Innovative Strategies for Biofilm Disruption in Persistent Infections: From Mechanisms to Clinical Applications
This article provides a comprehensive analysis of the current and emerging strategies to combat biofilm-associated persistent infections, which are responsible for 65-80% of all human microbial diseases and exhibit up...
Innovative Strategies for Biofilm Disruption in Persistent Infections: From Mechanisms to Clinical Applications
Abstract
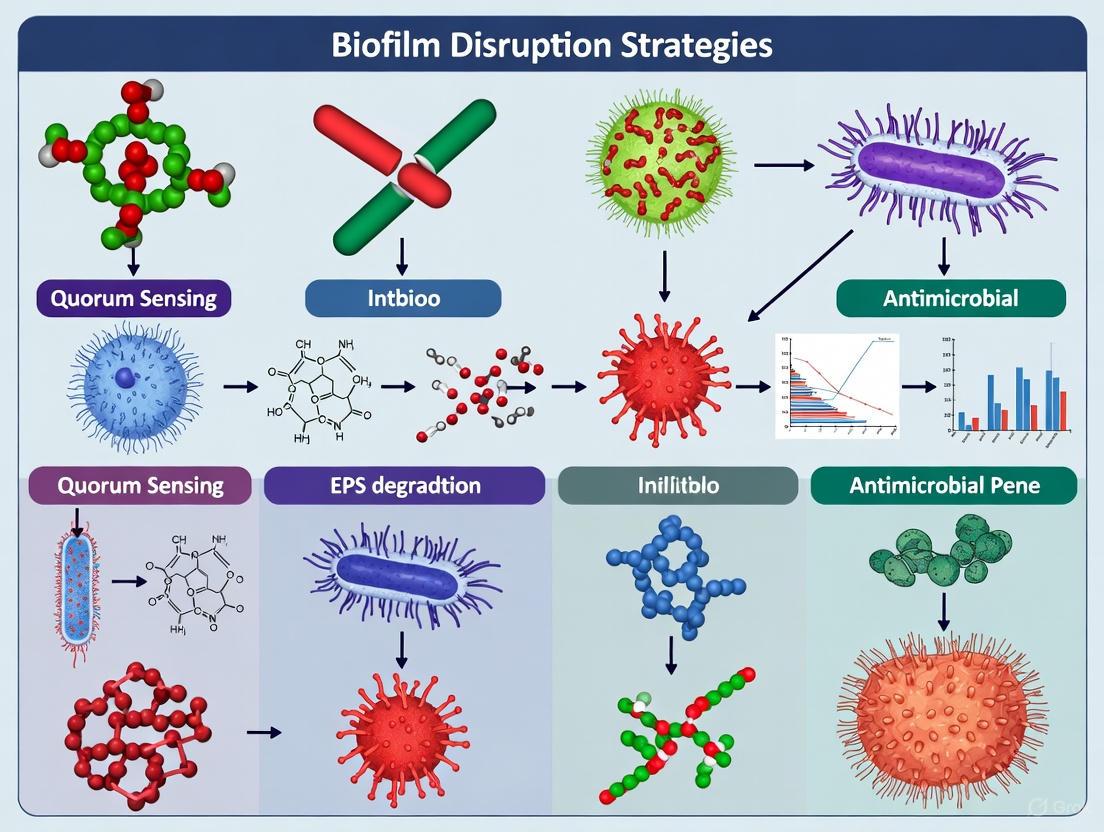
This article provides a comprehensive analysis of the current and emerging strategies to combat biofilm-associated persistent infections, which are responsible for 65-80% of all human microbial diseases and exhibit up to 1000-fold increased antibiotic resistance. Targeting researchers, scientists, and drug development professionals, it explores the complex biofilm lifecycle and resistance mechanisms, evaluates disruptive technologies including enzymatic agents, quorum sensing inhibitors, and nanoparticle-based delivery systems, addresses translational challenges from laboratory to clinical settings, and compares the efficacy of conventional versus novel therapeutic approaches. The synthesis of foundational science with applied clinical perspectives aims to bridge critical knowledge gaps and accelerate the development of effective anti-biofilm therapeutics.
Understanding Biofilm Pathogenesis: Architecture, Resistance Mechanisms, and Clinical Impact
Bacterial biofilms are complex, structured communities of microorganisms encased in a self-produced extracellular polymeric substance (EPS) matrix. They are a predominant form of microbial life and play a significant role in persistent infections, contributing to an estimated 65-80% of all human microbial infections [1]. The classic understanding of the biofilm lifecycle depicted a linear, five-stage process: reversible attachment, irreversible attachment, maturation I, maturation II, and dispersion [2]. However, contemporary research emphasizes that this model, largely based on in vitro studies of Pseudomonas aeruginosa, does not fully capture the diversity of biofilm development, especially in clinical, industrial, and natural environments [2] [1].
An expanded, more inclusive model conceptualizes the biofilm lifecycle around three core processes: aggregation, growth, and disaggregation [2] [1]. This model accommodates both surface-attached biofilms and non-surface-attached aggregates, which are now recognized as critical in many chronic infections, such as those in the viscous airway mucus of cystic fibrosis patients or in non-healing wounds [2]. Understanding this dynamic lifecycle is fundamental to developing effective strategies for biofilm disruption in persistent infections research.
Core Concepts and Definitions
To ensure clarity in troubleshooting and experimental design, the following definitions are provided [2]:
- Biofilm: A microbial aggregate attached to a surface or existing as a non-surface-attached aggregate, embedded in an extracellular matrix.
- Aggregation: Any biological, chemical, or physical process that allows microbial cells to form a cohesive group. This includes microbial growth, autoaggregation, and polymer depletion aggregation.
- Adherence/Attachment: The process by which suspended single cells or aggregates stick to a biotic or abiotic surface.
- Accumulation: The net result of attachment, aggregation, growth, disaggregation, and detachment processes that lead to the expansion or shrinkage of a biofilm.
- Disaggregation: The process by which aggregated cells, whether in suspension or surface-associated, shed smaller aggregates or individual cells into the fluid phase. This includes:
- Erosion: Loss of single cells or very small aggregates due to physical forces.
- Dispersal: A biologically regulated, active release of cells.
- Cohesive Fracture: The breakage of aggregates due to internal mechanical failure.
- Sloughing: The release of large, coherent layers of surface-attached biofilm.
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: Our anti-biofilm compound shows efficacy in microtiter plate assays but fails in more complex wound models. What could be the reason?
- Answer: This is a common translational challenge. Microtiter plate assays are valuable for high-throughput screening but are a significant simplification of in vivo conditions [3]. The failure likely stems from:
- Lack of Host Components: Simple models lack host-derived components like plasma, blood cells, and immune factors present in wound models (e.g., the Lubbock model), which can alter biofilm structure and increase tolerance to antimicrobials [3].
- Biofilm Maturity: Many in vitro models use 12-24 hour biofilms, whereas chronic wounds can harbor biofilms that are weeks old, exhibiting vastly different physiological states and resilience [3].
- 3D Architecture: Biofilms grown in 3D hydrogel models demonstrate different architecture and increased tolerance compared to 2D biofilms on plastic surfaces [3].
- Troubleshooting Guide:
- Validate Early: Incorporate more relevant models early in the discovery pipeline.
- Use Multiple Models: Do not rely solely on microtiter plates. Use a tiered approach, progressing from simple to complex models (e.g., microtiter plate → CDC biofilm reactor → 3D hydrogel or tissue culture model) to confirm activity [3].
- Check Compound Compatibility: Ensure your compound is not inactivated by host components like serum albumin.
FAQ 2: How can we effectively visualize and differentiate the biofilm matrix from bacterial cells without access to advanced microscopy?
- Answer: Advanced techniques like Confocal Laser Scanning Microscopy (CLSM) and Scanning Electron Microscopy (SEM) provide high-resolution images but are costly and complex [4] [5]. A recently developed, cost-effective alternative is the dual-staining method using Maneval's stain [5].
- Protocol: Dual-Staining with Maneval's for Biofilm Visualization [5]:
- Grow Biofilm: Grow biofilm on a sterile glass slide submerged in nutrient broth for 24-72 hours.
- Rinse: Gently rinse the slide in distilled water for 5 seconds to remove non-adhered cells.
- Fix: Fix the biofilm with 4% formaldehyde (in distilled water) for 15-30 minutes at room temperature.
- Stain with Congo Red: Apply 1% Congo red stain and allow it to air-dry completely.
- Stain with Maneval's: Treat the sample with Maneval's stain for 10 minutes.
- Visualize: Remove excess stain, air-dry, and observe under a light microscope with 100x oil immersion.
- Expected Outcome: Bacterial cells appear magenta-red, surrounded by a blue-stained polysaccharide biofilm matrix, allowing for clear differentiation [5].
FAQ 3: Why are biofilm-dispersing enzymes considered a promising strategy, and what are the main classes?
- Answer: Dispersing enzymes degrade the EPS that constitutes the protective shield of the biofilm. This strategy is promising because enzymes are highly specific, effective at low concentrations, and less likely to induce antibiotic resistance as they act extracellularly [1]. By breaking down the biofilm matrix, they revert protected sessile cells to a vulnerable planktonic state, making them susceptible to conventional antibiotics and host immune responses [1].
- The main enzyme classes and their targets are:
FAQ 4: What are the key reasons for the high antibiotic tolerance of biofilms, and how can our assays account for them?
- Answer: Biofilm tolerance is multifactorial. Your experimental models should be designed to probe these specific mechanisms [6] [1]:
- Physical Barrier: The EPS matrix can restrict antibiotic penetration.
- Metabolic Heterogeneity: Gradients of nutrients and oxygen within the biofilm create subpopulations of slow-growing or dormant persister cells that are highly tolerant to antibiotics [1].
- Altered Microenvironment: Conditions like low pH within the biofilm can neutralize some antibiotics.
- Troubleshooting Guide for Assay Design:
- Measure Penetration: Use fluorescently tagged antibiotics and CLSM to visualize penetration depth.
- Assay Metabolic State: Use probes like CTC for metabolic activity or stain for live/dead cells to identify heterogeneous zones.
- Test against Persisters: After antibiotic treatment, disrupt the biofilm physically and plate the cells to check for regrowth from dormant persister cells.
Key Signaling Pathways and Molecular Regulation
The transition from planktonic to biofilm growth is tightly regulated by molecular signaling. Two key systems are Quorum Sensing (QS) and the secondary messenger c-di-GMP.
Quorum Sensing (QS) Pathway
QS is a cell-cell communication process allowing bacteria to coordinate gene expression based on population density. This regulates collective behaviors, including biofilm formation and dispersal [7].
Diagram Title: Quorum Sensing Regulatory Pathway
c-di-GMP Signaling Pathway
Cyclic diguanylate (c-di-GMP) is a ubiquitous secondary messenger that acts as a central switch between motile and sessile lifestyles. High intracellular c-di-GMP promotes biofilm formation, while low levels favor dispersal and motility [6] [7].
Diagram Title: c-di-GMP Signaling Switch
Experimental Protocols for Biofilm Disruption
Protocol: Evaluating Biofilm Dispersal Enzymes
This protocol outlines a method for testing the efficacy of glycoside hydrolases, proteases, and DNases in disrupting pre-formed biofilms [1].
Workflow:
Diagram Title: Enzyme Dispersal Assay Workflow
Detailed Steps:
- Biofilm Growth: Grow a standardized biofilm (e.g., of Staphylococcus aureus or Pseudomonas aeruginosa) for 24-48 hours in a suitable model system (microtiter plate, Calgary device, or CDC biofilm reactor) [1].
- Enzyme Treatment: Gently wash the mature biofilm to remove non-adherent cells. Add the dispersal enzyme (e.g., DNase I, dispersin B, proteases) diluted in an appropriate buffer to the biofilm. Include a buffer-only negative control.
- Incubation: Incubate under optimal conditions for the enzyme (e.g., 37°C for 1-4 hours).
- Quantification of Dispersal:
- Crystal Violet Staining: Measure the remaining attached biomass after staining.
- ATP Assay: Measure the ATP content of dispersed cells in the supernatant as an indicator of released, viable biomass.
- Microscopy: Use light or confocal microscopy to visually confirm structural disintegration of the biofilm.
- Synergy with Antibiotics: Following enzyme treatment, add a conventional antibiotic to the system. Compare the reduction in viable cell counts (CFU/mL) between "antibiotic alone" and "enzyme + antibiotic" groups to demonstrate synergy.
Protocol: Advanced Microscopy for Anti-biofilm Evaluation (SEM)
SEM provides unparalleled image quality for assessing the ultrastructural effects of anti-biofilm treatments [4].
Key Steps:
- Fixation: Fix biofilm samples with a customized protocol, e.g., 2.5% glutaraldehyde, sometimes supplemented with ruthenium red or tannic acid to better preserve the EPS matrix [4].
- Dehydration: Dehydrate the sample through a graded ethanol series (e.g., 50%, 70%, 80%, 90%, 100%) [4] [5].
- Drying: Use critical point drying to avoid structural collapse from surface tension.
- Coating: Sputter-coat the sample with a thin layer of gold or another conductive material.
- Imaging and Analysis: Image the biofilm using SEM. Use image analysis software to extract quantitative parameters like biofilm coverage, roughness, or matrix thickness from the micrographs [4].
Research Reagent Solutions
The following table details key reagents and their applications in biofilm research.
| Reagent/Material | Function/Brief Explanation | Primary Application |
|---|---|---|
| Maneval's Stain [5] | A cost-effective staining solution that differentially stains bacterial cells (magenta-red) and the polysaccharide matrix (blue). | Visualization and differentiation of biofilm components using light microscopy. |
| Crystal Violet [8] [5] | A basic dye that binds to negatively charged surface molecules and polysaccharides, quantifying total adhered biomass. | Basic, high-throughput quantification of biofilm biomass. Not suitable for viability assessment. |
| Dispersin B [1] | A glycoside hydrolase enzyme that specifically hydrolyzes the poly-N-acetylglucosamine (dPNAG) exopolysaccharide. | Enzymatic dispersal of biofilms formed by pathogens like S. aureus and E. coli. |
| Deoxyribonuclease I (DNase I) [1] | An enzyme that degrades extracellular DNA (eDNA), a critical structural component in many bacterial biofilms. | Disruption of biofilms where eDNA is a major matrix constituent; reduces biofilm integrity. |
| Calcofluor White [5] | A fluorescent dye that binds to polysaccharides containing β-linked glucans (e.g., cellulose). | Fluorescence-based visualization of specific exopolysaccharides in the biofilm matrix. |
| c-di-GMP [6] | A key bacterial second messenger; high intracellular levels promote biofilm formation, low levels induce dispersal. | A critical target for small molecules aimed at manipulating the biofilm lifecycle. |
Quantitative Data on Biofilm Resistance and Enzyme Efficacy
The tables below summarize key quantitative data relevant to biofilm challenges and therapeutic strategies.
Table 1: Biofilm-Associated Challenges in Healthcare
| Metric | Value | Context / Significance |
|---|---|---|
| Percentage of Human Microbial Infections | 65 - 80% [1] | Highlights the clinical prevalence and importance of biofilms. |
| Estimated Global Economic Impact | ~$5 Trillion USD annually [3] | Includes health, food/water security, and industrial costs. |
| Chronic Wounds with Biofilms | 78.2% [3] | Systematic review finding, underscores role in chronicity. |
| Increased Antibiotic Tolerance | Up to 1000-fold [6] | Biofilm cells can be much more tolerant than planktonic cells. |
Table 2: Representative Biofilm-Dispersing Enzymes and Targets
| Enzyme Class | Example Enzyme | Target in EPS | Mechanism & Effect |
|---|---|---|---|
| Glycoside Hydrolase | Dispersin B [1] | dPNAG / PIA | Hydrolyzes β-1,6-glycosidic bonds in dPNAG, dissolving the structural scaffold for many staphylococcal and Gram-negative biofilms. |
| Protease | Proteinase K [1] | Matrix Proteins & Adhesins | Degrades proteinaceous components of the EPS and surface adhesins, disrupting biofilm integrity and attachment. |
| Deoxyribonuclease | DNase I [1] | extracellular DNA (eDNA) | Cleaves eDNA, which acts as a structural "glue" in many biofilms, leading to destabilization and dispersal. |
FAQ: Core Concepts and Composition
What is the primary function of the EPS matrix in bacterial biofilms? The extracellular polymeric substance (EPS) matrix is the fundamental component that establishes the functional and structural integrity of biofilms. It acts as a protective barrier, safeguarding microbial communities from harsh environmental conditions, including antibiotic attacks and host immune responses. The matrix provides mechanical stability, mediates interactions between cells, and is a source of nutrients and enzymes [9] [10]. Its complex structure limits the penetration of antimicrobial agents, contributing significantly to the high antibiotic tolerance observed in biofilm-based infections [10] [6].
What are the main chemical components of the EPS? The EPS is a complex, highly hydrated mixture of biomolecules, primarily consisting of polysaccharides, proteins, and extracellular DNA (eDNA). Other constituents include lipids and humic substances [9] [11]. The composition is not homogeneous and can vary significantly between different bacterial species and even between strains of the same species [10].
Table 1: Major Components of the Extracellular Polymeric Substance (EPS)
| Component Class | Key Subcategories | Primary Functions in the Biofilm Matrix |
|---|---|---|
| Polysaccharides | Exopolysaccharides (e.g., Alginate, Cellulose, Pel, Psl) | Form a scaffold and structural network; provide mechanical stability; act as a diffusion barrier; enable cell-surface and cell-cell interactions [9] [10] [6]. |
| Proteins | Structural proteins, Enzymes (e.g., proteases, glycosidases) | Stabilize biofilm architecture (structural proteins); degrade matrix components for nutrients and reorganization (enzymes) [10] [11]. |
| Extracellular DNA (eDNA) | - | Contributes to structural integrity and stability; facilitates horizontal gene transfer, including antibiotic resistance genes [10] [11]. |
| Lipids & Other Molecules | Lipids, Lipopolysaccharides, Humic substances | Contribute to matrix structure and properties; can influence hydrophobicity and adhesion [9] [11]. |
How does the EPS matrix confer resistance to antibiotics? The EPS matrix contributes to antibiotic resistance through multiple, interconnected mechanisms [10] [6]:
- Physical Barrier: The dense matrix physically hinders the diffusion of antibiotic molecules into the deeper layers of the biofilm, preventing them from reaching bacteria at bactericidal concentrations.
- Chemical Deactivation: Antibiotics can interact with and be deactivated by EPS components through binding, chelation, or enzymatic degradation (e.g., by β-lactamases).
- Physiological Heterogeneity: The biofilm structure creates gradients of nutrients, oxygen, and waste products. This leads to zones where bacterial cells enter a slow-growing or dormant state, making them less susceptible to many antibiotics that target active cellular processes.
- Facilitated Resistance Gene Transfer: The close proximity of cells within the EPS matrix enhances the exchange of genetic material, such as plasmids carrying antibiotic resistance genes.
FAQ: Analytical and Methodological Approaches
How can I analyze the overall chemical composition of a biofilm? Fourier Transform Infrared (FT-IR) Spectroscopy is a valuable technique for the non-destructive analysis of biofilm composition. It detects specific molecular vibrations from functional groups, providing a spectral fingerprint of the main biomolecule classes present [11].
Table 2: Key FT-IR Spectral Windows for Biofilm Analysis
| Spectral Range | Primary EPS Components Detected | Corresponding Functional Groups |
|---|---|---|
| 2800–3000 cm⁻¹ | Lipids | C-H, CH₂, CH₃ |
| 1500–1800 cm⁻¹ | Proteins | C=O, N-H, C-N (Amide I, Amide II bands) |
| 900–1250 cm⁻¹ | Polysaccharides, Nucleic Acids | C-O, C-O-C, P=O |
What methodologies can be used to assess the functional role of specific EPS components? The sensitivity of biofilms to specific enzymatic treatments is a direct method to determine the functional importance of different EPS constituents. If an enzyme causes biofilm disruption, its target molecule is critical for matrix integrity [11].
Experimental Protocol: Enzymatic Disruption of Biofilms
- Biofilm Growth: Grow biofilms in suitable media under static or dynamic conditions on surfaces compatible with your assay (e.g., 96-well plates, silicone tubes).
- Enzyme Preparation: Prepare fresh solutions of enzymes in an appropriate buffer. Common examples include:
- Proteases (e.g., Savinase, Subtilisin A): Target protein components.
- Glycosidases (e.g., α-amylase): Target polysaccharide components.
- DNases (e.g., DNase I): Target extracellular DNA (eDNA).
- Treatment: Gently wash the mature biofilms to remove non-adherent cells. Add the enzyme solution to the biofilm and incubate at the optimal temperature for enzyme activity for a defined period (e.g., 24 hours).
- Analysis: Quantify the remaining biofilm using methods like:
- Crystal Violet (CV) Staining: Measures total adhered biomass.
- Colony Forming Unit (CFU) Counting: Quantifies viable bacteria.
- Confocal Laser Scanning Microscopy (CLSM): Visualizes live/dead bacteria and biofilm structure in 3D.
Experimental Guide: Advanced Biofilm Disruption Strategies
Combined Shockwave and Antibiotic Therapy
Recent research highlights the efficacy of combining physical disruption methods with antibiotics. The following protocol is adapted from a 2025 study investigating the disruption of Pseudomonas aeruginosa biofilms in tubular structures, a model relevant to catheter-associated infections [12].
Detailed Experimental Protocol
Aim: To degrade biofilms on tubular structures and enhance subsequent antibiotic efficacy using shockwave treatment.
Materials:
- Bacterial Strain: Pseudomonas aeruginosa (e.g., KCTC 22073)
- Growth Medium: Tryptic Soy Broth (TSB) and Tryptic Soy Agar (TSA)
- Biofilm Substrate: Silicone tube (Inner diameter: 4 mm)
- Shockwave Source: Intravascular Lithotripsy (IVL) balloon catheter (e.g., Shockwave C2+)
- Antibiotic: Ciprofloxacin
- Staining Reagents: Crystal Violet (CV) solution, LIVE/DEAD BacLight Bacterial Viability Kit (SYTO9/PI)
- Equipment: Peristaltic pumps, confocal laser scanning microscope (CLSM), scanning electron microscope (SEM), sonication bath.
Procedure:
- Biofilm Formation:
- Circulate a diluted P. aeruginosa culture through the silicone tube system for 72 hours at 35°C using a pump.
- Continuously supply fresh TSB medium and air to promote robust biofilm growth [12].
- Treatment:
- Cut the biofilm-colonized tube into 3 cm long pieces.
- Shockwave Treatment: Place the sample in saline. Insert the IVL catheter and deliver shockwaves at 4 kV, 2 Hz for a total of 120 pulses (60 seconds).
- Antibiotic Treatment: Immediately after shockwave exposure, expose the biofilm to 4 µg/mL ciprofloxacin for 6 hours at 37°C.
- Analysis:
- Bacterial Viability:
- CFU Analysis: Sonicate and vortex treated samples to liberate bacteria, plate serial dilutions on TSA, and count colonies after 24h incubation.
- CLSM: Stain bacterial suspensions with SYTO9 (live, green) and PI (dead, red) to quantify live/dead ratios using image analysis software (e.g., ImageJ).
- Biofilm Detachment:
- Crystal Violet Staining: Stain the tube, dissolve the dye in ethanol, and measure optical density at 600 nm to quantify remaining biomass.
- SEM: Fix, dehydrate, and critically point-dry biofilm samples to visualize the structural integrity of the matrix.
- Bacterial Viability:
Expected Results: The combined treatment is expected to show significantly greater biofilm detachment (e.g., >97% surface area removal) and reduced bacterial viability (e.g., 40% reduction in CFU, 67% dead bacteria) compared to antibiotic treatment alone [12].
Targeting Intracellular Signaling for Biofilm Inhibition
Another strategic approach involves targeting the intracellular secondary messenger c-di-GMP, which centrally regulates the transition from planktonic to biofilm lifestyle. High intracellular levels of c-di-GMP promote the production of EPS components and adhesins, reinforcing biofilm formation [6].
Troubleshooting Guide: Common Issues in Biofilm Disruption Experiments
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| High variability in disruption assays (e.g., CV staining). | Inconsistent biofilm growth between replicates. | Standardize growth conditions (inoculum size, medium, temperature, flow rate for dynamic systems). Use internal controls in every experiment. |
| Enzyme treatment shows no effect. | Enzyme is inactive or cannot access its substrate within the dense matrix. | Use fresh, high-purity enzymes and verify their activity. Increase treatment time or combine with other matrix-disrupting agents (e.g., chelators) to improve access. |
| Shockwave treatment damages the underlying substrate. | Excessive energy or pulse number. | Optimize shockwave parameters (voltage, pulse count) in preliminary tests specific to your biofilm model. |
| Antibiotic alone is ineffective even after physical disruption. | Persister cells or high levels of inherited resistance. | Combine antibiotics with different mechanisms of action. Consider using anti-biofilm agents that target persister cells. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biofilm EPS Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Proteases (e.g., Savinase, Subtilisin A) | Degrade protein components of the EPS matrix; assess protein's role in integrity. | Disruption of P. aeruginosa and S. aureus biofilms [11]. |
| Glycosidases (e.g., α-amylase, Dispersin B) | Target polysaccharide components; study exopolysaccharide function. | Inhibition and detachment of S. aureus biofilms [10] [6]. |
| DNase I | Degrades extracellular DNA (eDNA); investigates eDNA's structural role. | Destabilization of biofilms where eDNA is a major matrix component (e.g., P. aeruginosa) [10]. |
| Crystal Violet (CV) | Stains total adhered biomass; standard quantitative and visual assessment of biofilms. | Measuring biofilm formation and detachment after experimental treatments [12]. |
| LIVE/DEAD BacLight Bacterial Viability Kit | Differentiates live (SYTO9, green) from dead (Propidium Iodide, red) cells via membrane integrity. | Confocal microscopy analysis of bactericidal effects after anti-biofilm treatment [12]. |
| Shockwave Intravascular Lithotripsy (IVL) Catheter | Generates high-pressure acoustic waves for the physical disruption of biofilm structure. | Loosening biofilm matrix on tubular structures to enhance antibiotic efficacy [12]. |
| Ciprofloxacin | Fluoroquinolone antibiotic; used to treat Gram-negative bacterial infections. | Assessing enhanced antibiotic killing following EPS disruption methods [12]. |
Molecular Mechanisms of Biofilm-Associated Antimicrobial Resistance
Within the context of developing strategies to disrupt persistent infections, understanding the molecular mechanisms of biofilm-associated antimicrobial resistance is a foundational prerequisite. Biofilms, which are structured communities of microorganisms encased in an extracellular polymeric substance (EPS), are a primary factor in chronic and recurrent infections [13]. Cells within a biofilm can exhibit a 10 to 1,000-fold increase in antibiotic resistance compared to their planktonic (free-floating) counterparts [14]. This dramatic tolerance makes biofilm-related infections—such as those associated with medical devices, cystic fibrosis lungs, and chronic wounds—notoriously difficult to treat [15] [16]. This technical resource details the core mechanisms behind this resistance and provides actionable experimental guidance for researchers in the field.
Frequently Asked Questions (FAQs): Core Concepts Explained
FAQ 1: What are the primary molecular mechanisms that drive antimicrobial resistance in biofilms? Biofilms employ a multi-layered defensive strategy that confers intrinsic resistance. The main mechanisms can be categorized as follows [14]:
- Physical Barrier: The EPS matrix, composed of exopolysaccharides, proteins, and extracellular DNA (eDNA), restricts the penetration of antimicrobial agents [15] [17].
- Metabolic Heterogeneity: Gradients of nutrients and oxygen within the biofilm create microenvironments where subpopulations of cells enter a slow-growing or dormant state, making them less susceptible to antibiotics that target active cellular processes [18] [1].
- Persister Cells: A small subpopulation of dormant bacterial cells, known as "persisters," exhibits extreme tolerance to antimicrobials. These cells are not genetically mutant but can repopulate the biofilm after antibiotic treatment is ceased [1] [17].
FAQ 2: How does the biofilm matrix physically impede antibiotic action? The EPS acts as a protective barrier through several interrelated processes [15] [19]:
- Diffration Limitation: The dense, anionic matrix physically slows down the diffusion of antimicrobial molecules into the deeper layers of the biofilm.
- Binding and Inactivation: Certain components of the matrix can directly bind and neutralize antibiotics. For example, positively charged aminoglycosides can be sequestered by negatively charged eDNA [15]. Additionally, enzymes like catalases within the matrix can inactivate antimicrobial molecules [17].
FAQ 3: What role does Quorum Sensing (QS) play in biofilm-associated resistance? Quorum Sensing is a cell-cell communication system that allows bacteria to coordinate gene expression based on population density. QS is a master regulator of biofilm development, including the production of the EPS matrix [13] [16]. By controlling biofilm maturation and architecture, QS indirectly contributes to the resistance phenotype. Disrupting QS signaling is therefore a key strategy being investigated for biofilm dispersal [20].
FAQ 4: Why are biofilms particularly problematic on medical devices? Medical devices, such as catheters and prosthetic joints, provide ideal abiotic surfaces for biofilm formation. It is estimated that approximately 65-80% of all human microbial infections are associated with biofilms, with a significant proportion being device-related [13] [1]. These biofilms act as a persistent source of infection, often requiring the removal of the device for successful treatment [13] [14].
