellow to pink within the expected incubation time confirms reagent functionality [29] [30].
- Negative Control: Include a sterility control well (broth and INT without bacteria) to confirm the reagent itself does not change color, indicating absence of contamination or auto-reduction.
Stability Storage and Testing Protocols
Recommended Storage Conditions
Based on general practices for critical laboratory reagents and stability guidelines, the following storage conditions are recommended for INT solutions.
Table 2: Recommended Storage Conditions for INT Solutions
| Solution Type | Short-Term Storage | Long-Term Storage | Container | Documentation |
|---|---|---|---|---|
| INT Working Solution | 4°C (refrigerator), protected from light for up to 24 hours. |
Not recommended. Prepare fresh from stock for each assay. | Sterile, light-protected microcentrifuge tubes. | Label with preparation date, time, and initials. |
| INT Stock Solution (0.02%) | Not recommended for extended periods. | -20°C or lower, protected from light [30]. |
Small, sterile aliquots in amber vials. | Label with reagent name, concentration, date prepared, and expiration date. |
Stability storage involves placing samples in controlled environments to determine how their quality varies with time under factors like temperature and light [31]. For a light-sensitive reagent like INT, photostability is a key concern. ICH guidelines recommend testing under exaggerated light conditions to establish appropriate handling and storage protocols [31].
Forced Degradation Study Protocol
Forced degradation studies provide knowledge about the degradation chemistry of a substance, which is used to develop stability-indicating methods [31]. This protocol helps establish the stability profile of INT solution.
- Objective: To determine the intrinsic stability of INT solution by subjecting it to stress conditions and evaluating its physical and functional integrity.
- Materials:
- Method:
- Aliquot Preparation: Dispense INT solution into multiple aliquots.
- Stress Application:
- Thermal Stress: Store aliquots at
40°Cand60°C[32]. - Photostress: Expose one aliquot to at least 1.2 million lux hours of visible light and 200-watt hours per square meter of UV energy in a light cabinet [31].
- Control: Maintain a control aliquot at the recommended long-term storage condition (
-20°C, dark).
- Thermal Stress: Store aliquots at
- Sampling and Analysis: At predetermined intervals (e.g., 24h, 72h, 1 week), retrieve aliquots for testing.
- Physical Inspection: Note any color change or precipitation.
- Functional QC: Perform the standard INT assay against the QC strain alongside a fresh INT solution control. Compare the color development time and intensity.
- Acceptance Criteria: The stressed INT solution is considered stable if it produces a functional response (color change) equivalent to the control within one doubling dilution in the MIC assay.
Real-Time Stability Study Protocol
Long-term stability testing determines the re-test period or shelf life under recommended storage conditions [31] [33].
- Objective: To establish the shelf-life of the INT stock solution by monitoring its performance over time under recommended storage conditions (
-20°C, dark). - Method:
- Study Design: Prepare multiple aliquots from a single, master batch of 0.02% INT stock solution.
- Storage: Store all aliquots at
-20°Cin the dark. - Testing Schedule: Pull aliquots at predefined time points (e.g., initial, 1, 3, 6, 9, 12 months) for functional QC testing against a standard strain.
- Data Recording: Document the physical appearance and the results of the functional QC assay at each interval.
- Defining Shelf-Life: The shelf-life is the period during which the INT solution consistently meets all acceptance criteria (physical and functional) compared to a fresh control.
Experimental Workflow for INT Stability Assessment
The following diagram illustrates the logical workflow for preparing the INT solution and conducting stability assessments to ensure its reliability in the MIC assay.
INT Solution Stability Assessment Workflow
Data Presentation and Analysis
The following table summarizes hypothetical data from a comprehensive stability study, illustrating how to document and analyze the results.
Table 3: Example Data from a Comprehensive INT Solution Stability Study
| Storage Condition | Time Point | Physical Appearance | Functional QC Result | MIC Correlation with Fresh Control | Conclusion |
|---|---|---|---|---|---|
Recommended (-20°C, dark) |
Initial | Clear, yellow | Pass | Essential Agreement: 100% | Suitable for use |
| 6 Months | Clear, yellow | Pass | Essential Agreement: 100% | Suitable for use | |
| 12 Months | Clear, yellow | Pass | Essential Agreement: 100% | Suitable for use | |
Accelerated (40°C, dark) |
2 Weeks | Slight darkening | Pass | Essential Agreement: 100% | Stable under short-term stress |
| 4 Weeks | Noticeable darkening | Fail (No color change) | Essential Agreement: 0% | Degradation evident | |
| Photostress (ICH Q1B) | 24 Hours | Faded yellow | Fail (Weak color change) | Essential Agreement: ≤50% | Highly light-sensitive |
Adherence to the detailed protocols for preparation, storage, and systematic stability testing of INT solution, as outlined in this application note, is fundamental for ensuring the generation of reliable and reproducible data in MIC determination research. Establishing a defined shelf-life through real-time studies and understanding the reagent's vulnerabilities via forced degradation minimizes experimental variability. Proper handling of this critical reagent, characterized by sterile aliquoting, light-protected storage at -20°C, and rigorous quality control, directly supports the integrity of antimicrobial efficacy studies and the broader fight against antimicrobial resistance.
Broth microdilution is the reference method for determining the Minimum Inhibitory Concentration (MIC) of antimicrobial substances, providing both quantitative and qualitative assessment of antimicrobial efficacy. The accuracy and reproducibility of this method fundamentally depend on precise inoculum preparation and standardization. This protocol details the optimized procedures for preparing a standardized bacterial inoculum specifically for broth microdilution MIC assays, with particular emphasis on integration with colorimetric endpoint detection. Adherence to this standardized methodology ensures reliable, reproducible results essential for research and drug development applications.
In antimicrobial susceptibility testing, the minimum inhibitory concentration (MIC) is defined as the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism [28]. The broth microdilution method, performed in 96-well plates, has become the gold standard for MIC determination in both clinical and research settings due to its quantitative nature, reproducibility, and capacity for high-throughput analysis [20] [28]. This method's reliability, however, is critically dependent on strict standardization of the bacterial inoculum used in the assay.
The preparation of a correct inoculum density is not merely a procedural step but a fundamental determinant of assay validity. An excessively heavy inoculum may lead to falsely elevated MIC values, suggesting resistance, while an overly light inoculum can result in artificially low MICs, indicating false susceptibility [34]. Furthermore, the move towards colorimetric assays, which use oxidation-reduction indicators like INT to provide a visual or spectrophotometric signal of microbial growth, demands even greater precision in inoculum preparation to ensure accurate and objective endpoint determination [35] [36].
This application note provides a detailed, step-by-step protocol for inoculum preparation and standardization, aligned with guidelines from the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [4] [28] and the Clinical and Laboratory Standards Institute (CLSI) [36]. The procedures are contextualized for research aimed at developing and optimizing colorimetric MIC assays.
Experimental Workflow
The following diagram illustrates the complete workflow for broth microdilution MIC determination, highlighting the critical stages of inoculum preparation.
Materials and Reagents
Research Reagent Solutions
Table 1: Essential materials and reagents for broth microdilution inoculum preparation.
| Item | Function/Description | Key Considerations |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standard growth medium for non-fastidious aerobic bacteria [28]. | For fastidious organisms, use supplemented broth (e.g., MH-F broth) [4]. |
| Sterile 0.85% Saline Solution | Diluent for adjusting bacterial suspension turbidity and performing serial dilutions [28]. | Must be isotonic to prevent osmotic shock to bacterial cells. |
| McFarland Turbidity Standards | Reference for standardizing the density of the bacterial inoculum [34]. | The 0.5 McFarland standard is equivalent to ~1-2 x 10⁸ CFU/mL for E. coli [34]. |
| 96-Well Microtiter Plate | Platform for broth microdilution assay. | Use sterile, U-bottom or flat-bottom plates compatible with plate readers [37]. |
| Antimicrobial Agent Stock Solutions | Source of the antimicrobial compound being tested. | Prepare at high concentration (e.g., 1000 µg/mL or 10x the highest test concentration) [34]. Filter-sterilize and store at ≤ -20°C. |
| INT or other Colorimetric Reagent | Oxidation-reduction indicator for visual growth detection. | Added post-incubation or incorporated into the medium. Turns from yellow to pink/red in the presence of microbial growth [35]. |
Protocol: Inoculum Preparation and Standardization
Preparation of Overnight Culture
- Day 1: Using a sterile inoculation loop, pick 3-5 well-isolated colonies from a fresh (18-24 hour) agar plate culture.
- Transfer the colonies into a tube containing 4-5 mL of appropriate broth medium (e.g., Mueller Hinton Broth).
- Incubate the broth culture for 16-20 hours at 35±2°C under ambient air with constant agitation at 220 RPM [28].
Standardization of Inoculum Density
- Day 2: Vortex the overnight culture thoroughly to ensure a homogeneous suspension.
- Transfer a portion of the culture to a sterile tube or cuvette.
- Adjust the turbidity of the suspension to match that of a 0.5 McFarland standard. This results in a suspension containing approximately 1-2 x 10⁸ CFU/mL for organisms like Escherichia coli [34] [28].
- Comparison can be performed visually against a McFarland card with contrasting lines or using a densitometer for greater precision.
- This standardized suspension must be used within 15-30 minutes of preparation to prevent significant changes in viable count [34].
Preparation of Working Inoculum
- Perform a 1:150 dilution of the adjusted 0.5 McFarland suspension in sterile saline or broth [34] [28].
- This dilution factor is critical and yields a working inoculum concentration of approximately 1 x 10⁶ CFU/mL.
- When this working inoculum is added to the microtiter plate (typically in a 1:1 ratio with the broth/antibiotic solution), the final bacterial density in each test well becomes approximately 5 x 10⁵ CFU/mL, which is the target specified by EUCAST and CLSI guidelines [28] [36].
Inoculation of Microtiter Plate
- Add 100 µL of the working inoculum (from step 4.3) to each well of the microtiter plate containing 100 µL of the serial antibiotic dilutions [34] [37].
- This step results in the desired 1:2 final dilution of both the antibiotic and the inoculum, achieving the target test concentration of ~5 x 10⁵ CFU/mL.
- Include appropriate controls in the plate layout:
- Growth Control Well: Broth + inoculum (no antibiotic).
- Sterility Control Well: Broth only (no inoculum, no antibiotic).
Enumeration of Colony Forming Units (CFU)
To validate the entire process, the actual inoculum density must be verified by colony counting.
Table 2: Colony Count Enumeration for Inoculum Verification.
| Step | Procedure | Target CFU/mL |
|---|---|---|
| 1. Serial Dilution | Perform a logarithmic serial dilution (10⁻¹ to 10⁻⁶) of the standardized 0.5 McFarland suspension in sterile saline [28]. | N/A |
| 2. Plating | Plate 20 µL spots from each dilution onto non-selective agar plates, in triplicate [28]. Alternatively, spread 100 µL of a 10⁻⁵ dilution. | N/A |
| 3. Incubation & Counting | Incubate plates for 18-24 hours. Count the colonies on plates with 30-300 colonies. Calculate the CFU/mL of the original suspension. | ~1-2 x 10⁸ CFU/mL for the 0.5 McFarland standard. ~5 x 10⁵ CFU/mL in the final test well. |
Quality Control and Troubleshooting
Rigorous quality control is essential for reliable MIC data. The following table outlines common issues and solutions related to inoculum preparation.
Table 3: Troubleshooting Guide for Inoculum-Related Issues.
| Problem | Potential Consequence | Corrective Action |
|---|---|---|
| Inconsistent MICs between replicates | Poor reproducibility, unreliable data. | Ensure thorough vortexing of the culture before standardization. Use the inoculum within the recommended 30-minute window [34]. |
| MICs consistently too high | False indication of resistance. | Likely due to an overly heavy inoculum. Verify the McFarland standard preparation and turbidity adjustment method. Confirm dilution calculations [34]. |
| MICs consistently too low | False indication of susceptibility. | Likely due to an overly light inoculum. Check the viability of the culture and ensure the incubation time is not exceeded. Confirm dilution calculations [34]. |
| Skipped wells or uneven growth | Inability to determine a clear MIC endpoint. | Check for contamination. Ensure the inoculum is mixed adequately before pipetting into the plate [34]. |
| Poor color development in colorimetric assays | Ambiguous or false-negative MIC reading. | Confirm the inoculum viability via CFU plating. Ensure the colorimetric reagent is fresh and compatible with the test organism and medium [35]. |
Use of Quality Control Strains
To ensure the entire test system is performing within specified limits, include quality control (QC) strains with known MIC ranges in each assay run. Recommended strains include [34] [28]:
- Escherichia coli ATCC 25922
- Staphylococcus aureus ATCC 29213
- Pseudomonas aeruginosa ATCC 27853
The MIC values obtained for these QC strains must fall within the published acceptable ranges for the test to be considered valid [28].
Integration with Colorimetric MIC Determination
The standardized inoculum protocol is perfectly suited for colorimetric MIC assays. After the standard incubation period (16-20 hours), a metabolically active inoculum will interact predictably with colorimetric reagents:
- Principle: Viable bacteria reduce the tetrazolium salt (INT), which changes from yellow to a visible pink or red formazan product [35] [36].
- Endpoint Determination: The MIC is read as the lowest concentration of antibiotic where the color change is absent, indicating inhibition of metabolic activity. This provides an objective, visual endpoint that can also be quantified using a plate reader [35].
- Advantage: A properly standardized inoculum ensures that the metabolic signal is strong enough to be detected, thereby increasing the accuracy and reliability of the colorimetric readout compared to subjective turbidity assessment.
The INT colorimetric assay is a vital tool in modern antimicrobial susceptibility testing, enabling the precise determination of the Minimum Inhibitory Concentration (MIC) of novel compounds. This method leverages the metabolic activity of viable microorganisms to reduce the pale yellow, water-soluble 2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride (INT) to a dark red, water-insoluble formazan product [1]. The ensuing color change provides a clear, quantifiable visual or spectrophotometric endpoint, circumventing the subjectivity associated with traditional turbidity measurements [38] [1]. This application note details a standardized and validated protocol for performing the INT colorimetric microdilution assay, designed to provide researchers with a robust framework for generating reliable and reproducible MIC, IC50%, and IC90% data within the broader context of antimicrobial drug discovery.
Materials and Reagents
Research Reagent Solutions
The following table lists the essential materials required for the successful execution of the INT colorimetric assay.
Table 1: Essential Reagents and Materials for the INT Colorimetric MIC Assay
| Item | Function/Description | Application Notes |
|---|---|---|
| 2,3,5-triphenyltetrazolium chloride (TTC) / INT | Colorimetric viability indicator; reduced by metabolically active cells to a red formazan product [1]. | INT is cited as a common tetrazolium salt for this purpose [1]. The solution is prepared at 0.125% (w/v) in water [38]. |
| Cation-adjusted Mueller Hinton Broth (CAMHB) | Standardized culture medium for bacterial growth [1]. | Used for bacteria (S. aureus, E. coli, P. aeruginosa). |
| Sabouraud Dextrose Broth | Culture medium optimized for yeast growth [1]. | Used for the yeast C. albicans. |
| Sterile 96-well Microtiter Plates | Platform for the microdilution assay. | Allows for testing of multiple compound concentrations and controls simultaneously, saving reagents [38]. |
| Dey-Engley (D/E) Neutralizing Broth | Formulated to inactivate common disinfectants and antiseptics in the test sample [2]. | Contains bromcresol purple as a pH indicator; color change to yellow indicates bacterial growth [2]. Critical for testing compounds like povidone-iodine [2]. |
| Dimethyl Sulfoxide (DMSO) | Solvent for dissolving hydrophobic antimicrobial compounds. | Final concentration in the assay should be ≤1% to avoid antimicrobial effects on the test organisms. |
| Sterile Physiological Saline (0.85-0.90% NaCl) | Diluent for adjusting microbial inoculum density. | - |
Experimental Protocol
Preparation of Inoculum
- Subculture: From fresh stock cultures (20-24 hours old), subculture the test microorganisms—Staphylococcus aureus (ATCC 6538), Escherichia coli (ATCC 8739), Pseudomonas aeruginosa (ATCC 9027), or Candida albicans (ATCC 10231)—onto the appropriate solid agar media [1].
- Suspension: Harvest colonies and prepare a suspension in sterile saline or broth.
- Standardization: Adjust the turbidity of the microbial suspension to match a 0.5 McFarland standard, which equates to approximately 1-5 x 10^8 CFU/mL for bacteria and 1-5 x 10^6 CFU/mL for C. albicans [1].
- Dilution: Further dilute the standardized suspension in the appropriate broth (CAMHB or Sabouraud) to achieve a working concentration that will deliver a final inoculum of approximately 5 x 10^5 CFU/mL per well in the microtiter plate [1].
Plate Inoculation and Setup
- Compound Dilution: In a sterile 96-well microtiter plate, prepare a two-fold serial dilution of the antimicrobial compound directly in the culture broth (100 µL final volume per well). The first well typically contains the highest concentration, with decreasing concentrations in subsequent wells [38] [1].
- Inoculation: Add 10 µL of the prepared standardized inoculum to all test wells and growth control wells [1].
- Controls: Include the following controls on each plate:
- Growth Control: Wells containing broth and inoculum only (no antimicrobial compound).
- Sterility Control: Wells containing broth only (no inoculum, no compound).
- Compound Control (Optional): Wells containing the highest concentration of the compound in broth (no inoculum) to confirm the compound does not cause interference in the colorimetric reading.
Incubation Parameters
- Orientation: Incubate the microtiter plates in an inverted position (agar up) to prevent condensation from dripping onto the agar surface and disrupting the microbial growth [39].
