Accelerating Anti-Infective Drug Development: A Comprehensive Guide to PBPK Modeling for Candidate Selection
This article provides a detailed guide for researchers and drug development professionals on applying Physiologically-Based Pharmacokinetic (PBPK) modeling to optimize anti-infective candidate selection.
Accelerating Anti-Infective Drug Development: A Comprehensive Guide to PBPK Modeling for Candidate Selection
Abstract
This article provides a detailed guide for researchers and drug development professionals on applying Physiologically-Based Pharmacokinetic (PBPK) modeling to optimize anti-infective candidate selection. The content spans foundational principles, methodological workflows, and practical applications, addressing how PBPK can de-risk early development. It explores mechanistic models integrating drug properties with pathogen-specific dynamics (e.g., intracellular concentrations for antivirals, site-specific penetration for antibacterials). The article also covers troubleshooting common pitfalls, validating models against preclinical and clinical data, and performing comparative analyses to prioritize lead candidates. By synthesizing current best practices and recent advancements, this guide aims to demonstrate how PBPK modeling serves as a critical, translational tool for making data-driven decisions, ultimately improving efficiency and success rates in the pipeline for novel anti-infective therapies.
What is PBPK Modeling and Why is it Transformative for Anti-Infective Development?
Physiologically Based Pharmacokinetic (PBPK) modeling is a critical tool in modern anti-infective drug development, a field defined by the urgent need to overcome resistance and optimize dosing regimens. Within the thesis of accelerating candidate selection, PBPK serves as a virtual bio-simulator. It integrates physiological parameters (organ sizes, blood flows), drug-specific properties (lipophilicity, permeability), and system-specific data (enzyme/transporter abundances) to mechanistically predict drug disposition in virtual populations. This predictive power is indispensable for rational candidate prioritization, first-in-human dose prediction, and simulating drug-drug interactions (DDIs) with concomitant antimicrobials or antiretrovirals, thereby de-risking and streamlining the pipeline from preclinical data to clinical trials.
Application Notes
Note 1: Prediction of Human Pharmacokinetics for a Novel Antiviral Candidate A PBPK model was developed for a novel hepatitis C virus (HCV) protease inhibitor, "CandiVir," using preclinical in vitro and in vivo data. The model aimed to predict human PK to support Investigational New Drug (IND) application.
- Objective: To predict human plasma concentration-time profiles following single and multiple oral doses.
- Model Structure: A full-PBPK model with compartments representing major organs (liver, gut, kidneys, etc.) linked by systemic circulation.
- Input Parameters:
- Physiological: Human population (age 20-50) physiology from built-in libraries.
- Drug-Specific: Measured LogP, pKa, blood-to-plasma ratio, intrinsic clearance from human liver microsomes, permeability from Caco-2 assays, and solubility.
- System-Specific: Abundance of CYP3A4 enzyme (primary metabolizing pathway) in liver and gut.
- Outcome: The simulated PK profiles aligned with later observed Phase I data within 2-fold error, successfully predicting C~max~ and AUC. The model highlighted a significant first-pass effect, guiding formulation strategy.
Note 2: Simulation of Drug-Drug Interaction with Rifampin for a TB Drug Candidate A PBPK DDI model was constructed for a new cytochrome P450 3A4 (CYP3A4)-substrate tuberculosis drug, "MycoFix," with the strong CYP3A4 inducer rifampin.
- Objective: To quantify the reduction in MycoFix exposure when co-administered with rifampin and to evaluate a potential dose-adjustment strategy.
- Model Workflow: A PBPK model for rifampin (perpetrator) was verified against literature DDI data. Its established induction parameters (EC~50~, E~max~) on CYP3A4 were then applied to the system parameters within the verified MycoFix (victim) model.
- Key Simulation: Virtual clinical trial (n=100) comparing MycoFix AUC alone vs. with steady-state rifampin.
- Outcome: The model predicted an 85% decrease in MycoFix AUC, confirming high interaction risk. Staggered dosing or a 3-fold dose increase was simulated to restore therapeutic exposure, providing a clear protocol for clinical evaluation.
Table 1: Summary of Key PBPK Simulation Outcomes in Anti-Infective Development
| Application | Drug Class | Key Predictor Variable | Predicted Outcome | Clinical Validation (Fold-Error) |
|---|---|---|---|---|
| First-in-Human PK | HCV Protease Inhibitor | Hepatic CYP3A4 Clearance | Plasma AUC = 12.3 µg·h/mL | 1.5 |
| Enzyme-Mediated DDI | TB Drug (CYP3A4 substrate) | CYP3A4 Induction by Rifampin | 85% reduction in AUC | Confirmed in Phase I |
| Organ Impairment PK | Broad-Spectrum Antifungal | Renal & Hepatic Clearance | 2.1-fold increase in AUC in Hepatic Impairment | 1.8 |
| Tissue Penetration | Lung-Targeted Macrolide | Tissue:Plasma Partition Coefficient (Kp) | Epithelial Lining Fluid AUC/Plasma AUC = 2.5 | 2.0 |
Experimental Protocols
Protocol 1: Generation of In Vitro Input Parameters for PBPK Model Development This protocol details the essential assays to obtain drug-specific parameters for a novel anti-infective compound.
I. Metabolic Stability & Intrinsic Clearance (CL~int~)
- Reagents: Test compound (1 mM stock in DMSO), pooled human liver microsomes (HLM, 0.5 mg/mL), NADPH regeneration system, phosphate buffer (pH 7.4), stop solution (acetonitrile with internal standard).
- Procedure: a. Prepare incubation mixtures containing HLM and test compound (1 µM final) in phosphate buffer. Pre-incubate for 5 min at 37°C. b. Initiate reaction by adding NADPH. Aliquot at times t=0, 5, 15, 30, 45, 60 minutes into stop solution. c. Centrifuge, analyze supernatant via LC-MS/MS to determine parent compound depletion. d. Calculate in vitro half-life and scale to in vivo hepatic CL~int~ using microsomal protein per gram of liver.
II. Apparent Permeability (P~app~) in Caco-2 Cells
- Reagents: Caco-2 cell monolayers (21-day culture on transwell inserts), test compound (10 µM in HBSS), transport buffer (HBSS, pH 7.4), lucifer yellow (integrity marker).
- Procedure: a. Wash monolayers. Add compound to donor compartment (apical for A→B, basolateral for B→A). b. Incubate at 37°C with gentle shaking. Sample from receiver compartment at e.g., 30, 60, 90, 120 min. c. Analyze samples by LC-MS/MS. Calculate P~app~ and efflux ratio (P~app~(B→A)/P~app~(A→B)).
Protocol 2: In Silico PBPK Model Verification and Virtual Population Simulation This protocol outlines steps for verifying a model against observed data and executing virtual trials.
- Software Setup: Launch a validated PBPK platform (e.g., GastroPlus, Simcyp, PK-Sim).
- Model Building: Populate compound file with all parameters from Protocol 1 and literature.
- Verification Simulation: Input the precise dosing regimen and subject demographics (age, weight, gender) from a published clinical study or internal preclinical in vivo study. Execute simulation.
- Goodness-of-Fit Assessment: Compare simulated vs. observed plasma concentration-time profiles. Accept if ≥90% of data points fall within 2-fold error and visual trend is captured.
- Virtual Trial Design: Define the virtual population (e.g., "Sim-North European," n=100, 50% female, age 20-50). Apply the desired clinical dosing regimen.
- Output Analysis: Run simulation. Extract population statistics (mean AUC, C~max~, T~max~) and variability (CV%). Generate prediction intervals for the PK profile.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in PBPK Research |
|---|---|
| Pooled Human Liver Microsomes (HLM) | Source of human metabolic enzymes to measure intrinsic clearance and identify major CYP isoforms involved. |
| Caco-2 Cell Line | Model of human intestinal permeability; provides critical input for predicting oral absorption. |
| Recombinant Human CYP Enzymes | Used in reaction phenotyping to definitively identify which specific enzyme(s) metabolize the drug candidate. |
| Human Plasma for Protein Binding | Used in equilibrium dialysis or ultrafiltration to determine fraction unbound (f~u~), critical for predicting tissue distribution. |
| NADPH Regeneration System | Essential cofactor for maintaining CYP enzyme activity during in vitro metabolic stability assays. |
| Validated PBPK Software | Platform (e.g., Simcyp Simulator, GastroPlus) containing physiological databases and algorithms to build, verify, and simulate models. |
Visualizations
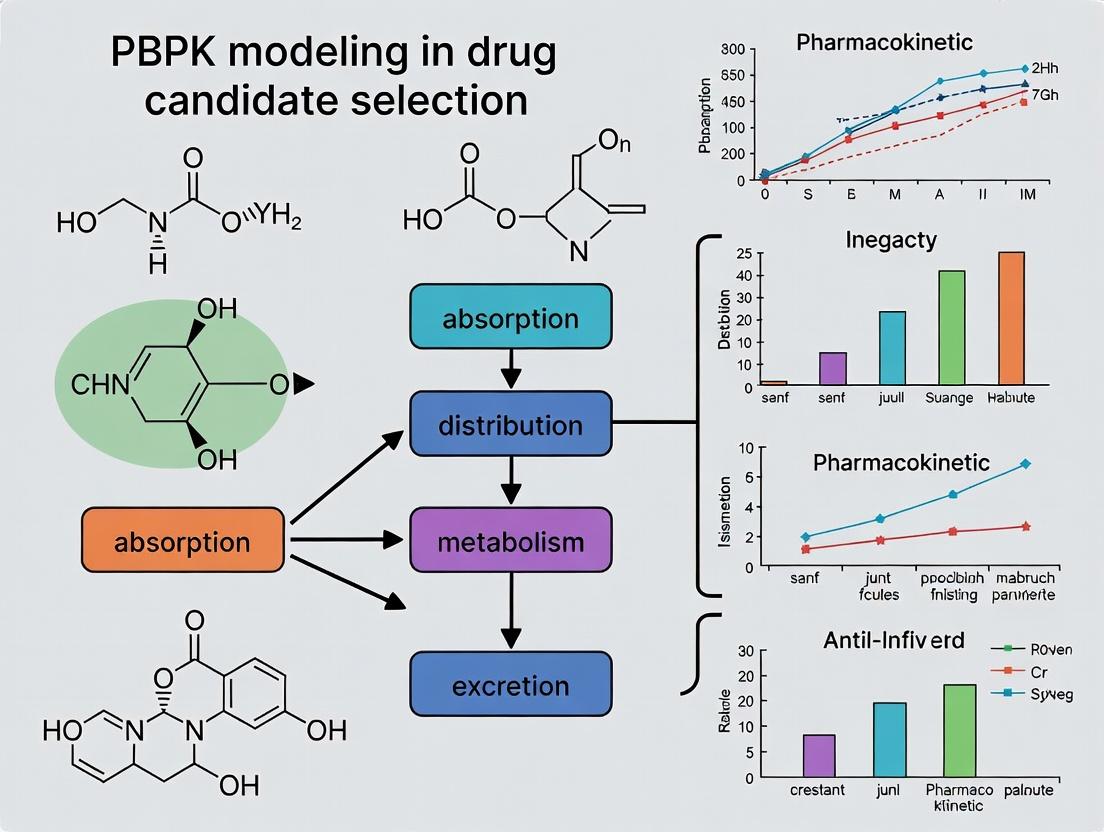
Title: PBPK Modeling Workflow in Drug Development
Title: Oral Drug Disposition Pathway in a PBPK Model
Within the framework of a PBPK modeling thesis for anti-infective candidate selection, understanding three specific pharmacokinetic (PK) challenges is critical. These challenges—tissue penetration, protein binding, and pathogen niche penetration—directly determine a drug's ability to reach and exert effect at the infection site. PBPK models that accurately parameterize these factors are indispensable for predicting human efficacy from preclinical data, de-risking clinical development, and optimizing dosing regimens against resistant or sanctuary-site infections.
Key PK Parameters & Quantitative Data
The following tables summarize critical parameters for PBPK model input and comparison.
Table 1: Tissue-to-Plasma Partition Coefficients (Kp) for Representative Anti-Infectives
| Drug Class | Example Drug | Lung Kp | Brain Kp | Bone Kp | Prostate Kp | Key Determinant |
|---|---|---|---|---|---|---|
| Fluoroquinolones | Levofloxacin | 2.5-4.0 | 0.5-1.2 | 1.5-2.5 | 1.0-1.8 | Lipophilicity, Active Transport |
| Glycopeptides | Vancomycin | 0.3-0.6 | 0.05-0.1 | 0.4-0.7 | 0.2-0.4 | Molecular Size, Capillary Permeability |
| Oxazolidinones | Linezolid | 1.0-1.8 | 0.7-1.0 | 0.8-1.2 | 0.9-1.3 | Passive Diffusion |
| Azoles (Antifungal) | Isavuconazole | 5.0-10 | 0.5-1.5 | 3.0-6.0 | N/A | High Lipophilicity, Tissue Binding |
Table 2: Protein Binding and Impact on PK/PD Indices
| Drug | Human Plasma Protein Binding (%) | Unbound Fraction (fu) | Key Binding Protein | Impact on PK/PD Target (e.g., fAUC/MIC) |
|---|---|---|---|---|
| Ceftriaxone | 85-95 | 0.05-0.15 | Albumin | Critical; only unbound drug is active |
| Dalbavancin | >93 | <0.07 | Albumin | High binding necessitates high total dose |
| Iclaprim | ~30 | ~0.70 | α1-Acid Glycoprotein | Moderate impact on tissue distribution |
| Tedizolid | ~70 | ~0.30 | Albumin | Considered in dose justification |
Table 3: Pathogen-Specific Niche Penetration Challenges
| Pathogen Niche | Example Pathogen | PK Challenge | Experimental Model for Assessment |
|---|---|---|---|
| Intracellular (Macrophage) | Mycobacterium tuberculosis, Legionella | Cellular uptake, lysosomal trapping, intracellular metabolism | THP-1 macrophage infection model, J774 cells |
| Biofilm | Pseudomonas aeruginosa, Staphylococcus epidermidis | Extracellular polymeric substance (EPS) barrier, altered microenvironment | CDC biofilm reactor, Calgary biofilm device |
| Cerebral Spinal Fluid (CSF) | Streptococcus pneumoniae (Meningitis) | Blood-Brain Barrier (BBB) permeability, efflux transport | In vitro BBB co-culture models, in vivo meningitis models |
| Prostate Tissue | Escherichia coli (Prostatitis) | pH gradient, lipid composition | Experimental bacterial prostatitis models |
Application Notes & Experimental Protocols
AN-001: Determining Unbound Drug Concentrations in Tissue Homogenates
Purpose: To measure the unbound fraction (fu,tissue) of an anti-infective drug in a specific tissue for PBPK model parameterization. Principle: Equilibrium dialysis separates unbound drug from protein-bound drug in tissue homogenate.
Protocol:
- Tissue Homogenate Preparation: Harvest target tissue (e.g., lung, liver) from dosed animals or use human tissue. Homogenize in pH 7.4 phosphate buffer (1:4 w/v) using a mechanical homogenizer on ice.
- Equilibrium Dialysis: Load 200 µL of tissue homogenate into one chamber of a 96-well equilibrium dialysis device (e.g., HTD96b). Load 350 µL of blank buffer into the adjacent chamber. Separate chambers with a regenerated cellulose membrane (MWCO 12-14 kDa).
- Incubation: Seal the device and incubate at 37°C with gentle rotation for 6 hours (validate time to equilibrium).
- Sample Analysis: Post-incubation, collect aliquots from both buffer and homogenate chambers. Precipitate proteins in homogenate samples with acetonitrile containing internal standard.
- Bioanalysis: Analyze samples using a validated LC-MS/MS method to determine drug concentrations in buffer (Cbuffer, unbound) and homogenate (Ctotal).
- Calculation: Calculate fu,tissue = Cbuffer / Ctotal. Correct for volume shift if necessary.
AN-002: Assessing Intracellular Accumulation in Phagocytic Cells
Purpose: To determine the intracellular-to-extracellular concentration ratio (CIC/CEX) of a drug candidate. Principle: Differentiated macrophage-like cells are exposed to drug, lysed, and intracellular concentration is quantified.
Protocol:
- Cell Culture & Differentiation: Culture THP-1 monocytes in RPMI-1640 + 10% FBS. Differentiate into adherent macrophages by adding 100 nM PMA for 48 hours. Wash and rest for 24 hours in fresh medium.
- Drug Exposure: Add the anti-infective candidate at a clinically relevant concentration (e.g., 1x-10x MIC) to the cells. Incubate at 37°C, 5% CO2 for a defined period (e.g., 2h, 24h). Include wells with transporter inhibitors (e.g., verapamil for P-gp) if efflux is suspected.
- Wash & Lysis: Terminate exposure by placing plates on ice. Wash cells three times with ice-cold PBS. Lyse cells with 200 µL of 0.1% Triton X-100 in water.
- Sample Analysis: Clarify lysate by centrifugation. Analyze drug concentration in lysate (Clysate) and the initial exposure medium (Cmedium) via LC-MS/MS.
- Calculation: Determine total cellular protein per well using a BCA assay. Express CIC as ng drug/mg protein. Calculate accumulation ratio = CIC (ng/mg) / C_medium (ng/µL), applying unit conversion factor.
AN-003: In Vitro Biofilm Penetration Assay
Purpose: To evaluate the ability of a drug to penetrate and kill bacteria within a mature biofilm. Principle: A static biofilm is grown, exposed to drug, and the reduction in viable cells at different biofilm depths is assessed.
Protocol:
- Biofilm Growth: Inoculate 96-well pegged lids (e.g., Calgary Biofilm Device) with bacterial suspension (~10^6 CFU/mL) in appropriate medium. Submerge pegs and incubate statically at 37°C for 48-72 hours to form mature biofilm.
- Drug Exposure: Transfer the pegged lid to a new 96-well plate containing serial dilutions of the anti-infective in fresh medium. Incubate for 24h.
- Biofilm Processing & Viability Counting:
- Total Viability: Transfer a set of pegs to a recovery plate with 200 µL of neutralizing broth. Sonicate for 5-10 minutes, then vortex vigorously to dislodge and disperse biofilm. Serially dilute and plate for CFU enumeration.
- Spatial Penetration (Optional): Use cryosectioning of biofilm grown on coupons, followed by staining with LIVE/DEAD BacLight and confocal microscopy, or sequential washing steps to remove outer layers before sonication of the inner core.
- Analysis: Determine log10 CFU reduction vs. drug-free control. Plot CFU/peg vs. drug concentration to generate an MBEC (Minimum Biofilm Eradication Concentration).