Troubleshooting Guide: Common Experimental Challenges
| Challenge | Potential Root Cause | Suggested Solution |
|---|---|---|
| High variability in biofilm assays | Inconsistent inoculation; poorly controlled growth conditions (flow, temperature); surface properties of substrate. | Standardize pre-culture conditions; use controlled flow cells for consistent shear force; utilize reproducible surface coatings [15] [16]. |
| Unexpectedly low antibiotic tolerance in a known biofilm-forming strain | Biofilm not fully matured; incorrect antibiotic concentration or exposure time; over-aggressive washing during assay. | Extend biofilm growth time (e.g., 48-72 hrs); perform a Minimum Biofilm Eradication Concentration (MBEC) assay; validate maturity via microscopy or EPS staining [18] [16]. |
| Failure to disrupt biofilm with a matrix-targeting enzyme (e.g., DNase, protease) | Enzyme activity is compromised; enzyme cannot access its substrate within the complex matrix; incorrect enzyme selection for the target biofilm. | Verify enzyme activity prior to use; pre-treat with a combination of enzymes (e.g., DNase + protease) to synergistically degrade the EPS; confirm the presence of the enzyme's target in your biofilm model [1]. |
| Inability to eradicate persister cells | Standard bactericidal antibiotics are ineffective against dormant persisters. | Combine antibiotics with agents that disrupt the membrane potential or target persistent cell metabolism; use sequential treatment strategies [1] [19]. |
Quantitative Data: Biofilm Resistance Metrics
Table 1: Documented Increases in Antimicrobial Resistance in Biofilm vs. Planktonic Cells.
| Bacterial Species | Antibiotic | Fold-Increase in Resistance (Biofilm vs. Planktonic) | Context / Notes |
|---|---|---|---|
| Staphylococcus epidermidis | Vancomycin | ~Infinite (100% susceptible to completely resistant in biofilm) | Clinical isolates from device-related infections [14]. |
| Staphylococcus aureus | Various | Up to 1000x | General observation for this common pathogen [14]. |
| Pseudomonas aeruginosa | Tobramycin | Significantly decreased susceptibility | eDNA and host NETs form a protective shield in CF lung models [15]. |
| Klebsiella pneumoniae | Certain antibiotics | Highly resistant in biofilm, susceptible in planktonic state | Pattern observed in biofilm models [14]. |
Table 2: Key Enzymes for Experimental Biofilm Disruption.
| Enzyme Class | Target in EPS | Example Enzyme | Mechanism of Action in Biofilm Dispersal |
|---|---|---|---|
| Glycoside Hydrolases | Exopolysaccharides | Dispersin B | Hydrolyzes poly-β-1,6-N-acetyl-D-glucosamine (dPNAG), a key polysaccharide in many biofilms [1]. |
| Proteases | Protein adhesins & matrix proteins | Various proteases (e.g., Lysostaphin) | Degrades protein-based structural components and adhesins, destabilizing the biofilm architecture [1]. |
| Deoxyribonucleases (DNases) | Extracellular DNA (eDNA) | DNase I | Degrades the eDNA scaffold, which is crucial for biofilm structural integrity in many species [18] [1]. |
Experimental Protocols: Key Methodologies
Protocol 1: Assessing Biofilm Permeability to Antibiotics
Principle: To visualize and quantify the penetration and binding of an antibiotic within the biofilm matrix.
Materials:
- Fluorescently tagged antibiotic (e.g., Vancomycin-FL)
- Confocal Laser Scanning Microscope (CLSM)
- Mature biofilm grown in a suitable chamber (e.g., flow cell or ibidi µ-Slide)
- Phosphate Buffered Saline (PBS)
Procedure:
- Grow a mature biofilm (e.g., 48-72 hours) under conditions relevant to your study.
- Gently wash the biofilm with PBS to remove non-adherent cells.
- Introduce a solution of the fluorescently tagged antibiotic at the desired concentration and incubate for a set time (e.g., 30-90 minutes).
- Carefully wash again with PBS to remove unbound antibiotic.
- Immediately image using CLSM. Use Z-stacking to capture the 3D distribution of the fluorescent signal throughout the biofilm depth.
- Troubleshooting Tip: If fluorescence is weak, confirm the activity of the tagged antibiotic and consider increasing the incubation time. Use controls to rule out non-specific binding [15].
Protocol 2: Generating and Isoling Persister Cells
Principle: To enrich for and isolate the dormant, antibiotic-tolerant persister cell subpopulation from a biofilm.
Materials:
- Mature biofilm
- High concentration of a bactericidal antibiotic (e.g., Ciprofloxacin at 10-100x MIC)
- Centrifuge and microtubes
- Fresh growth medium
Procedure:
- Harvest a mature biofilm by gently scraping or sonicating at a low power to dislodge cells. Suspend in fresh medium.
- Treat the cell suspension with a high concentration of a bactericidal antibiotic for a prolonged period (e.g., 4-6 hours) to kill all non-persister cells.
- Centrifuge the treated suspension and carefully remove the supernatant containing the antibiotic.
- Wash the pellet twice with PBS to ensure antibiotic removal.
- Resuspend the pellet in fresh, antibiotic-free medium. The surviving cells are highly enriched for persisters.
- Troubleshooting Tip: Validate the success of the enrichment by plating the suspension on agar plates and comparing colony counts before and after antibiotic treatment. The persister-enriched population should show a significant reduction in viable count after treatment, with only a small fraction surviving [1] [17].
Visualization: Mechanisms and Workflows
Diagram Title: Molecular Mechanisms of Biofilm-Associated Resistance
Diagram Title: Biofilm Dispersal Therapy Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Biofilm Resistance.
| Reagent / Material | Primary Function in Biofilm Research | Example Application |
|---|---|---|
| Flow Cells | Enables growth of biofilms under controlled, continuous-flow conditions that mimic natural environments. | Studying biofilm architecture via microscopy and real-time penetration assays [15]. |
| Congo Red Dye | Binds to exopolysaccharides like cellulose and dPNAG; used to visually identify matrix production. | Qualitative assessment of biofilm-forming capability of bacterial colonies on agar plates. |
| DNase I | Degrades extracellular DNA (eDNA), a critical structural component in many biofilms. | Experimental disruption of biofilms to study the role of eDNA and as a potential dispersal agent [18] [1]. |
| Dispersin B | A specific glycoside hydrolase that degrades the dPNAG exopolysaccharide. | Targeted dispersal of biofilms formed by pathogens like S. aureus and E. coli that rely on dPNAG [1]. |
| Quorum Sensing Inhibitors (QSIs) | Blocks cell-to-cell communication signals, preventing coordinated biofilm development. | Research into anti-biofilm strategies that do not exert selective pressure for classic resistance [20] [16]. |
| Fluorescent Antibiotics (e.g., Vancomycin-FL) | Allows for direct visualization of antibiotic penetration and localization within a biofilm. | Confocal microscopy studies to quantify diffusion barriers and binding within the EPS matrix [15]. |
Biofilms represent a significant mode of microbial existence, characterized by structured communities of bacteria encased in a self-produced extracellular polymeric substance (EPS) and adhering to biotic or abiotic surfaces [21]. In healthcare settings, these biofilms are a major source of persistent infections, contributing substantially to patient morbidity, mortality, and escalated healthcare costs [22] [23]. The National Institutes of Health (NIH) estimates that up to 80% of all human infections are biofilm-associated, with over 65% of hospital-acquired infections linked to biofilms on medical devices [24]. This technical resource provides scientists and researchers with targeted troubleshooting guides, experimental protocols, and analytical frameworks to support research efforts aimed at understanding and disrupting biofilms within the context of persistent infections.
FAQs: Core Concepts and Epidemiological Data
1. What is the quantitative economic and clinical impact of biofilm-associated healthcare infections?
Biofilms exert a substantial economic and clinical burden globally. The annual global economic impact of biofilms is estimated to surpass $5 trillion [21]. In clinical terms, biofilm formation on medical devices is alarmingly common, with prevalence estimates ranging from 65% to 80% across various healthcare settings worldwide [23]. These infections lead to elevated patient morbidity and mortality, prolonged hospital stays, and increased treatment costs [22].
Table 1: Documented Resistance Patterns in Biofilm-Forming Pathogens from Clinical Surveillance
| Pathogen | Clinical Source | Key Resistance Findings | Susceptibility of Notable Antibiotics |
|---|---|---|---|
| Pseudomonas aeruginosa [22] | Respiratory, skin/soft tissue infections | 100% of isolates classified as MDR; 22.2% DTR; 5.4% PDR | Amikacin: 76.8%; Carbapenems: ~52%; Colistin: 43.8% |
| Staphylococcus aureus [22] | Hemodialysis patients | Both MRSA & MSSA formed strong biofilms; carried numerous virulence genes | Data not specified in source |
| Staphylococcus epidermidis [14] | Medical devices | 100% susceptible to vancomycin in planktonic state, but ~75% resistant when tested from a biofilm | Vancomycin (planktonic vs. biofilm): 100% vs. ~25% |
2. Why are biofilms inherently more resistant to antimicrobials and host immune responses?
Biofilms confer resistance through multiple, concurrent mechanisms [14]:
- Physical Barrier: The EPS matrix, composed of exopolysaccharides, proteins, and extracellular DNA (eDNA), restricts the penetration of antimicrobial agents and shields bacteria from immune cells [23] [25].
- Metabolic Heterogeneity: Gradients of nutrients and oxygen within the biofilm create microenvironments containing subpopulations of slow-growing or dormant "persister cells" that are highly tolerant to antibiotics [25] [14].
- Altered Microenvironment: Accumulated waste products and low oxygen zones within the biofilm can neutralize the activity of certain antibiotics, such as aminoglycosides [14].
- Enhanced Evasion: The biofilm matrix can shield bacterial pathogen-associated molecular patterns (PAMPs), dampening the host's immune recognition and response [25].
3. What are the primary methodological challenges in visualizing and quantifying biofilms?
Researchers face several challenges in biofilm analysis:
- Structural Preservation: Sample preparation for techniques like conventional Scanning Electron Microscopy (SEM) often involves dehydration, which can cause collapse of the delicate EPS matrix and lead to artifactual shrinkage [4].
- Matrix Differentiation: Simple staining methods like Crystal Violet and Congo Red often fail to differentiate the bacterial cells from the surrounding EPS matrix [5].
- Cost and Complexity: Advanced techniques such as Confocal Laser Scanning Microscopy (CLSM) and high-resolution SEM require expensive equipment and specialized expertise, making them inaccessible for some laboratories [4] [5].
Troubleshooting Guides for Common Experimental Issues
Problem 1: Inconsistent Biofilm Formation in Static Models
- Potential Cause: Inoculum density variation; inadequate nutrient availability; surface properties of substrate.
- Solution: Standardize the inoculum preparation to a specific optical density (e.g., 0.5 McFarland standard) [5]. Use consistent, nutrient-rich broth and ensure the surface (e.g., polystyrene, glass) is sterile and physiochemically uniform. Validate formation with a reliable staining method.
Problem 2: Failure to Eradicate Mature Biofilms with Antimicrobial Agents
- Potential Cause: Standard antibiotics are ineffective against dormant persister cells and cannot penetrate the EPS matrix sufficiently.
- Solution: Consider combination therapies. Incorporate quorum sensing inhibitors (e.g., thymoquinone, Tanreqing preparation) to disrupt cell communication and biofilm integrity [22]. Utilize biofilm-disrupting agents such as enzymes (e.g., DNase to target eDNA) or nitric oxide (NO)-releasing compounds that can trigger biofilm dispersal [22] [24].
Problem 3: Inability to Distinguish Bacterial Cells from EPS Matrix via Light Microscopy
- Potential Cause: Conventional stains like Crystal Violet bind indiscriminately to biomass.
- Solution: Employ the dual-staining method using Congo Red and Maneval's stain [5]. This cost-effective technique differentiates cells (appearing magenta-red) from the surrounding polysaccharide matrix (appearing blue) under a light microscope, providing clear structural visualization.
Essential Experimental Protocols
This protocol is ideal for laboratories without access to advanced microscopy for distinguishing biofilm components.
Research Reagent Solutions:
| Reagent/Material | Function |
|---|---|
| Maneval's Stain | Differentiates bacterial cells (magenta-red) and EPS matrix (blue). |
| Congo Red Dye (1%) | Initial stain that works in conjunction with Maneval's. |
| Formaldehyde (4%) | Fixes the biofilm structure, preserving its architecture. |
| Nutrient Broth | Medium for growing the biofilm. |
| Sterilized Glass Slide | Substrate for biofilm growth. |
Methodology:
- Biofilm Growth: Place a sterilized glass slide in a petri dish and submerge it in nutrient broth inoculated with a 1:100 dilution of a 0.5 McFarland standard bacterial suspension. Incubate undisturbed at 37°C for 3 days.
- Rinsing and Fixation: Gently rinse the slide by dipping it in distilled water for 5 seconds to remove non-adherent cells. Fix the biofilm by immersing the slide in 4% formaldehyde for 15-30 minutes at room temperature.
- Staining Procedure:
- Treat the fixed biofilm with 1% Congo red and allow it to air-dry completely.
- Apply Maneval's stain to the sample for 10 minutes.
- Remove excess stain and air-dry the slide.
- Visualization: Observe the biofilm under a light microscope using 100x oil immersion. Bacterial cells will appear magenta-red, surrounded by a blue polysaccharide layer.
This protocol is for high-resolution imaging of biofilm ultrastructure, though it requires careful handling to minimize artifacts.
Methodology:
- Primary Fixation: Rinse the biofilm-grown substrate gently and fix with 4% formaldehyde in 0.1 M phosphate-buffered saline (PBS) for 15-30 minutes.
- Secondary Fixation and Cross-linking: Post-rinse with PBS, cross-link the sample with 2.5% glutaraldehyde in 0.1 M PBS for 2 hours at 4°C.
- Dehydration: Dehydrate the biofilm through a graded ethanol series (50%, 70%, 80%, 90%, and 100%), allowing 10 minutes at each concentration.
- Critical Point Drying and Coating: Subject the dehydrated sample to critical point drying. Sputter-coat the dried sample with a fine layer of gold or another conductive material.
- Imaging: Visualize the biofilm structure using a field-emission scanning electron microscope.
Analytical Frameworks: Pathways and Workflows
Biofilm Formation and Quorum Sensing Pathway
The following diagram illustrates the key stages of biofilm development and the central role of Quorum Sensing (QS) in its regulation, representing a primary target for disruption strategies.
Experimental Workflow for Biofilm Disruption Screening
This workflow outlines a systematic approach for screening and evaluating potential anti-biofilm compounds.
Bacterial biofilms are structured communities of microbial cells embedded in a self-produced matrix of extracellular polymeric substances (EPS) that adhere to both biotic and abiotic surfaces [26]. The National Institutes of Health (NIH) has revealed that 60-80% of microbial infections are linked to biofilm formation, making them a principal concern in clinical settings [26]. Biofilms demonstrate dramatically enhanced resistance to antimicrobial compounds and host immune defenses compared to their free-floating (planktonic) counterparts, facilitating persistent infections that are difficult to eradicate [26] [27]. This resistance is multifactorial, arising from reduced antibiotic penetration due to the extracellular matrix, metabolic alterations in biofilm-resident bacteria, inactivation of antibiotics by matrix components, and increased exchange of bacterial resistance mechanisms [26].
Within the context of persistent infections research, understanding the distinct biofilm formation mechanisms of key pathogens is essential for developing effective disruption strategies. Staphylococcus aureus, Pseudomonas aeruginosa, and Haemophilus influenzae represent three clinically significant pathogens with diverse biofilm lifestyles that contribute substantially to the burden of device-related and chronic infections [26] [28] [29]. This technical resource provides troubleshooting guidance and methodological support for researchers investigating biofilm disruption strategies against these problematic pathogens.
Pathogen-Specific Biofilm Composition and Formation
Quantitative Comparison of Major Biofilm Components
Table 1: Key components of biofilm matrices for major pathogenic species
| Pathogen | Major Matrix Components | Primary Regulatory Systems | Clinical Significance |
|---|---|---|---|
| Staphylococcus aureus | PIA/PNAG (polysaccharide), eDNA, proteins (FnBPs, Bap, PSMs) [27] | icaADBC operon (PIA synthesis), Agr system (quorum sensing) [27] | Medical device infections, chronic wounds, osteomyelitis [29] |
| Pseudomonas aeruginosa | Psl, Pel, alginate (polysaccharides), eDNA, proteins [30] [31] | Las, Rhl, Pqs, Iqs (quorum sensing systems) [31] | Cystic fibrosis lung infections, ventilator-associated pneumonia, catheter-associated UTIs [26] [30] |
| Haemophilus influenzae | Extracellular DNA, proteins, polysaccharides (less defined) [28] | Autoinducer-2 (quorum sensing) [28] | Otitis media, chronic rhinosinusitis, respiratory tract infections [28] |
Visualizing Biofilm Developmental Pathways
Figure 1: Generalized biofilm development cycle with pathogen-specific elements
Troubleshooting Guides & FAQs
Experimental Design & Methodology
Q: What are the key considerations when selecting an in vitro biofilm model for antimicrobial efficacy testing?
A: The choice of biofilm model significantly impacts experimental outcomes. For preliminary, high-throughput screening, static models like microtiter plates are ideal. When evaluating antimicrobial treatments under relevant shear forces, dynamic models such as flow cells or CDC biofilm reactors are more appropriate [32]. Microcosm models that incorporate host components (e.g., hydroxyapatite for dental biofilms, human cell-coated surfaces) provide the most clinically relevant conditions but are more complex to establish [32]. Consider these key factors: your research question, required throughput, need for real-time observation, and available resources when selecting a model system.
Q: How can I optimize biofilm growth conditions for Haemophilus influenzae, particularly non-typable strains (NTHi)?
A: NTHi requires specific growth conditions for robust biofilm formation. Use brain heart infusion (BHI) broth supplemented with 2% Fildes enrichment and NAD (nicotinamide adenine dinucleotide) [28]. Incubate under microaerophilic conditions (5-10% CO~2~) at 35-37°C for 48-72 hours. For biofilm quantification, consider using the Calgary Biofilm Device which provides consistent shear force across all samples, promoting more uniform biofilm development [32]. Recent epidemiological studies indicate that ST103 and ST57 are predominant sequence types for NTHi, which may be valuable reference strains for method optimization [28].
Technical Challenges & Solutions
Q: What are the common reasons for inconsistent biofilm formation across experimental replicates?
A: Inconsistent biofilms typically result from these factors:
- Surface variability: Ensure identical surface materials and pretreatment across replicates
- Inoculum preparation: Standardize bacterial growth phase (mid-log phase recommended) and normalization methods
- Nutrient availability: Use fresh, properly prepared media with consistent lot numbers for critical components
- Environmental controls: Maintain stable temperature, humidity, and CO~2~ levels throughout incubation
- Shear force variation: In flow systems, calibrate pumps regularly to ensure consistent flow rates
For S. aureus, note that strain differences significantly impact biofilm formation capacity due to variable expression of adhesion factors and the icaADBC operon [27] [29]. Always include positive control strains with known biofilm-forming capabilities.
Q: How can I effectively disrupt mature biofilms for quantitative analysis without compromising bacterial viability?
A: Effective biofilm disruption requires matrix-specific approaches:
- Enzymatic treatment: Use combination cocktails including DNase I (targets eDNA), dispersin B (targets PNAG), or proteases (targets protein components) [33]
- Physical methods: Ultrasonication at optimized frequencies (20-40 kHz) with precise timing to minimize cell damage, or vortexing with glass beads for mechanical disruption
- Chemical agents: Dithiothreitol (DTT) can break disulfide bonds in matrix proteins, while chelating agents like EDTA disrupt cation-mediated matrix stability
Always validate disruption efficiency by comparing CFU counts before and after treatment and confirm complete disruption microscopically. Note that different pathogens and even strains may require optimized disruption protocols due to matrix composition differences [33].
Data Interpretation & Validation
Q: What controls are essential for proper interpretation of anti-biofilm experiments?
A: Implement a comprehensive control strategy:
- Viability controls: Planktonic cells of the same strain to distinguish biofilm-specific vs. general antimicrobial effects
- Matrix controls: Include matrix-deficient mutants (e.g., ica-negative S. aureus, psl/pel-negative P. aeruginosa) to confirm matrix-targeting mechanisms
- Treatment controls: Vehicle-only treatments to account for solvent effects
- Reference controls: Include approved antimicrobials with known anti-biofilm efficacy as benchmarks
- Neutralization controls: For time-kill assays, include appropriate neutralizers to prevent carry-over effect
Q: How can I distinguish between biofilm inhibition and biofilm eradication in experimental results?
A: These distinct outcomes require different experimental designs:
- Biofilm inhibition: Treat before or during biofilm formation, measure reduction in final biomass compared to untreated controls
- Biofilm eradication: Treat pre-established, mature biofilms (typically 24-72 hours old), measure reduction in existing biomass or viability
For P. aeruginosa, note that mucoid strains producing alginate demonstrate significantly enhanced eradication resistance compared to non-mucoid variants [30] [31]. Always report both the developmental stage at treatment initiation and the percentage reduction in viable counts or biomass to clearly communicate your findings.
Research Reagent Solutions
Table 2: Essential reagents and materials for biofilm research
| Reagent/Material | Primary Function | Application Notes |
|---|---|---|
| Polysaccharide Intercellular Adhesion (PIA) Antibodies | Detection and quantification of S. aureus biofilm matrix [27] | Specific for deacetylated PNAG; critical for distinguishing PIA-dependent biofilms |
| Dispersin B | Enzymatic disruption of PNAG/PIA polysaccharide [33] | Effective against S. aureus and S. epidermidis biofilms; used at 10-100 µg/mL |
| DNase I | Degradation of extracellular DNA in biofilm matrix [30] [31] | Particularly effective against P. aeruginosa and H. influenzae biofilms; use concentration 10-100 U/mL |
| N-Acetylcysteine | Mucolytic agent that disrupts disulfide bonds in matrix [33] | Effective against alginate-rich P. aeruginosa biofilms; working concentration 0.5-5 mg/mL |
| Calgary Biofilm Device | High-throughput production of uniform biofilms [32] | Provides reproducible biofilm samples for antimicrobial susceptibility testing |
| Crystal Violet | Total biofilm biomass staining and quantification [32] | Standard static biofilm assessment; measure absorbance at 570-595 nm after elution |
| Resazurin Reduction Assay | Metabolic activity measurement in biofilms [32] | Non-destructive alternative to CFU counting; fluorescence measurement (560/590 nm) |
| Syto 9/Propidium Iodide | Live/dead visualization of biofilm architecture [32] | Confocal microscopy analysis of biofilm viability and structure |
Experimental Protocols
Standard Microtiter Plate Biofilm Assay
This fundamental protocol adapts to all three pathogens with modifications:
- Inoculum preparation: Grow bacteria to mid-log phase (OD~600~ = 0.5-0.8) and dilute in appropriate broth to approximately 10^6^ CFU/mL
- Biofilm formation: Aliquot 200 µL/well into 96-well plates, incubate statically:
- Biofilm quantification:
- Carefully remove planktonic cells by rinsing 3× with PBS
- Fix with 200 µL 99% methanol for 15 minutes
- Air dry, then stain with 200 µL 0.1% crystal violet for 15 minutes
- Rinse thoroughly with water to remove unbound stain
- Elute bound stain with 200 µL 33% acetic acid
- Measure absorbance at 570-595 nm
Troubleshooting note: For H. influenzae, supplement media with NAD and hematin for optimal growth and biofilm formation [28].
Biofilm Antimicrobial Susceptibility Testing
Standardized methods for evaluating anti-biofilm compounds:
- Biofilm establishment: Grow biofilms as described in section 5.1
- Treatment application: Replace medium with fresh medium containing test compounds at desired concentrations
- Incubation: Incubate for appropriate time based on compound mechanism (typically 24 hours)
- Viability assessment:
- Option 1: Disrupt biofilms by sonication or scraping, then perform serial dilution and plating for CFU enumeration
- Option 2: Use metabolic assays (XTT, resazurin) for indirect viability measurement
- Biomass assessment: Perform crystal violet staining as in section 5.1 to determine biomass reduction
Key consideration: For P. aeruginosa, note that aminoglycoside resistance is enhanced by Pel polysaccharide, while colistin resistance involves multiple matrix components [30] [31]. Always include both planktonic and biofilm-treated samples to determine biofilm-specific resistance ratios.
Advanced Methodologies
Flow Cell Biofilm Analysis for Real-Time Observation
Flow cells provide unparalleled analysis of biofilm architecture and development dynamics:
Figure 2: Flow cell biofilm analysis workflow with pathogen-specific modifications
Molecular Analysis of Biofilm Regulation
Key pathways and their investigation:
Quorum Sensing Inhibition Studies
- P. aeruginosa: Target LasR/LasI and RhlR/RhlI systems with furanone compounds or natural inhibitors [31]
- S. aureus: Target Agr system with RNAIII-inhibiting peptide (RIP) or ambuic acid analogs [27]
- H. influenzae: Investigate autoinducer-2 (AI-2) interference strategies [28]
Gene Expression Analysis in Biofilms
- Extract RNA from mechanically disrupted biofilms
- Validate reference genes for biofilm conditions (gyrA, rpoB often more stable than 16S rRNA)
- Key regulatory targets:
This technical support resource provides foundational methodologies and troubleshooting guidance for researchers developing biofilm disruption strategies against these clinically significant pathogens. As biofilm research evolves, continue to validate these approaches against emerging models and clinical isolates to ensure translational relevance.
Emerging Anti-Biofilm Technologies: From Enzymatic Disruption to Nanotechnology
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My glycoside hydrolase treatment failed to disperse a mature S. aureus biofilm in an in vivo wound model, even though it worked in vitro. What could be the reason?
A: This is a common issue related to the model system and potential changes in the biofilm's extracellular polymeric substance (EPS) composition. Biofilms grown in vivo often have a different EPS structure compared to those grown in simple in vitro systems [34]. S. aureus produces poly-N-acetylglucosamine (PNAG) as a key exopolysaccharide [35]. If your chosen glycoside hydrolase (e.g., cellulase or α-amylase) does not target the specific linkages in PNAG, it will have limited efficacy. It is crucial to select an enzyme, such as dispersin B, that specifically hydrolyzes β-1,6 linkages in PNAG [36] [35]. Furthermore, the in vivo environment includes host components that can integrate into the biofilm, potentially altering its architecture and accessibility to enzymes [34].
Q2: I am observing a strong inflammatory response in my animal model following successful enzymatic biofilm dispersal. Is this expected, and how can it be managed?
A: Yes, this is an expected consequence of effective biofilm disruption. Biofilms act as a physical shield, sequestering pathogens from the host immune system [36] [35]. Dispersing the biofilm releases a sudden, high load of planktonic bacteria and EPS components, triggering a significant localized immune response [37]. To manage this in an experimental setting, consider the following:
- Antimicrobial Synergy: Always pair enzymatic dispersal agents with an appropriate antibiotic. The goal of dispersal is to convert tolerant sessile cells into susceptible planktonic cells, which can then be killed by the antimicrobial, thereby reducing the antigenic load [38] [35].
- Monitor Host Response: Include biomarkers of inflammation (e.g., cytokine levels, neutrophil infiltration) as key metrics in your study to quantify this effect [35].
Q3: How do I determine the optimal concentration and treatment duration for a novel protease against a Pseudomonas aeruginosa biofilm?
A: A systematic, empirical approach is required, as efficacy is strain and model-dependent.
- Start with In Vitro Screening: Use a standard assay like a crystal violet biomass assay or a dispersal assay to test a range of enzyme concentrations (e.g., 0.0025% to 5%) and treatment times (e.g., 2 minutes to 2 hours) on pre-formed biofilms [38].
- Validate with Viability Counts: Follow up with colony forming unit (CFU) counts of both dispersed and remaining biofilm-associated cells to confirm that dispersal is increasing antibiotic efficacy without exhibiting bactericidal activity itself [38].
- Progress to Complex Models: Confirm the optimal dose in a more clinically relevant model, such as a wound microcosm or an in vivo infection model, as efficacy can differ significantly from in vitro results [34].
Q4: Can enzymatic agents effectively disrupt polymicrobial biofilms, and are there any special considerations?
A: Yes, enzymes can be effective against polymicrobial biofilms, which are common in clinical infections like chronic wounds [38]. However, the EPS composition might be more complex. A combination of enzymes targeting different components (e.g., a glycoside hydrolase with a DNase or protease) may be more effective than a single enzyme, as it can target the diverse structural elements contributed by different species [35]. Research shows that a 1:1 mixture of α-amylase and cellulase was effective at dispersing a dual-species S. aureus and P. aeruginosa biofilm [38].
Experimental Protocols
Protocol 1: In Vitro Well-Plate Biofilm Dispersal and Assessment
This protocol is adapted from methods used to evaluate glycoside hydrolase efficacy against mono- and dual-species biofilms [38] [34].
Objective: To quantify the dispersal efficacy of an enzymatic agent on a pre-formed biofilm in a 24-well plate format.
Materials:
- Bacterial strains (e.g., P. aeruginosa PAO1, S. aureus SA31)
- Glycoside hydrolase solution (e.g., α-amylase, cellulase) in 1x PBS
- 24-well non-tissue culture-treated plates
- Phosphate Buffered Saline (PBS)
- Crystal violet stain (0.1%) or materials for CFU plating
Method:
- Inoculation: Inoculate wells with 10^5 CFU of bacteria in 800 μL of appropriate growth medium. For polymicrobial biofilms, include 20% adult bovine serum to prevent one species from outcompeting the other [34].
- Biofilm Growth: Incubate plates for 48 hours at 37°C with gentle shaking (80 rpm).
- Rinsing: Gently remove the supernatant and rinse each well with 1 mL of PBS to remove non-adherent planktonic cells.
- Enzyme Treatment: Add 1 mL of the enzyme solution (or PBS vehicle control) to each well. Incubate for a predetermined time (e.g., 30 min to 2 h) at 37°C with shaking [38].
- Analysis:
- Biomass Assessment (Crystal Violet): After treatment, remove supernatant, stain biofilm with crystal violet, and elute for spectrophotometric quantification [38].
- Dispersal Assessment (CFU Count): Collect the treatment supernatant ("dispersed fraction"). Add 1 mL PBS to the well and sonicate or homogenize to resuspend the remaining biofilm ("biofilm fraction"). Serially dilute both fractions and spot plate to determine CFU counts. Calculate percent dispersal as: (Dispersed CFU / Total CFU) * 100 [34].
Troubleshooting Tip: If dispersal is low, confirm enzyme activity and test a range of concentrations. Heat-inactivated enzyme should be used as a negative control to rule out non-specific effects [38].
Protocol 2: In Vivo Murine Chronic Wound Biofilm Model for Enzyme Efficacy
This protocol outlines a method for assessing enzymatic dispersal in a clinically relevant animal model [38] [34].
