Confronting the Crisis: Decoding Antimicrobial Resistance Mechanisms in Gram-Negative Bacteria
This article provides a comprehensive analysis of the sophisticated mechanisms underpinning antimicrobial resistance (AMR) in Gram-negative bacteria, a critical global health threat.
Confronting the Crisis: Decoding Antimicrobial Resistance Mechanisms in Gram-Negative Bacteria
Abstract
This article provides a comprehensive analysis of the sophisticated mechanisms underpinning antimicrobial resistance (AMR) in Gram-negative bacteria, a critical global health threat. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational science, current methodological approaches for detection and treatment, strategies to overcome resistance, and comparative validation of novel therapeutics. Covering the unique tri-layered cell envelope, enzymatic inactivation, efflux pumps, and target modifications, the review also explores the dwindling antibiotic pipeline and innovative solutions like beta-lactamase inhibitors, novel antibiotic classes, and alternative therapies. The content is framed within the context of the WHO's Bacterial Priority Pathogen List and the latest 2024-2025 surveillance data, offering a roadmap for future research and clinical intervention.
The Gram-Negative Fortress: Structural and Genetic Foundations of Resistance
The escalating crisis of antimicrobial resistance (AMR) represents one of the most urgent global healthcare and economic threats, with Gram-negative bacterial pathogens at its epicenter [1]. The remarkable resilience of these organisms stems primarily from their complex cell envelope, a formidable macromolecular structure that effectively excludes diverse classes of therapeutic agents [1] [2]. In 2017, the World Health Organization classified several Gram-negative species as priority pathogens, emphasizing the critical need for novel therapeutic strategies to overcome this protective barrier [1]. The Gram-negative cell envelope is not merely a passive shield but a dynamically interactive compartment that employs multiple, overlapping resistance mechanisms. These include enzymatic antibiotic inactivation, restricted uptake through outer membrane remodelling, efflux pump-mediated antibiotic extrusion, and target site modification [1]. This whitepaper deconstructs the structural and functional complexity of the Gram-negative cell envelope, frames its role in antimicrobial resistance, and provides researchers with advanced methodological approaches for investigating this formidable barrier and developing countermeasures to overcome it.
Structural and Functional Organization of the Gram-Negative Cell Envelope
The Gram-negative cell envelope is a remarkable, multi-layered structure strong enough to withstand approximately 3 atmospheres of turgor pressure, tough enough to endure extreme temperatures and pH, and elastic enough to expand several times its normal surface area [3]. This composite architecture comprises three distinct yet interconnected components: the outer membrane (OM), the peptidoglycan cell wall, and the inner membrane (IM), which together create a sophisticated permeability barrier [1] [2].
The Asymmetric Outer Membrane
The outer membrane represents the defining feature of Gram-negative bacteria and the primary interface with the host environment [1] [2]. Its most distinctive characteristic is its asymmetric lipid distribution. The inner leaflet consists of phospholipids, while the outer leaflet is composed primarily of lipopolysaccharide (LPS) [2]. This asymmetry is fundamental to the membrane's barrier function. LPS is a glycolipid molecule consisting of three domains: lipid A (the hydrophobic anchor), a core oligosaccharide, and the O-antigen polysaccharide chain [2]. The LPS molecules pack tightly together, especially when stabilized by divalent cations like Mg²⁺ that neutralize the negative charges of phosphate groups, creating a highly ordered, non-fluid continuum that is exceptionally impermeable to hydrophobic molecules [2].
The outer membrane is studded with proteins that can be broadly categorized into lipoproteins and β-barrel outer membrane proteins (OMPs) [1] [2]. Lipoproteins are anchored to the inner leaflet via their lipid moieties and play essential roles in cell virulence, peptidoglycan remodelling, cell division, and OM biogenesis [1]. The β-barrel OMPs are transmembrane proteins whose β-sheets wrap into cylindrical pores. They include:
- Porins (e.g., OmpF, OmpC): Form water-filled channels allowing passive diffusion of small, hydrophilic molecules (typically <600 Da) [2] [4].
- Substrate-specific channels (e.g., LamB for maltodextrins): Facilitate transport of specific nutrients [2].
- Gated channels (e.g., for vitamin B12 transport): Mediate high-affinity uptake of larger ligands [2].
Table 1: Major Outer Membrane Components and Their Functions in Gram-Negative Bacteria
| Component | Chemical Structure | Primary Function | Role in Barrier Function |
|---|---|---|---|
| Lipopolysaccharide (LPS) | Glycolipid with Lipid A core, polysaccharide chains | Structural integrity; endotoxic activity | Creates highly impermeable outer leaflet to hydrophobic compounds |
| General Porins (OmpF, OmpC) | Trimeric β-barrel proteins | Passive diffusion of small hydrophilic molecules (<600 Da) | Governs influx of nutrients and antibiotics; mutation causes resistance |
| Specific Porins (LamB, PhoE) | Trimeric β-barrel with substrate specificity | Selective uptake of specific molecules (maltodextrins, phosphate) | Nutrient acquisition; can serve as entry points for antimicrobial analogs |
| Braun's Lipoprotein | Lipoprotein covalently linked to peptidoglycan | Anchors outer membrane to peptidoglycan layer | Stabilizes envelope structure; critical for mechanical integrity |
The Periplasm and Peptidoglycan Layer
Sandwiched between the outer and inner membranes lies the periplasm, an aqueous compartment that constitutes an integral part of the Gram-negative cell envelope [3] [5]. This concentrated gel-like matrix contains binding proteins for nutrients, degradative and detoxifying enzymes, and plays a crucial role in bacterial nutrition and stress response [3] [5]. The periplasm can also act as a reservoir for surface-associated components like pilins, S-layer proteins, and virulence factors [3].
Within the periplasmic space resides the peptidoglycan (or murein) layer, a thin, mesh-like scaffold that surrounds the bacterial inner membrane [1] [2]. In Gram-negative bacteria, this layer is substantially thinner than in Gram-positive organisms but remains essential for withstanding osmotic pressure and maintaining cell shape [1]. The peptidoglycan is composed of linear glycan strands of alternating N-acetylglucosamine (GlcNAc) and N-acetylmuramic acid (MurNAc) residues, cross-linked by short peptides to form a covalently closed, net-like structure called the sacculus [1].
The Inner Membrane
The inner membrane is a symmetric phospholipid bilayer that serves as the ultimate permeability barrier between the cytoplasm and the external environment [1]. It contains numerous proteins responsible for critical cellular functions, including lipid and protein biosynthesis, secretion, DNA anchoring, and chromosome separation [1] [6]. Unlike the outer membrane, the inner membrane lacks LPS and is a metabolically active structure involved in energy generation, solute transport, and macromolecular synthesis [1].
Resistance Mechanisms: How the Envelope Thwarts Antibiotic Therapy
The Gram-negative cell envelope contributes to antibiotic resistance through four primary mechanisms that can operate independently or synergistically to create clinically significant resistance phenotypes [1].
Restricted Antibiotic Permeation
The outer membrane serves as a formidable physical barrier that significantly limits antibiotic penetration [7] [4]. The LPS-rich outer leaflet is exceptionally effective at excluding hydrophobic antibiotics, while the size-restrictive porin channels constrain the entry of hydrophilic molecules [2] [4]. Systematic analyses in E. coli have demonstrated that different porins play distinct roles in antibiotic resistance. For instance, OmpF serves as the main penetration route for many antibiotics including β-lactams, while OmpA is primarily associated with maintaining membrane integrity [4]. OmpC appears to contribute to both functions [4]. Porin deficiencies, whether through mutational inactivation or downregulation of expression, are common resistance mechanisms in clinical isolates [7] [4].
Efflux Pump-Mediated Antibiotic Extrusion
Gram-negative bacteria express a plethora of efflux pumps that are capable of transporting structurally diverse molecules, including antibiotics, out of the bacterial cell [8] [7]. These tripartite efflux systems span both the inner and outer membranes, efficiently recognizing and extruding drugs from the periplasm before they reach their intracellular targets [7]. In Enterobacteriaceae, all parallel efflux pathways based on tripartite pumps converge at the outer membrane protein TolC, making it a central conduit for multidrug efflux [7]. Overexpression of these efflux systems can cause clinically relevant levels of antibiotic resistance [8]. Recent large-scale chemical analyses have revealed that alongside collective physicochemical properties, the presence or absence of specific chemical groups in compounds substantially influences their recognition by TolC-dependent efflux systems [7].
Table 2: Major Antibiotic Resistance Mechanisms Associated with the Gram-Negative Cell Envelope
| Resistance Mechanism | Molecular Basis | Antibiotic Classes Affected | Research Assessment Methods |
|---|---|---|---|
| Restricted Permeation | Porin loss/modification; LPS barrier | β-lactams, fluoroquinolones, chloramphenicol | MIC profiling; Porin expression analysis; Liposome swelling assays |
| Efflux Pump Expression | Overexpression of tripartite efflux systems (e.g., AcrAB-TolC) | Multiple classes including tetracyclines, macrolides, β-lactams | Ethidium bromide accumulation assays; RT-qPCR of efflux components; Checkerboard assays with efflux inhibitors |
| Enzyme-Mediated Inactivation | Production of β-lactamases, aminoglycoside-modifying enzymes in periplasm | β-lactams, aminoglycosides | Nitrocefin hydrolysis assays; Enzyme kinetics; Mass spectrometry of modified antibiotics |
| Target Modification | Alteration of PBPs, DNA gyrase, other targets accessed through envelope | β-lactams, fluoroquinolones | Target gene sequencing; Binding affinity measurements; Radioligand displacement assays |
Enzyme-Mediated Inactivation and Target Modification
The periplasmic space houses numerous antibiotic-inactivating enzymes, most notably β-lactamases, which hydrolyze β-lactam antibiotics before they can reach their penicillin-binding protein (PBP) targets [1] [5]. Additionally, bacteria can alter antibiotic target sites through mutations or post-translational modifications, further reducing antibiotic efficacy [1]. These target modifications are particularly effective when combined with reduced permeability and enhanced efflux, creating a multi-layered defense system that is extremely difficult to overcome with conventional antibiotics.
Experimental Approaches for Investigating Envelope-Mediated Resistance
Genetic Manipulation of Envelope Components
The construction of defined mutants provides a powerful approach for systematically analyzing the contribution of individual envelope components to antibiotic resistance. For example, researchers can create:
- Porin deletion mutants: Generate single, double, and triple porin mutants (e.g., ΔompA, ΔompC, ΔompF) to assess their individual and combined contributions to antibiotic susceptibility [4].
- Efflux-deficient strains: Create tolC mutants to disable the major efflux conduit in Enterobacteriaceae, allowing identification of efflux pump substrates [7].
- Membrane-permeable mutants: Utilize lpxC mutants with reduced LPS content to create hyperpermeable outer membranes for studying permeation limitations [7].
Protocol: Construction of Porin Deletion Mutants Using λ Red Recombinase
- Amplify a kanamycin-resistance gene from plasmid pKD13 using primers containing 50-nucleotide extensions homologous to the target porin gene.
- Electroporate the purified PCR product into E. coli MG1655 cells harboring the pKD46 plasmid (expressing λ Red recombinase).
- Select mutants on LB agar plates containing kanamycin (50 μg/mL) at 37°C.
- Eliminate the antibiotic resistance cassette by transforming with pCP20 plasmid expressing FLP recombinase.
- Verify gene deletion by colony PCR and DNA sequencing [4].
Phenotypic Characterization of Envelope Mutants
Comprehensive profiling of envelope mutants reveals the functional contribution of specific components to antibiotic resistance and membrane integrity.
Antibiotic Susceptibility Testing
- Determine Minimal Inhibitory Concentration (MIC) values using the agar dilution method according to CLSI guidelines.
- Spot 10 μL of bacterial suspension (10⁷ cells/mL) onto Müller-Hinton agar plates containing two-fold serial dilutions of antibiotics.
- Incubate at 37°C for 20 hours; define MIC as the lowest antibiotic concentration preventing visible growth [4].
Membrane Integrity Assays
- Spot serial dilutions of stationary-phase cells onto LB plates containing membrane stressors (2% SDS, 6% ethanol, 750 mM NaCl).
- Assess membrane permeability using fluorescent dyes (propidium iodide, SYTOX green) that are excluded by intact membranes but penetrate compromised envelopes.
- Visualize stained cells using fluorescence microscopy to quantify membrane damage [4].
Efflux Pump Activity Assessment
- Measure intracellular accumulation of efflux pump substrates (e.g., ethidium bromide) in wild-type versus efflux-deficient strains using fluorometry.
- Compare compound activity in wild-type versus tolC strains to classify compounds as efflux substrates or efflux evaders [7].
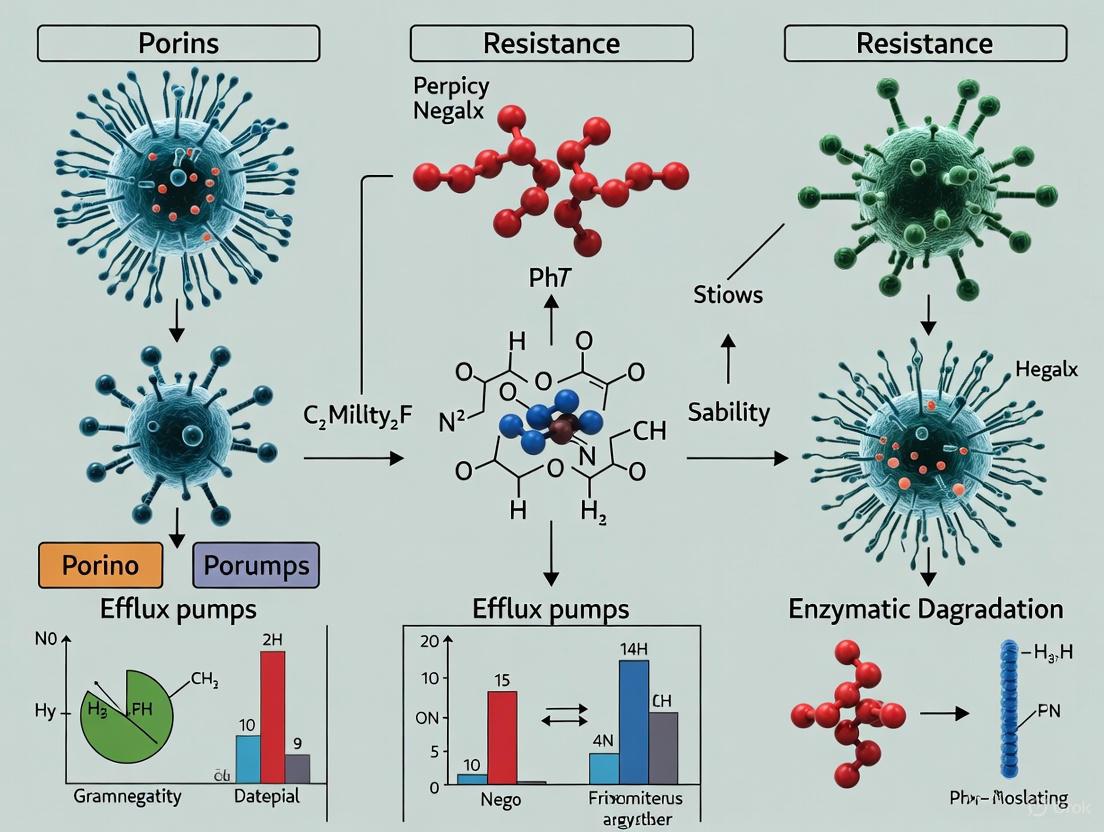
The following diagram illustrates the primary antibiotic resistance mechanisms employed by the Gram-negative cell envelope and their complex interrelationships:
Diagram 1: Multilayered antibiotic resistance mechanisms in Gram-negative bacteria. The diagram illustrates how antibiotics (yellow) must navigate the outer membrane (green), may be inactivated in the periplasm (red), or recognized by efflux pumps (blue) that extrude them from the cell.
Computational and High-Throughput Approaches
Modern resistance research employs large-scale screening and computational methods to identify chemical features associated with envelope penetration and efflux avoidance.
Large-Scale Compound Classification
- Source experimental growth inhibition data from public databases (e.g., CO-ADD) for wild-type, tolC, and lpxC E. coli strains.
- Classify compounds as efflux substrates (active in tolC only) or efflux evaders (active in both WT and tolC) using stringent activity thresholds.
- Apply matched molecular pair analysis to identify structural modifications that convert efflux substrates into evaders [7].
Physicochemical Property Analysis
- Calculate key molecular descriptors (logD, polar surface area, hydrogen bond donors/acceptors) for active and inactive compounds.
- Use machine learning to identify chemical features correlated with improved Gram-negative activity and reduced efflux recognition [7].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for Investigating the Gram-Negative Cell Envelope
| Reagent/Cell Line | Specific Function | Research Application | Key Considerations |
|---|---|---|---|
| E. coli MG1655 (WT) | Model Gram-negative organism | Baseline for phenotypic comparisons; genetic background for mutant construction | Well-characterized K-12 strain; amenable to genetic manipulation |
| E. coli tolC mutant | Deficient in major efflux conduit | Identification of efflux pump substrates; studies of efflux-mediated resistance | Hyper-susceptible to many antibiotics; used in efflux classification assays |
| E. coli lpxC mutant | Reduced LPS in outer membrane | Studies of outer membrane permeability barrier; identification of permeation-limited compounds | Temperature-sensitive; requires specific growth conditions |
| Porin-specific antibodies | Immunodetection of OMP expression | Quantification of porin expression levels in clinical isolates; monitoring porin regulation | Commercial availability varies; requires validation for different bacterial species |
| Fluorescent membrane dyes (SYTOX, PI) | Indicators of membrane integrity | Assessment of envelope damage in mutant strains; evaluation of membrane-targeting compounds | Differential permeability characteristics; compatibility with fluorescence detection |
| β-lactamase substrates (Nitrocefin) | Chromogenic β-lactamase detection | Measurement of β-lactamase activity in periplasmic extracts; enzyme kinetics | Real-time colorimetric change; useful for high-throughput screening |
The Gram-negative cell envelope represents one of nature's most effective protective barriers, enabling bacterial survival in hostile environments, including those containing therapeutic concentrations of antibiotics. Its multi-layered architecture, combining a restrictive outer membrane, enzymatic defenses in the periplasm, and powerful efflux systems, creates a formidable obstacle for antibiotic penetration and retention. Addressing the challenge of Gram-negative resistance requires integrated approaches combining structural biology, genetics, computational modeling, and advanced chemical design. Future research must focus on identifying novel targets within the envelope assembly pathways, developing efflux pump inhibitors for clinical use, and designing next-generation antibiotics that exploit underutilized penetration pathways or are less susceptible to efflux recognition. Only through a fundamental understanding of this impermeable barrier can we hope to develop effective therapeutic strategies against the growing threat of multidrug-resistant Gram-negative pathogens.
Antimicrobial resistance (AMR) in Gram-negative bacteria represents a critical and escalating global health threat, undermining the efficacy of modern medicine and jeopardizing routine medical procedures [9] [10]. The World Health Organization (WHO) has classified several Gram-negative pathogens, including Acinetobacter baumannii, Pseudomonas aeruginosa, and carbapenem-resistant Enterobacteriaceae, as critical priorities for research and development of new therapeutics [9] [11]. The specialized cell envelope of Gram-negative bacteria—comprising an outer membrane (OM) with lipopolysaccharides (LPS), a thin peptidoglycan layer, and an inner membrane (IM)—serves as a formidable permeability barrier and a platform for sophisticated resistance mechanisms [9] [10]. This in-depth technical guide examines the core molecular machinery underpinning the primary defense strategies employed by Gram-negative pathogens: enzymatic inactivation of antibiotics, efflux pump activity, target site modification, and reduced membrane permeability. Understanding these mechanisms at a granular level is essential for researchers and drug development professionals aiming to design novel interventions to combat the silent pandemic of AMR.
Core Resistance Mechanisms: A Molecular Perspective
Enzymatic Inactivation of Antibiotics
Bacteria produce a diverse array of enzymes that inactivate antimicrobial agents through degradation or modification, rendering the drugs ineffective before they reach their cellular targets [12] [11].
β-Lactamases are the most clinically significant group of inactivating enzymes. They hydrolyze the amide bond within the β-lactam ring, a structure central to penicillins, cephalosporins, and carbapenems [12] [11]. The evolution of extended-spectrum β-lactamases (ESBLs), such as TEM and CTX-M, confers resistance to later-generation cephalosporins. Furthermore, carbapenemases (e.g., KPC, NDM, OXA-48) hydrolyze carbapenems, which are often considered last-resort antibiotics [12] [11]. The genes encoding these enzymes are frequently located on plasmids, facilitating their rapid dissemination across bacterial populations through horizontal gene transfer (HGT) [12].
Other enzymatic mechanisms include aminoglycoside-modifying enzymes that catalyze the transfer of functional groups (e.g., acetyl, adenyl, phosphoryl) onto the antibiotic molecule, disrupting its ability to bind to the 16S rRNA of the 30S ribosomal subunit [12].
Table 1: Major Antibiotic-Inactivating Enzymes and Their Targets
| Enzyme Class | Antibiotic Target | Molecular Mechanism | Example Enzymes/Gene |
|---|---|---|---|
| β-Lactamases | β-Lactams (Penicillins, Cephalosporins, Carbapenems) | Hydrolysis of the β-lactam ring [12] [11] | CTX-M (ESBL), KPC, NDM (Carbapenemase) [11] |
| Aminoglycoside Modifying Enzymes | Aminoglycosides (Gentamicin, Amikacin) | Acetylation, adenylation, or phosphorylation of drug molecule [12] | aac, ant, aph [12] |
| Phosphotransferases | Aminoglycosides, Chloramphenicol | Phosphorylation of hydroxyl groups [13] | Not specified in search results |
| Transferases | Polymyxins (Colistin) | Transfer of phosphoethanolamine to lipid A, reducing drug binding [11] | mcr genes [11] |
Efflux Pump Systems
Multidrug efflux pumps are integral membrane proteins that actively export a wide range of structurally diverse antibiotics from the bacterial cell, reducing intracellular concentrations to subtoxic levels [9] [14]. In Gram-negative bacteria, these systems are often tripartite, spanning the entire cell envelope [14].
The Resistance-Nodulation-Division (RND) superfamily includes some of the most clinically relevant efflux systems, such as AcrAB-TolC in E. coli and MexAB-OprM in P. aeruginosa [14]. These complexes consist of an inner membrane transporter (e.g., AcrB), a periplasmic membrane fusion protein (e.g., AcrA), and an outer membrane channel (e.g., TolC) [14]. They utilize the proton motive force to expel antibiotics. Other families include the Major Facilitator Superfamily (MFS) and the ATP-Binding Cassette (ABC) superfamily, the latter of which uses ATP hydrolysis for energy [14].
Emerging research continues to identify novel efflux-associated proteins. For instance, the BON (bacterial OsmY and nodulation) domain-containing protein has been shown to form a trimeric, pore-shaped channel that functions in an "one-in, one-out" manner to transport antibiotics like carbapenems, contributing to intrinsic and acquired resistance [14].
Table 2: Major Efflux Pump Families in Gram-Negative Bacteria
| Efflux Pump Family | Energy Source | Key Examples | Antibiotic Substrates |
|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton Motive Force [14] | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) [14] | β-lactams, fluoroquinolones, tetracyclines, chloramphenicol, macrolides [14] |
| MFS (Major Facilitator Superfamily) | Proton Motive Force [14] | Not specified in search results | Tetracyclines, chloramphenicol [14] |
| ABC (ATP-Binding Cassette) | ATP Hydrolysis [14] [11] | Not specified in search results | Aminoglycosides, polymyxins [11] |
| MATE (Multidrug and Toxic Compound Extrusion) | Proton/Sodium Ion Gradient [14] | Not specified in search results | Fluoroquinolones [14] |
| PACE (Proteobacterial Antimicrobial Compound Efflux) | Proton Motive Force [14] | Not specified in search results | Chlorhexidine, acriflavine [14] |
Target Site Modification
Bacteria can alter the structure of an antibiotic's cellular target, diminishing the drug's binding affinity and rendering it ineffective [12] [13]. This can occur through mutation or enzymatic modification of the target.
A classic example is the modification of Penicillin-Binding Proteins (PBPs). In methicillin-resistant Staphylococcus aureus (MRSA), the acquired mecA gene encodes PBP2a, which has low affinity for β-lactam antibiotics [12]. In Gram-negative bacteria, mutations in DNA gyrase (gyrA) and topoisomerase IV (parC) are common mechanisms of resistance to fluoroquinolones [12] [11]. A single point mutation (e.g., C257T in gyrA) can lead to an amino acid substitution (e.g., S83L) that prevents drug binding [11].
Enzymatic modification is exemplified by methylation of the 16S rRNA molecule, which blocks the binding of aminoglycosides [11]. Similarly, mutations in the 23S rRNA or ribosomal proteins L3 and L4 can lead to resistance against macrolides and oxazolidinones [12].
Reduced Permeability
The Gram-negative outer membrane is a formidable permeability barrier that intrinsically protects against many antibiotics [9] [11]. Resistance is often achieved by a reduction in the influx of antimicrobials.
This is primarily mediated through the downregulation, loss, or mutation of porin proteins [9] [11]. Porins, such as OmpF and OmpC in E. coli, form water-filled channels that allow the passive diffusion of hydrophilic molecules, including many antibiotics like β-lactams and fluoroquinolones [9] [11]. Reduced expression of these porins limits the intracellular accumulation of drugs. For example, carbapenem resistance in A. baumannii is linked to the reduced expression of CarO and Omp porins [11]. Similarly, alterations in the lipopolysaccharide (LPS) structure can reduce the permeability of the outer membrane to large molecules like vancomycin and the polycationic peptide polymyxins [9] [13].
Diagram 1: Four Core AMR Mechanisms in Gram-Negative Bacteria. This diagram illustrates the primary molecular resistance mechanisms operating within the Gram-negative cell envelope, leading to antibiotic treatment failure.
Experimental Protocols for Investigating Resistance Mechanisms
Protocol 1: Frequency of Resistance (FoR) Assay
The FoR assay is a standard method for quantifying the spontaneous development of resistance in a bacterial population upon exposure to an antibiotic [15].
- Culture Preparation: Grow the bacterial strain of interest overnight in a suitable broth (e.g., Mueller-Hinton Broth) under standard conditions.
- Cell Counting: Determine the total viable count (CFU/mL) of the overnight culture by serial dilution and plating.
- Antibiotic Exposure: Plate approximately 10^10 bacterial cells onto agar plates containing the antibiotic at concentrations ranging from the MIC to 4x or 8x the MIC. Also, plate a dilution series onto drug-free agar to determine the exact input CFU.
- Incubation: Incubate the plates for 24-48 hours at the appropriate temperature.
- Calculation: Count the colonies growing on the antibiotic-containing plates. The frequency of resistance is calculated as the number of CFU on the antibiotic plate divided by the total number of CFU plated [15].
- Confirmation: Confirm the resistance level of the resulting mutants by determining their Minimum Inhibitory Concentration (MIC) and comparing it to the wild-type strain (relative MIC) [15].
Protocol 2: Adaptive Laboratory Evolution (ALE)
ALE experiments simulate long-term exposure to antibiotics to study the evolutionary trajectories of resistance development [15].
- Initial Inoculum: Start with a wild-type, susceptible bacterial strain.
- Passaging: Serially passage the bacteria in the presence of sub-inhibitory and gradually increasing concentrations of the antibiotic. This is typically done over a fixed period (e.g., 60 days or ~120 generations) in liquid culture or on solid agar [15].
- Monitoring: Regularly monitor bacterial growth and adjust the antibiotic concentration to maintain selective pressure. Sample the population at predetermined time points.
- Endpoint Analysis: At the end of the experiment, measure the MIC of the evolved population. Isolate individual clones from the endpoint population for whole-genome sequencing (WGS) to identify mutations (e.g., in target genes, efflux pump regulators, porins) that confer resistance [15].
- Validation: Use genetic techniques, such as gene knockout or complementation, to validate the role of identified mutations in the resistant phenotype.