Diagrams
Title: PBPK Integration of Anti-Infective PK Challenges
Title: Tissue Unbound Fraction Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Example Product/Solution | Function in Context |
|---|---|---|
| In Vitro BBB Model | MilliporeSigma In Vitro Blood-Brain Barrier Kit (Endothelial/ Astrocyte Co-culture) | Models the blood-brain barrier to assess CNS penetration potential for meningitis treatments. |
| Biofilm Reactor | BioSurface Technologies Corp. CDC Biofilm Reactor (Rotary) | Generates reproducible, high-throughput biofilms under shear stress for penetration and efficacy studies. |
| Equilibrium Dialysis Device | HTDialysis HTD96b 96-Well Equilibrium Dialyzer | High-throughput determination of plasma or tissue homogenate protein binding (unbound fraction). |
| Differentiated Macrophage Cells | ATCC THP-1 Cells + PMA (Phorbol Ester) | Consistent model for assessing intracellular accumulation of drugs against pathogens like M. tuberculosis. |
| LC-MS/MS Internal Standard | Cerilliant Stable-Labeled Isotopic Drug Standards (e.g., ^13C-^15N labeled analogs) | Ensures accuracy and precision in quantifying drug concentrations in complex matrices like tissue homogenate. |
| Biofilm Viability Stain | Thermo Fisher Scientific LIVE/DEAD BacLight Bacterial Viability Kit | Fluorescent staining to visualize and quantify live/dead bacteria within a biofilm spatial structure. |
| Tissue Homogenization System | Bertin Instruments Precellys Evolution Homogenizer with Cryolys Cooling | Provides rapid, reproducible, and cooled homogenization of tissues for drug concentration analysis. |
| PBPK Modeling Software | Simulations Plus GastroPlus (ADMET Predictor & PKPlus Modules) | Integrated platform for building, simulating, and optimizing PBPK models incorporating tissue penetration parameters. |
Application Notes: PBPK Modeling for Anti-Infective Development
Physiologically Based Pharmacokinetic (PBPK) modeling integrates compound-specific physicochemical and pharmacokinetic data with system-specific physiological parameters to predict drug disposition. For anti-infectives, this approach is critical to de-risk candidate selection and optimize First-in-Human (FIH) dose predictions by simulating drug exposure at the site of infection (e.g., epithelial lining fluid, intracellular space).
Core Quantitative Parameters for Anti-Infective PBPK
The following table summarizes key quantitative parameters required for building a robust PBPK model for anti-infective small molecules.
Table 1: Essential Input Parameters for Anti-Infective PBPK Model Development
| Parameter Category | Specific Parameters | Typical Experimental Method | Impact on Model Prediction |
|---|---|---|---|
| Compound Physicochemistry | pKa, LogP, Solubility (pH profile), Permeability (Papp) | Shake-flask, Potentiometric titration, Caco-2/PAMPA assay | Dictates ionization, partitioning, and passive diffusion. |
| In Vitro PK | Metabolic Stability (CLint), CYP Inhibition/Induction, Plasma Protein Binding (fu) | Hepatocyte/microsome incubations, Transporter assays (e.g., HEK293), Equilibrium dialysis | Scales to in vivo clearance, predicts DDIs, estimates free drug. |
| Distribution | Tissue-to-Plasma Partition Coefficients (Kp), Specific Tissue Binding | In vivo rat tissue distribution study, in vitro tissue slice binding | Predicts concentration at site of action (e.g., lung, liver). |
| Anti-infective Specific | MIC Distribution for Target Pathogen, Post-Antibiotic Effect | Broth microdilution, time-kill studies | Informs PK/PD target (e.g., fAUC/MIC, %T>MIC) for efficacy. |
| Physiological System | Organ weights/flows, Expression levels of enzymes/transporters, Pathophysiological changes (e.g., infection) | Literature data (e.g., ICRP), Proteomics databases | Provides biological context; critical for special populations. |
Application in Candidate Selection and FIH Dosing
A validated PBPK model enables virtual screening of candidates by simulating human PK and probability of target attainment (PTA). The workflow involves:
- Developing and validating a base model using preclinical in vitro and in vivo data (rat, dog).
- Performing a sensitivity analysis to identify critical parameters driving uncertainty.
- Scaling to human by replacing system parameters with human physiology.
- Conducting clinical trial simulations to predict FIH dose ranges that achieve the desired PK/PD target with high PTA (>90%) and acceptable safety margins (based on preclinical toxicology exposure).
Table 2: Example PBPK-Driven FIH Dose Prediction for a Novel Gram-Negative Agent
| Scenario | Predicted Human PK (Mean) | PK/PD Target (fAUC0-24/MIC) | PTA for MIC = 2 mg/L | Recommended FIH Dose Range | Rationale |
|---|---|---|---|---|---|
| Base Case | CL= 10 L/h, Vss= 50 L | Target = 50 (from preclinical models) | 95% | 500 mg Q12h | High probability of efficacy. |
| Worst-Case (High CL) | CL= 15 L/h, Vss= 40 L | Target = 50 | 70% | 750 mg Q8h | Dose adjustment to maintain PTA. |
| Safety Limit | Cmax at 1000 mg = 35 mg/L | NOAEL Cmax = 50 mg/L (10x safety margin) | - | Max 1000 mg single dose | Respects preclinical safety margin. |
Final Recommendation: Start FIH SAD at 250 mg, escalate to 500 mg and 750 mg. MAD study at 500 mg Q12h.
Detailed Experimental Protocols
Protocol: Determination of Tissue Partition Coefficients (Kp) Using Rat Tissue Homogenate
Objective: To estimate tissue-to-plasma partition coefficients (Kp) for input into PBPK models. Materials: See "Scientist's Toolkit" below. Procedure:
- Tissue Preparation: Sacrifice rat (n=3) and harvest key tissues (lung, liver, kidney, muscle, heart, spleen). Rinse in cold saline, blot dry, and weigh. Homogenize each tissue in pH 7.4 buffer (1:4 w/v) using a Potter-Elvehjem homogenizer on ice.
- Incubation: Spike the test compound into each tissue homogenate and blank plasma to achieve a final concentration of 5 µM. Incubate in a 37°C water bath for 4 hours to reach equilibrium.
- Termination & Analysis: Place samples on ice. Add two volumes of acetonitrile containing internal standard to precipitate proteins. Vortex and centrifuge at 4000g for 15 min.
- Calculation: Analyze supernatant via LC-MS/MS. Calculate Kp using the formula:
K_p = (C_tissue_homogenate / C_plasma) * Dilution Factorwhere the Dilution Factor accounts for the buffer used in homogenization (typically 4 or 5).
Protocol: In Vitro Time-Kill Assay for PK/PD Parameter Elucidation
Objective: To characterize the bactericidal activity and determine PK/PD indices (AUC/MIC, Cmax/MIC, Time > MIC). Materials: Cation-adjusted Mueller Hinton Broth (CAMHB), target bacterial isolate (e.g., Pseudomonas aeruginosa ATCC 27853), compound stock solutions, 96-well deep-well plates. Procedure:
- Inoculum Prep: Grow bacteria to mid-log phase (0.5 McFarland). Dilute in CAMHB to ~5 x 10^5 CFU/mL.
- Compound Addition: In a deep-well plate, prepare serial dilutions of the antibiotic (e.g., 0.25x to 32x MIC) in CAMHB. Add equal volume of bacterial inoculum. Final volume: 1 mL. Include growth and sterility controls.
- Sampling: Incubate at 35°C. At time points 0, 2, 4, 8, and 24h, remove 100 µL samples from selected wells. Perform serial 10-fold dilutions in saline and spot-plate 10 µL onto Mueller-Hinton Agar plates for CFU enumeration.
- Data Analysis: Plot Log10 CFU/mL vs. Time for each concentration. Fit data using a sigmoidal Emax model in software like Phoenix WinNonlin to determine the PK/PD index (e.g., fAUC/MIC) best correlating with a 1-log10 kill endpoint.
Visualizations
Title: PBPK Modeling Workflow for Anti-Infectives
Title: PK/PD Target Attainment Feedback Loop
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for PBPK-Related Experiments
| Item | Function in Context | Example Supplier/Catalog |
|---|---|---|
| Pooled Human Liver Microsomes (HLM) | Contains major CYP enzymes for measuring intrinsic metabolic clearance (CLint) and conducting reaction phenotyping. | Corning, Xenotech |
| Cryopreserved Human Hepatocytes | Provides a more complete metabolic system (Phase I & II enzymes, transporters) for advanced clearance and DDI studies. | BioIVT, Lonza |
| Caco-2 Cell Line | Model of human intestinal permeability; used to determine apparent permeability (Papp) and assess efflux transporter effects. | ATCC (HTB-37) |
| Rapid Equilibrium Dialysis (RED) Device | High-throughput method for determining unbound fraction of drug in plasma (fu) or tissue homogenate. | Thermo Fisher Scientific |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing (MIC) and time-kill assays, ensuring consistent ion concentrations. | Becton Dickinson |
| PBPK Modeling Software | Platform for building, simulating, and validating PBPK models (e.g., Simcyp Simulator, GastroPlus, PK-Sim). | Certara, Simulations Plus |
| LC-MS/MS System | Essential for quantifying drug concentrations in complex biological matrices (plasma, tissue homogenate) with high sensitivity and specificity. | Sciex, Waters, Agilent |
Within the context of physiologically based pharmacokinetic (PBPK) modeling for anti-infective candidate selection, the rigorous differentiation and accurate parameterization of drug-specific and physiological system components is paramount. This delineation directly impacts the predictive accuracy of models for scaling from preclinical species to humans, optimizing dosing regimens, and predicting drug-drug interactions. These models integrate compound-specific physicochemical and biochemical properties with system-specific anatomical, physiological, and genetic data to simulate drug concentration-time profiles in plasma and target tissues, such as sites of infection.
Table 1: Core Drug-Specific Parameters for Anti-Infectives
| Parameter Category | Specific Parameters | Typical Values/Examples (Anti-Infectives) | Primary Experimental Method |
|---|---|---|---|
| Physicochemical | Molecular Weight, pKa, Log P, Solubility, Permeability | MW: 300-800 Da; Log P: -0.4 (Ciprofloxacin) to 5.0 (Itraconazole) | Potentiometric titration, HPLC, PAMPA, Caco-2 assay |
| Binding & Partitioning | Plasma Protein Binding (fu), Blood-to-Plasma Ratio, Tissue-to-Plasma Partition Coefficients (Kp) | fu: 2% (Dalbavancin) to 70% (Fluconazole) | Equilibrium dialysis, in vivo tissue distribution studies |
| Metabolism | Enzyme Kinetic Constants (Km, Vmax), CLint for specific CYPs/UGTs | Vmax: pmol/min/pmol enzyme; Km: µM range | Human liver microsomes/ hepatocytes, recombinant enzymes |
| Transport | Transporter Affinity (Km), Capacity (Jmax), Directionality (Uptake/Efflux) | For OATs, OCTs, P-gp, BCRP | Transfected cell systems (e.g., MDCK, HEK293) |
| Excretion | Fraction excreted unchanged in urine (fe), Biliary clearance | fe: 80% (Levofloxacin) to <5% (Voriconazole) | Mass balance studies (radiolabeled) |
Table 2: Key Physiological System Parameters in PBPK
| System Compartment | Physiological Parameters | Typical Adult Human Values | Source of Interindividual Variability |
|---|---|---|---|
| Anatomical | Organ volumes (L), Blood flow rates (L/h) | Liver: 1.5 L; Hepatic blood flow: 90 L/h | Age, body weight, BMI, ethnicity |
| Biochemical | Enzyme abundances (pmol/mg protein), Transporter expression levels | CYP3A4: 80-150 pmol/mg microsomal protein | Genetics (polymorphisms), disease, drug induction/inhibition |
| Physiological | Gastric emptying time, Intestinal pH, Glomerular Filtration Rate (GFR) | GFR: ~120 mL/min | Age, renal function, disease states (e.g., CKD) |
| Demographic | Population distributions for age, weight, height, genetic polymorphisms | - | Population databases (NHANES) |
| Pathophysiological | Infection site characteristics (e.g., abscess pH, perfusion) | e.g., Epithelial lining fluid volume in pneumonia | Specific disease (e.g., cystic fibrosis, meningitis) |
Experimental Protocols for Parameter Generation
Protocol 1: Determination of Intrinsic Clearance (CLint) Using Human Liver Microsomes
Purpose: To quantify the metabolic stability and obtain enzyme kinetic parameters (Km, Vmax) for a new anti-infective candidate. Materials: Test compound, human liver microsomes (HLM, pooled or individual), NADPH regenerating system, phosphate buffer (pH 7.4), analytical instrument (LC-MS/MS). Procedure:
- Prepare incubation mixtures containing HLM (0.1-1 mg protein/mL), test compound (at least 8 concentrations spanning expected Km), and buffer.
- Pre-incubate at 37°C for 5 min. Initiate reaction by adding NADPH regenerating system.
- At predetermined time points (e.g., 0, 5, 15, 30, 45, 60 min), withdraw aliquots and quench with acetonitrile containing internal standard.
- Centrifuge, analyze supernatant via LC-MS/MS to determine parent compound depletion.
- Fit depletion data to calculate in vitro half-life and intrinsic clearance (CLint = (0.693 / t1/2) * (incubation volume / microsomal protein)).
- For kinetics, plot reaction velocity vs. substrate concentration and fit to Michaelis-Menten model to derive Km and Vmax.
Protocol 2: Determination of Fraction Unbound (fu) in Plasma via Rapid Equilibrium Dialysis (RED)
Purpose: To measure the free fraction of drug available for pharmacological activity or metabolism. Materials: RED device, test compound, human plasma, dialysis buffer (PBS, pH 7.4), LC-MS/MS. Procedure:
- Spike the test compound into plasma to a relevant therapeutic concentration.
- Load plasma sample (~150 µL) into the sample chamber and buffer into the adjacent buffer chamber.
- Assemble the RED plate and incubate at 37°C with gentle agitation for 4-8 hours (validate time to equilibrium).
- Post-incubation, aliquot equal volumes from both plasma and buffer chambers.
- Process samples (matrix matching is critical: add blank buffer to plasma aliquots and blank plasma to buffer aliquots before protein precipitation).
- Analyze using LC-MS/MS. Calculate fu = (concentration in buffer chamber) / (concentration in plasma chamber).
Protocol 3: In Vitro Transporter Studies Using MDCKII Monolayers
Purpose: To assess if a drug is a substrate for key efflux transporters (e.g., P-gp). Materials: MDCKII cells, MDCKII cells overexpressing human MDR1, Transwell plates, HBSS transport buffer, test compound, selective inhibitor (e.g., Elacridar for P-gp). Procedure:
- Seed cells on permeable Transwell filters and culture until confluent monolayers with tight junctions form (~3-5 days). Monitor Transepithelial Electrical Resistance (TEER).
- Pre-incubate both apical (A) and basolateral (B) sides with buffer ± inhibitor for 30 min.
- For A-to-B transport: add compound to A compartment, sample from B compartment over time. For B-to-A transport: add compound to B compartment, sample from A compartment over time.
- Maintain sink conditions. Analyze samples by LC-MS/MS.
- Calculate apparent permeability (Papp) and efflux ratio (ER = Papp(B-to-A)/Papp(A-to-B)). An ER > 2 that is diminished by inhibitor suggests active efflux.
Visualization of Relationships and Workflows
Diagram 1: PBPK Model Parameter Integration Flow
Diagram 2: From Compound to Model-Ready Parameters
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PBPK Parameterization
| Item/Category | Example Product/Source | Function in Parameterization |
|---|---|---|
| In Vitro Metabolism Systems | Pooled Human Liver Microsomes (HLM); Cryopreserved Human Hepatocytes (CHH) | Provide the enzymatic machinery to measure intrinsic metabolic clearance and identify involved enzymes. |
| Transporter Assay Systems | MDCKII, HEK293, or CHO cells overexpressing human transporters (e.g., MDR1, BCRP, OATP1B1) | Determine substrate affinity for uptake/efflux transporters impacting distribution and clearance. |
| Protein Binding Assay Kits | Rapid Equilibrium Dialysis (RED) devices; Ultracentrifugation supplies | Measure fraction unbound in plasma (fu) and tissue homogenates for accurate free concentration estimation. |
| Biomatrices for Calibration | Charcoal-stripped human plasma; Human tissue homogenates (liver, kidney, lung) | Provide analyte-free matrices for creating standard curves in binding/partitioning studies. |
| CYP Reaction Phenotyping Kits | Recombinant CYP isoforms; CYP-selective chemical inhibitors | Identify specific cytochrome P450 enzymes responsible for metabolism to anticipate genetic variability and DDIs. |
| LC-MS/MS Instrumentation & Columns | UHPLC systems coupled to triple quadrupole MS; C18 and HILIC columns | Essential for sensitive and specific quantification of drugs and metabolites in complex biological matrices. |
| PBPK Software Platforms | GastroPlus, Simcyp Simulator, PK-Sim | Commercial platforms containing built-in physiological databases for integrating drug and system parameters. |
Physiologically-Based Pharmacokinetic (PBPK) modeling has become an integral tool in the development of anti-infective drugs, offering a mechanistic framework to predict drug disposition in specific populations and under various clinical scenarios. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have issued specific guidance documents outlining the contexts in which PBPK analyses are encouraged and the standards for model submission and validation. Within the broader thesis on using PBPK for anti-infective candidate selection, understanding these regulatory perspectives is crucial for designing predictive, clinically relevant models that can streamline development and support key regulatory decisions.
Comparative Analysis of FDA and EMA Guidance on PBPK for Anti-Infectives
The following table summarizes key aspects of regulatory guidance from the FDA and EMA relevant to PBPK modeling for anti-infectives.
Table 1: Comparison of FDA and EMA Perspectives on PBPK for Anti-Infectives
| Aspect | FDA Perspective (Guidance/Specific Reviews) | EMA Perspective (Guideline/Specific Reviews) |
|---|---|---|
| Primary Guidance | "Physiologically Based Pharmacokinetic Analyses — Format and Content" (2024 draft), "General Clinical Pharmacology Considerations for Antibacterial Drug Development" (2024) | "Guideline on the qualification and reporting of physiologically based pharmacokinetic (PBPK) modelling and simulation" (2021), "Guideline on the use of pharmacokinetics and pharmacodynamics in the development of antibacterial medicinal products" (2016) |
| Encouraged Applications | Drug-drug interaction (DDI) risk assessment, dose selection for special populations (e.g., pediatrics, organ impairment), bridging from adults to pediatrics, informing clinical trial design. | Similar to FDA, with strong emphasis on pediatrics, organ impairment, and DDI assessment. Support for justifying alternative dosing regimens. |
| Model Qualification Expectations | Prior qualification is not mandatory but recommended. Submission package must include: Input Parameters (system, drug, trial), Model Verification (against observed data), Model Validation (predictive performance), and Sensitivity Analysis. | A "qualified" PBPK platform/model is expected for regulatory submissions. The qualification package should demonstrate the model's predictive capability within a defined "scope of application." |
| Key Model Components | Well-characterized system parameters (e.g., from published databases), reliable in vitro drug parameters (solubility, permeability, metabolic stability), and robust clinical verification data. | Emphasis on transparency and scientific rationale for all system- and drug-related input parameters. Justification for any model simplification is required. |
| Specific Anti-Infective Context | Recognizes utility in optimizing dosing for resistant infections, simulating epithelial lining fluid (ELF) penetration for pulmonary infections, and supporting breakpoint assessments. | Acknowledges role in dose optimization for prevention of resistance, and in understanding pharmacokinetics at the site of infection (e.g., bone, CSF). |
| Submission Format | Structured data following the Pharmacometrics Data Standards. Recommends use of standardized model file formats (e.g., PK-Sim, Simcyp). | Detailed Scientific Report within the CTD (Module 2.7.1). Model files (executable and code) must be submitted upon request. |
Detailed Application Notes
Application Note 1: PBPK to Support Pediatric Dose Selection for a Novel Beta-Lactam
Objective: To extrapolate adult pharmacokinetics (PK) to pediatric populations (ages 2 to 18) for a new intravenous beta-lactam antibiotic using a verified PBPK model, supporting Pediatric Investigational Plan (PIP) and dose justification.
