Boosting Drug Success Rates: A 2024 Guide to PK/PD Target Attainment Analysis and Optimization
This comprehensive guide explores advanced strategies for improving Pharmacokinetic/Pharmacodynamic (PK/PD) target attainment rates in modern drug development.
Boosting Drug Success Rates: A 2024 Guide to PK/PD Target Attainment Analysis and Optimization
Abstract
This comprehensive guide explores advanced strategies for improving Pharmacokinetic/Pharmacodynamic (PK/PD) target attainment rates in modern drug development. Targeting researchers and drug development professionals, it systematically covers the foundational principles of PK/PD relationships, state-of-the-art methodologies including population PK/PD and machine learning applications, common challenges in clinical translation, and rigorous validation techniques. The article provides a practical framework for designing more efficacious and precise dosing regimens, ultimately aiming to increase clinical trial success rates and accelerate the delivery of optimized therapeutics to patients.
Understanding PK/PD Target Attainment: The Bedrock of Rational Dosing
Troubleshooting Guides & FAQs
Q1: My in vivo efficacy results are inconsistent with predictions based on a static PK/PD index. What could be wrong? A: This is often due to overlooking the dynamic nature of the PK/PD relationship. Static indices (single-point Cmax/MIC or AUC/MIC) ignore the time-course of concentration. For time-dependent antibiotics (e.g., β-lactams), failing to maintain T>MIC above the target threshold (e.g., 40-70% of dosing interval) is a common culprit. Ensure your in vitro PK/PD model simulates human or animal pharmacokinetics accurately, including the appropriate elimination half-life.
Q2: How do I decide whether Cmax/MIC, AUC/MIC, or T>MIC is the correct predictive index for my new antimicrobial? A: The primary driver is the mechanism of action and pattern of bacterial killing.
- T>MIC: Primary index for time-dependent antibiotics with minimal to moderate persistent effects (e.g., β-lactams, glycopeptides). Killing plateaus above 4-5x MIC.
- AUC/MIC: Primary index for concentration-dependent antibiotics with significant persistent effects (e.g., fluoroquinolones, aminoglycosides, azithromycin). Correlates with both killing and resistance suppression.
- Cmax/MIC: Critical for concentration-dependent antibiotics where high peak levels enhance efficacy and/or suppress resistance (e.g., aminoglycosides, daptomycin). Often targeted to be >8-10 for optimal effect.
Table 1: Primary PK/PD Indices and Characteristics for Key Antibiotic Classes
| Antibiotic Class | Primary PK/PD Index | Typical Target for Stasis | Key Mechanism/Reasoning |
|---|---|---|---|
| β-Lactams (Penicillins, Cephalosporins) | T>MIC | 30-70% of dosing interval | Time-dependent killing; minimal post-antibiotic effect (PAE). |
| Glycopeptides (Vancomycin) | AUC/MIC (AUC24/MIC) | ≥400 (for S. aureus) | Time-dependent killing; moderate PAE. AUC/MIC is a surrogate for T>MIC. |
| Fluoroquinolones | AUC/MIC | 30-100 (varies by organism) | Concentration-dependent killing; long PAE; prevents resistance. |
| Aminoglycosides | Cmax/MIC | 8-10 | Concentration-dependent killing; moderate PAE; efficacy and resistance suppression linked to peak. |
| Azithromycin | AUC/MIC | >25 | Long PAE and extensive tissue distribution make AUC/MIC most predictive. |
Q3: During dose fractionation studies, my results are inconclusive. What are the critical protocol steps? A: Dose fractionation is the gold standard experimental method to identify the definitive PK/PD index. Common pitfalls include:
- Insufficient Dose Range: The study must include a wide range of total daily doses (e.g., spanning from non-effective to fully effective) and fractionate each total dose into different dosing intervals (e.g., Q24h, Q12h, Q8h, Q6h).
- Incorrect PK Simulation: The in vitro model (or animal model dosing regimen) must accurately simulate human single-dose PK profiles for each regimen. Validate the simulated half-life and AUC.
- Endpoint Sensitivity: Use multiple endpoints (e.g., log10 CFU reduction at 24h, net stasis, area under the bacterial kill curve) to robustly differentiate between index correlations.
Experimental Protocol: Standard Dose Fractionation Study in a Neutropenic Murine Thigh Infection Model
Objective: To determine the primary PK/PD index (AUC/MIC, Cmax/MIC, T>MIC) predictive of efficacy for a novel antimicrobial.
Key Reagent Solutions:
- Test Organism: Clinical isolate with precisely determined MIC in CAMHB.
- Animals: Immunosuppressed (neutropenic) mice (e.g., ICR or Swiss Webster).
- Drug Formulation: Sterile, pH-adjusted solution suitable for subcutaneous (SC) or intraperitoneal (IP) administration.
- Growth Medium: Cation-adjusted Mueller Hinton Broth (CAMHB).
- Homogenization Medium: Sterile saline with inactivators (e.g., charcoal for fluoroquinolones).
Methodology:
- Induce Neutropenia: Administer cyclophosphamide (e.g., 150 mg/kg and 100 mg/kg IP) 4 days and 1 day pre-infection.
- Infect Thighs: Inoculate both thighs of anesthetized mice with ~10^6 CFU of bacteria in a small volume (0.1 mL).
- Initiate Therapy: Two hours post-infection, begin treatment with the test compound.
- PK/PD Regimen Design:
- Total Dose Range: Include 4-5 total daily doses (from sub-therapeutic to maximally effective).
- Fractionation: For each total dose, administer via SC route in 1, 2, 4, 8, or 12 equally divided doses over 24h.
- Control Groups: Include untreated (growth control) and zero-time (initial inoculum) cohorts.
- Assess Outcome: Sacrifice mice 24h after therapy start. Excise and homogenize thighs. Perform serial dilutions and plate for CFU determination.
- Data Analysis:
- Plot the log10 CFU/thigh against each of the three PK/PD indices (AUC/MIC, Cmax/MIC, %T>MIC) for all regimens.
- The index that produces the tightest correlation (highest R²) and collapses all data onto a single exposure-response curve is identified as the predictive driver.
Research Reagent Solutions Toolkit
Table 2: Essential Materials for PK/PD Index Determination Experiments
| Item | Function & Importance |
|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for MIC determination and in vitro PK/PD models, ensuring consistent cation concentrations. |
| In Vitro Pharmacodynamic Models (e.g., Hollow Fiber, Biofilm Reactors) | Systems that simulate human PK profiles (multi-exponential half-lives) for concentration-time course studies without animal use. |
| Murine Infection Model Supplies (Cyclophosphamide, Homogenizer) | Enables creation of a neutropenic host environment to study drug effect without immune interference. |
| LC-MS/MS System | Gold standard for accurate, specific measurement of drug concentrations in plasma/tissue for PK parameter calculation. |
| Population PK/PD Modeling Software (e.g., NONMEM, Monolix) | For integrating sparse or heterogeneous data to quantify exposure-response relationships and identify covariates. |
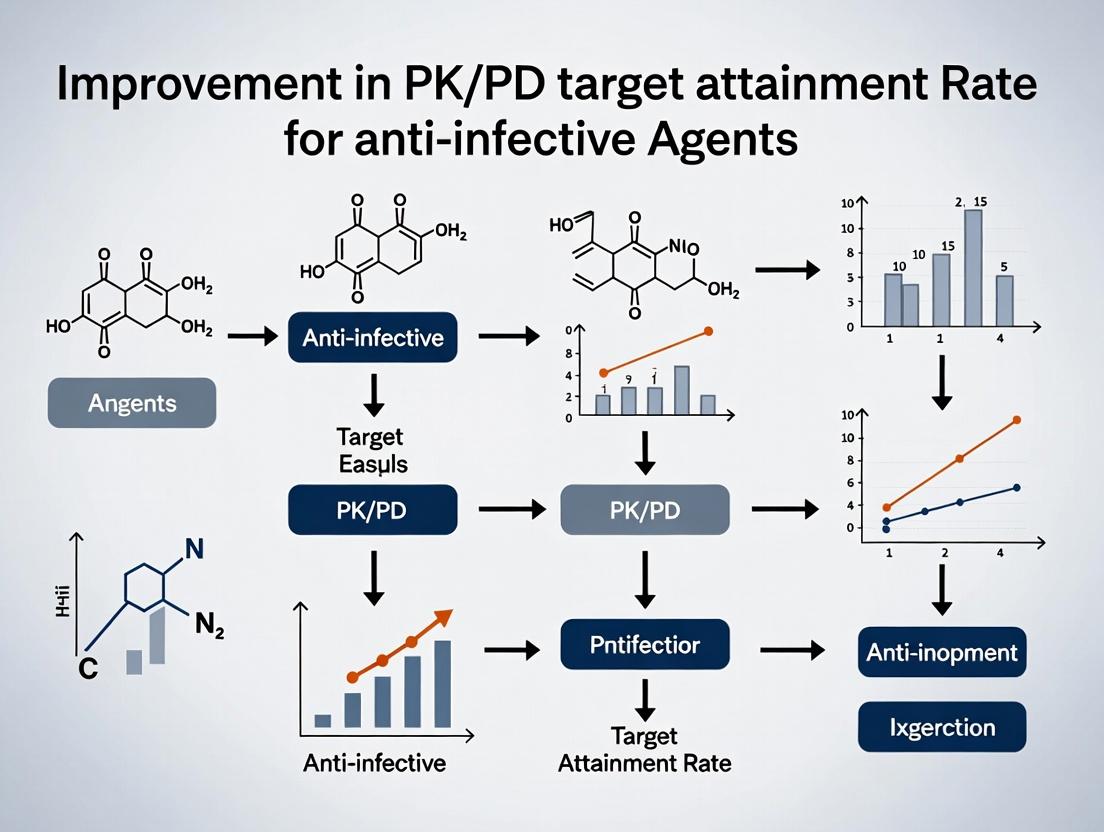
Visualizing PK/PD Index Determination
Title: Workflow to Determine Predictive PK/PD Index
Title: How PK Indices Predict Microbial Kill Curves
The Role of Target Attainment Analysis in Dose Selection and Rationale.
Technical Support Center: Troubleshooting Target Attainment Analysis
This support center addresses common challenges in PK/PD target attainment analysis, a core methodology for dose rationale. Effective troubleshooting ensures robust data for improving target attainment rates in drug development.
FAQs & Troubleshooting Guides
Q1: My stochastic simulations show wildly variable target attainment rates (TAR) for the same dose. What could be the cause? A: This often points to inadequate characterization of pharmacokinetic (PK) and pharmacodynamic (PD) variability. Key checks:
- Verify Parameter Distributions: Ensure the mean, variance, and covariance of your PK parameters (e.g., Clearance, Volume) are correctly specified in your population model. Incorrect covariance (e.g., between CL and Vd) can inflate variability.
- Check for Model Misspecification: A one-compartment model may be insufficient for your drug. Re-evaluate structural PK and PD models using diagnostic plots.
- Confirm Number of Simulated Subjects: For robust TAR estimation, simulate at least 1000-2000 virtual subjects per trial. Fewer subjects lead to unstable TAR estimates.
Q2: During external validation, my model-predicted TAR does not match observed clinical outcomes. How should I proceed? A: This discrepancy calls for a systematic review of the target attainment analysis pipeline.
- Reassess the PK/PD Target: The most common issue is an inappropriate PK/PD index (e.g., fAUC/MIC vs. fT>MIC) or target value. Revisit preclinical and early clinical data.
- Audit Input Data: Ensure the MIC distribution or target biomarker distribution used for simulation reflects the validation population.
- Evaluate Model Transportability: Did the patient population, supportive care, or clinical practice differ significantly? The model may need refinement for the new context.
Q3: What is the optimal way to present dose rationale based on TAR to regulatory agencies? A: Clarity and justification are paramount. Structure your submission with:
- A clear statement of the PK/PD target and its justification.
- A summary table of TAR for candidate doses (see Table 1).
- A visualization of the decision logic (see Diagram 1).
- Sensitivity analyses showing TAR robustness to key assumptions.
Q4: How do I handle time-dependent toxicity when defining the therapeutic window for TAR? A: Integrate safety endpoints into your analysis.
- Step 1: Define a safety PK metric (e.g., Cmax, AUC over a period) and a threshold from Phase I data.
- Step 2: Run simulations that capture both efficacy (TAR) and the probability of exceeding the safety metric.
- Step 3: Present a combined probability plot or table to identify doses that maximize TAR while keeping the safety exceedance probability below an acceptable limit (e.g., <5%).
Experimental Protocol: Performing a Monte Carlo Simulation for Target Attainment
Objective: To estimate the probability of attaining a predefined PK/PD target for a proposed dosing regimen in a target patient population.
Materials & Reagents (The Scientist's Toolkit):
| Research Reagent / Solution | Function in Experiment |
|---|---|
| Validated Population PK Model | Describes the typical PK parameters and their inter-individual variability (IIV) and covariance in the population. |
| Pathogen MIC Distribution (for anti-infectives) | A database of minimum inhibitory concentrations for the target pathogen, defining the ecological challenge. |
| PD Target Value (e.g., fAUC/MIC > 50) | The breakpoint value linked to clinical efficacy, derived from preclinical/clinical studies. |
| Statistical Software (e.g., R, NONMEM, SAS) | Platform for running stochastic simulations and calculating probabilities. |
| Virtual Population Demographics | Covariate distributions (weight, age, renal function) to inform parameter sampling. |
Methodology:
- Define Scenario: Fix the dosing regimen (dose, interval, infusion time).
- Generate Virtual Population: Sample covariates for 2000 virtual subjects from the target demographic distributions.
- Sample PK Parameters: For each virtual subject, sample a set of PK parameters (CL, Vd, etc.) from the multivariate distribution defined by the population PK model, incorporating the subject's covariates.
- Simulate PK Profiles: Using the sampled parameters, simulate the concentration-time profile for each subject over the desired interval.
- Calculate PK/PD Index: For each subject, calculate the relevant PK/PD index (e.g., free drug AUC over 24h).
- Introduce PD Variability: Sample a "challenge" for each subject (e.g., an MIC from the pathogen distribution) or apply a fixed PD target.
- Determine Attainment: For each subject, check if the calculated PK/PD index meets or exceeds the target value.
- Compute TAR: The TAR is the proportion of the virtual population achieving target attainment.
Data Presentation
Table 1: Example TAR Comparison for Candidate Dosing Regimens Against a Pathogen MIC Distribution PD Target: fAUC₀₂₄/MIC ≥ 100 for stasis. Target Population: 2000 virtual patients with community-acquired pneumonia.
| Dosing Regimen | Probability of Target Attainment (PTA) at MIC (mg/L) | Overall TAR | ||||
|---|---|---|---|---|---|---|
| 0.12 mg/L | 0.5 mg/L | 1 mg/L | 2 mg/L | 4 mg/L | ||
| Drug A 500 mg q24h | 99.8% | 98.5% | 85.2% | 52.1% | 15.3% | 70.2% |
| Drug A 750 mg q24h | 100% | 99.7% | 96.0% | 78.9% | 35.4% | 81.8% |
| Drug A 500 mg q12h | 100% | 100% | 99.5% | 92.3% | 65.7% | 91.5% |
Mandatory Visualizations
Diagram 1: Target Attainment Analysis Workflow for Dose Selection
Diagram 2: PK/PD Target Attainment Logic Tree
Technical Support Center: PK/PD Target Attainment Troubleshooting
Troubleshooting Guides & FAQs
FAQ 1: Why is my observed PK variability in the target population much higher than in pre-clinical species?
- Answer: Higher-than-expected pharmacokinetic (PK) variability in humans is common. Key culprits to investigate include:
- Uncharacterized Polymorphisms: Check for genetic polymorphisms in metabolizing enzymes (e.g., CYP2C9, CYP2C19) or transporters (e.g., P-gp, OATP1B1) relevant to your compound.
- Drug-Drug Interactions (DDIs): Review concomitant medications in your study population. Unanticipated enzyme inhibition/induction can drastically alter exposure.
- Formulation Issues: In vivo dissolution and bioavailability may differ from predictions. Consider conducting a bioequivalence assessment.
- Protocol Non-Adherence: Review sample timing accuracy and subject compliance records.
- Recommended Action: Implement population PK (PopPK) modeling to quantify variability sources and covariate effects (e.g., weight, renal function).
FAQ 2: My exposure-response (E-R) analysis shows a flat relationship. What could be wrong?
- Answer: A flat E-R curve suggests a lack of association between drug exposure and the measured pharmacodynamic (PD) endpoint. Potential issues are:
- Incorrect Exposure Metric: The tested metric (e.g., C~trough~, C~max~, AUC) may not drive the effect. Explore other PK metrics (e.g., time above MIC, average concentration).
- Insufficient Exposure Range: The administered doses may not produce a wide enough exposure spread to see a response gradient.
- Inappropriate PD Biomarker: The biomarker may not be mechanistically linked to the clinical outcome or may have a high measurement error or lag time.
- Saturation of Effect: The response may already be maximal at the lowest doses tested.
- Recommended Action: Re-analyze using exposure metrics aligned with the drug's mechanism. If possible, include data from a wider dose range.
FAQ 3: How can I define the therapeutic window when clinical efficacy data is limited?
- Answer: In early development, the therapeutic window can be informed by integrating all available data:
- Preclinical Safety Margins: Use exposure multiples (e.g., human C~max~ at proposed dose vs. NOAEL in toxicology species).
- Target Engagement Biomarkers: Define the exposure required for ≥90% target occupancy or pathway modulation.
- Surrogate Efficacy Endpoints: Use quantitative systems pharmacology (QSP) models to link preclinical PD to predicted human efficacy.
- Early Clinical Safety Signals: Integrate PK data from SAD/MAD studies with emerging safety signals (e.g., QTc prolongation) to establish an initial upper bound.
- Recommended Action: Create an integrated PK/PD/Safety model to simulate probability of target attainment and toxicity across doses.
FAQ 4: My PopPK model fails to converge. What are the typical fixes?
- Answer: Non-convergence often stems from model over-parameterization or data issues.
- Simplify the Model: Remove non-significant covariates one at a time. Consider reducing the number of random effects.