- Temperature and Duration: Incubate the plates at 35 ± 2 °C for a period of 22 hours [38] [1]. Incubating below human body temperature (30°C or lower) reduces the risk of cultivating human pathogens [39].
- Atmosphere: Incubate under aerobic conditions. Plates should not be completely sealed; instead, secure the lid with 2-4 short strips of adhesive tape at opposite edges to prevent accidental opening while allowing oxygen diffusion [39].
Colorimetric Development and Reading
- INT Addition: After the 22-hour incubation period, add 20 µL of 0.125% (w/v) INT solution to each well [38] [1].
- Secondary Incubation: Return the plates to the incubator for an additional 2 hours at 35 °C to allow for color development [38].
- Endpoint Determination:
- Visual Reading: The MIC is defined as the lowest concentration of the antimicrobial compound that prevents a color change from yellow to dark red. A clear well indicates no microbial growth and full inhibition [1].
- Spectrophotometric Reading: For quantitative determination of IC50% and IC90%, measure the absorbance of the formazan product at a suitable wavelength (e.g., 490-540 nm) using a microplate reader. The absorbance is directly proportional to the quantity of viable cells [38] [1].
Diagram 1: INT colorimetric MIC assay workflow
Data Interpretation and Analysis
Defining Key Metrics
The validated colorimetric method allows for the conversion of absorbance values into quantitative measures of antimicrobial potency [38].
Table 2: Key Quantitative Metrics in Antimicrobial Susceptibility Testing
| Metric | Definition | Interpretation |
|---|---|---|
| Minimum Inhibitory Concentration (MIC) | The lowest concentration of an antimicrobial agent that visually inhibits the growth of a microorganism (prevents color change to red) [38] [1]. | A lower MIC indicates greater potency of the antimicrobial agent against the test organism. |
| Half-Maximal Inhibitory Concentration (IC50%) | The concentration of an antimicrobial that reduces the microbial growth (as measured by formazan absorbance) by 50% compared to the growth control [38]. | Provides a quantitative measure of compound potency, useful for comparing different agents. |
| 90% Inhibitory Concentration (IC90%) | The concentration of an antimicrobial that reduces the microbial growth by 90% compared to the growth control [38]. | Indicates the concentration required for near-complete inhibition of the microbial population. |
Method Validation Parameters
The INT colorimetric microdilution assay should be validated to ensure data reliability. Key validation parameters include [38]:
- Linearity: A coefficient of determination (R²) greater than 0.95 confirms a direct correlation between absorbance and viable microbial concentration (CFU mL⁻¹).
- Precision: A relative standard deviation (RSD) of less than 26% demonstrates acceptable repeatability.
- Accuracy: Recovery rates between 75% and 122% ensure the method yields results close to the true value.
Troubleshooting and Best Practices
Table 3: Common Issues and Resolution Strategies in the INT Assay
| Issue | Potential Cause | Recommended Solution |
|---|---|---|
| No color change in growth control wells. | Non-viable inoculum, incorrect incubation temperature, INT solution degradation. | Check inoculum viability on agar plates, verify incubator temperature, prepare fresh INT solution [1]. |
| Excessive or rapid color development. | Inoculum concentration too high. | Re-standardize the inoculum to the 0.5 McFarland standard and verify dilution factors [1]. |
| Color development in sterility control. | Contamination of reagents or plates. | Use sterile technique, ensure all reagents and equipment are sterile. |
| High background in compound control wells. | Compound interference with the INT dye. | Include a neutralization step (e.g., using D/E Neutralizing Broth) for colored or reactive compounds like povidone-iodine [2]. |
| Poor reproducibility between replicates. | Inconsistent pipetting or inoculum preparation. | Use calibrated pipettes and ensure the inoculum is a homogeneous suspension before transfer. |
Colorimetric assays are fundamental tools in biological research and drug development, providing a means to quantify biological and chemical reactions through visual color changes or spectrophotometric analysis. These assays are particularly valuable in determining the Minimum Inhibitory Concentration (MIC) of antimicrobial agents, a critical parameter in pharmaceutical development and microbiology. The core principle relies on the measurement of light absorbance by a colored compound, the formation of which is directly proportional to the concentration of the analyte or the activity of a biological system [40]. This document provides detailed application notes and protocols for implementing colorimetric detection within the context of INT colorimetric assay-based MIC determination, enabling researchers to accurately assess microbial viability and metabolic activity.
Core Principles and Assay Configuration
Colorimetric detection functions by establishing a direct relationship between the concentration of an analyte in a solution and its light absorbance at a specific wavelength, as described by Beer's Law [40]. In the specific context of INT (2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride) assays for MIC determination, the fundamental mechanism involves the enzymatic reduction of the nearly colorless INT substrate to a brightly colored, pink-red formazan product by metabolically active microbial cells [41]. The intensity of the resulting color is therefore directly proportional to the number of viable, metabolically active cells present, providing a quantitative measure of cell proliferation or, conversely, the inhibitory effects of antimicrobial compounds.
Proper configuration of the assay is essential for accurate results. This involves selecting appropriate wavelengths, preparing a standard curve, and understanding the limits of detection. The standard curve is a critical component, transforming raw absorbance values into meaningful concentration data [40].
Table 1: Key Configuration Parameters for INT-MIC Colorimetric Assay
| Parameter | Description | Typical Configuration for INT-MIC |
|---|---|---|
| Detection Principle | Measurement of formazan dye produced by microbial reduction of INT | Metabolic activity of viable cells [41] |
| Primary Wavelength | Absorbance maximum for the formazan product | 490 nm (recommended optimization) |
| Standard Curve | Plot of absorbance vs. known cell count or metabolic standard | Essential for quantification [40] |
| Linear Range | The range of analyte concentration where absorbance is linearly proportional | Must be determined empirically for each microbe |
| Limit of Detection (LOD) | The lowest analyte concentration that can be reliably detected | Must be established [40] |
Research Reagent Solutions and Essential Materials
A successful INT-MIC assay requires specific reagents and materials to ensure consistency, accuracy, and reproducibility. The following toolkit details the core components.
Table 2: Essential Research Reagent Solutions and Materials for INT-MIC Assay
| Item | Function/Description | Application Note |
|---|---|---|
| INT Solution | Tetrazolium salt substrate; reduced by active microbial dehydrogenases to pink-red formazan. | Prepare fresh or store frozen aliquots; final concentration must be optimized for specific microorganisms. |
| Test Compound/ Drug | The antimicrobial agent for which the MIC is being determined. | Serially diluted in a suitable solvent that does not inhibit microbial growth. |
| Microbial Inoculum | Standardized suspension of the target microorganism. | Adjust to a specific density (e.g., 0.5 McFarland) for consistent baseline metabolic activity. |
| Growth Medium | Culture medium supporting microbial growth. | Must be compatible with both the microbe and the colorimetric reaction (e.g., phenol-red free). |
| Positive Control | Medium with microbial inoculum but no drug. | Represents 100% metabolic activity. |
| Negative Control | Medium without inoculum. | Accounts for background absorbance of the medium and reagents. |
| Spectrophotometer/ Microplate Reader | Instrument for measuring absorbance of the formazan product. | Must be capable of reading at the appropriate wavelength (e.g., 490 nm). |
| 96-well Microtiter Plate | Platform for conducting the assay with drug dilutions and replicates. | Flat-bottom plates are ideal for absorbance measurements [42]. |
Experimental Protocol for INT-MIC Determination
The following diagram illustrates the logical workflow for the INT-MIC determination assay, from preparation to data analysis.
Detailed Step-by-Step Methodology
Step 1: Preparation of Drug Dilutions Prepare a stock solution of the test antimicrobial agent. Using a 96-well microtiter plate, perform a two-fold serial dilution of the drug in the appropriate growth medium. A typical range is from 128 µg/mL to 0.125 µg/mL or wider, depending on the expected potency. Each concentration should be tested in duplicate or triplicate.
Step 2: Inoculation Prepare a standardized suspension of the target microorganism (e.g., bacteria or yeast) in growth medium, typically adjusted to a 0.5 McFarland standard. Add a consistent volume of this inoculum to all test wells and control wells, ensuring a final cell density that is within the linear range of the assay (e.g., ~1 x 10^5 CFU/mL for bacteria). The positive control wells receive inoculum but no drug, while the negative control wells receive medium only.
Step 3: Initial Incubation Incubate the sealed microtiter plate under optimal conditions for the microorganism (e.g., 35±2°C for 18-24 hours for most bacteria). This allows the drug to interact with the growing cells.
Step 4: Addition of INT Substrate After the initial incubation, add a predetermined volume of INT solution to each well. The final concentration of INT must be optimized in preliminary experiments to provide a clear signal without being toxic to the cells. Gently mix the plate.
Step 5: Secondary Incubation and Color Development Re-incubate the plate for a shorter period (e.g., 1-4 hours) to allow for the metabolic conversion of INT to formazan. The development of a pink-red color indicates metabolic activity.
Step 6: Spectrophotometric Reading and Visual Interpretation Shake the plate gently to ensure homogeneity and read the absorbance at 490 nm using a microplate reader. The MIC is determined spectrophotometrically as the lowest drug concentration that results in a pre-defined reduction (e.g., ≥90%) in absorbance compared to the positive control. Simultaneously, the MIC can be determined visually as the lowest drug concentration that shows no visible pink color (indicating complete inhibition of metabolic activity) [41].
Data Analysis and Interpretation
Analysis Pathway
The data analysis process involves transforming raw absorbance data into a reliable MIC value, as shown in the following pathway.
Advanced and Alternative Detection Modalities
While traditional spectrophotometry is the gold standard, recent technological advances offer complementary and highly accessible detection methods.
Smartphone-Based Colorimetric Analysis Smartphones can be powerful tools for colorimetric detection, serving as portable, cost-effective analytical devices. The general operation flow involves colorimetric transduction (the chemical reaction producing color), image capture (using the smartphone camera, often with accessories to control lighting), and data processing (using embedded applications to analyze color values in RGB, HSV, or CIE LAB* color spaces) [42]. This method can achieve a high degree of precision and a low limit of detection (LOD), making it suitable for point-of-care testing and field applications [42] [43].
Nanoparticle-Based Detection Functionalized gold nanoparticles (AuNPs) represent another advanced colorimetric platform. Well-dispersed AuNPs solutions are red, but they undergo a visible color shift to blue upon aggregation, which can be induced by the presence of a target analyte. This principle has been successfully used to detect various ions and molecules with high sensitivity, as the aggregation causes a shift in the surface plasmon resonance band [43]. Such systems can be integrated with smartphone-based digital image analysis for quantitative results.
Table 3: Comparison of Colorimetric Detection Modalities
| Detection Modality | Principle | Advantages | Considerations for INT-MIC |
|---|---|---|---|
| Spectrophotometry | Measures light absorbance at a specific wavelength (490 nm for formazan). | High precision, quantitative, well-established. | Requires access to a plate reader. |
| Visual Interpretation | Direct observation of color change (pink/red) by the human eye. | Rapid, no equipment needed, excellent for initial screening. | Subjective; limited to qualitative/semi-quantitative data. |
| Smartphone Analysis | Uses phone camera and app to quantify color intensity in various color spaces. | Portable, accessible, can improve objectivity over visual inspection. | Requires standardization of lighting and camera settings [42]. |
The minimum inhibitory concentration (MIC) is defined as the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism [44]. Its accurate determination is critical in both clinical and research settings for guiding patient therapy, studying resistance mechanisms, and evaluating novel antimicrobial candidates [44]. Colorimetric MIC assays utilize biochemical indicators that undergo a visible color change in response to microbial metabolic activity. These assays provide a robust, quantitative alternative to traditional visual turbidity assessments, enabling more precise and objective endpoint determination [45].
The underlying principle of these assays involves the use of tetrazolium salts, such as INT (Iodonitrotetrazolium) or XTT, which are cleaved by active microbial dehydrogenase enzymes. This reduction process transforms the colorless or lightly-colored tetrazolium compound into a intensely colored formazan product [45]. The resulting color development in a well indicates active microbial growth, while a clear well (the "clear-well endpoint") signifies complete inhibition of metabolic activity at that antimicrobial concentration. This colorimetric change provides a clear, measurable signal for MIC determination, often correlating excellently with standardized reference methods [45].
Key Reagents and Materials
Successful execution of a colorimetric MIC assay requires specific reagents and equipment to ensure standardized and reproducible results. The core components are listed in the table below.
Table 1: Essential Research Reagent Solutions and Materials for Colorimetric MIC Assays
| Item | Function/Description |
|---|---|
| Tetrazolium Salt (e.g., INT) | A colorless substrate that is reduced by microbial dehydrogenases to a colored formazan product, serving as the colorimetric indicator for metabolic activity [45]. |
| RPMI 1640 Medium | A standardized growth medium buffered with MOPS, commonly used for susceptibility testing of fungi and other fastidious organisms to support spore germination and growth [45] [46]. |
| Mueller-Hinton Broth (MHB) | The recommended medium for routine broth dilution antibacterial susceptibility testing for non-fastidious organisms [44]. |
| Cation-Adjusted MHB | A specially prepared MHB used for testing certain antibiotics like polymyxins (e.g., colistin), where cation concentrations can significantly impact the MIC result [44]. |
| Antimicrobial Stock Solutions | Serial two-fold dilutions of the antimicrobial agent being tested, prepared from a high-concentration stock solution [44]. |
| Inoculum Standardization | A saline suspension of the test organism, standardized to a specific density (e.g., 0.5 McFarland standard, equating to ~1-5 x 10^8 CFU/mL for bacteria) and then further diluted in broth to the final testing concentration [44]. |
| Flat-Bottom Microtiter Plates | Plates used for broth microdilution assays. Flat-bottom wells are often specified for facilitating optical density reading and biofilm assays [45] [46]. |
| Microplate Spectrophotometer | An instrument capable of measuring absorbance at specific wavelengths (e.g., 490 nm for XTT-formazan) for quantitative endpoint determination [45]. |
Experimental Protocol: Broth Microdilution with INT
This protocol outlines the steps for performing a broth microdilution MIC assay using INT as the colorimetric indicator, adapted from standardized guidelines [44] [46].
Preparation Phase (Day 1)
- Antimicrobial Solution Preparation: Prepare a stock solution of the antimicrobial agent at a concentration significantly higher than the highest concentration to be tested. Using a serial two-fold dilution scheme, create a dilution series in a sterile tube or directly in the first column of a sterile, flat-bottom 96-well microtiter plate. Common final testing concentrations range from 0.06 µg/mL to 128 µg/mL.
- Inoculum Preparation:
- Subculture the test microbial strain at least twice on appropriate solid agar to ensure purity and viability [46].
- Using a sterile loop, select several colonies and suspend them in sterile saline (0.85% w/v).
- Adjust the turbidity of the suspension to match a 0.5 McFarland standard, which equates to approximately 1-5 x 10^8 Colony Forming Units (CFU)/mL for bacteria [44].
- Further dilute this suspension in the appropriate broth (e.g., RPMI 1640 or Mueller-Hinton) to achieve a final working inoculum of approximately 5 x 10^5 CFU/mL [44].
Assay Inoculation and Incubation (Day 1)
- Plate Setup: The final assay volume in each well is typically 100 µL or 200 µL. The layout should include:
- Test Wells: Containing antimicrobial dilution + inoculum.
- Growth Control Well: Containing only inoculum + broth (no antimicrobial).
- Sterility Control Well: Containing only broth (no antimicrobial, no inoculum).
- Inoculation: Transfer the standardized inoculum into all test wells and the growth control well. Add sterile broth to the sterility control well.
- Incubation: Seal the microtiter plate with a lid or adhesive film and incubate under conditions optimal for the test organism (e.g., 35±2°C for 16-20 hours for non-fastidious bacteria) [44].
Colorimetric Development and Reading (Day 2)
- INT Solution Preparation: Following incubation, prepare a fresh solution of INT. A common working concentration is 0.2 mg/mL in sterile phosphate-buffered saline (PBS) [45].
- Indicator Addition: Add a small volume of the INT solution (e.g., 10-20 µL per 100 µL of broth) to every well of the plate, including the controls.
- Secondary Incubation: Re-incubate the plate for 1-4 hours, protected from light, to allow for color development. The duration may require optimization based on the organism's metabolic rate.
- Endpoint Determination: Visually inspect the plate or read the absorbance using a microplate spectrophotometer at 490 nm.
- A color change to red/pink indicates microbial reduction of INT to formazan, signifying metabolic activity and growth.
- A clear, colorless well indicates a lack of metabolic activity and inhibition of growth.
The workflow for this protocol is detailed in the diagram below.
Data Interpretation and Establishing the MIC
Defining the Clear-Well Endpoint
The fundamental principle of MIC determination is to identify the lowest antimicrobial concentration that produces a clear well after the color development step. This "clear-well endpoint" corresponds to the minimum concentration that inhibits microbial metabolic activity beyond the threshold detectable by the INT reduction assay.
Data interpretation should follow a systematic approach:
- Validate Controls: The growth control well must show a clear color change (e.g., red/pink for INT), confirming adequate microbial viability and assay functionality. The sterility control must remain colorless, confirming the absence of contamination.
- Read the Test Wells: Examine the wells containing the antimicrobial agent from the lowest to the highest concentration.
- Identify the MIC: The MIC is recorded as the concentration of the first well in the dilution series that remains completely colorless after the designated incubation period with INT. The well immediately before this clear well will typically show a visible color change, indicating growth.