Diagram 2: Adaptive Laboratory Evolution Workflow. This flowchart outlines the process of using serial passaging under antibiotic pressure to evolve and identify resistance mutations.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for AMR Mechanism Research
| Research Tool / Reagent | Function/Application | Specific Example / Context of Use |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CA-MHB) | Standardized medium for antibiotic susceptibility testing (MIC, FoR) [15] | Provides consistent ion concentrations for reliable and reproducible MIC results. |
| Agar Plates with Antibiotic Gradients | For FoR assays and isolating resistant mutants [15] | Used to determine the frequency of spontaneous resistance at specific drug concentrations. |
| PCR & Sanger Sequencing Reagents | To amplify and sequence specific resistance genes (e.g., gyrA, parC, bla genes) [11] | Identifies point mutations (e.g., C257T in gyrA) or the presence of specific β-lactamase genes. |
| Whole-Genome Sequencing (WGS) Kit | For comprehensive analysis of genomic changes in evolved resistant strains [15] | Used in ALE experiments to discover all chromosomal mutations conferring resistance. |
| Plasmid Extraction Kit | To isolate and characterize mobile genetic elements carrying resistance genes [12] | Essential for studying the horizontal transfer of genes like blaKPC or mcr-1. |
| Real-Time PCR (qPCR) Reagents | To quantify the expression levels of efflux pump genes (e.g., acrB, mexB) or porin genes [11] | Detects upregulation of efflux pumps or downregulation of porins in response to antibiotic stress. |
| CRISPR-Cas9 Gene Editing System | For functional validation of resistance mutations via gene knockout or complementation [10] | Used to confirm the causal role of a specific mutation (e.g., in pmrB) in the resistant phenotype. |
The molecular machinery of defense in Gram-negative bacteria is complex, dynamic, and highly effective. The interplay between enzymatic inactivation, efflux, target modification, and reduced permeability creates a multi-layered shield that significantly complicates treatment. The ongoing discovery of novel resistance proteins, such as BON-domain proteins and potent efflux pump variants like RE-CmeABC, underscores the adaptive ingenuity of bacterial pathogens [14]. For the research community, countering this threat requires a deep and nuanced understanding of these mechanisms, facilitated by robust experimental methodologies like FoR assays and ALE, and empowered by modern tools such as WGS and CRISPR-Cas9. The future of anti-infective therapy lies in developing innovative strategies, such as dual-targeting permeabilizers [15], efflux pump inhibitors, and β-lactamase adjuvants, that can outmaneuver these evolutionary defenses and preserve the utility of our antimicrobial armamentarium.
Antimicrobial resistance (AMR) represents a critical global health threat, directly causing an estimated 1.27 million deaths worldwide in 2019 [16]. The rapid evolution and dissemination of resistance among Gram-negative pathogens are largely driven by horizontal gene transfer (HGT), a process that allows for the sharing of genetic material, including antibiotic resistance genes (ARGs), between bacteria. This whitepaper details the mechanisms of genetic mobility, focusing on the roles of plasmids, Integrative and Conjugative Elements (ICEs), and other mobile genetic elements (MGEs) in propagating AMR. Framed within a One Health perspective, which recognizes the interconnectedness of human, animal, and environmental health, this document synthesizes current research to provide drug development professionals and scientists with a technical guide to the pathways, experimental models, and methodologies essential for combating this crisis [16] [17].
Horizontal gene transfer is a more significant driver of bacterial evolution than random mutation, as it facilitates the acquisition of entire genes, enabling the rapid expression of new resistance phenotypes [18]. In the context of AMR, HGT allows susceptible bacteria to acquire ARGs from resistant neighbors, effectively spreading resistance across different species and genera. This transfer occurs with high frequency in complex microbial communities, such as biofilms, and is exacerbated by selective pressures from antibiotic use [19]. The three primary mechanisms of HGT are:
- Conjugation: The direct, cell-to-cell transfer of genetic material via a conjugative pilus, mediated by plasmids and ICEs.
- Transformation: The uptake and incorporation of free environmental DNA by bacterial cells.
- Transduction: The transfer of bacterial DNA from one cell to another via bacteriophages (viruses that infect bacteria).
Among these, conjugation is considered the most significant route for the spread of ARGs [18]. The gut of animals and humans, wastewater treatment plants (WWTPs), and soil are potent reservoirs where this HGT occurs, acting as breeding grounds for the emergence of multidrug-resistant (MDR) pathogens [16] [18] [19].
Key Mobile Genetic Elements and Their Mechanisms
The dissemination of ARGs is facilitated by a suite of MGEs that can move within and between bacterial genomes.
Plasmids
Plasmids are extrachromosomal, self-replicating DNA elements that are cornerstone players in the global spread of AMR.
- Function and Role in AMR: Plasmids often carry accessory genes, including ARGs, that are beneficial to the host bacterium under antibiotic stress. They can transfer these genes across taxonomic boundaries, sometimes over large phylogenetic distances, making them a primary vehicle for ARG dissemination [16].
- Classification and Host Range: Plasmids are broadly categorized based on their ability to self-transfer:
- Conjugative plasmids encode all the necessary machinery (e.g., a Type IV Secretion System, T4SS) for their own transfer via conjugation.
- Mobilizable plasmids possess only an origin-of-transfer (oriT) and can be transferred using the conjugation machinery of a coexisting conjugative plasmid.
- Non-mobilizable plasmids lack the genes for transfer [16]. Some plasmids, known as broad-host-range (BHR) plasmids (e.g., IncP-1), can replicate in a wide variety of bacterial species, dramatically expanding the potential reservoir for ARGs [16].
- Resistance Islands and Mosaic Plasmids: Plasmids are highly dynamic. A recent analysis of 6,784 plasmids from Escherichia, Salmonella, and Klebsiella isolates found that 84% of ARGs in MDR plasmids are clustered in resistance islands [20]. These islands are agglomerations of ARGs and other MGEs, such as insertion sequences (IS) and transposons, which facilitate the copying and shuffling of genes between DNA molecules. This results in the creation of mosaic plasmids—genetic elements composed of parts from distinct sources, which are common in clinical genera like Escherichia and Klebsiella [16] [20].
Integrative and Conjugative Elements (ICEs)
ICEs are mobile genetic elements that reside integrated into the host bacterium's chromosome but can excise themselves, form a circular intermediate, and be transferred via conjugation.
- Function and Role in AMR: Like plasmids, ICEs contain genes required for their own excision, transfer, and integration. They are modular and can acquire new genes, including ARGs, through recombination [18]. Unlike plasmids, ICEs replicate as part of the host chromosome and do not exist as extrachromosomal elements for most of their life cycle.
- Mechanism of Integration and Transfer: Integration into specific target DNA sequences is typically dependent on attachment sites (attP on the ICE and attB on the chromosome) and is mediated by integrases. Upon excision, the ICE transfers to a recipient cell and integrates into its chromosome, often in a site-specific manner, though some ICEs use DDE recombinases for site-independent integration [18].
Integrons
Integrons are genetic assembly platforms that are not mobile themselves but are frequently carried on plasmids and ICEs. They play a central role in the acquisition and expression of ARGs.
- Structure and Function: An integron is defined by the presence of:
- An integrase gene (intI), which catalyzes site-specific recombination.
- A primary recombination site (attI).
- A promoter (Pc) that drives expression of captured genes [17].
- Gene Cassette Capture and Expression: Integrons can capture promoterless gene cassettes, which typically contain a single ARG and an associated recombination site (attC). The integrase enzyme integrates these cassettes at the attI site, allowing them to be expressed from the common Pc promoter. This system functions as a natural cloning and expression system, enabling bacteria to stockpile and express multiple ARGs from a single platform [17]. Class 1 integrons are frequently associated with AMR in human pathogens and are considered a dangerous pool of resistance determinants from a One Health perspective [17].
Table 1: Key Mobile Genetic Elements in AMR Dissemination
| Element | Genetic Nature | Mobility | Primary Role in AMR | Notable Features |
|---|---|---|---|---|
| Plasmid | Extrachromosomal DNA | Conjugative, Mobilizable, or Non-mobilizable | Primary vehicle for intercellular ARG transfer | Broad-host-range variants; carries resistance islands; mosaic structure [16] [20] |
| ICE | Chromosomally integrated | Conjugative (upon excision) | Horizontal transfer of ARGs from the chromosome | Modular structure; site-specific integration; replicates with chromosome [18] |
| Integron | Platform on MGEs | Non-mobile (hitchhikes on plasmids/ICEs) | Acquisition and expression of ARG cassettes | Natural gene capture system; common in clinical isolates (e.g., Class 1) [17] |
The following diagram illustrates the core mechanism of conjugative plasmid transfer, a primary pathway for AMR dissemination.
Quantitative Analysis of ARG Distribution and Mobility
Understanding the prevalence and genetic organization of ARGs is crucial for assessing their dissemination risk. Large-scale genomic analyses reveal clear patterns.
- Dominance of Resistance Islands: As noted, the vast majority (84%) of ARGs in MDR plasmids from key Gram-negative genera are organized in compact resistance islands within collinear syntenic blocks (CSBs). These CSBs have a median length of 8 genes, with 65% comprising 10 or fewer genes, indicating dense clustering of resistance determinants [20].
- Association with Mobile Genetic Elements: The evolution of these resistance islands is driven by specific MGEs. Analysis has identified 76 gene families encoding site-specific recombinases (SSRs) and transposases that co-occur with ARGs within these islands. The most frequent SSR gene families associated with ARG islands include IS26, Tn3 transposase, and class 1 integron integrase, which collectively comprise 66% of the SSR genes found in plasmid-borne resistance islands [20].
- Barriers to Dissemination: The agglomeration of ARGs is biased towards specific plasmid lineages. Resistance islands identified in one plasmid lineage are rarely shared among distantly related plasmids, suggesting barriers to ARG dissemination between plasmid types, potentially related to plasmid genetic properties, host range, and evolutionary history [20].
Table 2: Prevalence of Key Mobile Genetic Elements in Antibiotic Resistance Islands (Based on KES Plasmid Analysis)
| Mobile Genetic Element Type | Specific Gene Family Example | Function | Approximate Contribution to SSR Genes in Resistance Islands |
|---|---|---|---|
| DDE Transposase | IS26, IS6100 | DNA cutting and pasting via DDE enzymatic activity | 66% (collectively for top families) [20] |
| Serine Recombinase | Tn3 Resolvase | Resolution of co-integrate structures during transposition | |
| Tyrosine Recombinase | Class 1 Integron Integrase | Site-specific integration of gene cassettes | |
| HUH Endonuclease | IS91 Transposase | Replication and single-stranded DNA transfer |
Experimental Models and Methodologies for Studying HGT
Research into HGT and AMR dissemination relies on a combination of in silico, in vitro, and in vivo models, each offering unique insights.
In Silico and Genomic Analyses
Computational methods are indispensable for large-scale analysis of MGEs and HGT patterns.
- Methodology: Large datasets of bacterial genomes and plasmids are assembled. Protein-coding genes are clustered into homologous families, and ARGs are identified using specialized databases like the Comprehensive Antibiotic Resistance Database (CARD). Algorithms are then used to identify collinear syntenic blocks (CSBs) of co-occurring ARGs and MGEs to define resistance islands and quantify their distribution across plasmid taxonomic units (PTUs) [20].
In Vitro Models
- Standard Conjugation Assay: This is a fundamental protocol for measuring plasmid transfer frequencies.
- Procedure: Donor and recipient strains are grown separately to mid-log phase, mixed at a specific ratio (e.g., 1:10 donor to recipient), and allowed to conjugate on a filter placed on solid agar or in a liquid medium for a set period. The mixture is then resuspended, diluted, and plated on selective media that counterselects against the donor and the recipient while allowing transconjugants (successful recipient cells that acquired the plasmid) to grow. The transfer frequency is calculated as the number of transconjugants per recipient [18].
- Key Reagents: Selective antibiotics, solid agar media, membrane filters.
- Biofilm Models: As HGT occurs more frequently in biofilms than in planktonic culture, these models are critical.
- Procedure: Biofilms are cultivated in flow cells, on pegs (e.g., Calgary Biofilm Device), or in microtiter plates. Donor and recipient strains are co-cultured to form a biofilm. After incubation, the biofilm is disaggregated, and transconjugants are enumerated by plating on selective media, similar to the standard conjugation assay [19].
- Key Reagents: Flow cells, peg lids, specialized growth media for biofilm formation (e.g., with low nutrient levels).
- Morbidostat-Based Resistomics Workflow: This sophisticated approach studies the evolution of resistance in real-time.
- Procedure: A morbidostat is a computer-controlled continuous culturing device that constantly monitors bacterial growth (via OD600) and dynamically adjusts the concentration of an antimicrobial agent in the media. If bacteria grow faster than the dilution rate, the drug concentration is increased; if growth slows, the drug concentration is decreased. This applies gradual selective pressure, driving the evolution of resistance. Evolved isolates are periodically sequenced to identify resistance-conferring mutations [21].
- Key Reagents: Morbidostat device, antimicrobial agent of interest (e.g., novel drug TGV-49), sequencing reagents.
In Vivo Models
Studying HGT in a live host provides the most clinically relevant context but is also the most complex.
- Animal Models: Common models include mice (Mus musculus), rats (Mus rattus), chickens (Gallus gallus), and insects like fruit flies (Drosophila melanogaster). These models allow researchers to investigate how host factors (immunity, diet, gut microbiota) influence conjugation and the transfer of ARGs in the gut and other body sites [18].
The workflow for a typical morbidostat experiment, used to study resistance evolution, is detailed below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for HGT and AMR Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Selective Media & Antibiotics | Selection and counterselection of donor, recipient, and transconjugant bacteria in conjugation experiments. | Plating bacterial mixtures from a conjugation assay to quantify transconjugants [18]. |
| Morbidostat Device | Continuous culturing with automated feedback to maintain bacterial growth under constant drug pressure, driving experimental evolution. | Studying the development of resistance to a novel antimicrobial agent like TGV-49 in Acinetobacter baumannii [21]. |
| Comprehensive Antibiotic Resistance Database (CARD) | A curated resource of ARGs, their products, and associated phenotypes for in silico identification of resistance determinants. | Annotating ARGs in whole genome sequences of bacterial isolates or plasmids [20]. |
| Microfluidic Chips & Flow Cells | Creating controlled, small-scale environments for studying biofilm development and HGT under fluid shear stress. | Observing real-time conjugation events within a structured multispecies biofilm [19]. |
| Class 1 Integron-Specific Primers/Probes | PCR-based detection and surveillance of a clinically prevalent integron class that is a major reservoir for ARG cassettes. | Screening clinical or environmental isolates for the presence and cassette content of class 1 integrons [17]. |
The battle against antimicrobial resistance necessitates a deep understanding of the genetic mobility facilitated by plasmids, ICEs, and integrons. The quantitative data confirms that ARGs are not randomly distributed but are concentrated in resistance islands within specific plasmid lineages, driven by the activity of MGEs like IS26 and integrons. Combating this threat requires a multi-pronged approach: leveraging advanced experimental models like the morbidostat to predict resistance evolution, employing genomic surveillance to track the spread of high-risk MGEs, and developing novel therapeutic strategies that target the conjugation machinery or the stability of MGEs themselves. Through the collaborative efforts of researchers and drug development professionals, informed by the intricate mechanisms detailed in this whitepaper, we can work towards mitigating the global AMR crisis.
The World Health Organization (WHO) Bacterial Priority Pathogens List (BPPL) for 2024 categorizes antibiotic-resistant bacterial pathogens into critical, high, and medium priority groups to guide research, development, and public health interventions against antimicrobial resistance (AMR) [22]. Among the most critical threats are Gram-negative ESKAPE pathogens—Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacterales (including Klebsiella pneumoniae and Enterobacter spp.)—notorious for their ability to "escape" biocidal action and rapidly develop multidrug resistance [23] [24]. These organisms employ sophisticated resistance mechanisms, including enzymatic antibiotic inactivation, efflux pumps, and target site modifications, leading to persistently high mortality rates in healthcare settings worldwide [25] [23]. Surveillance data from 2023, encompassing over 23 million confirmed infections across 104 countries, underscores the escalating global burden, necessitating enhanced stewardship, innovative therapeutics, and robust surveillance systems [26]. This whitepaper provides a comprehensive technical analysis of these priority pathogens, detailing their global resistance profiles, molecular resistance mechanisms, and standardized experimental methodologies essential for advancing AMR research.
Global Priority Classifications and Resistance Burden
The WHO 2024 BPPL builds upon its 2017 predecessor, refining the prioritization of 24 antibiotic-resistant bacterial pathogens across 15 families to address evolving AMR challenges [22]. This list serves as a critical tool for directing research and development (R&D) efforts and investments, particularly targeting developers of antibacterial medicines, academic institutions, and policymakers [22].
Acinetobacter baumannii, Pseudomonas aeruginosa, and carbapenem-resistant Enterobacterales are ranked as critical priority pathogens due to their extensive multidrug resistance and significant associated mortality [22] [23]. The ESKAPE group collectively represents leading causes of healthcare-associated infections (HAIs), with substantial prevalence in intensive care units (ICUs) and among immunocompromised patients [25] [27].
Table 1: Global Resistance Profiles of WHO-Critical Gram-Negative ESKAPE Pathogens
| Pathogen | Key Resistance Phenotype | Prevalence & Burden | Noteworthy Resistance Patterns |
|---|---|---|---|
| Acinetobacter baumannii | Carbapenem-resistant | 33.9% prevalence in ICU isolates (10-yr study) [27]; 100% MDR rate in SSI isolates [24] | Universal MDR; high resistance to levofloxacin (97.1%), cefepime (94.4%) [23] |
| Pseudomonas aeruginosa | Carbapenem-resistant, MDR | 28.3% prevalence in ICU isolates [27]; lower overall AMR but significant in SSIs [24] | Preserved colistin susceptibility; notable ceftriaxone resistance (75%) [23] |
| Klebsiella pneumoniae | Carbapenem-resistant (CRKP), ESBL-producing | 25.6% prevalence in ICU isolates [25]; 88.2% MDR rate in SSIs [24] | Rising carbapenemase-producers (including dual NDM+OXA-48); ampicillin/ceftazidime resistance >93% [25] [23] |
| Enterobacter spp. | Carbapenem-resistant | 7.4% prevalence in ICU isolates [27]; fully carbapenem-susceptible in some cohorts [25] | Variable resistance profiles; concerning potential for ESBL and carbapenemase production [22] |
The economic and clinical impact of infections caused by these pathogens is profound. Patients with HAIs experience significantly longer hospital stays (averaging 20.3 days versus 8.7 days for non-infected patients) and generate substantially higher healthcare costs [25]. In 2019, AMR was directly responsible for 1.27 million deaths globally and contributed to nearly 5 million more [23].
Molecular Mechanisms of Antimicrobial Resistance
Gram-negative ESKAPE pathogens deploy a complex arsenal of resistance mechanisms, which can be intrinsic (innate to the species), acquired (via mutation or horizontal gene transfer), or adaptive (in response to environmental pressure) [23].
Key Resistance Pathways and Mechanisms
The primary molecular strategies employed by these bacteria include:
- Enzymatic Inactivation of Antibiotics: Production of β-lactamases, including extended-spectrum β-lactamases (ESBLs), AmpC cephalosporinases, and carbapenemases (e.g., KPC, NDM, OXA-48-like), which hydrolyze and inactivate β-lactam antibiotics [23]. The Aztreonam-Avibactam combination, for instance, is designed to overcome this by combining a monocyclic β-lactam (stable against metallo-β-lactamases) with a non-β-lactam β-lactamase inhibitor (avibactam) that inactivates serine-based enzymes [28] [29].
- Reduced Drug Permeability: The asymmetric, double-membrane structure of Gram-negative bacteria, with narrow porin channels, significantly restricts antibiotic penetration into the cell [23].
- Efflux Pump Systems: Overexpression of multi-component efflux pumps (e.g., AcrAB-TolC in Enterobacterales, MexAB-OprM in P. aeruginosa) actively exports a wide range of antibiotics from the cell, contributing to multidrug resistance [23].
- Target Site Modification: Mutations in genes encoding antibiotic target sites, such as penicillin-binding proteins (PBPs), DNA gyrase, or topoisomerase IV, reduce drug binding affinity [23].
These mechanisms are not mutually exclusive; their convergence in a single bacterial cell often results in difficult-to-treat multidrug-resistant (MDR), extensively drug-resistant (XDR), or even pandrug-resistant (PDR) phenotypes [23].
Diagram Title: Core AMR Mechanisms in WHO-Critical Gram-Negative Pathogens
Experimental Evolution of Resistance
Laboratory evolution studies demonstrate that Gram-negative ESKAPE pathogens can develop resistance to both established antibiotics and novel drug candidates within a remarkably short timeframe. Research shows that within 60 days (approximately 120 generations) of controlled antibiotic exposure, bacteria can achieve a median 64-fold increase in minimum inhibitory concentration (MIC) [30].
These studies reveal that resistance mutations selected in the laboratory are frequently already present in natural pathogen populations. This indicates that clinical resistance can emerge rapidly through the selection of pre-existing genetic variants rather than requiring de novo mutation [30]. Furthermore, mobile resistance genes (ARGs) effective against antibiotic candidates are prevalent not only in clinical isolates but also in environmental and human gut microbiomes, facilitating their global dissemination [30].
Surveillance and Antimicrobial Susceptibility Testing (AST)
Continuous, standardized surveillance is the cornerstone for understanding AMR epidemiology, informing empirical therapy, and guiding stewardship interventions [25]. The WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) report for 2025 provides a critical analysis of antibiotic resistance prevalence and trends, drawing from over 23 million bacteriologically confirmed cases from 110 countries [26].
Standardized Methodologies for AST
Table 2: Core Methodologies for Antimicrobial Susceptibility Testing & Surveillance
| Method/Technique | Core Function/Purpose | Key Procedural Steps | Interpretive Standards |
|---|---|---|---|
| Broth Microdilution | Reference quantitative method for determining Minimum Inhibitory Concentration (MIC) [21] | 1. Prepare serial dilutions of antimicrobial in broth. 2. Inoculate with standardized bacterial suspension. 3. Incubate (e.g., 35°C, 16-20 hrs). 4. Determine MIC as lowest concentration inhibiting visible growth [21]. | CLSI M27-A3 / EUCAST guidelines [21]. |
| Disk Diffusion (Kirby-Bauer) | Qualitative/semi-quantitative susceptibility testing [24] | 1. Inoculate Mueller-Hinton agar plate. 2. Apply antibiotic-impregnated disks. 3. Incubate (35°C, 16-18 hrs). 4. Measure zone diameters of inhibition [24]. | CLSI / EUCAST breakpoint tables [24]. |
| Automated Systems (e.g., VITEK 2) | High-throughput, automated AST and bacterial identification [25] | 1. Load standardized bacterial suspension into AST card. 2. Insert into instrument. 3. System monitors growth kinetically via optical changes. 4. Software reports MIC and susceptibility category [25]. | Built-in interpretive algorithms based on CLSI/EUCAST. |
| Phenotypic Confirmatory Tests | Detect specific resistance mechanisms (e.g., ESBL, carbapenemase) [25] | ESBL: Double-disk synergy test (DDST) with clavulanate [25]. Carbapenemase: Modified Carbapenem Inactivation Method (mCIM) or molecular assays [25]. | CLSI-defined criteria for synergy or inhibition. |
| Molecular Detection (PCR, LFA) | Identify specific resistance genes (e.g., blaKPC, blaNDM) [25] | 1. Extract bacterial DNA. 2. Amplify target genes via PCR or isothermal methods. 3. Detect amplicons via electrophoresis or lateral flow immunoassay (LFA) [25]. | Positive/internal control amplification. |
Workflow for Integrated Pathogen Surveillance
The following diagram outlines a comprehensive workflow for processing clinical specimens to characterize WHO-priority pathogens, integrating identification, AST, and resistance mechanism detection.
Diagram Title: Workflow for Laboratory Surveillance of Priority Pathogens
Emerging Therapeutic Strategies and Resistance
The development of novel antimicrobial agents is a critical frontline defense against MDR Gram-negative pathogens. Promising strategies include combination therapies with novel β-lactamase inhibitors and agents with new mechanisms of action, such as membrane-targeting compounds.
Aztreonam-avibactam represents a significant advancement for treating infections caused by metallo-β-lactamase (MBL)-producing Enterobacterales. Aztreonam is stable against MBLs, while avibactam inhibits accompanying serine β-lactamases (e.g., ESBLs, KPC) [28] [29]. Analysis of 70 in vitro studies encompassing 490,231 Enterobacterales isolates found resistance to aztreonam-avibactam to be very rare (0-1.8%) in consecutive (non-selected) clinical isolates [28] [29]. However, higher resistance rates are noted in preselected multidrug-resistant strains and among lactose non-fermenters like Acinetobacter baumannii, underscoring the necessity for ongoing susceptibility testing [28].
Novel compounds like TGV-49, a broad-spectrum antimicrobial derived from Mul-1867, exhibit a unique membrane-disrupting mechanism. Its positively charged hexanediamine groups bind to negatively charged membrane components, while hydrazine groups react with carbonyl groups, collectively causing membrane disruption, content leakage, and cell lysis [21]. Experimental evolution of A. baumannii against TGV-49 using a morbidostat device revealed minimal development of resistance, suggesting its potential as a therapeutic alternative [21].
Despite these innovations, a systematic evaluation of 13 antibiotics introduced post-2017 or in development revealed that they are, on average, equally prone to de novo resistance evolution as traditional antibiotics in laboratory settings [30]. This highlights the relentless capacity of bacterial evolution and the need for strategies that proactively anticipate and counter resistance.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for AMR Studies
| Reagent / Material | Core Function in Research | Specific Application Examples |
|---|---|---|
| Mueller-Hinton Broth/Agar | Standardized medium for antimicrobial susceptibility testing (AST). | Determining MIC by broth microdilution; conducting disk diffusion assays [21] [24]. |
| CLSI / EUCAST Panels | Reference antibiotic powders and predefined panels for AST. | Generating standardized MIC data against a range of antibiotics [21]. |
| VITEK 2 AST Cards | Automated, cartridge-based panels for high-throughput AST. | Rapid phenotypic profiling of clinical isolates (e.g., AST-N331 for Gram-negatives) [25]. |
| MALDI-TOF MS Reagents | Matrix and calibration standards for mass spectrometry. | Rapid, accurate identification of bacterial pathogens from culture [25]. |
| PCR Master Mixes & Primers | Reagents for amplification of DNA. | Detecting specific resistance genes (e.g., blaKPC, blaNDM, mecA) [25]. |
| Morbidostat Device | Computer-controlled continuous culturing bioreactor for experimental evolution. | Studying resistance development under controlled, escalating antibiotic pressure [21] [30]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Broth for AST, adjusted for divalent cations to standardize results. | Reference method AST, particularly for cationic antibiotics like colistin [25]. |
| Quality Control Strains | Reference strains (e.g., P. aeruginosa ATCC 27853, E. coli ATCC 25922). | Ensuring accuracy and precision of AST methods and reagent performance [25]. |
From Bench to Bedside: Detection, Surveillance, and Current Treatment Paradigms
The escalating crisis of antimicrobial resistance (AMR), particularly in Gram-negative bacteria, represents one of the most serious global health threats of our time [1]. Gram-negative pathogens, with their complex cell envelope structure and sophisticated resistance mechanisms, have become increasingly resistant to nearly all available antibiotic classes, culminating in rising mortality rates worldwide [31]. In 2017, the World Health Organization (WHO) published a list of priority pathogens, predominantly Gram-negative species, categorized by the urgency of need for new treatments [1]. Despite this warning, the progress in generating new therapeutic options has proven insufficient, with AMR continuing to escalate as a "global ticking time bomb" [1].
The development of innovative antibacterial agents is hampered by both scientific and economic challenges. The unique structure of the Gram-negative cell envelope, comprising an outer membrane with lipopolysaccharides, a thin peptidoglycan layer, and an inner membrane, creates a formidable permeability barrier that naturally limits drug access [1] [31]. Furthermore, bacteria employ four primary resistance mechanisms: drug inactivation through enzymes like β-lactamases; reduced drug uptake via porin remodeling; enhanced efflux pump activity; and alteration of antibiotic target sites [1] [32]. Meanwhile, the antibacterial development pipeline faces a dual crisis of scarcity and lack of innovation, with many large pharmaceutical companies having de-invested in antibiotic research due to limited economic returns [33] [34].
This whitepaper provides a comprehensive analysis of the current clinical pipeline for antibacterial agents, encompassing both traditional and non-traditional approaches, with a specific focus on combating resistant Gram-negative pathogens. We examine quantitative data on agents in development, detail emerging therapeutic modalities, and present standardized methodological frameworks for their evaluation, providing researchers and drug development professionals with a strategic overview of this critical landscape.
Analysis of the Current Clinical Development Pipeline
The Shrinking Traditional Antibiotic Pipeline
According to the latest WHO analysis from 2025, the clinical pipeline for antibacterial agents is contracting and lacks sufficient innovation to address the most dangerous drug-resistant bacteria [33]. The number of antibacterials in clinical development has decreased from 97 in 2023 to 90 in 2025 [33] [35]. Among these 90 agents, only 50 are traditional antibacterial agents, while 40 employ non-traditional approaches such as bacteriophages, antibodies, and microbiome-modulating agents [33]. This decline occurs despite the growing threat of AMR, which was associated with over 6 million deaths in 2019 alone [36].
Most concerning is the limited activity against critical priority pathogens. Of the 90 agents in development, only 15 are considered truly innovative, and for 10 of these, available data are insufficient to confirm the absence of cross-resistance [33]. Merely 5 of the agents in development demonstrate effectiveness against at least one of the WHO "critical" priority pathogens - the highest risk category that includes carbapenem-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacteriaceae [33]. The preclinical pipeline remains more active, with 232 programs across 148 groups worldwide, though 90% of these companies are small firms with fewer than 50 employees, highlighting the fragility of the research and development ecosystem [33].