- Check Data: Identify and review outliers. Ensure dose and sampling records are accurate. Confirm units are consistent.
- Adjust Estimation Settings: Increase the number of significant digits (SIGDIG). Try a different estimation method (e.g., FOCE with INTERACTION).
- Improve Initial Estimates: Use results from a base model or literature to provide better initial parameter estimates.
- Recommended Action: Use a stepwise covariate modeling approach. Always start with a robust base model before adding complexity.
Table 1: Common Sources of PK Variability and Their Magnitude Impact
| Variability Source | Typical Impact on AUC Variability (CV%) | Mitigation Strategy |
|---|---|---|
| Food Effects | 20% - 50% | Standardize dosing conditions in trials |
| Hepatic Impairment (Moderate) | 40% - 100%+ | Conduct dedicated hepatic impairment study |
| Strong CYP3A4 Inhibitor (Co-administration) | 200% - 500%+ | Include DDI assessment in development plan |
| Genetic Polymorphism (e.g., CYP2D6 PM vs EM) | 300% - 1000%+ | Consider pre-emptive genotyping in trials |
| Formulation Change (Major) | 25% - 70% | Early investment in formulation development |
Table 2: Key PK/PD Indices for Common Drug Classes
| Drug/Therapeutic Class | Critical PK/PD Index | Typical Target Attainment Goal | Notes |
|---|---|---|---|
| Beta-lactam Antibiotics | %T > MIC (Time above MIC) | 50-70% of dosing interval | Target depends on pathogen and site of infection. |
| Antivirals (e.g., HIV Protease Inhibitors) | C~trough~ / IC~50~ | Ratio > 1 | Prevents resistance emergence. |
| Oncology Kinase Inhibitors | AUC~0-24~ / IC~50~ or C~trough~ / IC~50~ | Ratio > 1 | Target varies by mechanism (cytostatic vs. cytotoxic). |
| Antihypertensives | Average Steady-State Concentration (C~ss,av~) | Maintain within population-defined range | E-R often flat within window; goal is to minimize variability. |
Experimental Protocols
Protocol 1: Establishing an Exposure-Response Relationship for a Novel Analgesic
- Objective: To quantify the relationship between drug exposure and pain score reduction.
- Design: Randomized, placebo-controlled, multiple ascending dose study with intensive PK and PD sampling.
- Methodology:
- Dosing: Subjects receive placebo or one of four active doses (BID) for 7 days.
- PK Sampling: Serial blood samples over 12h on Day 1 and Day 7 for full PK profile. Trough samples on other days.
- PD Assessment: Pain intensity scores (0-10 NRS) recorded electronically at pre-dose and at 0.5, 1, 2, 4, 6, 8, 12h post-dose on Days 1 & 7. AUC of pain relief calculated.
- Analysis: Link model-predicted individual exposure (AUC~0-12~, C~max~) to change in pain AUC using an E~max~ model: E = E~0~ + (E~max~ * C) / (EC~50~ + C). Model parameters are estimated using non-linear mixed-effects modeling.
Protocol 2: Evaluating the Impact of a Covariate on PK via Population PK Modeling
- Objective: To quantify the effect of renal impairment on drug clearance.
- Design: Retrospective analysis of pooled Phase I and II data.
- Methodology:
- Data Assembly: Pool all PK concentrations, dosing records, and subject covariates (weight, age, sex, creatinine clearance [CrCl]).
- Base Model Development: Develop structural (1- or 2-compartment) and statistical (inter-individual, residual variability) models using NONMEM or similar.
- Covariate Testing: Test the relationship between CrCl and clearance (CL) using a power model: CL~i~ = θ~pop~ * (CrCl~i~ / 100)^θ~CrCl~ * exp(η~i~).
- Model Evaluation: Use diagnostic plots (GOF, VPC), likelihood ratio test (for nested models), and impact on shrinkage to select the final model. Simulate exposures in severe renal impairment to guide dose adjustment.
Visualizations
Diagram Title: Interplay of Key PK/PD Determinants
Diagram Title: Target Attainment Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Function in PK/PD Research | Example Vendor/Product (Illustrative) |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Essential for precise and accurate quantitation of drug and metabolite concentrations in complex biological matrices (plasma, tissue) using LC-MS/MS. | Cambridge Isotope Laboratories; Clearsynth |
| Recombinant Human CYP Enzymes & Cofactors | Used for in vitro reaction phenotyping to identify primary metabolic pathways and predict risk of DDIs and polymorphic metabolism. | Corning Gentest Supersomes; Thermo Fisher Scientific Baculosomes |
| Human Hepatocytes (Cryopreserved) | Gold-standard in vitro system for assessing hepatic clearance, metabolic stability, and metabolite profiling. | BioIVT; Lonza |
| Phospho-Specific Antibodies & ELISA Kits | To measure target engagement and downstream pathway modulation (PD biomarkers) in preclinical studies and clinical trial samples. | Cell Signaling Technology; R&D Systems |
| Population PK/PD Modeling Software | For data analysis, model development, and simulation to quantify variability, E-R relationships, and predict target attainment. | NONMEM; Monolix; Phoenix NLME |
| PBPK Simulation Software | To predict human PK, assess DDI potential, and explore covariate effects (e.g., organ impairment) prior to first-in-human studies. | GastroPlus; Simcyp Simulator |
The pursuit of optimal target attainment (TA) rates is central to modern pharmacokinetic-pharmacodynamic (PK/PD) research and drug development. A "good" TA rate is not a universal constant but is highly context-dependent, influenced by disease severity, therapeutic index, and the consequences of subtherapeutic or toxic exposure. This technical support center provides troubleshooting guidance for common experimental challenges in this field, framed within a thesis on improving TA rates.
Key Benchmark Data for 2024
The following table summarizes recent industry benchmarks for TA rates across different therapeutic areas, based on current literature and clinical development targets.
| Therapeutic Area / Context | "Good" Target Attainment Rate Benchmark (2024) | Key Influencing Factors | Typical PK/PD Index Targeted |
|---|---|---|---|
| Non-severe Bacterial Infections (Oral Outpatient) | ≥ 90% | Pathogen MIC distribution, drug PK variability, adherence. | fT > MIC, AUC/MIC |
| Severe/Hospital-Acquired Infections (IV) | ≥ 95% | Highly variable PK in critically ill, resistant pathogens. | fT > MIC, AUC/MIC |
| Oncology (Cytotoxic) | 80 - 90% | Narrow therapeutic index, high inter-patient variability. | AUC, Cmax |
| Oncology (Targeted Therapies) | ≥ 85% | Presence of biomarkers, saturation of target pathway. | Ctrough, AUC |
| Chronic Diseases (e.g., Hypertension, Diabetes) | ≥ 80% | Long-term safety, pill burden, quality of life. | Ctrough |
| Drug Development (Phase II/III Goal) | ≥ 80% (POC) → ≥ 90% (Pivotal) | Proof-of-concept vs. definitive trial requirements. | Context-specific |
Troubleshooting Guides & FAQs
FAQ 1: During a population PK (PopPK) simulation to predict TA, my results show wide variability (>40% CV) for key parameters. How can I troubleshoot this?
- Answer: High variability in simulated exposure can stem from several sources in your model.
- Check Structural Model Inputs: Verify the covariance matrix from your base PopPK model. Ensure the omega (η) and sigma (ε) values (variance for inter-individual and residual variability) are correctly input into your simulation software (e.g.,
mrgsolve,NONMEM). Overestimated omegas will inflate variability. - Examine Covariate Relationships: Poorly estimated covariate relationships (e.g., renal function on clearance) can propagate error. Re-evaluate the strength of these relationships in your source model. Consider if your virtual population accurately reflects the target population's covariate distributions.
- Validate Sampling Times: Ensure your simulated sampling schedule aligns with real-world scenarios. Sparse sampling in critical absorption/distribution phases can artificially increase variability.
- Protocol: Re-run the simulation using a fixed set of parameters (no variability) to establish a baseline. Then, reintroduce variability components (IIV, RUV) one at a time to identify the primary source of the inflated CV.
- Check Structural Model Inputs: Verify the covariance matrix from your base PopPK model. Ensure the omega (η) and sigma (ε) values (variance for inter-individual and residual variability) are correctly input into your simulation software (e.g.,
FAQ 2: When validating a PD biomarker as a surrogate for target attainment, the correlation with clinical outcome is weak (R² < 0.4). What are the next steps?
- Answer: A weak correlation suggests the biomarker may not be a suitable standalone surrogate.
- Troubleshoot Biomarker Measurement:
- Assay Validation: Confirm the precision and accuracy of your biomarker assay. High intra-assay variability can obscure true correlations.
- Temporal Misalignment: Ensure the biomarker is measured at the optimal time point relative to drug exposure and clinical effect. Create a detailed PK/PD sampling timeline.
- Pathway Specificity: Verify the biomarker is directly on the intended drug's MOA pathway. Upstream/downstream factors may cause disconnect.
- Protocol for Correlation Improvement: Design a focused study:
- Cohort: Enroll a homogeneous patient subgroup (e.g., specific genotype, disease stage).
- Sampling: Take rich PK samples concurrently with biomarker measurement.
- Analysis: Use a model-based approach (e.g., indirect response model) to relate drug concentration to biomarker response over time, rather than a simple linear correlation at a single time point.
- Troubleshoot Biomarker Measurement:
FAQ 3: My model-based meta-analysis (MBMA) for deriving a TA benchmark is highly sensitive to one or two outlier studies. How should I proceed?
- Answer: Sensitivity to outliers is common and must be transparently addressed.
- Systematic Outlier Investigation:
- Quality Assessment: Re-appraise the outlier studies using a tool like Cochrane Risk of Bias. Differences in study design, patient population, or endpoint measurement can justify their exclusion.
- Dose/Exposure Reconciliation: Check if dosing regimens or reported exposures in the outlier studies are plausible. Conversion errors (e.g., mg/kg to flat dose) are common.
- Protocol for Robust Analysis:
- Perform the MBMA with and without the outlier studies.
- Use statistical methods robust to outliers (e.g., median-based pooling, Bayesian models with heavy-tailed distributions) if exclusion is not justified.
- Clearly report both results in your thesis, discussing the potential reasons for the outlier effect and its implications for the proposed benchmark.
- Systematic Outlier Investigation:
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in PK/PD TA Research |
|---|---|
| Stable Isotope-Labeled Internal Standards (e.g., ¹³C, ²H) | Essential for LC-MS/MS bioanalysis to ensure accurate and precise quantification of drug concentrations in complex biological matrices by correcting for matrix effects and recovery variability. |
| Recombinant Human Enzymes / Transporters | Used in in vitro studies to characterize metabolic pathways (CYP450) and transporter interactions (P-gp, BCRP), informing potential DDIs and variability sources. |
| Validated Phospho-Specific Antibodies | For quantifying target engagement and downstream pathway modulation (PD biomarkers) in cell-based assays or tissue samples via Western blot or immunofluorescence. |
| Physiologically Based PK (PBPK) Software (e.g., GastroPlus, Simcyp) | Platform for in silico simulation of drug absorption, distribution, and elimination, crucial for predicting TA in special populations and planning clinical studies. |
| Population PK/PD Modeling Software (e.g., NONMEM, Monolix) | Gold-standard tools for analyzing sparse, real-world PK/PD data, quantifying variability, and performing Monte Carlo simulations to predict TA rates. |
Experimental & Conceptual Diagrams
Diagram 1: PK/PD TA Rate Improvement Research Workflow (77 chars)
Diagram 2: Factors Influencing Target Attainment Rate (74 chars)
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During preclinical PK/PD bridging, the predicted human efficacious dose from my allometric scaling is several-fold higher than expected from the animal NOAEL. What could be the cause and how should I proceed?
A: This discrepancy often arises from species differences in target expression, binding affinity, or metabolic clearance pathways.
- Troubleshooting Steps:
- Re-evaluate Scaling Exponent: Verify you used the correct allometric exponent (e.g., 0.75 for clearance, 0.90 for volume). Consider using species-invariant time methods (e.g., Dedrick plots) as a cross-check.
- Assess Protein Binding: Measure unbound fraction (fu) in human and preclinical species plasma. Use unbound drug concentrations for cross-species PK/PD comparisons.
- Validate Target Engagement Assays: Confirm that your PD biomarker (e.g., receptor occupancy, pathway modulation) shows similar saturation kinetics relative to unbound plasma concentrations across species.
- PBPK Modeling: Develop a preliminary PBPK model to integrate in vitro data (metabolism, permeability) and identify nonlinear processes.
Q2: My lead candidate shows excellent efficacy in murine disease models, but the required target engagement (>90% receptor occupancy) is not sustained through the dosing interval in non-human primate (NHP) studies. How can I modify the formulation or dosing regimen?
A: This indicates a potential mismatch between drug half-life and the required PD effect duration.
- Troubleshooting Steps:
- PK/PD Modeling: Fit an Emax or indirect response model to the NHP data. Determine if increasing the dose (Cmax-driven) or dosing frequency (time above threshold) would achieve the target.
- Formulation Strategies: Explore controlled-release formulations (e.g., sustained-release injectables, osmotic pumps) if the issue is short half-life.
- Prodrug Approach: Investigate a prodrug to improve solubility or absorption, thereby flattering the PK profile.
- Safety Margin Check: Ensure any proposed dose increase remains within the projected human safety window from toxicology studies.
Q3: When transitioning from total plasma concentration to unbound concentration modeling for target attainment, what are the critical assay validation parameters for measuring protein binding?
A: Accurate measurement of the unbound fraction (fu) is critical for translational predictions.
- Key Validation Parameters:
- Equilibrium Confirmation: Demonstrate that equilibrium is reached within the incubation time.
- Nonspecific Binding: Account for drug binding to the assay apparatus (e.g., ultrafiltration device, dialysis membrane) using buffer controls.
- Concentration Independence: Test fu across a relevant concentration range (including expected Cmax) to rule out saturation of binding sites.
- Stability: Confirm drug stability in the matrix under assay conditions (pH, temperature, time).
- Reproducibility: Establish intra- and inter-assay precision (CV < 15%).
Table 1: Common Allometric Scaling Exponents for Human PK Prediction
| PK Parameter | Allometric Exponent (Y=a·W^b) | Typical Range | Key Consideration |
|---|---|---|---|
| Clearance (CL) | 0.75 | 0.65 - 0.80 | Use unbound CL if drug exhibits high species difference in protein binding. |
| Volume of Distribution (Vd) | 1.00 | 0.80 - 1.20 | Often scales linearly with body weight. Highly lipophilic drugs may deviate. |
| Half-life (t1/2) | 0.25 | (Derived) | Not scaled directly; calculated from scaled CL and Vd. |
Table 2: Common In Vitro to In Vivo Scaling Factors for Hepatic Clearance
| Scaling System | Scaling Factor | Purpose | Common Assumption/Limitation |
|---|---|---|---|
| Hepatocytes (Suspension) | Microsomal Protein per gram liver (MPPGL) ~45 mg/g | Scale intrinsic clearance (CLint) from microsomes. | Assumes all clearance is microsomal. Underpredicts for phase II or extra-hepatic metabolism. |
| Hepatocytes (Suspension) | Hepatocyte count per gram liver (~120 million cells/g) | Scale CLint from hepatocytes. | More comprehensive than microsomes. Sensitive to cell viability and functionality. |
| Well-Stirred Model | Liver Blood Flow (QH), Blood-to-Plasma Ratio | Predict in vivo hepatic clearance (CLH). | CLH = (QH · fu · CLint) / (QH + fu · CLint) |
Experimental Protocols
Protocol 1: Determination of Unbound Fraction (fu) Using Rapid Equilibrium Dialysis (RED)
- Principle: Equilibrium dialysis separates buffer from plasma containing the drug via a semi-permeable membrane, allowing unbound drug to equilibrate.
- Methodology:
- Spiking: Spike the test compound into pooled human or animal plasma to a concentration ~10x above anticipated KD.
- Assembly: Load the plasma chamber with 100 µL of spiked plasma. Load the buffer chamber (opposite side of membrane) with PBS (pH 7.4).
- Incubation: Assemble RED device and incubate at 37°C with gentle orbital rotation for 4-6 hours (validate equilibrium time).
- Post-Incubation: Post-incubation, aliquot equal volumes from both plasma and buffer chambers.
- Matrix Matching: To the buffer sample, add an equal volume of blank plasma. To the plasma sample, add an equal volume of blank PBS. This corrects for matrix effects in LC-MS/MS analysis.
- Analysis: Quantify drug concentrations in both matrices via LC-MS/MS.
- Calculation: fu = (Concentration in Buffer Chamber) / (Concentration in Plasma Chamber).
Protocol 2: In Vivo Target Engagement Assay (Receptor Occupancy via PET)
- Principle: A radiolabeled tracer ligand competes with the unlabeled therapeutic for target binding. Displacement indicates target engagement by the drug.
- Methodology:
- Tracer Selection: Select a high-affinity, selective PET radioligand for the target (e.g., [¹¹C]raclopride for D2 receptors).
- Baseline Scan: Administer tracer to an animal/subject and perform a baseline PET scan to determine total binding potential (BPND).
- Drug Administration: Administer the therapeutic candidate at a planned dose.
- Post-Dose Scan: At a predetermined time post-dose (e.g., Tmax), administer the same dose of tracer and perform a second PET scan.
- Image Analysis: Generate parametric maps of BPND for both scans using a reference tissue model.
- Calculation: Receptor Occupancy (%) = [(BPNDbaseline – BPNDpost-dose) / BPND_baseline] × 100.