Protocol:
- Model Development (Adult):
- System Parameters: Utilize an age-dependent PBPK platform (e.g., Simcyp Pediatric, PK-Sim Ontogeny). Select a healthy volunteer population.
- Drug Parameters: Incorporate in vitro data: plasma protein binding (fu), blood-to-plasma ratio (B/P), renal clearance (CLrenal) from human kidney models, and non-renal clearance (e.g., from hepatocyte stability assays).
- Model Verification: Simulate Phase I single- and multiple-dose IV infusion trials in virtual adult populations (n=100). Optimize system parameters (e.g., GFR scaling) only if needed to match observed plasma concentration-time profiles. Accept if >90% of observed data falls within the 5th-95th percentile of the simulated population prediction.
Pediatric Extrapolation:
- Scale System Parameters: Apply established ontogeny functions for organ sizes, blood flows, glomerular filtration rate (GFR), and protein levels relevant to the drug's clearance pathways.
- Simulation Scenarios: Simulate the proposed pediatric dosing regimen (e.g., mg/kg q8h) across virtual pediatric cohorts stratified by age (e.g., 2-<6, 6-<12, 12-18 years, n≥50 per cohort).
- Target Exposure Analysis: Calculate key PK metrics (AUC0-24, Cmax, %fT>MIC) for each virtual subject. Compare the simulated median pediatric exposure to the target exposure established as efficacious in adults (e.g., %fT>MIC of 60% for beta-lactams).
Output and Justification: Generate a summary table comparing simulated pediatric PK parameters to the adult target. Provide visual predictive checks (VPCs) for the adult model and simulated pediatric concentration-time curves.
Application Note 2: DDI Risk Assessment for a Novel Azole Antifungal with CYP3A4 Substrates
Objective: To predict the magnitude of drug-drug interactions (DDIs) when a new strong CYP3A4 inhibitor (azole antifungal, Drug I) is co-administered with sensitive CYP3A4 substrates (e.g., midazolam, Drug V), as required for labeling.
Protocol:
- Model Development (Perpetrator - Drug I):
- Develop and verify a PBPK model for the azole antifungal using clinical PK data from single and multiple doses.
- Key parameters:
Ki(inhibition constant) for CYP3A4 from human liver microsomes, fraction metabolized by CYP3A4 (fmCYP3A4), and mechanism (time-dependent inhibition if applicable).
- Model Development (Victim - Drug V):
- Utilize or develop a verified substrate model (e.g., the Simcyp or FDA midazolam model).
- Ensure model accurately captures clearance via CYP3A4 (
fmCYP3A4 > 0.9).
- DDI Simulation:
- Design virtual trial: 100 healthy subjects receive Drug V alone (reference) and then co-administered with Drug I at steady-state.
- Simulate the worst-case clinical scenario (e.g., highest recommended dose of Drug I).
- Analysis and Classification:
- Calculate the geometric mean ratio (GMR) of AUC and Cmax for Drug V (with inhibitor / alone).
- Classify interaction strength based on FDA/EMA criteria (e.g., AUC increase ≥5-fold = strong inhibitor). Compare predictions against any available clinical DDI study data.
Table 2: Example DDI Risk Assessment Output Table (Simulated)
| Victim Drug (CYP3A4 Substrate) | Predicted AUC Ratio (GMR) [90% CI] | Predicted Cmax Ratio (GMR) [90% CI] | Recommended Labeling Statement (Based on Simulation) |
|---|---|---|---|
| Midazolam (sensitive probe) | 8.5 [6.9, 10.4] | 3.2 [2.7, 3.8] | Contraindicated or significant dose reduction required. |
A Substrate X (fmCYP3A4=0.6) |
4.1 [3.3, 5.0] | 2.1 [1.8, 2.5] | Avoid concomitant use; if necessary, monitor for adverse reactions and consider dose reduction. |
Experimental Protocols for KeyIn VitroAssays
Protocol: Determination of Fraction Unbound (fu) in Plasma and Target Tissue Homogenate
Objective: To measure the unbound fraction of an anti-infective drug in human plasma and homogenate from a target tissue (e.g., lung, bone) for accurate PBPK model parameterization of tissue distribution.
Materials:
- Test compound (stable isotope-labeled preferred for LC-MS/MS)
- Pooled human plasma
- Human target tissue (e.g., obtained from biorepository)
- Phosphate-buffered saline (PBS), pH 7.4
- 96-well equilibrium dialysis device (e.g., HTD96b) with semi-permeable membranes (MWCO 12-14 kDa)
- Orbital shaker in a 37°C incubator
- LC-MS/MS system
Procedure:
- Tissue Homogenate Preparation: Homogenize tissue in PBS (e.g., 1:4 w/v) using a mechanical homogenizer. Centrifuge at 10,000 g for 10 min at 4°C. Use supernatant.
- Sample Spiking: Spike the test compound into plasma and tissue homogenate to a physiologically relevant concentration (e.g., 1-10 µM). Prepare in triplicate.
- Equilibrium Dialysis: Load donor chamber (200 µL) with spiked plasma/homogenate. Load receiver chamber (350 µL) with PBS. Assemble plate and seal.
- Incubation: Shake plate at 150 rpm for 6 hours at 37°C to reach equilibrium.
- Sample Collection: Post-incubation, collect 50 µL from both donor and receiver chambers. For donor samples, collect matching "buffer" samples from receiver side. For receiver samples, collect matching "matrix" samples from donor side.
- Matrix Matching: Mix donor samples with blank PBS. Mix receiver samples with blank plasma/homogenate to equalize matrix effects for analysis.
- Quantification: Analyze samples using a validated LC-MS/MS method.
- Calculation: Calculate
fu = (Conc_receiver / Conc_donor)after correcting for any volume shift. Report mean ± SD of triplicates.
Protocol:In VitroHepatocyte Assay for Metabolism and CYP Reaction Phenotyping
Objective: To estimate hepatic metabolic clearance and identify major cytochrome P450 (CYP) enzymes involved in the metabolism of a new anti-infective.
Materials:
- Cryopreserved human hepatocytes (pooled, 3+ donors)
- Williams' E medium with incubation supplements
- Test compound
- Selective chemical inhibitors for major CYP isoforms (e.g., α-Naphthoflavone for CYP1A2, Quinidine for CYP2D6, Ketoconazole for CYP3A4)
- Stable isotope-labeled internal standards
- UPLC-MS/MS system
Procedure:
- Hepatocyte Incubation for Intrinsic Clearance (CLint):
- Thaw and viability-check hepatocytes. Incubate at 0.5 million cells/mL with test compound (1 µM) in a 96-well plate.
- Take time-point aliquots (e.g., 0, 15, 30, 60, 90 min). Stop reaction with cold acetonitrile containing internal standard.
- Centrifuge and analyze supernatant by LC-MS/MS.
- Calculate in vitro
CLintfrom the disappearance half-life of the parent drug.
- Reaction Phenotyping with Chemical Inhibitors:
- Pre-incubate hepatocytes with a selective CYP inhibitor or vehicle control (DMSO) for 15 min.
- Add test compound and incubate for a single, linear time-point (e.g., 30 min).
- Process and analyze samples as above.
- Calculate the percentage inhibition of metabolite formation or parent loss for each inhibitor compared to control. Contribution of a specific CYP =
(1 - AUCinhibitor/AUCcontrol) * 100%.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PBPK-Oriented Anti-Infective Research
| Item | Function in PBPK Context |
|---|---|
| Pooled Human Liver Microsomes (pHLM) | To determine kinetic parameters (Km, Vmax) for phase I oxidative metabolism and obtain inhibition constants (Ki) for DDI assessment. |
| Cryopreserved Human Hepatocytes (Pooled) | Gold standard for estimating intrinsic metabolic clearance (CLint) and identifying metabolic pathways in a physiologically relevant cellular system. |
| Recombinant Human CYP Isozymes | For definitive reaction phenotyping to attribute metabolism to specific CYP enzymes (e.g., CYP3A4, 2C9). |
| Caco-2 or MDCK-MDR1 Cell Lines | To measure apparent permeability (Papp) and assess the role of efflux transporters (e.g., P-gp) in intestinal absorption and tissue distribution. |
| Equilibrium Dialysis Devices | To measure the critical parameter of fraction unbound (fu) in plasma and tissue homogenates, governing drug distribution. |
| PBPK Software Platform (e.g., Simcyp, GastroPlus, PK-Sim) | Integrated simulation environment containing system parameters, algorithms for scaling, and tools for population variability and trial simulation. |
| Validated Probe Substrates & Inhibitors | Essential for in vitro assay validation and calibrating system parameters within PBPK platforms (e.g., midazolam for CYP3A4 activity). |
Visualizations
PBPK Model Development and Extrapolation Workflow
Key Components of a PBPK Regulatory Submission
Building and Applying a PBPK Model: A Step-by-Step Workflow for Anti-Infectives
This application note details the critical first step in a Physiologically-Based Pharmacokinetic (PBPK) modeling workflow for anti-infective drug candidate selection. The reliable prediction of human pharmacokinetics and tissue penetration to infection sites hinges on the systematic collation and integration of high-quality in vitro data. This protocol establishes a standardized framework for gathering, curating, and organizing three foundational data classes: ADME (Absorption, Distribution, Metabolism, Excretion), physicochemical properties, and target binding parameters.
Key Data Tables for Candidate Comparison
Table 1: Core Physicochemical & In Vitro ADME Data
Data required for initial PBPK model parameterization and ranking of anti-infective candidates.
| Parameter | Assay Description | Units | Typical Range (Anti-Infectives) | Relevance to PBPK |
|---|---|---|---|---|
| logP/logD7.4 | Octanol-water partition/distribution coefficient at pH 7.4 | Unitless | -2 to 6 | Predicts passive membrane permeability, tissue partitioning. |
| Solubility (Thermodynamic) | Equilibrium solubility in biorelevant media (e.g., FaSSIF/FeSSIF) | µg/mL | Wide range; >10 µg/mL often desirable | Informs absorption limitation risk and formulation needs. |
| pKa | Acid dissociation constant(s) | Unitless | Multiple possible | Governs pH-dependent solubility, permeability, and distribution. |
| Permeability (Papp) | Caco-2 or MDCK cell monolayer | 10-6 cm/s | Low: <1, Med: 1-10, High: >10 | Predicts intestinal absorption and passive cellular uptake. |
| Microsomal/ Hepatocyte CLint | Intrinsic clearance in human liver microsomes/cryopreserved hepatocytes | µL/min/mg protein or mL/min/10^6 cells | Low: <10, Med: 10-50, High: >50 | Primary input for predicting hepatic metabolic clearance. |
| Plasma Protein Binding (fu) | Equilibrium dialysis or ultrafiltration | % Unbound (fu) | Often <30% for anti-infectives | Impacts free drug concentration, efficacy, and clearance. |
| Transporter Kinetics (Km, Vmax) | Uptake/efflux in overexpressed cell lines (e.g., HEK293, CHO) | Km (µM), Vmax (pmol/min/mg) | Compound-specific | Critical for modeling organ-specific disposition (e.g., liver, kidney, BBB). |
Table 2: Target Binding & In Vitro Potency Data
Essential for linking PK to Pharmacodynamics (PD) in PBPK-PD models for anti-infectives.
| Parameter | Assay Description | Units | Relevance to PBPK-PD |
|---|---|---|---|
| Binding Affinity (Kd, Ki) | Isothermal titration calorimetry (ITC), surface plasmon resonance (SPR) | nM or µM | Defines target engagement constant for effect site modeling. |
| Enzymatic Inhibition (IC50) | Target enzyme inhibition assay (e.g., bacterial polymerase, viral protease) | nM or µM | Informs potency for pharmacodynamic driver selection. |
| Cellular Potency (MIC, EC50) | Minimum inhibitory concentration (bacteria), or half-maximal effective concentration (virus) | µg/mL or µM | Primary in vitro efficacy metric for PK-PD index (e.g., AUC/MIC) calculation. |
| Time-Kill Kinetics | Bacterial kill over time at multiples of MIC | Log10 CFU/mL vs. Time | Informs mechanism (bactericidal/static) and dynamic PD model structure. |
Detailed Experimental Protocols
Protocol 3.1: Determination of Metabolic Stability in Human Liver Microsomes (HLM)
Purpose: To quantify the intrinsic metabolic clearance (CLint) for hepatic clearance prediction. Reagents: Test compound (10 mM stock in DMSO), Human Liver Microsomes (0.5 mg/mL final), NADPH Regenerating System (Solution A: NADP+, Glucose-6-phosphate; Solution B: Glucose-6-phosphate dehydrogenase in MgCl2), Potassium Phosphate Buffer (0.1 M, pH 7.4), Control Compound (e.g., Verapamil for High CL, Warfarin for Low CL). Procedure:
- Prepare incubation mix: 395 µL of pre-warmed (37°C) buffer containing HLM.
- Add 5 µL of test compound (final concentration 1-5 µM, DMSO ≤0.5%).
- Pre-incubate for 5 min at 37°C in a shaking water bath.
- Initiate reaction by adding 100 µL of pre-warmed NADPH Regenerating System (final vol. 500 µL).
- At predetermined time points (0, 5, 10, 20, 30 min), withdraw 50 µL aliquots and quench in 100 µL of ice-cold acetonitrile containing internal standard.
- Centrifuge at 4000xg for 15 min (4°C) to precipitate proteins.
- Analyze supernatant using LC-MS/MS to determine parent compound remaining.
- Calculate in vitro half-life and CLint, in vitro using: t1/2 = 0.693 / k, where k is the elimination rate constant; CLint, in vitro = (0.693 / t1/2>) * (Incubation Volume / Microsomal Protein Amount).
Protocol 3.2: Measurement of Plasma Protein Binding via Equilibrium Dialysis
Purpose: To determine the fraction unbound (fu) in plasma, a critical parameter for free drug concentration. Reagents: Test compound, Human Plasma (fresh or frozen), Dialysis Buffer (0.1 M phosphate buffer, pH 7.4), Equilibrium Dialysis Device (e.g., 96-well format, 8-10 kDa MWCO membranes), Internal Standard Solution. Procedure:
- Spike test compound into plasma to a pharmacologically relevant concentration (e.g., 1-10 µM).
- Load 150 µL of spiked plasma into the donor chamber (plasma side).
- Load 150 µL of dialysis buffer into the receiver chamber (buffer side).
- Seal plate and incubate at 37°C with gentle agitation for 4-6 hours (ensure equilibrium is reached).
- Post-incubation, aliquot equal volumes from both donor (plasma) and receiver (buffer) chambers.
- Prepare matrix-matched samples: Quench buffer-side aliquots with blank plasma, and plasma-side aliquots with blank buffer, to equalize matrix effects for LC-MS/MS analysis.
- Quantify compound concentration in both sides. Calculate fu: fu (%) = [Cbuffer / Cplasma] * 100, where C is the concentration post-dialysis.
Protocol 3.3: Determination of Cellular Permeability (Caco-2)
Purpose: To assess intestinal absorption potential and transporter involvement. Reagents: Caco-2 cells (passage 40-60, grown on 12-well Transwell inserts for 21-25 days), Hanks' Balanced Salt Solution (HBSS, pH 7.4), Test Compound, Lucifer Yellow (paracellular marker), Propranolol (high permeability control), Atenolol (low permeability control), Buffer with/without inhibitors (e.g., for P-gp). Procedure:
- Wash cell monolayers twice with pre-warmed HBSS.
- Add test compound (typically 5-10 µM) to the donor compartment (apical for A→B, basolateral for B→A). Receiver compartment contains blank HBSS.
- Incubate at 37°C on an orbital shaker. Sample from receiver at e.g., 30, 60, 90, 120 min, replenishing with fresh buffer.
- At end, sample donor for mass balance. Analyze all samples by LC-MS/MS.
- Calculate Apparent Permeability: Papp = (dQ/dt) / (A * C0), where dQ/dt is the flux rate, A is the insert membrane area, and C0 is the initial donor concentration.
- Assess efflux ratio: ER = Papp (B→A) / Papp (A→B). ER > 2 suggests active efflux.
Visualization of Workflow and Relationships
Diagram 1: Integrated Data Collation Workflow for PBPK
Diagram 2: PBPK-PD Integration Logic for Anti-Infectives
The Scientist's Toolkit: Research Reagent Solutions
| Item/Vendor | Function/Application in Data Collation |
|---|---|
| Cryopreserved Human Hepatocytes (e.g., Thermo Fisher, BioIVT) | Gold-standard cell system for predicting intrinsic metabolic clearance and metabolite identification. |
| Human Liver Microsomes & S9 Fractions (e.g., Corning, XenoTech) | Subcellular fractions for high-throughput metabolic stability and reaction phenotyping assays. |
| Transporter-Overexpressing Cell Lines (e.g., Solvo Biotechnology, GenoMembrane) | Essential for characterizing substrate affinity (Km, Vmax) for key uptake/efflux transporters (P-gp, BCRP, OATPs). |
| Biorelevant Dissolution Media (FaSSIF/FeSSIF, Biorelevant.com) | Simulates fasted/fed state intestinal fluids for accurate solubility and dissolution measurements. |
| Equilibrium Dialysis Plates (HTD 96b, RED Plate) | Standardized, high-throughput format for reliable plasma protein binding determination. |
| Caco-2/TC7 Cell Line (ECACC, ATCC) | Well-characterized intestinal epithelial cell model for predicting passive/active permeability. |
| SPR/Biacore Systems (Cytiva) | Label-free technology for measuring precise binding kinetics (Ka, Kd) to therapeutic targets. |
| LC-MS/MS System with Acquity/HPLC (Waters, Agilent, Sciex) | Core analytical platform for quantifying drugs and metabolites in complex in vitro matrices. |
| Automated Liquid Handlers (Tecan, Hamilton) | Enables robust, high-throughput, and reproducible sample preparation for ADME assays. |
| PBPK Modeling Software (GastroPlus, Simcyp, PK-Sim) | Platforms that ingest collated in vitro data to build, simulate, and refine mechanistic models. |
Within the broader thesis on PBPK modeling for anti-infective drug candidate selection, the strategic choice of model structure is a critical determinant of success. This decision balances the need for predictive, mechanistic insight against the constraints of early-stage data availability and computational efficiency. For anti-infectives, where targeting specific infection sites (e.g., lung epithelial lining fluid for pneumonia, brain tissue for meningitis) is paramount, the model must adequately capture the relevant physiology without becoming intractable. This application note provides a framework for selecting between Whole-Body (WB) and Minimal (or Reduced) PBPK models, supported by current data, protocols, and tools.