Table 1: Analysis of the Clinical Antibacterial Pipeline (2025 WHO Data)
| Pipeline Category | Number of Agents | Key Characteristics | Activity Against WHO Critical Pathogens |
|---|---|---|---|
| Total Clinical Pipeline | 90 | Decreased from 97 in 2023 | Limited |
| Traditional Agents | 50 | Small-molecule drugs | 45 target priority pathogens (18 focused on drug-resistant M. tuberculosis) |
| Non-Traditional Agents | 40 | Bacteriophages, antibodies, microbiome modulators | Varies by approach |
| Innovative Agents | 15 | Novel mechanisms/chemical classes | Only 5 effective against ≥1 critical pathogen |
| Preclinical Programs | 232 | Across 148 groups | Heavy focus on Gram-negative pathogens |
Categorization of Therapeutic Development Approaches
Antibacterial agents in development can be classified according to their structural characteristics and therapeutic goals, though the distinction between "traditional" and "non-traditional" has limited regulatory relevance [34]. A more instructive framework categorizes both traditional and non-traditional products into four development archetypes known as the STAR categories [34]:
- Standalone: Products effective as monotherapy, including most traditional small molecules and some direct-acting bactericidal products with non-traditional structures.
- Transform: Products that extend the activity range of an existing drug to enable action against previously insusceptible microorganisms.
- Augment: Products that improve the activity of an otherwise effective antibiotic, such as those reducing bacterial virulence or neutralizing toxins.
- Restore: Products that reinstate the efficacy of existing drugs that have lost effectiveness due to resistance development (e.g., β-lactamase inhibitors).
This categorization helps identify appropriate regulatory pathways and clinical trial designs for different therapeutic approaches, with non-inferiority trials generally appropriate for Standalone, Transform, and Restore categories, while superiority designs may be needed for Augment products [34].
Emerging Non-Traditional Antibacterial Approaches
Bacteriophage Therapy
Bacteriophage (phage) therapy represents one of the most clinically advanced non-traditional approaches, with a wealth of evidence from compassionate use cases against multidrug-resistant Gram-negative infections [36]. Phages are viruses that specifically infect and lyse bacteria through a precise mechanism: tail fibers recognize and adsorb to host cell receptors, followed by genome ejection into the cytoplasm. The phage then utilizes host machinery to replicate, ultimately inducing cell lysis through endolysins that degrade peptidoglycan [36].
Two predominant development models exist for phage therapy. The first involves on-demand phage cocktails formulated based on susceptibility testing of the patient's specific isolate against phage banks [36]. The Magistral Phage system in Belgium exemplifies a successful regulatory model for this personalized approach. The second model employs fixed-composition phage products designed to treat specific pathogens or conditions, which offers a clearer regulatory pathway but cannot adapt to emerging strains [36]. Currently, the FDA has not approved any phage product for clinical use, though over a dozen commercial phage products against Gram-negative bacteria are in phase I-III trials targeting various infections including lung infections, urinary tract infections, and chronic wounds [36].
Clinical evidence primarily stems from compassionate use cases where all antibiotic options have been exhausted. Phage therapy has demonstrated efficacy against a wide variety of Gram-negative infections including those caused by E. coli, K. pneumoniae, and A. baumannii, with the majority of case studies targeting P. aeruginosa [36]. Administration routes are tailored to infection sites—intravenous for systemic infections, inhalation for respiratory infections, and topical for wound infections. A recent retrospective study of 100 consecutive phage therapy cases revealed clinical improvement and bacterial eradication in 77.2% and 61.3% of infections, respectively, highlighting the importance of concurrent antibiotics for optimal outcomes [36].
Table 2: Emerging Non-Traditional Antibacterial Approaches Against Gram-Negative Pathogens
| Therapeutic Approach | Mechanism of Action | Development Stage | Key Examples/Targets |
|---|---|---|---|
| Bacteriophage Therapy | Lytic phage replication and bacterial lysis | Compassionate use; Phase I-III trials | OMKO1 phage targeting P. aeruginosa porin M |
| Anti-Virulence Agents | Target virulence factors without killing | Preclinical; early clinical | Quorum sensing inhibitors; toxin neutralization |
| Monoclonal Antibodies | Neutralize specific bacterial toxins | Approved for specific toxins | Raxibacumab (anthrax toxin); bezlotoxumab (C. difficile toxin) |
| Microbiome-Modifying Therapies | Restore protective commensal microbiota | Phase I-III trials | Fecal microbiota transplantation; defined consortia |
| Antimicrobial Peptides | Membrane disruption; immunomodulation | Preclinical; early clinical | Naturally derived peptides; synthetic analogs |
| Nanomaterial-Based Therapies | Physical membrane disruption; targeted delivery | Preclinical | Metal nanoparticles; functionalized liposomes |
Other Promising Non-Traditional Modalities
Beyond phage therapy, several other non-traditional approaches show promise for combating resistant Gram-negative infections:
Anti-virulence therapies aim to disarm pathogens rather than kill them, potentially reducing selective pressure for resistance [37]. These agents target bacterial virulence mechanisms including toxin production, secretion systems, adhesion factors, and quorum-sensing communication systems [37]. For instance, quorum sensing inhibitors disrupt the chemical signaling pathways that coordinate bacterial pathogenicity and biofilm formation [32].
Immunotherapy approaches leverage or enhance the host immune response against bacterial pathogens [36]. This includes monoclonal antibodies targeting specific bacterial surface antigens or toxins, such as raxibacumab for anthrax toxin and bezlotoxumab for Clostridium difficile toxin [34]. These approaches offer high specificity and can neutralize the most damaging aspects of bacterial infections.
Microbiome-modifying therapies seek to restore protective commensal communities to prevent colonization by resistant pathogens [36] [34]. Fecal microbial transplantation has proven highly effective against recurrent C. difficile infections, and research is ongoing to develop defined consortia of beneficial bacteria for other clinical applications [36].
Antimicrobial peptides (AMPs) and nanomaterial-based therapies represent additional innovative approaches [32] [36]. AMPs are naturally occurring or synthetic peptides that can disrupt bacterial membranes or modulate immune responses, while engineered nanoparticles can physically damage bacterial membranes or serve as targeted delivery vehicles for conventional antibiotics [32].
Resistance Mechanisms in Gram-Negative Bacteria and Therapeutic Implications
The effectiveness of both traditional and non-traditional antibacterial agents is fundamentally challenged by the sophisticated resistance mechanisms of Gram-negative bacteria. These mechanisms can be categorized into four primary groups that impact drug efficacy through different pathways [1] [31].
Enzymatic inactivation represents a foremost resistance mechanism, particularly β-lactamases that hydrolyze the β-lactam ring of penicillins, cephalosporins, and carbapenems [1] [32]. The evolution of extended-spectrum β-lactamases (ESBLs) and carbapenemases (such as KPC, NDM, and OXA-48) has severely limited treatment options for common Gram-negative pathogens [31] [32]. Newer β-lactam-β-lactamase inhibitor combinations aim to counter this mechanism, but emerging resistance to these combinations underscores the continuous evolutionary battle [38].
Reduced drug uptake occurs through modifications to the Gram-negative outer membrane, particularly changes in porin proteins that serve as entry channels for hydrophilic antibiotics [1] [32]. Mutations in non-specific porins like OmpF can confer resistance to multiple antibiotic classes, including β-lactams and fluoroquinolones [32]. Additionally, structural modifications to lipopolysaccharides can reduce membrane permeability to hydrophobic compounds [31].
Efflux pump systems actively export antibiotics from the bacterial cell, maintaining subtherapeutic intracellular concentrations [1] [32]. Resistance-nodulation-division (RND) superfamily pumps are particularly effective in Gram-negative bacteria and can recognize a wide range of structurally unrelated antimicrobials, contributing to multidrug resistance phenotypes [32]. These pumps often work synergistically with reduced influx mechanisms to confer high-level resistance.
Target site modifications protect essential bacterial structures from antibiotic binding without affecting bacterial viability [32]. Mutations in genes encoding antibiotic targets—such as DNA gyrase (fluoroquinolone target), penicillin-binding proteins (β-lactam targets), and ribosomal components (aminoglycoside targets)—can reduce drug affinity and confer resistance [31] [32]. These alterations often arise through spontaneous mutation and selective pressure during antibiotic treatment.
The alarming spread of resistance genes through horizontal gene transfer via plasmids, transposons, and integrons further accelerates the dissemination of these resistance mechanisms among bacterial populations [1]. This genetic mobility, combined with selective pressure from antibiotic use, has created a perfect storm for the rapid global spread of multidrug-resistant Gram-negative pathogens.
Experimental Frameworks and Research Methodologies
Standardized Susceptibility Testing Protocols
Accurate assessment of bacterial susceptibility to both traditional and non-traditional agents requires standardized methodologies. For conventional antibiotics, the Clinical and Laboratory Standards Institute (CLSI) provides reference methods including broth microdilution and disk diffusion [38]. These protocols involve:
- Bacterial Inoculum Preparation: Adjusting bacterial suspensions to a standardized turbidity (0.5 McFarland standard, approximately 1-2 × 10^8 CFU/mL) in appropriate media [38].
- Antibiotic Dilution Series: Preparing two-fold serial dilutions of antibiotics in cation-adjusted Mueller-Hinton broth for minimal inhibitory concentration (MIC) determination [38].
- Inoculation and Incubation: Adding standardized bacterial inoculum to antibiotic dilutions and incubating at 35±2°C for 16-20 hours [38].
- Endpoint Determination: MIC is defined as the lowest concentration that completely inhibits visible growth [38].
For non-traditional agents, modified approaches are often required. For phage therapy, susceptibility testing typically involves spot testing or efficiency of plating assays to determine the host range of phages against clinical isolates [36]. For β-lactam-β-lactamase inhibitor combinations, the broth disk elution method has been endorsed by CLSI to test the activity of ceftazidime-avibactam in combination with aztreonam against metallo-β-lactamase-producing Enterobacterales [38].
Clinical Trial Design Considerations
Developing appropriate clinical trial designs for novel antibacterial agents presents unique challenges. For traditional antibiotics with direct bactericidal activity, non-inferiority trials are often appropriate when effective standard treatments exist [34]. These designs aim to demonstrate that the new agent is not unacceptably less effective than existing therapy. Key considerations include:
- Non-inferiority Margin Selection: Based on historical evidence of drug efficacy and clinical judgement about acceptable loss of efficacy [34].
- Patient Population Definition: Typically focused on specific infection sites (e.g., complicated urinary tract infections, hospital-acquired pneumonia) with microbiological confirmation of causative pathogens [34].
- Endpoint Selection: Often composite endpoints incorporating clinical and microbiological outcomes at a defined test-of-cure visit (typically 7-14 days after end of treatment) [34].
For agents with non-traditional goals or mechanisms, alternative endpoints may be necessary. Anti-virulence agents that don't directly kill bacteria may require demonstration of reduced disease severity or complication rates [34]. Microbiome-modifying therapies might be evaluated based on colonization resistance or reduction in recurrent infections [34]. In some cases, innovative trial designs such as platform trials or studies using external controls may be appropriate, particularly for pathogens with limited treatment options [34].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Antibacterial Development
| Reagent/Platform | Function/Application | Specific Examples |
|---|---|---|
| Cation-adjusted Mueller-Hinton broth | Standardized medium for antibiotic susceptibility testing | CLSI-recommended for broth microdilution MIC determination |
| PCR and sequencing reagents | Detection and characterization of resistance genes | Identification of blaKPC, blaNDM, blaOXA-48 carbapenemase genes |
| Cell culture models | Assessment of host-pathogen interactions and drug penetration | Human epithelial cell lines for intracellular activity studies |
| Animal infection models | In vivo efficacy assessment | Mouse thigh infection model; neutropenic lung infection models |
| Mass spectrometry systems | Characterization of bacterial metabolites and antibiotic concentrations | LC-MS/MS for therapeutic drug monitoring |
| Flow cytometers | Analysis of bacterial viability and host immune responses | Assessment of membrane permeability and efflux pump activity |
| Biofilm reactors | Study of biofilm-associated infections | CDC biofilm reactor; Calgary biofilm device |
| Genome editing tools | Bacterial gene knockout and modification | CRISPR-Cas9 systems; allelic exchange techniques |
| Protein expression systems | Production of bacterial enzymes for biochemical studies | Recombinant β-lactamase expression for inhibitor screening |
| Artificial intelligence platforms | Drug discovery and resistance prediction | Machine learning for compound screening; AMR gene identification |
The clinical pipeline for antibacterial agents against resistant Gram-negative pathogens remains insufficient despite the escalating global threat of antimicrobial resistance. While the traditional antibiotic pipeline continues to contract, promising non-traditional approaches—particularly bacteriophage therapy, anti-virulence strategies, and immunotherapies—are advancing through clinical development. The continued evolution of sophisticated resistance mechanisms in Gram-negative bacteria, including enzymatic inactivation, efflux pumps, and target site modifications, necessitates innovative therapeutic strategies and robust diagnostic approaches.
Success in this field will require coordinated efforts across multiple domains: sustained investment in research and development, particularly for non-traditional approaches; regulatory frameworks adaptable to novel therapeutic paradigms; clinical trial designs that efficiently demonstrate efficacy for diverse product types; and global surveillance of emerging resistance patterns. The fragile ecosystem of antibacterial development, dominated by small companies with limited resources, underscores the need for continued public and private support to ensure that promising agents reach patients. Without such comprehensive efforts, the threat of untreatable Gram-negative infections will continue to escalate, undermining modern medical advances and global public health security.
The relentless expansion of antimicrobial resistance (AMR) in Gram-negative bacteria represents one of the most pressing challenges in modern infectious disease management. Particularly concerning is the rapid dissemination of carbapenem-resistant Enterobacterales (CRE) and Pseudomonas spp. (CR-PS), which have become serious causes of recalcitrant healthcare-associated infections that are often resistant to common therapeutic options [39]. Within this landscape, metallo-β-lactamases (MBLs) have emerged as a formidable resistance mechanism, conferring broad resistance to β-lactam drugs including carbapenems, and complicating clinical management worldwide [39] [40].
The global AMR crisis, often termed a "Silent Pandemic," demands urgent attention. If unaddressed, AMR is projected to cause over 10 million deaths annually by 2050 [41]. Gram-negative pathogens, particularly the ESKAPE organisms (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.), pose a significant healthcare risk due to their propensity for multidrug resistance [40] [41]. The declining effectiveness of current treatments against these pathogens has led to increased disease burden and mortality rates globally [40].
Against this backdrop, accurate antimicrobial susceptibility testing (AST) becomes paramount for effective patient management and antimicrobial stewardship. This technical guide examines the current landscape of AST methodologies, with a particular focus on detecting challenging resistance patterns such as MBL production in Gram-negative pathogens, and explores advanced diagnostic technologies that are revolutionizing the field.
Mechanisms of Antimicrobial Resistance in Gram-Negative Bacteria
Gram-negative bacteria employ four principal biochemical strategies to counteract antimicrobial agents, each with distinct genetic foundations and clinical implications.
Antibiotic Inactivation Enzymes
β-lactamases represent the most prevalent resistance mechanism, with over 2,000 variants identified. These enzymes hydrolyze the β-lactam ring of penicillins, cephalosporins, and carbapenems. MBLs, a subclass of β-lactamases, require zinc at their active site and hydrolyze all β-lactams except monobactams [39]. Their genes are often plasmid-encoded, facilitating horizontal transfer across species. The npmA gene, encoding a 16S rRNA methyltransferase, confers pan-aminoglycoside resistance and has been identified in globally distributed Clostridioides difficile ST11 lineages and vancomycin-resistant Enterococcus faecium [42].
Efflux Pump Systems
Multidrug efflux pumps, such as AcrAB-TolC in Escherichia coli and MexAB-OprM in P. aeruginosa, actively export diverse antibiotic classes from the cell. These membrane-spanning protein complexes contribute to intrinsic and acquired resistance through overexpression or mutation, often resulting in cross-resistance to unrelated antimicrobials [41].
Target Site Modification
Alterations in antibiotic targets preempt drug binding and neutralization. Examples include mutations in:
- Penicillin-binding proteins (PBPs) reducing β-lactam affinity
- DNA gyrase and topoisomerase IV conferring quinolone resistance
- rpsL and rsmG mutations leading to aminoglycoside resistance [43] Recent data document ATM/AVI resistance mechanisms among E. coli and P. aeruginosa isolates due to mutations in ftsI, encoding PBP-3, an essential class B PBP with transpeptidase activity [39].
Membrane Permeability Barriers
The Gram-negative outer membrane, with its asymmetric lipid bilayer and porin channels, constitutes a formidable physical barrier. Porin loss or modification, particularly of OmpF and OmpC, restricts antibiotic penetration. This mechanism often acts synergistically with efflux pump overexpression to confer multidrug resistance [41].
Table 1: Key Resistance Mechanisms in Gram-Negative Bacteria
| Mechanism | Genetic Determinants | Antibiotic Classes Affected | Example Organisms |
|---|---|---|---|
| Enzymatic Inactivation | MBL genes (NDM, VIM, IMP), npmA | β-lactams, Aminoglycosides | K. pneumoniae, P. aeruginosa |
| Efflux Systems | acrAB, mexAB, adeABC | Multiple classes including β-lactams, fluoroquinolones | A. baumannii, E. coli |
| Target Modification | ftsI, rpsL, gyrA, parC | β-lactams, Aminoglycosides, Fluoroquinolones | M. intracellulare, E. coli |
| Membrane Permeability | ompF, ompC, oprD | β-lactams, Carbapenems | K. pneumoniae, Enterobacter spp. |
Antimicrobial Susceptibility Testing Methodologies
Conventional and Phenotypic Methods
Traditional AST methods remain foundational in clinical microbiology laboratories, providing reliable detection of resistance patterns.
Disk Diffusion Testing offers a qualitative assessment of susceptibility based on zone diameter measurements. The RESIST-4 O.K.N.V. immunochromatographic assay exemplifies rapid phenotypic detection of carbapenemase-producing Enterobacteriaceae directly from positive blood cultures [39]. While cost-effective and straightforward, this method lacks precision for determining minimal inhibitory concentrations (MICs).
Broth Dilution Methods, both macrodilution and microdilution, provide quantitative MIC data essential for guiding antimicrobial therapy. Standardized per CLSI guidelines, these methods determine the lowest antimicrobial concentration that inhibits visible bacterial growth [21]. The Sensititre, Vitek 2 Compact System, and MicroScan WalkAway plus systems represent FDA-approved automated instruments that streamline this process [41].
Gradient Strip Methods (E-test) combine aspects of disk diffusion and dilution testing, using plastic strips with impregnated antibiotic gradients. Recent innovations include gradient strip stacking and crossing for evaluating antibiotic combinations against multidrug-resistant pathogens [39].
Advanced Methodologies for Challenging Resistances
The complexity of modern resistance patterns necessitates sophisticated testing approaches, particularly for MBL-producing isolates.
The Epsilon Test (E-test) employs a predefined gradient of antimicrobial agents on a plastic strip. For MBL detection, this method can demonstrate synergy between novel β-lactam/β-lactamase inhibitor combinations and established antibiotics [39].
Gradient Strip Stacking has emerged as a practical solution for clinical laboratories to assess combination therapies. This method involves applying strips containing different antibiotics perpendicularly or parallel to each other on inoculated agar plates. The resulting elliptical inhibition zone indicates synergistic activity [39]. This approach is particularly valuable for evaluating promising combinations like aztreonam/avibactam (ATM/AVI) against MBL-producing Enterobacterales, as recommended by the 2022 European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines [39].
Checkerboard Assays and Time-Kill Curves, while methodologically complex and labor-intensive, remain reference standards for evaluating antibiotic interactions. These techniques provide comprehensive data on synergistic, additive, or antagonistic effects between drug combinations [39].
Table 2: Comparison of AST Methods for Detecting Challenging Resistances
| Method | Principle | Turnaround Time | Advantages | Limitations | Best Applications |
|---|---|---|---|---|---|
| Disk Diffusion | Zone of inhibition measurement | 16-24 hours | Cost-effective, simple to perform | Qualitative only, subjective interpretation | Initial screening for resistance |
| Broth Microdilution | MIC determination in liquid media | 16-24 hours | Quantitative, automated systems available | Standardized inoculum required | Routine susceptibility testing |
| Gradient Strip Stacking | Synergy detection with multiple strips | 16-24 hours | Practical for clinical labs, tests combinations | More expensive than single strips | MBL detection with ATM/AVI combinations |
| Epsilon Test | Predefined antibiotic gradient | 16-24 hours | Simple implementation, quantitative | Limited to available strip formulations | MBL confirmation and synergy testing |
| Automated Systems | Growth detection in liquid media | 4-15 hours | Rapid, high-throughput, minimal hands-on time | High equipment cost, limited drug panels | High-volume laboratories |
Experimental Protocols for Key Methodologies
Gradient Strip Stacking for ATM/AVI Synergy Detection
Background: This protocol evaluates the synergistic activity of ceftazidime/avibactam (CZA) with aztreonam (ATM) against MBL-producing Gram-negative bacteria, addressing the challenge of detecting susceptibility to combination therapies [39].
Materials:
- Mueller-Hinton Agar (MHA) plates: Standardized medium for AST
- Aztreonam (ATM) and Ceftazidime/Avibactam (CZA) gradient strips: Commercially available E-test strips
- Sterile cotton swabs or adjustable nephelometer: For inoculum preparation
- McFarland 0.5 standard: For inoculum standardization
- Incubator (35±2°C): For controlled incubation
- Clinical isolates with confirmed MBL production: Test organisms
Procedure:
- Inoculum Preparation: Prepare a bacterial suspension equivalent to a 0.5 McFarland standard (approximately 1.5 × 10^8 CFU/mL) in sterile saline or broth.
- Inoculation: Evenly spread the inoculum over the entire surface of an MHA plate using a sterile swab and allow to dry for 3-5 minutes.
- Strip Application: Apply the ATM gradient strip first, followed by perpendicular placement of the CZA strip, ensuring they intersect at their respective MIC values.
- Incubation: Invert plates and incubate at 35±2°C for 16-20 hours in an ambient air incubator.
- Interpretation: Examine for an elliptical or synergistic extension of the inhibition zone at the intersection of the two strips. A decrease in MIC for either antibiotic at the intersection indicates synergistic activity.
Quality Control: Include reference strains with known susceptibility profiles (e.g., E. coli ATCC 25922) to ensure accuracy and reproducibility.
Broth Microdilution for MIC Determination
Background: This CLSI-standardized method determines the minimal inhibitory concentration (MIC) of antimicrobial agents, providing essential quantitative data for clinical decision-making [21].
Materials:
- Cation-adjusted Mueller-Hinton Broth (CA-MHB): Standardized growth medium
- Sterile 96-well microtiter plates: With U- or V-bottom wells
- Antibiotic stock solutions: At appropriate concentrations
- Multichannel pipettes: For accurate liquid handling
- Microplate reader: For optical density measurement
Procedure:
- Preparation of Antibiotic Dilutions: Create two-fold serial dilutions of the antibiotic in CA-MHB across the microtiter plate wells.
- Inoculum Standardization: Prepare a bacterial suspension equivalent to a 0.5 McFarland standard, then dilute to achieve a final inoculum of approximately 5 × 10^5 CFU/mL in each well.
- Incubation: Cover plates and incubate at 35±2°C for 16-20 hours without shaking.
- Reading Results: Examine wells for visible growth inhibition. The MIC is defined as the lowest concentration of antibiotic that completely inhibits visible growth.
Quality Control: Include growth control (inoculum without antibiotic), sterility control (medium only), and reference strains with known MIC ranges.
Advanced Diagnostic Technologies in AMR
Technological innovations are transforming AMR diagnostics, enabling faster, more precise detection of resistance mechanisms.
CRISPR-Based Diagnostics leverage the gene-editing capability of CRISPR systems for ultra-specific detection of resistance genes, even in complex samples. This precision enables detection of AMR at its genetic foundation, facilitating targeted therapies [41].
Mass Spectrometry, particularly MALDI-TOF (Matrix-Assisted Laser Desorption/Ionization Time-of-Flight), provides rapid identification of pathogens and resistance mechanisms through precise analysis of microbial protein profiles. This technology is increasingly used in clinical settings to deliver both pathogen identification and resistance profiling in record time [41].
Flow Cytometry enables real-time, single-cell analysis, permitting dynamic monitoring of phenotypic resistance and treatment response. This technology enhances the ability to detect subtle changes in bacterial populations, providing critical insights into AMR development [41].
Biosensors offer rapid, cost-effective, and portable detection of AMR. With their high sensitivity and capacity for multiplex pathogen detection, biosensors are emerging as essential tools for point-of-care diagnostics [41].
Table 3: Research Reagent Solutions for Advanced AMR Detection
| Reagent/Technology | Function/Application | Example Uses | Key Features |
|---|---|---|---|
| CRISPR-Cas Systems | Gene-specific detection | Identification of blaNDM, blaKPC genes | Ultra-high specificity, rapid results |
| MALDI-TOF Mass Spectrometry | Pathogen identification & resistance profiling | Detection of carbapenemase activity | High-throughput, minimal sample processing |
| Flow Cytometry Reagents | Viability staining & single-cell analysis | Monitoring antibiotic killing kinetics | Real-time monitoring, phenotypic assessment |
| Microfluidic Chips | Miniaturized assay platforms | Point-of-care AMR detection | Low sample volume, portable |
| Whole Genome Sequencing Kits | Comprehensive genetic analysis | Identification of resistance mutations | Unbiased detection, discovery potential |
Detection Workflow and Resistance Mechanisms
The following diagram illustrates the integrated workflow for detecting challenging resistances like MBL in Gram-negative bacteria, incorporating both phenotypic and genotypic methods:
Integrated Workflow for MBL Detection in Gram-Negative Bacteria
The molecular mechanisms underlying resistance in Gram-negative bacteria involve complex interactions between genetic determinants and cellular pathways, as illustrated below:
Molecular Mechanisms of Antibiotic Resistance in Gram-Negative Bacteria
The evolving landscape of antimicrobial resistance in Gram-negative pathogens necessitates continuous refinement of susceptibility testing methodologies. The emergence of strains producing carbapenemases, particularly MBLs, poses significant challenges in treating CRE and CR-PS infections. While novel combinations like aztreonam/avibactam offer valuable additions to the treatment arsenal for MBL-producing Enterobacteriaceae, their role in treating Pseudomonas spp. remains uncertain and requires further investigation [39].
Advanced diagnostic technologies, including CRISPR-based systems, mass spectrometry, and biosensors, are revolutionizing AMR detection by providing faster, more accurate results. These innovations are critical for addressing the global AMR crisis. The gradient strip stacking method represents a practical approach for clinical laboratories to evaluate combination therapies against multidrug-resistant pathogens, bridging the gap between complex reference methods and routine clinical practice [39].
Future directions in AMR diagnostics will likely focus on developing standardized methods for testing antibiotic combinations, integrating genomic and phenotypic data for comprehensive resistance profiling, and creating point-of-care platforms for rapid detection. As resistance mechanisms continue to evolve, ongoing research and development of novel AST methodologies will remain essential for effective patient management and antimicrobial stewardship.
The management of antimicrobial-resistant (AMR) Gram-negative infections represents a critical frontier in clinical practice and biomedical research. The Infectious Diseases Society of America (IDSA) 2024 guidance provides updated recommendations for treating infections caused by extended-spectrum β-lactamase-producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Acinetobacter baumannii (CRAB), and difficult-to-treat resistant Pseudomonas aeruginosa (DTR P. aeruginosa) [38]. These pathogens have been designated urgent or serious threats by the CDC, causing significant morbidity and mortality worldwide [38]. This guidance document, distinct from formal practice guidelines, is prepared by a team of experts who answer specific treatment questions based on comprehensive literature review, clinical experience, and expert opinion, with updates provided annually to address the highly dynamic field of AMR [38] [44]. For researchers investigating resistance mechanisms and novel therapeutic approaches, understanding these evidence-based clinical recommendations provides essential context for prioritizing research directions and translating basic science discoveries into clinical practice.