Diagrams
Diagram 1: Translational PK/PD Workflow from Preclinical to FIH
Translational PK/PD Workflow from Preclinical to FIH
Diagram 2: Key Relationships for Target Attainment Analysis
Key Relationships for Target Attainment Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Translational PK/PD Experiments
| Item | Function/Benefit | Example/Consideration |
|---|---|---|
| Species-Specific Plasma | For protein binding (fu) assays and matrix-matched calibration standards. | Use pooled, anticoagulated plasma from ≥3 donors. K2EDTA is common. |
| Recombinant Human Target Protein | For developing binding (SPR/BLI) or activity assays to determine KD/IC50. | Ensure correct post-translational modifications. |
| Validated PD Biomarker Assay Kit | To quantify target modulation (e.g., phospho-protein, gene expression). | Prioritize kits validated for relevant species (mouse, rat, NHP, human). |
| Stable Isotope-Labeled Internal Standards | For accurate, precise LC-MS/MS bioanalysis of drug concentrations in complex matrices. | Use deuterated or ¹³C-labeled analogs of the analyte. |
| PBPK/PD Modeling Software | To integrate in vitro, preclinical, and physicochemical data for human prediction. | Platforms: GastroPlus, Simcyp, PK-Sim, Berkeley Madonna. |
Advanced Methods for Modeling and Maximizing Target Attainment
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During model estimation with NONMEM, I encounter error messages like "TERMINATED DUE TO ROUNDING ERRORS" or "MINIMIZATION SUCCESSFUL BUT HESSIAN FAILED." What are the primary causes and solutions?
- A: These errors typically indicate problems with the model structure, initial estimates, or data.
- Check Initial Estimates: Ensure your initial parameter estimates (
THETA,OMEGA,SIGMA) are biologically plausible and not too close to zero or boundary values. Use simple models (e.g., base structural model) to get stable estimates first. - Simplify the Model: Temporarily remove random effects (e.g., set
OMEGAto a small fixed value) or covariates to see if estimation succeeds. Re-introduce complexity gradually. - Examine Data: Look for outliers, dosing records without corresponding concentrations, or extremely sparse profiles that may cause instability. Consider data stratification.
- Boundary Parameters: Check if parameters (e.g., clearance, volume) are hitting upper/lower bounds. Redefine boundaries or reparameterize the model.
- Use Alternative Estimation Methods: Switch from First Order Conditional Estimation (FOCE) to Importance Sampling (IMP) or Stochastic Approximation Expectation-Maximization (SAEM).
- Check Initial Estimates: Ensure your initial parameter estimates (
Q2: How should I handle BLOQ (Below Limit of Quantification) data in my population PK analysis to avoid bias?
- A: The M3 and M6 methods (as described by Beal) are recommended over discarding or simple substitution.
- Protocol: Implement the
M3method in NONMEM. This uses the likelihood for measurements above the LOQ and the cumulative probability for BLOQ observations. It requires the$M3data item flag and appropriate$ESTIMATIONsettings (e.g.,METHOD=COND LAPLACEorMETHOD=SAEM). - Key Consideration: The M3 method can be computationally intensive. For datasets with a high percentage of BLOQ (>20%), consider the M6/M7 methods which model the likelihood of being BLOQ.
- Protocol: Implement the
Q3: My visual predictive check (VPC) shows a systematic misfit, but the objective function value (OFV) change was significant for adding a parameter. How do I resolve this conflict between diagnostic tools?
- A: A significant OFV drop does not guarantee a model is predictively accurate. Prioritize the VPC.
- Action Protocol: 1) Generate a VPC for the competing models (e.g., with and without the new parameter). 2) If the VPC shows misfit (e.g., predictions do not encapsulate the central trend or variability of the observed data), the model is inadequate for simulation. 3) Investigate if the misfit is in a specific patient subgroup (e.g., renal impaired) by performing a stratified VPC. 4) Consider alternative structural models (e.g., nonlinear clearance, time-varying parameters) or residual error models that the OFV may not have captured optimally.
Q4: When quantifying inter-individual variability (IIV), how do I decide between an exponential (additive on log-scale) and a proportional error model for OMEGA?
- A: The choice is based on the parameter's distribution and biological plausibility.
- Exponential Model (Default):
PV = TVP * exp(η)whereη ~ N(0, ω²). This ensures the parameter (PV) is always positive and typically results in a log-normal distribution, which is common for biological parameters (e.g., clearance, volume). Use this as the standard approach. - Proportional/Additive Model:
PV = TVP * (1 + η)whereη ~ N(0, ω²). Can lead to negative parameter values ifη < -1. Use with caution, typically for parameters like bioavailability (F) bounded between 0 and 1, where a logit-transform might be more appropriate. - Protocol: Start with an exponential model for all IIV terms. If the
η-shrinkagefor a parameter is high (>20-30%), it indicates the data poorly informs that IIV, and the model may be over-parameterized. Consider removing the IIV for that parameter.
- Exponential Model (Default):
Q5: What are the best practices for designing a study to robustly estimate intra-individual variability (residual error) and IIV separately?
- A: Study design is critical for precise variability estimation.
- Rich Sampling: Include studies with dense pharmacokinetic sampling in a subset of subjects. Multiple samples per individual around key PK events (absorption, distribution, elimination phases) are needed to separate within-subject noise from between-subject differences.
- Repeated Dosing: Collect data at steady-state (e.g., trough concentrations at multiple visits) to better quantify time-dependent (inter-occasion) variability versus pure IIV.
- Protocol Summary: A hybrid design combining sparse sampling in a large population (for IIV and covariate detection) with rich sampling in a smaller cohort (for precise residual error and structural model estimation) is often optimal.
Data Presentation: Key Variability Parameters from a Hypothetical Monoclonal Antibody PK Study
Table 1: Estimated Population PK Parameters and Variability
| Parameter (Symbol) | Typical Value (TVP) | Inter-individual Variability (IIV, CV%) | Intra-individual/Residual Error (Proportional) | Intra-individual/Residual Error (Additive) |
|---|---|---|---|---|
| Clearance (CL) | 0.015 L/day | 35.2% | - | - |
| Volume (Vc) | 3.8 L | 24.7% | - | - |
| Inter-compartment CL (Q) | 0.008 L/day | Fixed | - | - |
| Peripheral Volume (Vp) | 2.5 L | 51.0% | - | - |
| - | - | - | - | - |
| Residual Unexplained Variability | - | - | 18.5% | 0.4 μg/mL |
Table 2: Impact of Covariates on Target Attainment Rate (Simulation)
| Covariate Scenario | Steady-State Trough Conc. (μg/mL, median [5th-95th %ile]) | Probability of Target Attainment (>10 μg/mL) |
|---|---|---|
| Baseline (70kg, Normal Albumin) | 15.2 [6.8, 28.1] | 92.1% |
| Low Body Weight (40kg) | 18.5 [9.1, 32.4] | 97.5% |
| Low Albumin | 9.8 [3.9, 20.5] | 72.3% |
| Presence of ADA (High Titer) | 5.1 [1.2, 12.7] | 35.6% |
Experimental Protocols
Protocol 1: Bootstrap for Model Validation and Confidence Interval Estimation
- Objective: Assess the robustness of final parameter estimates and generate non-parametric confidence intervals.
- Method:
a. From your original dataset of
Nsubjects, randomly sampleNsubjects with replacement to create a new dataset. b. Fit the final population PK/PD model to this bootstrapped dataset. c. Record the resulting parameter estimates. d. Repeat steps a-c a large number of times (typically 1000). e. For each parameter, calculate the 2.5th, 50th (median), and 97.5th percentiles from the distribution of bootstrap estimates. The interval between the 2.5th and 97.5th percentiles represents the 95% confidence interval. - Success Criteria: The original model estimates should fall near the median of the bootstrap distributions. Narrow confidence intervals indicate precise estimation.
Protocol 2: Visual Predictive Check (VPC) for Model Predictive Performance
- Objective: Evaluate if the final model can simulate data that accurately reflects the central tendency and variability of the original observed data.
- Method:
a. Using the final model and its parameter estimates (fixed and random effects), simulate
M(e.g., 1000) replicate datasets identical in structure to the original dataset (same subjects, doses, sampling times, covariates). b. For each time bin (e.g., pre-dose, 0-2h, 2-8h post-dose), calculate the median and specific percentiles (e.g., 5th and 95th) of the simulated concentrations across all replicates. c. Overlay the observed data percentiles (median, 5th, 95th) on the same plot. d. Shade the areas between the simulated prediction intervals (e.g., 5th-95th). - Success Criteria: The observed data percentiles should generally fall within the shaded prediction intervals of the simulated data, with no major systematic trends.
Mandatory Visualizations
Title: Population PK/PD Modeling & Target Attainment Workflow
Title: PK/PD Variability Links to Target Attainment
The Scientist's Toolkit: Research Reagent & Software Solutions
Table 3: Essential Tools for Population PK/PD Modeling
| Item/Category | Example(s) | Primary Function in Research |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software | NONMEM, Monolix, Phoenix NLME, nlmixr (R) |
Gold-standard platforms for fitting population PK/PD models, estimating fixed/random effects. |
| Scripting & Data Wrangling Environment | R (with dplyr, tidyr), Python (Pandas), SAS |
Data preparation, cleaning, dataset creation for modeling software, and post-processing of results. |
| Model Diagnostics & Visualization Packages | xpose (R), ggPMX (R), Piranha (for Monolix) |
Generate standard diagnostic plots (GOF, VPC, shrinkage) to evaluate model performance. |
| Stochastic Simulation Engine | mrgsolve (R), Simulx (within Monolix), RxODE (R) |
Perform model-based simulations (e.g., for VPC, clinical trial simulations, target attainment). |
| Bioanalytical Assay Kits | ELISA, MSD, LC-MS/MS Assays | Quantify drug concentrations (PK) and relevant biomarkers (PD) in biological matrices (plasma, tissue). |
| Covariate Data Management System | Electronic Data Capture (EDC) systems, REDCap | Accurately collect and manage patient covariates (demographics, lab values, genetics) for analysis. |
Technical Support Center: Troubleshooting PTA-MCS Experiments
FAQs & Troubleshooting
Q1: My PTA curves appear jagged or non-monotonic, unlike the smooth sigmoidal curves in literature. What is the cause and how can I fix it? A: Jagged curves are typically due to an insufficient number of MCS iterations.
- Cause: Low sample size leads to high stochastic error. The inherent randomness of MCS is not adequately averaged out.
- Solution: Increase the number of simulated subjects (
N) in your MCS. A minimum of 5,000-10,000 subjects per scenario is standard. For stable estimation of tails (e.g., PTA >90% or <10%), 50,000 or more may be required. Always perform a convergence analysis.
Q2: How do I incorporate between-subject variability (BSV) and residual error models correctly into the simulation? A: Incorrect error model implementation is a common source of inaccurate PTA.
- Protocol: For a PK parameter like clearance (CL), model BSV as:
CL_i = TVCL * exp(η_i), whereTVCLis the typical value andη_i ~ N(0, ω²). The residual error (e.g., additive/proportional) is added at the observation stage. Ensure the random effects (η) are generated once per virtual subject and applied consistently across related parameters (e.g., CL and Vd may be correlated). - Troubleshooting: Validate your simulation by replicating the original population model statistics (mean, variance) without dosing. The simulated population's parameter distribution should match the input model.
Q3: When comparing dosing regimens, the PTA differences are statistically insignificant. How can I improve the discriminatory power of my analysis? A: This often relates to study design power within the simulation.
- Solutions:
- Increase
N: As in Q1, more subjects reduce noise. - Refine the Target: Ensure your PK/PD target (e.g., fT>MIC, AUC/MIC) is clinically relevant and sufficiently precise. An overly broad target blurs distinctions.
- Scenario Selection: Simulate across a wider, clinically meaningful range of MIC values or patient covariates (e.g., renal function extremes) to reveal differences.
- Increase
Q4: My PTA results contradict clinical trial findings or other published simulations. What are the key areas to audit? A: Conduct a systematic verification of your simulation framework.
- Audit Checklist:
- Model Verification: Ensure the implemented PK/PD model and its parameters (fixed and random effects) are identical to the reference.
- Dosing Regimen Accuracy: Confirm dosing intervals, infusion durations, and loading doses.
- Target Definition: Verify the PK/PD index and its critical value (e.g., 40% fT>MIC vs. 100% fT>MIC).
- MCS Settings: Confirm the random number seed for reproducibility and the number of iterations.
Table 1: Impact of MCS Iterations on PTA Estimate Stability (Target: PTA ≥ 90%)
| Scenario (MIC, Dose) | PTA at N=1,000 | PTA at N=10,000 | PTA at N=50,000 | Standard Error (N=10,000) |
|---|---|---|---|---|
| MIC=2 mg/L, 500 mg q12h | 87.5% | 89.1% | 89.0% | ±0.31% |
| MIC=4 mg/L, 500 mg q12h | 65.3% | 63.8% | 63.9% | ±0.48% |
| MIC=2 mg/L, 750 mg q12h | 94.2% | 95.5% | 95.4% | ±0.21% |
Table 2: PTA Across Patient Renal Function Subgroups
| Dosing Regimen | Normal Renal Function (CrCl=100 mL/min) PTA | Moderate Impairment (CrCl=40 mL/min) PTA | Severe Impairment (CrCl=20 mL/min) PTA |
|---|---|---|---|
| 500 mg q24h | 78% | 92% | 99%* |
| 500 mg q12h | 95% | 99%* | >99%* (Risk of Toxicity) |
| 250 mg q12h | 65% | 88% | 98%* |
Note: High PTA may be associated with increased toxicity risk, requiring a toxicity model.
Experimental Protocol: Standard PTA-MCS Workflow
Protocol Title: Deterministic and Stochastic PTA Assessment for Dosing Regimen Optimization.
Methodology:
- Define Population Model: Implement a published or developed population PK/PD model, specifying fixed parameters, covariance matrix for BSV (Ω), and residual error model (Σ).
- Define Scenarios: Create a grid of:
- Dosing regimens (dose, interval, infusion time).
- Patient covariate distributions (e.g., weight, renal function).
- Pathogen susceptibility (MIC distribution or a specific MIC range).
- Generate Virtual Population: For
i = 1toN(e.g., 10,000):- Sample covariates from defined distributions.
- Sample individual random effects (
η_i) fromN(0, Ω). - Calculate individual PK/PD parameters.
- Simulate Drug Exposure: For each virtual subject, solve the PK model equations over time to generate concentration-time profiles.
- Calculate PK/PD Index: For each profile, compute the relevant index (e.g., AUC0-24/MIC, fT>MIC).
- Determine Target Attainment: Compare each subject's index to the predefined target (e.g., AUC/MIC > 100). Count successes.
- Compute PTA: PTA = (Number of subjects attaining target / N) * 100%.
- Repeat for All Scenarios: Generate PTA curves (PTA vs. MIC) or surfaces (PTA vs. dose/MIC).
Visualizations
Diagram 1: PTA-MCS Core Workflow
Diagram 2: Integration in PK PD Improvement Research Thesis
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PTA-MCS Research
| Item | Function in PTA-MCS Context |
|---|---|
| Nonlinear Mixed-Effects Modeling (NONMEM) | Industry-standard software for building the foundational population PK/PD models that inform the MCS. |
R with mrgsolve/RxODE packages |
Open-source environment for implementing custom MCS, performing data wrangling, and generating PTA plots. |
| PDXpert or similar | Database software for managing complex non-clinical and clinical pharmacological data used as model inputs. |
| Monolix Suite | Integrated platform for population analysis, model diagnosis, and subsequent simulation. |
| High-Performance Computing (HPC) Cluster | Crucial for running large-scale, computationally intensive simulations (e.g., 100,000+ subjects, multiple scenarios). |
| Clinical MIC Distribution Databases (e.g., SENTRY, EUCAST) | Provides the real-world pathogen susceptibility data necessary for defining simulation scenarios. |
Integrating Real-World Data and EHRs to Refine Population Models
Troubleshooting Guides & FAQs
Q1: Our integrated EHR data for a PK/PD study shows implausible creatinine clearance values, skewing our renal function covariate model. What are the primary data quality checks? A1: Implausible lab values are common. Implement these checks sequentially:
- Range Validation: Flag values outside physiological limits (e.g., CrCl < 10 or > 250 mL/min).
- Temporal Consistency: Identify abrupt, non-physiological changes (e.g., CrCl doubling in 24 hours).
- Unit Harmonization: Confirm all serum creatinine values are in mg/dL; standardize CrCl calculation (Cockcroft-Gault) across all data sources.
- Contextual Filtering: Exclude values from inpatient/ICU settings if modeling chronic outpatient disease, as acute illness distorts measures.
Q2: When linking RWD cohorts to a clinical trial population for model extrapolation, patient matching yields very low sample sizes. How can we improve cohort alignment? A2: Low matching rates indicate poor feature definition. Refine your protocol:
- Broaden Key Covariates: Beyond age/sex/gender, include disease severity scores (e.g., ECOG status), line of therapy, and concomitant medications.
- Use Propensity Score Widening: Instead of 1:1 exact matching, use propensity score stratification or weighting to retain more RWD patients.
- Validate with Clinical Endpoints: Ensure the matched cohort shows similar time-to-event distributions for a common baseline outcome (e.g., hospitalization) before PK/PD analysis.
Q3: Missing dosing timestamps in EHR data invalidate our adherence correction algorithm for the population PK model. What is the standard imputation method? A3: Do not impute single timestamps. Use a model-based approach:
- Categorize Missings: Classify records as "structured" (time known), "unstructured" (text note), or "missing".
- For Outpatient Oral Drugs: Assume dosing within a plausible window (e.g., 6-10 AM for once-daily morning doses). Perform sensitivity analysis by shifting this window ±4 hours.
- Incorporate as Uncertainty: Use the
MCMCmethod in NONMEM orsaemin Monolix with aMDVflag to estimate parameters while accounting for dose time uncertainty.
Q4: The target attainment probability from our RWD-informed model conflicts with the Phase 3 clinical trial result. How should we investigate the discrepancy? A4: This is a critical validation step. Execute this diagnostic workflow:
Q5: Our EHR-derived biomarker data is from multiple assay platforms. How do we harmonize it for a longitudinal PD model? A5: Use a calibration protocol:
- Identify a Reference Lab Method from the clinical trial.
- Obain a Bridging Dataset: For a subset of patients (n≥30), acquire paired measurements (old platform & reference platform).
- Fit a Linear Regression Model:
Reference = α + β * Local_Assay. Store α and β for each source platform. - Apply Transformation: Convert all historical values to the reference scale before pooling data into the population model.