Comparative Analysis: Whole-Body vs. Minimal PBPK Models
Table 1: Core Characteristics and Applications of PBPK Model Types
| Feature | Whole-Body PBPK Model | Minimal PBPK Model |
|---|---|---|
| Structural Resolution | High. Represents all major organs as discrete, perfusion-limited compartments (e.g., lung, liver, muscle, skin, gut, kidney, brain, heart). | Low. Aggregates richly perfused and poorly perfused tissue groups; often uses a central "plasma" compartment linked to 1-3 tissue compartments. |
| Number of Compartments | Typically 12-18+ physiological compartments. | Typically 2-5 lumped compartments. |
| Parameter Requirements | High. Requires extensive physiological (tissue volumes, blood flows), drug-specific (tissue-to-plasma partition coefficients - Kp), and system data. | Low. Requires fewer parameters; often estimates distribution using a limited number of fitted parameters. |
| Predictive Capability | Strong for extrapolation (e.g., first-in-human dose prediction, drug-drug interactions, organ impairment). Mechanistically sound. | Strong for interpolation and rapid fitting to observed PK data. Less predictive for untested scenarios. |
| Computational Cost | Higher. More differential equations; longer run times, especially for population or sensitivity analysis. | Lower. Faster execution, enabling rapid scenario testing and model fitting. |
| Ideal Phase in Anti-Infective R&D | Candidate Selection (late) & Preclinical Development. For site-of-action predictions in deep tissues. | Lead Optimization & Candidate Selection (early). For rapid screening of analogs and initial PK parameter estimation. |
| Handling of Target Site (e.g., lung, brain) | Explicit compartment allows direct prediction of concentration-time profiles at the infection site. | Requires an additional "effect compartment" linked to plasma; less physiologically reflective of tissue barriers. |
Table 2: Quantitative Decision Metrics for Anti-Infective Programs
| Decision Factor | Favors Whole-Body PBPK | Favors Minimal PBPK |
|---|---|---|
| Available PK Data | Rich data from multiple tissues in preclinical species. | Only plasma PK data available. |
| Critical PK Question | Predicting penetration into a specific, hard-to-reach organ (e.g., CNS, bone). | Estimating overall clearance and volume of distribution. |
| Compound Properties | High logP, extensive tissue distribution, suspected transporter involvement. | Low-to-moderate logP, primarily confined to plasma and well-perfused tissues. |
| Project Timeline | Longer timeline allowing for model development and verification. | Accelerated timeline requiring quick "go/no-go" decisions. |
| Regulatory Strategy | Planning for a Clinically Relevant PK/PD Target justification to FDA/EMA. | Internal decision-making; early screening. |
Experimental Protocols for Parameterization
Protocol 3.1:In VivoTissue Distribution Study for Whole-Body PBPK
Objective: To obtain experimental tissue-to-plasma partition coefficients (Kp) for key organs, including the target infection site. Materials: See "Scientist's Toolkit" below. Procedure:
- Dosing & Sampling: Administer a single IV bolus of the anti-infective candidate to rodents (n=3-5/time point) at a pharmacologically relevant dose.
- Terminal Sampling: At pre-defined time points (e.g., 0.25, 1, 4, 8, 24h post-dose), anesthetize animals and collect blood via cardiac puncture into heparinized tubes.
- Tissue Collection: Immediately perfuse animals with saline via the heart. Excise and weigh target tissues: lung, liver, kidney, spleen, brain, muscle, skin, and the site of infection (e.g., infected lung lobe).
- Bioanalysis: Homogenize tissues in a suitable buffer (e.g., phosphate buffer, 1:4 w/v). Analyze drug concentrations in plasma and tissue homogenates using a validated LC-MS/MS method.
- Data Analysis: Calculate Kp for each tissue as AUCtissue / AUCplasma (using non-compartmental analysis) or by fitting a preliminary PBPK model.
Protocol 3.2: Rapid Plasma PK Study for Minimal PBPK
Objective: To generate plasma concentration-time data for initial fitting of a minimal PBPK model. Procedure:
- Dosing: Administer the candidate via IV and PO routes to preclinical species (e.g., mice, rats).
- Serial Blood Sampling: Collect small volume serial blood samples (e.g., via tail vein) at 8-10 time points up to 24-48 hours.
- Sample Processing: Centrifuge blood to obtain plasma. Store at -80°C until analysis.
- Bioanalysis: Quantify plasma drug concentrations using LC-MS/MS.
- Model Fitting: Fit a 2- or 3-compartment minimal PBPK model to the IV data to estimate central clearance and inter-compartmental rate constants. Use these parameters to simulate oral absorption.
Model Implementation Workflow
Title: Decision Workflow for PBPK Model Complexity Selection
Title: Structural Comparison of Whole-Body vs. Minimal PBPK Models
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PBPK Model Parameterization Studies
| Item / Reagent | Function & Application | Example Vendor/Product |
|---|---|---|
| LC-MS/MS System | Gold-standard bioanalysis for quantifying drug concentrations in plasma and tissue homogenates with high sensitivity and specificity. | Waters ACQUITY UPLC with Xevo TQ-S, Sciex Triple Quad 6500+ |
| Stable Isotope-Labeled Internal Standards | Critical for accurate LC-MS/MS quantification, correcting for matrix effects and recovery variations during sample preparation. | Cayman Chemical, Sigma-Aldridge (Custom Synthesis) |
| Physiological Buffer (PBS) | Used for tissue homogenization and as a matrix for calibration standards in tissue concentration assays. | Gibco Phosphate-Buffered Saline |
| Pharmacokinetic Modeling Software | Platform for building, simulating, and fitting both Whole-Body and Minimal PBPK models. | GastroPlus (Simulations Plus), PK-Sim (Open Systems Pharmacology), MATLAB/Simbiology |
| In Vitro Transporter Assay Kits | To determine if active transport influences tissue distribution (especially for brain, liver, kidney), informing model structure. | Solvo Transporter Assay Services, Corning Gentest |
| Tissue Partition Coefficient Prediction Software | Estimates Kp values in silico when experimental data is lacking, using methods by Rodgers & Rowland or Poulin & Theil. | ADMET Predictor (Simulations Plus), GastroPlus's PBPK Module |
Within the paradigm of Physiologically Based Pharmacokinetic (PBPK) modeling for anti-infective drug candidate selection, accurate prediction of drug exposure at the site of infection is paramount. This necessitates sophisticated modeling of tissue-to-plasma (Kp) ratios and intracellular concentrations. For anti-infectives targeting pathogens residing in specific tissues (e.g., lung for pneumonia, brain for encephalitis) or within host cells (e.g., macrophages for Mycobacterium tuberculosis, hepatocytes for hepatitis), traditional plasma PK is a poor surrogate for efficacy. This protocol details the integrated in vitro, in silico, and in vivo approaches required to generate robust parameters for PBPK models, thereby de-risking candidate selection and optimizing dosing regimens.
Table 1: Critical Input Parameters for PBPK Modeling of Tissue Distribution
| Parameter | Definition | Typical Experimental Method | Key Considerations for Anti-Infectives |
|---|---|---|---|
| Fraction Unbound in Plasma (fu) | Proportion of drug unbound to plasma proteins. | Equilibrium dialysis, ultrafiltration. | Species-specific (human, mouse). Impacts free drug hypothesis. |
| Fraction Unbound in Tissue (fut) | Proportion of drug unbound in tissue homogenate. | Equilibrium dialysis with tissue homogenate. | Tissue-specific (lung, liver, brain). Critical for Kp prediction. |
| Passive Permeability (Papp) | Rate of passive transcellular diffusion. | Caco-2 or MDCK cell monolayers. | Influences intracellular uptake and tissue penetration. |
| Transporter Kinetics (Km, Jmax) | Affinity and capacity for active uptake/efflux. | Transfected cell systems (HEK293, CHO). | Key for organs with barriers (BBB, placenta) and liver/kidney clearance. |
| Lysosomal Trapping Ratio | Ratio of drug accumulation in lysosomes vs. cytosol. | Cell-based assays with lysosomotropic agents. | Critical for weak bases targeting intracellular pathogens. |
| Observed In Vivo Kp | Tissue-to-plasma concentration ratio at steady state. | Terminal sampling in preclinical species (rodent). | Used for model validation and refinement. |
Table 2: Model-Predicted vs. Observed Kp Values for Representative Anti-Infective Classes
| Drug Class / Example | Predicted Kp (Lung) | Observed Kp (Lung) | Predicted Kp (Brain) | Observed Kp (Brain) | Major Distribution Mechanism |
|---|---|---|---|---|---|
| Fluoroquinolones (Levofloxacin) | 2.5 - 4.0 | 3.0 - 5.5 | 0.2 - 0.4 | 0.1 - 0.3 | Passive diffusion, moderate tissue binding. |
| Macrolides (Azithromycin) | 50 - 100 | 80 - 150 | 0.5 - 1.5 | 1 - 2 | Extensive lysosomal trapping, active uptake. |
| Rifamycins (Rifampin) | 3.0 - 5.0 | 4.0 - 6.0 | 0.05 - 0.15 | <0.1 | High protein binding, efflux transporter substrate. |
| Nitroimidazoles (Metronidazole) | 0.8 - 1.2 | ~1.0 | 0.8 - 1.2 | ~1.0 | Passive diffusion, low binding. |
Experimental Protocols
Protocol 3.1: Determination of Intracellular Concentration and Lysosomal Trapping
Objective: To quantify the intracellular accumulation and subcellular distribution of an anti-infective candidate in a macrophage cell line (e.g., THP-1). Materials: See "The Scientist's Toolkit" below. Procedure:
- Differentiate THP-1 monocytes into macrophages using 100 nM PMA for 48 hours.
- Wash cells and incubate with the test compound (at relevant free plasma concentrations) in complete medium for 2, 4, 8, and 24 hours. Include parallel wells with 50 mM ammonium chloride (NH4Cl) to neutralize lysosomal pH.
- Terminate incubation: wash cells 3x with ice-cold PBS.
- Lyse cells with 70:30 methanol:water containing internal standard. Centrifuge (13,000 g, 15 min, 4°C).
- Analyze supernatant via LC-MS/MS for drug concentration. Normalize to total cellular protein (BCA assay).
- Calculate: Intracellular-to-extracellular concentration ratio (Ccell/Cmedium). The difference in accumulation with/without NH4Cl indicates lysosomal trapping.
Protocol 3.2:In VivoTissue Distribution Study for Kp Validation
Objective: To obtain experimental tissue-to-plasma ratios in a rodent model for PBPK model validation. Materials: Cannulated rats/mice, test compound, heparinized saline, validated LC-MS/MS method. Procedure:
- Administer test compound via IV bolus or infusion to achieve steady-state (minimum 5 half-lives).
- At designated time points (n=3-5 animals/point), collect blood via cardiac puncture into heparin tubes under anesthesia.
- Immediately perfuse animal intracardially with ice-cold saline to clear blood from tissues.
- Harvest relevant tissues (lung, liver, kidney, brain, spleen). Weigh and snap-freeze in liquid N2.
- Process plasma (centrifuge blood) and homogenize tissues in a 4-fold volume of PBS.
- Perform bioanalysis via LC-MS/MS for drug concentrations in plasma and tissue homogenates.
- Calculate: Kp = (Tissue drug concentration [ng/g]) / (Plasma drug concentration [ng/mL]).
Visualizations
Diagram 1: PBPK Model Structure for Tissue Distribution
Title: PBPK Model Structure for Anti-Infective Tissue Distribution
Diagram 2: Workflow for Kp and Intracellular Modeling
Title: Integrated Workflow for Distribution Modeling
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Distribution Studies
| Item | Function/Application | Example Product/Assay |
|---|---|---|
| Human/Mouse Tissue Homogenates | For experimental determination of tissue binding (fut). | BioIVT Human Tissue Homogenates; Xenofresh mouse tissues. |
| Transporter-Expressing Cell Lines | To characterize SLC/OATP uptake and ABC efflux transporter interactions. | Solvo Transporter Assay Services; Corning Gentest. |
| Polarized Epithelial Cell Monolayers (Caco-2, MDCK) | Assessment of passive permeability and transporter-mediated flux. | Matrigel-coated transwell inserts. |
| Lysosomotropic Modulators (e.g., NH4Cl, Bafilomycin A1) | To inhibit lysosomal trapping and quantify its contribution. | Sigma-Aldrich ammonium chloride. |
| Stable Isotope-Labeled Internal Standards | For accurate and precise LC-MS/MS quantitation in complex matrices. | Cayman Chemical; Alsachim. |
| PBPK Modeling Software Platform | Integrated platform for building, simulating, and validating distribution models. | GastroPlus, Simcyp Simulator, PK-Sim. |
| Validated LC-MS/MS Method Kits | For bioanalysis of drug concentrations in plasma and tissue homogenates. | ChromSystems MassTox kits (modified for tissues). |
This Application Note outlines the critical integration of Pharmacodynamic (PD) targets into Physiologically-Based Pharmacokinetic (PBPK) models for anti-infective drug development. Within the thesis context of using PBPK for candidate selection, this step translates predicted plasma and tissue concentration-time profiles (PK) into quantifiable antibacterial effects. The primary PD indices linked are the Minimum Inhibitory Concentration (MIC), the Mutant Prevention Concentration (MPC), and the shape of Time-Kill Curves. Successfully linking PK to these PD targets allows for the prediction of efficacy, suppression of resistance, and optimization of dosing regimens in silico prior to costly clinical trials.
The efficacy of antibiotics is commonly described by three key PD indices derived from in vitro experiments. The relationship between PK profiles and these indices defines the antibacterial effect.
Table 1: Key Pharmacodynamic Indices for Anti-Infectives
| PD Index | Definition | Typical Unit | PK/PD Linking Parameter | Common Target for Efficacy* |
|---|---|---|---|---|
| MIC | Minimum Inhibitory Concentration: Lowest concentration that inhibits visible bacterial growth after 18-24h incubation. | µg/mL | - | Baseline for PK/PD ratio calculations (e.g., AUC/MIC). |
| MPC | Mutant Prevention Concentration: Concentration that prevents the growth of the least susceptible single-step mutant in a large bacterial population. | µg/mL | - | Target for resistance suppression (Time > MPC). |
| Time-Kill Curve Parameters | Describes the rate and extent of bacterial killing over time at fixed antibiotic concentrations. | log10 CFU/mL vs. Time | - | Informs model structure (e.g., linear vs. nonlinear killing). |
| ƒAUC/MIC | Area Under the free (unbound) concentration-time curve over 24h divided by the MIC. | unitless | AUC | Primary driver for efficacy of concentration-dependent antibiotics (e.g., fluoroquinolones, aminoglycosides). |
| ƒT>MIC | Percentage of dosing interval that the free drug concentration exceeds the MIC. | % | Concentration | Primary driver for efficacy of time-dependent antibiotics (e.g., β-lactams, vancomycin). |
| ƒCmax/MIC | Ratio of peak free drug concentration to the MIC. | unitless | Cmax | Correlate for efficacy and resistance suppression for some agents (e.g., aminoglycosides). |
| ƒT>MPC | Percentage of dosing interval that the free drug concentration exceeds the MPC. | % | Concentration | Key predictor for suppression of resistance emergence. |
*Target values are drug- and pathogen-specific. Example: For β-lactams, ƒT>MIC of 40-70% is often targeted for stasis, while >60-70% is targeted for 1-2 log kill.
Experimental Protocols
Protocol 3.1: Determination of Minimum Inhibitory Concentration (MIC)
Objective: To determine the lowest concentration of an antibiotic that inhibits the visible growth of a microorganism.
Materials:
- Cation-adjusted Mueller-Hinton Broth (CAMHB) or other appropriate medium.
- Sterile 96-well microtiter plates with lids.
- Test antibiotic stock solution.
- Bacterial inoculum at ~5 x 105 CFU/mL.
- Incubator.
Methodology:
- Prepare a serial two-fold dilution of the antibiotic in broth across the wells of a microtiter plate (e.g., 64 µg/mL to 0.06 µg/mL).
- Add an equal volume of the standardized bacterial inoculum to each well. Include growth control (bacteria, no drug) and sterility control (broth only) wells.
- Seal the plate and incubate under appropriate conditions (e.g., 35±2°C for 18-24 hours for most bacteria).
- Visualize growth (turbidity). The MIC is the lowest concentration of antibiotic that completely inhibits visible growth.
Protocol 3.2: Determination of Mutant Prevention Concentration (MPC)
Objective: To determine the antibiotic concentration that blocks the growth of the least susceptible single-step mutant.
Materials:
- Agar plates with antibiotic at various concentrations (typically 2x, 4x, 8x, 16x MIC).
- High-density bacterial inoculum (~1010 CFU from multiple colonies).
- Spreader.
Methodology:
- Prepare a series of agar plates containing the test antibiotic at concentrations above the MIC (e.g., 1x, 2x, 4x, 8x, 16x MIC).
- Prepare a high-density bacterial suspension (~1010 CFU/mL) in saline from an overnight culture.
- Plate 100 µL of the high-density inoculum onto each antibiotic-containing plate. Spread evenly.
- Incubate plates for 48-72 hours.
- The MPC is defined as the lowest antibiotic concentration that prevents any colony formation after 72 hours of incubation.
Protocol 3.3: Time-Kill Curve Assay
Objective: To characterize the rate and extent of bactericidal activity over time at fixed antibiotic concentrations.
Materials:
- Erlenmeyer flasks or tubes with appropriate broth.
- Test antibiotic solutions at multiples of MIC (e.g., 0x, 1x, 2x, 4x, 8x MIC).
- Bacterial inoculum at ~5 x 105 CFU/mL.
- Water bath shaker at 37°C.
- Microcentrifuge tubes and sterile saline for serial dilution and plating.
Methodology:
- Inoculate flasks containing broth and pre-determined antibiotic concentrations with the standardized bacterial suspension.
- Immediately after mixing (time 0), remove a sample for viable count determination.
- Incubate flasks under constant agitation. Remove samples at predetermined time points (e.g., 0, 1, 2, 4, 6, 8, 24 hours).
- Perform serial 10-fold dilutions of each sample in saline and plate onto antibiotic-free agar plates.
- Count colonies after incubation. Plot log10 CFU/mL versus time for each concentration.
- Analyze data for patterns: bactericidal (≥3-log kill), bacteriostatic, or regrowth.