Pathogen-Specific Treatment Recommendations
Extended-Spectrum β-Lactamase-Producing Enterobacterales (ESBL-E)
Table 1: Recommended Treatment Approaches for ESBL-E Infections
| Infection Type | Preferred Agents | Alternative Agents | Key Updates & Clinical Considerations |
|---|---|---|---|
| Uncomplicated Cystitis | Nitrofurantoin, TMP-SMX [45] | Fluoroquinolones, carbapenems (should be reserved) [45] | Amoxicillin-clavulanic acid not preferred but may be used if resistance or toxicities preclude alternatives; patients should be cautioned about increased recurrence risk [38] [44]. |
| Pyelonephritis or complicated UTI (cUTI) | TMP-SMX, ciprofloxacin, levofloxacin [45] | Carbapenems (when resistance precludes other options) [45] | Piperacillin-tazobactam not recommended; if initiated and clinical improvement occurs, decision to continue should consider theoretical risk of microbiological failure [38]. Fosfomycin not suggested for pyelonephritis/cUTI [38]. |
| Systemic Infections (non-UTI) | Carbapenems [46] | Ceftolozane-tazobactam (should be preserved for DTR P. aeruginosa or polymicrobial infections) [38] | Ceftolozane-tazobactam likely effective against ESBL-E but reserved for more severe cases [38] [44]. |
Carbapenem-Resistant Enterobacterales (CRE)
Table 2: Recommended Treatment Approaches for CRE Infections
| Resistance Mechanism | Preferred Agents | Alternative Agents | Key Updates & Clinical Considerations |
|---|---|---|---|
| Metallo-β-lactamase (MBL)-producing CRE (e.g., NDM, VIM, IMP) | Ceftazidime-avibactam + aztreonam [38] [45] | Cefiderocol [47] | Updated dosing: both agents administered every 8 hours to facilitate simultaneous administration [38]. CLSI-endorsed broth disk elution method recommended for testing combination activity [38]. |
| Serine Carbapenemase-producing CRE | Ceftazidime-avibactam, meropenem-vaborbactam [46] | Imipenem-cilastatin-relebactam, cefiderocol [46] [47] | Increased prevalence of MBL-producing CRE isolates acknowledged in the U.S. [38] [44]. |
Carbapenem-ResistantAcinetobacter baumannii(CRAB)
Table 3: Recommended Treatment Approaches for CRAB Infections
| Treatment Category | Recommended Agents | Dosing Regimen | Key Updates & Clinical Considerations |
|---|---|---|---|
| Preferred Regimen | Sulbactam-durlobactam + meropenem or imipenem-cilastatin [38] [45] [44] | Per manufacturer recommendations | New preferred regimen for CRAB infections in 2024 guidance; addresses challenges of drug availability and susceptibility testing implementation [44]. |
| Alternative Regimen (if preferred not available) | High-dose ampicillin-sulbactam + at least one other agent [38] [44] | 27 grams daily (18g ampicillin, 9g sulbactam) [38] [44] | Changed from preferred to alternative regimen; typically combined with additional agents such as polymyxins or tetracycline derivatives [38]. |
| Other Options | Cefiderocol, eravacycline, minocycline, tigecycline [48] | Varies by agent | Consider based on susceptibility patterns and clinical context [48]. |
Difficult-to-Treat ResistantPseudomonas aeruginosa(DTR P. aeruginosa)
DTR P. aeruginosa is defined as resistance to all first-line agents, including piperacillin-tazobactam, ceftazidime, cefepime, aztreonam, meropenem, imipenem-cilastatin, ciprofloxacin, and levofloxacin [47].
Table 4: Recommended Treatment Approaches for DTR P. aeruginosa Infections
| Infection Type | Preferred Agents | Alternative Agents | Key Updates & Clinical Considerations |
|---|---|---|---|
| Uncomplicated UTI | Ceftolozane-tazobactam, ceftazidime-avibactam, imipenem-cilastatin-relebactam, cefiderocol [47] | Single-dose tobramycin or amikacin [47] | Based on clinical trials showing noninferiority for uUTI [47]. |
| Complicated UTI | Ceftolozane-tazobactam, ceftazidime-avibactam, imipenem-cilastatin-relebactam, cefiderocol [47] | Once-daily tobramycin or amikacin [38] [44] | Once-daily aminoglycosides added as alternatives due to prolonged renal cortex activity and dosing convenience [38]. |
| Infections outside urinary tract | Ceftolozane-tazobactam, ceftazidime-avibactam, imipenem-cilastatin-relebactam [47] | Cefiderocol [47] | Based on in-vitro activity and clinical trial data [47]. Traditional β-lactams (e.g., cefepime) with high-dose extended-infusion suggested for isolates susceptible to traditional agents but not carbapenems [38] [45]. |
Experimental Protocols for Antimicrobial Susceptibility Testing
Broth Disk Elution Method for MBL-Producing Enterobacterales
Purpose: To determine the efficacy of ceftazidime-avibactam and aztreonam combination against metallo-β-lactamase (MBL)-producing CRE, as endorsed by the Clinical and Laboratory Standards Institute (CLSI) [38].
Materials:
- Cation-adjusted Mueller-Hinton broth (CA-MHB)
- Ceftazidime-avibactam and aztreonam disks
- Sterile saline
- Standardized bacterial inoculum (0.5 McFarland standard)
- 96-well microtiter plates
- Incubator set to 35°C ± 2°C
Methodology:
- Prepare antibiotic solutions by eluting disks in CA-MHB to achieve desired concentration gradients.
- Prepare bacterial suspension adjusted to 0.5 McFarland standard (approximately 1-5 × 10^8 CFU/mL).
- Further dilute bacterial suspension to achieve final inoculum of 5 × 10^5 CFU/mL in each well.
- Combine ceftazidime-avibactam and aztreonam in broth medium across serial dilutions.
- Incubate plates for 16-20 hours at 35°C ± 2°C.
- Determine Minimum Inhibitory Concentration (MIC) as the lowest concentration completely inhibiting visible growth.
Interpretation: Synergy is demonstrated by a reduction in MIC of the combination compared to either agent alone, indicating potential clinical efficacy against MBL-producing organisms [38].
Susceptibility Testing for DTR P. aeruginosa Against Novel β-Lactams
Purpose: To guide treatment selection for DTR P. aeruginosa by testing susceptibility to newer β-lactam agents [47].
Materials:
- CA-MHB
- Novel β-lactam agents: ceftolozane-tazobactam, ceftazidime-avibactam, imipenem-cilastatin-relebactam, cefiderocol
- Standardized bacterial inoculum
- Microtiter plates
- Incubator
Methodology:
- Conduct standard broth microdilution according to CLSI guidelines.
- For cefiderocol, incorporate iron-depleted conditions to properly assess activity [47].
- Test all four novel β-lactams simultaneously when DTR P. aeruginosa is identified.
- Incubate for 16-20 hours at 35°C ± 2°C.
- Determine MIC values for each agent.
Interpretation:
- If recent treatment with ceftolozane-tazobactam or ceftazidime-avibactam and recurrent infection is suspected, prioritize imipenem-cilastatin-relebactam or cefiderocol initially while awaiting susceptibility results due to risk of cross-resistance [47].
- Be aware of regional differences in enzymatic resistance mechanisms that may affect susceptibility patterns [38].
Research Reagent Solutions for Antimicrobial Resistance Studies
Table 5: Essential Research Reagents for Investigating Resistant Gram-Negative Pathogens
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Novel β-Lactam Agents | Ceftolozane-tazobactam, ceftazidime-avibactam, imipenem-cilastatin-relebactam, meropenem-vaborbactam, cefiderocol [46] [47] | Mechanism of action studies, resistance development investigations | Target penicillin-binding proteins with enhanced stability against β-lactamases; cefiderocol utilizes iron transport systems for cellular entry [47]. |
| β-Lactamase Inhibitors | Avibactam, vaborbactam, relebactam, durlobactam [38] [45] | Enzyme inhibition kinetics, combination therapy efficacy | Protect companion β-lactams from hydrolysis by targeting specific β-lactamase enzymes (e.g., durlobactam against CRAB carbapenemases) [38] [45]. |
| Specialized Culture Media | Iron-depleted Mueller-Hinton broth [47] | Cefiderocol susceptibility testing | Creates iron-deficient conditions essential for proper function of siderophore cephalosporin antibiotics [47]. |
| Resistance Mechanism Probes | Specific β-lactamase gene primers (e.g., for NDM, VIM, KPC, OXA-type) [38] | Molecular epidemiology studies, resistance gene detection | Enable identification and tracking of specific resistance determinants across clinical isolates. |
| Efflux Pump Inhibitors | Phe-Arg-β-naphthylamide (PAβN), carbonyl cyanide m-chlorophenyl hydrazone (CCCP) [47] | Efflux pump activity studies | Differentiate efflux-mediated resistance from other mechanisms; useful for investigating multidrug resistance phenotypes. |
Resistance Mechanism Visualization
Figure 1: Mechanisms of antimicrobial resistance in Gram-negative bacteria and corresponding therapeutic strategies. Resistance pathways (red) illustrate common mechanisms employed by ESBL-E, CRE, CRAB, and DTR P. aeruginosa. Treatment approaches (blue) and their methods of overcoming resistance (green) demonstrate how novel agents target specific resistance mechanisms, such as enhanced β-lactamase stability, siderophore-mediated transport, and combination strategies [38] [47] [49].
Research Implications and Future Directions
The IDSA 2024 guidance highlights critical knowledge gaps that represent opportunities for future research. For CRAB infections, the recommendation of sulbactam-durlobactam represents a significant advancement, yet clinical experience remains limited, and implementation challenges related to cost and susceptibility testing availability persist [44]. Research into optimizing combination regimens and understanding resistance emergence to this new agent is warranted. For DTR P. aeruginosa, the recognition of substantial cross-resistance between ceftolozane-tazobactam and ceftazidime-avibactam, even without prior exposure to the latter, underscores the need to investigate shared resistance pathways and develop strategies to prevent cross-resistance development [47]. Additionally, the rising incidence of MBL-producing CRE in the United States highlights the growing importance of the ceftazidime-avibactam plus aztreonam combination, necessiting further research on optimal dosing, synergy testing standardization, and prevention of resistance emergence during therapy [38] [44]. These clinical challenges represent fertile ground for basic and translational research aimed at understanding resistance mechanisms and developing next-generation antimicrobial agents.
The World Health Organization (WHO) established the Global Antimicrobial Resistance and Use Surveillance System (GLASS) to generate standardized, comparable data on antimicrobial resistance (AMR) worldwide. The GLASS 2025 report represents the most comprehensive assessment since the system's launch, providing the first global resistance prevalence estimates across 22 antibiotics used to treat common infections [50] [26]. This technical guide interprets these critical findings within the broader context of Gram-negative bacterial resistance mechanisms, offering researchers and drug development professionals methodologies for analyzing surveillance data and translating findings into targeted therapeutic strategies.
The 2025 report draws on more than 23 million bacteriologically confirmed cases of bloodstream infections, urinary tract infections, gastrointestinal infections, and urogenital gonorrhea reported by 104 countries in 2023, with trend analysis spanning 2018-2023 [26]. This vast dataset enables unprecedented analysis of resistance patterns across eight common bacterial pathogens, with particular significance for understanding the evolution of resistance mechanisms in Gram-negative bacteria such as Escherichia coli, Klebsiella pneumoniae, and Acinetobacter spp. [50]
The GLASS 2025 report reveals that one in six laboratory-confirmed bacterial infections globally were resistant to antibiotic treatments in 2023 [50]. Between 2018 and 2023, antibiotic resistance increased in over 40% of the pathogen-antibiotic combinations monitored, with an average annual increase of 5-15% [50] [51]. This trend is particularly alarming for Gram-negative bacteria, where resistance to first-line and last-resort antibiotics continues to escalate, narrowing therapeutic options and threatening modern medical advancements.
The report highlights significant regional disparities in resistance prevalence, with the highest burdens in health systems with limited diagnostic capacity and restricted access to essential antibiotics [51]. The surveillance data confirms that drug-resistant Gram-negative bacteria pose the most severe threat, with E. coli and K. pneumoniae leading resistance in life-threatening bloodstream infections [50].
Global Resistance Prevalence: Quantitative Analysis
Regional Resistance Patterns
Table 1: Regional Variation in Antibiotic Resistance Prevalence (2023)
| WHO Region | Resistance Prevalence | Key Observations |
|---|---|---|
| South-East Asia | 1 in 3 infections resistant | Highest regional burden |
| Eastern Mediterranean | 1 in 3 infections resistant | Similar to South-East Asia |
| Africa | 1 in 5 infections resistant | Exceeds 70% resistance to third-generation cephalosporins for some pathogens |
| Americas | 1 in 7 infections resistant | Slightly better than global average |
| Europe | 1 in 10 infections resistant | Lowest regional prevalence [50] [51] [52] |
The disparities in resistance prevalence reflect variations in health system capacity, diagnostic capabilities, antimicrobial stewardship, and access to essential medicines [51]. Countries with weaker health systems and limited surveillance capacity face the dual challenge of higher resistance rates and less comprehensive data, creating significant gaps in the global AMR picture [50].
Pathogen-Specific Resistance Profiles
Table 2: Resistance in Key Gram-Negative Pathogens to First-Line Antibiotics
| Pathogen | Infection Type | Antibiotic Class | Global Resistance Rate | High-Burden Region |
|---|---|---|---|---|
| Escherichia coli | Bloodstream | Third-generation cephalosporins | 44.8% | Africa (>70%) |
| Klebsiella pneumoniae | Bloodstream | Third-generation cephalosporins | 55.2% | Africa (>70%) |
| Acinetobacter spp. | Bloodstream | Carbapenems | 54.3% | South-East Asia (K. pneumoniae: 41.2% carbapenem resistance) |
| E. coli and K. pneumoniae | Various | Fluoroquinolones | Increasing | Multiple regions [50] [51] |
The data reveals concerning trends in resistance to "Watch" antibiotics - broad-spectrum agents that WHO recommends should be used with caution and prioritized as second-line treatments [51]. The progression of resistance in Gram-negative pathogens follows a predictable pattern, beginning with resistance to first-line antibiotics like third-generation cephalosporins, followed by development of resistance to broader-spectrum alternatives like fluoroquinolones, and ultimately extending to last-resort carbapenems [50] [53].
Resistance Mechanisms in Gram-Negative Bacteria: Connecting Surveillance to Molecular Pathways
Surveillance data from GLASS must be interpreted through the lens of the fundamental resistance mechanisms employed by Gram-negative bacteria. The following diagram illustrates the primary biochemical pathways through which Gram-negative pathogens achieve resistance to critical antibiotic classes.
The molecular mechanisms illustrated above manifest in the resistance patterns documented in GLASS surveillance data:
Enzymatic inactivation: The high prevalence of resistance to third-generation cephalosporins (44.8% in E. coli, 55.2% in K. pneumoniae) primarily results from extended-spectrum β-lactamase (ESBL) production [50] [54]. These enzymes hydrolyze the β-lactam ring, rendering cephalosporins ineffective.
Membrane permeability and efflux: The increasing carbapenem resistance (54.3% in Acinetobacter spp.) often involves porin mutations combined with efflux pump upregulation, reducing intracellular antibiotic accumulation [54]. This mechanism is particularly concerning as carbapenems are last-resort antibiotics for multidrug-resistant infections.
Target modification: Resistance to fluoroquinolones frequently results from mutations in DNA gyrase and topoisomerase IV genes, preventing antibiotic binding while maintaining enzyme function [55].
The convergence of these mechanisms in multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains creates therapeutic challenges evident in the GLASS report, where nearly 40% of Klebsiella spp. isolates were classified as MDR/XDR, with significant increases in resistance to cephalosporins, fluoroquinolones, and carbapenems between 2022-2024 [55].
Methodological Framework: GLASS Surveillance Protocols
Core Surveillance Methodology
The WHO GLASS system employs standardized protocols for data collection, analysis, and reporting to ensure comparability across participating countries. The following diagram outlines the integrated surveillance workflow from sample collection to data dissemination.
Laboratory Methods for Antimicrobial Susceptibility Testing
The GLASS 2025 report integrates data generated through standardized laboratory methodologies. The following experimental protocols detail the key procedures for generating reliable antimicrobial susceptibility data:
Protocol 1: Bacterial Identification and Antimicrobial Susceptibility Testing (AST)
- Sample Processing: Clinical specimens (blood, urine, respiratory secretions, etc.) are processed following standardized collection protocols. Blood samples are collected in specialized aerobic and anaerobic culture bottles (e.g., Bact/Alert 70 3D system) [55].
- Bacterial Identification: Gram-negative isolates are identified using automated systems such as Vitek 2 Compact (Biomerieux) with GN identification cards [55].
- Susceptibility Testing: Antimicrobial susceptibility testing is performed using:
- Vitek 2 AST cards (AST-N233 and AST-XN05 for extended antibiogram) for minimum inhibitory concentration (MIC) determination
- Compliance with Clinical Laboratory Standard Institute (CLSI) guidelines [55]
- Broth microdilution method (e.g., ComASP Colistin Test Panel) for polymyxin resistance testing [55]
- Quality Control: Implementation of external quality assurance programs and quality management systems to ensure result reliability.
Protocol 2: Resistance Mechanism Characterization
- Phenotypic Detection: Automated systems (e.g., Vitek 2 software version 9.02.4.531) report resistance mechanisms including ESBL and carbapenemase production [55].
- Molecular Confirmation: For critical resistance patterns (e.g., carbapenem resistance), confirmatory testing using:
- PCR-based detection of resistance genes (e.g., KPC, NDM, OXA-48-like)
- Whole-genome sequencing for outbreak investigation and novel mechanism identification [54]
- Classification Criteria: Isolates categorized as MDR (non-susceptible to ≥3 antimicrobial categories), XDR (non-susceptible to all but ≤2 categories), or PDR (non-susceptible to all antimicrobial categories) [55].
Data Management and Statistical Analysis
Protocol 3: Data Management and Resistance Trend Analysis
- Data Standardization: National data standardized using WHONET software, a free Windows application for microbiology laboratory data management and AMR surveillance, available in 28 languages and supporting more than 2300 laboratories worldwide [56].
- Statistical Analysis:
- Resistance rates expressed as percentage of resistant isolates among all tested isolates
- Trend analysis using chi-square test or Fisher's exact test for small groups [55]
- Mixed-effect regression models with beta distribution to assess impact of antimicrobial consumption on resistance prevalence [53]
- Adjustment for sampling bias and population representation in national estimates
- Surveillance Quality Assessment: Implementation of scoring framework to assess completeness of national data and representativeness of surveillance systems [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for AMR Surveillance and Mechanism Studies
| Reagent/Material | Application | Technical Specifications | Research Utility |
|---|---|---|---|
| Vitek 2 Compact System | Bacterial identification & AST | GN cards for identification; AST-N233/XNO5 for MIC testing | Automated, standardized susceptibility testing for GLASS compliance [55] |
| WHONET Software | AMR data management | Desktop application, 28 language interfaces | Laboratory data analysis, trend detection, & GLASS reporting [56] |
| ComASP Colistin Test Panel | Polymyxin resistance testing | Broth microdilution format | Reference method for last-resort antibiotic susceptibility [55] |
| Bact/Alert 70 3D Culture Bottles | Bloodstream infection detection | Aerobic/anaerobic paired bottles | Optimal recovery of pathogens from blood cultures [55] |
| CRGNB Reference Strains | Resistance mechanism studies | Characterized carbapenem-resistant isolates | Controls for molecular assays & therapeutic studies [54] |
| β-Lactam/β-Lactamase Inhibitor Combinations | Novel therapeutic assessment | e.g., sulbactam-durlobactam, imipenem-relebactam | Evaluation of emerging treatment options [54] |
Research Implications and Future Directions
The GLASS 2025 data reveals several critical priorities for the research community. First, the accelerating resistance in Gram-negative pathogens, particularly to carbapenems, demands urgent development of novel antimicrobial classes with activity against MDR strains [50] [54]. Promising agents in development include siderophore antibiotics, novel β-lactam/β-lactamase inhibitors, and antimicrobial peptides [54].
Second, the regional disparities in resistance prevalence highlight the need for context-specific interventions. Research should focus on developing rapid diagnostic tools suitable for low-resource settings, enabling targeted antibiotic therapy and reducing selective pressure from inappropriate antimicrobial use [51] [53].
Finally, the integrated analysis of antimicrobial consumption and resistance patterns provides critical insights for stewardship programs. Recent studies using GLASS data have established statistically significant correlations between beta-lactam/cephalosporin consumption and resistance in E. coli and K. pneumoniae, with each unit increase in defined daily dose (DDD) increasing resistant isolates by 11-22% [53]. This relationship underscores the importance of coupling surveillance of resistance with monitoring of antimicrobial use.
The future of AMR control depends on strengthening global surveillance systems while accelerating basic research on resistance mechanisms and therapeutic innovations. The WHO GLASS platform provides the essential framework for monitoring progress toward these goals and targeting interventions where they are most urgently needed.
Overcoming Resistance: Strategic Countermeasures and Novel Therapeutic Avenues
The escalating crisis of antimicrobial resistance (AMR) represents one of the most pressing challenges to modern medical practice, with Gram-negative bacteria constituting a particularly formidable threat due to their complex cell envelope structure and sophisticated resistance mechanisms [1] [31]. The World Health Organization (WHO) has classified several Gram-negative pathogens as priority pathogens for urgent research and development, emphasizing the critical need for new therapeutic options [1] [31]. β-lactam antibiotics, characterized by their β-lactam ring and constituting approximately 65% of the global antibiotics market, have seen their efficacy progressively eroded by bacterial enzyme production [57] [58]. The most prevalent resistance mechanism in Gram-negative bacteria involves the production of β-lactamase enzymes, which hydrolyze the amide bond within the β-lactam ring, rendering the antibiotic inactive [59]. In response, the strategic development of β-lactam/β-lactamase inhibitor (BL/BLI) combinations has emerged as a cornerstone approach to overcoming bacterial resistance mechanisms and preserving the utility of these essential antimicrobial agents [57] [60].
Resistance Mechanisms in Gram-Negative Bacteria
The Gram-Negative Cell Envelope: A Formidable Barrier
The intrinsic resistance of Gram-negative bacteria is largely attributable to their unique cell envelope structure, which consists of three primary layers: an outer membrane (OM) containing lipopolysaccharides (LPS) and porin channels, a thin peptidoglycan cell wall, and an inner cytoplasmic membrane (IM) [1] [31]. This complex structure acts as a selective barrier, significantly limiting antibiotic penetration and accumulation within the cell. The outer membrane serves as a particularly effective permeability barrier, with hydrophilic antibiotics such as β-lactams requiring passage through porin channels to reach their targets [31]. Additionally, the lipopolysaccharide components of the outer membrane contribute to structural integrity and play a key role in pathogen virulence by modulating host immune responses [1].
Molecular Mechanisms of Antibiotic Resistance
Gram-negative bacteria employ four principal mechanisms to evade the activity of β-lactam antibiotics:
- Enzymatic Inactivation: Production of β-lactamase enzymes that hydrolyze the β-lactam ring is the most common resistance mechanism. These enzymes are classified into four Ambler classes (A-D) based on molecular structure [58] [59].
- Reduced Permeability: Modifications to outer membrane porins limit antibiotic penetration into the bacterial cell, effectively reducing intracellular drug concentrations [1] [61].
- Efflux Pump Systems: Overexpression of Resistance-Nodulation-Division (RND) efflux pumps actively exports antibiotics from the cell, contributing to multidrug resistance phenotypes [61].
- Target Modification: Alterations in penicillin-binding proteins (PBPs) reduce antibiotic binding affinity and efficacy, particularly in Gram-positive bacteria but with some relevance to Gram-negative pathogens [58].
Table 1: Major β-Lactamase Classes and Their Characteristics
| Ambler Class | Catalytic Mechanism | Key Enzymes | Inhibitors | Hydrolysis Profile |
|---|---|---|---|---|
| Class A | Serine-based | ESBLs (CTX-M, SHV, TEM), KPC | Clavulanic acid, avibactam | Penicillins, cephalosporins, carbapenems (KPC) |
| Class B | Metallo-β-lactamases (MBLs) requiring Zn²⁺ | NDM, VIM, IMP | No clinically available inhibitors (EDTA in lab) | Nearly all β-lactams except monobactams |
| Class C | Serine-based | AmpC (CMY, FOX, DHA) | Boronic acid derivatives, avibactam | Cephalosporins, cephamycins |
| Class D | Serine-based | OXA-type | Limited inhibition by available inhibitors | Penicillins, carbapenems (OXA-48) |
Recently Approved BL/BLI Combinations and Their Clinical Applications
The urgent need to combat multidrug-resistant Gram-negative infections has driven the approval of several innovative BL/BLI combinations in recent years. These agents are strategically designed to target specific resistance mechanisms prevalent in clinical settings.
Cefepime/Enmetazobactam
Cefepime/enmetazobactam combines a fourth-generation cephalosporin with a novel β-lactamase inhibitor (penicillin acid sulfone) that primarily targets extended-spectrum β-lactamases (ESBLs) [57]. Enmetazobactam, a tazobactam derivative, exhibits enhanced activity against Class A β-lactamases, including ESBLs and some carbapenemases [57]. This combination is approved for treating complicated urinary tract infections (cUTIs), including pyelonephritis, in both the US and Europe, with additional indications for hospital-acquired pneumonia (HAP), ventilator-associated pneumonia (VAP), and associated bacteremia in Europe [57]. Its spectrum specifically covers ESBL-producing Pseudomonas aeruginosa and Enterobacterales [57].
Aztreonam/Avibactam
Aztreonam/avibactam represents a strategic approach to overcoming metallo-β-lactamase (MBL)-mediated resistance. While aztreonam, a monobactam, remains stable against MBLs (Class B), it is vulnerable to hydrolysis by coexisting ESBLs, AmpC, and carbapenemases [57]. Avibactam, a diazabicyclooctane (DBO) inhibitor, protects aztreonam by inhibiting these accompanying serine β-lactamases (Classes A, C, and some D) [57] [59]. This combination is indicated for complicated intra-abdominal infections (cIAI), cUTI, HAP, and VAP caused by carbapenem-resistant Enterobacterales, including those producing MBLs [57].
Sulbactam/Durlobactam
Sulbactam/durlobactam employs a unique dual-inhibitor strategy to combat carbapenem-resistant Acinetobacter baumannii (CRAB) [57]. Sulbactam possesses intrinsic antibacterial activity against A. baumannii by targeting PBP1 and PBP3, while durlobactam, a diazabicyclooctane β-lactamase inhibitor, protects sulbactam from hydrolysis by neutralizing serine β-lactamases, including Class D OXA-type carbapenemases [57]. This combination is approved for treating hospital-acquired and ventilator-associated bacterial pneumonia (HABP/VABP) caused by the Acinetobacter baumannii-calcoaceticus complex [57].
Table 2: Recently Approved BL/BLI Combinations (2023-2024)
| Generic Name | Brand Name | Approval Year | Antibiotic Class | Target Pathogens | Approved Indications |
|---|---|---|---|---|---|
| Cefepime/Enmetazobactam | EXBLIFEP | 2024 | 4th-gen cephalosporin/penicillin acid sulfone | ESBL-producing P. aeruginosa and Enterobacterales | cUTI, pyelonephritis; HAP, VAP (Europe) |
| Aztreonam/Avibactam | EMBLAVEO | 2023 | Monobactam/DBO inhibitor | Carbapenem-resistant Enterobacterales (including MBL-producers) | cIAI, cUTI, HAP, VAP in adults with limited options |
| Sulbactam/Durlobactam | XACDURO | 2023 | β-lactamase inhibitor/β-lactamase inhibitor | A. baumannii-calcoaceticus complex (CRAB) | HABP, VABP in adults |
Investigational Agents in the Developmental Pipeline
The pipeline of novel BL/BLI combinations remains robust, with several promising candidates advancing through clinical trials to address persistent resistance challenges, particularly against MBL-producing pathogens.
Cefepime/Taniborbactam
Cefepime/taniborbactam combines a fourth-generation cephalosporin with a novel cyclic boronate β-lactamase inhibitor [58] [59]. Taniborbactam (VNRX-5133) demonstrates potent activity against both serine-β-lactamases (Classes A, C, D) and metallo-β-lactamases (Class B), representing one of the first broad-spectrum inhibitors with dual serine/MBL coverage [58]. This combination exhibits in vitro activity against a wide range of β-lactamase-producing Enterobacterales and Pseudomonas aeruginosa, including strains producing ESBLs, KPC, and MBLs [59]. It is currently undergoing phase 3 clinical evaluation for the treatment of cUTI and HAP/VAP [59].
Cefepime/Zidebactam
Cefepime/zidebactam features an innovative "enhancer" mechanism, wherein zidebactam (a DBO) not only inhibits β-lactamases (Classes A, C, and some D) but also binds with high affinity to penicillin-binding protein 2 (PBP2), thereby exhibiting intrinsic antibacterial activity [59]. This dual action enhances the activity of cefepime against MDR Gram-negative pathogens, including Enterobacterales and Pseudomonas aeruginosa producing ESBL, KPC, and MBL [59]. The combination has shown efficacy as salvage therapy in compassionate use cases involving extensively drug-resistant (XDR) Pseudomonas aeruginosa producing NDM carbapenemase [59]. A phase 3 clinical trial for cUTI is currently nearing completion [59].
Imipenem/Cilastatin/Funobactam
Imipenem/cilastatin/funobactam adds a novel non-β-lactam β-lactamase inhibitor to a established carbapenem combination [59]. Funobactam demonstrates broad inhibitory activity against Ambler Class A, C, and D serine β-lactamases, including KPC and OXA-48-like enzymes [59]. This combination is being developed to address carbapenem-resistant infections, particularly those mediated by serine carbapenemases, and is currently in phase 3 trials for HAP/VAP and cUTI [59].
Experimental Approaches for Resistance Mechanism Investigation
Phenotypic Detection of β-Lactamase Production
Double Disk Synergy Test (DDST) for ESBL Detection: This phenotypic method detects ESBL production by demonstrating synergy between a β-lactam antibiotic and clavulanic acid [62].