Objective: To evaluate the efficacy of a dispersal enzyme on biofilms established within a murine wound.
Materials:
- Mice (e.g., SKH1-Elite immunocompromised mice for chronic wound model)
- Bacterial inoculum
- Enzyme solution in 1x PBS
- Surgical tools for wound creation and biofilm extraction
Method:
- Wound Creation and Infection: Create a full-thickness wound on the dorsal surface of an anesthetized mouse. Infect the wound with the bacterial strain(s) of interest and cover with a semi-occlusive dressing [34].
- Biofilm Establishment: Allow the biofilm to develop for 3-7 days.
- Biofilm Extraction and Ex Vivo Treatment: Euthanize the animal and surgically extract the biofilm-containing wound bed tissue.
- Treatment: Weigh the extracted tissue and treat it ex vivo with the enzyme solution or a control for 1 hour at 37°C with shaking [38].
- Analysis:
- Biomass Degradation: Weigh the tissue after treatment and calculate the percent reduction in weight compared to the control [38].
- Cell Dispersal: After treatment, serially dilute the treatment solution ("dispersed fraction") and homogenize the remaining tissue ("biofilm fraction") to determine viable CFU counts and calculate percent dispersal [38].
Troubleshooting Tip: The in vivo biofilm microenvironment is complex. Include a group that receives enzyme followed by a systemic antibiotic to demonstrate the full therapeutic potential of the dispersal strategy [38].
Research Reagent Solutions
Table 1: Key Enzymatic Agents for Biofilm Dispersal and Their Applications
| Reagent | Target | Function in Biofilm Dispersal | Example Applications |
|---|---|---|---|
| α-Amylase [38] [34] | α-1,4 glycosidic linkages | Hydrolyzes polysaccharides with α-1,4 bonds (e.g., starch, P. aeruginosa Pel polysaccharide) [34]. | Dispersal of P. aeruginosa and S. aureus mono- and polymicrobial biofilms [38]. |
| Cellulase [38] [34] | β-1,4 glycosidic linkages | Hydrolyzes polysaccharides with β-1,4 bonds (e.g., cellulose, P. aeruginosa Psl and Alginate) [38] [34]. | Dispersal of P. aeruginosa and Burkholderia cepacia biofilms; effective in polymicrobial wound biofilms [38]. |
| Dispersin B [38] [35] | β-1,6 glycosidic linkages in PNAG | Specifically hydrolyzes poly-N-acetylglucosamine (PNAG), a key biofilm polysaccharide in many bacteria [35]. | Prevention and disruption of biofilms from Staphylococcus aureus, Escherichia coli, and other PNAG-producing pathogens [38]. |
| Proteases (e.g., Trypsin, Proteinase K) [35] | Proteinaceous adhesins and matrix proteins | Degrades protein components within the EPS, disrupting structural integrity and cellular adhesion [35]. | Dispersal of biofilms where proteins are a major matrix component; often used in combination with other enzymes [35]. |
| Deoxyribonucleases (DNases) [35] | Extracellular DNA (eDNA) | Hydrolyzes the eDNA backbone, a crucial structural and adhesive component in many bacterial biofilms [35]. | Dispersal of biofilms from species like P. aeruginosa and S. aureus that rely on eDNA for matrix stability [35]. |
Table 2: Quantitative Efficacy of Glycoside Hydrolases in Different Biofilm Models
| Biofilm Model | Species | Enzyme | Concentration | Key Quantitative Result | Reference |
|---|---|---|---|---|---|
| In Vitro Well-Plate | S. aureus & P. aeruginosa (coculture) | α-Amylase | 0.25% | Significant reduction in biofilm biomass (crystal violet assay) [38]. | |
| In Vitro Well-Plate | S. aureus & P. aeruginosa (coculture) | Cellulase | 0.25% | Significant reduction in biofilm biomass (crystal violet assay) [38]. | |
| In Vitro Well-Plate | S. aureus & P. aeruginosa (coculture) | α-Amylase & Cellulase (1:1) | 5% | Significant increase in total cell dispersal compared to vehicle control [38]. | |
| Ex Vivo Murine Wound | S. aureus & P. aeruginosa (coculture) | α-Amylase | 5% | Degraded biofilm biomass and increased bacterial cell dispersal from infected wound beds [38]. | |
| Ex Vivo Murine Wound | S. aureus & P. aeruginosa (coculture) | Cellulase | 5% | Degraded biofilm biomass and increased bacterial cell dispersal from infected wound beds [38]. | |
| In Vitro Microcosm | S. aureus (monospecies) | Cellulase | 5% | Striking loss of dispersal efficacy compared to in vitro well-plate model [34]. |
Experimental Workflows and Pathways
Biofilm Dispersal Experimental Workflow
Enzyme Targeting of Biofilm EPS
Quorum Sensing Inhibitors and Signal Interference Strategies
Frequently Asked Questions (FAQs)
1. What is the primary advantage of using Quorum Sensing Inhibitors (QSIs) over traditional antibiotics? QSIs offer a novel anti-virulence strategy by disrupting bacterial communication without exerting a lethal selection pressure. This approach can attenuate pathogenicity and biofilm formation, thereby reducing the likelihood of resistance development compared to conventional antibiotics that kill or inhibit growth and promote resistance selection [39] [40].
2. Why are my QSI assays against Pseudomonas aeruginosa showing inconsistent results? P. aeruginosa possesses multiple, redundant QS systems (Las, Rhl, PQS, IQS). Inhibiting only one pathway may be insufficient due to compensatory crosstalk. For consistent results, consider using a combination of inhibitors targeting different systems or validate efficacy using reporter gene assays for each specific pathway [39].
3. What are common reasons for the lack of antibiofilm effect in a QSI compound that shows promise in initial screening? This discrepancy can occur due to several factors:
- Poor Biofilm Penetration: The compound may not effectively diffuse through the dense extracellular polymeric substance (EPS) matrix [6] [15].
- Wrong Timing: QSIs are most effective when applied during early-stage biofilm formation. If added to a mature biofilm, their efficacy is significantly reduced [41].
- Compound Degradation: The QSI might be degraded by bacterial enzymes or host factors in the experimental system [40].
4. Which bacterial strains are recommended for initial validation of broad-spectrum QSI activity? For an initial broad-spectrum screening, use reporter strains responsive to the universal signal Autoinducer-2 (AI-2). Vibrio harveyi bioluminescence assays or engineered E. coli AI-2 reporter strains are standard models. For Gram-negative specific AHL inhibition, Chromobacterium violaceum CV026 is excellent for visual screening based on violacein pigment inhibition [40].
5. How can I differentiate between QSI activity and general antibacterial toxicity in my assays? It is crucial to include control experiments that measure bacterial growth (e.g., OD600). A true QSI will inhibit QS-regulated phenotypes (e.g., virulence factor production, biofilm formation) without significantly affecting microbial growth rates. If growth is inhibited, the observed effect may be due to bacteriostatic or bactericidal activity [39] [40].
Troubleshooting Guides
Problem: High Cytotoxicity of QSI Compounds in Mammalian Cell Lines
Potential Causes and Solutions:
- Cause 1: Inherent Toxicity of Lead Compound. The chemical structure of the QSI may have non-specific cytotoxic effects.
- Solution: Perform structure-activity relationship (SAR) studies to identify and modify the toxic pharmacophore. Explore synthetic derivatives or analogs with lower cytotoxicity [40].
- Cause 2: Solvent Toxicity. The solvent used (e.g., DMSO) may be at a cytotoxic concentration.
- Solution: Ensure the final concentration of the solvent (e.g., DMSO <0.1%) is non-toxic to the cell line in control experiments.
- Cause 3: Low Therapeutic Index. The effective QSI concentration is close to the cytotoxic concentration.
Problem: QSI Loses Efficacy in Complex In Vivo Models
Potential Causes and Solutions:
- Cause 1: Serum Protein Binding. The QSI may bind to serum proteins, reducing its free, active concentration.
- Solution: Modify the compound to reduce protein binding or use delivery vehicles that protect the payload until it reaches the infection site [40].
- Cause 2: Rapid Clearance or Metabolism. The compound may be quickly metabolized or cleared from the host system.
- Solution: Investigate the pharmacokinetic profile and chemically modify the compound to improve its stability and half-life [40].
- Cause 3: Inadequate Biofilm Penetration.
Problem: Rapid Development of Bacterial Resistance to QSI Monotherapy
Potential Causes and Solutions:
- Cause: Evolutionary Adaptation. While QSIs impose less selective pressure than antibiotics, bacteria can still develop resistance through mutations in QS receptor genes or upregulation of efflux pumps [40].
Quantitative Data on Common QSIs and Their Efficacy
The following table summarizes key quantitative data for selected natural QSIs, which is essential for dose selection and experimental design.
Table 1: Efficacy Parameters of Selected Natural Quorum Sensing Inhibitors
| QSI Compound | Source | Target Bacteria / QS System | Key Effect | MIC/MBIC/IC₅₀ Value | Reference Context |
|---|---|---|---|---|---|
| Curcumin | Plant (Turmeric) | P. aeruginosa (Las/Rhl) | Inhibits AHL synthesis, reduces biofilm | MBIC₅₀: ~50 µM | [40] [44] |
| Patulin | Fungal Metabolite | P. aeruginosa (LasB) | Inhibits LasR, reduces virulence factor (elastase) | IC₅₀: 17.8 µM | [40] |
| Caffeine | Plant | P. aeruginosa | Reduces pyocyanin, elastase; inhibits biofilm | ~2-4 mg/mL for significant inhibition | [6] |
| Salicylic Acid | Plant (Willow Bark) | P. aeruginosa & E. coli | Reduces AHL production, inhibits swarming | 0.5 - 1 mg/mL for biofilm inhibition | [6] |
| AiiA Lactonase | Enzyme (Bacillus sp.) | Broad-spectrum (AHL degrader) | Degrades AHL signals, inhibits biofilm formation | Effective in nanomolar ranges | [40] [44] |
| RNAIII-Inhibiting Peptide (RIP) | Synthetic Peptide | S. aureus (Agr) | Blocks Agr QS, reduces biofilm & virulence | 10 - 50 µM for inhibition | [44] |
MIC: Minimum Inhibitory Concentration; MBIC: Minimum Biofilm Inhibitory Concentration; IC₅₀: Half Maximal Inhibitory Concentration; AHL: Acyl-Homoserine Lactone
Experimental Protocols for Key QSI Assays
Protocol 1: Qualitative Screening for Anti-Virulence Activity usingChromobacterium violaceumCV026
Principle: The CV026 mutant is deficient in AHL production but produces the purple pigment violacein in response to exogenous AHLs. QSIs that antagonize the receptor or degrade AHLs will inhibit violacein production.
Materials:
- C. violaceum CV026 reporter strain
- AHL signal (e.g., C6-HSL)
- Luria-Bertani (LB) agar plates
- Test compounds and controls (e.g., solvent control, known QSI)
Method:
- Prepare a soft agar overlay: Mix an overnight culture of CV026 with molten LB agar (0.75% agar) and the inducing AHL (e.g., 10 µM C6-HSL). Pour over a base LB agar plate.
- Apply test compounds: Using a sterile tip, spot 10-20 µL of the test compound solution onto the solidified overlay. Alternatively, use paper discs impregnated with the compound.
- Incubate: Incubate the plates at 28-30°C for 24-48 hours.
- Interpretation: Observe for a zone of colorless, non-pigmented bacterial growth around the spot/disc, indicating successful QS inhibition. No zone of growth inhibition should be present, confirming the effect is anti-virulence and not antibacterial [40].
Protocol 2: Quantitative Assessment of Biofilm Inhibition using Microtiter Plate Assay
Principle: This high-throughput crystal violet (CV) staining method quantifies total biofilm biomass. It is used to determine the Minimum Biofilm Inhibitory Concentration (MBIC) of QSIs.
Materials:
- 96-well flat-bottom polystyrene microtiter plates
- Test bacterial culture (e.g., P. aeruginosa PAO1, S. aureus)
- Crystal violet solution (0.1% w/v)
- Acetic acid (30% v/v) or ethanol (95-100%)
- Microplate reader
Method:
- Inoculation: Grow bacteria to mid-log phase and dilute in fresh medium. Add 100 µL per well containing serially diluted QSIs. Include a growth control (bacteria, no QSI) and a sterility control (medium only).
- Incubation: Incubate statically at 37°C for 24-48 hours to allow biofilm formation.
- Staining:
- Carefully remove the planktonic cells by inverting and shaking the plate.
- Wash the adhered biofilms gently with phosphate-buffered saline (PBS) twice.
- Fix the biofilms by air-drying for 30-45 minutes.
- Add 125 µL of 0.1% crystal violet to each well and stain for 15-20 minutes.
- Destaining and Quantification:
- Wash the stained plates thoroughly under running tap water to remove unbound dye.
- Add 125 µL of 30% acetic acid (or 95% ethanol) to solubilize the crystal violet bound to the biofilm.
- Incubate for 10-15 minutes with shaking.
- Transfer 100 µL of the solubilized dye to a new microtiter plate (if using acetic acid with the original plate).
- Measure the absorbance at 570-600 nm.
- Analysis: The MBIC is defined as the lowest concentration of QSI that results in a ≥50% reduction (MBIC₅₀) or ≥90% reduction (MBIC₉₀) in absorbance compared to the untreated growth control [6] [42].
Research Reagent Solutions
Table 2: Essential Reagents for QSI and Biofilm Research
| Reagent / Material | Function & Application in QSI Research |
|---|---|
| Reporter Strains (e.g., C. violaceum CV026, V. harveyi BB170, P. aeruginosa lasB-gfp*) | Essential for visualizing and quantifying QS inhibition. Used in initial screening and mechanism elucidation [40]. |
| Acyl-Homoserine Lactones (AHLs) | Native QS signaling molecules in Gram-negative bacteria. Used as positive controls and to induce QS in reporter assays [39]. |
| Autoinducing Peptides (AIPs) | Native QS signaling molecules in Gram-positive bacteria. Used for studying and inhibiting Agr-like systems [39] [44]. |
| Crystal Violet | A basic dye used in microtiter plate assays to stain and quantify total biofilm biomass [6] [42]. |
| DNase I | An enzyme that degrades extracellular DNA (eDNA) in the biofilm matrix. Used in combination studies to enhance QSI penetration [6] [15]. |
| Dispersin B | A glycoside hydrolase enzyme that degrades poly-N-acetylglucosamine (PNAG), a key polysaccharide in many biofilms. Used as a biofilm-dispersing agent [15]. |
| Microtiter Plates (Polystyrene, U-bottom/F-bottom) | The standard platform for high-throughput, quantitative biofilm cultivation and antibiofilm susceptibility testing [42]. |
Signaling Pathways and Experimental Workflows
Quorum Sensing Signaling Pathways in Bacteria
Diagram 1: Bacterial Quorum Sensing Signaling Pathways
High-Throughput Screening Workflow for QSIs
Diagram 2: QSI High-Throughput Screening Workflow
Core Concepts: AMPs as Anti-Biofilm Agents
Framing within Biofilm Disruption Thesis: Biofilms are structured communities of microbial cells enclosed in a self-produced extracellular polymeric substance (EPS) matrix that are responsible for up to 80% of all human bacterial infections. [45] These communities can be up to 1000 times more resistant to conventional antibiotics than their free-floating (planktonic) counterparts, making biofilm-associated infections a central challenge in persistent infections research. [45] Antimicrobial Peptides (AMPs), also known as host defense peptides, are emerging as a promising therapeutic alternative due to their broad-spectrum activity against multi-drug resistant pathogens and their unique mechanisms of action that can prevent biofilm formation and disrupt mature biofilms. [46] [47] [48]
FAQ: What makes biofilms so difficult to eradicate in persistent infections? Biofilms pose a significant challenge due to multiple synergistic resistance mechanisms: (1) The EPS matrix acts as a physical barrier that limits antimicrobial penetration; (2) Bacterial cells within biofilms exhibit heterogeneous metabolic activity, including dormant persister cells that survive antibiotic treatment; (3) Biofilms facilitate horizontal gene transfer, accelerating the spread of resistance genes; and (4) Altered microenvironments (e.g., low oxygen, nutrient limitation) further reduce antibiotic efficacy. [19] [45] [1]
FAQ: How do AMPs overcome biofilm resistance compared to conventional antibiotics? Unlike many conventional antibiotics that target specific intracellular processes, AMPs primarily disrupt bacterial membranes through electrostatic interactions, making resistance development more difficult. [47] Additionally, many AMPs employ multiple mechanisms simultaneously, including membrane permeabilization, inhibition of intracellular functions, immunomodulation, and direct biofilm matrix degradation. [45] [47] This multi-target approach is particularly effective against biofilms, as it addresses both the bacterial cells and their protective matrix.
Table 1: Key Advantages of AMPs for Biofilm Eradication
| Advantage | Mechanistic Basis | Research Implication |
|---|---|---|
| Broad-Spectrum Activity | Targets conserved membrane components rather than species-specific pathways | Effective against polymicrobial biofilms commonly found in clinical settings |
| Multiple Mechanisms of Action | Combines membrane disruption with intracellular targeting & matrix degradation | Reduces likelihood of resistance development compared to single-target antibiotics |
| Anti-Biofilm Specificity | Targets biofilm-specific features like EPS matrix and quorum sensing systems | Can disrupt mature biofilms rather than just preventing formation |
| Synergy with Antibiotics | Membrane permeabilization enhances antibiotic penetration into biofilms | Enables revitalization of conventional antibiotics against resistant infections |
| Immunomodulatory Properties | Modulates host immune responses while directly attacking pathogens | Addresses both microbial and host factors in persistent infections |
Mechanisms of Action: Technical Analysis
Primary Anti-Biofilm Mechanisms of AMPs
Troubleshooting Guide: My AMP shows good planktonic inhibition but poor biofilm eradication. What might be happening? This common issue typically stems from three main causes: (1) Inadequate penetration through the EPS matrix - consider combination therapy with matrix-degrading enzymes; (2) Sub-lethal dosing at the biofilm core - perform penetration assays and consider higher/localized dosing; or (3) Peptide degradation by biofilm-associated proteases - modify peptide sequence to enhance stability or use protease inhibitors.
Table 2: Detailed Mechanisms of AMP Action Against Biofilms
| Mechanism Category | Specific Actions | Experimental Evidence |
|---|---|---|
| Membrane Disruption | Disrupts membrane potential of biofilm-embedded cells; Forms pores via barrel-stave, toroidal pore, or carpet models | Live-cell imaging shows rapid membrane permeabilization; SEM confirms structural damage to bacterial membranes [45] [49] [50] |
| Signaling Interference | Interrupts bacterial quorum sensing systems; Downregulates genes responsible for biofilm formation | QS mutant studies show reduced AMP efficacy; Transcriptomic analyses reveal altered expression of biofilm-related genes [45] [47] |
| Matrix Degradation | Directly degrades polysaccharide and biofilm matrix components; Targets extracellular DNA in EPS | Enzyme-linked assays show matrix component degradation; CLSM demonstrates reduced matrix integrity post-treatment [45] [1] |
| Cellular Detachment | Encourages microbial detachment from mature biofilms; Reduces adhesion to surfaces | Crystal violet staining shows reduced biofilm biomass; Flow cells demonstrate enhanced dispersal [45] [50] |
| Stringent Response Inhibition | Inhibits the alarmone system (ppGpp) to avoid bacterial stringent response | HPLC detection of reduced (p)ppGpp levels; Mutant studies with relA/spoT genes [45] |
Visualization of AMP Mechanisms Against Biofilms
Figure 1: Comprehensive Anti-Biofilm Mechanisms of AMPs - This diagram illustrates the multifaceted strategies AMPs employ against both developing and mature biofilms, highlighting their potential as comprehensive anti-biofilm agents.
Experimental Protocols & Methodologies
Standardized Anti-Biofilm Screening Assay
Protocol: Assessment of AMP Efficacy Against Pre-formed Biofilms
This standardized protocol evaluates AMP activity against mature biofilms, providing quantitative data on both biofilm disruption and bacterial viability.
Materials & Reagents:
- Peptide Solutions: Prepare AMP stock solutions (1-10 mg/mL in sterile water or appropriate buffer)
- Biofilm Growth Medium: Tryptic soy broth (TSB) or Mueller Hinton broth (MHB) supplemented with 1% glucose
- Staining Reagents: Crystal violet (0.1% for biomass), resazurin (0.15 mM for viability), or SYTO9/propidium iodide for viability imaging
- 96-well Polystyrene Microtiter Plates: Tissue culture-treated for optimal biofilm formation
Procedure:
- Biofilm Formation:
- Inoculate wells with 100 μL of bacterial suspension (1×10^6 CFU/mL in appropriate medium)
- Incubate statically for 24-48 hours at optimal growth temperature (e.g., 37°C for human pathogens)
- Gently wash wells twice with sterile PBS to remove non-adherent cells
AMP Treatment:
- Add 100 μL of AMP solution (serial dilutions in fresh medium) to pre-formed biofilms
- Include untreated (medium only) and vehicle control wells
- Incubate for 2-24 hours depending on experimental design
Biofilm Assessment:
- Biomass Quantification (Crystal Violet):
- Fix biofilms with 99% methanol for 15 minutes
- Stain with 0.1% crystal violet for 20 minutes
- Wash to remove excess stain, solubilize in 30% acetic acid
- Measure absorbance at 595 nm
- Metabolic Activity (Resazurin):
- After treatment, add 10% resazurin solution in PBS
- Incubate 1-4 hours, measure fluorescence (Ex560/Em590)
- Viable Cell Counts:
- Scrape biofilm cells into PBS, vortex vigorously
- Serial dilute and plate on appropriate agar
- Count CFU after 24-48 hours incubation
- Biomass Quantification (Crystal Violet):
Troubleshooting Guide: Inconsistent biofilm formation across wells
- Problem: High variability in baseline biofilm formation
- Solution: Use tissue culture-treated plates; standardize inoculum preparation (adjust to exact OD); ensure consistent medium batch; pre-condition plates with growth medium for 1 hour before inoculation; use specialized biofilm incubators with precise humidity control
Advanced Mechanism of Action Studies
Protocol: Bacterial Cytological Profiling for AMP Mechanism Elucidation
This advanced methodology uses microscopy and fluorescent probes to determine the temporal sequence of AMP-induced cellular damage.
Materials & Reagents:
- Fluorescent Dyes:
- Membrane potential: DiOC₂(3) or TMRM
- Membrane integrity: SYTO9/PI (LIVE/DEAD BacLight)
- Cell wall integrity: Wheat Germ Agglutinin conjugates
- DNA damage: DAPI or Hoechst stains
- Imaging: Confocal laser scanning microscope with environmental chamber
- Microfluidic chambers: For real-time imaging of biofilm treatment
Procedure:
- Sample Preparation:
- Grow biofilms on appropriate surfaces (glass coverslips, MBEC assay pegs)
- Treat with sub-MIC and MIC concentrations of AMP
- Include time points from 5 minutes to 4 hours post-treatment
Staining Protocol:
- For membrane potential: Incubate with 30 μM DiOC₂(3) for 30 minutes
- For viability: Apply SYTO9 (3.34 μM) and PI (20 μM) mixture for 15 minutes
- For cell wall staining: Fix samples with 4% PFA, then stain with WGA-AlexaFluor conjugates
Image Acquisition & Analysis:
- Acquire z-stacks at multiple positions using appropriate laser settings
- Quantify fluorescence intensity changes over time
- Analyze spatial distribution of damage within biofilm structures
Experimental Workflow Visualization:
Figure 2: Experimental Workflow for AMP Mechanism of Action Studies - This workflow outlines the key steps in elucidating how AMPs exert their anti-biofilm effects, from sample preparation through advanced imaging and data analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for AMP Anti-Biofilm Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Model AMPs | LL-37 (human cathelicidin), Defensins, Magainin, Synthetically designed peptides like (LKKL)₃ [50] | Mechanism studies, Positive controls, Assay development | Vary in charge, hydrophobicity, and secondary structure; Choose based on research focus |
| Biofilm Matrix-Targeting Enzymes | Glycoside hydrolases (Dispersin B), Proteases, Deoxyribonucleases (DNase I) [1] | Matrix disruption studies, Combination therapy with AMPs | Enzyme specificity must match matrix composition; Consider timing of application |
| Membrane Integrity Probes | DiOC₂(3) (membrane potential), SYTO9/PI (LIVE/DEAD), FM dyes | Mechanism of action studies, Time-kill assays | DiOC₂(3) requires specific red/green ratio analysis; SYTO9 can bind to EPS |
| Quorum Sensing Reporters | AHL biosensors, Autoinducer analogs, QS mutant strains | Signaling disruption studies, Anti-virulence screening | Species-specific; Requires understanding of target organism's QS system |
| Standardized Biofilm Culturing Systems | Calgary biofilm device, Flow cell systems, Microtiter plate assays | High-throughput screening, Biofilm architecture studies | Flow cells better mimic in vivo conditions but are lower throughput |
Troubleshooting Guide: My AMP is cytotoxic to mammalian cells at anti-biofilm concentrations
- Problem: Lack of selectivity between bacterial and mammalian cells
- Solution: Modify peptide sequence to increase selectivity index; consider cyclization or D-amino acid incorporation; test different delivery methods (localized vs. systemic); evaluate combination approaches to reduce effective AMP concentration
Quantitative Data Analysis & Interpretation
Table 4: Key Efficacy Metrics for AMP Anti-Biofilm Activity
| Parameter | Measurement Method | Interpretation Guidelines | Benchmark Values |
|---|---|---|---|
| MBIC (Minimum Biofilm Inhibitory Concentration) | Crystal violet, resazurin assay | Concentration that prevents biofilm formation | Compare to planktonic MIC; MBIC/MIC ratio >8 indicates biofilm-specific resistance [45] |
| MBEC (Minimum Biofilm Eradication Concentration) | Viable counts after treatment | Concentration that eradicates pre-formed biofilm | Typically 10-1000× higher than MIC; Lower ratios indicate better biofilm penetration [45] |
| Biofilm Removal Efficiency | Biomass reduction compared to control | Percentage of biofilm removed by treatment | >50% significant; >90% high efficacy; Confirms visual observations [50] |
| Synergy Index (FIC) | Checkerboard assays with antibiotics | Quantifies combination therapy efficacy | FIC ≤0.5: synergy; 0.5-4: additive/indifferent; >4: antagonism [47] |
| Selectivity Index | Mammalian cell cytotoxicity vs. anti-biofilm activity | Therapeutic window determination | SI >10 desirable for therapeutic development; varies by application [51] |
FAQ: How do I determine if my AMP's anti-biofilm activity is clinically relevant? Clinical relevance requires evaluating multiple parameters: (1) MBEC values should be achievable at the infection site; (2) Activity against clinical isolates rather than just lab strains; (3) Demonstration of efficacy in complex, multi-species biofilms; (4) Activity in presence of biological fluids that might inhibit AMP function; and (5) Evidence of biofilm disruption rather than just inhibition of formation. The most promising candidates typically show MBEC values ≤64 μg/mL against clinical isolates and maintain activity in biological relevant conditions. [52] [48]
Advanced Applications & Combination Strategies
Synergistic Approaches with Conventional Antibiotics
Protocol: Checkerboard Assay for AMP-Antibiotic Synergy Screening
This protocol systematically evaluates combination therapies that may enhance conventional antibiotic efficacy against biofilm-associated infections.
Materials & Reagents:
- AMP stock solutions (2× highest test concentration)
- Antibiotic stock solutions (2× highest test concentration)
- 96-well microtiter plates
- Bacterial inoculum (5×10^5 CFU/mL in appropriate medium)
Procedure:
- Prepare two-fold serial dilutions of AMP in one direction and antibiotic in the perpendicular direction
- Add 50 μL of each dilution to assigned wells
- Inoculate with 100 μL bacterial suspension
- Incubate for 20-24 hours at appropriate temperature
- Measure growth (OD600) or viability (resazurin)
- Calculate Fractional Inhibitory Concentration (FIC) index: FIC index = (MIC of AMP in combination/MIC of AMP alone) + (MIC of antibiotic in combination/MIC of antibiotic alone)
Troubleshooting Guide: Inconsistent results in synergy assays
- Problem: High variability in combination therapy outcomes
- Solution: Use fresh antibiotic stocks; include appropriate controls for drug interactions; ensure proper mixing of compounds; consider temporal aspects (simultaneous vs. sequential addition); repeat with multiple biological replicates
Design Strategies for Synthetic AMPs
FAQ: What design principles optimize synthetic AMPs for anti-biofilm applications? Rational design of synthetic AMPs for enhanced anti-biofilm activity follows several key principles: (1) Idealized facial amphiphilicity with segregated cationic and hydrophobic residues; (2) Optimal charge density (+4 to +10) for initial membrane interaction; (3) Balanced hydrophobicity for sufficient membrane insertion without excessive mammalian cell toxicity; (4) Incorporation of protease-resistant residues (D-amino acids, cyclization) for stability in biofilm environments; and (5) Specific sequences that target biofilm matrix components. [46] [50] The backbone sequence (X₁Y₁Y₂X₂)ₙ, where X are hydrophobic residues and Y are cationic residues, has demonstrated particular efficacy with potent broad-spectrum activity and biofilm disruption capabilities. [50]
Nanoparticle-Based Drug Delivery Systems for Enhanced Biofilm Penetration
Frequently Asked Questions (FAQs)
FAQ 1: Why are traditional antibiotics often ineffective against biofilms, and how do nanoparticles help?
Biofilms are structured communities of bacteria encased in a self-produced extracellular polymeric substance (EPS) matrix. This matrix acts as a formidable physical and chemical barrier [53] [54]. The EPS, which can comprise up to 85% of the biofilm, hinders antibiotic penetration through steric obstruction and charge interactions [54] [55]. Furthermore, it contains high concentrations of enzymes, such as β-lactamases, that inactivate antibiotics [54]. Bacteria within biofilms can also exhibit reduced metabolic activity, making them less susceptible to drugs that target rapidly dividing cells [1]. This combination of factors can increase bacterial resistance by up to 1000 times compared to their planktonic (free-floating) counterparts [53].