Integration into PBPK/PD Modeling: Logical Framework & Workflow
The incorporation of PD targets into a PBPK model follows a sequential workflow where in vitro data inform the structure and parameters of a quantitative systems pharmacology model.
Title: Workflow for Integrating PD Targets into a PBPK Model
Title: Logical Structure of the Integrated PBPK/PD Model
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PK/PD Integration Experiments
| Item | Function in PD Studies | Key Consideration |
|---|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standard medium for MIC and time-kill assays against non-fastidious bacteria. Ensures reproducible cation concentrations (Ca2+, Mg2+) that affect aminoglycoside and polymyxin activity. | Use CLSI/EUCAST recommended formulations for compliance. |
| Sensitive & Resistant Bacterial Isolates | Test strains with known MICs and defined resistance mechanisms. Includes quality control strains (e.g., S. aureus ATCC 29213, P. aeruginosa ATCC 27853). | Maintain in cryopreserved stocks to ensure genetic stability. |
| 96-Well Microtiter Plates (Sterile, with Lid) | Vessel for broth microdilution MIC testing. Allows high-throughput testing of multiple concentrations and strains. | Use tissue culture-treated, non-pyrogenic plates to prevent cell adhesion. |
| Pre-Defined Antibiotic Plates (e.g., Sensititre) | Dried antibiotic panels for MIC testing. Increases reproducibility and throughput. | Ensure panels cover the expected dynamic range for the drug class. |
| Automated Liquid Handling System | For precise, high-throughput serial dilutions and plating in time-kill studies. Reduces human error and increases throughput. | Calibrate regularly for volumetric accuracy. |
| Colony Counter (Automated or Manual) | For accurate enumeration of bacterial colonies from time-kill and MPC assays. | Manual counting with a penlight magnifier is acceptable but automated systems improve reproducibility for high sample numbers. |
| PD Modeling Software (e.g., Phoenix WinNonlin, R, NONMEM) | To fit mathematical functions (e.g., Emax, logistic) to time-kill data and simulate PK/PD relationships. | Choose based on required model complexity and user expertise. R offers flexibility and open-source packages. |
| PBPK Software Platform (e.g., GastroPlus, Simcyp, PK-Sim) | Platform to build the compound PBPK model and integrate the PD effect model. | Selection depends on available compound and system databases, and PD linking capabilities. |
Within the framework of a broader thesis on Physiologically Based Pharmacokinetic (PBPK) modeling for anti-infective drug candidate selection, simulating drug exposure at specific infection sites is critical. This Application Note details protocols for predicting pharmacokinetic (PK) and pharmacodynamic (PD) profiles in challenging compartments: lungs, central nervous system (CNS), skin, and microbial biofilms. Accurate prediction at these sites enables prioritization of lead compounds with a higher probability of clinical success.
Key Quantitative Parameters for Site-Specific PBPK Modeling
Table 1: Physiological and Drug-Specific Parameters for Infection Site Simulation
| Parameter | Lungs (Pulmonary Epithelium) | CNS (Brain Parenchyma) | Skin (Dermis/Epidermis) | Biofilm Matrix |
|---|---|---|---|---|
| pH | 6.6-7.2 (Alveolar lining fluid) | 7.14-7.28 (Interstitial fluid) | 4.0-7.0 (Stratum corneum) | 5.5-7.5 (Variable) |
| Penetration Metric (Typical) | Epithelial Lining Fluid (ELF)/Plasma Ratio | Cerebrospinal Fluid (CSF)/Plasma Ratio | Dermal Interstitial Fluid/Plasma Ratio | Biofilm/Plasma Ratio |
| Key Barrier | Alveolar-capillary membrane, active efflux (e.g., P-gp) | Blood-Brain Barrier (BBB), Blood-CSF Barrier | Stratum corneum, dermal capillaries | Extracellular Polymeric Substance (EPS), slow diffusion |
| Permeability Coefficient (Papp x10^-6 cm/s) Range | 1-500 (for various compounds) | 0.1-10 (BBB specific) | 0.01-1.0 (transdermal) | Not typically measured |
| Critical PK/PD Index | fAUC/MIC, fCmax/MIC in ELF | fAUC/MIC in CSF or Brain ISF | fAUC/MIC in dermal ISF | Biofilm-specific MBEC or minimal biofilm inhibitory concentration (MBIC) |
Table 2: Example Simulated Exposure Output for a Hypothetical Fluoroquinolone
| Infection Site | Simulated fAUC0-24 (mg·h/L) | Target fAUC/MIC (for MIC=0.25 mg/L) | Probability of Target Attainment (PTA) at 600 mg q24h |
|---|---|---|---|
| Plasma | 35.2 | 140.8 | 98% |
| Lung (ELF) | 25.4 | 101.6 | 85% |
| CNS (CSF) | 8.7 | 34.8 | 45% |
| Skin (ISF) | 28.9 | 115.6 | 92% |
| Biofilm | 4.5 | 18.0 | 15% |
Detailed Experimental Protocols for Model Verification
Protocol 3.1: Microdialysis for Lung and Skin Interstitial Fluid (ISF) Sampling
Objective: To measure unbound antibiotic concentrations in the interstitial fluid of rat lung or skin for PBPK model verification. Materials: See "The Scientist's Toolkit" below. Procedure:
- Anesthetize and intubate rat. Place in lateral recumbency.
- For Lung: Make a small skin incision over the thorax. Insert a linear microdialysis probe (20 kDa MWCO) into the lung parenchyma under guided imaging.
- For Skin: Insert a probe subcutaneously or into the dermal layer of the designated skin area.
- Perfuse the probe with sterile saline or Ringer's solution at 1.0 µL/min using a precision pump.
- After 60-min equilibration, collect microdialysate samples over defined intervals (e.g., 30-min) synchronized with plasma sampling after IV/PO drug administration.
- Analyze microdialysate and corresponding plasma samples using a validated LC-MS/MS method.
- Calculate unbound tissue concentration. Use recovery (determined via retrodialysis) to correct dialysate concentrations.
Protocol 3.2: In Vitro Static Biofilm Model for PK/PD Analysis
Objective: To determine the penetration and time-kill kinetics of an antibiotic against a bacterial biofilm. Materials: 96-well peg lid biofilm reactor, cation-adjusted Mueller Hinton Broth (CAMHB), Calgary Biofilm Device. Procedure:
- Inoculate CAMHB with a standardized bacterial suspension (e.g., Pseudomonas aeruginosa PAO1) at ~10^6 CFU/mL.
- Immerse the peg lid into the inoculated broth. Incubate statically for 24h at 37°C to form biofilms on pegs.
- Gently rinse pegs twice in saline to remove planktonic cells.
- Transfer the peg lid to a new 96-well plate containing serial dilutions of the antibiotic in broth (simulating systemic Cmax or sustained concentrations).
- Expose biofilms to antibiotic for 0, 2, 4, 8, 24h at 37°C.
- At each time point, remove corresponding pegs, sonicate in saline to dislodge biofilm, and vortex vigorously.
- Viable count the resulting suspension to determine biofilm-bacterial density (CFU/peg). Plot time-kill curves and estimate biofilm MBIC.
Visualization of Workflows and Relationships
Diagram 1: PBPK Workflow for Site Exposure Prediction
Diagram 2: Drug Distribution from Plasma to Infection Site
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Site-Specific Exposure Studies
| Item | Function & Application | Example Product/Model |
|---|---|---|
| In Vitro BBB Kit | Co-culture of brain endothelial cells and astrocytes to measure transcellular permeability and efflux. | Millicell EZ Plate or proprietary co-culture inserts. |
| Artificial Epithelial Lining Fluid (aELF) | Physiologically relevant simulated lung fluid for solubility and stability testing of inhaled antibiotics. | Prepared per EPAG formulation (Ca2+, Na+, Cl-, DPPC). |
| Microdialysis System | For continuous sampling of unbound drug from tissue ISF in vivo (rat, mouse). | CMA 63 or 71 probes with 20 kDa MWCO, CMA 402 pump. |
| Biofilm Reactor | Generates high-throughput, reproducible biofilms for penetration and kill kinetic studies. | Calgary Biofilm Device (peg lid), MBEC Assay. |
| Skin Permeation Model | Ex vivo or reconstructed human epidermis for transdermal permeation studies. | Franz Diffusion Cell, EpiDerm or SkinEthic tissues. |
| LC-MS/MS Kit | Sensitive and specific quantification of antibiotics in complex biological matrices (plasma, ISF, homogenate). | Supported methods for, e.g., beta-lactams, vancomycin. |
| PBPK Software | Platform for developing, simulating, and validating mechanistic PBPK models. | GastroPlus, Simcyp Simulator, PK-Sim. |
Overcoming Common PBPK Modeling Pitfalls and Optimizing for Candidate Selection
Within the thesis "Development and Application of PBPK Models for the Rational Selection of Anti-Infective Drug Candidates," a critical challenge arises when model simulations diverge significantly from observed clinical or preclinical pharmacokinetic (PK) data. This discrepancy undermines the model's utility for predicting drug-drug interactions, optimizing dosing regimens, and selecting candidates with the highest probability of success. This document outlines a systematic, protocol-driven approach to diagnose such poor predictions using sensitivity analysis (SA) as the core investigative tool, focusing on identifying which physiological, drug-specific, and system parameters exert the most influence on key PK outputs.
Theoretical Foundation: Sensitivity Analysis in PBPK
Sensitivity Analysis quantifies how uncertainty in a model's output can be apportioned to different sources of uncertainty in its input parameters. For PBPK models, Local Sensitivity Analysis (LSA) is used to probe the local impact of a single parameter, while Global Sensitivity Analysis (GSA) assesses the combined effects of multiple parameters varying simultaneously over their plausible ranges.
- Local Sensitivity Analysis (LSA): Calculates partial derivatives or normalized sensitivity coefficients (NSC). It is computationally efficient and ideal for initial screening.
- Global Sensitivity Analysis (GSA): Employs methods like Morris Screening or Sobol' indices to explore the entire parameter space, capturing interactions between parameters.
Core Protocols for Sensitivity Analysis
Protocol 3.1: Local Sensitivity Analysis (LSA) Screening
Objective: To rapidly identify parameters with the largest linear effect on a specific PK endpoint (e.g., AUC, Cmax, Tmax) near the nominal parameter values.
Materials & Software: PBPK platform (e.g., GastroPlus, Simcyp, PK-Sim, or MATLAB/Python with model code), parameter database, visualization tool.
Methodology:
- Define Output of Interest (OoI): Select the PK metric where model discrepancy is observed (e.g., Plasma AUC0-24h).
- Select Parameter Set (P): Create a list of candidate uncertain parameters (e.g., solubility, permeability, intrinsic clearance, tissue partition coefficients, blood flow rates).
- Set Perturbation Factor (Δ): Define a small variation (e.g., ±1%, ±5%) from the nominal value for each parameter.
- Run Simulations: For each parameter pᵢ in P: a. Run simulation with pᵢ increased by Δ. b. Run simulation with pᵢ decreased by Δ. c. Record the resulting OoI values.
- Calculate Normalized Sensitivity Coefficient (NSC):
NSCᵢ = [(OoI₊ - OoI₋) / OoIₙₒₘᵢₙₐₗ] / [(pᵢ₊ - pᵢ₋) / pᵢₙₒₘᵢₙₐₗ]
Where
+and-denote results from the ±Δ perturbations. - Rank Parameters: Sort parameters by the absolute value of their NSC. High |NSC| indicates high local sensitivity.
Table 1: Example LSA Results for a Hypothetical Oral Anti-Infective (Impact on AUC0-24)
| Parameter (pᵢ) | Nominal Value | NSC (Δ=5%) | Rank | Interpretation |
|---|---|---|---|---|
| Fraction Unbound in Plasma (fu) | 0.10 | 0.85 | 1 | Highly sensitive: critical for accurate clearance prediction. |
| Enterocyte Permeability (Peff) | 5.0e-4 cm/s | 0.72 | 2 | Highly sensitive: key driver of absorption for this BCS class. |
| Hepatic Intrinsic Clearance (CLint) | 50 µL/min/mg | -0.68 | 3 | Highly sensitive: primary elimination route. |
| Luminal Solubility (pH 6.5) | 100 µg/mL | 0.15 | 4 | Moderately sensitive. |
| Intestinal Transit Time | 3.0 h | -0.08 | 5 | Low sensitivity for this endpoint. |
Protocol 3.2: Global Sensitivity Analysis using Morris Screening
Objective: To identify the most influential parameters and detect potential interactions over their full physiological ranges, prioritizing parameters for refinement.
Methodology:
- Define Parameter Ranges: For each parameter in set P, define a physiologically or experimentally plausible minimum and maximum value.
- Generate Trajectories: Use the Morris method to generate r random trajectories through the parameter space. Each parameter is discretized into k levels.
- Run Ensemble Simulations: Execute the PBPK model for each parameter set defined by the trajectories.
- Compute Elementary Effects (EE): For each parameter pᵢ in each trajectory, calculate: EEᵢ = [OoI(p₁,..., pᵢ+Δ,..., pₖ) - OoI(p)] / Δ
- Compute Sensitivity Metrics:
- μ* (mu-star): The mean of the absolute EE. A high μ* indicates a parameter with overall influence on the output.
- σ (sigma): The standard deviation of the EE. A high σ indicates a parameter involved in non-linear interactions or whose effect depends on the values of other parameters.
- Plot & Interpret: Create a μ* vs σ plot to classify parameters.
Table 2: Example GSA (Morris) Metrics for Systemic Cmax
| Parameter | μ* (Main Effect) | Rank | σ (Interaction) | Interpretation |
|---|---|---|---|---|
| fu | 0.89 | 1 | 0.10 | High main effect, low interaction. Key driver. |
| CLint | 0.75 | 2 | 0.45 | High main effect AND high interaction. Effect depends on other params (e.g., fu, blood flow). |
| Peff | 0.70 | 3 | 0.15 | High main effect, low interaction. |
| Cardiac Output | 0.25 | 4 | 0.30 | Moderate effect with notable interactions. |
Title: SA Troubleshooting Workflow for PBPK Models
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Parameter Refinement Following SA
| Item / Solution | Function in Context | Example / Vendor |
|---|---|---|
| Parallel Artificial Membrane Permeability Assay (PAMPA) | Validates and refines critical permeability (Peff) predictions identified by SA. | Corning Gentest Pre-coated PAMPA Plate System |
| Human Liver Microsomes (HLM) / Hepatocytes | Measures and refines hepatic intrinsic clearance (CLint) parameters flagged as sensitive. | BioIVT Human Liver Microsomes; Corning UltraPool HLM |
| Equilibrium Dialysis or Ultracentrifugation Devices | Accurately determines fraction unbound in plasma (fu), a typically high-sensitivity parameter. | HTDialysis RED Device; Thermo Fisher Single-Use Ultracentrifugation Tubes |
| Physiologically Relevant Solubility Assay Kits | Refines solubility parameters in biorelevant media (FaSSIF/FeSSIF). | Biorelevant.com FaSSIF/FeSSIF powders |
| P-gp / BCRP Inhibition/Substrate Assays | Characterizes transporter-mediated processes if SA indicates sensitivity to gut/hepatic transport. | Solvo Transporter Assay Kits; MDR1-MDCKII cells |
| Parameter Estimation Software Module | Integrated tool within PBPK platforms to formally optimize sensitive parameters against in vivo data. | GastroPlus Parameter Estimation; Simcyp Population-based Optimizer |
Case Application: Troubleshooting an Anti-Infective Candidate
Scenario: A PBPK model for a novel oral protease inhibitor (BCS Class II) under-predicts human AUC by 50%.
Application of Protocols:
- LSA (Protocol 3.1) on the initial model identifies
fu(NSC=0.92),Peff(NSC=0.78), andsolubility in fed state(NSC=0.41) as the top three locally sensitive parameters for AUC. - GSA (Protocol 3.2) confirms
fuandPeffhave high μ*, and reveals a high σ forsolubility, indicating its effect is highly dependent on other conditions (e.g., bile salt levels). - Action: The toolkit is deployed:
- Redetermine
fuusing human plasma via equilibrium dialysis (Toolkit Item 3). - Refine
Peffusing PAMPA assays correlating to human in vivo data (Toolkit Item 1). - Conduct solubility studies in Fed-State Simulated Intestinal Fluid (FeSSIF) to obtain a more accurate input (Toolkit Item 4).
- Redetermine
- Re-simulate: Updated parameters are incorporated, resulting in a model prediction within 15% of the observed clinical AUC.
Title: Case Study: From SA to Parameter Refinement
Application Notes
Within PBPK modeling for anti-infective drug candidate selection, critical decisions on compound progression must often be made with incomplete preclinical datasets. This necessitates a framework for transparently quantifying uncertainty and strategically planning experiments to maximize informative value. The core strategy involves integrating prior knowledge, adaptive experimental design, and advanced modeling techniques to guide selection.
Key Quantitative Challenges in Anti-infective PBPK: The table below summarizes common data gaps and their quantitative impact on PBPK model parameters for anti-infectives.
Table 1: Common Preclinical Data Gaps and Their Impact on PBPK Parameters
| Data Gap | Affected PBPK Parameters | Typical Uncertainty Range (Without Data) | Primary Mitigation Strategy |
|---|---|---|---|
| Unmeasured tissue-to-plasma partition coefficients (Kp) | Tissue volumes of distribution (Vt) | Predicted Vss can vary by 2-5 fold | Use in silico prediction (e.g., Poulin & Rodgers, mechanistic) with sensitivity analysis. |
| Limited protein binding across species | Free drug fraction (fu), hepatic clearance | fu extrapolation error ~30-50% | Measure fu in human plasma in vitro early; use species-specific values. |
| Sparse metabolite identification/pathway | Metabolic clearance (CLmet), enzyme kinetics | CLh uncertainty >100% | Use human hepatocyte or microsome data to identify major pathways. |
| Unknown biliary clearance contribution | Biliary clearance (CLbile) | May miss >20% of total CL | Sandwich-cultured hepatocyte assays; transporter phenotyping. |
| Limited target site (e.g., lung, CSF) concentration data | Target site penetration (Kp,uu) | Kp,uu assumed 1.0 (error unknown) | Design focused tissue PK study or use relevant in vitro surrogate (e.g., epithelial cell layers). |
Strategic Protocol 1: Tiered In Vitro to In Vivo Scaling for Clearance Objective: To estimate human hepatic clearance (CLh) with quantified uncertainty when in vivo preclinical PK data is sparse. Materials:
- Cryopreserved human hepatocytes (pooled, 3+ donors) or human liver microsomes.
- Substrate (test compound) at 1 µM (non-saturating).
- Positive control compounds (e.g., testosterone for CYP3A4).
- LC-MS/MS system for bioanalysis. Method:
- Incubation: Incubate test compound (in triplicate) with hepatocytes (0.5-1.0 million cells/mL) or microsomes (0.1-1 mg protein/mL) in appropriate buffer at 37°C. Use a time course (e.g., 0, 15, 30, 60, 90 min).