- Prepare a 0.5 McFarland standard suspension of the test isolate.
- Inoculate Mueller-Hinton agar (MHA) plates uniformly using a sterile swab.
- Place disks containing ceftazidime (30 µg) and ceftazidime/clavulanic acid (30/10 µg) 24 mm apart (center to center).
- Incubate plates at 37°C for 16-18 hours.
- Interpret as ESBL-positive if the inhibition zone around ceftazidime/clavulanic acid is ≥5 mm larger than around ceftazidime alone [62].
Modified Carbapenem Inactivation Method (mCIM) for Carbapenemase Detection: This test detects carbapenemase production through enzymatic inactivation of a meropenem disk [62].
- Emulsify a 1 µL loopful of test bacteria in 2 mL tryptic soy broth (TSB).
- Add a 10 µg meropenem disk to the broth and incubate at 37°C for 4 hours.
- Remove the disk and place it on an MHA plate seeded with E. coli ATCC 25922 (0.5 McFarland standard).
- Incubate at 37°C for 18-24 hours.
- Interpret as carbapenemase-positive if the inhibition zone diameter is ≤15 mm; ≥19 mm indicates no carbapenemase activity [62].
EDTA-modified Carbapenem Inactivation Method (eCIM) for MBL Detection: This method differentiates MBLs from other carbapenemases using the metal chelator EDTA [62].
- Repeat mCIM procedure, adding parallel TSB tubes with and without EDTA.
- Compare inhibition zones between mCIM (without EDTA) and eCIM (with EDTA).
- An increase in zone diameter of ≥5 mm with EDTA suggests MBL production [62].
Molecular Characterization of Resistance Genes
PCR Amplification and Sequencing:
- Extract bacterial DNA using commercial kits or boiling preparation.
- Perform PCR amplification with primers specific for target β-lactamase genes (e.g., blaCTX-M, blaNDM, blaKPC, blaOXA-48, blaVIM).
- Visualize PCR products using gel electrophoresis.
- Sequence amplified products and analyze sequences against reference databases (e.g., NCBI, CARD).
- Correlate genotypic findings with phenotypic resistance profiles [62].
Figure 1: Experimental Workflow for Characterizing Bacterial Resistance Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for BL/BLI Resistance Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Culture Media | Mueller-Hinton Agar (MHA), Cation-adjusted MHB, CLED Agar | Standardized antimicrobial susceptibility testing (AST) and bacterial cultivation |
| β-Lactamase Inhibitors | Clavulanic acid, avibactam, relebactam, vaborbactam, taniborbactam | Inhibition profiling and synergy studies with β-lactam antibiotics |
| Antibiotic disks | Ceftazidime, meropenem, cefepime, aztreonam, with/without inhibitors | Phenotypic detection of resistance mechanisms (DDST, mCIM) |
| Molecular Biology Reagents | PCR primers for blaCTX-M, blaNDM, blaKPC, blaOXA-48; DNA extraction kits; Sequencing reagents | Genotypic characterization of resistance determinants |
| Reference Strains | E. coli ATCC 25922, K. pneumoniae ATCC 700603, K. pneumoniae ATCC BAA-1705 (positive control), BAA-1706 (negative control) | Quality control for phenotypic and genotypic assays |
| Efflux Pump Inhibitors | Phe-Arg-β-naphthylamide (PAβN), carbonyl cyanide m-chlorophenyl hydrazone (CCCP) | Investigation of efflux-mediated resistance mechanisms |
Emerging Resistance and Future Challenges
Despite these therapeutic advances, the relentless evolution of bacterial resistance continues to present substantial challenges. The emergence of resistance to novel BL/BLI combinations has already been documented, often mediated by mutations affecting RND-type efflux pump systems and their regulatory networks [61]. In Pseudomonas aeruginosa, mutations leading to overexpression of the MexAB-OprM efflux system contribute to resistance against ceftazidime-avibactam (CZA) and ceftolozane-tazobactam (C/T) [61]. Similarly, mutations in other RND pumps like MexVW and MexMN have been associated with reduced susceptibility to these newer agents [61]. The global dissemination of metallo-β-lactamases (MBLs), particularly NDM, VIM, and IMP variants, continues to escalate, threatening the efficacy of all β-lactam antibiotics except monobactams [60]. Furthermore, the co-carriage of multiple resistance genes on mobile genetic elements facilitates the rapid horizontal transfer of resistance determinants among bacterial populations, as evidenced by the simultaneous presence of blaVIM and blaNDM genes in 5.3% of MBL isolates in recent surveillance [62].
Figure 2: Mechanism of β-Lactamase Inhibition Protecting Antibiotic Activity
The strategic development of novel β-lactam/β-lactamase inhibitor combinations represents a critical advancement in the ongoing battle against antimicrobial resistance in Gram-negative pathogens. The recent approvals of cefepime/enmetazobactam, aztreonam/avibactam, and sulbactam/durlobactam, coupled with promising agents in late-stage clinical development like cefepime/taniborbactam and cefepime/zidebactam, provide renewed hope for treating infections caused by multidrug-resistant organisms. However, the persistent emergence of resistance mechanisms, particularly involving efflux pump overexpression and metallo-β-lactamase dissemination, underscores the imperative for continued research, vigilant surveillance, and innovative drug development. Future strategies must incorporate enhanced understanding of resistance dynamics, exploration of non-traditional antimicrobial approaches, and implementation of comprehensive antimicrobial stewardship programs to preserve the efficacy of these invaluable therapeutic agents.
The formidable defense systems of Gram-negative bacteria pose a significant challenge in antimicrobial therapy. Their complex, multi-layered cell envelope, consisting of an inner membrane, a thin peptidoglycan layer, and a distinctive outer membrane, creates a formidable permeability barrier [9]. This outer membrane is structurally asymmetric, with an inner leaflet composed of phospholipids and an outer leaflet composed of lipopolysaccharides (LPS), and is dispersed with integral proteins such as β-barrel outer membrane proteins (OMPs) and lipoproteins [9]. This structure acts as a highly effective barrier, preventing the entry of many harmful compounds, including antibiotics.
Compounding this intrinsic physical barrier, Gram-negative bacteria have evolved sophisticated active mechanisms to evade antimicrobial killing. Multidrug-resistant (MDR) Gram-negative pathogens, particularly the ESKAPE pathogens classified as priority by the World Health Organization, represent one of the most urgent global healthcare threats [9]. The World Health Organization (WHO) continues to highlight the gravity of the situation, noting that the antibacterial pipeline is both scarce and lacking in innovation [33]. The escalation of antimicrobial resistance (AMR) underscores the critical need for innovative strategies that bypass these bacterial barriers, including novel antibiotic delivery methods and the inhibition of efflux systems [9].
The Clinical and Pipeline Landscape of AMR
The Burden of Resistance
Antimicrobial resistance is a growing global threat, undermining the effectiveness of life-saving treatments. The Centers for Disease Control and Prevention (CDC) reports that in the United States alone, more than 2.8 million antimicrobial-resistant infections occur each year, resulting in more than 35,000 deaths [63]. Globally, the WHO's GLASS report provides a stark analysis from over 23 million confirmed infections, indicating widespread resistance [26]. The economic burden is equally massive, with the cost to treat infections from just six frequent antimicrobial-resistant germs in the U.S. estimated at over $4.6 billion annually [63].
Analysis of the Current Antibacterial Pipeline
The development of new antibacterial agents is not keeping pace with the spread of resistance. According to a 2025 WHO analysis, the number of antibacterials in the clinical pipeline has decreased from 97 in 2023 to 90 in 2025 [33]. This pipeline faces a dual crisis of scarcity and lack of innovation.
Table: Analysis of the Antibacterial Clinical Pipeline (2025 WHO Data)
| Pipeline Metric | Number/Description | Implication |
|---|---|---|
| Total Clinical Agents | 90 | Decrease from 97 in 2023 |
| Traditional Antibacterial Agents | 50 | Focus on modifying existing scaffolds |
| Non-traditional Agents | 40 | Includes bacteriophages, antibodies, microbiome modulators |
| Innovative Agents | 15 | Only a fraction of the total pipeline |
| Agents for WHO "Critical" Pathogens | 5 | Highest unmet need for pathogens like CRAB and CRE |
The preclinical pipeline, with 232 programs across 148 groups worldwide, offers some hope, but its fragility is highlighted by the fact that 90% of the companies involved are small firms with fewer than 50 employees [33]. This underscores the economic hurdles in antibiotic development, where short-duration therapies often yield a limited return on investment compared to chronic disease treatments [64].
Efflux Pumps: A Major Multidrug Resistance Mechanism
Efflux Pump Families and Physiological Roles
Multidrug efflux pumps are inner membrane transporters that actively export a wide range of structurally unrelated antibiotics from the cell, thereby reducing intracellular drug accumulation and conferring resistance [65]. It is crucial to recognize that these pumps predate the clinical use of antibiotics and play vital roles in bacterial physiology, including in pathogenicity, metabolism, and relieving cellular stress [66]. Their primary function is not solely antibiotic extrusion; they are involved in regulating nutrient and heavy metal levels and expelling toxins like bile [66].
In Gram-negative bacteria, these pumps are often organized into multi-component complexes that span the entire cell envelope. Based on their structure and energy coupling mechanism, they are classified into several families [65] [66]:
- RND (Resistance-Nodulation-Division): Clinically the most significant in Gram-negative bacteria. These are tripartite complexes (e.g., AcrAB-TolC in E. coli, AdeABC in A. baumannii) that use the proton motive force to export substrates.
- MFS (Major Facilitator Superfamily): The largest and most diverse superfamily of secondary transporters.
- ABC (ATP-Binding Cassette): Utilize energy from ATP hydrolysis to drive transport (e.g., MacAB in Salmonella).
- MATE (Multidrug and Toxic Compound Extrusion): Exchange cations like H+ or Na+ for drug substrates.
- SMR (Small Multidrug Resistance): Small proteins that typically efflux amphipathic cations.
- PACE (Proteobacterial Antimicrobial Compound Efflux): A relatively newly identified family involved in efflux of biocides.
The following diagram illustrates the structure and functional mechanism of a typical RND-type efflux pump, the most clinically relevant system in Gram-negative bacteria.
Diagram: Tripartite RND Efflux Pump Mechanism. The pump complex spans the inner membrane (IM), periplasm, and outer membrane (OM) of Gram-negative bacteria. The RND transporter uses proton motive force (H+ influx) to bind and propel antibiotics from the periplasm and cytoplasm through the Membrane Fusion Protein (MFP) and out of the cell via the Outer Membrane Protein (OMP).
Efflux-Mediated Resistance in Key Pathogens
In pathogens like Acinetobacter baumannii, the overexpression of chromosomally encoded efflux pumps is a major contributor to multidrug resistance. The RND family pumps, in particular, are frequently implicated in clinical resistance.
Table: Major RND Efflux Pumps in Acinetobacter baumannii and Their Substrates
| Efflux Pump | Regulator(s) | Key Antibiotic Substrates | Additional Substrates |
|---|---|---|---|
| AdeABC | AdeRS, BaeSR | Aminoglycosides, Fluoroquinolones, β-lactams, Tetracyclines, Tigecycline* | Chloramphenicol, Erythromycin, Trimethoprim, Benzalkonium chloride, SDS [66] |
| AdeFGH | AdeL, ddrR, abaI | Trimethoprim, Chloramphenicol, Clindamycin, Tetracycline-Tigecycline, Sulfonamides, Fluoroquinolones | EtBr, SDS, Safranin O, Acridine orange [66] |
| AdeIJK | AdeN, BaeSR | β-lactams (Meropenem, Imipenem), Tetracyclines, Cephalosporins, Fluoroquinolones | Chloramphenicol, Rifampin, Fusidic acid, Erythromycin, Lincosamides, Novobiocin [66] |
| AdeDE | Unknown | Meropenem, Erythromycin, Chloramphenicol, Ceftazidime, Tetracycline, Amikacin, Ciprofloxacin | EtBr, Rifampin [66] |
Innovative Strategies to Overcome Efflux and Barriers
Efflux Pump Inhibitors (EPIs) as Therapeutic Adjuvants
A promising strategy to overcome multidrug resistance is the use of efflux pump inhibitors (EPIs), small molecules that block the function of MDR efflux pumps [67]. By inhibiting these pumps, EPIs can resensitize bacteria to existing conventional antibiotics, effectively restoring their efficacy. The discovery of EPIs involves a range of approaches, from high-throughput screening (HTS) of compound libraries to bioassay-guided purification of natural products [67]. The co-crystal structural analysis of multidrug efflux pumps like AcrB and MexB has been instrumental in revealing the drug recognition, export, and inhibitory mechanisms, providing a rational basis for EPI design [65].
The development of EPIs must account for the complexity of efflux systems. For instance, RND pumps have proximal and distal binding pockets with broad substrate specificity, and inhibitors can act as competitive, uncompetitive, or non-competitive blockers [67] [65]. Furthermore, because efflux pumps have physiological roles, their complete inhibition could potentially impact bacterial viability or pathogenicity, adding another layer to their therapeutic potential [66] [65].
Novel Antibiotics with Innovative Mechanisms
Beyond inhibiting efflux pumps, another strategy is to develop entirely new classes of antibiotics that bypass the classic resistance pathways. A landmark example is zosurabalpin, the first new antibiotic class in over 50 years developed to tackle CRAB [64]. Zosurabalpin represents a breakthrough in innovation, as it acts through a novel mechanism. Rather than targeting traditional intracellular processes, it inhibits the LptB2FGC complex, a protein complex responsible for transporting lipopolysaccharide (LPS) from the inner membrane to the outer membrane [64]. By hindering this transport, zosurabalpin prevents the formation of the critical LPS-containing outer membrane, which is essential for the bacterium's survival. This mechanism is visually summarized below.
Diagram: Novel Mechanism of Zosurabalpin. Zosurabalpin inhibits the LptB2FGC complex, which is responsible for transporting lipopolysaccharide (LPS) to the outer membrane. This disruption prevents proper biogenesis of the outer membrane, leading to bacterial cell death.
This approach is particularly innovative because it targets a key component of the Gram-negative cell envelope itself—the very structure that confers intrinsic resistance. Zosurabalpin has demonstrated effectiveness in preclinical models and has progressed to phase 3 clinical trials, highlighting the potential of targeting non-traditional, barrier-related pathways [64].
The Scientist's Toolkit: Research Reagent Solutions
Research into efflux pump inhibition and novel antibiotic mechanisms relies on a suite of specialized reagents and methodologies. The table below details key tools and their applications for researchers in this field.
Table: Essential Research Reagents and Methods for Efflux Pump Studies
| Reagent / Method | Function / Application | Specific Examples / Notes |
|---|---|---|
| Genetically Modified Efflux Mutants | Used to identify pump substrates and quantify their contribution to resistance by comparing susceptibility between wild-type and mutant strains [67]. | P. aeruginosa MES mutants; E. coli ΔacrB; A. baumannii ΔadeB [67] [66]. |
| Fluorescent Efflux Substrates | Enable real-time, quantitative measurement of efflux pump activity via accumulation assays. Commonly used in high-throughput screening (HTS) for EPIs [67]. | Ethidium Bromide (EtBr), Berberine; accumulation increases in the presence of a functional EPI [67] [66]. |
| Broth Microdilution Checkerboard Assay | Standard method to determine the Minimum Inhibitory Concentration (MIC) of an antibiotic in combination with an EPI, assessing synergistic activity [38]. | Used to confirm that an EPI lowers the MIC of a known antibiotic substrate [66]. |
| Molecular Modeling & Crystallography | Reveals the structural basis of substrate recognition and inhibition, guiding rational drug design of novel EPIs and antibiotics [67] [65]. | Crystal structures of AcrB/MexB (RND), EmrD (MFS), and MacB (ABC) inform binding site analysis [67] [65]. |
| CLSI-Endorsed Combination Testing | Standardized phenotypic tests for evaluating the efficacy of antibiotic-inhibitor combinations against specific resistance mechanisms [38]. | Broth disk elution method for ceftazidime-avibactam + aztreonam vs. MBL-producing Enterobacterales [38]. |
The fight against antimicrobial resistance in Gram-negative bacteria necessitates a paradigm shift from traditional antibiotic discovery toward innovative strategies that directly target the pathogen's defensive barriers. As highlighted by the WHO, the current pipeline is insufficient, underscoring the urgency of these approaches [33]. The dual strategy of inhibiting efflux pumps with EPIs to resurrect existing antibiotics, coupled with the development of novel agents like zosurabalpin that disrupt the integrity of the cell envelope, represents the vanguard of this effort. These innovative approaches, firmly rooted in a deep understanding of bacterial physiology and resistance mechanisms, offer a promising path forward in overcoming the formidable defenses of Gram-negative pathogens and mitigating the global AMR crisis.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most severe threats to modern medicine, with drug-resistant infections causing approximately 1.3 million deaths globally each year [38]. Gram-negative bacteria pose a particularly formidable challenge due to their complex cell envelope architecture, characterized by an outer membrane containing lipopolysaccharide, which confers low permeability and intrinsic resistance to many antimicrobial agents [68] [69]. This crisis is exacerbated by the limited pipeline of new antibiotics—only 13 new antibiotics were approved between 2017 and 2023, with just two meeting at least one of the World Health Organization's innovation criteria [70]. Consequently, the exploration of non-traditional antimicrobial approaches has become a research imperative. This technical guide examines three promising alternative therapeutic strategies—bacteriophages, quorum sensing inhibitors, and antimicrobial peptides—within the context of AMR mechanisms in Gram-negative pathogens, providing detailed methodologies and analytical frameworks for research and development professionals.
Bacteriophage Therapy: Harnessing Viral Predation
Mechanisms of Action and Therapeutic Potential
Bacteriophages (phages) are viruses that specifically infect and replicate within bacteria, employing two primary life cycles: lytic and lysogenic. Lytic phages are of principal therapeutic interest due to their bactericidal activity, which culminates in host cell lysis and the release of progeny virions [71]. The lytic process involves a sequence of molecular events: receptor recognition and attachment, genomic injection, hijacking of bacterial biosynthesis machinery, assembly of new virions, and ultimately, cell lysis mediated by holins (membrane pore-forming proteins), endolysins (peptidoglycan-degrading enzymes), and spanins (which fuse the inner and outer membranes in Gram-negative bacteria) [68].
The therapeutic application of phages offers several advantages over conventional antibiotics, including high target specificity that preserves commensal microbiota, self-amplification at infection sites, and efficacy against multidrug-resistant (MDR) pathogens [72] [68]. Phages can penetrate and disrupt bacterial biofilms, a significant contributor to treatment failure in device-related and chronic infections, through the production of depolymerases that degrade the extracellular polymeric matrix [72].
Experimental Protocols and Assessment Methods
Phage Isolation and Characterization:
- Isolation from Environmental Samples: Collect water, soil, or sewage samples. Enrich by incubating with the target bacterial strain (e.g., Pseudomonas aeruginosa, Acinetobacter baumannii) in nutrient broth for 6-18 hours. Remove debris by centrifugation (10,000 × g, 10 min) and filter through 0.22-μm membrane [68].
- Plaque Assay: Serially dilute phage lysate in SM buffer. Mix with soft agar (0.7%) containing the bacterial host and pour onto nutrient agar plates. Incubate overnight at 37°C. Count plaque-forming units (PFU) to determine titer [72].
- Host Range Determination: Spot phage lysate onto lawns of different bacterial strains. Assess efficiency of plating (EOP) by comparing plaque formation to that on the isolation host. EOP >0.5 is considered high, 0.1-0.5 intermediate, and <0.1 low [71].
- Phage-Antibiotic Synergy (PAS) Testing: Conduct time-kill assays comparing bacterial reduction with phage alone, antibiotic alone, and their combination. A >2-log10 reduction in the combination compared to the most effective single agent indicates synergy [72]. Test sub-inhibitory concentrations of antibiotics (1/4-1/8 × MIC) for their effect on plaque size and phage burst size [72].
Quantitative Assessment of Bacteriophage Therapy
Table 1: In Vivo Efficacy of Bacteriophage Therapy Against Gram-Negative Pneumonia
| Pathogen | Animal Model | Administration Route | Bacterial Reduction (log₁₀ CFU) | Survival Benefit | Key Findings | Citation |
|---|---|---|---|---|---|---|
| A. baumannii | Mouse pneumonia | Intranasal (IN) | >2-log reduction by day 1; clearance by day 3 | MOI=10: 100%; MOI=1: 60% | Mild histopathology in treated vs. severe in untreated | [68] |
| P. aeruginosa | Mouse lung infection | IN | 3.5-log reduction in lungs at 24h | 92% survival at 5 days | Reduced TNF-α and IL-6 levels | [68] |
| K. pneumoniae | Mouse pneumonia | IN | 4-log reduction in lungs at 6h | 100% survival at 7 days | Phage titers increased then cleared as bacteria eliminated | [68] |
Table 2: Phage-Antibiotic Synergy (PAS) Combinations Against Gram-Negative Pathogens
| Bacterial Pathogen | Phage | Antibiotic | Synergy Mechanism | Efficacy Enhancement | Citation |
|---|---|---|---|---|---|
| P. aeruginosa | Siphoviridae phage σ-1 | Ceftriaxone (sub-MIC) | Cell filamentation | Increased plaque size and burst size | [72] |
| Burkholderia cepacia | Not specified | Meropenem (low-dose) | Not specified | Increased Galleria mellonella survival | [72] |
| Citrobacter amalonaticus | Phage MRM57 | Carbenicillin, Colistin (1/10×MIC) | Multiple | Synergy with 7/8 antibiotics tested | [72] |
Quorum Sensing Inhibitors: Disrupting Bacterial Communication
Molecular Mechanisms of Quorum Sensing Inhibition
Quorum sensing (QS) is a cell-density-dependent communication system that enables bacteria to coordinate gene expression collectively, regulating processes including virulence factor production, biofilm formation, sporulation, and antibiotic resistance [73]. In Gram-negative bacteria, QS typically employs acyl-homoserine lactones (AHLs) as signaling molecules, which are synthesized by LuxI-type synthases and detected by LuxR-type transcriptional regulators [73].
Quorum sensing inhibitors (QSIs) interfere with this communication system through several mechanistic approaches: (1) inhibition of AHL synthesis through competitive inhibition of LuxI-type synthases; (2) degradation of AHL signals via lactonases, acylases, or oxidoreductases (a process known as quorum quenching); (3) competitive antagonism of LuxR-type receptors by AHL analogs; and (4) interference with downstream signal transduction [73]. By disrupting QS, these compounds attenuate bacterial virulence without exerting direct bactericidal pressure, potentially reducing the selection for resistance.
Experimental Protocols for QSI Evaluation
QS Inhibition Assays:
- AHL Reporter Strain Assay: Utilize engineered biosensor strains (e.g., Chromobacterium violaceum for violacein production, Agrobacterium tumefaciens with traG::lacZ fusion) [73]. Grow reporter strain with sub-MIC concentrations of test QSI with or without exogenous AHLs. Measure pigment production or β-galactosidase activity spectrophotometrically.
- Virulence Factor Quantification: Culture target pathogens (e.g., P. aeruginosa) with sub-inhibitory QSI concentrations. Assess protease production using azocasein hydrolysis assay (absorbance at 440nm), pyocyanin extraction with chloroform and acidification (absorbance at 520nm), and rhamnolipid quantification using the orcinol method [73].
- Biofilm Inhibition Assay: Grow biofilms in 96-well plates with sub-MIC QSI concentrations. Stain with crystal violet (0.1%), solubilize with ethanol-acetate (80:20), and measure absorbance at 590nm. Visualize architecture by scanning electron microscopy or confocal laser scanning microscopy with LIVE/DEAD staining [73].
- Gene Expression Analysis: Extract RNA from QSI-treated and control cultures. Perform RT-qPCR for QS-regulated genes (e.g., lasA, lasB, rhIA in P. aeruginosa). Use housekeeping genes (e.g., rpoD) for normalization [73].
Quorum Sensing Systems in Gram-Negative Pathogens
Table 3: Quorum Sensing Systems in Clinically Relevant Gram-Negative Bacteria
| Microorganism | QS System | Signaling Molecules | Regulated Phenotypes | Potential QSI Targets | Citation |
|---|---|---|---|---|---|
| P. aeruginosa | Las, Rhl, PQS, IQS | 3OC12-HSL, C4-HSL, PQS | Elastase, protease, rhamnolipids, pyocyanin, biofilm, motility | LasI, LasR, RhlI, RhlR, PqsR | [73] |
| A. baumannii | Lux, abaI/abaR | 3OHC12-HSL | Biofilm formation, motility, morphology | AbaI, AbaR | [73] |
| E. coli | SdiA | Unknown (detects AHLs) | Biofilm formation, motility | SdiA | [73] |
| V. fischeri | LuxI, Ain, LuxS | 3OC6-HSL | Bioluminescence, host colonization | LuxI, LuxR | [73] |
Antimicrobial Peptides and Nanotechnology Approaches
Mechanisms of Action and Resistance
Antimicrobial peptides (AMPs) are small, cationic amphipathic peptides that function as crucial components of innate immunity across all kingdoms of life [74]. Their mechanism of action primarily involves electrostatic interactions with the anionic components of the bacterial outer membrane (e.g., lipopolysaccharide), leading to membrane disruption through various models including the "barrel-stave," "carpet," or "toroidal-pore" mechanisms [74] [75]. Following membrane permeabilization, AMPs may also have intracellular targets such as inhibition of DNA, RNA, or protein synthesis.
Gram-negative bacteria have evolved multiple resistance mechanisms against AMPs, including: (1) modification of membrane lipids to reduce net negative charge (e.g., with phosphoethanolamine by MCR enzymes); (2) production of proteases that degrade AMPs; (3) upregulation of efflux pumps; and (4) formation of protective capsules [74] [69]. The mobilizable colistin resistance (MCR) genes, particularly mcr-9 and mcr-10 variants, represent a significant concern as they are plasmid-borne and can transfer between bacterial species [69].
Nano-Formulation Strategies and Assessment
Nanocarrier Synthesis and AMP Loading:
- Liposome Preparation: Use thin-film hydration method with phospholipids (e.g., DPPC, DSPC) and cholesterol (70:30 molar ratio). Hydrate with AMP solution and extrude through polycarbonate membranes (100-400nm). Determine encapsulation efficiency using ultracentrifugation and HPLC analysis [75].
- Polymeric Nanoparticle Formulation: Prepare PLGA nanoparticles using double emulsion (W/O/W) technique. Dissolve PLGA in dichloromethane, add AMP solution, and emulsify by sonication. Pour into PVA solution and stir overnight to evaporate solvent. Characterize size by dynamic light scattering, zeta potential by electrophoretic mobility, and morphology by TEM [75].
- Antimicrobial Susceptibility Testing: Determine MIC and MBC using broth microdilution according to CLSI guidelines. Assess membrane disruption using SYTOX Green uptake assay (fluorescence upon DNA binding) and diSC3-5 assay (membrane depolarization) [74] [75].
- Hemolysis Assay: Incubate AMP formulations with erythrocyte suspension (2% in PBS) at 37°C for 1h. Measure hemoglobin release at 540nm. Calculate hemolysis percentage relative to Triton X-100 (100%) and PBS (0%) controls. Select compounds with <10% hemolysis at 2× MIC [75].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Alternative Antimicrobial Therapies
| Reagent/Category | Specific Examples | Research Application | Key Considerations | Citation |
|---|---|---|---|---|
| Reporter Strains | C. violaceum CV026, A. tumefaciens A136 | QSI screening and validation | Monitor pigment production (violacein) or β-galactosidase activity | [73] |
| Animal Infection Models | Mouse pneumonia, neutropenic thigh, burn wound | In vivo therapeutic efficacy | Immunocompetent vs. immunosuppressed models; route of administration | [68] |
| Biofilm Assessment | Calgary biofilm device, flow cells, crystal violet | Anti-biofilm activity quantification | Combine with confocal microscopy for structural analysis | [73] |
| Membrane Integrity Probes | SYTOX Green, diSC3-5, NPN | AMP mechanism of action | Differentiate between membrane depolarization and permeabilization | [74] |
| Chromatography-Mass Spectrometry | LC-MS/MS, GC-MS | AHL quantification and identification | Requires authentic AHL standards for quantification | [73] |
| Genetic Tools | CRISPR-Cas, knockout mutants, qPCR arrays | Resistance mechanism studies | Enable targeted gene deletion or expression modulation | [69] |
The escalating crisis of antimicrobial resistance necessitates a paradigm shift in our therapeutic approaches to Gram-negative infections. Bacteriophages, quorum sensing inhibitors, and antimicrobial peptides represent three distinct but complementary strategies that operate through mechanisms fundamentally different from conventional antibiotics. The experimental frameworks outlined in this technical guide provide foundational methodologies for advancing research in these innovative antimicrobial approaches.