Quantitative Data and QC Considerations
For higher precision, spectrophotometric reading is preferred. The absorbance data can be used to generate a plot of metabolic activity (absorbance) versus antimicrobial concentration. The MIC can be determined from the intersection of the baseline noise level and the growth curve, or defined as the concentration that produces a 90% reduction in absorbance (MIC90) compared to the growth control [45].
To ensure reliability, testing should include quality control (QC) strains with known and stable MIC ranges for the antimicrobials being tested [44]. Furthermore, for research purposes, it is recommended to perform assays in biological triplicate (on different days) to ensure reproducibility [44]. The table below summarizes a sample data set and its interpretation.
Table 2: Sample Data and MIC Interpretation from a Colorimetric INT Assay
| Well Number | Antimicrobial Concentration (µg/mL) | Visual Color (Post-INT) | Absorbance (490 nm) | Interpretation |
|---|---|---|---|---|
| Growth Control | 0 | Red | 0.85 | Growth |
| 1 | 0.5 | Red | 0.78 | Growth |
| 2 | 1 | Red | 0.71 | Growth |
| 3 | 2 | Faint Pink | 0.15 | Growth (Partial Inhibition) |
| 4 | 4 | Colorless | 0.05 | No Growth (MIC = 4 µg/mL) |
| 5 | 8 | Colorless | 0.04 | No Growth |
| 6 | 16 | Colorless | 0.04 | No Growth |
| Sterility Control | 0 | Colorless | 0.03 | Sterile |
Troubleshooting and Methodological Considerations
Several factors can influence the outcome and reliability of colorimetric MIC assays. Key considerations and potential solutions are outlined below.
- Inoculum Density Effect: An inoculum that is too dense can lead to falsely elevated MICs, as a higher microbial load may require a higher drug concentration for inhibition. Conversely, a light inoculum may result in falsely low MICs. Adherence to standardized inoculum preparation is critical [44] [46].
- Incubation Time: The optimal incubation time before adding INT is organism-dependent. Insufficient incubation may not allow for adequate growth in control wells, while over-incubation might allow "skipped growth" or trailing effects in higher concentrations, making endpoint determination difficult.
- INT Incubation Duration: The development time for the colorimetric signal must be optimized. Short incubation may yield a weak signal, while prolonged incubation can lead to non-specific background color formation in wells with inhibited, but not dead, cells.
- Broth Medium Composition: The choice of medium (e.g., RPMI vs. Mueller-Hinton) and its supplements (e.g., cation adjustment) can profoundly affect the activity of certain antimicrobials and must be selected according to established guidelines [44] [46].
- Reporting Standards: When reporting MIC values, it is essential to specify the standard method followed (e.g., EUCAST or CLSI), the version year of the guidelines, and the type of colorimetric assay used. This ensures proper interpretation and allows for cross-comparison with other studies [44].
The logical relationship between common issues and their resolutions is illustrated in the following flowchart.
The colorimetric broth microdilution assay using p-iodonitrophenyltetrazolium violet (INT) represents a significant advancement in antimicrobial susceptibility testing (AST). This method provides a reliable, rapid, and economical approach for determining the minimum inhibitory concentration (MIC) of antimicrobial agents against fastidious pathogens like Helicobacter pylori. The assay operates on the principle that viable bacterial cells containing dehydrogenase enzymes metabolize the tetrazolium substrate INT, reducing it to a brightly colored, insoluble red formazan compound [47]. This color change serves as a clear, visual indicator of bacterial cell viability, enabling straightforward endpoint determination. The integration of such colorimetric methods into microbiological practice is crucial for addressing the global challenge of antibiotic resistance, particularly for pathogens where conventional AST is complicated by slow growth and fastidious requirements [47] [48].
This application note details the use of the INT colorimetric assay within the broader context of MIC determination research, featuring a specific case study on H. pylori and its validation against other common pathogens. We provide detailed protocols, data on performance characteristics, and resources to facilitate the adoption of this method in research and clinical laboratories.
Case Study: INT Colorimetric Assay forHelicobacter pyloriMIC Determination
Background and Rationale
H. pylori, a Gram-negative, spiral-shaped bacterium, is a major human pathogen associated with chronic gastritis, peptic ulcers, and gastric cancer [49] [47]. Eradication of H. pylori typically requires combination antibiotic therapy, but rising global antibiotic resistance rates have led to increasing treatment failures [50] [51]. Consequently, accurate and efficient antimicrobial susceptibility testing (AST) is paramount for guiding effective, personalized treatment regimens.
Traditional AST methods for H. pylori, such as agar dilution (the CLSI gold standard), E-test, and standard broth microdilution, can be time-consuming, labor-intensive, and require specific expertise and equipment [50] [47]. The INT colorimetric assay was developed to overcome these limitations by offering an easy, rapid, and H. pylori-specific method with unambiguous, colorimetric endpoints [47].
Experimental Protocol
Method: INT Colorimetric Broth Microdilution for H. pylori MIC Determination [47].
Principle: Viable H. pylori cells reduce the colorless INT substrate to a red formazan product. The presence of a red color indicates bacterial growth, while inhibition of growth by an antimicrobial agent prevents color development.
Materials and Reagents
- PureLine H. pylori Urease Positive Control: Serves as a positive control for the assay, confirming urease activity and viability [47].
- Brain Heart Infusion (BHI) Broth: Supplemented with 5% fetal calf serum, used as the growth medium for H. pylori [47].
- p-Iodonitrophenyltetrazolium Violet (INT): Prepared as a 0.2 mg/mL solution in distilled water. This is the key colorimetric indicator of cell viability [47].
- 96-well U-bottom Microtiter Plates: Used for preparing serial dilutions of antimicrobial agents and incubating the assay [47].
- Test Antimicrobial Agents: These may include conventional antibiotics (e.g., clarithromycin, amoxicillin, metronidazole, levofloxacin) or novel compounds like plant essential oils [47].
- Sterile Physiological Saline: Used for preparing bacterial suspensions [47].
- Microaerophilic Atmosphere Generation System: Essential for creating the required microaerophilic conditions (5% O₂, 10% CO₂, 85% N₂) for H. pylori growth [47].
Procedure
- Inoculum Preparation: Harvest a 72-hour culture of H. pylori and prepare a suspension in sterile physiological saline, adjusted to a density of 10⁷ CFU/mL.
- Antimicrobial Dilution: In the 96-well microtiter plate, perform two-fold serial dilutions of the antimicrobial agent in BHI broth, resulting in a final volume of 100 µL per well.
- Inoculation: Add 100 µL of the standardized bacterial inoculum to each well containing the antimicrobial agent. Include growth control wells (bacteria without antimicrobial) and sterility control wells (media only).
- Incubation: Seal the plates and incubate under microaerophilic conditions at 37°C for 72 hours.
- INT Addition: After incubation, add 40 µL of the INT solution (0.2 mg/mL) to each well.
- Re-incubation: Incubate the plates for a further 1-2 hours to allow for color development.
- Result Interpretation: The Minimum Inhibitory Concentration (MIC) is defined as the lowest concentration of the antimicrobial agent that completely prevents the reduction of INT, as indicated by the absence of a red color.
Key Findings and Advantages
The INT colorimetric method has demonstrated high reproducibility and clear-cut endpoints for determining the MIC of various antimicrobials against H. pylori [47]. Its utility extends beyond conventional antibiotics to the evaluation of natural products, such as essential oils from Hyssopus officinalis and Thymus serpyllum, for which anti-H. pylori activity was confirmed for the first time using this assay [47].
The primary advantages of this method include:
- H. pylori-specific: The assay is optimized for this fastidious organism.
- Rapid and Clear Endpoints: Color change provides an unambiguous visual readout.
- Cost-effective: Requires standard laboratory equipment and inexpensive reagents.
- Reproducible: Shows consistent results across replicate experiments.
- Versatile: Applicable for testing both conventional antibiotics and novel antimicrobial agents.
Comparison with Other Modern Detection and AST Methods
The landscape of H. pylori diagnosis and resistance profiling includes several other advanced technologies. The INT colorimetric MIC assay fits into a broader toolkit of methods, each with distinct applications and performance characteristics, as summarized in the table below.
Table 1: Comparison of H. pylori Detection and Antimicrobial Susceptibility Testing Methods
| Method | Principle | Application in H. pylori | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|---|
| INT Colorimetric Broth Microdilution [47] | Bacterial dehydrogenase reduces INT to red formazan. | MIC determination for antibiotics & novel agents. | Reproducible, clear-cut MIC endpoints. | Cost-effective, specific, versatile for new compounds. | Requires culture; 3-day incubation. |
| Colorimetric LAMP (C-LAMP) [49] | Isothermal DNA amplification with colorimetric pH detection. | Direct detection from biopsy samples. | Sensitivity: 80% (vs culture), Specificity: 98% (vs culture); LOD: 1 CFU/mL. | Rapid (15 min), high sensitivity, no thermocycler. | Does not provide antibiotic susceptibility data. |
| Gold Nanoparticle (AuNP) Colorimetric Biosensor [52] | Aptamer-target binding causes AuNP deaggregation (color shift). | Detection of antigens in feces. | LOD: 25 CFU/mL. | Non-invasive, rapid, no dietary/medication limitations. | Not for AST; detects presence/absence only. |
| Molecular Methods (qPCR, ARMS-PCR, NGS) [50] | Detection of genetic mutations associated with resistance. | Identifying clarithromycin/levofloxacin resistance. | High sensitivity & specificity for specific mutations (e.g., >97% for ARMS-PCR). | Rapid, can detect heteroresistance, high-throughput. | Limited to known genetic mechanisms; cannot detect novel or phenotypic resistance. |
| Efflux Pump Analysis (qPCR) [51] | Quantification of efflux pump gene expression (e.g., hefA). | Investigating alternative clarithromycin resistance. | Correlates hefA overexpression with increased MIC. | Reveals non-mutational resistance mechanisms. | Complex, requires specific expertise and instrumentation. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for INT Colorimetric Assays and H. pylori Research
| Item | Function/Application | Example/Description |
|---|---|---|
| p-Iodonitrophenyltetrazolium Violet (INT) [47] | Colorimetric viability indicator in broth microdilution assays. | Dehydrogenase substrate reduced to red formazan by metabolically active cells. |
| WarmStart Colorimetric LAMP Master Mix [49] | Enzymatic mix for isothermal nucleic acid amplification. | Enables rapid, single-tube C-LAMP detection of H. pylori with visual readout. |
| Peptide Nucleic Acid (PNA) Probes [50] | Synthetic probes for qPCR-based resistance detection. | Used in PNA-qPCR to block wild-type amplification, enhancing specificity for SNP detection. |
| Clinoptilolite-based Materials (Ag-/Zn-) [53] | Antimicrobial carrier and ammonium sequestrant for novel therapy research. | Natural zeolite used to deliver antimicrobial metal ions (Ag+, Zn2+) and absorb NH4+. |
| H. pylori-specific Aptamers [52] | Recognition elements in biosensors for pathogen detection. | Short oligonucleotides that bind H. pylori targets with high affinity and specificity. |
| PureLink Genomic DNA Mini Kit [49] | Extraction of high-quality genomic DNA from bacterial cultures or clinical samples. | Essential for downstream molecular applications like PCR, LAMP, and sequencing. |
| Microtiter Plates (U-bottom) [47] | Platform for performing broth microdilution and colorimetric assays. | Standard 96-well plates used for serial drug dilutions and incubation. |
Experimental Workflow and Diagnostic Pathways
The following diagrams illustrate the logical workflow of the INT colorimetric assay and its place within the broader context of H. pylori diagnostic and resistance profiling strategies.
Workflow of INT Colorimetric MIC Assay
Diagram 1: INT Assay Workflow
Integrated Diagnostic Pathway for H. pylori
Diagram 2: H. pylori Diagnostic Pathway
Troubleshooting the INT Assay: Identifying and Mitigating Sources of Variability for Enhanced Precision
The INT (Iodonitrotetrazolium chloride) colorimetric assay is a fundamental tool for rapid, quantitative determination of Minimum Inhibitory Concentration (MIC) in antimicrobial drug development. It functions on the principle that metabolically active bacterial cells reduce the nearly colorless INT to a brightly colored, insoluble formazan product, typically pink to red. The intensity of this color development is directly proportional to the number of viable cells, allowing for a visual or spectrophotometric assessment of microbial growth inhibition. However, the reliability of this assay is critically dependent on optimal protocol execution. Two of the most frequent and detrimental challenges faced by researchers are weak color development, which compromises detection sensitivity, and high background signal, which reduces the assay's signal-to-noise ratio and dynamic range. This application note provides a detailed, practical guide for identifying, troubleshooting, and resolving these issues to ensure robust and reproducible MIC data.
Troubleshooting Weak Color Development
Weak or absent formazan color formation can lead to false-negative results or an overestimation of a drug's potency. The causes are often multi-factorial and require systematic investigation. The following table summarizes the primary culprits, their diagnostic signs, and recommended corrective actions.
Table 1: Troubleshooting Guide for Weak Color Development
| Primary Cause | Underlying Issue | Recommended Solution |
|---|---|---|
| Insufficient Microbial Metabolism | Low inoculum viability or density Inappropriate growth medium/nutrients Incubation conditions (temp, gas, time) suboptimal | Standardize inoculum to ~1 x 10^8 CFU/mL using optical density [54]. Use fresh, log-phase cultures and verify CFU. Ensure medium supports robust growth; pre-warm if necessary. |
| INT Reagent Issues | INT concentration too low INT stock solution degraded (light exposure) Incubation time with INT too short | Titrate INT concentration (0.2-2.0 mg/mL is a common range). Prepare INT stock fresh or store aliquoted at -20°C, protected from light. Extend INT incubation time (e.g., 30 mins to 2 hours); determine optimal duration empirically. |
| Chemical Interference | Test drug inhibits microbial reductase enzymes Reaction buffer pH is suboptimal | Include proper controls (e.g., solvent, viability). Ensure buffer pH is suitable for both bacterial growth and reductase activity (typically pH ~7.4). |
| Signal Detection Problems | Incorrect spectrophotometer wavelength Plate reader is improperly calibrated | Use the correct absorbance wavelength, typically near 490 nm for formazan [54]. Calibrate instruments regularly and ensure clean, clear microplates are used. |
Experimental Protocol: Optimizing INT Concentration and Incubation Time
This protocol outlines a systematic approach to determine the optimal INT conditions for a specific microorganism.
- Prepare Microbial Suspension: Grow the target microorganism to mid-log phase and dilute in appropriate broth to a standardized density of 1 x 10^8 CFU/mL.
- Set Up INT Titration Plate: In a sterile 96-well plate, add 100 µL of microbial suspension to all wells. Add 100 µL of sterile broth to columns 1-12 for a no-INT control.
- Add INT Stock: Prepare a sterile, filter-sterilized stock of INT in water (e.g., 4 mg/mL). Serially dilute this stock and add 20 µL to the test wells to achieve a final concentration range (e.g., 0.1, 0.2, 0.5, 1.0, 2.0 mg/mL). Perform in triplicate.
- Incubate and Monitor: Incubate the plate under optimal growth conditions. Monitor color development visually and spectrophotometrically at 490 nm every 30 minutes for up to 4 hours.
- Analyze Data: Plot absorbance versus time for each INT concentration. The optimal condition is the lowest concentration that yields a strong, stable signal (Abs > 0.8) without excessive background, within a reasonable time frame (1-2 hours).
INT Optimization Workflow
Mitigating High Background Signal
A high background signal, manifesting as excessive color in negative controls (e.g., sterile broth with INT), obscures the true signal from viable cells and severely compromises assay sensitivity. The following table outlines common sources and solutions.
Table 2: Troubleshooting Guide for High Background Signal
| Primary Cause | Underlying Issue | Recommended Solution |
|---|---|---|
| Non-Specific INT Reduction | Chemical reduction by components in growth medium (e.g., sulfhydryl groups) Auto-reduction at high temperatures or extreme pH | Test different broth batches and formulations; use low-reactivity media. Include a "medium + INT" control in every experiment. Ensure reaction pH is neutral and avoid excessive heat during preparation. |
| Contamination | Microbial contamination in reagents, medium, or assay plates | Filter-sterilize INT stock solutions (0.2 µm filter). Maintain strict aseptic technique. Inspect medium and reagents for clarity before use. |
| Poor Solubility/Precipitation | Formazan crystals precipitating unevenly, causing light scatter | Include a solubilization step with DMSO or SDS after incubation to dissolve formazan crystals uniformly [55]. |
| Detection Artifacts | Bubbles in wells during reading Scratches or fingerprints on microplate Contaminated optics in plate reader | Centrifuge plate briefly before reading to remove bubbles. Handle plates carefully by the edges. Follow manufacturer's guidelines for plate reader maintenance. |
Experimental Protocol: Establishing a Robust Background Correction Method
This protocol details how to quantify and correct for background interference.
- Prepare Control Wells:
- Test Well: Microbial suspension + Broth + INT
- Background Control 1: Sterile Broth + INT (measures non-specific reduction)
- Background Control 2: Microbial suspension + Broth + Sterile Water (no INT; measures cell turbidity)
- Blank: Sterile Broth + Sterile Water (for instrument zeroing)
- Run Assay: Execute the MIC assay under standard conditions.
- Data Calculation: After incubation and signal development, measure the absorbance at 490 nm.
- Corrected Absorbance = Abs(Test Well) - Abs(Background Control 1)
This correction subtracts the signal generated from the medium and INT alone, providing a more accurate measure of microbial INT reduction. For a more refined correction that also accounts for turbidity, a second wavelength (e.g., 630-660 nm) can be used, and the corrected absorbance is calculated as: Abs(490nm, corrected) = Abs(Test Well, 490nm) - Abs(Test Well, 630nm) - Abs(Background Control 1, 490nm).