Key Experimental Protocols
Protocol 1: EHR-to-PK/PD Cohort Construction
Objective: Build a research-ready cohort from raw EHR for a vancomycin PK/PD target attainment study.
- Extraction: Identify adult (≥18y) inpatient encounters with (a) vancomycin order, (b) ≥1 serum creatinine, (c) ≥2 vancomycin trough levels.
- Cleaning: Calculate CrCl using Cockcroft-Gault. Flag and exclude values if weight > 300 kg or height > 220 cm.
- Dose/Time Alignment: Align infusion start times to medication administration record (MAR). Trough levels must be drawn within 30 minutes prior to next dose.
- Outcome Definition: Attainment = proportion of patients with trough (15-20 mg/L) at steady state.
Protocol 2: Propensity Score Matching for External Control Arm
Objective: Create a comparator arm from RWD for a Phase 2 oncology PK/PD trial.
- Feature Selection: Define covariates: age (±5 years), sex, prior lines of therapy, baseline tumor size, ECOG status, key lab values.
- Model Fitting: Fit a logistic regression model (trial=1, RWD=0) using all covariates.
- Matching: Use nearest-neighbor matching on the logit of the propensity score with a caliper of 0.2 standard deviations.
- Balance Assessment: Calculate standardized mean differences (SMD) for all covariates post-match. Successful match requires all SMD < 0.1.
Table 1: Impact of RWD Source Cleaning on PK Parameter Estimates (Vancomycin Example)
| Data Cleaning Step | Number of Patients Remaining | Estimated CL (L/h) (Mean ± SE) | Estimated Vd (L) (Mean ± SE) | Target Attainment Rate (%) |
|---|---|---|---|---|
| Raw EHR Extraction | 1250 | 4.2 ± 1.8 | 45.5 ± 22.1 | 31 |
| After Dose-Time Alignment | 980 | 4.8 ± 1.2 | 48.2 ± 18.5 | 38 |
| After CrCl Validation | 910 | 5.1 ± 0.9 | 50.1 ± 15.3 | 42 |
| After Removing ICU Stays | 720 | 5.4 ± 0.7 | 52.3 ± 10.1 | 51 |
Table 2: Assay Harmonization Impact on PD Biomarker Variability
| Biomarker (Platforms) | Before Harmonization (CV%) | After Linear Calibration (CV%) | Required Bridging Sample Size (n) |
|---|---|---|---|
| CRP (3 different) | 45% | 18% | 30 |
| Neutrophil Count (2 different) | 15% | 12% | 20 |
| PSA (4 different) | 62% | 22% | 40 |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in RWD-EHR Integration for PK/PD |
|---|---|
| OMOP Common Data Model | Standardized vocabulary and schema to map heterogeneous EHR data from multiple institutions into a single, queryable format for cohort building. |
| FHIR (Fast Healthcare Interoperability Resources) API | Modern standard for retrieving discrete clinical data (labs, medications) directly from EHR systems in real-time for prospective studies. |
| PsyC (Pharmacometric co-working) NONMEM Toolkit | A suite of utilities for efficient data preparation, visualization, and model diagnostics within the NONMEM workflow. |
R Package: PatientLevelPrediction |
An open-source tool for constructing and validating predictive models (e.g., propensity scores, outcome risk) using observational data in the OMOP CDM. |
| Phoenix WinNonlin / NLME | Industry-standard software for performing population PK/PD modeling and simulation, including covariate model building with RWD. |
| REDCap (Research Electronic Data Capture) | Secure web platform for capturing and managing dedicated prospective data (e.g., patient-reported outcomes) to supplement retrospective EHR data. |
Visualization: Core Integration Workflow
RWD-EHR Model Refinement Pathway
Machine Learning Applications for Identifying Covariates and Predicting PTA
Technical Support Center & FAQs
FAQ 1: Data Preprocessing & Feature Engineering
- Q: My model performance is poor despite using a large dataset of patient covariates. What could be the issue?
- A: Poor performance often stems from inadequate preprocessing. Common issues include:
- Missing Data: ML algorithms cannot handle missing values. Impute using methods like multivariate imputation by chained equations (MICE) or k-nearest neighbors (KNN), but document the method's impact on variance.
- High Collinearity: Highly correlated covariates (e.g., weight, BMI, BSA) can destabilize models. Use variance inflation factor (VIF) analysis to identify and remove redundant features (VIF > 5-10 indicates high collinearity).
- Improper Scaling: Algorithms like SVM or neural networks require feature scaling. Standardize (zero mean, unit variance) or normalize (scale to a [0,1] range) all continuous covariates.
- A: Poor performance often stems from inadequate preprocessing. Common issues include:
FAQ 2: Model Selection & Validation
- Q: How do I choose the right ML algorithm for PTA prediction and covariate identification?
- A: The choice depends on your data structure and goal. Use this structured comparison:
Table 1: Comparison of ML Algorithms for PK/PD PTA Research
| Algorithm | Best For | Pros for PK/PD | Cons for PK/PD | Key Hyperparameters to Tune |
|---|---|---|---|---|
| Random Forest | Identifying non-linear covariate interactions. | Handles mixed data types, provides feature importance scores. | Can overfit, less interpretable than linear models. | n_estimators, max_depth, min_samples_split |
| Gradient Boosting (XGBoost/LightGBM) | High-accuracy prediction of continuous or binary PTA outcomes. | State-of-the-art predictive performance, efficient with large data. | Prone to overfitting without careful tuning. | learning_rate, n_estimators, max_depth, subsample |
| LASSO Regression | Sparse covariate selection from a large pool. | Creates interpretable, parsimonious models by driving coefficients to zero. | Assumes linear relationships. | Regularization strength (alpha or lambda) |
| Neural Networks | Capturing extremely complex, high-dimensional relationships. | High flexibility and predictive power. | Requires very large datasets, "black box" nature. | Number of layers/neurons, dropout rate, learning rate |
- Protocol for Nested Cross-Validation: To ensure robust model selection and performance estimation without data leakage, follow this workflow:
- Outer Loop (Performance Estimation): Split data into k folds (e.g., 5). Hold out one fold as the test set.
- Inner Loop (Model Selection/Tuning): On the remaining k-1 folds, perform another k-fold cross-validation to grid search over hyperparameter combinations.
- Train & Evaluate: Train the model with the best hyperparameters on the k-1 folds and evaluate on the held-out outer test fold.
- Repeat: Repeat for each outer fold. The final model performance is the average across all outer test folds.
FAQ 3: Interpretation & Integration with PK/PD Modeling
- Q: My ML model identified unexpected covariates. How can I validate these findings biologically?
- A: ML output is hypothesis-generating. Validation requires integration into traditional pharmacometric workflows:
- Step 1 - Prior Inclusion: Introduce the ML-identified covariate as a prior in a non-linear mixed-effects (NLME) model using NONMEM or Monolix.
- Step 2 - Stepwise Covariate Modeling: Use a formal stepwise approach (forward inclusion p<0.05, backward elimination p<0.01) to test if the covariate provides a statistically significant reduction in objective function value (OFV).
- Step 3 - Clinical Relevance: Assess if the covariate's effect size (e.g., on clearance or volume) is clinically meaningful (>20% change typically warrants consideration).
- A: ML output is hypothesis-generating. Validation requires integration into traditional pharmacometric workflows:
Visualization: ML-Enhanced PK/PD Workflow
Diagram Title: Integrated ML and PK/PD Modeling Workflow for PTA
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Tools for ML-Enhanced PTA Research
| Item/Category | Function in Research | Example/Note |
|---|---|---|
| NLME Software | Gold-standard for building population PK/PD models and final PTA simulation. | NONMEM, Monolix, Phoenix NLME. |
| ML Programming Environment | Flexible platform for data preprocessing, model development, and visualization. | Python (scikit-learn, XGBoost, PyTorch) or R (tidymodels, caret). |
| Clinical Data Standard | Ensures covariate data is structured and interoperable between systems. | CDISC SDTM/ADaM formats. Critical for automating data pipelines. |
| Virtual Population Generator | Creates physiologically plausible virtual patients for simulation. | Simcyp Simulator, R mrgsolve/PKSim. Used for external validation of ML-predicted PTA. |
| Model Diagnostic Suite | Evaluates and compares model performance objectively. | Python scikit-learn metrics, R shap for interpretability, xpose for NLME diagnostics. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: My Monte Carlo Simulation (MCS) results show poor target attainment rates (TAR) even at high doses. What are the primary PK/PD parameters to investigate first? A: First, verify the accuracy of your input distributions. The most common culprits are underestimation of Volume of Distribution (Vd) or overestimation of Clearance (CL). Re-examine your in vitro-to-in vivo scaling for CL and ensure your protein binding assays are accurate, as high free fraction can drastically alter unbound drug concentrations. Next, confirm the MIC distribution for your pathogen panel is representative of the current clinical landscape.
Q2: During the integration of a protein binding model, the simulated unbound concentration is negligible. How should I troubleshoot this? A: This indicates a potential error in the binding constant or the fraction unbound (fu) input. 1) Validate your fu assay protocol (e.g., equilibrium dialysis, ultracentrifugation). 2) Ensure the fu value is applied as a distribution (e.g., beta distribution) rather than a static point estimate to reflect inter-individual variability. 3) Check for logical errors in your code where total concentration might be incorrectly multiplied instead of divided by the binding ratio.
Q3: The MCS-predicted optimal dose is significantly higher than the dose predicted to be safe in toxicology studies. What steps should a researcher take? A: This is a critical PK/PD disconnection. Follow this protocol:
- Refine the PD Target: Re-evaluate the fAUC/MIC or fT>MIC target from preclinical models. Is it too conservative?
- Explore Alternative Regimens: Simulate prolonged infusion or more frequent dosing (e.g., q8h vs. q24h) to increase TAR without increasing peak concentration (Cmax), which often drives toxicity.
- Incorporate Covariates: Run a Population PK (PopPK)-informed MCS. Identify subpopulations (e.g., renally impaired) that may require separate, optimized dosing regimens.
- Consider Combination Therapy: If monotherapy cannot achieve TAR safely, propose MCS for a combination regimen with a second agent.
Q4: How do I handle time-dependent killing (fT>MIC) vs. concentration-dependent killing (fAUC/MIC) models in the same MCS workflow? A: Implement a logic gate in your simulation script based on the antibiotic class. Use the appropriate PD index for each drug. The workflow diagram below illustrates this decision process.
Diagram Title: PK/PD Model Selection Logic for MCS
Q5: The MCS for a pediatric indication lacks PK data. What is the best practice for extrapolation? A: Allometric scaling is the standard approach. Use the formula: CLchild = CLadult * (Weightchild / Weightadult)^0.75. Vd scales linearly with weight. Crucially, incorporate high variability (e.g., coefficient of variation >40%) around these scaled parameters to account for maturation uncertainty. Always perform a sensitivity analysis on the allometric exponents.
Key Experimental Protocols
Protocol 1: In Vitro PK/PD Hollow-Fiber Infection Model (HFIM) for MCS Validation
- Objective: Validate MCS-predicted dosing regimens against dynamic bacterial kinetics.
- Methodology:
- Prepare a bacterial inoculum (~10^8 CFU/mL) of the target pathogen in the central cartridge.
- Program the syringe pump to simulate the human PK profile (derived from MCS) in the extracapillary space.
- Sample from the system at predefined timepoints (e.g., 0, 1, 2, 4, 8, 24, 48h).
- Quantify bacterial density (CFU/mL) and assess for resistance emergence via plating on drug-containing agar.
- Compare the observed bacterial kill curve to the MCS-predicted PK/PD target attainment.
Diagram Title: Hollow-Fiber Infection Model Experimental Workflow
Protocol 2: Population PK Model Development for MCS Input
- Objective: Develop a PopPK model to define mean parameter estimates and their inter-individual variability (IIV).
- Methodology:
- Collect rich or sparse PK data from Phase 1 clinical trials.
- Using non-linear mixed-effects modeling software (e.g., NONMEM, Monolix), fit structural (1-, 2-compartment) and statistical models.
- Identify significant covariates (e.g., weight, renal function, age) via stepwise covariate modeling.
- The final model outputs parameter estimates (THETA), IIV (OMEGA), and residual error (SIGMA). These distributions are directly used to parameterize the MCS.
Research Reagent Solutions Toolkit
| Item | Function in MCS Dosing Optimization |
|---|---|
| Semi-Permeable Hollow Fiber Cartridges | Creates a bioreactor for simulating human PK profiles and their effect on bacteria in vitro (HFIM). |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold standard for quantifying drug concentrations in complex biological matrices for PK model development. |
| Mueller Hinton Broth II | Standardized broth for MIC determination and HFIM studies, ensuring reproducible PD endpoints. |
| Non-Linear Mixed Effects Modeling Software (NONMEM) | Industry standard for building Population PK models, the primary source of parameter distributions for MCS. |
| Monte Carlo Simulation Engine (e.g., R, MATLAB, Phoenix WinNonlin) | Platform to perform stochastic simulations of thousands of virtual patients to compute TAR. |
| Clinical & Laboratory Standards Institute (CLSI) MIC Guidelines | Provides standardized methodology for generating the MIC distributions used as PD inputs in MCS. |
Table 1: MCS Results for Candidate Dosing Regimens (fT>MIC target of 50%)
| Regimen | Dose (mg) | Dosing Interval | Simulated TAR (%) (Mean ± SD) | Probability of Toxicity (>Cmax threshold) |
|---|---|---|---|---|
| A | 500 | q12h | 78.2 ± 3.1 | <0.1% |
| B | 750 | q12h | 91.5 ± 2.4 | 2.3% |
| C | 1000 | q24h | 65.8 ± 4.2 | 0.5% |
| D | 500 | q8h | 95.1 ± 1.8 | <0.1% |
Table 2: Key PopPK Parameter Distributions for MCS Input
| Parameter | Unit | Typical Value (Mean) | Inter-Individual Variability (IIV, CV%) | Distribution Type |
|---|---|---|---|---|
| Clearance (CL) | L/h | 5.0 | 30% | Lognormal |
| Volume (Vd) | L | 25.0 | 25% | Lognormal |
| Fraction Unbound (fu) | - | 0.15 | 20% | Beta |
| Absorption Rate (Ka) | 1/h | 1.2 | 45% | Lognormal |
Overcoming Hurdles: Diagnosing and Improving Suboptimal Attainment
Troubleshooting Guides & FAQs
Q1: Our clinical trial simulation for target attainment rate (TAR) shows unexpectedly wide confidence intervals. How do we determine if primary noise is from PK variability or PD uncertainty?
A: This is a classic root cause investigation. Follow this diagnostic protocol:
- Fix PD, Vary PK: Run a simulation holding your PD parameters (e.g., EC50, Emax, Hill coefficient) at their point estimates. Use the full variance-covariance matrix of your population PK model to simulate PK variability. Calculate TAR.
- Fix PK, Vary PD: Now hold PK parameters (e.g., Clearance, Volume) at point estimates and sample PD parameters from their estimated distribution (including uncertainty). Calculate TAR.
- Compare Results: Use the coefficient of variation (CV) in the resulting TAR distributions from steps 1 and 2.
- High CV from Step 1: PK variability is a major driver.
- High CV from Step 2: PD parameter uncertainty is a major driver.
- Similar CVs: Both contribute significantly.
Key Experimental Protocol (Monte Carlo Simulation):
- Software: Use validated platforms like
mrgsolve,R/PKPDsim,NONMEM, orPhoenix. - Population: Simulate a virtual patient population (n ≥ 1000) representative of your trial (demographics, covariates).
- Sampling: For PK variability, sample individual PK parameters from a multivariate normal distribution defined by the population PK model's Omegas (IIV) and Sigmas (residual error). For PD uncertainty, sample PD parameters from the variance-covariance matrix of the PD model fit.
- Exposure Metric: Calculate relevant exposure (AUC, Cmax, Ctrough) for each virtual subject.
- PD Response: Apply the PD model to link exposure to effect (e.g., probability of response, tumor size change).
- Target Attainment: Determine if the effect meets the pre-defined target (e.g., PTA >90% for efficacy) for each subject.
- Aggregation: Calculate the overall TAR and its distribution across simulation replicates (≥1000).
Q2: We suspect our Emax model is misspecified, leading to poor TAR predictions. What systematic checks can we perform?
A: Perform a model misspecification analysis:
- Visual Predictive Check (VPC) for PD: Plot observed PD data with simulation-based prediction intervals from your model. Systematic deviations indicate misspecification.
- Bootstrap Robustness: Refit your PD model to 200-500 bootstrap resamples of your original data. Examine the distribution of parameter estimates. Wide, bimodal, or unstable distributions suggest a poorly identified model.
- Alternative Model Testing: Fit competing models (e.g., Linear vs. Emax vs. Sigmoid Emax). Use objective criteria (AIC, BIC) and clinical plausibility for selection.
- Covariate Analysis: Test if inclusion of patient covariates (e.g., disease status, biomarkers) on PD parameters improves fit and reduces uncertainty.
Detailed Protocol for Bootstrap Robustness Check:
- Data Preparation: Start with your original dataset of
Nsubjects. - Resampling: Create
Bbootstrap datasets (B=500) by randomly samplingNsubjects with replacement. - Model Refitting: Automate the process to refit your PD model to each bootstrap dataset.
- Parameter Collection: Record the final parameter estimates from each successful fit.
- Analysis: Calculate median and 95% confidence intervals for each parameter. Plot the distributions.
Q3: Our PK model shows high inter-occasion variability (IOV), but its impact on TAR is unclear. How should we quantify this?
A: IOV can significantly impact TAR for chronic therapies. Quantify its effect by designing a simulation that separates IIV from IOV.
Protocol for IOV Impact Assessment:
- Base Simulation (IIV only): Simulate TAR using your PK model with IIV but without IOV.
- Full Variability Simulation: Simulate TAR using the full model with both IIV and IOV included.
- Comparative Metric: Calculate the absolute difference in TAR between the two scenarios at key dosing intervals. A difference >5-10% is typically considered impactful.