Nanoparticles (NPs) overcome these challenges through several key mechanisms:
- Enhanced Penetration: Their small size and tunable surface properties allow them to diffuse through the EPS matrix more effectively than conventional antibiotics [53].
- Targeted Delivery: NPs can be engineered to carry antibiotics directly to the biofilm site, increasing the local drug concentration [53] [55].
- Intrinsic Anti-biofilm Activity: Certain NPs, like metal and metal oxide nanoparticles, can generate reactive oxygen species (ROS) that directly damage bacterial cells and disrupt the biofilm structure [53].
- Multi-Functional Action: NPs can be designed to simultaneously degrade the EPS matrix (e.g., by releasing matrix-degrading enzymes) and deliver antimicrobial payloads [1].
FAQ 2: What are the key properties of nanoparticles that determine their efficacy in penetrating biofilms?
The efficacy of nanoparticle penetration is governed by a combination of physicochemical properties. The table below summarizes these key factors.
Table 1: Key Nanoparticle Properties Affecting Biofilm Penetration
| Property | Impact on Biofilm Penetration and Efficacy | Design Considerations |
|---|---|---|
| Size | Smaller nanoparticles (typically < 100 nm) can more easily navigate the dense mesh of the EPS. Size must be balanced with drug-loading capacity [55]. | Aim for a hydrodynamic diameter that is smaller than the mesh pore size of the target biofilm EPS. |
| Surface Charge | A positive surface charge can facilitate interaction with the negatively charged components of the EPS (e.g., eDNA, polysaccharides), but strong electrostatic adhesion can also hinder deep penetration. Neutral or "stealth" coatings can improve diffusion [55]. | Use coatings like PEG to create a neutral surface charge and minimize non-specific adhesion for deeper penetration. |
| Hydrophobicity/Hydrophilicity | Hydrophobic interactions can cause NPs to stick to the biofilm surface. A hydrophilic surface is generally preferred for improved diffusion through the hydrated EPS matrix [55]. | Employ hydrophilic polymers or surfactants in the NP formulation. |
| Shape | The shape of the nanoparticle (e.g., spherical, rod-shaped) influences its diffusion coefficient and ability to move through porous structures [55]. | Spherical nanoparticles are most common and often show favorable penetration profiles. |
| Functionalization | Surface functionalization with targeting ligands (e.g., antibodies, peptides) or biofilm matrix-degrading enzymes (e.g., DNase, dispersin B) can actively enhance penetration and targeting [53] [1]. | Conjugate enzymes that degrade specific EPS components (e.g., DNase I for eDNA) to the NP surface. |
FAQ 3: How can I quantify the penetration and efficacy of my nanoparticle formulation in a biofilm model?
Quantifying NP performance involves a suite of assays that assess both the physical distribution of the NPs and their functional anti-biofilm outcome.
Table 2: Key Methods for Quantifying Nanoparticle Penetration and Efficacy
| Assay Type | What It Measures | Typical Protocol Outline |
|---|---|---|
| Confocal Laser Scanning Microscopy (CLSM) | 3D spatial distribution and penetration depth of fluorescently labeled NPs within a biofilm. | 1. Grow a biofilm on a coverslip or in a microscopy chamber.2. Treat with fluorescent NPs for a set time.3. Wash to remove unbound NPs.4. Image using CLSM with Z-stacking.5. Analyze fluorescence intensity profiles across the Z-axis to determine penetration depth. |
| Biofilm Viability Assay | Reduction in metabolic activity or colony-forming units (CFUs) of biofilm-resident bacteria after NP treatment. | 1. Grow a standard biofilm in a 96-well plate.2. Treat with NPs or controls (e.g., free antibiotic).3. Incubate.4. Use a metabolic dye (e.g., MTT, XTT) or disperse the biofilm and plate for CFU counts.5. Calculate the percentage reduction in viability/CFUs compared to the untreated control. |
| EPS Degradation Assay | The ability of enzyme-functionalized NPs to break down specific EPS components. | 1. Isclude purified EPS component (e.g., eDNA, polysaccharides) or use a pre-formed biofilm.2. Treat with NPs carrying a specific enzyme (e.g., DNase I, glycoside hydrolase).3. Measure the release of degradation products (e.g., reducing sugars for polysaccharides, increase in fluorescence for DNA-intercalating dyes) over time. |
| Minimum Biofilm Eradication Concentration (MBEC) | The lowest concentration of an NP formulation required to eradicate a pre-formed biofilm. | 1. Grow biofilms in a specialized MBEC assay device.2. Expose biofilms to a range of NP concentrations.3. Rinse and allow surviving cells to recover in fresh media.4. The MBEC is the lowest concentration that results in no bacterial growth upon recovery. |
Troubleshooting Guides
Problem 1: Poor Nanoparticle Penetration into the Biofilm
Potential Causes and Solutions:
- Cause: NP Aggregation. Nanoparticles may be aggregating in the growth media or at the biofilm surface, preventing deep penetration.
- Solution: Ensure NP dispersion using sonication or vortexing immediately before use. Characterize the hydrodynamic size and polydispersity index (PDI) of your NPs in the relevant biological medium using dynamic light scattering (DLS).
- Cause: Excessive Non-specific Binding. A highly charged NP surface may be binding strongly to the first layers of the EPS.
- Solution: Modify the NP surface with a stealth coating, such as polyethylene glycol (PEG), to reduce non-specific interactions and improve diffusion [55].
- Cause: Size Exclusion. The nanoparticles may simply be too large for the biofilm's mesh pores.
- Solution: Synthesize smaller nanoparticles. If using a polymer-based NP, consider formulations that can shrink in size upon reaching the biofilm environment (e.g., pH-responsive particles).
Problem 2: High Antibiotic Loading but Low Therapeutic Efficacy
Potential Causes and Solutions:
- Cause: Inefficient Drug Release. The antibiotic may be trapped inside the nanoparticle and not released at the biofilm site.
- Solution: Design a stimulus-responsive release system. Use NPs that release their payload in response to the unique biofilm microenvironment, such as low pH, specific enzymes (e.g., matrix-degrading enzymes), or hypoxia [53].
- Cause: Loss of Antibiotic Activity. The encapsulation process or the material of the NP itself may be degrading the antibiotic.
- Solution: Use milder encapsulation techniques (e.g., nanoprecipitation instead of high-energy sonication for sensitive drugs). Test the stability and activity of the encapsulated drug after release from the NPs.
- Cause: Targeting the Wrong Population. The NPs may be effective against surface bacteria but not against the dormant persister cells in the biofilm core.
- Solution: Employ a combination therapy approach. Use NPs that can disrupt the EPS to expose persister cells, followed by or co-delivered with antibiotics that are effective against slow-growing bacteria [1].
Problem 3: Inconsistent Results Between Biological Replicates
Potential Causes and Solutions:
- Cause: Biofilm Heterogeneity. Biofilms are inherently heterogeneous, and small differences in growth conditions can lead to significant variations in EPS composition and thickness.
- Solution: Standardize biofilm growth conditions meticulously (inoculum size, growth medium, incubation time, and temperature). Increase the number of biological replicates (n ≥ 6 is recommended for biofilm assays). Use assays like crystal violet staining to normalize results to total biofilm biomass.
- Cause: Unstable NP Formulation. The NP formulation may be degrading or precipitating over time.
- Solution: Characterize the size, charge, and drug loading of your NPs immediately before each experiment. Use freshly prepared NP dispersions or establish a stable storage protocol (e.g., lyophilization).
Experimental Workflow & Mechanisms
The following diagram illustrates a generalized experimental workflow for developing and testing an anti-biofilm nanoparticle formulation, from design to validation.
Diagram 1: NP Development Workflow
The effectiveness of nanoparticles stems from their multi-mechanistic action against the biofilm structure, as visualized below.
Diagram 2: NP Anti-Biofilm Mechanisms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Anti-Biofilm Nanoparticle Research
| Reagent/Material | Function in Experimentation | Specific Examples & Notes |
|---|---|---|
| Nanoparticle Cores | Serves as the drug carrier; can have intrinsic anti-biofilm properties. | Metal/Metal Oxide: Silver (AgNPs), Gold (AuNPs), Zinc Oxide (ZnO NPs). Effective for ROS generation [53].Polymeric: Chitosan, PLGA. Biocompatible and allow for controlled drug release [53].Lipid-based: Solid Lipid NPs (SLNs), Liposomes. High drug loading capacity [53]. |
| Surface Modifiers | Improve stability, penetration, and targeting of nanoparticles. | PEG: Creates a "stealth" effect, reducing non-specific binding [55].Peptides: Targeting motifs (e.g., for specific bacterial species).Chitosan: Provides a positive charge for EPS interaction. |
| Biofilm Dispersing Enzymes | Functionalize NPs to actively break down the EPS matrix. | DNase I: Degrades extracellular DNA (eDNA), a key EPS component [1].Dispersin B: A glycoside hydrolase that degrades poly-N-acetylglucosamine (PNAG) polysaccharides [1].Proteinase K: Degrades extracellular proteins in the EPS [1]. |
| Model Biofilm Strains | Standardized in vitro models for testing NP efficacy. | Pseudomonas aeruginosa (e.g., PAO1): A model for cystic fibrosis lung infections [55].Staphylococcus aureus (e.g., USA300): A model for wound and implant infections [54] [56].Escherichia coli: Commonly found in urinary tract and implant-related infections [54]. |
| Viability Assay Kits | Quantify the reduction in live bacteria within a biofilm after NP treatment. | MTT/XTT Assays: Measure metabolic activity via colorimetric change.Resazurin Assay: A fluorescent/prefluorescent indicator of metabolic activity.ATP Assays: Measure cellular ATP levels as a marker of viability. |
| Fluorescent Labels | Track nanoparticle penetration and localization within biofilms. | FITC, Rhodamine B: Common fluorescent dyes for labeling NPs for CLSM.Cyanine Dyes (Cy3, Cy5): Offer brighter fluorescence and different excitation/emission spectra. |
Phage Therapy and Enzyme-Assisted Antibiotic Penetration
Frequently Asked Questions (FAQs)
1. What are the primary advantages of using bacteriophages over conventional antibiotics for biofilm eradication? Bacteriophages offer several key advantages for combating biofilms: (1) Self-replication and self-limitation: They amplify at the infection site while the bacterial host is present and are cleared when the infection is resolved [57]. (2) Biofilm matrix degradation: Many phages produce polysaccharide-depolymerizing enzymes that break down the extracellular polymeric substance (EPS), disrupting the biofilm's structural integrity and enhancing penetration [58] [59]. (3) High specificity: They target specific bacterial pathogens without significantly disrupting the commensal microbiome [57] [60]. (4) Ability to penetrate biofilms: Their small size and enzymatic activity allow them to diffuse into the biofilm depth [58].
2. How do biofilm-dispersing enzymes enhance the efficacy of conventional antibiotics? Biofilm-dispersing enzymes, such as glycoside hydrolases, DNases, and proteases, selectively degrade the major components of the EPS matrix [61]. This enzymatic disruption serves two main functions: (1) It physically breaks apart the biofilm architecture, releasing the embedded bacterial cells into a planktonic state where they are up to 1000 times more susceptible to antibiotics [58] [59]. (2) It creates channels within the biofilm, thereby improving the diffusion and penetration of co-administered antimicrobial agents to their cellular targets [61].
3. What are the common reasons for phage therapy failure against established biofilms, and how can they be addressed? Therapies can fail due to several biological and technical hurdles. The table below summarizes common causes and potential solutions.
Table: Troubleshooting Phage Therapy Failures Against Biofilms
| Cause of Failure | Underlying Reason | Potential Solutions |
|---|---|---|
| Limited Phage Penetration | The dense EPS matrix acts as a physical barrier, preventing phages from reaching all target cells [58]. | Use phages encoding EPS-degrading enzymes (depolymerases) [58] [62] or pre-treat with purified dispersing enzymes [61]. |
| Narrow Host Range | A single phage may not infect all bacterial strains within a polymicrobial biofilm [57] [59]. | Employ well-designed phage cocktails containing multiple phages with complementary host ranges [58] [60]. |
| Emergence of Phage Resistance | Bacteria can evolve resistance through surface receptor modification or CRISPR-Cas systems [58] [57]. | Implement combination therapy with antibiotics or use genetically modified phages to circumvent common resistance mechanisms [58] [62]. |
| Inadequate Phage Selection | The use of temperate (lysogenic) phages, which integrate into the bacterial genome rather than lysing the cell, can fail to reduce bacterial load and may even transfer virulence genes [57]. | Strictly select and purify lytic phages for therapeutic applications [57] [60]. |
4. Can phage therapy be used in conjunction with antibiotics? Yes, and this is often a recommended strategy. This approach, sometimes termed Phage-Antibiotic Synergy (PAS), can be highly effective [62]. Sub-lethal concentrations of certain antibiotics can enhance the replication of phages, leading to more efficient bacterial killing. Furthermore, by dispersing the biofilm, phages and enzymes can make the bacteria susceptible to an antibiotic that was previously ineffective [61] [62]. It is crucial to note that the interaction can be complex, and some antagonistic effects have been reported, so combination pairs should be validated experimentally [62].
Troubleshooting Guide: Common Experimental Issues
Problem 1: Poor Penetration of Antimicrobials into the Biofilm Model
- Observation: Minimal killing effect despite high antibiotic concentrations in the supernatant. Confocal microscopy shows limited diffusion beyond the biofilm surface.
- Potential Causes and Solutions:
- Cause: Dense EPS matrix blocking diffusion.
- Solution: Incorporate a biofilm-dispersing enzyme as a pre-treatment or co-treatment. Dispersin B (degrades poly-N-acetylglucosamine, or PNAG) or Alginate lyase (targets alginate in Pseudomonas aeruginosa biofilms) are common choices [61]. See the reagent table for details.
- Solution: Use engineered phages that express and secrete depolymerases. These can create their own penetration pathways [58] [62].
- Cause: Sub-optimal dosing or enzyme stability.
- Cause: Dense EPS matrix blocking diffusion.
Problem 2: Rapid Development of Bacterial Resistance
- Observation: Initial treatment efficacy is high, but bacterial regrowth occurs quickly in subsequent passages or experiments.
- Potential Causes and Solutions:
- Cause: Monotherapy with a single, highly specific phage.
- Solution: Employ combination therapy with an antibiotic. Phage predation can resensitize bacteria to antibiotics, and the dual attack presents two evolutionary challenges for the bacteria [62].
- Cause: Use of a phage against which pre-existing resistance is common.
- Solution: Perform pre-screening of your bacterial strain against a panel of phages to select the most effective one(s). Consider using genetically modified phages engineered with expanded host ranges or to target essential genes [62].
Quantitative Data on Biofilm Dispersal Efficacy
The following table summarizes experimental data for various biofilm-disrupting agents, providing a benchmark for expected outcomes.
Table: Efficacy of Selected Enzymes and Phages in Biofilm Disruption
| Agent | Target Biofilm Component | Model System | Key Quantitative Outcome | Citation |
|---|---|---|---|---|
| Dornase Alfa (DNase I) | Extracellular DNA (eDNA) | In vitro CF sputum model | Reduced sputum viscoelasticity and disrupted biofilm structure [61]. | [61] |
| Dispersin B | Poly-N-acetylglucosamine (PNAG) | Staphylococcus epidermidis biofilm | Effectively degraded the polysaccharide matrix, sensitizing bacteria to antibiotics like teicoplanin [61]. | [61] |
| Phage-Derived Depolymerase (Dpo71) | Capsular polysaccharide | MDR Acinetobacter baumannii (Mouse model) | Degraded capsule, making bacteria more sensitive to colistin and host immune clearance [62]. | [62] |
| Phage PEV20 + Ciprofloxacin | P. aeruginosa cells & matrix | P. aeruginosa lung infection (Mouse model) | Aerosol delivery reduced bacterial load in lungs by 5.9 log₁₀ [62]. | [62] |
Essential Experimental Protocols
Protocol 1: Standard Assay for Evaluating Phage & Enzyme Biofilm Disruption
This protocol provides a foundational method for testing the efficacy of anti-biofilm agents in vitro.
- Biofilm Formation: Grow a standardized biofilm of your target bacterium (e.g., P. aeruginosa, S. aureus) in a 96-well polystyrene plate or on a relevant substrate (e.g., catheter piece) for 24-48 hours.
- Treatment:
- Enzyme Group: Aspirate spent media and add fresh media containing the biofilm-dispersing enzyme (e.g., 10-100 µg/mL Alginate Lyase for P. aeruginosa).
- Phage Group: Add a suspension of phage at a known Multiplicity of Infection (MOI, e.g., 0.1-10) in fresh media.
- Combination Group: Apply both enzyme and phage.
- Control Groups: Include a media-only control (negative) and a relevant antibiotic control (positive).
- Incubation: Incubate the plate under appropriate conditions for a set period (e.g., 4-24 hours).
- Analysis:
- Biomass Quantification: Use the Crystal Violet (CV) staining assay. Fix the biofilm with methanol, stain with 0.1% CV, solubilize with acetic acid, and measure absorbance at 595nm to quantify remaining biomass.
- Viability Assessment: Use the Colony Forming Unit (CFU) count assay. Gently wash the biofilm to remove non-adherent cells, then scrape the biofilm into a saline solution, vortex vigorously, serially dilute, and plate on agar to count viable bacteria.
- Visualization: Use Confocal Laser Scanning Microscopy (CLSM) with live/dead staining (e.g., SYTO9/propidium iodide) to visualize the 3D architecture of the biofilm and the spatial distribution of live vs. dead cells.
Protocol 2: Assessing Antibiotic Re-sensitization Post-Dispersal
This protocol measures the synergistic effect of biofilm dispersal on subsequent antibiotic efficacy.
- Pre-treatment and Dispersal: Grow a mature biofilm as in Protocol 1. Treat with the chosen dispersing agent (enzyme or phage) for a period sufficient to cause dispersal (e.g., 4-6 hours), as determined in preliminary experiments.
- Antibiotic Challenge: After the dispersal phase, carefully aspirate the supernatant (which contains dispersed planktonic cells) and add fresh media containing a gradient of sub-inhibitory to inhibitory concentrations of the antibiotic of interest.
- Incubation and Analysis: Incubate for an additional 18-24 hours. Analyze the results using CFU counts from the biofilm and supernatant to determine the reduction in viable bacteria compared to antibiotic-only and dispersal-agent-only controls. A significant enhancement of antibiotic killing in the combination group indicates successful re-sensitization.
Visualizing the Strategy: Mechanisms and Workflows
Biofilm Disruption Mechanism
The following diagram illustrates the core mechanisms by which phages and enzymes disrupt biofilms and facilitate antibiotic penetration.
Experimental Workflow for Testing
This diagram outlines a standard experimental workflow for evaluating phage and enzyme therapies against biofilms.
The Scientist's Toolkit: Key Research Reagents
Table: Essential Reagents for Phage and Enzyme Biofilm Research
| Reagent / Material | Function / Description | Key Considerations |
|---|---|---|
| Lytic Bacteriophages | Viruses that specifically infect and lyse bacterial hosts, disrupting the biofilm from within [57]. | Must be purified from endotoxins and confirmed to be strictly lytic (not temperate). Host range should be characterized for the target strain [57] [60]. |
| Biofilm-Dispersing Enzymes | Proteins that degrade specific components of the EPS matrix (e.g., DNases, glycoside hydrolases, proteases) [61]. | Select based on the primary composition of the target biofilm (e.g., Alginate lyase for P. aeruginosa). Purity, specific activity, and stability are critical [61] [63]. |
| Crystal Violet (CV) | A dye that binds to biomass and is used in a colorimetric assay to quantify total biofilm formation and dispersal [59]. | A standard, high-throughput method. It does not distinguish between live and dead cells, so should be paired with a viability assay [59]. |
| Live/Dead Staining Kits (e.g., SYTO9/PI) | Fluorescent stains used with confocal microscopy to visualize the spatial distribution of live (green) and dead (red) cells within a biofilm [64]. | Provides powerful visual evidence of treatment efficacy and biofilm architecture. |
| Smart Delivery Systems (e.g., Liposomes, Hydrogels) | Carrier systems designed to protect enzymatic therapeutics from degradation and allow for targeted, triggered release at the biofilm site [61] [63]. | Can significantly enhance the stability and in vivo performance of biofilm-dispersing enzymes. |
Combination Therapies and Synergistic Approaches
Frequently Asked Questions (FAQs)
1. What is the primary rationale behind using combination therapies against biofilms? Combination therapies are used because biofilms can be up to 1,000 times more tolerant to antibiotics than their planktonic counterparts. Using a biofilm-dispersing agent alongside a conventional antibiotic simultaneously breaks down the protective extracellular matrix and eradicates the now-vulnerable bacterial cells. This synergistic approach is often more effective than either agent used alone, helping to overcome the physical barrier of the EPS, metabolic heterogeneity within the biofilm, and the presence of dormant persister cells [65] [6] [1].
2. Why do my dispersal agent and antibiotic combinations work in vitro but fail in my animal model? This common issue can arise from several factors. The pharmacokinetics and pharmacodynamics (PK/PD) of the agents in vivo may not be optimized; the dispersal agent and antibiotic might not reach the target site at the same time or at sufficient concentrations. The in vivo biofilm microenvironment (e.g., hypoxia, host proteins) can also impair drug activity. It is crucial to ensure your animal model appropriately recapitulates the human infection and to conduct detailed PK/PD studies to optimize dosing regimens and timing [65] [66].
3. How do I choose the right enzymatic dispersal agent for my biofilm model? The choice of enzyme must be guided by the specific composition of the extracellular polymeric substance (EPS) of your target biofilm.
- Glycoside Hydrolases (e.g., Dispersin B): Target exopolysaccharides like poly-β-(1,6)-N-acetyl-D-glucosamine (dPNAG/PNAG), which is common in pathogens like Staphylococcus aureus, Escherichia coli, and Klebsiella pneumoniae [1].
- Proteases (e.g., Proteinase K): Degrade protein components of the EPS matrix [1].
- Deoxyribonucleases (DNases): Target extracellular DNA (eDNA), a key structural component in many biofilms, such as those formed by Pseudomonas aeruginosa and Streptococcus species [1]. Conduct a preliminary analysis of your biofilm's EPS composition to select the most appropriate enzyme.
4. What are the best practices for testing combination therapies in a static microtiter plate assay? While static assays like the Calgary Biofilm Device or crystal violet staining in 96-well plates are useful for initial screening, they have limitations. They do not expose biofilms to the shear forces found in many physiological settings, which can affect biofilm structure and drug penetration. For more clinically relevant results, it is highly recommended to validate hits from static assays in dynamic biofilm models such as flow cells or bioreactor systems, which produce more mature and robust biofilms [67].
Troubleshooting Guides
Problem: Inconsistent Biofilm Eradication with Combination Treatment
Potential Causes and Solutions:
Cause 1: Sub-optimal Dosing or Timing. The concentration of the dispersal agent may be insufficient to effectively disrupt the EPS, or it may be administered at a time when the antibiotic concentration is no longer at its peak.
Cause 2: Inadequate Penetration of Agents. The biofilm may be too thick or dense, preventing the agents from reaching all cell layers.
- Solution: Consider using nanoparticles as drug carriers. Polymeric nanoparticles can be engineered to enhance penetration through the Gram-negative bacterial membrane and the biofilm matrix. Alternatively, combining chemical dispersal agents with physical methods like microsprays or jet flows can mechanically disrupt the biofilm structure, improving drug access [69] [68].
Cause 3: Presence of High Levels of Persister Cells. Standard antibiotics primarily kill metabolically active cells. Dormant persister cells can survive treatment and lead to biofilm regrowth.
- Solution: Incorporate agents that target persister cells or disrupt their dormant state. Some antimicrobial peptides (AMPs) and nitroxides have shown efficacy against persister cells. Another strategy is to use a second antibiotic with activity against slow-growing or non-growing cells following the initial combination therapy [65] [1].
Problem: High Cytotoxicity in Cell Culture Models When Testing Novel Anti-biofilm Compounds
Potential Causes and Solutions:
- Cause: The anti-biofilm compound or its formulation is inherently toxic to mammalian cells.
- Solution:
- Re-formulate: Encapsulate the compound in a nanoparticle system (e.g., liposomes, polymeric NPs) to reduce its non-specific toxicity and enable targeted delivery [66].
- Optimize the Delivery Method: Consider local delivery approaches, such as microneedle patches for skin biofilm infections or coated medical implants, which can achieve high local concentrations while minimizing systemic exposure and toxicity [66].
- Screen Analogues: If cytotoxicity remains high, screen structural analogues of the compound to identify one with a better therapeutic index [6].
- Solution:
Quantitative Data on Promising Combination Therapies
The table below summarizes selected combination therapies that have demonstrated significant efficacy in eradicating biofilms in vitro and in some in vivo models [65].
Table 1: Efficacy of Selected Anti-biofilm Combination Therapies
| Dispersal Agent | Antibiotic | Tested Species | Treatment Efficacy (Reduction vs. Untreated Biofilm) | In vivo Model |
|---|---|---|---|---|
| Hamamelitannin analogue 38 (QSI) | Vancomycin | Staphylococcus aureus | 5.75-log reduction (Combination) vs. ≤1-log (Agent alone) | Yes |
| C11 (QSI) | Ciprofloxacin | Pseudomonas aeruginosa | 4-6-log reduction (Combination) vs. 1-2-log (Antibiotic alone) | Not Specified |
| Nitric Oxide (NO) nanoparticles | Tobramycin | Pseudomonas aeruginosa | 90% reduction (Combination) vs. ≤30% (Either agent alone) | Not Specified |
| G10KHc (AMP) | Tobramycin | Pseudomonas aeruginosa | 4-log reduction (Combination) vs. <1-log (Either agent alone) | Not Specified |
| Ambroxol (Repurposed Drug) | Vancomycin | Staphylococcus epidermidis | 7-log reduction (Combination) vs. ~3-log (Antibiotic alone) | Yes |
QSI: Quorum Sensing Inhibitor; AMP: Antimicrobial Peptide
Experimental Protocols
Protocol 1: Standard Checkerboard Assay for Synergy Screening in Biofilms
Method: [65] [68] This protocol helps determine the synergistic potential between a biofilm-dispersing agent and an antibiotic.
- Biofilm Growth: Grow biofilms in a 96-well microtiter plate for 24-48 hours using an appropriate medium.
- Agent Preparation: Prepare two-fold serial dilutions of the antibiotic in one direction of the plate and two-fold serial dilutions of the dispersal agent in the perpendicular direction. This creates a matrix where each well contains a unique combination of both agents.
- Treatment and Incubation: Carefully remove the spent medium from the biofilm plates and add the prepared drug mixtures. Incubate the plate for a further 24 hours at the appropriate temperature.
- Viability Assessment:
- Option A (CFU enumeration): Remove the treatment, gently wash the biofilm, and disrupt it by sonication or scraping. Serially dilute the suspension and plate on agar to determine the Colony Forming Units (CFU).
- Option B (Metabolic assay): Use a metabolic dye like resazurin or XTT to assess the viability of the treated biofilm.
- Data Analysis: Calculate the Fractional Inhibitory Concentration (FIC) index to quantify synergy (FIC ≤0.5), indifference (0.5 < FIC ≤4), or antagonism (FIC >4).
Protocol 2: Biofilm Disruption using Enzymatic Agents
Method: [1] This protocol describes how to test the efficacy of EPS-degrading enzymes.
- Biofilm Preparation: Grow a mature biofilm (typically 48-72 hours) on a suitable substrate (e.g., peg lids, glass coverslips).
- Enzyme Solution: Prepare a solution of the target enzyme (e.g., Dispersin B, DNase I, protease) in an appropriate buffer. Include a buffer-only control.
- Treatment: Submerge the biofilm-containing substrate in the enzyme solution or add the solution directly to the biofilm. Incubate for 1-2 hours at the enzyme's optimal temperature (e.g., 37°C).
- Analysis of Disruption:
- Biomass Quantification: Use crystal violet staining to measure the remaining biofilm biomass after enzymatic treatment.
- Viability and Dispersal: Perform CFU counts on the biofilm remaining on the substrate and the dispersed cells in the supernatant to differentiate between killing and dispersal.
- Visualization: Use scanning electron microscopy (SEM) or confocal laser scanning microscopy (CLSM) to visually confirm structural disruption of the biofilm matrix.
Mechanism of Action Diagrams
Diagram 1: Synergistic biofilm eradication pathway.
Research Reagent Solutions
Table 2: Essential Reagents for Anti-biofilm Combination Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Dispersin B | Glycoside hydrolase that targets PNAG polysaccharide in biofilm EPS. | Dispersal of biofilms formed by Staphylococcus epidermidis, E. coli, and other PNAG-producing species [1]. |
| DNase I | Enzyme that degrades extracellular DNA (eDNA) in the biofilm matrix. | Disruption of biofilms where eDNA is a major structural component, such as in Pseudomonas aeruginosa and Streptococcus mutans biofilms [1]. |
| Sodium Dodecyl Sulphate (SDS) | Ionic detergent that kills non-growing cells in the inner layers of biofilms. | Used as an adjuvant in combination with antibiotics to permeabilize cells and enhance killing efficacy [68]. |
| N-Acetylcysteine (NAC) | Mucolytic agent that disrupts disulfide bonds in polysaccharides and proteins. | Breaking down the viscoelastic structure of the EPS matrix in Pseudomonas aeruginosa biofilms, often combined with Ciprofloxacin [68]. |
| Nitric Oxide (NO) Donors (e.g., DETA-NO) | Signaling molecule that induces biofilm dispersal. | Used in combination with tobramycin or gentamicin to disperse and eradicate P. aeruginosa biofilms [65]. |
| Flow Cell System | Device for growing biofilms under dynamic, nutrient-flowing conditions. | Culturing mature, structurally relevant biofilms for testing penetration and efficacy of combination therapies [67]. |
Overcoming Translational Hurdles: From In Vitro Efficacy to Clinical Implementation
Addressing Limited In Vivo Efficacy and Host Cytotoxicity Concerns
Troubleshooting Guides
Guide: Overcoming Limited Efficacy in Animal Models
Problem: Your anti-biofilm compound shows excellent in vitro activity but fails to reduce bacterial burden in mouse wound infection models.