Background Correction Protocol
The Scientist's Toolkit: Research Reagent Solutions
The reliability of an INT colorimetric assay hinges on the quality and appropriate selection of key reagents. The following table catalogs essential materials and their critical functions.
Table 3: Essential Reagents for INT Colorimetric MIC Assays
| Reagent/Material | Function & Role in Assay | Key Considerations for Use |
|---|---|---|
| INT (Iodonitrotetrazolium Chloride) | A tetrazolium salt that acts as an electron acceptor; reduced by metabolically active microbes to a red formazan product. | Stability: Light-sensitive; prepare fresh solutions or store frozen, aliquoted, in the dark.Concentration: Requires optimization (see Protocol 2.1); typically 0.2-2.0 mg/mL final concentration. |
| Culture Broth (e.g., Mueller-Hinton) | Provides nutrients and environment to support microbial growth during drug exposure. | Batch Variability: Different lots can vary in components that cause non-specific INT reduction; pre-test and select low-background batches.Cation Adjustment: For Pseudomonas aeruginosa, use cation-adjusted Mueller-Hinton broth for reliable results. |
| Reference Strains (e.g., ATCC) | Quality control organisms used to validate the entire assay system, from inoculum preparation to INT reduction. | Routine Use: Include strains like S. aureus ATCC 29213 and E. coli ATCC 25922 in each assay run to ensure performance meets established MIC ranges. |
| DMSO or SDS | A solvent used to dissolve the insoluble formazan crystals after the incubation period, creating a homogeneous colored solution. | Timing: Add after initial absorbance reading to confirm if low signal is due to precipitation.Concentration: Typically 10-50% final concentration of DMSO; validate for your system. |
| 96-well Microplates | The platform for hosting the assay, allowing for high-throughput testing of multiple drug concentrations and replicates. | Optical Quality: Use plates with clear, flat bottoms for spectrophotometric reading.Sterility: Must be sterile for aseptic incubation over 18-24 hours. |
| UV-Vis Spectrophotometer/Plate Reader | Instrument for quantifying the intensity of the formazan color development, providing objective MIC data. | Wavelength: Set to ~490 nm, the absorbance peak for INT-formazan [54].Validation: Regular calibration is essential for data integrity and reproducibility. |
Validated Spectrophotometric Method for INT-Formazan Quantification
As demonstrated in the validation of colorimetric methods for other compounds like Rifampicin, a rigorous approach is required for bioanalytical assays [54]. While the following parameters are specific to INT-formazan, the validation framework is universal.
- Selectivity/Specificity: The method should distinguish between the formazan signal in test wells and background signals in negative controls (sterile broth + INT).
- Linearity and Range: Prepare a dilution series of a standard formazan product (if available) or a serially diluted, viable cell culture to establish a standard curve. The assay should demonstrate excellent linearity (r² > 0.98) over the expected range of microbial densities [54].
- Limit of Detection (LOD) and Quantification (LOQ):
- LOD: The lowest number of CFU/mL that produces a signal significantly different from the background. Estimated as: LOD = 3.3 * σ / S, where σ is the standard deviation of the background response and S is the slope of the standard curve.
- LOQ: The lowest number of CFU/mL that can be quantified with acceptable precision and accuracy (e.g., %RSD < 20%). Estimated as: LOQ = 10 * σ / S [54].
- Accuracy and Precision: Assessed by testing replicate samples (n≥5) at low, medium, and high microbial densities within the same day (intra-day precision) and on different days (inter-day precision). Accuracy is reported as % Relative Error (%RE) and precision as % Relative Standard Deviation (%RSD) [54].
- Robustness: Deliberately introduce small variations in critical parameters (e.g., INT incubation time ± 10 minutes, incubation temperature ± 1°C) to demonstrate the method's reliability.
Assay Validation Pathway
In the determination of minimum inhibitory concentration (MIC) using INT colorimetric assays, controlling and quantifying sources of variability is paramount for ensuring reliable and reproducible results. Bioassay variability can originate from multiple sources, including differences between analysts performing the assays (analyst-to-analyst variation) and fluctuations in results obtained on different days (day-to-day variation). These factors are critical in MIC determinations, where precise endpoint identification directly impacts therapeutic decisions and resistance monitoring. Understanding these variability components enables researchers to establish appropriate acceptance criteria, improve assay robustness, and generate more reliable data for drug development applications.
The INT colorimetric assay, which utilizes 2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride as a redox indicator, is particularly susceptible to technical variation due to its multiple procedural steps and dependence on consistent cellular metabolic activity. As outlined in United States Pharmacopeia (USP) guidelines, identifying and controlling these variability sources through proper experimental design and statistical analysis is essential for developing robust bioanalytical methods [56]. This application note provides detailed protocols for quantifying and mitigating analyst-to-analyst and day-to-day variations specifically within the context of INT colorimetric MIC determination research.
Variance Components Analysis
Statistical variance components analysis provides a quantitative framework for partitioning total variability into identifiable sources. According to USP <1033>, this approach is recommended for understanding bioassay performance characteristics [56]. The following calculations are essential for interpreting variation in INT colorimetric MIC assays:
- Percentage Coefficient of Variation (%CV): Calculated as %CV = 100 × √[exp(Variance Component) - 1]
- Percentage Geometric Coefficient of Variation (%GCV): Calculated as %GCV = 100 × [exp(√Variance Component) - 1]
For well-behaved bioassays with %CV < 20%, the difference between %GCV and %CV is minimal, with %CV being more widely used by practitioners [56]. The table below illustrates typical variance components in bioassay validation:
Table 1: Illustrative Variance Components in Bioassay Validation
| Variation Source | Variance Component Estimate | %CV | % of Total Variation |
|---|---|---|---|
| Analyst-to-Analyst | 0.0215 | 14.8% | 52% |
| Day-to-Day | 0.0112 | 10.7% | 27% |
| Inter-Assay | 0.0058 | 7.6% | 14% |
| Intra-Assay | 0.0024 | 4.9% | 7% |
Acceptance Criteria for Variation Components
Establishing appropriate acceptance criteria is essential for maintaining bioassay quality. For colorimetric assays used in MIC determination, the following performance benchmarks are recommended based on industry standards:
Table 2: Acceptance Criteria for Colorimetric Bioassay Variation
| Performance Measure | Recommended Acceptance Criteria | Application to INT Colorimetric MIC Assay |
|---|---|---|
| Inter-Assay CV | < 15% [57] | Plate-to-plate consistency in MIC determination |
| Intra-Assay CV | < 10% [57] | Variation between replicates on the same plate |
| Analyst-to-Analyst | Comparable means and variances | Different analysts performing the same INT assay |
| Day-to-Day | Consistent control values | Same protocol performed on different days |
Experimental Protocols
Protocol for Assessing Analyst-to-Analyst Variation
Purpose: To quantify and compare the variation introduced by different analysts when performing the INT colorimetric MIC assay.
Materials:
- INT solution (2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride)
- Bacterial suspensions at 0.5 McFarland standard
- Mueller-Hinton broth
- 96-well microtiter plates
- Positive control (reference antibiotic)
- Negative control (sterile broth)
Procedure:
- Prepare identical sets of antibiotic serial dilutions in 96-well plates (8 replicates per concentration)
- Assign three analysts with varying experience levels to independently perform the INT assay
- Each analyst inoculates plates with standardized bacterial suspension
- Incubate at 35±2°C for 16-20 hours
- Each analyst adds INT solution (0.2 mg/mL final concentration) to all wells
- Incubate for additional 30-60 minutes until color development in positive control wells
- Each analyst independently reads MIC endpoints (lowest concentration showing complete inhibition of color change)
- Analyze results using variance components analysis
Data Analysis:
- Calculate MIC values for each analyst across all replicates
- Perform logarithmic transformation of MIC values
- Conduct variance components analysis to partition total variability
- Compare mean MIC values between analysts using appropriate statistical tests (e.g., ANOVA)
- Calculate inter-analyst %CV
Acceptance Criteria: Analyst-to-analyst variation should contribute less than 15% to total variability, and mean MIC values should not differ significantly between analysts (p > 0.05).
Protocol for Assessing Day-to-Day Variation
Purpose: To evaluate consistency of INT colorimetric MIC results when performed on different days.
Materials: (Same as Protocol 3.1)
Procedure:
- A single analyst performs the complete INT colorimetric MIC assay on three separate days
- Use the same bacterial strain, antibiotic, and reagent batches across all days
- Prepare fresh antibiotic serial dilutions each day
- Follow standardized INT assay protocol consistently each day
- Include quality control strains with known MIC ranges each day
- Record MIC values for test and control strains daily
Data Analysis:
- Calculate daily mean MIC values for each antibiotic concentration
- Perform variance components analysis with "day" as a random factor
- Calculate inter-day %CV
- Assess trend in control values over time
Acceptance Criteria: Day-to-day variation should contribute less than 20% to total variability, and control values should remain within established quality control ranges.
Protocol for Integrated Variation Analysis
Purpose: To simultaneously evaluate multiple sources of variation in a single efficient experimental design.
Materials: (Same as Protocol 3.1)
Procedure:
- Implement an integrated Design of Experiments (ixDoE) approach [58]
- Design experiment with three analysts, three days, with two assays per analyst per day
- Include duplicate wells for each antibiotic concentration
- Distribute experimental runs randomly to avoid confounding effects
- Perform INT colorimetric MIC assay according to standardized protocol
- Record all MIC endpoints independently
Data Analysis:
- Perform comprehensive variance components analysis
- Calculate % contribution of each variability source to total variation
- Generate variability charts to visualize different variation sources
- Establish assay precision profile across the measurement range
Acceptance Criteria: Total assay %CV should be < 20%, with no single source of variation accounting for >50% of total variability.
Visualization of Variation Analysis
Experimental Workflow for Variation Analysis
Variance Components Partitioning
Research Reagent Solutions
Table 3: Essential Reagents for INT Colorimetric MIC Assays
| Reagent/Material | Function in INT Assay | Technical Considerations |
|---|---|---|
| INT Salt (2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyltetrazolium chloride) | Redox indicator; reduced to colored formazan by metabolically active cells [59] | Prepare fresh solution (0.2 mg/mL) in sterile water or PBS; protect from light |
| Cation-adjusted Mueller-Hinton Broth | Standardized growth medium for MIC determination | Verify calcium and magnesium concentrations; store at 2-8°C |
| 96-well Microtiter Plates | Platform for antibiotic serial dilutions and bacterial inoculation | Use sterile, flat-bottom plates; ensure consistent well volumes |
| Reference Antibiotics | Quality control and standardization | Obtain from certified suppliers; prepare stock solutions according to CLSI guidelines |
| Bacterial QC Strains | Assay performance verification | Use CLSI-recommended strains with known MIC ranges; maintain proper storage |
| DMSO or Ethanol | Solvent for antibiotic stock solutions | Use reagent-grade solvents; ensure compatibility with bacterial growth |
Systematic analysis of analyst-to-analyst and day-to-day variation is essential for developing robust INT colorimetric MIC assays. The protocols outlined in this application note provide researchers with standardized approaches for quantifying these variability components, enabling improved assay design and more reliable MIC determinations. Through proper experimental design and statistical analysis, laboratories can identify predominant sources of variation, implement targeted improvements, and establish scientifically justified acceptance criteria that ensure data quality while maintaining assay practicality for routine use in drug development pipelines.
The colorimetric broth microdilution method using p-iodonitrophenyltetrazolium violet (INT) has emerged as a vital technique in antimicrobial susceptibility testing (AST), enabling accurate determination of the Minimum Inhibitory Concentration (MIC) of antimicrobial agents against fastidious microorganisms. This method provides a simple, accurate, and reproducible alternative to traditional agar dilution techniques that are often time- and material-consuming [60]. Within the broader context of INT colorimetric assay research, optimization of key parameters—INT concentration, incubation time, and temperature—represents a critical pathway toward enhancing assay precision, reliability, and translational applicability in both research and clinical settings. The fundamental principle of the INT assay relies on the bacterial conversion of the nearly colorless INT, a tetrazolium salt, into pink-red INT-formazan in the presence of NADH-generating metabolic pathways, providing a visual indicator of bacterial cell viability and growth [60]. This application note delineates evidence-based optimization strategies and detailed protocols for implementing the INT colorimetric MIC determination assay, providing researchers and drug development professionals with a standardized framework for assessing antimicrobial efficacy.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation and optimization of the INT colorimetric MIC assay necessitate specific reagents and materials. The following table details the essential components and their respective functions within the experimental workflow.
Table 1: Key Research Reagents and Materials for INT Colorimetric MIC Assays
| Item | Function/Description | Application Notes |
|---|---|---|
| p-Iodonitrophenyltetrazolium violet (INT) | Colorimetric viability indicator; reduced to pink-red formazan by metabolically active bacteria [60]. | Concentration requires optimization; typically used at 0.2 mg/mL. Must be prepared fresh or stored frozen, protected from light. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution AST [61] [62]. | Ensures reproducible ion content, critical for accurate antibiotic activity, especially for polymyxins [62]. |
| 96-Well Microtiter Plates | Platform for broth microdilution assays. | Enables high-throughput testing of multiple antimicrobial concentrations and samples simultaneously. |
| Test Antimicrobial Agents | Essential oils, antibiotics, or novel compounds for efficacy testing [60]. | Serial twofold dilutions are prepared in the microtiter plate to establish a concentration gradient. |
| Bacterial Inoculum | Standardized microbial suspension of the target organism. | Must be adjusted to a final density of ~5 × 10⁵ CFU/mL in each well for most bacteria, per EUCAST/CLSI guidelines [62]. |
| Positive (Bacteria only) & Negative (Sterile Media) Controls | Assay validation controls. | Verify adequate bacterial growth and confirm sterility of the procedure, respectively. |
Optimization of Critical Parameters
Systematic optimization of the INT colorimetric assay is paramount for achieving reliable and reproducible MIC endpoints. The following parameters have been identified as most critical for assay performance.
INT Concentration and Preparation
The concentration of the INT indicator directly influences the sensitivity and clarity of the colorimetric reaction.
- Optimal Concentration: A final concentration of 0.2 mg/mL of INT in the broth medium is widely effective for generating a distinct color change without imparting background color or antibacterial effects [60].
- Preparation: Prepare a stock solution of INT in sterile water or physiological saline. The solution should be filter-sterilized and stored in aliquots at -20°C, protected from light. Thawed aliquots should be used promptly, and repeated freeze-thaw cycles must be avoided to maintain reagent integrity.
- Quality Control: A working INT solution should be clear and colorless. Any pink discoloration indicates degradation and potential formazan formation, rendering the batch unsuitable for use.
Incubation Time and Temperature
The dynamics of bacterial metabolism and, consequently, INT reduction are highly dependent on incubation conditions. Optimization must balance rapid results with complete phenotypic expression.
- General Guidance: For most non-fastidious bacteria, an initial incubation of 16-24 hours at 35±2°C is standard prior to adding INT, aligning with EUCAST and CLSI guidelines for broth microdilution [62].
- Post-INT Incubation: Following the addition of INT, a secondary incubation of 1-4 hours at 35±2°C is typically sufficient for color development in viable wells [60].
- Optimization Strategy: Initial incubation time may be extended for slow-growing organisms. The optimal post-INT incubation period should be determined empirically by monitoring color development; prolonged incubation can lead to false positives due to formazan crystal precipitation or continued slow growth in marginally inhibited wells.
- Temperature Considerations: The standard incubation temperature of 35±2°C supports the growth of most human pathogens [63]. Dual-incubation regimes (e.g., 20-25°C followed by 30-35°C) can be employed when recovering a broader range of environmental or stressed microorganisms, though the order (low-to-high is common) can impact the recovery of bacteria versus fungi [63].
Table 2: Summary of Optimized Parameters for INT Colorimetric MIC Assay
| Parameter | Recommended Condition | Rationale & Variations |
|---|---|---|
| INT Final Concentration | 0.2 mg/mL | Provides a clear colorimetric signal without antibacterial activity or background interference [60]. |
| Primary Incubation (Pre-INT) | 16-24 hours at 35±2°C | Standard time for observable growth in broth microdilution; extended for slow-growers [62]. |
| Secondary Incubation (Post-INT) | 1-4 hours at 35±2°C | Allows metabolic reduction of INT by viable cells; duration is organism- and inoculum-dependent. |
| Total Assay Duration | ~18-28 hours | Faster than traditional agar dilution methods [60]. |
| Inoculum Density | 5 x 10⁵ CFU/mL | Standardized cell density ensures reproducibility and accuracy in MIC determination [62]. |
Detailed Experimental Protocols
Protocol: INT Colorimetric Broth Microdilution for MIC Determination
This protocol describes the standardized procedure for determining the MIC of antibiotics or essential oils against bacterial strains using the INT colorimetric method [60] [62].
Materials:
- Tryptone Soya Broth (TSB) or Cation-Adjusted Mueller-Hinton Broth (CAMHB)
- 96-well U-bottom microtiter plates
- INT stock solution (2 mg/mL, filter-sterilized)
- Test antimicrobial agent (antibiotic or essential oil)
- Bacterial inoculum, standardized to 0.5 McFarland
Procedure:
- Prepare Antimicrobial Dilutions: In a 96-well plate, perform twofold serial dilutions of the antimicrobial agent in the appropriate broth medium (e.g., 100 µL per well).
- Inoculate Plate: Add 100 µL of the standardized bacterial inoculum (diluted from the 0.5 McFarland standard to achieve a final density of ~5 × 10⁵ CFU/mL) to each test well. Include growth control (bacteria + medium) and sterility control (medium only) wells.