- Termination: At each time point, remove aliquot and quench with acetonitrile containing internal standard.
- Analysis: Quantify parent compound depletion via LC-MS/MS.
- Scaling: Calculate in vitro intrinsic clearance (CLint, in vitro). Scale to in vivo CLint using hepatocellularity (120 million cells/g liver) or microsomal protein per gram liver. Apply appropriate liver models (e.g., well-stirred, parallel tube).
- Uncertainty Quantification: Perform Monte Carlo simulation (n=1000) incorporating variability in in vitro depletion rate, scaling factors, and human liver weight/flow. Report CLh prediction as median with 5th-95th percentile range.
Strategic Protocol 2: Optimal Design for Tissue Distribution Study Objective: To prioritize tissues for Kp measurement based on PBPK model sensitivity and drug properties. Materials:
- Radiolabeled ([14C]) drug candidate.
- Relevant animal model (e.g., rat, 3-4 animals per time point).
- Terminal anesthesia and surgical tools.
- Tissue homogenizer and scintillation counter/accelerator mass spectrometry. Method:
- Sensitivity Analysis: Run a preliminary PBPK model with estimated Kp values. Perform local or global sensitivity analysis to identify which tissue Kp parameters most influence key PK metrics (AUC, Cmax, Vss).
- Dosing & Sampling: Administer a single IV dose of radiolabeled compound. Sacrifice animals at strategically chosen time points (e.g., 0.25h, 1h, 4h, 8h) to capture distribution and elimination phases.
- Tissue Collection: Collect blood (for plasma) and top 5-6 tissues identified as sensitive (e.g., liver, lung, kidney, muscle, adipose, target tissue).
- Quantification: Homogenize tissues and quantify total radioactivity concentration in each tissue and plasma.
- Calculation & Integration: Calculate observed Kp (Ctissue/Cplasma) at each time point. Input mean Kp values into the PBPK model to refine Vss and tissue exposure predictions.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Pooled Cryopreserved Human Hepatocytes | Gold-standard in vitro system for assessing metabolic clearance, enzyme induction, and transporter activity relevant to humans. |
| Transfected Cell Lines (e.g., OATP1B1/1B3, BCRP, P-gp) | Used to phenotype specific transporter-mediated uptake or efflux, informing tissue distribution and clearance pathways. |
| Rapid Equilibrium Dialysis (RED) Device | Efficient plate-based method for determining unbound fraction (fu) in plasma or tissue homogenates. |
| Physiologically Relevant Buffer (e.g., FaSSIF/FeSSIF) | Simulates intestinal fluid for in vitro dissolution and permeability studies, improving prediction of oral absorption. |
| [14C]-Labeled Drug Compound | Enables definitive mass balance studies, precise quantification of tissue distribution, and metabolite profiling. |
| PBPK Software Platform (e.g., GastroPlus, Simcyp, PK-Sim) | Enables integration of in vitro and physicochemical data, simulation of PK, and quantitative uncertainty analysis. |
Visualizations
Title: Strategy for Managing Data Gaps in PBPK Modeling
Title: Data Gap Impact Pathway
Within the thesis framework on PBPK modeling for anti-infective candidate selection, the predictive power of models is fundamentally constrained by the quality and traceability of input parameters. Successful IVIVE is paramount for predicting human pharmacokinetics (PK) and pharmacodynamics (PD) of novel anti-infectives. This document details application notes and protocols for sourcing and optimizing critical parameters.
The following table categorizes essential PBPK model parameters, their primary sources, and a credibility score based on consensus from current literature.
Table 1: Core PBPK Parameters for Anti-Infectives: Sources & Credibility
| Parameter Category | Specific Parameters | Primary In Vitro Source | Recommended In Vivo/Ex Vivo Refinement | Credibility (1-5, Low-High) | Key Assumptions/Limitations |
|---|---|---|---|---|---|
| Physicochemical | logP, pKa, Solubility | Shake-flask, Potentiometric titration | NA | 5 | Buffer/medium composition critical. |
| Binding | Plasma Protein Binding (fup) | Equilibrium dialysis, Ultrafiltration | Compare across preclinical species | 4 | Temperature, pH, and buffer effects must be controlled. |
| Metabolic Stability | CLint (Liver) | Human liver microsomes (HLM), Hepatocytes (suspended/plated) | Scaling via REF (relative abundance) and ISEF (inter-system extrapolation factor). | 3-4 | Correct for non-specific binding; enzyme activity loss in vitro. |
| Transport | Km, Vmax/Jmax for transporters (e.g., OATP1B1, P-gp) | Transfected cell lines (e.g., HEK293, MDCK) | Probe drug comparisons; tissue slice uptake. | 2-3 | Overexpression may distort kinetics; need cell system controls. |
| Tissue Partitioning | Kp values (Tissue:Plasma) | In silico prediction (Poulin & Theil, Berezhkovskiy), in vitro assay (tissue homogenate) | Rodent tissue distribution studies (µPET where possible). | 3 | Assumes steady-state, passive distribution. Poor for active transport organs. |
| Target Engagement | MIC (bacterial), IC50 (viral/host) | Standardized in vitro susceptibility assays (e.g., broth microdilution) | Infection model PK/PD correlation (e.g., murine thigh/lung). | 4 | In vitro conditions may not reflect in vivo milieu. |
Detailed Experimental Protocols
Protocol 3.1: Determination of Intrinsic Clearance (CLint) Using Cryopreserved Human Hepatocytes
Objective: To generate high-quality metabolic stability data for IVIVE scaling to human hepatic clearance.
Materials (Research Reagent Solutions Toolkit):
- Cryopreserved Human Hepatocytes: Pooled donors (e.g., 5-donor, gender-balanced). Function: Biologically relevant metabolic system containing full complement of phase I/II enzymes and cofactors.
- Williams' E Medium (+ supplements): Function: Maintenance medium supporting hepatocyte viability and metabolic function.
- Test Compound (Anti-infective): Prepared in DMSO (final concentration ≤0.1%). Function: Substrate for metabolic reactions.
- Control Compounds (e.g., Verapamil, Propranolol): Function: High and low clearance benchmarks for assay validation.
- Pre-Warmed Incubation Buffer (Krebs-Henseleit or similar): Function: Physiologically relevant incubation matrix.
- Stop Solution (Acetonitrile with Internal Standard): Function: Terminates enzymatic reaction and precipitates protein for LC-MS/MS analysis.
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) System: Function: Quantification of parent compound depletion over time.
Procedure:
- Thawing & Viability Check: Rapidly thaw hepatocytes in a 37°C water bath. Wash and resuspend in Williams' E medium. Determine viability via Trypan Blue exclusion (accept ≥80%).
- Incubation Setup: Pre-warm incubation buffer to 37°C. Dispense hepatocyte suspension (e.g., 0.5 million viable cells/mL) into incubation tubes. Pre-incubate for 5-10 minutes.
- Reaction Initiation: Spike in test/control compound to start reaction (final typical concentration: 1 µM, well below Km). Maintain gentle agitation.
- Time-Point Sampling: At designated times (e.g., 0, 5, 15, 30, 45, 60 min), withdraw an aliquot and immediately quench in cold stop solution.
- Sample Analysis: Vortex, centrifuge, and analyze supernatant via LC-MS/MS to determine parent compound concentration.
- Data Analysis: Plot ln(peak area ratio) vs. time. The slope (k, min⁻¹) is the depletion rate. Calculate in vitro CLint, in vitro = k / (number of cells per mL * incubation volume). Scale to in vivo CLint, in vivo using scaling factors: Hepatocellularity (e.g., 120 million cells/g liver) and liver mass (e.g., 25.7 g/kg body weight).
Protocol 3.2: Assessment of P-glycoprotein (P-gp) Interaction Using Bidirectional Transport Assay
Objective: To quantify the transporter-mediated flux of an anti-infective candidate, informing gut and brain penetration predictions.
Materials (Research Reagent Solutions Toolkit):
- MDCKII-MDR1 or Caco-2 Cell Monolayers: Function: Well-characterized in vitro models expressing human P-gp. MDCKII-MDR1 preferred for specificity.
- Transwell Plates (e.g., 24-well, 0.4 µm pore): Function: Support cell monolayer growth and allow separate access to apical (A) and basolateral (B) compartments.
- Transport Buffer (HBSS-HEPES, pH 7.4): Function: Isotonic buffer for transport studies.
- Test Compound: Prepared in DMSO. Function: Putative P-gp substrate or inhibitor.
- Model P-gp Substrates/Inhibitors (e.g., Digoxin, Loperamide / Zosuquidar): Function: Positive controls for assay validation.
- LC-MS/MS System: Function: Sensitive quantification of compound in A and B compartments.
- Transepithelial Electrical Resistance (TEER) Meter: Function: Monitors monolayer integrity pre- and post-assay.
Procedure:
- Monolayer Preparation & Validation: Culture cells on Transwell filters until confluent and differentiated. Measure TEER prior to assay (e.g., >300 Ω·cm² for MDCKII-MDR1).
- Pre-incubation: Wash monolayers twice with warm transport buffer.
- Bidirectional Transport:
- A-to-B (Absorption): Add compound to donor apical compartment. Sample from receiver basolateral compartment over time (e.g., 30, 60, 90, 120 min).
- B-to-A (Efflux): Add compound to donor basolateral compartment. Sample from receiver apical compartment over same intervals.
- Include a set with a known P-gp inhibitor (e.g., 2 µM zosuquidar) to confirm P-gp-specific efflux.
- Sample Analysis: Quantify compound concentration in all samples using LC-MS/MS.
- Data Analysis: Calculate apparent permeability (Papp) for each direction. Determine Efflux Ratio (ER) = Papp (B-A) / Papp (A-B). An ER > 2 with significant inhibition (>50% reduction) by inhibitor indicates active P-gp-mediated efflux.
Visualizing Parameter Integration and Impact
Diagram 1: IVIVE-PBPK Workflow for Anti-Infectives
Diagram 2: Key Parameter Influence on Anti-Infective PK Prediction
Application Notes
Within the framework of PBPK modeling for anti-infective drug candidate selection, addressing complex pharmacokinetic (PK) properties is critical for accurate human dose prediction and efficacy/safety profiling. This document details the application notes and protocols for integrating three key complexities: prodrug activation, nonlinear PK, and active metabolite formation.
1. Prodrugs (e.g., Remdesivir, Tenofovir Alafenamide)
- PBPK Context: A prodrug PBPK model consists of linked parent (prodrug) and metabolite (active drug) sub-models. The rate and site of enzymatic conversion (e.g., by CES1, CES2, CYP450s) are crucial determinants of systemic exposure to the active moiety.
- Key Consideration: Tissue-specific expression of activating enzymes must be incorporated to predict targeted activation (e.g., hepatic activation vs. lymphatic activation for nucleoside analogs). Drug-drug interactions (DDIs) at the activation enzyme level can significantly alter efficacy.
2. Nonlinear PK (e.g., Saturation of Transporters or Enzymes)
- PBPK Context: Nonlinearity often arises from capacity-limited processes such as:
- Saturable Active Hepatic Uptake (OATP1B1/1B3): Leads to more than proportional increases in systemic exposure (AUC) with dose.
- Saturable Metabolism (CYP3A4, CYP2C8): Leads to less than proportional increases in AUC with dose (auto-inhibition).
- Key Consideration: Accurate in vitro determination of Michaelis-Menten constants (Km, Vmax) for the saturable process is essential for model parameterization and scaling.
3. Active Metabolites (e.g., Desmethyl-Linezolid, Voriconazole-N-Oxide)
- PBPK Context: The PBPK model must simultaneously describe the PK of the parent drug and its active metabolite(s), including their formation, distribution, and elimination. The metabolite may have different target affinity (PD), plasma protein binding, and clearance pathways.
- Key Consideration: The relative contribution of parent and metabolite to overall pharmacodynamic (PD) effect (e.g., antimicrobial kill) must be quantified via an integrated PBPK/PD model.
Table 1: Quantitative Parameters for Complex Anti-Infective Drug Properties
| Property | Example Compound | Key Parameter | Typical Value (Range) | PBPK Model Input |
|---|---|---|---|---|
| Prodrug | Tenofovir Alafenamide | Intestinal CES2 Conversion Fraction | 0.80 - 0.95 | Fraction metabolized to metabolite via enzyme. |
| Nonlinear PK | Cefadroxil (OATP-mediated uptake) | Hepatic Uptake Km (µM) | ~100 - 500 µM | Michaelis constant for saturable transporter. |
| Active Metabolite | Linezolid | Metabolic Ratio (AUCm/AUCp) | ~0.3 - 0.5 | In vitro CLint for formation or observed in vivo ratio. |
Experimental Protocols
Protocol 1: In Vitro Determination of Prodrug Activation Kinetics Objective: To quantify the enzymatic conversion rate (CLint,act) of a prodrug to its active moiety. Materials: Human liver S9 fraction or recombinant enzyme (e.g., hCES1), prodrug substrate, LC-MS/MS system. Procedure:
- Prepare incubation mixtures (n=3) containing S9 fraction (0.5 mg/mL) in phosphate buffer (pH 7.4).
- Spike in prodrug at 5 concentrations (e.g., 1-100 µM) below expected Km.
- Incubate at 37°C for a time within linear range (e.g., 10 min).
- Terminate reaction with acetonitrile containing internal standard.
- Quantify formed active drug using a validated LC-MS/MS method.
- Calculate reaction velocity (v). Plot v vs. [S] to derive Vmax and Km. Intrinsic clearance for activation (CLint,act) = Vmax / Km.
Protocol 2: Assessing Saturable Hepatic Uptake in Sandwich-Cultured Human Hepatocytes (SCHH) Objective: To obtain Km and Vmax for saturable hepatic uptake. Materials: Fresh or cryopreserved SCHH, test compound, reference OATP inhibitor (e.g., Rifampin), LC-MS/MS. Procedure:
- Culture human hepatocytes in a sandwich configuration for 5-7 days to repolarize and express functional transporters.
- Pre-incubate SCHH with/without inhibitor in uptake buffer (10 min).
- Initiate uptake by adding test compound at 6-8 concentrations spanning expected Km (e.g., 0.1xKm to 10xKm).
- Terminate uptake at multiple time points (e.g., 1, 2.5, 5 min) to determine initial linear rate by washing with ice-cold buffer.
- Lyse cells and quantify intracellular drug accumulation via LC-MS/MS.
- Fit uptake velocity vs. concentration data to a Michaelis-Menten model with passive diffusion: v = (Vmax * [S]) / (Km + [S]) + Pdiff * [S].
Protocol 3: Characterizing Active Metabolite PK in a Rodent Study Objective: To obtain simultaneous PK profiles of parent drug and active metabolite for PBPK model verification. Materials: Rats (n=6), formulated drug, cannulated jugular vein, LC-MS/MS. Procedure:
- Administer a therapeutically relevant IV and PO dose of the parent drug to rats.
- Collect serial blood samples (e.g., 0.083, 0.25, 0.5, 1, 2, 4, 8, 12, 24 h) post-dose.
- Immediately centrifuge samples to obtain plasma.
- Analyze plasma samples using a multiplexed LC-MS/MS method validated for simultaneous quantification of parent and metabolite.
- Perform non-compartmental analysis (NCA) to determine AUC, Cmax, t1/2 for both entities. Calculate metabolic ratio.
- Use these data to verify and refine the coupled parent-metabolite PBPK model.
Visualization
PBPK Modeling Workflow for Prodrugs
Mechanistic Causes of Nonlinear Pharmacokinetics
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Characterizing Complex Drug Properties
| Item | Function/Application |
|---|---|
| Recombinant Human Enzymes (CES1, CES2, CYP450s) | To isolate and quantify the contribution of specific enzymes to prodrug activation or metabolite formation. |
| Sandwich-Cultured Human Hepatocytes (SCHH) | Gold-standard in vitro system to study hepatic uptake, metabolism, biliary excretion, and their saturation. |
| Transfected Cell Lines (e.g., MDCK-OATP1B1) | To characterize saturable transporter-mediated uptake or efflux kinetics in isolation. |
| Stable Isotope-Labeled Internal Standards (^13C, ^2H) | For accurate and precise LC-MS/MS quantification of parent drug and metabolites in complex biological matrices. |
| Physiologically Relevant In Vitro Buffers (e.g., Hanks' Balanced Salt Solution) | To maintain physiological ion concentrations and pH during transport/metabolism assays. |
| PBPK Software Platform (e.g., GastroPlus, Simcyp, PK-Sim) | To integrate in vitro and in silico data, build mechanistic models, and simulate human PK. |
Physiologically Based Pharmacokinetic (PBPK) modeling is a critical, mechanistic tool in modern anti-infective drug development. It enables researchers to predict drug disposition in virtual patient populations, simulate drug-drug interactions, and optimize dosing regimens prior to costly clinical trials. The selection of appropriate PBPK software is a pivotal decision that directly impacts research efficiency and model reliability. This document provides application notes and protocols for evaluating and deploying PBPK tools, focusing on the central trade-off between user-friendly interfaces and flexible, customizable modeling capabilities within the context of anti-infective research.
Comparative Analysis of Primary PBPK Software Platforms
The following table summarizes key features, data requirements, and suitability of leading commercial and open-source PBPK platforms for anti-infective applications. Data is synthesized from recent vendor documentation, peer-reviewed literature, and user community feedback (as of late 2023/early 2024).
Table 1: Comparative Overview of PBPK Software Platforms for Anti-Infective Research
| Software Platform | Primary Licensing Model | Key Anti-Infective Features | User-Friendliness (Scale 1-5) | Model Flexibility (Scale 1-5) | Typical Use Case in Anti-Infectives |
|---|---|---|---|---|---|
| GastroPlus | Commercial | Advanced Compartmental Absorption & Transit (ACAT) model; robust DDI module; extensive ADMET property prediction. | 5 | 4 | Oral absorption simulation for antivirals; complex enzyme-transporter mediated DDIs. |
| Simcyp Simulator | Commercial (now part of Certara) | Population-based simulator; tailored "Virtual Populations"; specialized disease (e.g., hepatic impairment) models. | 5 | 3 | Population PK variability in special populations (elderly, pediatric); perpetrator DDI risk assessment. |
| PK-Sim | Open-Source (part of Open Systems Pharmacology Suite) | Full-body PBPK; comprehensive ontologies for tissues & processes; MoBi for detailed model extension. | 3 | 5 | Mechanistic tissue distribution of novel antibiotic classes; custom intracellular target binding. |
| MATLAB/Simulink with Toolboxes | Commercial | Ultimate flexibility; allows coding of any physiological structure or process; requires significant programming. | 1 | 5 | Prototype novel PBPK structures (e.g., for host-pathogen-drug interactions); method development research. |
| Berkeley Madonna | Commercial | Efficient differential equation solver; model structure is entirely user-defined. | 2 | 5 | Educational/training models; rapid prototyping of core PK/PD linked systems. |
Note: Ratings are relative and based on typical user experience. Flexibility often inversely correlates with out-of-the-box user-friendliness.