Solution: The limited efficacy likely stems from poor biofilm penetration and the complex polymicrobial environment not captured in simple in vitro assays [70].
Action 1: Re-evaluate Biofilm Model Complexity
- Procedure: Transition from single-species to dual-species or polymicrobial in vitro biofilm models before moving to in vivo studies. Use an electrospun gelatin-glucose matrix (Gel-Gluc) to mimic skin substrate [71].
- Rationale: Polybacterial biofilms significantly impair wound healing compared to single-species biofilms and trigger a greater host inflammatory response. Your compound's efficacy may be reduced against interacting microbial consortia [71].
Action 2: Enhance Biofilm Penetration
Action 3: Implement a Synergistic Combination
- Procedure: Test your compound in combination with conventional antibiotics (e.g., ciprofloxacin) using a checkerboard assay. Subsequently, validate efficacy in a dual-species biofilm model (e.g., S. aureus and P. aeruginosa on Gel-Gluc) [71] [66].
- Rationale: Combinatorial therapy can target both planktonic cells dispersed from the biofilm and the persistent cells within it. This approach can lower the required dose of individual agents, potentially reducing toxicity [66].
Guide: Mitigating Host Cytotoxicity
Problem: Your potent anti-biofilm agent shows significant cytotoxicity in mammalian cell lines (e.g., HEK-293), limiting its therapeutic potential.
Solution: Cytotoxicity can arise from non-specific mechanisms. The strategy is to redesign the therapeutic formulation to enhance its selectivity for bacterial targets over host cells [74].
Action 1: Explore Green-Synthesized Nanocomposites
- Procedure: Synthesize silver-based nanocomposites (e.g., Ag/AgCl) using plant extracts (e.g., Prunus mahaleb). Compare their anti-biofilm efficacy and cytotoxicity (using Brine Shrimp Lethality Assay or mammalian cell lines) against your current compound [74].
- Rationale: The composition and synthesis method critically determine the therapeutic window. Ag/AgCl nanocomposites have demonstrated strong anti-biofilm activity with low cytotoxicity (LC₅₀ > 300 µg/ml), unlike other silver forms [74].
Action 2: Utilize Natural Biofilm Disruptors as Adjuvants
- Procedure: Use sub-toxic concentrations of natural agents like curcumin, berberine, or N-acetylcysteine (NAC) to weaken the biofilm [72]. Follow with a lower, less toxic dose of your primary antimicrobial agent.
- Rationale: These disruptors interfere with quorum sensing and EPS integrity without high cytotoxicity. This adjuvant strategy can reduce the required dose of the primary, more toxic agent [66] [72].
Action 3: Employ Localized Delivery Systems
- Procedure: Incorporate your compound into a localized delivery system, such as an electrospun polycaprolactone (PCL) fibrous wound dressing [71]. This confines the high concentration of the agent to the infection site, minimizing systemic exposure and off-target effects [71] [66].
- Rationale: This physical containment strategy directly addresses the cause of cytotoxicity by limiting the interaction between the active compound and host cells.
Frequently Asked Questions (FAQs)
FAQ 1: Why are in vitro biofilm models often poor predictors of in vivo efficacy?
In vitro models frequently use single-species biofilms grown on plastic, lacking the physiological complexity of real infections. In contrast, in vivo environments feature polymicrobial interactions, host proteins, and an immune response that can alter drug penetration and efficacy [70] [71]. The shift to more biorelevant models, such as dual-species biofilms on artificial skin, is crucial for better predictive value [71].
FAQ 2: What are the primary mechanisms by which biofilms resist antimicrobials?
Biofilm resistance is multifactorial [21]:
- Physical Barrier: The EPS matrix limits drug penetration [33].
- Metabolic Heterogeneity: Gradients of nutrients and waste create zones of dormant, persistent cells that are highly tolerant to antibiotics [33].
- Upregulated Efflux Pumps: Expression of drug efflux pumps can be enhanced in biofilm cells [66].
- Enhanced Horizontal Gene Transfer: The close proximity of cells in a biofilm facilitates the spread of antibiotic resistance genes [70].
FAQ 3: Which rapid viability assay is recommended for treated biofilms?
While the SYTO9/PI staining (Live/Dead) is common, it can be unreliable. The combination of calcein AM (for esterase activity in live cells) and TMA-DPH (a membrane probe for residual biomass) has been proposed as a promising and reliable alternative for assessing biofilm viability after treatment [75].
FAQ 4: Are there non-antibiotic approaches to disrupting biofilms?
Yes, several promising strategies are in development [66] [73] [75]:
- Physical Disruption: Using microwave radiation or ultrasound to break apart the EPS structure [73].
- Enzymatic Degradation: Utilizing enzymes like DNase, dispersin B, or proteinases to target specific EPS components [33] [21].
- Quorum Sensing Inhibition: Employing small molecules (e.g., cinnamoyl hydroxamates) or natural compounds (e.g., curcumin) to block bacterial communication and virulence without killing them [21] [66] [75].
- Phage Therapy: Using bacteriophages (viruses that infect bacteria) and their enzymes (endolysins) to specifically target and lyse biofilm-forming bacteria [66] [75].
The following tables summarize key quantitative findings from recent studies on anti-biofilm agents and their cytotoxicity.
Table 1: Efficacy and Cytotoxicity of Silver Nanocomposites Data derived from green-synthesized nanoparticles using Prunus mahaleb, demonstrating the critical link between composition and therapeutic window [74].
| Nanocomposite Type | Source Plant Part | Anti-biofilm Inhibition (%) | Cytotoxicity (LC₅₀) | Therapeutic Index Note |
|---|---|---|---|---|
| Ag/AgO | Stem | Moderate | 28 ± 0.42 µg/ml | Higher cytotoxicity |
| Ag/Ag₂O | Leaf | Moderate | 28 ± 0.40 µg/ml | Higher cytotoxicity |
| Ag/AgCl | Fruit Pericarp | Strong (up to 145.7%) | > 300 µg/ml | Favorable profile |
Table 2: Physical Biofilm Disruption Methods A comparison of non-chemical methods for biofilm eradication on abiotic surfaces [73].
| Method | Key Parameter | Reduction in Cell Viability | Reduction in Regrowth | Key Advantage |
|---|---|---|---|---|
| Microwave Radiation | 2.45 GHz, 15 min | Up to 95% | Up to 75% | Rapid, no chemical residues |
| Ultraviolet (UV) Radiation | Biosafety cabinet, 20 min | Variable (Often lower than microwave) | Not specified | Surface sterilization |
| Dry Heat (Control) | 56°C, 15 min | Significantly lower than microwave | Not specified | Highlights non-thermal effects of microwaves |
Experimental Protocols
Title: Establishing a Biorelevant Dual-Species Biofilm Model for Efficacy Testing.
Principle: This protocol uses an electrospun gelatin-glucose (Gel-Gluc) matrix to mimic skin, providing a more physiologically relevant substrate for growing interacting wound pathogens like S. aureus, E. coli, and P. aeruginosa.
Workflow Diagram:
Materials:
- Strains: Wound pathogens (e.g., S. aureus DSM 2569, P. aeruginosa DSM 1117).
- Substrate: Electrospun Gelatin-Glucose (Gel-Gluc) matrix.
- Media: Dulbecco’s Modified Eagle Medium (DMEM/F-12) with 10% FBS for biofilm growth.
- Selective Agars: Mannitol Salt Phenol Red Agar (for S. aureus), Tergitol-7 agar (for E. coli/Pseudomonas differentiation).
Step-by-Step Method:
- Preparation of Inoculum: Suspend colonies of each bacterial strain in phosphate-buffered saline (PBS) and normalize to an optical density (OD₆₀₀) of 0.1 (~10⁸ CFU/mL).
- Inoculation: Combine the normalized bacterial suspensions in pairs. Apply the mixed inoculum onto the sterile Gel-Gluc matrix in a well plate.
- Biofilm Growth: Add DMEM/F-12 medium with 10% FBS and incubate under static conditions at 37°C for 24-48 hours to establish a mature dual-species biofilm.
- Treatment: Apply the test compound or fibrous wound dressing directly to the biofilm-on-matrix.
- Analysis: After treatment, dislodge the biofilm from the matrix by vortexing or sonication in PBS. Serially dilute the suspension and plate on the appropriate selective agars.
- Enumeration: Incubate plates and count colony-forming units (CFUs) for each species separately to determine the log reduction compared to an untreated control.
Title: A Simple Zoological Model for Preliminary Cytotoxicity Screening.
Principle: This assay uses Artemia salina (brine shrimp) nauplii to assess the toxicity of anti-biofilm compounds. The mortality rate after 24 hours of exposure provides an LC₅₀ value, a reliable indicator of general cytotoxicity.
Workflow Diagram:
Materials:
- Test Organism: Brine shrimp (Artemia salina) eggs.
- Artificial Seawater: 3.8% NaCl solution in distilled water.
- Compounds: Test anti-biofilm compounds dissolved in <3.2% DMSO.
- Controls: Vincristine sulfate (positive control), DMSO in seawater (negative control).
Step-by-Step Method:
- Hatching: Hatch brine shrimp eggs in a conical tube containing artificial seawater (3.8% NaCl) for 48 hours at 30°C with constant illumination and aeration.
- Sample Preparation: Prepare a series of concentrations of the test compound (e.g., from 0.1 to 300 µg/mL) in artificial seawater, ensuring the final concentration of DMSO does not exceed 3.2%.
- Exposure: Transfer 10 mature, phototactic nauplii into each tube containing the test solution or controls. Top up the volume to 5 mL with seawater.
- Incubation: Leave the tubes under illumination for 24 hours at room temperature.
- Assessment: After 24 hours, count the number of surviving nauplii in each tube.
- Calculation:
- Calculate the percentage of lethality for each concentration using the formula:
% Lethality = [(m - M) / S] × 100wherem= average dead larvae in sample,M= average dead larvae in blank control,S= average live larvae in blank control. - The LC₅₀ (concentration that kills 50% of the nauplii) is determined from a plot of percentage lethality versus log concentration.
- Calculate the percentage of lethality for each concentration using the formula:
Research Reagent Solutions
Table 3: Essential Materials for Advanced Anti-Biofilm Research
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Electrospun Gel-Gluc Matrix [71] | Acts as an artificial skin substrate for growing biorelevant biofilms. | Provides a more physiologically relevant 3D environment than polystyrene plates, improving translation to in vivo models. |
| Selective Bacterial Agars (e.g., Mannitol Salt, Tergitol-7) [71] | Differentiation and quantification of individual species in a polymicrobial biofilm after treatment. | Critical for deconvoluting the efficacy of a treatment against each pathogen in a mixed culture. |
| N-Acetylcysteine (NAC) [72] | Thiol-containing compound that disrupts disulfide bonds in the EPS matrix; used as a positive control for dispersal. | A well-known biofilm-disrupting agent useful for benchmarking new compounds or combination therapies. |
| Ciprofloxacin-loaded PCL Fibers [71] | A reference electrospun wound dressing for testing against biofilm-infected wound models. | Serves as a benchmark for local, sustained release of antimicrobials in efficacy studies. |
| Natural Biofilm Disruptors (e.g., Curcumin, Berberine) [72] | Herbal compounds with anti-quorum sensing and biofilm inhibitory properties; used as adjuvant therapies. | Their multi-target mechanisms can enhance the efficacy of conventional antibiotics and reduce resistance development. |
| Brine Shrimp (Artemia salina) [74] | A simple, inexpensive model for preliminary cytotoxicity screening of novel anti-biofilm compounds. | Provides a rapid LC₅₀ value that correlates with mammalian cell cytotoxicity, helping prioritize lead compounds. |
Optimizing Drug Formulations and Delivery Systems for Biofilm Penetration
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: Why are conventional antibiotics often ineffective against biofilm-associated infections?
Biofilms exhibit profound tolerance to antibiotics through multiple, concurrent mechanisms. The Extracellular Polymeric Substance (EPS) matrix acts as a barrier, physically impeding and adsorbing antibiotic molecules, preventing their penetration to the bacterial cells within [6] [76]. Furthermore, biofilms harbor heterogeneous bacterial subpopulations, including metabolically dormant cells and persister cells, which are highly tolerant to antibiotics that typically target active cellular processes [6] [1]. The biofilm microenvironment can also feature conditions like hypoxia and nutrient gradients that further reduce metabolic activity and antibiotic efficacy [6] [76]. Combined, these factors can lead to a requirement for antibiotic doses 10 to 1000 times higher than those needed to eradicate their planktonic counterparts [6] [76].
FAQ 2: What are the key physicochemical properties of a drug delivery system that enhance biofilm penetration?
The design of a delivery system must account for the unique properties of the biofilm matrix. Key characteristics include:
- Charge-Reversal Capability: Systems that are neutral or negatively charged in circulation (for stability) but become positively charged in the slightly acidic biofilm microenvironment can enhance penetration by interacting with negatively charged components of the EPS [76].
- Size and Surface Functionality: Nanoparticles and vesicles, particularly those with a protein-repellent outer corona (e.g., poly(ethylene oxide)), can more easily navigate the dense biofilm matrix [76] [6].
- Stimuli-Responsiveness: Systems designed to release their antimicrobial payload in response to specific biofilm stimuli (e.g., pH, enzymes, hypoxia) ensure targeted drug delivery and release [76].
FAQ 3: Which enzymatic strategies can disrupt the biofilm matrix to improve antibiotic efficacy?
Enzymes that degrade key structural components of the EPS are highly effective dispersal agents. The main classes include:
- Glycoside Hydrolases: Target exopolysaccharides. For example, Dispersin B hydrolyzes poly-β-(1,6)-N-acetyl-D-glucosamine (dPNAG), a common polysaccharide in many pathogens [1].
- Proteases: Degrade proteinaceous components of the matrix and can disrupt cellular surface proteins involved in adhesion [6] [1].
- Deoxyribonucleases (DNases): Break down extracellular DNA (eDNA), which is a crucial structural and adhesive element in many biofilms [6] [1]. Using these enzymes in combination with antibiotics can significantly improve treatment outcomes.
FAQ 4: What are some emerging non-antibiotic technologies for biofilm eradication?
Research is exploring several innovative approaches:
- Physical Energy: Using hyperthermia (via photothermal or magnetocaloric effects) or reactive oxygen species (ROS) (via photodynamic, sonodynamic, or chemodynamic effects) to physically disrupt and kill biofilms [76].
- Biological Control: Employing bacteriophages (phage therapy) or predatory bacteria like Bdellovibrio bacteriovorus that can lyse and prey on biofilm inhabitants [23] [77]. Engineered versions of these predators can also be used as "living antibiotics" or drug delivery vehicles [77].
- Quorum Sensing Inhibitors (QSIs): These molecules interfere with bacterial cell-to-cell communication, preventing the coordination needed for biofilm development and virulence [20].
Troubleshooting Guides
Problem 1: Poor Antibiotic Penetration in a Static Biofilm Model
| Symptom | Possible Cause | Solution |
|---|---|---|
| High Minimum Biofilm Inhibitory Concentration (MBIC) in vitro. | Dense EPS matrix blocking diffusion. | Pre-treat biofilms with matrix-degrading enzymes (e.g., DNase I, Protease K) or chelating agents (e.g., EDTA) to weaken the EPS [78] [1]. |
| Inconsistent results between replicate wells. | Non-uniform biofilm growth in static plates. | Transition to a dynamic biofilm model (e.g., flow cell or bioreactor) that provides constant nutrient flow and shear stress, generating more uniform and mature biofilms [67]. |
| Antibiotic is ineffective despite low MIC against planktonic cells. | Presence of persister cells. | Consider combination therapy that includes an antibiotic effective against dormant cells (e.g., a fluoroquinolone) or use a strategy that disrupts the metabolic dormancy, such as hyperbaric oxygen treatment [78]. |
Problem 2: Inefficient Performance of a Nano-formulation in an In Vivo Model
| Symptom | Possible Cause | Solution |
|---|---|---|
| Nanoparticles accumulate at the biofilm periphery but fail to penetrate the core. | The surface charge or size of the particles is not optimal for deep penetration. | Redesign particles to be smaller or incorporate a charge-reversal polymer that activates in the acidic biofilm pH [76]. |
| The formulation shows high efficacy in vitro but low efficacy in vivo. | The nanoparticles are being opsonized and cleared by the host immune system, or the in vivo biofilm structure is more complex. | Modify the nanoparticle surface with "stealth" coatings (e.g., PEG) to evade immune clearance and re-validate penetration in a more advanced biofilm model [76]. |
| Rapid clearance from the infection site. | Lack of targeting or sustained release mechanism. | Functionalize nanoparticles with targeting ligands (e.g., antibodies, peptides) specific to biofilm components and ensure the release kinetics are tuned for prolonged action [76]. |
Quantitative Data on Combination Therapies
Table 1: Selected Combination Therapies for Biofilm Eradication [78]
| Combination Therapy | Target Pathogen(s) | Proposed Mechanism of Action | Key Findings |
|---|---|---|---|
| N-Acetylcysteine (NAC) + Ciprofloxacin | Pseudomonas aeruginosa and others in cystic fibrosis | NAC inhibits EPS matrix production, disrupting biofilm integrity and allowing ciprofloxacin to penetrate. | Synergistic effect observed; NAC (4890 µg/mL) with Ciprofloxacin (32-64 µg/mL) showed significant antibiofilm activity. |
| Clarithromycin + Vancomycin | Pseudomonas aeruginosa, Staphylococcus spp. | Targets the alginate component of the EPS matrix, breaking down the protective barrier. | Effective in destroying both biofilm-forming and planktonic cells, particularly in UTIs. |
| Inhaled Fosfomycin + Tobramycin | Gram-negative and Gram-positive organisms | Synergistic antibiotic action; the combination overcomes individual resistance mechanisms. | Proven to be an effective strategy against a broad spectrum of biofilm-producing pathogens. |
| Anti-cancer Agent Repurposing (e.g., Cisplatin) | Pseudomonas aeruginosa | The specific antibiofilm mechanism is under investigation; shows efficacy in complex models. | Successfully eradicated biofilms in a murine keratitis model. |
Experimental Protocols
Protocol 1: Assessing Biofilm Penetration of a Nano-formulation using Confocal Microscopy
This protocol outlines the steps to visually confirm and quantify the penetration of a fluorescently labeled drug delivery system into a pre-formed biofilm.
Biofilm Growth:
- Grow a standardized biofilm (e.g., P. aeruginosa or S. aureus) in a flow cell system or on a relevant substrate (e.g, a glass coverslip) within a multi-well plate for 48-72 hours to ensure maturity [67].
- For dynamic growth, use a flow cell system with a peristaltic pump to provide a constant flow of fresh medium [67].
Formulation Incubation:
- Carefully introduce the fluorescently labeled nano-formulation (e.g., nanoparticles, polymer vesicles) into the biofilm system at the desired concentration in an appropriate buffer.
- Incubate under static or dynamic conditions for a predetermined time (e.g., 1-4 hours).
Biofilm Washing and Fixation:
- Gently wash the biofilm three times with phosphate-buffered saline (PBS) to remove non-adherent particles.
- Fix the biofilm with a suitable fixative (e.g., 4% paraformaldehyde for 30 minutes) if necessary for downstream analysis.
Staining and Imaging:
- Counterstain the biofilm biomass using a compatible fluorescent dye (e.g., SYTO 9 for bacterial cells, Concanavalin A for polysaccharides).
- Mount the sample and image using a confocal laser scanning microscope (CLSM).
- Acquire Z-stack images through the entire depth of the biofilm.
Image Analysis:
- Use image analysis software (e.g., ImageJ, IMARIS) to generate 3D reconstructions and orthogonal views of the biofilm.
- Quantify the fluorescence intensity of the nano-formulation at different depths (from top to bottom) to create a penetration profile.
Protocol 2: Evaluating Synergy of an Enzyme-Antibiotic Combination using a Microtiter Plate Assay
This protocol describes a standard method to test whether an EPS-degrading enzyme can synergize with an antibiotic to reduce biofilm biomass.
Biofilm Formation:
- In a 96-well microtiter plate, grow biofilms of the target pathogen for 24-48 hours in a suitable medium.
- After incubation, carefully remove the planktonic cells and spent medium by inverting and shaking the plate.
Treatment with Enzyme and Antibiotic:
- Prepare treatment solutions in fresh medium:
- Group A: Medium only (negative control).
- Group B: Antibiotic alone at sub-inhibitory concentrations (e.g., 1/4x or 1/2x MBIC).
- Group C: Enzyme alone (e.g., Dispersin B, DNase).
- Group D: Combination of antibiotic and enzyme.
- Add the treatments to the pre-formed biofilms and incubate for an additional 18-24 hours.
- Prepare treatment solutions in fresh medium:
Biofilm Quantification (Crystal Violet Staining):
- Wash the biofilms gently with PBS to remove non-adherent cells.
- Fix the biofilms with absolute methanol for 15 minutes, then air-dry.
- Stain with 0.1% crystal violet solution for 15 minutes.
- Wash thoroughly with water to remove excess stain.
- Elute the bound stain with 33% glacial acetic acid.
- Measure the absorbance of the eluent at 570 nm using a plate reader.
Data Interpretation:
- A significant reduction in absorbance in Group D compared to Group B and Group C indicates a synergistic effect between the enzyme and the antibiotic.
Research Reagent Solutions
Table 2: Essential Materials for Biofilm Penetration and Eradication Studies
| Reagent / Material | Function in Experiment | Example & Notes |
|---|---|---|
| Flow Cell System | To grow mature, heterogeneous biofilms under dynamic, nutrient-rich conditions that better mimic in vivo environments [67]. | Typical systems include a glass chamber, a peristaltic pump, medium reservoir, and tubing. Allows for real-time, non-destructive imaging. |
| Constant Depth Film Fermenter (CDFF) | To generate multiple, highly reproducible biofilms of a constant depth, useful for high-throughput testing of antimicrobials [67]. | More complex equipment with a rotating turntable and scraper blade to maintain biofilm depth. |
| Glycoside Hydrolases | To enzymatically disrupt the polysaccharide components of the biofilm EPS, facilitating antibiotic penetration [1]. | Dispersin B: Specific for dPNAG/PIA. Alginate Lyase: Specific for alginate in P. aeruginosa biofilms. |
| Deoxyribonucleases (DNases) | To degrade extracellular DNA (eDNA), a key structural and adhesive element in many bacterial biofilms [6] [1]. | DNase I: Commonly used to disrupt biofilms of species like S. aureus and P. aeruginosa. |
| Charge-Reversal Nanocarriers | A smart drug delivery system that enhances penetration by changing surface charge in response to the acidic biofilm microenvironment [76]. | Often composed of polymers with pH-sensitive functional groups (e.g., dimethylmaleic acid). |
| Quorum Sensing Inhibitors (QSIs) | To attenuate bacterial virulence and biofilm formation by interfering with cell-to-cell communication, without exerting a lethal pressure [20]. | Can be natural compounds (e.g., furanones) or synthetic molecules. Used as adjuvant therapy. |
Visualizations
Diagram 1: Mechanisms of Smart Drug Delivery for Biofilm Penetration
Diagram 2: Experimental Workflow for Evaluating Anti-Biofilm Formulations
Preventing Resistance to Anti-Biofilm Agents
Frequently Asked Questions & Troubleshooting Guides
This technical support resource addresses common challenges in research aimed at preventing resistance to anti-biofilm agents. The guidance is framed within the broader thesis context of developing robust strategies for biofilm disruption in persistent infections.
Understanding Biofilm Resistance Mechanisms
Why do biofilms exhibit intrinsic resistance to antimicrobial agents, and how does this relate to anti-biofilm agent resistance? Biofilms possess multiple intrinsic mechanisms of tolerance that can pre-dispose them to develop higher-level, stable resistance. The extracellular polymeric substance (EPS) matrix acts as a barrier, restricting the penetration of anti-biofilm agents and antimicrobials [79]. Furthermore, biofilms contain metabolically heterogeneous bacterial subpopulations, including persister cells, which are highly tolerant to treatment [15]. This inherent tolerance provides a window of opportunity for bacteria to acquire genetic mutations or horizontally transfer resistance genes, leading to stable resistance against your anti-biofilm compounds [15] [80].
What are the primary mechanisms by which biofilms develop resistance to specific anti-biofilm agents? Resistance can emerge through several mechanisms, often categorized as either innate or induced [80]:
- Innate (Pre-existing) Tolerance: This includes the physical barrier of the EPS matrix and the presence of dormant persister cells.
- Induced Resistance: This occurs in response to the anti-biofilm agent and can involve:
- Enzymatic Inactivation: Components of the biofilm matrix, such as enzymes, may inactivate the penetrated agent [17].
- Efflux Pump Upregulation: Bacteria can upregulate efflux systems to pump out the anti-biofilm agent [66].
- Genetic Adaptation: The close proximity of cells in a biofilm facilitates horizontal gene transfer, allowing resistance genes to spread rapidly through the community [15] [80].
- Mutation: Exposure to sub-lethal concentrations of an agent can select for mutants with enhanced resistance traits [6].
Experimental Design & Optimization
How can I prevent resistance from developing during my in vitro anti-biofilm assays? Resistance is often a consequence of sub-lethal dosing. To minimize this risk:
- Use Combination Therapies: Never rely on a single anti-biofilm agent. Combine agents that target different pathways, such as an EPS-degrading enzyme (e.g., DNase, dispersin B) with a conventional antibiotic or a quorum sensing inhibitor [33] [17] [66]. This multi-target approach makes it much harder for the biofilm to develop resistance.
- Ensure Sufficient Dosing and Contact Time: Conduct proper dose-response and time-kill assays to determine the Minimum Biofilm Inhibitory Concentration (MBIC) and Minimum Biofilm Eradication Concentration (MBEC), not just the MIC for planktonic cells [6]. Treatment concentrations must be sufficient to eradicate persister cells.
- Monitor for Early Resistance: Implement periodic susceptibility testing on biofilm-derived cells after exposure to your anti-biofilm agents to detect any shift in the MBIC/MBEC values.
My anti-biofilm agent was effective initially but lost efficacy in subsequent experiments. What could be happening? This is a classic sign of emerging resistance. We recommend the following troubleshooting steps:
- Check for Contamination: Rule out contamination of your bacterial stocks or agent solutions.
- Re-evaluate Agent Stability: Ensure your anti-biofilm agent is stable under your experimental storage and assay conditions (e.g., pH, temperature).
- Passage Experiment: Perform a serial passage experiment where you repeatedly expose the biofilm to sub-inhibitory concentrations of the agent. Measure the MBIC every few passages. A steady increase in MBIC is a clear indicator that the biofilm population is developing resistance [6].
- Analyze the Evolved Biofilm: Isolate the passaged, less-susceptible biofilm and use genomic techniques (e.g., whole-genome sequencing) to identify potential resistance mutations.
What are the best practices for quantifying biofilm formation and resistance in a high-throughput manner? Traditional methods like the Crystal Violet (CV) assay are common but have limitations, including low reproducibility and an inability to distinguish between live and dead cells [81] [82]. Consider these alternatives:
- Metabolic Assays: Use assays like resazurin which measures metabolic activity of viable cells within the biofilm [81].
- Advanced Staining Assays: The LIVE/DEAD BacLight assay uses fluorescent stains to differentiate between live and dead cells in a biofilm, providing a more accurate picture of viability after treatment [81].
- BioFilm Ring Test (BRT): This method is based on the immobilization of magnetic beads by the growing biofilm matrix and can provide a standardized, reproducible readout of biofilm formation in as little as 5 hours, making it suitable for screening [82].
Quantitative Data on Biofilm Resistance Mechanisms
Table 1: Key Mechanisms Contributing to Biofilm-Associated Tolerance and Resistance
| Mechanism Category | Specific Factor | Impact on Resistance/Tolerance | Experimental Evidence |
|---|---|---|---|
| Physical Barrier | Extracellular Polymeric Substance (EPS) Matrix [79] [15] | Restricts agent penetration; binds and neutralizes charged molecules [17]. | Up to 1000-fold increase in antibiotic tolerance compared to planktonic cells [6]. |
| Physiological Heterogeneity | Persister Cells [15] [80] | Dormant, metabolically inactive cells highly tolerant to antimicrobials. | Toxin-antitoxin systems block translation, leading to transient, high-level tolerance [17]. |
| Genetic Adaptation | Horizontal Gene Transfer (HGT) [15] [80] | Facilitates rapid spread of resistance genes within the biofilm community. | 10-fold increase in plasmid transfer efficiency in biofilms exposed to sub-lethal antibiotics [6]. |
| Biochemical Defense | Matrix Enzymes (e.g., catalase, β-lactamase) [6] [17] | Enzymatic degradation or modification of the anti-biofilm agent. | β-lactamase in K. pneumoniae biofilm degrades ampicillin, preventing penetration [6]. |
Table 2: Common Assays for Anti-Biofilm Efficacy and Resistance Monitoring
| Assay Type | What It Measures | Advantages | Limitations |
|---|---|---|---|
| Crystal Violet (CV) [81] | Total biofilm biomass (cells + matrix). | Inexpensive, simple, high-throughput. | Does not distinguish live/dead cells; low reproducibility [82]. |
| LIVE/DEAD BacLight & Fluorescence Microscopy [81] | Cell viability and spatial organization within the biofilm. | Distinguishes live vs. dead cells; provides structural data. | Semi-quantitative; requires specialized equipment. |
| BioFilm Ring Test (BRT) [82] | Early-stage biofilm formation strength. | Rapid (5h), standardized, high specificity and accuracy. | Requires specific equipment and magnetic beads. |
| Minimum Biofilm Eradication Concentration (MBEC) [6] | Minimum concentration required to eradicate a biofilm. | Clinically relevant; measures killing, not just inhibition. | Time-consuming (24-48h). |
Detailed Experimental Protocols
Protocol 1: Assessing Resistance Development via Serial Passage
Objective: To monitor the potential for a bacterial biofilm to develop resistance to a novel anti-biofilm agent over multiple generations.
Materials:
- Bacterial strain of interest
- Growth medium (e.g., Tryptic Soy Broth, LB Broth)
- Novel anti-biofilm agent solution
- Sterile 96-well flat-bottom polystyrene plates
- Plate reader or qPCR equipment
- Crystal violet solution (0.1%) or resazurin solution
Method:
- Day 1 - Initial Biofilm Formation: Grow a biofilm in a 96-well plate for 24-48 hours [6].