- Primary Incubation: Seal the plate with a lid or parafilm and incubate statically for 16-24 hours at 35±2°C.
- Add INT Indicator: After primary incubation, add 20 µL of the INT stock solution (2 mg/mL) to each well. The final INT concentration will be approximately 0.2 mg/mL.
- Secondary Incubation: Re-incubate the plate for 1-4 hours at 35±2°C. Monitor wells periodically for color development.
- MIC Determination: The MIC is defined as the lowest concentration of the antimicrobial agent that completely inhibits bacterial metabolism, indicated by the absence of a pink-red color change (the well remains clear or the color of the original INT solution). The growth control well should show a distinct color change, while the sterility control should show no color change.
Protocol Modification for Fastidious Organisms: Helicobacter pylori Example
For fastidious organisms like Helicobacter pylori, the protocol can be adapted as demonstrated in foundational research [60].
- Medium: Use a specialized broth medium that supports the growth of the target fastidious organism.
- Inoculum Preparation: Harvest fresh colonies and standardize the inoculum carefully, as viability can decrease rapidly.
- Incubation Atmosphere: Incubate under required microaerophilic conditions for H. pylori.
- INT and Reading: The addition of INT and interpretation of results remain consistent. The developed assay was shown to be "simple to handle, accurate, reproducible and not as time- and material-consuming as traditional agar dilution techniques" [60].
Workflow and Pathway Diagrams
The following diagrams illustrate the logical workflow of the optimized INT assay and the strategic approach to parameter optimization.
INT Assay Workflow
Optimization Strategy Map
Within antibacterial drug development, accurate determination of the minimum inhibitory concentration (MIC) is fundamental for assessing compound efficacy. The p-iodonitrotetrazolium chloride (INT) colorimetric assay has emerged as a valuable tool for this purpose, offering a visual and quantitative method to rapidly determine bacterial viability [21]. However, the reliability of this assay is contingent upon successfully addressing two persistent technical challenges: the precise quantitation of initial cell density and ensuring solvent compatibility with both the microbial inoculum and the assay's colorimetric chemistry. This Application Note details standardized protocols to overcome these challenges, enhancing the reproducibility and accuracy of MIC determinations in early-stage research.
Technical Challenge 1: Cell Density Quantitation
A foundational step in any antimicrobial susceptibility test is the standardization of the bacterial inoculum. Inconsistent cell densities can lead to significant MIC variability, compromising data reliability and cross-study comparisons.
Carmine Staining as a Precise Cell Density Verification Method
Direct cell counting is laborious, while other indirect methods can suffer from non-specific interference. As an alternative, a colorimetric cell density quantitation method using carmine, a natural chromosome-specific stain, provides an easy, precise, and reliable method [64].
Key Advantages:
- Wide Applicability: Validated across a wide range of cell types, including normal or transformed murine fibroblasts, avian normal fibroblasts, human epithelial HeLa cells, and insect cells [64].
- Broad Dynamic Range: Demonstrates high correlation between cell number and absorbance within a range of 5 × 10³ to 5 × 10⁵ cells [64].
- High Correlation: Produces identical cell growth curves when compared to direct cell counting methods, confirming its accuracy [64].
Table 1: Protocol for Cell Density Quantitation Using Carmine Staining
| Step | Parameter | Specification |
|---|---|---|
| 1. Cell Fixation | Fixative | 4% Formaldehyde in PBS [64] |
| 2. Staining | Carmine Solution | 0.4% alcoholic-HCl carmine [64] |
| 3. Dye Extraction | Extraction Solution | 0.01 M NaOH [64] |
| 4. Measurement | Wavelength | 531 nm [64] |
Alternative Tetrazolium Salt-Based Assays
Other colorimetric assays based on tetrazolium salt reduction by metabolically active cells are also widely used for quantifying viable cells. Table 2 compares three common tetrazolium salts used in cell viability and proliferation assays, which can be adapted for inoculum viability checks [65].
Table 2: Comparison of Tetrazolium Salt-Based Colorimetric Assays
| Assay | Formazan Product Solubility | Detection Wavelength | Key Traits & Considerations |
|---|---|---|---|
| MTT | Water-insoluble (requires solubilization with DMSO) [65] | 490 nm [65] | Powder form; requires organic solvent; increased workload [65] |
| XTT | Water-soluble [65] | 450 nm [65] | Ready-to-use solution; requires an electron-coupling agent [65] |
| CCK-8/WST-8 | Water-soluble [65] | 450 nm [65] | Ready-to-use solution; no pre-processing; low cytotoxicity [65] |
Technical Challenge 2: Solvent Compatibility
Many antimicrobial compounds, particularly plant extracts and natural products, require organic solvents for solubilization. These solvents can exert antimicrobial activity themselves or interfere with the colorimetric reaction of the INT assay.
Syringe Filter Solvent Compatibility for Sterile Filtration
The sterile filtration of solvent-containing stock solutions is a common step. The choice of filter membrane material is critical, as incompatible solvents can degrade the filter, leading to contamination or loss of the analyte. Polytetrafluoroethylene (PTFE) membranes demonstrate exceptional broad-spectrum chemical resistance, making them the recommended choice for filtering a wide range of solvents, including acids, alcohols, and halogenated hydrocarbons [66].
Table 3: Syringe Filter Membrane Compatibility with Common Solvents
| Chemical Reagent | PTFE | Nylon | Polypropylene (PP) | Cellulose Acetate |
|---|---|---|---|---|
| Acetic Acid, Glacial | R [66] | N [66] | R [66] | N [66] |
| Ethanol (98%) | R [66] | R [66] | R [66] | N [66] |
| Methanol (98%) | R [66] | R [66] | R [66] | N [66] |
| Dimethyl Sulfoxide (DMSO) | R [66] | R [66] | R [66] | N [66] |
| Acetone | R [66] | R [66] | R [66] | N [66] |
| Chloroform | R [66] | N [66] | L [66] | N [66] |
| Ethyl Acetate | R [66] | R [66] | L [66] | N [66] |
Legend: R = Recommended; L = Limited Recommended Use; N = Not Recommended [66].
Managing Solvent Toxicity in Microbial Assays
Even at low concentrations, solvents can inhibit microbial growth, artificially lowering the MIC value of the co-administered test compound. Absolute ethanol is a commonly used solvent for preparing stock solutions of plant extracts [21]. A key control is the inclusion of wells containing the highest concentration of the solvent used in the assay (e.g., 20% aqueous ethanol) alongside the growth medium and inoculum to rule out solvent-mediated inhibition [60]. If the solvent exhibits intrinsic antimicrobial activity, its concentration must be reduced to a non-inhibitory level or an alternative, compatible solvent must be identified.
Integrated Protocol for INT Colorimetric MIC Assay
This section provides a detailed methodology for determining the MIC of test compounds against bacterial strains using the INT colorimetric assay, incorporating solutions to the cell density and solvent compatibility challenges.
Reagents and Materials
Table 4: Research Reagent Solutions for INT Colorimetric MIC Assay
| Item | Function / Specification |
|---|---|
| p-Iodonitrotetrazolium Chloride (INT) | Viability Indicator: Colorless tetrazolium salt reduced to pink-red formazan by metabolically active bacteria, providing visual growth indication [21]. |
| Mueller Hinton Broth (MHB) | Standardized Growth Medium: Provides nutrients for bacterial growth, ensuring reproducible assay conditions [21]. |
| Sterile Dimethyl Sulfoxide (DMSO) or Ethanol | Solvent: For preparing stock solutions of hydrophobic test compounds and antibiotics. Must be tested for non-interference [21]. |
| PTFE Syringe Filters (0.22 µm) | Sterile Filtration: For sterilizing solvent-containing stock solutions without membrane degradation [66]. |
| 96-Well Microplates | Assay Platform: Used for serial dilution of compounds and incubation with bacterial inoculum [21]. |
| Multichannel Pipette | Liquid Handling: Ensures accurate and reproducible transfer of liquids across multiple wells. |
| Microplate Reader (Spectrophotometer) | Absorbance Measurement: Optional for quantitative endpoint determination, though MIC is typically determined visually [1]. |
Step-by-Step Procedure
Preparation of Stock Solutions
- Dissolve the test compound (e.g., plant extract) in a suitable solvent like absolute ethanol to a typical concentration of 100 mg/mL [21]. For antibiotics, use sterilized distilled water [21].
- Prior to the assay, dilute the stock solution with sterilized distilled water to a working concentration (e.g., 12.5 mg/mL) [21].
- Sterile filtration: Pass solvent-containing solutions through a PTFE syringe filter (0.22 µm) to ensure sterility without compromising filter integrity [66].
Standardization of Bacterial Inoculum
- Culture the bacterial strain overnight at 37°C in Mueller Hinton Broth (MHB) [21].
- Adjust the optical density of the culture to match a 0.5 McFarland standard, which corresponds to approximately 1-2 x 10⁸ CFU/mL.
- Further dilute the suspension with MHB to achieve a final density of 10⁶ CFU/mL to be used as the inoculum [21]. For precise verification of cell density, the carmine staining protocol (Section 2.1) can be employed.
Broth Microdilution in 96-Well Plate
- Add Mueller Hinton Broth (MHB) to the wells. Add the test compound (plant extracts or antibiotics) and perform a two-fold serial dilution in the microplate to achieve the desired concentration range (e.g., 3120–24 µg/mL for plant extracts) [21].
- Add 100 µL of the standardized inoculum (10⁶ CFU/mL) to each well [21].
- Include essential controls:
- Negative Control: Well containing MHB, inoculum, and the highest concentration of solvent used (e.g., 20% aqueous ethanol) to confirm the solvent does not inhibit growth [21].
- Growth Control: Well containing MHB and inoculum only to confirm normal bacterial growth.
- The total volume in each well should be 200 µL [21].
- Cover the plate with a sterile sealer and incubate at 37°C for 20 hours [21].
INT Staining and MIC Determination
- After the initial incubation, add 40 µL of INT solution (0.2 mg/mL) to each well [21].
- Return the plate to the incubator for 30 minutes [21].
- Visually examine the wells for a color change. Metabolically active bacteria will reduce the yellow INT to a pink-red formazan product. The MIC is defined as the lowest concentration of the test compound that completely inhibits bacterial growth, indicated by a clear well with no pink-red color formation [21].
The integrity of MIC data generated via the INT colorimetric assay is highly dependent on rigorous technical execution. By implementing carmine-based cell density verification to ensure inoculum precision and adhering to PTFE-filter based sterilization protocols for solvent-compatible stock solution preparation, researchers can significantly mitigate two major sources of variability. These standardized protocols provide a robust framework for generating reliable, reproducible susceptibility data, thereby accelerating the early-stage discovery and development of novel antibacterial agents in the critical fight against antimicrobial resistance.
In the context of INT colorimetric assay research for minimum inhibitory concentration (MIC) determination, implementing robust controls is not merely a procedural formality—it is the fundamental practice that ensures data integrity, assay reproducibility, and clinical translatability. The INT (2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride) assay functions by detecting bacterial metabolic activity through a color change, where active bacterial respiration reduces the yellow INT substrate to a visible pink formazan product. Without appropriate controls, technical variations in reagents, bacterial inoculum, or assay conditions can produce misleading results, compromising the entire diagnostic pipeline. This protocol details the implementation of a comprehensive control framework aligned with international standards from the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [44] [4]. By systematically integrating the controls described herein, researchers can validate their INT colorimetric MIC assays, generating reliable, publication-ready data that accurately defines antimicrobial susceptibility.
Essential Control Concepts and Categorization
Controls in MIC assays serve distinct, critical functions. They are categorized based on their purpose in validating the assay components and processes.
Growth Controls verify that the test organism is viable and capable of growth under the assay conditions. The positive growth control (wells containing bacteria without antimicrobial agent) must show robust color change, confirming bacterial viability and proper INT reduction. Conversely, the negative growth control (sterile medium only) must remain colorless, confirming the absence of contaminating microorganisms [44] [6].
Technical and Methodological Controls ensure the accuracy of the testing process. Inoculum density controls are plated and enumerated to verify the final bacterial concentration is within the recommended range of 5 × 10^5 CFU/mL [44]. Solvent controls are crucial when testing antimicrobials or compounds dissolved in carriers like ethanol or DMSO; these controls contain the same concentration of solvent as the test wells to rule out any inhibitory effect of the solvent itself [67] [6].
Reference Controls provide a benchmark for assay performance. Quality control (QC) strains with known, stable MIC ranges are run in parallel with test isolates. Examples include E. coli ATCC 25922 and Staphylococcus aureus ATCC 29213 [68] [6]. The MIC results for these strains must fall within their established QC ranges for the entire assay to be considered valid.
Table 1: Categorization of Essential Controls for INT Colorimetric MIC Assays
| Control Category | Specific Control Type | Purpose | Acceptance Criterion |
|---|---|---|---|
| Growth Controls | Positive Growth Control | Verify bacterial viability and metabolic activity | Robust color change (yellow to pink) |
| Negative Growth Control (Sterility) | Confirm medium sterility and absence of contamination | No color change (remains yellow) | |
| Technical Controls | Inoculum Density Control | Standardize initial bacterial concentration | 5 × 10^5 CFU/mL (confirmed via plating) |
| Solvent Control | Rule out antimicrobial effect of compound solvent | No inhibition of growth/color change | |
| Reference Controls | Quality Control (QC) Strains | Benchmark assay performance and precision | MIC within established QC range [68] |
Experimental Protocol: A Controlled INT Colorimetric Broth Microdilution Assay
The following detailed protocol is adapted from EUCAST standards and current research for the execution of a controlled INT colorimetric MIC assay [44] [6].
Materials and Reagent Preparation
- Cation-Adjusted Mueller-Hinton Broth (CAMHB): Prepare according to manufacturer instructions. This is the standard medium for non-fastidious organisms [44] [6].
- INT Solution: Prepare a 0.2 mg/mL solution of INT in sterile water. Filter-sterilize and protect from light. The solution can be stored at 4°C for up to one month.
- Antibiotic Stock Solutions: Prepare antibiotic stocks at a high concentration (e.g., 10 mg/mL or as appropriate) in the recommended solvent (water, ethanol, methanol). Store aliquots at -20°C or as per stability requirements [6].
- Test Organism: Subculture the bacterial isolate(s) onto appropriate solid medium (e.g., Mueller-Hinton Agar) and incubate overnight at 37°C.
- Quality Control Strains: Include relevant QC strains such as E. coli ATCC 25922 and S. aureus ATCC 29213 [68].
Procedure Workflow and Control Integration
The diagram below illustrates the key steps of the protocol and the points at which critical controls are implemented.
Title: INT Assay Workflow with Control Points
Step-by-Step Instructions:
Prepare the Inoculum.
- Using a sterile loop, pick 3-5 well-isolated colonies from the fresh subculture.
- Suspend the colonies in sterile saline or CAMHB to achieve a turbidity equivalent to a 0.5 McFarland standard (approximately 1-2 x 10^8 CFU/mL).
- Control Step (Inoculum Density): Perform a viable count by serially diluting the suspension and plating onto agar. After incubation, count the colonies to confirm the final inoculum density in the assay is approximately 5 × 10^5 CFU/mL [44].
Prepare the MIC Plate.
- Prepare a 96-well microtiter plate with serial two-fold dilutions of the antibiotic in CAMHB.
- Control Step (Plate Layout):
- Column 1 (no antibiotic): Positive Growth Control. Add 100 µL of standardized inoculum to these wells.
- Column 12: Negative Growth Control (Sterility Control). Add 100 µL of sterile CAMHB only.
- For solvent controls, include additional wells containing the highest concentration of solvent used.
Incubate and Develop the Colorimetric Reaction.
- Cover the plate with a lid or sealing film and incubate at 37°C for 16-20 hours.
- After incubation, add 20-50 µL of INT solution to each well.
- Re-incubate the plate for 30-60 minutes at 37°C to allow for color development.
Read and Interpret the MIC Endpoint.
- The MIC is defined as the lowest concentration of antibiotic that completely inhibits bacterial metabolism, indicated by the absence of a pink color (the well remains yellow) [69].
- Compare the color in the test wells to the controls:
- Positive Growth Control: Must show a clear pink color. If not, the test is invalid.
- Negative Growth Control: Must remain yellow. Any pink color indicates contamination, and the test is invalid.
Performance Metrics and Validation of Controls
For an assay to be considered valid and its results reliable, the control results must meet predefined acceptance criteria. Furthermore, the performance of the entire method should be benchmarked against a reference standard.
Control Acceptance Criteria
Table 2: Acceptance Criteria for Essential Controls in a Validated INT Assay
| Control | Required Result | Action if Criterion Not Met |
|---|---|---|
| Positive Growth Control | Distinct pink color change | Repeat assay; check bacterial viability, INT reagent, incubation conditions |
| Negative Growth Control | No color change (yellow) | Repeat assay with fresh sterile media; aseptically review technique |
| Inoculum Density Control | Final concentration of 5 x 10^5 CFU/mL (± 1 log) | Adjust initial bacterial suspension and repeat standardization |
| QC Strains (e.g., E. coli ATCC 25922) | MIC within established QC range [68] | Review antibiotic dilution procedure, reagent preparation, and incubation |
Benchmarking Against Reference Methods
To validate the accuracy of the INT colorimetric method, its results should be compared to the gold standard broth microdilution (BMD) method. The comparison is quantified using specific metrics defined by CLSI/EUCAST [69] [68].
- Essential Agreement (EA): The percentage of MIC results by the INT method that are within one two-fold dilution of the BMD reference result. A value of >90% is generally considered acceptable [69].
- Categorical Agreement (CA): The percentage of interpretations (Susceptible, Intermediate, Resistant) by the INT method that agree with the interpretations based on the reference MIC. A value of >90% is targeted.