Table 1: Quantitative Impact Analysis of Variability Sources on Target Attainment Rate (Hypothetical Case Study)
| Variability Source | Scenario Description | Simulated TAR (% > Target) | 95% CI for TAR | Coefficient of Variation (CV) |
|---|---|---|---|---|
| Baseline (Total Uncertainty) | Full PK & PD uncertainty | 78% | [65%, 88%] | 8.2% |
| PK Variability Only | PD parameters fixed | 85% | [78%, 90%] | 4.1% |
| PD Uncertainty Only | PK parameters fixed | 80% | [70%, 85%] | 5.0% |
| High IOV Scenario | Includes Inter-Occasion Variability | 72% | [60%, 82%] | 8.5% |
| Reduced PD Uncertainty | PD model with covariate | 82% | [77%, 86%] | 3.0% |
Research Reagent & Solutions Toolkit
Table 2: Essential Research Toolkit for PK/PD TAR Improvement Studies
| Item / Solution | Function & Application in Troubleshooting |
|---|---|
| Monte Carlo Simulation Software (e.g., mrgsolve, R/PKPDsim) | Core engine for performing stochastic simulations to estimate TAR under variability and uncertainty. |
| Population PK/PD Modeling Software (e.g., NONMEM, Monolix, Phoenix NLME) | For developing and refining the mathematical models that describe drug kinetics and dynamics. |
| Bootstrap/Jackknife Resampling Algorithms | To assess the robustness and uncertainty of model parameter estimates. |
| Visual Predictive Check (VPC) Scripts | Diagnostic tool to evaluate model misspecification by comparing observations with model predictions. |
| Sobol Sensitivity Analysis Tools | Advanced global sensitivity analysis to rank-order sources of variability impacting TAR. |
| Standardized Biomarker Assay Kits | To obtain high-quality, reproducible PD endpoint data (e.g., cytokine levels, receptor occupancy). |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold standard for generating accurate PK concentration data for model building. |
Visualizations
Diagram Title: Root Cause Analysis Workflow for Low Target Attainment
Diagram Title: Monte Carlo Simulation for Target Attainment Rate
Troubleshooting Guides & FAQs
FAQ 1: Why is my population PK model failing to converge when analyzing sparse TDM data for a highly variable drug?
- Answer: This is commonly due to over-parameterization relative to sparse data density or mis-specified residual error models. For high variability drugs, the variability (η) on parameters like clearance (CL) and volume of distribution (Vd) can be large. First, simplify the model. Use a one-compartment model as a starting point. For the residual error, test a combined (additive + proportional) error structure, as a purely additive model may fail with wide concentration ranges. Ensure your dosing and sampling times are accurately recorded. Consider using the SAEM estimation algorithm (in NONMEM or Monolix) which is more robust for sparse data. If identifiability issues persist, Bayesian priors from a prior rich sampling study may be necessary.
FAQ 2: During adaptive dosing, my Bayesian forecasting returns unrealistic dose recommendations (extremely high or low). What could be wrong?
- Answer: This typically indicates a mismatch between the individual's observed concentrations and the prior population model. Troubleshoot in this order:
- Check TDM Sample Timing: Verify the exact time of the last dose and the exact time of the TDM blood draw. Errors of even 30 minutes can drastically bias forecasted parameters for drugs with short half-lives.
- Review Prior Model: Ensure the population PK model used as the prior is appropriate for your specific patient subpopulation (e.g., same disease state, organ function). A model derived from healthy volunteers may fail in critically ill patients.
- Inspect Observed Concentration: Rule out assay error or dosing administration errors. A single outlier concentration will skew forecasts.
- Adjust Bayesian Priors: The weighting between the prior and the observed data can be tuned. You can artificially inflate the prior variance (OMEGA) to reduce its influence if you suspect the model is a poor fit, forcing the forecast to rely more on the individual's TDM data.
FAQ 3: How do I validate a limited sampling strategy (LSS) for TDM of a drug with high inter-occasion variability (IOV)?
- Answer: Validation must account for IOV. Follow this protocol:
- Use a separate validation dataset not used for LSS model development.
- The dataset should contain full PK profiles (e.g., 8-12 samples per dosing interval) from subjects demonstrating high IOV.
- Apply the LSS (e.g., 2-3 specific timepoints) to estimate the AUC or trough (Cmin) for each profile in the validation set.
- Compare the LSS-estimated PK metrics to those calculated from the full profile using the reference method (e.g., non-compartmental analysis).
- Acceptance criteria: ≥90% of predictions should fall within ±20% of the reference value (or ±30% for Cmin). The Prediction Error (PE%) and Absolute Prediction Error (APE%) should be summarized. A mean PE% (bias) near 0 and a mean APE% (precision) <15% are good targets.
FAQ 4: What are common pitfalls when implementing model-informed precision dosing (MIPD) software for adaptive dosing in a clinical trial?
- Answer:
- Data Integration Errors: Inconsistent formatting of patient covariates (e.g., creatinine clearance formulas) between the electronic health record (EHR) and the MIPD platform.
- Model Version Control: Using an outdated or incorrect version of the underlying PK/PD model for forecasting. Implement strict model governance.
- Ignoring PD Feedback: Relying solely on PK targets (e.g., target AUC) without integrating emerging PD biomarkers or clinical response data, which is crucial if the PK/PD relationship is variable.
- Lack of Clinical Override Logic: The software must allow for clinical judgment overrides with mandatory documentation fields when a recommended dose is not feasible (e.g., due to toxicity concerns).
Table 1: Examples of High Variability Drugs and Key PK Parameters Impacting TDM Strategy
| Drug/Therapeutic Area | Typical Intra-individual CV% for AUC | Typical Inter-individual CV% for AUC | Primary PK Driver for Variability | Key TDM Metric & Common Target |
|---|---|---|---|---|
| Tacrolimus (Immunosuppressant) | 20-40% | 40-60% | CYP3A5 genotype, drug-drug interactions | Trough (Cmin): 5-15 ng/mL (post-transplant) |
| Vancomycin (Antibiotic) | 15-30% | 30-70% | Renal function (CLcr), weight | AUC over 24h/MIC: 400-600 (for MRSA) |
| Busulfan (Chemotherapy) | 20-35% | 50-80% | Weight, age, metabolic rate | Cumulative AUC: 900-1350 µM•min |
| Clozapine (Antipsychotic) | 20-40% | 35-50% | CYP1A2 activity (smoking, diet) | Trough (Cmin): 350-600 ng/mL |
Table 2: Comparison of Dosing Strategy Performance in Improving Target Attainment Rates (Simulated Data)
| Dosing Strategy | Typical Target Attainment Rate (Fixed Dose) | Typical Target Attainment Rate (Strategy) | Required Number of TDM Samples | Time to Stable Dosing |
|---|---|---|---|---|
| Empirical (Weight-Based) | 30-50% | N/A | 0 | N/A |
| Reactive TDM (Trough-Based) | 30-50% | 60-75% | 3-5 over adjustment period | 7-14 days |
| Model-Informed Precision Dosing (Bayesian) | 30-50% | 75-90% | 1-2 for initial forecast | 2-5 days |
| Full Adaptive Control (with PD feedback) | 30-50% | >90% | 2-3 + PD biomarkers | Continuous |
Experimental Protocols
Protocol 1: Development and Validation of a Bayesian Forecasting Algorithm for Adaptive Dosing
Objective: To develop a algorithm that estimates individual PK parameters using 1-2 TDM samples and a population PK model, and to validate its prediction accuracy. Materials: See "The Scientist's Toolkit" below. Methodology:
- Model Priors: Embed a published population PK model (defining typical parameters, between-subject variability ω², and residual error σ²) into the algorithm's backend.
- Individual Data Input: For a new patient, input covariates (weight, serum creatinine, etc.), exact dosing history, and exact timing/concentration of 1-2 TDM samples.
- Bayesian Estimation: The algorithm computes the maximum a posteriori probability (MAP) estimate using the Bayes rule: Posterior ∝ Likelihood × Prior. It finds the individual parameter set (e.g., CL, Vd) that maximizes the probability of observing the measured TDM concentrations.
- Dose Prediction: Using the estimated individual parameters, the model simulates the PK profile for the next dosing interval and recommends a dose to achieve a predefined PK target (e.g., AUC or Cmin).
- Validation: Validate using a virtual patient population (Monte Carlo simulation) and a separate clinical dataset. Assess bias (Mean Prediction Error) and precision (Root Mean Square Error) of predicted vs. observed concentrations and AUCs.
Protocol 2: Conducting a Target Attainment Analysis for a High Variability Drug
Objective: To quantify the improvement in PK/PD target attainment rate after implementing a TDM-guided adaptive dosing strategy in a research cohort. Materials: Patient dosing/TDM records, PK/PD target definition, statistical software (R, SAS). Methodology:
- Define PK/PD Target: Establish a clinically validated target (e.g., vancomycin AUC₂₄/MIC ≥ 400).
- Cohort Definition: Define two matched cohorts: a historical control (empirical dosing) and a prospective intervention (TDM-guided adaptive dosing).
- PK Analysis: For each patient, estimate the key PK metric (e.g., AUC). Use non-compartmental analysis for rich data or Bayesian estimation for sparse TDM data.
- Attainment Classification: For each patient, classify as "Target Attained" or "Target Not Attained" based on Step 1.
- Statistical Comparison: Calculate the target attainment rate (%) for each cohort. Compare using a Chi-square test or logistic regression adjusting for key covariates (e.g., disease severity). Report Odds Ratio and 95% Confidence Interval.
Visualizations
Title: Adaptive Dosing with Bayesian TDM Workflow
Title: Research Thesis Framework for Dosing Strategies
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in HV Drug/TDM Research |
|---|---|
| LC-MS/MS System | Gold-standard for quantitative bioanalysis of drugs and metabolites in plasma/serum with high sensitivity and specificity, essential for accurate TDM. |
| Population PK Modeling Software (e.g., NONMEM, Monolix, Phoenix NLME) | Used to develop the prior population PK models that quantify variability and serve as the engine for Bayesian forecasting algorithms. |
| Model-Informed Precision Dosing (MIPD) Platform (e.g., InsightRX, Tucuxi, TDMx) | Clinical software that integrates the population model, patient data, and Bayesian algorithms to generate real-time, individualized dose recommendations. |
| Stable Isotope Labeled Internal Standards | Used in LC-MS/MS assay development to correct for matrix effects and recovery losses, improving assay accuracy and precision for variable matrices. |
| In Vitro Transport/Metabolism Assay Kits (e.g., CYP450, P-gp) | To identify and characterize sources of variability (e.g., drug-drug interactions, genetic polymorphisms) during early drug development. |
| Pharmacokinetic Simulator (e.g., Simcyp, GastroPlus) | For virtual trial simulations to predict variability, design optimal TDM sampling times, and assess target attainment probability of different dosing strategies. |
Technical Support Center: Troubleshooting PK/PD Target Attainment in Special Population Studies
Thesis Context: This support content is framed within a broader thesis aimed at improving pharmacokinetic-pharmacodynamic (PK/PD) target attainment rates through optimized study design and analysis for special populations.
FAQs & Troubleshooting Guides
Q1: During a pediatric population PK study, our model consistently fails to achieve acceptable covariate diagnostics (e.g., npde vs. time plots show trends). What are the primary troubleshooting steps?
A: This often indicates a misspecification of the allometric scaling approach or maturation function.
- Step 1: Verify the allometric exponents. Standard allometric scaling uses fixed exponents of 0.75 for clearance and 1 for volume. For neonates and infants, consider if these are appropriate or if empirical exponents should be estimated.
- Step 2: Re-evaluate the maturation model. For drugs cleared renally or hepatically, glomerular filtration rate (GFR) or cytochrome P450 maturation models (e.g., postmenstrual age, body weight) must be incorporated. The Hill-type maturation function is common:
MF = (PMA^HILL) / (TM50^HILL + PMA^HILL), where PMA is postmenstrual age and TM50 is maturity at 50% of adult activity. - Step 3: Check for overlooked covariates specific to pediatrics, such as formulation differences (e.g., syrup vs. tablet bioavailability) or disease state effects (e.g., organ failure in critically ill children).
Q2: In a hepatic impairment study, we observe high inter-individual variability in drug exposure that does not correlate well with Child-Pugh score alone. How should we refine our analysis?
A: Child-Pugh score has limitations in predicting metabolic capacity. Follow this protocol:
- Step 1: Incorporate quantitative liver function tests (QLFTs). Measure specific biomarkers like cholate clearance, antipyrine clearance, or albumin synthesis rate alongside PK sampling.
- Step 2: Use a physiologically based pharmacokinetic (PBPK) modeling approach. Populate the model with system-specific parameters (e.g., hepatic blood flow, enzyme abundance from in vitro data, albumin levels) for each impairment severity.
- Step 3: Perform a sensitivity analysis to identify the dominant physiological driver (e.g., hepatic blood flow vs. intrinsic clearance) for your specific drug's disposition.
Q3: When extrapolating doses from normal-weight to obese patients, volume of distribution (Vd) predictions using total body weight (TBW) lead to overdosing. What is the best practice for size descriptor selection?
A: The optimal size descriptor is drug-specific and related to its physicochemical properties.
- Protocol: Conduct a pilot analysis using a range of size metrics in your base PK model:
- Fit the model using TBW, ideal body weight (IBW), lean body weight (LBW), fat-free mass (FFM), and normalized fat mass.
- Compare objective function values (OFV) and precision of parameter estimates.
- For hydrophilic drugs, LBW or FFM often best predict Vd. For lipophilic drugs, a combination of LBW and fat mass may be required.
- Critical Step: Always validate the chosen descriptor with observed data from the target obese population.
Q4: For renal impairment studies, what is the optimal method to design a study that accurately captures the non-linear relationship between renal function (eGFR) and drug clearance (CL) for a renally eliminated compound?
A: Avoid stratifying solely by CKD category. Implement a continuous design.
- Methodology:
- Recruitment: Enroll participants across a continuous spectrum of estimated glomerular filtration rate (eGFR), from normal (>90 mL/min) to severe impairment (<30 mL/min), including those on dialysis.
- PK Sampling: Use rich or semi-rich sampling to characterize each individual's PK profile adequately.
- Modeling: Fit a population PK model where renal clearance (
CL_R) is related to eGFR via a parametric function (e.g., linear, power, or saturableEmaxrelationship):CL_R = θ1 * (eGFR/100)^θ2. The parameterθ2determines the linearity. - Dialysis Effect: Include a binary covariate (on/off dialysis) and estimate the fractional removal during the dialysis period.
Key Quantitative Data in Special Population PK
Table 1: Common Size Descriptors for Obesity PK Scaling
| Descriptor | Calculation (Male) | Calculation (Female) | Primary Use |
|---|---|---|---|
| Total Body Weight (TBW) | Measured Weight | Measured Weight | Often over-predicts Vd for hydrophilic drugs. |
| Ideal Body Weight (IBW) | 50 kg + 2.3 kg/inch >5ft | 45.5 kg + 2.3 kg/inch >5ft | Alternative for hydrophilic drugs; limited in severe obesity. |
| Lean Body Weight (LBW) | (9270 * TBW) / (6680 + 216 * BMI) |
(9270 * TBW) / (8780 + 244 * BMI) |
Often best for hydrophilic drug Vd and CL. |
| Fat-Free Mass (FFM) | (0.28 + 0.73*(HT^3)/TBW) |
(0.29 + 0.73*(HT^3)/TBW) |
Similar to LBW; commonly used in allometric scaling. |
Table 2: Hepatic Impairment Classification & PK Impact Expectation
| Child-Pugh Class | Score | Expected Hepatic CL Change | Key Study Design Consideration |
|---|---|---|---|
| A (Mild) | 5-6 | ↓ 20-50% | Include drugs with high hepatic extraction ratio for sensitive detection. |
| B (Moderate) | 7-9 | ↓ 50-80% | Crucial dose adjustment range; require stratified sampling. |
| C (Severe) | 10-15 | ↓ >80% | Assess impact on protein binding and consider portal-systemic shunting. |
Table 3: Pediatric Age Stratification & Physiological Considerations
| Age Group | Approximate Age | Key Physiological Covariates | Typical Allometric Exponent (CL) |
|---|---|---|---|
| Preterm | <37 wk PMA | PMA, GFR maturation, serum protein levels | Often < 0.75 |
| Term Neonate | 0-1 mo | PMA, weight, CYP enzyme maturation | 0.75-1.0 (variable) |
| Infant/Toddler | 1 mo - 2 yr | Weight, CYP maturation (rapid change) | Approaches 0.75 |
| Children | 2-12 yr | Weight, organ function mature | ~0.75 |
| Adolescent | 12-18 yr | Weight, puberty hormones (may affect enzymes) | 0.75 |
Experimental Protocols
Protocol 1: Population PK Study in Obese Patients
- Objective: To characterize the PK of Drug X in obese patients and identify optimal body size descriptor for dose individualization.
- Design: Single-dose, open-label, parallel-group study in 4 BMI cohorts (Normal: 18.5-25, Obese I: 30-35, Obese II: 35-40, Obese III: >40), n=10 per group.
- Dosing: Administer a fixed test dose intravenously.
- PK Sampling: Serial blood samples pre-dose and at 0.5, 1, 2, 4, 8, 12, 24, 36, 48 hours post-dose.
- Bioanalysis: Validate an LC-MS/MS method for Drug X quantification in plasma.
- Modeling: Develop a 2-compartment popPK model. Test TBW, IBW, LBW, FFM as covariates on CL and Vd using stepwise covariate modeling.
Protocol 2: Hepatic Impairment Study with PBPK Verification
- Objective: To determine the PK of a hepatically cleared Drug Y in subjects with varying hepatic impairment and verify with a PBPK model.
- Design: Single-dose study in 8 subjects per Child-Pugh A, B, C, and matched healthy controls.
- Dosing: Oral administration of Drug Y.
- PK Sampling: Rich sampling over 5 half-lives.
- QLFT: Intravenous cholate clearance test performed pre-dose.
- PBPK Modeling: Build model (e.g., in Simcyp or GastroPlus) using in vitro metabolism data. Adjust liver blood flow, CYP abundance, and plasma proteins per severity class. Compare simulated vs. observed profiles to validate.