- Day 2 - First Treatment & Sub-Culturing:
- Treat the mature biofilm with a sub-inhibitory concentration (e.g., 0.5x MBIC) of your anti-biofilm agent for a set period (e.g., 24h).
- Gently disperse the biofilm from one well (e.g., via sonication or pipetting) and use this cell suspension to inoculate a new well with fresh medium containing the same sub-inhibitory concentration of the agent. This is Passage 1.
- In parallel, quantify the biofilm in the original treated well using a CV or resazurin assay to establish a baseline.
- Repetition: Repeat Step 2 every 24 hours for 10-15 passages, always sub-culturing the dispersed biofilm into a well with the same concentration of the anti-biofilm agent.
- Monitoring: Every 3-4 passages, use the dispersed cells to form a biofilm in a separate, agent-free plate. Then, perform a full MBIC assay to see if the susceptibility profile has changed. An increasing MBIC indicates developing resistance.
Protocol 2: Evaluating Synergy in Combination Therapy
Objective: To determine if combining two anti-biofilm agents with different mechanisms of action can prevent resistance and enhance efficacy.
Materials:
- As in Protocol 1, plus a second anti-biofilm agent (e.g., a quorum sensing inhibitor and an EPS-degrading enzyme).
Method:
- Biofilm Formation: Grow a standard biofilm as in Protocol 1.
- Checkerboard Assay Setup:
- Prepare a dilution series of Agent A along the rows of a 96-well plate.
- Prepare a dilution series of Agent B along the columns.
- Ensure the final volume in each well is consistent. Include controls for growth (no agent) and sterility (medium only).
- Treatment and Incubation: Gently add the pre-formed biofilm to each well of the checkerboard plate. Incubate for the desired treatment time.
- Analysis:
- Quantify the remaining biofilm using a metabolic assay like resazurin.
- Calculate the Fractional Inhibitory Concentration Index (FICI). A FICI of ≤0.5 indicates synergy, meaning the combination is significantly more effective than either agent alone and can help overcome intrinsic tolerance [33] [66].
Signaling Pathways and Experimental Workflows
Biofilm Resistance Development Pathway
Combination Therapy Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Anti-Biofilm Resistance Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Dispersin B (Enzyme) | Degrades poly-N-acetylglucosamin (PNAG), a key polysaccharide in staphylococcal biofilm matrices [33] [6]. | Effective against biofilms reliant on polysaccharide adhesion; used to disrupt EPS barrier. |
| DNase I (Enzyme) | Degrades extracellular DNA (eDNA) in the biofilm matrix, weakening structure and enhancing penetration [33] [15]. | Crucial for biofilms where eDNA is a major matrix component (e.g., P. aeruginosa). |
| Quorum Sensing Inhibitors (e.g., Furanones, AHL analogs) | Block cell-to-cell communication, preventing coordinated biofilm development and virulence [6] [80]. | Target the regulation of biofilm formation rather than killing cells, potentially reducing selective pressure. |
| Magnetic Beads (for BRT) | Used in the BioFilm Ring Test to quantify early-stage biofilm formation by measuring immobilization [82]. | Enables rapid, standardized screening of biofilm formation and anti-biofilm agent efficacy. |
| Resazurin Dye | A metabolic indicator used to quantify the number of viable cells in a biofilm after treatment [81]. | Provides a more relevant measure of biocidal activity than biomass stains like crystal violet. |
| Crystal Violet Stain | A basic dye that binds negatively charged molecules, providing a classic measure of total biofilm biomass [81]. | Use with caution; best for initial screening but should be complemented with viability assays. |
Challenges in Biofilm Detection and Diagnostic Limitations
Within the context of developing strategies to disrupt biofilms in persistent infections, a significant initial hurdle is their reliable detection and diagnosis. Biofilms are structured communities of microbial cells encased in a self-produced matrix of Extracellular Polymeric Substances (EPS) that can exhibit up to a thousand-fold increased tolerance to antibiotics compared to their free-floating (planktonic) counterparts [23] [1]. This inherent resistance makes biofilm-associated infections particularly challenging to eradicate. The diagnostic process is complicated by the biofilm's protective EPS, which can lead to false-negative results in conventional culture-based diagnostics and mask the true severity and nature of an infection [23]. Accurately identifying the presence and composition of a biofilm is therefore the critical first step in deploying effective, targeted countermeasures, a challenge that researchers and clinicians continue to grapple with due to the complex and variable nature of biofilm infrastructure.
Frequently Asked Questions (FAQs)
Q1: Why do standard diagnostic methods often fail to accurately detect biofilm-associated infections? Standard diagnostic methods, which typically rely on culturing planktonic bacteria from body fluids or tissue samples, often fail because bacterial cells within a mature biofilm are tightly embedded in the EPS matrix and are not readily released into samples sent for analysis [23]. This can lead to false-negative results or an underestimation of the bacterial load. Furthermore, cells in a biofilm state have different metabolic and physiological profiles, which can make them less detectable by conventional means.
Q2: What makes the Extracellular Polymeric Substance (EPS) a challenging target for analysis? The EPS matrix is a complex and dynamic mixture of macromolecules, primarily polysaccharides, proteins, lipids, and extracellular DNA (eDNA) [83] [19]. Its exact composition is highly variable and is influenced by the specific microbial species present, environmental conditions (e.g., nutrient availability, shear forces), and interactions between different EPS components [83]. This heterogeneity means there is no single, universal "biofilm marker" that can be easily identified and measured across different infections or industrial settings [83] [84].
Q3: How do polymicrobial biofilms complicate diagnosis and treatment? Many clinical biofilms are polymicrobial, containing multiple species of bacteria and sometimes fungi [70]. These different microorganisms engage in complex interkingdom interactions, which can enhance the biofilm's overall structural integrity and resistance profile. A diagnostic test that identifies only one species may miss other key contributors to the infection. Moreover, treating a single species within a polymicrobial consortium is often ineffective, as the remaining species can maintain the biofilm structure and re-populate the community [70].
Q4: What are the limitations of current biofilm monitoring techniques in industrial and clinical settings? There is a lack of standardized, rapid techniques for biofilm monitoring. Many current methods are:
- Labor-intensive and not real-time: Requiring sample collection and offline analysis.
- Inconsistent: Lacking harmonization across sectors, leading to regulatory ambiguity [85].
- Not correlative: For instance, visual inspection alone does not correlate with microbial cell counts, and a surface can be visibly clean yet harbor biofilms [83].
Troubleshooting Guides
Issue: Inconsistent Biofilm Detection in a Research Model
Problem: Your in vitro biofilm model yields highly variable results between experimental runs, making it difficult to assess the efficacy of anti-biofilm compounds.
Solution:
- Standardize Growth Conditions: Meticulously control and document environmental factors such as temperature, nutrient media, shear forces (agitation speed), and incubation time, as these profoundly influence EPS composition and biofilm architecture [83].
- Characterize Your Baseline: Instead of relying on a single quantification method (e.g., crystal violet), use complementary techniques to profile your specific biofilm. This includes quantifying key EPS components like eDNA, proteins, and polysaccharides to establish a baseline "fingerprint" for your model system [83] [1].
- Include Appropriate Controls: Always include a known strong biofilm-forming strain (e.g., Pseudomonas aeruginosa or Staphylococcus aureus) and a non-biofilm forming mutant or strain as positive and negative controls, respectively, to validate your assay conditions.
Issue: Suspected Biofilm Infection with Negative Culture
Problem: A patient presents with strong clinical signs of a persistent infection (e.g., on a medical implant), but standard microbiological cultures repeatedly return negative.
Solution:
- Suspect Biofilm: Consider a biofilm-associated infection as a primary hypothesis.
- Employ Biofilm-Sensitive Diagnostics: Utilize diagnostic tools that can disrupt the EPS matrix or detect biofilm-specific components.
- Sonication: Vigorous sonication of explanted medical devices (e.g., prosthetic joints, catheters) can dislodge biofilm cells, significantly improving microbial recovery in culture compared to standard swabbing [23].
- Molecular Methods: Use PCR or next-generation sequencing to detect microbial DNA, which can remain present even when cells are not culturable [70].
- Microscopy: If tissue or device material is available, techniques like Scanning Electron Microscopy (SEM) or Confocal Laser Scanning Microscopy (CLSM) can visually confirm the presence of the three-dimensional biofilm structure [83].
Quantitative Data on Biofilm-Related Challenges
Table 1: Impact of Biofilms on Human Health and Detection
| Aspect | Quantitative Data | Context / Implication |
|---|---|---|
| Prevalence in Infections | 65-80% of all human microbial infections [1] | Highlights that the vast majority of persistent infections are biofilm-based. |
| Prevalence on Medical Devices | 65-80% across various healthcare settings [23] | Underscores the major risk posed by indwelling devices like catheters and prosthetics. |
| Antibiotic Tolerance | Up to 1000x increased tolerance compared to planktonic cells [1] | Explains the frequent failure of conventional antibiotic therapies. |
| Polymicrobial Biofilm Resistance | ~10x more resistant to antibiotics than mono-species biofilms [70] | Demonstrates the enhanced defense offered by multi-species communities. |
Table 2: Key Macromolecular Components of the Biofilm EPS Matrix [83] [1] [19]
| EPS Component | Main Functions | Research Analysis Techniques |
|---|---|---|
| Polysaccharides | Structural integrity, adhesion, cohesion, water retention. | Colorimetric assays (e.g., phenol-sulfuric acid), HPLC, GC-MS. |
| Proteins | Structural support, enzymatic activity, adhesion. | Bradford/Lowry assays, SDS-PAGE, proteomics. |
| Extracellular DNA (eDNA) | Structural support, horizontal gene transfer, nutrient source. | Fluorometric assays (e.g., PicoGreen), agarose gel electrophoresis. |
| Lipids | Hydrophobicity, adhesion, signaling. | Gravimetric analysis, thin-layer chromatography, GC. |
Experimental Protocols for EPS Analysis
Protocol 1: Extraction and Quantification of extracellular DNA (eDNA) from Biofilms
Principle: eDNA is a critical structural component in many biofilms, such as those formed by Pseudomonas aeruginosa and Staphylococcus aureus. This protocol isolates and quantifies eDNA to assess its contribution to biofilm integrity [1] [19].
Methodology:
- Biofilm Growth: Grow biofilms in a desired in vitro model (e.g., Calgary biofilm device, flow cell, or multi-well plate).
- Harvesting: Carefully scrape the biofilm biomass from the surface and suspend it in a suitable buffer (e.g., phosphate-buffered saline).
- eDNA Extraction: Separate the eDNA from cellular DNA. This can be achieved by:
- Centrifuging the biofilm suspension at low speed (e.g., 2,000 x g for 10 minutes) to pellet cells, then collecting the eDNA-containing supernatant.
- Alternatively, incubating the suspension with a chelating agent (e.g., Chelex resin) to protect eDNA from degradation.
- Quantification: Measure the concentration of eDNA in the supernatant using a fluorescent DNA-binding dye, such as PicoGreen, according to the manufacturer's instructions. Compare against a standard curve of known DNA concentrations.
Protocol 2: Enzymatic Disruption of Biofilms using Glycoside Hydrolases
Principle: Enzymes that degrade key EPS components can effectively disperse biofilms, rendering the cells more susceptible to antimicrobials. This protocol uses glycoside hydrolases to target exopolysaccharides [1].
Methodology:
- Biofilm Formation: Grow a mature biofilm in a multi-well plate.
- Enzyme Treatment: Gently wash the biofilm and treat it with a solution containing a specific glycoside hydrolase (e.g., Dispersin B, which targets poly-N-acetylglucosamine/PNAG, or alginate lyase for P. aeruginosa alginate).
- Incubation: Incubate the plate at the optimal temperature and pH for the enzyme activity (e.g., 37°C for 1-2 hours).
- Assessment of Dispersal:
- Quantitative: Use a crystal violet staining assay to measure the remaining biofilm biomass after enzymatic treatment.
- Viability: Combine the enzyme treatment with a sub-lethal dose of a conventional antibiotic and perform a colony-forming unit (CFU) count to demonstrate enhanced killing of the dispersed cells.
Visualization of Biofilm Diagnostics and Challenges
Biofilm Diagnostic Pathway
EPS Complexity and Detection Challenge
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biofilm Detection and Analysis
| Item | Function / Application | Example Use Case |
|---|---|---|
| Glycoside Hydrolases (e.g., Dispersin B, Alginate Lyase) | Enzymatic disruption of polysaccharide components in the EPS matrix [1]. | Used to evaluate the structural role of specific exopolysaccharides and to sensitize biofilms to antibiotics. |
| Proteases (e.g., Proteinase K) | Degradation of protein components within the EPS [1]. | Determines the contribution of proteins to biofilm adhesion and stability. |
| Deoxyribonucleases (DNases) | Degradation of extracellular DNA (eDNA) in the matrix [1]. | Used to assess the structural role of eDNA and to reduce biofilm biomass. |
| Fluorescent DNA-binding Dyes (e.g., PicoGreen) | Quantification of eDNA content in biofilm extracts [19]. | Provides a quantitative measure of a key EPS component. |
| Crystal Violet Stain | A common dye used to quantify total biofilm biomass attached to a surface. | Standard, high-throughput method for assessing biofilm formation and eradication in microtiter plates. |
| Quorum Sensing Inhibitors (QSIs) | Small molecules that disrupt bacterial cell-to-cell communication, preventing coordinated biofilm behaviors [20]. | Investigated as potential anti-biofilm agents that do not kill bacteria but rather render them less virulent and organized. |
| Microtiter Plates & Flow Cells | Core platforms for growing in vitro biofilms under static (plates) or dynamic, shear-controlled (flow cells) conditions. | Foundational tools for creating reproducible and controllable biofilm models for research. |
Economic Considerations and Healthcare System Implementation Barriers
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary economic factors driving the need for novel biofilm disruption strategies? The economic burden of biofilm-associated infections is substantial, driven by prolonged hospital stays, treatment complexities, and high management costs. The global biofilm treatment market is projected to grow from USD 2.38 billion in 2025 to USD 4.13 billion by 2032, reflecting the escalating financial impact. Chronic wound infections, which are frequently complicated by biofilms, represent the largest segment by infection type, accounting for an estimated 35.2% of the market in 2025 [86]. The intrinsic resistance of biofilms to conventional antibiotics necessitates costly combination therapies and advanced treatment modalities, contributing to this economic burden [87].
FAQ 2: What are the key implementation barriers for new antibiofilm technologies in healthcare systems? Key barriers include high research and development costs, regulatory hurdles for combination therapies, and the need for specialized equipment and training. For instance, while shockwave therapy and nanoparticle-based treatments show promise, their translation to clinical practice requires significant investment and adaptation of existing clinical workflows [12] [73]. Furthermore, the scalability and material compatibility of novel physical methods like microwave radiation need to be thoroughly evaluated for widespread hospital adoption [73].
FAQ 3: How does biofilm formation increase treatment costs compared to planktonic infections? Biofilms can increase treatment costs significantly due to their high resistance to antimicrobials, which can be 10 to 1000-fold greater than that of planktonic cells [73]. This resistance leads to persistent infections, extended patient hospitalization, and the requirement for repeated treatments or surgical interventions. The complexity of eradicating biofilms often demands integrative approaches combining mechanical debridement, advanced antimicrobials, and novel disruption technologies, all of which contribute to higher overall healthcare costs [87] [86].
FAQ 4: Which biofilm disruption technologies are most ready for clinical adoption? Currently, debridement equipment dominates the product segment of the biofilm treatment market, holding a 34.2% share, as it is a foundational step for physically removing biofilm biomass [86]. Advanced technologies such as nanoparticle-enabled drug delivery [88] [87], phage-antibiotic synergistic (PAS) therapies [87] [75], and quorum-sensing inhibitors [88] [75] are showing strong translational potential in research settings. Physical methods like shockwave treatment [12] are also moving toward clinical validation for specific applications, such as disrupting biofilms on medical implants.
Troubleshooting Guides
Guide 1: Addressing Variable Efficacy in Physical Biofilm Disruption Methods
Problem: Inconsistent biofilm disruption results when using physical methods like shockwave or microwave treatment.
Solution:
- Step 1: Verify Parameter Calibration. Ensure all physical parameters are meticulously controlled. For shockwave therapy, confirm pulse count (e.g., 120 pulses), frequency (e.g., 2 Hz), and energy settings (e.g., 4 kV) [12]. For microwave radiation, standardize exposure time (e.g., 15 minutes) and power output to ensure reproducible dielectric heating [73].
- Step 2: Standardize Biofilm Growth Conditions. Biofilm architecture is highly sensitive to growth conditions. Use consistent media (e.g., TSB for Pseudomonas aeruginosa [12] or YESCA for Escherichia coli [73]), incubation temperature, and surface materials (e.g., silicone tubes [12] or glass coverslips [73]) across experiments to minimize biological variability.
- Step 3: Include Appropriate Controls. Always include controls for thermal effects. For microwave experiments, use dry heat controls (e.g., 45°C for 10 minutes) to decouple electromagnetic effects from plain thermal degradation [73].
Guide 2: Overcoming Limited Penetration of Antimicrobials into Biofilms
Problem: Antimicrobial agents fail to penetrate the biofilm's extracellular polymeric substance (EPS) matrix, leading to treatment failure.
Solution:
- Step 1: Pre-treat with Matrix-Degrading Agents. Incorporate enzymes such as Dispersin B (targets polysaccharides) or DNase I (degrades extracellular DNA) to weaken the EPS scaffold before antibiotic application [87]. This enhances diffusion and access to embedded bacterial cells.
- Step 2: Utilize Nanoparticle Carriers. Employ engineered nanoparticles (e.g., silver, zinc oxide, or graphene-based) [87] or lipid-based nanocarriers to encapsulate antibiotics. These systems can improve penetration and provide sustained release within the biofilm microenvironment [88].
- Step 3: Combine with Physical Disruption. Pair antimicrobial treatment with a physical disruption method. For example, applying low-energy shockwaves [12] or microwave radiation [73] can create micro-fractures in the biofilm, significantly improving antibiotic efficacy, as demonstrated by a 40% reduction in bacterial viability when ciprofloxacin was combined with shockwaves [12].
Quantitative Data on Biofilm Disruption Technologies
Table 1: Efficacy and Parameters of Physical Biofilm Disruption Methods
| Technology | Test Organism | Key Parameters | Reported Efficacy | Reference |
|---|---|---|---|---|
| Shockwave Treatment | Pseudomonas aeruginosa | 120 pulses, 2 Hz, 4 kV | 97.5% biofilm area removal; 40% reduction in viability with ciprofloxacin | [12] |
| Microwave Radiation | Escherichia coli UTI89 | 2.45 GHz, 15 min exposure | 95% reduction in cell viability; 25% regrowth potential | [73] |
Table 2: Market and Economic Data for Biofilm Treatment (2025 Projections)
| Segment | Leading Category | Projected Market Share (2025) | Key Driver | Reference |
|---|---|---|---|---|
| Treatment Method | Antimicrobial Agents (Antibiotics) | 35.2% | Broad-spectrum efficacy and established clinical use | [86] |
| Product Type | Debridement Equipment | 34.2% | Essential role in mechanical biofilm disruption | [86] |
| Infection Type | Chronic Wound Infections | 35.2% | Rising incidence and complexity of care (e.g., diabetic foot ulcers) | [86] |
| Geography | North America | 38.3% | Advanced healthcare infrastructure and stringent regulations | [86] |
Detailed Experimental Protocols
Protocol 1: Shockwave Treatment for Biofilm Disruption in Tubular Structures
This protocol is adapted from a study investigating the disruption of Pseudomonas aeruginosa biofilms on silicone tubes using an intravascular lithotripsy system [12].
1. Biofilm Formation:
- Materials: Silicone tube (inner diameter: 4 mm), Tryptic Soy Broth (TSB), P. aeruginosa culture (e.g., KCTC 22073).
- Method:
- Circulate the bacterial culture (OD₆₀₀ ≈ 0.5) through the silicone tube system for 72 hours at 35°C using a peristaltic pump.
- Supply fresh TSB medium three times daily and provide a continuous air supply to promote robust biofilm formation under dynamic conditions.
2. Shockwave Treatment:
- Materials: Shockwave C2+ intravascular lithotripsy (IVL) balloon catheter, customized holder, water bath.
- Method:
- Cut the biofilm-colonized tube into 3 cm segments.
- Fix each segment in a conical tube filled with saline, submerged in a 37°C water bath.
- Position the IVL catheter inside the tube so the emitter contacts the inner wall.
- Apply shockwaves at 4 kV, with a frequency of 2 Hz, for a total of 120 pulses (60 seconds).
3. Post-Treatment Analysis:
- Viability Assessment (CFU): Sonicate and vortex treated tubes to dislodge bacteria. Serially dilute the suspension, plate on Tryptic Soy Agar, and count colonies after 24-hour incubation at 37°C [12].
- Biomass Assessment (Crystal Violet): Stain treated tubes with 1% crystal violet for 20 minutes. Dissolve the bound dye in ethanol and measure the optical density at 600 nm [12].
- Visualization (SEM/CLSM): Use scanning electron microscopy (SEM) for structural analysis or confocal laser scanning microscopy (CLSM) with LIVE/DEAD BacLight stain (SYTO9/PI) to visualize live/dead bacteria [12].
Protocol 2: Microwave Radiation for Biofilm Eradication on Surfaces
This protocol details the use of microwave radiation to disrupt Escherichia coli biofilms formed on glass and catheter-mimicking surfaces [73].
1. Biofilm Preparation:
- Materials: Glass coverslips or catheter tubing segments, LB Broth, YESCA Medium with 4% DMSO, E. coli UTI89 culture.
- Method:
- Inoculate sterile 12-well plates containing coverslips or catheter pieces with a diluted bacterial culture in YESCA medium.
- Incubate statically at 25°C for 4 days to allow mature biofilm development.
2. Microwave Exposure:
- Materials: Domestic microwave oven (operating at 2.45 GHz), thermal gun.
- Method:
- Aseptically retrieve biofilm-covered samples and place them on butter paper.
- Expose to microwave radiation for 15 minutes. Monitor surface temperature with a thermal gun to ensure consistency and avoid excessive heating.
3. Post-Exposure Analysis:
- Viability and Regrowth Assay: Resuspend dislodged biofilms in PBS. Measure CFU immediately post-treatment and after re-incubation to assess regrowth potential [73].
- Structural Analysis (FE-SEM/CLSM): Use field-emission scanning electron microscopy (FE-SEM) to examine structural disintegration and CLSM with membrane integrity dyes to confirm cellular damage [73].
Signaling Pathways and Experimental Workflows
Diagram 1: Key Pathways in Biofilm Formation and Disruption
Diagram 2: Shockwave Disruption Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biofilm Disruption Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Silicone Tubing | Abiotic surface for growing flow-condition biofilms | Modeling catheter-associated biofilms [12] |
| Crystal Violet | Colorimetric dye for quantifying total biofilm biomass | Standard CV assay for high-throughput screening [12] [42] |
| LIVE/DEAD BacLight Kit (SYTO9/PI) | Fluorescent viability staining for CLSM | Differentiating live/dead bacteria in treated biofilms [12] |
| Dispersin B & DNase I | Enzymatic degradation of polysaccharides and eDNA in EPS | Weakening biofilm matrix to enhance antibiotic efficacy [87] |
| Ciprofloxacin | Fluoroquinolone antibiotic for anti-biofilm efficacy studies | Testing combination therapies with physical disruption [12] |
| Shockwave IVL Catheter | Device for generating focused acoustic pressure waves | Physical disruption of biofilms on medical implants [12] |
| YESCA Medium + DMSO | Culture medium for promoting robust E. coli biofilm growth | Standardized in vitro biofilm model formation [73] |
Evaluating Anti-Biofilm Strategies: Efficacy Metrics, Model Systems, and Clinical Evidence
Definitions and Core Concepts
What are MBIC and MBEC, and how do they differ from MIC?
The Minimum Biofilm Inhibitory Concentration (MBIC) is defined as the lowest concentration of an antimicrobial agent that prevents biofilm formation, typically by inhibiting the time-dependent increase in viable biofilm cells [89]. In contrast, the Minimum Biofilm Eradication Concentration (MBEC) is the lowest concentration that eradicates a pre-established, mature biofilm, often defined as achieving a 99.9% (3 log₁₀) reduction in colony-forming units (CFU) compared to the baseline pre-treatment biofilm [89] [90].
Unlike the Minimum Inhibitory Concentration (MIC), which is determined against free-floating (planktonic) bacteria, both MBIC and MBEC measure the much higher tolerance of biofilm-associated bacteria to antimicrobial agents [89] [91]. This distinction is clinically critical, as biofilms can be 100 to 1000 times more tolerant to antibiotics than their planktonic counterparts [92].
Why is quantifying the pre-treatment biofilm essential for accurate MBEC determination?
A crucial, yet often overlooked, step in MBEC assays is the individual quantification of the mature biofilm before antimicrobial exposure [89]. Relying solely on the untreated control biofilm at the experiment endpoint can lead to misinterpretation of the results.
The table below illustrates how changes in the untreated control biofilm over time affect the interpretation of the anti-biofilm effect [89]:
| Scenario | Pre-Treatment Biofilm (CFU/mL) | Untreated Control at Endpoint (CFU/mL) | Treated Biofilm at Endpoint (CFU/mL) | Correct Interpretation | Misinterpretation if Pre-Treatment is Not Measured |
|---|---|---|---|---|---|
| A | 10⁵ | 10⁸ | 10⁵ | 3 log₁₀ inhibition of growth (MBIC) | 3 log₁₀ reduction (incorrect) |
| B | 10⁷ | 10⁸ | 10⁵ | 2 log₁₀ biofilm reduction | 3 log₁₀ reduction (incorrect) |
| C | 10⁸ | 10⁸ | 10⁵ | 3 log₁₀ biofilm reduction (MBEC) | 3 log₁₀ reduction (correct) |
| D | 10⁹ | 10⁸ | 10⁵ | 3 log₁₀ biofilm reduction (MBEC) | 3 log₁₀ reduction (correct) |
Table 1: The critical importance of quantifying the pre-treatment biofilm for accurate MBEC and MBIC interpretation. Scenarios A and B show how a lack of pre-treatment data leads to incorrect conclusions about the effect size and type [89].
Standardized Experimental Protocols
Protocol 1: MBIC and MBEC Assay using a Peg-Lid System (Calgary Biofilm Device)
This protocol is adapted for high-throughput screening and uses a peg-lid device, which allows biofilms to form on pegs suspended in a standard 96-well microtiter plate [93] [92].
Materials:
- MBEC Assay Biofilm Inoculator (or similar peg-lid device) [93]
- Appropriate culture media (e.g., Tryptic Soy Broth (TSB), Mueller Hinton Broth (MHB))
- Antimicrobial agent stock solutions
- Phosphate Buffered Saline (PBS)
- Sonicator with a solid tray insert [93]
- Equipment for endpoint analysis (e.g., microplate reader)
Procedure:
- Inoculation: Prepare a bacterial suspension of 1 x 10⁵ to 1 x 10⁶ CFU/mL in a suitable growth medium [93] [90]. Dispense 150-200 µL per well into a 96-well plate.
- Biofilm Growth: Place the peg-lid onto the plate, ensuring the pegs are submerged. Incubate under optimal conditions (e.g., 37°C) for 24-48 hours with shaking (e.g., 110 rpm) to form mature biofilms. Maintain humidity at 75-90% to prevent evaporation [93].
- MBIC Assay:
- For MBIC, transfer the peg-lid with newly forming biofilms to a new plate containing serial dilutions of the antimicrobial agent.
- Incubate for a further 20-24 hours.
- Assess the inhibition of biofilm formation using a viability stain (e.g., resazurin) or CV staining [92].
- MBEC Assay:
- For MBEC, first allow mature biofilms to form on the pegs over 24-48 hours.
- Quantify Pre-Treatment Biofilm (Critical Step): Snap off several pegs into a recovery medium, sonicate, and vortex to disaggregate cells. Perform serial dilution and plate to determine the baseline CFU/mL [89].
- Transfer the peg-lid with mature biofilms to a new plate containing serial dilutions of the antimicrobial agent.
- Incubate for 20-24 hours.
- Assess biofilm eradication by processing the pegs for viable cell counts.
- Biofilm Recovery and Analysis:
- Wash the peg-lid gently in PBS to remove non-adherent cells.
- Transfer the lid to a new plate containing a recovery medium (e.g., PBS).
- Sonicate the plate for 30 minutes in a water bath sonicator to dislodge biofilm cells [93].
- Vortex the plate to create a homogeneous cell suspension.
- Determine viable counts by serial dilution and plating, or use a metabolic dye like resazurin.
Protocol 2: Biofilm Viability Staining with Resazurin
Resazurin is a redox dye that changes from blue, non-fluorescent to pink, highly fluorescent resorufin in the presence of metabolically active cells [90]. It is ideal for assessing MBIC and the metabolic state of a biofilm.
Optimized Conditions for Resazurin Assay [90]:
| Parameter | Gram-Positive Bacteria (e.g., Staphylococci) | Gram-Positive Bacteria (e.g., Enterococci) |
|---|---|---|
| Resazurin Concentration | 4 µg/mL | 8 µg/mL |
| Incubation Temperature | 25°C | 25°C |
| Incubation Time | 20 minutes | 40 minutes |
| Detection | Fluorescence (λEx 530 nm / λEm 590 nm) | Fluorescence (λEx 530 nm / λEm 590 nm) |
Table 2: Standardized resazurin assay conditions for Gram-positive clinical reference strains, as optimized for reliable results (Z' > 0.5) [90].
Procedure:
- After antimicrobial treatment, carefully aspirate the medium and wash the biofilm once with PBS.
- Add the diluted resazurin solution to the wells containing biofilm and to negative control wells (medium only).
- Incubate in the dark under the conditions specified in Table 2.
- Measure the fluorescence. The MBIC is the lowest antimicrobial concentration that results in a significant reduction in fluorescence compared to the untreated growth control.