- Error Rates:
- Very Major Error (VME): The reference method calls the isolate "Resistant," but the INT method calls it "Susceptible." This is the most critical error to minimize.
- Major Error (ME): The reference method calls the isolate "Susceptible," but the INT method calls it "Resistant."
- Minor Error (mE): The result of one method is "Intermediate," and the other is either "Susceptible" or "Resistant."
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for INT Colorimetric MIC Assays
| Item | Function/Description | Example Sources / Notes |
|---|---|---|
| INT (2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride) | Colorimetric redox indicator; reduced by metabolically active bacteria to pink formazan | Sigma-Aldrich, Thermo Fisher; prepare fresh solution or store protected from light [69] |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing; ensures consistent ion concentration | BD Biosciences, Oxoid; mandatory for reliable, reproducible results [44] [6] |
| Quality Control Strains | Strains with well-defined MIC ranges to validate each assay run | ATCC (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) [68] [6] |
| Sterile 96-Well Microtiter Plates | Platform for conducting broth microdilution tests | Flat-bottom plates are preferred for accurate visual or spectrophotometric reading |
| Multichannel Pipettes | For efficient and accurate reagent and inoculum dispensing across the plate | Essential for minimizing technical variation and improving workflow efficiency |
Troubleshooting Common Issues Related to Controls
The diagram below outlines a logical approach to diagnosing and resolving common problems identified through control failures.
Title: Troubleshooting No Color in Positive Control
Issue: Unacceptable Variation in QC Strain MICs.
- Potential Cause: Inaccurate preparation of antibiotic stock solutions or serial dilutions.
- Solution: Confirm the purity and solubility of the antibiotic. Use calibrated pipettes and rigorously document the dilution process. Prepare fresh stock solutions if degradation is suspected [6].
Issue: Faint or Indistinct Color Change in All Wells.
- Potential Cause: Incubation time with INT was too short, the INT solution is degraded, or the inoculum density was too low.
- Solution: Extend the INT development time. Prepare a fresh INT stock solution. Verify the inoculum density via plating.
By systematically implementing this control framework, researchers can ensure that their INT colorimetric MIC data is robust, reproducible, and ready to inform critical decisions in both basic research and the drug development pipeline.
Validating Your Assay: Ensuring Reliability, Reproducibility, and Regulatory Compliance
The accurate determination of minimum inhibitory concentration (MIC) is a cornerstone of antimicrobial research and drug development. Within this field, the INT colorimetric assay has emerged as a vital tool, leveraging the reduction of 2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride (INT) to pink-colored INT-formazan by metabolically active cells [70] [71]. This color change provides a visual and spectrophotometric means to quantify microbial viability, making the assay particularly valuable for high-throughput screening of novel therapeutic compounds [70]. However, the reliability of this method hinges on the rigorous validation of its key analytical parameters. This application note provides detailed protocols and considerations for establishing the validation parameters of linearity, limit of detection (LOD), limit of quantitation (LOQ), precision, and accuracy, specifically contextualized within INT colorimetric assays for MIC determination. Robust method validation ensures that experimental results are scientifically sound, reproducible, and suitable for informing critical decisions in the drug development pipeline [72].
Core Validation Parameters: Definitions and Acceptance Criteria
For an analytical method like the INT colorimetric assay to be considered valid and "fit for purpose," a set of core performance characteristics must be empirically demonstrated [72]. The following parameters are fundamental, and their typical acceptance criteria for a well-developed assay are summarized in Table 1.
Table 1: Key Validation Parameters and Their General Acceptance Criteria
| Parameter | Definition | Typical Acceptance Criteria |
|---|---|---|
| Linearity | The ability of the method to obtain test results directly proportional to the analyte concentration [72]. | Coefficient of determination (r²) ≥ 0.990 (or correlation coefficient r ≥ 0.995) [54]. |
| Limit of Detection (LOD) | The lowest analyte concentration that can be reliably detected, but not necessarily quantified [73]. | Signal-to-noise ratio ~3:1 [74]. Analyte response should be distinguishable from the blank with a defined confidence level [73]. |
| Limit of Quantitation (LOQ) | The lowest analyte concentration that can be quantified with acceptable precision and accuracy [73]. | Signal-to-noise ratio ~10:1 [74]. Precision (RSD) ≤ 20% and Accuracy (%RE) within ±20% [73]. |
| Precision | The closeness of agreement between independent test results under stipulated conditions [72]. | Relative Standard Deviation (RSD) ≤ 15% for intermediate precision [54] [72]. |
| Accuracy | The closeness of agreement between the average value obtained from a large series of test results and an accepted reference value [72]. | Percent Relative Error (%RE) within ±15% [54]. |
Experimental Protocols for Parameter Determination
Linearity and Range
Principle: This protocol establishes the relationship between the concentration of the viable microorganism (as indicated by INT-formazan production) and the measured absorbance.
Materials:
- Test microorganism (e.g., E. coli, S. aureus)
- INT solution (e.g., 0.2 mg/mL in water or buffer)
- Appropriate culture medium (e.g., Mueller-Hinton Broth)
- Sterile 96-well microtiter plates
- Microplate reader capable of measuring absorbance at ~505-511 nm [70] [75]
Procedure:
- Prepare a series of microbial suspensions covering a range of expected densities (e.g., 10¹ to 10⁷ CFU/mL) using serial dilution in culture medium.
- Dispense 100 µL of each suspension into individual wells of a 96-well plate, including blanks containing medium only.
- Add 20-50 µL of INT solution to each well.
- Incubate the plate under optimal conditions for the test organism (e.g., 37°C for 1-4 hours) until a distinct pink color develops in the wells with the highest cell density.
- Measure the absorbance of each well at the predetermined λmax for INT-formazan (typically ~505 nm) [70].
- Data Analysis: Plot the mean absorbance of the blank-corrected readings against the logarithm of the microbial concentration. Perform linear regression analysis. The method is considered linear if the coefficient of determination (r²) meets or exceeds 0.990 [54].
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
Principle: LOD and LOQ can be determined based on the standard deviation of the blank response and the slope of the calibration curve, as per ICH Q2(R1) guidelines [74].
Materials:
- Sterile culture medium (blank matrix)
- Low-concentration microbial suspension (near the expected detection limit)
- INT solution and microplate reader
Procedure:
- Prepare the Blank: Measure the absorbance of at least 6-10 independent replicates of the blank (culture medium with INT, but no microorganisms).
- Prepare the Low-Concentration Sample: Prepare and measure at least 6-10 independent replicates of a low-concentration microbial suspension that is near the expected LOD/LOQ.
- Data Analysis:
- Calculate the standard deviation (SD) of the blank responses (SDblank) and the low-concentration sample responses (SDlow).
- Calculate the slope (S) of the linearity curve from section 3.1.
- Apply the ICH formulas [74]:
- LOD = 3.3 × σ / S
- LOQ = 10 × σ / S
- Where σ is the standard deviation of the response. This can be the standard error of the regression from the calibration curve, the SD of the blank, or the SD of the y-intercept of the regression line [74].
- Experimental Verification: Prepare and analyze a number of samples (e.g., n=6) at the calculated LOD and LOQ concentrations. The LOD concentration should produce a peak (absorbance signal) distinguishable from the blank. The LOQ concentration should demonstrate a precision (RSD) of ≤20% and an accuracy (%RE) of ±20% [73] [74].
Precision
Principle: Precision is assessed at multiple levels to account for variations occurring within a single run (repeatability) and between different runs, days, or analysts (intermediate precision) [72].
Materials:
- Microbial suspensions at three concentrations: low, medium, and high (within the linear range of the assay)
- INT solution and microplate reader
Procedure:
- Repeatability (Intra-assay):
- On the same day, using the same instruments and reagents, analyze the three concentrations with at least six replicates each.
- Calculate the Relative Standard Deviation (RSD) for each concentration.
- Intermediate Precision (Inter-assay):
- Repeat the assay for the three concentrations on three different days, with different analysts if possible.
- Calculate the RSD for each concentration across all the different runs.
- Acceptance Criteria: The precision is typically considered acceptable if the RSD is ≤15% for both repeatability and intermediate precision [54] [72].
Accuracy
Principle: Accuracy is measured by determining the recovery of known amounts of the analyte (microorganisms) spiked into the matrix.
Materials:
- Pre-quantified microbial stock solution
- Appropriate culture medium
- INT solution and microplate reader
Procedure:
- Prepare samples by spiking the blank matrix (culture medium) with known concentrations of the test microorganism at three levels (low, medium, high within the linear range).
- Analyze the spiked samples using the INT assay protocol.
- Data Analysis: Calculate the percent recovery for each level.
- % Recovery = (Measured Concentration / Known Concentration) × 100
- Acceptance Criteria: The method is accurate if the mean recovery at each level is within ±15% of the known value [54].
Workflow and Signaling Pathway Visualization
INT Assay Validation Workflow
The following diagram illustrates the logical sequence and decision points in the comprehensive validation of an INT colorimetric assay.
INT Formazan Formation Pathway
This diagram outlines the biochemical signaling pathway underlying the INT colorimetric assay, which is fundamental to its principle of detection.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for INT Colorimetric Assays
| Item | Function/Description | Example/Note |
|---|---|---|
| INT (Iodonitrotetrazolium Chloride) | Tetrazolium salt substrate; reduced by active microbial dehydrogenases/reductases to a pink formazan product [70] [71]. | Prepare a stock solution (e.g., 0.2 mg/mL) in water or buffer. Filter sterilize [70]. |
| Cell Culture Medium | Provides nutrients and environment to maintain microbial viability during the assay. | e.g., Mueller-Hinton Broth (for bacteria), RPMI-1640 (for fungi). Must be sterile [70]. |
| Microtiter Plates | Platform for high-throughput assay execution. | 96-well clear flat-bottom plates are standard. Polystyrene plates with high protein-binding capacity are typical [76]. |
| Microplate Reader | Instrument for quantifying the colorimetric signal. | Spectrophotometer capable of reading absorbance at 505-511 nm (λmax for INT-formazan) [70] [75]. |
| Reference Antimicrobials | Controls used to validate the assay system and for comparison with test compounds. | Use standard antibiotics with known MIC values (e.g., Ciprofloxacin, Fluconazole). |
| Buffer Systems | Maintain optimal pH for microbial growth and enzymatic (reductase) activity. | Phosphate-buffered saline (PBS), carbonate-bicarbonate buffer. pH 7.4 is commonly used [54] [76]. |
The rigorous validation of analytical parameters is not a mere formality but a fundamental requirement for generating reliable and meaningful MIC data using the INT colorimetric assay. By systematically determining linearity, LOD, LOQ, precision, and accuracy according to established protocols and acceptance criteria, researchers can ensure their methods are sensitive, reproducible, and accurate. This diligence is paramount in the context of drug discovery, where the INT assay serves as a powerful tool for the high-throughput screening of novel antimicrobial agents. A properly validated assay provides the confidence needed to make critical go/no-go decisions in the development pipeline, ultimately contributing to the fight against antimicrobial resistance.
The INT colorimetric assay represents a significant advancement in rapid minimum inhibitory concentration (MIC) determination, bridging the gap between classical phenotypic methods and modern rapid diagnostics. This protocol details the cross-validation of this colorimetric method against two established techniques: the Etest (epislometer test) and standard broth microdilution. We provide a comprehensive framework for evaluating the agreement between these methods, including standardized protocols, statistical analysis procedures, and criteria for interpreting validation results. The application of this cross-validation approach ensures that the INT assay meets the rigorous reliability standards required for research and potential clinical application in antimicrobial susceptibility testing (AST), particularly within the broader context of accelerating antibiotic discovery and combating multidrug-resistant pathogens.
The global rise of antimicrobial resistance (AMR) necessitates the development of rapid, reliable, and accessible antimicrobial susceptibility testing (AST) methods. The colorimetric microdilution assay has emerged as a promising tool, offering several advantages over traditional methods, including reduced turnaround time and the potential for automation [38]. These assays utilize oxidation-reduction indicators, such as INT (2,3,5-triphenyltetrazolium chloride) or resazurin, which undergo a visible color change in the presence of metabolically active bacteria, thereby providing a visual endpoint for MIC determination [38] [30].
Before a novel AST method can be widely adopted, it must be rigorously validated against internationally recognized reference methods. The Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptible Testing (EUCAST) endorse broth microdilution (BMD) as the reference standard for quantitative MIC determination [77] [78]. The Etest, a gradient diffusion method, is also widely used in clinical and research settings and provides a convenient and reliable approximation of the MIC [77] [78].
This application note provides a detailed protocol for cross-validating an INT colorimetric assay against these two established methods. The focus is on generating robust, reproducible data that accurately quantifies the correlation and agreement between the methods, ensuring the integrity of research findings in drug development and AMR surveillance.
Comparative Analysis of AST Methods
A clear understanding of the principles, strengths, and limitations of each method is fundamental to designing a valid cross-validation study. The following table summarizes the key characteristics of the three methods discussed in this protocol.
Table 1: Comparison of AST Methods Used in Cross-Validation
| Method Feature | INT Colorimetric Microdilution | Standard Broth Microdilution (Reference) | Etest (Gradient Diffusion) |
|---|---|---|---|
| Principle | Metabolic reduction of INT (colorless to red formazan) in liquid medium [38]. | Visual inspection of growth inhibition in liquid medium with serial drug dilutions [77] [78]. | Diffusion of antibiotic from a gradient strip to form an elliptical inhibition zone on agar [77] [78]. |
| Output | Minimum Inhibitory Concentration (MIC), IC50, IC90 [38]. | Minimum Inhibitory Concentration (MIC) [77]. | Minimum Inhibitory Concentration (MIC) read at the intersection of the ellipse and the strip [77]. |
| Time to Result | ~4-6 hours (post-incubation) [38] [30]. | 16-24 hours (standard incubation) [77]. | 16-24 hours (standard incubation) [77]. |
| Quantitative Nature | Quantitative | Quantitative | Semi-quantitative |
| Throughput | High (96-well format) | High (96-well format) | Low to Medium (individual strips) |
| Cost per Test | Low (standard microtiter plates) | Low (standard microtiter plates) | High (~$2-3 per strip) [78] |
| Key Advantage | Speed, objectivity with spectrophotometry, high-throughput. | Reference standard, high reproducibility. | Flexibility, ease of use, no specialized equipment needed. |
| Key Disadvantage | Optimization required for some fastidious organisms. | Subjective endpoint determination, longer turnaround. | Higher cost per test, limited scalability. |
The quantitative performance of these methods has been demonstrated in multiple studies. For instance, a validation study for a colorimetric method using 2,3,5-triphenyltetrazolium chloride (TTC) showed excellent linearity (R² > 0.95), precision (RSD <26%), and accuracy (75% to 122%) when correlated with viable cell counts [38]. Similarly, a study on the resazurin microplate method (RMM) for E. coli reported categorical agreement values ranging from 95.45% to 100% and essential agreement ratios from 82.72% to 100% when compared to the reference broth microdilution method [30].
Experimental Protocol for Cross-Validation
Materials and Reagent Preparation
Table 2: Research Reagent Solutions for INT Colorimetric Assay Cross-Validation
| Reagent/Material | Function/Application | Preparation and Storage |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for broth microdilution and INT assay to ensure reproducible cation concentrations. | Prepare according to manufacturer's instructions. Sterilize by autoclaving. |
| Mueller-Hinton Agar (MHA) Plates | Solid medium for Etest. Provides a standardized surface for antibiotic gradient diffusion. | Pour into sterile Petri dishes to a uniform depth of 4 mm. |
| INT (2,3,5-triphenyltetrazolium chloride) | Colorimetric indicator. Reduced by metabolically active bacteria to red formazan. | Prepare a 0.125% (w/v) stock solution in water. Sterilize by filtration (0.22 µm). Store protected from light at 4°C [38]. |
| Antibiotic Stock Solutions | Active pharmaceutical ingredients for MIC testing. | Obtain certified standard powders. Prepare stock solutions at high concentration (e.g., 5120 µg/mL or 10x the highest test concentration) in the appropriate solvent (water, methanol, DMSO). Store at -80°C in small aliquots [30]. |
| Etest Strips | Pre-defined antibiotic gradient strips for MIC determination on agar. | Store as recommended by the manufacturer, typically at -20°C or below. |
| Quality Control Strains | To verify the accuracy and precision of the test procedures. | Use ATCC strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213). Maintain on appropriate agar slants [30]. |
Workflow for Cross-Validation
The following diagram illustrates the integrated experimental workflow for the cross-validation study, from sample preparation through data analysis.
Figure 1: Integrated workflow for the cross-validation of INT assay with reference methods.
Detailed Step-by-Step Procedures
INT Colorimetric Microdilution Assay
This protocol is adapted from validated colorimetric methods [38] [30].
- Plate Preparation: Prepare a 96-well U-bottom microtiter plate with serial two-fold dilutions of the antimicrobial agent in CAMHB. The final volume in each well should be 50 µL. Include growth control (CAMHB + inoculum) and sterility control (CAMHB only) wells.
- Inoculation: Prepare a bacterial inoculum suspension equivalent to a 0.5 McFarland standard, then dilute it 1:10 in CAMHB to achieve approximately 1 x 10^7 CFU/mL. Add 50 µL of the diluted inoculum to all test and growth control wells. The final inoculum density is ~5 x 10^5 CFU/mL per well.
- Incubation and Staining: Incub the plate at 35 ± 2°C for 4 hours. After this pre-incubation, add 10-30 µL of the 0.125% INT solution to each well.