Diagrams
Title: Workflow for PK/PD Optimization in Special Populations
Title: PBPK Modeling Approach for Hepatic Impairment (HI)
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for Special Population PK/PD Research
| Item / Reagent | Function & Application |
|---|---|
| Stable Isotope-Labeled Drug Standards | Essential for developing highly sensitive and specific LC-MS/MS bioanalytical assays to quantify drugs in small volume pediatric samples or complex matrices. |
| Human Liver Microsomes (HLM) & Hepatocytes | Used in in vitro metabolism studies to determine intrinsic clearance and metabolic pathways. Critical for PBPK model input, especially from donors with specific diseases. |
| Recombinant Human CYP Enzymes | To identify which specific cytochrome P450 enzymes metabolize a drug, informing potential drug-drug interaction and hepatic impairment risk. |
| Human Serum Albumin (HSA) & α-1-Acid Glycoprotein (AAG) | For in vitro plasma protein binding studies using techniques like equilibrium dialysis. Binding alterations in renal/hepatic disease are a key covariate. |
| Validated eGFR Calculators (CKD-EPI, Schwartz) | Software/scripts to accurately estimate renal function, the primary covariate for dose adjustment in renal impairment studies. |
| Allometric Scaling Software (e.g., Winnonlin, NONMEM, R/PK packages) | Population PK modeling software capable of implementing complex allometric and covariate models (maturation, size descriptors). |
| PBPK Simulation Platform (e.g., Simcyp Simulator, GastroPlus) | Industry-standard platforms containing libraries of population demographics and physiological parameters for special population simulations. |
| Biomarker Assay Kits (e.g., Cystatin C, Cholate) | For quantifying biomarkers of organ function (renal, hepatic) that serve as superior covariates compared to clinical scores alone. |
Addressing Drug-Drug Interactions and Food Effects in PTA Simulations
Technical Support Center
Troubleshooting Guides
Issue: PTA simulation results show unexpectedly low target attainment when a DDI is modeled.
- Step 1: Verify the inhibition/induction constant (Ki, IC50, or fold-induction) for the perpetrator drug in your model. Compare against authoritative sources like the FDA label or recent literature.
- Step 2: Check the enzyme/transporter abundance values in your population PK model. Ensure they are appropriate for your simulated population (e.g., healthy volunteers vs. patients with liver disease).
- Step 3: Confirm the fraction metabolized (fm) by the affected pathway for the victim drug. An incorrect fm can dramatically over- or under-predict DDI magnitude.
- Step 4: Validate the simulation time course. Ensure the perpetrator drug dosing leads to steady-state concentrations before assessing the DDI impact on the victim drug's PTA.
Issue: Simulated food effects do not match observed clinical data.
- Step 1: Review the implemented food effect model. Is it a simple bioavailability (F) increase, a change in absorption rate (Ka), or a more complex dissolution/profile model?
- Step 2: Calibrate the model using pilot study data. Use a sensitivity analysis to determine which parameter (e.g., Ka, lag time) most influences the Cmax and Tmax shifts.
- Step 3: Check for food-type specificity (high-fat vs. low-fat meal). Ensure the correct meal conditions are parameterized in your simulation scenario.
- Step 4: For drugs with complex solubility-limited absorption, verify that the in vitro biorelevant media data (e.g., FaSSIF/FeSSIF) are correctly linked to the in vivo model parameters.
Issue: High uncertainty (wide confidence intervals) in PTA estimates when variability is included.
- Step 1: Increase the number of virtual subjects in your Monte Carlo simulation. Start with at least 1000 subjects per trial, and consider 5000-10000 for stable estimates of tails of the distribution.
- Step 2: Examine the correlation structure between model parameters (e.g., between clearance and volume). Incorrect or missing correlations can inflate variability.
- Step 3: Verify the source and magnitude of inter-individual variability (IIV) and inter-occasion variability (IOV) assigned to key parameters. Overly high IIV can lead to unreliably wide PTA confidence intervals.
Frequently Asked Questions (FAQs)
Q1: What is the most reliable source for DDI parameters (Ki, IC50) to use in my PTA simulations? A: The most reliable sources are dedicated DDI databases (e.g., University of Washington's Metabolism and Transport Drug Interaction Database) and comprehensive, peer-reviewed systematic reviews. Always cross-reference with the latest clinical DDI study reports or FDA/EMA assessment documents, as in vitro parameters can be assay-dependent.
Q2: How should I model mechanism-based inactivation (MBI) of enzymes in a PTA simulation? A: MBI requires a dynamic model incorporating the inactivation rate constant (kinact) and the concentration required for half-maximal inactivation (KI). You must simulate the time-dependent loss of enzyme activity, which often requires a systems pharmacology framework (e.g., using Simcyp, GastroPlus, or custom PML in NONMEM) rather than simple static models.
Q3: Can I simulate the combined effect of a DDI and a food effect simultaneously? A: Yes, but it requires an integrated model where both mechanisms are accurately represented. The food effect may alter the perpetrator drug's exposure, thereby modulating the DDI magnitude. This necessitates sequential or simultaneous modeling of both processes and careful validation against clinical studies where both factors were assessed.
Q4: How do I translate a simulated PTA change due to DDI/Food into a clinically actionable dosing recommendation? A: Run scenario-based simulations: compare PTA under DDI/food vs. baseline. If PTA falls below a target threshold (e.g., 90%), simulate alternative dosing regimens (dose adjustment, timing change) until the target PTA is restored. The output is a data-supported proposal for a label recommendation (e.g., "Avoid concomitant use" or "Take with food").
Q5: My PTA for efficacy is acceptable, but the PTA for toxicity is exceeded under DDI conditions. How should this be interpreted? A: This indicates a narrowing of the therapeutic window. The dosing regimen may need to be modified to balance risks and benefits. Present the joint probability of efficacy and toxicity (a two-dimensional PTA) to inform decision-making. This is a critical component of comprehensive PK/PD target attainment rate improvement research.
Table 1: Common CYP450 Enzyme Parameters for DDI Simulation
| Enzyme | Typical Abundance (pmol/mg protein) | Common Probe Substrate | Typical Fold Induction Range (Strong Inducer) |
|---|---|---|---|
| CYP3A4 | 80 - 150 | Midazolam | 5 - 10 (Rifampin) |
| CYP2D6 | 5 - 15 | Dextromethorphan | Not typically inducible |
| CYP2C9 | 45 - 75 | S-Warfarin | 3 - 6 (Rifampin) |
| CYP2C19 | 10 - 25 | Omeprazole | 3 - 8 (Rifampin) |
| CYP1A2 | 30 - 60 | Caffeine | 2 - 5 (Smoking) |
Table 2: Impact of Food on Key PK Parameters for BCS Classes
| BCS Class | Typical Effect on Bioavailability (F) | Typical Effect on Cmax | Typical Effect on Tmax |
|---|---|---|---|
| I (High Solubility, High Permeability) | Minimal Change (±10%) | Minimal Change (±15%) | Variable (May delay) |
| II (Low Solubility, High Permeability) | Increase (20-100%+) | Variable (Often Increase) | Delayed |
| III (High Solubility, Low Permeability) | Variable (May Increase) | Decrease | Delayed |
| IV (Low Solubility, Low Permeability) | Unpredictable | Unpredictable | Significantly Delayed |
Experimental Protocols
Protocol 1: In Vitro-to-In Vivo Extrapolation (IVIVE) for DDI Risk Assessment
- Purpose: To predict clinical DDI magnitude from in vitro inhibition data.
- Materials: Human liver microsomes (HLM) or recombinant enzymes, test compound (inhibitor), probe substrate, co-factor regeneration system, LC-MS/MS.
- Method: a. Conduct time-dependent inhibition (TDI) assays if MBI is suspected, measuring pre-incubation effects. b. Determine IC50 values for the test compound against major CYP enzymes using validated probe reactions. c. Calculate the [I]/Ki or [I]/IC50 ratio, where [I] is the estimated maximal unbound plasma concentration of the inhibitor. d. Use a static model (e.g., FDA/EMA decision tree) or incorporate parameters into a dynamic PBPK model for simulation.
Protocol 2: Assessing Food Effect Using a PBPK Modeling Approach
- Purpose: To simulate the impact of food on drug absorption and exposure (AUC, Cmax).
- Materials: Drug physicochemical properties (pKa, logP), biorelevant solubility data (FaSSGF, FeSSGF, FaSSIF, FeSSIF), dissolution profiles, population simulator (e.g., Simcyp, GastroPlus).
- Method: a. Develop a base fasted-state PBPK model validated against clinical PK data. b. Integrate food effect components: changes in gastric pH, bile salt secretion, and gastric emptying time into the model's advanced dissolution, absorption, and metabolism (ADAM) or compartmental absorption and transit (CAT) module. c. Input drug-specific data on food-induced solubility/permeability changes. d. Simulate fed-state conditions (e.g., high-fat meal) and compare PK profiles and PTA outcomes against fasted-state simulations.
Diagrams
Title: Workflow for PTA Simulation with DDI/Food Effects
Title: Key Mechanism of Drug-Drug Interaction
The Scientist's Toolkit: Research Reagent & Software Solutions
| Item | Function / Purpose | Example(s) |
|---|---|---|
| PBPK/PD Simulation Software | Platform for building, validating, and running complex simulations integrating DDI, food effects, and population variability. | Simcyp Simulator, GastroPlus, PK-Sim, Berkeley Madonna. |
| DDI Parameter Database | Curated source of reliable in vitro inhibition/induction constants (Ki, IC50, kinact) and clinical DDI outcomes. | University of Washington DDI Database, DrugBank, Lexicomp. |
| Biorelevant Dissolution Media | In vitro media mimicking fasted and fed state intestinal fluids to measure solubility and dissolution for food effect modeling. | FaSSGF, FeSSGF, FaSSIF, FeSSIF (Biorelevant.com). |
| Human Liver Microsomes (HLM) / Hepatocytes | In vitro system for determining metabolic stability, reaction phenotyping, and obtaining enzyme kinetic parameters for IVIVE. | Xenotech, BioIVT, Corning Life Sciences. |
| Population PK/PD Model Repository | Source of published, peer-reviewed models that can serve as a starting point for developing a base simulation model. | Model repositories within software, NIH DDI Working Group templates, published literature. |
| Statistical & Scripting Environment | For data analysis, custom model coding, and automating simulation workflows and result summarization. | R (with mrgsolve, RxODE), Python (with PySB, SciPy), MATLAB. |
Troubleshooting Guides & FAQs
This technical support center addresses common challenges in PK/PD target attainment research, a critical component of improving drug development success rates.
FAQ 1: How do I determine if my target attainment failure is due to an incorrect PK/PD target index or poor drug-like properties?
Answer: A systematic deconvolution experiment is required. First, conduct a robust in vivo PK study in the relevant disease model to obtain accurate AUC, Cmax, and T>MIC (Time above Minimum Inhibitory Concentration) values. Compare these against your in vitro-derived PD target (e.g., fAUC/MIC). If the achieved exposure (PK) meets or exceeds the in vitro target but efficacy is still lacking, the in vitro PK/PD target index itself may not translate to the in vivo setting. Conversely, if exposure consistently falls short of the target despite adequate dosing, the issue likely lies with the drug candidate's pharmacokinetic properties (e.g., poor solubility, high clearance, inadequate tissue penetration).
Protocol: Translational PK/PD Target Validation
- Define PD Target: Establish a robust in vitro PK/PD index (e.g., %fT>MIC, AUC/MIC) using a static time-kill assay.
- In Vivo PK Study: Administer the drug candidate to infected or diseased animal models (n≥5/group) at three dose levels. Collect serial plasma and target tissue samples over 24-48 hours. Analyze using a validated LC-MS/MS method.
- PK/PD Linking: Use non-compartmental analysis (NCA) to calculate PK parameters. Link individual animal PK profiles to the observed PD outcome (e.g., bacterial burden, tumor size reduction, biomarker change) using an Emax model or logistic regression.
- Compare Targets: The in vivo PK/PD target (e.g., the AUC/MIC yielding a 50% maximal effect) is derived from the linked model. Statistically compare this value to your original in vitro target.
FAQ 2: What are the key experimental steps when re-evaluating a PK/PD target?
Answer: Re-evaluation requires moving beyond standard in vitro models to more physiologically relevant systems. The core steps are:
- Challenge the In Vitro Assay Conditions: Repeat PD assays in the presence of physiological protein levels, in biofilm models, or in co-cultures with immune cells.
- Incorrate Host Factors: Evaluate the target in an in vivo neutropenic vs. immunocompetent model to assess the impact of immune system contribution.
- Model Disease State: Use models that replicate the human disease pathology (e.g., acidotic infection sites, hypoxic tumors) as these can drastically alter drug activity.
- Utilize Humanized Models/Translational Biomarkers: If available, use humanized mouse models or identify a translational biomarker that can bridge from preclinical models to human patients.
Protocol: In Vitro PD Assay in a Physiologically Relevant Environment
- Prepare Media: Supplement standard assay media with 50-100% human serum or ascites fluid from diseased patients to mimic protein binding and tissue environment.
- Inoculum Preparation: For antibiotics, use high-density inocula (e.g., 10^8 CFU/mL) or pre-formed biofilms. For oncology, use 3D spheroid cultures.
- Drug Exposure: Use a hollow-fiber infection model (for antibiotics) or a programmable bioreactor to simulate human PK profiles (multi-exponential decay) rather than static concentrations.
- Outcome Measures: Sample at multiple timepoints to measure not just endpoint effect, but the rate of kill or tumor growth inhibition. Fit data to a dynamic PK/PD model.
FAQ 3: What are the primary experiments to run when considering a drug candidate modification?
Answer: Focus on ADME (Absorption, Distribution, Metabolism, Excretion) optimization. Key experiments include:
- For Poor Exposure: Conduct in vitro metabolic stability assays in human liver microsomes (HLM) and hepatocytes. Perform permeability assays (Caco-2, PAMPA) and assess efflux transporter liability.
- For High Variability: Investigate the potential for drug-drug interactions (CYP inhibition/induction) and assess food effect in vivo.
- For Inadequate Tissue Penetration: Measure plasma vs. tissue drug concentrations in target organs (e.g., lung, brain, bone). Use quantitative whole-body autoradiography (QWBA) for distribution visualization.
- For High Clearance: Perform bile-duct cannulated studies to determine the fraction excreted unchanged vs. metabolized.
Protocol: Tiered ADME Optimization Screening
- Tier 1 (High-Throughput): Screen analogues for solubility (thermodynamic & kinetic), metabolic stability in HLM, and passive permeability.
- Tier 2 (Mechanistic): For compounds passing Tier 1, identify major metabolites (using LC-HRMS), determine CYP reaction phenotyping, and assess active transport (using transfected cell lines).
- Tier 3 (In Vivo Confirmation): Select 2-3 lead analogues from Tier 2. Conduct cassette dosing or standalone PK studies in rodents to confirm improved AUC, half-life, and bioavailability compared to the parent candidate.
Data Presentation
Table 1: Decision Matrix: Re-evaluate Target vs. Modify Drug Candidate
| Observation / Data Outcome | Suggested Action | Key Supporting Experiments |
|---|---|---|
| In vivo efficacy requires exposure 5-10x higher than in vitro target predicts. | Re-evaluate PK/PD Target | In vitro PD assay in host-mimicking conditions; In vivo PK/PD linking in immunocompetent model. |
| Excellent in vitro potency, but very short half-life (<1 hr) and low bioavailability (<10%) in multiple animal models. | Modify Drug Candidate | Metabolic stability screening; prodrug strategy; formulation optimization (e.g., nano-sizing). |
| PK/PD target is consistently met in healthy animals but not in diseased state models. | Re-evaluate PK/PD Target | PK study in robust disease model; measure free drug concentration at effect site. |
| Good exposure but poor efficacy, and in vitro activity is highly dependent on specific assay conditions (e.g., pH). | Re-evaluate PK/PD Target | PD assays across a range of physiologically relevant conditions (pH, oxygen tension). |
| Exposure is highly variable and correlates with the expression of a specific efflux transporter. | Modify Drug Candidate | Transporter inhibition assays; medicinal chemistry to remove transporter substrate motif. |
| The original in vitro PK/PD target was derived from a surrogate endpoint, not the primary clinical endpoint. | Re-evaluate PK/PD Target (Critical) | Establish a translational biomarker bridge; develop a clinical PK/PD model from early phase data. |
Table 2: Quantitative Outcomes from Common Pivot Strategies
| Pivot Strategy | Typical Experimental Timeline | Success Rate* (Lead to Candidate) | Key Quantitative Metrics Improved |
|---|---|---|---|
| PK/PD Target Re-evaluation | 6-12 months | ~40-50% | In vivo EC50/EC90, Stochastic Target Attainment Rate, PTA |
| Lead Optimization (ADME) | 12-24 months | ~20-30% | Clearance (CL), Volume (Vd), Half-life (t1/2), Bioavailability (F%) |
| Formulation Change | 9-18 months | ~30-40% | Cmax, AUC, Variability (CV%), T>MIC |
| Prodrug Strategy | 18-30 months | ~15-25% | F%, Time to Cmax (Tmax), Tissue/Plasma Ratio |
| Combination Therapy Strategy | 12-24 months | ~50-60% | Fraction Affected (Fa), Combination Index (CI), Synergy Score |
Based on industry benchmarking data. *Higher as it bypasses some single-agent development hurdles.