Application Note: Protocol for Software Selection and Evaluation
Protocol Title: Systematic Evaluation of PBPK Software for a Novel Antiviral Candidate
Objective: To establish a reproducible workflow for selecting a PBPK software platform that balances an intuitive interface for routine simulations with sufficient flexibility to incorporate a novel mechanism of intracellular metabolism.
Background: Candidate drug X is a nucleoside analog pro-drug with complex, non-linear activation involving host and viral enzymes. Standard PBPK software libraries may not contain this specific metabolic pathway.
Materials & Reagent Solutions:
Table 2: Essential Research Toolkit for PBPK Software Evaluation
| Item/Reagent | Function in Evaluation |
|---|---|
| Compound Physicochemical & ADME Data | In vitro CLint, fu, Log P, pKa, B:P ratio. Serves as mandatory input for all software. |
| In Vitro Enzyme Kinetic Data (Vmax, Km) | For novel activation pathway. Used to test flexibility for custom enzyme module implementation. |
| Pilot Rat PK Dataset (IV & PO) | Used for initial "base model" validation within each software. Tests user-friendliness of data import and fitting procedures. |
| Software Trial Licenses | Essential for hands-on testing of shortlisted platforms (GastroPlus, Simcyp, PK-Sim). |
| Standard Operating Procedure (SOP) for PBPK Modeling | Internal document ensuring consistent modeling practices (e.g., sensitivity analysis criteria, validation steps) across tested platforms. |
Methodology:
- Define Core Requirements: List non-negotiable features (e.g., ability to simulate target patient population, FDA acceptance track record) and desirable flexibility features (e.g., custom compartment addition, user-defined rate equations).
- Develop a "Benchmark" Model: Code a minimal, verified PBPK model for a well-known drug (e.g., midazolam) in the most flexible tool available (e.g., MATLAB). This establishes a "gold standard" for output comparison.
- Conduct Structured Software Trials:
- Phase 1 - Base Model Build: Using the toolkit data (Table 2), replicate the systemic PK of drug X in a healthy volunteer population in each shortlisted software. Document the time, number of steps, and required training to achieve this.
- Phase 2 - Flexibility Challenge: Attempt to implement the novel intracellular activation pathway. Document the method required: a) selection from a pre-built library, b) modification of a pre-built module, or c) creation of a de novo module/script.
- Phase 3 - Output and Validation: Execute a standard simulation (e.g., DDI with a common CYP inhibitor). Export results and compare key AUC and Cmax ratios against the "benchmark" model and literature values.
- Scoring and Selection: Use a weighted scoring matrix incorporating ease-of-use metrics (time to first successful simulation), flexibility metrics (success of custom pathway implementation), and output accuracy.
Diagram 1: PBPK Software Evaluation Workflow
Protocol: Implementing a Custom Hepatic Uptake Model in a PBPK Platform
Protocol Title: Incorporation of Saturable Hepatic OATP-Mediated Uptake for a Novel Hepatitis B Virus (HBV) Drug
Objective: To provide a step-by-step methodology for extending a PBPK model within a flexible software environment (using PK-Sim/MoBi as an example) to include a saturable hepatic uptake process not available in the standard library.
Background: Drug Y is a new anti-HBV agent, a substrate for OATP1B1/1B3. In vitro data shows clear saturation of uptake. Accurate prediction of liver concentration and potential DDIs requires moving beyond passive diffusion and linear uptake assumptions.
Experimental Workflow:
Base Model Construction in PK-Sim:
- Create a new compound "Drug Y". Enter basic physicochemical parameters (MW, LogP, pKa, fu).
- Select "PK-Sim Standard PBPK Model". Define administration (e.g., oral tablet).
- Under "Processes", assign standard systemic clearance (e.g., CYP3A4 metabolism) using in vitro CLint data.
- Run initial simulation and compare to observed plasma PK. Note under-prediction of early exposure due to missing active uptake.
Custom Process Creation in MoBi:
- Export the PK-Sim model to MoBi.
- Navigate to the "Liver" organ and its "Pericentral" cell compartment.
- Add a new transporter protein entity: Define "OATP1B" with a concentration parameter.
- Create a new reaction:
- Name: "SaturableOATPUptake"
- Formula:
(Vmax * C_plasma_unbound) / (Km + C_plasma_unbound) - Where
VmaxandKmare parameters from in vitro uptake studies, andC_plasma_unboundis the unbound concentration in liver capillary blood.
- Add the reaction to the liver cell: Specify the reaction increases the intracellular concentration of "Drug Y".
Parameterization and Simulation:
- Input the experimentally derived
Vmax(pmol/min/mg protein) andKm(µM) values. Scale to in vivo using standard scaling factors (hepatic protein mass). - Run the simulation in MoBi or re-import the extended model into PK-Sim for execution.
- Input the experimentally derived
Sensitivity and DDI Analysis:
- Perform a local sensitivity analysis on the
VmaxandKmparameters. - Simulate a DDI with an OATP inhibitor (e.g., rifampin) by competitively inhibiting the custom uptake process (reduce
Vmaxor increase apparentKm).
- Perform a local sensitivity analysis on the
Diagram 2: Custom Hepatic Uptake Model Extension
The strategic selection of PBPK software is a critical determinant of success in anti-infective drug candidate selection. A platform that offers an intuitive, guided interface for common tasks (e.g., population DDI simulation) dramatically accelerates early screening. However, the mechanistic nature of PBPK and the unique targets and pathways of anti-infectives often demand model flexibility. Establishing an internal protocol for software evaluation, as outlined herein, ensures a balanced choice. The ideal solution may involve a primary user-friendly platform for most projects, coupled with access to a more flexible tool or scripting environment for novel mechanistic challenges, ensuring both efficiency and scientific rigor in PBPK-informed drug development.
Validating PBPK Models and Conducting Comparative Simulations for Lead Prioritization
Within the framework of a thesis on PBPK modeling for anti-infective drug candidate selection, validation is the critical bridge between model development and its application in decision-making. A robust PBPK model must undergo a multi-tiered validation strategy to ensure its predictive reliability for pharmacokinetic (PK) and pharmacodynamic (PD) outcomes in target populations. This document outlines detailed application notes and protocols for internal, external, and prospective validation, integrating preclinical and clinical data.
Internal Validation
Internal validation assesses the model's self-consistency and its ability to describe the data used for its development (training data).
Application Notes
Internal validation ensures the model structure and parameters are logically consistent and that the model can adequately fit the training dataset. Techniques include goodness-of-fit plots, visual predictive checks (VPC), and bootstrapping. For anti-infective PBPK models, this often involves validating against rich PK data from preclinical species (mouse, rat, dog) used for parameter estimation.
Protocol: Non-Parametric Bootstrap for Parameter Confidence Intervals
Objective: To estimate the uncertainty and robustness of model parameters (e.g., clearance, volume of distribution) derived from preclinical PK data.
Materials & Software: PBPK platform (e.g., GastroPlus, Simcyp, PK-Sim), scripting interface, preclinical PK dataset (plasma concentrations vs. time).
Procedure:
- Dataset Preparation: Compile N observed PK profiles from a preclinical study (e.g., N=8 rats following IV administration).
- Bootstrap Sample Generation: Using a random number generator, create M (e.g., M=1000) bootstrap samples. Each sample is created by randomly selecting N profiles from the original dataset with replacement.
- Parameter Re-estimation: For each of the M bootstrap samples, re-run the parameter estimation algorithm to obtain a new set of model parameters.
- Analysis: Compile the M sets of parameters. Calculate the 2.5th, 50th (median), and 97.5th percentiles for each parameter to define the 95% confidence interval.
- Diagnostic: Assess the symmetry and width of the confidence intervals. Narrow, symmetric intervals indicate precise and identifiable parameters.
Data Presentation: Internal Validation of Drug X in Rat
Table 1: Parameter estimates from bootstrapping of a rat PBPK model for Drug X (N=8, M=1000).
| Parameter | Original Estimate | Bootstrap Median | 95% CI (2.5% - 97.5%) |
|---|---|---|---|
| CL (L/h/kg) | 0.85 | 0.86 | [0.72, 1.01] |
| Vc (L/kg) | 0.25 | 0.24 | [0.20, 0.29] |
| Kp (Tissue:Plasma) | 1.50 | 1.48 | [1.20, 1.85] |
External Validation
External validation evaluates the model's predictive power using data not used in model development (test data).
Application Notes
This is the most stringent test before prospective use. For anti-infective PBPK, a model built on preclinical data (e.g., rat and dog PK, in vitro metabolism) is used to predict human PK. Validation is achieved by comparing these predictions to observed early clinical data (e.g., Phase I single ascending dose study). Success here supports the model's translational utility.
Protocol: Prediction-Corrected Visual Predictive Check (pcVPC)
Objective: To graphically compare model predictions with external observed data, accounting for differences in dosing regimens and study designs.
Materials & Software: PBPK platform, observed clinical PK data (Phase I), simulation engine.
Procedure:
- Simulation: Using the finalized PBPK model (with parameters fixed from preclinical data), simulate the exact clinical trial design (doses, demographics, sampling times) for a virtual population (e.g., n=1000 subjects).
- Prediction Correction: Normalize the observed and simulated concentrations based on the typical population prediction for each observation's dose and time bin to remove the influence of design variability.
- Percentile Calculation: From the simulated data, calculate the 5th, 50th, and 95th prediction intervals for the prediction-corrected concentrations in each time bin.
- Plotting: Generate a pcVPC plot. Overlay the observed clinical data (as points) on the shaded prediction intervals. A successful validation is indicated when ~90% of observed points fall within the 5th-95th prediction interval band.
Data Presentation: External Validation of Drug X in Humans
Table 2: Comparison of predicted vs. observed human PK parameters for Drug X (50 mg oral dose).
| PK Parameter | PBPK Prediction (Mean ± SD) | Observed Clinical (Mean ± SD) | Prediction Error (%) |
|---|---|---|---|
| Cmax (µg/mL) | 1.21 ± 0.30 | 1.15 ± 0.28 | +5.2% |
| AUC0-∞ (h·µg/mL) | 12.5 ± 3.1 | 13.2 ± 3.5 | -5.3% |
| t1/2 (h) | 6.8 ± 1.5 | 7.2 ± 1.8 | -5.6% |
Prospective Validation
Prospective validation tests the model's ability to predict the outcome of a future clinical study or scenario not yet conducted.
Application Notes
This represents the highest level of model credibility. In anti-infective candidate selection, a prospectively validated PBPK/PD model can be used to select the optimal dose for a Phase II trial in a specific patient population (e.g., critically ill patients with renal impairment) or to predict the likelihood of achieving a target PD index (e.g., fAUC/MIC).
Protocol: Using a Validated PBPK/PD Model to Design a Phase II Dose
Objective: To simulate a planned clinical trial to identify the dose with the highest probability of target attainment (PTA) for a defined PD endpoint.
Materials & Software: Validated PBPK model integrated with a PD model (e.g., Emax model for bacterial kill), epidemiological data on pathogen MIC distribution.
Procedure:
- Define PD Target: Establish the PK/PD index target (e.g., fAUC/MIC > 100 for efficacy).
- Define Virtual Population: Simulate the target patient population (e.g., 5000 virtual patients with demographics and pathophysiological changes representative of the infected population).
- Dose Simulation: Simulate a range of candidate doses (e.g., 200 mg, 500 mg, 1000 mg q12h) in the virtual population.
- PTA Calculation: For each dose and across a relevant MIC range (e.g., 0.06 to 16 mg/L), calculate the percentage of virtual patients achieving the PD target.
- Dose Selection: Select the dose that provides ≥90% PTA at the clinical breakpoint MIC (e.g., 4 mg/L). This dose is then recommended for the prospective trial.
Data Presentation: Prospective PTA Analysis for Drug X
Table 3: Probability of Target Attainment (fAUC/MIC > 100) for Drug X across doses and MICs.
| MIC (mg/L) | PTA (%) - 200 mg | PTA (%) - 500 mg | PTA (%) - 1000 mg |
|---|---|---|---|
| 0.5 | 99.9 | 100 | 100 |
| 1 | 98.5 | 99.9 | 100 |
| 2 | 75.2 | 98.0 | 99.8 |
| 4 | 35.5 | 85.7 | 98.9 |
| 8 | 5.1 | 45.2 | 85.0 |
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions & Essential Materials for PBPK Model Validation.
| Item | Function in Validation |
|---|---|
| PBPK Software Platform (e.g., Simcyp, GastroPlus) | Core engine for model building, simulation, and running validation protocols like VPC and PTA. |
| Clinical PK Dataset (Phase I) | Gold-standard dataset for external validation; used as the comparator for model predictions. |
| Preclinical PK Datasets (Rodent/Non-rodent) | Used for model development, parameter estimation, and internal validation (bootstrapping). |
| In Vitro ADME Assay Data (e.g., microsomal clearance, plasma protein binding) | Provides essential system-independent input parameters for the PBPK model. |
| Virtual Population Generator | Creates physiologically realistic virtual subjects or patients for trial simulations in external/prospective validation. |
| Statistical Software (e.g., R, Phoenix WinNonlin) | Used for data analysis, generation of diagnostic plots, and calculation of confidence intervals/prediction intervals. |
| Pathogen MIC Distribution Data | Epidemiological data critical for linking PK predictions to PD outcomes (PTA) in anti-infective prospective validation. |
Visualizations
Title: Internal Validation Workflow for PBPK Models
Title: External Validation Decision Pathway
Title: Prospective PBPK/PD Dose Selection Workflow
1. Introduction and Thesis Context Within the broader thesis on leveraging Physiologically-Based Pharmacokinetic (PBPK) modeling for rational anti-infective drug candidate selection, defining quantitative success criteria is paramount. This document establishes formal acceptance ranges for key pharmacokinetic (PK) metrics—Area Under the Curve (AUC), maximum concentration (Cmax), and tissue concentration predictions—used to validate PBPK models prior to their application in candidate prioritization and dose projection. These criteria ensure model predictive performance is scientifically credible and fit-for-purpose in a high-stakes research environment.
2. Current Industry and Regulatory Standards for PBPK Model Acceptance A live search of recent literature (2022-2024) and regulatory assessment reports indicates a convergence on criteria based on the prediction error of simulated versus observed PK parameters.
Table 1: Summary of Proposed Acceptance Ranges for PBPK Model Validation
| PK Metric | Acceptance Range (Predicted/Observed) | Basis & Rationale |
|---|---|---|
| AUC (AUC₀–t, AUC₀–∞) | 0.80 – 1.25 (± 20% error) | Aligns with bioequivalence standards; critical for efficacy (AUC/MIC). |
| Cmax | 0.75 – 1.33 (± 33% error) | Wider range than AUC due to higher sensitivity to absorption/vascular dynamics; ensures safety margins. |
| Tissue:Plasma Ratio | 0.5 – 2.0 (± 100% error) | Reflects greater uncertainty in tissue composition, partitioning, and measurement; qualitative trend confirmation is often complementary. |
Note: For anti-infectives, successful prediction of free drug concentrations in target tissue (e.g., epithelial lining fluid, alveolar macrophages) relative to the pathogen's Minimum Inhibitory Concentration (MIC) is the ultimate goal, even if absolute tissue concentration accuracy falls within the wider range above.
3. Detailed Protocol: Establishing Model Acceptance for an Anti-Infective Candidate
Protocol Title: In Vitro-to-In Vivo PBPK Model Validation and Acceptance Testing for a Novel Anti-Bacterial Compound
Objective: To develop, calibrate, and validate a whole-body PBPK model using preclinical data, and to apply defined success criteria for AUC, Cmax, and tissue concentration predictions.
3.1. Key Research Reagent Solutions & Materials Table 2: Scientist's Toolkit for PBPK Model Development
| Item/Category | Example/Supplier | Function in Protocol |
|---|---|---|
| PBPK Software Platform | GastroPlus, Simcyp Simulator, PK-Sim | Provides mechanistic framework for model construction, simulation, and virtual population generation. |
| In Vitro ADME Assay Kit | Solubility/Dissolution (pION), Metabolic Stability (Corning Gentest), Permeability (Caco-2) | Generates essential input parameters for model parameterization (e.g., CLint, Peff). |
| Physicochemical Analyzer | HPLC-MS/MS System | Quantifies drug concentrations in biological matrices (plasma, tissue homogenates) for PK studies. |
| Biomatrix Collection | Mouse/Rat Plasma & Tissue Homogenates (BioIVT) | Provides observed PK data for model calibration (plasma) and key validation (tissue). |
| Tissue Partitioning Tool | Rodgers & Rowland, Poulin & Theil methods | Algorithms within software to predict tissue:plasma partition coefficients (Kp) from drug properties. |
| Virtual Population | Simcyp Rat, PK-Sim Population Library | Generates demographically diverse virtual subjects for simulating population variability and comparing to observed data. |
3.2. Experimental Workflow and Methodology
Phase 1: In Vitro Data Generation and Model Parameterization
- Determine key physicochemical properties (pKa, LogP, BPP).
- Measure in vitro metabolic stability in human/microsomal hepatocytes to estimate intrinsic clearance (CLint).
- Assess permeability using Caco-2 or MDCK cells.
- Measure plasma protein binding (fu) via equilibrium dialysis.
- Input these parameters into the PBPK platform. Use built-in algorithms to estimate tissue partitioning and base model structure.
Phase 2: Model Calibration with Preclinical In Vivo PK Data
- Conduct single IV and oral PK studies in rodent species (e.g., Sprague-Dawley rats, n=6).
- Collect serial plasma samples up to 24 hours post-dose. Analyze using LC-MS/MS.
- Import observed mean plasma concentration-time profiles into the PBPK software.
- Calibrate the model by minimally adjusting only poorly characterized parameters (e.g., enterocyte permeability scaling factor) within biologically plausible bounds to achieve visual fit to the observed plasma data.
Phase 3: Model Validation and Application of Success Criteria
- Predictive Validation: Simulate a separate, independent preclinical PK study (e.g., different dose, fed state) without further parameter adjustment.
- Output Simulation Results: Extract the predicted mean AUC and Cmax from the virtual population.
- Calculate Prediction Error: For AUC and Cmax, compute the geometric mean ratio (GMR) of predicted/observed values.
- Apply Acceptance Criteria:
- If AUC and Cmax GMRs fall within the ranges specified in Table 1 (0.80-1.25 and 0.75-1.33, respectively), the model is considered validated for systemic PK.
- Tissue Concentration Validation:
- Conduct a tissue distribution study in rats. Collect key target tissues (e.g., lung, kidney, liver) at multiple time points.
- Compare simulated tissue concentration-time profiles and steady-state tissue:plasma ratios to observed data.
- Apply Acceptance Criteria: If the GMR for tissue concentration AUC or the predicted/observed tissue:plasma ratio falls within 0.5-2.0, the tissue model is acceptable. Confirm the model correctly predicts whether tissue concentrations exceed the MIC for the target pathogen.