- MIC Determination: Continue incubation for another 1-2 hours. Monitor the growth control well for a color change from yellow to red. The MIC is defined as the lowest concentration of antibiotic that prevents this color change, indicated by a clear, yellow well. For objective results, measure the absorbance with a spectrophotometer (e.g., at 490-520 nm) after the incubation period. The MIC is the lowest concentration where absorbance falls below a predetermined threshold.
Reference Broth Microdilution Method
This method follows CLSI/EUCAST standards [77] [78] [30].
- Plate Setup: Prepare the microdilution plate identically to the INT assay (Steps 1-2 in section 3.3.1), but without the INT solution.
- Incubation: Incubate the plate at 35 ± 2°C for 16-20 hours.
- MIC Determination: After incubation, examine the wells for visible turbidity. The MIC is defined as the lowest concentration of antimicrobial agent that completely inhibits visible growth of the organism.
Etest Method
- Inoculation: Using a sterile swab, inoculate the surface of a Mueller-Hinton Agar (MHA) plate by swabbing in three directions to ensure a confluent lawn of growth from the prepared 0.5 McFarland suspension.
- Strip Application: Allow the plate surface to dry for a few minutes, then apply the appropriate Etest strip to the agar surface using forceps, ensuring full contact.
- Incubation: Incubate the plate at 35 ± 2°C for 16-20 hours.
- MIC Determination: After incubation, observe the symmetrical inhibition ellipse. The MIC value is read directly from the strip at the point where the edge of the inhibition ellipse intersects the strip.
Data and Statistical Analysis for Correlation
The correlation between the INT assay and the reference methods is assessed using two primary agreement metrics.
Table 3: Statistical Metrics for Method Correlation
| Metric | Definition | Acceptance Criterion |
|---|---|---|
| Essential Agreement (EA) | The percentage of MIC results from the new test (INT) that are within one two-fold dilution of the reference method (BMD) result. | ≥ 90% is considered acceptable. |
| Categorical Agreement (CA) | The percentage of results interpreted with the same susceptibility category (Sensitive, Intermediate, Resistant) by both methods, based on CLSI/EUCAST breakpoints. | ≥ 90% is considered acceptable. |
| Very Major Error (VME) | The reference method result is "Resistant," but the new test result is "Sensitive." (False Susceptible) | < 3% |
| Major Error (ME) | The reference method result is "Sensitive," but the new test result is "Resistant." (False Resistant) | < 3% |
The high agreement of colorimetric methods with reference standards is well-documented. For example, one study reported that the resazurin microplate method (RMM) showed essential agreement from 82.72% to 100% and categorical agreement from 95.45% to 100% for a panel of antibiotics against E. coli [30]. Furthermore, studies have confirmed that Etest exhibits strong agreement with broth microdilution, with sensitivity and specificity often exceeding 95% [78].
Application Notes and Troubleshooting
- Critical Step: The inoculum density and incubation time for the INT assay are critical. Deviations can lead to overestimation (too dense/inoculum) or underestimation (too dilute/inoculum) of the MIC. Always use fresh, log-phase cultures and standardize the turbidity carefully.
- Troubleshooting Atypical Results: If the color change in the INT plate is weak or absent, check the viability of the bacterial inoculum and the storage conditions of the INT solution, which should be protected from light and stored at 4°C. If there is significant discrepancy between the INT and BMD results, confirm that the antibiotic dilutions were prepared accurately and that the plates were incubated at the correct temperature.
- Assay Scope: While this INT assay is optimized for rapid-growing aerobic bacteria, modifications (e.g., extended incubation, specialized media) are necessary for slow-growing or fastidious organisms like Mycobacterium tuberculosis, where a resazurin-based assay (REMA) is well-established [79].
The cross-validation protocol outlined herein provides a robust and standardized framework for establishing the reliability of the INT colorimetric assay against the reference broth microdilution and the commonly used Etest. The demonstrated high degree of essential and categorical agreement, coupled with a significantly reduced time-to-result, positions the INT assay as a powerful tool for high-throughput screening in antibiotic development and antimicrobial resistance research. By adhering to this detailed protocol, researchers can generate validated, reproducible data that confidently contributes to the global effort against antimicrobial resistance.
In the context of research focused on INT colorimetric assays for minimum inhibitory concentration (MIC) determination, the reliability of results is paramount. Assessing precision through intra-assay and inter-assay repeatability metrics is a critical step in validating that your assay performs consistently, both within a single run and over multiple experiments. These metrics, typically expressed as the Coefficient of Variation (% CV), provide quantitative evidence that your colorimetric MIC results are robust and reproducible, thereby strengthening the conclusions of your research [80]. This document provides detailed protocols and application notes to guide researchers and drug development professionals in rigorously evaluating assay precision.
Defining Precision Metrics
Precision, the closeness of agreement between independent measurement results, is primarily assessed through two key metrics: intra-assay and inter-assay CV [81]. The CV is a dimensionless number calculated as the standard deviation of a set of measurements divided by their mean, expressed as a percentage [57] [81].
- Intra-Assay Precision (Repeatability): This measures the precision under the same operating conditions over a short interval of time. It reflects the well-to-well variability within a single assay plate or run [81] [80]. For an INT colorimetric MIC assay, this could involve testing multiple replicates of the same bacterial strain with a specific antibiotic concentration on one plate.
- Inter-Assay Precision (Within-Laboratory Precision): This measures the precision over longer time periods and under potentially varied conditions, such as different days, different operators, or different reagent lots. It reflects the plate-to-plate or run-to-run consistency [81] [80]. For MIC determination, this would involve repeating the same assay over several days to ensure consistent results.
The table below summarizes the typical acceptance criteria for these metrics in immunoassays and colorimetric methods, which can be applied to INT assay development.
Table 1: Acceptance Criteria for Precision Metrics
| Precision Type | Description | Typical Acceptance Criteria (% CV) | Relevance to INT Colorimetric MIC Assays |
|---|---|---|---|
| Intra-Assay | Variation within a single run or plate [80]. | < 10% [57] [80] | Ensures replicates at each antibiotic concentration yield consistent results in one test. |
| Inter-Assay | Variation between different runs, days, or operators [80]. | < 15% [82] [57] | Confirms that the MIC value for a control strain is reproducible across multiple experiments. |
Experimental Protocols for Precision Assessment
The following protocols are adapted from guidelines established by the Clinical and Laboratory Standards Institute (CLSI) and best practices in the field [81].
Protocol for Intra-Assay Precision (Repeatability)
This protocol determines the well-to-well variability in a single run.
Materials:
- Test samples (e.g., bacterial suspension with a known MIC in the mid-range of your assay)
- INT colorimetric assay reagents
- Microplate reader
- Calibrated pipettes and tips
Procedure:
- Prepare a homogenous test sample. For an MIC assay, this could be a bacterial suspension at a standard density treated with a specific antibiotic concentration.
- Aliquot this sample into a minimum of 10 replicates on the same microplate [80].
- Run the entire INT colorimetric assay procedure according to your established protocol (incubation, INT reagent addition, signal development).
- Measure the absorbance for each well using a microplate reader.
- Calculations:
- Calculate the mean absorbance and standard deviation (SD) for the 10 replicates.
- Compute the % CV using the formula: % CV = (SD / Mean) × 100 [57].
- The calculated % CV represents the intra-assay precision for that sample.
Protocol for Inter-Assay Precision
This protocol determines the variability of results between different assay runs performed over time.
Materials:
- Aliquots of at least two different test samples (e.g., low and high controls, or samples with different MICs) stored at -80°C or in conditions that ensure stability [81].
- INT colorimetric assay reagents from the same lot.
- Microplate reader
- Calibrated pipettes
Procedure:
- For each sample, run the assay in triplicate on each day [81].
- Repeat this process for a minimum of 5 days [81].
- On each day, perform the assay as per your standard operating procedure, ensuring to include fresh calibration curves and controls.
- Calculations (Using CLSI EP15-A2 Guidelines [81]):
- Calculate Repeatability (Within-Run Precision): This is similar to the intra-assay CV but pools the data from all days.
- For each day, calculate the mean of the triplicates.
- For each result on a given day, subtract the daily mean and square the resultant value.
- Sum all the squared differences from all days.
- Divide this sum by the degrees of freedom, which is the total number of days multiplied by (number of replicates per day - 1). The square root of this value is the repeatability SD (sr).
- Calculate Between-Run Variance (sb²):
- Calculate the overall mean of all results from all days.
- For each day, calculate the square of the difference between the daily mean and the overall mean.
- Sum these squared differences and use them to calculate the variance of the daily means.
- Calculate Total Within-Laboratory Precision (Inter-Assay SD):
- Use the formula: sl = √( sb² + sr² ) [81].
- Finally, calculate the inter-assay % CV: % CV = (sl / Overall Mean) × 100.
- Calculate Repeatability (Within-Run Precision): This is similar to the intra-assay CV but pools the data from all days.
The following workflow summarizes the key steps for assessing inter-assay precision:
Inter-Assay Precision Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Successful precision testing requires high-quality, consistent materials. The following table lists key research reagent solutions for INT colorimetric MIC assays.
Table 2: Essential Research Reagent Solutions for INT Colorimetric MIC Assays
| Item | Function/Description | Key Considerations for Precision |
|---|---|---|
| INT Reagent | (2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride). A tetrazolium salt reduced by metabolically active bacteria to a colored formazan product, serving as the colorimetric indicator [83]. | Consistent purity and preparation are critical. Use a standardized stock solution and storage conditions to minimize background variation. |
| Culture Media | The broth medium (e.g., Mueller-Hinton Broth) used to support bacterial growth during the antibiotic exposure. | Lot-to-lot consistency in pH and cation concentration is vital for reproducible antibiotic activity and MIC results. |
| Reference Strains | Quality control strains with well-defined and published MIC values (e.g., ATCC strains). | Used to validate each assay run. Stable, frozen stocks ensure long-term comparability of data. |
| Calibrated Pipettes | Instruments for accurate and precise liquid handling. | Regular calibration and maintenance are non-negotiable. Poor pipetting is a major source of high CVs [82] [57]. |
| Microplate Reader | Instrument for measuring absorbance of the formazan product. | Ensure the light source, filters, and optics are functioning correctly. Perform regular calibration checks [82]. |
Troubleshooting Poor Precision
If your intra- or inter-assay % CV values exceed acceptable limits, consider investigating these common issues:
- Pipetting Technique: This is a frequent cause of poor precision. Ensure pipettes are properly calibrated and that operators are trained in consistent technique. For viscous samples, pre-wetting pipette tips can improve accuracy [57].
- Reagent Contamination: Trace contamination of reagents with the analyte or other interfering substances can cause high variability. Handle reagents carefully and store them appropriately [82].
- Instrumentation: A failing microplate reader light source or optical component can introduce noise. Check the instrument's performance by reading an empty plate or a plate with a non-adsorbing liquid; the standard deviation between wells should be very low [82].
- Assay Procedure: Inconsistent washing (if applicable), incubation times, or temperatures can increase variation. Standardize all procedural steps [82].
In the context of research utilizing INT (2-(4-Iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride) colorimetric assays for minimum inhibitory concentration (MIC) determination, assessing the accuracy of the method is paramount. The spike recovery experiment serves as a fundamental quality assessment tool to evaluate an analytical method's accuracy and identify potential matrix effects [84]. It determines whether the presence of a sample matrix (such as bacterial lysate, growth media, or test compounds) interferes with the detection of the analyte, in this case, the formazan product formed by microbial metabolic activity.
A well-validated INT colorimetric assay for MIC determination must demonstrate that it can accurately quantify the target signal despite the complex sample background. Percentage recovery provides a quantitative measure of this capability, ensuring that MIC endpoints are reliable and reproducible for screening antimicrobial agents.
Quantitative Data on Recovery Acceptance
The acceptance criteria for percentage recovery are influenced by the sample matrix and the analyte's concentration. While specific recovery targets can vary, general guidelines derived from analytical chemistry provide a framework for evaluation [84]. The following table summarizes typical acceptance criteria for spike recovery in analytical methods:
Table 1: Typical Acceptance Criteria for Percentage Recovery
| Sample Matrix Complexity | Analyte Concentration Level | Acceptable Recovery Range (%) |
|---|---|---|
| Simple (e.g., buffer) | High | 95 - 105 |
| Simple (e.g., buffer) | Low | 90 - 107 |
| Complex (e.g., cell lysate) | High | 90 - 107 |
| Complex (e.g., cell lysate) | Low | 80 - 115 |
The calculation of percentage recovery is straightforward [84]: Percentage Recovery = (Measured Concentration of Spiked Sample / Expected Concentration) × 100
The expected concentration is the sum of the endogenous concentration (if any) and the spiked concentration.
Detailed Experimental Protocol for Spike Recovery
This protocol outlines the procedure for performing a spike recovery experiment to validate an INT colorimetric MIC assay.
Materials and Reagents
- INT Solution: Prepare a stock solution of INT in a suitable solvent (e.g., water or DMSO) at a defined concentration.
- Reducing Agent / Positive Control: Sodium hydrosulfite (dithionite) solution to chemically reduce INT to formazan, creating a standard spike solution [85].
- Sample Matrix: The biological matrix used in the MIC assay, such as:
- Sterile, uninoculated culture broth.
- Bacterial lysate from the target microorganism at a standard cell density (e.g., 1 × 10^8 CFU/mL), heat-killed to eliminate metabolic activity.
- Assay Medium: The complete medium used in the colorimetric assay, including all additives.
- Solvent for Formazan Dissolution: Dimethyl sulfoxide (DMSO) or isopropanol, if required to solubilize formazan crystals [85].
- Equipment: Microtiter plates, multi-channel pipettes, plate reader capable of measuring absorbance at 490-520 nm, incubator.
Procedure
Sample Preparation:
- Unspiked Sample (Endogenous Control): Add the sample matrix (e.g., 100 µL of bacterial lysate) to a microtiter plate well. Add the standard volume of assay medium. This sample measures the background signal.
- Spiked Sample: Add the sample matrix to a well. Spike with a known volume and concentration of the formazan standard solution (or INT solution + reducing agent). Add assay medium to the same total volume as the unspiked sample.
- Standard in Solvent: Add the same volume of the formazan standard spike to a well containing only assay medium. This sample represents the 100% recovery control, as there is no matrix interference.
- Blank: A well containing only assay medium.
Assay Execution:
- Follow the standard incubation and processing steps of your INT colorimetric MIC protocol.
- If the formazan product is insoluble, add the required volume of solvent (e.g., DMSO) to all wells to dissolve the crystals completely [85].
- Measure the absorbance of all samples at the appropriate wavelength (e.g., 490 nm for formazan).
Data Analysis:
- Calculate the net absorbance for each sample by subtracting the blank absorbance.
- The measured concentration for the spiked sample is derived from the net absorbance of the (spiked sample - unspiked sample).
- The expected concentration is derived from the net absorbance of the (standard in solvent).
- Calculate the percentage recovery using the formula provided in Section 2.
Figure 1: Experimental workflow for a spike recovery study.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their functions in the context of INT colorimetric assays and spike recovery experiments.
Table 2: Essential Research Reagents for INT Colorimetric Assays
| Reagent / Solution | Function / Explanation | Application in Protocol |
|---|---|---|
| INT (Tetrazolium Salt) | A yellow, water-soluble compound that is reduced to pink-red, insoluble formazan by metabolically active microbes; serves as the core indicator of cell viability [85]. | Used in the main MIC assay to detect microbial growth inhibition. |
| Formazan Standard | The reduced, colored product of INT. A pre-formed standard is used to spike samples without relying on enzymatic reduction, providing a known concentration for recovery calculations. | Used as the spike in recovery experiments to quantify accuracy. |
| Sodium Hydrosulfite (Dithionite) | A chemical reducing agent used to quantitatively convert INT to formazan for the preparation of the standard spike solution. | Preparation of the formazan standard solution. |
| Dimethyl Sulfoxide (DMSO) | An organic solvent used to dissolve water-insoluble formazan crystals, creating a homogeneous solution for accurate absorbance measurement [85]. | Added after incubation to solubilize formazan precipitates before reading the plate. |
| Cell Culture Medium & Lysis Buffer | Provides the sample matrix for the recovery study. The lysate mimics the chemical background of a real sample without introducing variable metabolic activity. | Serves as the complex matrix in which recovery is tested. |
Underlying Principles and Pathway
Spike recovery experiments validate the final, colorimetric readout step of the INT assay. The core principle being tested is that the generation of the formazan chromophore is linear and reproducible within the sample matrix. The biochemical pathway involves the acceptance of electrons from the microbial electron transport chain by the INT molecule, which is then reduced to the colored formazan. Matrix effects could potentially interfere with this process by quenching the signal, reacting with INT or formazan, or contributing to background absorbance.
Figure 2: INT assay signaling pathway and potential matrix interference points validated by spike recovery.
In drug discovery and development, the reliability of biological assays is paramount. Assay quality metrics, particularly the Z'-factor, serve as critical tools for researchers to quantitatively evaluate and validate the robustness of their experimental systems before embarking on high-throughput screening (HTS) campaigns [86]. This is especially true for colorimetric assays, such as those used for minimum inhibitory concentration (MIC) determination, where consistent and reproducible results are fundamental for accurately assessing compound efficacy. A well-characterized assay ensures that observed changes in signal are attributable to the compound's biological activity rather than systematic experimental noise, thereby protecting valuable resources and time from being wasted on false leads.
This application note provides a detailed framework for establishing assay robustness using the Z'-factor and related metrics, framed within the context of colorimetric MIC assays. It includes standardized protocols for assay execution and quantification, along with visualization of key concepts to aid implementation.