Future development will likely focus on combination therapies that leverage synergistic interactions between these modalities and conventional antibiotics, such as the observed phage-antibiotic synergy that can enhance bacterial eradication and suppress resistance emergence [72] [71]. Additionally, nanotechnology approaches offer promising strategies to overcome delivery challenges, particularly for AMPs, by protecting them from proteolytic degradation and improving target site accumulation [75]. The integration of artificial intelligence and machine learning in compound screening and design will further accelerate the identification of novel therapeutic candidates with activity against multidrug-resistant Gram-negative pathogens [70] [69].
As these alternative therapies progress through development pipelines, considerations of formulation, delivery, resistance monitoring, and regulatory pathways will be critical for successful clinical translation. The innovative approaches detailed herein offer promising avenues for addressing the mounting threat of antimicrobial resistance and safeguarding our future therapeutic arsenal.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most severe threats to global public health, with Gram-negative bacteria posing particularly formidable challenges due to their complex cell envelope structure and sophisticated resistance mechanisms. These pathogens are responsible for a significant proportion of nosocomial infections, including ventilator-associated pneumonia, catheter-related bloodstream infections, and urinary tract infections, especially in immunocompromised patients [31]. The World Health Organization (WHO) has classified multiple Gram-negative bacteria as priority pathogens, with carbapenem-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacteriaceae designated as critical priorities requiring urgent research and development of new antibiotics [1]. The economic burden is staggering, with treating resistant infections adding up to $29,000 per patient in hospitals and the global economy facing potential costs of $1 trillion annually [76].
Despite this urgent need, the antibiotic development pipeline has significantly dwindled, creating a dangerous therapeutic void. Major pharmaceutical companies have largely exited antibiotic research and development due to scientific challenges and lack of economic viability [76] [77]. This review examines the complex interplay between Gram-negative bacterial resistance mechanisms, the economic barriers to antibiotic development, and the push/pull incentives and regulatory strategies being implemented to revitalize the antimicrobial pipeline and address this global health emergency.
Resistance Mechanisms in Gram-Negative Bacteria
Structural Defense Systems
Gram-negative bacteria possess a unique multi-layered cell envelope that functions as a formidable permeability barrier against antibiotics. This envelope consists of three primary components: an outer membrane (OM) containing lipopolysaccharides (LPS) and porin proteins, a thin peptidoglycan layer, and an inner cytoplasmic membrane (IM) [1] [31]. The asymmetric outer membrane, with its lipopolysaccharide-rich outer leaflet, serves as the first line of defense, restricting antibiotic penetration and differentiating Gram-negative from Gram-positive bacteria [1].
Porins, which are β-barrel proteins dispersed throughout the outer membrane, modulate the entry of hydrophilic antibiotics and nutrients. Bacteria can remodel these porins or acquire mutations to further limit antibiotic influx [1] [31]. This structural complexity means that even after an antibiotic successfully penetrates the cell envelope, Gram-negative bacteria can employ additional resistance mechanisms, including enzymatic inactivation, efflux pumps, and target site modification [1].
Molecular Resistance Strategies
Gram-negative bacteria utilize four primary molecular strategies to circumvent antibiotic activity:
- Enzymatic inactivation or modification: Production of antibiotic-inactivating enzymes such as extended-spectrum β-lactamases (ESBLs), AmpC β-lactamases, and carbapenemases (KPC, NDM, VIM, OXA-48) that hydrolyze β-lactam antibiotics [1] [31].
- Enhanced efflux pump activity: Overexpression of efflux systems (e.g., MexAB-OprM in P. aeruginosa, AcrAB-TolC in E. coli) that actively export antibiotics from the cell, reducing intracellular concentrations [1].
- Target site modification: Genetic mutations that alter antibiotic binding sites, such as modifications to penicillin-binding proteins (PBPs), DNA gyrase, or topoisomerase IV [1].
- Membrane permeability reduction: Modifications to lipopolysaccharide structure or porin expression that limit antibiotic penetration [31].
The genetic flexibility of Gram-negative bacteria, facilitated by horizontal gene transfer through conjugation, transformation, and transduction, allows rapid dissemination of resistance genes across species and genera, accelerating the emergence of multidrug-resistant (MDR) strains [1].
The Dwindling Antibiotic Pipeline: Economic and Scientific Challenges
Market Failures in Antibiotic Development
The economic model for antibiotic development is fundamentally broken, creating what has been termed an "antibiotic discovery void" since 1987 [76]. Unlike medications for chronic conditions, antibiotics are typically prescribed for short durations, resulting in limited revenue potential despite similar development costs. The mean cost for developing a systemic anti-infective is approximately $1.3 billion, matching the average across all drug classes, yet the commercial returns are substantially lower [77].
Table 1: Economic Challenges in Antibiotic Development
| Challenge | Impact | Reference |
|---|---|---|
| Low revenue potential | Average sales of $240M total in first 8 years vs. $300M annually needed for sustainability | [77] |
| High development costs | Mean cost of $1.3B for systemic anti-infectives | [77] |
| Post-approval expenses | Additional $240-622M over 5 years for commercialization | [77] |
| Clinical trial challenges | Cost of ~$1M per patient for CRE trials due to enrollment difficulties | [77] |
| Limited investment | Only 3,000 AMR researchers active globally | [77] |
The exit of major pharmaceutical companies from antibacterial R&D has been precipitous. Since the 1990s, 18 major pharmaceutical companies have abandoned the field, with Pfizer, AstraZeneca, Novartis, Sanofi, and Allergan among those who have departed since 2011 [76] [77]. This corporate exodus has resulted in a devastating "brain drain" of specialized expertise, with only approximately 3,000 AMR researchers currently active worldwide [77].
Scientific and Regulatory Hurdles
The scientific challenges in developing antibiotics against Gram-negative pathogens are substantial. The impermeable outer membrane and efficient efflux systems create significant hurdles for compound penetration and retention [1] [31]. Additionally, the rapid evolutionary capacity of bacteria means resistance can emerge during clinical trials or even within individual patients during treatment [77].
Clinical development faces practical obstacles, including difficulties in patient enrollment for infections caused by resistant pathogens. The Achaogen trial for plazomicin against carbapenem-resistant Enterobacteriaceae (CRE) exemplifies this challenge, with the study halted prematurely after enrolling only 39 of 2000 screened patients at an estimated cost of $1 million per recruited patient [77]. Regulatory requirements for non-inferiority trials often necessitate large sample sizes across multiple sites, further increasing costs and complexity [77].
Push and Pull Incentives: Revitalizing the Antibiotic Pipeline
Push Funding Mechanisms
Push incentives focus on reducing early-stage R&D costs through direct funding, research grants, and public-private partnerships. These mechanisms aim to de-risk the discovery and development phases, encouraging biotech companies and academic researchers to pursue antibacterial innovation.
Notable push initiatives include:
- CARB-X: Combats antimicrobial resistance by accelerating global antibacterial innovation, providing funding and support from early discovery through phase 1 clinical trials [77].
- Global AMR Fund: A partnership that invests in companies developing innovative antimicrobial treatments and diagnostics [78].
- Public-private partnerships: Collaborative models that share resources, expertise, and risk between public institutions and private companies [76].
These push mechanisms have helped maintain some level of innovation in the antibacterial pipeline. As of 2023, the pipeline included 97 antibacterial agents, with 57 traditional antibiotics and 40 non-traditional therapies. However, only 12 of these agents meet at least one of WHO's innovation criteria, highlighting continued limitations in truly novel approaches [76].
Pull Incentive Models
Pull incentives create guaranteed markets or revenue streams for successfully developed antibiotics, ensuring economic viability upon approval. These mechanisms are critical for attracting renewed investment to the field.
Table 2: Pull Incentive Models and Implementation Status
| Model Type | Key Features | Implementation Examples |
|---|---|---|
| Subscription ("Netflix") Model | Upfront payment for antibiotic access regardless of volume used | UK (pioneered), Italy, under discussion in US, Canada, Australia |
| Revenue Guarantees | Minimum annual revenue guaranteed to manufacturers | Analysis shows need for ~$300M/year per antibiotic |
| Market Entry Rewards | Significant financial reward upon regulatory approval | Proposed in various forms globally |
| Transferable Exclusivity Vouchers | Extends market exclusivity for another product | Proposed but not widely implemented |
Recent analyses of "fair share" contributions for pull incentives indicate that a global annual investment of $310 million (in 2024 USD) over 10 years would create an effective incentive [79]. Progress has been made in some countries, with the UK and Italy implementing subscription-style models. Analysis of two representative antibiotics (cefiderocol and ceftazidime-avibactam) shows that Italy has met its fair share target for both drugs, while the US has achieved this for ceftazidime-avibactam [79]. However, significant gaps remain in most countries, with the EU27 as a whole facing an $800 million gap [79].
Despite the demonstrated need, the current global pull investment would rank only #230 in global pharmaceutical revenue rankings, representing a modest investment relative to the threat [79]. The power of these pull mechanisms is particularly important in the early years following market introduction when sales revenues are typically insufficient to support commercialization costs [79].
Regulatory Strategies for Sustainable Antibiotic Use
Antimicrobial Stewardship and Controlled Access
Regulatory strategies are essential to preserve the efficacy of new antibiotics once developed. Evidence indicates that resistance tends to emerge rapidly following the introduction of new antibiotics, as demonstrated by ceftazidime-avibactam, where resistance was observed in 37.6% of E. coli isolates and 74.9% of K. pneumoniae isolates in India shortly after introduction [80].
To address this challenge, experts recommend restricting new antimicrobials in the Watch and Reserve categories to hospital formularies rather than retail pharmacies [80]. Hospitals seeking to procure these antimicrobials should be required to:
- Provide documentary evidence of compliance with infection prevention and control standards
- Maintain a functional antimicrobial stewardship (AMS) committee
- Periodically submit AMR surveillance data to national platforms
- Have in-house pharmacy services, clinical pharmacists, and diagnostic capacity [80]
This approach mirrors successful tuberculosis programs in India, where access to new TB drugs is restricted to registered DOTS-Plus centers, ensuring appropriate use and monitoring [80].
Global Regulatory Harmonization and Best Practices
International cooperation and harmonization of regulatory approaches are critical for effective AMR containment. Several countries have implemented innovative regulatory frameworks:
- Sweden's Strama programme: Combines real-time surveillance, professional and public engagement, and national targets through a bottom-up model that directly links prescribers with policymakers [80].
- Australia's National Antimicrobial Prescribing Survey: Emphasizes systematic auditing with detailed feedback to healthcare facilities, enabling data-driven interventions and informed national policy [80].
- China's Administrative Regulations for Clinical Use of Antibacterial Agents (2012): Classifies antibiotics into non-restricted, restricted, and special-grade categories, linking prescribing privileges to physicians' qualifications and institutional levels [80].
- Brazil's Health Regulatory Agency: Develops guidelines for implementing AMS programs in hospitals based on local needs and resources, while strengthening surveillance systems like BR-GLASS [80].
A survey of infectious disease experts identified diagnostic uncertainty (73.1%) and lack of antibiogram availability (51.9%) as key drivers of unnecessary antimicrobial use, highlighting areas for regulatory focus [80]. Nearly all participants (98.1%) advocated for a new antimicrobial regulatory policy to prevent misuse [80].
Experimental Approaches and Research Methodologies
Research Reagent Solutions for Gram-Negative Resistance Studies
Table 3: Essential Research Reagents for Antibiotic Resistance Studies
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| β-lactamase inhibitors | Antibiotic adjuvants that deactivate resistance mechanisms | Avibactam, vaborbactam, relebactam |
| Porin expression systems | Study membrane permeability and antibiotic transport | OmpF, OmpC, OprD porin models |
| Efflux pump inhibitors | Block antibiotic export systems | PAbN, DNP, novel synthetic inhibitors |
| Lipopolysaccharide modulators | Target outer membrane integrity | Polymyxin derivatives, novel LPS binders |
| Bacterial cytological profiling | Rapid mechanism of action determination | Fluorescent probes, membrane potential dyes |
| Genome editing tools | Genetic manipulation of resistance genes | CRISPR-Cas, recombinase systems |
| Membrane permeability assays | Quantify compound penetration | NPN uptake, ethidium bromide accumulation |
| MIC/MBC determination panels | Assess antibacterial activity and resistance | Broth microdilution, Etest, automated systems |
Key Experimental Protocols
Protocol 1: Assessment of Outer Membrane Permeability Using 1-N-Phenylnaphthylamine (NPN) NPN is a hydrophobic fluorescent probe excluded by intact outer membranes but incorporated into disrupted membranes. Log-phase bacteria are washed and resuspended in buffer with 10μM NPN. Fluorescence is measured (excitation 350nm, emission 420nm) before and after antibiotic exposure. Increased fluorescence indicates outer membrane disruption and enhanced permeability [31].
Protocol 2: Efflux Pump Inhibition Assay Bacterial strains are subjected to broth microdilution MIC testing with antibiotics alone and in combination with efflux pump inhibitors like phenylalanine-arginine β-naphthylamide (PAbN). A ≥4-fold reduction in MIC in the presence of the inhibitor indicates efflux pump activity contributing to resistance. Real-time efflux can be measured using ethidium bromide accumulation and extrusion assays with fluorometric detection [1] [31].
Protocol 3: β-Lactamase Inhibition Kinetics Purified β-lactamases are incubated with nitrocefin substrate alone or with inhibitor pre-incubation. Hydrolysis rates are measured spectrophotometrically at 482nm. IC50 values are determined from inhibitor dose-response curves. Second-order rate constants (k2/K) for inactivation are calculated from progress curves with varying inhibitor concentrations to assess inhibition potency [1].
Visualizing Incentive Structures and Resistance Pathways
Push and Pull Incentive Framework
Diagram 1: Integrated Push-Pull Incentive Cycle
Gram-Negative Resistance Mechanisms
Diagram 2: Gram-Negative Bacterial Resistance Mechanisms
The convergence of scientific innovation, economic incentives, and regulatory intelligence offers a path forward in addressing the antimicrobial resistance crisis, particularly for formidable Gram-negative pathogens. The complex structural and genetic resistance mechanisms of these bacteria necessitate continued scientific advancement, while the broken antibiotic market demands creative economic solutions.
The recent progress in implementing pull incentives, particularly in the UK and Italy, provides promising models for other nations. The upcoming UN General Assembly High-Level Meeting on AMR in 2024 presents a critical opportunity to build on this momentum, with leaders pledging to reduce AMR-associated deaths by 10% by 2030 and calling for catalytic funding of $100 million [76].
Success will require coordinated global action across multiple fronts: sustained investment in basic research, implementation of delinked pull incentives that guarantee sustainable markets for innovative antibiotics, and robust regulatory frameworks that ensure appropriate use and preserve efficacy. With Gram-negative bacteria continuing to evolve resistance even to last-resort antibiotics, the time for concerted action is now. By aligning scientific, economic, and regulatory strategies, we can reinvigorate the antibiotic pipeline and address one of the most pressing global health threats of our time.
Validating Solutions: Efficacy, Resistance Emergence, and Comparative Clinical Outcomes
The rise of multidrug-resistant (MDR) Gram-negative bacteria represents one of the most pressing challenges in modern infectious disease management and antimicrobial development. These pathogens, particularly the "Critical Priority" group defined by the World Health Organization—including carbapenem-resistant Enterobacterales (CRE), Pseudomonas aeruginosa (CR-Pa), and Acinetobacter baumannii (CRAB)—are associated with devastating mortality rates and dwindling therapeutic options [81] [82]. Resistance to last-resort carbapenems has necessitated the development of novel agents capable of overcoming sophisticated bacterial defense mechanisms, such as enzymatic inactivation (β-lactamases), reduced membrane permeability (porin loss), and active efflux [82]. In response, a new generation of antibiotics has emerged, including siderophore cephalosporins and innovative β-lactam/β-lactamase inhibitor (BL-BLI) combinations. This whitepaper provides a head-to-head comparison of three leading agents—cefiderocol, ceftazidime-avibactam, and sulbactam-durlobactam—synthesizing current evidence on their mechanisms, spectra of activity, and clinical efficacy to inform research and development strategies.
Comparative Mechanisms of Action and Resistance
Understanding the distinct mechanisms by which these agents overcome resistance is fundamental to predicting their efficacy and the potential for cross-resistance.
2.1 Cefiderocol: The "Trojan Horse" Siderophore Cephalosporin Cefiderocol is a novel siderophore cephalosporin that exploits bacterial iron-uptake systems. Its structure features a chlorocatechol group that chelates ferric iron, forming a complex actively transported across the outer membrane via TonB-dependent siderophore receptors. This "Trojan horse" strategy bypasses traditional porin pathways and efflux pumps. Once in the periplasm, the iron is reduced and released, allowing the cephalosporin core to bind to penicillin-binding protein 3 (PBP3) and inhibit cell wall synthesis [82] [83]. Its structure also confers stability against a broad range of β-lactamases, including AmpC, KPC, and some ESBLs [82].
Despite its innovative mechanism, resistance has been observed, primarily driven by:
- Mutations in Iron Transport: Loss-of-function mutations in siderophore receptors (e.g., cirA, fiuA) or associated genes (e.g., tonB, envZ) reduce drug influx [83] [84].
- β-Lactamase Production: Certain enzymes, notably metallo-β-lactamases (NDM, VIM), KPC variants (e.g., KPC-41, KPC-50), and PER- or SHV-type ESBLs, can hydrolyze or bind cefiderocol [82] [85].
- Efflux and Target Modification: Overexpression of efflux pumps (e.g., Ade, Mex) and mutations in the target PBP3 can also contribute to resistance [82] [83].
2.2 Ceftazidime-Avibactam: A BL-BLI Against KPC and OXA-48 This combination pairs the third-generation cephalosporin, ceftazidime, with the non-β-lactam β-lactamase inhibitor, avibactam. Avibactam is a diazabicyclooctane that reversibly inhibits a wide spectrum of Ambler class A (KPC, ESBLs), class C (AmpC), and some class D (OXA-48) β-lactamases [81] [85]. By protecting ceftazidime from hydrolysis, this combination restores activity against many MDR Enterobacterales.
Its primary vulnerability is its lack of activity against metallo-β-lactamases (MBLs; e.g., NDM, VIM). Resistance can emerge via:
- Production of MBLs: These enzymes are not inhibited by avibactam [85].
- Mutations in Porins or Efflux Pumps: Changes in membrane permeability can reduce efficacy.
- Modification of Target PBPs.
- Emergence of Ceftazidime-Avibactam Resistant Variants: Mutations in KPC (e.g., KPC-41) can lead to resistance both to this agent and, concerningly, show cross-resistance to cefiderocol [82].
2.3 Sulbactam-Durlobactam: A Targeted Anti-Acinetobacter Agent Sulbactam-durlobactam is a recently approved, targeted therapy for CRAB infections. Sulbactam is a penicillanic acid sulfone that possesses intrinsic bactericidal activity against A. baumannii by binding to PBP1a/1b and PBP3. Durlobactam is a novel diazabicyclooctanone (DBO) β-lactamase inhibitor that protects sulbactam from hydrolysis by a broad range of class A, C, and D (including OXA-23, OXA-24/40) carbapenemases prevalent in CRAB [86] [87].
The primary drivers of resistance to this combination in CRAB are:
- Metallo-β-Lactamases (MBLs): Durlobactam does not inhibit MBLs [86].
- Mutations in PBP3: Alterations in the target site can reduce sulbactam binding [86].
- Efflux Pumps: Increased expression of efflux systems like AdeIJK can reduce the intracellular concentration of durlobactam [86].
Table 1: Core Mechanisms and Primary Resistance Profiles
| Agent | Drug Class | Primary Mechanism | Key Resistance Mechanisms |
|---|---|---|---|
| Cefiderocol | Siderophore cephalosporin | Trojan horse iron transport; PBP3 inhibition | Mutations in siderophore receptors (e.g., cirA, tonB); NDM, KPC-variants, PER/SHV ESBLs; efflux pumps; PBP3 mutations [81] [82] [83] |
| Ceftazidime-Avibactam | BL-BLI combination | Ceftazidime: PBP inhibition; Avibactam: β-lactamase inhibition (Class A, C, some D) | MBL production (NDM, VIM); porin/efflux mutations; KPC variants [82] [85] |
| Sulbactam-Durlobactam | BL-BLI combination | Sulbactam: Intrinsic PBP inhibition; Durlobactam: β-lactamase inhibition (Class A, C, D) | MBL production; PBP3 mutations; efflux pump overexpression [86] [87] |
Diagram 1: Comparative Antibiotic Mechanisms
In Vitro Susceptibility and Spectrum of Activity
Surveillance and in vitro studies reveal distinct spectra of activity for each agent, crucial for empiric and targeted therapy selection.
3.1 Cefiderocol: Broad-Spectrum Activity with Notable Exceptions Cefiderocol demonstrates potent in vitro activity against a wide range of MDR Gram-negative pathogens. Data from the SENTRY Antimicrobial Surveillance Program (2020-2024) shows consistently high susceptibility rates among Enterobacterales, P. aeruginosa, and A. baumannii, including carbapenem-non-susceptible isolates [88]. It remains one of the most active agents against CR-Pa, with one surveillance study reporting 95.8% susceptibility, surpassing ceftazidime-avibactam (81.7%) and ceftolozane-tazobactam (79.2%) [85]. It also shows promise as one of the few agents with activity against MBL-carrying A. baumannii [88]. However, susceptibility can be significantly lower in isolates harboring specific resistance determinants, particularly NDM enzymes and certain KPC variants associated with ceftazidime-avibactam resistance [82].
3.2 Ceftazidime-Avibactam: A Strong Option for KPC and OXA-48 Producers Ceftazidime-avibactam is a cornerstone for treating infections caused by KPC-producing CRE and those with OXA-48-like enzymes. Its weakness against MBL-producing strains is a critical limitation. A multicenter study in Southern Italy confirmed its high activity (81.7% susceptibility) against P. aeruginosa, though resistance was primarily linked to the presence of VIM-type MBLs and PER-1 ESBL, often in high-risk clones like ST111 and ST235 [85].
3.3 Sulbactam-Durlobactam: A Precision Tool for the CRAB Crisis Sulbactam-durlobactam exhibits targeted efficacy against CRAB. In a global surveillance study of 5,032 A. baumannii-calcoaceticus complex (ABC) isolates, less than 2% had SUL-DUR MIC values >4 µg/mL, underscoring its potency against this challenging pathogen [86]. Its activity is largely unaffected by the common OXA-type carbapenemases in CRAB but is compromised by the co-production of MBLs.
Table 2: Comparative In Vitro Susceptibility Profiles Against MDR Pathogens
| Pathogen / Resistance Phenotype | Cefiderocol | Ceftazidime-Avibactam | Sulbactam-Durlobactam |
|---|---|---|---|
| Carbapenem-Resistant Enterobacterales (CRE) | High activity, but reduced against NDM+ and CZA-R KPC+ isolates [81] [82] | High activity against KPC+ and OXA-48+, but inactive against MBL+ [82] [85] | Not a primary agent |
| KPC-producing K. pneumoniae | Variable (susceptible vs. resistant based on KPC variant) [82] | High activity (primary indication) [85] | Not a primary agent |
| NDM-producing Enterobacterales | Reduced activity [82] | Inactive [85] | Not a primary agent |
| Carbapenem-Resistant P. aeruginosa (CR-Pa) | High activity (e.g., 95.8% susceptible); a leading option [85] | Good activity (e.g., 81.7% susceptible); compromised by MBL/PER-1 [85] | Not a primary agent |
| Carbapenem-Resistant A. baumannii (CRAB) | Good activity, including some MBL+ strains [81] [88] | Generally poor activity | High activity (primary indication); >98% susceptible in surveillance [86] [87] |
| MBL-producing A. baumannii | One of the few active agents [88] | Inactive | Inactive [86] |
Synergy and Cross-Resistance: Implications for Combination Therapy
Combining antibiotics is a common strategy to enhance efficacy and prevent resistance. Research indicates potential for synergy, particularly with cefiderocol.
Cefiderocol Combinations: A 2024 study investigated cefiderocol combined with β-lactamase inhibitors (avibactam, sulbactam, tazobactam) against CRE, CR-Pa, and CRAB. The cefiderocol/sulbactam combination emerged as the most promising, demonstrating synergistic activity against all three pathogen groups. Cefiderocol/avibactam was synergistic against CRE, and cefiderocol/tazobactam against CRE and CR-Pa. These combinations also enhanced cefiderocol's activity against some cefiderocol-resistant isolates [81]. This suggests that BLIs can protect cefiderocol from enzymatic degradation, expanding its utility.
Cross-Resistance Concerns: A critical consideration is cross-resistance between newer agents. Isolates harboring specific KPC variants (e.g., KPC-41) can be resistant to both ceftazidime-avibactam and cefiderocol [82]. Furthermore, evolution experiments with P. aeruginosa show that exposure to ceftazidime-avibactam can select for cross-resistance to other drug classes, including ciprofloxacin, and may close the door on potential collateral sensitivity-based therapeutic strategies [89].
Clinical and Real-World Outcomes
Real-world evidence is accumulating to support the efficacy of these new agents.
Cefiderocol: The international, retrospective PROVE study evaluated real-world cefiderocol use in seriously ill patients. The overall clinical cure rate across infection sites was 70.1%. Outcomes were superior when cefiderocol was used empirically (* 73.7%* cure) compared to as salvage therapy (54.3%) [88]. In patients with bloodstream infections, the clinical cure rate was 63.7% [88]. Importantly, cefiderocol was effective against pathogens non-susceptible to other BL-BLI combinations, with a clinical cure rate of 70.2% in this group [88].
Sulbactam-Durlobactam: This agent was approved based on the phase 3 ATTACK trial, which demonstrated non-inferiority to colistin-based regimens for CRAB infections, with a significantly improved safety profile, particularly regarding nephrotoxicity [87]. It is now the IDSA-preferred treatment strategy (in combination with a carbapenem) for CRAB infections [87].
Essential Research Toolkit: Methodologies for Efficacy and Resistance Studies
For researchers investigating these agents, standardized and specialized methodologies are required.
6.1 Antimicrobial Susceptibility Testing (AST)
- Cefiderocol: Requires iron-depleted cation-adjusted Mueller-Hinton broth (ID-CA-MHB) to induce the expression of bacterial iron-transport systems, a critical factor for its activity. Standard broth microdilution is performed in this medium per EUCAST guidelines [81] [84].
- Ceftazidime-Avibactam & Sulbactam-Durlobactam: Can be tested using standard broth microdilution or commercial automated systems with appropriate drug concentrations and clinical breakpoints.
6.2 Time-Kill Curve Assays for Synergy This method is key for evaluating combination therapy.
- Protocol: Organisms are inoculated (~5 x 10^5 CFU/mL) in ID-CA-MHB containing the antibiotic alone and in combination. Samples are removed at defined timepoints (e.g., 0, 2, 4, 8, 24 h), serially diluted, and plated on agar to determine viable bacterial counts (log10 CFU/mL). Synergism is typically defined as a ≥2 log10 CFU/mL reduction in bacterial growth with the combination compared to the most active single agent [81].
6.3 Investigating Resistance Mechanisms
- In Vitro Resistance Development Models: Strains are serially passaged in media with incrementally increasing antibiotic concentrations. Isolates with stabilized resistance are then sequenced to identify acquired mutations, providing insights into potential resistance pathways [83].
- Whole-Genome Sequencing (WGS): DNA is extracted, libraries are prepared, and sequencing is performed on platforms like Illumina iSeq 100 or MiSeq. Bioinformatic analysis includes assembly, annotation, and screening for mutations in resistance-associated genes (e.g., siderophore receptors, PBPs, β-lactamases) and known AMR determinants using tools like AMRFinderPlus [81] [83] [84].
Diagram 2: Resistance Mechanism Investigation Workflow
Table 3: The Scientist's Toolkit: Key Reagents and Methods
| Tool / Reagent | Function / Application | Key Consideration |
|---|---|---|
| Iron-Depleted Cation-Adjusted Mueller-Hinton Broth (ID-CA-MHB) | Essential for valid cefiderocol susceptibility testing; induces bacterial iron transport systems [84]. | Must be prepared in-house with chelating agents or purchased from specialized suppliers. |
| Broth Microdilution Plates | Gold-standard for determining Minimum Inhibitory Concentration (MIC). | Available as custom or commercial panels with predefined antibiotic gradients. |
| Dipicolinic Acid (DPA) | A metal chelator used to inhibit metallo-β-lactamase (MBL) activity in confirmatory tests [84]. | Used to differentiate MBL-mediated resistance from other mechanisms. |
| Whole-Genome Sequencing (WGS) Platforms (e.g., Illumina) | For comprehensive genomic analysis of resistant isolates to identify mutations and resistance genes [81] [83]. | Critical for associating genotypic changes with phenotypic resistance. |
| Time-Kill Curve Assay Components | To evaluate bactericidal activity and synergistic effects of antibiotic combinations [81]. | Requires precise timing and serial dilutions for colony counting. |
The arrival of cefiderocol, ceftazidime-avibactam, and sulbactam-durlobactam marks a significant advance in the fight against MDR Gram-negative infections. Each agent occupies a distinct niche: cefiderocol offers a broad-spectrum, last-resort option with a unique siderophore mechanism; ceftazidime-avibactam is a key agent for KPC- and OXA-48-producing Enterobacterales; and sulbactam-durlobactam provides a targeted, potent, and safer option for the devastating CRAB infections. However, the emergence of resistance, including cross-resistance between these newer agents, underscores that the arms race is far from over. Future research must focus on several key areas: the clinical translation of synergistic combinations, continuous surveillance of resistance patterns using standardized methods, and the development of rapid diagnostics to guide their optimal use. Furthermore, exploring the potential of durlobactam to enhance other β-lactams beyond sulbactam represents an exciting research avenue [87]. For the research and development community, a deep understanding of the comparative strengths and vulnerabilities of these agents is paramount for designing the next generation of antimicrobial therapies and stewardship strategies to preserve their efficacy.