Visualizations
Diagram 1: PK/PD Target Attainment Analysis Workflow
Diagram 2: Key ADME Properties & Optimization Levers
The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Example Product/Model | Primary Function in PK/PD Target Research |
|---|---|---|
| Physiologically Relevant Assay Media | Human Serum (Charcoal-stripped or disease-state), SynVivo systems | Mimics in vivo protein binding, cytokine milieu, and cell-to-cell interactions for more predictive in vitro PD. |
| Hollow Fiber Infection Model (HFIM) | FiberCell Systems, customized bioreactors | Simulates human PK profiles in vitro for antibiotics/antivirals, allowing precise PK/PD index determination without animal use. |
| In Vivo Imaging System (IVIS) | PerkinElmer IVIS Spectrum, Bruker Xtreme | Enables longitudinal, quantitative tracking of disease progression (e.g., bioluminescent infection, tumor growth) and drug distribution in live animals. |
| LC-MS/MS System | Sciex Triple Quad, Waters Xevo TQ-S | Quantifies drug and metabolite concentrations in biological matrices (plasma, tissue) with high sensitivity and specificity for PK studies. |
| Automated Blood Samplers | Culex, BASi AccuSampler | Allows frequent, precise blood sampling from rodents without human intervention or stress, generating rich PK profiles. |
| PBPK Modeling Software | GastroPlus, Simcyp Simulator | Integrates in vitro ADME and system data to predict human PK, explore formulation effects, and model target attainment probabilistically. |
| 3D Cell Culture Systems | Corning Spheroid Microplates, Merck Biowire | Provides a more pathophysiological model for oncology and virology PD studies, assessing drug penetration and efficacy in tissue-like structures. |
| CYP & Transporter Assay Kits | Reaction Phenotyping Kits (BD Biosciences), Transporter Assay Systems (Solvo) | Identifies key enzymes/transporters involved in drug clearance and distribution, guiding candidate modification strategies. |
Validating Success: From Simulation to Clinical Confirmation
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During internal validation of my PTA model, the prediction error is unacceptably high (>30%) for the test subset. What are the primary steps to diagnose this issue?
A1: High prediction error typically indicates model overfitting or issues with data partitioning.
- Verify Data Splitting: Ensure your training and test sets are truly independent and representative of the overall population. Check for temporal or demographic biases in the split.
- Re-check Structural Model: Re-evaluate the base pharmacokinetic (PK) and pharmacodynamic (PD) models. Use diagnostic plots (e.g., observed vs. predicted, residuals) from the training data only to identify structural model misspecification.
- Simplify the Model: If a complex covariance model was used, reduce random effects or simplify the omega matrix. Over-parameterization is a common cause of poor external predictive performance.
- Check for Influential Individuals: Perform an influence analysis (e.g., case deletion diagnostics) on the training set to see if the model is unduly influenced by outliers.
Q2: My externally validated model performs well on one cohort but fails on a new patient population. What does this imply and how should I proceed?
A2: This indicates a lack of transportability and possible covariate misspecification.
- Conduct Covariate Analysis: Systematically compare the demographic (weight, age, renal/hepatic function) and pathophysiological (disease state, concomitant medications) covariates between the development and new validation cohorts.
- Perform a Simulation-Based Assessment: Use your final model to simulate the new study's design and outcomes. Compare the simulated distribution of exposures (e.g., AUC, Cmin) to the observed data from the new cohort using prediction-corrected visual predictive checks (pcVPC).
- Update the Model: If a clinically relevant covariate is identified, consider a model update with appropriate documentation, treating the new cohort as part of an expanded development dataset. This refined model will require a new round of validation.
Q3: What is the best metric to use for comparing the predictive performance of two different PTA models for the same drug?
A3: No single metric is sufficient. A combination should be used, as summarized in the table below.
Table 1: Key Metrics for Comparing PTA Model Predictive Performance
| Metric | Description | Interpretation for PTA Models | Target Threshold |
|---|---|---|---|
| Mean Absolute Error (MAE) | Average absolute difference between predicted and observed concentrations. | Measures average prediction accuracy. Lower is better. | Context-dependent; <20% of typical concentration is desirable. |
| Root Mean Squared Error (RMSE) | Square root of the average squared differences. | Penalizes large prediction errors more heavily than MAE. | Lower is better. Compare between models. |
| Prediction-Based Confidence Interval (CI) | Non-parametric CI around the prediction error. | Assesses precision of predictions. | The 90% CI should be narrow and contain zero. |
| Normalized Prediction Distribution Errors (NPDE) | Measures if the distribution of predictions matches observations. | Superior to individual prediction errors for distribution assessment. | Mean NPDE ~0, variance ~1, and a normal Q-Q plot. |
| Simulation-Based PTA Comparison | Compare the PTA curve (e.g., %PTA vs. MIC) generated from model-predicted vs. observed data. | Directly assesses the impact on the target clinical metric. | The PTA curves should be visually and statistically congruent. |
Q4: My PTA simulations for a prolonged infusion regimen are not matching observed clinical outcomes. What could be wrong with the in vitro PK/PD index assumptions?
A4: This often stems from mismatched static in vitro PK/PD indices (e.g., fT>MIC) and dynamic in vivo conditions.
- Re-visit the PD Driver: Verify the correct PK/PD index (fT>MIC, fAUC/MIC, fCmax/MIC) for your drug class and regimen. For example, beta-lactams with prolonged infusion are tightly linked to fT>MIC, but the optimal target may shift with the dosing schedule.
- Check Protein Binding: Ensure the unbound (free) fraction (f) used in simulations is correct for the patient population (e.g., critically ill patients often have altered protein binding).
- Validate the PK/PD Target: The specific target value (e.g., fT>MIC of 60%) may be regimen-dependent. Conduct a sensitivity analysis around the literature-derived target using your specific population PK model.
Experimental Protocols for Key Validation Experiments
Protocol 1: Bootstrap Internal Validation for a Population PK/PD Model Objective: To assess the internal stability and precision of model parameter estimates. Method:
- Generate 1000 bootstrap datasets by randomly sampling individuals from the original dataset with replacement, maintaining the original sample size.
- Fit the final population PK/PD model to each bootstrap dataset.
- Collect the estimated parameters (fixed effects, random effects variances) from each successful run.
- Calculate the median and 2.5th-97.5th percentiles (95% confidence intervals) of the parameter distributions.
- Compare the original model parameter estimates to the median and confidence intervals from the bootstrap. Agreement indicates robustness.
Protocol 2: External Validation Using a Prediction-Corrected Visual Predictive Check (pcVPC) Objective: To visually evaluate how well model simulations match observed data from a new, external cohort. Method:
- Using the finalized model and the original dataset, simulate 1000 replicates of the external validation dataset, matching its design exactly (doses, covariates, sampling times).
- For each observation in the external dataset, calculate the prediction-corrected observed value to account for variability in dosing and sampling times.
- For each simulated replicate, calculate the same prediction-corrected values.
- Bin the data (typically by time or predicted concentration). In each bin, calculate the median and 5th/95th percentiles of the simulated prediction-corrected data.
- Overlay the median and 5th/95th percentiles of the observed prediction-corrected data on the same plot.
- Interpretation: The observed percentiles should generally fall within the confidence intervals of the simulated percentiles, indicating adequate predictive performance.
Signaling Pathway & Workflow Diagrams
Title: Workflow for PTA Model Internal and External Validation
Title: Logical Relationship from PK Model to PTA and CFR Prediction
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for PTA Model Development and Validation
| Item / Software | Category | Function in PTA Research |
|---|---|---|
| NONMEM | Modeling Software | Industry-standard for nonlinear mixed-effects modeling (pop PK/PD). Estimates population parameters and variability. |
| R (with packages) | Statistical Programming | Critical for data preparation (dplyr), diagnostic plotting (ggplot2), model evaluation (xpose), and running simulation-based validations (PsN, mrgsolve). |
| Perl Speaks NONMEM (PsN) | Toolkit | Automates complex modeling tasks, including bootstrap, VPC, and stepwise covariate model building. |
| Monolix | Modeling Software | Alternative to NONMEM; uses stochastic approximation expectation-maximization (SAEM) algorithm. User-friendly interface. |
| Pumas | Modeling Software | Modern, Julia-based platform for PK/PD modeling, simulation, and AI/ML integration. Enables efficient workflow. |
| Xpose | R Package | Specialized for creating diagnostic plots (e.g., goodness-of-fit, residuals) for NONMEM models. |
| mrgsolve | R Package | Efficiently simulates from PK/PD models (described in R/C++) within R. Ideal for internal simulation-based validation. |
| Patient/Pathogen Database | Data Source | Curated repository of historical patient PK data and local/regional pathogen MIC distributions. Essential for model building and CFR calculation. |
Technical Support Center
Troubleshooting Guides & FAQs
1. Model Discrepancy & Fit Issues
Q1: Our prior PBPK model, built from Phase 1 data, fails to predict the observed Phase 2a PK profiles. The predicted concentrations are systematically biased. What are the primary troubleshooting steps?
- A: This often indicates unaccounted-for patient factors in Phase 2. Follow this protocol:
- Verify Input Parameters: Re-check and update the model's population simulator with the exact demographic (e.g., age, weight, renal function), comedication, and disease severity profiles of your Phase 2a cohort.
- Check for Disease Effect: Implement a systematic evaluation of disease impact on PK parameters (CL, Vd, F). Design a sensitivity analysis workflow where you incrementally alter these parameters within physiologically plausible ranges (see Table 1) and re-simulate.
- Protocol-Specific Factors: Ensure dosing conditions (fasted/fed) and formulation used in Phase 2a are correctly reflected in the model's absorption subroutine.
- Model Re-estimation: If bias remains, use the Phase 2a PK data to re-estimate a limited set of key parameters (e.g., typical clearance and its variance) within the existing model structure, formally bridging Phase 1 and 2a.
- A: This often indicates unaccounted-for patient factors in Phase 2. Follow this protocol:
Q2: When integrating PD biomarkers, the model predicts target attainment rates far higher than the observed clinical response. How should we investigate this disconnect?
- A: This suggests a flaw in the PK/PD linkage. Execute this protocol:
- Verify Biomarker Fidelity: Confirm the in vivo biomarker is a direct and reliable surrogate for the intended pharmacological effect. Review preclinical validation data.
- Incorporate Temporal Disconnect: Model a delay between plasma PK and PD effect using an effect compartment or indirect response model. Estimate the rate constant for effect compartment equilibration (
k_e0). - Account for Pathway Saturation: Your model may assume linear transduction. Implement an
Emaxmodel to capture saturation of the target engagement or downstream signaling. - Validate with Individual Patient Data: Plot individual PK/PD pairs (not just population means) to identify subpopulations with different PD characteristics.
- A: This suggests a flaw in the PK/PD linkage. Execute this protocol:
2. Data Integration & Workflow Challenges
- Q3: What is the optimal method to visually and quantitatively bridge population simulations with sparse Phase 2b data to confirm attainment?
- A: Use a Visual Predictive Check (VPC) stratified by key covariates (e.g., renal impairment). The protocol:
- Simulate: Use the final model to simulate 1000+ virtual trials matching the Phase 2b study design and population.
- Calculate Percentiles: For each post-dose time bin, calculate the 5th, 50th, and 95th percentiles of the simulated concentration (or PD effect) distributions.
- Overlay & Compare: Overlay the observed Phase 2b data (as percentiles or individual points) on the simulation intervals.
- Quantitative Check: Calculate the percentage of observed data points falling within the 90% prediction interval (PI). A well-calibrated model will have ~90% of observations inside the PI. See Table 2 for an example.
- A: Use a Visual Predictive Check (VPC) stratified by key covariates (e.g., renal impairment). The protocol:
Data Presentation
Table 1: Sensitivity Analysis for Disease Impact on PK
| Parameter | Baseline (Healthy) | Tested Range (Disease) | Impact on AUC (Simulated) | Impact on Cmax (Simulated) |
|---|---|---|---|---|
| Clearance (CL) | 10 L/h | 5 - 15 L/h (+50%/-50%) | -33% to +100% | -25% to +50% |
| Volume (Vd) | 100 L | 70 - 130 L (+30%/-30%) | No change | -23% to +18% |
| Bioavailability (F) | 80% | 50% - 100% | -38% to +25% | -38% to +25% |
Table 2: Visual Predictive Check Results for Phase 2b PK Attainment
| Time Bin (hr) | Observed Median (ng/mL) | Simulated 90% PI (ng/mL) | Observed Data within PI | Model Pass? |
|---|---|---|---|---|
| 0-2 | 145 | [98 - 210] | 92% | Yes |
| 2-8 | 89 | [60 - 155] | 88% | Yes |
| 8-24 | 32 | [20 - 58] | 95% | Yes (over-predictive) |
| Overall | - | - | 91.7% | Yes |
Experimental Protocols
Protocol: Bayesian Forecasting for Dose Adjustment in Phase 2b
- Objective: Utilize early Phase 2b PK data from a patient to refine their subsequent dose and improve individual target attainment.
- Method: a. Start with the population PK model as the prior. b. After obtaining 1-2 PK samples from the patient at pre-specified times (e.g., trough and post-dose), use Bayesian estimation (software: NONMEM, Monolix) to compute the posterior estimates of CL and Vd for that individual. c. Using the individualized posterior model, simulate the PK profile for the remainder of the dosing regimen. d. If the simulated exposure falls outside the target AUC or Cmax window, calculate an adjusted dose (Dosenew = Doseoriginal * (TargetAUC / PredictedAUC)). e. Administer the adjusted dose for subsequent cycles.
- Endpoint: Proportion of patients maintained within the target exposure window compared to a fixed-dosing cohort.
Mandatory Visualization
Title: PK/PD Model Bridging & Validation Workflow
Title: Integrated PK/PD/Outcome Cascade Model
The Scientist's Toolkit: Research Reagent & Software Solutions
| Item | Category | Function in Attainment Research |
|---|---|---|
| Validated PD Biomarker Assay | Reagent/Kit | Quantifies target engagement or proximal downstream effect; critical for building the PD model component. |
| Population PK/PD Software (NONMEM, Monolix) | Software | Performs nonlinear mixed-effects modeling, simulation, and Bayesian forecasting for population & individual predictions. |
| PBPK Platform (GastroPlus, Simcyp) | Software | Simulates absorption and PK in virtual populations; used for first-in-human to patient translation. |
| Clinical Data Manager (e.g., R, Python Pandas) | Software Tool | Cleans, merges, and formats sparse clinical PK/PD data for analysis in modeling software. |
| Virtual Population Generator | Software Module | Creates physiologically plausible virtual patients matching trial inclusion/exclusion criteria for trial simulations. |
Technical Support Center: Troubleshooting & FAQs
Frequently Asked Questions
Q1: During a PK/PD target attainment simulation in Phoenix, my model run fails with "Integration Error" or "Matrix Singularity". What are the most common causes and fixes?
A: This error typically originates from the model specification or the data. Common causes and solutions are:
- Initial Estimates: Poor initial parameter estimates can cause the solver to fail. Use preliminary graphical analysis or a simpler model to obtain better estimates.
- Dosing Records: Check for inconsistencies in dosing records (e.g., time of dose vs. first observation). Ensure infusion doses are correctly specified with rate and duration.
- Structural Model Identifiability: The chosen structural model (e.g., three-compartment) may be too complex for your data. Simplify the model or fix certain parameters to known values.
- Error Model: An inappropriate residual error model can cause instability. Try switching from proportional to additive or combined error models.
- Action: In Phoenix, use the "Model Validation" tools to check data alignment. Re-run with
NLMEengine options like "Use Stochastic Approximation Expectation-Maximization (SAEM)" for more robustness in initial phases.
Q2: In Monolix, what does the warning "Likelihood calculation issues" mean and how does it impact the reliability of my parameter estimates for target attainment predictions?
A: This warning indicates problems during the likelihood computation, often due to the stochastic approximation algorithm. Impact and solutions include:
- Impact: The log-likelihood (LL), AIC, and BIC values may be inaccurate, complicating model selection. Population parameter estimates are usually stable, but standard errors and individual parameter (ETA) distributions may be biased.
- Solutions:
- Increase the number of iterations in the "Stochastic Approximation" and "Standard Error Estimation" tasks.
- Check the "Individual fits" plot for outliers; consider removing problematic subjects if justified.
- Simplify the statistical model (e.g., reduce covariance blocks).
- For final model, switch to the "Importance Sampling" algorithm for an exact LL calculation.
Q3: When using NONMEM for a covariate model building to explain variability in drug exposure, I encounter termination errors like "TERMINATION DUE TO ROUNDING ERRORS". What steps should I take?
A: This is a common NONMEM error indicating numerical problems. Follow this protocol:
- Bounds: Apply realistic bounds (
$THETA...(...)) to parameters (e.g., volumes > 0, clearances > 0). - Rescale Parameters: If parameters differ by orders of magnitude (e.g., Ka=1.5, V=500), rescale them (e.g., V=0.5 and adjust units).
- Initial Estimates: Re-evaluate your initial estimates from a previous, successful run.
- Data Check: Look for individuals with extremely high or low concentrations that might destabilize the model.
- Control Stream: Use
SIGL=9, SIGDIG=3in$ESTIMATIONto increase numerical precision. Ensure$ABBREVIATEDcode is correctly written.
Q4: For R/Python (RxODE/rxode2, mrgsolve, PyPKPD) users performing Bayesian forecasting for dose individualization, how can I diagnose and fix slow or non-converging MCMC chains (Stan/pymc)?
A: Slow convergence in MCMC is often a model specification issue.
- Diagnosis: Use trace plots (chains should be "fuzzy caterpillar") and the Gelman-Rubin statistic (R-hat > 1.01 indicates non-convergence).
- Fixes:
- Reparameterize: Use non-centered parameterizations for hierarchical models (e.g.,
theta ~ normal(mu, tau)becomesz ~ normal(0,1); theta = mu + tau * z). - Priors: Use informative, weakly regularizing priors instead of flat priors to guide sampling.
- Scaling: Standardize continuous covariates (mean=0, sd=1).
- Thinning & Adaptation: Increase the
adapt_delta(Stan) to reduce divergent transitions. In PyMC, tune samplers for longer.