Troubleshooting Common Experimental Issues
FAQ 1: I am having trouble growing a consistent, robust biofilm. What can I do?
Poor biofilm growth is a common issue. Consider the following troubleshooting steps [93] [90] [92]:
- Check the Inoculum: Start with a standardized inoculum between 10⁵ and 10⁶ CFU/mL.
- Optimize Media and Supplements: For many Gram-positive strains like Staphylococcus aureus and Enterococcus faecalis, Tryptic Soy Broth (TSB) supplemented with 1% glucose (TSBG) promotes maximum biofilm production [90]. Test different media for your specific strain.
- Control Humidity: Incubate plates in a humidified environment (75-90% humidity) to prevent wells from drying out during extended incubation [93].
- Use Agitation: Place the assay plate on an orbital shaker at ~110 rpm during incubation to create low shear stress, which enhances nutrient exchange and attachment [93].
- Consider Surface Coating: For strains that form weak biofilms, use peg-lids coated with hydroxyapatite to simulate bone/teeth surfaces, which can significantly enhance attachment and growth [93].
- Extend Incubation Time: Some species, such as Enterococci, may require a longer incubation period (e.g., 48 hours) to form substantial biofilms [90].
FAQ 2: Why is there high variability in my biofilm viability measurements?
High variability can stem from several sources [92]:
- Inconsistent Biofilm Handling: Aggressive washing or pipetting can dislodge biofilms. Always handle plates gently and standardize wash steps.
- Non-Homogeneous Recovery: Biofilms are difficult to disaggregate. Ensure a robust recovery protocol is followed, including sonication and vortexing of pegs or well contents to create a uniform cell suspension for plating or staining [93].
- Dye-Based Assay Limitations:
- Crystal Violet stains total biomass (live and dead cells and the extracellular matrix) and cannot confirm viability [92].
- Resazurin measures metabolic activity, which can be affected by the bacterial growth phase and environmental conditions. Dormant or persister cells in the biofilm core may show low metabolic activity even if they are viable [90].
- Solution: Where possible, use CFU enumeration as the gold standard for MBEC determination, as viability stains like resazurin have a detection limit that may not accurately reflect complete eradication [90]. Use staining methods as a complementary, high-throughput tool.
FAQ 3: How do I decide whether my experiment measures an MBIC or an MBEC effect?
The key differentiator is the state of the biofilm at the time of antimicrobial exposure [89]:
- You are measuring MBIC if the antimicrobial agent is present during the process of biofilm formation. The effect is the inhibition of biofilm development.
- You are measuring MBEC if the antimicrobial agent is added to a pre-formed, mature biofilm. The effect is the eradication of an established biofilm.
To correctly interpret the effect size (e.g., 3 log reduction vs. 3 log inhibition), you must quantify the biofilm viable cell count before antimicrobial treatment and compare it to the post-treatment count and the endpoint control, as detailed in Table 1 [89].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials and their functions for standardized biofilm susceptibility testing.
| Item | Function/Benefit | Example Use Case |
|---|---|---|
| Peg-Lid Assay System (e.g., MBEC Assay Kit) | Allows high-throughput formation of multiple, uniform biofilms on pegs; lids can be transferred for treatment and staining [93] [92]. | Core device for MBIC/MBEC protocols. |
| Hydroxyapatite-Coated Pegs | Simulates biotic surfaces like bone and tooth enamel; enhances biofilm formation for difficult strains [93]. | Growing biofilms of dental pathogens (e.g., S. mutans) or weak biofilm formers. |
| Crystal Violet Staining Solution | Stains total adhered biomass (polysaccharides, proteins, DNA); inexpensive and simple for quantifying biofilm formation or inhibition [90] [92]. | Initial screening for biofilm-forming capacity or anti-biofilm adhesion agents. |
| Resazurin Viability Dye | Measures metabolic activity of live cells within a biofilm; used for MBIC determination and cell viability assessment [94] [90]. | Determining the MBIC of an antimicrobial compound. |
| Ultrasonic Cleaner with Tray | Essential for efficient and standardized disaggregation of biofilm cells from pegs for viable counting [93]. | Recovery of biofilm cells for CFU enumeration in MBEC assays. |
Table 3: Key research reagent solutions for biofilm susceptibility testing.
Experimental Workflow and Decision Pathway
The following diagram outlines the key steps and decision points in a standardized biofilm susceptibility assay.
Diagram 1: Standardized workflow for biofilm susceptibility testing (MBIC/MBEC), highlighting critical steps like pre-treatment quantification and appropriate endpoint analysis selection.
Comparative Analysis of Conventional Antibiotics vs. Novel Anti-Biofilm Agents
Biofilm-associated infections represent a significant clinical challenge, accounting for 65-80% of all human microbial infections [75] [1]. These structured communities of microorganisms, encased in a self-produced extracellular polymeric substance (EPS), exhibit dramatically increased tolerance to antimicrobial treatments—often between 10 to 1,000-fold higher than their planktonic counterparts [6] [14]. This review establishes a technical support framework for researchers investigating biofilm disruption strategies, with a comparative focus on the limitations of conventional antibiotics and the mechanisms of emerging anti-biofilm agents.
The persistent nature of biofilms stems from multiple factors: the EPS matrix acts as a physical barrier to antibiotic penetration, metabolic heterogeneity within biofilms creates protected niches, and the presence of dormant "persister" cells allows for regrowth after treatment cessation [95] [14]. Understanding these mechanisms is crucial for developing effective strategies against chronic infections associated with medical devices, compromised wounds, and cystic fibrosis lungs [1] [14].
Technical FAQs: Core Concepts in Biofilm Management
Q1: Why do conventional antibiotics often fail against biofilm-associated infections? Conventional antibiotics primarily target actively growing cells and face multiple barriers in biofilm environments. The EPS matrix limits antibiotic penetration through electrostatic interactions and enzyme-mediated inactivation [6] [17]. Within biofilms, metabolic gradients create heterogeneous microenvironments where oxygen and nutrient depletion reduce bacterial metabolic activity, diminishing the efficacy of time-dependent antibiotics [95]. Additionally, biofilms harbor persister cells—dormant subpopulations that survive antibiotic exposure and can repopulate the biofilm once treatment ceases [1].
Q2: What are the key mechanistic differences between conventional antibiotics and novel anti-biofilm agents? Conventional antibiotics typically target essential bacterial processes like cell wall synthesis, protein synthesis, or DNA replication. In contrast, novel anti-biofilm agents employ alternative strategies including EPS matrix disruption, quorum sensing interference, and biofilm dispersal induction without directly killing bacteria [1] [17]. The following table summarizes these distinctions:
Table 1: Comparative Mechanisms of Conventional Antibiotics vs. Novel Anti-Biofilm Agents
| Agent Category | Primary Target | Mode of Action | Effect on Biofilms |
|---|---|---|---|
| Conventional Antibiotics | Cellular processes (e.g., cell wall synthesis, protein synthesis) | Bactericidal or bacteriostatic activity against actively growing cells | Limited penetration; effective primarily against surface-layer cells; often fail to eradicate entire biofilm |
| Novel Anti-Biofilm Agents | EPS components, signaling pathways, or biofilm structure | Matrix degradation, quorum sensing inhibition, or dispersal induction | Disrupts biofilm integrity, increases antibiotic penetration, and reduces virulence without direct killing |
Q3: What quantitative metrics should researchers use to evaluate anti-biofilm efficacy? Beyond minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC), researchers should employ biofilm-specific metrics including Minimum Biofilm Inhibitory Concentration (MBIC), which measures the lowest concentration that prevents biofilm formation, and biofilm eradication concentration (BEC), which determines the concentration required to eliminate pre-formed biofilms [96] [6]. Additional quantitative assessments include measuring EPS component reduction, quantifying metabolic activity within biofilms via ATP assays, and evaluating synergistic effects with conventional antibiotics using checkerboard titration assays and fractional inhibitory concentration (FIC) indices [96].
Troubleshooting Guide: Experimental Challenges in Biofilm Research
Challenge: Inconsistent MBIC Results Across Replicates
Potential Causes and Solutions:
- Biofilm maturation variability: Standardize incubation times and growth conditions. Most biofilms require 24-72 hours for full maturation [6].
- Nutrient medium composition: Use consistent, well-defined media formulations as subtle variations can significantly impact EPS production [95].
- Inoculum preparation method: Implement standardized protocols for transitioning planktonic cultures to biofilm models to ensure consistent starting populations [43].
Challenge: Poor Antibiotic Penetration in Biofilm Models
Potential Causes and Solutions:
- Insufficient agent contact time: Extend treatment duration as penetration through EPS is diffusion-limited [95].
- High EPS density: Incorporate EPS-disrupting enzymes (e.g., DNase, dispersin B, proteases) as adjuvants to enhance penetration [1].
- Agent molecular properties: Consider molecular weight and charge of antimicrobials; smaller, positively charged molecules often penetrate better [14].
Challenge: Difficulty Distinguishing Between Biofilm Inhibition and Dispersal
Experimental Clarification:
- Timing of intervention: Anti-biofilm agents added during initial attachment phase indicate inhibition activity, while agents added to mature biofilms (24-72 hours) test dispersal capability [1].
- Assessment methods: Use microscopy (e.g., SEM, CLSM) to visualize architectural changes and crystal violet staining to quantify biomass reduction [6].
- Viability testing: Combine metabolic assays (e.g., XTT, resazurin) with colony-forming unit (CFU) counts to distinguish between bactericidal effects and physical dispersal [96].
Research Reagent Solutions: Essential Materials for Anti-Biofilm Studies
Table 2: Key Research Reagents for Anti-Biofilm Investigations
| Reagent Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| EPS-Targeting Enzymes | DNase I, Dispersin B, Alginate lyase, Proteases | Disruption of mature biofilms; enhancement of antibiotic penetration | Targets structural components of EPS (eDNA, polysaccharides, proteins) [1] |
| Quorum Sensing Inhibitors | Cinnamoyl hydroxamates, Raspberry ketone, Ibuprofen | Inhibition of virulence factor production and biofilm maturation | Interferes with bacterial cell-to-cell communication systems [96] [75] |
| Natural Anti-Biofilm Compounds | Eugenol, Octyl gallate, Crocetin, β-caryophyllene | Prevention of biofilm formation; synergy with conventional antibiotics | Multiple targets including membrane permeability, EPS production, and cellular adhesion [96] [75] [17] |
| Nanoparticle Systems | Biogenic zinc nanoparticles (ZnNPs), β-caryophyllene-coated gold nanoparticles (β-c-AuNPs) | Enhanced drug delivery; combined physical and chemical disruption | Provides high surface area for interaction with biofilm components; can be functionalized with multiple agents [75] |
| Potentiator Compounds | Octyl gallate, Efflux pump inhibitors | Enhancement of conventional antibiotic efficacy against biofilms | Increases cell membrane permeability; blocks antibiotic extrusion mechanisms [96] [95] |
Quantitative Comparison: Efficacy Metrics for Anti-Biofilm Agents
Table 3: Quantitative Efficacy Data for Selected Anti-Biofilm Agents
| Agent | Target Organism | Anti-Biofilm Activity | Synergy with Antibiotics | Key Findings |
|---|---|---|---|---|
| Octyl gallate (OG) | Staphylococcus epidermidis | Reduced biofilm formation via microcolony inhibition | 8-fold reduction in penicillin MIC; 4-fold reduction in bacitracin MIC [96] | Increased bacterial cell wall permeability; specific to cell wall-targeting antibiotics |
| Raspberry Ketone (RK) | Salmonella enterica Typhimurium | Inhibited biofilm formation at 200 µg/mL without planktonic growth effect [96] | Not specifically reported | Disrupted rdar morphotype; reduced cellulose levels and motility; downregulated csgD and csgB genes |
| β-caryophyllene gold nanoparticles (β-c-AuNPs) | S. aureus and C. albicans (mixed biofilms) | MIC of 512 µg/mL; concentration-dependent inhibition of initial biofilm formation [96] | Enhanced activity compared to β-caryophyllene alone | Effective against both single-species and mixed-species biofilms; reduced CFU in mature biofilms |
| Eugenol-based polymeric materials | Various pathogens | Effective biofilm prevention and disruption on stainless steel | Reduced cytotoxicity while maintaining antimicrobial efficacy [96] | Improved stability and prolonged antimicrobial action compared to free eugenol |
| Lactic Acid (LA) | Campylobacter spp. | MBIC of 1024-2048 µg/mL for monocultures; 4096 µg/mL for mixed biofilms [96] | Naturally occurring in fermented foods | Mixed biofilms exhibited heightened tolerance, emphasizing protective effect of microbial interactions |
Experimental Protocols: Standardized Methodologies for Anti-Biofilm Research
Checkerboard Titration Assay for Synergy Screening
Purpose: To evaluate synergistic effects between conventional antibiotics and novel anti-biofilm agents [96].
Procedure:
- Prepare serial dilutions of the antibiotic in sterile tubes across horizontal rows of a 96-well microtiter plate.
- Prepare serial dilutions of the anti-biofilm agent down vertical columns of the same plate.
- Inoculate each well with standardized bacterial suspension (approximately 5 × 10^5 CFU/mL).
- Include growth control (inoculum without antimicrobials), sterility control (media only), and individual agent controls.
- Incubate at appropriate conditions (typically 37°C for 16-20 hours).
- Measure optical density at 600 nm to determine growth inhibition.
- Calculate Fractional Inhibitory Concentration (FIC) index using the formula: FIC index = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone)
- Interpret results: FIC index ≤0.5 indicates synergy; >0.5-4 indicates additive or indifferent effects; >4 indicates antagonism [96].
Microtiter Plate Biofilm Formation Assay
Purpose: To quantitatively assess biofilm formation and anti-biofilm activity [6].
Procedure:
- Grow overnight cultures of test organisms in appropriate broth medium.
- Dilute cultures to approximately 1 × 10^6 CFU/mL in fresh medium.
- Aliquot 200 µL diluted cultures into 96-well flat-bottom polystyrene microtiter plates.
- Include negative control wells with sterile medium only.
- Incubate under static conditions at appropriate temperature for biofilm formation (typically 37°C for 24-48 hours).
- Carefully remove planktonic cells by inverting and tapping the plate.
- Wash adhered biofilms twice with phosphate-buffered saline (PBS).
- Fix biofilms with 200 µL of 99% methanol for 15 minutes.
- Remove methanol and air dry plates.
- Stain biofilms with 200 µL of 0.1% crystal violet solution for 5-15 minutes.
- Wash plates thoroughly under running tap water to remove excess stain.
- Elute bound crystal violet with 200 µL of 33% glacial acetic acid or 95% ethanol.
- Measure optical density at 570-595 nm.
- Compare OD values to controls to quantify biofilm formation inhibition.
Microscopic Analysis of Biofilm Architecture
Purpose: To visualize structural changes in biofilms following treatment with anti-biofilm agents.
Procedure (SEM Sample Preparation):
- Grow biofilms on appropriate substrates (e.g., glass coverslips, medical device materials).
- Treat with test compounds at predetermined concentrations for specified durations.
- Wash gently with buffer to remove non-adherent cells.
- Fix with 2.5% glutaraldehyde in 0.1 M cacodylate buffer for 2-4 hours at 4°C.
- Wash with cacodylate buffer (3 × 10 minutes).
- Dehydrate through ethanol series (30%, 50%, 70%, 80%, 90%, 100%; 10-15 minutes each).
- Critical point dry or air dry samples.
- Sputter coat with gold/palladium.
- Examine under scanning electron microscope at appropriate accelerating voltages [96].
Mechanism Visualization: Biofilm Resistance and Anti-Biofilm Strategies
Diagram 1: Biofilm Resistance Mechanisms and Anti-Biofilm Strategies. This figure illustrates how biofilms resist conventional antibiotics through physical barriers, metabolic heterogeneity, and persister cells (red arrows), and how novel anti-biofilm strategies target these specific mechanisms (blue arrows).
The comparative analysis reveals that conventional antibiotics and novel anti-biofilm agents operate through distinct yet complementary mechanisms. While antibiotics directly target bacterial viability, anti-biofilm agents disrupt the structural and functional integrity of biofilms, potentially restoring antibiotic susceptibility. Future research directions should focus on optimizing combination therapies, developing standardized efficacy metrics specific to biofilms, and advancing delivery systems that effectively penetrate the EPS matrix. The continued development of this technical support framework will provide researchers with standardized methodologies and troubleshooting resources to accelerate the translation of novel anti-biofilm strategies from laboratory models to clinical applications.
Frequently Asked Questions (FAQs)
Q1: Why do conventional in vitro biofilm models often fail to predict therapeutic efficacy in complex infections?
Conventional in vitro models, such as multiwell plates or flow cells grown on plastic or glass surfaces, poorly mimic the critical chemical gradients (e.g., oxygen, nutrients, ions) and host tissue interactions present in actual infections [97]. The transcriptomic profiles of bacteria grown in synthetic media can differ significantly from those in clinical samples [97]. For instance, Pseudomonas aeruginosa biofilms in artificial sputum show overproduction of alginate compared to biofilms in real cystic fibrosis sputum, leading to an inaccurate representation of biofilm architecture and subsequent therapeutic resistance [97]. Therefore, a drug effective in a simple static biofilm model may fail against a biofilm established in a more realistic, complex environment.
Q2: What are the key advantages of using ex vivo tissue models for biofilm studies?
Ex vivo models utilize actual animal or human tissues (e.g., lung slices, dentin slabs), preserving the original tissue topography and inorganic components [97]. This provides a more clinically relevant interface for biofilm formation. For example, dentin slabs used to study Enterococcus faecalis root canal infections mimic the natural mineralized surface that can be degraded by microbial fermentation products, creating local ion gradients that influence bacterial physiology and antibiotic tolerance [97]. These models act as a crucial bridge between simplistic in vitro systems and costly in vivo animal studies.
Q3: How can inducing biofilm dispersion be a double-edged sword in therapeutic strategy?
Inducing biofilm dispersion can be a strategy to revert resilient, sessile bacteria to a more vulnerable planktonic state [98]. However, it must be carefully controlled. Active dispersion, often triggered by a decrease in intracellular c-di-GMP levels, can lead to the production of matrix-degrading enzymes, breaking down the biofilm and releasing cells [98]. A significant risk is that this controlled release could potentially lead to the dissemination of infection and new colonization sites if not coupled with immediate and effective antimicrobial treatment to kill the dispersed cells [98].
Q4: What are the primary mechanisms behind biofilm-associated antibiotic resistance?
Biofilm resistance is multifactorial, not stemming from a single mechanism but from a combination of factors [6] [19]:
- Physical Barrier: The extracellular polymeric substance (EPS) matrix can restrict the penetration of antimicrobial agents, though it does not always act as a complete physical barrier. In some cases, antibiotics penetrate but are inactivated by binding to matrix components like eDNA or proteins [6] [19].
- Metabolic Heterogeneity: Nutrient and oxygen gradients within the biofilm create zones of slow or non-growing bacteria. Since many antibiotics target active cellular processes, these dormant cells exhibit heightened tolerance [6] [1].
- Persister Cells: A subpopulation of bacteria enters a dormant, metabolically inactive state that is highly tolerant to antibiotics and can repopulate the biofilm after treatment ceases [1].
- Altered Microenvironment: The local biofilm environment, such as low pH, can further reduce antibiotic efficacy [19].
Troubleshooting Common Experimental Challenges
Problem: High Variability in Biofilm Biomass Across Replicates in a Static Microtiter Plate Assay.
- Potential Cause 1: Inconsistent inoculation, such as variations in bacterial cell concentration or inadequate mixing of the bacterial suspension before aliquoting into wells.
- Solution: Standardize the inoculum preparation. Always use bacteria from the same growth phase (e.g., mid-logarithmic) and measure the optical density precisely. Vortex the bacterial culture thoroughly before pipetting into the assay plate.
- Potential Cause 2: Edge effects in the microtiter plate, where wells on the perimeter evaporate faster than central wells, altering medium concentration and growth conditions.
- Solution: Use plates with low evaporation lids and fill all perimeter wells with sterile water or PBS to create a humidified chamber. Alternatively, only use the inner wells for experimental samples.
- Potential Cause 3: Irregular washing steps that dislodge biofilm unevenly.
- Solution: Establish a strict and consistent washing protocol. Use a multichannel pipette to ensure equal volume and pressure is applied to each well, and always aspirate from the same side or corner of the well.
Problem: Failure to Eradicate Mature Biofilm with a Known Antibiotic in a Flow Cell Model.
- Potential Cause 1: The antibiotic concentration is insufficient to penetrate and act on the deeply embedded, slow-growing cells within the biofilm.
- Solution: Consider using the antibiotic in combination with a biofilm-dispersing agent. For example, co-administration with Dispersin B (a glycoside hydrolase that degrades PNAG) or DNase I (which breaks down eDNA) can disrupt the matrix structure, enhancing antibiotic penetration [1]. Always check the compatibility of the enzyme with your flow system (e.g., buffer conditions).
- Potential Cause 2: The flow rate is too high, preventing adequate contact time between the antibiotic and the biofilm.
- Solution: Optimize the therapeutic protocol by incorporating a "static treatment" phase where the flow is temporarily stopped during antibiotic administration, allowing for longer diffusion and contact time before resuming flow to wash away the agent.
Table 1: Comparison of Preclinical Models for Biofilm Infection Research
| Model Type | Key Characteristics | Advantages | Limitations | Common Read-Outs |
|---|---|---|---|---|
| In Vitro (Static) [97] [42] | Biofilms grown in multiwell plates or on coupons/slides under non-flow conditions. | High-throughput, cost-effective, simple setup, excellent for initial screening. | Poor mimicry of host gradients; homogeneous, compact biofilm structure. | Crystal Violet staining (biomass), CFU counts, ATP assays. |
| In Vitro (Dynamic) [97] | Biofilms grown under constant flow of fresh media (e.g., flow cells, bioreactors). | Mimics shear stress; removes waste products; creates nutrient/oxygen gradients; allows for real-time imaging. | More complex setup; higher reagent consumption; not a true host environment. | Confocal Microscopy (structure, viability), CFU, RNA/DNA sequencing. |
| Ex Vivo [97] | Biofilms grown on explained tissues (e.g., dentin slabs, lung tissue). | Preserves natural tissue topography and composition; clinically relevant interfaces. | Tissue viability is limited (days); requires specialized tissue handling skills. | CFU, Microscopy (SEM/CLSM), qPCR for virulence genes. |
| Organ-on-a-Chip [97] | Microfluidic devices with human cells mimicking organ-specific structures and functions. | Can incorporate human cells and fluid flow; high human physiological relevance. | Technically complex; expensive; not yet widely standardized for biofilm studies. | TEER, cytokine analysis, microscopy, bacterial load. |
| In Vivo (Animal) [1] [68] | Biofilm infections established in live animals (e.g., rodent catheter, lung, wound models). | Includes full complexity of a living immune system and host-pathogen interactions. | High cost, ethical considerations, interspecies differences from humans. | CFU from explanted tissue/device, histopathology, survival curves. |
Detailed Experimental Protocols
Protocol 1: Establishing an Ex Vivo Dentin Slab Model for Enterococcus faecalis Biofilms [97]
Purpose: To create a clinically relevant model for studying biofilms on a mineralized surface, mimicking root canal infections.
Materials:
- Tooth specimens (e.g., extracted human teeth)
- Low-speed saw with a diamond-coated blade and water cooling system
- Ethylene oxide gas or an autoclave for sterilization
- Enterococcus faecalis culture
- Brain Heart Infusion (BHI) broth
- Sterile phosphate-buffered saline (PBS)
- 12-well or 24-well cell culture plates
Methodology:
- Dentin Slab Preparation: Remove the crown of the selected tooth. Using the low-speed saw under continuous water cooling to prevent heat damage, cut the root perpendicular to its long axis to obtain multiple dentin slabs of uniform thickness (e.g., 1-2 mm).
- Sterilization: Sterilize the dentin slabs by exposure to ethylene oxide gas overnight. Alternatively, autoclaving can be used, but it may alter the dentin structure more significantly.
- Biofilm Inoculation: Place each sterilized dentin slab into a well of a culture plate. Inoculate each slab with a standardized suspension of E. faecalis (e.g., 10^7 CFU/mL) in BHI broth.
- Incubation: Incubate the plates under appropriate conditions (e.g., 37°C, with 5% CO2 if required) for 1-3 days to allow for mature biofilm formation. Refresh the medium every 24 hours.
- Post-Incubation Processing: After incubation, gently wash the slabs with PBS to remove non-adherent planktonic cells. The biofilm-coated slabs can now be used for antimicrobial efficacy tests, microscopic analysis, or CFU enumeration.
Protocol 2: Combination Therapy with a Biofilm-Dispersing Enzyme and Antibiotic [1] [68]
Purpose: To evaluate the synergistic effect of a matrix-degrading enzyme and a conventional antibiotic on pre-established biofilms.
Materials:
- Pre-formed biofilms in a 96-well plate or on relevant substrate
- Glycoside Hydrolase (e.g., Dispersin B) or DNase I
- Selected antibiotic (e.g., Ciprofloxacin)
- Buffer suitable for the enzyme (e.g., PBS with Mg2+ for DNase I)
- Crystal Violet stain or SYTO9/PI live-dead stain
Methodology:
- Biofilm Formation: Grow biofilms to maturity in a 96-well plate as per standard protocols.
- Treatment: Gently wash the mature biofilms with PBS.
- Enzyme Pre-treatment: Add the solution of the biofilm-dispersing enzyme (e.g., Dispersin B at 10-100 µg/mL in the appropriate buffer) to the wells. Incubate for a predetermined time (e.g., 1-2 hours) at the optimal temperature for enzyme activity.
- Antibiotic Challenge: Without removing the enzyme solution, add the antibiotic at the desired concentration (e.g., 4 µg/mL ciprofloxacin [12]). Incubate for a further period (e.g., 6-24 hours).
- Viability Assessment:
- For CFU counts: Scrape and vortex the biofilms from the wells, perform serial dilution, and plate on agar to enumerate viable bacteria.
- For staining: Perform Crystal Violet staining for total biomass quantification or use a live/dead bacterial viability kit (e.g., SYTO9 and Propidium Iodide) for confocal microscopy analysis to visualize live and dead cells within the biofilm structure.
Key Signaling Pathways and Workflows
Diagram Title: Strategies for Inducing Biofilm Dispersion to Enhance Treatment
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Biofilm Disruption Studies
| Reagent / Material | Function / Role in Experimentation | Example Application |
|---|---|---|
| Dispersin B [1] | A glycoside hydrolase that specifically hydrolyzes poly-N-acetylglucosamine (PNAG), a key exopolysaccharide in many bacterial biofilms. | Dispersing biofilms of Staphylococcus aureus, Escherichia coli, and other PNAG-producing species to sensitize them to antibiotics. |
| DNase I [19] [1] | An enzyme that degrades extracellular DNA (eDNA), a critical structural component of the biofilm matrix for many species. | Disrupting the structural integrity of Pseudomonas aeruginosa and other biofilms where eDNA provides scaffold stability. |
| Proteases [1] | Enzymes that break down proteinaceous components within the extracellular polymeric substance (EPS). | Targeting matrix proteins in biofilms where proteins are a major structural element. |
| N-Acetylcysteine (NAC) [68] | A mucolytic agent that breaks disulfide bonds in polysaccharides and other polymers, disrupting the biofilm matrix. | Used in combination with Ciprofloxacin to enhance efficacy against P. aeruginosa biofilms, particularly in cystic fibrosis models. |
| Crystal Violet [42] | A dye that binds to cells and polysaccharides in the biofilm matrix, used for total biomass quantification. | Standard staining protocol for high-throughput assessment of biofilm formation or eradication in microtiter plates. |
| SYTO9 & Propidium Iodide (PI) [12] | Fluorescent nucleic acid stains for differentiating live (SYTO9, green) and dead (PI, red) bacterial cells. | Assessing bacterial viability within a biofilm after antimicrobial treatment using confocal laser scanning microscopy (CLSM). |
| Shockwave Intravascular Lithotripsy (IVL) System [12] | Generates acoustic pressure waves that cause physical damage and cavitation, disrupting the biofilm structure. | A physical method to detach P. aeruginosa biofilms from silicone tubes (simulating catheters) prior to antibiotic application. |
FAQs: Biofilm Fundamentals and Challenges
Q1: What is the clinical significance of biofilms in persistent infections? Biofilms are structured communities of microorganisms encased in a protective extracellular polymeric substance (EPS). This biofilm state makes them up to 1000 times more resistant to antimicrobials and host immune responses compared to their free-floating (planktonic) counterparts. They are a major contributor to the persistence and chronicity of infections, as the EPS matrix acts as a barrier and harbors microbial cells with varied metabolic states, including dormant "persister" cells. It is estimated that biofilms are implicated in 65-80% of all microbial infections in the human body [99] [100] [101].
Q2: What is the prevalence of biofilms in different types of chronic wounds? Biofilms are a dominant feature in hard-to-heal wounds, with prevalence varying by wound etiology. The table below summarizes key prevalence data.
Table 1: Biofilm Prevalence in Chronic Wounds
| Wound Type | Reported Biofilm Prevalence | Key Contextual Information |
|---|---|---|
| Chronic Wounds (Overall) | Up to 60% | Compared to only ~6% in acute wounds [99]. |
| Diabetic Foot Ulcers (DFUs) | Major contributing factor | Biofilms contribute to chronicity and impaired healing [99]. |
| Burn Wounds | More than half | Biofilms are a significant complication [99]. |
| Hard-to-Heal Wounds (General) | 60% to 100% | True prevalence is considered likely to approach 100% in open, non-healing wounds [102]. |
Q3: What are the common clinical signs of a biofilm-infected wound? Clinical signs have been outlined by expert consensus (e.g., the World Biofilm Symposium) and include [99]:
- Delayed healing despite standard care.
- Recurrent or worsening infection.
- Excessive or yellow exudate.
- Low-grade, chronic inflammation, mild swelling, and redness.
- Pale, edematous, and fragile granulation tissue.
- Failure to respond to antibiotic therapy, with worsening after cessation.