PBPK Model Development & Validation Workflow
4. Conclusion Integrating these explicit, quantitative acceptance criteria into the PBPK modeling workflow provides a rigorous, standardized framework for the thesis research. Successfully validated models, meeting the defined ranges for AUC, Cmax, and tissue concentration predictions, can be deployed with high confidence to simulate human PK, optimize dosing regimens, and rationally select anti-infective drug candidates with the highest probability of clinical success.
Thesis Context
This work is presented as a core chapter in a broader thesis investigating the systematic application of Physiologically-Based Pharmacokinetic (PBPK) modeling as a decision-making tool in the preclinical pipeline for anti-infective therapeutics. The thesis posits that early integration of PBPK can de-risk candidate selection, optimize experimental design, and accelerate the development of treatments for resistant infections.
Selecting the optimal lead candidate from a pool of novel compounds targeting a specific infection is a critical, resource-intensive challenge. This case study demonstrates a PBPK-driven framework for the comparative evaluation of three hypothetical antifungal drug candidates (CandA, CandB, CandC) targeting a deep-seated Candida albicans infection. By simulating drug disposition at the site of infection (e.g., renal medulla), PBPK modeling provides a quantitative basis for predicting efficacy and informing go/no-go decisions prior to costly late-stage preclinical studies.
PBPK Model Development & Parameterization
A whole-body PBPK model was developed for each candidate using a middle-out approach, integrating in vitro data and in silico predictions.
Table 1: Compound-Specific Input Parameters for PBPK Models
| Parameter | CandA | CandB | CandC | Source/Protocol |
|---|---|---|---|---|
| MW (g/mol) | 350.2 | 402.5 | 389.4 | HRMS Analysis |
| logP | 2.1 | 1.5 | 3.8 | In vitro shake-flask method |
| pKa (acid/base) | Base (8.9) | Neutral | Acid (4.2) | Potentiometric titration |
| fu (Fraction Unbound) | 0.25 | 0.70 | 0.05 | Equilibrium dialysis vs. human plasma |
| Blood-to-Plasma Ratio | 0.9 | 1.1 | 0.6 | In vitro blood incubation & centrifugation |
| CLint (µL/min/mg protein) | 18.5 | 5.2 | 45.0 | Human liver microsome incubation |
| Papp (x10-6 cm/s) | 22 | 15 | 8 | Caco-2 monolayer assay |
| P-gp Substrate (B→A/A→B ratio) | 1.5 (No) | 5.2 (Yes) | 1.2 (No) | MDR1-MDCKII cell assay |
Protocol 2.1: Determination of Metabolic Clearance (CLint)
Objective: To obtain intrinsic clearance data for PBPK model input. Materials: Human liver microsomes (HLM, 0.5 mg/mL), NADPH regenerating system, substrate (1 µM candidate in DMSO <0.1%), LC-MS/MS. Procedure:
- Incubate candidate with HLM and NADPH in potassium phosphate buffer (37°C).
- At times 0, 5, 10, 20, and 30 minutes, aliquot 50 µL into 150 µL of cold acetonitrile to stop reaction.
- Centrifuge, analyze supernatant via LC-MS/MS to determine parent compound depletion.
- Fit logarithmic depletion curve to calculate in vitro half-life and CLint.
- Scale to hepatic CL using the well-stirred model.
Infection Site Model & Target Engagement
A critical module simulating the renal medulla—a known site for C. albicans dissemination—was incorporated. The model accounts for infection-induced pathophysiological changes: increased capillary permeability, decreased renal filtration, and presence of fungal burden.
Table 2: Simulated PK/PD Target Attainment at Renal Medulla (Criterion: fAUC0-24/MIC > 25 for static effect)
| Candidate | Dose (mg, IV) | Cmax,site (mg/L) | fAUC0-24,site (mg·h/L) | MIC (mg/L) | fAUC/MIC | Probability of Target Attainment (PTA) |
|---|---|---|---|---|---|---|
| CandA | 200 | 4.8 | 55 | 1.0 | 55 | 92% |
| CandB | 200 | 3.1 | 42 | 2.0 | 21 | 45% |
| CandC | 200 | 8.5* | 120* | 0.5 | 240 | 100% |
*High total but low free concentration due to high protein binding.
Title: PBPK Candidate Selection Workflow
Virtual Population Simulation & Comparative Output
A virtual population (n=500) of critically ill patients was simulated to assess inter-individual variability and PTA.
Table 3: Comparative Summary of Key PBPK Simulation Outputs
| Metric | CandA | CandB | CandC | Clinical Implication |
|---|---|---|---|---|
| Plasma CL (L/h) | 8.5 ± 2.1 | 5.0 ± 1.5 | 12.0 ± 3.8 | CandC has high clearance |
| Vss (L) | 25 ± 5 | 15 ± 3 | 8 ± 2 | CandA has extensive tissue distribution |
| t½ (h) | 3.4 | 3.5 | 0.7 | CandC has short half-life |
| Renal Medulla fAUC/MIC (Median) | 55 | 21 | 240 | CandC exceeds target robustly |
| PTA > Target (%) | 92 | 45 | 100 | CandC highest probability of efficacy |
| CYP3A4 DDI Risk (AUC ratio) | 2.5 | 1.1 | 5.8 | CandC has high DDI risk |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for PBPK Model Parameterization
| Item | Function in PBPK Workflow | Example Vendor/Product |
|---|---|---|
| Pooled Human Liver Microsomes | Determine intrinsic metabolic clearance (CLint). | Corning Gentest, BioIVT |
| Human Hepatocytes (Cryopreserved) | Assess phase I/II metabolism & transporter activity. | Lonza, BioIVT |
| Caco-2 Cell Line | Measure intestinal permeability (Papp). | ATCC, Sigma-Aldrich |
| MDR1-MDCKII Cells | Identify P-glycoprotein substrate potential. | Netherlands Cancer Institute |
| Human Plasma (for fu) | Determine plasma protein binding via equilibrium dialysis. | BioIVT, commercial blood banks |
| Simcyp Simulator or GastroPlus | Industry-standard platforms for PBPK modeling & simulation. | Certara, Simulations Plus |
| ADMET Predictor Software | In silico prediction of key physicochemical/ADME properties. | Simulations Plus |
This case study validates the thesis that PBPK modeling is a powerful comparative tool for anti-infective candidate selection. While CandC demonstrated superior target attainment, the model also revealed its high DDI risk—a critical differentiator. The integrated protocol enables researchers to efficiently prioritize compounds with the highest likelihood of clinical success, directly supporting the thesis argument for model-informed drug discovery in infectious diseases.
1. Introduction & Context Within the broader thesis on PBPK modeling for anti-infective drug candidate selection, establishing the superiority of the developed PBPK model is critical. This application note details the protocols for benchmarking a PBPK model against two standard methods: allometric scaling for first-in-human (FIH) dose prediction and traditional compartmental pharmacokinetic (PK) analysis for efficacy/safety index prediction. The goal is to demonstrate the enhanced predictive accuracy and mechanistic insight offered by PBPK in the context of anti-infective development.
2. Quantitative Comparison of Predictive Performance
Table 1: Benchmarking Outcomes for a Novel Anti-infective (Example: Candidate X)
| Benchmarking Metric | Allometric Scaling (2-species) | 2-Compartment PK Model | Whole-Body PBPK Model | Clinical Outcome (Actual) |
|---|---|---|---|---|
| Predicted Human CL (L/h) | 8.5 | N/A (Fitted to human data) | 7.2 | 6.9 |
| Predicted Human Vss (L) | 125 | N/A (Fitted to human data) | 98 | 105 |
| FIH Dose for Target AUC (mg) | 750 | 600 (from extrapolated PK) | 550 | 580 (administered) |
| Predicted AUC/MIC in Lung Tissue | Not Addressable | 55 (from plasma PK, assumed ratio) | 125 (mechanistic tissue model) | ~120 (estimated from biomarker) |
| Predicted DDI Magnitude (with CYP3A4 inhibitor) | Not Predictable | ~2.0-fold AUC increase | 3.5-fold AUC increase | 3.2-fold AUC increase |
3. Experimental Protocols
Protocol 1: Benchmarking FIH Dose Prediction vs. Allometric Scaling
- Objective: To compare the accuracy of PBPK-predicted human PK and FIH dose against simple allometric scaling.
- Materials: See "Scientist's Toolkit" (Section 5).
- Methods:
- Allometric Scaling: Plot IV clearance (CL) and volume of distribution at steady state (Vss) from in vivo PK studies in rat and dog (log scale) against body weight (log scale). Extrapolate to 70 kg human using fixed exponents (CL: 0.75, Vss: 1.0) and species-invariant protein binding correction.
- PBPK Prediction: Populate the PBPK software with:
- In vitro inputs: Metabolic stability (human liver microsomes), permeability (Caco-2), plasma protein binding.
- Physicochemical properties: logP, pKa.
- System parameters: Use built-in human physiology.
- Simulation: Perform a simulated IV bolus administration in the PBPK model.
- Comparison: Calculate the predicted human CL and Vss from both methods. Determine the FIH dose required to achieve a target AUC (derived from animal efficacy models) using both sets of parameters. Compare predictions against actual early clinical data (if available).
Protocol 2: Benchmarking Tissue Exposure & Efficacy Prediction vs. Compartmental PK
- Objective: To demonstrate the advantage of PBPK in predicting site-of-action (e.g., lung) exposure over plasma-centric compartmental models.
- Materials: See "Scientist's Toolkit" (Section 5).
- Methods:
- Compartmental PK Analysis: Fit Phase I plasma concentration-time data for the candidate drug to a 2- or 3-compartment model using nonlinear mixed-effects modeling (e.g., NONMEM).
- Derive Efficacy Index: Use the fitted model to simulate plasma AUC. Estimate lung exposure by applying a literature-based lung:plasma partition coefficient (Kp).
- PBPK Simulation: Using the previously verified PBPK model, simulate the same dosing regimen as in Phase I. Extract the predicted concentration-time profile directly from the lung tissue compartment.
- Comparison: Calculate the AUC/MIC (Minimum Inhibitory Concentration) ratio for a target pathogen in both plasma (compartmental) and lung tissue (PBPK and estimated from compartmental). Compare against preclinical efficacy thresholds or clinical response biomarkers.
4. Visualizations
5. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PBPK Benchmarking Studies
| Item / Reagent | Function in Benchmarking Protocol |
|---|---|
| Human Liver Microsomes (HLM) | To determine in vitro intrinsic metabolic clearance (CLint) for PBPK model input. |
| Caco-2 Cell Line | To assay apparent permeability (Papp), informing intestinal absorption and distribution in PBPK. |
| Equilibrium Dialysis Apparatus | To measure in vitro plasma protein binding (fu) for correction in allometry and PBPK. |
| PBPK Software (e.g., GastroPlus, Simcyp, PK-Sim) | Platform to build, simulate, and validate the mechanistic PBPK model. |
| NONMEM / Monolix | Industry-standard software for nonlinear mixed-effects modeling to develop compartmental PK models. |
| Species-Specific Plasma | For determining protein binding across species (rat, dog, human) for allometric correction. |
| Validated LC-MS/MS System | For quantitative bioanalysis of drug concentrations in plasma and tissue homogenates from preclinical studies. |
Within the broader thesis on PBPK modeling for anti-infective drug candidate selection, the integration of physiologically based pharmacokinetic (PBPK) predictions with efficacy and toxicity data represents a critical methodology for de-risking development. This approach moves beyond simple exposure metrics, enabling a quantitative framework to inform pivotal Go/No-Go decisions by predicting the therapeutic index (TI) in target populations, including special groups like pediatrics or patients with organ impairment.
Core Integration Framework and Data Synthesis
The integration framework synthesizes three core data streams: PBPK-predicted exposure, in vitro/in vivo efficacy, and in vitro/in vivo toxicity. The primary output is a predicted clinical safety margin.
Table 1: Key Data Inputs for Integrated Go/No-Go Analysis
| Data Stream | Source/Experiment | Key Output Metrics | Use in Integration |
|---|---|---|---|
| PBPK-Predicted Exposure | Developed & verified PBPK model simulating Phase I/II doses in virtual populations. | AUC, C~max~, C~trough~ at site of action (e.g., lung epithelial lining fluid). | Provides the range of predicted drug concentrations (PK) in humans. |
| Efficacy | In vitro time-kill assays against target pathogens (e.g., S. aureus, P. aeruginosa). | Static concentration, fAUC/MIC, %T>MIC. | Defines PK/PD index and target magnitude for stasis/1-log kill/etc. |
| Toxicity | In vitro cytotoxicity assays (e.g., HepG2, cardiomyocytes); in vivo animal toxicology studies. | IC~50~ (cell viability), NOAEL (No Observed Adverse Effect Level). | Defines concentration or exposure thresholds for adverse effects. |
Table 2: Example Quantitative Output for a Notational Anti-Pseudomonal Agent
| Parameter | Value | Source & Notes |
|---|---|---|
| PBPK Prediction (Simulated 500 mg IV q8h) | Virtual Population (n=1000) with COPD | |
| Median Plasma AUC~0-24~ (mg·h/L) | 480 (90% CI: 385-605) | PBPK Model Output |
| Median Lung Epithelial Lining Fluid C~max~ (mg/L) | 35.2 (90% CI: 24.8-48.1) | PBPK Model with Tissue Distribution |
| Efficacy (PK/PD Target) | In Vitro Time-Kill vs. P. aeruginosa | |
| fAUC/MIC for 1-log kill | 125 | Derived from hollow-fiber infection model |
| Toxicity Threshold | In Vitro Cardiotoxicity Assay (hERG) | |
| Plasma C~max~ associated with 10% QTc prolongation | 58 mg/L | In vitro IC~50~ scaled with safety factor |
| Calculated Safety Margin | Integration | |
| Probability of Target Attainment (PTA) at MIC=2 mg/L | 92% | PBPK + PK/PD Target |
| Predicted Clinical Safety Margin (C~max~ Tox / C~max~ Pred) | 1.65 | 58 mg/L / 35.2 mg/L |
Detailed Experimental Protocols
Protocol 3.1:In VitroTime-Kill Assay for PK/PD Index Identification
Objective: To determine the pharmacokinetic/pharmacodynamic (PK/PD) index (AUC/MIC, C~max~/MIC, %T>MIC) and magnitude most predictive of efficacy for a novel anti-infective.
Materials:
- Test compound stock solution.
- Cation-adjusted Mueller Hinton Broth (CAMHB).
- Target bacterial strain(s) (e.g., ATCC reference strains).
- Sterile 96-well deep-well plates or flasks.
- Automated liquid handler, incubator, plate reader/viable count plates.
Procedure:
- Prepare logarithmic-phase bacterial inoculum at ~1 x 10^6 CFU/mL in CAMHB.
- Using a liquid handler, serially dilute the test compound across a range of concentrations (e.g., 0.25x to 32x MIC) in multiple vessels.
- Add the standardized inoculum to each vessel. Maintain growth and vehicle controls.
- Incubate at 37°C. Sample aliquots from each vessel at pre-defined timepoints (e.g., 0, 1, 2, 4, 8, 24h).
- Perform serial dilution and viable counts on agar plates to quantify bacterial density (CFU/mL).
- Plot time-kill curves. Use mathematical modeling (e.g., Emax model) to relate static, 1-log kill, and 2-log kill endpoints to different PK/PD indices (AUC, C~max~, Time above MIC).
Protocol 3.2: PBPK Model Verification and Clinical Dose Simulation
Objective: To verify a developed PBPK model against available human PK data and simulate exposure in target and special populations.
Materials:
- PBPK software platform (e.g., GastroPlus, Simcyp, PK-Sim).
- Compound-specific parameters (logP, pKa, blood-to-plasma ratio, in vitro clearance data).
- Human in vivo PK data from Phase I (plasma concentration-time profiles).
- Virtual population demographics (age, weight, genotype prevalence, disease status).
Procedure:
- Model Construction: Input compound ADME properties into the software's system model. Incorporate mechanisms of absorption, distribution (tissue partition coefficients), metabolism (enzyme Km/Vmax), and excretion.
- Verification: Simulate the Phase I clinical trial design (dose, regimen, subject demographics). Overlay simulated concentration-time profiles with observed Phase I data. Use statistical criteria (e.g., predicted/observed ratios for AUC, C~max~, visual predictive checks) to assess model adequacy.
- Clinical Simulation: Apply the verified model to simulate the proposed Phase II/III dosing regimen in a large virtual population (n=1000) representing the target patient group (e.g., patients with pneumonia, renal impairment). Output key exposure metrics (AUC, C~max~) and their variability.
Visualization of the Integrated Decision Framework
Title: Integrated PBPK Efficacy Toxicity Decision Framework
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Integrated PBPK/PD/Tox Experiments
| Item / Reagent Solution | Function in Context | Example Vendor/Catalog |
|---|---|---|
| PBPK Simulation Software | Platform for building, verifying, and simulating drug disposition in virtual human populations. Critical for predicting human exposure. | Certara (Simcyp), Simulations Plus (GastroPlus), Open Systems Pharmacology (PK-Sim) |
| Hollow-Fiber Infection Model (HFIM) System | Advanced in vitro system that simulates human PK profiles to identify PK/PD targets and suppress resistance. | FiberCell Systems, Inc. |
| hERG Inhibition Assay Kit | In vitro screening for compound interaction with the hERG potassium channel, a key predictor of cardiotoxicity (QTc prolongation). | Eurofins Discovery (ChanTest), Charles River |
| Cryopreserved Human Hepatocytes | Primary cells used to measure in vitro intrinsic clearance and metabolite identification for PBPK model parameterization. | Thermo Fisher (Gibco), BioIVT, Lonza |
| Phospholipidosis & Cytotoxicity Assay Kits | High-content screening assays to assess cellular toxicity mechanisms relevant to long-term dosing of anti-infectives. | Thermo Fisher (Cellomics), Enzo Life Sciences |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility and time-kill assays, ensuring reproducible MIC and PK/PD results. | Hardy Diagnostics, BD Diagnostics |
| Biomimetic Chromatography Columns (IAM, HSA) | Tools for rapid estimation of tissue partition coefficients and plasma protein binding, key inputs for PBPK distribution models. | Regis Technologies (IAM), ChromTech (HSA) |
Conclusion
PBPK modeling has evolved from a research tool into a cornerstone of modern, model-informed drug development for anti-infectives. By integrating mechanistic understanding of drug disposition with pathogen-specific PK/PD targets, it provides a powerful framework for candidate selection, dose rationale, and trial design. Success hinges on robust foundational knowledge, a systematic methodological approach, proactive troubleshooting, and rigorous validation. The future lies in further integration with quantitative systems pharmacology (QSP) to model host-pathogen-drug interactions dynamically, and in expanding virtual twin populations to ensure equity in dosing across diverse patient groups. For research teams, adopting and refining PBPK strategies is no longer optional but essential to de-risk pipelines, conserve resources, and accelerate the delivery of novel anti-infective therapies to patients in need.