The relentless expansion of antimicrobial resistance (AMR), particularly in Gram-negative bacteria, represents one of the most pressing global health crises of our time. The World Health Organization (WHO) has declared AMR among the top ten global public health threats, with bacterial infections increasingly evading conventional antibiotic treatments [1] [51]. In 2023, approximately 1 in 6 laboratory-confirmed common bacterial infections demonstrated resistance to antibiotics, with resistance rates increasing by 5-15% annually across numerous bug-drug combinations [51]. The challenge is particularly acute for Gram-negative pathogens—classified as "critical priority" in the 2024 WHO Bacterial Priority Pathogens List—due to their structurally dynamic cell envelope which confers intrinsic resistance to multiple antibiotic classes [1] [22].
The development of novel antimicrobial therapies has become an urgent necessity, yet these advances are immediately threatened by the emergence of resistance mechanisms that compromise their efficacy. Gram-negative bacteria, including the ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species), possess a formidable array of resistance mechanisms including antibiotic-inactivating enzymes, enhanced efflux systems, reduced membrane permeability, and target site modifications [40] [1]. The recent introduction of novel therapeutic agents, including new beta-lactam/beta-lactamase inhibitor combinations (BL/BLIc), siderophore antibiotics, and antimicrobial peptides, has been met with rapid bacterial adaptation through both enzymatic and non-enzymatic resistance pathways [21] [90] [91].
This technical guide examines the current landscape of resistance to novel anti-Gram-negative therapies, with a focus on the molecular mechanisms underlying resistance emergence, surveillance methodologies for tracking resistance patterns, and experimental approaches for investigating resistance development. By synthesizing the most recent evidence and technological advances, this review provides researchers, scientists, and drug development professionals with a comprehensive framework for understanding and addressing the challenge of resistance to newer antimicrobial agents within the broader context of Gram-negative bacterial resistance mechanisms.
Resistance Mechanisms to Novel Therapeutic Agents
Beta-Lactam/Beta-Lactamase Inhibitor Combinations (BL/BLIc)
The development of novel beta-lactam/beta-lactamase inhibitor combinations represents a cornerstone strategy for overcoming resistance in Gram-negative pathogens. However, resistance to these newer agents has increasingly been reported through multiple mechanisms [91]. Enzymatic inactivation remains a primary resistance pathway, with certain metallo-β-lactamases (MBLs) and serine-based carbapenemases demonstrating the ability to hydrolyze even the most recently developed beta-lactams. Additionally, resistance emergence has been linked to porin mutations that reduce membrane permeability, overexpression of efflux pumps that actively export antibiotics, and modifications in penicillin-binding proteins that reduce drug-target binding affinity [91].
The pharmacokinetic/pharmacodynamic (PK/PD) profile of BL/BLIc significantly influences resistance development. Evidence suggests that achieving aggressive joint PK/PD targets through optimized dosing strategies—such as prolonged or continuous infusion of time-dependent agents—may help suppress resistance emergence. Therapeutic drug monitoring has consequently emerged as a valuable tool for maintaining drug concentrations above the resistance suppression threshold throughout the dosing interval [91]. The efficacy of combination therapy versus monotherapy for preventing resistance remains uncertain, with current studies limited in size and quality, and resistance emergence rarely serving as a primary endpoint in clinical trials [91].
Siderophore Cephalosporins
Cefiderocol, a novel siderophore cephalosporin, employs a unique "Trojan horse" strategy to penetrate the outer membrane of Gram-negative bacteria by exploiting their iron transport systems [90]. Despite this innovative mechanism, resistance has already been documented through diverse pathways as illustrated in Figure 1. Efflux pump activation plays a significant role in cefiderocol resistance, with inhibition assays using carbonyl cyanide m-chlorophenyl hydrazone (CCCP) demonstrating significantly reduced minimum inhibitory concentrations (MICs) in resistant strains [90].
Genomic analyses have identified key resistance mechanisms including specific β-lactamase gene variants (particularly blaOXA-66, blaOXA-23, and blaSHV-12), mutations in iron transport-associated genes (envZ, cirA, nuoC), and alterations in ampC expression [90]. Particularly noteworthy is the identification of mutations and loss-of-function events in iron transporter genes (piuA, pirA, fepA) that normally facilitate cefiderocol uptake. Porin mutations (such as those affecting OmpK35, OmpK36 in K. pneumoniae and OprD in P. aeruginosa) have also been associated with elevated MICs in isogenic mutants [90]. The amplification of specific β-lactamase genes, notably blaSHV-12, has been correlated with progressively increasing resistance levels in Klebsiella pneumoniae, highlighting the potential for resistance development under selective pressure [90].
Figure 1. Cefiderocol uptake and resistance mechanisms. The diagram illustrates cefiderocol's "Trojan horse" mechanism exploiting bacterial iron transport systems, alongside key documented resistance pathways including enzymatic inactivation, efflux pump activation, and impaired uptake [90].
Novel Antimicrobial Agents and Non-Traditional Therapies
Beyond conventional antibiotics, several novel chemical entities and non-traditional therapeutic approaches face similar challenges with resistance development. TGV-49, a novel broad-spectrum antimicrobial agent derived from Mul-1867, exhibits activity against multidrug-resistant Gram-negative bacteria through a mechanism involving disruption of the microbial membrane [21]. The compound's positively charged hexanediamine groups bind to negatively charged bacterial membrane components, while hydrazine groups react with carbonyl groups, collectively resulting in membrane disruption, leakage of intracellular contents, and eventual cell lysis [21].
Experimental evolution studies using morbidostat devices have demonstrated minimal development of resistance to TGV-49 in Acinetobacter baumannii, suggesting a lower propensity for resistance compared to conventional antibiotics [21]. This characteristic may be attributed to its mechanism of action targeting fundamental membrane structures rather than specific molecular targets that can be modified through single mutations.
Bacteriophage therapy represents another promising alternative, yet faces similar challenges with resistance development. Bacteria can develop resistance to phage through multiple mechanisms including receptor modification, restriction-modification systems, and CRISPR-Cas systems [36]. The use of phage cocktails rather than single phage preparations has emerged as a strategy to reduce the emergence of resistance, as simultaneous mutations conferring resistance to multiple phages are statistically less likely [36].
Table 1: Resistance Mechanisms to Novel Anti-Gram-Negative Therapies
| Therapeutic Class | Example Agents | Primary Resistance Mechanisms | Key Genetic Determinants |
|---|---|---|---|
| BL/BLIc | Novel β-lactam/β-lactamase inhibitor combinations | Enzymatic hydrolysis, porin mutations, efflux pump overexpression, target site modifications | MBL genes, serine carbapenemases, porin genes (ompK35, ompK36, oprD), efflux regulators |
| Siderophore Antibiotics | Cefiderocol | Efflux pump activation, β-lactamase variants, iron transporter alterations, porin mutations | blaOXA-23, blaOXA-66, blaSHV-12, envZ, cirA, piuA, pirA, fepA |
| Membrane-Targeting Agents | TGV-49 | Reduced susceptibility observed in experimental evolution | Minimal resistance development in morbidostat studies |
| Bacteriophage Therapy | Phage cocktails | Receptor modification, restriction-modification systems, CRISPR-Cas systems | Genes encoding phage receptors, restriction enzymes, CRISPR arrays |
Surveillance Methodologies and Resistance Trends
Global Surveillance Systems and Data
The WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) represents the most comprehensive effort to track resistance patterns worldwide, with 104 participating countries representing 70% of the global population [51]. The 2025 GLASS report analyzed over 23 million bacterial infections, providing resistance prevalence estimates across 22 antibiotics used to treat infections caused by eight bacterial pathogens [51]. The data reveal significant geographic variation in resistance patterns, with the WHO's Southeast Asian and Eastern Mediterranean regions experiencing approximately 1 in 3 common bacterial infections being drug-resistant, compared to 1 in 10 in Europe and 1 in 5 in Africa [51].
Notably, resistance to "Watch" antibiotics—broad-spectrum agents recommended for more severe infections—is increasing concerningly. For example, 54.3% of Acinetobacter bloodstream infections demonstrated resistance to carbapenems, with resistance rates reaching 41.2% for K. pneumoniae bloodstream infections in Southeast Asia [51]. In urinary tract infections caused by E. coli and K. pneumoniae—among the most common bacterial infections in women worldwide—resistance to first-line antibiotics typically exceeded 30% in most countries [51].
Table 2: Global Resistance Patterns in Gram-Negative Pathogens (2023 GLASS Data)
| Pathogen | Infection Type | Resistance Pattern | Regional Variation |
|---|---|---|---|
| Escherichia coli | Bloodstream | 44.8% resistant to 3rd-generation cephalosporins | >70% resistance in Africa |
| Klebsiella pneumoniae | Bloodstream | 55.2% resistant to 3rd-generation cephalosporins | >70% resistance in Africa |
| Acinetobacter spp. | Bloodstream | 54.3% carbapenem-resistant | Highest in Southeast Asia |
| Klebsiella pneumoniae | Bloodstream | 41.2% carbapenem-resistant (Southeast Asia) | Regional hot spots identified |
| Escherichia coli | Urinary tract | Typically >30% resistance to first-line antibiotics | Consistent across most regions |
Laboratory Detection Methods
Surveillance of resistance to novel therapies requires specialized laboratory methods and conditions. For cefiderocol susceptibility testing, the Clinical and Laboratory Standards Institute (CLSI) recommends the use of iron-depleted cation-adjusted Mueller-Hinton broth (ID-CAMHB) to properly induce bacterial iron transport systems [90]. Preparation of ID-CAMHB involves treatment with Chelex 100 resin to reduce iron concentrations to <0.03 μg/mL, followed by supplementation with specific cations (Zn²⁺, Ca²⁺, Mg²⁺) to standardize growth conditions [90].
Antimicrobial susceptibility testing for novel agents typically employs broth microdilution methods according to CLSI guidelines, with the minimum inhibitory concentration (MIC) defined as the lowest concentration that inhibits visible bacterial growth [21] [90]. For investigational agents, breakpoints may not be fully established, requiring researchers to apply epidemiological cutoffs (ECOFFs) to distinguish wild-type from non-wild-type populations [21].
Advanced molecular techniques including whole genome sequencing, RT-qPCR for resistance gene expression analysis, and efflux pump inhibition assays provide critical insights into resistance mechanisms [90]. These methodologies enable researchers to identify specific resistance mutations, quantify expression changes in resistance genes, and determine the contribution of efflux activity to resistant phenotypes.
Experimental Approaches for Investigating Resistance Development
Morbidostat-Based Resistomics
The morbidostat device represents a sophisticated approach for investigating resistance development in laboratory environments. This computer-controlled continuous culturing system automatically adjusts antibiotic concentrations in response to bacterial growth dynamics, applying gradual selective pressure that drives the evolution of resistance [21]. As illustrated in Figure 2, the system continuously monitors optical density (OD₆₀₀) of bacterial cultures, initiating dilution with drug-containing media when growth rates exceed target thresholds, and with drug-free media when growth inhibition occurs [21].
This experimental evolution approach enables real-time observation of resistance development and identification of resistance mechanisms through whole-genome sequencing of evolved isolates. Morbidostat studies with TGV-49 demonstrated minimal resistance development in Acinetobacter baumannii, in contrast to the rapid resistance emergence typically observed with conventional antibiotics [21]. The integration of experimental evolution with genomic analysis—termed "resistomics"—provides a powerful workflow for profiling the resistance potential of novel antimicrobial agents during early development stages.
Figure 2. Morbidostat workflow for resistance evolution studies. The diagram illustrates the continuous culturing system that applies escalating selective pressure to drive resistance development, followed by genomic analysis of evolved isolates [21].
Molecular Characterization of Resistance Mechanisms
Comprehensive characterization of resistance mechanisms requires integrated molecular approaches. Efflux pump inhibition assays using agents such as carbonyl cyanide m-chlorophenyl hydrazone (CCCP) can determine the contribution of efflux activity to resistance phenotypes by comparing MIC values with and without efflux pump inhibition [90]. For cefiderocol, CCCP treatment significantly reduced MICs in resistant strains, confirming the role of efflux systems in resistance to this agent [90].
Gene expression analysis through RT-qPCR enables quantification of resistance gene expression under antimicrobial pressure. Studies have demonstrated upregulated expression of β-lactamase genes (blaSHV-12, blaOXA variants) and efflux pump regulators in resistant isolates [90]. Whole genome sequencing identifies mutations in key resistance-associated loci including porin genes, iron transporters, and two-component regulatory systems [90]. Complementary experimental approaches include porin expression analysis, membrane permeability assays, and biochemical characterization of antibiotic-modifying enzymes to fully elucidate resistance mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for Investigating Resistance to Novel Therapies
| Reagent/Method | Application | Technical Considerations |
|---|---|---|
| Iron-depleted Cation-Adjusted Mueller-Hinton Broth (ID-CAMHB) | Cefiderocol susceptibility testing | Iron concentration must be <0.03 μg/mL; requires cation supplementation after Chelex treatment [90] |
| Morbidostat Device | Experimental evolution of resistance | Computer-controlled continuous culturing system; enables real-time adjustment of antimicrobial pressure [21] |
| Carboxyl Cyanide m-Chlorophenyl Hydrazone (CCCP) | Efflux pump inhibition studies | Protonophore that dissipates proton motive force; use at subinhibitory concentrations to assess efflux contribution [90] |
| Chelex 100 Resin | Preparation of iron-depleted media | Chelating resin for iron removal; requires 6-hour stirring followed by verification of iron concentration [90] |
| Whole Genome Sequencing Platforms | Identification of resistance mutations | Enables comprehensive analysis of single nucleotide polymorphisms, insertions/deletions, and gene amplification events [90] |
| RT-qPCR Assays | Resistance gene expression quantification | Requires validation of reference genes; targets include β-lactamase genes, efflux pump regulators, porin genes [90] |
| Broth Microdilution Systems | MIC determination for novel agents | Follows CLSI guidelines; requires appropriate quality control strains and media specifications [21] [90] |
The ongoing challenge of resistance to novel antimicrobial therapies demands continuous surveillance, sophisticated research methodologies, and interdisciplinary approaches to understand and mitigate resistance mechanisms. The investigational frameworks and technical approaches outlined in this review provide a foundation for tracking and studying resistance to newer anti-Gram-negative agents. As the field advances, several priorities emerge: First, enhanced global surveillance with improved geographic representation, particularly from low- and middle-income countries where surveillance capacity remains limited. Second, standardized methodologies for resistance detection and characterization specific to novel therapeutic classes. Third, integrative approaches that combine experimental evolution with multi-omics technologies to comprehensively profile resistance development. Finally, translational research bridging basic resistance mechanisms with clinical practice to inform stewardship strategies that preserve the efficacy of novel agents. Through coordinated efforts across the scientific community, we can track, understand, and ultimately counter the relentless evolution of bacterial resistance, preserving the efficacy of essential antimicrobial therapies for future generations.
Antimicrobial resistance (AMR) represents one of the most severe global health threats, with drug-resistant infections causing approximately 1.27 million deaths annually and projected to cause millions more without effective intervention [92]. The One Health approach recognizes that the health of people, animals, and ecosystems is interconnected, and that AMR emerges at the intersections of these domains [93]. Gram-negative bacteria, particularly carbapenem-resistant Enterobacterales (CRE), difficult-to-treat resistant Pseudomonas aeruginosa (DTR P. aeruginosa), and carbapenem-resistant Acinetobacter baumannii (CRAB), represent particularly urgent threats due to their complex resistance mechanisms and ability to transfer resistance genes across species and environments [38] [54]. This technical guide provides a comprehensive framework for validating interventions against Gram-negative bacterial resistance across human, animal, and environmental reservoirs, with specific methodological protocols for researchers and drug development professionals.
The fundamental premise of One Health is that successful public health interventions require the cooperation of human, animal, and environmental health partners [93]. This approach is particularly relevant for AMR because resistant zoonotic bacteria can be found in soil and from there can infect plants, vegetables, and fruits, while antimicrobial residues from human and animal use can persist in aquatic environments, exerting selective pressure and facilitating resistance gene transfer [94]. The global spread of resistance is further exacerbated by migration of people and animals infected with resistant bacteria, international travel and trade, and environmental contamination from agricultural and pharmaceutical waste [94] [93].
Gram-Negative Bacterial Resistance Mechanisms
Structural and Molecular Basis of Resistance
Gram-negative bacteria possess a complex, multi-layered cell envelope that constitutes a formidable permeability barrier and contributes significantly to their resistance profile. This envelope consists of three primary components: an outer membrane (OM) containing lipopolysaccharides (LPS) and porin proteins, a thin peptidoglycan layer, and an inner membrane (IM) [1]. The asymmetric structure of the OM, with its lipopolysaccharide-rich outer leaflet, acts as an effective barrier against hydrophobic compounds, while the channel properties of porin proteins (OMPs) regulate the influx of hydrophilic antibiotics and nutrients [1].
The major resistance mechanisms in Gram-negative bacteria can be categorized into four primary groups: (1) drug inactivation or modification through enzymatic degradation; (2) limited drug uptake via membrane permeability barriers or porin remodeling; (3) alteration of drug target sites through mutation or modification; and (4) enhanced drug efflux through overexpression of efflux pump systems [1]. These mechanisms are often combined in multidrug-resistant (MDR) strains, creating infections that are exceptionally difficult to treat with conventional antibiotics.
Key Resistance Pathways in Priority Pathogens
The World Health Organization has classified several Gram-negative bacterial families as priority pathogens requiring urgent research and development of new therapies. These include Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacteriaceae such as Klebsiella pneumoniae and Escherichia coli [1]. These pathogens employ diverse resistance strategies:
Enzymatic Inactivation: Production of β-lactamases (including extended-spectrum β-lactamases [ESBLs], AmpC β-lactamases, and carbapenemases) that hydrolyze β-lactam antibiotics [38]. Carbapenemase production, particularly by K. pneumoniae and E. coli, represents a major global concern [54].
Membrane Permeability Alterations: Modifications to outer membrane porins reduce antibiotic influx, while overexpression of efflux pumps (particularly Resistance-Nodulation-Division [RND] family transporters) actively expel antibiotics from bacterial cells [95]. Mutations in porins and efflux pumps play a crucial role in antibiotic resistance by altering drug permeability and active efflux [95].
Target Site Modification: Alteration of penicillin-binding proteins (PBPs), DNA gyrase, topoisomerase IV, and ribosomal target sites reduces antibiotic binding affinity and efficacy [1].
Table 1: Major Resistance Mechanisms in Priority Gram-Negative Pathogens
| Pathogen | Primary Resistance Mechanisms | Key Resistance Elements | Clinical Impact |
|---|---|---|---|
| Carbapenem-resistant Enterobacterales (CRE) | Carbapenemase production, porin mutations, efflux pumps | KPC, NDM, VIM, IMP enzymes; OmpK35/36 porin changes | Mortality rates up to 50% in bloodstream infections |
| Difficult-to-treat resistant P. aeruginosa | AmpC β-lactamase overexpression, efflux pump upregulation, porin modifications | MexAB-OprM efflux system; OprD porin loss | Limited treatment options; requires combination therapy |
| Carbapenem-resistant A. baumannii (CRAB) | OXA-type carbapenemases, efflux systems, permeability barriers | AdeABC efflux pump; OXA-23, OXA-48-like enzymes | Nosocomial outbreaks with limited therapeutic options |
| ESBL-producing Enterobacterales | Extended-spectrum β-lactamase production | CTX-M, TEM, SHV enzymes | Resistance to penicillins and cephalosporins |
The following diagram illustrates the major antibiotic resistance mechanisms in Gram-negative bacteria:
One Health Surveillance Methodologies
Integrated AMR Surveillance Framework
The Global Antimicrobial Resistance Surveillance System (GLASS) was established by the World Health Organization to fill knowledge gaps and guide strategies at all levels [94]. GLASS provides a standardized approach to collecting, analyzing, interpreting, and sharing data by country, region, and area, allowing for monitoring of new or existing national surveillance systems with emphasis on representativeness and data quality [94]. An effective One Health surveillance framework encompasses human, animal, and environmental sampling with standardized methodologies:
Human Health Sector Surveillance: Collection of clinical isolates from healthcare facilities with comprehensive antimicrobial susceptibility testing (AST) and molecular characterization of resistance mechanisms. The Infectious Diseases Society of America (IDSA) provides updated guidance on testing methodologies, including CLSI-endorsed methods such as the broth disk elution method to test for activity of combination therapies [38].
Animal Health Sector Surveillance: Monitoring antimicrobial use and resistance patterns in livestock, companion animals, and aquaculture systems. This includes tracking the volume of antimicrobials used for therapeutic, prophylactic, and growth promotion purposes, which is estimated to be greater in animals than in humans globally [94].
Environmental Surveillance: Sampling of wastewater, agricultural run-off, and natural water bodies to detect antimicrobial residues and resistant bacteria. Environmental samples can provide early warning of emerging resistance patterns and trace the dissemination of resistance genes across ecosystems [94] [93].
Table 2: One Health Surveillance Matrix for Gram-Negative Bacterial Resistance
| Reservoir | Sampling Sites | Target Analytes | Standard Methods | Frequency |
|---|---|---|---|---|
| Human | Hospitals, clinics, communities | Clinical isolates, resistance rates | CLSI/EUCAST standards, molecular typing | Continuous |
| Animal (Livestock) | Farms, slaughterhouses | Fecal samples, meat products | Culture-based AST, whole-genome sequencing | Quarterly |
| Animal (Companion) | Veterinary clinics | Urine, wound, fecal isolates | Disk diffusion, MIC determination | Annual |
| Environment (Water) | Wastewater, rivers, lakes | Antimicrobial residues, resistant bacteria | LC-MS/MS, culture methods, qPCR | Monthly |
| Environment (Soil) | Agricultural fields, parks | Resistant bacteria, resistance genes | Metagenomics, functional gene arrays | Seasonal |
Quantitative One Health Assessment Tools
The One Health Community Assessment (OHCA) represents the first reliable and validated instrument to measure the impacts of pets on One Health [96]. This 115-item instrument employs Likert scales and consists of five subscales: community health (Cronbach's α = 0.897), human health (α = 0.842), pet health (α = 0.899), environmental health (α = 0.789), and connections between domains of One Health (α = 0.762) [96]. The OHCA was validated for use in both English and Spanish and demonstrated effectiveness in both urban and rural underserved communities.
The development of the OHCA followed an exploratory sequential mixed methods approach, beginning with semi-structured qualitative interviews to understand community perspectives on how pets impact the health of people, other animals, and the natural environment [96]. Transcripts were coded using standard, software-mediated qualitative analysis methodologies (Dedoose, Inc., Hermosa Beach, CA), with in vivo coding methods used for the first round of coding, followed by axial coding methods to refine the final sub-scales for use in the quantitative instrument [96].
Experimental Validation Protocols
Cross-Sectoral Intervention Testing
Validating interventions across One Health reservoirs requires integrated experimental protocols that account for the complex interactions between humans, animals, and environments. The following workflow provides a methodological framework for cross-sectoral intervention testing:
Environmental Reservoir Validation Methods
Environmental monitoring for antimicrobial residues and resistance elements requires specialized methodologies:
Water and Soil Sampling Protocols: Collect water samples (1L) in sterile containers, filter through 0.45μm membranes, and culture on selective media containing antibiotics. For soil samples, suspend 10g in 90mL buffered peptone water, homogenize, and perform serial dilutions for culture [94]. Molecular detection of resistance genes can be performed using PCR or metagenomic sequencing.
Antimicrobial Residue Analysis: Liquid chromatography with tandem mass spectrometry (LC-MS/MS) methods can detect antimicrobial residues at nanogram-per-liter levels in environmental samples. Solid-phase extraction (SPE) is used for sample concentration and cleanup prior to analysis.
Resistance Gene Transfer Studies: Laboratory models simulating natural environments can assess horizontal gene transfer rates. Filter mating assays or liquid culture systems containing environmental samples can quantify conjugation frequencies under various conditions.
Animal Reservoir Validation Methods
Animal studies should assess both the efficacy of interventions and their impact on resistance selection:
Therapeutic Efficacy Trials: Randomized controlled trials in naturally infected or challenged animals, measuring clinical outcomes, microbiological eradication, and resistance emergence. For food animals, follow the WHO guidelines on use of antimicrobials in animal production [94].
Transmission Blocking Studies: Models that evaluate the intervention's ability to prevent transmission of resistant bacteria between animals and to humans. This includes environmental contamination monitoring and contact animal surveillance.
Microbiome Impact Assessment: 16S rRNA sequencing and functional metagenomics to evaluate the intervention's effect on the animal gut microbiome and resistome, particularly selection for resistance genes.
Emerging Interventions and Assessment
Novel Therapeutic Agents
The development of new antimicrobials against multidrug-resistant Gram-negative bacteria has seen important advances in recent years. Several new agents with activity against carbapenem-resistant pathogens have been developed, including ceftazidime-avibactam, imipenem-relebactam, ceftolozane-tazobactam, meropenem-vaborbactam, aztreonam-avibactam, delafloxacin, temocillin, plazomicin, cefiderocol, and eravacycline [95]. These agents employ various strategies to overcome resistance, including β-lactamase inhibition, siderophore-mediated iron transport, and evasion of efflux pump recognition.
Promising research highlights include a newly developed polymer prodrug that becomes activated at sites of infection and shows potent antimicrobial activity in several mouse models of Gram-negative bacterial infection [97]. This host defense peptide-mimicking prodrug represents an innovative approach against drug-resistant Gram-negative bacterial infections [97].
Table 3: Recently Approved Antimicrobial Agents for Resistant Gram-Negative Infections
| Antibiotic Agent | Class/Type | Target Pathogens | Resistance Mechanisms Addressed | One Health Considerations |
|---|---|---|---|---|
| Ceftazidime-avibactam | Cephalosporin-β-lactamase inhibitor | CRE, ESBL-E | KPC carbapenemase inhibition | Human use only; environmental persistence studies needed |
| Cefiderocol | Siderophore cephalosporin | CRAB, DTR P. aeruginosa | Trojan horse approach; evades porin mutations | Iron-dependent uptake; limited animal use data |
| Sulbactam-durlobactam | β-lactam-β-lactamase inhibitor | CRAB | OXA-type carbapenemase inhibition | Used in combination with meropenem or imipenem-cilastatin |
| Imipenem-relebactam | Carbapenem-β-lactamase inhibitor | CRE, DTR P. aeruginosa | Class A/C β-lactamase inhibition | Similar spectrum to ceftazidime-avibactam |
| Aztreonam-avibactam | Monobactam-β-lactamase inhibitor | MBL-producing Enterobacterales | MBL stability with serine β-lactamase inhibition | Effective against NDM, VIM, IMP producers |
Non-Antibiotic Interventions
Beyond traditional antibiotics, several non-antibiotic approaches show promise for integrated One Health interventions:
Phage Therapy: Bacteriophages and phage-derived enzymes (endolysins) can target resistant Gram-negative bacteria with high specificity. Validation requires assessment of host range, resistance development, and impact on commensal microbiota.
Prevention Strategies: Vaccines, probiotics, and prebiotics can reduce the need for antimicrobial use in both human and animal populations. The One Health approach encourages development of animal vaccines that reduce zoonotic transmission and subsequent human infections [93].
Infection Control Measures: Enhanced sanitation, water quality improvement, and hospital infection prevention protocols can reduce transmission of resistant bacteria across reservoirs.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for One Health AMR Studies
| Reagent/Category | Specific Examples | Application Function | One Health Relevance |
|---|---|---|---|
| Selective Culture Media | CHROMagar ESBL, CHROMagar KPC, MacConkey with carbapenems | Isolation and presumptive identification of resistant Gram-negative bacteria | Standardized across human, animal, environmental samples |
| Molecular Detection Kits | PCR kits for blaKPC, blaNDM, blaOXA-48-like; RT-PCR for gene expression | Detection and quantification of resistance genes | Track resistance elements across reservoirs |
| Whole Genome Sequencing Kits | Illumina Nextera XT; Oxford Nanopore ligation sequencing | Comprehensive resistance gene identification, phylogenetic analysis | Understand transmission pathways and evolution |
| Antibiotic Susceptibility Testing | CLSI-compliant broth microdilution panels; Etest strips | Determination of MIC values; resistance phenotype confirmation | Standardized comparison across sectors |
| Efflux Pump Inhibitors | Phenylalanine-arginine β-naphthylamide (PAβN); carbonyl cyanide m-chlorophenyl hydrazone (CCCP) | Assessment of efflux pump contribution to resistance | Evaluate combination therapy approaches |
| Cell Line Models | Human epithelial cells (Caco-2, A549); Galleria mellonella | Infection and host-pathogen interaction studies | Bridge between in vitro and in vivo models |
| Metagenomic Analysis Tools | QIIME 2; HUMAnN2; CARD database | Microbiome and resistome characterization | Assess ecological impact of interventions |
Data Integration and Analysis Frameworks
Multidimensional Data Synthesis
Integrating data across One Health reservoirs requires sophisticated analytical approaches. Bibliometric analysis of global carbapenem-resistant Gram-negative bacteria research has identified major research clusters encompassing hypervirulent strains, resistance mechanisms, emerging therapeutic strategies, and One Health perspectives [54]. These analyses reveal that research is increasingly directed toward elucidating resistance mechanisms, improving diagnostic tools, and exploring non-antibiotic therapeutic options [54].