Q4: How do biofilms form on medical devices and what are the consequences? Biofilm formation on devices is a multi-stage process: 1) Attachment of planktonic bacteria to the surface; 2) Formation of microcolonies and irreversible attachment; 3) Maturation with robust EPS production, creating a three-dimensional structure; and 4) Dispersion of cells to seed new infection sites [100] [103]. This leads to Device-Associated Infections (e.g., on catheters, implants), which are difficult to eradicate, often leading to device failure, systemic infection (sepsis), prolonged hospital stays, and increased healthcare costs [100] [103].
Troubleshooting Common Experimental & Clinical Problems
Q1: The biofilm biomass in my assay is not consistently reduced after antimicrobial treatment. What could be wrong? This is a common challenge. Consider the following:
- Biofilm Maturity: Newly formed biofilms (within 48 hours) are more susceptible to antimicrobials. Mature biofilms (72+ hours) have a fully developed EPS matrix, conferring significant resistance. Standardize and report the age of your biofilms [99].
- Agent Penetration: The EPS can physically block the diffusion of antimicrobial agents. Consider combining your treatment with EPS-disrupting agents, such as enzymes (DNase, dispersin B) or chelating agents like EDTA [99] [103].
- Dosing and Contact Time: Ensure the concentration and contact time of the antimicrobial are sufficient to penetrate and act on the biofilm. Sub-inhibitory concentrations can even promote further biofilm formation.
Q2: My in vitro biofilm disruption results do not translate to an in vivo wound model. What factors should I investigate? The in vivo environment is vastly more complex. Key factors to account for include:
- The Host Immune Response: Biofilms perpetuate a state of chronic inflammation, altering the wound microenvironment. They drive leukocyte infiltration and increase protease activity, which can degrade growth factors and the extracellular matrix. Your agent must be effective in this inflammatory milieu [99] [101].
- Polymicrobial Nature: Clinical biofilms are often polymicrobial, containing synergistic communities of bacteria and fungi. In vitro tests with single species may not reflect this complexity. Develop a mixed-species biofilm model (e.g., S. mutans, P. aeruginosa, and C. albicans) for more predictive screening [104].
- Biofilm Re-formation: Biofilms can rapidly reform after disruption—within hours in some cases. Your treatment protocol must include a strategy for maintenance suppression, such as sustained-release dressings or repeated application of anti-biofilm agents [99] [102].
Q3: I am testing a new anti-biofilm coating for a medical device, but microbial adhesion still occurs. How can I improve the coating's efficacy? Surface modification strategies must prevent the initial attachment phase. Current advanced approaches include [100] [103]:
- Hydrophilic and Zwitterionic Coatings: These create a surface that binds water molecules tightly, forming a physical and energetic barrier that reduces protein adsorption and bacterial adhesion.
- Slippery Liquid-Infused Porous Surfaces (SLIPS): Inspired by the pitcher plant, these surfaces hold a lubricating liquid layer that makes it extremely difficult for bacteria to attach.
- Antimicrobial-Eluting or Contact-Killing Coatings: Incorporate substances like silver nanoparticles, antimicrobial peptides (AMPs), or copper nanoparticles that actively kill approaching or adherent microorganisms.
Experimental Protocols for Biofilm Research and Validation
Protocol 1: Assessing Anti-biofilm Efficacy of a Novel Compound (e.g., Rutin)
This protocol is adapted from a study investigating the flavonoid rutin against oral biofilms [104].
1. Pathogen Isolation and Identification:
- Isolate clinical pathogens (e.g., from wound or oral samples) using selective media like Blood Agar, MacConkey Agar, or Sabouraud's Dextrose Agar.
- Identify species using an automated system like VITEK2 or standard microbiological techniques. Always include relevant ATCC control strains.
2. Initial Screening of Antimicrobial Activity:
- Use the well diffusion method. Create wells in Mueller-Hinton agar plates inoculated with a lawn of the test pathogen.
- Add the test compound (e.g., rutin dissolved in DMSO) to the well. Include positive (standard antibiotic) and negative (solvent) controls.
- Measure the zone of inhibition (ZOI) after 24 hours of incubation at 37°C.
3. Determining Minimum Inhibitory Concentration (MIC):
- Use the broth microdilution method in a 96-well microtiter plate.
- Prepare serial two-fold dilutions of the test compound in a suitable broth.
- Inoculate each well with a standardized microbial suspension (~1-2 x 10^8 CFU/mL).
- Incubate for 24 hours at 37°C. The MIC is the lowest concentration that prevents visible growth.
4. Antibiofilm Assay (Crystal Violet Staining):
- Grow a biofilm in a 96-well plate for 24-48 hours (for initial adhesion) or 5-7 days (for mature biofilms).
- Treat the pre-formed biofilm with the test compound at desired concentrations (e.g., 1x MIC, 2x MIC) for 24 hours.
- Gently wash the biofilm to remove non-adherent cells.
- Fix the biofilm with methanol and stain with 0.1% crystal violet for 15-20 minutes.
- Wash, solubilize the bound dye with acetic acid or ethanol, and measure the absorbance at 570-600 nm. Calculate the percentage reduction in biofilm biomass compared to an untreated control.
5. Analysis of Biofilm Cell Viability (Live/Dead Staining):
- Grow and treat biofilms on a suitable surface (e.g., glass coverslips in a 24-well plate).
- After treatment, stain using a commercial live/dead viability kit (e.g., SYTO 9 and propidium iodide).
- Visualize using Confocal Laser Scanning Microscopy (CLSM). Green fluorescence indicates live cells with intact membranes; red fluorescence indicates dead cells with compromised membranes. This provides a direct, visual confirmation of bactericidal activity within the biofilm structure [104].
Protocol 2: Clinical Evaluation of a Biofilm Disruption Strategy in Wounds
This protocol is based on a case series combining a biofilm-disrupting agent with Negative Pressure Wound Therapy (NPWT) [105].
Objective: To evaluate the clinical effectiveness of a combination therapy on biofilm reduction and wound healing in hard-to-heal pressure ulcers.
Method:
- Patient Selection: Recruit patients with recalcitrant, hard-to-heal wounds (e.g., Stage 3 or 4 pressure ulcers that have shown no improvement with standard care).
- Baseline Assessment:
- Measure wound dimensions (length, width, depth) to calculate surface area and volume.
- Use bacterial fluorescence imaging (e.g., MolecuLight i:X) to detect and document the location and extent of bacterial burden.
- Test for elevated protease activity in wound fluid if possible.
- Intervention:
- Apply a topical biofilm-disrupting agent (e.g., a surfactant-based gel) to the entire wound bed.
- Apply NPWT according to standard protocols. The negative pressure setting (e.g., -125 mmHg) and type of foam should be consistent.
- Treatment Schedule: Perform dressing changes and reapplication of the anti-biofilm agent three times per week for a defined period (e.g., 4 weeks).
- Outcome Monitoring: At weekly intervals, repeat the baseline assessments (wound measurement, fluorescence imaging, protease test). Document any adverse events.
Key Outcome Measures:
- Reduction in wound surface area and volume.
- Reduction in bacterial fluorescence signal as visualized and quantified by imaging.
- Reduction in protease activity.
- Time to progression towards healing (e.g., granulation tissue formation).
Research Reagent Solutions: Essential Materials for Biofilm Studies
Table 2: Key Reagents and Materials for Biofilm Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Rutin | A flavonoid glycoside with demonstrated antimicrobial and antibiofilm activity. Disrupts cell walls and inhibits quorum sensing [104]. | Investigate natural product-based disruption of mixed-species oral biofilms [104]. |
| Crystal Violet | A dye that binds to biomass; used to quantify total biofilm formation in a high-throughput manner [104]. | Standard microtiter plate assay for screening anti-biofilm compounds. |
| SYTO 9 / Propidium Iodide | Fluorescent stains for cell viability; part of live/dead bacterial viability kits. | Confocal microscopy to visualize live vs. dead cells within a biofilm structure after treatment [104]. |
| Biofilm-Disrupting Agents (e.g., Blast-X) | Topical wound gels designed to break down the biofilm matrix and enhance antimicrobial penetration [105]. | Clinical case studies evaluating combination therapy with NPWT for hard-to-heal wounds [105]. |
| DNase I | Enzyme that degrades extracellular DNA (eDNA), a critical component of the biofilm matrix. | Used in vitro to weaken biofilm structure and study the role of eDNA. |
| Silver Nanoparticles (AgNPs) | Broad-spectrum antimicrobial additive for medical device coatings and wound dressings [103]. | Coating for urinary catheters or orthopedic implants to prevent biofilm-associated infections [103]. |
Signaling Pathways and Experimental Workflows
Biofilm Lifecycle and Pathogenesis
Anti-biofilm Compound Testing Workflow
Safety and Toxicity Profiles of Emerging Anti-Biofilm Therapies
FAQs on Mechanism and Application
FAQ 1: What are the primary safety advantages of anti-biofilm enzymes over conventional antibiotics?
Anti-biofilm enzymes, such as glycoside hydrolases, proteases, and deoxyribonucleases (DNases), offer enhanced safety for several key reasons. They function extracellularly by degrading the biofilm's extracellular polymeric substance (EPS) and do not need to penetrate bacterial cells or interfere with internal biochemical pathways. This extracellular action means there is less selective pressure for the development of traditional antibiotic resistance. Furthermore, their high specificity for biofilm matrix components reduces the risk of collateral damage to the host's beneficial microbiota and human cells [1].
FAQ 2: How do nanoparticle-based delivery systems improve the safety profile of anti-biofilm agents?
Nanocarriers improve safety and efficacy through targeted delivery and controlled release. By encapsulating active agents, they protect the drugs from premature degradation and minimize systemic exposure. Their small size enables penetration into the dense biofilm matrix, allowing therapeutic doses to reach the infection site while reducing the overall drug concentration required. This targeted approach helps to lower off-target toxicity and mitigates potential side effects [106] [107].
FAQ 3: What are the key toxicity concerns with quorum sensing inhibitors (QSIs), and how are they addressed?
The main concern with QSIs is their potential to interfere with human host cell signaling pathways, given that some bacterial signaling molecules have structural analogs in eukaryotic cells. To address this, research focuses on highly specific QSIs that target unique bacterial communication systems without cross-reacting with host processes. Comprehensive cytotoxicity screening using human cell lines and extensive in vivo toxicological studies are essential steps in the development pipeline to ensure specificity and safety [106] [108].
FAQ 4: Why is phage therapy considered a promising safe alternative, and what are its unique toxicity challenges?
Phage therapy is promising due to its high specificity for target bacterial species, which minimizes disruption to the normal microbiome. However, unique challenges include the potential for rapid clearance by the host immune system, which can limit efficacy. More concerning is the risk of immunogenicity, where the phage particles themselves provoke an inflammatory immune response. Furthermore, the genetic flexibility of phages requires rigorous purification and characterization to ensure that therapeutic preparations do not inadvertently transfer virulence or antibiotic resistance genes between bacteria [107] [109].
Troubleshooting Guides for Experimental Research
Challenge 1: Inconsistent Biofilm Dispersal Efficacy with Enzymatic Treatments
- Potential Cause: Inactivation of enzymes by proteases or inhibitory ions in the biofilm environment or test medium.
- Solution:
- Stabilize the Enzyme: Include protease inhibitors in the enzyme preparation buffer if proteolytic degradation is suspected.
- Optimize Conditions: Systematically test different pH buffers and divalent cation chelators (e.g., EDTA) to find the optimal activity window for your specific enzyme.
- Confirm Activity: Use a fluorogenic or colorimetric substrate assay to verify the enzyme remains active in your experimental setup prior to biofilm treatment [1].
Challenge 2: High Cytotoxicity Observed in In Vitro Models with Novel Anti-Biofilm Peptides
- Potential Cause: The cationic and amphipathic nature of many anti-biofilm peptides, which disrupt bacterial membranes, can also lead to non-specific lysis of mammalian cells.
- Solution:
- Structural Optimization: Explore peptide analogs with reduced helicity, lower net positive charge, or incorporation of D-amino acids to enhance stability and selectivity.
- Dosage and Timing: Perform a detailed time-kill assay and cytotoxicity assay to establish a therapeutic window where biofilm eradication occurs before significant host cell damage.
- Delivery Systems: Incorporate peptides into nanoparticle carriers or hydrogels for localized, sustained release, which can lower the effective concentration and reduce systemic toxicity [106] [6].
Challenge 3: Poor Penetration of Anti-Biofilm Agents into Mature Biofilms
- Potential Cause: The dense, negatively charged EPS matrix acts as a diffusion barrier and can sequester positively charged molecules.
- Solution:
- Use Penetration Enhancers: Combine your primary agent with EPS-degrading enzymes (e.g., DNase I, dispersin B) to disrupt the matrix architecture and facilitate deeper penetration.
- Employ Nanotechnology: Utilize enzyme-functionalized nanocarriers or nanoparticles that are specifically designed to be small and surface-modified to evade matrix trapping [107] [1].
- Model the Process: Use confocal microscopy with fluorescently tagged agents to visually confirm and quantify penetration depth in real-time [67].
Quantitative Safety and Efficacy Data
Table 1: Comparative Safety and Efficacy Profiles of Select Anti-Biofilm Therapies
| Therapy Class | Example Agents | Primary Mechanism | Reported Efficacy (Biofilm Reduction) | Key Toxicity Findings (In Vitro/In Vivo) |
|---|---|---|---|---|
| Enzymes | Dispersin B, DNase I, Proteases | Degradation of exopolysaccharides, eDNA, or matrix proteins | 60-90% dispersal of pre-formed biofilms [1] | Low cytotoxicity to mammalian cells; potential immunogenicity with repeated dosing [1] |
| Quorum Sensing Inhibitors (QSIs) | Natural and synthetic small molecules | Interference with bacterial communication and virulence gene expression | 50-80% inhibition of biofilm formation [106] [108] | Variable; some show no toxicity in zebrafish models, others may inhibit host cell pathways [106] [6] |
| Anti-biofilm Peptides | Cationic antimicrobial peptides (AMPs) | Membrane disruption and inhibition of biofilm attachment | 70-95% eradication of mature biofilms [106] [6] | Hemolytic activity and cytotoxicity to host cells at higher concentrations; therapeutic window is key [6] |
| Nanoparticles | Metal nanoparticles (Ag, ZnO), Liposomes | Reactive oxygen species (ROS) generation, targeted drug delivery, membrane perturbation | 80-99% reduction in bacterial viability within biofilms [107] [109] | Size, shape, and coating-dependent; can cause oxidative stress and inflammation in host tissues [107] |
| Bacteriophages | CRISPR-Cas modified phages | Specific bacterial lysis and degradation of bacterial DNA | Effective against antibiotic-tolerant persister cells [107] | Can trigger inflammatory immune responses; risk of horizontal gene transfer requires purification [107] [109] |
Experimental Protocols for Safety Assessment
Protocol 1: Standardized Cytotoxicity Assay for Anti-Biofilm Agents
Objective: To evaluate the in vitro cytotoxicity of a novel anti-biofilm compound on mammalian cell lines.
- Cell Culture: Seed a 96-well plate with an appropriate mammalian cell line (e.g., HEK293, HaCaT, or primary fibroblasts) at a density of 1x10^4 cells per well. Culture in complete medium until ~80% confluent.
- Agent Exposure: Prepare serial dilutions of the anti-biofilm agent in cell culture medium. Remove growth medium from the cells and add the agent-containing medium. Include wells with medium only (blank) and untreated cells (negative control). A well-known cytotoxic agent (e.g., Triton X-100) should be used as a positive control.
- Incubation: Incubate the plate for 24 hours at 37°C and 5% CO₂.
- Viability Assessment: Perform an MTT or XTT assay. Add the reagent to each well and incubate for 2-4 hours. Metabolically active cells will reduce the tetrazolium salt to a colored formazan product.
- Quantification: Measure the absorbance of the formazan product at 570 nm using a microplate reader. Calculate the percentage of cell viability relative to the untreated control cells. The IC₅₀ (concentration that inhibits 50% of cell viability) can be determined from the dose-response curve [6].
Protocol 2: In Vivo Toxicity Screening in a Murine Model
Objective: To assess acute systemic toxicity of a lead anti-biofilm compound.
- Animal Groups: House female BALB/c mice (6-8 weeks old) under standard conditions. Divide into groups (n=5-6): vehicle control and multiple dose groups of the test compound.
- Dosing: Administer a single intraperitoneal or intravenous injection of the test compound at escalating doses. The vehicle control group receives the buffer/solvent alone.
- Monitoring: Monitor animals closely for 14 days for signs of acute toxicity, including changes in body weight, food and water intake, locomotor activity, and any signs of distress (e.g., piloerection, lethargy).
- Termination and Analysis: On day 14, euthanize the animals and collect blood for hematological and clinical biochemistry analysis (e.g., liver enzymes ALT/AST, creatinine). Harvest major organs (liver, kidney, spleen, heart, lung) for gross necropsy and histopathological examination to identify any tissue damage or lesions [109].
Research Reagent Solutions
Table 2: Essential Reagents for Anti-Biofilm and Toxicity Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Crystal Violet | Stains total biofilm biomass (cells and matrix) | Quantitative assessment of biofilm formation and eradication in microtiter plate assays [107] [67] |
| Calgary Biofilm Device | Generates uniform, high-density biofilms for susceptibility testing | Producing standardized biofilms for MBIC (Minimum Biofilm Inhibitory Concentration) determination [67] |
| Flow Cell System | Grows biofilms under dynamic, nutrient-rich conditions | Real-time, high-resolution imaging of biofilm structure and disruption using confocal microscopy [67] |
| MTT/XTT Assay Kits | Measure metabolic activity as a proxy for cell viability | Standardized in vitro cytotoxicity testing for mammalian cells [6] |
| Fluorescent Probes (e.g., SYTO9, PI) | Differentiate between live and dead cells | Assessing bactericidal activity and membrane integrity within biofilms and on host cells [67] |
| DNase I | Degrades extracellular DNA (eDNA) in the biofilm matrix | Used as a positive control for biofilm dispersal studies and to enhance penetration of other agents [1] |
| Specific Substrate Kits | Quantify enzyme activity (e.g., for proteases, glycosidases) | Confirming the activity and stability of enzymatic anti-biofilm agents during experiments [1] |
Visualized Workflows and Pathways
Integrated Workflow for Anti-Biofilm Therapy Safety Assessment
QSI Mechanism Blocking Biofilm Formation
Conclusion
The fight against biofilm-associated persistent infections requires a paradigm shift from conventional antimicrobial approaches to innovative, multi-targeted strategies. Key takeaways include the critical need to understand biofilm-specific resistance mechanisms, the promising potential of enzymatic disruption and nanotechnology-enhanced delivery, the importance of addressing translational challenges for clinical success, and the value of rigorous comparative validation. Future directions should prioritize interdisciplinary collaboration, development of standardized biofilm detection and assessment methods, optimization of combination therapies that target multiple biofilm components simultaneously, and clinical trials that evaluate these novel approaches under conditions mimicking human infections. Success in this field promises to significantly reduce the global burden of chronic infections, transform treatment outcomes for countless patients, and fundamentally advance our approach to antimicrobial resistance.
References
- 1. Strategy to combat biofilms: a focus on biofilm dispersal ... [https://www.nature.com/articles/s41522-023-00427-y]
- 2. The biofilm life cycle– expanding the conceptual model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9841534/]
- 3. Translational challenges and opportunities in biofilm science [https://www.nature.com/articles/s41522-022-00327-7]
- 4. Microscopy Methods for Biofilm Imaging: Focus on SEM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7828176/]
- 5. A novel dual-staining method for cost-effective visualization ... [https://www.nature.com/articles/s41598-024-80644-3]
- 6. Strategies for combating bacterial biofilms: A focus on anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5955472/]
- 7. Biofilm Dispersal | Bonnie L. Bassler - Princeton University [https://basslerlab.scholar.princeton.edu/biofilm-dispersal]
- 8. A guide to publishing in Biofilm: how to avoid a desk rejection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206335/]
- 9. - Wikipedia Extracellular polymeric substance [https://en.wikipedia.org/wiki/Extracellular_polymeric_substance]
- 10. Innovative Strategies Toward the Disassembly of the EPS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7264105/]
- 11. , a key element in understanding... Extracellular polymeric substances [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604936/]
- 12. Investigation of shockwave treatment for disruption ... [https://www.nature.com/articles/s41598-025-19955-y]
- 13. Biofilm Formation in Chronic Infections - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11527504/]
- 14. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 15. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 16. Combating Bacterial Biofilms: Current and Emerging ... [https://www.mdpi.com/2079-6382/12/6/1005]
- 17. Natural Anti-biofilm Agents: Strategies to Control ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.566325/full]
- 18. Biofilm Resilience: Molecular Mechanisms Driving Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852148/]
- 19. Therapeutic Strategies against Biofilm Infections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9866932/]
- 20. Combatting biofilm-mediated infections in clinical settings ... [https://www.sciencedirect.com/science/article/pii/S246823302400015X]
- 21. Biofilm battleground: Unveiling the hidden challenges, ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401024006223]
- 22. Editorial: Controlling biofilm-related infections in healthcare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423059/]
- 23. Impact of Biofilms on Chronic Infections and Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10693677/]
- 24. Ways to control harmful biofilms: Prevention, inhibition, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7954276/]
- 25. Biofilm tolerance, resistance and infections increasing ... [http://microbialcell.com/researcharticles/2023a-yang-microbial-cell/]
- 26. Biofilms by bacterial human pathogens: Clinical relevance [https://pmc.ncbi.nlm.nih.gov/articles/PMC7841849/]
- 27. A Review of Biofilm Formation of Staphylococcus aureus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9854888/]
- 28. Epidemic Trends and Biofilm Formation Mechanisms of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10440118/]
- 29. Prevention and treatment of Staphylococcus aureus biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC5142822/]
- 30. Pseudomonas aeruginosa Biofilms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7698413/]
- 31. Treatment of Pseudomonas aeruginosa infectious biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459144/]
- 32. From in vitro to in vivo Models of Bacterial Biofilm-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4235718/]
- 33. Eradicating Biofilms: Decoding Persistent Mechanisms and ... [https://pubmed.ncbi.nlm.nih.gov/41178163/]
- 34. Differential Efficacy of Glycoside Hydrolases to Disperse ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.00379/full]
- 35. a focus on biofilm dispersal enzymes - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10485009/]
- 36. dispersion of Enzymatic : An emerging biocatalytic avenue to... biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9478923/]
- 37. Biofilms: Understanding Their Health Impact [https://www.dominickhussey.ca/biofilms/]
- 38. Glycoside Hydrolases Degrade Polymicrobial Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5278739/]
- 39. Quorum Sensing Inhibitors: An Alternative Strategy to Win ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11313800/]
- 40. Natural product-based inhibitors of quorum sensing: A novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242448/]
- 41. Strategies for Interfering With Bacterial Early Stage Biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC8217469/]
- 42. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://www.mdpi.com/2079-6382/14/9/865]
- 43. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 44. Persistent Threats: A Comprehensive Review of Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388178/]
- 45. Action of Antimicrobial Peptides against Bacterial Biofilms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6317029/]
- 46. Synthetic antimicrobial peptides: Characteristics, design ... [https://www.sciencedirect.com/science/article/pii/S0024320521006330]
- 47. Antimicrobial Peptides: A Potent Alternative to Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466391/]
- 48. Antimicrobial peptides as potential anti-biofilm agents ... [https://www.sciencedirect.com/science/article/pii/S1684118217300804]
- 49. A How-To Guide for Mode of Action Analysis of Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7604286/]
- 50. Disruption of drug-resistant biofilms using de novo ... [https://www.sciencedirect.com/science/article/pii/S1742706117302581]
- 51. An Emerging Alternative for Treating Drug-Resistant Bacteria [https://pmc.ncbi.nlm.nih.gov/articles/PMC9765339/]
- 52. Antimicrobial Peptides as an Alternative for the Eradication of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8950055/]
- 53. Nanoparticles Targeting Biofilms: A New Era in Combating ... [https://www.sciencedirect.com/science/article/pii/S2590097825000370]
- 54. Emerging strategies for the prevention of bacterial biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11157393/]
- 55. Nanotechnology-Based Drug Delivery Systems to Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10674810/]
- 56. How Nanoparticles Help in Combating Chronic Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11575445/]
- 57. Phage therapy: An alternative to antibiotics in the age of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5547374/]
- 58. Bacteriophage-mediated approaches for biofilm control [https://pmc.ncbi.nlm.nih.gov/articles/PMC11491440/]
- 59. Bacteriophage-Mediated Control of Biofilm - Frontiers [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.825828/full]
- 60. Bacteriophages and their use in combating antimicrobial ... [https://www.who.int/europe/news-room/fact-sheets/item/bacteriophages-and-their-use-in-combating-antimicrobial-resistance]
- 61. Enhancing the therapeutic use of biofilm-dispersing ... [https://www.sciencedirect.com/science/article/pii/S0169409X21003094]
- 62. 综述:噬菌体疗法治疗难治性肺部感染的创新方法 [https://www.ebiotrade.com/newsf/2025-10/20251026002731115.htm]
- 63. Enhancing the therapeutic use of biofilm-dispersing enzymes ... [https://pubmed.ncbi.nlm.nih.gov/34371086/]
- 64. 慢性创面细菌生物膜形成机制及其诊断的研究进展 [https://pmc.ncbi.nlm.nih.gov/articles/PMC11917344/]
- 65. Combination Therapies for Biofilm Inhibition and Eradication [https://pmc.ncbi.nlm.nih.gov/articles/PMC8915430/]
- 66. New transformative tactics to tackle the bacterial biofilm ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401025000026]
- 67. How to study biofilms: technological advancements in ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1335389/full]
- 68. Combination drug strategies for biofilm eradication using ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1155699/full]
- 69. Computational and Experimental Investigation of Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6946800/]
- 70. Polymicrobial Biofilms: Interkingdom Interactions, Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373980/]
- 71. Preparing a Dual-Species In Vitro Biofilm Model for Testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587443/]
- 72. Biofilm Disruptors 101: The Key To Gut Healing? [https://drwillcole.com/biofilm-disruptors-key-to-gut-healing/]
- 73. Breaking the barrier: disruption of bacterial biofilms using ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1670237/full]
- 74. Comparison of anti-biofilm and cytotoxic activity of Ag/AgO, ... [https://www.nature.com/articles/s41598-025-11756-7]
- 75. Editorial: Fighting microbial biofilms: novel therapeutics ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1680391/full]
- 76. Drug delivery approaches for enhanced antibiofilm therapy [https://www.sciencedirect.com/science/article/abs/pii/S0168365922008161]
- 77. Engineered Bdellovibrio bacteriovorus enhances antibiotic ... [https://pubmed.ncbi.nlm.nih.gov/39894266/]
- 78. Combination drug strategies for biofilm eradication using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10149696/]
- 79. Mechanisms of biofilm resistance to antimicrobial agents [https://pubmed.ncbi.nlm.nih.gov/11166241/]
- 80. Biofilm and Antimicrobial Resistance: Mechanisms, ... [https://www.mdpi.com/2036-7481/16/8/183]
- 81. Biofilm Analysis: Tools and Techniques [https://www.news-medical.net/life-sciences/Biofilm-Analysis-Tools-and-Techniques.aspx]
- 82. Development of an in vitro Assay, Based on the BioFilm Ring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5030256/]
- 83. Biofilm detection in the food industry: Challenges ... [https://www.sciencedirect.com/science/article/pii/S0168160525000364]
- 84. Challenges in identifying biofilm eps markers and ... [https://pubmed.ncbi.nlm.nih.gov/39923351/]
- 85. Biofilm Alliance Forum 2025 [https://www.biofilm-alliance.org/blog/biofilm-alliance-forum-2025]
- 86. Biofilm Treatment Market Trends, Share & Forecast, 2025- ... [https://www.coherentmarketinsights.com/industry-reports/biofilm-treatment-market]
- 87. Biofilms and multidrug resistance: an emerging crisis and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237878/]
- 88. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://pubmed.ncbi.nlm.nih.gov/41009844/]
- 89. MBEC Versus MBIC: the Lack of Differentiation between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6743098/]
- 90. Defining conditions for biofilm inhibition and eradication ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-018-1321-6]
- 91. Strategies for combating antibiotic resistance in bacterial ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1352273/full]
- 92. Critical Assessment of Methods to Quantify Biofilm Growth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6022921/]
- 93. MBEC Assay® Kits Product FAQ [https://innovotech.ca/biofilm-products/mbec-faq/]
- 94. Biofilm Viability Assay Kit [https://www.dojindo.com/products/B603/]
- 95. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 96. The Battle Against Biofilms: A Focus on Novel Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852117/]
- 97. Targeting Persistent Biofilm Infections: Reconsidering the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9231179/]
- 98. Biofilm dispersion: The key to biofilm eradication or ... [https://www.sciencedirect.com/science/article/pii/S2590207520300095]
- 99. Biofilms and Chronic Wounds: Pathogenesis and Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610832/]
- 100. Medical Device-Associated Infections Caused by Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274200/]
- 101. Biofilms and Wounds: An Overview of the Evidence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4486148/]
- 102. Advancing Wound Hygiene as a standard protocol for hard ... [https://woundsinternational.com/supplements/advancing-wound-hygiene-as-a-standard-protocol-for-hard-to-heal-wounds-in-apac-and-turkey-findings-from-an-international-meeting/]
- 103. Battling Biofilms Formation with Medical Device Coatings [https://hydromer.com/battling-biofilms-formation-medical-device-coatings/]
- 104. Effective treatment of oral microbial infections and biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11982453/]
- 105. Evaluation of the combination of a biofilm-disrupting agent ... [https://moleculight.com/publications/evaluation-of-the-combination-of-a-biofilm-disrupting-agent-and-negative-pressure-wound-therapy-a-case-series-2/]
- 106. Pharmacological strategies for targeting biofilms in... [https://www.spandidos-publications.com/10.3892/br.2025.1973?text=fulltext]
- 107. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466655/]
- 108. Biofilm, resistance, and quorum sensing: The triple threat in ... [https://www.sciencedirect.com/science/article/pii/S2950194625003462]
- 109. Molecular Mechanisms Driving Antibiotic Resistance in ... [https://pubmed.ncbi.nlm.nih.gov/40001933/]