Theoretical Foundations of the Z'-Factor
The Z'-factor is a statistical metric specifically designed for the assessment of assay quality in HTS. Its primary utility lies in its use of positive and negative control data to predict the suitability of an assay for use in a screening environment, independent of test compounds [86].
Mathematical Definition
The Z'-factor is calculated using the means and standard deviations of the positive and negative control signals, as defined by the following equation [86]:
Z' = 1 - [ (3σ₊ + 3σ₋) / |μ₊ - μ₋| ]
Where:
- μ₊ and μ₋ are the mean signals of the positive and negative controls.
- σ₊ and σ₋ are the standard deviations of the positive and negative controls.
- |μ₊ - μ₋| represents the dynamic range, or signal window, between the controls.
The Z'-factor incorporates both the separation between the control means (the signal) and the variability of the control data (the noise) into a single, dimensionless value.
Interpretation of Z'-factor Values
The Z'-factor provides a clear, quantitative scale for judging assay quality, as summarized in the table below [86].
Table 1: Interpretation of Z'-factor Values
| Z'-factor Value | Assay Quality Assessment |
|---|---|
| Z' > 0.5 | An excellent assay. |
| 0 < Z' ≤ 0.5 | A marginal to weak assay. |
| Z' ≤ 0 | The assay is not usable. |
A Z'-factor greater than 0.5 indicates a robust assay with a wide dynamic range and low data variation, making it well-suited for HTS. It is important to note that while this threshold is a widely accepted benchmark, a more nuanced approach may be necessary for inherently variable assay types, such as complex cell-based models [87] [86]. For these, the fundamental interpretation of the Z'-factor remains, but the acceptable threshold might be adjusted based on the specific biological context and unmet need.
Establishing a Colorimetric MIC Assay Protocol
The following protocol details the steps for performing a broth microdilution MIC assay using a colorimetric readout, such as the reduction of a tetrazolium dye (e.g., XTT), to determine the minimum inhibitory concentration of antimicrobial compounds.
Principle
Viable metabolically active bacteria can reduce the yellow, water-soluble tetrazolium dye XTT to a water-soluble, orange formazan product. This conversion provides a colorimetric signal proportional to the number of live bacteria in a well [88]. In the presence of an effective antimicrobial compound, bacterial metabolism is inhibited, reducing formazan production and resulting in less color change.
Materials and Reagents
Table 2: Research Reagent Solutions for Colorimetric MIC Assay
| Reagent / Solution | Function |
|---|---|
| Cation-adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for MIC determination. |
| Bacterial Inoculum | Target microorganisms, prepared to a standardized density (e.g., 5 x 10⁵ CFU/mL) in CAMHB. |
| Antimicrobial Compound | Test agent, serially diluted in CAMHB. |
| XTT Solution | Chromogenic substrate (e.g., 0.5 mg/mL in PBS) [88]. Converted by live bacteria to formazan. |
| Menadione or Coenzyme Q | Electron-coupling agent added to enhance the efficiency of XTT reduction by bacteria [88]. |
| Positive Control (μ₊) | Growth control well (bacteria + media, no compound). |
| Negative Control (μ₋) | Sterility control well (media only, no bacteria or compound). |
Step-by-Step Procedure
- Plate Preparation: Dispense 100 µL of CAMHB into all wells of a sterile, clear-bottom 96-well microtiter plate.
- Compound Dilution:
- Add 100 µL of the highest concentration of the antimicrobial compound to the first well of a column.
- Perform two-fold serial dilutions across the plate using a multichannel pipette.
- Discard 100 µL from the final well to maintain equal volume.
- Inoculation:
- Add 10 µL of the standardized bacterial inoculum to all test and positive control wells.
- Add 10 µL of sterile CAMHB to the negative control (sterility) wells.
- Incubation: Seal the plate and incubate at 35±2°C for 18-24 hours under appropriate atmospheric conditions.
- Chromogenic Development:
- After incubation, add 20-50 µL of the prepared XTT/menadione solution to each well.
- Incubate the plate for a predetermined period (e.g., 1-4 hours at 37°C) to allow for color development [88].
- Absorbance Measurement: Measure the absorbance of each well at 450 nm (for XTT formazan) using a microplate reader.
Data Analysis and MIC Determination
- Calculate the mean absorbance (OD₄₅₀) for the negative controls (μ₋).
- The MIC is defined as the lowest concentration of the antimicrobial compound that results in an OD₄₅₀ ≤ μ₋ + 0.1 (or a predetermined threshold above the background).
- Visually, the MIC is the first well in the dilution series that shows no visible color change compared to the negative control.
Workflow for Assay Development and Validation Using Z'-factor
The following diagram illustrates the logical workflow for developing and validating a robust assay, culminating in the calculation and interpretation of the Z'-factor.
Advanced Considerations and Related Metrics
Robust Z'-factor for Complex Assays
For assays with data that deviates from a normal distribution, such as certain electrophysiological readings from neuronal cultures, a robust Z'-factor can be applied. This version uses the median and median absolute deviation (MAD) instead of the mean and standard deviation, making it less sensitive to outliers [87]. This approach was successfully used to achieve an "excellent" Z'-factor of 0.61 in a complex microelectrode array-based screening assay using primary neurons [87].
The Z-factor for Performance Monitoring
Once an assay is validated and screening commences, the Z-factor (or Z value) is used to monitor performance during the screen. It is calculated similarly to the Z'-factor but includes data from test samples, providing a measure of the actual screening assay quality [86].
Z = 1 - [ (3σₛ + 3σ꜀) / |μₛ - μ꜀| ]
Where s refers to the sample and c to the control. Its interpretation aligns with that of the Z'-factor.
Comparison of Quality Metrics
While the Z'-factor is a comprehensive metric, other parameters are also useful for assay characterization.
Table 3: Comparison of Common Assay Quality Metrics
| Metric | Formula | Application | Advantage |
|---|---|---|---|
| Z'-factor | 1 - [ (3σ₊ + 3σ₋)/|μ₊ - μ₋| ] | Assay development & validation; uses controls only. [86] | Predicts screening feasibility; incorporates dynamic range and variation. |
| Signal-to-Noise (S/N) | (μ₊ - μ₋) / σ₋ | General assay assessment. | Simple to calculate. |
| Signal-to-Background (S/B) | μ₊ / μ₋ | General assay assessment. | Simple to calculate. |
| Dynamic Range | |μ₊ - μ₋| | Understanding the absolute signal separation. | Intuitive. |
| Coefficient of Variation (CV) | (σ / μ) * 100 | Measuring data dispersion for a single control. | Standardized measure of variability, expressed as a percentage. |
The rigorous application of the Z'-factor and related metrics provides a solid statistical foundation for establishing robust and reliable colorimetric MIC assays. By systematically optimizing assay conditions, validating with controls, and calculating the Z'-factor, researchers can confidently generate high-quality data. This disciplined approach is essential for successful drug discovery, ensuring that downstream decisions are based on biologically relevant results rather than experimental artifact.
Conclusion
The INT colorimetric assay represents a significant methodological advancement in MIC determination, offering a simple, accurate, and material-efficient alternative to traditional techniques. By integrating a clear understanding of its foundational principles with a robust methodological protocol, proactive troubleshooting, and rigorous validation, researchers can reliably deploy this assay for high-quality antimicrobial susceptibility testing. The future of this technique is bright, with implications for accelerating the screening of novel antimicrobials, such as essential oils, in drug discovery pipelines. Further integration with digital color analysis tools and automation holds the potential to enhance throughput, reduce subjective interpretation, and establish this method as a gold standard in both research and clinical laboratories.
References
- 1. Validation of a standard method for determination of MIC ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701219302106]
- 2. In-Vitro Determination of Minimum Inhibitory ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037336/]
- 3. M07 | Methods for Dilution Antimicrobial Susceptibility ... [https://clsi.org/shop/standards/m07/]
- 4. MIC Determination [https://www.eucast.org/bacteria/methodology-and-instructions/mic-determination/]
- 5. Resources | Antimicrobial Susceptibility Testing, MIC [https://www.sanfordguide.com/stewardship/educational-resources/susceptibility-mic/?srsltid=AfmBOopP5w66X1QDiWYawisr1FUsvCy7b4Adbz7B2AZcq67yv9Xbp8XP]
- 6. Antimicrobial susceptibility testing to evaluate minimum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10448204/]
- 7. Tetrazolium - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/tetrazolium]
- 8. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 9. Colorimetric method for rapid detection of Oxacillin ... [https://www.nature.com/articles/srep23013]
- 10. Rapid Determination of Methicillin Resistance among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405631/]
- 11. Detecting antibiotic resistance: classical, molecular, advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531165/]
- 12. ColorPhAST: a visual rapid colorimetric assay for detecting ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1638204/full]
- 13. The golden age of colorimetry in diagnostics and drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624004308]
- 14. Colorimetric Detection and Quantification of Glutathione in ... [https://www.sciencedirect.com/science/article/pii/S1573412925000593]
- 15. Integrated Colorimetric and Fluorescent Assay Using Gold ... [https://link.springer.com/article/10.1007/s13206-025-00223-0]
- 16. The Minimum Inhibitory Concentration of Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913839/]
- 17. Agar dilution [https://en.wikipedia.org/wiki/Agar_dilution]
- 18. Agar and broth dilution methods to determine the minimal ... [https://www.nature.com/articles/nprot.2007.521]
- 19. Agar Dilution - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/agar-dilution]
- 20. Broth Dilution - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/broth-dilution]
- 21. Determination of minimum inhibitory concentration (MIC) [https://bio-protocol.org/exchange/minidetail?id=188211&type=30]
- 22. Comparison of Broth Microdilution, Agar Dilution, and Etest ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2937674/]
- 23. Comparison of Broth Microdilution, E Test, and Agar Dilution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC150256/]
- 24. Antimicrobial Activity of Some Essential Oils—Present ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5622393/]
- 25. Need for Susceptibility Testing Guidelines for Fastidious or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC344523/]
- 26. Fastidious and Furious: Reporting Antimicrobial ... [https://www.sciencedirect.com/science/article/abs/pii/S0196439917301046]
- 27. Methods for Determination of Antimicrobial Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11478843/]
- 28. Antibiotic susceptibility testing using minimum inhibitory ... [https://www.nature.com/articles/s44259-024-00051-6]
- 29. 2.4.2. Minimum Inhibitory Concentration and ... [https://bio-protocol.org/exchange/minidetail?id=17025503&type=30]
- 30. A New Colorimetric Method for Rapid Detection of ... [https://brieflands.com/journals/jjm/articles/119858]
- 31. A Q&A guide to stability storage [https://q1scientific.com/a-guide-to-stability-storage/]
- 32. E&L Study: ICH Stability Storage [https://gatewayanalytical.com/ich-stability-storage/]
- 33. Expiration Dating and Stability Testing for Human Drug ... [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-technical-guides/expiration-dating-and-stability-testing-human-drug-products]
- 34. Broth Dilution Method for MIC Determination • Microbe Online [https://microbeonline.com/minimum-inhibitory-concentration-mic-broth-dilution-method-procedure-interpretation/]
- 35. Quantitative Point-of-Care Colorimetric Assay Modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8412955/]
- 36. Methods for in vitro evaluating antimicrobial activity: A review [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762448/]
- 37. MIC Determination By Microtitre Broth Dilution Method - Hancock Lab [https://cmdr.ubc.ca/bobh/method/mic-determination-by-microtitre-broth-dilution-method/]
- 38. Colorimetric microdilution assay: Validation of a standard method for determination of MIC, IC50%, and IC90% of antimicrobial compounds - PubMed [https://pubmed.ncbi.nlm.nih.gov/31078627/]
- 39. Incubating and viewing plates [https://practicalbiology.org/standard-techniques/incubating-and-viewing-plates]
- 40. Setting up a colorimetric assay [https://www.ruf.rice.edu/~bioslabs/methods/protein/protcurve.html]
- 41. Rapid colorimetric for cellular growth and survival: application... assay [https://pubmed.ncbi.nlm.nih.gov/6606682/]
- 42. Colorimetric Detection - an overview [https://www.sciencedirect.com/topics/physics-and-astronomy/colorimetric-detection]
- 43. Colorimetric detection of mercury (Hg2+) using UV–vis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10073354/]
- 44. Antibiotic susceptibility testing using minimum inhibitory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721449/]
- 45. Colorimetric micro-assay for accelerated screening of ... [https://www.sciencedirect.com/science/article/abs/pii/S0964830512002892]
- 46. Antifungal Susceptibility Testing: Current Approaches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7194854/]
- 47. A colorimetric broth microdilution method for assessment of ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708517325876]
- 48. Detecting antibiotic resistance: classical, molecular ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1673343/full]
- 49. Development of a colorimetric loop-mediated isothermal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321649/]
- 50. Antimicrobial drug susceptibility testing for the ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1626930/full]
- 51. High Prevalence of hefA Efflux Pump Overexpression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561303/]
- 52. The development of a colorimetric biosensing assay for ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269722001932]
- 53. Ag- and Zn-clinoptilolite: a comparison of their in-vitro ... [https://link.springer.com/article/10.1007/s10653-025-02868-0]
- 54. Validation of UV-Vis spectrophotometric colorimetric ... [https://pubmed.ncbi.nlm.nih.gov/40366746/]
- 55. Characterization and optimization of a quantitative ... [https://www.sciencedirect.com/science/article/pii/S0925400524002971]
- 56. Certain Approaches to Understanding Sources of Bioassay ... [https://www.bioprocessintl.com/assays/certain-approaches-to-understanding-sources-of-bioassay-variability]
- 57. Calculating Inter- and Intra-Assay Coefficients of Variability [https://salimetrics.com/calculating-inter-and-intra-assay-coefficients-of-variability/]
- 58. Optimising cell-based bioassays via integrated design of ... [https://www.sciencedirect.com/science/article/pii/S2472555222137056]
- 59. Comparison of four different colorimetric and fluorometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2438350/]
- 60. A novel colorimetric broth microdilution method to determine the... [https://pubmed.ncbi.nlm.nih.gov/16076074/]
- 61. High-throughput clinical antimicrobial susceptibility testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12211026/]
- 62. Antibiotic susceptibility testing using minimum ... inhibitory [https://www.nature.com/articles/s44259-024-00051-6?error=cookies_not_supported&code=185a98cf-fbbf-46b3-992d-f5a296d950f0]
- 63. Incubation Times in Environmental Monitoring [https://www.bioprocessintl.com/qa-qc/a-case-study-in-environmental-monitoring-reviewing-incubation-times-upon-recovery-of-microorganisms]
- 64. Colorimetric Quantitation of in Vitro Cell Density Using ... [https://pubmed.ncbi.nlm.nih.gov/12206824/]
- 65. Colorimetric Cell Viability Assay [https://www.creative-bioarray.com/support/colorimetric-cell-viability-assay.htm]
- 66. Syringe Filters Solvent Compatibility Chart [https://www.restek.com/articles/syringe-filters-solvent-compatibility-chart?srsltid=AfmBOooVdZarwx2QGFRI8thGFc4A7NrTcw48kHHDa9XYLgxvgZxPQFon]
- 67. Methods for Determination of Antimicrobial Activity ... [https://www.mdpi.com/2223-7747/13/19/2784]
- 68. Agreement of Quantitative and Qualitative Antimicrobial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.570975/full]
- 69. Rapid colorimetric antimicrobial susceptibilities direct from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584658/]
- 70. Novel Tetrazolium-Based Colorimetric Assay for Helicase ... [https://www.mdpi.com/2673-6411/4/2/6]
- 71. Colorimetry - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/chemistry/colorimetry]
- 72. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 73. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 74. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 75. Development and validation of simple colorimetric methods for ... [https://bmcpharmacoltoxicol.biomedcentral.com/articles/10.1186/s40360-025-00916-0]
- 76. Overview of ELISA | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa.html]
- 77. 细菌耐药性检测技术方法及其应用 [https://www.jbjc.org/JBJC/html/article_9034.htm]
- 78. 综述:抗生素耐药性检测- 先进生物工程与人工智能增强策略 [https://www.ebiotrade.com/newsf/2025-10/20251006103842078.htm]
- 79. 使用刃天青微量滴定和棋盘测定法检测结核分枝杆菌的药物 ... [https://www.jove.com/cn/t/67672/detection-drug-susceptibility-drug-interactions-mycobacterium]
- 80. Why is ELISA lot-to-lot Reproducibility Critical for your ... [https://www.enzo.com/note/why-is-elisa-lot-to-lot-reproducibility-critical-for-your-research/]
- 81. Evaluating Assay Precision - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556577/]
- 82. ELISA Assay Qualification: Precision & Reproducibility Tips [https://www.cygnustechnologies.com/evaluating-precision-and-reproducibility-in-your-elisa?srsltid=AfmBOoqlyOEK22w3WL0QtBFfAfu7hpmEUrva-In56MPjfbSDBpvonf81]
- 83. Recent Advances in Colorimetric Tests for the Detection of ... [https://www.mdpi.com/2075-4418/13/14/2427]
- 84. 15.3: Quality Assessment - Chemistry LibreTexts [https://chem.libretexts.org/Courses/Northeastern_University/CHEM_1000%3A_General_Chemistry/15%3A_Quality_Assurance/15.3%3A_Quality_Assessment]
- 85. Colorimetric Cytotoxicity Assays [https://www.intechopen.com/chapters/83164]
- 86. The Z prime value (Z´) [https://www.bmglabtech.com/en/blog/the-z-prime-value/]
- 87. Adaptation of robust Z' factor for assay quality assessment in ... [https://pubmed.ncbi.nlm.nih.gov/32224158/]
- 88. Chromogenic Assay Measuring Opsonophagocytic Killing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC96095/]