Artificial intelligence and machine learning approaches are being employed for early diagnosis and rapid screening of carbapenem resistance, exemplified by CRISPR-based detection and AI-driven MALDI-TOF analysis [54]. These technologies can accelerate intervention validation and implementation across reservoirs.
Statistical Considerations for One Health Studies
Sample Size Calculation: Multilevel modeling approaches that account for clustering within reservoirs and correlations between observations from the same geographical area.
Longitudinal Analysis: Methods for analyzing temporal patterns in resistance emergence and spread across interconnected reservoirs.
Network Analysis: Approaches to model transmission pathways and identify critical control points for interventions.
Validating interventions across human, animal, and environmental reservoirs requires a integrated approach that acknowledges the interconnected nature of antimicrobial resistance. The One Health perspective provides the necessary conceptual framework for developing and assessing interventions that target the complex ecology of Gram-negative bacterial resistance. As new therapeutic modalities emerge—from novel antibiotics to phage therapies and preventive vaccines—their validation must encompass impacts across all reservoirs to ensure sustainable efficacy and minimize unintended ecological consequences.
Strengthening international collaboration and fostering multidisciplinary approaches are imperative to advance high-quality research and address the growing threat of antimicrobial resistance [54]. The protocols and methodologies outlined in this technical guide provide a foundation for rigorous, reproducible intervention validation across the One Health spectrum.
Antimicrobial resistance (AMR) represents one of the most severe global health threats, with antibacterial resistant infections causing an estimated 1.1 million deaths annually and projected to rise to 8.22 million by 2050 [98] [99]. The recent WHO GLASS report reveals that one in six laboratory-confirmed bacterial infections is now resistant to antibiotic treatments, with resistance increasing at an average annual rate of 5-15% for over 40% of monitored pathogen-antibiotic combinations [50]. Gram-negative bacteria present particularly formidable challenges due to their complex cell envelope structure, which includes an outer membrane that acts as a permeability barrier, periplasmic space, and efflux pump systems that actively export antibiotics [1] [31]. The World Health Organization has classified several Gram-negative pathogens as critical priority for research and development of new antibiotics, including Acinetobacter baumannii, Pseudomonas aeruginosa, and carbapenem-resistant Enterobacteriaceae [1] [31].
The economic burden of AMR is equally alarming, with projections suggesting that without effective intervention, AMR could cost the global economy $100 trillion in cumulative lost economic output by 2050 [99]. This comprehensive analysis examines the cost-benefit considerations of next-generation antibiotics targeting resistant Gram-negative pathogens, incorporating both traditional health economic metrics and novel value frameworks that capture the full societal impact of preserving antimicrobial effectiveness.
Resistance Mechanisms in Gram-Negative Bacteria
Gram-negative bacteria possess sophisticated structural and biochemical adaptations that confer resistance to antimicrobial agents. Understanding these mechanisms is fundamental to developing effective next-generation antibiotics and conducting accurate cost-benefit assessments.
Structural Defense Systems
The Gram-negative bacterial envelope consists of three primary layers that each contribute to antibiotic resistance:
Outer Membrane (OM): This asymmetric lipid bilayer contains lipopolysaccharides (LPS) in the outer leaflet and phospholipids in the inner leaflet, creating a formidable permeability barrier [1] [31]. Integral outer membrane proteins (OMPs), particularly β-barrel proteins such as porins, regulate the passage of hydrophilic molecules including many antibiotics. Modifications to LPS structure or porin expression significantly reduce antibiotic penetration [1].
Peptidoglycan Layer: This mesh-like polymer provides structural integrity while being considerably thinner in Gram-negative bacteria compared to Gram-positive species [1]. While not a major permeability barrier itself, it serves as an anchor point for various proteins and structures involved in resistance.
Inner Membrane (IM): This phospholipid bilayer houses numerous transport proteins, including efflux pump components that work in concert with outer membrane channels to expel antibiotics [1].
Biochemical Resistance Mechanisms
Gram-negative bacteria employ four primary biochemical strategies to circumvent antibiotic activity:
Enzymatic Inactivation: Production of β-lactamases (including extended-spectrum β-lactamases [ESBLs] and carbapenemases) that hydrolyze β-lactam antibiotics [1] [31]. Other enzyme classes include aminoglycoside-modifying enzymes and chloramphenicol acetyltransferases.
Efflux Pump Systems: Multi-component complexes (e.g., AcrAB-TolC in E. coli) that span the entire cell envelope and actively export diverse antibiotics including fluoroquinolones, tetracyclines, and β-lactams [1].
Target Modification: Genetic mutations or post-translational modifications that alter antibiotic binding sites, such as changes to DNA gyrase/topoisomerase IV for fluoroquinolones or penicillin-binding proteins for β-lactams [1].
Reduced Permeability: Downregulation of porin expression (e.g., OmpF/C in E. coli) or structural modifications to LPS that limit antibiotic influx [1] [31].
The following diagram illustrates the coordinated nature of these resistance mechanisms in a Gram-negative bacterium:
Mobile Genetic Elements and Horizontal Gene Transfer
The rapid dissemination of resistance genes among Gram-negative bacteria occurs primarily through horizontal gene transfer via plasmids, transposons, and integrons [1]. Conjugation represents the most efficient mechanism for spreading resistance determinants, enabling the emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains in clinical settings [1]. This mobility complicates containment strategies and accelerates the obsolescence of existing antibiotics.
Frameworks for Economic Evaluation of Novel Antibiotics
Traditional cost-effectiveness analyses often fail to capture the full value of novel antibiotics, particularly their role in preserving effectiveness against resistant pathogens. Comprehensive economic evaluation requires expanded frameworks that account for both direct patient benefits and broader societal value.
The STEDI Value Framework
The STEDI framework encompasses five critical value dimensions for antibiotics [100]:
- Spectrum: Ability to treat multidrug-resistant infections
- Transmission: Reduction in spread of resistant strains
- Enablement: Support for modern medical procedures (e.g., surgery, chemotherapy)
- Diversity: Increased treatment options reducing selection pressure
- Insurance: Security against future resistance threats
Dynamic Transmission Modeling
Advanced economic evaluations incorporate dynamic transmission models that account for how antibiotic use affects resistance evolution and spread within populations [100] [101]. These models recognize that antibiotic effectiveness is a common-pool resource diminished by overuse and preserved by stewardship [101]. A Chinese study evaluating ceftazidime/avibactam demonstrated that incorporating transmission dynamics and diversity value revealed substantially greater economic benefits than traditional analysis, with incremental net monetary benefit up to $3.55 billion over 10 years [100].
Threshold-Based Approach for Uncertainty
Given substantial uncertainties in resistance evolution, a threshold-based approach estimates the minimum resistance-related costs that must be averted for an intervention to be cost-effective [101]. If probable costs without intervention exceed this threshold, the intervention is deemed cost-effective despite uncertainties. This approach parallels methods used in climate change economics, acknowledging that precise quantification may be impossible but decision-making cannot be deferred [101].
Table 1: Key Economic Evaluation Frameworks for Novel Antibiotics
| Framework | Key Components | Advantages | Limitations |
|---|---|---|---|
| Traditional Cost-Effectiveness Analysis | Direct medical costs, QALYs, ICER | Standardized methodology, Widely accepted | Fails to capture resistance-related externalities |
| STEDI Framework [100] | Spectrum, Transmission, Enablement, Diversity, Insurance | Comprehensive value assessment | Qualitative dimensions difficult to quantify |
| Dynamic Transmission Modeling [100] [101] | Resistance spread, Population-level effects | Captures key externalities | Data intensive, Complex modeling requirements |
| Threshold Approach [101] | Minimum cost threshold, Uncertainty ranges | Practical despite uncertainty | Does not provide precise cost-benefit ratio |
Quantitative Clinical and Economic Outcomes
Recent studies provide substantial evidence for the clinical benefits and economic value of next-generation antibiotics, particularly when deployed strategically within antimicrobial stewardship programs.
Real-World Effectiveness Studies
The PROVE study, a retrospective analysis of cefiderocol in over 1,000 patients with serious Gram-negative infections, demonstrated overall clinical cure rates of 70.1% across different infection sites [102]. Importantly, cure rates were significantly higher when cefiderocol was used empirically (73.7%) compared to salvage therapy (54.3%), highlighting the importance of appropriate positioning in the treatment pathway [102]. For bloodstream infections specifically, the cure rate was 63.7% overall, increasing to 72.0% with empirical use [102].
Cost-Effectiveness of Antibiotic Stewardship Strategies
A trial-based cost-effectiveness analysis of antibiotic prescription strategies for pediatric respiratory tract infections found that delayed antibiotic prescription (DAP) was the most cost-effective approach, with quality-adjusted life days (QALDs) of 27.94 compared to 27.88 for immediate antibiotic prescription and 27.82 for no antibiotics [103]. While direct costs for DAP (€100.90) were higher than for no antibiotics (€97.48), they were lower than immediate prescription (€109.68), demonstrating that optimal antibiotic use can simultaneously improve outcomes and reduce costs [103].
Value of Treatment Diversification
Research on ceftazidime/avibactam introduction in China demonstrated that diversifying treatment options early in the treatment pathway yielded the greatest benefits, gaining between 68,284 and 78,571 QALYs over 10 years while saving up to $236.37 per QALY gained [100]. This illustrates how strategic introduction of novel antibiotics can enhance population health while containing healthcare costs through reduced transmission of resistant strains and improved patient outcomes.
Table 2: Clinical and Economic Outcomes of Next-Generation Antibiotics
| Antibiotic/Strategy | Population/Setting | Clinical Outcome | Economic Outcome |
|---|---|---|---|
| Cefiderocol [102] | 508 patients with serious Gram-negative infections (PROVE study) | 70.1% overall clinical cure; 73.7% when used empirically | N/A (Real-world effectiveness supporting appropriate use) |
| Ceftazidime/Avibactam [100] | Chinese hospital patients with resistant Gram-negative infections | Improved treatment success against resistant pathogens | INMB up to $3.55B over 10 years; $236.37 per QALY saved |
| Delayed Antibiotic Prescription [103] | Children with RTIs in primary care | 27.94 QALDs (vs 27.88 for immediate) | €100.90 cost (vs €109.68 for immediate) |
| GSK/Fleming Initiative [98] | AMR research partnership | 6 new research programmes targeting WHO priority pathogens | £45 million funding; ~50 scientific roles |
Experimental Approaches and Research Methodologies
Cutting-edge research methodologies are essential for advancing our understanding of resistance evolution and developing more effective antimicrobial agents.
AI-Enabled Antibiotic Discovery
The GSK and Fleming Initiative partnership employs advanced AI and machine learning to accelerate antibiotic discovery against priority pathogens [98]. Their methodology includes:
- High-Throughput Screening: Automated systems generate novel datasets on diverse molecular structures
- Machine Learning Modeling: AI models predict compound activity against Gram-negative bacteria
- Cellular Penetration Prediction: Computational models focus on overcoming the Gram-negative permeability barrier
- Open Science Approach: Data and AI models are shared globally to accelerate community-wide discovery efforts
This approach specifically targets the challenge of compound accumulation in Gram-negative bacteria by modeling interactions with the complex cell envelope and efflux pump systems [98].
Quantitative Evolutionary Prediction
Systems biology approaches integrate quantitative models with multiscale data from microbial evolution experiments to predict AMR evolution [104]. Key methodological components include:
- High-Replicate Evolution Experiments: Multiple parallel microbial populations evolved under antibiotic selection pressure
- Temporal Genomic Sequencing: Tracking mutation emergence and dynamics across evolutionary trajectories
- Phenotypic Resistance Profiling: Correlating genotypic changes with resistance phenotypes
- Fitness Landscape Mapping: Modeling epistatic interactions between resistance mutations
- Stochastic Population Modeling: Predicting mutation appearance probabilities and fixation times
These methods enable researchers to quantify evolutionary predictability (existence of a probability distribution for evolutionary outcomes) and evolutionary repeatability (likelihood of specific evolutionary trajectories) [104]. Recent research indicates that despite inherent stochasticity, AMR evolution demonstrates substantial predictability, especially under strong antibiotic selection pressure [104].
The following diagram illustrates the experimental workflow for AI-enabled antibiotic discovery and resistance prediction:
Dynamic Disease Transmission and Cost-Effectiveness Modeling
The economic evaluation of novel antibiotics requires sophisticated modeling approaches that integrate clinical efficacy, resistance dynamics, and economic outcomes [100]. Key methodological aspects include:
- Model Structure: Compartmental models tracking susceptible and resistant bacterial populations
- Parameter Estimation: Real-world data on resistance prevalence, treatment outcomes, and costs
- Time Horizon: Extended timeframes (e.g., 10+ years) capturing long-term resistance evolution
- Intervention Scenarios: Comparison of multiple antibiotic deployment strategies
- Sensitivity Analysis: Probabilistic analyses quantifying parameter uncertainty
The Chinese study of ceftazidime/avibactam employed such a model, evaluating six different treatment strategies over a 10-year timeframe to assess how positioning within treatment pathways influenced both clinical and economic outcomes [100].
Table 3: Key Research Reagent Solutions for Gram-Negative AMR Research
| Research Tool | Specific Examples | Application in AMR Research |
|---|---|---|
| Bacterial Strains | WHO priority pathogens: A. baumannii, P. aeruginosa, carbapenem-resistant Enterobacteriaceae [1] [31] | Phenotypic screening, resistance mechanism studies, in vitro and in vivo efficacy testing |
| AI/ML Platforms | Imperial College Drug Discovery Hub AI models [98] | Compound screening, penetration prediction, resistance forecasting |
| Genomic Tools | Whole genome sequencing, Mutational scanning, Plasmid analysis [104] | Resistance gene identification, evolutionary tracking, horizontal gene transfer studies |
| Cell-Free Systems | Bacterial membrane mimics, Porin isolation [1] | Permeability studies, compound penetration assessment, efflux pump characterization |
| Animal Models | Mouse thigh infection, Pneumonia models, Sepsis models | In vivo efficacy testing, pharmacokinetic/pharmacodynamic analysis |
| Chemical Probes | β-Lactamase substrates, Efflux pump indicators, Membrane permeability markers | Mechanism of action studies, resistance detection, compound optimization |
The cost-benefit analysis of next-generation antibiotics must evolve to fully capture their value in addressing the global AMR crisis. Traditional economic evaluations favoring cheaper, older antibiotics fail to account for the negative externalities of resistance development and the positive externalities of effective antimicrobial preservation [101]. The frameworks and data presented herein demonstrate that when appropriately valued, novel antibiotics targeting Gram-negative pathogens provide substantial clinical and economic benefits that justify strategic investment and premium pricing.
Future approaches to antibiotic valuation should incorporate the broader societal benefits of antimicrobial effectiveness, including enablement of modern medical care, reduced transmission of resistant strains, and insurance value against future outbreaks [100] [101]. Additionally, innovative business models delinking antibiotic reimbursement from volume-based sales may be necessary to align economic incentives with antimicrobial stewardship objectives [101]. As Gram-negative bacteria continue to develop resistance mechanisms outpacing traditional discovery approaches, AI-enabled platforms and evolutionary prediction methodologies offer promising avenues for maintaining our antibiotic armamentarium [98] [104].
The economic case for next-generation antibiotics is compelling when analyzed through comprehensive frameworks that acknowledge both the unique challenges of Gram-negative resistance and the profound societal costs of antimicrobial failure.
Conclusion
The fight against antimicrobial resistance in Gram-negative bacteria demands a multi-pronged, globally coordinated strategy. A deep understanding of the foundational resistance mechanisms—from the impermeable cell envelope to the mobile genetic elements that spread resistance genes—is non-negotiable. While current methodologies and treatment guidelines provide a critical framework for action, the alarming rise in resistance to last-resort antibiotics, as highlighted in the latest WHO report, underscores the inadequacy of the existing pipeline. The future of infectious disease treatment hinges on our ability to validate and deploy innovative solutions, including novel antibiotic classes, targeted adjuvant therapies, and non-traditional approaches. Success will require sustained investment, international surveillance, and policies that incentivize antibiotic development, ensuring that the scientific community can outpace the evolutionary ingenuity of these formidable pathogens.
References
- 1. Evaluation of Antibiotic Resistance Mechanisms in Gram ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668847/]
- 2. The Bacterial Cell Envelope - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2857177/]
- 3. Structures of Gram-Negative Cell Walls and Their Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC93954/]
- 4. Distinct Roles of Outer Membrane Porins in Antibiotic ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00953/full]
- 5. 3.4.2: Gram-Negative Wall [https://bio.libretexts.org/Courses/Prince_Georges_Community_College/PGCC_Microbiology/03%3A_Cell_Structure_and_Function/3.04%3A_Prokaryote_Cell_Wall/3.4.02%3A_Gram-Negative_Wall]
- 6. Differing envelope composition of Gram-negative and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425005771]
- 7. Multidrug efflux in Gram-negative bacteria - Nature [https://www.nature.com/articles/s44259-024-00023-w]
- 8. Multidrug efflux pumps in Gram-negative bacteria and their ... [https://pubmed.ncbi.nlm.nih.gov/25405886/]
- 9. Evaluation of Antibiotic Resistance Mechanisms in Gram ... [https://www.mdpi.com/2079-6382/12/11/1590]
- 10. Antibiotic Resistance: A Genetic and Physiological Perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579171/]
- 11. Strategies to combat Gram-negative bacterial resistance ... [https://ophrp.org/journal/view.php?number=740]
- 12. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 13. Mechanism of antibacterial resistance, strategies and next- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1444781/full]
- 14. Emerging antibiotic resistance by various novel proteins/ ... [https://link.springer.com/article/10.1007/s10096-025-05126-4]
- 15. Exploring the principles behind antibiotics with limited ... [https://www.nature.com/articles/s41467-025-56934-3]
- 16. Plasmids, a Molecular Cornerstone of Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440250/]
- 17. Integrons in the development of antimicrobial resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC10500605/]
- 18. Models for Gut-Mediated Horizontal Gene Transfer by ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.891548/full]
- 19. Horizontal Gene Transfer of Antibiotic Resistance Genes in ... [https://www.mdpi.com/2079-6382/12/2/328]
- 20. The evolution of antibiotic resistance islands occurs within ... [https://www.nature.com/articles/s41467-024-48352-8]
- 21. Susceptibility and resistance of Gram-negative bacteria to ... [https://www.frontiersin.org/journals/antibiotics/articles/10.3389/frabi.2025.1615821/full]
- 22. WHO bacterial priority pathogens list, 2024 [https://www.who.int/publications/i/item/9789240093461]
- 23. Mechanisms of Multidrug Antimicrobial Resistance in Gram ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762671/]
- 24. Antimicrobial resistance patterns of WHO priority pathogens at ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03783-1]
- 25. ESKAPE Pathogens in Bloodstream Infections - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524968/]
- 26. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 27. The evolving epidemiology of antimicrobial resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889325001270]
- 28. Resistance of Gram-negative bacteria to aztreonam ... [https://pubmed.ncbi.nlm.nih.gov/40975187/]
- 29. Resistance of Gram-negative bacteria to aztreonam ... [https://www.sciencedirect.com/science/article/abs/pii/S0924857925001797]
- 30. ESKAPE pathogens rapidly develop resistance against ... [https://www.nature.com/articles/s41564-024-01891-8]
- 31. Resistance of Gram-Negative Bacteria to Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7144564/]
- 32. Strategies to combat Gram-negative bacterial resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10626324/]
- 33. WHO releases new reports on new tests and treatments in ... [https://www.who.int/news/item/02-10-2025-who-releases-new-reports-on-new-tests-and-treatments-in-development-for-bacterial-infections]
- 34. Designing development programs for non-traditional ... [https://www.nature.com/articles/s41467-019-11303-9]
- 35. WHO: Reviews of antibacterial therapeutics and ... [https://amr.solutions/2025/10/04/who-reviews-of-antibacterial-therapeutics-and-diagnostics/]
- 36. Emerging antimicrobial therapies for Gram-negative ... [https://www.nature.com/articles/s44259-025-00087-2]
- 37. Non-traditional Antibacterial Therapeutic Options and ... [https://www.sciencedirect.com/science/article/pii/S1931312819302938]
- 38. IDSA 2024 Guidance on the Treatment of Antimicrobial ... [https://www.idsociety.org/practice-guideline/amr-guidance/]
- 39. “Evaluating the susceptibility of MBL carbapenemase ... [https://www.sciencedirect.com/science/article/pii/S0167701225002271]
- 40. Mechanisms of Multidrug Antimicrobial Resistance in Gram ... [https://pubmed.ncbi.nlm.nih.gov/39858349/]
- 41. Understanding antimicrobial resistance (AMR) ... [https://www.sciencedirect.com/science/article/abs/pii/S073288932500272X]
- 42. Global dissemination of npmA mediated pan ... [https://www.nature.com/articles/s41467-025-61152-y]
- 43. Genetic variations underlying aminoglycoside resistance in ... [https://pubmed.ncbi.nlm.nih.gov/39837360/]
- 44. IDSA 2024 Guidance: Managing Antimicrobial-Resistant ... [https://www.contagionlive.com/view/idsa-2024-guidance-key-updates-on-managing-antimicrobial-resistant-gram-negative-infections]
- 45. IDSA 2024 Guidelines for Treatment of Antimicrobial ... [https://www.linksmedicus.com/news/idsa-2024-guidelines-for-treatment-of-antimicrobial-resistant-gram-negative-infections-clin-infect-dis/]
- 46. Infectious Diseases Society of America 2022 ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/35439291/]
- 47. IDSA Guideline Recommendations: Treating Multi-Drug ... [https://www.pharmacytimes.com/view/idsa-guideline-recommendations-treating-multi-drug-resistant-and-difficult-to-treat-resistant-p-aeruginosa]
- 48. Infectious Diseases Society of America 2022 Guidance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9890506/]
- 49. Antimicrobial resistance of Pseudomonas aeruginosa [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1374466/full]
- 50. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 51. WHO: Antimicrobial resistance is widespread globally and ... [https://www.cidrap.umn.edu/antimicrobial-stewardship/who-antimicrobial-resistance-widespread-globally-and-increasing]
- 52. WHO warns of widespread resistance to common ... [https://www.paho.org/en/news/13-10-2025-who-warns-widespread-resistance-common-antibiotics-worldwide]
- 53. Global antimicrobial resistance and use surveillance system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843100/]
- 54. Global Trends in Carbapenem-Resistant Gram-Negative ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1690417/full]
- 55. Trends in the Antimicrobial Resistance Pattern of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566077/]
- 56. Global Antimicrobial Resistance and Use Surveillance ... [https://www.who.int/initiatives/glass]
- 57. New β-Lactam/β-Lactamase Inhibitor Combination Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029989/]
- 58. Promising Future of Novel Beta-Lactam Antibiotics Against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12517300/]
- 59. β-Lactam/β-Lactamase Inhibitor Combination Antibiotics ... [https://www.mdpi.com/2076-0817/14/2/168]
- 60. Breakthrough Advances in Beta-Lactamase Inhibitors [https://www.mdpi.com/1424-8247/18/2/206]
- 61. Efflux pump-mediated resistance to new beta lactam ... [https://www.nature.com/articles/s43856-024-00591-y]
- 62. Antimicrobial resistance and beta-lactamase gene ... [https://www.nature.com/articles/s41598-025-08445-w]
- 63. Antimicrobial Resistance Facts and Stats [https://www.cdc.gov/antimicrobial-resistance/data-research/facts-stats/index.html]
- 64. First antibiotic in 50 years to tackle superbug nears approval [https://www.labiotech.eu/trends-news/antibiotic-development-landscape/]
- 65. Function and Inhibitory Mechanisms of Multidrug Efflux ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.737288/full]
- 66. Types and Mechanisms of Efflux Pump Systems and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10974122/]
- 67. Microbial Efflux Pump Inhibition: Tactics and Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3717411/]
- 68. Therapeutic Bacteriophages for Gram-Negative Bacterial Infections in Animals and Humans - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9596135/]
- 69. Beyond the Resistome: Molecular Insights, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561093/]
- 70. Innovative perspectives on the discovery of small molecule ... [https://www.nature.com/articles/s44259-025-00089-0]
- 71. Frontiers | Emerging roles of bacteriophage-based therapeutics in combating antibiotic resistance [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1384164/full]
- 72. Bacteriophages and antibiotic interactions in clinical practice: what we have learned so far | Journal of Biomedical Science | Full Text [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-022-00806-1]
- 73. Quorum Sensing Inhibitors: An Alternative Strategy to Win ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11313800/]
- 74. Mechanisms of Antimicrobial Peptide Resistance in Gram ... [https://pubmed.ncbi.nlm.nih.gov/25927010/]
- 75. Combating Gram-Negative Infections: The Role of ... [https://www.sciencedirect.com/science/article/pii/S2590006425009524]
- 76. Current economic and regulatory challenges in developing ... [https://www.nature.com/articles/s44259-025-00123-1]
- 77. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 78. Revitalizing the antibiotic pipeline by implementing new ... [https://www.ifpma.org/publications/revitalizing-the-antibiotic-pipeline-by-implementing-new-rd-pull-incentives/]
- 79. Progress (at least some!) towards a global pull incentive [https://amr.solutions/2025/09/15/progress-at-least-some-towards-a-global-pull-incentive/]
- 80. A strategic approach to regulating new antimicrobials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363153/]
- 81. Synergistic Activity of Cefiderocol in Combination with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11352988/]
- 82. Cefiderocol: Systematic Review of Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9220290/]
- 83. In vitro resistance development gives insights into ... [https://www.nature.com/articles/s41429-024-00762-y]
- 84. Investigation of cefiderocol resistance prevalence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584512/]
- 85. Resistance to ceftazidime-avibactam and other new β ... [https://pubmed.ncbi.nlm.nih.gov/38934607/]
- 86. Molecular drivers of resistance to sulbactam-durlobactam ... [https://pubmed.ncbi.nlm.nih.gov/37843305/]
- 87. New Perspectives on Antimicrobial Agents - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486857/]
- 88. IDWeek 2025: Shionogi Presents Real-World and ... [https://www.shionogi.com/us/en/news/2025/10/idweek-2025-shionogi-presents-real-world-and-surveillance-data-reinforcing-role-of-cefiderocol-across-range-of-patient-populations-and-difficult-to-treat-infections.html]
- 89. Ceftazidime-avibactam use selects multidrug-resistance ... [https://www.nature.com/articles/s41467-025-58597-6]
- 90. In vitro antimicrobial activity and resistance mechanisms of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1670179/full]
- 91. Avoiding resistance development to newer drugs [https://pubmed.ncbi.nlm.nih.gov/41241177/]
- 92. Antimicrobial resistance (AMR) [https://www.healthdata.org/research-analysis/health-topics/antimicrobial-resistance-amr]
- 93. About One Health [https://www.cdc.gov/one-health/about/index.html]
- 94. Antimicrobial resistance: One Health approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047147/]
- 95. Newly developed antibiotics against multidrug-resistant ... [https://pubmed.ncbi.nlm.nih.gov/40172627/]
- 96. The development and validation of the One Health Community ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11017337/]
- 97. Stealthy polymer attacks Gram-negative bacteria [https://www.nature.com/articles/d41573-025-00118-7]
- 98. GSK and Fleming Initiative scientists unite to target AMR ... [https://www.gsk.com/en-gb/media/press-releases/gsk-and-fleming-initiative-scientists-unite-to-target-amr-with-advanced-ai/]
- 99. The social burden of antimicrobial resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11891513/]
- 100. Estimating the value of new antibiotic treatment strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11367305/]
- 101. Overcoming challenges in the economic evaluation of ... [https://www.nature.com/articles/s43856-024-00516-9]
- 102. Drugmakers announce encouraging new antibiotic data at ... [https://www.cidrap.umn.edu/antimicrobial-stewardship/drugmakers-announce-encouraging-new-antibiotic-data-idweek]
- 103. A trial-based cost-effectiveness analysis of antibiotic ... [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-023-04235-3]
- 104. Quantitative systems-based prediction of antimicrobial ... [https://www.nature.com/articles/s41540-023-00304-6]