- Reparameterize: Use non-centered parameterizations for hierarchical models (e.g.,
Table 1: Core Technical Specifications & Performance
| Feature | Certara Phoenix NLME | Monolix (Lixoft) | NONMEM (ICON) | R/Python (Open-Source) |
|---|---|---|---|---|
| Primary Engine | Dual: LS (for classical) & NLME | SAEM + Importance Sampling | SAEM, IMP, FO, FOCE | Multiple: SAEM (nlmixr), Hamiltonian MCMC (Stan) |
| Execution Interface | GUI with workflow wizards | GUI (Simulx) & Command-line | Command-line / Text files | Script-based (RStudio, Jupyter) |
| Parallel Computing | Built-in (local & grid) | Built-in (local & grid) | Requires external wrappers (PsN) | Native via parallel, future, or Dask |
| Model Syntax | GUI-based or PML | MLXTRAN (text-based) | NM-TRAN (control stream) | R: nlmixr, lme4 / Python: domain-specific code |
| Visual Diagnostics | Extensive, automated | Comprehensive, automated | Limited, requires scripting (e.g., Xpose) | Highly customizable (ggplot2, Matplotlib) |
| Typical Run Time | Fast (GUI optimized) | Fast (C++ engine) | Variable, often slower | Highly variable (model/code dependent) |
Table 2: PK/PD Target Attainment Analysis Features
| Capability | Phoenix | Monolix | NONMEM | R/Python |
|---|---|---|---|---|
| Built-in TAR Simulation | Yes (via Phoenix Validate) | Yes (via Simulx Suite) | No, requires manual scripting | Requires full custom development |
| FDA/EMA Compliance Tools | Full audit trail, 21 CFR Part 11 | Audit trail, validation package | Minimal, depends on practices | None inherently; requires framework |
| Covariate Model Building | Stepwise COV, SCM | Correlation plots, COV steps | Manual or via PsN | Manual, stepwise, or machine learning |
| VPC for TAR Validation | Automated generation | Automated generation | Requires PsN (vpc) |
Packages available (vpc, Miryx) |
| License Cost | High (Commercial) | Moderate (Commercial) | High (Commercial) | Free (Open-Source) |
Experimental Protocols
Protocol 1: Benchmarking Estimation Accuracy for a Two-Compartment IV Model
- Objective: Compare the accuracy and precision of parameter estimates (CL, Vd, Q, Vp) across tools using a simulated dataset with known parameters.
- Dataset: Simulate 1000 subjects with 8 samples each using
mrgsolve(R), introducing proportional (20%) and additive (0.1 ug/mL) error. Introduce known covariate relationships (e.g., CL ~ CrCl). - Method:
- Export the true dataset to CSV format.
- Fit the true structural model in each software:
- Phoenix/NONMEM/Monolix: Use identical initial estimates (20% offset from true values).
- R (
nlmixr2): Usefoceiestimator.
- For each tool, run the estimation 100 times using different random seeds on a subset (n=50) via bootstrapping.
- Calculate % bias and relative root mean square error (RMSE) for each parameter vs. the known simulation values.
- Record computation time per run.
Protocol 2: Workflow for PK/PD Target Attainment Rate Simulation & Optimization
- Objective: Determine the optimal dosing regimen to achieve >90% probability of target attainment (PTA) for a bacteriostatic antibiotic (fAUC/MIC > 30).
- Method:
- Base Model: Develop a final population PK model from Phase 1 data in your primary software (e.g., Monolix).
- Export Parameters: Save the final parameter estimates, including the variance-covariance matrix of ETAs.
- Virtual Population: Generate a virtual patient population (n=5000) matching Phase 3 demographics using the
simulx(Monolix) orrxSolve(R) function, incorporating the parameter uncertainty. - PD Target: Define the PD target (fAUC/MIC > 30) and a range of MIC values (0.125 to 32 mg/L).
- Regimen Simulation: Simulate PK profiles for multiple dosing regimens (e.g., 500mg q12h, 750mg q24h, 1000mg q24h).
- PTA Calculation: For each regimen/MIC combination, calculate the PTA as the proportion of virtual patients achieving the target.
- Optimal Dose: Identify the regimen that yields PTA >90% at the clinical breakpoint MIC (e.g., 2 mg/L). Validate with a visual predictive check of the simulated exposures.
Diagrams
Title: PK/PD Target Attainment Analysis Workflow
Title: Software Tool Selection Logic for PK/PD Research
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for PK/PD Target Attainment Research
| Item | Function in Research | Example/Note |
|---|---|---|
| Validated PopPK/PD Software | Core engine for nonlinear mixed-effects modeling, essential for quantifying inter-individual variability. | Phoenix NLME, Monolix, NONMEM. |
| Scripting Environment (R/Python) | For data wrangling, custom simulations, advanced diagnostics, and creating reproducible analysis pipelines. | RStudio with tidyverse, nlmixr2. Jupyter with PyPKPD, pandas. |
| Clinical Dataset (ADaM Format) | Standardized analysis-ready subject-level data containing PK concentrations, dosing records, and covariates. | Requires proper anonymization and ethical approval. |
| PD Target Value | The specific exposure metric (e.g., fAUC/MIC) and its critical threshold defining efficacy/toxicity. | Derived from preclinical/clinical literature (e.g., fAUC/MIC > 100 for bactericidal effect). |
| Virtual Population Simulator | Tool to generate realistic virtual patients reflecting target population demographics and covariate distributions. | Built into Monolix/Simulx, mrgsolve (R), or custom in Python. |
| Visual Predictive Check (VPC) Tool | To validate that simulations from the final model adequately reproduce the original observed data. | vpc package in R, PsN for NONMEM, built-in in Phoenix/Monolix. |
| Statistical Distribution Library | To model uncertainty in parameters, covariates, and PD targets for probabilistic simulations. | truncnorm (R/Python), mvtnorm for correlated ETAs. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our hollow-fiber infection model (HFIM) for an antibacterial shows rapid drug depletion, leading to inconsistent PK/PD target attainment. How can we troubleshoot this? A1: Rapid depletion often stems from drug adsorption to system components or chemical instability.
- Troubleshooting Steps:
- Pre-conditioning: Flush new fibers with drug-containing media for 24h before initiating the experiment to saturate binding sites.
- Stability Check: Incubate the drug in fresh media within the experiment's reservoir under precise conditions (temperature, pH, light). Sample at 0, 6, 12, and 24h for bioanalysis.
- System Recovery Test: Spiked a known concentration into the central reservoir. Measure concentration in the central reservoir and peripheral cartridges immediately and at 1h. Recovery <85% indicates significant adsorption.
- Protocol - Drug Stability & Adsorption Assessment:
- Prepare triplicate solutions of your drug at the target concentration in the exact media used in HFIM.
- Divide each into two vials: one stored in the reservoir conditions (e.g., 37°C, dark), one frozen immediately (T=0 control).
- Sample from the incubated vials at T=6, 12, 24h, and immediately freeze.
- Analyze all samples via validated LC-MS/MS. Calculate % remaining relative to T=0 control.
Q2: When modeling tumor growth inhibition (TKI) for an oncology candidate, how do we address high inter-animal variability in xenograft studies that obscures PK/PD relationships? A2: High variability can originate from inconsistent tumor inoculation or animal health status.
- Troubleshooting Steps:
- Standardize Inoculation: Use a single cell batch, ensure consistent cell viability (>95%), injection volume, and site. One dedicated, trained technician should perform all inoculations.
- Stratified Randomization: Measure tumor volumes just prior to dosing initiation. Randomize animals into treatment groups based on tumor volume stratification to ensure equal mean and distribution of starting sizes across all groups.
- PK Sampling: Implement sparse serial sampling or a pharmacokinetic satellite group to obtain individual animal PK parameters for correlation with individual PD (tumor volume) response.
- Protocol - Stratified Randomization for Xenograft Studies:
- On Day -1 relative to dosing, measure all tumors using digital calipers.
- Calculate the mean and standard deviation of tumor volume.
- Create bins (e.g., small, medium, large) based on the distribution.
- Assign each animal within a bin randomly to the planned treatment groups using statistical software.
- Verify no significant difference in starting mean tumor volume between groups via one-way ANOVA.
Q3: In a chronic disease model (e.g., hypertension), target engagement biomarkers show high circadian variability. How do we time PK sampling to best inform PK/PD? A3: Circadian rhythm can profoundly affect both PK (e.g., metabolism) and PD biomarkers.
- Troubleshooting Steps:
- Characterize Rhythm: Run a pilot study with untreated or vehicle-treated animals. Collect the target biomarker (e.g., blood pressure, cytokine) every 4-6 hours over a 24-48h period to map the endogenous rhythm.
- Fix Sampling Times: Align all future PK sampling times to consistent, specific timepoints relative to the light/dark cycle and circadian nadir/peak of your biomarker.
- Include Time-Matched Controls: Every experimental run must include concurrent vehicle-dosed controls sampled at the exact same times as treated animals to account for any baseline rhythmic fluctuations.
- Protocol - Circadian Biomarker Profiling:
- House animals under standardized light/dark cycles (e.g., 12h:12h) for at least two weeks.
- Implant telemetry probes or prepare for serial micro-sampling.
- At designated Zeitgeber Times (ZT), collect biomarker measurements (n=6-8 per time point).
- Plot results to visualize the circadian pattern. Use cosine wave analysis to identify acrophase and nadir.
Table 1: Benchmarking Phase Transition Success Rates (2020-2024)
| Therapeutic Area | Phase I → II | Phase II → III | Phase III → Approval | Key PK/PD Challenge Impacting Success |
|---|---|---|---|---|
| Antibacterials | 65% | 45% | 70% | Achieving sufficient time above MIC for resistant pathogens; overcoming efflux pumps. |
| Oncology | 52% | 28% | 55% | Defining optimal biological dose vs. MTD; high inter-patient PK variability. |
| Chronic Therapies (e.g., CV, Metabolic) | 58% | 40% | 65% | Sustaining target coverage over long dosing intervals; managing tolerance development. |
Data synthesized from recent industry reports (e.g., BIO, IQVIA, FDA CDER).
Table 2: Common PK/PD Targets & Attainment Hurdles
| Therapeutic Area | Primary PK/PD Index | Typical Target | Major Attainment Hurdle |
|---|---|---|---|
| Antibacterials | fT>MIC, fAUC/MIC | 40-70% fT>MIC (for β-lactams) | Protein binding shifts, inoculum effect in HFIM. |
| Oncology (Cytotoxic) | AUC, Cmax | Tumor growth inhibition linked to AUC | Preclinical to clinical translatability of TGI models. |
| Oncology (Targeted) | fCmin > IC90 | >90% fCmin > IC90 | Intra-tumoral penetration, on-target/off-tumor toxicity. |
| Chronic Therapies | fCavg, fCmin | >50% receptor occupancy | Adherence simulation in trials, active metabolites. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for PK/PD Target Attainment Studies
| Item | Function in PK/PD Research |
|---|---|
| Hollow Fiber Bioreactor Cartridges | Creates a in vitro two-compartment system to simulate human PK profiles against bacteria. |
| LC-MS/MS Qualified Matrix | Lot-verified, analyte-free biological matrix (plasma, serum) for robust bioanalytical method development. |
| Stable Isotope Labeled Internal Standards | Essential for accurate quantification of drug concentrations in complex biological samples via mass spectrometry. |
| Telemetry Implants (e.g., for BP) | Enables continuous, stress-free monitoring of physiological PD biomarkers in chronic disease models. |
| PD Biomarker ELISA/Kits (Matched Antibody Pairs) | For quantifying target engagement (e.g., phosphorylated proteins, cytokines) in preclinical and clinical samples. |
| Humanized Mouse Models (e.g., CD34+) | Evaluates PK, efficacy, and toxicity of biologics in a system with relevant human drug target expression. |
Experimental Workflow & Pathway Diagrams
Title: PK/PD Target Attainment Optimization Workflow
Title: PK/PD Driver Comparison: Antibacterials vs. Targeted Oncology
Title: Hollow Fiber Infection Model (HFIM) Experimental Protocol
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our Monte Carlo simulation (MCS) results show high target attainment rates (TAR), but the variability (e.g., 95% CI) is wide. How can we improve precision for regulatory review?
A: Wide confidence intervals often stem from insufficient characterization of pharmacokinetic (PK) and pharmacodynamic (PD) variability.
- Solution: Increase the virtual patient population in your MCS. For robust Phase 3 dosing justification, >10,000 subjects is standard. Ensure your PK parameter distributions (e.g., clearance, volume) are derived from a well-powered population PK model that includes key covariate effects (weight, renal function). Narrow, physiological covariate distributions reduce unexplained variability.
- Protocol: To generate a refined MCS:
- Extract the final population PK model parameter estimates (fixed effects) and variance-covariance matrix (random effects, Ω).
- Using software like
RorNONMEM, simulate 10,000 virtual subjects. For each subject, sample individual PK parameters from a multivariate log-normal distribution defined by the model's Ω. - Apply relevant covariate relationships (e.g., CL ~ (WT/70)^0.75 * (CrCL/90)^1.2).
- Simulate concentration-time profiles for the proposed dosing regimen.
- Calculate the PD target (e.g., fT>MIC, AUC/MIC) for each subject against a range of MICs.
- Determine TAR as the percentage of subjects achieving the target at each MIC. Calculate 95% CIs using percentile bootstrap methods.
Q2: The FDA asked for a "bridging study" justification for a new patient population (e.g., pediatrics, critically ill). What PK/PD data is essential?
A: Bridging requires demonstrating similar exposure-response relationships. The core need is population-specific PK data to support MCS.
- Solution: Conduct a dedicated, albeit small, PK study in the new population. Key measurements are drug clearance and protein binding.
- Protocol:
- Study Design: A sparse sampling (population PK) design in 20-30 patients from the new population is often acceptable.
- Assay: Use a validated bioanalytical method. Measure free (unbound) drug concentrations if protein binding is expected to differ.
- Analysis: Develop a population PK model for the new cohort, or preferably, a pooled model integrating original and new data to estimate covariate effects (e.g., maturation function for pediatrics).
- MCS Bridge: Use the new population's parameter distributions to run a target attainment simulation. Compare TAR curves with the original licensed population. Dosing can be justified if TARs are comparable or superior.
Q3: How do we select and defend the primary PD target (e.g., fAUC/MIC vs. fT>MIC) for a novel antibacterial in the EMA submission?
A: Target selection must be based on pre-clinical in vivo infection model data.
- Solution: Conduct a robust dose-ranging, hollow-fiber infection model (HFIM) study to identify the PK/PD index most predictive of efficacy.
- Protocol: HFIM for PK/PD Index Determination
- Bacterial Strain: Use 3-5 clinically relevant isolates with a range of MICs.
- Dosing Regimens: Simulate 6-8 different human PK profiles in the HFIM system that systematically vary the components of AUC, Peak, and Time > threshold.
- Endpoint: Measure bacterial kill and resistance suppression over 7-10 days.
- Analysis: Fit the data using non-linear regression or Emax models to correlate efficacy with three candidate indices: fAUC/MIC, fCmax/MIC, and %fT>MIC. The index with the highest coefficient of determination (R²) is the most predictive.
Q4: Our drug shows high inter-individual variability in PD response biomarkers. How can we strengthen the exposure-response analysis?
A: Move beyond correlation to demonstrate a direct, predictive relationship using modeling.
- Solution: Develop an integrated PK-PD model that links drug exposure to a quantitative biomarker response, then to clinical outcome.
- Protocol: Integrated PK-PD-Clinical Outcome Analysis
- Data: Pool Phase 2b/3 data: rich/sparse PK, longitudinal PD biomarker (e.g., cytokine level, target engagement marker), and clinical endpoint (e.g., symptom score).
- Step 1 (PK-PD): Fit a direct or indirect response model where drug exposure drives biomarker change. Estimate EC50.
- Step 2 (PD-Clinical): Link the predicted biomarker time course to the clinical endpoint using an Emax or logistic model.
- MCS Application: Use the final model to simulate the probability of clinical success across different exposures/doses, creating a target attainment curve for clinical response.
Data Presentation
Table 1: Regulatory Expectations for Key PK/PD Analysis Components
| Component | FDA Draft Guidance (2022) Considerations | EMA Guideline (CPMP/EWP/2655/99) Considerations |
|---|---|---|
| Target Value | Justification from pre-clinical in vivo models and clinical data. Bridge non-clinical targets using PK. | Defined based on pre-clinical data and confirmed in Phase 2. Population variability must be considered. |
| MCS Population | Virtual population should reflect the intended patient population, including extremes of covariates. | At least 5000-10000 subjects recommended to ensure stability of the TAR estimate. |
| Variability Input | Include between-subject, within-subject (if applicable), and between-occasion variability from popPK. | Include all identifiable sources of variability; covariate distributions should be clinically plausible. |
| Acceptable TAR | Typically ≥90% probability of target attainment at the epidemiological cutoff (ECOFF) for antibacterials. | ≥90% TAR is standard for aggressive targets; may accept 80% for less critical targets or based on clinical context. |
Table 2: Example Reagent & Material Toolkit for PK/PD Target Attainment Research
| Item | Function in Experiment | Example Vendor/Type |
|---|---|---|
| Validated Bioanalytical Assay | Quantifies total and free drug concentrations in complex matrices (plasma, tissue). | LC-MS/MS method following FDA/EMA bioanalysis guidance. |
| Hollow-Fiber Infection Model (HFIM) System | Simulates human PK profiles in vitro for PK/PD index identification and resistance studies. | CellPharmac, Inc. or custom-built system. |
| Population PK Modeling Software | Develops mathematical models to describe PK variability and identify covariates. | NONMEM, Monolix, R with nlmixr2. |
| Monte Carlo Simulation Engine | Performs stochastic simulations to predict TAR across a population. | R, Python (with NumPy), SAS, or integrated within PK software (Phoenix, Simcyp). |
| Frozen Bacterial Panel | Provides characterized isolates with known MICs for PK/PD studies. | ATCC, EUCAST/CLSI resistance surveillance panels. |
Visualizations
Diagram 1: PK/PD Target Attainment Analysis Workflow
Diagram 2: Integrated PK-PD-Clinical Outcome Model Structure
Conclusion
Improving PK/PD target attainment rates is not a single-step process but a continuous, integrative framework that spans from early discovery through clinical development. Success hinges on a deep foundational understanding, the adept application of sophisticated modeling tools like population PK/PD and Monte Carlo simulation, proactive troubleshooting of variability sources, and rigorous clinical validation. As drug development embraces more complex modalities and personalized medicine approaches, the strategies outlined here will become increasingly critical. The future lies in leveraging AI/ML for real-time PTA prediction and the development of adaptive, patient-centric dosing algorithms, ultimately ensuring that the right dose reaches the right patient with a higher probability of success, improving outcomes and streamlining the path to regulatory approval.